Target Validation Techniques: A Comprehensive Guide for Drug Development Success
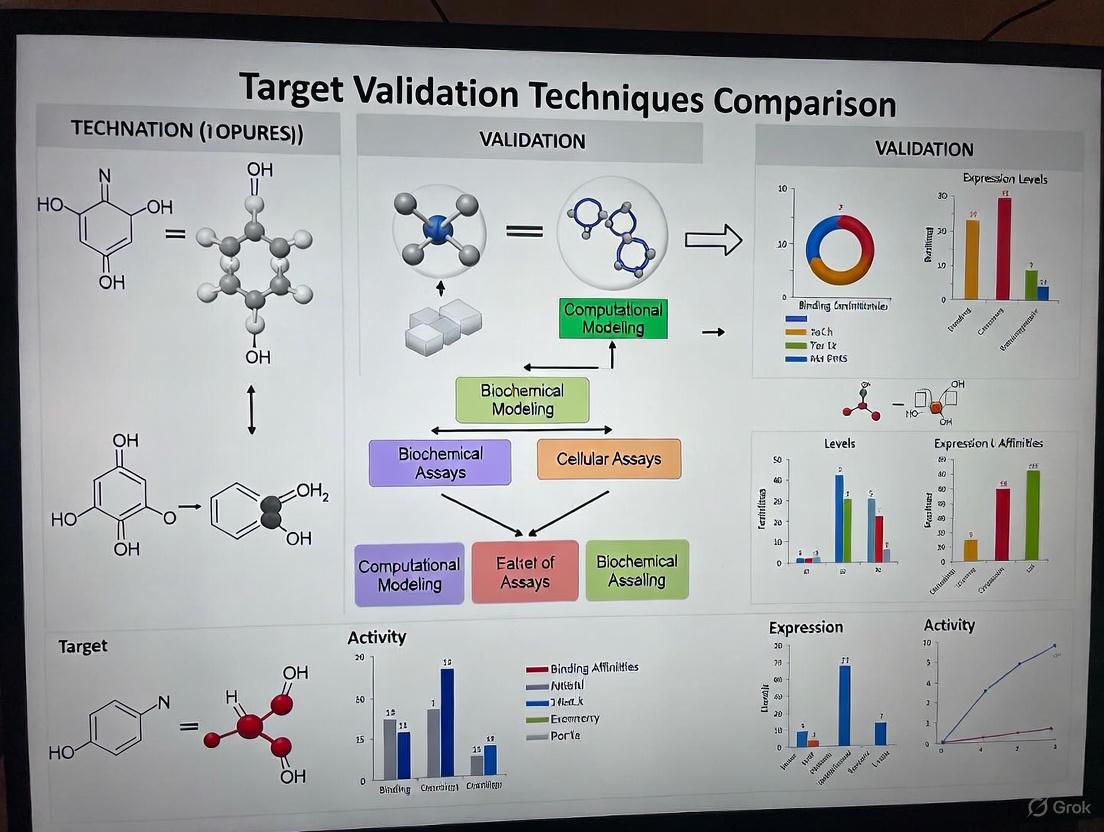
This article provides a detailed comparison of target validation techniques, a critical process in drug discovery that confirms a biological target's role in disease and its potential for therapeutic intervention.
Target Validation Techniques: A Comprehensive Guide for Drug Development Success
Abstract
This article provides a detailed comparison of target validation techniques, a critical process in drug discovery that confirms a biological target's role in disease and its potential for therapeutic intervention. Aimed at researchers and drug development professionals, it explores foundational concepts, key methodological approaches, common troubleshooting strategies, and a comparative analysis of techniques from RNAi to emerging AI-powered tools. The content synthesizes current best practices to help scientists build robust evidence for their targets, mitigate clinical failure risks, and accelerate the development of safer, more effective therapies.
What is Target Validation and Why is it the Cornerstone of Drug Discovery?
Target validation is a critical, early-stage process in drug discovery that focuses on establishing a causal relationship between a biological target and a disease. It provides the foundational evidence that modulating a specific target (e.g., a protein, gene, or RNA) will produce a therapeutic effect with an acceptable safety profile [1]. This process typically takes 2-6 months to complete and is essential for de-risking drug development, as inadequate validation is a major contributor to the high failure rates seen in clinical trials, often due to lack of efficacy [1] [2]. This guide objectively compares the performance, experimental protocols, and data outputs of the primary techniques used to establish the functional role of a target in disease.
Core Methodologies in Target Validation
The following table summarizes the key characteristics, applications, and data outputs of the primary target validation methodologies.
Table 1: Comparison of Core Target Validation Methodologies
| Methodology | Core Principle | Key Application / Context | Typical Experimental Readout | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| In Silico Target Prediction [3] [4] | Uses AI/ML and similarity principles to predict drug-target interactions from chemical and biological data. | Prioritizing targets for novel compounds; generating MoA hypotheses; initial triage. | - Ranked list of potential targets.- Probability scores (e.g., pChEMBL value).- Similarity to known ligands. | - High speed; can screen thousands of targets.- Low resource consumption.- Reveals hidden polypharmacology. | - Predictive performance varies.- Relies on quality/completeness of existing data.- Requires experimental confirmation. |
| Functional Analysis (In Vitro) [1] | Uses "tool" molecules in cell-based assays to measure biological activity and the effect of target modulation. | Establishing a direct, causal link between target function and a cellular phenotype. | - Changes in cell viability, signaling, or reporter gene expression.- Quantification of biomarkers (qPCR, Luminex). | - Provides direct evidence of pharmacological effect.- Controlled, reductionist environment.- Amenable to high-throughput screening. | - May not capture full systemic physiology.- Can lack translational predictivity. |
| Genetic Approaches (In Vitro/In Vivo) [5] | Employs gene editing (e.g., CRISPR-Cas9) to knock out or knock in a gene to study the consequent phenotype. | Establishing a causal link between a gene and a disease process in a biological system. | - Presence or absence of a disease-relevant phenotype (e.g., cell death, morphological defect).- Changes in biomarker expression. | - Provides strong causal evidence.- Highly versatile and precise.- Enables study of loss-of-function and gain-of-function. | - Potential for compensatory mechanisms.- Off-target effects of gene editing. |
| In Vivo Validation (Mammalian Models) [6] | Tests the therapeutic hypothesis in a living mammal, typically a mouse model with disease pathology. | Proof-of-concept studies to show disease modification in a complex, systemic organism. | - Improvement in disease symptoms/scores.- Protection of relevant cells (e.g., motor neurons).- Extension of survival. | - Captures full systemic physiology and PK/PD.- Highest preclinical translatability for human efficacy. | - Very high cost and time-intensive.- Low- to medium-throughput.- Ethical considerations. |
| In Vivo Validation (Zebrafish Models) [5] | Uses zebrafish, particularly CRISPR-generated F0 "crispants," for rapid functional gene assessment in a whole organism. | Rapidly narrowing down gene lists from GWAS; validating causal involvement in a living organism. | - Phenotypic outputs in systems like nervous or cardiovascular system (e.g., behavioral alterations, cardiac defects). | - High genetic and physiological similarity to humans.- Rapid results (within days).- Amenable to medium-throughput screening. | - Not a mammal; some physiological differences.- Less established for some complex diseases. |
| Target Engagement Assays (e.g., CETSA) [7] | Directly measures the physical binding of a drug molecule to its intended target in a physiologically relevant environment (e.g., intact cells). | Confirming that a drug candidate engages its target within the complex cellular milieu. | - Quantified, dose-dependent stabilization of the target protein.- Shift in protein melting temperature. | - Confirms mechanistic link between binding and phenotypic effect.- Provides quantitative, system-level validation. | - Does not, by itself, establish therapeutic effect. |
Experimental Protocols for Key Validation Techniques
Protocol for In Silico Target Prediction and Validation
This protocol leverages computational tools like MolTarPred, which was identified as a highly effective method in a 2025 systematic comparison [3].
Step 1: Database Curation
- Retrieve bioactivity data from a structured database like ChEMBL (e.g., version 34) [3].
- Filter records for high-confidence interactions (e.g., confidence score ≥ 7) and standard values (IC50, Ki, EC50) below 10,000 nM [3].
- Exclude entries associated with non-specific or multi-protein targets and remove duplicate compound-target pairs.
Step 2: Model Application and Prediction
- Input the query molecule's structure (e.g., as a SMILES string).
- Run the target prediction algorithm (e.g., MolTarPred using Morgan fingerprints with Tanimoto scores for optimal performance) [3].
- Generate a ranked list of potential targets based on similarity to known active ligands or other prediction metrics.
Step 3: Validation and Hypothesis Generation
- The top predictions, such as the potential repurposing of fenofibric acid as a THRB modulator for thyroid cancer, serve as testable hypotheses for experimental validation [3].
Protocol for Rapid In Vivo Validation Using Zebrafish
Zebrafish offer a powerful platform for rapid functional validation, especially when combined with CRISPR/Cas9 [5].
Step 1: Model Generation
- Design CRISPR/Cas9 guide RNAs targeting the candidate gene's zebrafish ortholog.
- Inject embryos to create F0 "crispant" models, which exhibit mosaic gene inactivation within days, bypassing the need for stable lines [5].
Step 2: Phenotypic Screening
- Screen the crispants for disease-relevant phenotypes using optimized injection and screening protocols to select embryos with a high mutational load [5].
- Assay phenotypes across different biological systems (e.g., behavioral assays for neuroscience, cardiac function monitoring for cardiovascular disease, or tumor development for oncology) [5].
Step 3: Data Analysis and Target Prioritization
- Correlate gene inactivation with the emergence of a phenotype to establish causal involvement. This approach serves as a functional filter to prioritize targets from large gene lists derived from sources like genome-wide association studies (GWAS) [5].
The workflow for this rapid in vivo validation is summarized in the diagram below.
Protocol for In Vivo Proof-of-Concept in Mammalian Models
The In Vivo Target Validation Program by Target ALS exemplifies a robust protocol for testing therapeutic strategies in mammalian models of disease [6].
Step 1: Model and Therapeutic Selection
Step 2: In Vivo Dosing and Monitoring
- Administer the therapeutic compound to the model organism according to a defined dosing regimen.
- Monitor animals for disease symptoms and functional outcomes over time.
Step 3: Endpoint Analysis
- Assess primary efficacy endpoints, such as improvement in motor function, protection of vulnerable cells (e.g., motor neurons), and extension of survival [6].
- Conduct ex vivo analyses to confirm engagement of the intended target and understand the mechanism of action (e.g., reduction in TDP-43 phosphorylation) [6].
Quantitative Performance Metrics for Method Evaluation
Evaluating the performance of target validation methods, particularly computational ones, requires rigorous metrics. Standard n-fold cross-validation can produce over-optimistic results; therefore, more challenging validation schemes like time-splits or clustering compounds by scaffold are recommended for a realistic performance estimate [4]. The following table compares key metrics for assessing target prediction models, highlighting the limitations of generic metrics for the imbalanced datasets common in drug discovery.
Table 2: Metrics for Evaluating Target Prediction Model Performance
| Metric | Calculation / Principle | Relevance to Target Validation | Limitations in Biopharma Context |
|---|---|---|---|
| Accuracy | (True Positives + True Negatives) / Total Predictions | Provides an overall measure of correct predictions. | Can be highly misleading with imbalanced datasets (e.g., many more inactive than active compounds), as simply predicting "inactive" for all will yield high accuracy [8]. |
| Precision | True Positives / (True Positives + False Positives) | Measures the reliability of a positive prediction. High precision reduces wasted resources on false leads [8]. | Does not account for false negatives, so a high-precision model might miss many true interactions [8]. |
| Recall (Sensitivity) | True Positives / (True Positives + False Negatives) | Measures the ability to find all true positives. High recall ensures promising targets are not missed [8]. | A high-recall model may generate many false positives, increasing the validation burden [8]. |
| F1 Score | 2 * (Precision * Recall) / (Precision + Recall) | Balances precision and recall into a single metric. | May dilute focus on top-ranking predictions, which are most critical for lead prioritization [8]. |
| Precision-at-K | Precision calculated only for the top K ranked predictions. | Directly relevant for prioritizing the most promising drug candidates or targets from a screened list [8]. | Does not evaluate the performance of the model beyond the top K results. |
| Rare Event Sensitivity | A metric tailored to detect low-frequency events (e.g., specific toxicities). | Critical for identifying rare but critical events, such as adverse drug reactions or activity against rare target classes [8]. | Requires specialized dataset construction and is not a standard metric. |
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful experimental validation relies on a suite of reliable reagents and tools. The following table details key solutions used across the featured methodologies.
Table 3: Key Research Reagent Solutions for Target Validation
| Research Reagent / Solution | Function in Validation | Example Application Context |
|---|---|---|
| CRISPR/Cas9 System | Precise gene knockout or knock-in to study gene function and create disease models. | Generating F0 zebrafish "crispants" for rapid gene validation [5]. |
| Tool Molecules (e.g., selective agonists/antagonists) | To pharmacologically modulate a target's activity in a functional assay. | Demonstrating the desired biological effect in vitro during functional analysis [1]. |
| CETSA (Cellular Thermal Shift Assay) | To confirm direct binding of a drug to its protein target in a physiologically relevant cellular context. | Quantifying target engagement of a compound, such as for DPP9 in rat tissue [7]. |
| Validated Antibodies | To detect and quantify protein expression, localization, and post-translational modifications. | Assessing expression profiles and biomarker changes in healthy vs. diseased states [1]. |
| qPCR Assays & Panels | To accurately measure mRNA expression levels of targets and biomarkers. | Biomarker identification and validation via transcriptomics [1]. |
| iPSCs (Induced Pluripotent Stem Cells) | To create disease-relevant human cell types (e.g., neurons) for physiologically accurate in vitro testing. | Using human stem cell-derived models in functional cell-based assays [1]. |
| ChEMBL Database | A curated database of bioactive molecules with drug-target interactions to train and benchmark predictive models. | Providing the reference dataset for ligand-centric target prediction methods like MolTarPred [3]. |
Target validation is not a one-size-fits-all process but a multi-faceted endeavor requiring a strategic combination of techniques. Computational methods like MolTarPred offer high-speed prioritization, while cellular assays establish pharmacological proof-of-concept. In vivo models, from the rapid zebrafish to the physiologically complex mouse, provide critical evidence of efficacy in a whole organism. The emerging trend is the integration of these approaches into cross-disciplinary pipelines, augmented by AI and functional validation tools like CETSA, to build an irrefutable case for a target's role in disease before committing to the costly later stages of drug development [6] [7]. This rigorous, multi-technique comparison empowers researchers to select the optimal validation strategy, thereby increasing the likelihood of clinical success.
Clinical trials are the cornerstone of drug development, yet approximately 90% fail to achieve regulatory approval [9]. A significant portion of these failures, particularly in early phases, can be traced back to a single, fundamental problem: inadequate target validation. When the underlying biology of a drug target is not thoroughly understood and validated, clinical trials are built on a fragile foundation, leading to costly late-stage failures. This analysis compares contemporary target validation techniques, highlighting how rigorous, multi-faceted validation strategies are critical for de-risking the drug development pipeline and reducing the staggering rate of clinical trial attrition.
The Staggering Cost of Clinical Trial Failure
Failed clinical trials represent one of the most significant financial drains in the biopharmaceutical industry. The average cost of a failed Phase III trial alone can exceed $100 million [9]. Beyond the financial loss, these failures delay life-saving treatments and raise ethical concerns regarding participant exposure without therapeutic benefit. An analysis of failure reasons reveals that a substantial number of programs collapse because the selected target is poorly understood or turns out to be less relevant in humans than in preclinical models [9]. This underscores that the failure often begins not during the trial's execution, but much earlier, during the drug discovery and design phases.
A Comparative Analysis of Target Validation Techniques
A robust validation strategy employs a combination of computational and experimental methods to build confidence in a target's role in disease. The table below summarizes the core methodologies.
Table 1: Comparison of Key Target Validation Techniques
| Method Category | Specific Technique | Key Principle | Key Output/Readout | Relative Cost | Key Limitations |
|---|---|---|---|---|---|
| Computational Prediction | In-silico Target Fishing [3] | Ligand-based similarity searching against known bioactive molecules | Ranked list of potential protein targets | Low | Dependent on quality and scope of underlying database |
| AI/ML Models (e.g., CMTNN, RF-QSAR) [3] | Machine learning trained on chemogenomic data to predict drug-target interactions | Target interaction probability scores | Low to Medium | Model accuracy depends on training data; "black box" concern | |
| Genetic Manipulation | Antisense Oligonucleotides [10] | Chemically modified oligonucleotides bind mRNA, blocking protein synthesis | Measurement of target protein reduction and phenotypic effect | Medium | Toxicity and bioavailability issues; non-specific actions |
| Small Interfering RNA (siRNA) [10] | Double-stranded RNA activates cellular machinery to degrade specific mRNA | Measurement of target protein reduction and phenotypic effect | Medium | Challenges with in vivo delivery and potential off-target effects | |
| Transgenic Animals (Knockout/Knock-in) [10] | Generation of animals lacking or with an altered target gene | Observation of phenotypic endpoints in a whole organism | Very High | Expensive, time-consuming; potential for compensatory mechanisms | |
| Pharmacological Modulation | Monoclonal Antibodies (mAbs) [10] | High-specificity binding to extracellular targets to modulate function | In vivo efficacy and safety profiling | High | Generally restricted to cell surface and secreted proteins |
| Tool Compounds/Chemical Genomics [10] | Use of small bioactive molecules to modulate target protein function | Demonstration of phenotypic change with pharmacological intervention | Medium | Difficulty in finding highly specific tool compounds | |
| Direct Binding Assessment | Cellular Thermal Shift Assay (CETSA) [7] | Measure of target protein thermal stability shift upon ligand binding in cells | Quantitative confirmation of direct target engagement in a physiologically relevant context | Medium | Requires specific reagents and instrumentation |
Detailed Experimental Protocols for Key Validation Methods
To ensure reproducibility and informed selection, detailed protocols for three critical techniques are outlined below.
Protocol: In-silico Target Prediction with MolTarPred
MolTarPred is a ligand-centric method identified as one of the most effective for predicting molecular targets [3].
- Objective: To identify potential protein targets for a query small molecule based on structural similarity to known ligands.
- Database Setup: A validated database of ligand-target interactions, such as ChEMBL 34, is hosted locally. This database contains over 2.4 million compounds and 2.1 million interactions [3].
- Fingerprint Calculation: The canonical SMILES of both the query molecule and all database molecules are converted into molecular fingerprints. The Morgan fingerprint (radius 2, 2048 bits) has been shown to outperform others like MACCS [3].
- Similarity Searching: The Tanimoto similarity coefficient is calculated between the query molecule's fingerprint and every molecule in the database.
- Hit Identification: Database molecules are ranked by similarity score. The top 1, 5, 10, or 15 most similar ligands are selected, and their annotated targets are retrieved as the predicted targets for the query molecule [3].
Protocol: Target Engagement Validation with CETSA
CETSA bridges the gap between biochemical potency and cellular efficacy by confirming direct binding in physiologically relevant environments [7].
- Objective: To provide quantitative, system-level validation of direct drug-target engagement in intact cells or tissues.
- Cell Treatment: Live cells or tissue samples are treated with the compound of interest or a vehicle control (DMSO) across a range of concentrations and for specified time periods.
- Heat Challenge: Aliquots of the treated cell suspension are heated to different temperatures (e.g., from 45°C to 65°C) for a fixed time (e.g., 3 minutes) in a thermal cycler.
- Cell Lysis & Soluble Protein Extraction: Heated samples are subjected to freeze-thaw cycles or chemical lysis to break open the cells. The soluble protein fraction is separated from insoluble aggregates by high-speed centrifugation.
- Target Protein Quantification: The amount of soluble, non-aggregated target protein in each sample is quantified. This is typically done via immunoblotting (Western blot) or, for higher throughput and precision, high-resolution mass spectrometry [7].
- Data Analysis: The melting curve of the target protein (amount of soluble protein vs. temperature) is plotted for both compound-treated and vehicle-treated samples. A rightward shift in the melting curve (increased thermal stability) in the compound-treated samples confirms direct target engagement.
Protocol: Phenotypic Validation with siRNA
siRNA provides a reversible means of validating target function by selectively reducing its expression [10].
- Objective: To silence a specific target gene and observe the resulting phenotypic consequences in a cellular model of disease.
- siRNA Design: Commercially available or custom-designed double-stranded siRNAs (21-25 base pairs) targeting specific mRNA sequences of the gene of interest are acquired. A non-targeting (scrambled) siRNA must be used as a negative control.
- Cell Culture & Transfection: Relevant cell lines are cultured under standard conditions. The siRNA is introduced into the cells using a transfection reagent (e.g., lipofectamine), optimizing the reagent:siRNA ratio for maximum efficiency and minimal toxicity.
- Validation of Knockdown: 48-72 hours post-transfection, the efficiency of gene knockdown is confirmed. This is typically done by measuring a reduction in target mRNA levels using quantitative PCR (qPCR) and/or a reduction in target protein levels using immunoblotting.
- Phenotypic Assay: Cells with confirmed knockdown are subjected to disease-relevant phenotypic assays. These could include proliferation assays (for oncology), migration assays, or measurements of specific biochemical outputs. The phenotype of siRNA-treated cells is compared to cells treated with the non-targeting control siRNA.
Visualizing the Link Between Validation and Attrition
The following diagram illustrates the critical decision points in the drug discovery pipeline where rigorous target validation acts as a filter to prevent costly clinical trial failures.
Diagram: The Target Validation Funnel. Each validation stage filters out targets with poor translatability, preventing their progression to costly clinical trials where attrition is high. Bypassing or performing weak validation at any stage (red arrows) significantly increases the risk of failure [9].
Essential Research Reagent Solutions for Validation
A successful validation campaign relies on a suite of high-quality reagents and tools. The following table details key solutions.
Table 2: Key Research Reagent Solutions for Target Validation
| Reagent/Tool | Primary Function in Validation | Key Considerations for Selection |
|---|---|---|
| Validated Antibodies | Detection and quantification of target protein levels (e.g., via Western blot) after genetic or pharmacological perturbation. | Specificity (monoclonal vs. polyclonal), application validation (e.g., ICC, IHC, WB), and species reactivity. |
| siRNA/shRNA Libraries | Selective knockdown of target gene expression to study consequent phenotypic changes in cellular models. | On-target efficiency and validated minimal off-target effects; use of pooled vs. arrayed formats. |
| CRISPR-Cas9 Systems | Complete knockout of the target gene in cell lines to establish its necessity for a phenotype. | Efficiency of delivery (lentivirus, electroporation) and need for single-cell clone validation. |
| Tool Compounds | Pharmacological modulation of the target protein to establish a causal link between target function and phenotype. | High specificity and potency; careful matching of mechanism of action (agonist, antagonist, etc.) to the biological question. |
| Bioactive Compound Libraries | Used in chemical genomics to probe cellular function and identify novel targets through phenotypic screening. | Library diversity, chemical tractability, and availability of structural information. |
| ChEMBL / Public Databases | Provide a vast repository of known ligand-target interactions for in-silico target prediction and model training. | Data confidence scores, size of the database, and frequency of updates [3]. |
| AI-Powered Discovery Platforms | Accelerate data mining and hypothesis generation by uncovering hidden relationships between targets, diseases, and drugs from literature. | Ability to synthesize evidence from multiple sources and provide transparent citation of supporting data [11]. |
The high failure rate of clinical trials is a systemic challenge, but a significant portion of it is addressable through rigorous, front-loaded target validation. As the comparison of techniques demonstrates, no single method is sufficient; confidence is built through a convergence of evidence from computational, genetic, and pharmacological approaches. The integration of modern tools like AI for predictive analysis and CETSA for direct binding confirmation in cells provides an unprecedented ability to de-risk drug candidates before they enter the clinical phase. For researchers and drug developers, investing in a comprehensive, multi-faceted validation strategy is not merely a scientific best practice—it is a critical financial and ethical imperative to overcome the high cost of clinical trial failure.
The process of validating a drug target is a critical foundation upon which successful drug discovery and development is built. This initial phase determines whether a hypothesized biological target, typically a protein, is genuinely involved in a disease pathway and can be safely and effectively modulated by a therapeutic agent. The high failure rates in clinical development, often exceeding 90%, are frequently attributed to inadequate target validation, highlighting the crucial importance of this preliminary stage [12] [13]. The ideal drug target must satisfy three fundamental properties: demonstrated druggability (the ability to bind to drug-like molecules with high affinity), established safety (modulation does not produce unacceptable adverse effects), and clear disease-modifying potential (intervention alters the underlying disease pathology) [13].
Target validation has evolved significantly from traditional methods to incorporate sophisticated multi-omics approaches and artificial intelligence. The Open Targets initiative exemplifies this modern approach, systematically integrating evidence from human genetics, perturbation studies, transcriptomics, and proteomics to generate and prioritize therapeutic hypotheses [13]. This comprehensive evidence-gathering is essential for mitigating the substantial risks inherent in drug development, where the average cost exceeds $2 billion per approved therapy and the timeline spans 10-15 years [14] [12]. This guide provides a comparative analysis of contemporary target validation techniques, supported by experimental data and protocols, to equip researchers with practical frameworks for assessing the core properties of promising drug targets.
Core Properties of an Ideal Drug Target
Druggability: Structural and Functional Considerations
Druggability refers to the likelihood that a target can bind to a drug-like molecule with sufficient affinity and specificity to produce a therapeutic effect. This property is fundamentally determined by the target's structural characteristics, including the presence of suitable binding pockets, and its biochemical function.
Structural Druggability: The presence of well-defined binding pockets is a primary determinant of structural druggability. For instance, the discovery of cryptic allosteric pockets in mutant KRAS (G12C), once considered undruggable, enabled the development of covalent inhibitors like sotorasib and adagrasib [13]. Modern computational approaches have dramatically advanced structural assessment. AlphaFold2-generated protein structures have demonstrated remarkable utility in molecular docking for protein-protein interactions (PPIs), performing comparably to experimentally solved structures in virtual screening protocols [15]. As shown in Table 1, specific benchmarking against 16 PPI targets revealed that high-quality AlphaFold2 models (interface pTM + pTM > 0.7) achieved docking performance metrics similar to native structures, validating their use when experimental structures are unavailable [15].
Functional Druggability: Beyond structure, functional druggability considers the target's role in cellular pathways and the feasibility of modulating its activity. As Michelle Arkin notes, researchers may pursue multiple mechanistic hypotheses for the same target: "I want to inhibit the expression of the transcription factor; speed the degradation of this transcription factor; block the transcription factor binding to certain proteins it interacts with; stop its binding to DNA; stop the transcription of some of its downstream targets that I think are bad" [13]. Each approach represents a distinct druggability hypothesis with different implications for modality selection.
Table 1: Benchmarking AlphaFold2 Models for Druggability Assessment in Protein-Protein Interactions
| Metric | Performance in PPI Docking | Implication for Druggability Assessment |
|---|---|---|
| Model Quality (ipTM+pTM) | >0.7 (high-quality) for most complexes [15] | Suitable for initial binding site identification |
| TM-score | Median: 0.972 vs. experimental structures [15] | Accurate backbone prediction for binding pocket analysis |
| DockQ Score | Median: 0.838; 9/16 complexes high-quality (DockQ > 0.8) [15] | Reliable complex structure for interface targeting |
| Docking Performance | Comparable to native structures in virtual screening [15] | Validated use in absence of experimental structures |
| MD Refinement Impact | Improved outcomes in selected cases; significant variability [15] | Ensemble docking may enhance hit identification |
Safety: Therapeutic Index and Genetic Validation
Safety considerations for a drug target extend beyond compound-specific toxicities to include inherent risks associated with modulating the target itself. Ideal targets should offer a wide therapeutic index, where efficacy is achieved well below doses that cause mechanism-based adverse effects.
Genetic Evidence for Safety: Human genetics provides powerful insights into target safety profiles. As David Ochoa explains, "The more you understand about the problem, the less risks you have" [13]. Targets with human loss-of-function variants that are not associated with serious health consequences often represent safer intervention points. The presence of a target in essential biological processes or its expression in critical tissues may raise safety concerns that require careful evaluation during target selection [13].
Predictive Toxicology: Advanced computational models are increasingly employed to predict safety liabilities early in the validation process. Large language models (LLMs) and specialized AI tools can predict drug efficacy and safety profiles by analyzing historical data and chemical structures [14]. For example, the FP-ADMET and MapLight frameworks combine molecular fingerprints with machine learning models to establish robust prediction frameworks for a wide range of ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) properties, enabling earlier identification of potential safety issues [16].
Disease-Modifying Potential: Biomarkers and Clinical Translation
The ultimate validation of a target's disease-modifying potential requires demonstration that its modulation alters the underlying disease pathology and produces clinically meaningful benefits. This requires establishing a clear causal relationship between target activity and disease progression.
Biomarker Development: Biomarkers serve as essential tools for establishing disease-modifying potential throughout the drug development pipeline. In Alzheimer's disease, for example, the recent FDA approval of the Lumipulse G blood test measuring plasma pTau217/Aβ1-42 ratio provides a less invasive method for diagnosing cerebral amyloid plaques in symptomatic patients [17]. The 2018 and 2024 NIA-AA diagnostic criteria recognize multiple categories of biomarkers, including diagnostic, monitoring, prognostic, predictive, pharmacodynamic response, safety, and susceptibility biomarkers [17]. As shown in recent Alzheimer's trials, biomarker changes can provide early evidence of disease-modifying effects. Treatment with buntanetap reduced levels of neurofilament light (NfL), a protein fragment released from damaged neurons, indicating improved cellular integrity and neuronal health [18].
Clinical Endpoint Correlation: For a target to demonstrate genuine disease-modifying potential, its modulation must ultimately translate to improved clinical outcomes. In Huntington's disease research, the AMT-130 gene therapy reportedly showed approximately 75% slowing of disease progression based on the cUHDRS, a comprehensive clinical metric [19]. Similarly, Alzheimer's disease-modifying therapies lecanemab and donanemab showed 25% and 22.3% slowing of cognitive decline, respectively, in phase 3 trials, though these modest benefits highlight the challenges in achieving robust disease modification [17].
Table 2: Biomarker Classes for Establishing Disease-Modifying Potential
| Biomarker Category | Role in Target Validation | Examples |
|---|---|---|
| Diagnostic | Identify disease presence and involvement of specific targets [17] | Plasma pTau217/Aβ1-42 ratio for amyloid plaques [17] |
| Pharmacodynamic | Demonstrate target engagement and biological activity [17] | Reduction in IL-6, S100A12, IFN-γ, IGF1R with buntanetap [18] |
| Prognostic | Identify disease trajectory and treatment-responsive populations [17] | Neurofilament light (NfL) for neuronal damage [18] |
| Monitoring | Track treatment response and disease progression [17] | EEG changes in pre-symptomatic Huntington's disease [19] |
| Predictive | Identify patients most likely to respond to specific interventions [17] | APOE4 homozygosity status for ARIA risk with anti-amyloid antibodies [17] |
Comparative Analysis of Target Validation Techniques
Computational and AI-Driven Approaches
Artificial intelligence, particularly large language models, has introduced transformative capabilities for target validation. LLMs can process vast scientific literature and complex biomedical data to uncover target-disease linkages, predict drug-target interactions, and identify novel target opportunities [14]. Two distinct paradigms have emerged for applying LLMs in drug discovery:
Specialized Language Models: These models are trained on domain-specific scientific language, such as SMILES for small molecules and FASTA for proteins and polynucleotides. They learn statistical patterns from raw biochemical and genomic data to perform specialized tasks including predicting protein-ligand binding affinities when provided with a ligand's SMILES string and a protein's amino acid sequence [14].
General-Purpose Language Models: Pretrained on diverse text collections including scientific literature, these models possess capabilities such as reasoning, planning, tool use, and information retrieval. Researchers interact with these models as conversational assistants to solve specific problems in target validation [14].
The maturity of these approaches varies across different stages of target validation. For understanding disease mechanisms, specialized LLMs have reached "advanced" maturity (demonstrated efficacy in laboratory studies), while general LLMs remain at "nascent" stage (primarily investigated in silico) [14]. The optSAE + HSAPSO framework exemplifies advanced computational approaches, integrating stacked autoencoders with hierarchically self-adaptive particle swarm optimization to achieve 95.52% accuracy in drug classification and target identification tasks on DrugBank and Swiss-Prot datasets [12].
Experimental and Biochemical Methods
While computational approaches provide valuable initial insights, experimental validation remains essential for confirming a target's therapeutic potential. Several established methodologies provide critical evidence for druggability, safety, and disease-modifying potential.
Cellular and Molecular Profiling: Modern molecular representation methods have significantly advanced experimental target validation. AI-driven strategies such as graph neural networks, variational autoencoders, and transformers extend beyond traditional structural data, facilitating exploration of broader chemical spaces [16]. These approaches enable more effective characterization of the relationship between molecular structure and biological activity, which is crucial for assessing a target's druggability.
Biomarker Validation: As previously discussed, biomarkers provide critical evidence for a target's disease-modifying potential. The reduction of inflammatory markers (IL-5, IL-6, S100A12, IFN-γ, IGF1R) and neurofilament light chain in response to buntanetap treatment in Alzheimer's patients exemplifies how biomarker changes can demonstrate target engagement and biological effects [18]. Such pharmacodynamic biomarkers are increasingly incorporated into early-phase trials to provide proof-of-concept for a target's role in disease pathogenesis.
Structural Biology Techniques: Experimental methods for determining protein structure, such as X-ray crystallography and cryo-electron microscopy, provide the gold standard for assessing structural druggability. When experimental structures are unavailable, AlphaFold2 models have proven valuable alternatives, particularly for protein-protein interactions. Benchmarking studies reveal that local docking strategies using TankBind_local and Glide provided the best results across different structural types, with performance similar between native and AF2 models [15].
Integrated Workflow for Target Validation
The most effective target validation strategies combine computational and experimental approaches in a sequential workflow. The following diagram illustrates a comprehensive framework for evaluating druggability, safety, and disease-modifying potential:
Diagram Title: Integrated Target Validation Workflow
This integrated approach ensures comprehensive evaluation across all three critical properties. As emphasized throughout this guide, successful target validation requires evidence from multiple complementary methods rather than reliance on a single technique.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Advancing a target through validation requires specialized research tools and platforms. The following table details key solutions used in contemporary target validation studies:
Table 3: Essential Research Reagent Solutions for Target Validation
| Research Tool | Primary Function | Application in Target Validation |
|---|---|---|
| AlphaFold2 Models | Protein structure prediction [15] | Druggability assessment when experimental structures unavailable [15] |
| Molecular Docking Platforms (Glide, TankBind) | Binding pose and affinity prediction [15] | Virtual screening for initial hit identification [15] |
| LLM-Based Target-Disease Linkage Tools (Geneformer) | Disease mechanism understanding [14] | Identifying therapeutic targets through in silico perturbation [14] |
| Biomarker Assay Platforms (Lumipulse G) | Target engagement measurement [17] | Quantifying pharmacodynamic response in clinical trials [17] [18] |
| AI-Driven Molecular Representation (GNNs, VAEs, Transformers) | Chemical space exploration [16] | Scaffold hopping and lead compound optimization [16] |
| Automated Drug Design Frameworks (optSAE+HSAPSO) | Drug classification and target identification [12] | High-accuracy prediction of drug-target relationships [12] |
These tools represent the current state-of-the-art in target validation methodology. Their integrated application enables researchers to systematically evaluate the three fundamental properties of an ideal drug target before committing substantial resources to clinical development.
The validation of drug targets with ideal properties—demonstrated druggability, established safety, and clear disease-modifying potential—remains a complex but essential process in therapeutic development. As this comparison guide illustrates, successful validation requires integrating multiple lines of evidence from computational predictions, experimental data, and clinical observations. The emergence of sophisticated AI tools, particularly large language models and advanced molecular representation methods, has enhanced our ability to assess these properties earlier in the discovery process [14] [16]. However, these computational approaches complement rather than replace rigorous experimental validation.
The modest clinical benefits observed with recently approved disease-modifying therapies for Alzheimer's disease highlight the challenges in translating target validation to patient outcomes [17]. These experiences underscore the importance of continued refinement in validation methodologies, including the development of more predictive biomarkers and improved understanding of disease heterogeneity. As the field advances, the integration of multi-omics data, AI-driven analytics, and human clinical evidence will provide increasingly robust frameworks for identifying targets with genuine potential to address unmet medical needs safely and effectively.
In the intricate journey of drug discovery, target identification and target validation represent two fundamentally distinct yet deeply interconnected phases. For researchers and drug development professionals, understanding this critical distinction is not merely academic—it is essential for de-risking development pipelines and avoiding costly late-stage failures. Target identification encompasses the process of discovering biological molecules (proteins, genes, RNA) that play a key role in disease pathology. In contrast, target validation is the rigorous process of confirming that modulating the identified target will produce a meaningful therapeutic effect [20].
The distinction matters profoundly because many drug programs fail not due to compound inefficacy, but because the biological target itself was flawed—being non-essential, redundant, or insufficiently disease-modifying [20]. This guide provides a comparative analysis of these critical processes, examining their methodologies, experimental protocols, and technological frameworks within the broader context of target validation techniques research.
Core Conceptual Distinctions
At its essence, target identification is a discovery process, while target validation is a confirmation process. Target identification aims to pinpoint a "druggable" biological molecule that can be modulated—inhibited, activated, or altered—to produce a therapeutic effect. The output is typically a list of potential targets with established disease relevance and druggability [20].
Target validation, however, asks a more definitive question: Does modulating this target actually produce the desired therapeutic effect in a biologically relevant system? This phase focuses on establishing causal relationships between target modulation and disease phenotype, providing critical evidence for go/no-go decisions in the drug development pipeline [20].
Table 1: Fundamental Distinctions Between Target Identification and Validation
| Aspect | Target Identification | Target Validation |
|---|---|---|
| Primary Objective | Discover disease-relevant biological targets | Confirm therapeutic relevance of identified targets |
| Key Question | "What target should we pursue?" | "Does this target actually work as expected?" |
| Output | List of potential targets with disease relevance | Evidence of causal relationship between target and disease |
| Stage in Pipeline | Early discovery | Late discovery/early preclinical |
| Risk Mitigation | Identifies potential targets | Reduces attrition by validating target biology |
Methodological Comparison: Techniques and Technologies
Target Identification Methodologies
Modern target identification employs increasingly sophisticated technologies ranging from classical biochemical approaches to cutting-edge computational methods. Affinity purification, a cornerstone technique, operates on the principle of specific physical interactions between ligands and their targets. This "target fishing" approach uses immobilized compound bait to capture functional proteins from cell or tissue lysates for identification, typically via mass spectrometry [21] [22].
Advanced methods include photoaffinity labeling (PAL), which incorporates photoreactive moieties that form covalent bonds with target proteins upon light exposure, enabling the identification of even transient interactions [21] [22]. Click chemistry approaches utilize bioorthogonal reactions to label and identify target proteins within complex biological systems [21].
Computational approaches represent a paradigm shift in target identification. Artificial intelligence platforms now leverage knowledge graphs integrating trillions of data points from multi-omics datasets, scientific literature, and clinical databases. For instance, the PandaOmics platform analyzes over 1.9 trillion data points from more than 10 million biological samples to identify novel therapeutic targets [23]. Deep learning models can predict drug-target interactions with accuracies exceeding 95% in some implementations [12].
Target Validation Techniques
Target validation employs functional assays to establish causal relationships. CRISPR/Cas9 and RNA interference (RNAi) technologies enable targeted gene knockout or knockdown to observe resulting phenotypic changes [20]. Small-molecule inhibitor or activator assays test whether pharmacological modulation produces the expected therapeutic effects [20].
Cellular Thermal Shift Assay (CETSA) has emerged as a powerful label-free method for validating target engagement in physiologically relevant contexts. CETSA detects changes in protein thermal stability induced by ligand binding, providing direct evidence of compound-target interactions within intact cells and tissues [7]. Recent advances have coupled CETSA with high-resolution mass spectrometry to quantify drug-target engagement ex vivo and in vivo, confirming dose-dependent stabilization of targets like DPP9 in rat tissue [7].
Table 2: Comparative Analysis of Key Methodologies
| Methodology | Primary Application | Key Advantages | Technical Limitations |
|---|---|---|---|
| Affinity Purification | Target identification | Direct physical interaction capture; works with native proteins | Requires compound modification; may miss weak/transient interactions |
| Photoaffinity Labeling (PAL) | Target identification | Captures transient interactions; suitable for membrane proteins | Complex probe design; potential for non-specific labeling |
| AI/Knowledge Graphs | Target identification | Holistic biology perspective; integrates multimodal data | Dependent on data quality; "black box" interpretability challenges |
| CRISPR/Cas9 | Target validation | Precise genetic manipulation; establishes causal relationships | Off-target effects; may not reflect pharmacological modulation |
| CETSA | Target validation | Confirms binding in intact cells; no labeling required | Limited to interactions that alter thermal stability |
Experimental Protocols: Key Workflows
Affinity-Based Pull-Down Assay for Target Identification
The affinity purification protocol begins with chemical probe design, where the compound of interest is modified with a functional handle (e.g., biotin, alkyne/azide for click chemistry) while preserving its biological activity [21] [22]. The modified compound is then immobilized on a solid support (e.g., streptavidin beads for biotinylated probes).
Cell lysates are prepared under non-denaturing conditions to preserve native protein structures and interactions. The lysate is incubated with the compound-immobilized beads to allow specific binding between the target proteins and the compound bait. After extensive washing to remove non-specifically bound proteins, the specifically bound proteins are eluted and identified using liquid chromatography-tandem mass spectrometry (LC-MS/MS) [22].
Data analysis involves comparing the identified proteins against appropriate controls (e.g., beads with immobilized compound versus blank beads or beads with an inactive analog) to distinguish specific binders from non-specific interactions.
Cellular Thermal Shift Assay (CETSA) for Target Validation
The CETSA protocol begins by treating intact cells or cell lysates with the compound of interest or vehicle control across a range of concentrations. Following compound treatment, the samples are divided into aliquots and heated to different temperatures (typically spanning 37-65°C) for a fixed duration (e.g., 3 minutes) [7].
The heated samples are then cooled, and soluble proteins are separated from aggregated proteins by centrifugation or filtration. The remaining soluble target protein in each sample is quantified using immunoblotting, enzyme activity assays, or mass spectrometry. The resulting melting curves, plotting protein abundance against temperature, are compared between compound-treated and control samples [7].
A rightward shift in the melting curve (increased thermal stability) in compound-treated samples indicates direct binding and stabilization of the target protein. This shift can be quantified to determine the temperature at which 50% of the protein is denatured (Tm), providing a robust measure of target engagement.
Visualizing Workflows and Relationships
Sequential Relationship in Drug Discovery
Affinity Purification Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Target Identification and Validation
| Reagent/Category | Primary Function | Application Context |
|---|---|---|
| Biotin/Azide Handles | Enable compound immobilization or click chemistry conjugation | Affinity purification probes; photoaffinity labeling |
| Streptavidin Beads | Solid support for immobilizing biotinylated compound baits | Affinity pull-down assays |
| Photoactivatable Groups | (e.g., diazirines, aryl azides) form covalent bonds upon UV exposure | Photoaffinity labeling probes |
| CRISPR/Cas9 Systems | Precise gene editing for functional gene knockout | Target validation via genetic perturbation |
| siRNA/shRNA Libraries | Gene silencing through RNA interference | High-throughput target validation screening |
| CETSA Reagents | Buffer systems, detection antibodies, thermal cyclers | Cellular thermal shift assays for target engagement |
| Activity-Based Probes | Covalently label active sites of enzyme families | Activity-based protein profiling (ABPP) |
Emerging Technologies and Future Outlook
The landscape of target identification and validation is being transformed by artificial intelligence and novel chemical biology approaches. AI platforms now leverage multi-modal data integration, combining chemical, omics, text, and image data to construct comprehensive biological representations [23]. Generative AI models are being used not only for target identification but also for designing novel molecular entities optimized for binding affinity and metabolic stability [23] [24].
Label-free target deconvolution methods are gaining prominence, with techniques like solvent-induced denaturation shift assays enabling the study of compound-protein interactions under native conditions without chemical modifications that might disrupt biological activity [22]. These approaches are particularly valuable for identifying the targets of natural products, which often possess complex structures that challenge conventional modification strategies [21].
Integrated platforms that combine target identification and validation in seamless workflows represent the future of early drug discovery. Companies like Recursion and Verge Genomics have developed closed-loop systems where computational predictions are experimentally validated in-house, creating continuous feedback that refines both biological hypotheses and model performance [23]. As these technologies mature, the distinction between target identification and validation may blur, ultimately accelerating the translation of biological insights into therapeutic breakthroughs.
In modern drug development, establishing a therapeutic window—the dose range between efficacy and toxicity—is paramount for delivering safe medicines. A compound's safety profile is profoundly influenced by its interaction with both intended and off-target proteins, a concept known as polypharmacology [3]. While off-target effects can cause adverse reactions, they also present opportunities for drug repurposing, as exemplified by drugs like Gleevec and Viagra [3]. Consequently, accurately predicting drug-target interactions during early discovery phases is crucial for hypothesizing a molecule's eventual therapeutic window.
This guide objectively compares the performance of leading computational target prediction methods, which have become indispensable for initial target identification and validation. By enabling more precise identification of a compound's primary targets and potential off-targets, these in silico methods help researchers prioritize molecules with a higher probability of success, thereby de-risking the long and costly journey toward establishing a clinical therapeutic window [25].
Performance Comparison of Target Prediction Methods
A precise comparative study published in 2025 systematically evaluated seven stand-alone codes and web servers using a shared benchmark of FDA-approved drugs [3]. The performance was measured using Recall, which indicates the method's ability to identify all known targets for a drug, and Precision, which reflects the accuracy of its predictions. High recall is particularly valuable for drug repurposing, as it minimizes missed opportunities, while high precision provides greater confidence for downstream experimental validation [3].
The table below summarizes the key performance metrics and characteristics of the evaluated methods.
Table 1: Comprehensive Comparison of Target Prediction Method Performance and Characteristics
| Method Name | Type | Core Algorithm | Key Database Source | Recall (Top 1) | Precision (Top 1) | Key Findings |
|---|---|---|---|---|---|---|
| MolTarPred [3] | Ligand-centric | 2D Similarity | ChEMBL 20 | 0.410 | 0.310 | Most effective overall; Morgan fingerprints with Tanimoto score recommended. |
| PPB2 [3] | Ligand-centric | Nearest Neighbor/Naïve Bayes/Deep Neural Network | ChEMBL 22 | 0.250 | 0.160 | - |
| RF-QSAR [3] | Target-centric | Random Forest | ChEMBL 20 & 21 | 0.230 | 0.160 | - |
| TargetNet [3] | Target-centric | Naïve Bayes | BindingDB | 0.210 | 0.130 | - |
| ChEMBL [3] | Target-centric | Random Forest | ChEMBL 24 | 0.200 | 0.130 | - |
| CMTNN [3] | Target-centric | ONNX Runtime | ChEMBL 34 | 0.190 | 0.120 | - |
| SuperPred [3] | Ligand-centric | 2D/Fragment/3D Similarity | ChEMBL & BindingDB | 0.180 | 0.110 | - |
Key Performance Insights
- Performance Trade-offs: The data reveals a clear performance gap, with MolTarPred significantly outperforming other methods in both recall and precision [3]. This makes it a superior choice for applications where maximizing the identification of true targets is critical.
- Ligand-centric vs. Target-centric: On average, ligand-centric methods (MolTarPred, PPB2) in this evaluation demonstrated higher recall than target-centric approaches (RF-QSAR, TargetNet). Ligand-centric methods predict targets based on the similarity of a query molecule to known active ligands, while target-centric methods use predictive models built for specific targets [3].
- Impact of High-Confidence Filtering: Applying a high-confidence filter (e.g., using only interactions with a ChEMBL confidence score ≥ 7) improves precision but at the cost of reduced recall. This makes such filtering less ideal for exploratory drug repurposing projects where the goal is to uncover all possible opportunities [3].
Experimental Protocols for Method Evaluation
To ensure a fair and unbiased comparison, the evaluation of the seven target prediction methods followed a rigorous and standardized experimental protocol [3].
Database Preparation and Curation
- Data Source: The ChEMBL database (version 34) was used as the primary source of bioactivity data. It contained over 2.4 million compounds and 20.7 million interactions against 15,598 targets at the time of the study [3].
- Data Filtering:
- Bioactivity records were selected based on standard values (IC50, Ki, or EC50) below 10,000 nM.
- Entries associated with non-specific or multi-protein targets were excluded.
- Duplicate compound-target pairs were removed, resulting in 1,150,487 unique ligand-target interactions for the main database [3].
- Benchmark Dataset: A separate benchmark dataset was created from 100 randomly selected FDA-approved drugs. Critically, these molecules were excluded from the main database to prevent any overlap and avoid over-optimistic performance estimates during prediction [3].
Prediction and Validation Methodology
- Method Execution: The seven methods were run against the prepared database. MolTarPred and CMTNN were executed locally using stand-alone codes, while the others were accessed via their respective web servers [3].
- Performance Metrics Calculation: For each method, predictions were generated for the 100 benchmark drugs. Recall and Precision at the top prediction (Top 1) were calculated based on the methods' ability to correctly identify the known annotated targets from the curated ChEMBL data [3].
The following workflow diagram illustrates the complete experimental process from data preparation to performance evaluation.
Case Study: Target Prediction in Action
A practical application of this pipeline was demonstrated through a case study on fenofibric acid, a drug used for lipid management. The target prediction and MoA hypothesis generation pipeline suggested the Thyroid Hormone Receptor Beta (THRB) as a potential target, indicating opportunities for repurposing fenofibric acid for thyroid cancer treatment [3].
This case exemplifies how computational target prediction can generate testable mechanistic hypotheses. By proposing a new target and potential indication, it lays the groundwork for subsequent experimental validation, a critical step in translating a computational finding into a therapeutic strategy with a viable clinical window.
Successful target prediction and validation rely on a foundation of high-quality data and software tools. The table below lists key resources utilized in the benchmark study and the wider field.
Table 2: Key Research Reagents and Resources for Target Prediction
| Resource Name | Type | Primary Function in Research | Key Features |
|---|---|---|---|
| ChEMBL Database [3] | Bioactivity Database | Provides curated, experimentally validated bioactivity data (IC50, Ki, etc.) for training and validating prediction models. | Contains over 2.4 million compounds and 20 million interactions; includes confidence scores. |
| MolTarPred [3] | Stand-alone Software | Predicts drug targets based on 2D chemical similarity to known active ligands. | Open-source; allows local execution; configurable fingerprints and similarity metrics. |
| PPB2, RF-QSAR, etc. [3] | Web Server / Software | Provides alternative algorithms (Neural Networks, Random Forest) for target prediction via web interface or code. | Accessible without local installation; some integrate multiple data sources and methods. |
| CETSA [7] | Experimental Assay | Validates target engagement in intact cells or tissues, bridging computational prediction and physiological relevance. | Measures thermal stabilization of target proteins upon ligand binding in a cellular context. |
| AlphaFold [25] | AI Software | Generates highly accurate 3D protein structures from amino acid sequences, enabling structure-based prediction. | Expands target coverage for methods requiring protein structures (e.g., molecular docking). |
The systematic comparison establishes MolTarPred as the most effective method for comprehensive target identification, a critical first step in hypothesizing a compound's therapeutic window [3]. The broader trend in drug discovery is the integration of such computational methods with experimental validation techniques like CETSA to create robust, data-rich workflows [7]. This synergy between in silico prediction and empirical validation helps de-risk the drug development process, enabling more informed decisions earlier in the pipeline.
As the field evolves, the emergence of agentic AI systems and more sophisticated foundation models promises to further augment this process [26]. However, these computational tools remain powerful complements to, rather than replacements for, traditional medicinal chemistry and experimental biology. The ultimate goal of establishing a safe and efficacious therapeutic window is best served by a hybrid human-AI approach that leverages the strengths of both [26].
A Practical Guide to Key Target Validation Methods and Techniques
In modern drug discovery, establishing a direct causal relationship between a gene target and a disease phenotype is paramount. Genetic perturbation tools—technologies that allow researchers to selectively reduce or eliminate the function of a gene—form the backbone of this functional validation process. For over a decade, RNA interference (RNAi) served as the primary method for gene silencing. However, the emergence of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9 has fundamentally transformed the landscape [27] [28]. This guide provides an objective, data-driven comparison of these two foundational technologies, focusing on their mechanisms, performance, and optimal applications within target validation workflows. Understanding their distinct operational frameworks, strengths, and limitations enables researchers to select the most appropriate tool, thereby de-risking the early stages of therapeutic development.
RNA Interference (RNAi): The Knockdown Pioneer
RNAi is an endogenous biological process that harnesses a natural cellular pathway for gene regulation. Experimental RNAi utilizes synthetic small interfering RNAs (siRNAs) or vector-encoded short hairpin RNAs (shRNAs) that are introduced into cells. The core mechanism involves several steps. First, the cytoplasmic double-stranded RNA (dsRNA) is processed by the endonuclease Dicer into small fragments approximately 21 nucleotides long. These siRNAs then load into the RNA-induced silencing complex (RISC). Within RISC, the antisense strand guides the complex to complementary messenger RNA (mRNA) sequences. Finally, the Argonaute protein within RISC cleaves the target mRNA, preventing its translation into protein. This results in a knockdown—a reduction, but not complete elimination, of gene expression at the mRNA level [27]. The effect is typically transient and reversible, which can be advantageous for studying essential genes.
CRISPR-Cas9: The Genome Editing Powerhouse
The CRISPR-Cas9 system functions as a programmable DNA-editing tool, adapted from a bacterial immune defense mechanism. Its operation occurs at the genomic DNA level and requires two components: a Cas9 nuclease and a guide RNA (gRNA). The gRNA, designed to be complementary to a specific DNA locus, directs the Cas9 nuclease to the target site in the genome. Upon binding, the Cas9 nuclease creates a precise double-strand break (DSB) in the DNA. The cell's repair machinery, specifically the error-prone non-homologous end joining (NHEJ) pathway, then fixes this break. This repair often introduces small insertions or deletions (indels), which can disrupt the coding sequence of the gene. If a frameshift mutation occurs, it leads to a premature stop codon and a complete loss of functional protein, resulting in a permanent knockout [27] [29]. This fundamental difference—operating at the DNA level versus the mRNA level—is the primary source of the contrasting performance profiles of CRISPR and RNAi.
The following diagram illustrates the core mechanistic differences between these two technologies.
Performance Comparison: Quantitative Data
Direct comparative studies and user surveys provide critical insights into the real-world performance of RNAi and CRISPR-Cas9. The data below summarize key performance metrics from published literature and industry reports.
Table 1: Performance Comparison of RNAi and CRISPR-Cas9
| Performance Metric | RNAi (shRNA/siRNA) | CRISPR/Cas9 Knockout | Supporting Data |
|---|---|---|---|
| Genetic Outcome | Reversible knockdown (mRNA level) | Permanent knockout (DNA level) | [27] [29] |
| Silencing Efficiency | Moderate to low (variable protein reduction) | High (complete, stable silencing) | [30] [31] |
| Off-Target Effects | High (due to miRNA-like off-targeting) | Low (with optimized gRNA design) | [27] [31] |
| Primary Use in Screens | ~34% of researchers (non-commercial) | ~49% of researchers (non-commercial) | [32] |
| Essential Gene Detection (AUC) | >0.90 | >0.90 | [33] |
| Typical Workflow Duration | Weeks | 3-6 months for stable cell lines | [32] |
A systematic comparison in the K562 chronic myelogenous leukemia cell line demonstrated that both technologies are highly capable of identifying essential genes, with Area Under the Curve (AUC) values exceeding 0.90 for both [33]. However, the same study revealed a surprisingly low correlation between the specific hits identified by each technology, suggesting that they may reveal distinct aspects of biology or be susceptible to different technical artifacts [33].
Industry adoption data from a recent survey underscores the shifting preference, with 48.5% of researchers in non-commercial institutions reporting CRISPR as their primary genetic modification method, compared to 34.6% for RNAi [32]. Notably, the survey also highlighted that CRISPR workflows are often more time-consuming, with researchers reporting a median of 3 months to generate knockouts and needing to repeat the entire workflow a median of 3 times before success [32].
Experimental Protocols and Workflows
RNAi Workflow for Gene Knockdown
The standard workflow for an RNAi experiment involves a series of defined steps. First, siRNA/shRNA Design: Sequences of 21-22 nucleotides are designed to be complementary to the target mRNA, often using algorithms to maximize specificity and efficacy [27]. Next is Delivery: The designed siRNAs (synthetic) or shRNA-encoding plasmids are introduced into cells via transfection. A key advantage of RNAi is that cells possess the endogenous machinery (Dicer, RISC) required for the process, simplifying delivery [27]. Finally, Validation: The efficiency of gene silencing is typically measured 48-72 hours post-transfection by quantifying mRNA transcript levels (using qRT-PCR) and/or protein levels (using immunoblotting or immunofluorescence) [27].
CRISPR-Cas9 Workflow for Gene Knockout
The CRISPR-Cas9 workflow, while more complex, enables permanent genetic modification. A critical first step is gRNA Design and Selection: A 20-nucleotide guide RNA sequence is designed to target a specific genomic locus adjacent to a PAM sequence. The use of state-of-the-art design tools and algorithms (e.g., Benchling) is critical for predicting cleavage efficiency and minimizing off-target effects [27] [34]. The next step is Delivery of CRISPR Components: The Cas9 nuclease and gRNA can be delivered in various formats, including plasmids, in vitro transcribed RNAs (IVT), or pre-complexed ribonucleoprotein (RNP) complexes. The RNP format is increasingly the preferred choice due to its high editing efficiency and reduced off-target effects [27] [34]. Following delivery, a Clonal Isolation and Expansion step is often necessary. After editing, cells are single-cell sorted and expanded into clonal populations to isolate those with homozygous knockouts. This step is notoriously time-consuming, often requiring repetition to obtain the desired edit [32] [34]. The process concludes with Validation and Genotyping: The editing efficiency is analyzed in the cell pool using tools like T7E1 assay or TIDE. For clonal lines, Sanger sequencing of the target locus is performed, with analysis by tools like ICE (Inference of CRISPR Edits) to determine the exact indel sequences [27] [34]. Western blotting is recommended to confirm the complete absence of the target protein, as some indels may not result in a frameshift and functional knockout [34].
The following workflow provides a visual summary of the key steps in a CRISPR knockout experiment.
Research Reagent Solutions
Successful genetic perturbation experiments rely on a suite of critical reagents and tools. The table below details essential materials and their functions.
Table 2: Key Research Reagents for Genetic Perturbation Experiments
| Reagent / Tool | Function | Application Notes |
|---|---|---|
| siRNA (synthetic) | Chemically synthesized double-stranded RNA for transient knockdown. | Ideal for rapid, short-term experiments; high potential for off-target effects [27]. |
| shRNA (lentiviral) | DNA vector encoding a short hairpin RNA for stable, long-term knockdown. | Allows for selection of transduced cells; potential for integration-related artifacts [33]. |
| Cas9 Nuclease | Bacterial-derived or recombinant enzyme that cuts DNA. | High-fidelity variants are available to reduce off-target activity [27] [34]. |
| Guide RNA (gRNA) | Synthetic RNA that directs Cas9 to a specific DNA sequence. | Chemically modified sgRNAs (CSM-sgRNA) enhance stability and efficiency [34]. |
| RNP Complex | Pre-assembled complex of Cas9 protein and gRNA. | Gold standard for delivery; high efficiency, rapid action, and reduced off-target effects [27]. |
| ICE / TIDE Analysis | Bioinformatics tools for analyzing Sanger sequencing data from edited cell pools. | Provides a quantitative estimate of indel efficiency without needing full NGS [27] [34]. |
The choice between RNAi and CRISPR-Cas9 is not a simple matter of one technology being universally superior. Instead, it is a strategic decision based on the specific research question, the gene of interest, and the desired experimental outcome.
CRISPR-Cas9 has rightfully become the gold standard for most loss-of-function studies due to its high efficiency, permanence, and DNA-level precision. It is the preferred tool for definitive target validation, creating stable knockout cell lines, and screening for non-essential genes. However, its permanent nature and the lengthy process of generating clonal lines are significant drawbacks for certain applications [32] [29].
RNAi remains a valuable and complementary tool. Its transient nature is advantageous for studying essential genes, whose complete knockout would be lethal to cells. It also allows for the verification of phenotypes by observing reversal upon restoration of gene expression. The simpler and faster workflow makes it suitable for initial, high-throughput pilot screens [27] [28].
A powerful emerging strategy is to use both technologies in tandem. Initial hits from a genome-wide CRISPR screen can be validated using RNAi-mediated knockdown. The convergence of phenotypes across both technologies provides strong evidence for a true genotype-phenotype link, minimizing the risk of technology-specific artifacts [33] [31]. As the field advances, the integration of these perturbation tools with other cutting-edge technologies like AI-driven target prediction [3] and cellular target engagement assays [7] will further strengthen the rigor of target validation and accelerate the development of novel therapeutics.
Chemical probes are highly characterized small molecules that serve as essential tools for determining the function of specific proteins in experimental systems, from biochemical assays to complex in vivo settings [35]. These probes represent powerful reagents in chemical biology for investigating protein function and establishing the therapeutic potential of molecular targets [36]. The critical importance of high-quality chemical probes lies in their ability to increase the robustness of fundamental and applied research, ultimately supporting the development of new therapeutic agents, including cancer drugs [36].
The field has evolved significantly from earlier periods when researchers frequently used weak and non-selective compounds, which generated an abundance of erroneous conclusions in the scientific literature [35]. Contemporary guidelines have established minimal criteria or "fitness factors" that define high-quality chemical probes, requiring high potency (IC50 or Kd < 100 nM in biochemical assays, EC50 < 1 μM in cellular assays) and strong selectivity (selectivity >30-fold within the protein target family) [35]. Additionally, best practices mandate the use of appropriate controls, including inactive analogs and structurally distinct probes targeting the same protein, to confirm on-target effects [35].
With the growing importance of chemical probes in biomedical research, several resources have emerged to help scientists select the most appropriate tools for their experiments. The table below provides a comparative overview of the major publicly available chemical probe resources:
Table 1: Comparison of Major Chemical Probe Resources
| Resource Name | Primary Focus | Key Features | Coverage | Assessment Method |
|---|---|---|---|---|
| Chemical Probes Portal | Expert-curated probe recommendations | "TripAdvisor-style" star ratings (1-4 stars), expert reviews, usage guidelines [36] [37] | ~800 expert-annotated chemical probes, 570 human protein targets [36] | International expert panel review (Scientific Expert Review Panel) [36] |
| Probe Miner | Comprehensive bioactivity data analysis | Statistically-based ranking derived from mining bioactivity data [35] | >1.8 million small molecules, >2,200 human targets [35] | Computational analysis of medicinal chemistry literature from ChEMBL and canSAR [35] |
| SGC Chemical Probes Collection | Unencumbered access to chemical probes | Openly available probes without intellectual property restrictions [35] | >100 chemical probes targeting epigenetic proteins, kinases, GPCRs [35] | Collaborative development between academia and pharmaceutical companies [35] |
| OpnMe Portal | Pharmaceutical company-developed probes | Freely available high-quality small molecules from Boehringer Ingelheim [35] | In-house developed chemical probes | Pharmaceutical company curation and distribution [35] |
Each resource offers distinct advantages depending on researcher needs. The Chemical Probes Portal provides expert guidance on optimal usage conditions and limitations, while Probe Miner offers comprehensive data-driven rankings across a broader chemical space [35]. The SGC Chemical Probes Collection and OpnMe Portal provide direct access to physical compounds, with the former specializing in unencumbered probes that stimulate open research [35].
Experimental Approaches for Probe Characterization
Target Engagement Validation with CETSA
A critical step in confirming chemical probe utility involves demonstrating direct engagement with the intended protein target in physiologically relevant environments. The Cellular Thermal Shift Assay (CETSA) has emerged as a leading approach for validating direct binding in intact cells and tissues [7]. This method is particularly valuable for confirming that chemical probes effectively engage their targets in complex biological systems rather than merely under simplified biochemical conditions.
Table 2: Key Applications of CETSA in Probe Characterization
| Application Area | Experimental Approach | Key Outcome Measures |
|---|---|---|
| Cellular Target Engagement | Heating probe-treated cells, measuring thermal stabilization of target protein [7] | Dose-dependent and temperature-dependent stabilization of target protein [7] |
| Tissue Penetration Assessment | Ex vivo CETSA on tissues from probe-treated animals [7] | Confirmation of target engagement in relevant physiological environments [7] |
| Mechanistic Profiling | CETSA combined with high-resolution mass spectrometry [7] | System-level validation of drug-target engagement across multiple protein targets [7] |
Recent work by Mazur et al. (2024) applied CETSA in combination with high-resolution mass spectrometry to quantitatively measure drug-target engagement of DPP9 in rat tissue, successfully confirming dose- and temperature-dependent stabilization both ex vivo and in vivo [7]. This approach provides crucial evidence bridging the gap between biochemical potency and cellular efficacy, addressing a fundamental challenge in chemical biology and drug discovery.
Proximity-Based Target Validation for Heterobifunctional Molecules
For novel modalities such as proteolysis-targeting chimeras (PROTACs) and other heterobifunctional molecules, conventional binding assays may not adequately capture the complex proximity-inducing mechanisms of these compounds. A 2025 study developed an innovative method using AirID, a proximity biotinylation enzyme, to validate proteins that interact with heterobifunctional molecules in cells [38].
The experimental workflow involves fusing AirID to E3 ligase binders such as CRBN or VHL, which are commonly used in PROTAC designs. When heterobifunctional molecules bring target proteins into proximity with these fused constructs, AirID biotinylates the nearby proteins, enabling their isolation and identification through streptavidin pull-down assays and liquid chromatography-tandem mass spectrometry (LC-MS/MS) [38].
Diagram 1: Proximity Validation Workflow for Heterobifunctional Molecules. The diagram illustrates the experimental workflow for validating targets of heterobifunctional molecules using AirID-based proximity biotinylation, from compound treatment to interactome profiling.
This methodology enabled researchers to compare the interactome profiles of PROTACs sharing the same target binder but different E3 ligase binders. For example, the approach revealed different interaction patterns between ARV-825 (which uses a CRBN binder) and MZ1 (which uses a VHL binder), despite both targeting BET proteins with the JQ-1 target binder [38]. The system also demonstrated the ability to identify nuclear interactions between the androgen receptor and the clinical-stage PROTAC ARV-110 [38].
Essential Research Reagent Solutions
The following table details key reagents and materials essential for conducting rigorous chemical probe experiments:
Table 3: Essential Research Reagent Solutions for Chemical Probe Studies
| Reagent/Material | Primary Function | Application Examples |
|---|---|---|
| High-Quality Chemical Probes | Selective modulation of specific protein targets | Investigating protein function in cells and model organisms [36] [35] |
| Inactive Analogues | Control compounds for confirming on-target effects | Distinguishing specific from non-specific effects in experimental systems [35] |
| CETSA Reagents | Validation of target engagement in physiologically relevant contexts | Confirming cellular target engagement; assessing tissue penetration [7] |
| AirID Fusion Constructs | Proximity-dependent biotinylation of protein interactors | Identifying intracellular interactomes of heterobifunctional molecules [38] |
| Streptavidin Pull-Down Materials | Isolation of biotinylated proteins | Enriching target proteins for identification by mass spectrometry [38] |
| LC-MS/MS Systems | Protein identification and quantification | Comprehensive interactome mapping and biotinylation site identification [38] |
Decision Framework for Chemical Probe Selection and Use
Selecting appropriate chemical probes requires careful consideration of multiple factors to ensure experimental validity. The following diagram outlines a systematic approach to probe selection and validation:
Diagram 2: Chemical Probe Selection and Validation Framework. This decision workflow outlines the key steps and evaluation criteria for selecting and validating high-quality chemical probes for biological research.
Approximately 85% of probes reviewed on the Chemical Probes Portal receive ratings of three or four stars, indicating they can be used with especially high confidence in biological experiments [36]. The Portal also identifies "The Unsuitables" – 258 compounds not appropriate for use as chemical probes, including molecules that were once useful as pathfinders but have been superseded by higher-quality alternatives, as well as compounds long recognized as promiscuously active [36].
Chemical probes represent indispensable tools in modern chemical biology and drug discovery when selected and used appropriately. The expanding landscape of chemical probe resources, coupled with advanced validation methodologies like CETSA and AirID-based proximity labeling, provides researchers with powerful frameworks for conducting robust, reproducible research. By adhering to established best practices for probe selection and validation, and leveraging the growing repertoire of publicly available resources, scientists can significantly enhance the quality and translational potential of both fundamental and applied biomedical research. As the field progresses toward goals like Target 2035's aim to develop a chemical probe for every human protein, these rigorous approaches to probe characterization and usage will become increasingly critical for advancing our understanding of protein function and accelerating therapeutic development.
Validating that a therapeutic compound physically engages its intended protein target is a critical step in modern drug discovery, providing the essential link between a molecule's biochemical interaction and its observed biological effect [39] [40]. Without direct evidence of target binding, it is impossible to confidently establish a compound's mechanism of action. Among the powerful label-free techniques developed for this purpose, the Cellular Thermal Shift Assay (CETSA) has emerged as a premier biophysical method for studying drug-target interactions directly in physiological environments [41] [42]. First introduced in 2013, CETSA exploits the fundamental principle that ligand binding often enhances the thermal stability of proteins by reducing their conformational flexibility [41] [43]. Unlike traditional methods that require chemical modification of compounds or proteins, CETSA directly assesses changes in protein thermal stability upon small molecule binding, providing a straightforward and physiologically relevant approach for confirming target engagement under native conditions [41] [40].
CETSA's key advantage lies in its ability to bridge the gap between simplified biochemical assays and complex cellular environments. While conventional biochemical assays measure interactions using purified proteins in non-physiological buffers, CETSA can be performed in intact cells, lysates, and even tissues, preserving the native cellular context including protein-protein interactions, post-translational modifications, and the presence of natural co-factors [42]. This capability is crucial because intracellular physicochemical conditions—including molecular crowding, viscosity, ion composition, and cosolvent content—differ significantly from standard assay buffers and can profoundly influence binding equilibria [44]. By measuring target engagement where it matters most, CETSA provides translational confidence that a compound not only binds its purified target but also reaches and engages the target in a biologically relevant system [7] [45].
CETSA Principles and Comparative Analysis with Alternative Methods
Fundamental Principles of CETSA
The CETSA methodology is grounded in the biophysical phenomenon of ligand-induced thermal stabilization. When a small molecule binds to its target protein, it frequently stabilizes the protein's native conformation, making it more resistant to heat-induced denaturation. This stabilization manifests as an increase in the protein's melting temperature (Tm), which represents the temperature at which 50% of the protein remains in its folded state [39] [41].
The standard CETSA workflow involves several key steps: First, biological samples (intact cells, lysates, or tissues) are treated with the compound of interest or vehicle control. These samples are then subjected to a temperature gradient in a thermal cycler or water bath. Upon heating, unbound proteins denature and aggregate, while ligand-bound proteins remain soluble. The samples are subsequently cooled, lysed (if intact cells were used), and centrifuged to separate soluble (folded) proteins from insoluble (aggregated) proteins. Finally, the remaining soluble target protein is quantified using detection methods such as Western blot, immunoassays, or mass spectrometry [41] [39] [42].
Two primary experimental formats are employed in CETSA: the thermal melt curve assay and the isothermal dose-response (ITDR) assay. In melt curve experiments, samples treated with a saturating compound concentration are heated across a temperature range to generate sigmoidal melting curves and determine Tm shifts (ΔTm). This format confirms binding but does not directly indicate compound potency. In ITDR-CETSA, samples are treated with a concentration gradient of the compound and heated at a single fixed temperature (typically near the protein's Tm) to generate dose-response curves and calculate EC50 values, enabling quantitative assessment of binding affinity and compound ranking [41] [42].
Comparative Analysis of Target Engagement Techniques
While CETSA has gained significant adoption, several other label-free techniques are available for studying target engagement, each with distinct principles, advantages, and limitations. The most prominent alternatives include Drug Affinity Responsive Target Stability (DARTS), Stability of Proteins from Rates of Oxidation (SPROX), and Limited Proteolysis (LiP) [40] [42].
The table below provides a comprehensive comparison of these key techniques across multiple performance dimensions:
Table 1: Comparative Analysis of Label-Free Target Engagement Techniques
| Feature | CETSA | DARTS | SPROX | Limited Proteolysis (LiP) |
|---|---|---|---|---|
| Principle | Detects thermal stabilization upon ligand binding | Detects protection from protease digestion | Detects changes in methionine oxidation patterns | Detects altered protease accessibility |
| Sample Type | Live cells, lysates, tissues | Cell lysates, purified proteins | Cell lysates | Cell lysates |
| Detection Methods | Western blot, AlphaLISA, MS | SDS-PAGE, Western blot, MS | Mass spectrometry | Mass spectrometry |
| Throughput | High (especially CETSA HT/MS) | Low to moderate | Medium to high | Medium to high |
| Quantitative Capability | Strong (dose-response curves) | Limited; semi-quantitative | Quantitative | Semi-quantitative |
| Physiological Relevance | High (in live cells) | Medium (native-like environment) | Medium (lysate environment) | Medium (lysate environment) |
| Binding Site Information | No | Limited | Yes (domain-level) | Yes (peptide-level) |
| Key Advantage | Works in physiologically relevant environments | No labeling; cost-effective | Provides binding site information | Identifies binding regions |
| Main Limitation | Some interactions don't cause thermal shifts | Protease optimization challenging | Limited to methionine-containing peptides | Relies on single peptide data |
DARTS operates on a different principle than CETSA, detecting ligand-induced protection against proteolytic degradation rather than thermal stabilization. When a small molecule binds to its target protein, it can cause conformational changes that protect specific regions from protease attack. The DARTS workflow involves incubating protein mixtures with the test compound, followed by limited proteolysis and analysis of the remaining target protein [40]. While DARTS doesn't require specialized equipment and is cost-effective, it typically offers lower throughput and less quantitative results compared to CETSA [40].
SPROX and LiP utilize mass spectrometry to detect ligand-induced conformational changes through different mechanisms. SPROX employs a chemical denaturant gradient with methionine oxidation to detect domain-level stability shifts, while LiP uses proteolysis to identify protein regions with altered accessibility upon ligand binding [42]. Both methods can provide binding site information that CETSA cannot, but they are primarily limited to lysate applications and may generate more false positives due to reliance on limited peptide data [42].
Table 2: Method Selection Guide Based on Research Objectives
| Research Objective | Recommended Method | Rationale |
|---|---|---|
| Live cell target engagement | CETSA (intact cells) | Preserves native cellular environment and physiology |
| High-throughput screening | CETSA HT (bead-based) | Enables screening of thousands of compounds |
| Proteome-wide off-target profiling | CETSA MS (TPP) | Simultaneously monitors ~7,000 proteins |
| Binding site identification | SPROX or LiP | Provides domain or peptide-level resolution |
| Early-stage validation with limited resources | DARTS | Low cost, no special equipment needed |
| Membrane protein targets | CETSA | Effective for studying kinases and membrane proteins |
| Weak binders or subtle conformers | DARTS | Detects subtle conformational changes |
CETSA Workflow and Experimental Design
Key CETSA Formats and Methodologies
CETSA has evolved into several specialized formats tailored to different research applications and detection capabilities. The primary variants include:
Western Blot-based CETSA (WB-CETSA) represents the original implementation, using protein-specific antibodies for detection through Western blotting. This format is relatively simple to implement in standard laboratories without specialized equipment but has limited throughput due to antibody requirements. WB-CETSA is best suited for hypothesis-driven studies validating known target proteins rather than discovering novel targets [41] [42].
Mass Spectrometry-based CETSA (MS-CETSA), also known as Thermal Proteome Profiling (TPP), replaces Western blotting with mass spectrometry to simultaneously monitor thermal stability changes across thousands of proteins. This unbiased approach enables comprehensive identification of drug targets and off-targets across the proteome. MS-CETSA is particularly powerful for mechanism of action studies and polypharmacology assessment but requires advanced instrumentation, complex data processing, and significant expertise [41] [42].
High-Throughput CETSA (HT-CETSA) utilizes bead-based immunoassays like AlphaLISA or split-luciferase systems (BiTSA) to enable screening of large compound libraries. This format is ideal for structure-activity relationship (SAR) studies and lead optimization campaigns, bridging the gap between biochemical assays and cellular phenotypes [46] [42].
Two-Dimensional TPP (2D-TPP) combines temperature and compound concentration gradients in a single experiment, providing a multidimensional view of ligand-target interactions. This integrated approach simultaneously assesses thermal stability and binding affinity, offering high-resolution insights into both binding dynamics and engagement potency [41] [42].
The following workflow diagram illustrates the key decision points and methodologies in designing a CETSA experiment:
Detailed Experimental Protocol for WB-CETSA
For researchers implementing CETSA for the first time, the Western blot-based format provides an accessible entry point. The following protocol outlines a standardized approach for intact cell WB-CETSA:
Sample Preparation:
- Culture adherent or suspension cells under standard conditions until they reach 70-90% confluence.
- Treat experimental groups with compound of interest dissolved in appropriate vehicle (typically DMSO). Include vehicle-only controls.
- Incubate for predetermined time (typically 30 minutes to 2 hours) at 37°C to allow compound uptake and target engagement.
- Harvest cells using gentle trypsinization (adherent cells) or centrifugation (suspension cells).
- Wash cells with PBS and resuspend in PBS or culture medium at a density of 3-5 million cells/mL.
- Aliquot cell suspensions into PCR tubes (typically 50-100 μL per tube) for heating.
Heat Challenge and Protein Extraction:
- Program thermal cycler with a temperature gradient spanning the expected melting range of the target protein (e.g., 40-65°C in 2-3°C increments).
- Include a no-heat control (4°C) and a full-denaturation control (95-99°C).
- Subject samples to heat challenge for 3-30 minutes (typically 3 minutes).
- Immediately cool samples to 4°C.
- Lyse cells using multiple freeze-thaw cycles (rapid freezing in liquid nitrogen followed by thawing at room temperature) or by adding lysis buffer with protease inhibitors.
- Centrifuge lysates at 15,000-20,000 × g for 20 minutes at 4°C to separate soluble protein from aggregates.
Protein Quantification and Analysis:
- Transfer soluble protein fraction to new tubes.
- Quantify protein concentration using BCA or Bradford assay.
- Prepare samples for Western blotting with equal protein loading.
- Perform standard Western blot protocol with target-specific antibodies.
- Include loading controls such as SOD1, β-actin, or GAPDH.
- Quantify band intensities using densitometry software.
- Plot percentage soluble protein versus temperature to generate melt curves.
- Calculate Tm values by fitting data to sigmoidal curve and determine ΔTm between treated and control samples.
Critical Optimization Parameters:
- Cell density and viability significantly impact results; maintain consistent cell numbers across replicates.
- Compound solubility and stability should be verified under assay conditions.
- Heating time must be optimized for each target protein; longer heating (30 minutes) may be required for some targets.
- Antibody specificity and sensitivity must be validated for the denatured protein states encountered after heating.
- Include appropriate controls: vehicle-only, known binder (positive control), and inactive analog (negative control) [41] [39] [42].
Research Reagent Solutions for CETSA Implementation
Successful implementation of CETSA requires specific reagents and tools optimized for thermal shift assays. The following table catalogues essential research solutions for establishing robust CETSA workflows:
Table 3: Essential Research Reagents and Solutions for CETSA
| Reagent Category | Specific Examples | Function in CETSA | Technical Considerations |
|---|---|---|---|
| Detection Antibodies | Target-specific validated antibodies | Quantification of soluble target protein after heating | Must recognize denatured epitopes; validate for CETSA specificity |
| Bead-Based Detection Kits | AlphaLISA, MSD, Lantha | High-throughput detection without gels | Enable 384-well format screening; require specific equipment |
| Mass Spectrometry Tags | TMT (Tandem Mass Tags), iTRAQ | Multiplexed protein quantification in MS-CETSA | Enable simultaneous analysis of multiple temperature points |
| Loading Control Proteins | SOD1, β-actin, GAPDH, HSC70 | Normalization of protein amounts | Select heat-stable proteins (SOD1 stable to 95°C) |
| Cell Lysis Reagents | NP-40, RIPA buffers, freeze-thaw cycles | Release of soluble protein fraction | Optimize to minimize target proteolysis; include protease inhibitors |
| Thermal Stable Assay Plates | PCR plates, 384-well plates | Withstand thermal cycling without deformation | Ensure good thermal conductivity for uniform heating |
| Protein Quantification Assays | BCA, Bradford | Measurement of soluble protein concentration | Compatible with detergents in lysis buffers |
| Crowding Agents | Ficoll, dextran, BSA | Mimic intracellular environment in lysate CETSA | Recreate cytoplasmic macromolecular crowding [44] |
CETSA Applications in Drug Discovery Workflows
CETSA has become integrated throughout modern drug discovery pipelines, from early target validation to clinical development. Its applications span multiple domains:
Target Identification and Validation: CETSA provides direct evidence that compounds engage with presumed molecular targets in physiologically relevant environments. For natural products with complex mechanisms, CETSA has been particularly valuable in identifying molecular targets that were previously obscure [41] [21]. For example, CETSA has helped elucidate protein targets for various natural products including ginsenosides, with one study identifying adenylate kinase 5 as a direct target in brain tissues [21].
Hit-to-Lead Optimization: In lead optimization campaigns, CETSA enables ranking of compound series based on cellular target engagement potency, providing critical structure-activity relationship data that complements biochemical potency measurements. The high-throughput CETSA formats allow rapid screening of analog series to select compounds with optimal cellular penetration and engagement [7] [46].
Off-Target Profiling: The MS-CETSA (TPP) format enables proteome-wide assessment of compound selectivity by monitoring thermal stability changes across thousands of proteins simultaneously. This application is crucial for identifying potential off-target liabilities early in development, potentially avoiding costly late-stage failures due to toxicity or side effects [42].
Mechanism of Action Studies: Beyond direct target engagement, CETSA can provide insights into downstream pathway effects and mechanism of action. By monitoring thermal stability changes in multiple proteins within a pathway, researchers can infer compound-induced biological effects and pathway modulation [42].
Physiological and Clinical Translation: CETSA has been successfully applied in complex biological systems including tissue samples, whole blood, and in vivo models. This capability bridges the gap between simplified cell culture models and physiological environments, providing critical translational data. For instance, researchers have applied CETSA to measure target engagement of RIPK1 and Akt inhibitors in human whole blood, demonstrating relevance to clinical settings [45].
The following diagram illustrates the integration of CETSA across the drug discovery continuum:
Technical Considerations and Troubleshooting
Implementing robust CETSA assays requires attention to several technical considerations and potential pitfalls:
Sample Matrix Selection: The choice between intact cells and cell lysates significantly impacts results. Intact cells preserve the native cellular environment, including membrane permeability, metabolism, and signaling context, but introduce compound uptake as a variable. Lysates provide direct access to intracellular targets but disrupt natural protein complexes and physiological conditions. For targets where the intracellular environment affects binding, intact cells are preferred, while lysates are suitable for initial binding assessments and troubleshooting [42].
Buffer Composition: For lysate-based CETSA, buffer composition critically influences protein stability and ligand binding. Standard phosphate-buffered saline (PBS) mimics extracellular conditions with high sodium (157 mM) and low potassium (4.5 mM), while intracellular conditions feature reversed ratios (~140-150 mM K+, ~14 mM Na+). Incorporating macromolecular crowding agents (e.g., Ficoll, dextran) and adjusting ion composition to match cytoplasmic conditions can improve physiological relevance [44].
Temperature Optimization: Inadequate temperature range selection is a common pitfall. Pilot experiments should establish the baseline Tm of the target protein to define appropriate temperature gradients for melt curves (typically Tm ± 10°C) and isothermal points for ITDR (typically near Tm). Proteins with very high or low inherent thermal stability may require extended temperature ranges [39].
Troubleshooting Poor Signal-to-Noise: Several factors can compromise CETSA data quality:
- Compound solubility: Precipitated compound can cause non-specific effects; include vehicle controls and monitor solubility.
- Antibody quality: Antibodies must recognize partially denatured protein; validate specifically for CETSA.
- Cell permeability: For intact cell CETSA without observed shifts, verify compound penetration using lysate CETSA.
- Protein aggregation: Some proteins aggregate independently of ligand binding; optimize lysis conditions to recover soluble protein.
- Loading controls: Use heat-stable proteins (SOD1, HSC70) rather than conventional housekeeping proteins that may denature [39] [42].
Complementary Assays: CETSA should be viewed as part of a comprehensive target engagement toolkit rather than a standalone solution. Techniques like DARTS, SPROX, and NanoBRET provide orthogonal validation through different biophysical principles. DARTS is particularly complementary as it detects ligand-induced protease resistance rather than thermal stabilization, making it suitable for targets that don't exhibit significant thermal shifts [40] [42].
CETSA has established itself as a cornerstone technology for measuring cellular target engagement in drug discovery. Its ability to directly quantify compound binding to endogenous targets in physiologically relevant environments addresses a critical gap between biochemical assays and functional cellular responses. The methodology continues to evolve with advancements in high-throughput automation, mass spectrometry sensitivity, and computational analysis, further expanding its applications across the drug development continuum [7] [46] [42].
While CETSA offers significant advantages through its label-free nature and physiological relevance, researchers should carefully consider its limitations and complementarity with other techniques. Proteins that don't exhibit thermal stabilization upon ligand binding, or that have inherently high thermal stability, may require alternative approaches like DARTS. Furthermore, the resource requirements for proteome-wide CETSA applications remain substantial, necessitating specialized expertise and instrumentation [41] [40].
As drug discovery increasingly focuses on complex targets and challenging therapeutic modalities, the integration of CETSA into orthogonal target engagement strategies provides a robust framework for validating compound mechanism of action. The ongoing development of standardized protocols, data analysis workflows, and quality control metrics will further solidify CETSA's role as an essential component of modern drug development pipelines [39] [46].
In the rigorous process of drug discovery and development, selecting the appropriate biological model is a foundational decision that significantly influences the predictive accuracy, cost, and timeline of research. Target validation—the process of establishing that a molecular target is directly involved in a disease and can be therapeutically modulated—requires models that faithfully recapitulate human biology. For decades, the scientific community has relied on a spectrum of tools, from traditional two-dimensional (2D) cell cultures to complex animal models. However, the limitations of these systems, including the poor translatability of 2D data and the species-specific differences of animal models, have driven the development of more sophisticated alternatives [47] [48].
Three-dimensional (3D) cell cultures have emerged as a powerful intermediary, bridging the gap between simple in vitro systems and whole-animal in vivo studies [49]. These models, which include spheroids, organoids, and organs-on-chips, allow cells to grow and interact in a three-dimensional space, more closely mimicking the tissue architecture, cell-cell interactions, and biochemical gradients found in living organs [48]. Concurrently, advanced animal models, particularly those refined through genetic engineering, have become more precise tools for studying complex systemic physiology and disease pathogenesis [50].
This guide provides an objective comparison of 3D cell cultures and animal models, focusing on their applications, performance, and limitations within target validation and drug development workflows. By presenting structured experimental data, detailed protocols, and key technical considerations, we aim to equip researchers with the information needed to select the optimal model system for their specific research objectives.
Comparative Analysis of Model Systems
The choice between a 3D cell culture and an animal model involves a multi-factorial decision-making process, balancing physiological relevance with practical experimental constraints. The table below summarizes the core characteristics of these systems to provide a foundational comparison.
Table 1: Core Characteristics of 3D Cell Cultures and Advanced Animal Models
| Feature | 3D Cell Cultures | Advanced Animal Models (e.g., GEAMs, Humanized) |
|---|---|---|
| Physiological Relevance | Recapitulates human tissue microarchitecture, cell-ECM interactions, and nutrient gradients [47] [49]. | Provides a whole-organism context with integrated systemic physiology (e.g., neuro-immune, circulatory systems) [50] [51]. |
| Species Specificity | Can be established from human cells, avoiding species-specific translation gaps [52] [53]. | Inherently non-human; humanized models attempt to bridge this gap by engrafting human cells or tissues [50]. |
| Genetic Control | Enables precise gene editing (e.g., CRISPR in organoids) and use of patient-derived cells for personalized medicine [49]. | Transgenic techniques (e.g., CRISPR, Cre-Lox) allow for sophisticated, tissue-specific disease modeling [50]. |
| Complexity & Integration | Models a single organ or tissue type; multi-organ interactions are limited but explored via microfluidic "body-on-a-chip" systems [49] [48]. | Naturally includes multi-organ crosstalk, systemic metabolism, and immune responses [51]. |
| Throughput & Cost | High-to-medium throughput; suitable for screening large compound libraries at a lower cost than animal studies [47] [54]. | Low throughput; associated with high costs for breeding, housing, and long-term maintenance [50] [51]. |
| Ethical Considerations | Aligns with the 3Rs principle (Replacement, Reduction, Refinement) by reducing reliance on animal testing [49] [51]. | Raises significant ethical concerns and is subject to strict regulatory oversight for animal welfare [51] [53]. |
Quantitative Performance Data in Key Applications
To move beyond theoretical advantages, it is crucial to examine quantitative performance data from preclinical applications. The following table compiles experimental findings from recent studies, highlighting how these models perform in critical areas like drug response and disease modeling.
Table 2: Experimental Performance Data in Preclinical Applications
| Application | 3D Culture Model & Findings | Animal Model & Findings |
|---|---|---|
| Drug Efficacy & Resistance | CRC spheroids show up to 100-fold increased resistance to chemotherapeutic agents (e.g., 5-FU) compared to 2D cultures, better mimicking clinical responses [47] [54]. | Humanized mouse models for cardiac implants showed a 30% increase in endothelialization rate, reducing thrombosis risk and predicting better implant integration [50]. |
| Tumor Biology | MCTSs naturally develop gradients of proliferation and cell death, with a hypoxic core that can be >60 μm in diameter, driving chemoresistance [47] [48]. | Patient-derived xenografts (PDX) in immunodeficient mice can incorporate the human tumor, stromal, and immune cell compartments for therapy screening [50]. |
| Toxicology & Safety | Liver organoids cultivated in clinostat bioreactors demonstrate highly reproducible and uniform responses to compound exposure, enabling robust toxicity screening [53]. | Smart implants with drug-delivery systems in genetically modified diabetic rodent models achieved 60% faster wound healing, showcasing predictive power for combined device-drug therapies [50]. |
| Implant Integration | Co-culture spheroid models of cancer-associated fibroblasts (CAFs) and tumor cells have been shown to significantly alter the transcriptional profile of cancer cells, modeling the tumor stroma [54]. | Immune-humanized mouse models demonstrate improved implant integration and longevity, with qualitative data showing decreased rejection and inflammatory responses [50]. |
Experimental Protocols for Key Methodologies
Reproducibility is paramount in preclinical research. This section provides detailed protocols for establishing a standard 3D model and generating a genetically engineered animal model, as commonly cited in the literature.
Protocol 1: Generating Multicellular Tumor Spheroids (MCTS) Using Ultra-Low Attachment Plates
This protocol, adapted from a 2025 study comparing 3D-culture techniques for colorectal cancer, is a widely used scaffold-free method for producing uniform spheroids [54].
1. Materials:
- Cell line of interest (e.g., HCT116, SW480 colorectal cancer cells).
- Standard cell culture medium with serum.
- Phosphate Buffered Saline (PBS).
- Trypsin-EDTA solution.
- Cell-repellent, U-bottom 96-well plates (commercially available) or standard plates coated with poly-HEMA.
- Centrifuge.
2. Method: 1. Cell Harvesting: Culture your chosen cell line in 2D until they reach 70-80% confluency. Wash the monolayer with PBS and detach the cells using Trypsin-EDTA. Inactivate the trypsin with complete medium. 2. Cell Suspension Preparation: Count the cells and prepare a single-cell suspension. Adjust the cell density to a concentration that will yield a spheroid of the desired size. A common starting point is 5,000 - 10,000 cells per spheroid in 100-200 µL of medium [47] [54]. 3. Seeding: Gently pipette the cell suspension into the wells of the U-bottom, cell-repellent plate. Avoid creating bubbles. 4. Centrifugation (Optional but Recommended): Centrifuge the plate at a low speed (e.g., 500 x g for 5 minutes). This step encourages cell aggregation at the bottom of the well, leading to more consistent spheroid formation [54]. 5. Incubation: Place the plate in a 37°C, 5% CO₂ incubator. Spheroids should form within 24-72 hours. 6. Maintenance: Monitor spheroid formation daily under a microscope. Change the medium carefully every 2-3 days by slowly removing 50-70% of the conditioned medium and adding fresh, pre-warmed medium without disrupting the spheroid.
3. Key Considerations:
- Optimization: The ideal cell number and medium composition may vary significantly between cell lines and must be optimized [54].
- Co-culture: To incorporate stromal components, simply mix the tumor cells with other cell types (e.g., fibroblasts) in the desired ratio during step 2 [54].
This protocol outlines the key steps for creating a knockout mouse model, one of the most common applications of CRISPR/Cas9 technology, based on techniques reviewed by [50].
1. Materials:
- Single-guide RNA (sgRNA) designed for the target mouse gene.
- Cas9 mRNA or protein.
- Fertilized mouse embryos (C57BL/6J is a common strain).
- Microinjection apparatus.
- Pseudopregnant female mice to serve as embryo recipients.
2. Method: 1. sgRNA Design: Design and synthesize sgRNAs with high on-target efficiency and minimal off-target effects for the gene of interest. 2. Microinjection Mixture: Prepare a mixture containing the sgRNA and Cas9 mRNA/protein in nuclease-free buffer. 3. Microinjection: Using a fine glass needle, microinject the CRISPR/Cas9 mixture into the pronucleus or cytoplasm of fertilized single-cell mouse embryos [50]. 4. Embryo Transfer: Surgically transfer the viable, injected embryos into the oviducts of pseudopregnant female mice. 5. Genotyping: After the pups are born (approximately 21 days), take tissue samples (e.g., tail clips) for DNA extraction. Screen the founders (F0 generation) for the desired mutation using PCR and DNA sequencing. 6. Breeding: Breed the founder mice with wild-type mice to assess germline transmission and establish a stable transgenic line.
3. Key Considerations:
- Complexity and Expertise: This is a highly complex procedure requiring specialized skills in molecular biology and animal surgery.
- Off-Target Effects: A key limitation of CRISPR/Cas9 is the potential for unintended genomic modifications, which must be carefully evaluated [50].
- Ethical Approval: All procedures must be reviewed and approved by an Institutional Animal Care and Use Committee (IACUC).
Workflow Visualization for Model Selection and Application
The following diagram illustrates a logical workflow for selecting and applying these model systems in a typical drug discovery pipeline, from initial screening to preclinical validation.
Diagram 1: A workflow for model system selection in drug discovery, highlighting the complementary roles of 3D cultures and animal models.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of advanced model systems relies on a suite of specialized reagents and tools. The table below details key solutions for working with 3D cell cultures and genetically engineered animal models.
Table 3: Key Research Reagent Solutions for Advanced Model Systems
| Item | Function/Application | Example Use-Case |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Polymer-coated surfaces that inhibit cell attachment, forcing cells to aggregate and form spheroids [47] [54]. | Generating uniform multicellular tumor spheroids (MCTS) for high-throughput drug screening. |
| Basement Membrane Matrix (e.g., Matrigel) | A natural, complex hydrogel derived from mouse tumors that provides a scaffold for 3D cell growth and differentiation [54]. | Culturing organoids to model glandular tissues like intestine, breast, or pancreas. |
| Magnetic 3D Bioprinting Systems | Use magnetic forces to levitate and assemble cells into 3D structures, simplifying the creation of co-cultures and complex tissues [52]. | Creating 3D co-culture models of the aortic valve for studying tissue development and disease. |
| CRISPR/Cas9 System | A genome-editing tool that uses a guide RNA and Cas9 nuclease to introduce targeted DNA double-strand breaks [50]. | Generating knockout or knock-in mutations in mouse embryos to create disease-specific animal models. |
| Cre-lox Recombinase System | A site-specific recombination technology that allows for precise, conditional gene deletion or activation in specific tissues or at certain times [50]. | Studying gene function in a particular cell type without causing embryonic lethality. |
| Microfluidic Organ-on-a-Chip Devices | Chip-based systems containing micro-channels lined with living cells that simulate organ-level physiology and dynamic mechanical forces [49] [48]. | Creating a "lung-on-a-chip" to model breathing motions and study drug absorption in the alveolar barrier. |
The landscape of preclinical model systems is evolving from a linear pathway to an integrated ecosystem where 3D cell cultures and advanced animal models are used complementarily. As the data and protocols in this guide illustrate, 3D cultures offer an unparalleled platform for human-specific, high-throughput mechanistic studies and screening, directly addressing the high attrition rates in early drug discovery [48]. Their ability to model the tumor microenvironment and predict drug resistance makes them indispensable for oncology target validation [47] [54].
Advanced animal models, particularly GEAMs and humanized systems, remain irreplaceable for assessing systemic efficacy, complex immune responses, and overall in vivo biocompatibility [50]. They provide the physiological context necessary for lead candidate selection and regulatory approval.
The future lies in leveraging the strengths of each system in a staggered, complementary strategy. Initial high-throughput screening and mechanistic dissection can be performed in sophisticated 3D human models, filtering out ineffective compounds early. The most promising candidates can then advance to sophisticated, targeted animal studies for final preclinical validation. This integrated approach, supported by regulatory shifts toward human-relevant methods [53], promises to enhance the predictive power of preclinical research, accelerate the development of new therapies, and responsibly implement the 3Rs principles in biomedical science.
Biomarker Identification and Validation for Tracking Target Modulation
In the modern paradigm of precision medicine, biomarkers have become indispensable tools, defined as "objectively measurable indicators of biological processes" [55]. They provide crucial insights into disease mechanisms, drug-target interactions, and treatment responses, thereby enabling more informed decision-making throughout the drug development pipeline. The validation of biomarkers for tracking target modulation—the measurement of a drug's effect on its intended biological target—represents a particularly critical application. This process confirms that a therapeutic agent is engaging its target and modulating the intended biological pathway, thereby establishing a chain of mechanistic evidence from target engagement to clinical effect [56] [57].
The validation landscape is evolving rapidly, with regulatory agencies including the U.S. Food and Drug Administration (FDA) providing updated guidance in 2025 that recognizes the fundamental differences between biomarker assays and traditional pharmacokinetic assays [58]. This guidance emphasizes a "fit-for-purpose" approach, where the extent of validation is tailored to the biomarker's specific Context of Use (COU) in drug development [58]. The COU encompasses both the biomarker category and its proposed application, which can range from understanding mechanisms of action and signs of clinical activity to supporting decisions on patient selection, drug safety, pharmacodynamic effects, or efficacy [58].
Despite their critical importance, the path to successful biomarker validation remains challenging. Current estimates indicate that approximately 95% of biomarker candidates fail to progress from discovery to clinical use, primarily during the validation phase [59]. This high attrition rate underscores the necessity for robust validation strategies, advanced technological platforms, and rigorous statistical approaches. This guide provides a comprehensive comparison of current methodologies, experimental protocols, and technological platforms for biomarker identification and validation, with a specific focus on applications in tracking target modulation.
Biomarker Categories and Context of Use
Biomarkers for tracking target modulation fall into several distinct categories, each with specific validation requirements and performance considerations. Understanding these categories is essential for selecting appropriate validation strategies and analytical platforms.
Table 1: Biomarker Categories in Target Modulation
| Category | Primary Function | Validation Focus | Common Technologies |
|---|---|---|---|
| Target Engagement Biomarkers | Directly measure drug binding to the intended target | Specificity, sensitivity, dynamic range | LC-MS/MS, ELISA, MSD, SPR |
| Pharmacodynamic Biomarkers | Measure downstream effects of target modulation | Relationship to target modulation, variability | Multiplex immunoassays, transcriptomics, proteomics |
| Mechanistic Biomarkers | Provide insights into biological pathways affected | Biological plausibility, pathway mapping | Multi-omics approaches, single-cell analysis |
| Predictive Biomarkers | Identify patients likely to respond to treatment | Diagnostic accuracy, clinical utility | Genomic sequencing, IHC, flow cytometry |
| Safety Biomarkers | Detect early signs of target-related toxicity | Specificity for adverse events, predictive value | Clinical chemistry, metabolomics |
The FDA's 2025 guidance on Bioanalytical Method Validation for Biomarkers (BMVB) explicitly recognizes that biomarker assays differ fundamentally from pharmacokinetic assays, necessitating distinct validation approaches [58]. Unlike pharmacokinetic assays that measure drug concentrations using fully characterized reference standards, biomarker assays frequently lack reference materials identical to the endogenous analyte [58]. This distinction necessitates alternative validation approaches, particularly for protein biomarkers where recombinant proteins used as calibrators may differ from endogenous biomarkers in critical characteristics such as molecular structure, folding, truncation, and glycosylation patterns [58].
The concept of "fit-for-purpose" validation is central to modern biomarker development [58]. This approach tailors the validation strategy to the specific context of use, acknowledging that biomarkers intended for internal decision-making may require different validation stringency compared to those supporting regulatory approval or clinical decision-making. For biomarkers tracking target modulation, key validation parameters typically include demonstration of specificity for the intended target, appropriate sensitivity to detect physiologically relevant modulation, and a dynamic range encompassing both baseline and modulated states [58] [59].
Technology Platform Comparison
Selecting appropriate analytical technologies is crucial for successful biomarker validation. The choice of platform depends on multiple factors including the biomarker's chemical nature, required sensitivity, sample volume, and throughput requirements.
Table 2: Analytical Platform Comparison for Biomarker Validation
| Platform | Sensitivity | Dynamic Range | Multiplexing Capability | Sample Throughput | Relative Cost per Sample | Best Suited Applications |
|---|---|---|---|---|---|---|
| ELISA | Moderate (pg/mL) | 1-2 logs | Low (single-plex) | Moderate | $$ (e.g., $61.53 for 4 biomarkers) | High-abundance proteins, established targets |
| Meso Scale Discovery (MSD) | High (fg-pg/mL) | 3-4 logs | High (10-100 plex) | High | $ (e.g., $19.20 for 4 biomarkers) | Cytokines, signaling phosphoproteins, low abundance targets |
| LC-MS/MS | High (fg-pg/mL) | 3-4 logs | Moderate (10-100s) | Moderate | $$$ | Metabolites, modified proteins, precise quantification |
| Next-Generation Sequencing | Variable | N/A | High (1000s) | Moderate-High | $$$ | Genetic biomarkers, expression signatures, splice variants |
| Single-Cell Analysis | Single cell | N/A | High (10-100s) | Low | $$$$ | Tumor heterogeneity, rare cell populations, cellular mechanisms |
Advanced technologies like MSD and LC-MS/MS offer significant advantages over traditional ELISA methods. MSD utilizes electrochemiluminescence detection, providing up to 100 times greater sensitivity than traditional ELISA and a broader dynamic range [60]. The U-PLEX multiplexed immunoassay platform from MSD allows researchers to design custom biomarker panels and measure multiple analytes simultaneously within a single sample, significantly enhancing efficiency while reducing costs [60]. For example, measuring four inflammatory biomarkers (IL-1β, IL-6, TNF-α, and IFN-γ) using individual ELISAs costs approximately $61.53 per sample, while MSD's multiplex assay reduces the cost to $19.20 per sample—a saving of $42.33 per sample [60].
LC-MS/MS platforms offer complementary advantages, particularly for novel biomarkers without established immunoassays or for applications requiring absolute quantification. Modern LC-MS/MS systems can identify and quantify over 10,000 proteins in a single run, providing unprecedented coverage of the proteome [60]. This comprehensive approach is particularly valuable for discovering novel biomarkers of target modulation without prior hypothesis about specific proteins involved.
The integration of artificial intelligence and machine learning with these analytical platforms is further transforming biomarker validation. AI-driven algorithms can process complex datasets to identify subtle patterns that might escape conventional analysis, enabling more sophisticated predictive models of target modulation [61]. By 2025, enhanced integration of AI and machine learning is expected to revolutionize data processing and analysis, leading to improved predictive analytics, automated data interpretation, and personalized treatment plans based on biomarker profiles [61].
Experimental Protocols for Biomarker Validation
Fit-for-Purpose Validation Framework
The 2025 FDA BMVB guidance emphasizes a fit-for-purpose approach to biomarker validation, which should be scientifically driven and aimed at producing robust, reproducible data to support the biomarker's specific context of use [58]. The following experimental protocols provide detailed methodologies for key validation experiments.
Parallelism Assessment Protocol
Purpose: To demonstrate similarity between the endogenous analyte and reference standards by evaluating serial dilutions of sample matrix [58].
Materials:
- Minimum 6 individual subject samples containing endogenous analyte
- Reference standard in authentic matrix
- Minimum 5 concentrations spanning the assay range
- Assay reagents and buffers as optimized during development
Procedure:
- Prepare serial dilutions (e.g., 1:2, 1:4, 1:8, 1:16) of at least 6 individual subject samples using the appropriate assay buffer or authentic matrix.
- Prepare identical dilutions of the reference standard in authentic matrix.
- Analyze all dilutions in the same assay run.
- Plot observed concentration versus dilution factor for each sample.
- Calculate percent parallelism as (observed concentration/expected concentration) × 100 for each dilution.
Acceptance Criteria: Parallelism should be 80-120% for all dilutions, with dose-response curves of study samples parallel to the reference standard curve [58].
Stability Assessment Protocol for Endogenous Analytes
Purpose: To evaluate stability of the endogenous biomarker under conditions mimicking sample collection, storage, and processing.
Materials:
- Freshly collected patient samples (minimum n=6)
- Appropriate collection tubes and storage containers
- Conditions to be tested: freeze-thaw cycles, benchtop stability, long-term frozen storage
Procedure:
- Aliquot freshly collected samples for each stability condition to be tested.
- For freeze-thaw stability: Subject aliquots to 3 cycles of freezing at -70°C and thawing at room temperature. Analyze alongside fresh controls.
- For benchtop stability: Maintain aliquots at room temperature for 4-24 hours (depending on expected handling conditions). Analyze at predetermined timepoints.
- For long-term stability: Store aliquots at recommended storage temperature (-70°C or -80°C). Analyze at predetermined intervals (1, 3, 6, 12 months).
Acceptance Criteria: Mean concentration should be within 80-120% of fresh controls with precision ≤20% CV [58].
Precision and Accuracy Profile Protocol
Purpose: To characterize assay performance across the analytical measurement range using quality control samples prepared in authentic matrix.
Materials:
- Quality control samples at low, medium, and high concentrations (minimum n=5 each)
- Calibration standards
- Assay reagents as optimized
Procedure:
- Prepare quality control samples using the same matrix as study samples at concentrations spanning the measurement range.
- Analyze QC samples in replicates (minimum n=5) across multiple runs (minimum 3 runs) by multiple analysts if possible.
- Calculate intra-assay (within-run) and inter-assay (between-run) precision as coefficient of variation (%CV).
- Calculate accuracy as percent deviation from nominal concentration.
Acceptance Criteria: Total precision ≤20% CV, accuracy 80-120% of nominal concentration [59].
Signaling Pathways and Experimental Workflows
The validation of biomarkers for target modulation requires understanding of the biological pathways involved and systematic workflows for assay development. The following diagrams illustrate key relationships and processes.
Biomarker Validation Decision Pathway
Target Modulation Signaling Pathway
The Scientist's Toolkit: Research Reagent Solutions
Successful biomarker validation requires carefully selected reagents and materials. The following table details essential research reagent solutions for biomarker validation studies.
Table 3: Essential Research Reagents for Biomarker Validation
| Reagent Type | Function | Key Considerations | Representative Examples |
|---|---|---|---|
| Reference Standards | Serve as calibration material for quantitative assays | Purity, characterization, similarity to endogenous analyte | Recombinant proteins, synthetic peptides, certified reference materials |
| Capture and Detection Antibodies | Enable specific recognition and quantification of biomarkers | Specificity, affinity, lot-to-lot consistency, cross-reactivity profiling | Monoclonal antibodies, polyclonal antibodies, validated pairs |
| Assay Diluents and Matrix | Provide appropriate environment for antigen-antibody interaction | Matrix matching, interference mitigation, signal-to-noise optimization | Biological matrix (plasma, serum), artificial matrix, proprietary diluents |
| Quality Control Materials | Monitor assay performance over time | Commutability with patient samples, stability, concentration assignment | Pooled patient samples, commercial QC materials, spiked samples |
| Signal Detection Reagents | Generate measurable signal proportional to analyte concentration | Sensitivity, dynamic range, compatibility with instrumentation | Enzymes, electrochemiluminescent labels, fluorescent dyes, substrates |
| Solid Surfaces | Provide platform for immobilization of capture reagents | Binding capacity, uniformity, low non-specific binding | Microplates, beads, chips, membranes |
| Sample Collection Materials | Maintain biomarker integrity during collection and storage | Tube additives, stability during processing, compatibility | EDTA tubes, PAXgene tubes, specialized collection devices |
A critical challenge in biomarker validation is that reference materials may differ from endogenous analytes in critical characteristics such as molecular structure, folding, truncation, glycosylation patterns, and other post-translational modifications [58]. This fundamental difference necessitates thorough parallelism assessments to demonstrate similarity between the reference standard and endogenous biomarker [58]. For biomarkers measured using ligand binding or hybrid LBA-mass spectrometry-based assays, parallelism assessment is particularly critical to establish this similarity [58].
The emergence of multi-omics approaches represents a significant trend in biomarker development, with researchers increasingly leveraging data from genomics, proteomics, metabolomics, and transcriptomics to achieve a holistic understanding of disease mechanisms [61]. Multi-omics approaches enable the identification of comprehensive biomarker signatures that reflect disease complexity, facilitating improved diagnostic accuracy and treatment personalization [61]. The integration of single-cell analysis technologies with multi-omics data provides an even more comprehensive view of cellular mechanisms, paving the way for novel biomarker discovery [61].
Regulatory Considerations and Future Trends
The regulatory landscape for biomarker validation continues to evolve, with the FDA's 2025 BMVB guidance providing specific direction for biomarker assays distinct from pharmacokinetic assays [58]. A key recommendation from this guidance is that sponsors should "include justifications for these differences in their method validation reports" when biomarker validation approaches differ from traditional pharmacokinetic validation frameworks [58].
The guidance also clarifies terminology, recommending use of "validation" rather than "qualification" for biomarker assays to prevent confusion with the regulatory term "biomarker qualification" used when a biomarker is formally qualified for specific clinical applications irrespective of the particular drug under development [58]. This distinction is important for maintaining regulatory clarity.
Future trends in biomarker validation point toward increased integration of artificial intelligence and machine learning, with AI-driven algorithms expected to enhance predictive analytics, automate data interpretation, and facilitate personalized treatment plans [61]. Liquid biopsy technologies are also poised to become standard tools, with advances in circulating tumor DNA (ctDNA) analysis and exosome profiling increasing sensitivity and specificity for non-invasive disease monitoring [61]. These technologies facilitate real-time monitoring of disease progression and treatment responses, allowing for timely adjustments in therapeutic strategies [61].
The rise of patient-centric approaches will also influence biomarker validation, with increased emphasis on informed consent and data sharing, incorporation of patient-reported outcomes, and engagement of diverse patient populations to ensure that new biomarkers are relevant across different demographics [61]. These trends reflect the ongoing evolution of biomarker validation from a purely technical exercise to an integrated process encompassing analytical performance, clinical utility, and patient perspective.
Biomarker identification and validation for tracking target modulation represents a critical capability in modern drug development. The evolving regulatory landscape, exemplified by the FDA's 2025 BMVB guidance, emphasizes fit-for-purpose approaches that recognize the fundamental differences between biomarker assays and traditional pharmacokinetic methods. Successful validation requires careful consideration of context of use, appropriate selection of analytical platforms, and rigorous assessment of key validation parameters including parallelism, precision, accuracy, and stability.
Advanced technologies including MSD, LC-MS/MS, and multi-omics platforms offer significant advantages over traditional methods in terms of sensitivity, multiplexing capability, and cost efficiency. The integration of artificial intelligence and machine learning further enhances biomarker discovery and validation, enabling identification of complex patterns and relationships that would be difficult to detect through conventional approaches. As the field continues to evolve, biomarkers for target modulation will play an increasingly important role in bridging the gap between drug discovery and clinical application, ultimately enabling more effective and personalized therapeutic interventions.
The Rise of AI and In Silico Tools for Predictive Validation
Target validation is a critical, early-stage process in drug discovery that determines whether a specific biological molecule (a "target") is genuinely involved in a disease and can be modulated by a drug to produce a therapeutic effect. The failure to select a valid target is a primary reason for the high attrition rates in clinical development, with nearly 90% of candidates failing in trials, often due to poor target selection [62]. Traditional validation relies heavily on in vitro (test tube) and in vivo (living organism) experimental assays. While these methods provide direct biological evidence, they are often low-throughput, costly, and time-consuming, creating a bottleneck in the research pipeline [63] [64].
The rise of artificial intelligence (AI) and sophisticated in silico (computer-simulated) tools has introduced a paradigm shift. These computational approaches leverage machine learning, multi-omics data integration, and complex simulations to predict target validity with unprecedented speed and scale. In silico models have evolved from static simulations to dynamic, AI-powered frameworks that can integrate genomics, transcriptomics, proteomics, and clinical data for a more holistic understanding of target biology [65]. This guide provides an objective comparison of leading AI-driven in silico platforms, evaluating their performance against traditional methods and each other, based on current experimental data and standardized benchmarking.
Comparative Performance of AI and Traditional Models
The predictive performance of AI models is increasingly being benchmarked against established methods, such as population pharmacokinetic (PK) models and in vitro assays. The following tables summarize key quantitative comparisons from recent studies.
Table 1: Comparison of AI vs. Population PK Models in Predicting Antiepileptic Drug Concentrations [66]
| Model Type | Specific Model | Drug | Performance (Root Mean Squared Error - μg/mL) |
|---|---|---|---|
| Best-Performing AI Models | Adaboost, XGBoost, Random Forest | Carbamazepine (CBZ) | 2.71 |
| Phenobarbital (PHB) | 27.45 | ||
| Phenytoin (PHE) | 4.15 | ||
| Valproic Acid (VPA) | 13.68 | ||
| Traditional Population PK Models | Various Published Models | Carbamazepine (CBZ) | 3.09 |
| Phenobarbital (PHB) | 26.04 | ||
| Phenytoin (PHE) | 16.12 | ||
| Valproic Acid (VPA) | 25.02 |
This study demonstrated that ensemble AI models generally outperformed traditional population PK models in predicting drug concentrations, particularly for phenytoin and valproic acid. The authors noted that AI models can quickly learn complex patterns from high-dimensional clinical data without relying on pre-defined mathematical assumptions [66].
Table 2: Benchmarking of AI Target Identification Platforms (TargetBench 1.0) [62]
| Platform / Model | Clinical Target Retrieval Rate | Novel Targets with 3D Structure | Novel Targets Classified as Druggable |
|---|---|---|---|
| Insilico Medicine (TargetPro) | 71.6% | 95.7% | 86.5% |
| Large Language Models (e.g., GPT-4o, Claude Opus) | 15% - 40% | 60% - 91% | 39% - 70% |
| Public Platforms (e.g., Open Targets) | ~20% | Information Not Available | Information Not Available |
This head-to-head benchmarking, using Insilico's TargetBench 1.0 framework, shows that disease-specific AI models like TargetPro significantly outperform general-purpose large language models and public platforms in retrieving known clinical targets and nominating novel, druggable candidates with high translational potential [62].
Table 3: Comparison of In Silico Predictions vs. In Vitro Enzymatic Assays for GALT Gene Variants [67]
| GALT Variant | In Vitro Enzymatic Activity (Vmax vs. Native) | In Silico Prediction (Molecular Dynamics RMSD) | Consistency Between Methods? |
|---|---|---|---|
| Alanine81Threonine (A81T) | 51.66% | Not Significant | No |
| Histidine47Aspartate (H47D) | 26.36% | Not Significant | No |
| Glutamate58Lysine (E58K) | 3.38% | Not Significant | No |
| Glutamine188Arginine (Q188R - Pathogenic Control) | Minimal Activity | Not Significant | No |
This comparative study highlights a critical limitation of some in silico tools. While the in vitro assays showed a statistically significant decrease in enzymatic activity for all variants, the in silico molecular dynamics simulations and predictive programs (PredictSNP, EVE, SIFT) yielded mixed results and were not consistent with the experimental enzyme activity, suggesting they may not be reliable for determining the pathogenicity of all gene variants [67].
Experimental Protocols for AI Model Validation
To ensure the reliability and objectivity of AI model comparisons, rigorous and standardized experimental protocols are essential. Below are detailed methodologies for two key types of validation studies cited in this guide.
Protocol 1: Benchmarking AI Target Identification Models
This protocol is based on the methodology used to develop and validate Insilico Medicine's TargetPro and TargetBench 1.0 [62].
- Objective: To compare the performance of different AI models and platforms in identifying known clinical targets and novel, druggable candidates.
- Data Curation:
- Data Sources: Compile multi-modal data from 22 sources, including genomics (e.g., TCGA), transcriptomics, proteomics, pathway databases, clinical trial records (e.g., ClinicalTrials.gov), and scientific literature.
- Gold Standard Dataset: Create a benchmark set of known clinical-stage targets across a range of diseases (e.g., 38 diseases spanning oncology, neurology, immunology).
- Model Training & Testing:
- Disease-Specific Modeling: Train individual machine learning models (e.g., TargetPro) for each disease area rather than using a single general model.
- Feature Importance Analysis: Use explainable AI (XAI) techniques, such as SHAP analysis, to interpret model decisions and identify the most predictive data types for each disease.
- Performance Metrics:
- Clinical Target Retrieval Rate: The percentage of known clinical targets successfully identified by the model from the gold standard dataset.
- Druggability: The percentage of novel predicted targets that are classified as druggable based on established criteria (e.g., presence of binding pockets, similarity to known drug targets).
- Structural Availability: The percentage of novel predicted targets with resolved 3D protein structures in databases (e.g., PDB).
- Comparison: Execute the same benchmark against competing models, including large language models (LLMs) like GPT-4o and public platforms like Open Targets, using the same dataset and metrics.
Protocol 2: Comparing AI and PK Models for Drug Concentration Prediction
This protocol is derived from the study comparing AI and population PK models for antiepileptic drugs [66].
- Objective: To compare the predictive accuracy of AI models and established population pharmacokinetic (PK) models for forecasting drug concentrations in patients.
- Data Source:
- Therapeutic Drug Monitoring (TDM): Extract concentration data for specific drugs (e.g., carbamazepine, valproic acid) from hospital TDM records, along with patient demographics, dosage regimens, and time of last dose.
- Electronic Medical Records (EMR): Integrate additional patient-specific variables from EMRs, including laboratory results (e.g., creatinine, liver enzymes) and comorbidities.
- Data Preprocessing:
- Handling Missing Data: Impute missing continuous variables using methods like Multivariate Imputation by Chained Equations (MICE).
- Feature Scaling: Scale continuous variables using appropriate techniques like MinMaxScaler.
- Model Development and Validation:
- AI Models: Develop a suite of AI models, including ensemble methods (e.g., Random Forest, XGBoost) and neural networks. The dataset is randomly split into training, validation, and test sets (e.g., 60:20:20). Hyperparameters are tuned to minimize overfitting on the validation set.
- Population PK Models: Select relevant, previously published population PK models for the drugs in question.
- Performance Evaluation:
- Metric: Calculate the Root Mean Squared Error (RMSE) of the predicted concentrations versus the actual measured concentrations in the test dataset for both AI and PK models.
- Comparison: Statistically compare the RMSE values to determine if the performance of the AI models is superior to that of the traditional PK models.
Workflow Visualization of AI-Driven Target Validation
The following diagram illustrates a generalized, integrated workflow for AI-driven target validation, synthesizing elements from the leading platforms discussed.
(AI-Driven Target Validation Workflow)
This workflow highlights the closed-loop, iterative nature of modern AI-driven discovery. It begins with the integration of vast, multi-modal datasets, which are processed by disease-specific AI models. The use of explainable AI (XAI) techniques, such as SHAP analysis, makes the model's decision-making transparent, revealing which biological features were most important for target nomination—a critical step for gaining researcher trust [65] [62]. The top-priority targets are then forwarded for experimental validation using in vitro and in vivo models. Crucially, the results from these wet-lab experiments are fed back into the AI system to refine and improve its predictive accuracy continuously [65].
The Scientist's Toolkit: Essential Research Reagents and Platforms
For researchers embarking on AI-enhanced target validation, the following table details key computational platforms, data resources, and experimental tools referenced in this guide.
Table 4: Essential Resources for AI-Enhanced Predictive Validation
| Tool / Resource Name | Type | Primary Function in Validation | Example Use Case |
|---|---|---|---|
| TargetPro (Insilico Medicine) [62] | AI Software Platform | Disease-specific target identification and prioritization. | Nominating novel, druggable targets with high clinical potential for specific diseases like fibrosis or oncology. |
| Exscientia AI Platform [68] | AI Software Platform | Generative AI for de novo molecular design and optimization. | Designing novel small-molecule drug candidates with optimized properties against a validated target. |
| Pharma.AI (Insilico) [62] | AI Software Platform | End-to-end drug discovery suite spanning biology and chemistry. | Accelerating the entire pipeline from target identification to preclinical candidate nomination. |
| TargetBench 1.0 [62] | Benchmarking Framework | Standardized evaluation of target identification models. | Objectively comparing the performance of different AI platforms and LLMs for target discovery tasks. |
| Patient-Derived Xenografts (PDXs) & Organoids [65] | Biological Model | Preclinical in vivo and complex in vitro validation. | Testing the efficacy of a drug candidate against a specific target in a model that closely mimics human disease biology. |
| Molecular Dynamics Simulations (e.g., YASARA) [67] | Computational Modeling | Simulating the physical movements of atoms and molecules over time. | Predicting the structural impact of a genetic variant on a protein's function and stability. |
| PredictSNP / EVE / SIFT [67] | Predictive Bioinformatics Tool | Predicting the pathogenicity of genetic variants. | An initial, computational assessment of whether a newly discovered gene variant is likely to cause disease. |
| Electronic Medical Records (EMRs) [66] | Data Resource | Source of real-world patient data for model training and validation. | Training AI models to predict real-world drug concentrations and responses based on patient clinical profiles. |
The integration of AI and in silico tools into the target validation process represents a fundamental advancement in drug discovery. Objective comparisons show that these platforms can significantly accelerate early-stage research, with some companies reporting the nomination of developmental candidates in 12-18 months, a fraction of the traditional timeline [62]. Furthermore, specialized AI models like TargetPro demonstrate a 2-3x improvement in retrieving known clinical targets over general-purpose LLMs, establishing a new benchmark for accuracy [62].
However, the rise of computational tools does not render traditional experimental methods obsolete. As the comparison of in silico and in vitro assessments for GALT variants revealed, computational predictions can sometimes diverge from experimental results, underscoring the critical need for experimental validation [67]. The most robust and reliable approach is a hybrid one, where AI is used to rapidly generate high-quality, data-driven hypotheses that are then rigorously tested and refined through established experimental protocols. This synergistic workflow, combining the speed of silicon with the validation of the lab, holds the greatest promise for de-risking drug development and delivering new therapies to patients more efficiently.
Overcoming Common Pitfalls and Optimizing Your Validation Strategy
The reproducibility of experimental results is a cornerstone of scientific progress, yet functional genomics faces a significant challenge: off-target effects in gene modulation technologies. RNA interference (RNAi) and CRISPR-Cas9 have revolutionized biological research and therapeutic development by enabling precise manipulation of gene expression. However, their propensity for off-target activity—unintended modification of non-target genes—represents a critical source of experimental variability and misinterpretation. Off-target effects compromise data integrity, lead to erroneous conclusions about gene function, and ultimately contribute to the reproducibility crisis in life sciences. Understanding the distinct mechanisms, frequencies, and mitigation strategies for these artifacts in RNAi versus CRISPR is therefore essential for rigorous experimental design and valid biological interpretation. This guide provides a comparative analysis of off-target effects across these platforms, offering researchers a framework for selecting appropriate tools and implementing best practices to enhance the reliability of their findings.
Molecular Mechanisms: How RNAi and CRISPR Introduce Off-Target Effects
The fundamental differences in how RNAi and CRISPR operate at the molecular level explain their distinct off-target profiles. RNAi functions at the post-transcriptional level, mediating mRNA degradation or translational inhibition, while CRISPR acts directly at the DNA level, creating double-strand breaks. These different starting points dictate their unique pathways for unintended effects.
RNAi Off-Target Mechanisms
RNAi silences gene expression through the introduction of double-stranded RNA (dsRNA), which is processed by the RNase III enzyme Dicer into small interfering RNAs (siRNAs) of approximately 21-24 nucleotides. These siRNAs load into the RNA-induced silencing complex (RISC), which uses the siRNA's guide strand to identify complementary mRNA targets for cleavage by Argonaute proteins [27] [69]. Off-target effects occur through two primary mechanisms:
- Sequence-dependent off-targeting: siRNAs can tolerate mismatches, particularly in the seed region (nucleotides 2-8), leading to silencing of mRNAs with partial complementarity. Even minimal homology of 7-8 nucleotides can trigger unintended mRNA degradation [27].
- Sequence-independent off-targeting: siRNAs can activate innate immune responses, such as the interferon pathway, leading to global changes in gene expression that are unrelated to the intended target [27].
CRISPR Off-Target Mechanisms
CRISPR-Cas9 genome editing employs a Cas nuclease complexed with a guide RNA (gRNA) that directs it to complementary DNA sequences. Upon binding to target DNA, Cas9 creates double-strand breaks that are repaired by non-homologous end joining (NHEJ) or homology-directed repair (HDR) [27]. Off-target effects primarily arise from:
- Non-canonical PAM recognition: Cas9 may bind to DNA sequences with similar but not identical protospacer adjacent motifs (PAMs).
- Seed region mismatches: Similar to RNAi, the seed region of the gRNA (typically nucleotides 3-10 proximal to the PAM) is critical for target recognition, but mismatches outside this region can still permit cleavage.
- DNA/RNA bulges: Structural deformations in the DNA-RNA heteroduplex can lead to recognition of sequences with insertions or deletions relative to the gRNA [70].
Figure 1: Molecular pathways leading to off-target effects in RNAi and CRISPR technologies. RNAi off-targets primarily occur through seed region mismatches and immune activation, while CRISPR off-targets result from flexible PAM recognition and DNA-RNA heteroduplex tolerance.
Comparative Analysis: RNAi vs. CRISPR Off-Target Profiles
Direct comparison of RNAi and CRISPR reveals significant differences in their off-target propensities and characteristics. Understanding these distinctions enables researchers to select the most appropriate technology for their specific application and implement appropriate controls.
Table 1: Comparative Analysis of Off-Target Effects in RNAi vs. CRISPR
| Parameter | RNAi | CRISPR-Cas9 |
|---|---|---|
| Primary Mechanism | mRNA degradation/translational inhibition | DNA double-strand breaks |
| Typical Off-Target Rate | High (varies by design and concentration) | Lower (significantly improved with optimized systems) |
| Nature of Off-Target Effects | Sequence-dependent (partial complementarity) and sequence-independent (immune activation) | Primarily sequence-dependent (PAM flexibility, gRNA mismatches) |
| Persistence of Effects | Transient (knockdown) | Permanent (knockout) |
| Key Determinants | siRNA seed region complementarity, concentration | gRNA specificity, PAM recognition, delivery format |
| Primary Detection Methods | Transcriptomics (RNA-seq), qRT-PCR | Whole-genome sequencing, GUIDE-seq, CIRCLE-seq |
| Optimization Strategies | Chemical modifications, pooled siRNAs, bioinformatic design | High-fidelity Cas variants, optimized gRNA design, RNP delivery |
Recent comparative studies indicate that CRISPR exhibits significantly fewer off-target effects than RNAi when using state-of-the-art design tools and delivery methods [27]. The development of ribonucleoprotein (RNP) delivery formats with chemically modified sgRNAs has substantially reduced CRISPR off-target effects compared to earlier plasmid-based systems [27]. Nevertheless, RNAi maintains utility for applications requiring transient suppression or when targeting essential genes where complete knockout would be lethal.
Experimental Protocols for Off-Target Assessment
Robust experimental design includes systematic assessment of off-target activity. Below are detailed protocols for evaluating off-target effects in both RNAi and CRISPR systems.
RNAi Off-Target Validation Protocol
This protocol outlines a comprehensive approach for identifying RNAi off-target effects using transcriptomic analysis:
- Treatment Conditions: Transferd cells with target-specific siRNA and non-targeting control siRNA in biological triplicate.
- RNA Extraction: 48 hours post-transfection, extract total RNA using TRIzol reagent and quantify with spectrophotometry.
- Library Preparation and Sequencing: Prepare stranded mRNA-seq libraries using Illumina TruSeq kit and sequence on Illumina platform (minimum 30 million reads/sample).
- Bioinformatic Analysis:
- Align reads to reference genome using STAR aligner.
- Perform differential expression analysis with DESeq2.
- Identify significantly dysregulated genes (FDR < 0.05, fold change > 2).
- Conduct pathway enrichment analysis using GO and KEGG databases.
- Experimental Validation: Confirm key off-target hits using qRT-PCR with SYBR Green chemistry.
CRISPR Off-Target Validation Protocol
This protocol utilizes next-generation sequencing-based methods to comprehensively identify CRISPR off-target sites:
- In Silico Prediction: Predict potential off-target sites using Cas-OFFinder tool allowing up to 5 mismatches.
- GUIDE-seq Library Preparation:
- Electroporate cells with Cas9-gRNA RNP complex plus GUIDE-seq oligo.
- Culture cells for 72 hours followed by genomic DNA extraction.
- Library Preparation and Sequencing:
- Fragment genomic DNA to 400bp using ultrasonication.
- Prepare sequencing libraries with GUIDE-seq adaptors.
- Amplify integration sites and sequence on Illumina MiSeq.
- Bioinformatic Analysis:
- Process reads using GUIDE-seq computational pipeline.
- Identify significant off-target sites (read count > 10, present in replicates).
- Annotate sites with genomic features using HOMER.
- Validation: Confirm top off-target sites by amplicon sequencing.
Current Research and Screening Applications
Both RNAi and CRISPR technologies have been extensively employed in large-scale genetic screens to identify novel therapeutic targets, with CRISPR increasingly becoming the preferred method due to its superior specificity.
Table 2: Comparison of RNAi and CRISPR in High-Throughput Screening Applications
| Application | RNAi Screening | CRISPR Screening |
|---|---|---|
| Typical Format | Arrayed or pooled siRNA/shRNA libraries | Pooled sgRNA libraries with NGS readout |
| Library Size | ~5-10 siRNAs per gene | ~3-10 sgRNAs per gene |
| Screen Duration | 5-7 days (transient) or stable lines | 10-21 days (selection based) |
| Hit Validation | Required (high false positives) | More reliable (lower false positives) |
| Key Advantages | Established protocols, dose titration possible | Higher specificity, permanent knockout |
| Key Limitations | High false positive/negative rates, incomplete knockdown | Clone-to-clone variability, essential gene lethality |
CRISPR screening has demonstrated particular utility in target identification and validation for drug discovery, with applications spanning oncology, infectious diseases, and metabolic disorders [71]. For example, genome-wide CRISPR screens have identified novel therapeutic targets such as SETDB1 in uveal melanoma and HDAC3 in small cell lung cancer [72] [73]. The technology has also been integrated with organoid models to enable more physiologically relevant screening in complex tissue contexts [71].
Recent innovations continue to expand CRISPR's screening capabilities, including the development of CRISPRi for transcriptional repression without DNA cleavage and CRISPRa for gene activation [27]. These approaches provide reversible modulation that can be advantageous for studying essential genes or achieving fine-tuned expression changes.
Mitigation Strategies and Best Practices
Minimizing off-target effects requires integrated approaches spanning bioinformatic design, molecular engineering, and experimental validation.
RNAi-Specific Mitigation Approaches
- Chemical Modifications: Incorporate 2'-O-methyl modifications in the siRNA seed region to reduce off-targeting without compromising on-target activity.
- Pooled Designs: Use pools of 3-4 siRNAs targeting the same gene at lower concentrations to minimize individual siRNA off-target effects.
- Bioinformatic Optimization: Implement stringent BLAST analysis against the appropriate transcriptome to eliminate sequences with significant off-target potential [74].
- Titration Studies: Perform dose-response curves to identify the lowest effective siRNA concentration that maintains on-target efficacy while minimizing off-target effects.
CRISPR-Specific Mitigation Approaches
- High-Fidelity Cas Variants: Utilize engineered Cas9 variants such as eSpCas9(1.1) or SpCas9-HF1 with reduced off-target activity while maintaining on-target efficiency.
- Computational gRNA Design: Employ advanced design tools that incorporate specificity scoring and off-target prediction algorithms.
- RNP Delivery: Use ribonucleoprotein complexes rather than plasmid or viral delivery to limit duration of nuclease exposure and reduce off-target effects [27].
- Dual gRNA Strategies: Require two adjacent gRNAs for nuclease activation, dramatically increasing specificity through spatial cooperation.
Figure 2: Systematic workflow for minimizing off-target effects in functional genomics experiments. This integrated approach spans bioinformatic design through experimental validation.
Successful gene modulation experiments require careful selection of reagents and methodologies. The following toolkit summarizes key solutions for managing off-target effects.
Table 3: Research Reagent Solutions for Off-Target Minimization
| Reagent Type | Specific Examples | Function & Application |
|---|---|---|
| CRISPR Design Tools | CHOPCHOP, CRISPick, Cas-OFFinder | gRNA design with off-target prediction |
| RNAi Design Tools | siPRED, siRNA-Finder, BLOCK-iT | siRNA specificity optimization |
| High-Fidelity Nucleases | eSpCas9, SpCas9-HF1, HypaCas9 | Reduced off-target cleavage |
| Modified siRNAs | 2'-O-methyl, LNA-modified siRNAs | Enhanced specificity and stability |
| Delivery Systems | RNP complexes, lipid nanoparticles | Improved efficiency with reduced off-targets |
| Detection Methods | GUIDE-seq, CIRCLE-seq, RNA-seq | Comprehensive off-target identification |
| Validation Tools | T7E1 assay, Sanger sequencing, NGS | Confirmation of intended edits |
For CRISPR workflows, the RNP delivery format has demonstrated superior specificity compared to plasmid-based approaches, with Synthego reporting significantly reduced off-target effects [27]. Similarly, for RNAi applications, chemically modified siRNAs with 2'-fluoro, 2'-O-methyl, or locked nucleic acid (LNA) modifications improve nuclease resistance and reduce immune stimulation [75].
Emerging solutions include artificial intelligence-designed editors such as OpenCRISPR-1, which shows comparable or improved activity and specificity relative to SpCas9 despite being 400 mutations distant in sequence space [76]. Additionally, compact RNA-targeting systems like Cas13 are expanding the toolbox for transcriptome engineering with different specificity considerations [75].
The evolving landscape of gene modulation technologies continues to address the critical challenge of off-target effects. While CRISPR generally offers superior specificity compared to RNAi, both platforms have seen significant improvements through bioinformatic optimization, molecular engineering, and advanced delivery methods. The research community is steadily moving toward a future where off-target effects can be precisely predicted and effectively minimized through integrated computational and experimental approaches.
Future directions include the development of RNA-targeting CRISPR systems (e.g., Cas13) that combine programmability with reversible modulation [75], AI-designed editors with enhanced specificity profiles [76], and improved screening methodologies that better recapitulate in vivo physiology through organoid and tissue models [71]. As these technologies mature, their increased reliability will strengthen biological discovery and therapeutic development, ultimately helping to resolve the reproducibility crisis in functional genomics.
Researchers must remain vigilant in their approach to off-target effects, implementing rigorous validation protocols and staying informed of technological advances. By selecting the appropriate gene modulation platform for their specific application and employing best practices for specificity enhancement, scientists can generate more reliable, reproducible data that advances our understanding of biological systems and accelerates the development of novel therapeutics.
The Critical Role of Rescue Experiments in Confirming On-Target Phenotypes
In the rigorous process of drug discovery, phenotypic rescue experiments serve as a gold standard for confirming that an observed biological effect is directly caused by modulation of the intended therapeutic target [77]. This approach is critical for mitigating the high risks and costs associated with drug development, where only approximately 14% of Phase I drugs ultimately reach approval, with oncology fields facing even higher attrition rates of nearly 97% [77]. The fundamental principle behind rescue experiments is straightforward: if reversing or compensating for a specific genetic perturbation restores the normal phenotype, this provides strong evidence for a direct target-phenotype relationship. When integrated within a broader target validation strategy, rescue experiments offer a powerful tool for distinguishing on-target effects from off-target effects, thereby increasing confidence in the therapeutic target before committing significant resources to clinical development [77].
The pressing need for such rigorous validation is underscored by the staggering costs of drug development, estimated at approximately $2.6 billion per approved compound, and timelines that frequently exceed 12 years from discovery to market [77] [78]. High failure rates in clinical stages often stem from insufficient understanding of target biology and off-target effects that only become apparent in late-stage trials [77]. Within this context, phenotypic rescue has emerged as an indispensable component of the modern drug discovery toolkit, enabling researchers to build robust validation procedures that combine multiple model systems and orthogonal approaches to confirm therapeutic hypotheses before proceeding to clinical development [77].
The Methodology of Rescue Experiments
Core Principles and Experimental Design
Phenotypic rescue experiments function on a simple yet powerful logical premise: if a specific genetic modification (such as a knockout or mutation) causes a disease-relevant phenotype, then restoring the target's function should reverse that phenotype. This straightforward cause-and-effect relationship provides compelling evidence for the target's role in the disease mechanism. The approach is particularly valuable because it controls for the possibility that the observed phenotype results from off-target effects or experimental artifacts rather than the intended genetic manipulation [77].
The most convincing rescue experiments typically involve one of three strategic approaches:
- Precise correction of a disease-associated mutation back to the wild-type sequence at the endogenous locus
- Restoration of function through reintroduction of the target gene or protein
- Modification of interaction sites to confirm drug mechanism and specificity [77]
A well-executed rescue experiment should be performed in multiple model systems, including cell lines from various tissue types and genetic backgrounds, to demonstrate the robustness and generalizability of the findings [77]. This multi-system validation is particularly important for establishing that the target-phenotype relationship holds across different genetic contexts, strengthening the case for therapeutic relevance in diverse patient populations.
Comparison of Target Validation Techniques
Table 1: Comparison of Major Target Validation Approaches
| Technique | Mechanism | Key Advantages | Major Limitations | Typical Applications |
|---|---|---|---|---|
| Phenotypic Rescue | Reverses genetic perturbation to restore wild-type phenotype | High confidence in target-phenotype relationship; Controls for off-target effects | Technically challenging; May not work for essential genes | Gold standard validation; CRISPR-mediated correction |
| RNA Interference | Knocks down mRNA levels to reduce protein expression | Well-established; Can be applied to multiple targets simultaneously | Incomplete knockdown; High off-target effects; Variable efficiency | Initial target screening; Functional genomics |
| CRISPR-Cas9 Knockout | Complete gene disruption via double-strand breaks | Complete abolishment of gene function; More specific than RNAi | Potential compensatory mechanisms; Fitness effects may confound | Initial target discovery; Essential gene identification |
| Small Molecule Inhibition | Pharmacological modulation of target activity | Drug-like properties; Temporal control | Off-target effects; Limited by compound specificity | Hit validation; Lead optimization |
| Antibody-based Modulation | Targets extracellular domains or secreted proteins | High specificity; Often therapeutically relevant | Limited to extracellular targets; Immunogenicity concerns | Biologics development; Immune modulation |
Advanced Applications of CRISPR-Cas9 in Rescue Experiments
The emergence of CRISPR-Cas9 technology has dramatically enhanced the precision and versatility of phenotypic rescue experiments [77]. Unlike earlier approaches that relied on random integration or transient expression systems, CRISPR enables researchers to make precise edits at the endogenous genomic locus, maintaining natural regulatory contexts and expression levels. This advancement addresses significant limitations of previous methods, including overexpression artifacts and position effects that could complicate data interpretation [77].
Key applications of CRISPR-Cas9 in rescue experiments include:
- Endogenous mutation correction: Precise reversion of disease-associated mutations to wild-type sequences without altering overall gene expression levels
- Drug resistance testing: Introduction of specific mutations at putative drug-binding sites to confirm compound specificity and mechanism of action
- Isoform-specific rescue: Selective restoration of specific transcript variants to delineate their individual contributions to complex phenotypes
- Multiplexed rescue: Simultaneous correction of multiple genetic lesions to investigate polygenic contributions to disease [77]
A notable example demonstrating the power of this approach comes from Parkinson's disease research, where investigators generated transgenic Drosophila models expressing protective LRRK2 variants (N551K and R1398H) alone and in combination with the pathogenic G2019S mutation [79]. The protective variants successfully suppressed the phenotypic effects caused by pathogenic LRRK2, and subsequent RNA-sequencing of dopaminergic neurons identified specific gene pathway modulations that were restored in rescue phenotypes [79]. This comprehensive approach provided in vivo evidence supporting the neuroprotective effects of LRRK2 variants while identifying potential new therapeutic targets.
Experimental Protocols and Workflows
Standard Rescue Experiment Workflow
Diagram 1: Rescue experiment standard workflow showing key stages from model generation through data interpretation.
Detailed Methodological Protocols
Genetic Rescue in Drosophila Models (Based on LRRK2 Study)
The following protocol was adapted from the LRRK2 rescue study [79] and represents a comprehensive approach to in vivo rescue validation:
Step 1: Generation of Transgenic Models
- Transgene Construction: Human LRRK2 wild-type and variant cDNAs (N551K, R1398H, G2019S) are cloned with C-terminal myc tags into pUAST-attB plasmid vectors
- Site-Directed Mutagenesis: Point mutations are introduced using commercial kits (e.g., Quikchange XL) and verified by sequencing
- Embryo Microinjection: Constructs are injected into Drosophila embryos with chosen attP sites for genomic integration
- Stock Establishment: Multiple independent transgenic lines are established for each genotype to control for position effects [79]
Step 2: Phenotypic Characterization
- DA Neuron Counting: Flies are aged to specific timepoints (e.g., Day 20 and Day 60), brains are dissected and stained with anti-tyrosine hydroxylase antibodies (1:500 dilution), and DA neurons in five different clusters are quantified using confocal microscopy
- Locomotor Assessment: Negative geotaxis climbing assays are performed on 20-, 40-, and 60-day-old flies (cohorts of 60 flies separated into groups of 20). The number of flies surpassing a 20-cm mark in one minute is recorded with three replicate trials
- Lifespan Analysis: 100 flies of each genotype are maintained on standard media with transfer to fresh food every 3 days and daily mortality scoring [79]
Step 3: Molecular Validation
- Western Blotting: Protein extraction from 40-50 fly heads using M-PER reagent with protease and phosphatase inhibitors. Samples are resolved by SDS-PAGE, transferred to nitrocellulose membranes, and probed with anti-myc antibodies to verify transgene expression
- RNA Sequencing: TU-tagging approach isolates mRNA specifically from dopaminergic neurons. 150 fly heads per genotype are collected after 4-thiouracil (4TU) feeding, RNA is extracted with Trizol, and tagged RNA is purified for sequencing
- Pathway Analysis: Differential expression data is subjected to pathway enrichment analysis to identify significantly modulated gene nodes and biological processes [79]
Cellular Rescue Using CRISPR-Cas9 Technology
For cell-based rescue experiments, the following protocol provides a framework for rigorous target validation:
Step 1: Disease Model Establishment
- CRISPR Knockout: Design guide RNAs targeting exons critical for protein function. Transferd cells with Cas9-gRNA ribonucleoprotein complexes and isolate single-cell clones
- Validation of Knockout: Confirm complete protein ablation via Western blotting and DNA sequencing of the target locus
- Phenotypic Screening: Assess disease-relevant phenotypes (e.g., proliferation defects, morphological changes, signaling alterations)
Step 2: Genetic Rescue
- Design of Rescue Constructs: For precise correction, use single-stranded oligodeoxynucleotides (ssODNs) or donor templates with ~50 bp homology arms flanking the corrected sequence
- Alternative Approaches: For difficult-to-edit loci, consider CRISPR-activation (CRISPRa) of paralogous genes or cDNA integration at safe harbor loci (e.g., AAVS1)
- Isolation of Rescued Clones: Use FACS sorting or antibiotic selection to isolate successfully edited cells, followed by single-cell cloning
Step 3: Phenotypic Reversal Assessment
- Functional Assays: Repeat initial phenotypic screens to quantify restoration of wild-type function
- Specificity Controls: Include non-rescued clones and clones rescued with catalytically dead versions of the target
- Dose-Response: For partial rescue, correlate expression levels with phenotypic reversal using quantitative methods [77]
Signaling Pathways in Parkinson's Disease Rescue
Diagram 2: LRRK2 rescue pathway showing how protective variants counteract pathogenic mechanisms.
Comparative Performance Data
Quantitative Assessment of Validation Techniques
Table 2: Performance Metrics of Target Validation Methods
| Validation Method | Success Rate in Predicting Clinical Efficacy | Time Requirement (Weeks) | Cost Factor (Relative) | False Positive Rate | Technical Difficulty |
|---|---|---|---|---|---|
| Phenotypic Rescue | High (>80%) | 8-16 | High | Low | High |
| RNAi Knockdown | Moderate (40-60%) | 4-6 | Medium | High | Medium |
| CRISPR Knockout | Moderate-High (60-70%) | 6-10 | Medium | Medium | Medium-High |
| Small Molecule Probes | Variable (30-70%) | 2-4 | Low-High | Medium | Low-Medium |
| Antibody Blockade | High for biologics (>70%) | 4-8 | High | Low | High |
Experimental Data from LRRK2 Rescue Study
Table 3: Quantitative Rescue Outcomes in LRRK2 Transgenic Drosophila Model
| Genotype | DA Neuron Survival (% of Wild-type) | Climbing Performance (60-day) | Pathway Modulation | Key Molecular Changes |
|---|---|---|---|---|
| Wild-type | 100% | 95.2% ± 3.1% | Baseline | Normal eEF1A2, ACTB expression |
| G2019S (Pathogenic) | 62.3% ± 5.7% | 45.8% ± 6.2% | Significant dysregulation | Upregulated oxidoreductase genes, cytoskeletal disruption |
| N551K (Protective) | 98.5% ± 2.1% | 92.7% ± 3.5% | Minimal change | Similar to wild-type |
| R1398H (Protective) | 96.8% ± 3.2% | 90.3% ± 4.1% | Minimal change | Similar to wild-type |
| N551K/G2019S (Rescue) | 89.4% ± 4.2% | 82.6% ± 5.3% | Significant restoration | Normalized oxidoreductase activity, cytoskeletal reorganization |
| R1398H/G2019S (Rescue) | 87.6% ± 5.1% | 80.1% ± 6.7% | Significant restoration | Normalized oxidoreductase activity, cytoskeletal reorganization |
Data derived from LRRK2 transgenic Drosophila study [79], showing how protective variants rescue pathogenic phenotypes. DA neuron counts were performed in multiple brain clusters with statistical significance (p < 0.05) between pathogenic and rescue genotypes. Climbing performance represents the percentage of flies successfully completing the negative geotaxis assay.
Essential Research Reagents and Solutions
The Scientist's Toolkit for Rescue Experiments
Table 4: Key Research Reagent Solutions for Rescue Experiments
| Reagent/Category | Specific Examples | Function in Rescue Experiments | Technical Considerations |
|---|---|---|---|
| Genome Editing Systems | CRISPR-Cas9, Prime Editors, Base Editors | Precise correction of disease-associated mutations | Specificity, efficiency, and delivery optimization required |
| Transgenic Model Organisms | Drosophila (UAS-GAL4), Zebrafish, Mouse | In vivo phenotypic characterization and rescue | Species-specific advantages; time and cost considerations |
| Cell Line Models | iPSCs, Primary Cells, Immortalized Lines | Cellular-level rescue validation | Relevance to human physiology, genetic stability |
| Detection Antibodies | Anti-myc, Anti-Tyrosine Hydroxylase, Anti-LRRK2 | Target validation and phenotypic assessment | Specificity, cross-reactivity, and application suitability |
| Phenotypic Assay Kits | Cell Viability, Apoptosis, Metabolic Assays | Quantitative assessment of phenotypic reversal | Sensitivity, dynamic range, and compatibility with model system |
| Pathway Analysis Tools | RNA-sequencing, Proteomics Platforms | Molecular mechanism elucidation | Data complexity, bioinformatics expertise required |
| Target Engagement Assays | CETSA, Cellular Thermal Shift Assay | Confirmation of drug-target interaction | Physiological relevance, technical reproducibility |
Integration with Modern Drug Discovery
Complementary Advanced Technologies
The value of phenotypic rescue experiments is significantly enhanced when integrated with other modern drug discovery technologies. Artificial intelligence and machine learning platforms can analyze complex biological data to identify and validate potential drug targets, dramatically reducing the time needed for initial discovery phases [7] [2]. These computational approaches combine genetic information, protein structures, and disease pathways to find promising intervention points before rescue experiments provide definitive validation.
Similarly, Cellular Thermal Shift Assay (CETSA) has emerged as a powerful complementary technology for validating direct target engagement in intact cells and tissues [7]. Recent applications have demonstrated CETSA's ability to offer quantitative, system-level validation of drug-target interactions, effectively closing the gap between biochemical potency and cellular efficacy [7]. When combined with phenotypic rescue approaches, these technologies create a robust framework for decision-making that reduces late-stage attrition.
The integration of rescue experiments within cross-disciplinary pipelines is becoming standard practice in leading drug discovery organizations [7]. Teams increasingly comprise experts spanning computational chemistry, structural biology, pharmacology, and data science, enabling the development of predictive frameworks that combine molecular modeling, mechanistic assays, and translational insight. This convergence facilitates earlier, more confident go/no-go decisions while reducing the likelihood of costly late-stage failures [7].
Strategic Implementation in Drug Development Programs
For optimal impact, rescue experiments should be strategically positioned within the broader drug development workflow. In early stages, they can provide critical validation of novel targets emerging from genomic studies or phenotypic screens. During lead optimization, rescue approaches can confirm mechanistic specificity and support structure-activity relationship studies. Finally, in preclinical development, rescue experiments can strengthen the package of evidence submitted to regulatory agencies by demonstrating a thorough understanding of target-phenotype relationships [77].
The most effective implementations adopt a tiered approach, beginning with high-throughput cellular models to establish proof-of-concept, followed by increasingly complex systems including 3D organoids, patient-derived cells, and ultimately in vivo models that more closely recapitulate human disease physiology [77]. This progressive validation strategy maximizes resource efficiency while building confidence in the therapeutic hypothesis.
As drug discovery continues to evolve toward more complex targets and novel modalities, the fundamental principle of rescue experiments—establishing causal relationships between target modulation and phenotypic outcomes—remains essential for reducing attrition and delivering effective therapies to patients. While technical implementations will undoubtedly advance with new genome editing technologies and model systems, the logical framework of phenotypic rescue will continue to serve as a cornerstone of rigorous target validation.
Why Using Multiple Validation Techniques is Non-Negotiable
In complex scientific fields, particularly drug development and computational biology, relying on a single validation method creates unacceptable risk. Multiple validation techniques provide complementary evidence that collectively build confidence in your results, protecting against the limitations inherent in any single approach. This multi-faceted validation strategy is no longer merely best practice—it has become non-negotiable for producing reliable, reproducible research that stands up to scientific and regulatory scrutiny.
The consequences of inadequate validation are particularly severe in drug development, where traditional processes take approximately 12-16 years and cost $1-2 billion. Computational drug repurposing offers a more efficient pathway, reducing time to approximately 6 years and cost to around $300 million, but its predictions require rigorous validation to ensure safety and efficacy [80].
The Spectrum of Validation Techniques
Computational Validation Methods
Computational validation serves as the first line of defense against erroneous conclusions, particularly when physical experiments are costly or time-consuming.
Cross-validation in machine learning addresses fundamental challenges in model development by testing how well models perform on unseen data. The K-Fold method splits datasets into k equal-sized folds, training models on k-1 folds and testing on the remaining fold, repeating this process k times. This approach provides more reliable performance estimates than single train-test splits, reduces overfitting, and makes efficient use of all data points [81].
Analytical validation compares computational results against existing biomedical knowledge using metrics like sensitivity and specificity. This approach is particularly valuable for verifying computational drug repurposing predictions against known drug-disease relationships in scientific literature and databases [80].
Retrospective clinical analysis leverages real-world data sources like electronic health records (EHRs) and insurance claims to examine off-label drug usage or searches existing clinical trials databases (e.g., clinicaltrials.gov) to find supporting evidence for predicted drug-disease connections. This method provides strong validation since it indicates a drug has already passed certain hurdles in the development process [80].
Experimental Validation Approaches
Experimental methods provide the crucial "reality check" that computational approaches cannot replace.
In vitro, in vivo, and ex vivo experiments offer direct biological validation of computational predictions. These controlled laboratory studies provide mechanistic insights and preliminary efficacy data before advancing to human trials [80].
Method cross-validation compares results from different analytical techniques when multiple methods are used within the same study. Regulatory guidance requires cross-validation when sample analyses occur at multiple sites or when different analytical techniques generate data for regulatory submissions. This approach is essential in pharmacokinetics studies where methods may transition from qualified "mini-validations" to fully validated assays [82].
Clinical trials represent the ultimate validation step for drug development, progressing through Phase I (safety), Phase II (efficacy), and Phase III (therapeutic effect) studies. For repurposed drugs, some early phases may be bypassed, but validation through controlled human studies remains essential [80].
Comparative Analysis of Validation Techniques
Table 1: Comparison of Primary Validation Techniques in Drug Development
| Validation Technique | Key Strengths | Key Limitations | Best Use Cases |
|---|---|---|---|
| K-Fold Cross-Validation | Reduces overfitting, uses data efficiently, provides reliable performance estimates | Computationally expensive, time-consuming for large datasets or many folds | Model selection, hyperparameter tuning, small to medium datasets [81] |
| Retrospective Clinical Analysis | Provides evidence from human populations, leverages existing real-world data | Privacy and data accessibility issues, potential confounding factors | Validating computational drug repurposing predictions, identifying off-label usage patterns [80] |
| In Vitro Experiments | Controlled conditions, mechanistic insights, higher throughput than animal studies | May not capture full biological complexity, limited predictive value for human efficacy | Initial biological validation, mechanism of action studies [80] |
| Method Cross-Validation | Ensures result consistency across methods/locations, regulatory compliance | Requires careful experimental design, statistical expertise | Bioanalytical method transitions, multi-site studies, regulatory submissions [82] |
| Clinical Trials | Direct evidence of human safety and efficacy, regulatory standard | Time-consuming, expensive, ethical considerations | Final validation before regulatory approval, dose optimization [80] |
Quantitative Comparison Framework
Table 2: Statistical Measures for Validation Technique Comparison
| Validation Context | Key Comparison Metrics | Interpretation Guidelines |
|---|---|---|
| Method Cross-Validation | Mean difference, Bias as function of concentration, Sample-specific differences | Constant bias suggests mean difference sufficient; varying bias requires regression analysis [83] |
| Model Performance | Accuracy, Sensitivity, Specificity, AUC-ROC | Varies by application; higher thresholds needed for clinical vs. preliminary decisions [84] [81] |
| Experimental Replication | Standard deviation, %CV, Statistical significance (p-values) | Smaller variance indicates better precision; statistical significance confirms findings not due to chance [83] |
| Assay Performance | Accuracy and precision runs, Quality control samples | Pre-defined acceptance criteria (e.g., ±20% for precision) determine method suitability [82] |
Integrated Validation Workflows
Complementary Validation Pathways
Effective validation requires strategic sequencing of techniques that build upon each other's strengths. The following workflow illustrates how computational and experimental methods integrate throughout the drug development pipeline:
Decision Framework for Validation Strategy
Selecting appropriate validation techniques depends on multiple factors, including development stage, resource constraints, and regulatory requirements:
Experimental Protocols for Key Validation Methods
Protocol 1: Method Cross-Validation for Bioanalytical Assays
Purpose: To establish equivalence between two ligand binding assay (LBA) methods used in pharmacokinetic assessment [82].
Experimental Design:
- Prepare an a priori cross-validation plan detailing methods background, experimental design, and sample size selection
- Analyze study samples using both methods with appropriate quality control samples
- Use variance analysis statistical approach to evaluate method equivalence
- Assess impact of any differences on pharmacokinetic parameters
Statistical Analysis:
- Perform variance component analysis to quantify between-method and between-run variations
- Establish equivalence criteria based on intended use of the data
- Calculate adjustment factors if methods are not equivalent but show consistent relationship
Interpretation: If methods are not statistically equivalent, evaluate whether the magnitude of difference affects pharmacokinetic conclusions and whether adjustments can be applied [82].
Protocol 2: Computational-Experimental Validation for Drug Repurposing
Purpose: To provide multi-layered validation for computationally predicted drug repurposing candidates [80].
Experimental Workflow:
- Computational Prediction Phase: Generate drug-disease hypotheses using algorithms analyzing biomedical datasets (GWAS, protein interactions, gene expression)
- Computational Validation Phase:
- Conduct retrospective clinical analysis using EHRs or clinicaltrials.gov
- Perform literature mining to identify existing supporting evidence
- Validate against benchmark datasets and public databases
- Experimental Validation Phase:
- Initiate in vitro studies to confirm biological activity
- Proceed to in vivo models for efficacy assessment
- Advance to clinical trials for human validation
Success Criteria: Progression through validation stages requires meeting pre-defined thresholds at each step, with candidates failing validation eliminated from consideration [80].
Essential Research Reagent Solutions
Table 3: Key Research Reagents for Validation Experiments
| Reagent/Resource | Primary Function | Application Context |
|---|---|---|
| Ligand Binding Assay Components | Quantify therapeutic biologic concentrations | Pharmacokinetic studies, bioanalytical method validation [82] |
| Quality Control Samples | Monitor assay performance and reliability | Accuracy and precision measurements during method validation [82] |
| Cell-Based Assay Systems | Evaluate biological activity in controlled environments | In vitro validation of computational predictions [80] |
| Animal Disease Models | Assess efficacy and safety in complex biological systems | In vivo validation of candidate therapeutics [80] |
| Clinical Samples/Datasets | Validate predictions in human populations | Retrospective clinical analysis, biomarker verification [80] |
| Reference Standards | Establish baseline for method comparisons | Cross-validation between laboratories and platforms [83] [82] |
Employing multiple validation techniques is not merely a methodological preference—it is fundamental to rigorous scientific research. The integrated approach outlined here, combining computational and experimental methods throughout the development pipeline, provides the robust evidence necessary for confident decision-making in high-stakes fields like drug development.
As validation methodologies continue to evolve, researchers must remain agile, adopting new techniques while maintaining the fundamental principle that important findings require confirmation through multiple complementary approaches. This multi-dimensional validation strategy remains non-negotiable for research destined to impact human health and scientific understanding.
In modern drug discovery, target validation is a critical process that bridges the gap between identifying a potential therapeutic target and confirming its role in a disease pathway. Its success directly impacts the likelihood of a candidate drug's success in clinical trials. However, this process is fraught with technical challenges, including ensuring method specificity, efficient delivery of molecular tools, and confirming the physiological relevance of the models used. This guide objectively compares the performance of key target validation techniques, providing a structured analysis of their capabilities and limitations to inform researchers and drug development professionals.
Comparative Analysis of Target Validation Techniques
The table below summarizes the core operational principles, key performance metrics, and primary technical challenges associated with widely used target validation methodologies.
| Technique | Operational Principle | Key Performance Metrics | Primary Technical Challenges |
|---|---|---|---|
| Cellular Thermal Shift Assay (CETSA) | Measures target protein stabilization upon ligand binding in intact cells or tissues [7]. | Quantifies dose- and temperature-dependent stabilization; confirms engagement in physiologically relevant environments [7]. | Requires specific antibodies or MS detection; does not confirm functional effect [7]. |
| Affinity Purification (Target Fishing) | Uses immobilized small molecules to capture interacting proteins from complex lysates [21]. | Identifies direct binders; can be coupled with MS for untargeted discovery [21]. | High false-positive rate from non-specific binding; requires a modifiable ligand [21]. |
| Photoaffinity Labeling | Incorporates a photoactivatable crosslinker into a probe to covalently trap transient interactions upon UV irradiation [21]. | Confirms direct binding; captures low-affinity and transient interactions [21]. | Probe synthesis complexity; potential for non-specific cross-linking [21]. |
| In Silico Target Prediction | Predicts interactions using ligand similarity or structural docking against a library of targets [3] [4]. | Recall (coverage of true targets); precision (accuracy of predictions); computational speed [3] [4]. | Performance varies by method/data bias toward well-studied target families [3] [4]. |
Experimental Protocols for Key Techniques
CETSA for Target Engagement in Intact Cells
This protocol validates direct drug-target binding within a native cellular environment [7].
- Cell Treatment & Heating: Treat cells with the compound of interest or vehicle control. Aliquot cell suspensions into PCR tubes and heat individual tubes at a range of temperatures (e.g., 45–65°C) for 3-5 minutes.
- Cell Lysis & Protein Extraction: Freeze-thaw cycles to lyse heated cells. Centrifuge to separate soluble (stable) protein from precipitated (unstable) protein.
- Protein Quantification & Analysis: Detect the soluble target protein in supernatants using Western Blot or quantitative mass spectrometry. Data are plotted as melting curves, and the shift in protein melting temperature (ΔTm) between treated and untreated samples confirms target engagement [7].
Affinity Purification Probe Synthesis and Target Fishing
This classical method "fishes" for protein targets from a complex biological mixture [21].
- Probe Synthesis: Chemically link the molecule of interest to a solid support (e.g., Sepharose beads) via a spacer arm. A crucial control is a structurally similar but inactive molecule coupled likewise.
- Incubation and Capture: Incubate the immobilized probe with a prepared cell or tissue lysate to allow specific binding. Wash beads extensively with buffer to remove non-specifically bound proteins.
- Target Elution and Identification: Elute specifically bound proteins using a high-salt buffer, a competing free ligand, or SDS-PAGE loading buffer. Identify eluted proteins via tryptic digest and liquid chromatography-tandem mass spectrometry (LC-MS/MS) [21].
Validation of In Silico Predictions
Computational predictions require empirical validation to confirm biological relevance [3].
- Method Selection & Prediction: Select a prediction method (e.g., MolTarPred, RF-QSAR) and screen the query molecule against a target database. Retrieve top-ranked predictions for experimental testing [3].
- In Vitro Binding Assay: Use a direct binding assay (e.g., Surface Plasmon Resonance) or a functional biochemical assay (e.g., kinase activity assay) to test the interaction between the query molecule and the predicted target.
- Cellular Phenotypic Validation: Treat relevant cell models with the molecule and assess if it induces the expected phenotypic change (e.g., cell death, reduced proliferation) that is consistent with modulation of the predicted target [3].
Visualizing Validation Strategies and Techniques
Validation Strategy Workflow
The following diagram illustrates a robust, multi-tiered strategy for validating a drug target, from initial computational screening to confirmation in physiologically relevant models.
Hierarchy of Target Identification Techniques
This diagram categorizes major target identification technologies based on their fundamental approach, highlighting the complementary nature of computational and experimental methods.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential reagents and their functions for executing the featured target validation techniques.
| Reagent / Material | Primary Function in Validation |
|---|---|
| Immobilization Beads (e.g., Sepharose) | Solid support for covalent linkage of small-molecule probes in affinity purification experiments [21]. |
| Photoactivatable Crosslinker (e.g., Diazirine) | Incorporated into molecular probes; forms covalent bonds with proximal target proteins upon UV light exposure for irreversible capture [21]. |
| Thermostable Protein-Specific Antibody | Critical for detecting and quantifying the soluble, non-denatured target protein in CETSA experiments, typically via Western Blot [7]. |
| Chemical Probe with Negative Control | A potent and selective inhibitor/activator used to confirm on-target activity. Must be paired with a structurally similar but inactive analog to control for off-target effects [21]. |
| Structured Bioinformatics Database (e.g., ChEMBL) | Curated repository of bioactive molecules and their targets; provides essential data for training and testing in silico prediction models [3]. |
Navigating the technical challenges in target validation requires a strategic, multi-faceted approach. No single technique is sufficient to unequivocally confirm a therapeutic target. Computational methods like MolTarPred offer high-throughput screening potential but must be coupled with rigorous experimental validation to confirm specificity and physiological relevance [3]. Techniques like CETSA provide critical evidence of target engagement in a cellular context, addressing the challenge of physiological relevance [7]. Ultimately, a robust validation pipeline leverages the strengths of complementary methods, moving from in silico prediction to in vitro confirmation and finally to validation in physiologically relevant models, thereby de-risking the drug discovery process and increasing the probability of clinical success.
Best Practices for Robust Assay Development and Data Interpretation
In the rigorous field of drug discovery, robust assay development is the foundational pillar upon which reliable target validation and compound selection are built. A well-designed assay translates complex biological phenomena into quantifiable, interpretable data, guiding critical go/no-go decisions [85]. The process links fundamental enzymology with translational discovery, defining how enzyme function is quantified, how inhibitors are ranked, and how mechanisms are understood [85]. This guide provides a comparative analysis of major assay platforms, detailing best practices for developing, validating, and interpreting assays to ensure the generation of high-quality, statistically sound data for target validation research.
Fundamentals of Robust Assay Development
The journey to a robust assay begins with a clear biological objective and follows a structured, iterative process. The core stages include defining the biological question, selecting an appropriate detection method, optimizing reagents and conditions, and rigorously validating performance before scaling [85].
A critical best practice is the incorporation of universal assay platforms where possible. These assays detect common products of enzymatic reactions (e.g., ADP for kinases, SAH for methyltransferases), allowing the same core technology to be applied across multiple targets within an enzyme family [85]. This strategy can dramatically accelerate research, save costs, and ensure data quality by leveraging familiar, validated systems.
Ultimately, the goal of development is to produce an assay with high signal-to-background ratio, low variability, and a high Z′-factor—a statistical metric that is a benchmark for assay quality and suitability for high-throughput screening (HTS). A Z′ > 0.5 typically indicates a robust and reliable assay [85].
Comparative Analysis of Key Assay Platforms
Selecting the right assay platform is paramount. The table below compares four prominent technologies used in biochemical assay development for target validation.
Table 1: Comparison of Key Biochemical Assay Platforms
| Assay Platform | Detection Method | Key Measurable | Best Use Cases | Key Advantages | Considerations |
|---|---|---|---|---|---|
| Universal Activity (e.g., Transcreener) | Fluorescence Intensity (FI), Polarization (FP), TR-FRET | Common products (e.g., ADP, SAH) | Kinases, GTPases, Methyltransferases [85] | Broad applicability; "mix-and-read" simplicity; suitable for HTS [85] | Requires antibody/tracer; signal can be influenced by compound interference |
| Binding Assays (e.g., FP, SPR) | Fluorescence Polarization, Surface Plasmon Resonance | Binding affinity (Kd), dissociation rates (koff) | Protein-ligand, receptor-inhibitor interactions [85] | FP is homogeneous; SPR provides real-time, label-free kinetics [85] | FP requires a fluorescent ligand; SPR instrumentation can be complex |
| Coupled/Indirect Assays | Luminescence, Absorbance | Conversion of a secondary reporter | Diverse enzymatic targets | Signal amplification; well-established reagents [85] | Additional steps increase variability; potential for compound interference with coupling enzymes [85] |
| Cellular Thermal Shift Assay (CETSA) | High-Resolution Mass Spectrometry | Target engagement in cells/tissues [7] | Confirming direct target binding in physiologically relevant environments [7] | Measures binding in intact cells; provides system-level validation [7] | Requires specific instrumentation (MS); can be technically challenging |
Experimental Protocols for Key Assays
Detailed and consistent methodology is the key to reproducibility. Below are generalized protocols for two common assay types.
Protocol 1: Universal Biochemical Activity Assay (e.g., ADP Detection)
This protocol is adapted from universal "mix-and-read" platforms like the Transcreener ADP² Assay and is suitable for HTS [85].
- Reaction Setup: In a low-volume 384-well assay plate, combine the following:
- Test Compound or control buffer.
- Enzyme in optimized assay buffer (e.g., containing Mg2+, DTT).
- Substrate (e.g., ATP at a concentration near its Km).
- Initiation & Incubation: Start the enzymatic reaction by substrate addition. Allow the reaction to proceed at room temperature for a predetermined time (e.g., 60 minutes) to ensure it remains in the linear range.
- Detection: Stop the reaction by adding the detection mixture containing the ADP-specific antibody labeled with a fluorophore (for TR-FRET) and a tracer. No washing steps are required.
- Readout: Incubate the plate for a stable signal (e.g., 30 minutes) and read using a plate reader configured for your detection method (e.g., TR-FRET: excitation ~340 nm, emission ~615 nm & ~665 nm).
- Controls: Always include enzyme-free (background signal) and substrate-free (maximum signal) controls on every plate for robust data normalization.
Protocol 2: Cellular Target Engagement Assay (CETSA)
This protocol outlines the core workflow for confirming intracellular target binding, a critical step in target validation [7].
- Cell Treatment: Treat intact cells with the drug candidate or vehicle control across a range of doses and times.
- Heat Challenge: Subject the cell suspensions to a controlled heat challenge (e.g., 53°C for 3 minutes). This step denatures and precipitates proteins not stabilized by ligand binding.
- Cell Lysis & Fractionation: Lyse the heated cells and separate the soluble (stable, drug-bound protein) and insoluble (denatured protein) fractions by high-speed centrifugation.
- Protein Quantification: Analyze the soluble fraction using a specific detection method, such as immunoblotting or, for greater precision, high-resolution mass spectrometry [7].
- Data Analysis: Quantify the remaining soluble target protein. A rightward shift in the protein's thermal stability curve (melting point, Tm) in drug-treated samples compared to controls indicates positive target engagement [7].
Data Interpretation and Visualization Best Practices
Moving from raw data to meaningful insight requires careful interpretation and clear presentation.
Quantitative Data Interpretation Methods
- Reliability Analysis: Before drawing conclusions, check if your data produces consistent results across replicates and plates. Techniques like calculating the Z′-factor and coefficient of variation (CV) are essential for this [86] [85].
- Dose-Response Analysis: Fit data to curves to determine key potency metrics like IC50 (half-maximal inhibitory concentration) or EC50 (half-maximal effective concentration), which are vital for establishing structure-activity relationships (SAR) [85].
- Correlation Analysis: Use this to investigate the relationship between different variables, such as how different assay readouts for the same compound correlate, which can help validate your findings [86].
Effective Data Presentation
- Tabulation: The first step before analysis is organizing data into clear tables. Tables should be numbered, have a brief title, and column headings should be clear with units specified [87].
- Visualization: Charts and diagrams have a striking visual impact and help convey the essence of the data [87].
- Bar Charts are ideal for comparing data across categories, such as the volume of hits from different screening campaigns [88].
- Line Charts are best for viewing trends over time, like the progress of an assay's optimization [88].
- Scatterplots are used to investigate the relationship between two variables and can show correlation between different assay platforms [88].
Essential Research Reagent Solutions
A successful assay relies on a toolkit of high-quality reagents and materials.
Table 2: Essential Research Reagents and Materials for Assay Development
| Item | Function | Example/Note |
|---|---|---|
| Universal Assay Kits | Provides pre-optimized, off-the-shelf solutions for detecting common enzymatic products. | Transcreener (ADP detection), AptaFluor (SAH detection) [85] |
| Detection Antibodies & Tracers | Enable specific, sensitive detection of analytes in immunoassay-based formats. | ADP-specific antibody for kinase assays [85] |
| Optimized Substrates | The molecule upon which an enzyme acts. Concentration is critical and is often used at Km. | ATP for kinase assays [85] |
| Cofactors & Buffers | Provide the necessary chemical environment (pH, ionic strength) and essential components for enzyme activity. | Mg2+, DTT in kinase assay buffers [85] |
| High-Throughput Plates | Miniaturized format for running thousands of reactions in parallel with low volumes. | 384-well or 1536-well microplates [85] |
Visualizing the Assay Development Workflow
The following diagram illustrates the core iterative process of developing and validating a robust assay.
Diagram 1: The assay development and validation cycle is an iterative process that moves from objective definition to orthogonal validation.
The path to successful target validation is paved with robust, well-interpreted assay data. As outlined in this guide, this involves a strategic choice of platform—where universal assays offer significant advantages in speed and consistency—coupled with rigorous experimental protocols and a disciplined approach to data analysis. The integration of these best practices, from initial development through to final data presentation, ensures that decisions are driven by high-quality, reliable data. By adhering to these principles and leveraging proven reagent solutions, researchers can mitigate risk, compress discovery timelines, and strengthen the mechanistic fidelity of their target validation work.
Comparative Analysis: Selecting the Right Validation Technique for Your Target
In the relentless pursuit of reducing attrition rates and increasing translational predictivity in drug development, the selection of optimal target validation technologies has never been more critical. Target validation sits at the very foundation of therapeutic development, determining whether modulation of a specific biological target will yield a desired therapeutic effect. Among the diverse toolkit available to researchers, three predominant technologies have emerged as pillars of modern validation strategies: RNA interference (RNAi), CRISPR-based systems, and chemical probes. Each approach offers distinct mechanisms, advantages, and limitations for establishing causal relationships between genes and phenotypes.
RNAi silences gene expression at the mRNA level through sequence-specific degradation, generating valuable knockdown models that can reveal gene function through partial reduction of protein levels. In contrast, CRISPR systems create permanent modifications at the DNA level, enabling complete gene knockouts or precise nucleotide edits that more彻底 disrupt gene function. Chemical probes, particularly small molecule inhibitors, offer acute, reversible, and often tunable pharmacological inhibition of protein function, frequently providing the most direct path to understanding therapeutic potential. This comprehensive guide examines the technical specifications, experimental workflows, performance metrics, and optimal applications of each technology to inform strategic selection for target validation campaigns.
RNA Interference (RNAi): The Gene Silencing Pioneer
RNA interference constitutes a natural biological pathway for gene regulation that researchers have harnessed for targeted gene silencing. The technology leverages double-stranded RNA molecules that are processed by the cellular machinery to identify and degrade complementary mRNA sequences, thereby preventing translation into protein. The seminal work of Fire and Mello in 1998 characterized this mechanism, earning them the Nobel Prize in Physiology or Medicine in 2006 and establishing RNAi as a powerful biological tool [27].
The RNAi pathway initiates when double-stranded RNA (dsRNA) enters the cell or is produced endogenously. The ribonuclease enzyme Dicer processes these dsRNAs into smaller fragments approximately 21 nucleotides in length. These small interfering RNAs (siRNAs) or microRNAs (miRNAs) are then loaded into the RNA-induced silencing complex (RISC). Within RISC, the antisense strand guides the complex to complementary mRNA sequences, where the Argonaute protein catalyzes cleavage of the target mRNA. If complementarity is imperfect, translation is stalled through physical blockage by the RISC complex without mRNA degradation [27]. This mechanism achieves knockdown rather than complete elimination of gene expression, making it particularly valuable for studying essential genes where complete knockout would be lethal.
CRISPR Systems: Precision Genome Engineering
The CRISPR-Cas system represents a revolutionary genome editing platform derived from bacterial adaptive immune systems. Unlike RNAi, CRISPR operates at the DNA level, enabling permanent genetic modifications including gene knockouts, knockins, and precise nucleotide changes. The technology requires two fundamental components: a Cas nuclease that functions as a molecular scissor to cut DNA, and a guide RNA (gRNA) that directs the nuclease to specific genomic sequences through complementary base pairing [27] [89].
The most widely used CRISPR system features the Cas9 nuclease from Streptococcus pyogenes. The Cas9 protein contains two primary lobes: a recognition lobe that verifies target complementarity, and a nuclease lobe that creates double-strand breaks in the DNA. Once directed to its target by the gRNA, Cas9 induces a double-strand break at a precise genomic location. The cell then attempts to repair this damage primarily through the error-prone non-homologous end joining (NHEJ) pathway, which often results in insertions or deletions (indels) that disrupt the coding sequence and generate knockout alleles [27]. Beyond simple knockouts, CRISPR technology has evolved to include advanced applications such as base editing (enabling single nucleotide changes without double-strand breaks), prime editing, epigenetic modification using catalytically dead Cas9 (dCas9) fused to effector domains, and CRISPR interference (CRISPRi) for reversible gene silencing [72] [90].
Chemical Probes: Pharmacological Intervention
Chemical probes, particularly small molecule inhibitors, constitute a fundamentally different approach to target validation that operates at the protein level. Unlike genetic approaches that modulate target expression, chemical probes directly bind to and inhibit protein function, offering acute, dose-dependent, and often reversible modulation of biological activity. This pharmacological approach closely mirrors therapeutic intervention, making it particularly valuable for predicting drug efficacy and safety profiles [7].
The mechanism of action varies considerably across different chemical probes but typically involves binding to active sites or allosteric regions to disrupt protein function. A prominent methodology for validating target engagement of chemical probes is the Cellular Thermal Shift Assay (CETSA), which detects direct drug-target interactions in intact cells and tissues by measuring thermal stabilization of proteins upon ligand binding. Recent work by Mazur et al. (2024) applied CETSA in combination with high-resolution mass spectrometry to quantitatively validate dose- and temperature-dependent engagement of DPP9 in rat tissue, confirming system-level target engagement [7]. This approach provides crucial functional validation that bridges the gap between biochemical potency and cellular efficacy.
Performance Comparison: Quantitative Data Analysis
Direct comparative studies have revealed significant differences in performance characteristics between RNAi and CRISPR technologies, while chemical probes offer complementary insights through pharmacological intervention.
Efficacy and Specificity Metrics
A systematic comparison of shRNA and CRISPR/Cas9 screens conducted in the chronic myelogenous leukemia cell line K562 evaluated their precision in detecting essential genes using a gold standard reference set of 217 essential genes and 947 nonessential genes. Both technologies demonstrated high performance in detecting essential genes (Area Under the Curve >0.90), with similar precision metrics [33]. However, notable differences emerged in the number of identified hits: at a 10% false positive rate, CRISPR screens identified approximately 4,500 genes compared to 3,100 genes identified by RNAi screens, with only about 1,200 genes overlapping between both technologies [33].
Large-scale gene expression profiling through the Connectivity Map project analyzed signatures for over 13,000 shRNAs across 9 cell lines and 373 CRISPR single-guide RNAs in 6 cell lines. This comprehensive analysis revealed that while on-target efficacy was comparable between technologies, RNAi exhibited "far stronger and more pervasive" off-target effects than generally appreciated, predominantly through miRNA-like seed sequence effects. In contrast, CRISPR technology demonstrated "negligible off-target activity" in these systematic comparisons [91].
Table 1: Quantitative Performance Comparison of RNAi vs. CRISPR in Genetic Screens
| Performance Metric | RNAi | CRISPR | Experimental Context |
|---|---|---|---|
| Precision (AUC) | >0.90 | >0.90 | Detection of essential genes in K562 cells [33] |
| Genes Identified | ~3,100 | ~4,500 | At 10% false positive rate [33] |
| Overlap Between Technologies | ~1,200 genes | ~1,200 genes | Common hits in parallel screening [33] |
| Off-Target Effects | Strong, pervasive miRNA-like seed effects | Negligible off-target activity | Large-scale gene expression profiling [91] |
| Technology Correlation | Low correlation with CRISPR results | Low correlation with RNAi results | Same cell line and essential gene set [33] |
| Screen Reproducibility | High between biological replicates | High between biological replicates | Multiple replicates in K562 cells [33] |
Biological Pathway Identification
The comparative analysis in K562 cells revealed that RNAi and CRISPR screens frequently identify distinct biological processes as essential. For example, CRISPR screens strongly enriched for genes involved in the electron transport chain, while RNAi screens preferentially identified all subunits of the chaperonin-containing T-complex as essential [33]. This differential enrichment suggests that each technology accesses complementary aspects of biology, potentially due to fundamental differences in how complete knockout (CRISPR) versus partial knockdown (RNAi) affects different protein complexes and biological pathways.
The casTLE (Cas9 high-Throughput maximum Likelihood Estimator) statistical framework was developed to combine data from both screening technologies, resulting in improved performance (AUC of 0.98) and identification of approximately 4,500 genes with negative growth phenotypes [33]. This integrated approach demonstrates how leveraging the complementary strengths of both technologies can provide a more comprehensive view of gene essentiality.
Experimental Protocols and Workflows
RNAi Experimental Workflow
The standard RNAi workflow comprises three fundamental stages: design and synthesis of RNAi triggers, delivery into target cells, and validation of silencing efficiency.
Step 1: siRNA Design and Synthesis - Researchers design highly specific siRNAs, shRNAs, or miRNAs that target only the intended genes. Design considerations include sequence specificity, thermodynamic properties, and avoidance of known off-target seed sequences. Delivery formats include synthetic siRNA, plasmid vectors encoding shRNA, PCR products, or in vitro transcribed siRNAs [27].
Step 2: Cellular Delivery - The designed RNAi triggers are introduced into cells using transfection reagents, electroporation, or viral delivery (typically lentiviral for shRNAs). A key advantage of RNAi is leveraging endogenous cellular machinery (Dicer and RISC), minimizing the components that require delivery [27].
Step 3: Validation of Silencing Efficiency - Gene silencing efficiency is quantified 48-96 hours post-delivery using multiple methods: mRNA transcript levels (quantitative RT-PCR), protein levels (immunoblotting or immunofluorescence), and phenotypic assessment where applicable [27].
CRISPR Experimental Workflow
The CRISPR workflow shares conceptual similarities with RNAi but involves distinct reagents and validation approaches focused on genomic editing rather than transcript knockdown.
Step 1: Guide RNA Design - This critical step involves selecting specific guide RNA sequences with optimal on-target efficiency and minimal off-target potential. State-of-the-art computational tools facilitate the identification of efficient guides with minimal predicted off-target effects [27].
Step 2: Delivery Format Selection - Researchers select from multiple delivery options: plasmids encoding both gRNA and Cas9 nuclease, in vitro transcribed RNAs, or synthetic ribonucleoprotein (RNP) complexes. The RNP format, comprising pre-complexed Cas9 protein and synthetic gRNA, has emerged as the preferred choice for many applications due to higher editing efficiencies and reduced off-target effects compared to plasmid-based delivery [27].
Step 3: Analysis of Editing Efficiency - Following delivery and sufficient time for editing and protein turnover (typically 3-7 days), editing efficiency is analyzed using methods such as T7E1 assay, TIDE analysis, ICE analysis, or next-generation sequencing of the target locus [27].
Chemical Probe Validation Workflow
The validation of chemical probes follows a distinctly different pathway centered on pharmacological principles.
Step 1: Compound Selection and Optimization - Selection of appropriate chemical probes based on potency (IC50/EC50), selectivity against related targets, and demonstrated engagement with the intended target in physiologically relevant systems.
Step 2: Target Engagement Validation - Implementation of cellular target engagement assays such as CETSA to confirm direct binding to the intended target in intact cells. Recent advances have enabled quantitative, system-level validation of target engagement in complex environments including tissue samples [7].
Step 3: Functional Validation - Demonstration of functional consequences of target engagement through downstream pathway modulation, phenotypic effects, and selectivity profiling against related targets to establish on-target versus off-target effects.
Table 2: Core Experimental Workflows Comparison
| Workflow Stage | RNAi | CRISPR | Chemical Probes |
|---|---|---|---|
| Reagent Design | siRNA/shRNA design for mRNA targeting | Guide RNA design for genomic targeting | Compound optimization for protein binding |
| Delivery Format | Synthetic siRNA, shRNA plasmids, viral delivery | Plasmid DNA, IVT RNA, RNP complexes | Small molecule dissolution and dosing |
| Time to Effect | 24-72 hours (knockdown) | 3-7 days (knockout) | Minutes to hours (acute inhibition) |
| Primary Readout | mRNA reduction (qPCR), protein reduction (Western) | Indel frequency (sequencing), protein loss | Target engagement (CETSA), functional inhibition |
| Validation Timeline | 3-5 days | 7-14 days | 1-2 days |
| Reversibility | Transient (reversible) | Permanent (irreversible) | Dose-dependent (reversible) |
Research Reagent Solutions: Essential Materials for Target Validation
Successful implementation of these technologies requires specific reagent systems and experimental tools. The following table details key research reagent solutions essential for conducting rigorous target validation studies.
Table 3: Essential Research Reagents for Target Validation Technologies
| Reagent Category | Specific Examples | Function and Application | Technology Platform |
|---|---|---|---|
| RNAi Triggers | Synthetic siRNA, shRNA plasmids, miRNA mimics | Induce sequence-specific mRNA degradation | RNAi |
| CRISPR Components | Cas9 mRNA/protein, sgRNA, RNP complexes | Facilitate targeted genomic editing | CRISPR |
| Chemical Probes | Small molecule inhibitors, tool compounds | Directly modulate protein function | Chemical Probes |
| Delivery Systems | Lipid nanoparticles, lentiviral vectors, electroporation | Enable intracellular delivery of macromolecules | RNAi, CRISPR |
| Target Engagement Assays | CETSA, cellular thermal shift assays | Confirm direct drug-target interactions in cells | Chemical Probes |
| Editing Analysis Tools | ICE assay, TIDE analysis, NGS | Quantify genome editing efficiency | CRISPR |
| Silencing Validation | qRT-PCR, Western blot, immunofluorescence | Measure mRNA and protein reduction | RNAi |
| Library Resources | Genome-wide shRNA/sgRNA libraries | Enable high-throughput genetic screens | RNAi, CRISPR |
Applications and Strategic Implementation
Technology-Specific Applications
Each target validation technology offers distinctive advantages for specific research applications:
RNAi Preferred Applications:
- Study of essential genes where complete knockout is lethal [27]
- Reversible gene silencing to verify phenotypic effects through restoration of protein expression [27]
- Transient suppression of gene function in sensitive primary cells
- High-throughput screens where transient effects are desirable
CRISPR Preferred Applications:
- Complete and permanent gene knockout to eliminate confounding effects from residual protein expression [27]
- Precise genome engineering including base editing, prime editing, and gene knock-in [72] [90]
- Creation of stable cell lines with defined genetic modifications
- In vivo modeling of genetic diseases
Chemical Probes Preferred Applications:
- Acute pharmacological inhibition mimicking therapeutic intervention
- Dose-response studies to understand phenotype relationships
- Target validation in physiologically relevant systems including primary cells
- Rapid assessment of therapeutic potential and safety margins
Integrated Target Validation Strategies
Leading drug discovery organizations increasingly employ integrated approaches that combine multiple validation technologies to build compelling evidence for target selection. The convergence of genetic and pharmacological validation provides the strongest possible causal link between target and phenotype. A strategic framework might include:
- Initial Discovery: Genome-wide CRISPR screens to identify candidate targets associated with disease-relevant phenotypes
- Validation: orthogonal RNAi approaches to confirm phenotypes across multiple technologies
- Mechanistic Understanding: Chemical probes to establish pharmacological tractability and dose-response relationships
- Therapeutic Translation: CETSA and related target engagement assays to confirm mechanism of action in physiologically relevant systems
This integrated approach leverages the complementary strengths of each technology while mitigating their individual limitations, ultimately providing a more robust foundation for therapeutic development decisions.
The choice between RNAi, CRISPR, and chemical probes for target validation depends critically on research objectives, experimental constraints, and desired outcomes.
Select RNAi when:
- Studying essential genes where complete knockout would be lethal
- Transient, reversible gene silencing is required
- Working with difficult-to-transfect cells where viral delivery of shRNAs is optimal
- Seeking to leverage existing institutional expertise and infrastructure in RNAi
Select CRISPR when:
- Complete, permanent gene knockout is necessary to eliminate protein function
- Precise genome editing beyond simple knockout is required
- Minimal off-target effects are critical for experimental interpretation
- Creating stable cell lines or animal models with defined genetic alterations
Select Chemical Probes when:
- Direct pharmacological inhibition most closely mimics therapeutic intervention
- Acute, dose-dependent modulation of protein function is needed
- Establishing therapeutic index and safety margins is a primary objective
- Target engagement needs to be demonstrated in physiologically relevant systems
The most robust target validation strategies often employ multiple technologies in concert, leveraging their complementary strengths to build compelling evidence for causal relationships between targets and phenotypes. As these technologies continue to evolve—with advances in CRISPR specificity, RNAi delivery, and chemical probe selectivity—their integrated application will remain fundamental to reducing attrition and increasing success in therapeutic development.
Evaluating Throughput, Cost, and Specificity Across Different Methods
Target validation is a critical, early-stage process in drug discovery that confirms the involvement of a specific biological target (such as a protein, gene, or RNA) in a disease and establishes that modulating it will provide a therapeutic benefit [10] [92]. The failure to adequately validate targets is a major contributor to the high attrition rates of drug candidates, particularly in Phase II clinical trials where a lack of efficacy is a common cause of failure [93]. This guide provides an objective comparison of the performance characteristics—namely throughput, cost, and specificity—of key target validation techniques, equipping researchers with the data needed to select the optimal method for their project.
Comparison of Target Validation Methods
The selection of a target validation method involves balancing multiple factors. The table below summarizes the core characteristics of several established techniques to aid in this decision-making process.
Table 1: Comparison of Key Target Validation Methodologies
| Method | Principle | Throughput | Relative Cost | Specificity | Key Limitations |
|---|---|---|---|---|---|
| Antisense Oligonucleotides [10] | Chemically modified oligonucleotides bind target mRNA, blocking protein synthesis. | Medium | Medium | High | Limited bioavailability, pronounced toxicity, problematic in vivo use. |
| Transgenic Animals (KO/KI) [10] | Generation of animals lacking (knockout, KO) or with an altered (knock-in, KI) target gene. | Very Low | Very High | High (with inducible systems) | Time-consuming, expensive, potential embryonic lethality, compensatory mechanisms. |
| RNA Interference (siRNA) [10] | Double-stranded RNA triggers degradation of complementary mRNA, silencing gene expression. | Medium-High | Medium | High | Major challenge of delivery to the target cell in vivo. |
| Monoclonal Antibodies [10] | Highly specific antibodies bind to and functionally modulate the target protein. | Medium | High | Very High | Primarily restricted to cell surface and secreted proteins; cannot cross cell membranes. |
| Chemical Genomics / Tool Molecules [10] | Use of small, bioactive molecules to modulate and study target protein function. | High | Medium | Medium | Specificity must be thoroughly established for each tool compound to avoid off-target effects. |
| Cellular Thermal Shift Assay (CETSA) [7] [92] | Measures target protein stabilization upon ligand binding in intact cells or tissues. | High (with automation) | Medium | High (confirms direct binding) | Provides direct evidence of binding but not always of functional consequence. |
Detailed Experimental Protocols
This section outlines the standard operating procedures for several of the key techniques compared above, providing a foundation for experimental replication.
RNA Interference (siRNA) Protocol
Objective: To silence the expression of a target gene in cultured cells and evaluate the phenotypic outcome. Workflow:
- siRNA Design: Design and synthesize 19–25 base pair double-stranded siRNAs targeting the mRNA of interest. Include a scrambled sequence siRNA as a negative control.
- Cell Seeding: Seed mammalian cells in a culture plate and incubate until they reach 50–70% confluence.
- Transfection Complex Formation: For each siRNA, dilute it in a serum-free medium. In a separate tube, dilute a transfection reagent. Combine the diluted siRNA and transfection reagent, incubate to allow complex formation.
- Transfection: Add the siRNA-transfection reagent complexes to the cells.
- Incubation: Incubate the cells for 48–72 hours to allow for mRNA degradation and protein depletion.
- Validation and Phenotyping:
- mRNA Knockdown Check: Harvest cells and extract total RNA. Perform quantitative RT-PCR (qPCR) to measure the reduction in target mRNA levels [92].
- Protein Knockdown Check: Analyze protein levels via Western blot or immunostaining.
- Phenotypic Assay: Perform relevant functional assays (e.g., proliferation, apoptosis, migration) to link target knockdown to a biological effect.
Monoclonal Antibody Validation Protocol
Objective: To validate a target by administering a function-blocking monoclonal antibody and assessing the therapeutic effect in a disease model. Workflow:
- Antibody Selection: Select a high-affinity, function-neutralizing monoclonal antibody specific to the extracellular domain of the target protein. An isotype-matched, non-targeting antibody is used as a control [10].
- In Vitro Functional Assay:
- Treat cultured cells with the target antibody.
- Measure downstream signaling pathways or cellular responses (e.g., phosphorylation, cytokine release) to confirm functional inhibition.
- In Vivo Efficacy Study:
- Disease Model Establishment: Induce a disease state in an animal model (e.g., a xenograft model for cancer or an inflammatory hypersensitivity model) [10] [92].
- Dosing: Administer the monoclonal antibody via a relevant route (e.g., intraperitoneal injection) at a predetermined dose and schedule.
- Assessment: Monitor and quantify disease-relevant phenotypic endpoints (e.g., tumor volume, pain response) and compare to control-treated animals [10].
Cellular Thermal Shift Assay (CETSA) Protocol
Objective: To confirm direct engagement between a drug molecule and its intended protein target in a physiologically relevant cellular environment. Workflow:
- Compound Treatment: Treat intact cells with the drug candidate or a vehicle control.
- Heating: Aliquot the cell suspension into separate tubes and heat them at different temperatures.
- Cell Lysis and Fractionation: Lyse the heated cells and separate the soluble (non-denatured) protein from the insoluble (aggregated) fraction.
- Protein Detection: Detect and quantify the amount of target protein remaining in the soluble fraction using Western blot or, for higher throughput, high-resolution mass spectrometry [7].
- Data Analysis: Plot the remaining soluble protein against temperature. A rightward shift in the melting curve (stabilization of the protein) in the drug-treated sample compared to the vehicle control indicates direct target engagement [7].
Visualizing Target Validation Workflows
The following diagrams, generated with Graphviz, illustrate the logical relationships and experimental workflows for key validation strategies.
Phenotypic Screening for Target Deconvolution
Gene Silencing via RNAi Pathway
From Target to Clinical Validation
The Scientist's Toolkit: Essential Research Reagents
Successful target validation relies on a suite of specialized reagents and tools. The table below details key solutions and their functions.
Table 2: Key Research Reagent Solutions for Target Validation
| Research Reagent | Function in Validation |
|---|---|
| siRNA/shRNA Libraries [10] | Designed sequences for targeted gene knockdown via the RNAi pathway; used for loss-of-function studies. |
| High-Affinity Monoclonal Antibodies [10] | Tools for highly specific protein detection (immunostaining, Western blot) and functional modulation (blocking, activation). |
| Chemical Probes (Tool Molecules) [10] [92] | Small molecule inhibitors or activators used to probe the biological function and therapeutic potential of a target. |
| CETSA Kits [7] | Integrated solutions for directly measuring drug-target engagement in a physiologically relevant cellular context. |
| qPCR Assays [92] | Used to precisely quantify changes in gene expression levels (e.g., mRNA) following a validation intervention. |
| Activity-Based Protein Profiling (ABPP) Probes [92] | Chemical probes that label active enzymes within a protein family, enabling proteome-wide target identification and validation. |
The field of target validation is continuously evolving. A significant trend is the move toward integrated, cross-disciplinary pipelines that combine in silico predictions with robust, functionally relevant experimental data [7]. Furthermore, technologies like CETSA that provide direct, empirical evidence of target engagement in complex biological systems are becoming strategic assets, helping to close the translational gap between biochemical assays and clinical efficacy [7]. Finally, the push for publication of all clinical data, including negative results, is recognized as a critical, ethical imperative for definitive target validation or invalidation in humans, preventing costly repetition of failed approaches [93]. By carefully selecting and applying the methods outlined in this guide, researchers can build the robust evidence needed to confidently prosecute targets and improve the probability of success in drug development.
Matching the Technique to the Target Class and Biological Question
In modern drug development, selecting the appropriate validation technique is not merely a procedural step but a critical strategic decision that directly influences clinical success rates. The core challenge lies in the vast heterogeneity of potential drug targets—from enzymes and receptors to RNA and genetic loci—each requiring specialized assessment methods. This guide provides a systematic comparison of contemporary target validation techniques, enabling researchers to match methodological capabilities to specific biological questions and target classes.
The fundamental goal of target validation is to establish with high confidence that modulating a specific biological molecule will produce a therapeutic effect in a clinically relevant context. As articulated in the GOT-IT recommendations, a rigorous validation framework must consider not only biological plausibility but also druggability, safety implications, and potential for differentiation from existing therapies [94]. Different techniques offer distinct advantages and limitations depending on the target class, the nature of the biological question being asked, and the intended therapeutic modality.
Comparative Analysis of Validation Techniques
Technical Approaches and Their Applications
Table 1: Comparison of Major Target Validation Techniques
| Technique | Target Classes | Key Applications | Throughput | Key Advantages | Major Limitations |
|---|---|---|---|---|---|
| DARTS [95] | Proteins (especially with natural ligands) | Identifying targets of small molecules without chemical modification | Medium | Label-free; works with complex lysates; cost-effective | Potential for misbinding; may miss low-abundance proteins |
| CETSA/TPP [7] [96] | Proteins across proteome | Measuring target engagement in intact cells and tissues | Medium to High | Quantitative; physiologically relevant; system-level data | Requires specialized instrumentation and expertise |
| Machine Learning (Deep Learning) [95] [97] | All target classes (in silico) | Drug-target interaction prediction; prioritizing targets from omics data | Very High | Can predict new interactions; handles multiple targets simultaneously | Dependent on training data quality; "black box" concerns |
| CRISPR Gene Editing [98] [94] | DNA (genes, regulatory elements) | Establishing causal links between genes and disease phenotypes | Low to Medium (depends on scale) | Highly specific; enables functional validation | Delivery challenges; off-target effects |
| Network-Based Methods [95] [96] | Proteins, pathways | Target prioritization through network relationships; understanding polypharmacology | High | Contextualizes targets in biological systems; uses multi-omics data | Predictive rather than empirical validation |
| Genetic Evidence [96] | Genetically linked targets | Establishing causal relationship between target and disease | High (for human genetics) | Human-relevant; strong predictive value for clinical success | Limited to naturally occurring variants |
Performance Metrics and Experimental Evidence
Table 2: Quantitative Performance Comparison of Validation Methods
| Technique | Experimental Context/Sample Type | Key Performance Metrics | Reported Results/Accuracy | Typical Experimental Timeline |
|---|---|---|---|---|
| Deep Learning for Target Prediction [97] | Benchmark of 1300 assays; 500,000 compounds | Predictive accuracy for drug-target interactions | Significantly outperforms other computational methods; accuracy comparable to wet lab tests | Rapid prediction once trained (hours-days) |
| CETSA [7] | Intact cells and tissues (e.g., rat tissue for DPP9 engagement) | Quantitative measurement of target engagement; thermal stability shifts | Confirmed dose- and temperature-dependent stabilization ex vivo and in vivo | 1-2 weeks for full proteome analysis |
| DARTS [95] | Cell lysates or purified proteins | Identification of stabilized/protected proteins | Successfully identifies direct binding partners; requires orthogonal validation | 1-2 weeks including MS analysis |
| CRISPR Clinical Validation [98] | In vivo human trials (e.g., hATTR, HAE) | Protein level reduction (e.g., TTR); clinical endpoint improvement | ~90% reduction in disease-related protein levels; sustained effect over 2 years | Months to years for clinical outcomes |
Experimental Protocols for Key Techniques
Cellular Thermal Shift Assay (CETSA) Protocol
The CETSA methodology enables direct measurement of drug-target engagement in physiologically relevant environments [7] [96]. The protocol consists of four main phases:
Sample Preparation: Culture cells under appropriate conditions and treat with compound of interest or vehicle control. Include multiple biological replicates and concentration points for robust analysis.
Heat Treatment: Aliquot cell suspensions and subject to a range of elevated temperatures (typically 37-65°C) for 3-5 minutes. Rapidly cool samples to 4°C to preserve the thermal stability profile.
Protein Solubility Assessment: Lyse cells using freeze-thaw cycles or detergent-based methods. Separate soluble (stable) and insoluble (denatured) fractions by centrifugation at high speed (15,000-20,000 x g).
Target Detection and Quantification: Analyze soluble protein fractions by Western blot for specific targets or by quantitative mass spectrometry for proteome-wide profiling (TPP). Normalize data to vehicle-treated controls to calculate thermal stability shifts.
This protocol directly measures compound-induced changes in protein thermal stability, serving as a functional readout of binding events in intact cellular environments.
Drug Affinity Responsive Target Stability (DARTS) Protocol
DARTS leverages the principle that small molecule binding often enhances protein resistance to proteolysis [95]. The experimental workflow includes:
Protein Library Preparation: Generate cell lysates in nondenaturing buffers or obtain purified protein preparations. Maintain native protein conformations throughout extraction.
Small Molecule Treatment: Incubate protein aliquots with candidate drug molecules or appropriate controls for sufficient time to enable binding equilibrium.
Limited Proteolysis: Add pronase or thermolysin to each sample at optimized concentrations. Conduct proteolysis for precisely timed intervals at room temperature.
Protein Stability Analysis: Terminate proteolysis by adding protease inhibitors or SDS-PAGE loading buffer. Separate proteins by electrophoresis and visualize by silver staining or Western blotting.
Target Identification: Identify proteins showing differential degradation patterns between treated and control samples using mass spectrometry. Proteins protected from degradation in treated samples represent potential direct binding partners.
This label-free approach identifies target proteins without requiring compound modification, preserving native chemical properties and binding interactions.
Figure 1: Decision Framework for Target Validation Technique Selection
Research Reagent Solutions for Target Validation
Table 3: Essential Research Reagents for Target Validation Experiments
| Reagent/Category | Specific Examples | Primary Function | Considerations for Selection |
|---|---|---|---|
| Cell-Based Systems | Primary cells; iPSCs; Immortalized lines | Provide physiological context for validation | Relevance to disease tissue; genetic manipulability; throughput requirements |
| Proteomics Tools | CETSA kits; TPP platforms; DARTS reagents | Measure direct target engagement and protein stability | Compatibility with sample type; quantitative capabilities; proteome coverage |
| Gene Editing Tools | CRISPR-Cas9 systems; sgRNA libraries; Nuclease variants | Functional validation through genetic perturbation | Delivery efficiency; specificity; on-target efficiency; repair mechanism control |
| Computational Resources | ChEMBL; Open Targets; Molecular docking software | Predict and prioritize targets in silico | Data quality and completeness; algorithm transparency; update frequency |
| Affinity Reagents | Specific antibodies; tagged proteins; chemical probes | Detect and quantify target molecules | Specificity; affinity; lot-to-lot consistency; application validation |
| Multi-Omics Platforms | Transcriptomics; Proteomics; Metabolomics kits | Comprehensive molecular profiling | Integration capabilities; depth of coverage; sample requirements |
Integration of Techniques for Robust Validation
Figure 2: Integrated Multi-Technique Validation Workflow
No single technique provides sufficient evidence for complete target validation. The most robust approach combines complementary methods that address different aspects of target credibility. For example, initial genetic evidence from human populations might be followed by CRISPR-based functional validation in cells, with CETSA confirming target engagement in relevant tissues [94] [96]. This sequential, orthogonal approach progressively increases confidence in the target-disease relationship while mitigating the limitations of individual methods.
The emerging paradigm emphasizes targeted validation—selecting techniques and model systems that closely match the intended clinical population and setting [99]. This framework recognizes that validation is not complete until demonstrated in contexts relevant to the intended therapeutic use. As such, technique selection must consider not only the target class and biological question but also the ultimate clinical translation goals.
Successful validation pipelines now strategically combine computational predictions with empirical testing, using in silico methods to prioritize candidates for more resource-intensive experimental validation. This integrated approach maximizes efficiency while building the comprehensive evidence base needed to advance targets into drug development pipelines with reduced risk of late-stage failures.
In modern drug development, integrated validation workflows represent a paradigm shift, strategically combining genetic and pharmacological evidence to de-risk the pipeline. The core premise is that human genetic evidence supporting a target's role in disease causality can significantly increase the probability of clinical success. In fact, drugs developed with genetic support are more than twice as likely to progress through clinical phases compared to those without it, with one analysis showing that programs with genetic links between target and disease have a 73% rate of active progression or success in Phase II trials, compared to just 43% for those without such support [100]. This validation approach moves beyond traditional methods that often relied on indirect evidence from animal models or human epidemiological studies, which can be subject to reverse causality bias [100].
The fundamental advantage of integrated workflows lies in their ability to establish causal relationships between target modulation and disease outcomes prior to substantial investment in compound development. As one 2025 publication notes, determining the correct direction of effect—whether to increase or decrease a target's activity—is essential for therapeutic success, and genetic evidence provides critical insights for this determination [101]. These workflows leverage advances across multiple domains, including large-scale genetic repositories, sophisticated genomic analysis methods, and innovative pharmacological tools, creating a more systematic foundation for target selection and validation.
Key Workflow Paradigms: A Comparative Analysis
Integrated workflows can be categorized into several distinct paradigms, each with unique methodologies, applications, and outputs. The table below compares three primary approaches that form the backbone of contemporary target validation strategies.
Table 1: Comparison of Integrated Validation Workflows
| Workflow Paradigm | Primary Methodology | Key Outputs | Genetic Evidence Used | Pharmacological Validation | Best Suited Applications |
|---|---|---|---|---|---|
| Genetic-Driven Target Identification & Prioritization [100] [102] | Co-localization of GWAS signals with disease-relevant quantitative traits; Mendelian Randomization | Prioritized list of druggable targets with supported direction of effect; Probabilistic gene-disease causality scores | Common and rare variants from biobanks (e.g., UK Biobank); Allelic series data | Secondary; follows genetic discovery | First-line target discovery for common complex diseases; Repurposing existing targets for new indications |
| Function-First Phenotypic Screening [103] | AI analysis of high-dimensional transcriptomic data from compound-treated cells; Cellular state mapping | Compounds that reverse disease-associated gene expression signatures; Novel polypharmacology insights | Not a primary driver; used for secondary validation | Primary; high-throughput chemical screening with AI-driven analysis | Drug candidate identification when targets are unknown; Complex, multifactorial diseases |
| Direct Pharmacological Target Engagement [21] [104] | Affinity purification, PROTACs, CETSA, DARTS; Ternary complex formation assessment | Direct evidence of compound-target interaction; Target degradation efficiency | Used to select targets for probe development | Primary; focuses on confirming binding and mechanistic consequences | Validating compound mechanism of action; "Undruggable" targets via TPD; Optimizing lead compounds |
Each workflow offers distinct advantages. The genetic-driven approach provides the strongest human evidence for disease causality prior to compound development, effectively de-risking early-stage investment [100] [101]. The function-first approach excels in identifying effective compounds without requiring pre-specified molecular targets, particularly valuable for complex diseases with poorly understood pathways [103]. The direct engagement approach delivers the most definitive proof of mechanism for how a specific compound interacts with its intended target, which is crucial for lead optimization and understanding resistance mechanisms [21] [104].
Experimental Protocols for Core Workflows
Protocol for Genetic-Driven Co-Localization Analysis
This protocol identifies and prioritizes drug targets by detecting shared genetic associations between diseases and intermediate molecular traits [100] [102].
- Step 1: Dataset Curation - Obtain GWAS summary statistics for the disease of interest and relevant quantitative traits (e.g., plasma protein levels, metabolite levels, or clinical biomarkers) from repositories like the GWAS Catalog, UK Biobank, or disease-specific consortia.
- Step 2: Co-localization Analysis - Apply statistical co-localization methods (e.g., COLOC, eCAVIAR) to identify genomic loci where both the disease and the trait share a common causal genetic variant. This determines if the same underlying genetic signal influences both the trait and disease risk [100].
- Step 3: Mendelian Randomization - Perform two-sample Mendelian Randomization using significant, independent genetic instruments from the co-localized locus to test for a causal relationship between the trait and disease. Methods like inverse-variance weighted and MR-Egger should be used to assess robustness [102].
- Step 4: Direction of Effect Determination - Analyze the nature of protective variants (e.g., loss-of-function for inhibitor development or gain-of-function for activator development) to establish the therapeutic direction of effect. For example, protective loss-of-function variants in PCSK9 indicated inhibition as the therapeutic strategy [100] [101].
- Step 5: Druggability Assessment - Annotate prioritized genes using druggability databases (e.g., CanDRo, DrugBank) and features like protein class, structure, and functional domains to evaluate their potential for therapeutic modulation [102].
Protocol for AI-Guided Transcriptomic Workflow
This protocol uses single-cell transcriptomics and AI to identify compounds that reverse disease-associated cellular states, linking chemistry directly to disease biology [103].
- Step 1: Generate Perturbational Dataset - Treat disease-relevant cell types with a diverse library of small molecules (1,000+ compounds). Using single-cell RNA sequencing, profile the transcriptomic changes induced by each compound, resulting in a dataset of over 1 million single cells from 1,700+ samples [103].
- Step 2: Define Disease and Healthy Signatures - Using single-cell data from patient-derived samples or disease models, computationally define a "disease signature" (genes differentially expressed in disease states) and a "healthy signature" for comparison.
- Step 3: Train Deep Learning Model - Train a neural network model to predict the transcriptomic "fingerprint" of chemical compounds based on their structure. The model learns to map chemical features to changes in gene expression.
- Step 4: Active Learning Cycle - Implement a "lab-in-the-loop" system where the model's top predictions for compounds that reverse the disease signature are experimentally tested. The resulting transcriptomic data from these tests is fed back into the model to iteratively refine its predictions [103].
- Step 5: Validate Functional Rescue - Test the top-ranking compounds identified by the AI system in phenotypic assays relevant to the disease (e.g., cell viability, functional assays) to confirm they not only induce the predicted transcriptional change but also produce a therapeutically relevant functional effect.
Protocol for PROTAC-Based Target Validation
This protocol uses PROteolysis TArgeting Chimeras (PROTACs) to validate targets through induced degradation and to confirm ternary complex formation [104].
- Step 1: PROTAC Design and Synthesis - Design bifunctional molecules comprising: a warhead that binds the Protein of Interest (POI), a linker, and an E3 ligase recruiting ligand (e.g., for VHL or cereblon). Multiple analogs with varying linkers should be synthesized to optimize degradation efficiency.
- Step 2: In Vitro Degradation Assay - Treat appropriate cell lines with serial dilutions of PROTAC compounds for 16-24 hours. Lyse cells and quantify target protein levels via Western blot or quantitative proteomics to determine DC50 (half-maximal degradation concentration) and Dmax (maximal degradation) [104].
- Step 3: Ternary Complex Assessment - Validate formation of the POI:PROTAC:E3 ligase ternary complex using techniques such as:
- Surface Plasmon Resonance (SPR) to measure binding affinity and kinetics.
- Cellular Thermal Shift Assay (CETSA) to confirm target engagement in cells.
- X-ray crystallography or Cryo-EM if possible, to structurally characterize the ternary complex [104].
- Step 4: Functional Consequences - Assess phenotypic outcomes of degradation in disease-relevant cellular models (e.g., proliferation arrest, reversal of pathogenic signaling) and compare these effects to those of traditional inhibitors to distinguish degradation-specific effects from mere inhibition.
- Step 5: Selectivity Profiling - Use global proteomic analyses (e.g., TMT-based mass spectrometry) to identify off-target degradation effects and confirm the selectivity of the PROTAC for the intended target [104].
Workflow Visualization with DOT Language
Genetic-Driven Target Prioritization Workflow
AI-Guided Transcriptomic Screening Workflow
Quantitative Performance Comparison
The performance of integrated workflows can be quantitatively assessed across multiple dimensions, including genetic prediction accuracy, experimental efficiency, and clinical translation potential.
Table 2: Quantitative Performance Metrics Across Workflow Types
| Performance Metric | Genetic-Driven Workflow [100] [101] | AI-Guided Transcriptomic [103] | Direct Engagement (PROTAC) [104] |
|---|---|---|---|
| Genetic Prediction Accuracy (AUROC) | 0.95 (druggability)0.85 (DOE)0.59 (gene-disease) | Not primarily genetic | Not primarily genetic |
| Experimental Efficiency Gain | ~2.6x higher clinical success rate [100] | 13-17x improvement in recovering active compounds vs. traditional screening [103] | Enables targeting of ~80% of non-enzymes previously considered "undruggable" [104] |
| Typical Validation Timeline | 12-24 months (prior to lead optimization) | 6-12 months (candidate identification) | 3-9 months (target engagement confirmation) |
| Key Success Metrics | • Direction of Effect accuracy• Druggability prediction• Clinical success correlation | • Phenotypic rescue efficiency• Signature reversal score• Multi-target engagement | • Degradation efficiency (DC50)• Ternary complex stability• Selectivity ratio |
| Primary Application Stage | Early discovery: target selection & prioritization | Early-mid discovery: compound identification & optimization | Mid-late discovery: mechanism confirmation & lead optimization |
| Clinical Translation Rate | 73% active/successful in Phase II vs. 43% without genetic support [100] | Under evaluation (emerging technology) | High for established targets; novel targets require further validation |
These quantitative comparisons reveal a crucial trade-off: genetic-driven workflows provide superior confidence in clinical translation but require extensive population data, while AI-guided and direct engagement approaches offer substantial efficiency gains in experimental stages but with less established track records for predicting clinical outcomes [100] [101] [103]. The direction of effect prediction accuracy of 85% for genetic-driven approaches is particularly noteworthy, as incorrect determination of whether to activate or inhibit a target is a major cause of clinical failure [101].
Essential Research Reagents and Solutions
Successful implementation of integrated workflows requires specific research reagents and tools. The following table details key solutions for executing the described protocols.
Table 3: Essential Research Reagent Solutions for Integrated Validation
| Reagent/Tool Category | Specific Examples | Primary Function | Workflow Application |
|---|---|---|---|
| Genetic Databases | UK Biobank, GWAS Catalog, gnomAD, GTEx, FinnGen | Source of genetic associations, variant frequencies, and QTL data for co-localization analysis | Genetic-driven target identification [100] [102] |
| Co-localization Software | COLOC, eCAVIAR, Sum of Single Effects (SuSiE) | Statistical determination of shared causal variants between traits and diseases | Genetic-driven target identification [100] |
| scRNA-seq Platforms | 10x Genomics, Parse Biosciences | High-throughput single-cell transcriptomic profiling of compound-treated cells | AI-guided transcriptomic screening [103] |
| PROTAC Components | VHL ligands (VH032), CRBN ligands (lenalidomide), diverse linkers | Modular components for constructing bifunctional degraders with varied properties | PROTAC-based target validation [104] |
| Target Engagement Assays | Cellular Thermal Shift Assay (CETSA), Drug Affinity Responsive Target Stability (DARTS) | Confirmation of compound-target interaction in physiologically relevant cellular environments | All workflows, especially direct engagement [21] |
| Proteomic Analysis | TMT-based mass spectrometry, affinity purification + MS | Global assessment of protein level changes and degradation selectivity | PROTAC validation and off-target profiling [21] [104] |
These research solutions enable the technical execution of integrated workflows, with specific tools optimized for each validation paradigm. The selection of appropriate databases, chemical tools, and analytical methods is critical for generating robust, reproducible validation data [21] [103] [104].
Integrated workflows combining genetic and pharmacological validation represent a transformative approach to drug development. The comparative analysis presented here demonstrates that while each paradigm has distinct strengths, they share a common objective: leveraging complementary evidence streams to build stronger cases for therapeutic targets before committing substantial resources to clinical development. Genetic-driven approaches provide the foundational human evidence for disease causality, AI-guided methods efficiently identify functional compounds that reverse disease states, and direct engagement strategies offer mechanistic confirmation of target modulation.
The quantitative performance data reveals that genetic support approximately doubles the likelihood of clinical success, making it arguably the most impactful single factor in de-risking drug development [100] [101]. However, the most powerful applications likely emerge from strategic combinations of these workflows—using genetic evidence to prioritize targets, AI-guided screening to identify effective compounds, and direct engagement methods to confirm their mechanisms. As these integrated approaches mature and datasets expand, they promise to systematically address the high failure rates that have long plagued drug development, particularly in complex diseases where single-target approaches have proven insufficient.
Target validation is a critical stage in the drug discovery pipeline, serving to confirm the causal role of a specific biomolecule in a disease process and to determine whether its pharmacological modulation will provide therapeutic benefit [105] [5]. This process ensures that engaging a target has genuine potential therapeutic value; if a target cannot be validated, it will not proceed further in development [105]. High failure rates in Phase II clinical trials, often due to inadequate efficacy or safety, underscore the necessity of robust early target validation [105]. This guide objectively compares successful target validation strategies and their associated experimental protocols across two complex therapeutic areas: oncology and neuroscience.
Effective target validation relies on a multi-faceted approach integrating human data (for validation) and preclinical models (for qualification) [105]. Key components for validation using human data include tissue expression, genetics, and clinical experience, while preclinical qualification involves pharmacology, genetically engineered models, and translational endpoints [105]. The following case studies from oncology and neuroscience illustrate how these components are successfully applied using modern technologies and methodologies.
Oncology Target Validation Case Study
Multi-Cancer Early Detection (MCED) Target Validation
A prime example of large-scale clinical validation in oncology is the development of a targeted methylation-based multi-cancer early detection (MCED) test. In a pre-specified, large-scale observational study, this blood-based test validated its ability to detect cancer signals across more than 50 cancer types by analyzing cell-free DNA (cfDNA) sequencing data combined with machine learning [106].
Experimental Protocol and Key Results: The clinical validation followed a rigorous prospective case-control design (NCT02889978) [106]. The independent validation set included 4,077 participants (2,823 with cancer, 1,254 without, with non-cancer status confirmed at one-year follow-up). The core methodology involved:
- Blood Sample Collection: Drawing blood from all participants.
- cfDNA Extraction and Sequencing: Isolating cell-free DNA from plasma and performing targeted methylation sequencing.
- Machine Learning Analysis: Applying a trained algorithm to the sequencing data to identify the presence of a cancer signal and predict the tissue of origin, known as the Cancer Signal Origin (CSO).
The quantitative outcomes of this validation are summarized in the table below:
Table 1: Key Performance Metrics from the MCED Clinical Validation Study
| Metric | Result | 95% Confidence Interval |
|---|---|---|
| Specificity | 99.5% | 99.0% to 99.8% |
| Overall Sensitivity | 51.5% | 49.6% to 53.3% |
| Sensitivity by Stage (I/II/III/IV) | 16.8% / 40.4% / 77.0% / 90.1% | Stage I: 14.5-19.5% / Stage II: 36.8-44.1% / Stage III: 73.4-80.3% / Stage IV: 87.5-92.2% |
| CSO Prediction Accuracy | 88.7% | 87.0% to 90.2% |
This study demonstrated that a well-validated MCED test could function as a powerful complement to existing single-cancer screening tests, with high specificity minimizing false positives [106].
Real-World Evidence for Target Validation and Approval
Real-world evidence (RWE) is increasingly critical for validating unmet need and supporting regulatory decisions. In one oncology case study, researchers used de-identified electronic health record data to analyze treatment patterns and outcomes in patients with mantle cell lymphoma (MCL) after discontinuation of a covalent BTK inhibitor (cBTKi) [107].
The study retrospectively examined a cohort of 1,150 patients. The key findings validated a significant unmet medical need: there was considerable heterogeneity in post-cBTKi treatments, the median time to next treatment failure or death was only 3.0 months, and median overall survival from the start of the next therapy was 13.2 months [107]. This RWE successfully supported the accelerated FDA approval of a new therapy for relapsed/refractory MCL, showcasing how real-world data can validate a target population and inform regulatory strategy [107].
Neuroscience Target Validation Case Study
Sodium Channel Nav1.8 Validation in Neuropathic Pain
Neuroscience research has successfully validated specific voltage-gated sodium channels as targets for treating neuropathic pain. Investigation of gain-of-function mutations in the SCN10A gene, which encodes the Nav1.8 sodium channel, in patients with painful neuropathy revealed that these mutations alter channel physiology and kinetics, leading to hyperexcitability and spontaneous firing of dorsal root ganglion (DRG) neurons [108].
Experimental Protocol and Key Results: The validation of Nav1.8 combined human genetic evidence with detailed in vitro and in vivo models.
- Human Genetic Analysis: Identification of specific missense mutations (e.g., in the Domain II S4-S5 linker of Nav1.9) in patients with painful small fiber neuropathy [108].
- Electrophysiological Studies: Characterization of the functional consequences of these mutations in human DRG neurons, showing enhanced persistent and ramp currents that contribute to distinct, hyperexcitable firing properties [108].
- Animal Model Correlation: Studies in transgenic mouse models and other systems to confirm the role of Nav1.8 and related channels in pain pathologies.
This multi-level approach established a causal link between target modulation and disease pathology, strongly validating Nav1.8 and the related channel Nav1.9 as promising targets for analgesic therapy [108].
Novel Target Validation for Alzheimer's Disease
Another successful neuroscience validation strategy involved a novel approach to targeting Alzheimer's disease (AD) pathology. Research focused on the discovery that depolarization of synaptosomes (isolated nerve terminals) from a transgenic mouse model with the human APP gene selectively activated secretases that produced β-amyloid42, but not β-amyloid40 [105].
Experimental Protocol:
- Synaptosome Depolarization: Synaptosomes were depolarized in vitro, and the selective production of Aβ42 was measured.
- Signaling Pathway Identification: Researchers identified that an agonist for the Group II metabotropic glutamate receptor (mGluR) could mimic depolarization and selectively produce Aβ42.
- Target Modulation: Pretreatment with a Group II mGluR antagonist successfully inhibited the generation of Aβ42 in the synaptosomal model.
- In Vivo Validation: Administering two different Group II mGluR antagonists to the transgenic mouse model reduced oligomeric β-amyloid accumulation, improved learning, reduced anxiety behaviors, and increased neurogenesis [105].
This work validated the Group II mGluR pathway as a potential therapeutic target for Alzheimer's disease, leading to Phase I clinical trials for the antagonist BCI-838, which was shown to be well-tolerated in healthy controls [105].
Comparative Analysis of Validation Techniques
Methodologies and Workflows
The following diagram illustrates the core experimental workflow for functional target validation in an animal model, as exemplified by the zebrafish platform.
The workflow for the Alzheimer's disease target validation study can be summarized as follows:
Quantitative Comparison of Validation Outcomes
Table 2: Cross-Domain Comparison of Target Validation Case Studies
| Case Study | Therapeutic Area | Primary Validation Method | Key Quantitative Outcome | Translational Result |
|---|---|---|---|---|
| MCL RWE Study [107] | Oncology | Retrospective analysis of real-world data | Median OS post-cBTKi: 13.2 months; Median TTNT: 3.0 months | Supported FDA accelerated approval |
| MCED Test [106] | Oncology | Clinical validation of diagnostic (cfDNA, ML) | Sensitivity: 51.5%; Specificity: 99.5%; CSO Accuracy: 88.7% | Complement to standard cancer screening |
| Nav1.8 Channel [108] | Neuroscience | Human genetics & electrophysiology | Identification of gain-of-function mutations in patients | Strong causal link to neuropathic pain |
| Group II mGluR [105] | Neuroscience | In vitro synaptosome & transgenic mouse models | Antagonist reduced oligomeric Aβ and improved learning | Led to Phase I clinical trials (BCI-838) |
Essential Research Reagent Solutions
Table 3: Key Reagents and Platforms for Target Validation
| Research Reagent / Platform | Function in Validation | Application Context |
|---|---|---|
| CRISPR/Cas9 Gene Editing | Rapid generation of knock-out/knock-in models to assess gene function | Zebrafish F0 "Crispant" models [5]; general functional genetics |
| CETSA (Cellular Thermal Shift Assay) | Measures target engagement and binding in intact cells/tissues [7] | Confirming direct drug-target interaction in physiologically relevant systems |
| Zebrafish In Vivo Model | High-throughput phenotypic screening in a complex living organism [5] | Filtering GWAS-derived gene lists; studying neuro, cardio, and cancer biology |
| AI-Powered Literature Mining (e.g., Causaly) | Uncovers relationships between targets, pathways, and diseases from vast literature [11] | Accelerating initial hypothesis generation and evidence assessment |
| Real-World Evidence (RWD/E) Platforms | Analyzes de-identified electronic health records for treatment patterns and outcomes [107] | Understanding unmet need, validating patient population, supporting regulatory approval |
| cfDNA Methylation Sequencing | Detects and classifies cancer signals from blood-based liquid biopsies [106] | Non-invasive cancer screening and minimal residual disease monitoring |
The case studies presented herein demonstrate that successful target validation requires a convergent, multi-pronged strategy. While the specific tools differ, the underlying principle is universal: to build causal linkage from molecular target to disease phenotype using orthogonal lines of evidence.
In oncology, trends are shifting towards leveraging large-scale clinical datasets (both from trials and real-world settings) and sophisticated bioinformatic analyses for validation [106] [107]. In neuroscience, validation still heavily relies on deep mechanistic biology, often starting with human genetics and dissecting pathways in highly specific in vitro and in vivo models [108] [105]. A key emerging theme is the importance of human data (genetics, transcriptomics, clinical experience) for initial validation, followed by preclinical model systems (zebrafish, mice, synaptosome preparations) for functional qualification and pathway de-risking [105] [5].
The integration of novel AI and computational tools is accelerating this process by providing a more systematic, evidence-based view of target biology, thereby helping researchers prioritize the most promising candidates and avoid costly late-stage failures [11] [7]. Ultimately, a robust validation strategy that combines human clinical insights, advanced genetic tools, and physiologically relevant functional models across species offers the highest probability of translating a putative target into an effective therapy.
Targeted protein degradation (TPD), particularly through Proteolysis-Targeting Chimeras (PROTACs), represents a revolutionary therapeutic strategy that has fundamentally shifted the paradigm in drug discovery. Unlike conventional small-molecule inhibitors that merely block protein function, PROTACs harness the cell's own natural protein disposal systems to completely remove disease-causing proteins [109]. This innovative approach addresses critical limitations of traditional therapeutics, including drug resistance, off-target effects, and the "undruggability" of certain protein classes that lack well-defined binding pockets [110] [111].
The PROTAC technology was first conceptualized and developed by Sakamoto et al. in 2001, with the first heterobifunctional molecule designed to target methionine aminopeptidase-2 (MetAP-2) for degradation [110] [112]. These initial compounds established the foundational architecture of all PROTACs: a bifunctional molecule consisting of a ligand that binds the protein of interest (POI) connected via a chemical linker to a ligand that recruits an E3 ubiquitin ligase [113]. This design enables the PROTAC to form a ternary complex that brings the target protein into close proximity with the cellular degradation machinery, leading to ubiquitination and subsequent proteasomal destruction of the target [114].
The clinical potential of this technology is now being realized, with over 40 PROTAC drug candidates currently in clinical trials as of 2025, targeting various proteins including androgen receptor (AR), estrogen receptor (ER), Bruton's tyrosine kinase (BTK), and interleukin-1 receptor-associated kinase 4 (IRAK4) for applications spanning hematological malignancies, solid tumors, and autoimmune disorders [115]. The most advanced candidates, including ARV-471 (vepdegestrant), BMS-986365, and BGB-16673, have progressed to Phase III trials, signaling the maturing of this once-nascent technology into a promising therapeutic modality [115].
PROTACs: Mechanism of Action and Key Advantages
Molecular Mechanism of Targeted Degradation
PROTACs operate through a sophisticated hijacking of the ubiquitin-proteasome system (UPS), the primary cellular pathway for maintaining protein homeostasis by eliminating damaged or unnecessary proteins [109] [113]. The degradation process initiates when the heterobifunctional PROTAC molecule simultaneously engages both the target protein (via its warhead ligand) and an E3 ubiquitin ligase (via its recruiter ligand), forming a productive POI-PROTAC-E3 ligase ternary complex [110] [114]. This spatial repositioning is crucial, as it enables the E2 ubiquitin-conjugating enzyme, which is already charged with ubiquitin, to transfer ubiquitin molecules onto lysine residues of the target protein [109].
The ubiquitination process occurs through a well-orchestrated enzymatic cascade: first, a ubiquitin-activating enzyme (E1) activates ubiquitin in an ATP-dependent manner; next, the activated ubiquitin is transferred to a ubiquitin-conjugating enzyme (E2); finally, the E3 ligase facilitates the transfer of ubiquitin from E2 to the substrate protein [109] [111]. Once the target protein is polyubiquitinated with a chain of at least four ubiquitin molecules linked through lysine 48 (K48), it is recognized by the 26S proteasome, which unfolds the protein and degrades it into small peptide fragments [109]. Remarkably, the PROTAC molecule itself is not consumed in this process and can be recycled to catalyze multiple rounds of degradation, operating in a sub-stoichiometric or catalytic manner that often requires lower drug concentrations than traditional inhibitors [110].
Comparative Advantages Over Conventional Therapeutics
PROTAC technology offers several transformative advantages that address fundamental limitations of conventional small-molecule therapeutics. Perhaps most significantly, PROTACs act catalytically rather than stoichiometrically—a single PROTAC molecule can facilitate the degradation of multiple copies of the target protein, enabling lower dosing frequencies and reducing the potential for off-target effects associated with high drug concentrations [110]. This catalytic efficiency is particularly valuable for targeting proteins that require high inhibitor concentrations for functional suppression, as PROTACs can achieve profound pharmacological effects at substantially lower concentrations [110].
Another pivotal advantage is the ability to target proteins traditionally considered "undruggable" by conventional approaches. Many disease-relevant proteins, including transcription factors, scaffolding proteins, and regulatory proteins, lack well-defined active sites that can be effectively targeted by inhibitors [110] [111]. Since PROTACs require only binding affinity rather than functional inhibition, they can potentially target these previously inaccessible proteins. Additionally, PROTACs achieve complete ablation of all protein functions (catalytic, structural, and scaffolding), whereas inhibitors typically block only specific functions [109].
The technology also shows promise in overcoming drug resistance mechanisms that frequently limit the efficacy of targeted therapies. Resistance often develops through mutations in the drug-binding site, target protein overexpression, or activation of compensatory pathways [111]. Because PROTACs physically remove the target protein from the cell, they can potentially circumvent these resistance mechanisms, including those that arise from target overexpression or mutations outside the binding domain [110] [109]. Furthermore, the modular nature of PROTAC design allows researchers to repurpose existing inhibitors that were abandoned due to toxicity or poor pharmacokinetics by converting them into degradation warheads that may be effective at lower, better-tolerated doses [110].
Current Clinical Landscape of PROTACs
PROTACs in Advanced Clinical Development
The PROTAC clinical landscape has expanded dramatically, with multiple candidates demonstrating promising efficacy across various disease indications. The most advanced PROTACs have progressed to Phase III trials, representing significant milestones for the entire TPD field. The following table summarizes key PROTAC candidates in clinical development:
Table 1: PROTACs in Clinical Trials (2025 Update)
| Drug Candidate | Company/Sponsor | Target | Indication | Development Phase | Key Findings |
|---|---|---|---|---|---|
| Vepdegestran (ARV-471) | Arvinas/Pfizer | Estrogen Receptor (ER) | ER+/HER2- Breast Cancer | Phase III | Met primary endpoint in ESR1-mutated patients in VERITAC-2 trial; improved PFS vs. fulvestrant [115] |
| BMS-986365 (CC-94676) | Bristol Myers Squibb | Androgen Receptor (AR) | mCRPC | Phase III | First AR-targeting PROTAC in Phase III; 55% PSA30 response at 900 mg BID in Phase I [115] |
| BGB-16673 | BeiGene | BTK | R/R B-Cell Malignancies | Phase III | BTK-degrading PROTAC; shows activity in resistant malignancies [115] |
| ARV-110 | Arvinas | Androgen Receptor (AR) | mCRPC | Phase II | First PROTAC to enter clinical trials; demonstrated tumor regression in patients with AR T878X/H875Y mutations [115] |
| KT-253 | Kymera | MDM2 | Liquid and Solid Tumors | Phase I | Potent MDM2-based PROTAC; >200-fold more potent than traditional MDM2 inhibitors [111] |
| NX-2127 | Nurix | BTK, IKZF1/3 | R/R B-Cell Malignancies | Phase I | Dual degrader of BTK and transcription factors Ikaros (IKZF1) and Aiolos (IKZF3) [115] |
The clinical progress of these candidates demonstrates the therapeutic potential of PROTAC technology across diverse disease areas, particularly in oncology. ARV-471 (vepdegestrant) has emerged as a leading candidate, with the Phase III VERITAC-2 trial showing statistically significant and clinically meaningful improvement in progression-free survival (PFS) compared to fulvestrant in patients with ESR1 mutations, though it did not reach statistical significance in the overall intent-to-treat population [115]. This highlights both the promise and complexities of PROTAC therapies, suggesting potential biomarker-defined patient populations that may derive particular benefit.
Analysis of Clinical Trial Outcomes
The growing body of clinical data provides important insights into the real-world performance of PROTAC therapeutics. Earlier-stage clinical results have demonstrated proof-of-concept for the PROTAC mechanism in humans. For instance, ARV-110, the first PROTAC to enter clinical trials, showed promising activity in patients with metastatic castration-resistant prostate cancer (mCRPC) who had progressed on multiple prior therapies, including novel hormonal agents [112] [113]. Importantly, tumor regression was observed in patients whose tumors harbored specific AR mutations (T878X/H875Y), providing early evidence that PROTACs can effectively target mutated proteins that often drive resistance to conventional therapies [115].
The clinical development of PROTACs has also revealed some challenges unique to this modality. The "hook effect"—where high concentrations of PROTAC lead to self-competition and reduced efficacy due to formation of non-productive binary complexes—has been observed in clinical settings and necessitates careful dose optimization [110] [111]. Additionally, the relatively high molecular weight and structural complexity of PROTACs present formulation challenges that must be addressed to ensure adequate oral bioavailability, though several candidates including ARV-471 and ARV-110 have demonstrated successful oral administration in clinical trials [115].
Despite these challenges, the favorable safety profiles observed with several PROTAC candidates in early-phase trials have been encouraging. The catalytic mechanism of action allows for intermittent dosing strategies that may reduce cumulative exposure while maintaining efficacy. As the field advances, later-stage trials will be crucial for establishing the long-term safety and definitive efficacy of PROTAC therapeutics across broader patient populations.
Experimental Framework for PROTAC Development
PROTAC Design and Optimization Workflow
The development of effective PROTAC degraders follows a systematic workflow that integrates structural biology, medicinal chemistry, and cellular validation. The process begins with comprehensive target assessment and ligand selection, proceeds through rational design and synthesis, and culminates in rigorous mechanistic validation. The following diagram illustrates this iterative development process:
The initial phase involves thorough evaluation of the target protein and available binders. Researchers must assess the target's "degradability" by examining factors such as solvent-accessible lysine residues (potential ubiquitination sites) and protein turnover rates [114]. Publicly available databases like PROTACpedia and PROTAC-DB provide valuable information on existing degraders and their characteristics, while computational tools like Model-based Analysis of Protein Degradability (MAPD) can predict target suitability for TPD approaches [114]. Simultaneously, suitable ligands for both the target protein and E3 ligase must be identified through databases such as ChEMBL, BindingDB, and DrugBank, which compile ligand-protein interaction data from diverse sources [114].
The design phase focuses on assembling the three PROTAC components: the POI-binding warhead, the E3 ligase recruiter, and the connecting linker. While warheads are typically derived from known inhibitors or binders of the target protein, they need not possess intrinsic inhibitory activity—even silent binders or imaging agents can be effective in PROTAC format [114]. The selection of E3 ligase recruiter is equally critical, with most current PROTACs utilizing ligands for CRBN, VHL, MDM2, or IAP E3 ligases, though efforts to expand the E3 ligase toolbox are ongoing [111] [114]. Linker design represents a key optimization parameter, as linker length, composition, and rigidity significantly impact ternary complex formation, degradation efficiency, and physicochemical properties [114]. Initial linker strategies often employ simple hydrocarbon or polyethylene glycol (PEG) chains of varying lengths, with subsequent optimization informed by structural data and structure-activity relationships.
Key Validation Experiments and Methodologies
Rigorous mechanistic validation is essential to confirm that observed protein loss results from genuine PROTAC-mediated degradation rather than alternative mechanisms. A comprehensive validation workflow includes multiple orthogonal assays:
Table 2: Essential Validation Experiments for PROTAC Development
| Validation Method | Experimental Approach | Key Outcome Measures | Interpretation |
|---|---|---|---|
| Cellular Degradation Assays | Western blot, immunofluorescence, cellular thermal shift assay (CETSA) | DC50 (half-maximal degradation), Dmax (maximal degradation), degradation kinetics | Confirms target protein loss and establishes degradation potency [114] |
| Ternary Complex Formation | Isothermal titration calorimetry (ITC), surface plasmon resonance (SPR), competitive fluorescence polarization | Binding affinity, cooperativity factor (α) | Demonstrates formation of productive POI-PROTAC-E3 complex [114] |
| Mechanism Confirmation | Proteasome inhibition (MG132, bortezomib), E1 ubiquitination inhibition (MLN4924), NEDD8 pathway inhibition | Rescue of protein degradation | Confirms ubiquitin-proteasome system dependence [114] |
| Selectivity Profiling | Global proteomics (TMT, SILAC), kinase profiling panels | Changes in global proteome, selectivity ratios | Identifies on-target vs. off-target degradation effects [114] |
| Hook Effect Assessment | Dose-response curves at high PROTAC concentrations | Biphasic degradation response | Characterizes self-inhibition at high concentrations [110] |
Cellular degradation assays represent the first critical validation step, typically employing Western blotting or immunofluorescence to quantify target protein levels after PROTAC treatment. These experiments establish fundamental parameters including DC50 (concentration achieving 50% degradation), Dmax (maximal degradation achieved), and the time course of degradation [114]. The catalytic nature of PROTAC action often results in sub-stoichiometric activity, with significant degradation occurring at concentrations lower than required for inhibition by the warhead alone.
Mechanistic confirmation experiments are crucial to verify that protein loss occurs specifically through the ubiquitin-proteasome pathway. Treatment with proteasome inhibitors (e.g., MG132, bortezomib) should rescue degradation, while inhibition of the NEDD8 pathway (which activates cullin-RING E3 ligases) or the E1 ubiquitin-activating enzyme should similarly block PROTAC activity [114]. Additionally, assessment of the "hook effect"—where degradation efficiency decreases at high PROTAC concentrations due to formation of non-productive binary complexes—provides important mechanistic validation and practical guidance for dosing in subsequent experiments [110].
Global proteomic analyses offer comprehensive assessment of PROTAC selectivity by quantifying changes across the entire proteome. Techniques such as tandem mass tag (TMT) multiplexing or stable isotope labeling with amino acids in cell culture (SILAC) can identify off-target degradation events and validate target specificity [114]. For kinase-targeting PROTACs, specialized kinase profiling panels may provide additional selectivity assessment. Together, these validation experiments build a compelling case for true PROTAC-mediated degradation and inform subsequent optimization cycles.
The Scientist's Toolkit: Essential Research Reagents
The successful development and validation of PROTAC degraders relies on a comprehensive toolkit of specialized reagents and methodologies. The table below outlines essential resources for PROTAC research:
Table 3: Essential Research Reagents for PROTAC Development
| Reagent Category | Specific Examples | Function/Purpose | Key Applications |
|---|---|---|---|
| E3 Ligase Ligands | Thalidomide derivatives (CRBN), VH032 (VHL), Nutlin-3 (MDM2), Bestatin/MV1 (IAP) | Recruit specific E3 ubiquitin ligases to enable target ubiquitination | Core component of PROTAC molecules; determines tissue specificity and efficiency [111] [114] |
| Mechanistic Probes | MG132, Bortezomib (proteasome inhibitors), MLN4924 (NEDD8 activation inhibitor) | Confirm ubiquitin-proteasome system dependence | Validation that degradation occurs via intended mechanism [114] |
| Public Databases | PROTAC-DB, PROTACpedia, ChEMBL, BindingDB, DrugBank | Access existing degrader designs and ligand-protein interaction data | Initial design phase; survey existing degraders and identify potential ligands [114] |
| Linker Libraries | Polyethylene glycol (PEG) chains, alkyl chains, conformationally constrained linkers | Connect warhead and E3 ligand; optimize molecular orientation and properties | Ternary complex formation; improve physicochemical properties and degradation efficiency [114] |
| Proteomics Resources | Global proteomics databases (e.g., Fischer lab portal), MAPD predictive model | Assess target degradability and selectivity profiles | Predict target suitability for TPD; identify off-target effects [114] |
This toolkit enables researchers to navigate the complex process of PROTAC development, from initial design to mechanistic validation. Publicly accessible databases are particularly valuable for newcomers to the field, providing curated information on existing degraders, ligand interactions, and predictive models of target degradability [114]. The expanding repertoire of E3 ligase ligands continues to broaden the scope of PROTAC applications, while specialized mechanistic probes remain essential for confirming the intended mode of action.
As the field advances, additional resources are emerging to support PROTAC development, including computational modeling tools for predicting ternary complex formation, structural biology resources providing atomic-level insights into productive PROTAC interactions, and specialized screening platforms for high-throughput assessment of degrader efficiency. Together, these resources empower researchers to design, optimize, and validate novel PROTAC molecules with increasing efficiency and success.
Digital Twins: Enhancing Targeted Degradation Research
Conceptual Framework and Applications
Digital twins (DTs) represent a transformative approach in biomedical research, creating virtual representations of physical entities—from individual cells to entire human populations—that enable in silico simulations and experiments [116] [117]. In the context of PROTAC development and targeted protein degradation research, DTs offer powerful capabilities to accelerate discovery, optimize clinical translation, and reduce experimental burden. These AI-generated models integrate diverse data sources—including genomic profiles, protein expression data, clinical parameters, and real-world evidence—to create dynamic, patient-specific simulations that predict responses to interventions [116].
The application framework for DTs in drug development spans multiple stages. In early discovery, DTs can model disease mechanisms and identify potential therapeutic targets by simulating the biological processes involved in pathology [116]. During preclinical development, DTs create virtual cohorts that mirror real-world population diversity, enabling researchers to simulate clinical trials, optimize dosing regimens, and predict potential adverse events before human testing [116] [117]. In clinical development, DTs can serve as synthetic control arms, reducing the number of patients receiving placebo while maintaining statistical power, and enabling more efficient trial designs [116]. The following diagram illustrates the operational framework for DT-enhanced clinical trials:
The integration of DTs in PROTAC development is particularly valuable given the complex, catalytic mechanism of action and potential for tissue-specific effects based on E3 ligase expression patterns. DT simulations can help predict how PROTAC efficacy might vary across patient subpopulations with different genetic backgrounds, protein expression profiles, or comorbidities, enabling more targeted clinical development strategies [116]. Furthermore, DTs can model the hook effect and other nonlinear pharmacokinetic phenomena characteristic of PROTACs, informing dose selection and scheduling decisions before costly clinical experiments [110] [116].
Implementation in Drug Development and Clinical Trials
The practical implementation of DTs in pharmaceutical research and development follows a structured process that leverages artificial intelligence and machine learning technologies. The first step involves comprehensive data collection and integration from multiple sources, including electronic health records (EHRs), genomic databases, biomarker data, and historical clinical trial datasets [116]. These diverse data streams are then processed using generative AI and deep learning algorithms to create virtual patient cohorts that accurately reflect the statistical distributions and correlations present in real-world populations [116] [118].
Once virtual cohorts are established, researchers can simulate clinical trials by applying the expected biological effects of investigational PROTACs—inferred from preclinical data and early clinical results—to predict patient responses, identify potential safety signals, and optimize trial parameters such as sample size, enrollment criteria, and endpoint selection [116]. The continuous refinement of these models through comparison with real-world outcomes creates an iterative learning loop that improves predictive accuracy over time [116] [117].
Notable examples of DT implementation are already emerging in clinical research. The inEurHeart trial, a multicenter randomized controlled trial launched in 2022, enrolled 112 patients to compare AI-guided ventricular tachycardia ablation planned on a cardiac digital twin with standard catheter techniques [116]. Early results demonstrated 60% shorter procedure times and a 15% absolute increase in acute success rates, illustrating the potential of DT approaches to significantly improve therapeutic outcomes [116]. While PROTAC-specific DT applications are still in earlier stages of development, the principles demonstrated in these pioneering trials provide a template for how DTs might enhance the development of targeted protein degraders.
The combination of DTs with PROTAC technology holds particular promise for personalized medicine applications. By creating patient-specific models that incorporate individual E3 ligase expression patterns, proteasome activity, and target protein dependencies, researchers could potentially predict which patients are most likely to respond to specific PROTAC therapies, optimizing treatment selection and sequencing [116] [117]. As both technologies continue to mature, their integration is expected to play an increasingly important role in advancing precision medicine and reducing the time and cost of drug development.
Comparative Analysis and Future Directions
Technology Comparison and Synergies
PROTACs and digital twins represent complementary technological advances with distinct yet synergistic capabilities in drug discovery and development. The following comparative analysis highlights their respective strengths and potential integration points:
Table 4: Comparative Analysis of PROTACs and Digital Twins in Drug Development
| Parameter | PROTAC Technology | Digital Twin Technology | Synergistic Potential |
|---|---|---|---|
| Primary Function | Induces degradation of disease-causing proteins | Creates virtual patient models for simulation and prediction | DT models can predict PROTAC efficacy/toxicity across populations |
| Key Advantage | Targets "undruggable" proteins; catalytic activity | Reduces clinical trial burden; enables personalized forecasting | Optimizes PROTAC clinical trial design and patient stratification |
| Development Stage | Multiple candidates in Phase III trials | Emerging applications in clinical research | Early stage but rapidly evolving integration |
| Technical Challenges | Hook effect; pharmacokinetic optimization | Model validation; data quality and integration | Combined approaches could address both mechanistic and clinical challenges |
| Regulatory Status | Advanced clinical programs; regulatory pathways emerging | Regulatory frameworks under development (FDA discussions) | Co-development of regulatory standards for combined approaches |
The integration of these technologies creates powerful synergies that can accelerate and de-risk the drug development process. Digital twins can leverage proteomic and genomic data to predict which targets are most amenable to degradation approaches, guiding initial PROTAC development decisions [116] [114]. During optimization, DT simulations can model how variations in linker composition, E3 ligase selection, and warhead properties might influence degradation efficiency across different cellular contexts, prioritizing the most promising candidates for synthesis and testing [116] [117]. In clinical development, virtual trials using digital twins can optimize PROTAC dosing regimens, predict potential adverse events, and identify patient subpopulations most likely to respond, enabling more efficient and targeted clinical programs [116].
This integrated approach is particularly valuable for addressing the complex pharmacological behavior of PROTACs, including their catalytic mechanism, potential hook effects, and tissue-specific activity based on E3 ligase expression patterns [110] [116]. Digital twins can incorporate these nonlinear relationships into patient models, generating more accurate predictions of real-world PROTAC performance than traditional pharmacokinetic/pharmacodynamic modeling approaches. Furthermore, as real-world evidence accumulates from PROTAC clinical trials, these data can continuously refine and validate digital twin models, creating a virtuous cycle of improvement for both technologies.
Future Perspectives and Challenges
The continued advancement of PROTAC and digital twin technologies faces both exciting opportunities and significant challenges. For PROTACs, key priorities include expanding the repertoire of available E3 ligase ligands beyond the current focus on CRBN, VHL, MDM2, and IAP ligases [111] [114]. With over 600 E3 ligases in the human genome, tapping into a broader range of these enzymes could enable tissue-specific targeting and reduce potential resistance mechanisms [110] [111]. Additionally, overcoming delivery challenges—particularly for targets requiring blood-brain barrier penetration—represents a critical frontier for expanding PROTAC applications to neurological disorders [112].
Digital twin technology must address challenges related to model validation, data quality, and regulatory acceptance [116] [118]. Establishing standardized frameworks for verifying and validating digital twin predictions will be essential for regulatory endorsement and clinical adoption. Furthermore, ensuring that the data used to generate digital twins represents diverse populations is crucial to avoid perpetuating health disparities and to ensure equitable benefits from these advanced technologies [116].
The convergence of PROTACs with emerging targeted degradation modalities—including molecular glues, lysosome-targeting chimeras (LYTACs), and antibody-based PROTACs (AbTACs)—promises to further expand the scope of addressable targets [109] [111]. Molecular glues, in particular, represent a complementary approach to PROTACs that often feature more favorable drug-like properties, though their discovery remains largely serendipitous [109] [111]. As rational design strategies for molecular glues improve, they may provide alternative pathways to targeting challenging proteins.
Looking ahead, the integration of artificial intelligence and machine learning across both PROTAC development and digital twin creation is expected to dramatically accelerate progress [114] [118]. AI-driven predictive models for ternary complex formation, degradation efficiency, and selectivity could streamline PROTAC design, while generative AI approaches for digital twin creation could enable more sophisticated and accurate patient simulations [118]. As these technologies mature and converge, they hold the potential to transform drug discovery from a largely empirical process to a more predictive and precision-guided endeavor, ultimately delivering better therapies to patients faster and more efficiently.
Conclusion
Effective target validation is not a single experiment but a multi-faceted, iterative process that requires converging evidence from complementary techniques. A robust validation strategy, which proactively addresses pitfalls like off-target effects and incorporates rescue experiments, is fundamental to derisking drug development. The future of target validation lies in the intelligent integration of established methods with cutting-edge technologies—including AI-powered prediction models, advanced assays for direct target engagement like CETSA, and novel modalities like PROTACs. By adopting a rigorous and comprehensive approach to validation, researchers can significantly increase the likelihood of clinical success, ultimately delivering safer and more effective medicines to patients.
References
- 1. Target Validation [https://www.sygnaturediscovery.com/drug-discovery/integrated-drug-discovery/target-validation/]
- 2. AI in Drug Discovery 2025: Accelerating Pharma Innovation [https://kanerika.com/blogs/ai-in-drug-discovery/]
- 3. A precise comparison of molecular target prediction methods [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d5dd00199d]
- 4. Validation strategies for target prediction methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC7299289/]
- 5. Target Validation with Zebrafish in Drug Discovery [https://www.zeclinics.com/blog/target-validation-drug-discovery-zebrafish]
- 6. Announcing the 2025 In Vivo Target Validation Grantees [https://www.targetals.org/2025/07/16/announcing-the-2025-in-vivo-target-validation-grantees/]
- 7. Top 5 Drug Discovery Trends 2025 Driving Breakthroughs [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/drug-discovery-trends-2025/]
- 8. Evaluation Metrics for ML Models in Drug Discovery [https://www.elucidata.io/blog/evaluation-metrics-for-ml-models-in-drug-discovery]
- 9. Why clinical trials fail - top reasons overviewed [https://clinicaltrialrisk.org/clinical-trial-design/why-clinical-trials-fail-top-reasons-overviewed/]
- 10. Principles of early drug discovery - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3058157/]
- 11. How a scientist accelerates target validation with Causaly [https://www.causaly.com/case-studies/from-complexity-to-clarity-how-a-scientist-accelerates-target-validation-with-causaly]
- 12. Automated drug design for druggable target identification ... [https://www.nature.com/articles/s41598-025-18091-x]
- 13. How to choose a disease-fighting molecule - C&EN [https://cen.acs.org/pharmaceuticals/drug-discovery/choose-disease-fighting-molecule/103/web/2025/04]
- 14. Large language models for drug discovery and development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12546459/]
- 15. Evaluating ligand docking methods for drugging protein ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-01067-4]
- 16. Recent advances in molecular representation methods and ... [https://www.nature.com/articles/s44386-025-00017-2]
- 17. Editorial: Real-World Outcomes of Disease-Modifying ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12499630/]
- 18. Annovis Announces Novel Biomarker Data in Alzheimer's ... [https://www.annovisbio.com/press-release/annovis-announces-novel-biomarker-data-in-alzheimers-patients-supporting-buntanetaps-potential-as-a-disease-modifying-treatment]
- 19. September 2025: This Month in Huntington's Disease ... [https://en.hdbuzz.net/september-2025-this-month-in-huntingtons-disease-research/]
- 20. What's the Difference Between Target Identification and ... [https://www.infinixbio.com/blog/target-identification-vs-validation/]
- 21. Recent advances in target identification technology of ... [https://www.sciencedirect.com/science/article/abs/pii/S0163725825000452]
- 22. The Deconvolution Revolution: Strategies for Target ... [https://momentum.bio/content/the-deconvolution-revolution-strategies-for-target-identification/]
- 23. Beyond Legacy Tools: Defining Modern AI Drug Discovery ... [https://www.biopharmatrend.com/business-intelligence/what-is-ai-drug-discovery/]
- 24. AI-Based Pharmaceutical R&D Services Market on a High- ... [https://finance.yahoo.com/news/ai-based-pharmaceutical-r-d-150000344.html]
- 25. Artificial intelligence revolution in drug discovery [https://www.sciencedirect.com/science/article/pii/S037851732500626X]
- 26. Artificial Intelligence in Small-Molecule Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472608/]
- 27. RNAi vs. CRISPR: Guide to Selecting the Best Gene ... [https://www.synthego.com/blog/rnai-vs-crispr-guide/]
- 28. Will CRISPR Cut Out the Competition or Can RNAi Help ... [https://www.sciencedirect.com/science/article/pii/S2472555222072720]
- 29. Gene Knockdown vs. Knockout: RNAi vs. CRISPR ... [https://synapse.patsnap.com/article/gene-knockdown-vs-knockout-rnai-vs-crispr-approaches]
- 30. CRISPR Knockout (KO) Cell Pools: Approach to Study ... [https://www.ubigene.us/application/knockout-cell-pool-gene-function-study.html]
- 31. CRISPR vs RNAi: Why CRISPR Excels in Genetic Research [https://www.ubigene.us/application/crispr-gene-editing.html]
- 32. State of CRISPR Gene Editing in the Drug Discovery Sector [https://www.synthego.com/blog/survey-report-crispr-therapeutics/]
- 33. Systematic comparison of CRISPR-Cas9 and RNAi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4900911/]
- 34. Optimization of gene knockout approaches and sgRNA ... [https://www.nature.com/articles/s41598-025-24184-4]
- 35. The era of high-quality chemical probes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9749956/]
- 36. Supporting scientists to choose the best chemical probes [https://www.icr.ac.uk/about-us/icr-news/detail/supporting-scientists-to-choose-the-best-chemical-probes]
- 37. Welcome to the Chemical Probes Portal [https://www.chemicalprobes.org/]
- 38. or VHL-binder using AirID [https://www.nature.com/articles/s42003-025-08761-x]
- 39. Thermal shift assays in drug discovery [https://www.sciencedirect.com/science/article/abs/pii/S1056871925008007]
- 40. DARTS vs CETSA: Choosing the Right Assay for Target ... [https://www.creative-proteomics.com/resource/darts-vs-cetsa-choosing-the-right-assay-for-target-validation.htm]
- 41. Applications of the Cellular Thermal Shift Assay to Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12072176/]
- 42. Current Advances in CETSA [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2022.866764/full]
- 43. Applications of the Cellular Thermal Shift Assay to Drug ... [https://pubmed.ncbi.nlm.nih.gov/40362180/]
- 44. Comparative Analysis of Biochemical and Cellular Assay ... [https://www.mdpi.com/1420-3049/30/17/3630]
- 45. CETSA®: Measuring Target Engagement in Whole Blood [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/cetsa-engagement-whole-blood/]
- 46. A robust CETSA data analysis automation workflow for ... [https://www.sciencedirect.com/science/article/pii/S2472555224000340]
- 47. Halfway between 2D and Animal Models: Are 3D Cultures ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5796130/]
- 48. A comprehensive review on 3D tissue models [https://www.sciencedirect.com/science/article/abs/pii/S0142961223004167]
- 49. Three-Dimensional Cell Cultures: The Bridge between In Vitro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10419178/]
- 50. Personalized and genetically engineered animal models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577965/]
- 51. Innovative Human Three-Dimensional Tissue-Engineered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7552665/]
- 52. 3D Cell Cultures are Better than Animal Models - Here´s Why! [https://focus.gbo.com/blog/3d/advantages-of-3d-cell-culture-over-animal-models-greiner-bio-one]
- 53. Blog: Refining Biomedical Research Beyond Animal Models [https://celvivo.com/blog-refining-biomedical-research-beyond-animal-models/]
- 54. Comparative analysis of 3D-culture techniques for ... [https://www.nature.com/articles/s41598-025-13588-x]
- 55. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 56. Target Identification and Validation in Drug Discovery [https://www.pharmidex.com/pharmidex-is-proud-to-sponsor-the-smr-meeting-target-identification-and-validation-in-drug-discovery]
- 57. Target identification [https://bostongene.com/biopharma/target-analysis]
- 58. Why is Biomarker Assay Validation Different from that of ... [https://link.springer.com/article/10.1208/s12248-025-01135-5]
- 59. Biomarker Validation Guide 2025: Discovery to FDA Approval [https://www.motif.bio/blog/biomarker-discovery-validation-guide-2025]
- 60. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 61. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 62. Transforming Drug Target Discovery ... [https://insilico.com/tpost/v49bfcu0r1-transforming-drug-target-discovery-insil]
- 63. In Vitro vs. In Vivo vs. In Silico: Preclinical Assay Differences [https://www.zeclinics.com/blog/differences-between-in-vitro-in-vivo-and-in-silico-assays-in-preclinical-research]
- 64. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 65. In Silico Models in Oncology: Validating AI-Driven ... [https://blog.crownbio.com/in-silico-models-in-oncology-validating-ai-driven-predictive-frameworks]
- 66. A Comparison of AI and Population PK Models to Predict the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547357/]
- 67. Comparison of In Vitro and In Silico Assessments ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9910814/]
- 68. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 69. Classification of and detection techniques for RNAi ... [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2025.1535384/full]
- 70. A simple validation and screening method for CRISPR/Cas9 ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0312722]
- 71. CRISPR screening redefines therapeutic target ... [https://www.sciencedirect.com/science/article/pii/S2095177925001741]
- 72. CMN Weekly (31 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-31-october-2025-your-weekly-crispr-medicine-news/]
- 73. CMN Weekly (3 October 2025) - Your ... [https://crisprmedicinenews.com/news/cmn-weekly-3-october-2025-your-weekly-crispr-medicine-news/]
- 74. Target gene screening and validation for RNAi-based ... [https://chembioagro.springeropen.com/articles/10.1186/s40538-025-00831-w]
- 75. RNA-Targeting Techniques: A Comparative Analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563179/]
- 76. Design of highly functional genome editors by modelling ... [https://www.nature.com/articles/s41586-025-09298-z]
- 77. Fail Early, Fail Fast - A phenotypic rescue approach [https://www.ddw-online.com/fail-early-fail-fast-a-phenotypic-rescue-approach-794-201908/]
- 78. Drug discovery and development: introduction to the ... [https://www.frontiersin.org/journals/drug-discovery/articles/10.3389/fddsv.2023.1201419/full]
- 79. Identification of Targets from LRRK2 Rescue Phenotypes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7824855/]
- 80. Validation approaches for computational drug repurposing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10785886/]
- 81. Cross Validation in Machine Learning [https://www.geeksforgeeks.org/machine-learning/cross-validation-machine-learning/]
- 82. Experimental and statistical approaches in method cross ... [https://www.sciencedirect.com/science/article/abs/pii/S073170850800647X]
- 83. A step by step guide to quantitative comparisons in ... [https://finbiosoft.com/a-step-by-step-guide-to-quantitative-comparisons-in-validation-manager/]
- 84. Model Validation Techniques, Explained: A Visual Guide ... [https://towardsdatascience.com/model-validation-techniques-explained-a-visual-guide-with-code-examples-eb13bbdc8f88/]
- 85. Biochemical Assay Development: Strategies to Speed Up ... [https://bellbrooklabs.com/accelerate-biochemical-assay-development/?srsltid=AfmBOopmu3r25PqK2oXXc_MluO850fSzT2H5HX_zCLMHwOsFLtkpBtHp]
- 86. What Is Data Interpretation? Methods, Tools, & Examples in ... [https://julius.ai/articles/data-interpretation]
- 87. Presentation of Quantitative Data [https://ihatepsm.com/blog/presentation-quantitative-data]
- 88. Visual Best Practices [https://help.tableau.com/current/blueprint/en-us/bp_visual_best_practices.htm]
- 89. The CRISPR therapeutics landscape in 2025 [https://www.kilburnstrode.com/knowledge/european-ip/the-crispr-therapeutics-landscape-in-2025]
- 90. CRISPR and RNA interference: revolutionary tools for ... [https://www.frontiersin.org/journals/food-science-and-technology/articles/10.3389/frfst.2025.1609948/full]
- 91. Evaluation of RNAi and CRISPR technologies by large-scale ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.2003213]
- 92. Importance of Target Identification & Validation in Drug ... [https://lifesciences.danaher.com/us/en/library/target-identification-validation-drug-discovery.html]
- 93. Key role of publication of clinical data for target validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC4520621/]
- 94. Improving target assessment in biomedical research [https://www.nature.com/articles/s41573-020-0087-3]
- 95. The Art of Finding the Right Drug Target: Emerging Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11334170/]
- 96. Target Identification and Validation in Drug Development [https://www.technologynetworks.com/drug-discovery/articles/target-identification-and-validation-in-drug-development-366706]
- 97. Large-scale comparison of machine learning methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6011237/]
- 98. CRISPR 临床试验:2025 年更新- 创新基因组学研究所(IGI) [https://innovativegenomics.org/zh-CN/%E6%96%B0%E9%97%BB/Crispr-%E4%B8%B4%E5%BA%8A%E8%AF%95%E9%AA%8C-2025/]
- 99. Targeted validation: validating clinical prediction models in ... [https://diagnprognres.biomedcentral.com/articles/10.1186/s41512-022-00136-8]
- 100. Genetic-Driven Druggable Target Identification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6088790/]
- 101. Genetic evidence informs the direction of therapeutic ... [https://www.nature.com/articles/s44386-025-00027-0]
- 102. Prioritising genetic findings for drug target identification ... [https://www.sciencedirect.com/science/article/pii/S0021915024000224]
- 103. How AI and cell data combine to make drug discovery faster [https://www.drugtargetreview.com/news/189880/how-ai-and-cell-data-combine-to-make-drug-discovery-faster/]
- 104. Advancing target validation with PROTAC technology [https://pubmed.ncbi.nlm.nih.gov/40188374/]
- 105. Target Validation - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK195039/]
- 106. Clinical validation of a targeted methylation-based multi-cancer early... [https://pubmed.ncbi.nlm.nih.gov/34176681/]
- 107. Oncology case studies: How two life sciences companies ... [https://resources.flatiron.com/real-world-evidence/oncology-case-studies-real-world-evidence]
- 108. New Target Identification for Nervous System Repair [https://medicine.yale.edu/cnrr/research/nervous-system/]
- 109. Targeted protein degradation: mechanisms, strategies and ... [https://www.nature.com/articles/s41392-022-00966-4]
- 110. PROTAC 2.0: Expanding the frontiers of targeted protein ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644625000893]
- 111. Targeted protein degradation: advances in drug discovery ... [https://www.nature.com/articles/s41392-024-02004-x]
- 112. PROTAC targeted protein degraders: the past is prologue [https://www.nature.com/articles/s41573-021-00371-6]
- 113. An overview of PROTACs: a promising drug discovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9763089/]
- 114. Targeted Protein Degradation: Design Considerations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9729011/]
- 115. PROTAC Degraders in Clinical Trails: 2025 Update [https://www.biochempeg.com/article/434.html]
- 116. Enhancing randomized clinical trials with digital twins [https://www.nature.com/articles/s41540-025-00592-0]
- 117. Transformative roles of digital twins from drug discovery to ... [https://www.sciencedirect.com/science/article/pii/S2590156725000945]
- 118. Generative artificial intelligence empowers digital twins in ... [https://pubmed.ncbi.nlm.nih.gov/37887266/]