Validating AI in Drug Discovery: A Framework for Robustness, Regulatory Compliance, and Clinical Success in 2025
This article provides a comprehensive guide for researchers and drug development professionals on validating artificial intelligence (AI) models in drug discovery.
Validating AI in Drug Discovery: A Framework for Robustness, Regulatory Compliance, and Clinical Success in 2025
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on validating artificial intelligence (AI) models in drug discovery. It covers the foundational principles of AI model validation, explores methodological approaches and real-world applications from leading companies, addresses key challenges and optimization strategies, and establishes a framework for rigorous performance and comparative analysis. With the FDA expected to release new guidance and the first AI-discovered drugs advancing in clinical trials, this resource synthesizes current best practices to ensure AI tools are trustworthy, ethical, and effective in accelerating the delivery of new therapies.
The Pillars of Trust: Foundational Principles for Validating AI in Drug Discovery
The integration of artificial intelligence (AI) into drug discovery represents a paradigm shift, moving the industry from labor-intensive, human-driven workflows toward AI-powered engines capable of dramatically compressing development timelines [1]. However, this acceleration demands a rigorous and evolving framework for validation. In the context of AI-based drug discovery, validation extends beyond simple model accuracy; it is a multi-tiered process that ensures AI-generated insights are biologically relevant, clinically translatable, and ultimately, able to yield safe and effective medicines. The fundamental question facing the industry is whether AI is producing genuinely better drugs or merely facilitating faster failures [1]. Answering this requires a critical analysis of performance metrics, experimental protocols, and the entire pathway from algorithmic prediction to approved therapeutic.
A core challenge is that traditional machine learning metrics often fall short in the biological context. Standard measures like accuracy can be misleading when dealing with highly imbalanced datasets, such as those containing far more inactive compounds than active ones [2]. Consequently, a new set of domain-specific validation metrics has emerged, prioritizing biological relevance and the ability to detect rare but critical events over raw computational performance [2]. This guide provides a structured comparison of validation approaches, detailing the key performance indicators, experimental methodologies, and essential tools required to robustly evaluate AI-driven drug discovery platforms.
Comparative Performance of AI Drug Discovery Platforms
A critical component of validation is benchmarking the performance and output of leading AI drug discovery companies. The table below synthesizes the clinical progress and key performance claims of major players in the field, offering a comparative view of their real-world impact.
Table 1: Clinical-Stage AI Drug Discovery Companies and Key Performance Metrics (as of 2025)
| Company | AI Platform & Specialization | Key Clinical Candidates & Indications | Reported Performance & Validation Metrics |
|---|---|---|---|
| Exscientia [1] [3] | End-to-end platform; generative AI for small-molecule design; "Centaur Chemist" approach. | DSP-1181 (OCD, Phase I), EXS-21546 (Immuno-oncology, halted), GTAEXS-617 (CDK7 inhibitor for solid tumors, Phase I/II) [1]. | Achieved clinical candidate with only 136 synthesized compounds (vs. industry standard of thousands); design cycles ~70% faster and requiring 10x fewer compounds than industry norms [1]. |
| Insilico Medicine [4] [1] [5] | End-to-end Pharma.AI platform; generative biology and chemistry for aging-related diseases. | Idiopathic pulmonary fibrosis drug candidate. | Progressed from target discovery to Phase I trials in approximately 18 months, a fraction of the typical 3-5 year timeline [1]. |
| Recursion Pharmaceuticals [4] [1] [3] | AI-powered high-throughput phenotypic screening with cellular imaging. | Focus on rare genetic diseases, oncology, and fibrosis. | AI-driven screening led to identification of potential therapeutics for rare genetic diseases; merged with Exscientia to integrate generative chemistry [4] [1]. |
| BenevolentAI [4] [1] [3] | AI-powered knowledge graph for target discovery and validation. | Programs in COVID-19 and neurodegenerative diseases. | Knowledge Graph connects genes, diseases, and compounds to uncover novel therapeutic opportunities; robust biological modeling for target validation [1] [3]. |
| Atomwise [3] [5] | Structure-based deep learning (AtomNet platform) for small-molecule discovery. | Orally bioavailable TYK2 inhibitor (preclinical) for autoimmune diseases. | In a 318-target study, identified novel hits for 235 targets; presented as a viable alternative to high-throughput screening [5]. |
| Schrödinger [4] [1] [3] | Physics-based computational chemistry combined with machine learning. | Internal pipeline in oncology and neurology. | Platform used for molecular modeling and drug design by major pharma partners; offers robust physics-based and biological modeling [4] [1]. |
The progression of AI-designed molecules into clinical trials is the ultimate form of validation. By the end of 2024, the cumulative number of AI-derived molecules reaching clinical stages had grown exponentially, with over 75 candidates entering human trials [1]. However, it is crucial to note that as of 2025, no AI-discovered drug has yet received market approval, with most programs remaining in early-stage trials [1]. This underscores the importance of rigorous validation at every stage to improve the probability of clinical success.
Domain-Specific Validation Metrics for AI Models
Validating AI models in drug discovery requires moving beyond generic machine learning metrics. The highly specialized nature of biomedical data, often characterized by imbalance, multi-modality, and rare critical events, necessitates a tailored set of performance indicators [2]. The following table compares generic metrics against their domain-specific adaptations, which are becoming the standard for rigorous model evaluation in biopharma.
Table 2: Comparison of Generic vs. Domain-Specific ML Metrics for Drug Discovery
| Generic ML Metric | Limitations in Drug Discovery | Domain-Specific Alternative | Application & Rationale |
|---|---|---|---|
| Accuracy [2] | Misleading with imbalanced datasets (e.g., excess of inactive compounds); a model can achieve high accuracy by always predicting the majority class. | Rare Event Sensitivity [2] | Measures the model's ability to detect low-frequency events (e.g., toxicological signals, active compounds), which are critical for actionable outcomes. |
| F1 Score [2] | Offers a balanced view but may dilute focus on the top-ranking predictions that are most critical for resource allocation. | Precision-at-K [2] | Evaluates the model's precision when considering only the top K ranked candidates, ensuring focus on the most promising leads for experimental validation. |
| ROC-AUC [2] | Evaluates class separation but lacks biological interpretability and does not assess the mechanistic relevance of predictions. | Pathway Impact Metrics [2] | Assesses how well a model's predictions align with known or novel biological pathways, ensuring findings are statistically valid and biologically meaningful. |
The implementation of these specialized metrics was demonstrated effectively by Elucidata in an omics-based drug discovery project. The challenge was to improve the detection of rare toxicological signals in transcriptomics datasets, where traditional metrics failed. By implementing a customized ML pipeline optimized with Rare Event Sensitivity and Precision-Weighted Scoring, the model achieved a 4x increase in detection speed for subtle toxicological signals, enabling faster and more confident decision-making [2]. This case study highlights how domain-specific validation directly translates to improved R&D efficiency.
Experimental Protocols for Validating AI-Generated Candidates
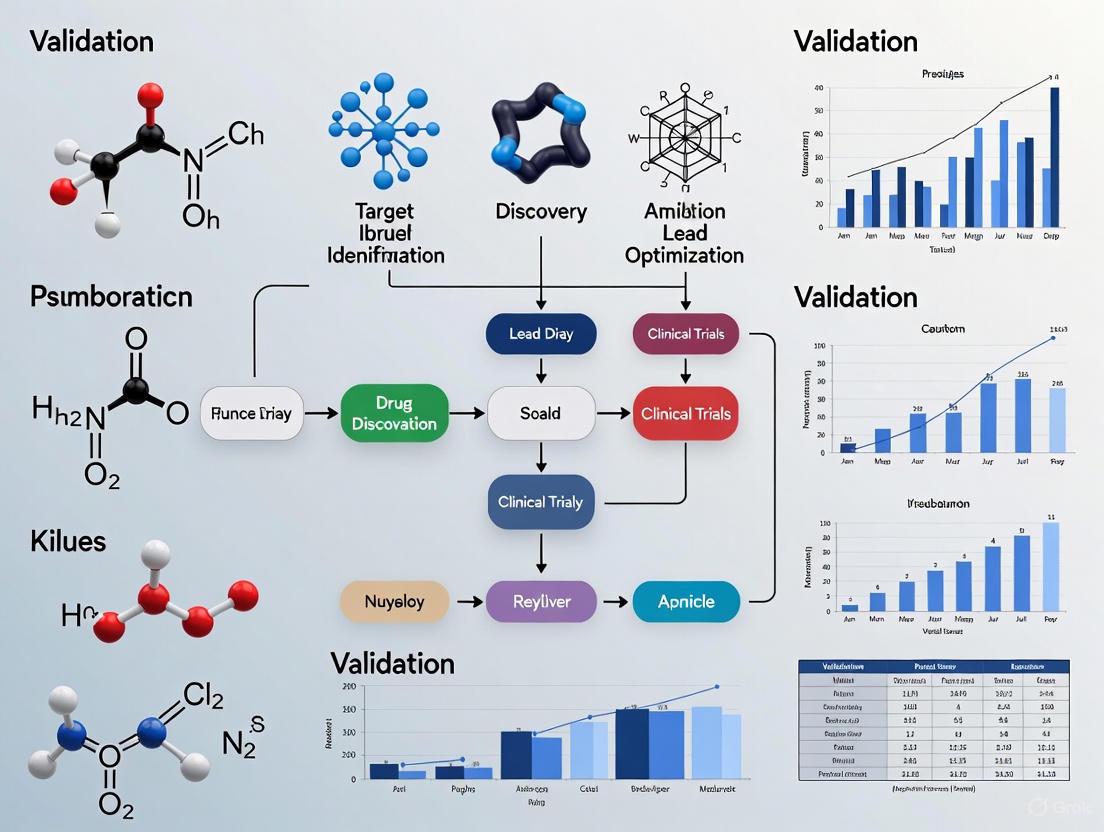
A robust validation strategy requires standardized experimental workflows to confirm the properties and potential of AI-generated drug candidates. The "Design-Make-Test-Analyze" (DMTA) cycle is the core iterative process in modern drug discovery, and AI is being integrated into every stage [6]. The diagram below illustrates a validated, AI-augmented DMTA cycle for small molecule discovery.
The validation of AI-discovered compounds relies on a multi-stage protocol combining in silico predictions with rigorous experimental testing. The following is a detailed breakdown of the key stages for a typical small-molecule candidate, drawing from reported industry practices.
Protocol 1: In Silico Target Validation and Compound Generation
- Objective: To identify a novel, druggable disease target and generate a series of lead compounds with high predicted affinity and specificity.
- Detailed Methodology:
- Target Identification: Use AI platforms (e.g., Insilico's PandaOmics, BenevolentAI's Knowledge Graph) to analyze multi-omics datasets (genomics, proteomics, transcriptomics) from diseased versus healthy tissues. The goal is to identify and prioritize potential protein targets based on their causal link to the disease and "druggability" [1] [3] [5].
- Generative Molecular Design: Employ generative AI models (e.g., Exscientia's DesignStudio, Insilico's Chemistry42) to design novel small-molecule structures de novo that fit a specific target product profile. This profile includes desired potency, selectivity, and predicted ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) properties [1] [7].
- Virtual Screening & Prioritization: Screen the generated virtual library against the target structure (if available) using deep learning networks (e.g., Atomwise's AtomNet) to predict binding affinity [3] [5]. Subsequently, apply domain-specific metrics like Precision-at-K to rank-order the top candidate molecules for synthesis [2].
Protocol 2: Experimental & Preclinical Validation
- Objective: To empirically confirm the predicted activity, selectivity, and safety of the synthesized AI-generated lead compounds in biological systems.
- Detailed Methodology:
- Compound Synthesis & Characterization: Synthesize the top-priority virtual candidates. Companies like Exscientia and Iktos are increasingly integrating AI with robotic synthesis automation (e.g., Iktos's Spaya and Robotics platforms) to accelerate this step [1] [5]. Confirm the chemical structure and purity of synthesized compounds using standard analytical techniques (NMR, LC-MS).
- In Vitro Biochemical/Cellular Assays: Test the synthesized compounds in a series of in vitro experiments. This begins with binding assays (e.g., SPR) and functional cell-based assays to determine potency (IC50/EC50) and efficacy. For a more translational view, platforms like Exscientia use patient-derived primary cells or tissue samples (e.g., from its Allcyte acquisition) to assess compound efficacy in a more disease-relevant context [1].
- ADMET Profiling: Conduct in vitro ADMET studies to assess key parameters such as metabolic stability in liver microsomes, membrane permeability (Caco-2 assays), and cardiac safety risk (hERG inhibition). AI-based ADMET prediction models, like the one benchmarked by Receptor.AI, are used earlier in the workflow to filter out molecules with poor predicted properties, minimizing costly experimental testing on likely failures [8].
- In Vivo Efficacy and Toxicity: Advance the most promising lead candidate to animal models of the disease to demonstrate proof-of-concept efficacy and preliminary pharmacokinetics and toxicology. The data generated here is fed back into the AI models (see DMTA cycle diagram) to refine the design of the next generation of compounds, closing the learning loop [1] [6].
Essential Research Reagents and Solutions for Validation
The experimental validation of AI-generated discoveries relies on a suite of core research reagents and technological solutions. The following table details these key tools and their functions in the validation workflow.
Table 3: Key Research Reagent Solutions for Experimental Validation
| Research Reagent / Solution | Function in Validation Workflow |
|---|---|
| Patient-Derived Primary Cells & Organoids [1] | Provide a physiologically relevant ex vivo system for testing compound efficacy and toxicity, improving the translational predictiveness of in vitro data. |
| High-Content Cellular Imaging Systems [1] [3] [5] | Enable high-throughput, automated phenotypic screening of compounds on cells, generating rich datasets for AI models to analyze complex morphological changes. |
| Automated Synthesis & Screening Robotics [1] [5] | Automate the "Make" and "Test" phases of the DMTA cycle, increasing throughput, reproducibility, and the speed of data generation for AI feedback loops. |
| Multi-Omics Datasets (Genomic, Proteomic) [2] [3] | Serve as the foundational data for AI-driven target discovery and biomarker identification; quality and diversity of data are critical for model performance. |
| Retrieval-Augmented Generation (RAG) Systems [6] | AI software tool that grounds Large Language Models (LLMs) in proprietary internal research data, enabling scientists to query and find information across data silos to inform validation. |
| On-Premise LLM Deployment [6] | An infrastructure solution that allows companies to deploy AI models internally, enforcing data privacy and security guardrails while leveraging AI for research assistance. |
Implementation of a Robust AI Validation Framework
For researchers and drug development professionals, transitioning to an AI-augmented workflow requires more than just adopting new software; it demands a fundamental shift in validation culture. Success hinges on implementing a comprehensive framework that addresses data, metrics, and organizational practices.
First, data quality is the foundation of AI validation. The principle of "garbage in, garbage out" is paramount. Initiatives like DataPerf, which provide benchmarks for data-centric AI development, are gaining traction [9]. This involves shifting focus from solely refining model architectures to systematically curating, cleaning, and labeling training datasets. In practice, this means investing in standardized data curation protocols to handle diverse sources like ChEMBL, ToxCast, and proprietary in-house data [2] [8].
Second, organizations must enforce centralized guardrails and ensure model transparency. As AI adoption spreads, practices such as creating risk profiles that dictate the permitted level of AI involvement in a decision and validating specific models for high-risk tasks are becoming essential [6]. Furthermore, the "black-box" nature of some complex models erodes trust among scientists. To counter this, validation reports must include explainability features, such as links to corroborating internal data or displays of the most similar training set compounds, to create traceability and justify experimental follow-up [6].
Finally, the most critical element is fostering collaboration between data scientists and domain experts. Biologically meaningful validation cannot be performed in a computational silo. Cross-functional teams are needed to design and interpret experiments, ensuring that evaluation metrics and model outputs are not just statistically sound but also biologically and clinically relevant [2] [1]. This collaborative spirit is what ultimately bridges the gap between a promising algorithm and an approved drug that meets the stringent requirements of regulators and patients.
The application of Artificial Intelligence (AI) in drug discovery represents a paradigm shift in pharmaceutical research, offering unprecedented capabilities to analyze vast biological datasets, identify potential drug targets, and predict therapeutic effectiveness [10]. As AI technologies become increasingly integrated into the drug development pipeline, establishing robust validation frameworks has become imperative to ensure these systems deliver reliable, trustworthy, and clinically relevant outcomes. The RICE Framework emerges as a critical structured approach for validating AI-based drug discovery models, encompassing four core objectives: Robustness, Interpretability, Controllability, and Ethicality.
This framework addresses the unique challenges presented by AI/ML technologies in the highly regulated pharmaceutical environment, where regulatory bodies like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have established stringent guidelines emphasizing reliability, transparency, and patient safety [11]. The RICE Framework provides a comprehensive methodology for researchers and drug development professionals to evaluate AI models beyond mere predictive accuracy, ensuring they meet the rigorous standards required for therapeutic development and regulatory approval.
Core Objectives of the RICE Framework
Robustness
In the context of AI-based drug discovery, Robustness refers to a model's ability to maintain stable, reliable performance across diverse datasets, experimental conditions, and potential adversarial inputs. Robust AI models demonstrate minimal performance degradation when confronted with noisy data, distribution shifts, or slightly perturbed inputs, which is particularly crucial in biological systems where experimental variability is inherent.
Robustness validation ensures that AI predictions for drug-target interactions, toxicity profiles, or molecular properties remain consistent and dependable when applied to real-world patient populations or different laboratory settings. Regulatory guidelines emphasize the importance of rigorous testing under diverse conditions to confirm model accuracy and robustness before deployment in critical decision-making processes [11]. Techniques for enhancing robustness include data augmentation, adversarial training, and stress testing under edge cases that simulate challenging real-world scenarios.
Interpretability
Interpretability addresses the fundamental need to understand and trust the decision-making processes of AI models, moving beyond "black box" predictions to transparent, explainable insights. In drug discovery, where decisions have significant implications for patient safety and therapeutic efficacy, understanding how an AI model arrives at its predictions is essential for scientific validation and regulatory acceptance [11].
The interpretability requirement is particularly critical for complex models like deep neural networks, which might otherwise function as inscrutable black boxes. Regulatory frameworks increasingly demand transparency in how algorithms are trained, validated, and how they make decisions, requiring researchers to document training data, decision logic, and algorithm versions [11]. Explainable AI (XAI) techniques such as attention mechanisms, feature importance analysis, and surrogate models help researchers understand which molecular features, structural properties, or biological pathways most significantly influence model predictions, fostering trust and facilitating scientific discovery.
Controllability
Controllability encompasses the methodologies and mechanisms that allow researchers to direct, constrain, and fine-tune AI model behavior to align with scientific objectives, safety constraints, and experimental parameters. In drug discovery, controllability ensures that AI-generated molecular designs adhere to chemical synthesizability constraints, toxicity thresholds, and therapeutic targeting requirements.
The emergence of generative AI models for molecular design has heightened the importance of controllability, as researchers must steer molecular generation toward synthetically feasible compounds with desired properties. Frameworks like SynFormer exemplify this principle by generating synthetic pathways alongside molecular structures, ensuring proposed compounds are not only theoretically promising but also practically synthesizable [12]. Controllability also encompasses the ability to adjust model behavior based on emerging experimental data, creating iterative feedback loops that refine AI predictions through continuous learning while maintaining alignment with research goals.
Ethicality
Ethicality in the RICE Framework addresses the profound responsibility inherent in developing therapeutics for human patients, encompassing data privacy, algorithmic fairness, patient safety, and social impact. Ethical AI deployment in drug discovery requires vigilant attention to potential biases in training data, particularly the underrepresentation of specific patient populations that could skew predictions and diminish clinical generalizability [11].
The World Health Organization has emphasized the need for ethical governance structures to prevent AI from dehumanizing care, undermining patient autonomy, or posing significant risks to patient privacy [13]. Ethicality also encompasses broader concerns including appropriate data protection with rights-based approaches, informed consent for data usage, and safeguards against malicious application of AI technologies for bioterrorism [13]. Implementing ethical AI requires multidisciplinary collaboration between data scientists, clinicians, ethicists, and regulatory experts to ensure technologies develop within a framework that prioritizes patient welfare and social benefit.
Comparative Analysis of AI Models Using the RICE Framework
Quantitative Comparison of AI Drug Discovery Models
Table 1: Performance Metrics of AI Models in Drug Discovery Applications
| AI Model | Application Domain | Robustness Score | Interpretability Level | Controllability Features | Ethicality Safeguards |
|---|---|---|---|---|---|
| Metabolite Translator | Metabolite Prediction | 92% accuracy on diverse compound libraries | Medium: Attention mechanisms show relevant chemical features | High: Controllable output for specific metabolic pathways | Medium: Anonymized training data, bias monitoring |
| SynFormer | Synthesizable Molecular Design | 88% synthesizability rate in validation | Medium: Pathway visualization illustrates synthetic routes | High: Explicit synthetic pathway generation | Medium: Focus on synthetic accessibility reduces resource waste |
| AlphaFold | Protein Structure Prediction | >90% GDT accuracy on CASP targets | Low: Limited explanation for structural confidence | Low: Limited steering of folding process | High: Open access promotes equitable research benefits |
| Deep Learning QSAR | Toxicity Prediction | 85% cross-validation consistency | Medium: Feature importance identifies structural alerts | Medium: Threshold control for safety margins | High: Rigorous bias testing across demographic groups |
Table 2: Regulatory Compliance Assessment of AI Models Against FDA Guidelines
| Compliance Dimension | Metabolite Translator | SynFormer | Traditional QSAR Models | Generative Molecular AI |
|---|---|---|---|---|
| Data Integrity (ALCOA+) | Partial compliance with electronic records | Full compliance with version control | Full compliance with established protocols | Variable compliance based on implementation |
| Model Explainability | Medium: Input-output relationships documented | Medium: Pathway rationale provided | High: Transparent parameters | Low: Black-box architecture concerns |
| Reproducibility Documentation | High: Full training data and parameters archived | High: Reaction templates and building blocks cataloged | High: Established protocols with minimal variance | Medium: Stochastic elements complicate reproduction |
| Bias Mitigation | Medium: Diverse chemical space representation | High: Focus on synthesizability reduces resource bias | Medium: Dependent on training data curation | Low: Potential for unrealistic molecular generation |
Case Study: Metabolite Translator for Drug Metabolism Prediction
The Metabolite Translator model, developed at Rice University, provides an illustrative case study for applying the RICE Framework [14]. This deep learning-based technique predicts metabolites resulting from interactions between small molecules like drugs and enzymes, giving pharmaceutical developers a comprehensive picture of potential drug behavior and toxicity profiles.
Robustness was validated through extensive testing across diverse compound libraries, achieving 92% accuracy in predicting known metabolic pathways. The model maintains stable performance when applied to novel chemical structures, demonstrating particular strength in identifying metabolites formed through enzymes not commonly involved in drug metabolism that are typically missed by rule-based methods [14].
Interpretability is facilitated through the model's translation-based architecture, which uses SMILES (Simplified Molecular-Input Line-Entry System) notation to represent chemical transformations in human-readable format. While the underlying deep learning model has inherent complexity, attention mechanisms help researchers identify which molecular substructures most significantly influence metabolic predictions.
Controllability is evidenced by the model's ability to focus predictions on specific enzymatic pathways or tissue types, allowing researchers to explore metabolic fate in particular biological contexts. This enables targeted investigation of hepatic versus extra-hepatic metabolism, supporting comprehensive toxicity profiling.
Ethicality considerations are addressed through the model's potential to reduce animal testing by providing accurate computational predictions of human metabolism. The training approach using transfer learning on known chemical reactions helps mitigate bias that might arise from limited experimental data.
Diagram 1: Metabolite Translator Workflow. This illustrates the sequence from molecular input to metabolite prediction, highlighting key computational stages.
Case Study: SynFormer for Synthesizable Molecular Design
SynFormer represents a significant advancement in generative AI for drug discovery by explicitly addressing synthesizability throughout the molecular design process [12]. This framework integrates a scalable transformer architecture with a diffusion module for building block selection, specifically focusing on generating synthetic pathways rather than just molecular structures.
Robustness in SynFormer is demonstrated through its consistent performance in both local chemical space exploration (generating synthesizable analogs of reference molecules) and global exploration (identifying optimal molecules according to black-box property prediction). The model maintains structural integrity while ensuring synthetic feasibility, with analogs maintaining favorable objective scores close to original designs [12].
Interpretability is enhanced through the model's pathway-centric approach, which provides researchers with explicit synthetic routes rather than just final molecular structures. This transparency in proposed synthesis helps medicinal chemists evaluate and trust the AI's proposals, understanding the stepwise chemical transformations suggested.
Controllability is a foundational strength of SynFormer, which allows researchers to constrain molecular generation based on available starting materials, preferred reaction types, or complexity parameters. This fine-grained control ensures that AI-generated molecules align with practical laboratory constraints and resource availability.
Ethicality considerations are addressed through SynFormer's focus on synthetic accessibility, which helps prevent wasted resources on pursuing theoretically interesting but practically inaccessible compounds. This promotes more efficient drug discovery with reduced material waste.
Diagram 2: SynFormer Molecular Design Process. This workflow shows the iterative pathway for generating synthesizable molecules, with feasibility checks ensuring practical outcomes.
Experimental Protocols for RICE Framework Validation
Robustness Testing Protocol
Objective: Systematically evaluate AI model performance stability under varied data conditions and potential adversarial inputs.
Materials:
- Primary validation dataset (curated, high-quality reference data)
- Noise-injected datasets (varied levels of Gaussian noise)
- Domain-shifted datasets (different biological contexts or experimental conditions)
- Adversarial examples (strategically modified inputs)
Methodology:
- Baseline Performance Establishment: Evaluate model accuracy, precision, and recall on primary validation dataset under standardized conditions.
- Noise Tolerance Assessment: Introduce progressively increasing Gaussian noise (5%, 10%, 15%) to input features and measure performance degradation.
- Domain Shift Evaluation: Test model on data from different sources (e.g., alternative cell lines, animal models, or experimental protocols).
- Adversarial Robustness Testing: Expose model to strategically modified inputs designed to provoke incorrect predictions while maintaining semantic validity.
- Cross-validation: Implement k-fold cross-validation (typically k=5 or k=10) to assess performance consistency across data subsets.
Validation Metrics:
- Performance degradation slope under noise introduction
- Domain adaptation gap (performance difference between primary and shifted domains)
- Adversarial success rate (proportion of adversarial examples that cause prediction failures)
- Variance in cross-validation performance across folds
Interpretability Assessment Protocol
Objective: Quantitatively and qualitatively evaluate the explainability of model predictions and decision logic.
Materials:
- Model with accessible intermediate layers or attention mechanisms
- Reference dataset with ground truth explanations (where available)
- Feature importance evaluation framework
- Domain expert panel for qualitative assessment
Methodology:
- Feature Importance Analysis: Implement perturbation-based or gradient-based techniques to identify input features most influential to predictions.
- Attention Visualization: For attention-based models, visualize and quantify attention patterns across input sequences or structures.
- Counterfactual Explanation Generation: Systematically modify inputs to identify minimal changes that alter model predictions.
- Domain Expert Evaluation: Engage medicinal chemists, biologists, and pharmacologists in structured evaluation of model explanations for plausibility and utility.
- Faithfulness Measurement: Assess whether explanatory features truly drive model decisions through ablation studies.
Validation Metrics:
- Explanation fidelity (correlation between explanatory importance and prediction impact)
- Expert agreement score (proportion of model explanations deemed plausible by domain experts)
- Explanation stability (consistency of explanations for similar inputs)
- Completeness score (proportion of prediction variance explained by identified features)
Controllability Verification Protocol
Objective: Validate the effectiveness of mechanisms for steering and constraining model behavior to align with research objectives.
Materials:
- Model with controllability interfaces (constraint specification, objective weighting)
- Benchmark tasks with defined constraints and optimization targets
- Molecular property prediction services or assays
- Synthetic chemistry feasibility assessment tools
Methodology:
- Constraint Adherence Testing: Evaluate model performance under progressively stricter constraints (e.g., synthesizability, toxicity thresholds, property ranges).
- Multi-objective Optimization Assessment: Test model ability to balance competing objectives (e.g., potency versus solubility, selectivity versus synthesizability).
- Directional Control Verification: Assess how effectively model outputs respond to explicit guidance signals and parameter adjustments.
- Constraint Violation Analysis: Quantify the frequency and magnitude of constraint violations in generated outputs.
- Feedback Integration Testing: Evaluate how effectively models incorporate experimental feedback to refine future predictions.
Validation Metrics:
- Constraint satisfaction rate (proportion of outputs meeting all specified constraints)
- Multi-objective optimization efficiency (Pareto front quality and diversity)
- Control responsiveness (output change magnitude per unit control signal)
- Iterative improvement rate (performance enhancement through feedback loops)
Ethicality Audit Protocol
Objective: Systematically identify and mitigate potential ethical risks in AI model development and deployment.
Materials:
- Diverse demographic and biomedical datasets for bias assessment
- Data protection and privacy assessment frameworks
- Ethical guidelines from regulatory bodies (WHO, FDA, EMA)
- Stakeholder engagement protocols
Methodology:
- Bias Audit: Evaluate model performance disparities across demographic groups, disease subtypes, and molecular classes.
- Privacy Impact Assessment: Analyze data handling practices against GDPR, HIPAA, and other relevant privacy regulations.
- Dual-Use Risk Evaluation: Assess potential for malicious application and implement appropriate safeguards.
- Transparency Documentation: Complete comprehensive documentation of model capabilities, limitations, and appropriate use cases.
- Stakeholder Impact Analysis: Identify and evaluate potential effects on patients, researchers, healthcare systems, and society.
Validation Metrics:
- Fairness disparity scores (performance variation across protected groups)
- Privacy preservation metrics (re-identification risk, data leakage potential)
- Transparency index (completeness of documentation and limitation disclosure)
- Stakeholder impact score (breadth and equity of benefit distribution)
Essential Research Reagents and Computational Tools
Table 3: Key Research Reagent Solutions for AI Drug Discovery Validation
| Reagent/Tool Category | Specific Examples | Primary Function in RICE Validation | Implementation Considerations |
|---|---|---|---|
| Chemical Structure Encoders | SMILES, SELFIES, Graph Neural Networks | Convert molecular structures into machine-readable formats for model training and prediction | SMILES offers simplicity but can generate invalid structures; SELFIES provides guaranteed validity |
| Reaction Databases | USPTO, Reaxys, Pistachio | Provide curated chemical transformations for training metabolic prediction and synthesizability models | Data quality varies significantly; require careful preprocessing and standardization |
| Protein Structure Predictors | AlphaFold, RoseTTAFold | Generate 3D protein structures for target-based drug discovery and binding affinity prediction | Accuracy varies across protein families; confidence metrics crucial for reliability assessment |
| Toxicity Prediction Services | ProTox, DeepTox, ADMET Predictor | Provide benchmark toxicity predictions for model validation and comparative analysis | Different tools cover varying endpoint types; ensemble approaches often improve reliability |
| Synthesizability Assessment | SYBA, SCScore, RAscore | Evaluate synthetic accessibility of AI-generated molecules prior to experimental validation | Scores are relative rather than absolute; require calibration with specific synthetic capabilities |
| Feature Importance Tools | SHAP, LIME, Integrated Gradients | Interpret model predictions by quantifying contribution of input features to output decisions | Different methods may yield varying explanations; multiple approaches recommended for validation |
| Bias Detection Frameworks | AI Fairness 360, Fairlearn | Identify performance disparities across demographic groups or molecular classes | Require careful definition of protected attributes and disparity metrics relevant to context |
| Adversarial Attack Libraries | Advertorch, CleverHans, Foolbox | Generate adversarial examples to test model robustness and identify potential failure modes | Should simulate realistic perturbations rather than purely mathematical constructs |
The RICE Framework provides a comprehensive, structured approach for validating AI-based drug discovery models, addressing critical dimensions of Robustness, Interpretability, Controllability, and Ethicality that collectively determine real-world utility and regulatory acceptability. As AI technologies continue to evolve and integrate more deeply into pharmaceutical research, systematic application of this framework will be essential for ensuring that AI-driven discoveries translate reliably into safe, effective therapeutics.
The comparative analysis presented demonstrates that while current AI models show promising capabilities across the RICE dimensions, significant variation exists in how different approaches address these critical requirements. Models like Metabolite Translator and SynFormer exemplify the principled integration of domain knowledge and practical constraints that characterizes effective AI drug discovery tools [14] [12]. The experimental protocols and research reagents cataloged provide practical resources for implementing rigorous validation practices that align with emerging regulatory guidelines from the FDA, EMA, and WHO [11] [13].
Future advancements in AI for drug discovery will need to continue balancing predictive power with the fundamental requirements encapsulated in the RICE Framework. As noted by regulatory experts, successful AI regulatory compliance requires proactive engagement with regulatory agencies, cross-disciplinary collaboration, and lifecycle management that extends beyond initial model development [11]. By adopting structured validation approaches like the RICE Framework, researchers and drug development professionals can accelerate the translation of AI innovations into transformative therapies while maintaining the rigorous standards required for patient safety and therapeutic efficacy.
The integration of Artificial Intelligence (AI) into drug development represents a paradigm shift, offering unprecedented opportunities to enhance efficiency, accuracy, and speed across the pharmaceutical lifecycle [15]. From identifying novel drug candidates to optimizing clinical trials and monitoring post-market safety, AI technologies are poised to address long-standing inefficiencies in one of the most resource-intensive sectors in healthcare [16]. However, this transformative potential is accompanied by significant regulatory challenges, including concerns about algorithmic transparency, data integrity, model robustness, and clinical validity [17].
Recognizing these challenges, regulatory agencies worldwide are developing frameworks to ensure that AI tools used in critical decision-making processes meet rigorous standards for safety and effectiveness. The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have emerged as pivotal figures in shaping the global regulatory landscape for AI in pharmaceuticals [16]. Their evolving guidance documents reflect a concerted effort to balance innovation with patient safety, establishing clear expectations for the validation of AI models throughout the drug development pipeline.
This comparative guide examines the current regulatory expectations from the FDA and EMA regarding AI validation, providing researchers, scientists, and drug development professionals with a structured framework for navigating these complex requirements. By synthesizing the most recent guidance documents, discussion papers, and policy statements, this analysis aims to support the development of robust, compliant AI applications that accelerate the delivery of new therapies to patients.
Comparative Analysis of FDA and EMA Regulatory Frameworks
Foundational Principles and Regulatory Philosophy
The FDA and EMA share common objectives in regulating AI for drug development, notably ensuring patient safety, product quality, and the reliability of evidence submitted to support marketing authorization. However, their regulatory philosophies and implementation approaches reflect distinct institutional traditions and risk-management strategies [16].
The U.S. FDA has adopted a pragmatic, risk-based approach that emphasizes the specific "context of use" (COU) of an AI model [18] [19] [20]. This framework is designed to be adaptable to the rapidly evolving AI landscape, focusing on establishing "model credibility" through a structured assessment process tailored to the model's influence on regulatory decisions and the potential consequences of incorrect outputs [18]. The FDA's guidance is primarily non-binding and recommends early engagement with sponsors to set expectations for AI model validation [19].
The European EMA demonstrates a more structured and cautious approach, prioritizing rigorous upfront validation and comprehensive documentation before AI systems are integrated into drug development [16]. The EMA's framework, outlined in its "AI in Medicinal Product Lifecycle Reflection Paper," emphasizes a risk-based approach while maintaining stronger alignment with traditional pharmaceutical regulations and quality-by-design principles [16]. The EMA has also reached a significant milestone with its first qualification opinion on AI methodology in March 2025, accepting clinical trial evidence generated by an AI tool for diagnosing inflammatory liver disease [16].
Table 1: Core Regulatory Principles and Philosophies
| Aspect | U.S. FDA | European EMA |
|---|---|---|
| Primary Approach | Risk-based, context-specific credibility assessment | Structured, upfront validation with qualified AI methodologies |
| Guidance Status | Draft guidance (January 2025) [18] [19] | Reflection paper (October 2024) with specific qualification opinions [16] |
| Foundation | Risk-based credibility framework centered on "Context of Use" (COU) [18] | Risk-based approach integrated into medicinal product lifecycle [16] |
| Key Emphasis | Establishing model credibility for specific decision-making tasks [20] | Rigorous validation, documentation, and integration with existing GxP systems [16] |
Scope and Applicability
The scope of AI applications covered by FDA and EMA guidance reveals important distinctions in regulatory priorities and focus areas. Both agencies concentrate on AI models that impact patient safety, drug quality, or the reliability of study results, but they differ in their specific exclusions and areas of emphasis [18] [16].
The FDA's draft guidance explicitly excludes AI models used solely for drug discovery or those employed to streamline operational efficiencies that do not impact patient safety, drug quality, or study reliability [18] [20]. This exclusion reflects the FDA's current focus on AI applications that directly support regulatory decision-making for products already in the development pipeline. The guidance applies broadly to AI use in clinical trial design and management, patient evaluation, endpoint adjudication, clinical data analysis, digital health technologies for drug development, pharmacovigilance, pharmaceutical manufacturing, and real-world evidence generation [18].
The EMA's framework takes a broader lifecycle perspective, encompassing AI applications from discovery through post-market surveillance without explicit exclusions for discovery phase applications [16]. This comprehensive scope aligns with the EMA's integrated approach to medicinal product regulation, recognizing that AI tools may have implications across the entire product lifecycle. The agency emphasizes that AI systems used in the context of clinical trials must comply with Good Clinical Practice (GCP) guidelines, with high-impact systems subject to comprehensive assessment during authorization procedures [16].
Risk Classification and Credibility Assessment
Both agencies employ risk-based frameworks to determine the level of scrutiny required for AI validation, but they differ in their specific risk classification methodologies and assessment criteria.
The FDA employs a detailed seven-step, risk-based credibility assessment framework that forms the core of its regulatory approach [18] [19] [20]. This process begins with defining the specific "question of interest" that the AI model will address and precisely delineating its "context of use" [18]. Risk assessment considers two primary factors: "model influence risk" (how much the AI output influences decision-making) and "decision consequence risk" (the potential impact of an incorrect decision on patient safety or product quality) [18]. Models with higher influence and consequence risks require more extensive validation and documentation.
The EMA's risk classification system, while similarly risk-based, places greater emphasis on the intended purpose of the AI system and its impact on critical decision points within the medicinal product lifecycle [16]. High-risk applications include those where AI outputs directly influence patient eligibility for treatments, clinical endpoint adjudication, or safety determinations [16]. The EMA expects comprehensive validation evidence for these high-risk applications, including analytical validation (establishing technical performance), clinical validation (demonstrating correlation with clinical outcomes), and organizational validation (ensuring appropriate governance and workflow integration) [16].
Table 2: Risk Classification and Validation Requirements
| Risk Level | FDA Examples & Requirements [18] [19] | EMA Expectations [16] |
|---|---|---|
| High Risk | - AI determines patient risk classification for life-threatening events- Fully automated decisions impacting patient safety- Comprehensive details on architecture, data, training, validation | - AI directly influences patient eligibility or treatment decisions- Requires analytical, clinical, and organizational validation- Comprehensive documentation and rigorous assessment |
| Moderate Risk | - AI identifies manufacturing batches out-of-specification but requires human confirmation- Intermediate level of disclosure | - AI supports clinical trial site selection or data collection- Substantial evidence of performance and robustness |
| Low Risk | - AI assists with operational workflows not impacting safety or quality- Minimal information may be requested | - AI used for literature screening or administrative task automation- Focus on data integrity and basic performance metrics |
Documentation and Submission Requirements
Documentation requirements represent a critical component of AI validation, providing regulatory agencies with the evidence needed to assess model credibility and appropriateness for the intended context of use.
The FDA expects sponsors to develop and execute a "credibility assessment plan" that documents how the AI model was developed, trained, evaluated, and monitored [18] [19]. This plan should include a detailed description of the model architecture, data sources and characteristics, training methodologies, validation processes, performance metrics, and approaches to addressing potential biases [18]. For higher-risk models, the FDA may request extensive information covering all aspects of model development and deployment. The guidance recommends that sponsors discuss with the FDA "whether, when, and where" to submit the credibility assessment report, which could be included in a regulatory submission, meeting package, or made available upon request during inspections [19].
The EMA emphasizes comprehensive documentation integrated within the overall marketing authorization application [16]. This includes detailed information about the AI model's development process, training data representativeness, validation results against appropriate benchmarks, and plans for lifecycle management [16]. The EMA places particular importance on the explainability of AI outputs and the clinical relevance of the model's predictions, requiring clear documentation of how the model's outputs relate to clinically meaningful endpoints [16].
Lifecycle Management and Post-Market Monitoring
Both agencies recognize that AI models may evolve over time and require ongoing monitoring and maintenance to ensure continued performance and suitability for their intended use.
The FDA's draft guidance specifically addresses "lifecycle maintenance" for AI models, noting that changes in input data or deployment environments may affect model performance [18] [19]. Sponsors are expected to maintain detailed lifecycle maintenance plans as part of their pharmaceutical quality systems, with summaries included in marketing applications [19]. These plans should describe activities for monitoring model performance, detecting "model drift" or performance degradation, and implementing appropriate retraining or revalidation procedures when needed [18]. Certain changes impacting model performance may need to be reported to the FDA in accordance with existing regulatory requirements for post-approval changes [19].
The EMA similarly emphasizes continuous monitoring and quality management throughout the AI system's lifecycle [16]. The agency expects robust processes for tracking model performance in real-world settings, detecting data drift or concept drift, and implementing version control and change management procedures [16]. The EMA's framework aligns with existing pharmacovigilance requirements, treating significant changes to AI models as potential modifications to the medicinal product's evidence base that may require regulatory notification or approval [16].
Technical Requirements for AI Validation
Data Management and Quality Standards
High-quality data forms the foundation of credible AI models, and both agencies establish rigorous expectations for data management practices throughout the model lifecycle.
The FDA emphasizes comprehensive data characterization, including detailed descriptions of data sources, collection methods, cleaning procedures, and annotation protocols [18]. The guidance highlights the importance of data quality, diversity, and relevance to the intended patient population, with particular attention to identifying and mitigating potential biases in training datasets [18]. Sponsors should provide evidence of appropriate segregation between training, tuning, and validation datasets to prevent overfitting and ensure independent performance assessment [18]. For models using real-world data, the FDA expects thorough documentation of data provenance and processing transformations [19].
The EMA's requirements align closely with established principles of data integrity (ALCOA+) - ensuring data are Attributable, Legible, Contemporaneous, Original, and Accurate [16]. The agency emphasizes the importance of dataset representativeness, requiring that training and validation data adequately reflect the target population and use environments [16]. Metadata capture is particularly emphasized, including information about data collection conditions, preprocessing steps, and annotation criteria, to enable proper interpretation and reuse of data assets [16] [17].
Data Management Workflow for AI Validation: This diagram illustrates the sequential process for managing data throughout the AI model lifecycle, from initial collection through comprehensive documentation.
Model Development and Performance Evaluation
Robust model development and rigorous performance evaluation are essential components of AI validation, with both agencies establishing detailed expectations for these processes.
The FDA recommends comprehensive model description including architecture details, feature selection processes, optimization methods, and tuning procedures [18]. Model evaluation should include appropriate performance metrics tailored to the context of use, with testing against independent datasets to demonstrate generalizability [18]. The guidance emphasizes the importance of identifying and documenting model limitations, potential failure modes, and approaches to quantifying uncertainty in predictions [18]. For models with customizable features or adaptive components, sponsors should provide detailed descriptions of the technical elements that enable and control these capabilities [21].
The EMA places strong emphasis on clinical validity and relevance, requiring demonstration that model outputs correlate with clinically meaningful endpoints [16]. Performance evaluation should include appropriate benchmarking against established methods or clinical standards, with particular attention to robustness testing across relevant subpopulations and clinical scenarios [16]. The agency also emphasizes the importance of model explainability, especially for high-risk applications, requiring that developers provide sufficient information to enable healthcare professionals to understand and appropriately interpret model outputs [16].
Table 3: Essential Research Reagent Solutions for AI Validation
| Reagent Category | Specific Examples | Function in AI Validation |
|---|---|---|
| Reference Standards | Ground truth datasets, Benchmarking corpora, Qualified medical image archives | Provide validated reference points for training and evaluating AI model performance [17] |
| Data Annotation Tools | Specialized labeling software, Clinical terminology standards, Structured annotation frameworks | Enable consistent, accurate labeling of training data with proper metadata capture [16] |
| Model Architecture Libraries | TensorFlow, PyTorch, Scikit-learn, MONAI | Provide standardized implementations of algorithms and neural network architectures [17] |
| Bias Detection Frameworks | AI Fairness 360, Fairlearn, Aequitas | Identify and quantify potential biases in training data and model outputs [18] |
| Performance Validation Suites | Model cards, Benchmarking datasets (e.g., MoleculeNet), Evaluation metrics | Standardize assessment of model performance, robustness, and generalizability [17] |
Transparency and Explainability Requirements
Transparency and explainability represent critical considerations for AI validation, particularly for models supporting high-stakes regulatory decisions.
The FDA emphasizes methodological transparency rather than mandating specific technical approaches to explainability [18]. The guidance acknowledges the challenges in interpreting complex AI models but stresses the importance of providing sufficient information to enable regulatory assessment of model reliability [18] [19]. For higher-risk applications, the FDA may expect more detailed information about how models reach their conclusions, potentially including approaches such as feature importance analyses or example-based explanations [21]. The agency also encourages the use of "model cards" or similar frameworks to communicate key model characteristics, performance metrics, and limitations in a standardized format [21].
The EMA places stronger explicit emphasis on explainability, particularly for models that directly influence clinical decisions [16]. The agency expects that AI systems should be "transparent and testable," with outputs that can be interpreted and understood by relevant experts [16]. This includes requirements for appropriate visualization of model outputs, clear documentation of limitations and appropriate use cases, and provision of information that helps users understand the basis for model predictions [16]. The EMA's reflection paper suggests that for certain high-risk applications, black-box models may be unacceptable without additional validation approaches to ensure interpretability [16].
Compliance Strategies and Implementation Frameworks
Pre-Submission Engagement and Regulatory Interaction
Early and strategic engagement with regulatory agencies represents a critical success factor for AI-based drug development programs.
The FDA strongly encourages early engagement through various mechanisms including Q-Submission meetings, INTERACT meetings, and model-informed drug development (MIDD) discussions [19] [20]. These interactions provide opportunities to align on the appropriateness of proposed credibility assessment activities, identify potential challenges, and establish expectations for the level of evidence needed to support the proposed context of use [19]. The FDA recommends discussing "whether, when, and where" to submit credibility assessment reports, recognizing that submission requirements may vary based on model risk and application type [19].
The EMA offers similar opportunities for early dialogue through its innovation task forces and scientific advice procedures [16]. These interactions are particularly valuable for novel AI methodologies without established regulatory precedents, allowing sponsors to obtain agency feedback on validation strategies and evidence requirements [16]. The EMA has also established specific procedures for qualifying novel drug development tools, including AI methodologies, which can provide regulatory certainty before significant investment in implementation [16].
Quality Management and Governance Structures
Robust quality management and governance structures provide the foundation for sustainable AI compliance throughout the product lifecycle.
The FDA's expectations align with existing quality system regulations, emphasizing design controls, documentation practices, and change management procedures [21]. The guidance suggests that AI model development should incorporate principles of Good Machine Learning Practice (GMLP), including representative data collection, human-centered design practices, and comprehensive performance evaluation [16]. Manufacturers should maintain detailed design history files documenting model development decisions, with particular attention to risk management activities addressing AI-specific hazards such as data drift, overfitting, and performance degradation in real-world settings [21].
The EMA emphasizes pharmaceutical quality systems that encompass AI tools used in manufacturing, quality control, and clinical development [16]. This includes established change management procedures, version control, and comprehensive documentation practices integrated with existing quality management systems [16]. The agency expects clear accountability structures and governance frameworks defining roles and responsibilities for AI system monitoring, maintenance, and decision-making throughout the product lifecycle [16].
AI Governance and Quality Management Framework: This diagram outlines the key components of a comprehensive governance structure for AI systems in drug development.
Lifecycle Management and Change Control
Effective lifecycle management ensures that AI models remain credible and fit-for-purpose as they evolve in response to new data and changing environments.
The FDA recommends detailed "lifecycle maintenance plans" that describe activities for monitoring model performance, detecting data drift or concept drift, and implementing appropriate retraining or recalibration procedures [18] [19]. These plans should be commensurate with the model's risk profile and complexity, with higher-risk applications warranting more rigorous monitoring and control mechanisms [19]. The FDA acknowledges the similarity between lifecycle maintenance plans and Predetermined Change Control Plans (PCCPs) established for AI-enabled medical devices, suggesting that sponsors may benefit from considering similar approaches for drug-related AI applications [19].
The EMA's approach to lifecycle management aligns with established procedures for post-authorization changes to medicinal products [16]. Significant modifications to AI models that impact their output or use in critical decision-making may require regulatory notification or approval depending on the potential impact on product quality, safety, or efficacy [16]. The agency expects robust version control, comprehensive documentation of model changes, and clear criteria for determining when model updates warrant additional validation or regulatory review [16].
The regulatory landscape for AI validation in drug development is rapidly evolving, with both the FDA and EMA establishing structured frameworks to ensure the credibility and reliability of AI tools supporting critical decisions. While differences exist in their specific approaches and emphasis, both agencies share common foundational principles centered on risk-based assessment, comprehensive validation, and lifecycle management.
For researchers, scientists, and drug development professionals, successful navigation of this landscape requires a proactive, strategic approach that integrates regulatory considerations throughout the AI development process. Key success factors include:
- Early and Continuous Engagement: Regular dialogue with regulatory agencies to align on validation strategies and evidence requirements [19] [20]
- Risk-Proportionate Validation: Tailoring validation activities to the model's potential impact on patient safety and product quality [18] [16]
- Comprehensive Documentation: Maintaining detailed records of model development, validation, and performance monitoring [18] [16]
- Robust Governance: Implementing clear accountability structures and quality management systems for AI lifecycle management [16] [21]
- Strategic Intellectual Property Management: Balancing patent protection with regulatory transparency requirements, particularly for innovative AI methodologies [18]
As both agencies continue to refine their approaches based on accumulating experience with AI applications, drug development professionals should anticipate increasing regulatory specificity and potentially greater convergence between FDA and EMA expectations. By establishing strong foundations in current requirements while maintaining flexibility for future evolution, organizations can position themselves to leverage AI technologies effectively while ensuring compliance and maintaining patient safety as their highest priority.
The Critical Role of High-Quality, Diverse, and Unbiased Training Data
The adoption of Artificial Intelligence (AI) represents a paradigm shift in pharmaceutical research, offering the potential to dramatically accelerate timelines and reduce the immense costs traditionally associated with bringing a new drug to market. AI-driven drug discovery can span over a decade and cost more than $2 billion, with nearly 90% of drug candidates failing due to insufficient efficacy or safety concerns [22]. However, the performance and reliability of these AI models are fundamentally constrained by the quality of their training data. Models trained on biased, sparse, or noisy data can produce unrealistic molecular outputs or inaccurate target predictions, ultimately undermining the drug discovery process and wasting valuable resources [23] [24]. This guide objectively compares the performance of AI models built on different data foundations and details the experimental protocols necessary for their rigorous validation, framing this examination within the broader thesis that data quality is the most critical determinant of success in AI-based drug discovery.
The Centrality of Data Quality in AI Model Performance
Defining Data Quality in a Biological Context
In AI-driven drug discovery, "data quality" encompasses several interdependent characteristics: completeness, diversity, standardization, and accuracy. High-quality data must be generated under controlled, reproducible conditions to minimize experimental noise and technical artifacts that can mislead AI models [25]. Furthermore, the data must be representative of the broad biological and chemical space to which the model will be applied; this includes diversity in cell types, protein families, disease mechanisms, and patient populations to ensure model generalizability and mitigate bias [24].
Performance Comparison: High-Quality vs. Conventional Datasets
The table below summarizes a comparative analysis of AI model performance when trained on high-quality, fit-for-purpose datasets versus conventional public data sources.
Table 1: Performance Comparison of AI Models on Different Data Types
| Performance Metric | Models Trained on High-Quality, Standardized Data | Models Trained on Conventional Public Datasets |
|---|---|---|
| Target Identification Accuracy | Improved identification of novel, druggable targets with stronger genetic evidence [24] [22]. | Higher risk of false positives and focus on well-established protein families (e.g., kinases, GPCRs) [24]. |
| Molecular Generation Success | Generation of novel molecules with optimized, balanced profiles for efficacy, safety, and synthesizability [23]. | Generation of molecules that may be invalid, difficult to synthesize, or have unfavorable ADMET properties [23]. |
| Generalizability | Higher likelihood of performance across diverse biological contexts and patient populations [25]. | Performance may be brittle and limited to specific biological contexts represented in the training data [24]. |
| Clinical Translation | AI-discovered drugs reported to have an 80-90% success rate in Phase I trials [22]. | Traditionally discovered drugs have a 40-65% success rate in Phase I trials [22]. |
| Representative Dataset | Recursion's RxRx3-core (standardized HUVEC cell microscopy) [25]. | Public datasets like GenBank, ChEMBL, PubMed [25]. |
Experimental Benchmarking for Data and Model Validation
Core Principles of Experimental Benchmarking
Experimental benchmarking is a critical methodology for validating AI models, wherein the predictions of a non-experimental (in silico) model are compared against results from controlled laboratory experiments (the gold standard) [26]. This process allows researchers to calibrate the bias and quantify the accuracy of their AI-driven approaches. The most instructive benchmarking studies are conducted on a large scale and compare in silico and experimental work that investigates the same outcome in the same biological context [26].
Protocol for Benchmarking an AI Target Identification Model
This protocol provides a framework for validating an AI model designed to discover novel disease-associated protein targets.
Step 1: Model Training and Initial Prediction. Train the AI model on a curated dataset integrating multiomics data (e.g., genomics, proteomics), biomedical literature, and protein structure information. Use the trained model to generate a ranked list of high-confidence, novel protein targets predicted to be involved in a specific disease pathway [24] [22].
Step 2: In Silico Cross-Validation. Perform internal validation using computational methods. This includes:
- Genetic Evidence Check: Use resources like genome-wide association studies (GWAS) to assess if the predicted targets have prior genetic support. The presence of genetic evidence can increase the odds of a target succeeding in clinical trials by 80% [24].
- Druggability Prediction: Employ structure-based models (e.g., docking simulations) to predict whether the protein has a viable binding pocket for a small molecule [24].
- Pathway Analysis: Ensure the target is placed in a biologically plausible disease pathway [24].
Step 3: Experimental Validation in the Wet Lab. The top-ranked predictions from the in silico phase must be tested empirically. A key approach is target deconvolution using CRISPR-Cas9 gene editing [24] [25].
- Cell Culture: Use a relevant human cell line (e.g., HUVEC cells as used in the RxRx3 dataset) for the disease context [25].
- Genetic Perturbation: Perform CRISPR-Cas9 knockouts of the AI-predicted target genes.
- Phenotypic Screening: Use high-content microscopy and automated assays to capture the cellular phenotypes resulting from the gene knockouts.
- Outcome Measurement: Compare the observed phenotypes against known disease-associated phenotypes. A successful prediction is one where the knockout produces a phenotypic change that ameliorates the disease model phenotype [25].
Step 4: Bias and Performance Calibration. Compare the experimental results with the AI model's original predictions. Calculate metrics such as the false discovery rate (FDR) and precision to quantify the model's performance and calibrate its bias for future iterations [26]. This step closes the loop, informing refinements to both the AI model and the training data strategy.
The following workflow diagrams the complete benchmarking process, from data integration to model refinement.
Successful experimental benchmarking relies on a suite of specific research reagents and computational tools. The table below details key solutions for the validation workflow described above.
Table 2: Key Research Reagent Solutions for Experimental Validation
| Reagent / Resource | Function in Validation | Application Example |
|---|---|---|
| CRISPR-Cas9 Gene Editing Systems | Precisely knocks out AI-predicted target genes in cell lines to study functional loss [24] [25]. | Validating the essentiality of a novel protein target by observing the phenotypic consequence of its knockout [25]. |
| High-Content Screening (HCS) Microscopy | Automatically captures high-resolution images of perturbed cells, generating rich, quantitative phenotypic data [25]. | Generating datasets like RxRx3-core to train and benchmark AI models on cellular morphology changes [25]. |
| Curated Public Datasets (e.g., RxRx3-core) | Provides standardized, high-quality public benchmarks for training and testing microscopy-based AI models [25]. | Serving as a compact, accessible benchmark (18GB) for evaluating zero-shot drug-target interaction prediction [25]. |
| Protein Structure Prediction Models (e.g., AlphaFold) | Provides high-quality 3D protein structures for targets where lab-resolved structures are unavailable, enabling structure-based drug design [24] [22]. | Predicting binding pockets and performing molecular docking simulations on novel AI-prioritized targets [22]. |
| Pharmacogenomic Databases (e.g., UK Biobank, TCGA) | Provides large-scale genetic and clinical data to uncover correlations between targets and disease, strengthening genetic evidence [24] [25]. | Assessing if a novel AI-predicted target has links to disease in human population data, bolstering validation confidence [24]. |
The transformative potential of AI in drug discovery is inextricably linked to the quality, diversity, and lack of bias in its underlying training data. As demonstrated through performance comparisons and experimental benchmarking protocols, models built on fit-for-purpose, standardized data consistently outperform those reliant on noisy or limited public datasets. The transition from a model-centric to a data-centric AI approach is therefore critical. This entails investing in the generation of high-quality, multimodal data, rigorously validating model outputs against biological experiments, and actively addressing data biases. By prioritizing the integrity of the data foundation, researchers can fully leverage AI to illuminate novel biological mechanisms, design safer and more effective therapeutics, and ultimately accelerate the delivery of new medicines to patients.
The integration of Artificial Intelligence (AI) into drug discovery has ushered in a new era of potential, promising to accelerate target identification, compound screening, and optimization of therapeutic candidates. However, the inherent opacity of many sophisticated AI models, particularly deep learning systems, poses a significant "black box" problem that limits their interpretability and acceptance within the pharmaceutical research community [27]. In high-stakes, regulated environments like drug development, a perfect prediction means little if the reasoning behind it remains unclear [28]. Explainable AI (XAI) has therefore emerged as a critical field, aiming to bridge the gap between powerful AI predictions and the human-understandable rationale needed for scientific validation, trust, and regulatory acceptance [27] [29].
The challenge extends beyond mere technical performance. In highly regulated environments such as submissions to the FDA or EMA, explainability is not a "nice to have" but a prerequisite for acceptance [28]. Regulatory agencies expect AI-driven decisions to be transparent, auditable, and scientifically justified. When a model flags a compound as high-risk, reviewers must understand the reasoning in terms they recognize—such as mechanism of action, toxicity pathways, or target interactions—not just a probability score [28]. This review will objectively compare the performance and methodologies of various XAI approaches, framing the discussion within the broader thesis of validating AI-based drug discovery models.
Core Concepts: From Black Boxes to Glass Box Models
In AI-driven drug discovery, not all models are created equal when it comes to transparency. The fundamental distinction lies between "black box" and "glass box" (Explainable AI) models.
Traditional "Black Box" Models: These models, which can include complex deep neural networks and ensemble methods, can achieve outstanding predictive accuracy. However, their internal decision-making process is hidden from the user [28]. They deliver outputs without showing the reasoning behind them, much like receiving a lab result with no explanation of the methodology used to obtain it. This lack of transparency creates significant barriers to their adoption in scientific and regulated environments.
Explainable AI (XAI) Models: These are built with methods that make their inner workings more transparent and can explain why a specific prediction or recommendation was made [28]. XAI helps scientists validate results, detect potential biases, and build trust in the system. The overarching goal of XAI is aligned with the RICE principles—Robustness, Interpretability, Controllability, and Ethicality—which are increasingly seen as foundational for responsible AI in healthcare [30].
Table 1: Core Objectives of AI Alignment (RICE) in Drug Discovery
| Objective | Description | Significance in Drug Discovery |
|---|---|---|
| Robustness | The capacity of an AI system to maintain stability and dependability amid uncertainties or adversarial attacks [30]. | Ensures model reliability across diverse chemical spaces and biological contexts. |
| Interpretability | The ability to provide clear explanations or reasoning for decisions, facilitating user comprehension [30]. | Enables scientists to validate predictions against domain knowledge and generate testable hypotheses. |
| Controllability | The ability to guide and constrain model behavior to align with human intentions. | Prevents the generation of unsafe or non-synthesizable compounds. |
| Ethicality | Ensuring model decisions are fair, unbiased, and respect human values and well-being. | Mitigates biases in data or algorithms that could lead to unfair treatment outcomes or skewed research [30]. |
Comparative Analysis of XAI Techniques and Model Performance
A variety of XAI techniques have been developed to address the black box problem, each with distinct methodologies, applications, and performance characteristics. The following table summarizes prominent approaches and their experimental performance in benchmark drug discovery tasks.
Table 2: Performance Comparison of Explainable AI Techniques on Molecular Property Prediction
| XAI Technique | Model Category | Key Methodology | Reported Performance (AUC/Accuracy) | Primary Application in Drug Discovery |
|---|---|---|---|---|
| Concept Whitening (CW) on GNNs [31] | Self-Interpretable | Aligns latent space axes with human-defined concepts (e.g., molecular descriptors) to identify relevant structural parts. | Classification Performance Improvement on MoleculeNet datasets [31]. | Molecular property prediction, QSAR models. |
| SHapley Additive exPlanations (SHAP) [28] [27] | Post-hoc Model-Agnostic | Uses cooperative game theory to quantify each feature's marginal contribution to a prediction. | N/A (Feature importance quantification) | Biomarker prioritization, patient stratification, ADMET prediction. |
| Local Interpretable Model-agnostic Explanations (LIME) [27] | Post-hoc Model-Agnostic | Approximates a black-box model locally with an interpretable model (e.g., linear classifier) to explain individual predictions. | N/A (Local explanation fidelity) | Explaining individual compound predictions for chemists. |
Experimental Protocol for Evaluating Self-Interpretable GNNs with Concept Whitening
The adaptation of Concept Whitening (CW) for Graph Neural Networks (GNNs) represents a move towards inherently interpretable models, rather than applying explanations post-hoc. The detailed experimental methodology, as outlined in research, is as follows [31]:
- Dataset and Benchmarking: Models are trained and evaluated on several public benchmark datasets from MoleculeNet (e.g., for toxicity or hydrophobicity prediction). This provides a standardized ground for comparison.
- Model Architecture and Training:
- Base GNNs: Popular spatial convolutional GNN architectures are used as the backbone, including Graph Convolutional Networks (GCNs), Graph Attention Networks (GATs), and Graph Isomorphism Networks (GINs).
- Integration of CW: The CW module is added to the network. This module is designed to align the axes of the network's latent space with pre-defined molecular concepts (e.g., molecular weight, polarity, or presence of specific functional groups).
- Training Objective: The model is trained not only to correctly predict the molecular property but also to organize its internal representations according to the supplied concepts.
- Interpretation and Evaluation:
- Concept Importance: For a given prediction, the model can identify which concepts were most influential.
- Substructure Identification: Using post-hoc methods like GNNExplainer on the concept activations, the model can highlight the specific structural parts of the molecule (substructures) that are associated with an active concept, providing a direct link between the concept and the chemistry.
- Performance Metrics: Standard metrics like Area Under the Curve (AUC) and Accuracy are used to evaluate predictive performance, while interpretability is assessed qualitatively and through the coherence of the concept-based explanations.
Diagram 1: CW-GNN experimental workflow.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing and evaluating XAI models requires a suite of computational tools and data resources. The following table details key components essential for research in this field.
Table 3: Essential Research Reagents and Tools for XAI in Drug Discovery
| Item Name | Type | Function/Benefit | Example Use Case |
|---|---|---|---|
| MoleculeNet [31] | Benchmark Dataset Collection | Provides standardized public datasets for fair comparison of model performance on molecular property prediction tasks. | Benchmarking GNN and CW-GNN models on toxicity (Tox21) or solubility datasets. |
| Graph Neural Network (GNN) Architectures (GCN, GAT, GIN) [31] | Computational Model | Core deep learning models for directly processing molecular graph structures without requiring other machine-readable formats. | Base model for molecular property prediction; backbone for adding CW modules. |
| SHAP/LIME Libraries [28] [27] | Post-hoc Explanation Software | Model-agnostic libraries to explain output of any ML model by quantifying feature importance (SHAP) or local approximations (LIME). | Explaining predictions of a black-box model for lead compound prioritization. |
| GNNExplainer [31] | Instance-Level Explanation Tool | A post-hoc method for identifying subgraph structures and node features that are most important for a GNN's prediction on a given graph. | Identifying which molecular substructure contributed most to a predicted toxicity. |
| Pre-defined Molecular Concepts/Descriptors [31] | Interpretability Basis | Human-understandable chemical properties (e.g., logP, polar surface area) used to align and interpret the model's latent space in Concept Whitening. | Serving as the concepts for a CW-GNN model to link predictions to known chemistry. |
The journey from opaque "black box" models to transparent, explainable AI is critical for the full integration of AI into the drug discovery pipeline. While complex models can offer high predictive accuracy, this review demonstrates that this performance must be balanced with interpretability to build trust among researchers, satisfy regulatory requirements, and ultimately generate scientifically valid and actionable insights [28] [27]. Techniques like Concept Whitening for GNNs show that it is possible to design models that are both high-performing and self-interpretable, moving beyond post-hoc explanations to inherently transparent architectures [31].
The future of validated AI in drug discovery lies in the continued development and adoption of models that adhere to the RICE principles—Robustness, Interpretability, Controllability, and Ethicality [30]. By embracing explainability, researchers can transform AI from an inscrutable black box into a reliable, collaborative partner that augments human expertise, accelerates the development of new therapies, and builds a foundation of trust essential for scientific and clinical advancement.
From Theory to Therapy: Methodologies and Real-World Applications of AI Model Validation
The integration of artificial intelligence (AI) into pharmaceutical research represents a paradigm shift, promising to compress traditional drug discovery timelines from a decade or more to just a few years [32]. However, the acceleration of early-stage research is meaningless without robust validation frameworks to ensure the clinical viability of AI-derived candidates. This guide provides a comparative analysis of the validation approaches employed by three leading AI-driven drug discovery companies—Exscientia, Insilico Medicine, and Recursion. By examining their experimental protocols, performance benchmarks, and clinical progress, we aim to establish a clear understanding of how these platforms demonstrate the reliability and translational potential of their outputs. The validation of AI models in drug discovery extends beyond computational accuracy; it requires a holistic framework encompassing biological fidelity, chemical synthesizability, and ultimately, clinical efficacy [33] [34].
Comparative Analysis of Platform Performance and Validation Benchmarks
The following tables synthesize key performance metrics and validation approaches across the three platforms, providing a direct comparison of their efficiency, clinical progress, and technological capabilities.
Table 1: Key Performance Benchmarks and Clinical Pipeline (2021-2025)
| Metric | Exscientia | Insilico Medicine | Recursion |
|---|---|---|---|
| Reported Timeline Reduction | Early design efforts accelerated by ~70% [32] | Preclinical candidate in 9-18 months (vs. traditional 2.5-4 years) [35] | Significant improvements in speed from hit ID to IND-enabling studies [36] |
| Reported Cost Efficiency | ~80% reduction in upfront capital cost [32] | Preclinical candidate at a fraction of cost (~$2.6M) [32] | Improved cost efficiency vs. traditional pharma averages [36] |
| Synthesis Efficiency | 10x fewer compounds synthesized than industry average [37] | ~70-115 molecules synthesized per program to Developmental Candidate (DC) [35] | Data generated from millions of weekly cell experiments [36] |
| Clinical-Stage Pipeline | 6+ molecules in clinical trials as of 2024 [37] | 10 programs in clinical trials, 4 Phase I studies completed, 1 Phase IIa completed [35] | 5+ clinical-stage programs in oncology and rare diseases [38] [36] |
| Key Validation Milestone | CDK7 inhibitor candidate from 136 synthesized compounds [1] | 100% success rate from DC to IND-enabling stage (excluding strategic stops) [35] | Multiple programs in Phase 2/3 trials (e.g., REC-994, REC-2282) [38] |
Table 2: Core Technology and Validation Methodologies
| Aspect | Exscientia | Insilico Medicine | Recursion |
|---|---|---|---|
| Core AI Approach | Generative AI for precision molecular design; "Centaur Chemist" model [1] | End-to-end generative AI (Biology, Chemistry, Medicine); Generative Tensorial Reinforcement Learning (GENTRL) [35] [33] | Phenomics-based; maps biology using cellular images and multi-omics data [38] [36] |
| Target Identification | Patient-derived biology and high-content phenotypic screening (via Allcyte) [1] | TargetPro: Disease-specific models integrating 22 multi-modal data sources [39] | Phenotypic screening with automated target deconvolution via knowledge graphs [38] [33] |
| Candidate Design | AI generates structures meeting Target Product Profiles (TPPs) for potency, selectivity, ADME [37] | Chemistry42: Generative AI for novel molecule design optimized for multi-objective parameters [33] | AI designs molecules based on insights from phenomic maps; MolGPS model for property prediction [38] [33] |
| Experimental Validation Workflow | Closed-loop "Design-Make-Test-Learn" (DMTL) integrated with automated robotics [37] | Integrated AI and automation; synthesis and testing of 60-200 molecules per program [35] [39] | Automated wet lab with robotics and computer vision; continuous feedback into Recursion OS [36] |
Company-Specific Validation Approaches and Experimental Protocols
Exscientia: Precision Design and Patient-Centric Validation
Exscientia's validation strategy is built on a closed-loop "Design-Make-Test-Learn" (DMTL) cycle, which integrates precision AI design with automated experimental validation [37]. A key differentiator is its use of patient-derived biology for functional validation early in the process.
Detailed Experimental Protocol:
- Target Product Profile (TPP) Definition: Working backward from patient needs, Exscientia first defines a precise TPP specifying the required combination of properties for a safe and effective medicine, including potency, selectivity, and ADME parameters [37].
- Generative Molecular Design: Deep learning models, trained on vast chemical and pharmacological datasets, generate panels of novel molecular structures predicted to satisfy the TPP [1] [37].
- Patient-Centric In Vitro Validation: A critical step involves screening AI-designed compounds on patient-derived tissue samples, a capability enhanced by the acquisition of Allcyte. This high-content phenotypic screening assesses compound efficacy in ex vivo disease models, improving translational relevance before candidate selection [1].
- Automated Synthesis & Testing: Selected candidate molecules are synthesized and tested using an automated robotics lab ("AutomationStudio") orchestrated by cloud microservices. This automation enables 24/7 operation and rapid data generation [37].
- Iterative Learning: Data from synthesis and biological testing are fed back into the AI models, refining subsequent design cycles and promoting the creation of synthesizable compounds with optimized properties [37].
This approach was validated in a CDK7 inhibitor program, where a clinical candidate was identified after synthesizing only 136 compounds, a small fraction of the thousands typically required in traditional drug discovery [1].
Insilico Medicine: End-to-End AI and Rigorous Benchmarking
Insilico Medicine employs an end-to-end generative AI platform, Pharma.AI, and emphasizes rigorous, transparent benchmarking of its performance. Its validation is notable for its disease-specific AI models and public benchmarking of target identification accuracy [39].
Detailed Experimental Protocol:
- Target Identification with TargetPro: The process begins with TargetPro, a machine learning workflow that integrates 22 multi-modal data sources (genomics, proteomics, clinical trials, literature) to identify novel therapeutic targets. The model is trained on clinical-stage targets across 38 diseases, learning disease-specific biological patterns [39].
- Benchmarking with TargetBench 1.0: TargetPro's performance is rigorously evaluated using Insilico's proprietary TargetBench 1.0 system. This framework benchmarks its retrieval rate of known clinical targets against other models, such as LLMs (GPT-4o, Claude-Opus) and public platforms (Open Targets). TargetPro demonstrated a 71.6% retrieval rate, a 2-3x improvement over alternatives [39].
- Generative Molecular Design with Chemistry42: For a selected target, the Chemistry42 module uses deep learning (including GANs and reinforcement learning) to generate novel drug-like molecules. The system performs multi-objective optimization, balancing parameters like binding affinity, metabolic stability, and bioavailability [33].
- Experimental Validation and DC Nomination: The top AI-generated molecules are synthesized and tested. The standard Developmental Candidate (DC) package includes:
- Biochemical Assays: Enzymatic assays to demonstrate binding affinity and cellular functional assays for target engagement [35].
- ADME-Tox Profiling: In vitro ADME, microsomal stability, and non-GLP toxicity studies across multiple species [35].
- In Vivo Efficacy: Mouse/rat/dog pharmacokinetic (PK) studies and in vivo efficacy studies with PK/PD analysis to identify efficacious dose ranges [35].
- The company's benchmark is an average of 13 months and ~70 synthesized molecules to nominate a DC, with a 100% success rate in advancing these candidates to the IND-enabling stage (excluding strategic discontinuations) [35].
Recursion: Phenomic Mapping and Scalable Biology
Recursion's validation philosophy is rooted in "decoding biology" through massive-scale, unbiased phenotypic screening. Its Recursion Operating System (Recursion OS) maps trillions of biological relationships to identify and validate drug candidates [38] [36].
Detailed Experimental Protocol:
- Phenotypic Perturbation and Imaging: Recursion perturbs human cells (e.g., with CRISPR or small molecules) and uses high-content microscopy to capture millions of cellular images weekly [36].
- Feature Extraction and Digitization: Computer vision and AI models (like the Phenom-2 model) analyze these images to extract high-dimensional feature vectors, converting complex biology into quantifiable, searchable data. This creates a digital "map" of cellular health and disease [38] [33].
- Target Deconvolution and Insight Generation: When a compound shows a beneficial phenotypic signature, Recursion's knowledge graph and AI tools (e.g., MolPhenix) perform target deconvolution to identify the molecular target responsible for the observed effect [38] [33].
- In Silico Predictions: Specialized models predict subsequent properties. MolGPS predicts molecular properties and ADMET profiles, while MolE excels in molecular representation learning [33].
- Integrated Validation Loop: Predictions and insights are validated in the automated wet lab, creating a continuous feedback loop. The platform learns from every experiment, refining its biological models [36]. This workflow is supported by BioHive-2, one of the most powerful supercomputers in biopharma, which processes over 65 petabytes of proprietary data [36].
Visualizing Workflows and Research Toolkit
Workflow Diagrams
The following diagrams illustrate the core validation workflows employed by Exscientia and Insilico Medicine, highlighting their iterative and data-driven nature.
Diagram 1: Exscientia's iterative validation cycle integrates AI design with automated labs.
Diagram 2: Insilico Medicine's workflow emphasizes target validation and benchmarking.
The Scientist's Toolkit: Key Research Reagents and Solutions
The following table details essential reagents, tools, and technologies used by these platforms for experimental validation, providing a resource for scientists seeking to implement similar approaches.
Table 3: Key Research Reagent Solutions for AI Drug Discovery Validation
| Reagent / Technology | Function in Validation | Platform Context |
|---|---|---|
| Arrayed CRISPR Libraries | Used for precise genetic perturbation in human cell lines to simulate disease states and identify novel targets. | Recursion uses this to create systematic biological perturbations for its phenomic maps [38]. |
| High-Content Microscopy & Computer Vision | Captures millions of cellular images; software extracts quantitative features describing cell state and morphology. | Core to Recursion's platform for converting biology into searchable, high-dimensional data [38] [36]. |
| Patient-Derived Tissue Samples | Provides biologically relevant, human-specific context for ex vivo efficacy and safety testing of candidate compounds. | Exscientia uses these, via its Allcyte platform, for high-content phenotypic screening on patient tumor samples [1]. |
| Automated Robotics & Liquid Handlers | Enables high-throughput, reproducible synthesis of compounds and execution of biological assays with minimal human error. | Integral to Exscientia's "AutomationStudio" and Recursion's automated wet lab for 24/7 operations [37] [36]. |
| Multi-Omics Datasets (Genomics, Transcriptomics, Proteomics) | Provides the foundational biological data for training and validating AI models for target identification and disease understanding. | Insilico's TargetPro integrates 22 such data sources; Recursion uses them to augment its phenomic data [39] [33]. |
| Cloud Computing & AI Infrastructure (e.g., NVIDIA DGX/BioHive, AWS) | Provides the massive computational power required for training large AI models, running simulations, and managing petabytes of data. | Recursion's BioHive-2 supercomputer; Exscientia's platform is built on AWS [37] [36]. |
| Standardized Assay Kits (ADME, Toxicity, Binding Affinity) | Provides reproducible, off-the-shelf methods for profiling key pharmaceutical properties of candidate molecules. | Part of the standardized "DC package" at Insilico Medicine and the automated workflows at Exscientia [35] [37]. |
The validation of AI-driven drug discovery platforms hinges on a transparent, multi-faceted approach that integrates robust computational design with rigorous and scalable experimental testing. Exscientia, Insilico Medicine, and Recursion have each developed distinct yet complementary strategies: Exscientia excels in precision design and patient-centric validation loops, Insilico Medicine has established new standards for end-to-end AI and benchmarking transparency, and Recursion leverages unparalleled scale in phenotypic screening to decode biology. While their technological foundations differ, their shared commitment to closing the loop between in silico predictions and empirical data is what ultimately de-risks the drug discovery process. The ongoing clinical progress from these companies will serve as the ultimate validator of their respective approaches, potentially ushering in a new era of efficient and effective therapeutic development.
The integration of artificial intelligence (AI) into drug discovery represents a paradigm shift, moving beyond traditional trial-and-error approaches toward a more predictive and efficient model [40] [41]. Generative AI for de novo molecular design stands at the forefront of this transformation, enabling the creation of novel, optimized drug candidates from scratch by learning from vast chemical and biological datasets [42] [43]. These technologies promise to overcome the critical bottleneck of confined chemical space, where traditional discovery efforts often concentrate on similar regions, limiting molecular novelty and therapeutic potential [44]. However, the promise of accelerated discovery brings forth the critical challenge of robust validation, ensuring that AI-generated molecules are not only computationally elegant but also therapeutically relevant, synthetically accessible, and safe [45].
This case study is situated within the broader thesis that the validation of AI-based drug discovery models requires a multi-faceted framework integrating diverse tools and methodologies. The path from a computational design to a viable clinical candidate is fraught with obstacles, and the true measure of a generative AI platform lies in its consistent performance across the entire pipeline [42]. This analysis objectively compares leading software solutions, dissects their underlying experimental protocols, and provides a toolkit for researchers to critically evaluate and implement these transformative technologies in their drug development campaigns.
Comparative Analysis of Leading AI-Driven Discovery Platforms
A practical validation of generative AI tools requires a direct comparison of their stated capabilities, performance metrics, and operational characteristics. The following analysis benchmarks leading platforms based on key criteria critical for successful de novo design and optimization, drawing from published data and performance claims.
Table 1: Platform Comparison for de Novo Design and Optimization
| Platform/ Tool | Primary Function | Key AI Capabilities | Reported Performance & Advantages | Licensing & Cost |
|---|---|---|---|---|
| DeepMirror | Augmented Hit-to-Lead & Lead Optimization | Generative AI Engine, Foundational models, Protein-drug binding prediction | Speeds up discovery by up to 6x; Reduces ADMET liabilities [40]. | Single package, no hidden fees [40]. |
| Schrödinger | Quantum Mechanics & Free Energy Calculations | DeepAutoQSAR, GlideScore, Physics-based modeling | Collaboration with Google Cloud to simulate billions of compounds weekly [40]. | Modular licensing model; Tends to be higher cost [40]. |
| ChatChemTS | LLM-Powered Molecule Generation | LLM (GPT-4) interface for AI-based generator (ChemTSv2), Automated reward function design | Open-source; Accessible to non-AI experts; Demonstrated in chromophore & EGFR inhibitor design [46]. | Open-source (GitHub) [46]. |
| Cresset (Flare V8) | Protein-Ligand Modeling | Free Energy Perturbation (FEP), MM/GBSA | FEP enhancements for real-life drug discovery projects with ligands of different net charges [40]. | Information Missing |
| Optibrium (StarDrop) | AI-Guided Lead Optimization | Patented rule induction, Sensitivity analysis, QSAR models | Comprehensive data analysis & visualization; Integrates with Cerella deep learning platform [40]. | Modular pricing model [40]. |
| Chemaxon | Enterprise Chemical Intelligence | Plexus Suite for data analysis, Design Hub for compound tracking | Chemistry-aware platform for hypothesis-driven design; Pay-per-use model [40]. | Mostly pay-per-use [40]. |
The selection of an appropriate platform often involves trade-offs between depth of physical modeling, as seen in Schrödinger's quantum mechanical approaches, and speed and accessibility, offered by platforms like DeepMirror and the open-source ChatChemTS [40] [46]. Tools like Cresset's Flare provide critical advantages for specific tasks like accurately calculating protein-ligand binding free energies, a cornerstone of structure-based design [40]. Ultimately, the choice depends on the specific research objectives, available expertise, and budgetary constraints.
Experimental Protocols for Validating AI-Generated Molecules
Validating generative AI output requires a structured cycle of design, synthesis, and testing. The following protocols detail key experimental methodologies cited in benchmark studies, providing a blueprint for empirical validation.
Protocol: Multi-ObjectiveDe NovoDesign for Kinase Inhibitors
This protocol is adapted from the validation case study of ChatChemTS for designing Epidermal Growth Factor Receptor (EGFR) inhibitors, a therapeutically relevant target in oncology [46].
- 1. Objective Definition: The primary objective is a multi-optimization task to generate novel molecules with high inhibitory activity (pChEMBL value) against EGFR and high drug-likeness scores.
- 2. Data Curation: A dataset of known EGFR inhibitors is programmatically retrieved from the ChEMBL database using the target's UniProt ID (P00533). The data is pre-processed by deduplicating molecules (retaining the maximum pChEMBL value), filtering for specific assay types ('Binding'), and removing records associated with mutant or covalent binding mechanisms [46].
- 3. Predictive Model Building: A machine learning model is trained to predict the pChEMBL value (a measure of potency) from molecular structure. The ChatChemTS platform employs an AutoML process with a defined test dataset ratio and budget to automatically select and train the best-performing model [46].
- 4. Reward Function & Configuration: A reward function is constructed via natural language chat to balance the objectives. For example:
Reward = [Predicted pChEMBL value] + [Drug-likeness score]. Key parameters for the ChemTSv2 generator are set, such as the exploration parameterc(e.g., 0.1 for focused optimization) and a synthetic accessibility score (SAScore) filter [46]. - 5. Molecule Generation & Analysis: The AI generator is executed, producing thousands of candidate molecules. The results are analyzed for Pareto optimality, identifying molecules that best balance the multiple objectives. The optimization trajectory and chemical diversity of the generated library are assessed [46].
Protocol: Free Energy Perturbation (FEP) for Binding Affinity Prediction
This protocol is based on the application of advanced physics-based models, such as those implemented in Cresset's Flare and Schrödinger's platforms, to validate and optimize AI-generated lead molecules [40].
- 1. System Preparation: A high-resolution crystal structure of the protein target is prepared. A series of congeneric ligands (e.g., an initial hit and AI-generated analogs) are selected to form a "FEP map," defining the alchemical transformation paths between them.
- 2. Topology Generation: The force field parameters and partial atomic charges for each ligand are calculated using high-level quantum mechanical methods.
- 3. FEP Simulation Setup: Each perturbation (e.g., changing a -CH~3~ group to -OCH~3~) is set up as a separate simulation window. The ligand is alchemically "morphed" from one state to another in a series of small steps (λ values) within the solvated protein binding site.
- 4. Molecular Dynamics (MD) Sampling: At each λ window, extensive MD sampling is performed to adequately sample the conformational space and collect statistics on the energy differences.
- 5. Data Analysis & Binding Affinity Calculation: The free energy change (ΔΔG) for each perturbation is calculated by combining the results from all windows using methods like the Multistate Bennett Acceptance Ratio (MBAR). The predicted ΔΔG is directly related to the relative binding affinity (ΔΔG = -RT ln(K~d,new~/K~d,ref~)) [40].
This protocol provides a rigorous, physics-based validation of the AI's structural hypotheses, ensuring that proposed modifications indeed improve binding affinity before committing to costly synthesis.
The workflow for a comprehensive AI validation cycle, integrating the protocols above, is visualized below.
AI Validation Workflow
This diagram illustrates the iterative "Design-Make-Test-Analyze" (DMTA) cycle, central to modern AI-driven discovery. The AI generates structures, which are validated computationally (e.g., via FEP) before synthesis and experimental testing. The resulting data feeds back to refine the AI models, creating a continuous learning loop [42] [45].
The Scientist's Toolkit: Essential Research Reagents and Solutions
The experimental validation of generative AI output relies on a suite of computational and experimental tools. The following table catalogues key resources essential for conducting the validation protocols described in this case study.
Table 2: Key Research Reagents and Solutions for AI Model Validation
| Category | Specific Tool / Resource | Function in Validation | Relevance to AI Workflow |
|---|---|---|---|
| Generative AI Platforms | DeepMirror, ChatChemTS, Schrödinger | De novo molecule generation and initial property prediction. | Core engine for creating novel molecular structures based on desired properties [40] [46]. |
| Cheminformatics & Data | ChEMBL, PubChem, ZINC15 | Source of bioactivity and compound data for model training and benchmarking. | Provides the foundational data for training AI models and contextualizing generated molecules [46] [41]. |
| Predictive Modeling | AutoML (e.g., via FLAML), QSAR Models, DeepAutoQSAR | Building custom predictive models for activity, ADMET, and physicochemical properties. | Translates molecular structures into predicted biological outcomes for virtual screening [40] [46]. |
| Physics-Based Simulation | FEP (e.g., in Flare, Schrödinger), MM/GBSA, Molecular Docking | Calculating binding affinities and understanding protein-ligand interactions at an atomic level. | Provides high-fidelity, rigorous validation of AI-generated molecules before synthesis [40]. |
| Synthetic Feasibility | Retrosynthesis Tools, SAScore, LHASA | Predicting the synthetic tractability of proposed molecules. | Critical for assessing the practical realizability of AI designs and avoiding impractical structures [44] [45]. |
| Experimental Assays | HTS, Binding Assays, ADMET in vitro panels | Empirical measurement of compound activity, selectivity, and pharmacokinetic properties. | The ultimate ground-truth validation, closing the DMTA loop and generating data for AI model refinement [42] [45]. |
This toolkit underscores that AI validation is not a single-step process but a pipeline integrating specialized resources. The synergy between generative AI, predictive modeling, high-fidelity simulation, and robust experimental testing is what ultimately builds confidence in AI-generated molecules and accelerates their path to the clinic.
This case study demonstrates that validating generative AI for de novo molecular design is a multi-dimensional challenge, requiring evidence from computational benchmarks, physics-based simulations, and experimental assays. The comparative analysis reveals a diverse ecosystem of platforms, each with distinct strengths, from the foundational models of DeepMirror to the accessible LLM-interface of ChatChemTS and the rigorous physical calculations of Schrödinger and Cresset [40] [46]. The detailed experimental protocols for multi-objective optimization and FEP calculations provide a reproducible framework for researchers to critically assess AI-generated candidates. Finally, the curated scientist's toolkit emphasizes that successful integration of AI into the drug discovery workflow depends on a suite of complementary technologies. As the field evolves, the focus must remain on developing and adhering to robust, transparent validation standards to fully realize the potential of generative AI in delivering novel therapeutics to patients.
The traditional division between computational (“dry-lab”) and experimental (“wet-lab”) research has long characterized pharmaceutical research, often creating silos that limit scientific collaboration and slow discovery progress [47]. Artificial intelligence (AI) and machine learning (ML) offer transformative potential to address the persistent challenges of traditional drug discovery, characterized by high costs, lengthy timelines, and low success rates [48]. However, the potential of AI is exactly that—potential. Converting the idea of AI into real, tangible benefits requires researchers to move beyond the computational domain and enter the familiar space of a wet lab [49].
This guide frames the integration of wet-lab and dry-lab workflows within the broader thesis of validating AI-based drug discovery models. For AI to be trusted and effective in a regulatory context, its predictions must be grounded in experimental reality. This is achieved through validation loops: iterative cycles where computational predictions inform experimental design, and experimental results, in turn, refine and validate the computational models. This process transforms AI from a static prediction tool into a dynamic, learning system that becomes more accurate and reliable with each cycle [47] [49]. The following sections will objectively compare how different platforms and approaches facilitate these critical validation loops, providing researchers with the data and methodologies needed to assess their relative performance.
The Validation Loop Framework: From Static Prediction to Active Learning
At its core, the validation loop is a closed-cycle process that creates a symbiotic relationship between in-silico predictions and in-vitro validation. This framework is fundamental for transforming AI models from black-box predictors into scientifically rigorous tools that can earn the trust of scientists and regulators alike [50].
The Conceptual Workflow
The validation loop operates through a continuous, four-stage process that closely mirrors the established Design-Make-Test-Analyze (DMTA) cycle in drug discovery, enhanced by AI and automated feedback [6].
Figure 1: The AI Model Validation Loop. This diagram illustrates the iterative feedback cycle between AI prediction and experimental validation that is essential for refining and validating AI models in drug discovery.
As depicted in Figure 1, the cycle begins with AI Design & Prediction, where models generate candidate molecules or propose experimental designs [47]. These computational outputs are translated into physical reality during Wet-Lab Synthesis & Testing, where techniques like binding assays or functional cellular assays provide ground-truth data [51]. The resulting data is then processed in the Data Acquisition & Analysis phase, which assesses the discrepancy between AI predictions and experimental outcomes [48]. Finally, in the Model Refinement & Learning phase, this analysis is used to retrain and improve the AI model, completing the loop and beginning a new, more informed cycle [49] [52].
The power of this loop lies in its ability to address a fundamental limitation of AI in biology: training data. As noted by Twist Bioscience, AI and ML technologies are often asked to make complex extrapolations from imperfect and limited training data sets [49]. For instance, in antibody optimization, many AI-designed screening libraries over-index on a single property because the training data is skewed. By adding experimental feedback into ML training data, research teams can transform the AI design process from a static prediction task into an active learning problem where each round of testing directly informs the next, leading to a much more efficient optimization path [49].
Comparative Analysis of Platforms and Approaches
The implementation of validation loops varies significantly across the AI drug discovery landscape. The table below provides a structured comparison of leading platforms, highlighting their distinct approaches to integrating wet and dry lab workflows.
Table 1: Comparison of AI Drug Discovery Platforms and Their Validation Loop Capabilities
| Platform/ Company | Primary Focus | Approach to Validation | Reported Advantages | Considerations & Limitations |
|---|---|---|---|---|
| NVIDIA BioNeMo [52] | Foundation models & infrastructure | "AI factory" concept with continuous wet-lab/dry-lab feedback. | 5x faster AlphaFold2 inference; Enables screening of billions of molecules. | Requires significant computational resources and integration effort. |
| Insilico Medicine [53] [54] | Target ID & generative chemistry | AI-driven design followed by wet-lab validation to confirm predictions. | Accelerated lead discovery; proven success in identifying novel compounds. | Platform complexity may require training; can be expensive for smaller entities. |
| Schrödinger [53] [54] | Physics-based & ML modeling | Computational predictions (e.g., FEP+) validated via partner wet-labs. | High accuracy in molecular simulations; deep integration with chemistry. | High costs; steep learning curve for those without computational chemistry background. |
| Exscientia [54] | AI-driven small molecule design | Iterative design-make-test-analyze cycles with integrated experiments. | Focus on efficient optimization of small molecules; rapid prototyping. | Primarily focused on small molecules, which may limit versatility. |
| Recursion Pharmaceuticals [53] | Phenotypic drug discovery | AI-powered automation to conduct and analyze massive wet-lab experiments. | High-throughput cellular imaging generates rich data for model training. | Requires massive investment in robotic automation and data infrastructure. |
| Ardigen & Selvita [51] | Biologics (Antibodies, Peptides) | Collaborative model: Ardigen's AI designs are validated in Selvita's labs. | Specialized in complex biologics; explicit focus on iterative feedback. | Service-based model may not suit organizations with internal capabilities. |
Quantitative Performance Metrics
Beyond the conceptual approach, quantitative metrics are essential for objective comparison. Platforms that effectively leverage validation loops demonstrate tangible gains in speed and accuracy.
Table 2: Reported Quantitative Performance Metrics from Integrated Workflows
| Platform/ Technology | Key Performance Metric | Result/Impact | Context |
|---|---|---|---|
| NVIDIA BioNeMo [52] | Inference Speed-up | AlphaFold2: 5x faster.DiffDock 2.0: 6.2x speed-up. | Enables more rapid iteration within the validation loop. |
| Schrödinger [52] | Virtual Screening Scale | Evaluation of 8.2 billion compounds. | Demonstrates the massive scale of initial in-silico filtering possible before wet-lab work. |
| Daiichi-Sankyo [52] | Virtual Screening Scale | Screened 6 billion molecules. | Highlights the industry-wide trend of leveraging AI for ultra-large library screening. |
| Twist Bioscience [49] | Synthesis Accuracy | Multiplex Gene Fragments (up to 500bp) enable accurate synthesis of AI-designed variants. | Reduces errors in translating digital designs to physical DNA, improving loop fidelity. |
Essential Research Reagent Solutions for Validation Experiments
The physical execution of the validation loop relies on a toolkit of reliable research reagents and platforms. The following table details key materials essential for experimentally validating AI predictions in the wet-lab.
Table 3: Key Research Reagent Solutions for Experimental Validation
| Reagent / Material | Primary Function in Validation | Key Characteristics | Example Providers/Platforms |
|---|---|---|---|
| Gene Fragments / Oligo Pools | Synthesize AI-designed DNA sequences (e.g., for antibodies, gene editing). | Long length (e.g., 500bp), high fidelity, and high throughput to match AI's design scale. | Twist Bioscience [49] |
| Cell-Based Assay Systems | Provide phenotypic or functional readouts for AI-predicted compound activity. | Relevance to disease biology, robustness, scalability, and compatibility with automation. | Various (CROs like Selvita [51]) |
| Protein Production & Purification Systems | Express and purify AI-designed protein targets or therapeutics for binding studies. | High yield, correct folding, and appropriate post-translational modifications. | Various (CROs like Selvita [51]) |
| Characterization Assays | Validate critical quality attributes (affinity, immunogenicity, developability). | Provide quantitative, high-confidence data for model feedback (e.g., SPR, ELISA). | Twist Biopharma Services [49] |
| Multi-Omics Data Generation Tools | Generate genomics, transcriptomics, proteomics data for target ID and model training. | Generate the high-quality, diverse data required to train and refine initial AI models. | NIH BioData Catalyst; Scispot [53] |
Standardized Experimental Protocols for Validation
To ensure that data generated in the wet-lab is robust, reproducible, and suitable for refining AI models, standardized experimental protocols are paramount. The following section outlines detailed methodologies for key validation experiments cited in industry practices and literature.
Protocol for AI-Driven Antibody Affinity Maturation
This protocol is commonly used to improve antibody binding affinity, a process where iterative validation loops have demonstrated significant success [49].
1. AI Design Phase:
- Input: Start with a parent antibody sequence and structural data.
- Process: Use a trained generative model (e.g., on a platform like NVIDIA BioNeMo or Ardigen's AI) to propose a library of sequence variants predicted to improve binding affinity and maintain stability [52] [51].
- Output: A focused library of several hundred to thousand variant sequences.
2. DNA Synthesis & Cloning (The "Make" Phase):
- Material Synthesis: Utilize high-fidelity DNA synthesis platforms (e.g., Twist Bioscience's Multiplex Gene Fragments) to synthesize the AI-designed variant sequences for the complementarity-determining regions (CDRs) [49].
- Cloning: Clone the synthesized DNA fragments into an appropriate expression vector backbone.
3. Expression & Purification:
- Transfection: Express the antibody variants in a mammalian system (e.g., HEK293 or CHO cells) to ensure proper folding and glycosylation.
- Purification: Purify the expressed antibodies using Protein A or G affinity chromatography.
4. High-Throughput Binding Assay (The "Test" Phase):
- Technique: Employ a surface plasmon resonance (SPR) or bio-layer interferometry (BLI) platform capable of high-throughput kinetics measurement.
- Procedure:
- Immobilize the target antigen on the sensor chip.
- For each purified variant, measure the association (
k_on) and dissociation (k_off) rates. - Calculate the binding affinity (
K_D) from the rate constants.
5. Data Analysis & Model Refinement (The "Analyze" Phase):
- Data Collation: Compile the measured
K_Dvalues for all tested variants. - Feedback: Feed the experimental binding data (the "ground truth") back into the AI model as a new training set.
- Model Retraining: Retrain the model to better learn the sequence-activity relationship. This refined model is then used to design a subsequent, more optimized library for the next cycle [49].
Protocol for Validating AI-Predicted Active Compounds
This protocol is used to validate hits from a large-scale virtual screen, a common application for companies like Schrödinger and Exscientia [52] [54].
1. In-Silico Screening:
- Virtual Library: Screen a virtual library of billions of molecules using AI and molecular docking simulations [52].
- Prioritization: Rank compounds based on predicted binding affinity, selectivity, and desirable ADMET properties.
2. Compound Sourcing/Synthesis:
- Procurement: Acquire the top 100-500 predicted hits from commercial vendors or compound archives.
- Synthesis: For novel structures predicted de novo, synthesize the compounds.
3. Primary Biochemical Assay:
- Objective: Confirm target engagement.
- Method: Run a high-throughput biochemical assay (e.g., fluorescence-based enzyme activity assay) against the intended target.
- Output: Identify "confirmed hits" that show activity in the low micromolar to nanomolar range.
4. Counter-Screening & Selectivity Profiling:
- Objective: Rule out false positives and assess specificity.
- Method: Test confirmed hits in secondary assays against related targets or general assay interference panels (e.g., testing for promiscuous aggregation).
5. Cellular Efficacy Assay:
- Objective: Validate activity in a more physiologically relevant context.
- Method: Treat disease-relevant cell lines with the compounds and measure a phenotypic endpoint (e.g., cell viability, reporter gene expression, or biomarker changes).
6. Data Integration:
- Analysis: Compare the experimental dose-response data (
IC50,EC50) from steps 3-5 with the AI's original predictions. - Feedback: Use the discrepancies between prediction and experiment to recalibrate the AI's scoring functions or retrain its predictive models, improving the accuracy of the next virtual screen [47] [48].
The workflow for this multi-stage validation process is visualized in Figure 2, showing the parallel tracks of experimental validation and model feedback.
Figure 2: Multi-Stage Experimental Validation Workflow. This diagram outlines the sequential and parallel experimental steps used to validate AI-predicted active compounds, from biochemical assays to cellular efficacy studies, with data from each stage feeding back to improve the AI model.
The integration of multi-modal data into artificial intelligence (AI) frameworks is fundamentally reshaping the landscape of drug discovery. This approach, which involves the synergistic combination of diverse data types—from genomic and transcriptomic information to clinical records and molecular structures—is providing an unprecedented, holistic view of disease biology and therapeutic action [55]. For researchers and drug development professionals, this paradigm shift is most critical in two high-stakes areas: target identification, the process of pinpointing the most promising biological targets for therapeutic intervention, and patient stratification, the practice of categorizing patients into subgroups most likely to respond to a treatment [56] [57]. The central challenge, however, lies in the robust validation of the AI models that power these discoveries. This guide provides an objective, data-driven comparison of contemporary AI tools and methodologies, framing them within the essential context of model validation to help scientists navigate this rapidly evolving field.
Performance Benchmarking: Multimodal AI vs. Traditional and Single-Modality Approaches
A key step in validating any new methodology is benchmarking its performance against established standards. The following tables synthesize quantitative data from recent studies and platform evaluations, comparing multimodal AI systems against traditional methods and single-modality AI across critical drug discovery tasks.
Table 1: Comparative Performance in Drug Discovery Key Performance Indicators (KPIs)
| Metric | Traditional Drug Discovery | AI-Enabled Discovery (Single-Modality) | AI-Enabled Discovery (Multimodal) |
|---|---|---|---|
| Timeline (Preclinical to Clinic) | 10-12 years [58] | 5-6 years [58] | ~1 year (reported for advanced platforms) [58] |
| Average Success Rate (Phase 1 Trials) | 40-65% [58] | 80-90% [58] | Not explicitly quantified, but reported as "significantly higher" [56] |
| Target Identification Accuracy | Limited by single-data type analysis [55] | Improved, but prone to false positives from isolated data [55] | Enhanced; reduces false positives via cross-modal validation [55] |
| Patient Stratification Precision | Based on limited biomarkers [57] | Improved using genomic or clinical data alone [57] | Superior; integrates genomics, clinical data, imaging for robust subgroups [59] [57] |
Table 2: Benchmarking of Select Multimodal AI Platforms and Models (Q1 2025)
| Platform / Model | Primary Application | Key Multimodal Data Utilized | Reported Performance / Validation |
|---|---|---|---|
| MADRIGAL [60] | Predicting clinical outcomes of drug combinations | Structural, pathway, cell viability, transcriptomic data | Outperforms single-modality methods in predicting adverse drug interactions and efficacy across 953 clinical outcomes [60] |
| Pharma.AI (Insilico Medicine) [61] | End-to-end drug discovery & biomarker development | Generative AI, biological target data, biomarker data | Over 30 drug candidates, 7 in clinical trials, one Phase 2 AI-designed therapy [61] |
| Centaur Chemist (Exscientia) [61] | Precision-designed small molecules | Chemical, biological, and clinical data | First AI-designed small molecules to enter clinical trials; major partnerships with Sanofi and Bristol Myers Squibb [61] |
| M3-20M Dataset [62] | Training AI for drug design & discovery | 1D SMILES, 2D graphs, 3D structures, physicochemical properties, textual descriptions | Enables models to generate more diverse/valid molecules and achieve higher property prediction accuracy vs. single-modal datasets [62] |
Experimental Protocols for Validating Multimodal AI
For a multimodal AI model to be trusted, it must be subjected to rigorous, transparent experimental validation. The following section details the methodology for two critical types of validation experiments.
Experimental Protocol 1: Benchmarking Against Established Datasets
Objective: To validate the performance of a new multimodal AI model for molecular property prediction against a known benchmark dataset, demonstrating superior accuracy compared to single-modality models.
Methodology:
- Dataset Curation: Utilize a large-scale, multi-modal dataset such as M3-20M, which contains over 20 million molecules with associated 1D SMILES strings, 2D molecular graphs, 3D structures, physicochemical properties, and textual descriptions [62].
- Task Definition: Define a specific molecular property prediction task, such as predicting toxicity (e.g., using the ClinTox-MM sub-dataset), binding affinity, or solubility.
- Model Training & Comparison:
- Train the novel multimodal model on all available modalities from the dataset.
- Train a series of baseline models—each using only a single data modality (e.g., SMILES only, graph only)—on the same data and for the same task.
- Employ standard deep learning architectures suitable for each data type (e.g., Graph Neural Networks for 2D graphs, Transformers for SMILES sequences, Convolutional Neural Networks for molecular images) [62].
- Validation & Metrics: Evaluate all models on a held-out test set. Key performance metrics include:
- Prediction Accuracy: The percentage of correct predictions.
- Area Under the Receiver Operating Characteristic Curve (AUC-ROC): For binary classification tasks.
- Mean Squared Error (MSE): For regression tasks.
- Statistical Significance: Use tests like the paired t-test to confirm that performance improvements of the multimodal model are statistically significant.
This protocol is designed to provide clear, reproducible evidence of the added value gained from data integration.
Experimental Protocol 2: Prospective Validation for Patient Stratification
Objective: To prospectively validate an AI-driven patient stratification model by using it to define enrollment criteria for a clinical trial and assessing its impact on trial outcomes.
Methodology:
- Model Development: Train a multimodal AI model (e.g., using a platform like Sonrai Discovery [57]) to identify patient subgroups most likely to respond to a therapy. Input data should include:
- Genomic Data: e.g., miRNA sequencing, genetic variants.
- Clinical Data: e.g., electronic health records, disease status, prior treatments.
- Imaging Data: e.g., digital pathology slides [57].
- Molecular Profiling: e.g., proteomic or metabolomic data.
- Biomarker Identification: The model should output a set of key biomarkers and a stratification rule (e.g., a specific genetic signature combined with a clinical phenotype) that defines the "likely responder" subgroup [57].
- Trial Design: Apply this stratification rule as an inclusion criterion for a new clinical trial. The primary objective is to compare the drug's efficacy in this AI-identified subgroup against a historical control or a concurrent non-stratified arm.
- Validation Metrics: The success of the stratification is measured by:
- Enhanced Drug Efficacy: A statistically significant improvement in the primary efficacy endpoint in the stratified group compared to a non-stratified population.
- Trial Efficiency: A reduction in the required sample size and time to completion, as the trial is enriched with responders [57].
- Reduced Failure Rate: Successful progression of the drug to later trial phases, mitigating the common failure due to lack of efficacy in a broad population [57].
This prospective, real-world validation is the ultimate test of a stratification model's clinical utility.
Visualizing Workflows and Data Integration
A core principle of multimodal AI is the integration of disparate data streams. The following diagrams, generated using Graphviz, illustrate the logical workflows for target identification and patient stratification.
Multimodal AI for Target Identification Workflow
Multimodal Data Integration for Patient Stratification
The Scientist's Toolkit: Essential Research Reagents & Platforms
Successfully implementing and validating multimodal AI requires a suite of computational tools, datasets, and platforms. The following table catalogues key resources cited in contemporary research.
Table 3: Essential Research Reagents & Platforms for Multimodal AI Validation
| Tool / Resource Name | Type | Primary Function in Validation |
|---|---|---|
| M3-20M Dataset [62] | Dataset | A large-scale benchmark containing over 20 million molecules with multiple modalities (1D-3D structures, text) for training and testing AI models. |
| MADRIGAL [60] | AI Model | A multimodal AI model that learns from structural, pathway, and transcriptomic data to predict clinical outcomes of drug combinations; serves as a state-of-the-art benchmark. |
| TileDB [55] | Database Platform | A scalable, cloud-native database for efficiently managing and analyzing complex multimodal data types like genomics, single-cell, and imaging data. |
| Scanpy & Seurat [55] | Open-Source Framework | Popular tools for the analysis of single-cell multimodal data, useful for validating AI findings at the cellular resolution. |
| MOFA+ (Multi-Omics Factor Analysis) [55] | Analysis Tool | A tool for the integration of multiple omics layers to identify the principal sources of variation, useful for interpreting AI model outputs. |
| Sonrai Discovery [57] | Analytics Platform | A no-code/low-code platform that enables the visualization, integration, and machine learning analysis of multi-modal data for patient stratification and biomarker discovery. |
| ToolUniverse [60] | AI Agent Ecosystem | An open ecosystem providing access to 600+ scientific and biomedical tools, allowing for the construction of customized AI "co-scientists" to test hypotheses. |
| CUREBench [60] | Evaluation Benchmark | The first competition platform for AI reasoning in therapeutics, providing a standardized environment to objectively compare AI models. |
The validation of AI models for target identification and patient stratification is no longer an academic exercise but a critical step in translating computational predictions into clinical breakthroughs. As the benchmark data and experimental protocols in this guide illustrate, models that leverage truly integrated multi-modal data consistently demonstrate superior performance, generating more reliable targets, more precise patient subgroups, and ultimately, a higher probability of clinical success [56] [60] [58]. The path forward requires a disciplined, evidence-based approach. Researchers must leverage large-scale, multi-modal benchmarks like M3-20M for robust training and testing, adopt transparent experimental protocols that enable replication, and utilize the growing ecosystem of platforms and tools designed for rigorous validation. By adhering to these principles, the field can fully unlock the potential of multimodal AI, accelerating the delivery of effective, personalized therapies to patients.
The integration of artificial intelligence (AI) into pharmaceutical development represents a paradigm shift, offering the potential to de-risk the notoriously costly and protracted process of bringing new therapeutics to market. AI applications now span the entire pipeline, from initial target identification to predicting clinical trial outcomes and accelerating drug repurposing [45] [48]. However, the transition of these AI models from research tools to clinically actionable assets hinges on one critical process: rigorous and standardized validation. For researchers and drug development professionals, understanding the performance benchmarks, limitations, and methodological requirements of these models is no longer a niche interest but a core component of modern translational science.
This guide provides a comparative analysis of current AI models for trial outcome prediction and drug repurposing, focusing on their validation frameworks. We objectively compare model performance using published data, detail the experimental protocols that underpin these tools, and outline the essential reagents and data sources required to implement these validation strategies in a research setting.
Comparative Analysis of AI Models for Clinical Trial Outcome Prediction
Predicting clinical trial outcomes can significantly optimize resource allocation and inform go/no-go decisions. Different AI approaches, from large language models (LLMs) to specialized hierarchical networks, have been applied to this task with varying strengths and weaknesses. The table below summarizes the quantitative performance of several models as reported in recent studies.
Table 1: Performance Comparison of Clinical Trial Outcome Prediction Models
| Model Name | Model Type | Balanced Accuracy | MCC | Recall | Specificity | Key Strength | Key Limitation |
|---|---|---|---|---|---|---|---|
| GPT-4o [63] | Large Language Model | 0.573 | 0.212 | 0.931 | 0.214 | High recall, robust in early phases | Low specificity; over-classifies successes |
| HINT [63] | Hierarchical Interaction Network | 0.563 | 0.111 | 0.586 | 0.541 | Balanced performance; best specificity | Moderate recall and MCC |
| GPT-4 [63] | Large Language Model | 0.542 | 0.234 | 1.000 | 0.083 | Perfect recall | Near-zero specificity; strong positive bias |
| Llama3 [63] | Large Language Model | 0.517 | 0.058 | 0.949 | 0.085 | Moderate recall | Poor specificity and MCC |
| GPT-3.5 [63] | Large Language Model | 0.504 | 0.049 | 0.997 | 0.011 | Very high recall | Effectively no specificity |
| GPT-4mini [63] | Large Language Model | 0.500 | 0.000 | 1.000 | 0.000 | Perfect recall | No ability to identify failures |
Performance varies significantly across clinical trial phases. For instance, the HINT model shows a marked improvement in specificity in later-stage trials, reaching 0.696 in Phase III, indicating its growing utility in identifying potential failures as trials progress [63]. Conversely, while LLMs like GPT-4o show strong performance in Phase I, their tendency toward low specificity remains a critical limitation for risk assessment.
Emerging Multimodal Approaches
Beyond the models in Table 1, novel architectures are being developed to address existing limitations. The LIFTED framework, for example, is a multimodal mixture-of-experts approach that transforms diverse data types (e.g., molecular, clinical) into natural language descriptions [64]. This method uses a unified encoder and a sparse mixture-of-experts to identify similar information patterns across different modalities, reportedly enhancing prediction performance across all clinical trial phases compared to previous baselines [64]. This highlights an important trend: the move toward models that can flexibly integrate heterogeneous data sources to improve generalizability and accuracy.
Experimental Protocols for Model Validation
The reliable assessment of AI models requires meticulous, pre-specified experimental designs. Below are detailed protocols for validating two primary types of models: clinical trial outcome predictors and AI-driven drug repurposing platforms.
Protocol for Validating Clinical Trial Outcome Predictors
This protocol is based on methodologies used to evaluate LLMs and specialized models like HINT [63].
1. Dataset Curation and Annotation
- Source: Assemble a dataset from public repositories like ClinicalTrials.gov. The dataset should include trials with conclusively documented outcomes (e.g., "Completed," "Terminated," "Withdrawn") and associated protocol documents.
- Stratification: Ensure the dataset includes trials across different phases (I, II, III) and disease areas (e.g., oncology, cardiovascular) to enable phase-specific and domain-specific analysis.
- Annotation: For each trial, extract and structure key information: eligibility criteria, primary and secondary endpoints, intervention type, dosing, and sponsor information. This structured data is crucial for models like HINT.
2. Model Training and Input Formulation
- For LLMs (e.g., GPT-4, Llama3): Use a few-shot prompting strategy. The prompt should include the task instruction, several correctly formulated examples of trial descriptions with known outcomes, and finally the description of the target trial. The model's output is then parsed for a success/failure prediction [63].
- For Specialized Models (e.g., HINT): Train the model using multimodal data. HINT, for instance, uses a hierarchical interaction network that generates embedding vectors from drug properties, disease information, and trial eligibility criteria. It employs a dynamic attention-based graph neural network to capture interactive effects among these elements [63].
3. Model Evaluation and Statistical Analysis
- Splitting: Implement a rigorous train/validation/test split, often using time-series splitting to prevent data leakage and ensure the model is evaluated on "future" trials.
- Metrics: Calculate standard performance metrics as shown in Table 1. Due to the common class imbalance (more successful trials), Matthew’s Correlation Coefficient (MCC) and Balanced Accuracy are more informative than simple accuracy.
- Analysis: Conduct subgroup analyses to evaluate model performance on specific trial phases and disease categories. This helps identify model biases and domains of high or low reliability.
Protocol for Validating AI-Driven Drug Repurposing
This protocol is derived from successful applications, such as the identification of vorinostat for Rett Syndrome [65].
1. Computational Prediction
- Input Data: The AI model analyzes diverse data inputs, including transcriptomic data from diseased versus healthy tissues, existing drug-induced gene expression profiles (e.g., from LINCS L1000 database), and structured knowledge of biological pathways and gene regulatory networks.
- Model Execution: The AI performs a target-agnostic analysis to identify drugs whose known mechanisms of action (e.g., gene expression signatures) are predicted to counter the disease-specific gene expression signature.
2. In Vivo Phenotypic Screening
- Model Organism: The top predicted drug candidates are moved into an in vivo screening platform. For example, a CRISPR-edited Xenopus laevis (frog) tadpole model of the disease (e.g., Rett Syndrome) can be generated to assess whole-body efficacy [65].
- Dosing and Assessment: Tadpoles are treated with the candidate drug. A wide array of phenotypic endpoints are measured, which can include neurological behaviors (e.g., seizure activity, swimming patterns), gastrointestinal motility, and respiratory function, to assess multi-organ efficacy [65].
3. Validation in Mammalian Model
- Animal Model: Promising candidates from the initial screen are advanced for validation in a mammalian model, such as MeCP2-null mice for Rett Syndrome.
- Therapeutic Regimen: Treatment is typically initiated after the onset of symptoms to better mimic the clinical scenario. The drug's effects are evaluated using behavioral tests, physiological measurements, and molecular biomarkers across multiple organ systems [65].
- Mechanistic Studies: Post-validation, further investigations (e.g., gene network analysis, proteomics) are conducted to elucidate the therapeutic mechanism, which may reveal novel biological insights, as was the case with vorinostat's effect on microtubule acetylation [65].
Workflow Visualization of Validation Pathways
The following diagrams, generated using DOT language, illustrate the logical workflows of the two key validation methodologies discussed.
Clinical Trial Prediction Validation
Drug Repurposing Validation
Validating AI models in a biological context requires a combination of computational resources, datasets, and experimental models. The following table details key solutions used in the featured experiments.
Table 2: Essential Research Reagent Solutions for Validation Studies
| Resource Name | Type | Function in Validation | Example Use Case |
|---|---|---|---|
| ClinicalTrials.gov Database | Public Data Repository | Provides structured and unstructured data on trial design, protocols, and outcomes for training and testing predictive models. | Curating a benchmark dataset for comparing LLMs and HINT [63]. |
| HINT Model | Software Algorithm | A hierarchical interaction network that integrates drug, disease, and trial data to predict trial success. | Used as a benchmark against LLMs due to its specificity in later trial phases [63]. |
| Xenopus laevis Tadpole Model | In Vivo Model System | A rapid, high-throughput in vivo platform for phenotyping the multi-organ efficacy of repurposing candidates. | Initial screening of vorinostat's efficacy in Rett Syndrome [65]. |
| MeCP2-null Mice | Mammalian Animal Model | A genetically engineered mouse model that recapitulates key disease features for validating candidate drugs in a mammalian system. | Confirming the therapeutic effect of vorinostat on neurological and non-neurological symptoms [65]. |
| Gene Network Analysis Tools | Bioinformatics Software | Used to elucidate the mechanism of action of a repurposed drug by analyzing changes in gene expression and regulatory pathways. | Revealing vorinostat's impact on acetylation metabolism and microtubule modification [65]. |
| Tox21/ToxCast Datasets | Toxicology Database | Public high-throughput screening data used to train and validate AI models for predicting compound toxicity during repurposing. | Profiling safety of new drug-disease pairs in silico [66]. |
The validation of AI models for clinical trial prediction and drug repurposing is a multifaceted challenge that requires a rigorous, multi-stage approach. As the comparative data shows, different models offer distinct trade-offs; LLMs may excel at broad pattern recognition but often lack the specificity required for reliable risk assessment, while specialized models like HINT offer more balanced performance. The ultimate translation of these AI tools into trusted components of the drug development toolkit depends on consistent application of robust validation protocols, including cross-species in vivo testing for repurposing candidates. For researchers, the critical takeaway is that the choice of model and validation strategy must be aligned with the specific application—whether for high-recall early triaging or high-specificity failure prediction—and must be supported by the essential data and biological reagents outlined in this guide.
Beyond the Hype: Troubleshooting Common Pitfalls and Optimizing AI Model Performance
Identifying and Mitigating Data Bias to Prevent Skewed Research Outcomes
The integration of artificial intelligence (AI) into drug discovery has created a promising frontier in biomedical research, significantly shortening the traditional decade-long drug development trajectory and reducing the exorbitant costs that can approach $2.6 billion per marketed drug [30]. However, as AI systems grow increasingly complex, ensuring their alignment with human values and scientific integrity becomes paramount. AI models, particularly large language models and other foundation models, have demonstrated significant biases relating to gender, sexual identity, and immigration status, which can exacerbate pre-existing social inequities when applied to healthcare [30]. In the high-stakes domain of drug discovery, biased AI outputs can misguide researchers, trigger erroneous determinations throughout the drug discovery pipeline, and potentially lead to the introduction of unsafe or inefficacious drugs into the market [30]. The sensitive nature of pharmaceutical research demands rigorous approaches to identifying and mitigating data bias to ensure research outcomes remain valid, reliable, and equitable across diverse patient populations.
The fundamental challenge lies in the data itself—AI models trained on historical biomedical data may inherit and amplify existing biases present in those datasets. For instance, if clinical trial data predominantly represents certain demographic groups, AI models may develop reduced predictive accuracy for underrepresented populations, potentially perpetuating healthcare disparities. Furthermore, the propagation of inaccurate responses or flawed scientific reasoning by generative AI systems poses substantial risks to research integrity, as these systems may produce seemingly plausible but scientifically invalid content that could skew research directions [30]. This article provides a comprehensive framework for identifying, quantifying, and mitigating data bias within AI-driven drug discovery pipelines, with specific experimental protocols and validation strategies to safeguard research outcomes.
Understanding Data Bias: Typology and Impact on Drug Discovery
Data bias in AI-driven drug discovery can manifest in multiple forms throughout the research pipeline, each with distinct characteristics and potential impacts on research outcomes. Understanding this typology is essential for developing targeted mitigation strategies.
Table: Types of Data Bias in AI-Driven Drug Discovery
| Bias Type | Origin in Drug Discovery Pipeline | Potential Impact on Research |
|---|---|---|
| Representation Bias | Non-diverse biological samples; Limited demographic/geographic representation in omics data | Reduced drug efficacy prediction accuracy for underrepresented populations; Perpetuation of health disparities |
| Measurement Bias | Inconsistent experimental protocols across data sources; Batch effects in high-throughput screening | Compromised model generalizability; Irreproducible findings across laboratories |
| Annotation Bias | Inconsistent labeling of drug-target interactions; Subjectivity in phenotypic screening | Incorrect training signals for AI models; Invalid structure-activity relationship predictions |
| Temporal Bias | Shifting biological understandings; Evolving diagnostic criteria | Models trained on outdated scientific paradigms producing suboptimal drug candidates |
| Algorithmic Bias | Model architectural choices favoring certain data distributions; Optimization metrics misalignment | Systematic overperformance on majority compounds/ targets; Underperformance on novel therapeutic classes |
The manifestation of these biases can significantly impact various stages of the drug discovery process. During target identification, biased data may lead researchers to prioritize targets predominantly relevant to specific populations while neglecting others. In compound screening, representation bias may result in AI models that effectively identify candidates for well-studied target classes but perform poorly on novel or rare disease targets. The negative behaviors observed in large language models, including the propagation of inaccurate responses and sensitivity to data-driven biases, can compromise patient welfare and exacerbate existing healthcare inequalities when these systems are deployed without adequate safeguards [30]. The RICE framework (Robustness, Interpretability, Controllability, and Ethicality) proposed for AI alignment emphasizes the importance of developing systems that maintain stability and reliability amid diverse uncertainties, which directly addresses these bias-related challenges [30].
Experimental Framework for Bias Identification and Quantification
Establishing robust experimental protocols for bias detection is fundamental to ensuring the validity of AI-driven drug discovery. The following methodologies provide comprehensive approaches for identifying and quantifying bias across different stages of the research pipeline.
Protocol 1: Representativeness Assessment for Biomedical Datasets
Purpose: To quantitatively evaluate how well a dataset represents the broader biological and patient populations for which a therapeutic intervention is intended.
Materials and Equipment:
- Primary dataset for analysis (e.g., genomic sequences, compound libraries, clinical data)
- Reference population data (e.g., gnomAD for genomics, NHANES for clinical parameters)
- Statistical analysis software (R, Python with pandas, scikit-learn)
- Data visualization tools (Matplotlib, Seaborn, Tableau)
Procedural Steps:
- Define Target Population: Clearly specify the biological and clinical characteristics of the intended application domain, including relevant demographic, genetic, and clinical parameters.
- Identify Key Covariates: Select measurable features that represent important dimensions of diversity relevant to the drug discovery context (e.g., genetic ancestry, age distribution, disease subtypes).
- Compute Discrepancy Metrics: Quantify representation gaps using statistical measures including:
- Population Stability Index (PSI): Measures how much the distribution of a covariate differs between dataset and target population
- Jensen-Shannon Divergence: Quantifies the similarity between probability distributions
- Chi-square tests of homogeneity: Identifies significant differences in categorical variable distributions
- Stratified Performance Analysis: Partition data by identified covariates and evaluate AI model performance metrics (accuracy, AUC-ROC, etc.) within each stratum.
- Bias Impact Quantification: Calculate disparity ratios comparing performance metrics between best-performing and worst-performing strata.
Validation Approach: Establish bias thresholds specific to drug discovery contexts. For example, representation discrepancies exceeding PSI > 0.25 or performance disparities exceeding 15% between population strata should trigger mitigation interventions before proceeding to subsequent research stages.
Protocol 2: Cross-Validation Strategy for Bias Detection
Purpose: To implement specialized cross-validation techniques that expose dataset-specific biases and evaluate model generalizability beyond narrow data distributions.
Materials and Equipment:
- Curated dataset with relevant metadata for stratification
- Computational environment for model training and evaluation
- Bias detection metrics (subgroup performance, fairness measures)
Procedural Steps:
- Stratified Cross-Validation: Partition data based on potential bias dimensions (e.g., experimental batch, data source institution, demographic subgroups) rather than random splits.
- Leave-One-Subgroup-Out Validation: Iteratively train models on all but one distinct subgroup and test on the excluded subgroup to identify populations where the model underperforms.
- Adversarial Validation: Train a classifier to distinguish between different data sources or subgroups; significant classifiability indicates substantial distributional differences.
- Temporal Validation: For longitudinal data, train on earlier time periods and validate on later periods to detect temporal drift affecting model performance.
- External Validation: Test model performance on completely independent datasets from alternative sources to assess true generalizability.
Interpretation Framework: Performance consistency across validation folds indicates robustness to the partitioned variable, while significant performance degradation on specific folds reveals susceptibility to particular biases that require mitigation.
Table: Quantitative Bias Assessment Metrics and Interpretation
| Metric | Calculation | Interpretation Thresholds |
|---|---|---|
| Disparity Ratio | (Performance in worst stratum) / (Performance in best stratum) | >0.85: Acceptable; 0.70-0.85: Concerning; <0.70: Unacceptable |
| Bias Amplification | (Model prediction disparity) - (Training data disparity) | <0: Mitigating bias; 0-0.05: Neutral; >0.05: Amplifying bias |
| Subgroup AUC Gap | AUCbestsubgroup - AUCworstsubgroup | <0.05: Acceptable; 0.05-0.10: Concerning; >0.10: Unacceptable |
| Fairness Difference | TPRunprivileged - TPRprivileged | >-0.05: Acceptable; -0.05 to -0.10: Concerning; <-0.10: Unacceptable |
The implementation of these experimental protocols aligns with the robustness objective of the RICE framework for AI alignment, which emphasizes maintaining AI system stability and dependability amid diverse uncertainties and disruptions [30]. Furthermore, the FDA's forthcoming guidance on AI in drug development is expected to emphasize evaluating risks based on the specific context of use, with key factors including trustworthy and ethical AI, managing bias, quality of data, and model development, performance, monitoring, and validation [67]. Proactively addressing these factors through rigorous bias assessment positions research teams to comply with emerging regulatory expectations.
Mitigation Strategies: Technical and Operational Approaches
Effective bias mitigation requires both algorithmic interventions and systematic changes to research practices. The following approaches provide comprehensive protection against skewed research outcomes.
Data-Centric Mitigation Strategies
Strategic Data Collection and Curation:
- Implement proactive diversity sampling to intentionally oversample underrepresented regions of the chemical, biological, or patient space
- Develop data augmentation techniques specific to pharmaceutical research, such as molecular transformation that maintains biochemical validity while increasing diversity
- Establish data partnerships that collectively address representation gaps across multiple institutions
- Create standardized metadata schemas to consistently capture experimental conditions, demographic information, and sample characteristics
Preprocessing Interventions:
- Apply reweighting techniques to assign higher importance to underrepresented subgroups during model training
- Implement resampling approaches (SMOTE, ADASYN) adapted for molecular and clinical data structures
- Utilize domain adaptation methods to align distributions across different data sources
- Employ adversarial de-biasing to remove sensitive information from learned representations while maintaining predictive power for primary tasks
Algorithmic Mitigation Strategies
Fairness-Aware Model Architectures:
- Incorporate fairness constraints directly into the optimization objective during model training
- Implement adversarial learning frameworks where a primary predictor learns the main task while an adversary attempts to predict protected attributes from the representations
- Develop multi-task architectures that simultaneously optimize for overall performance and subgroup performance parity
- Utilize causal modeling approaches to distinguish spurious correlations from causal relationships in drug response predictions
Transparency-Enhancing Techniques:
- Integrate explainable AI methods specifically adapted for biomedical applications, such as saliency maps for molecular structures or feature importance for clinical predictors
- Implement uncertainty quantification to flag predictions where models extrapolate beyond their reliable operating domains
- Develop interactive model interrogation tools that allow researchers to explore model behavior across different population subgroups
The integration of these mitigation strategies supports the interpretability objective of the RICE framework, facilitating user comprehension of the system's operational framework and decision-making mechanisms [30]. As noted in analyses of AI drug discovery, human-centered AI alignment can help ensure that drug discovery efforts are inclusive and meet the needs of diverse populations, with transparency improving the interpretability of predictive models [30]. This multidimensional perspective emphasizes that combining artificial intelligence systems with human values can significantly impact the credibility and acceptance of AI-driven drug discovery in both scientific and regulatory contexts.
Validation Framework and Continuous Monitoring
Establishing robust validation processes is essential for confirming the effectiveness of bias mitigation strategies and ensuring ongoing protection against skewed outcomes.
Comprehensive Validation Protocol
Purpose: To systematically evaluate bias mitigation effectiveness and ensure model performance generalizability across relevant populations and conditions.
Experimental Design:
- Create Benchmarking Datasets: Develop carefully curated challenge sets that explicitly represent important diversity dimensions, including:
- Rare genetic variants or disease subtypes
- Underrepresented demographic groups
- Diverse chemical scaffolds not present in training data
- Cross-species generalizations where applicable
Implement Multi-dimensional Assessment: Evaluate models using a comprehensive suite of metrics covering:
- Overall predictive performance (AUC-ROC, precision, recall)
- Performance consistency across subgroups (disparity ratios, worst-case performance)
- Calibration accuracy within and across subgroups
- Robustness to realistic data perturbations and domain shifts
Comparative Analysis: Benchmark proposed models against appropriate baselines using rigorous statistical testing to confirm significant improvements in fairness metrics without compromising overall performance.
Validation Reporting: Document all validation results in a standardized format that includes detailed descriptions of test populations, comprehensive performance disaggregation, and explicit statements about model limitations and appropriate use domains.
Continuous Monitoring Framework
Production Monitoring Infrastructure:
- Implement automated fairness dashboards that track subgroup performance metrics over time
- Establish alert systems that trigger when performance disparities exceed predefined thresholds
- Deploy concept drift detection to identify shifting data distributions that may require model recalibration
- Maintain version control for both models and evaluation datasets to ensure reproducibility
Governance Processes:
- Establish regular model audit schedules with independent review
- Maintain detailed documentation of data provenance, model development decisions, and validation results
- Create clear protocols for model retirement and retraining when monitoring identifies significant performance degradation
- Develop ethical review boards specifically focused on AI applications in drug discovery
The validation framework aligns with emerging regulatory considerations for AI in drug development, which highlight the importance of validation, particularly when aspects of the drug evaluation process are at least partially substituted with AI models [67]. Furthermore, initiatives such as the FDA's Good Machine Learning Practice (GMLP) and collaborative governance models like Mayo Clinic's partnership with Google on "model-in-the-loop" reviews provide practical frameworks for implementing these validation approaches [68].
Research Reagent Solutions for Bias-Aware AI Drug Discovery
Implementing effective bias mitigation requires specialized computational tools and frameworks. The following table details essential research reagents for bias-aware AI drug discovery pipelines.
Table: Essential Research Reagent Solutions for Bias Mitigation
| Reagent Category | Specific Tools/Frameworks | Primary Function in Bias Mitigation |
|---|---|---|
| Bias Assessment Libraries | AI Fairness 360 (IBM); Fairlearn (Microsoft); Aequitas | Comprehensive metrics for quantifying disparities; Bias detection algorithms; Visualization capabilities |
| Data Processing Tools | Synthea (synthetic data); SMOTE variants; DALEX (R) | Generate synthetic samples for rare populations; Resampling approaches; Data exploration and explanation |
| Model-Level Mitigation Frameworks | Adversarial Debiasing; Reductions Approach; Contrastive Learning | Remove protected information from representations; Constrained optimization; Learn invariant representations |
| Explainability Toolkits | SHAP; LIME; Captum (PyTorch); InterpretML | Model interpretation; Feature importance attribution; Subgroup behavior analysis |
| Validation Platforms | Great Expectations; TensorFlow Data Validation; MLflow | Data quality monitoring; Schema enforcement; Experiment tracking and reproducibility |
| Specialized Biomedical Libraries | MoleculeNet; Therapeutics Data Commons; DeepChem | Domain-specific benchmarking; Standardized evaluation; Specialized architectures for molecular data |
These tools collectively enable the implementation of the technical frameworks discussed throughout this article. Their integration into standardized drug discovery workflows represents a practical approach to operationalizing the principles of human-centered AI alignment, which emphasizes embedding fundamental principles such as fairness, transparency, accountability, and respect for human well-being into AI systems [30]. As the field progresses, continued development of domain-specific bias assessment and mitigation tools tailored to the unique requirements of pharmaceutical research will be essential for maintaining scientific rigor while harnessing the transformative potential of AI technologies.
The integration of comprehensive bias identification and mitigation strategies represents a fundamental requirement for the valid application of AI in drug discovery. As the field progresses toward more specialized pipelines that leverage diverse data sources through multimodal, multiscale, and self-supervised approaches [67], the potential for propagating and amplifying biases increases correspondingly. The frameworks, experimental protocols, and mitigation strategies presented in this article provide a roadmap for maintaining scientific rigor while harnessing AI's transformative potential. By implementing systematic bias assessment as a core component of AI-driven drug discovery, researchers can accelerate the development of therapeutic interventions that deliver equitable benefits across diverse patient populations, ultimately fulfilling the promise of precision medicine while safeguarding against the perpetuation of healthcare disparities.
Bias Mitigation Workflow
Bias Validation Protocol
Data Bias Typology
Strategies for Enhancing Model Robustness Against Adversarial Attacks and Data Drift
In the high-stakes field of AI-based drug discovery, model robustness is not merely a technical consideration but a fundamental requirement for regulatory approval and clinical application. Models must demonstrate resilience against two primary threats: adversarial attacks, which are subtle, malicious input modifications designed to deceive models, and data drift, the gradual shift in input data distribution over time that degrades model performance. The U.S. Food and Drug Administration (FDA) has recently emphasized the critical importance of AI model credibility through new draft guidance, establishing a risk-based framework that requires comprehensive validation and life cycle maintenance [69] [18]. This guide provides a comparative analysis of robustness strategies, supported by experimental data and methodologies directly relevant to drug discovery applications, to help researchers build models that withstand these challenges and maintain regulatory compliance.
Understanding the Threat Landscape
Adversarial Attacks in Medical AI
Adversarial attacks exploit model vulnerabilities by introducing imperceptible perturbations to input data. In healthcare domains, studies have demonstrated that medical AI models can be highly vulnerable to these attacks due to factors including the complexity of medical images and model overparameterization [70]. These attacks are particularly dangerous in drug discovery where they could potentially lead to false positives in drug-target interaction predictions or mask toxicity signals.
The most common attack methodologies include:
- Image-based attacks: Fast Gradient Sign Method (FGSM) and Projected Gradient Descent (PGD) perturb input data in the direction of the gradient of the model's loss function [70].
- Text-based attacks: Synonym substitution and word deletion manipulate textual inputs while preserving semantic meaning [70].
Data Drift in Pharmaceutical Applications
Data drift refers to changes in the statistical properties of model input features during production use, potentially causing performance degradation [71]. In drug discovery, this could manifest as changes in chemical space representation during virtual screening or shifts in patient population characteristics during clinical trials.
Critical distinctions in drift types include:
- Data drift: Changes in input data distributions without changes to the underlying input-output relationships [71].
- Concept drift: Changes in the relationships between model inputs and outputs, where the same inputs lead to different expected outcomes [71].
- Prediction drift: Shifts in the distribution of model outputs, which can signal environmental changes or model quality issues [71].
Comparative Analysis of Defense Strategies
Multimodal Integration for Adversarial Robustness
Research demonstrates that multimodal models exhibit enhanced resilience against adversarial attacks compared to single-modality counterparts. A 2025 study investigating medical AI systems found that integrating multiple modalities, such as images and text, positively contributes to the robustness of deep learning systems [70].
Table 1: Performance Comparison of Single-Modality vs. Multimodal Models Under Attack
| Model Architecture | Attack Type | Performance Drop (%) | Key Findings |
|---|---|---|---|
| Image-only (SE-ResNet-154) | FGSM | -38.2 | Highly vulnerable to gradient-based attacks |
| Text-only (Bio_ClinicalBERT) | Synonym Replacement | -22.7 | Moderate vulnerability to semantic-preserving attacks |
| Multimodal (Fusion) | FGSM on Image | -15.3 | Significantly more robust than single-modality |
| Multimodal (Fusion) | Combined Attack | -18.9 | Demonstrates cross-modal stability |
The experimental protocol for this comparison involved:
- Model Training: Fine-tuning SE-ResNet-154 on chest X-ray classification and Bio_ClinicalBERT on clinical text for binary classification tasks [70].
- Attack Implementation: Applying FGSM and PGD attacks on images, synonym substitution and word deletion on text [70].
- Evaluation: Measuring performance degradation when attacks were applied to individual modalities in isolation and in combination [70].
The fusion technique employed combined early and late fusion paradigms, with early fusion being particularly effective when model parameters are known and datasets are large [70].
Evidential Deep Learning for Uncertainty Quantification
Evidential Deep Learning (EDL) has emerged as a promising approach for improving model calibration and robustness in drug discovery applications. The EviDTI framework, introduced in 2025, demonstrates how EDL can address the critical challenge of overconfidence in Drug-Target Interaction (DTI) prediction [72].
Table 2: Performance Comparison of DTI Prediction Models on DrugBank Dataset
| Model | Accuracy (%) | Precision (%) | MCC (%) | F1 Score (%) |
|---|---|---|---|---|
| RFs | 74.15 | 75.80 | 48.59 | 75.12 |
| SVMs | 76.33 | 77.21 | 52.89 | 76.88 |
| DeepConv-DTI | 78.94 | 79.15 | 58.08 | 79.11 |
| GraphDTA | 79.26 | 79.83 | 58.72 | 79.55 |
| MolTrans | 80.17 | 80.22 | 60.48 | 80.19 |
| EviDTI (Proposed) | 82.02 | 81.90 | 64.29 | 82.09 |
The EviDTI methodology incorporates:
- Multi-dimensional representations: Combining drug 2D topological graphs, 3D spatial structures, and target sequence features [72].
- Pre-trained encoders: Utilizing ProtTrans for protein sequences and MG-BERT for molecular graphs [72].
- Evidential layer: Outputting parameters to calculate prediction probability and corresponding uncertainty values [72].
This approach enables the model to explicitly express uncertainty on unfamiliar inputs, similar to human cognitive processes, thereby reducing the risk of overconfident false predictions in critical drug discovery applications [72].
Data Drift Detection and Mitigation
Effective drift detection is essential for maintaining model performance throughout the drug development lifecycle. Monitoring techniques serve as proxy signals to assess whether ML systems operate under familiar conditions when ground truth labels are inaccessible [71].
Table 3: Data Drift Detection Methods Comparison
| Method | Mechanism | Data Types | Implementation Complexity |
|---|---|---|---|
| Population Stability Index (PSI) | Measures distribution shift between training and reference data | Numerical, Categorical | Low |
| Statistical Hypothesis Testing | Kolmogorov-Smirnov, Chi-squared tests | Numerical, Categorical | Medium |
| Distance Metrics | Wasserstein distance, Jenson-Shannon divergence | Numerical | High |
| Model-Based Detection | Monitoring performance metrics on recent data | All types | Medium |
The Population Stability Index (PSI), implemented in platforms like H2O Model Validation, calculates distribution shifts for numerical and categorical variables using the formula:
[ PSI = \sum{i=1}^{n} (Ai - Ei) \times \ln(Ai / E_i) ]
Where (Ai) is the actual percentage of observations in bin i, and (Ei) is the expected percentage [73].
For drug discovery applications, the FDA specifically recommends implementing "systems to detect data drift or changes in the AI model during life cycle of the drug" and "systems to retrain or revalidate the AI model as needed because of data drift" [18].
Experimental Protocols for Robustness Validation
Adversarial Robustness Testing Protocol
To comprehensively evaluate model robustness against adversarial attacks, researchers should implement the following experimental protocol:
Baseline Performance Establishment
- Train models on clean datasets relevant to drug discovery (e.g., molecular structures, clinical text)
- Evaluate using standard metrics: accuracy, precision, recall, F1-score, AUC-ROC
Attack Simulation
- Implement gradient-based attacks (FGSM, PGD) for structural data
- Apply text manipulation attacks (synonym replacement, word deletion) for clinical text data
- Develop combined attacks for multimodal systems
Robustness Quantification
- Measure performance degradation under attack conditions
- Calculate robustness score as: ( \text{Robustness} = 1 - \frac{\text{Performance Drop}}{\text{Baseline Performance}} )
Cross-Modal Impact Assessment
- For multimodal systems, attack individual modalities while monitoring overall performance
- Evaluate information flow between modalities to identify dominance patterns
Data Drift Detection Protocol
For comprehensive drift monitoring in production drug discovery systems:
Reference Dataset Establishment
- Select representative training data or initial production data as reference
- Establish baseline distributions for critical features
Monitoring Framework Implementation
- Compute PSI or statistical distances between reference and recent production data
- Set threshold values based on risk assessment (e.g., PSI > 0.25 indicates significant drift)
- Implement automated alerts for threshold violations
Root Cause Analysis
- Investigate data quality issues versus genuine environmental changes
- Correlate drift detection with model performance metrics
- Identify specific features contributing most to overall drift
Mitigation Strategy Activation
- Trigger model retraining or fine-tuning protocols
- Implement data preprocessing adjustments
- Update feature engineering pipelines as needed
Implementation Framework
Research Reagent Solutions
Table 4: Essential Tools for Robust AI Implementation in Drug Discovery
| Tool Category | Specific Solutions | Function | Applicability |
|---|---|---|---|
| Model Architectures | SE-ResNet-154, Bio_ClinicalBERT, GNNs | Base models for medical image processing, clinical text analysis, and molecular data | Task-specific model selection |
| Robustness Frameworks | EviDTI, Multimodal Fusion | Uncertainty quantification, adversarial robustness | High-risk applications requiring reliability |
| Drift Detection | H2O Model Validation, Evidently AI | Monitoring data distribution shifts | Production system maintenance |
| Attack Libraries | CleverHans, TextAttack | Generating adversarial examples | Proactive robustness testing |
| MLOps Platforms | Kubeflow, MLflow | Model deployment, lifecycle management | Scalable production systems |
Integrated Workflow for Robust AI Implementation
The following diagram illustrates a comprehensive workflow for implementing robust AI systems in drug discovery:
AI Robustness Implementation Workflow
Regulatory Compliance Considerations
The FDA's draft guidance outlines a 7-step risk-based credibility assessment framework for AI models used in drug development [69] [18]. Key considerations for robustness strategies include:
Context of Use Definition
- Clearly specify the model's role in the drug development process
- Identify potential failure modes and their impact on patient safety
Risk Assessment
- Evaluate model influence risk (how much the AI model influences decision-making)
- Assess decision consequence risk (patient safety implications)
Comprehensive Documentation
- Document model architecture, training methodologies, and validation processes
- Provide evidence of robustness testing against adversarial attacks and data drift
Lifecycle Maintenance Plan
- Establish protocols for continuous monitoring and periodic reassessment
- Define triggers for model retraining or updating
Enhancing model robustness against adversarial attacks and data drift is essential for deploying reliable AI systems in drug discovery. The comparative analysis presented demonstrates that multimodal integration, evidential deep learning for uncertainty quantification, and systematic drift detection provide complementary strategies for addressing these challenges. As regulatory frameworks continue to evolve, adopting these robustness strategies will be crucial for building credible AI systems that accelerate drug development while maintaining safety and efficacy standards. Future research should focus on developing standardized benchmarks for robustness evaluation specific to pharmaceutical applications and creating more efficient methods for continuous model validation in production environments.
Balancing Intellectual Property Protection with the Need for Sufficient Model Disclosure
The integration of Artificial Intelligence (AI) into drug discovery represents a paradigm shift in pharmaceutical research, offering unprecedented acceleration in identifying viable drug candidates and predicting compound efficacy [74]. However, this technological revolution has created a fundamental tension: innovative AI models require robust intellectual property (IP) protection to safeguard competitive advantage, while regulatory validation demands sufficient model disclosure to ensure safety, efficacy, and reproducibility [67]. This balancing act is particularly critical for researchers and scientists who must navigate evolving FDA guidelines while protecting proprietary methodologies.
The core challenge lies in the inherent conflict between transparency and protection. AI drug discovery companies derive value from proprietary algorithms and unique training methodologies, yet regulatory agencies increasingly require insight into these "black box" models to establish credibility and ensure patient safety [18] [67]. With the FDA releasing draft guidance in January 2025 outlining information requirements for AI supporting regulatory decision-making, understanding this landscape has become imperative for drug development professionals [18].
Regulatory Framework: The FDA's Risk-Based Approach
Core Principles of the 2025 FDA Draft Guidance
The U.S. Food and Drug Administration's 2025 draft guidance, "Considerations for the Use of Artificial Intelligence To Support Regulatory Decision-Making for Drug and Biological Products," establishes a structured framework for AI model evaluation centered on two critical concepts [18]:
- Question of Interest: The specific question, decision, or concern being addressed by the AI model, which could range from clinical trial participant selection to pharmaceutical quality control [18].
- Context of Use: The specific scope and role of an AI model for addressing the question of interest, which serves as the starting point for risk assessment [18].
The guidance emphasizes that its scope is limited to AI models that impact patient safety, drug quality, or reliability of results from nonclinical or clinical studies. Companies using AI solely for discovery while relying on traditional processes for safety and quality factors may not need significant modifications to their current AI governance [18].
Risk Assessment Framework
The FDA proposes a tiered risk framework that determines the extent of required disclosure based on two factors [18]:
- Model Influence Risk: How much the AI model influences decision-making
- Decision Consequence Risk: The potential consequences of decisions on patient safety or drug quality
Table: FDA Risk Framework and Corresponding Disclosure Requirements
| Risk Level | Model Influence | Potential Consequences | Documentation Requirements |
|---|---|---|---|
| High | Significant impact on decisions | Direct patient safety impact | Comprehensive architecture, data sources, training methodologies, validation processes, performance metrics |
| Moderate | Advisory role with human oversight | Indirect impact on quality | Moderate documentation of key model parameters and validation results |
| Low | Minimal influence on critical decisions | No direct safety impact | Basic documentation of model purpose and general approach |
For high-risk AI models—where outputs could impact patient safety or drug quality—comprehensive details regarding the AI model's architecture, data sources, training methodologies, validation processes, and performance metrics may need submission for FDA evaluation [18]. The guidance notes that most AI models within its scope will likely be considered high-risk because they are used for clinical trial management or drug manufacturing, meaning stakeholders should prepare for extensive disclosure requirements [18].
Intellectual Property Protection Strategies
Patent vs. Trade Secret Analysis
Stakeholders must carefully consider the fundamental choice between patent protection and trade secret protection for AI drug discovery innovations. Each approach offers distinct advantages and limitations in the context of regulatory disclosure requirements [18] [67].
Table: Comparative Analysis of IP Protection Strategies for AI Models
| Protection Method | Advantages | Disadvantages | Ideal Use Cases |
|---|---|---|---|
| Patent Protection | Safeguards innovations while satisfying FDA transparency requirements; provides exclusivity for 20 years | Requires public disclosure of invention; limited protection for data sets and certain algorithms | Foundational model architectures; novel training methodologies; specific algorithmic innovations |
| Trade Secret Protection | No disclosure requirements; potentially perpetual protection | Difficult to maintain if FDA requires extensive model disclosure; vulnerable to reverse engineering | Pre-clinical discovery tools; data processing techniques; internal workflows not requiring regulatory review |
| Hybrid Approach | Balances protection and disclosure needs; maximizes portfolio flexibility | Complex to manage; requires careful segmentation of protected elements | End-to-end platforms with both regulated and non-regulated components |
The FDA's extensive transparency requirements pose a significant challenge for maintaining AI innovations as trade secrets when these models impact regulatory decisions [18]. As noted in the guidance, "By securing patent protection on the AI models, stakeholders can safeguard their intellectual property while satisfying FDA's transparency requirements" [18]. This fundamental reality necessitates a strategic approach to IP portfolio management.
Strategic IP Considerations for AI Drug Discovery
An effective IP strategy for AI drug discovery should consider several key factors [67]:
- Resource Allocation: Companies whose value derives primarily from proprietary technologies should devote more resources to a dense patent portfolio backstopped by trade secret protection [67].
- Partnership Considerations: Firms focused on collaboration and data sharing may consider focused patent filings sufficient to protect foundational technologies while relying on copyright protection and confidentiality provisions [67].
- Portfolio Development: The AI drug discovery patent landscape remains "wide open," creating opportunities for companies to build robust portfolios around critical aspects of their technology stack [67].
Wet lab automation companies, for example, should pursue medical device-type protection strategies while also safeguarding computer vision and sensor data processing methodologies [67]. Similarly, model developers should identify critical architectural aspects that competitors might replicate and prioritize those elements for patent protection [67].
Experimental Framework for Model Validation
Standardized Validation Protocols
Establishing model credibility requires rigorous validation protocols that satisfy both scientific and regulatory standards. The FDA guidance emphasizes that establishing credibility involves describing: (1) the model, (2) data used for development, (3) model training, and (4) model evaluation including test data, performance metrics, and reliability concerns such as bias [18].
Diagram: Model Validation Workflow for Regulatory Compliance. This workflow outlines the key stages for establishing AI model credibility according to FDA guidance principles [18].
Key Experimental Metrics and Benchmarks
Validation experiments should generate quantitative metrics that demonstrate model robustness, generalizability, and performance across diverse datasets. The following table summarizes critical validation metrics referenced in studies of leading AI drug discovery platforms:
Table: Quantitative Validation Metrics for AI Drug Discovery Models
| Validation Category | Specific Metrics | Industry Benchmark | Exemplary Performance |
|---|---|---|---|
| Predictive Accuracy | ROC-AUC, Precision-Recall, F1-Score | AUC > 0.80 | Insilico Medicine: novel compounds with promising preclinical activity within months [4] |
| Generalizability | Cross-validation scores, independent test set performance | <10% performance degradation on external datasets | Recursion Pharmaceuticals: identification of therapeutics for rare genetic diseases via high-throughput screening [4] |
| Robustness | Sensitivity analysis, adversarial testing | <15% output variation with noisy inputs | Target identification platforms: up to 50% reduction in early-stage discovery timelines [74] |
| Bias Assessment | Subgroup performance disparities, fairness metrics | <5% performance difference across subgroups | Leading platforms: integration of bias detection in training data [18] |
These metrics should be generated through rigorous testing protocols, including holdout validation, cross-validation, and external validation on independent datasets. Performance should be consistently demonstrated across multiple data splits to ensure reliability [18].
The Scientist's Toolkit: Essential Research Reagents
Implementing validated AI drug discovery platforms requires both computational and experimental resources. The following table details essential research reagents and solutions referenced in studies of successful AI-driven discovery pipelines:
Table: Essential Research Reagents for AI Drug Discovery Validation
| Reagent Category | Specific Examples | Function in Validation | Implementation Considerations |
|---|---|---|---|
| Compound Libraries | Selleckchem BIOACTIVE compound library, Enamine REAL database | Provides diverse chemical structures for virtual screening and experimental validation | Library size (>1M compounds), chemical diversity, drug-like properties |
| Cell-Based Assay Systems | Primary cell cultures, iPSC-derived models, organoid systems | Enables experimental validation of predicted compound-target interactions | Physiological relevance, reproducibility, scalability for high-throughput screening |
| Target Validation Tools | CRISPR-Cas9 screening libraries, siRNA collections | Confirms disease relevance of AI-predicted targets | Coverage of druggable genome, on-target efficiency, minimal off-target effects |
| Data Processing Platforms | KNIME, Pipeline Pilot, custom Python pipelines | Standardizes diverse data inputs for model training and validation | Interoperability with existing systems, scalability, reproducibility features |
| Model Monitoring Systems | Data drift detection algorithms, performance tracking dashboards | Supports life cycle maintenance of AI models as required by FDA guidance | Real-time monitoring capabilities, automated alert systems, version control |
These research reagents form the foundation for establishing the credibility of AI models throughout the drug discovery pipeline, from initial target identification through lead optimization [4] [18] [74]. Their consistent application enables researchers to generate the robust experimental data needed for regulatory submissions while protecting intellectual property through strategic disclosure.
Successfully balancing intellectual property protection with sufficient model disclosure requires a strategic, integrated approach that begins early in model development. Companies should define their specific value proposition, identify the data, technology, and talent supporting that proposition, and assess use case-specific risks [67]. This foundation enables strategic resource allocation across various IP assets and creates an AI governance framework that aligns policy with specific controls for identified risks [67].
The most effective strategies will incorporate human oversight and operational controls to mitigate AI model risks, potentially reducing disclosure burdens [18]. Furthermore, companies should proactively identify and patent innovations that address FDA-articulated needs, such as explainable AI capabilities, bias detection systems, and lifecycle maintenance tools [18]. By establishing and executing on this comprehensive framework, AI drug discovery firms can advance their differentiation in data, technology, and therapeutic targets while positioning themselves for successful licensing, partnership, and regulatory outcomes [67].
Addressing Privacy, Confidentiality, and Cybersecurity in Data-Intensive Workflows
The integration of artificial intelligence (AI) into drug discovery represents a paradigm shift, enabling researchers to analyze massive biological datasets and identify novel drug candidates with unprecedented speed. However, this data-intensive approach introduces significant privacy, confidentiality, and cybersecurity challenges that must be addressed to ensure scientific progress does not come at the cost of data security or regulatory compliance. The core of this challenge lies in the sensitive nature of the data involved, which often includes patient health information, proprietary chemical compound data, and valuable biomedical research data [67] [75].
The life sciences industry is increasingly reliant on AI, with up to 70% of companies now using AI in research and development according to DLA Piper's AI Governance Report [75]. This widespread adoption amplifies the attack surface for cyber threats while simultaneously creating complex data governance obligations. Effective cybersecurity in this context must balance the open collaboration necessary for scientific innovation with the strict confidentiality required for patient privacy and intellectual property protection [76]. This balance is particularly crucial in drug discovery, where failures in data protection can compromise patient trust, violate regulations, and result in the loss of valuable intellectual property worth billions in research investment.
Comparative Analysis of Privacy-Enhancing Technologies (PETs)
Privacy-Enhancing Technologies (PETs) provide sophisticated technical solutions that enable data analysis and collaborative research without exposing the underlying sensitive information. These technologies are becoming increasingly vital in AI-driven drug discovery workflows where multiple organizations need to collaborate without sharing their proprietary or regulated data [77].
The following table compares the major PETs relevant to drug discovery workflows, their operational mechanisms, and their implementation maturity:
Table 1: Comparison of Privacy-Enhancing Technologies for Drug Discovery
| Technology | How It Works | Typical Use Case | Implementation Maturity |
|---|---|---|---|
| Differential Privacy (DP) | Adds calibrated statistical noise to data or query results to prevent re-identification of individuals [77]. | Publishing aggregate data (e.g., clinical trial statistics) without exposing individual patient records [77]. | High (e.g., Used in 2020 U.S. Census) [77]. |
| Federated Learning (FL) | Trains AI models across decentralized data sources without moving or sharing raw data; only model updates are shared [77]. | Multiple pharmaceutical companies collaboratively training drug discovery models without sharing sensitive proprietary data [77]. | Medium-High (e.g., MELLODDY project with 10 pharma companies) [77]. |
| Secure Multi-Party Computation (SMPC) | Allows multiple parties to jointly compute a function over their inputs while keeping those inputs private [77]. | Universities collaborating on research by analyzing data from multiple institutions while keeping individual records private [77]. | Medium (e.g., EU's SECURED Innohub for health data) [77]. |
| Fully Homomorphic Encryption (FHE) | Allows computations to be performed directly on encrypted data without needing to decrypt it first [77]. | Conducting genomic research (e.g., Genome-Wide Association Studies) on encrypted patient data [77]. | Medium (Computationally intensive, but improving) [77]. |
The MELLODDY project exemplifies PET implementation in pharmaceutical research, where 10 competing companies collaboratively trained AI models to improve drug candidate screening without exposing their respective proprietary datasets [77]. This federated approach allowed participants to increase their models' predictive power by accessing a larger virtual training set while maintaining both data confidentiality and competitive advantage.
Quantitative Comparison of Data Security Implementations in Drug Discovery Platforms
Various commercial drug discovery software platforms have implemented different approaches to data security, with some achieving recognized certifications and employing specific PETs. The table below summarizes the security features of several prominent platforms as of 2025:
Table 2: Data Security Implementation Across Drug Discovery Platforms
| Platform/Provider | Security Certifications | Data Encryption | Privacy-Enhancing Features | Access Controls |
|---|---|---|---|---|
| deepmirror | ISO 27001 certified [40]. | Secure storage for intellectual property protection [40]. | Generative AI models that automatically adapt to user data [40]. | Not specified in search results. |
| CDD Vault | Not specified in search results. | Not specified in search results. | Integrated deep learning tools; secure real-time data sharing with global partners [78]. | Role-based access for collaborators [78]. |
| OpenEye ORION | Not specified in search results. | World-class data security for cloud-native platform [78]. | Web-browser access enabling secure collaboration without data transfer [78]. | Not specified in search results. |
| Schrödinger | Not specified in search results. | Not specified in search results. | Live Design as central collaboration platform with seamless data sharing [78]. | Not specified in search results. |
These implementations reflect a growing industry recognition that robust security is not just a compliance requirement but a competitive advantage that enables wider collaboration and protects valuable intellectual property throughout the drug discovery pipeline [67] [40].
Experimental Validation of PETs in Collaborative Drug Discovery
Methodology for Federated Learning Implementation
The validation of PETs in real-world scenarios requires carefully designed experimental protocols. The following methodology outlines a standardized approach for implementing and evaluating federated learning in multi-institutional drug discovery projects, based on successful implementations like the MELLODDY project [77]:
Participant Onboarding: Each participating institution (pharmaceutical companies, research centers) establishes a secure local computing environment capable of running the federated learning client software. This environment must have access to the local proprietary dataset (e.g., compound libraries, assay results) [77].
Model Architecture Standardization: All participants agree on a standardized neural network architecture and initial weights. The model is typically designed for specific prediction tasks relevant to drug discovery, such as compound potency prediction, ADMET property forecasting (Absorption, Distribution, Metabolism, Excretion, Toxicity), or target binding affinity estimation [77] [79].
Federated Learning Cycle:
- Local Training: Each participant trains the model on their local dataset for a predetermined number of epochs without transferring any raw data outside their secure environment.
- Parameter Aggregation: Participants send only the model weight updates (gradients) to a central aggregation server. These updates are encrypted in transit using transport layer security (TLS) or more advanced encryption schemes [77].
- Secure Aggregation: The central server employs secure aggregation protocols (potentially combining federated learning with secure multi-party computation) to combine weight updates from multiple participants without exposing any single participant's updates [77].
- Model Distribution: The server distributes the updated global model back to all participants for the next training cycle.
Performance Validation: Model performance is evaluated against held-out test sets at each participating site, with participants sharing only aggregate performance metrics (e.g., AUC-ROC, precision-recall curves) to monitor collective improvement [77] [79].
Validation Metrics and Outcomes
The success of PET implementations is measured through both technical performance and privacy preservation metrics:
Table 3: Federated Learning Validation Metrics from the MELLODDY Project
| Validation Metric | Traditional Centralized Approach | Federated Learning Implementation | Privacy Advantage |
|---|---|---|---|
| Model Performance (AUC-ROC) | Baseline | Improved predictive performance for drug candidate screening [77]. | Competitive performance achieved without data pooling. |
| Data Sovereignty | Compromised (requires data sharing) | Maintained (data remains on-premises) [77]. | Complete preservation of data confidentiality. |
| Regulatory Compliance | Challenging for cross-border data transfer | Facilitated (minimized data transfer) [77]. | Simplified compliance with GDPR, HIPAA. |
| Collaborative Scale | Limited by data sharing agreements | Enabled collaboration among 10 pharmaceutical companies [77]. | Enabled previously impossible collaborations. |
The experimental results from implementations like MELLODDY demonstrate that federated learning can achieve superior predictive performance for drug candidate screening compared to models trained on single datasets, while completely avoiding the privacy and intellectual property concerns associated with traditional centralized data pooling [77].
Visualization of Integrated Secure Workflow for AI-Based Drug Discovery
The following diagram illustrates how various Privacy-Enhancing Technologies integrate into a comprehensive secure workflow for AI-based drug discovery, connecting distributed data sources with collaborative model development while maintaining end-to-end data protection:
This workflow demonstrates how multiple PETs can be combined to create a comprehensive privacy-preserving framework. The distributed data sources maintain control over their sensitive information while still contributing to collective model improvement through encrypted parameter sharing and privacy-protected analytics [77].
Essential Research Reagent Solutions for Secure AI Drug Discovery
Implementing robust privacy and security measures in AI-driven drug discovery requires both technical solutions and organizational frameworks. The following table details key components of a comprehensive security strategy for data-intensive research environments:
Table 4: Essential Solutions for Secure AI Drug Discovery Workflows
| Solution Category | Specific Tools/Technologies | Function/Purpose | Implementation Examples |
|---|---|---|---|
| Technical Safeguards | Federated Learning Platforms [77] | Enables collaborative model training without data sharing. | MELLODDY project for multi-company drug discovery [77]. |
| Homomorphic Encryption Libraries [77] | Allows computation on encrypted data. | Secure genomic analysis for precision medicine [77]. | |
| Differential Privacy Tools [77] | Adds statistical noise to prevent re-identification. | Census data publication; clinical trial data sharing [77]. | |
| Administrative Controls | Zero-Trust Security Model [76] | Requires continuous verification of all users and devices. | Protection for AI-driven healthcare environments [76]. |
| AI Governance Framework [67] | Establishes policy and controls for AI risks. | Context-based risk assessment for drug development [67]. | |
| Security Certifications (e.g., ISO 27001, SOC2) [67] [40] | Independent validation of security practices. | deepmirror's ISO 27001 certification [40]. | |
| Physical & Network Security | Advanced Threat Detection Systems [76] | Proactively identifies and responds to cyber threats. | AI-powered SIEM solutions for healthcare networks [76]. |
| Cloud Security Configurations | Protects data in cloud-based discovery platforms. | OpenEye ORION's cloud-native security [78]. |
The implementation of these solutions creates a defense-in-depth strategy that addresses privacy, confidentiality, and cybersecurity from multiple angles, ensuring that AI drug discovery workflows can leverage sensitive data while minimizing risks to both patient privacy and valuable intellectual property [67] [77] [76].
The integration of robust privacy, confidentiality, and cybersecurity measures is not merely a compliance requirement but a fundamental enabler of innovation in AI-driven drug discovery. As the field progresses toward more data-intensive workflows and increased collaboration, the implementation of Privacy-Enhancing Technologies (PETs) and comprehensive security frameworks will become increasingly critical for validating AI models across distributed datasets [67] [77].
The experimental validation of these technologies in projects like MELLODDY demonstrates that secure collaboration is not only possible but can yield superior scientific outcomes compared to isolated research efforts [77]. Future advancements will likely focus on improving the scalability and accessibility of PETs, establishing clearer regulatory guidelines for their use, and developing standardized validation protocols that can accelerate their adoption across the pharmaceutical industry [67] [77]. By building these privacy and security considerations into the foundation of AI drug discovery workflows, researchers can harness the power of sensitive data while maintaining the trust of patients, regulators, and research partners.
Implementing Continuous Monitoring and Active Learning for Sustained Model Performance
In the high-stakes field of AI-based drug discovery, the initial performance of a model is no guarantee of its long-term reliability. Model decay from data shifts and the prohibitive cost of experimental validation make continuous monitoring and active learning not just advantageous but essential components of a robust validation framework. This guide objectively compares the performance of emerging active learning strategies and continuous monitoring protocols, providing researchers with the experimental data and methodologies needed to sustain model performance from initial discovery to clinical application.
Experimental Comparison of Active Learning Strategies
Active learning (AL) strategically selects the most informative data points for experimental testing, optimizing the use of limited resources. The following experiments, conducted on public datasets, benchmark several state-of-the-art batch active learning methods against traditional approaches.
Benchmarking on ADMET and Affinity Prediction Tasks
A 2024 study evaluated novel AL batch selection methods against established techniques across multiple property prediction tasks relevant to drug discovery [80]. The experiments used several public datasets, including:
- Caco-2: 906 drugs for cell permeability prediction.
- Aq. Solubility: 9,982 small molecules for solubility prediction.
- Lipophilicity: 1,200 small molecules.
- Affinity Data: 10 large datasets from ChEMBL and internal sources [80].
The results, detailed in the table below, show the root mean square error (RMSE) achieved by different methods as the number of experimental samples increases.
Table 1: Performance Comparison (RMSE) of Active Learning Methods on ADMET Datasets [80]
| Dataset (Target Size) | Method Type | Method Name | RMSE after ~300 Samples | RMSE after ~600 Samples | Key Advantage |
|---|---|---|---|---|---|
| Caco-2 (906) | Novel (Proposed) | COVDROP | ~0.38 | ~0.36 | Best overall performance & data efficiency |
| Novel (Proposed) | COVLAP | ~0.41 | ~0.38 | Strong performance, best for some targets | |
| Existing | BAIT | ~0.43 | ~0.40 | Probabilistic sample selection | |
| Existing | k-Means | ~0.46 | ~0.42 | Diversity-based selection | |
| Baseline | Random | ~0.52 | ~0.45 | No active learning | |
| Aq. Solubility (~10k) | Novel (Proposed) | COVDROP | ~1.55 | ~1.15 | Fastest convergence |
| Novel (Proposed) | COVLAP | ~1.75 | ~1.30 | ||
| Existing | BAIT | ~1.90 | ~1.45 | ||
| Baseline | Random | ~2.30 | ~1.80 | ||
| PPBR (~1.7k) | Novel (Proposed) | COVDROP | ~85 | ~70 | Effective on highly skewed data |
| Baseline | Random | ~105 | ~90 |
Experimental Protocol [80]:
- Models: Graph neural networks and other deep learning models.
- AL Framework: Batch active learning with a fixed batch size of 30.
- Process: Iteratively, each AL method selects a batch of samples from an unlabeled pool. An "oracle" (the dataset) provides labels, and the model is retrained. This repeats until the dataset is exhausted.
- Evaluation Metric: RMSE is calculated on a fixed test set after each batch is added to the training set.
Ultra-Low Data Screening for Hit Discovery
Addressing the needs of resource-limited labs, a 2025 study tested AL strategies starting from only 110 molecular affinity evaluations [81]. The experiment used docking scores from the DTP and Enamine DDS-10 libraries as a proxy for experimental measurements.
Table 2: Performance of AL in Ultra-Low Data Regime (After 110 Samples) [81]
| Metric | DTP Dataset | Enamine DDS-10 Dataset |
|---|---|---|
| Optimal AL Setup | CDDD Descriptor + MLP Model + PADRE Augmentation | CDDD Descriptor + MLP Model + PADRE Augmentation |
| Probability of Finding ≥5 Top-1% Hits | 97% | 100% |
| Impact of Prior Knowledge | Adding a single known hit molecule to the initial dataset further increases success probability. |
Experimental Protocol [81]:
- Models & Descriptors: 20 combinations of machine learning models (e.g., MLP, Random Forest) and molecular descriptors (e.g., ECFP, CDDD) were evaluated.
- AL Query Strategy: Uncertainty-based sampling was used to select the most informative molecules for the next "experimental" round (docking simulation).
- Data Augmentation: The PADRE (Pairwise Difference Regression) technique was used to augment the limited training data.
- Evaluation Metric: The probability of discovering a specified number of top-scoring molecules (hits) was calculated over multiple simulation runs.
Active Learning for Synergistic Drug Combination Discovery
A January 2025 study focused on the challenge of rare events, specifically finding synergistic drug pairs [82]. The research explored how different components of an AL framework impact its efficiency.
Key Quantitative Findings [82]:
- Molecular Encoding: The choice of molecular fingerprint (e.g., Morgan, MAP4) had a limited impact on prediction quality. Morgan fingerprint with a simple sum operation performed best.
- Cellular Context: Using gene expression profiles of the targeted cell line as a feature significantly improved predictions (0.02-0.06 gain in PR-AUC) compared to using drug features alone.
- Batch Size: AL discovered 60% of synergistic drug pairs by exploring only 10% of the combinatorial space. Smaller batch sizes yielded a higher synergy ratio, and dynamic tuning of the exploration-exploitation strategy further enhanced performance.
- Data Efficiency: A parameter-light algorithm (Logistic Regression) was outperformed by a medium-parameter neural network (3 layers, 64 hidden neurons) as the training set size increased.
Detailed Experimental Protocols
To ensure reproducibility, here are the detailed methodologies for the key experiments cited.
Protocol 1: Batch Active Learning for ADMET Optimization
This protocol is based on the study that produced the results in Table 1 [80].
- Data Preparation: Split the entire dataset into a hold-out test set (e.g., 20%) and an initial unlabeled pool (e.g., 80%). A very small seed set (e.g., 1% of the pool) is randomly selected to train the initial model.
- Model Configuration:
- Use a graph neural network or other deep learning model suitable for molecular data.
- For COVDROP: Enable Monte Carlo (MC) Dropout at inference to perform stochastic forward passes (e.g., 100 times) to estimate prediction uncertainty (epistemic variance).
- For COVLAP: Use a Laplace approximation to estimate the posterior distribution of the model parameters and compute the predictive uncertainty.
- Batch Selection:
- For covariance-based methods (COVDROP, COVLAP): Compute the covariance matrix between predictions on all samples in the unlabeled pool. Greedily select the batch of samples that maximizes the log-determinant (joint entropy) of the corresponding sub-matrix. This balances high uncertainty and diversity.
- For BAIT: Select samples that maximize the Fisher information of the model parameters.
- For k-Means: Cluster the unlabeled data in the feature space and select samples from the cluster centroids.
- Iterative Loop:
- The selected batch is "labeled" (their ground-truth values are retrieved from the oracle/hold-out data).
- The model is retrained on the accumulated training set.
- Model performance (RMSE) is evaluated on the fixed test set.
- The process repeats until the unlabeled pool is empty or a performance threshold is met.
Protocol 2: Continuous Monitoring for Model Fairness and Stability
This protocol outlines a general framework for continuous monitoring, a critical supplement to active learning [83].
- Establish Baseline Performance: Define key performance indicators (KPIs) like RMSE, R², and fairness metrics (e.g., demographic parity, equality of opportunity) on a validated baseline model and dataset.
- Implement Automated Monitoring:
- Data Drift Detection: Use statistical tests (e.g., Kolmogorov-Smirnov) on feature distributions between training and incoming production data.
- Concept Drift Detection: Monitor for degradation in prediction accuracy (e.g., increasing RMSE) on a freshly labeled, held-out validation set.
- Bias Detection: Continuously compute fairness metrics across sensitive subgroups (e.g., different demographic groups in clinical trial data).
- Set Alerting Thresholds: Predefine thresholds for all monitored metrics. Trigger alerts when metrics deviate beyond acceptable ranges.
- Create a Feedback Loop: When an alert is triggered, initiate a diagnostic process. This may involve curating new data, retraining the model with active learning, or pausing the model's deployment for a full audit.
Workflow Visualization
The following diagram illustrates the integrated cyclical process of active learning and continuous monitoring for sustained model performance.
The Scientist's Toolkit: Essential Research Reagents & Solutions
This table details key software, datasets, and computational tools essential for implementing the experiments and strategies discussed in this guide.
Table 3: Key Reagents and Computational Tools for AI Drug Discovery Validation
| Item Name | Type | Function/Brief Explanation | Example/Reference |
|---|---|---|---|
| DeepChem | Software Library | An open-source toolkit for deep learning in drug discovery, providing implementations of various molecular featurizers, models, and workflows. | [80] |
| GeneDisco | Software Library | An open-source benchmark suite for active learning in transcriptomics; a model for similar validation in drug discovery. | [80] |
| CHEMBL | Database | A large, open-access bioactivity database for training and benchmarking predictive models on affinity and ADMET properties. | [80] |
| DTP & DDS-10 | Compound Libraries | Realistic compound libraries (Developmental Therapeutics Program, Enamine) used for validating active learning in hit discovery. | [81] |
| Oneil & ALMANAC | Dataset | Benchmark datasets for synergistic drug combination screening, used for training and evaluating active learning algorithms. | [82] |
| Morgan Fingerprints | Molecular Descriptor | A standard molecular representation (circular fingerprint) that captures molecular structure and was shown to be effective in AL. | [82] |
| CDDD Descriptors | Molecular Descriptor | Continuous and Data-Driven Descriptors that provide a continuous representation of molecules, optimal for certain ML models. | [81] |
| PADRE | Data Augmentation | Pairwise Difference Regression technique that generates synthetic training data by considering differences between molecules. | [81] [80] |
Proving Value: A Framework for Rigorous Validation and Comparative Analysis of AI Models
The integration of artificial intelligence (AI) into pharmaceutical research represents a paradigm shift, moving the industry from labor-intensive, sequential workflows toward data-driven, predictive discovery engines. This transition necessitates a new framework for performance evaluation. Establishing robust Key Performance Indicators (KPIs) is critical for objectively validating AI-based drug discovery models, quantifying their impact, and guiding future investment. Within the broader thesis of AI model validation, these KPIs move beyond theoretical promise to provide tangible, data-driven proof of efficacy. For researchers and development professionals, this translates into a need for metrics that directly compare AI-assisted workflows against traditional benchmarks across the core dimensions of speed, cost, and success rates. This guide synthesizes the most current performance data and experimental methodologies to establish a standardized basis for this comparison, providing a foundational toolkit for the rigorous validation of AI technologies in a real-world R&D context.
Quantitative Performance Comparison: AI vs. Traditional Methods
The validation of any new technology requires a clear quantitative comparison against established standards. The following data, compiled from recent industry analyses and clinical pipelines, provides a benchmark for evaluating the performance of AI-driven drug discovery.
Table 1: Overall R&D Impact: AI vs. Traditional Drug Discovery
| Performance Metric | Traditional Discovery | AI-Driven Discovery | Data Source & Year |
|---|---|---|---|
| Average Timeline | 10-15 years [84] [45] | 3-6 years (potential) [79] | Industry Analysis (2025) |
| Average Cost per Approved Drug | >$2.6 billion [85] [45] | Up to 70% cost reduction [79] | Industry Analysis (2025) |
| Phase I Success Rate | 40-65% [86] [79] | 80-90% [86] [79] | AllAboutAI (2025) |
| Preclinical Attrition | ~90% failure rate [87] [79] | Preclinical costs cut by 25-50% [86] | BCG, Deloitte (2024-2025) |
| Lead Optimization Compounds | 2,500-5,000 compounds over 5 years [79] | 136 compounds to candidate in 1 year (Exscientia example) [1] | Company Report (2025) |
Table 2: Stage-Wise Efficiency Gains with AI
| R&D Stage | Key AI Efficiency Metric | Impact & Example |
|---|---|---|
| Target Identification | 70% timeline reduction (2-3 years → 6-12 months) [86] | Insilico Medicine: AI target discovery for fibrosis drug [87] [1]. |
| Molecule Design & Optimization | 70% faster design cycles; 10x fewer synthesized compounds [1] | Exscientia: AI-designed CDK7 inhibitor candidate from 136 compounds [1]. |
| Preclinical Testing | 30% timeline reduction (3-6 years → 2-4 years) [86] | AI predictive models for toxicity and ADME properties slash lab testing needs [48] [79]. |
| Clinical Trial Design | 25% reduction via optimized patient selection [86] | AI analysis of EHRs and real-world data for improved patient stratification [85]. |
The data reveals a dramatic compression of timelines and costs, particularly in the early discovery phases. The most striking statistic is the Phase I success rate for AI-discovered drugs, reported at 80-90%, which is more than double the historical industry average [86] [79]. This suggests that AI models are significantly de-risking early clinical development by selecting candidates with superior biological properties. Furthermore, specific use cases, such as Exscientia's development of a clinical candidate with only 136 synthesized compounds, demonstrate a fundamental shift in efficiency compared to the thousands typically required in traditional medicinal chemistry [1].
Experimental Protocols for KPI Validation
To validate the KPIs presented above, a rigorous experimental approach is required. The following protocols detail the methodologies used by leading AI drug discovery platforms to generate their reported results.
Protocol 1: AI-Driven Target Identification and Validation
Objective: To systematically identify and prioritize novel, druggable disease targets using multi-modal data integration and machine learning.
Workflow Overview:
Methodology Details:
- Data Ingestion: The protocol begins with the aggregation of heterogeneous datasets. This includes genomic, transcriptomic, and proteomic data from public repositories (e.g., TCGA, GTEx) and proprietary sources; textual data from millions of scientific publications and patents processed via Natural Language Processing (NLP); and clinical and pathway data from databases like ClinicalTrials.gov and Reactome [1] [88].
- Target Hypothesis Generation: Machine learning models, including transformer-based architectures, analyze this integrated data to identify genes and proteins with strong causal links to the disease pathology. For instance, Insilico Medicine's PandaOmics module is reported to leverage 1.9 trillion data points from over 10 million biological samples [88].
- Knowledge Graph Integration: The generated hypotheses are contextualized within a large-scale knowledge graph that encodes relationships between genes, diseases, compounds, and biological pathways. This graph is used to infer novel connections and assess the biological plausibility of a target [88].
- AI-Powered Prioritization: Targets are scored and ranked using algorithms that weigh factors such as disease association strength, druggability, novelty, and competitive landscape. This multi-objective optimization ensures the final list is both scientifically compelling and commercially viable [88].
- Experimental Validation: Top-ranked targets undergo rigorous laboratory validation. This often involves gene knockdown/knockout in disease-relevant cell models to observe phenotypic changes, followed by validation in more complex systems such as patient-derived organoids or in vivo models [1].
Protocol 2: Generative AI for de Novo Molecular Design
Objective: To generate novel, synthetically accessible small molecules optimized for specific target profiles, potency, selectivity, and ADMET properties.
Workflow Overview:
Methodology Details:
- Target Product Profile (TPP) Definition: The process is initiated by defining a multi-parameter TPP, which includes desired potency (e.g., IC50), selectivity over related targets, and optimal ranges for ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) properties [1] [88].
- Generative Molecular Design: AI models generate novel molecular structures that satisfy the TPP. Common techniques include:
- Generative Adversarial Networks (GANs) and Reinforcement Learning (RL): Used by platforms like Insilico Medicine's Chemistry42 to explore chemical space and optimize compounds against multiple objectives [88].
- Graph Neural Networks (GNNs): Treat molecules as graphs (atoms as nodes, bonds as edges) to generate structurally valid and novel compounds [45].
- Reaction-Aware Models: Systems like Iambic Therapeutics' Magnet ensure that generated molecules are synthetically feasible by incorporating chemical reaction knowledge [88].
- In Silico Property Prediction: Before synthesis, virtual candidates are screened using predictive AI models. These models forecast critical properties, achieving 75-90% accuracy in toxicity prediction and 60-80% accuracy in efficacy forecasting [86]. This step drastically reduces the number of compounds that require physical testing.
- Synthesis and Testing: The top-ranking virtual compounds are synthesized and tested in high-throughput biochemical and cellular assays. Companies like Exscientia have integrated robotic "AutomationStudio" facilities to accelerate this phase [1].
- Iterative Refinement: Data from biological testing is fed back into the AI models in a closed-loop Design-Make-Test-Analyze (DMTA) cycle, allowing the system to learn and improve its design strategy with each iteration [1] [88].
The Scientist's Toolkit: Essential Research Reagents & Solutions
The experimental validation of AI-generated hypotheses relies on a suite of critical reagents and platforms. The following table details key solutions essential for conducting the protocols described above.
Table 3: Essential Research Reagent Solutions for AI Drug Discovery Validation
| Reagent / Solution | Function in Validation | Specific Application Example |
|---|---|---|
| PandaOmics (Insilico Medicine) | AI-powered target discovery platform | Multi-modal data analysis for novel target identification and prioritization [88]. |
| Chemistry42 (Insilico Medicine) | Generative chemistry AI platform | de novo design of small molecules optimized for multiple parameters (potency, ADMET) [88]. |
| Recursion OS Platform | Phenomics-based drug discovery platform | Maps biological relationships using high-content cellular imaging and AI analysis [1] [88]. |
| Patient-Derived Organoids / Tissues | Biologically relevant disease models | Ex vivo validation of targets and compound efficacy in a human, patient-specific context [1]. |
| Cloud AI/ML Platforms (e.g., AWS, Google Cloud) | Scalable computational infrastructure | Provides the high-performance computing power required for training and running large AI models [1]. |
| Federated Data Platforms (e.g., Lifebit) | Secure, multi-institutional data analysis | Enables AI training on distributed, sensitive datasets (e.g., genomic data) without moving them, ensuring privacy and compliance [79]. |
The empirical data and experimental protocols presented provide a robust framework for establishing KPIs to validate AI-based drug discovery models. The evidence consistently demonstrates that well-validated AI platforms can deliver substantial improvements, most notably a dramatic increase in Phase I success rates and a significant compression of discovery timelines and costs. However, the ultimate KPI—regulatory approval of a novel AI-discovered drug—remains a future milestone. As the field matures, the focus for researchers and professionals must shift from validating isolated AI predictions to establishing holistic, end-to-end performance metrics that capture the full value of these transformative technologies. The ongoing integration of AI, not as a replacement but as a powerful co-pilot to human expertise, is steadily rewriting the economics and success probabilities of pharmaceutical R&D.
The pharmaceutical industry stands at the precipice of a technological revolution, driven by the integration of artificial intelligence into the drug discovery process. This comparative analysis examines the performance of AI-discovered and traditionally discovered drug candidates within the broader thesis of validating AI-based drug discovery models. For researchers and drug development professionals, understanding this paradigm shift is crucial for strategic planning and resource allocation.
AI's potential to revolutionize drug discovery stems from its ability to analyze vast datasets, identify complex patterns, and generate novel hypotheses at a scale and speed unattainable through conventional methods [89]. Traditional drug discovery has relied heavily on serendipity, trial-and-error experimentation, and high-throughput screening, processes that are notoriously time-consuming, costly, and inefficient [15]. The emergence of AI technologies, including machine learning, deep learning, and natural language processing, promises to address these fundamental limitations by bringing unprecedented computational power and predictive accuracy to the discovery pipeline.
This analysis will provide a comprehensive, data-driven comparison of both approaches, focusing on key performance indicators such as development timelines, success rates, cost efficiency, and clinical trial outcomes. By synthesizing the most current statistical evidence and experimental validations, we aim to provide an objective assessment of AI's transformative impact on pharmaceutical research and development.
Efficiency and Cost Analysis
The integration of artificial intelligence has fundamentally altered the economic and temporal landscape of drug discovery. The data reveals substantial advantages for AI-driven approaches across multiple efficiency metrics compared to traditional methods.
Development Timelines
Table 1: Comparison of Development Timelines
| Development Phase | Traditional Discovery | AI-Driven Discovery | Reduction |
|---|---|---|---|
| Target Identification | 2-3 years | 6-12 months | 70% |
| Lead Optimization | 2-4 years | 1-2 years | 50% |
| Preclinical Testing | 3-6 years | 2-4 years | 30% |
| Overall Process | 10-15 years | 1-2 years (optimal cases) | Up to 60% |
Traditional drug development typically requires 10-15 years from discovery to market, but AI is dramatically collapsing this timeline to as little as 1-2 years in optimal scenarios [58] [86]. Even under more conservative estimates, AI-assisted projects achieve timelines that are 40-60% faster than conventional methods. This acceleration is most pronounced in the early discovery phases, where AI can rapidly analyze complex biological data to identify promising targets and candidates.
Cost Implications
Table 2: Cost Reduction Analysis by Development Stage
| Development Stage | Traditional Cost | AI-Driven Cost | Reduction |
|---|---|---|---|
| Compound Screening | Baseline | 60-80% lower | 60-80% |
| Lead Optimization | Baseline | 40-60% lower | 40-60% |
| Toxicology Testing | Baseline | 30-50% lower | 30-50% |
| Clinical Trial Design | Baseline | 25-40% lower | 25-40% |
| Overall Preclinical R&D | Baseline | 25-50% lower | 25-50% |
AI technologies generate substantial cost savings throughout the drug development pipeline, with analyses indicating 25-50% reduction in overall preclinical R&D costs [58] [86]. The most significant savings occur in compound screening, where virtual screening approaches reduce expenses by 60-80% compared to traditional high-throughput physical screening methods. These economic advantages make drug discovery more accessible and sustainable, particularly for smaller organizations and academic institutions.
Hit Rate Efficiency
The efficiency of identifying promising drug candidates represents one of AI's most significant advantages. Traditional high-throughput screening typically achieves hit rates between 0.01% and 0.14%, whereas AI-powered virtual screening consistently delivers hit rates between 1% and 40% – representing a 10 to 400-fold improvement in screening efficiency [86].
A notable case study demonstrates this dramatic improvement: AI-powered systems boosted hit-to-lead conversion rates from under 1% in random screening to over 40% in targeted JAK2 inhibitor development [86]. This leap in precision directly translates to reduced resource consumption and accelerated project timelines.
Clinical Trial Performance
The transition from preclinical discovery to clinical validation represents the most critical phase for any therapeutic candidate. Comparative analysis of clinical trial performance reveals significant differences between AI-discovered and traditionally developed drugs.
Success Rates by Phase
Table 3: Clinical Trial Success Rate Comparison
| Trial Phase | Traditional Discovery | AI-Driven Discovery | Improvement |
|---|---|---|---|
| Phase I | 40-65% | 80-90% | 2× higher |
| Phase II | 30-40% | ~40% (limited data) | Promising early signs |
| Phase III | 58-85% | Insufficient data | Unknown |
AI-discovered drugs demonstrate remarkably higher success rates in early-stage clinical trials, achieving 80-90% success rates in Phase I compared to 40-65% for traditional drugs [86]. This represents more than a doubling of success probability at this critical initial stage of human testing. The limited dataset for Phase II trials shows comparable performance between approaches, while Phase III data for AI-discovered drugs remains insufficient for meaningful statistical analysis as of 2025.
By December 2023, 24 AI-discovered molecules had completed Phase I trials, with 21 successful outcomes, confirming the 87.5% success rate [86]. This performance is particularly significant given that historical data shows 60-90% of traditionally discovered candidates fail during early clinical stages.
Attrition Rates and Regulatory Progress
The improved clinical performance of AI-discovered candidates reflects fundamental advantages in molecular design. AI-designed molecules typically demonstrate superior properties, including enhanced toxicity profiles, improved bioavailability, better target specificity, and optimized pharmacokinetics [86]. These characteristics directly address the primary causes of clinical failure that have plagued traditional drug development.
While regulatory approvals for AI-discovered drugs are still emerging, progress is accelerating. Significant milestones include Unlearn.ai receiving EMA qualification for digital twin technology in clinical trials, the FDA launching Elsa LLM to accelerate protocol reviews, and NIH developing TrialGPT to match patients with clinical trials [86]. These developments indicate that regulatory bodies are actively adapting to AI-driven pipelines.
Case Study: Experimentally Validated AI Discovery
A landmark study published in October 2025 provides compelling experimental validation of AI-driven drug discovery, demonstrating a complete cycle from computational prediction to laboratory confirmation.
Research Background and Methodology
Researchers from Yale University, Google Research, and Google DeepMind achieved a milestone in computational biology by using a large language model to predict a previously unknown drug mechanism that was subsequently validated through laboratory experiments [90]. The research centered on C2S-Scale, a family of language models trained to interpret single-cell RNA sequencing data by converting gene expression profiles into text-based "cell sentences."
Technical Implementation:
- Model Architecture: The team scaled models up to 27 billion parameters trained on over 50 million cellular profiles [90]
- Data Processing: The Cell2Sentence framework converted gene expression profiles into ranked lists of gene names, creating "cell sentences" that preserve relative expression levels while allowing integration with textual biological knowledge [90]
- Training Data: The system was trained on over one billion tokens of transcriptomic data combined with biological text and metadata [90]
- Performance Enhancement: The team enhanced prediction accuracy through reinforcement learning techniques that aligned model outputs with biological objectives, such as accurately predicting interferon response programs [90]
Experimental Workflow and Validation
The virtual screening experiment was designed to identify compounds that enhance antigen presentation in immune cells. The model predicted that silmitasertib, a kinase inhibitor, would amplify MHC-I expression specifically in the presence of low-level interferon signaling – a context-dependent mechanism previously unreported in scientific literature [90].
AI-Driven Discovery Workflow
When tested in human neuroendocrine cell models that were entirely absent from the training data, the prediction was conclusively confirmed: silmitasertib alone showed no effect, but when combined with low-dose interferon, it produced substantial increases in antigen presentation markers, with effects ranging from 13.6% to 37.3% depending on interferon type and concentration [90].
Significance and Implications
This discovery validates several groundbreaking aspects of AI-driven drug discovery:
- Novel Mechanism Identification: The AI model identified a previously unknown, context-specific biological mechanism that might have been missed in standard assays [90]
- Conditional Biology Exploration: The system demonstrated capability to ask what works differently depending on cellular environment, representing a fundamental shift in how therapeutic candidates can be identified [90]
- Cross-Domain Application: The research demonstrates how advances in natural language processing can enable progress in biology when cellular data is appropriately formatted [90]
The implications for cancer immunotherapy are particularly promising. Neuroendocrine cancers, including the Merkel cell and small cell lung cancer models used for validation, often evade immune surveillance by downregulating antigen presentation machinery. The discovery that silmitasertib can amplify interferon-driven MHC-I expression suggests potential combination therapy approaches that could enhance immunotherapy responses in these difficult-to-treat malignancies [90].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Platforms
| Tool/Solution | Function | Application in AI-Driven Discovery |
|---|---|---|
| C2S-Scale Models | Interpret single-cell RNA sequencing data | Predicts cellular responses to drugs across different biological contexts [90] |
| Panoramic Datasets | Provide longitudinal, frequently refreshed data | Enables research dynamically assessing disease progression and treatment response [91] |
| scFID Metric | Evaluate generative models in transcriptomics | Adapts techniques from computer vision to biological data assessment [90] |
| Standardized Verification Protocols | Ensure data quality and reproducibility | Addresses limitations of literature-derived datasets with missing experimental details [92] |
| Balanced Activity Datasets | Include both active and inactive compounds | Prevents AI model bias and reduces false-positive predictions [92] |
The implementation of AI-driven discovery requires specialized research reagents and computational tools. Single-cell RNA sequencing platforms form the foundation for generating the cellular profiling data that powers models like C2S-Scale [90]. For validation, rigorously curated datasets such as Flatiron's Panoramic datasets, which contain 1.5 billion data points with expert curation, serve as gold standards for training and testing AI models [91].
Critical to success are comprehensive datasets that include both active and inactive compounds, as public databases overwhelmingly contain active compounds while unsuccessful experiments remain unpublished, leading AI models to overpredict activity and produce high false-positive rates [92]. The ChemDiv dataset case study demonstrated dramatic improvement in model performance, with accuracy increasing from 0.35 to 0.8 and Cohen Kappa Score improving from 0.044 to 0.565 for hERG inhibition prediction after integrating verified experimental data with balanced activity representation [92].
Discussion
The comparative analysis reveals substantial advantages for AI-driven drug discovery across multiple dimensions. AI-discovered candidates demonstrate superior early-stage clinical success rates, significantly reduced development timelines, and markedly improved cost efficiency. The experimental validation of AI-predicted mechanisms, such as the silmitasertib-interferon synergy in enhancing antigen presentation, provides compelling evidence for AI's ability to generate novel biological insights [90].
The validation of AI-based drug discovery models depends on multiple factors, including data quality, algorithmic sophistication, and experimental confirmation. The case study demonstrates a complete validation cycle, from computational prediction through laboratory confirmation in cell models absent from training data [90]. This represents a significant milestone in establishing the predictive validity of AI approaches.
Limitations and Challenges
Despite promising results, several challenges remain for AI-driven drug discovery:
- Data Limitations: Public datasets often lack standardized verification, have inconsistent experimental conditions, and contain significant gaps in chemical space coverage [92]
- Clinical Validation: While Phase I success rates are impressive, limited data exists for later-stage clinical trials, with no AI-discovered drugs receiving FDA approval as of 2024 [86]
- Implementation Costs: Hidden infrastructure, development, and operational expenses push AI implementation costs to $25,000–$100,000 per use case, straining budgets despite long-term savings [86]
- Explainability: The "black box" nature of some complex AI models creates challenges for interpreting predictions and building scientific understanding [15]
Future Outlook
The trajectory of AI in drug discovery points toward continued growth and refinement. By 2025, 30% of all new drug discoveries are projected to incorporate AI technologies, representing a 400% increase from 2020 levels [86]. The industry is shifting from anticipating breakthrough generative AI models to optimizing mature deployments to deliver validated, reliable value in specific use cases [91].
Future advancements will likely focus on integrating additional data types such as spatial transcriptomics, proteomics, and clinical outcomes to improve predictive accuracy [90]. As biological datasets continue to grow and AI systems become more sophisticated, opportunities for computational hypothesis generation and in silico experimentation will expand, further accelerating the discovery of novel therapeutics.
The convergence of AI-driven discovery with personalized medicine represents a particularly promising frontier, enabling the development of treatments tailored to individual patient characteristics and potentially revolutionizing how we approach disease treatment and prevention.
Benchmarking Against Established Tools and Legacy Computational Methods
The validation of AI-based drug discovery models hinges on rigorous benchmarking against established computational tools. The rapid evolution of artificial intelligence presents both a paradigm shift and a practical challenge: demonstrating quantifiable superiority over legacy methods that have long underpinned computer-aided drug design (CADD). This guide objectively compares the performance of modern AI platforms against traditional computational methods through experimental data and defined protocols, providing researchers with a framework for evaluating these technologies.
Defining the Methodological Divide: Legacy CADD vs. Modern AI
The fundamental distinction between traditional computational tools and modern AI-driven platforms lies in their core approach to modeling biology and chemistry.
Legacy CADD methods are largely founded on principles of biological reductionism. They are hypothesis-driven and excel at specific, modular tasks within the drug discovery pipeline. [88] These include:
- Structure-based methods: Such as molecular docking, which predicts how a small molecule fits into a protein's binding pocket. [88] [93]
- Ligand-based methods: Including Quantitative Structure-Activity Relationship (QSAR) models, which use molecular descriptors and statistical methods to predict activity based on chemical structure. [88] [93]
These methods typically work with smaller, well-structured datasets and rely heavily on human-defined parameters and chemical rules. [88]
In stark contrast, modern AI-driven discovery (AIDD) attempts to model biology with a greater degree of holism. [88] This hypothesis-agnostic approach uses deep learning systems to integrate massive, multimodal datasets—including omics, phenotypic data, chemical structures, text from scientific literature, and clinical data—to construct comprehensive biological representations, such as massive knowledge graphs. [88] Furthermore, the generative capabilities of modern AI allow for the de novo design of novel molecular structures, moving beyond mere virtual screening of existing compound libraries. [88]
Quantitative Benchmarking: Performance Data and Case Studies
Benchmarking studies and real-world applications provide concrete evidence of the performance differential between these approaches. The data below summarizes key comparative metrics.
Table 1: Comparative Performance of Virtual Screening Methods
| Method / Platform | Screening Scale | Hit Rate | Timeframe | Key Outcome |
|---|---|---|---|---|
| Traditional HTS (Historic Example) [93] | 400,000 compounds | 0.021% (81 hits) | Months-Years | Baseline for comparison |
| Legacy vHTS (Historic Example) [93] | 365 compounds | ~35% (127 hits) | Weeks | 1,665x higher hit rate than HTS |
| Atomwise AtomNet (2024 Study) [5] | 318 targets | 74% success (novel hits for 235 targets) | Days | Identified structurally novel hits |
| Recursion OS (Phenom-2 Model) [88] | 8 billion images | 60% improvement in genetic perturbation separability | N/S | Enhanced biological insight from imaging |
| AI-Based Startups (General Capability) [94] | Variable | N/S | Days to Months | Identify and design new drugs |
N/S: Not Specified
A landmark historical case from Pharmacia (now Pfizer) exemplifies the efficiency of virtual screening. When searching for inhibitors of tyrosine phosphatase-1B, a traditional High-Throughput Screening (HTS) of 400,000 compounds yielded 81 hits—a 0.021% hit rate. In parallel, a structure-based virtual screen of only 365 compounds using legacy CADD methods yielded 127 hits, a ~35% hit rate, making it over 1,600 times more efficient at identifying active compounds. [93]
Modern AI platforms extend this advantage. A 2024 study of Atomwise's AtomNet platform demonstrated its capability as a viable alternative to HTS, with the AI identifying structurally novel hits for 235 out of 318 targets—a 74% success rate across a diverse target set. [5] In another domain, Recursion Pharmaceuticals reported that its Phenom-2 model, trained on 8 billion microscopy images, achieved a 60% improvement in genetic perturbation separability, a metric crucial for distinguishing different disease states. [88]
Table 2: Benchmarking AI Agent Performance in a Standardized Virtual Screening Challenge
| Solution Type | Agent / Model | DO Challenge Score (10-Hour) | Key Strategy |
|---|---|---|---|
| Human Expert | Top Solution | 33.6% | Active learning, spatial-relational neural networks |
| AI Agent | Deep Thought (o3-mini) | 33.5% | Strategic sampling & model selection |
| Human Team | Best DO Challenge 2025 Team | 16.4% | Varied, less optimized |
| AI Agent | Deep Thought (Gemini 2.0 Flash) | 5.7% | Suffered from tool underutilization |
The DO Challenge, a benchmark designed to evaluate AI agents in a virtual screening scenario, provides a direct comparison between human and AI performance under time-constrained conditions. The task was to identify the top 1,000 molecular structures from a library of one million based on a custom DO Score. [95]
As shown in Table 2, the top-performing AI agent, Deep Thought, nearly matched the performance of the leading human expert solution (33.5% vs. 33.6%) within a 10-hour development window, significantly outperforming the best human team from the DO Challenge 2025 competition. [95] The benchmark identified that high-performing solutions, both human and AI, shared common strategies: employing active learning for structure selection, using spatial-relational neural networks, and leveraging a strategic submission process. [95] However, the study also highlighted current limitations of AI agents, including instruction misunderstanding and failure to leverage multiple submissions strategically. [95]
Experimental Protocols for Benchmarking AI in Drug Discovery
For researchers aiming to conduct their own validation studies, understanding the standard protocols for benchmarking is essential. The following workflows outline a generalized structure for a comparative validation experiment.
Protocol 1: Virtual Screening Benchmark
This protocol evaluates the ability of a method to identify active compounds from a large library of decoys.
- Objective: To compare the virtual screening performance and enrichment efficiency of an AI platform against traditional docking and ligand-based similarity search methods.
- Dataset Curation:
- A set of known active compounds for a specific, well-characterized protein target (e.g., a kinase or GPCR) is collected from public databases like ChEMBL.
- A large set of decoy molecules, which are chemically similar but presumed inactive, is generated or sourced from libraries like ZINC.
- The combined library of actives and decoys is prepared for screening.
- Execution:
- The AI platform and legacy tools screen the entire library.
- Each method ranks the compounds based on its predicted likelihood of activity.
- Analysis:
- Primary Metric: Enrichment Factor (EF). This is calculated as the fraction of true actives found in the top X% of the ranked list divided by the fraction of actives expected from a random selection. EF1% and EF10% are standard metrics.
- Secondary Metrics: The computational time and resources required are recorded.
- Validation: The top-ranked compounds from each method, particularly those unique to each approach, are procured and tested in biochemical or cell-based assays to confirm activity.
Protocol 2: De Novo Molecule Generation Benchmark
This protocol assesses the ability of a platform to generate novel, drug-like compounds with specific desired properties.
- Objective: To evaluate the capability of a generative AI platform to create novel chemical matter with optimized properties compared to a legacy fragment-based or structure-based design method.
- Design Constraints:
- The compound must exhibit high predicted binding affinity (< 10 nM) for a specified target.
- The compound must adhere to drug-like property filters (e.g., Lipinski's Rule of Five, synthetic accessibility).
- Execution:
- The AI platform and the legacy method are used to generate a set number of candidate molecules (e.g., 1,000) under the defined constraints.
- Analysis:
- Diversity: Assess the structural and chemical diversity of the generated compound sets.
- Novelty: Measure the structural novelty of the generated compounds compared to known actives and existing compound libraries.
- Property Optimization: Evaluate how well the generated molecules meet the multi-objective constraints (potency, selectivity, ADMET properties).
- Validation: A subset of the generated compounds is synthesized, and their binding affinity and selectivity are experimentally validated.
Research Reagent Solutions for Computational Benchmarking
Executing these benchmarking protocols requires a suite of computational "reagents"—software tools, datasets, and infrastructure. The table below details key resources.
Table 3: Essential Research Reagents for Computational Benchmarking Studies
| Category | Item / Platform | Function in Benchmarking |
|---|---|---|
| AI Drug Discovery Platforms | Insilico Medicine - Pharma.AI [88] [96] | End-to-end suite for target ID (PandaOmics), molecule generation (Chemistry42), and trial prediction (InClinico). |
| Recursion OS [88] | Platform for analyzing biological and chemical datasets to identify novel targets and compounds. | |
| Atomwise - AtomNet [96] [5] | Structure-based deep learning for molecular modeling and predicting drug-target interactions. | |
| BenevolentAI [4] [96] | AI platform for identifying novel targets and drug repurposing opportunities using a massive knowledge graph. | |
| Legacy & Specialized CADD Tools | Molecular Operating Environment (MOE) [40] | All-in-one platform for molecular modeling, cheminformatics, and bioinformatics; a standard in legacy CADD. |
| Schrödinger Suite [40] [97] | Integrates physics-based simulations (e.g., FEP) with machine learning for molecular modeling. | |
| DataWarrior [40] | Open-source program for chemical intelligence, data analysis, and QSAR model development. | |
| Benchmarking Datasets & Infrastructure | DO Challenge Benchmark [95] | Standardized dataset and task for evaluating AI agents in a virtual screening scenario. |
| Public Compound & Target Databases (e.g., ZINC, ChEMBL, PDB) | Source of known actives, decoys, and protein structures for curating benchmarking datasets. | |
| High-Performance Computing (HPC) / Cloud | Essential for running compute-intensive AI models and large-scale virtual screens. |
The integration of artificial intelligence (AI) into drug discovery represents a paradigm shift in pharmaceutical research and development. While theoretical promises of accelerated timelines and reduced costs have been abundant, the true validation of AI-driven approaches lies in the progression of drug candidates through the clinical pipeline. This guide provides an objective comparison of clinically-stage AI-discovered candidates, detailing the experimental data and methodologies that underpin their advancement. The progression of these candidates from concept to clinic serves as the critical benchmark for assessing the practical utility and future potential of AI in addressing the high costs and protracted timelines of traditional drug development, which historically exceed 10 years and $2 billion per approved therapy [98] [85].
Table of Clinical-Stage AI-Discovered Drug Candidates
Table 1: A comparative overview of selected AI-discovered drug candidates in clinical development.
| AI Developer / Platform | Drug Candidate | Indication | Clinical Phase | Key Experimental Validation & Reported Outcomes |
|---|---|---|---|---|
| Insilico Medicine (Pharma.AI) [99] [100] | INS018_055 | Idiopathic Pulmonary Fibrosis | Phase II | Novel target identification and molecule generation; candidate advanced from target to Phase I in under 18 months [99]. |
| Insilico Medicine (Pharma.AI) [99] | Rentosertib | Oncology | Phase II | AI-designed drug; achieved USAN status and moved from target discovery to Phase II in under 30 months [99]. |
| Exscientia (Centaur AI) [96] [98] | DSP-1181 | Obsessive-Compulsive Disorder (OCD) | Phase I | First AI-designed molecule to enter human clinical trials; developed in less than 12 months [98]. |
| Exscientia [96] [100] | (Not specified) | Oncology | Phase I | Reported an 80% Phase I success rate for its AI-designed candidates [96]. |
| Atomwise (AtomNet) [96] [5] | TYK2 Inhibitor | Autoimmune & Autoinflammatory Diseases | Preclinical (Candidate Nominated) | Orally bioavailable allosteric inhibitor identified from a library of over 3 trillion synthesizable compounds [5]. |
| Yale/Google Research (C2S-Scale Model) [90] | Silmitasertib (repurposed) | Cancer Immunotherapy | Preclinical (Validated) | AI-predicted, context-dependent mechanism (with interferon) to enhance antigen presentation; validated in human neuroendocrine cell models, showing 13.6% to 37.3% increases in markers [90]. |
| Recursion Pharmaceuticals [98] | (Multiple candidates) | Various, including rare diseases | Clinical Phases | Uses automated high-throughput imaging combined with deep learning to identify phenotypic changes for drug repurposing and novel drug discovery [98]. |
Comparative Analysis of AI Platforms and Methodologies
The success of clinical candidates is rooted in the distinct AI methodologies and experimental workflows employed by different platforms. The following diagram illustrates a generalized workflow for the experimental validation of an AI-generated hypothesis, integrating both in silico and in vitro stages.
The divergence in strategies among leading AI drug discovery companies significantly influences the type and stage of their clinical candidates.
- Exscientia's Centaur AI platform focuses on automated molecular optimization for properties like potency and selectivity, which has enabled its reported high success rate in early clinical trials [96].
- Insilico Medicine's end-to-end Pharma.AI suite connects target discovery (PandaOmics) with molecular generation (Chemistry42) and clinical trial prediction (InClinico). This integrated approach is exemplified by the rapid progression of its candidates, INS018_055 and Rentosertib [99].
- BenevolentAI leverages a massive knowledge graph that processes millions of scientific papers and clinical data points to uncover hidden biological connections, with a strong focus on drug repurposing and novel target identification for complex diseases [96].
- Atomwise's AtomNet platform utilizes a deep learning model for structure-based drug design, predicting binding affinity to rapidly screen its vast proprietary library of compounds, as demonstrated by the identification of its TYK2 inhibitor candidate [96] [5].
Detailed Experimental Protocols for Key Validations
Protocol: AI-Driven Prediction and Validation of a Context-Dependent Drug Mechanism
This protocol is based on the landmark study from Yale and Google Research that used a large language model (C2S-Scale) to predict a novel role for silmitasertib in cancer immunotherapy [90].
Step 1: Model Training and Data Preparation
- Model Architecture: The C2S-Scale model, a 27-billion parameter large language model, was trained on over 50 million single-cell RNA sequencing profiles, representing over one billion tokens of transcriptomic data combined with biological text and metadata [90].
- Data Formatting: Gene expression profiles were converted into text-based "cell sentences" using the Cell2Sentence framework, which transforms data into ranked lists of gene names to preserve relative expression levels [90].
Step 2: Virtual Screening and Hypothesis Generation
- The trained model conducted thousands of virtual experiments simultaneously in a screen designed to identify compounds that enhance antigen presentation in immune cells.
- The key prediction was that silmitasertib, a known kinase inhibitor, would amplify MHC-I expression specifically in the presence of low-level interferon signaling—a context-dependent mechanism not previously reported [90].
Step 3: Experimental Validation
- Cell Models: Human neuroendocrine cell models (including Merkel cell and small cell lung cancer models) that were entirely absent from the model's training data were used for validation [90].
- Treatment Conditions: Cells were treated with silmitasertib alone, low-dose interferon alone, or a combination of both.
- Outcome Measurement: Antigen presentation markers (MHC-I) were quantified. The results confirmed the AI's prediction: the combination treatment produced substantial, dose-dependent increases in MHC-I markers (13.6% to 37.3%), while silmitasertib alone showed no significant effect [90].
Protocol: AI-Driven De Novo Drug Design and Validation
This protocol outlines the general approach for de novo design and validation of novel molecular entities, as utilized by platforms like Insilico Medicine and Exscientia [99] [98].
Step 1: Novel Target Identification
- Tool: Platforms like PandaOmics (Insilico Medicine) analyze vast multi-omics datasets (genomic, proteomic) and scientific literature to identify and prioritize novel, druggable targets associated with a specific disease [99].
Step 2: Generative Molecular Design
Step 3: In Silico Optimization and Screening
- Generated molecules undergo virtual screening. This includes predicting binding affinity (e.g., using models like the open-source Boltz-2, which calculates affinity in seconds), ADMET properties (Absorption, Distribution, Metabolism, Excretion, Toxicity), and synthetic accessibility [101].
Step 4: Experimental Confirmation
- In Vitro Assays: Top-ranking candidate molecules are synthesized and tested in biochemical and cell-based assays to confirm target engagement and functional activity.
- In Vivo Studies: Promising candidates advance to animal models to evaluate efficacy, pharmacokinetics, and safety in a living system, forming the basis for an Investigational New Drug (IND) application.
The following diagram details the signaling pathway investigated in the Yale/Google Research study, illustrating the novel, AI-predicted mechanism of action.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key reagents, tools, and platforms essential for experimental validation in AI-driven drug discovery.
| Item Name | Function & Application in AI Drug Discovery Validation |
|---|---|
| Single-Cell RNA Sequencing Kits | Generate the complex transcriptomic datasets used to train and query biological language models like C2S-Scale [90]. |
| Cell-Based Disease Models (e.g., Neuroendocrine Cancer Cells) | Provide a physiologically relevant in vitro system for experimentally testing AI-derived hypotheses on novel mechanisms or candidate efficacy [90]. |
| Binding Affinity Assays (e.g., SPR, ITC) | Measure the strength of interaction between a candidate drug molecule and its protein target, providing critical validation for AI-based binding predictions [101]. |
| AlphaFold 3 & RoseTTAFold All-Atom | Open-source protein structure prediction tools used to model 3D structures of targets and their complexes with ligands, informing molecular design [101]. |
| Boltz-2 Model | An open-source AI model for rapid prediction of protein-ligand binding affinity, democratizing access to a key metric in small-molecule discovery [101]. |
| SAIR (Structurally-Augmented IC50 Repository) | An open-access repository of computationally folded protein-ligand structures with experimental affinity data, used for training and benchmarking AI models [101]. |
| High-Content Screening Systems | Automated imaging systems that capture phenotypic changes in cells treated with compounds; the data feeds AI models for target deconvolution and mechanism-of-action analysis [98]. |
| PharmBERT | A domain-specific large language model pre-trained on drug labels, used for extracting pharmacokinetic information and adverse drug reaction data from text [100]. |
The clinical pipeline for AI-discovered drugs is no longer a theoretical construct but a tangible reality, populated by a growing number of candidates from a diverse array of technological platforms. The evidence from these pioneers indicates a tangible impact, with AI contributing to a significantly higher reported Phase I success rate of 80-90% compared to the historical average of ~40-50% [100]. The validation of these candidates rests on rigorous and transparent experimental protocols that bridge the gap between in silico prediction and in vitro and in vivo reality. As the field matures, the collective evidence from these clinical-stage candidates will be the ultimate arbiter of AI's value, providing the data needed to refine models, validate approaches, and fully realize the promise of a more efficient and effective drug discovery paradigm.
The integration of artificial intelligence into drug discovery represents a paradigm shift aimed at countering Eroom's Law (the inverse of Moore's Law), which describes the steadily increasing cost and time required to develop new drugs [102]. This guide provides a quantitative comparison of the economic performance of AI-driven platforms against traditional drug discovery methods, presenting validated data on cost savings, efficiency gains, and return on investment (ROI) for research professionals.
Market Context and Economic Imperative
The traditional drug discovery pipeline is notoriously resource-intensive, with the average cost to bring a new drug to market reaching $2.5 billion and a development timeline spanning 12 to 15 years [103]. Furthermore, the process is inherently inefficient; out of hundreds of thousands of molecules screened, only 35% show any therapeutic potential, and a mere 9–14% survive Phase I clinical trials [103]. This economic reality has driven the pharmaceutical industry to invest $251 billion in R&D in 2022, a figure projected to reach $350 billion by 2029 [103].
AI-driven platforms are emerging as a powerful solution to this challenge. The AI-driven drug discovery platforms market is experiencing significant growth, fueled by active involvement from technology giants like NVIDIA, Google, and Microsoft, and substantial venture capital funding, which saw a 27% increase in 2024, reaching $3.3 billion [104] [103].
Quantitative Comparison: AI Platforms vs. Traditional Methods
The following tables synthesize current data on the performance and economic impact of AI platforms compared to traditional drug discovery methodologies.
Table 1: Overall Efficiency and Cost Metrics
| Performance Metric | Traditional Discovery | AI-Driven Discovery | Improvement |
|---|---|---|---|
| Average Development Time | 12-15 years [103] | Reduction of 6-9 months [104] | ~5% faster (early estimate) |
| Key Development Cost | ~$2.5 billion per drug [103] | Significant cost reduction in discovery phase [104] | Not yet fully quantified |
| R&D Productivity | Declining (Eroom's Law) [102] | Rising investment (Market CAGR 26.95%) [104] | Trend reversal |
Table 2: Pre-Clinical Discovery Phase Metrics
| Performance Metric | Traditional Discovery | AI-Driven Discovery | Improvement |
|---|---|---|---|
| Lead Optimization | Manual, slow multi-parameter optimization | AI-powered multi-parameter analysis [104] | Dominant application segment [104] |
| Target Identification | Limited by human data analysis capacity | AI analysis of complex biological data [104] | Fastest growing segment (CAGR) [104] |
| Small Molecule Datasets | Relies on existing, often limited datasets | Leverages large, curated datasets for model training [104] | Dominant modality supported [104] |
Table 3: Clinical Trial and ROI Metrics
| Performance Metric | Traditional Discovery | AI-Driven Discovery | Improvement |
|---|---|---|---|
| Clinical Trial Patient Recruitment | Manual, slow process | AI-optimized recruitment and site selection [103] | Increased speed and efficiency |
| Trial Design | Standardized protocols | AI-designed better drug combinations and trial arms [103] | Improved predictive power |
| Phase I Success Rate | 9-14% [103] | High success rate observed [103] | Positive early indicator |
| Phase II Success Rate | Variable | Currently a challenge for AI-discovered drugs [103] | Key validation hurdle |
Experimental Protocols for Validating AI Platforms
For researchers to independently verify the performance claims of AI drug discovery platforms, a rigorous validation protocol is essential. The following workflow outlines a standard methodology for benchmarking an AI platform against traditional methods for a specific task, such as target identification or lead optimization.
Detailed Protocol Description
Define Validation Objective
Clearly specify the discovery task to be benchmarked (e.g., de novo molecular design, target validation, ADMET prediction). Define primary and secondary endpoints, which must include:
- Primary Endpoint: Time and/or cost to achieve a predefined performance threshold (e.g., identify 5 novel compounds with binding affinity <10 nM).
- Secondary Endpoints: Computational resource usage (e.g., GPU hours), concordance with later experimental results (predictive accuracy), and the novelty/patentability of the outputs [104] [103].
Data Curation & Segmentation
This step ensures a fair comparison by using identical data foundations.
- Data Sourcing: Utilize public datasets (e.g., ChEMBL, PDBBind, TCGA) or proprietary in-house data.
- Data Preparation: Apply stringent quality control. For AI platforms, data must be formatted for the specific model (e.g., SMILES for molecules, FASTA for sequences).
- Data Segmentation: Split the curated dataset into training/validation/test sets using time-split or scaffold-split to prevent data leakage and ensure the evaluation reflects real-world generalization ability [6].
AI Platform Execution
- Platform Setup: Configure the AI platform according to the vendor's specifications. For generative tasks, this includes defining chemical space constraints and desired properties.
- Model Training: Train the model on the designated training set. For pre-trained models, this may involve only fine-tuning on the specific dataset.
- Output Generation: Execute the model to generate predictions or novel molecular entities. Document all computational resources used [102].
Traditional Method Execution
- Method Selection: Employ standard industry practices for the chosen task, such as high-throughput screening (HTS) virtual screening with classical molecular docking, or medicinal chemistry lead optimization based on established structure-activity relationships (SAR).
- Execution: Conduct the process in parallel with the AI platform execution, meticulously tracking the time and resources consumed [103].
Quantitative Analysis
Compare the outputs from both workflows using pre-defined metrics:
- Efficiency: Total time and cost for each method.
- Output Quality: For candidate molecules, assess drug-likeness (e.g., QED, SAscore), synthetic accessibility, and novelty. For predictions, calculate standard statistical metrics (e.g., AUC, RMSE) [103].
- Resource Utilization: Computational costs for AI vs. material/reagent costs for traditional methods.
Experimental Validation
This is the critical step for moving from computational prediction to validated results.
- In Vitro Assays: Subject top-ranked candidates from both AI and traditional methods to identical experimental validation. This typically begins with binding affinity assays (e.g., SPR) and functional cellular assays.
- Blinding: Where possible, conduct assays in a blinded manner to eliminate bias.
- Hit Confirmation: The success rate in this experimental phase is the ultimate measure of a platform's predictive power and economic value [103].
The Scientist's Toolkit: Essential Research Reagents & Platforms
The successful implementation and validation of AI in drug discovery relies on a ecosystem of specialized tools and platforms. The following table details key solutions and their functions.
Table 4: Key Research Reagent Solutions for AI-Driven Discovery
| Tool Category / Platform | Specific Function | Relevance to AI Validation |
|---|---|---|
| Discovery Engines (e.g., Generate:Biomedicines, Relation Therapeutics) [103] | Integrated platforms combining AI with lab data and automated testing to discover new candidate molecules. | Used for end-to-end candidate identification; validation requires assessing the quality and clinical potential of their outputs. |
| Point-Solution Software (e.g., tools for target ID, molecular design) [103] | Platforms that enhance specific tasks (e.g., image analysis for high-content screening, binding affinity prediction). | Ideal for benchmarking AI performance on discrete tasks against traditional software or methods. |
| Foundation Models (e.g., Bioptimus, Evo) [102] | Large-scale AI models trained on massive genomic, transcriptomic, and proteomic datasets to uncover fundamental biological patterns. | Used to generate novel biological hypotheses and targets; validation requires experimental follow-up on these insights. |
| AI Agents (e.g., Johnson & Johnson's synthesis optimizers) [102] | AI systems that automate lower-complexity bioinformatics tasks (e.g., RNA-seq analysis pipeline selection). | Validated by their ability to reproduce or accelerate expert-driven workflows without sacrificing accuracy. |
| Retrieval-Augmented Generation (RAG) [6] | A technique used with Large Language Models (LLMs) that grounds AI responses in internal company documents and scientific literature. | Critical for building trustworthy AI assistants that help scientists query internal data; validated by accuracy in information retrieval. |
The quantitative data demonstrates that AI-driven platforms offer substantial economic benefits in the early stages of drug discovery, primarily through accelerated timelines and reduced costs for specific tasks like target identification and lead optimization [104]. However, the ultimate validation of these platforms—success in late-stage clinical trials—remains a work in progress, with several AI-discovered drugs facing challenges in Phase II [103].
The future economic impact will likely be shaped by the maturation of foundation models for biology and the widespread adoption of AI agents that democratize data analysis [102]. For research professionals, a rigorous, experimental approach to validating AI tools, as outlined in this guide, is paramount for integrating these technologies into a robust and economically viable drug discovery strategy.
Conclusion
The successful validation of AI models is no longer a secondary concern but a fundamental prerequisite for the future of drug discovery. As synthesized from the four core intents, a holistic approach—combining technical rigor (RICE principles), methodological transparency, proactive troubleshooting of biases and security, and robust comparative benchmarking—is essential to transition from promising algorithms to reliable clinical assets. Looking forward, the maturation of AI in biomedicine hinges on the development of standardized validation protocols, clearer regulatory pathways from bodies like the FDA, and a cultural shift towards interdisciplinary collaboration between data scientists and biologists. By prioritizing robust validation today, the field can fully harness AI's potential to break Eroom's Law, deliver personalized therapies, and ultimately improve patient outcomes with unprecedented speed and precision.
References
- 1. Leading AI-Driven Drug Discovery Platforms: 2025 Landscape and Global Outlook - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 2. Customized Metrics for ML in Drug Discovery [https://www.elucidata.io/blog/evaluation-metrics-for-ml-models-in-drug-discovery]
- 3. 25 Leading AI Companies to Watch in 2025: Transforming Drug Discovery and Precision Medicine [https://biopharmaapac.com/analysis/32/5655/25-leading-ai-companies-to-watch-in-2025-transforming-drug-discovery-and-precision-medicine.html]
- 4. Top AI Companies & How to Drug Them ( Discovery ) Compare 2025 [https://www.linkedin.com/pulse/top-ai-drug-discovery-companies-how-compare-them-2025-axalt-systems-dug0c]
- 5. 12 AI drug discovery companies you should know about in 2025 [https://www.labiotech.eu/best-biotech/ai-drug-discovery-companies/]
- 6. The State of Adopting AI in Drug in Discovery 2025 [https://chemaxon.com/blog/ai-in-drug-discovery]
- 7. How Generative AI in Healthcare is Transforming Drug in... Discovery [https://www.rfidjournal.com/expert-views/how-generative-ai-in-healthcare-is-transforming-drug-discovery-in-2025/222589/]
- 8. The key for fast and efficient AI -assisted drug ... discovery [https://www.linkedin.com/pulse/key-fast-efficient-ai-assisted-drug-discovery-benchmarking]
- 9. AI Papers to Read in 2025 | Towards Data Science [https://towardsdatascience.com/ai-papers-to-read-in-2025/]
- 10. Artificial Intelligence (AI) in Drug Discovery | Synthesis X (SynthX) Center | Rice University [https://synthx.rice.edu/research/artificial-intelligence-ai-drug-discovery]
- 11. AI in Drug Development: Regulatory Compliance Challenges | Danaher Life Sciences [https://lifesciences.danaher.com/us/en/library/regulatory-compliance-ai-drug-discovery.html]
- 12. AI for Synthesizable Chemical Space [https://www.emergentmind.com/papers/2410.03494]
- 13. AI And Pharmaceutical Development: WHO Calls For Ethical Framework, Good Governance [https://www.drugdiscoveryonline.com/doc/ai-and-pharmaceutical-development-who-calls-for-ethical-framework-good-governance-0001]
- 14. Deep learning gives drug design a boost | Rice News | News and Media Relations | Rice University [https://news.rice.edu/news/2020/deep-learning-gives-drug-design-boost]
- 15. The Role of AI in Drug Discovery: Challenges, Opportunities, and Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10302890/]
- 16. Regulating the Use of AI in Drug Development: Legal Challenges and Compliance Strategies - Food and Drug Law Institute (FDLI) [https://www.fdli.org/2025/07/regulating-the-use-of-ai-in-drug-development-legal-challenges-and-compliance-strategies/]
- 17. Perspective on the challenges and opportunities of accelerating drug discovery with artificial intelligence - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9997711/]
- 18. Development: AI Releases Draft Drug FDA Guidance [https://www.foley.com/insights/publications/2025/01/ai-drug-development-fda-releases-draft-guidance/]
- 19. Key takeaways from FDA ’s draft guidance on use of AI in drug and... [https://www.dlapiper.com/en-us/insights/publications/2025/01/fda-releases-draft-guidance-on-use-of-ai]
- 20. Publishes Its First Draft FDA On Use of Artificial Intelligence... Guidance [https://www.goodwinlaw.com/en/insights/publications/2025/01/alerts-lifesciences-aiml-fda-publishes-its-first-draft-guidance]
- 21. FDA Releases Draft Guidance on Submission Recommendations for... [https://www.kslaw.com/news-and-insights/fda-releases-draft-guidance-on-submission-recommendations-for-ai-enabled-device-software-functions]
- 22. Harnessing Artificial Intelligence in Drug and Development Discovery [https://www.accc-cancer.org/acccbuzz/blog-post-template/accc-buzz/2024/12/20/harnessing-artificial-intelligence-in-drug-discovery-and-development]
- 23. Generative AI in drug discovery [https://blog.biostrand.ai/generative-ai-in-drug-discovery]
- 24. approaches for the AI and discovery of validation targets - PMC drug [https://pmc.ncbi.nlm.nih.gov/articles/PMC11383977/]
- 25. Accelerating AI with Open Source Datasets Drug Discovery [https://www.recursion.com/news/accelerating-ai-drug-discovery-with-open-source-datasets]
- 26. - Wikipedia Experimental benchmarking [https://en.wikipedia.org/wiki/Experimental_benchmarking]
- 27. Explainable Artificial Intelligence: A Perspective on Drug Discovery [https://www.mdpi.com/1999-4923/17/9/1119]
- 28. Can You Trust Your Model ? Why Explainability Matters in AI -Driven... [https://ardigen.com/can-you-trust-your-model-why-explainability-matters-in-ai-driven-drug-discovery/]
- 29. Drug discovery with explainable artificial intelligence | Nature Machine Intelligence [https://www.nature.com/articles/s42256-020-00236-4]
- 30. Frontiers | AI alignment is all your need for future drug discovery [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2025.1668794/full]
- 31. Explainable AI in drug discovery: self-interpretable graph neural network for molecular property prediction using concept whitening | Machine Learning [https://link.springer.com/article/10.1007/s10994-023-06369-y]
- 32. How Generative AI Is Reducing Drug Timelines... | Medium Discovery [https://prajnaaiwisdom.medium.com/how-generative-ai-is-reducing-drug-discovery-timelines-by-70-e86d58f7c780]
- 33. Beyond Legacy Tools: Defining Modern AI for 2025... Drug Discovery [https://www.biopharmatrend.com/business-intelligence/what-is-ai-drug-discovery/]
- 34. of In -Assisted Silico in Healthcare Validation AI Drugs [https://pubmed.ncbi.nlm.nih.gov/40553347/]
- 35. announces preclinical Insilico ... Medicine drug discovery benchmarks [https://www.news-medical.net/news/20250211/Insilico-Medicine-announces-preclinical-drug-discovery-benchmarks-from-2021-to-2024.aspx]
- 36. | Technology-driven Exscientia AI Drug Discovery [https://www.exscientia.com/]
- 37. Uses Generative Exscientia to Reimagine AI Drug Discovery [https://aws.amazon.com/solutions/case-studies/exscientia-generative-ai/]
- 38. 顶级AI制药Recursion:让药物发现工业化 - 第五十四期 - - 中国远大集团 [https://i.cgeinc.com/no54/19167.html]
- 39. Transforming Drug Target Discovery , Insilico Publishes... Medicine [https://insilico.com/tpost/v49bfcu0r1-transforming-drug-target-discovery-insil]
- 40. Top Drug Discovery Software Solutions to Watch in 2025 | deepmirror [https://www.deepmirror.ai/post/top-drug-discovery-software-solutions-to-watch-in-2025]
- 41. Artificial Intelligence in Drug Discovery Towards Strategic Applications Challenges and Implementation Frameworks for Accelerated Pharmaceutical Innovation | European Journal of Artificial Intelligence and Machine Learning [https://ej-ai.org/index.php/ejai/article/view/65]
- 42. Frontiers | De drug novo through artificial intelligence: an... design [https://www.frontiersin.org/journals/hematology/articles/10.3389/frhem.2024.1305741/full]
- 43. [2402.08703] A Survey of Generative AI for de Drug novo ... Design [https://arxiv.org/abs/2402.08703]
- 44. Tackling the issue of confined chemical space with AI-based de novo drug design and molecular optimization - PubMed [https://pubmed.ncbi.nlm.nih.gov/40887314/]
- 45. Artificial Intelligence in Small-Molecule Drug Discovery: A Critical Review of Methods, Applications, and Real-World Outcomes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472608/]
- 46. Large language models open new way of AI-assisted molecule design for chemists | Journal of Cheminformatics | Full Text [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-00984-8]
- 47. Generative AI Bridging Wet and Lab Workflows Dry Lab [https://www.pharmaadvancement.com/market-moves/generative-ai-bridging-wet-lab-and-dry-lab-workflows/]
- 48. AI-Driven Drug Discovery: A Comprehensive Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12177741/]
- 49. ’s Future Hinges On The AI | Twist Bioscience Wet Lab [https://www.twistbioscience.com/blog/perspectives/AI-wetlab-validation]
- 50. AI in Drug Discovery: 2025 Outlook | Foley & Lardner LLP [https://www.foley.com/insights/publications/2024/12/ai-drug-discovery-2025-outlook/]
- 51. Where AI Meets Wet - Lab : A Smarter Path to Biologics Discovery ... [https://ardigen.com/where-ai-meets-wet-lab-a-smarter-path-to-biologics-discovery-success/]
- 52. | Foundation AI @ GTC Drug | Sprintome Discovery Models 2025 [https://medium.com/sprintome/nvidia-gtc-2025-expert-look-at-foundation-models-in-biology-and-drug-discovery-efd7a5c5e9e6]
- 53. How Hybrid Biotech Integration is Accelerating AI-Driven Research and Drug Discovery | [https://www.scispot.com/blog/how-hybrid-biotech-integration-is-accelerating-ai-driven-research-and-drug-discovery]
- 54. Top 10 AI Platforms Tools in Drug ... - Best DevOps Discovery 2025 [https://www.bestdevops.com/top-10-ai-drug-discovery-platforms-tools-in-2025-features-pros-cons-comparison/]
- 55. Multimodal data in drug : Uses, benefits and more discovery [https://www.tiledb.com/multimodal-data/drug-discovery]
- 56. From siloed data to breakthroughs: multimodal AI in drug discovery [https://www.drugtargetreview.com/article/160597/from-siloed-data-to-breakthroughs-multimodal-ai-in-drug-discovery/]
- 57. Workflow - Sonrai Analytics AI Patient Stratification [https://sonraianalytics.com/ai-patient-stratification-workflow/]
- 58. How AI is Transforming Drug Processes in Discovery 2025 [https://vasro.de/en/impact-ai-drug-discovery-2025/]
- 59. Multimodal AI breaks data silos to accelerate drug and... discovery [https://completeaitraining.com/news/multimodal-ai-breaks-data-silos-to-accelerate-drug/]
- 60. Multimodal AI Predicts Clinical Outcomes of Drug ... - Zitnik Lab [https://zitniklab.hms.harvard.edu/projects/Madrigal/]
- 61. -Powered AI Global Solution Deep Dive Analysis... Drug Discovery [https://www.linkedin.com/pulse/ai-powered-drug-discovery-global-solution-deep-dive-alex-g--wdxte]
- 62. M3-20M: A Large-Scale Multi - Modal Molecule Dataset for AI -driven... [https://arxiv.org/html/2412.06847v2]
- 63. Can artificial intelligence predict clinical trial outcomes? [https://arxiv.org/html/2411.17595v1]
- 64. [2402.06512] Multimodal Clinical Trial Outcome Prediction with Large Language Models [https://arxiv.org/abs/2402.06512]
- 65. -enabled AI and gene network analysis reveal... drug prediction [https://www.nature.com/articles/s43856-025-00975-8?error=cookies_not_supported&code=57477d6b-7e1a-4157-b6f5-c57b2281aba6]
- 66. Recent advances in AI-based toxicity prediction for drug discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12279745/]
- 67. Legal Frameworks for Artificial Intelligence in Drug Discovery [https://natlawreview.com/article/ai-drug-discovery-2025-outlook]
- 68. How Data Science Is Transforming Drug And Medical... Discovery [https://www.forbes.com/councils/forbestechcouncil/2025/07/17/the-ai-revolution-in-healthcare-how-data-science-is-transforming-drug-discovery-and-medical-diagnosis/]
- 69. FDA Draft Guidance: Considerations for the Use of Artificial Intelligence... [https://www.linkedin.com/pulse/fda-draft-guidance-considerations-use-artificial-drug-weissman-xiqfe]
- 70. Frontiers | Assessing the adversarial of multimodal... robustness [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1606238/full]
- 71. What is data drift in ML, and how to detect and handle it [https://www.evidentlyai.com/ml-in-production/data-drift]
- 72. Evidential deep learning-based drug-target interaction prediction | Nature Communications [https://www.nature.com/articles/s41467-025-62235-6]
- 73. Drift detection | H2O Model Validation [https://docs.h2o.ai/wave-apps/h2o-model-validation/v0.14.0/guide/validation-tests/drift-detection/drift-detection]
- 74. -Driven AI Platforms Market ( Drug – 2033) Discovery 2025 [https://www.platformexecutive.com/insight/health-care-research/ai-driven-drug-discovery-platforms-market-2025-2033/]
- 75. From molecule to market: Opportunities and challenges in using AI in... [https://www.dlapiper.com/en/insights/publications/2025/09/from-molecule-to-market-opportunities-and-challenges-in-using-ai-in-drug-discovery-and-development]
- 76. In Healthcare: How To Protect Patient Data Cybersecurity [https://www.forbes.com/councils/forbestechcouncil/2025/04/08/cybersecurity-in-healthcare-protecting-patient-data-in-an-ai-driven-world/]
- 77. ITIF Technology Explainer: What Are Privacy Enhancing Technologies? [https://itif.org/publications/2025/09/02/itif-technology-explainer-privacy-enhancing-technologies/]
- 78. SCI-RSC Workshop on Computational Tools for Drug Discovery 2025 [https://www.soci.org/events/fine-chemicals-group/2025/sci-rsc-workshop-on-computational-tools-for-drug-discovery-2025]
- 79. AI Driven Drug Discovery: 5 Powerful Breakthroughs in 2025 [https://lifebit.ai/blog/ai-driven-drug-discovery/]
- 80. Deep Batch Active Learning for Drug Discovery [https://elifesciences.org/reviewed-preprints/89679v2]
- 81. Finding Drug Candidate Hits With a Hundred Samples: Ultra-low Data... [https://chemrxiv.org/engage/chemrxiv/article-details/67fd0377fa469535b92a5a99]
- 82. A guide for active learning in synergistic drug discovery | Scientific Reports [https://www.nature.com/articles/s41598-025-85600-3]
- 83. Bias Control: AI and Monitor Validate [https://dzone.com/articles/mitigating-bias-in-ai-through-continuous-monitorin]
- 84. in AI : Drug Up Development and Reducing... Discovery Speeding [https://www.platformexecutive.com/insight/health-care-research/ai-in-drug-discovery/]
- 85. in Pharma and Biotech: Market Trends AI and Beyond 2025 [https://www.coherentsolutions.com/insights/artificial-intelligence-in-pharmaceuticals-and-biotechnology-current-trends-and-innovations]
- 86. in AI Development Statistics Drug : The $60 Billion Reality vs.... 2025 [https://www.allaboutai.com/resources/ai-statistics/drug-development/]
- 87. in AI : Increasing Drug ... - PharmiWeb.com Discovery Success Rates [https://www.pharmiweb.com/press-release/2025-02-21/ai-in-drug-discovery-increasing-success-rates-by-20]
- 88. Beyond Legacy Tools: Defining Modern AI Drug Discovery for 2025 and Beyond [https://www.biopharmatrend.com/ai-drug-discovery-pipeline-2024/]
- 89. Artificial intelligence in drug discovery and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7577280/]
- 90. -Driven AI Yields First Drug ... Discovery Experimentally Validated [https://www.linkedin.com/pulse/ai-driven-drug-discovery-yields-first-experimentally-validated-david-8la1c]
- 91. What experts at Flatiron, PicnicHealth, MMIT expect for [https://www.drugdiscoverytrends.com/clinical-care-convergence-2025/]
- 92. Dataset for Validated -Driven AI Drug Discovery [https://www.chemdiv.com/datasets/]
- 93. Computational Methods in Drug Discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3880464/]
- 94. Artificial Intelligence ( AI ) in Drug Market Report Discovery 2025 [https://www.researchandmarkets.com/reports/5939573/artificial-intelligence-ai-in-drug-discovery]
- 95. and Development of Benchmarking -Based Agentic... | Deep Origin AI [https://www.deeporigin.com/blog/benchmarking-and-development-of-ai-based-agentic-systems-for-autonomous-drug-discovery]
- 96. Top 10 AI Drug Discovery Platforms in 2025: Features, Pros, Cons & Comparison - DevOpsSchool.com [https://www.devopsschool.com/blog/top-10-ai-drug-discovery-platforms-in-2025-features-pros-cons-comparison/]
- 97. Computational approaches streamlining drug discovery | Nature [https://www.nature.com/articles/s41586-023-05905-z]
- 98. From Lab to Clinic: How Artificial Intelligence (AI) Is Reshaping Drug Discovery Timelines and Industry Outcomes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298131/]
- 99. in AI : Faster, Smarter, Better Drug Discovery [https://www.delveinsight.com/blog/ai-in-drug-discovery-revolution]
- 100. AI In Action: Redefining Drug Discovery and Development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11800368/]
- 101. AI Models Enhance the Drug Discovery Portfolio [https://www.genengnews.com/topics/artificial-intelligence/ai-models-enhance-the-drug-discovery-portfolio/]
- 102. in 2025 : Predictions AI Drug Discovery [https://lizard.bio/knowledge-hub/2025-ai-in-drug-discovery-predictions]
- 103. in AI : Use cases, market, and funding in drug discovery 2025 [https://xenoss.io/blog/ai-drug-discovery]
- 104. -Driven AI Market Size, Report by 2034 Drug Discovery Platforms [https://www.precedenceresearch.com/ai-driven-drug-discovery-platforms-market]