Target Product Profile vs. Actual Profile: A Strategic Framework for Drug Development Success
This article provides a comprehensive analysis of the Target Product Profile (TPP) as a strategic tool in drug development, contrasting its intended role with the realities of its application and...
Target Product Profile vs. Actual Profile: A Strategic Framework for Drug Development Success
Abstract
This article provides a comprehensive analysis of the Target Product Profile (TPP) as a strategic tool in drug development, contrasting its intended role with the realities of its application and the resulting 'Actual Profile.' Aimed at researchers, scientists, and drug development professionals, it explores the foundational principles of TPPs, methodologies for their effective creation and use, strategies for troubleshooting common pitfalls, and frameworks for validating and comparing the TPP against final outcomes. By synthesizing current research and industry insights, this guide aims to equip professionals with the knowledge to bridge the gap between strategic planning and execution, thereby enhancing development efficiency, regulatory success, and commercial viability.
What is a Target Product Profile? Defining Your Strategic Compass
In drug development, the Target Product Profile (TPP) serves as a strategic blueprint that outlines the desired characteristics of a final product. It embodies the principle of "beginning with the end goal in mind," guiding research and development from discovery through regulatory approval and commercialization [1]. This guide compares the intended goals defined in a TPP with the actual performance data of a developed product, providing a framework for researchers and developers to objectively assess development success.
Defining the Target Product Profile
A Target Product Profile (TPP) is a strategic development process tool that summarizes the key attributes of an intended commercial product. It acts as a planning tool to focus development activities on a clearly articulated set of goals [2] [1].
The World Health Organization (WHO) describes a TPP as a document that outlines the desired characteristics of a product aimed at a particular disease. It specifies the intended use, target populations, and other desired product attributes, including safety and efficacy-related characteristics [3]. WHO TPPs often describe both a preferred profile and a minimally acceptable profile for vaccines, therapeutics, diagnostics, or medical devices [3].
In industry, a well-designed TPP provides a framework for development candidates, typically structured with minimally acceptable targets and "stretch" goals. Failure to meet the "essential" parameters often leads to program termination, while meeting the "ideal" profile increases the product's value [2].
Table: Core Components of a Target Product Profile
| TPP Component | Description | Strategic Importance |
|---|---|---|
| Target Population | Defines the specific patient cohort with an unmet medical need [2]. | Guides clinical trial design and patient recruitment strategies. |
| Indication & Context of Use | Specifies the intended disease and clinical use case [4]. | Determines regulatory pathway and labeling claims. |
| Efficacy Endpoints | Outlines primary and secondary efficacy measures for Phase III trials [2]. | Serves as key benchmarks for regulatory success. |
| Safety Profile | Defines the required safety parameters and differentiation from standard of care [2]. | Establishes the product's benefit-risk profile. |
| Dosage & Administration | Details proposed route, schedule, and formulation [2]. | Impacts patient compliance and commercial potential. |
| Shelf Life & Stability | Specifies required product storage conditions and longevity [4]. | Critical for manufacturing, distribution, and market access. |
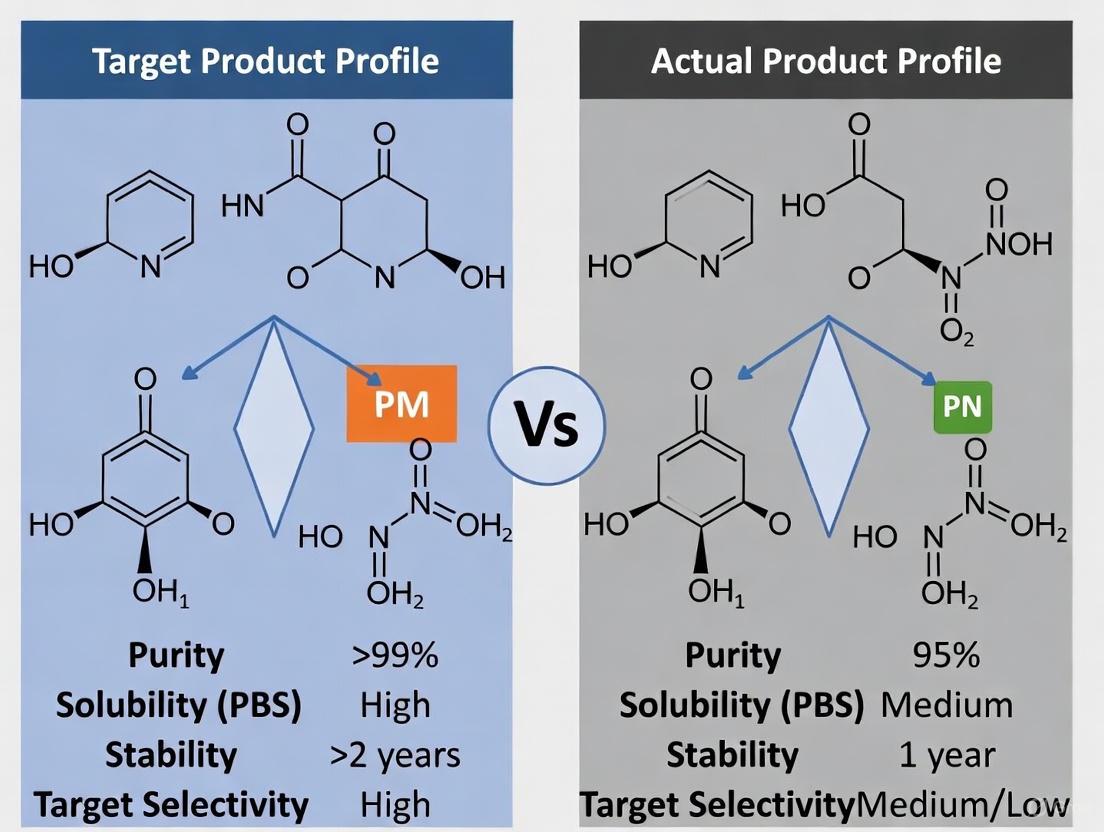
TPP vs. Actual Profile: A Quantitative Framework for Comparison
The true test of a development program's success lies in systematically comparing the Target Product Profile against the Actual Product Profile derived from experimental and clinical data. This comparison objectively measures how well the final product met its initial development goals.
Table: TPP vs. Actual Profile: Efficacy and Safety Comparison
| Performance Attribute | Target Profile (Goal) | Actual Profile (Experimental Data) | Variance Analysis |
|---|---|---|---|
| Primary Efficacy Endpoint | ≥15% improvement over standard of care (SOC) in disease-specific score [2]. | 12% improvement over SOC (p<0.05) from Phase III trial (N=450). | Marginally Missed: Statistically significant but below target delta. |
| Key Safety Metric | Incidence of severe adverse events (SAEs) <5% [2]. | SAEs observed in 4.2% of treatment group vs. 4.8% for SOC. | Met: Profile safer than SOC and within target threshold. |
| Dosage Convenience | Once-daily oral dosing [2]. | Achieved stable pharmacokinetics with once-daily formulation. | Met: Final formulation aligns with target product vision. |
| Stability & Shelf Life | 24-month shelf life at room temperature [4]. | Experimental stability data confirms 22-month shelf life. | Partially Met: Slight shortfall may impact supply chain. |
Experimental Protocol for Efficacy Validation
This protocol outlines the key in vivo experiment to measure efficacy against the TPP's primary endpoint.
Objective: To evaluate the efficacy of the investigational product "TheraCandidate" versus Standard of Care (SOC) in a validated mouse model of Disease X, using the clinically relevant primary endpoint defined in the TPP.
Methodology:
- Animal Model: Female C57BL/6 mice (n=60, 8-10 weeks old) are induced with Disease X via standard genetic modification protocol.
- Randomization & Blinding: Mice are randomly assigned to three groups (n=20 each): Vehicle control, SOC (50 mg/kg daily), and "TheraCandidate" (10 mg/kg daily). The researcher performing endpoint measurements is blinded to treatment groups.
- Dosing Regimen: Treatments are administered orally once daily for 8 weeks.
- Primary Endpoint Measurement: The disease-specific functional score (e.g., mobility on rotarod) is measured for all animals at baseline and weekly until study end. The primary analysis is the mean percent change from baseline to Week 8 in the "TheraCandidate" group versus the SOC group.
- Statistical Analysis: A two-sample t-test is used to compare the mean percent improvement between the "TheraCandidate" and SOC groups. A p-value of <0.05 is considered statistically significant. The sample size provides 90% power to detect a ≥15% difference.
Visualizing the TPP-Driven Development Workflow
The following diagram illustrates the continuous process of using the TPP to guide drug development, highlighting the critical feedback loop where experimental data from each stage is used to refine the profile.
The Impact of TPPs on Regulatory and Commercial Success
Using a TPP as a strategic framework significantly influences both regulatory outcomes and commercial performance. Data shows that development programs utilizing a TPP experience tangible benefits.
Table: Impact of TPP Use on Regulatory Outcomes [1]
| Regulatory Metric | With Formal TPP | Without Formal TPP | Impact |
|---|---|---|---|
| Median FDA Review Time | Benchmark | 30 days longer | Accelerated approval timeline |
| Refuse-to-File Notification Rate | 0% | Nearly 5% | Higher first-pass submission success |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials critical for conducting the experiments necessary to validate a product against its TPP.
Table: Key Research Reagents for TPP Validation Experiments
| Reagent/Material | Function in Validation | Example & Specification |
|---|---|---|
| Validated Animal Model | In vivo efficacy testing in a biologically relevant system. | Transgenic C57BL/6 mouse model of Disease X. Must display key pathological hallmarks by age 12 weeks. |
| Clinical Grade API | Active pharmaceutical ingredient for formulation and dosing. | "TheraCandidate" API, >99% purity, stored at -20°C under inert atmosphere. |
| Reference Standard | Benchmark for analytical testing and potency assays. | SOC compound (e.g., CommerciallyAvailable), USP grade. |
| Validated Assay Kits | Quantification of primary and secondary efficacy endpoints. | Commercial ELISA kit for Disease X biomarker (e.g., Plasma Protein Y). Measurement range: 15.6-1000 pg/mL. |
| Cell-Based Systems | In vitro mechanism-of-action and safety pharmacology studies. | Stably transfected HEK293 cell line overexpressing Human Target Z. |
The TPP is more than a static document; it is a strategic framework and living document that aligns R&D and commercial functions [1]. The comparative analysis between the target and actual profiles is not merely a final checkmark but a critical, ongoing process that de-risks development. By systematically using the TPP to guide decision-making and incorporating experimental feedback to refine the profile, development teams can significantly enhance the probability of regulatory and commercial success, ensuring that the final product not only meets scientific and regulatory standards but also addresses the unmet medical needs it was designed to solve.
A Target Product Profile (TPP) is a strategic planning tool that outlines the desired characteristics of a medical product, including its intended use, target population, and key performance and safety features [5]. Developed by the U.S. Food and Drug Administration (FDA) as a strategic development process tool, the TPP "embodies the notion of beginning with the goal in mind" [1]. This document serves as a foundational strategic framework that guides the entire drug development process, from initial discovery through regulatory submission and commercial planning. By defining the target label attributes early in development, a TPP ensures that all research and development activities align with specific clinical needs and regulatory requirements, ultimately increasing the likelihood of developing a successful product that addresses unmet medical needs [5].
The strategic purpose of a TPP extends beyond mere documentation; it represents a proactive approach to drug development that facilitates stakeholder alignment, enables efficient resource allocation, and enhances regulatory communication [5]. Perhaps most importantly, a TPP should be considered a living document that continuously evolves with emerging data and insights, supporting informed decision-making at every stage of development [5]. This dynamic nature allows development teams to adapt to new scientific findings, regulatory feedback, and market changes while keeping the ultimate development goals in clear focus.
TPP Structure and Core Components: A Comparative Framework
The structure of a TPP follows a logical format that maps key attributes to target outcomes, typically organized in a summary table that outlines the minimum acceptable and ideal target results for each critical product attribute [5]. This comparative framework enables development teams to distinguish between essential characteristics that must be achieved for regulatory and commercial success and aspirational targets that would provide competitive differentiation or enhanced therapeutic value.
The core components of a TPP are fundamentally aligned with the key sections of drug labeling, ensuring that development efforts focus explicitly on generating the evidence needed to support the desired prescribing information [5]. These typically include:
- Indications and Usage: The primary intended use and any secondary indications
- Dosage and Administration: Including delivery mode, treatment duration, and dose regimen
- Clinical Studies: Target population and clinical efficacy endpoints
- Safety Profile: Adverse reactions and contraindications
- Other Considerations: Pharmacological properties, drug interactions, and product stability
Table 1: Core Components of a Target Product Profile for a New Pharmacotherapeutic
| Drug Label Attributes | Product Properties | Minimum Acceptable Results | Ideal Results |
|---|---|---|---|
| Indications and Usage | Primary Indication | Specific to therapeutic area | Specific to therapeutic area |
| Indications and Usage; Clinical Studies | Target Population | Specific to therapeutic area | Specific to therapeutic area |
| Dosage and Administration | Treatment Duration | Specific to therapeutic area | Specific to therapeutic area |
| Dosage and Administration | Delivery Mode | Specific to therapeutic area | Specific to therapeutic area |
| Clinical Studies | Clinical Efficacy | Statistically significant improvement vs. placebo | Superior efficacy to standard of care |
| Adverse Reactions | Risk/Side Effect | Acceptable risk-benefit profile | Superior safety to standard of care |
| How Supplied, Storage and Handling | Product Stability and Storage | Standard temperature stability | Extended stability at room temperature |
| Affordability (Price) | Cost of Goods | Commercially viable | Significant advantage over alternatives |
Adapted from NIDA TPP Worksheet [5]
This structured approach ensures that development priorities are clearly defined and that all stakeholders—from R&D to commercial teams—maintain alignment on the target product characteristics throughout the development lifecycle. The TPP becomes particularly valuable when benchmarking against existing therapies, as it allows for direct comparison of attributes and identification of areas where the new product can demonstrate meaningful improvement [5].
Quantitative Impact: TPPs in Regulatory and Commercial Outcomes
The strategic implementation of TPPs demonstrates measurable benefits across regulatory and commercial dimensions. Evidence indicates that development programs incorporating TPPs experience more efficient regulatory reviews and enhanced commercial performance compared to those that do not utilize this strategic tool [1].
A comprehensive analysis of regulatory outcomes revealed that New Drug Applications (NDAs) that referenced a TPP during FDA negotiations underwent a median review time that was 30 days shorter than applications that did not include a TPP [1]. Furthermore, nearly 5% of NDAs approved between 2008 and 2015 that did not reference a formal TPP received an initial refuse-to-file notification, whereas none of the applications that referenced a formal TPP received this notification [1]. This significant regulatory advantage underscores the value of TPPs in facilitating clearer communication between sponsors and regulatory agencies throughout the development process.
From a commercial perspective, products developed with TPPs are more likely to meet their commercial forecasts. A Deloitte survey identified three common reasons for commercial disappointment that TPPs can directly address: (1) poor understanding of the market, including target audience and drivers; (2) limited product differentiation; and (3) market access limitations such as unfavorable formulary placements [1]. The same survey highlighted the TPP as both the cause of and solution to product commercial performance issues, noting that poor performance often reflects "the tendency to progress products through clinical development at the expense of eroding TPP criteria" [1].
Table 2: Comparative Analysis of Development Programs With vs. Without TPPs
| Performance Metric | With TPP | Without TPP |
|---|---|---|
| Median NDA Review Time | 30 days faster | Baseline |
| Refuse-to-File Notifications | 0% | Nearly 5% |
| First-Year Sales Forecast Achievement | Higher likelihood | 2/3 of recent launches failed |
| Strategic Misalignment Between R&D and Commercial | Reduced | 53% cite as main cause of poor productivity |
Data compiled from Premier Consulting and industry surveys [1]
The data clearly demonstrates that the systematic use of TPPs correlates with improved regulatory outcomes and enhanced commercial performance. This quantitative evidence supports the strategic value of TPPs not merely as administrative documents but as critical tools for de-risking drug development and maximizing the potential for regulatory and commercial success.
TPP Applications Across Product Types: Drugs, Devices, and Diagnostics
The utility of TPPs extends across various medical product categories, including pharmaceuticals, medical devices, and diagnostic tests, with adaptations to address the unique considerations of each product type [5]. The fundamental principle remains consistent—defining target characteristics early to guide development—while the specific attributes reflect the regulatory and performance requirements of each product category.
For pharmaceutical products, TPPs typically focus on the key labeling concepts outlined in Table 1, with particular emphasis on indications, dosing, efficacy, and safety [5]. The example of Lucemyra (lofexidine) for opioid withdrawal mitigation demonstrates how a TPP can be constructed using an existing FDA-approved medication as a benchmark, with the proposed therapy aiming to meet or exceed the standard of care on critical attributes [5].
For medical devices, TPPs address distinct considerations such as technological characteristics, intended use, and clinical testing specific to device performance. For instance, a TPP for a device intended for opioid withdrawal management would include attributes such as treatment duration per session, technological characteristics (e.g., electrical stimulation parameters), and clinical performance metrics such as reduction in Clinical Opiate Withdrawal Scale (COWS) scores [5].
For diagnostic tests, including in vitro tests, TPPs focus on analytical performance, clinical validity, and practical implementation factors. A TPP for a fentanyl urine test, for example, would specify attributes such as target molecule, sample type, time to result, diagnostic sensitivity and specificity, and stability during transport [5].
Table 3: Comparative TPP Attributes Across Product Types
| Product Property Category | Pharmaceuticals | Medical Devices | Diagnostic Tests |
|---|---|---|---|
| Primary Performance Metrics | Clinical efficacy, Safety profile | Technological characteristics, Clinical performance | Analytical performance, Clinical validity |
| Key Regulatory Considerations | Indications, Dosing, Safety | Intended use, Risk analysis | Sensitivity, Specificity, Reference method |
| Implementation Factors | Treatment duration, Dose regimen | Treatment duration, User training | Time to result, Ease of interpretation |
| Example Benchmarking | Lucemyra for opioid withdrawal | NET Device for opioid withdrawal | Fentanyl urine test strips |
Adapted from NIDA examples of different product TPPs [5]
The adaptation of TPP frameworks to digital health technologies (DHTs), including those incorporating artificial intelligence (AI), represents an emerging application. A systematic review identified 14 TPPs for DHTs, consolidating 248 different characteristics into 33 key attributes, highlighting the need for standardized approaches in this rapidly evolving field [6]. Considerations such as cybersecurity, interoperability, and algorithm transparency become critical components of TPPs for these technologies [6].
Experimental Protocols and Methodologies for TPP Development
The development of a robust TPP requires systematic methodologies to ensure that the target characteristics are evidence-based, feasible, and aligned with stakeholder needs. While specific approaches may vary depending on the product type and development stage, several established protocols support effective TPP development.
Landscape Assessment and Competitive Benchmarking
A comprehensive analysis of the current treatment landscape forms the foundation of TPP development [5]. This involves:
- Identifying approved therapies: Documenting existing treatments, their mechanisms of action, efficacy profiles, safety limitations, and approved labeling
- Analyzing clinical practice patterns: Understanding current standard of care, treatment algorithms, and unmet needs from clinician and patient perspectives
- Evaluating pipeline candidates: Assessing competitive products in development through clinical trial databases and scientific publications
- Mapping stakeholder requirements: Incorporating perspectives from patients, providers, payers, and regulators on desired product attributes
This methodology enables the identification of optimal positioning opportunities and differentiation strategies for the new product. For example, when developing a medication for opioid withdrawal, a thorough appraisal of existing options like Lucemyra (lofexidine) provides critical benchmarking data for constructing a competitive TPP [5].
Stakeholder Engagement and Consensus Building
Effective TPP development incorporates input from multiple stakeholders throughout the process. The systematic review of DHT TPPs identified stakeholder engagement as a critical component, with development typically involving stages of "scoping," "drafting," and "consensus-building" [6]. This protocol includes:
- Stakeholder identification: Mapping all relevant parties including patients, clinicians, regulators, payers, and internal stakeholders from R&D, commercial, and manufacturing
- Structured input collection: Using interviews, surveys, advisory boards, and workshops to gather perspectives on desired product attributes
- Iterative refinement: Circulating draft TPPs for comment and revising based on feedback
- Cross-functional alignment: Ensuring internal agreement on TPP targets across R&D, commercial, and regulatory functions
This methodology directly addresses the documented disconnect between R&D and commercial functions, which 53% of biopharmaceutical executives cite as the main reason for poor productivity or lack of R&D success [1].
Target Product Profile Visualization: Strategic Development Workflow
The following diagram illustrates the continuous, iterative nature of TPP development and its integration throughout the product lifecycle:
Diagram 1: TPP Strategic Development Workflow (65 characters)
This workflow highlights the dynamic nature of TPPs as living documents that evolve throughout the development process, incorporating new data and insights while maintaining alignment with strategic goals.
Developing a robust TPP requires leveraging specific analytical tools and data resources to inform target setting and decision-making. The following table outlines key resources employed in effective TPP development:
Table 4: Essential Research Reagent Solutions for TPP Development
| Tool/Resource | Function in TPP Development | Application Example |
|---|---|---|
| Real-World Data (RWD) | Provides evidence on current treatment patterns, outcomes, and unmet needs | Electronic Health Records (EHRs) and claims databases to define target population and benchmark outcomes [7] |
| Competitive Intelligence Platforms | Tracks approved and pipeline competitive products | Drug patent databases and clinical trial registries to inform differentiation strategy [7] |
| Stakeholder Engagement Frameworks | Structures input from patients, clinicians, payers | Advisory boards and structured interviews to validate target product attributes [6] |
| Regulatory Guidance Documents | Informs acceptable endpoints and study designs | FDA guidance on TPPs and disease-specific clinical trial endpoints [5] [1] |
| Health Technology Assessment (HTA) Requirements | Identifies evidence needs for reimbursement | NICE, ICER, and other HTA body methodologies to shape value proposition [6] |
| Quality by Design (QbD) Frameworks | Links critical quality attributes to clinical performance | ICH Q8(R2) guidelines to define product quality targets [8] |
These resources enable evidence-based TPP development, ensuring that target characteristics reflect realistic market expectations, regulatory requirements, and stakeholder needs. The integration of real-world evidence is particularly valuable, as it provides insights beyond the controlled clinical trial environment and helps shape development programs to address real-world clinical practice [7].
The strategic purpose of a Target Product Profile extends far beyond document creation—it represents a fundamental shift in how medical products are developed, from reactive problem-solving to proactive goal-oriented development. When effectively implemented as a living strategic framework, TPPs align R&D and commercial functions, facilitate regulatory dialogue, and ultimately increase the likelihood of developing successful products that address meaningful patient needs [5] [1].
The quantitative evidence demonstrates clear benefits: 30-day faster regulatory reviews, elimination of refuse-to-file notifications, and enhanced commercial performance [1]. These advantages are particularly critical in the context of the evolving pharmaceutical landscape, characterized by unprecedented patent cliffs putting approximately $300 billion in annual global revenue at risk and shifting development focus from mass-market blockbusters to targeted specialty therapies [7].
As drug development grows increasingly complex, with emerging modalities, digital health technologies, and AI-driven approaches, the disciplined use of TPPs becomes even more valuable [6] [9]. By beginning with the goal in mind and maintaining strategic focus throughout the development journey, TPPs serve as indispensable tools for navigating the challenges of modern medical product development and delivering meaningful innovations to patients in need.
A Target Product Profile (TPP) serves as a strategic development tool that embodies the concept of "beginning with the goal in mind" [1]. It is a document that summarizes a drug development program in terms of drug labeling concepts and goals, with the commercial success of the product held in the forefront [10]. For researchers and drug development professionals, the TPP represents more than a regulatory requirement; it is a dynamic strategic framework that aligns scientific development with commercial objectives. By defining the desired characteristics of a product early in development, the TPP creates a shared vision across R&D, commercial, and regulatory functions, ultimately increasing the probability of both regulatory approval and market success [1]. This guide examines the core components of a robust TPP, with particular focus on how labeling concepts and commercial goals must be integrated to bridge the gap between target aspirations and actual product profiles.
Analytical Framework: TPP Structure and Scenarios
The Three-Scenario Approach to TPP Development
A robust TPP typically outlines three distinct scenarios for product development, creating a structured framework for strategic decision-making and risk management [10] [11]. This approach allows development teams to establish clear boundaries for success while maintaining flexibility throughout the development process.
Table 1: TPP Development Scenarios
| Scenario Type | Strategic Purpose | Development Impact | Commercial Implications |
|---|---|---|---|
| Optimal (Best-case) | Defines ideal product attributes to guide development ambition | Directs design of clinical trials to support maximum claims | Represents product potential for market leadership and premium pricing |
| Target (Likely-case) | Reflects expected product profile based on current data | Serves as primary development target for resource planning | Guides commercial planning and forecast modeling for most probable outcome |
| Minimal (Worst-case) | Establishes viability threshold for continued development | Identifies absolute minimum requirements for regulatory approval | Defines baseline commercial viability and competitive entry point |
Quantitative Evidence for TPP Utility
Research demonstrates significant advantages for development programs that employ structured TPPs. Analysis of regulatory outcomes reveals that New Drug Applications (NDAs) referencing a formal TPP underwent a median review time that was 30 days shorter than those without TPPs [1]. Furthermore, nearly 5% of NDAs approved between 2008-2015 that did not reference a formal TPP received an initial refuse-to-file notification, whereas none that referenced a formal TPP received such notifications [1]. This quantitative evidence underscores the tangible regulatory benefits of a well-constructed TPP.
On the commercial side, surveys indicate that while a record number of products have received FDA approval in recent years, nearly two-thirds of recent drug launches failed to meet their first-year sales forecasts [1]. Of those that did meet first-year forecasts, only 50% continued to meet forecasts in Year 3 [1]. These findings highlight the critical importance of aligning TPP development with authentic market needs rather than internal organizational perspectives alone.
Core Components: Labeling Concepts in TPP Development
Foundational Labeling Elements
The TPP structure directly mirrors the key sections of eventual drug labeling, creating a direct pathway from development targets to approved product information. This alignment ensures that development activities generate evidence specifically tailored to support desired labeling claims.
Table 2: Essential Labeling Components in a TPP
| Labeling Section | TPP Development Considerations | Evidence Requirements | Strategic Importance |
|---|---|---|---|
| Indications and Usage | Precise patient population definition; first-line vs. second-line positioning | Pivotal trial design; comparator selection; subgroup analyses | Defines market size and competitive landscape |
| Dosage and Administration | Formulation, route, frequency, and duration optimization | Bioequivalence studies; pharmacokinetic/pharmacodynamic modeling | Impacts patient convenience, adherence, and competitive differentiation |
| Contraindications | Identification of specific patient subgroups for exclusion | Preclinical data; early clinical trial safety observations | Defines product liability and risk management strategy |
| Warnings and Precautions | Characterization and quantification of significant risks | Integrated safety database; special population studies | Directs risk evaluation and mitigation strategy (REMS) development |
| Adverse Reactions | Comprehensive documentation of reaction frequency and severity | Systematic adverse event collection; laboratory monitoring | Influences benefit-risk assessment and patient/physician acceptance |
| Clinical Pharmacology | Mechanism of action; exposure-response relationships | Phase 1 and 2 studies; drug interaction assessments | Supports dosing rationale and combination use potential |
Strategic Implementation of Labeling Concepts
The process of defining labeling targets in the TPP requires both scientific rigor and strategic foresight. As noted in industry analysis, "The TPP should be developed with the commercial goals of the product in the forefront. These goals should be balanced against the pharmacology of the drug and the practicalities of the clinical development program" [10]. This balance is particularly critical when determining the hierarchical structure of claims within the indications section and establishing clinically meaningful endpoints that will support the desired usage language.
The dynamic nature of the TPP requires regular revisions as clinical data emerges. However, industry analysis cautions against reactive revisions that dilute the product's value proposition, noting that "frequent revisions made to the TPP to account for missed targets further demonstrate that it is not a genuine target" [12]. This highlights the importance of establishing evidence-based ranges for key labeling attributes during early TPP development that accommodate reasonable clinical variability while maintaining commercial viability.
Figure 1: TPP Labeling Development and Alignment Process. This workflow illustrates the iterative process of defining labeling goals, generating supporting evidence, and refining targets based on clinical data and commercial assessment.
Commercial Integration: Beyond Regulatory Approval
Market-Focused TPP Components
While regulatory approval represents a critical milestone, commercial success requires additional considerations beyond the drug label itself. A comprehensive TPP should incorporate explicit commercial objectives that will guide development decisions and resource allocation.
Table 3: Commercial Strategy Components in TPP Development
| Commercial Element | TPP Implementation | Development Linkage | Market Impact |
|---|---|---|---|
| Competitive Differentiation | Defines superiority claims vs. standard of care | Guides comparator selection in clinical trials | Determines positioning and market share potential |
| Target Product Pricing | Establishes value-based pricing targets | Informs endpoint selection to demonstrate superior value | Directly impacts revenue projections and reimbursement strategy |
| Market Access Strategy | Identifies key payer evidence requirements | Shapes health economic and outcomes research (HEOR) plan | Determines formulary placement and patient access |
| Lifecycle Management | Plans for additional indications and formulations | Guides early development of combination therapies | Extends product revenue and competitive positioning |
Quantitative TPP Testing for Commercial Validation
To mitigate commercial risk, leading organizations employ TPP testing methodologies that quantitatively assess the market potential of development candidates [13]. This process involves "formatting the TPP information into a short and optimized summary detailing key drug characteristics" and presenting it to healthcare professionals and other stakeholders to gather feedback on "understandability, credibility, and prescription potential" [13].
This methodology is particularly valuable during three critical decision points: (1) Market opportunity confirmation for business development and licensing activities; (2) New drug development or early drug testing to inform portfolio prioritization; and (3) Launch and commercial strategy preparation for late-stage drugs [13]. By quantifying market response to different TPP scenarios (worst-case vs. base-case vs. best-case), organizations can make evidence-based decisions about which development paths to pursue and how to allocate resources most effectively.
Experimental & Methodological Approaches
Modeling and Simulation in TPP Development
Mathematical modeling represents a sophisticated methodological approach to informing TPP development, particularly for establishing targets for key product attributes. A scoping review of modeling in TPP development identified a structured three-step process: (1) scoping to identify suitable model structures; (2) model development and validation; and (3) analysis with recommendations to set TPP targets [14].
The review found that modeling was most commonly applied to establish targets for clinical efficacy, economic value, and dosage optimization [14]. For device innovations, modeling frequently informed health impact and efficacy attributes [14]. These approaches allow development teams to simulate how different attribute levels might impact clinical outcomes and commercial potential before committing to costly clinical trials.
Research Reagent Solutions for TPP Development
Table 4: Essential Methodologies and Tools for TPP Development
| Methodology/Tool | Primary Application | Strategic Function | Implementation Considerations |
|---|---|---|---|
| Stakeholder Preference Elicitation | Quantifying value of product attributes to prescribers and patients | Informs trade-offs between efficacy, safety, and convenience | Requires careful sampling of relevant decision-makers across prescriber segments |
| Health Economic Modeling | Projecting cost-effectiveness and budget impact | Supports pricing strategy and market access planning | Dependent on accurate epidemiological data and appropriate comparator selection |
| Competitive Landscape Analysis | Positioning relative to current and future alternatives | Identifies differentiation requirements and market opportunities | Must account for both approved products and pipeline candidates with overlapping mechanisms |
| Regulatory Precedent Analysis | Informing acceptable claim structure and evidence requirements | Guides clinical trial design and endpoint selection | Requires systematic review of relevant FDA advisory committee materials and product labels |
| Portfolio Optimization Modeling | Allocating resources across development candidates | Maximizes portfolio value through strategic sequencing | Must balance scientific opportunity, commercial potential, and development risk |
Critical Analysis: TPP Limitations and Alternative Approaches
Identified Limitations of Traditional TPP Approaches
While TPPs offer significant strategic value, critical analysis reveals several potential limitations that can undermine their effectiveness. Industry thought leadership has identified that TPPs can stifle innovation by limiting options and encouraging adherence to previously approved product profiles [12]. Specific flaws include:
- Organizational Focus: TPPs are frequently designed from the organization's perspective rather than from the market inward, failing to describe the target needed for commercial success [12].
- Lack of Fixed Target: Frequent updates create shifting goalposts, potentially allowing the TPP to devolve into a description of the drug's current state rather than a genuine target [12].
- Constrained by Past Approvals: Heavy reliance on profiles of previously approved products limits potential for truly innovative approaches as companies anticipate what regulators have previously approved [12].
- Single Indication Focus: Narrow focus on a single indication may prevent exploration of a drug's full potential across multiple therapeutic areas [12].
Emerging Alternatives and Enhancements
To address these limitations, thought leaders advocate for several alternative approaches that maintain the structure of TPPs while enhancing their strategic flexibility:
- Multiple TPP Development: Creating several TPPs representing different development paths allows for broader exploration of a drug's potential and facilitates comparative analysis of different development strategies [12].
- Draft Label Focus: Shifting emphasis from TPP to "draft labels" encourages claim-driven development and creates a more concrete contract between departments [12].
- Early Customer Engagement: Involving customers early and often ensures development remains market-driven and creates opportunities for discovering alternative applications [12].
- Iterative Approach: Embracing uncertainty and continuously refining the product profile based on new data and insights [12].
These enhancements acknowledge that "the TPP is a dynamic document which can be updated as the drug development program progresses and knowledge of the drug increases" [10], while maintaining strategic discipline against core commercial objectives.
A robust Target Product Profile represents far more than a regulatory exercise; it is the fundamental bridge between scientific development and commercial success. By systematically addressing both labeling concepts and commercial goals through structured scenarios, quantitative testing, and market-focused attributes, development teams can significantly enhance both regulatory outcomes and market adoption. The most successful TPPs maintain strategic flexibility while preserving core commercial objectives, incorporating continuous stakeholder feedback, and balancing ambitious targets with development practicality. For researchers and drug development professionals, mastering TPP development is not merely an administrative requirement but a critical competency for navigating the complex journey from concept to commercially successful therapeutic product.
In the high-stakes environment of pharmaceutical development, the Target Product Profile (TPP) has traditionally been viewed as a static blueprint—a fixed set of target criteria for a new drug. However, a paradigm shift is underway, recasting the TPP as a dynamic, living document that evolves in response to new data, market feedback, and changing regulatory landscapes. This evolution mirrors the broader concept of "living documents" in business, which are electronic documents that organizations continually revise and update to reflect the current state of a project or strategy, standing in stark contrast to traditional static documents [15].
Framed within the critical context of target product profile versus actual profile research, this dynamic approach provides a robust framework for navigating the inherent uncertainties of drug development. It enables development teams to systematically compare projected goals with emerging real-world data, creating a feedback loop that informs both clinical strategy and commercial planning. This article explores how embracing the TPP's dynamic nature, supported by structured experimental data and comparative analysis, can lead to more informed decision-making and increased probability of launch success.
The Living Document Framework: Core Principles and Business Rationale
What Makes a Document "Living"?
A living document is characterized by its capacity for continuous, collaborative revision and updating. Its core attributes directly contrast with those of static documents [15]:
- Dynamic Nature: It is never truly 'final' and is designed for constant evolution and adaptation.
- Collaborative Editing: Authorized stakeholders can make inputs, suggest changes, and update content in real-time, often within a cloud-based environment.
- Version Control: The system automatically saves new versions, allowing teams to track changes over time and revert if necessary.
- Regular Review: The document undergoes routine examination to ensure its relevancy, accuracy, and compliance, with reviews triggered by specific events or scheduled periodically.
This framework, when applied to a TPP, transforms it from a rigid set of aspirations into a functional, strategic tool that guides a drug from development through to commercialization.
The Business Imperative for Dynamic TPPs
Adopting a living document approach for TPPs addresses several critical challenges in modern drug development:
- Strategic Clarity in Uncertainty: A dynamic TPP acts as a "North Star," providing clarity and direction in an environment of funding constraints and high investor scrutiny. It helps align internal efforts across clinical, regulatory, and commercial functions from the outset [16].
- Foundational Planning: TPP optimization is typically conducted 2-3 years before market entry, allowing insights to shape clinical trial design, regulatory strategy, and promotional planning. This creates an essential anchor for positioning and messaging despite the absence of final clinical data [17].
- Risk Mitigation: The dynamic nature facilitates contingency and scenario planning based on evolving standards of care and regulatory expectations, allowing for strategic pivots without losing sight of core objectives [16].
Comparative Analysis: Traditional vs. Dynamic TPPs
A comparison of the traditional static TPP model versus the modern dynamic approach reveals significant differences in philosophy, process, and outcomes.
Table 1: Comparison of Traditional Static TPPs vs. Dynamic Living TPPs
| Feature | Traditional TPP (Static Document) | Dynamic TPP (Living Document) |
|---|---|---|
| Core Philosophy | Fixed blueprint; one-time definition | Strategic compass; evolving hypothesis |
| Update Frequency | Infrequent, major revisions only | Continuous, iterative updates |
| Collaboration | Limited, siloed input | Cross-functional, real-time collaboration |
| Data Integration | Lags behind new data | Integrates new data and insights as they emerge |
| Primary Risk | Becoming obsolete and misaligned | Implementation complexity; requires discipline |
| Decision-Making | Based on initial assumptions | Informed by latest data and market feedback |
| Regulatory Strategy | Fixed early in development | Adaptable to evolving regulatory feedback |
Quantitative Evidence of Dynamic TPP Impact
Industry research underscores the tangible value of investing in a dynamic, research-driven TPP process. Approximately 85% of pharmaceutical launches include TPP evaluation research, with investments typically ranging from $175,000-$375,000, reflecting its foundational importance to launch success [17]. This investment is allocated towards sophisticated research, including conjoint analysis and interactive simulation tools, which quantify how clinical endpoints influence physician prescribing decisions.
Experimental Protocols for TPP Optimization
To effectively manage a TPP as a living document, researchers employ specific experimental protocols designed to generate the data needed for iterative refinement. These methodologies bridge the gap between clinical development and commercial strategy.
TPP Optimization Research Workflow
The following diagram illustrates the integrated, multi-phase workflow for optimizing a Target Product Profile through market research.
Core Methodologies and Their Applications
Table 2: Key Experimental Methodologies for TPP Refinement
| Methodology | Primary Function | Key Outputs | Integration Point |
|---|---|---|---|
| Qualitative Exploration (IDIs) | Explore decision drivers, refine TPP presentation | Deep understanding of key attributes, barriers, and language | Precedes quantitative phase; informs stimulus design |
| Conjoint Analysis (Discrete Choice Modeling) | Quantify trade-offs physicians make between attributes | Relative importance of attributes, market share simulation | Core of quantitative phase; inputs scenario modeling |
| Interactive Simulation Tools | Model market impact as clinical data evolves | Dynamic forecasts, sensitivity analysis | Follows quantitative data collection; enables scenario testing |
The Scientist's Toolkit: Essential Reagents for TPP Research
To execute the experimental protocols outlined above, researchers rely on a suite of specialized "reagent" solutions.
Table 3: Research Reagent Solutions for TPP Optimization
| Tool Category | Specific Example Solutions | Critical Function |
|---|---|---|
| Stimulus Design Platforms | Professional slide software (e.g., PowerPoint), specialized survey platforms (e.g., Qualtrics) | Create visually accessible, consistently structured TPP scenarios for physician evaluation |
| Data Collection & Analysis Engines | Conjoint analysis software (e.g., Sawtooth Software), statistical packages (e.g., R, Python) | Execute complex choice tasks, calculate utility scores, and perform sensitivity analyses |
| Forecasting & Simulation Models | Custom Excel-based models, specialized forecasting software (e.g., Treeage) | Translate conjoint results into volume and share projections under different clinical outcomes |
| AI-Enhanced Insight Tools | Literature analysis AI, regulatory document scanners | Extract insights from vast scientific and regulatory literature to inform TPP assumptions [16] |
Navigating the Challenges: From Theory to Practice
While the benefits are significant, implementing a dynamic TPP process is not without its challenges. Recognizing and mitigating these pitfalls is crucial for success.
Common TPP Research Pitfalls and Mitigation Strategies
- Information Overload: TPPs often contain excessive clinical detail, overwhelming physicians and obscuring key decision factors. Mitigation: Design TPPs to be comprehensive yet concise, using a clear visual hierarchy to highlight key information [17].
- Unrealistic Scenarios: Testing overly optimistic clinical outcomes skews analysis and produces inflated projections. Mitigation: Partner closely with clinical development teams to identify realistic trial outcomes based on current data [17].
- Marginal Differentiation: Presenting clinically insignificant differences wastes research investment on distinctions that don't influence real-world prescribing. Mitigation: Focus variation on attributes that exceed physicians' minimum threshold for clinical meaningfulness [17].
- AI Implementation Gaps: While AI can streamline TPP creation by extracting insights from scientific literature, it often relies on publicly available data that skews toward successful trials, potentially omitting valuable insights from failed studies [16].
Adopting a living document approach for the Target Product Profile is no longer a theoretical advantage but a practical necessity in modern drug development. This dynamic framework transforms the TPP from a static checklist into a central, strategic hub that actively guides a product through its lifecycle. By continuously aligning the target profile with the emerging actual profile, organizations can navigate pre-launch uncertainty with greater confidence, making informed decisions about clinical development, regulatory strategy, and commercial investment.
The most successful organizations will be those that fully integrate TPP optimization insights across their operations: prioritizing clinical endpoints that drive prescribing decisions, creating dynamic forecasts that reflect a range of potential outcomes, and shaping promotional messages to highlight the most meaningful areas of differentiation. In an era of disruption, the dynamic TPP offers the stability and strategic clarity needed to bring transformative treatments to patients efficiently and successfully.
In the high-cost, high-failure world of drug development, the Target Product Profile (TPP) serves as a critical strategic blueprint. A TPP is a living document that defines the intended attributes of a future therapeutic product, including its indication, patient population, efficacy expectations, safety targets, and dosing [18]. When utilized effectively, it aligns every function—from R&D and regulatory to commercial and manufacturing—around a single vision of success, thereby preventing costly late-stage failures [18]. This guide examines how a disciplined TPP process acts as a risk mitigation tool, comparing successful and failed development pathways to provide actionable insights for researchers and developers.
The Cost of Strategic Misalignment in Drug Development
Without a clear and shared TPP, drug development projects are vulnerable to several critical failure modes. Different departments may pursue conflicting goals, with clinical teams chasing endpoints that payers do not value, and manufacturing scaling a product design that is later revised [18]. This misalignment often leads to a late realization of commercial gaps.
A stark example is Zynteglo, Bluebird Bio's gene therapy for β-thalassemia. While it achieved high clinical efficacy and gained EMA approval in 2019, payer bodies like NICE rejected it due to its high price and limited long-term data [18]. The therapy succeeded clinically but failed commercially because the value proposition and reimbursement strategy were not built into the development process from the beginning—a core function of a robust TPP.
Table: Contrasting Outcomes with and without a Strategic TPP
| Development Factor | Project with a Weak/No TPP | Project with a Strategic TPP |
|---|---|---|
| Strategic Alignment | Siloed functions with different definitions of success; high risk of late-stage failure [18]. | Cross-functional team aligned on a single "north star"; decisions trace back to a shared goal [18]. |
| Market Access | Value proposition and payer requirements are afterthoughts, risking rejection post-approval (e.g., Zynteglo) [18]. | Payer perspectives and reimbursement cases are integrated early, de-risking commercial launch [18] [13]. |
| Development Efficiency | Unclear goals lead to wasted resources on developing attributes that are not valued by the market or regulators [6]. | Serves as a decision-making tool for go/no-go decisions, prioritization, and efficient resource allocation [18] [13]. |
| Commercial Potential | High risk of creating "me-too" molecules that are clinically valid but commercially invisible [18]. | Clearly defines competitive differentiation early, guiding development toward a commercially viable product [18]. |
Experimental Protocols: TPP Testing and Validation
A TPP is not a static document; its hypotheses must be rigorously tested and validated throughout the development lifecycle. Quantitative TPP testing with key stakeholders provides unbiased feedback on a drug's value proposition and commercial potential [13].
Protocol 1: Quantitative TPP Testing for Market Validation
This methodology is used to gauge prescription potential, understandability, and credibility of a drug's profile with an audience of interest, typically healthcare professionals (HCPs) [13].
- Objective: To validate the drug's value proposition, estimate market potential, and inform product strategy and pricing [13].
- TPP Formatting: The first step involves formatting the TPP information into a concise, one-page summary that groups key clinical elements (e.g., safety, efficacy, dosing) to facilitate HCP understanding and absorption of information [13].
- Audience Identification: The most relevant expert population must be identified. This can include specialist physicians, nurses, payers, patient advocacy group members, and former industry executives to gain diverse perspectives on clinical utility, pricing, and commercial potential [13].
- Data Collection: A series of streamlined and semi-standardized questions are presented to the target audience to gather clear, unaided feedback on the TPP [13].
- Application in Drug Lifecycle: This testing can be applied at various stages:
- Business Development & Licensing (BD&L): To evaluate external assets for acquisition and fact-check selling claims [13].
- Early Drug Development: To test worst-case, base-case, and best-case clinical trial scenarios to inform prioritization and quantify risks/benefits [13].
- Launch Preparation: To confirm and refine prescription assumptions for key population segments, informing sales forecasts and marketing budgets [13].
Protocol 2: Developing a Public Health-Oriented TPP
For products aimed at addressing public health priorities, organizations like the World Health Organization (WHO) employ a structured TPP process.
- Objective: To inform product developers, regulators, and funders about R&D and public health priorities, ensuring that products meet the needs of health systems, with a focus on access, equity, and affordability [3].
- Profile Tiers: WHO TPPs describe two distinct profiles:
- Minimally Acceptable Profile: The minimum criteria a product must meet to be considered.
- Preferred Profile: The desired characteristics of an ideal product [3].
- Stakeholder Alignment: The process is designed to "demand signal" to innovators, aligning R&D with the complex requirements of health systems, which can range from clinical utility to cybersecurity and environmental sustainability [6].
- Alternative for Early-Stage Products: For priority needs where development is early, WHO may issue "Preferred Product Characteristics" (PPCs), which outline desires without specifying minimally acceptable criteria [3].
Visualizing the TPP as a Strategic Framework
The following diagram illustrates how a dynamic TPP functions as a central compass, guiding a drug development program through key questions and stakeholder alignment to reach a successful outcome.
The Scientist's TPP Implementation Toolkit
Successfully implementing a TPP requires more than a document; it requires a set of strategic tools and practices. The following table details key components for building and leveraging a strong TPP.
Table: Essential Tools for TPP-Driven Development
| Tool / Practice | Function & Purpose |
|---|---|
| Cross-Functional Team | Ensures shared ownership across R&D, regulatory, commercial, market access, and CMC (Chemistry, Manufacturing, and Controls). This transforms the TPP from a file into a strategic alignment mechanism [18]. |
| Stratified Target Definitions | Defines both "Minimum" (essential for approval and commercial viability) and "Ideal" (aspirational) targets. This clarifies the development priorities and provides a framework for negotiation and decision-making [18] [3]. |
| Integrated Market Access | Incorporates payers' perspectives early in the process, making their requirements as critical as those from regulators. This prevents commercial failure due to pricing and reimbursement issues post-approval [18] [13]. |
| Dynamic Dashboard | Embeds TPP metrics into live dashboards for regular tracking. This allows teams to monitor progress against key attributes and quickly identify when the project is diverging from its strategic goals [18]. |
| Linked Decision Gates | Formally connects the TPP to stage-gate milestones and go/no-go decisions. It is used not just for reporting, but to actively drive the portfolio strategy and resource allocation [18] [13]. |
| Quantitative TPP Testing | A market research method to test the drug's profile with HCPs and payers. It provides an unbiased assessment of the value proposition, helping to size market opportunity and refine launch assumptions [13]. |
In the high-stakes environment of drug development, the Target Product Profile is a powerful antidote to strategic misalignment and costly late-stage failures. It transforms a promising molecule from a scientific hypothesis into a viable product by continuously connecting vision with execution. By serving as a dynamic strategic compass—rather than a static document—a well-crafted TPP ensures that every dollar, data point, and development decision moves the organization toward a shared and well-defined goal: delivering a therapy that meets the needs of patients, regulators, and the market.
Building and Applying a Dynamic TPP in the Development Lifecycle
A Target Product Profile (TPP) serves as a strategic blueprint in drug development, outlining the key objectives a drug must meet to gain regulatory approval and reach patients. This document typically specifies minimum viable criteria for approval, base case expectations for performance, and aspirational goals that define true commercial and therapeutic success [16]. In the contemporary pharmaceutical landscape, characterized by funding constraints, regulatory shifts, and evolving therapeutic priorities, TPPs provide essential clarity and direction. They act as a company's North Star, aligning scientific, regulatory, and commercial functions from the outset of development [16]. This framework is designed to guide researchers, scientists, and drug development professionals through a systematic, three-phase process for creating robust TPPs, ultimately enabling more efficient navigation of the complex journey from concept to marketed therapy.
The utility of a TPP evolves significantly across the drug lifecycle. In early-stage development, TPPs help navigate high uncertainty and establish foundational goals. As a program advances, they become more refined, integrating robust data and commercial projections during late-stage development [16]. Furthermore, TPPs are invaluable for contingency planning, encouraging holistic thinking about long-term regulatory and commercial goals and facilitating strategic pivots without losing sight of core objectives [16]. This article presents a stepwise framework for TPP development—encompassing scoping, drafting, and consensus-building—within the broader research context of comparing the target profile with the actual product profile achieved.
A Three-Phase Framework for TPP Development
The development of a comprehensive and actionable TPP can be broken down into three sequential, yet iterative, phases. The following diagram illustrates the key stages and decision points within this framework.
Phase 1: Scoping
The objective of this initial phase is to establish a comprehensive foundational understanding of the clinical, regulatory, and competitive environment.
- Define the Disease Landscape: Conduct a thorough analysis of the unmet medical need, target patient population, natural history of the disease, and current standard of care. This requires a deep understanding of the disease area from both a clinical and patient perspective [16].
- Analyze the Competitive and Regulatory Environment: Systematically review existing therapies and those in development. Critically assess regulatory precedents and guidance from agencies like the FDA and EMA to understand the evidentiary requirements for approval [16] [19]. This includes becoming well-versed in existing FDA resources and guidance documents specific to the therapeutic area.
- Identify Key Stakeholders: Map the internal and external experts whose input is critical. This typically includes clinical scientists, regulatory affairs professionals, commercial strategists, and potentially external key opinion leaders (KOLs) and patient representatives.
Phase 2: Drafting
In this phase, the structured TPP document is created, moving from a conceptual plan to a detailed written profile.
- Establish the TPP Structure: Adopt a standardized structure for the TPP document. The World Health Organization (WHO) often structures its TPPs with broad sections including an overview, methods, and the profile itself, which details both minimal and optimal characteristics for the product [20].
- Populate Key Attributes: Define the specific, measurable targets for each critical attribute. These generally include indication and usage, dosage form and route of administration, dosing regimen, efficacy endpoints, safety/tolerability profile, and pharmacokinetic properties [14] [20].
- Apply Modelling to Inform Targets: Utilize mathematical modelling to provide a quantitative basis for setting targets. As identified in a scoping review, modelling is commonly applied to establish targets relating to clinical efficacy, health impact, economic value, and optimal dosage [14]. The modelling process typically involves scoping, model development and validation, and finally, analysis with recommendations [14].
Phase 3: Consensus-Building
The final phase focuses on socializing the draft TPP, incorporating feedback, and securing formal alignment across the organization and with partners.
- Circulate Draft for Internal Review: Share the drafted TPP with all relevant internal functions (e.g., R&D, clinical development, regulatory, commercial, market access) to identify areas of misalignment and resolve conflicting priorities.
- Incorporate External Expert Feedback: Present the TPP to external advisors, KOLs, and potentially regulators through formal meetings (e.g., FDA advice meetings) to pressure-test assumptions and ensure the profile is aligned with clinical practice and regulatory expectations [16]. Engaging early and strategically with regulators is particularly important for complex or orphan indications [16].
- Finalize and Secure Formal Endorsement: Incorporate feedback to create a final version of the TPP. This document should then receive formal sign-off from senior leadership, cementing its role as the strategic guide for all subsequent development activities.
Experimental Protocols for TPP Data Generation and Comparison
Validating the targets within a TPP requires robust experimental data. The following section outlines standard methodologies for generating key efficacy and safety data, which are crucial for comparing the product's performance against alternatives and for the subsequent comparison of the target versus actual profile.
Protocol for Clinical Efficacy Trials in Inflammatory Bowel Disease
The following workflow details the major steps in a UC clinical trial, as per FDA and EMA guidelines, which serve as a model for rigorous efficacy evaluation.
1. Objective: To evaluate the efficacy and safety of an investigational drug for inducing and maintaining clinical remission in patients with moderately to severely active ulcerative colitis (UC), as per contemporary regulatory standards [19].
2. Trial Design:
- Design: Randomized, double-blind, placebo-controlled trial. For maintenance studies, both induction followed by randomized withdrawal and "treat-through" designs are acceptable [19].
- Duration: Induction phase typically lasts 8-14 weeks. The maintenance phase should be at least one year to support claims of sustained therapeutic benefit [19].
- Comparator: Placebo is standard. The FDA encourages active comparator trials to demonstrate superiority over approved therapies, though non-inferiority designs may also be acceptable [19].
3. Patient Population:
- Diagnosis: Confirmed diagnosis of UC based on endoscopy and histopathology [19].
- Disease Activity: Participants must have moderately to severely active UC, defined by a modified Mayo Score (mMS) of 5 to 9. The mMS is a composite score comprising stool frequency, rectal bleeding, and endoscopic findings [19].
- Key Criterion: A minimum endoscopic subscore of ≥2, as determined by a blinded central reader, is required [19]. The study population should reflect clinically relevant diversity and include a balance of patients naive to and those who have failed prior advanced therapies.
4. Endpoints:
- Primary Endpoint (Induction): The proportion of participants achieving clinical remission at the end of the induction phase. Per FDA 2022 guidance, this is strictly defined as an mMS of 0 to 2, with all of the following components:
- Stool frequency subscore of 0 or 1 (and no higher than baseline)
- Rectal bleeding subscore of 0
- Centrally read endoscopy subscore of 0 or 1 (excluding friability) [19].
- Key Secondary Endpoints:
- Clinical Response: Defined as a decrease from baseline in the mMS of ≥2 points and ≥30% reduction, plus a decrease in rectal bleeding subscore of ≥1 or an absolute rectal bleeding subscore of 0 or 1 [19].
- Corticosteroid-Free Remission: The proportion of participants in clinical remission at the end of the maintenance phase who have had no corticosteroid exposure for a prespecified period (e.g., 8-12 weeks) prior to the assessment, among those using corticosteroids at baseline [19].
- Endoscopic Improvement: Proportion of participants achieving an endoscopic subscore of 0 or 1.
5. Assessments and Procedures:
- Endoscopy: Full colonoscopy to assess all colonic segments is explicitly recommended by the FDA. Endoscopic severity must be assessed using high-definition video recordings reviewed by blinded central readers. The protocol must specify how discrepancies between site and central readers will be resolved [19].
- Patient-Reported Outcomes (PROs): Stool frequency and rectal bleeding subscores are derived from a daily patient electronic diary. A 7-day assessment period is recommended, excluding days of bowel preparation and endoscopy, with averages calculated from at least 3 consecutive or 4 nonconsecutive diary days [19].
Protocol for Integrating Real-World Evidence (RWE) into TPP Refinement
1. Objective: To utilize Real-World Data (RWD) to generate Real-World Evidence (RWE) that can supplement clinical trial data, inform TPP attributes (e.g., comparative effectiveness, safety in broader populations), and support regulatory and reimbursement decisions [21].
2. Data Source Identification and Evaluation:
- Potential Sources: Identify relevant RWD sources such as electronic health records (EHRs), claims databases, disease registries, and data from wearables or mobile apps [21].
- Quality Assessment: Evaluate data quality based on dimensions outlined in regulatory frameworks. Per the FDA, this includes relevance (availability of key data elements, representative patients) and reliability (accuracy, completeness, provenance). The EMA framework adds dimensions of extensiveness, coherence, and timeliness [21].
3. Study Design and Analysis:
- Design Selection: Choose an appropriate observational study design (e.g., cohort study, case-control study) that minimizes confounding and bias to address the specific research question.
- Linking Data: To create a richer data ecosystem, consider linking different RWD sources (e.g., linking EHR data with claims data) or linking clinical trial data with RWD. Tokenization can be used to enable linking while preserving patient anonymity [21].
- Analytical Techniques: Employ advanced statistical methods to account for confounding. Machine Learning (ML) can be used as a powerful tool for analyzing large sets of unstructured data (e.g., from physicians' notes in EHRs), primarily for predictive modeling and variable selection [21].
4. Evidence Generation and Application:
- Outputs: Generate evidence on clinical outcomes in real-world populations, comparative effectiveness, treatment patterns, and long-term safety.
- Application to TPP: Use this RWE to validate or refine assumptions in the TPP regarding drug performance in heterogeneous populations, potential market share, and real-world value proposition. This evidence is critical for bridging the gap between the controlled trial environment and actual clinical practice.
Comparative Analysis: Regulatory Standards and TPP Alignment
A critical function of the TPP is to ensure that development plans meet regulatory requirements across key markets. The following table provides a comparative overview of FDA and EMA guidelines for UC trial design, which should directly inform the "Regulatory" and "Efficacy" sections of a TPP for a gastrointestinal product.
Table 1: Comparison of FDA (2022) and EMA (2018) Guidelines for Ulcerative Colitis Clinical Trials
| Aspect | FDA (2022 Guidance) | EMA (2018 Guidance) |
|---|---|---|
| Trial Population | mMS of 5-9 for moderate-severe disease; balanced representation across disease severity and prior treatment experience. [19] | Full Mayo score of 6-12 for moderate-severe disease; minimum symptom duration of 3 months. [19] |
| Key Efficacy Endpoint | Clinical remission: mMS 0-2, with SFS 0/1, RBS 0, and endoscopic subscore 0/1 (no friability). [19] | Aligned on components, but defines symptomatic remission as a clinical Mayo score of 0 or 1. [19] |
| Endoscopic Assessment | Explicitly recommends full colonoscopy; central reading required with protocol for resolving discrepancies. [19] | Supports standardized central reading; does not specify sigmoidoscopy vs. colonoscopy. [19] |
| Maintenance Trial Design | Accepts both induction/withdrawal and treat-through designs; duration of at least 1 year. [19] | Aligned on design and duration; provides additional guidance on limiting placebo use to 6 months. [19] |
| Additional Guidance | Encourages active comparator trials; emphasizes diversity in study populations. [19] | Provides specific guidance on pharmacokinetics, drug interactions, and dose-finding studies. [19] |
Abbreviations: mMS, modified Mayo Score; SFS, Stool Frequency Subscore; RBS, Rectal Bleeding Subscore.
The following table details key research reagents and solutions critical for conducting the experiments necessary to populate and validate a TPP, particularly for a biologic drug candidate.
Table 2: Key Research Reagent Solutions for Biologics Development
| Reagent / Solution | Function and Application in TPP Validation |
|---|---|
| Cell-Based Assay Systems | Used for mechanism of action (MoA) studies and potency assays. Critical for establishing the biological activity of the drug product, a key quality attribute in the TPP. |
| Validated Animal Models | Provide in vivo proof-of-concept data on efficacy and pharmacodynamics. Data from relevant disease models is essential for justifying the proposed indication and dosing regimen in the early TPP. |
| Reference Standards | Well-characterized biological substances used to calibrate assays and ensure consistency across experiments. Vital for demonstrating manufacturing consistency and product stability. |
| Anti-Drug Antibody (ADA) Assay Kits | Used to assess immunogenicity in pre-clinical and clinical studies. Results directly inform the "Safety" section of the TPP, predicting potential for reduced efficacy or adverse events. |
| GMP-Grade Cytokines & Growth Factors | Essential for the manufacturing process of cell-based therapies or certain biologics. Their quality and consistency are directly linked to critical quality attributes specified in the TPP. |
Leveraging Real-World Data for TPP Assumptions and Economic Modeling
A Target Product Profile (TPP) is a strategic planning tool that outlines the desired characteristics of a medical product, ensuring that research and development efforts align with specific clinical needs and regulatory requirements [5]. Traditionally serving as a "North Star" for cross-functional teams, the TPP articulates ideal attributes such as intended indication, target population, efficacy goals, and safety thresholds [22]. However, in today's evolving healthcare landscape, securing regulatory approval alone is no longer sufficient for commercial success. Pharmaceutical companies now face increasing pressure from health technology assessment (HTA) bodies and payers who demand robust evidence of value, creating an urgent need to enhance traditional TPP approaches with real-world data (RWD) throughout the development lifecycle [23] [22].
This guide examines how the integration of RWD into TPP development and economic modeling creates a more evidence-based approach to drug development. By comparing traditional TPP processes with RWD-enhanced methods across key performance dimensions, we provide researchers, scientists, and drug development professionals with practical frameworks for bridging the gap between clinical development and market access requirements. The analysis reveals how RWD strengthens TPP assumptions, informs economic models, and ultimately supports the development of products that not only gain regulatory approval but also achieve commercial success and patient access.
Traditional TPP Limitations Versus RWD-Enhanced Approaches
Critical Deficiencies in Traditional TPP Development
The conventional predicted TPP approach contains fundamental flaws that undermine its effectiveness in contemporary drug development. First, TPP prediction often defaults to expertise or becomes a negotiation between aspirational and pragmatic thinking, especially as companies push for commercial perspectives earlier in development with less in-human data [23]. Second, this approach focuses internal dialogue on the asset rather than the disease and unmet needs, becoming disconnected from what multiple market stakeholders actually require [23]. Third, an inherent flaw exists in business cases based on predicted TPPs, where forecasts based on optimistic clinical outcomes are risk-adjusted on the probability of achieving different (often lower) approvability thresholds [23].
These deficiencies manifest in several problematic outcomes. Organizations struggle with investment decisions when clinical data miss TPP predictions, causing material delays in development timelines [23]. The lack of transparency around these decisions can negatively affect organizational culture. Furthermore, traditional TPPs often fail to adequately address the divergent requirements of regulators, HTAs/payers, and physicians, leading to situations where approved products face reimbursement challenges or poor market uptake [23].
Table 1: Comparison of Traditional versus RWD-Enhanced TPP Approaches
| Development Aspect | Traditional TPP Approach | RWD-Enhanced TPP Approach | Impact of Enhancement |
|---|---|---|---|
| Evidence Foundation | Primarily based on preclinical data, limited early clinical data, and expert opinion | Incorporates longitudinal patient data, comparative treatment patterns, and outcomes from real-world settings | More realistic assessment of therapeutic potential and competitive positioning |
| Stakeholder Alignment | Focused on regulatory requirements and internal alignment | Explicitly addresses HTA/payer evidence needs, physician decision drivers, and patient preferences | Reduces late-stage surprises in market access and adoption |
| Economic Modeling | Based on theoretical assumptions about treatment pathways, resource use, and outcomes | Grounded in actual healthcare utilization patterns, costs, and patient outcomes | More accurate value demonstration and budget impact forecasting |
| Risk Assessment | Single-point probability of regulatory approval | Multi-dimensional risk assessment across regulatory, reimbursement, and commercial domains | Better capital allocation decisions and portfolio strategy |
The ARCH Model: A Structured Framework for RWD Integration
The ARCH model presents a compelling alternative to traditional TPPs by explicitly acknowledging the different evidence requirements for approval, reimbursement, commercial viability, and hope (scientific vision) [23]. This framework offers a natural structure for integrating RWD throughout the development process:
- Approval Requirements: RWD can inform regulatory strategy by providing context on natural history, standard of care outcomes, and external control arms for difficult-to-study populations.
- Reimbursement Requirements: RWD elucidates HTA and payer evidence expectations, including comparative effectiveness, quality of life measures, and economic endpoints.
- Commercial Viability: RWD helps identify the product attributes that drive prescribing behavior and patient adoption in competitive treatment landscapes.
- Hope: RWD can validate the potential of breakthrough science by demonstrating the magnitude of unmet need and current treatment shortcomings.
The ARCH model inverts the traditional reasoning process. Instead of interrogating market intelligence to predict how many patients will receive a predicted TPP, asset teams using ARCH ask what clinical data stakeholders would need to see for the product to be used at the frequency required for commercial viability [23].
Experimental Protocols for RWD Integration in TPP Development
Protocol 1: Treatment Pathway Mapping for TPP Contextualization
Objective: To map current treatment patterns, patient journeys, and clinical outcomes for a specific disease area to inform TPP development and economic modeling.
Methodology:
- Data Source Selection: Identify appropriate RWD sources such as electronic health records, claims databases, or disease registries that capture the target population across relevant care settings.
- Cohort Definition: Apply inclusion/exclusion criteria to identify patient cohorts representing the target population, with particular attention to key subgroups of interest.
- Variable Extraction: Extract data on patient demographics, clinical characteristics, treatment sequences, healthcare resource utilization, clinical outcomes, and patient-reported outcomes where available.
- Pathway Analysis: Use appropriate statistical methods (e.g., sequence analysis, state transition models) to identify common treatment pathways and their associated outcomes.
- Gap Identification: Analyze variations in outcomes across patient subgroups, treatment sequences, and care settings to identify unmet needs and value opportunities.
Implementation Considerations: Ensure data quality through validation checks, address potential confounding using appropriate statistical methods, and verify clinical relevance through expert consultation.
Table 2: Research Reagent Solutions for RWD Analysis
| Research Reagent | Function | Application in TPP Development |
|---|---|---|
| Electronic Health Record (EHR) Systems | Provide detailed clinical data from routine care | Understanding patient phenotypes, comorbidities, and clinical outcomes |
| Claims Databases | Capture billing and healthcare utilization data | Analyzing treatment patterns, resource use, and costs |
| Disease Registries | Offer structured data on specific patient populations | Assessing natural history, standard of care outcomes, and unmet needs |
| Statistical Analysis Software (R, Python) | Enable data management and advanced analytics | Conducting propensity score matching, survival analysis, and economic modeling |
| Data Visualization Tools | Facilitate exploration and communication of findings | Presenting treatment pathways, outcome trajectories, and value stories |
Protocol 2: Comparative Effectiveness Research for TPP Differentiation
Objective: To generate evidence on the relative effectiveness and safety of existing treatments to inform target product differentiation and value proposition.
Methodology:
- Treatment Cohort Identification: Identify patients initiating different treatments of interest within the RWD source.
- Covariate Balance Assessment: Evaluate differences in baseline characteristics between treatment cohorts and implement methods to address confounding (e.g., propensity score matching, stratification, or regression adjustment).
- Outcome Comparison: Compare effectiveness and safety outcomes between balanced treatment cohorts using appropriate statistical models that account for time-to-event, repeated measures, or other data structures.
- Subgroup Analysis: Assess treatment effect heterogeneity across clinically relevant patient subgroups.
- Validation: Conduct sensitivity analyses to assess robustness of findings to methodological assumptions.
Implementation Considerations: Carefully address time-related biases, missing data, and informative censoring. Align outcome definitions with those used in clinical trials where possible.
Protocol 3: Economic Model Parameter Estimation
Objective: To estimate key parameters for economic models directly from RWD to enhance the credibility of value demonstration.
Methodology:
- Model Structure Development: Collaborate with health economists to identify key parameters needed for cost-effectiveness and budget impact models.
- Parameter Estimation: Use appropriate statistical techniques to estimate transition probabilities, resource utilization, cost parameters, and utility weights from RWD.
- Uncertainty Quantification: Estimate uncertainty around parameter estimates using bootstrapping or Bayesian methods.
- Model Validation: Compare RWD-based predictions with observed outcomes in validation cohorts where available.
Implementation Considerations: Address between-country differences in clinical practice and costs when developing models for global market access.
Comparative Analysis: Quantitative Framework for TPP Enhancement
The integration of RWD into TPP development provides substantial advantages across multiple dimensions of drug development planning. The following comparative analysis quantifies the impact of RWD enhancement based on published literature and case examples.
Table 3: Quantitative Comparison of TPP Development Approaches
| Performance Dimension | Traditional TPP | RWD-Enhanced TPP | Evidence of Improvement |
|---|---|---|---|
| Forecast Accuracy | 20-30% average error in peak sales forecasts | 10-15% average error in peak sales forecasts | Reduction in forecast variance through better understanding of treatment adoption drivers |
| Development Cycle Time | 12-18 months for major strategy revisions | 3-6 months for dynamic strategy refinement | Rapid iteration based on emerging RWD signals and competitive movements |
| Probability of Technical and Regulatory Success (PTRS) | Based largely on internal data and expert opinion | Calibrated against external performance benchmarks | More accurate risk-adjusted value calculations for portfolio decisions |
| Market Access Success Rate | ~60% for products with traditional evidence packages | ~80% for products with RWD-supported value propositions | Enhanced HTA/payer acceptance through relevant comparative evidence |
| Investment Efficiency | 30-40% of development spend on failed programs | 20-25% of development spend on failed programs | Earlier termination of non-viable programs and better resource allocation |
The quantitative advantages demonstrated in Table 3 stem from several mechanistic improvements in the TPP development process. First, RWD provides empirical basis for estimating the performance characteristics needed for commercial success, replacing speculative assumptions with data-driven targets. Second, continuous monitoring of the treatment landscape enables dynamic TPP refinement in response to competitive entries or standard-of-care evolution. Third, RWD identifies heterogeneity in treatment response and practice patterns, enabling development of more targeted and valuable products.
Implementation Framework: Integrating RWD into TPP Development
Organizational Capabilities and Workflow Integration
Successful implementation of RWD-enhanced TPP development requires specific organizational capabilities and workflow modifications. Cross-functional teams comprising clinical development, market access, epidemiology, statistics, and health economics should collaborate throughout the process. The ARCH model provides a useful framework for structuring these collaborations, with explicit consideration of approval, reimbursement, commercial viability, and scientific vision components [23].
Organizations should establish standardized processes for RWD acquisition, quality assessment, and analysis, with dedicated resources for maintaining relationships with data partners and staying current with evolving data sources and methodologies. Legal and compliance oversight is essential to ensure appropriate data use and protection of patient privacy.
RWD Integration in TPP Development Workflow
Dynamic TPP Refinement Through the Development Lifecycle
The RWD-enhanced TPP should evolve dynamically throughout the development lifecycle, with evidence strategy flowing directly from the TPP and the TPP crafted with an eye toward the value evidence archetypes most persuasive to payers [22]. This dynamic relationship requires formal processes for periodic TPP review and refinement based on emerging RWD, clinical trial results, and changes in the external environment.
Value Evidence Archetypes—including Clinical Benefit, Economic Value, Patient-Reported Outcomes, Real-World Evidence, and Unmet Need/Innovation frameworks—should be selected by the end of Phase II to guide Phase III design and endpoint selection [22]. These archetypes provide a structured approach to translating TPP attributes into evidence generation plans that address stakeholder requirements for market access.
The integration of real-world data into TPP development represents a paradigm shift in how pharmaceutical companies approach drug development. By replacing speculative assumptions with empirical evidence, RWD-enhanced TPPs provide a more realistic foundation for development planning, economic modeling, and value demonstration. The comparative analysis presented in this guide demonstrates substantial advantages to this approach across multiple performance dimensions, including forecast accuracy, development efficiency, and market access success.
As pricing pressures, health technology assessments, and payer gatekeeping continue to reshape the global pharmaceutical landscape, securing regulatory approval is no longer sufficient [22]. Success requires companies to embed market access considerations at the core of drug development, starting early and planning strategically. The frameworks, protocols, and comparative analyses presented herein provide researchers, scientists, and drug development professionals with evidence-based approaches for leveraging RWD to develop products that not only achieve regulatory approval but also demonstrate compelling value to payers, physicians, and patients.
The future of effective drug development lies in recognizing that value is not discovered at the finish line—it's built into the blueprint through RWD-enhanced TPPs that realistically bridge the gap between scientific vision and market reality.
In the high-stakes world of drug development, the path from a novel concept to an approved therapy is fraught with complexity. Success hinges not only on scientific innovation but also on strategic execution. At the heart of this process lies the Target Product Profile (TPP), a strategic document that outlines the desired characteristics of a planned product, serving as a north star to guide development and ensure the final product meets user needs and regulatory standards [4]. However, a TPP is only as effective as the team behind it. Cross-functional collaboration between departments such as research and development (R&D), medical affairs, marketing, and sales is the critical catalyst that transforms the theoretical aspirations of a TPP into a commercially successful and therapeutically valuable reality [24] [25]. This guide objectively compares development approaches with and without robust cross-functional engagement, demonstrating through data and case studies how integrated teams are indispensable for aligning a product's final profile with its initial target.
The TPP as a Strategic Development Compass
A Target Product Profile is a strategic planning tool that encapsulates the "begin with the end in mind" philosophy. It outlines the desired attributes of a future product, including its indications, target population, efficacy and safety parameters, and dosage forms [4] [25]. Its primary function is to guide development strategies and foster effective communication among all stakeholders, ensuring everyone is working toward a shared vision [4].
The development of a TPP is not a one-time event but a dynamic, multidisciplinary process. As one analysis notes, a TPP should be used throughout the drug development process, from the pre-IND (Investigational New Drug) phase to the post-marketing phase [25]. When shared with regulatory bodies like the FDA, a TPP can facilitate efficient dialogue, minimize the risk of late-stage failures, and potentially decrease total development time [25]. Evidence of its value is seen in data showing that applications with a TPP had a significantly lower "refuse to file" decision from the FDA and were approved approximately one month faster on average [25].
Key Components of a Target Product Profile
The specific features within a TPP can vary widely, but they generally encompass several key categories that define the product's value proposition and critical path. The table below summarizes common TPP features based on a systematic review of their use.
Table 1: Common Features of a Target Product Profile (TPP)
| Feature Category | Description | Example Attributes |
|---|---|---|
| Purpose/Context of Use | The intended use case and clinical setting for the product [4]. | Target disease, patient population, care setting (e.g., hospital, clinic). |
| Efficacy & Safety | The desired therapeutic benefit and acceptable risk profile. | Primary endpoints, effect size, contraindications, adverse event tolerability. |
| Dosage & Formulation | The intended route of administration and product characteristics. | Dosage form (e.g., tablet, injectable), shelf life, storage conditions [4]. |
| Validation Aspects | Evidence required to demonstrate product performance and quality [4]. | Clinical trial data, analytical performance criteria, manufacturing standards. |
Cross-Functional Teams: Bridging Strategy and Execution
While the TPP sets the destination, cross-functional teams are the engine that drives the project toward it. Cross-functional collaboration is the process of combining expertise from various departments to work toward a shared goal [24]. In pharmaceutical development, this means breaking down traditional silos between R&D, medical affairs, marketing, and sales to create unified strategies.
The benefits of this integrated approach are substantial. Collaboration helps bridge critical gaps by combining diverse expertise. For instance, medical affairs provide valuable insights into clinical data, ensuring sales teams communicate accurate, evidence-based information, while marketing teams develop compelling messaging that resonates with target audiences [24]. This alignment is crucial for building trust and credibility among healthcare professionals and can directly translate to stronger relationships and higher prescription rates [24]. Furthermore, when sales and medical teams work together, they can better identify and address potential regulatory compliance issues before they become costly mistakes [24].
Table 2: Impact of Cross-Functional Collaboration on Drug Development Outcomes
| Performance Metric | Siloed Approach (Low Collaboration) | Integrated Cross-Functional Approach |
|---|---|---|
| Strategic Alignment | Conflicting messages and duplicated efforts [24]. | Unified messaging and streamlined processes [24]. |
| Regulatory Compliance | Higher risk of non-compliance and costly late-stage failures [24]. | Proactive issue identification; 1-month faster FDA approval time on average [25]. |
| Commercial Success | Underperforming sales and missed opportunities [24]. | Product launch surpassing sales targets within first year [24]. |
| Stakeholder Trust | Inconsistent information erodes credibility with healthcare providers [24]. | Consistent, evidence-based communication builds stronger relationships [24]. |
Experimental Protocol: Measuring Collaboration's Impact on TPP Alignment
To objectively assess the value of cross-functional teams, one can design a study that measures how effectively a product's final, actual profile matches its initial TPP.
Methodology
- Study Design: A retrospective cohort analysis comparing drug development projects within a portfolio or across companies.
- Group Definition:
- Cohort A (High Collaboration): Projects that implemented structured cross-functional collaboration (e.g., regular cross-functional meetings, joint KPIs, shared dashboards) from the TPP stage onward [24].
- Cohort B (Low Collaboration): Projects that operated primarily within functional silos with limited structured interaction.
- Data Collection: For each project, collect the following data points:
- Version 1.0 of the TPP document.
- The final product label approved by the regulatory authority.
- Development timeline data (e.g., from IND to NDA/BLA submission).
- Key decision-point documents (e.g., go/no-go decisions at stage gates).
- Primary Outcome Measure - TPP Alignment Score: A quantitative score reflecting the percentage of TPP attributes (from Table 1) that were successfully achieved in the final product label without significant modification or dilution.
- Secondary Outcome Measures: Total development time; incidence of major regulatory setbacks; first-year sales performance versus forecast.
The Cross-Functional TPP Development Workflow
The following diagram visualizes the integrated workflow that characterizes an effective, cross-functional approach to TPP development and execution. This process ensures all stakeholder perspectives are incorporated from the beginning.
The Researcher's Toolkit for Cross-Functional Alignment
Successfully implementing a cross-functional TPP process requires more than just goodwill; it requires specific tools and strategies to foster effective teamwork and measure outcomes.
Table 3: Essential Tools for Cross-Functional Team Management
| Tool or Strategy | Function in Development | Impact on TPP Alignment |
|---|---|---|
| Joint Key Performance Indicators (KPIs) [24] | Shared performance metrics that ensure all departments strive for the same goals. | Aligns incentives across functions, directly tying activities to the achievement of TPP attributes. |
| AI-Powered Analytics [24] | Analyzes data trends to predict healthcare professional needs and optimize engagement. | Provides data-driven insights to refine the TPP and commercial strategy based on real-world evidence. |
| Shared Communication Platforms [24] | Project management and communication channels for easy task management across teams. | Ensures transparency and keeps all stakeholders informed on progress and challenges related to TPP goals. |
| Frequent Cross-Functional Meetings [24] | Regular meetings to promote openness, stimulate idea sharing, and resolve disputes. | Provides a formal forum for addressing misalignments with the TPP early before they become major issues. |
| Stakeholder Engagement Plans | A proactive plan for managing communication with all key internal and external stakeholders [26]. | Facilitates efficient dialogue with regulators and partners, directly supporting the TPP's critical path [25]. |
The journey from a target product profile to a successful actual product is complex and non-linear. The evidence demonstrates that a TPP is a necessary but insufficient component for success. Its ultimate power is unlocked only when it is embraced and driven by a truly cross-functional team. The synergistic collaboration between R&D, medical, commercial, and regulatory functions ensures that the product vision is not only scientifically ambitious but also clinically relevant, commercially viable, and regulatorily sound. In an era of increasing development costs and heightened competition, fostering a culture of cross-functional collaboration is not merely a best practice—it is a critical strategic imperative for any organization aiming to deliver meaningful innovations to patients efficiently and successfully.
Target Product Profile (TPP) optimization serves as a foundational strategic process in pharmaceutical development, typically conducted 2-3 years before market entry. This research enables organizations to navigate the significant uncertainty of pre-launch planning when final clinical trial results remain unknown. By evaluating how various clinical trial outcomes influence physician prescribing decisions and market opportunity, TPP optimization allows teams to forecast multiple demand scenarios and create a working hypothesis for what the product will become. This strategic foundation directly informs clinical development decisions, regulatory negotiations, and promotional planning based on market potential, ultimately aligning commercial strategy with anticipated product characteristics [17].
When framed within the broader context of target product profile versus actual profile research, TPP optimization represents the proactive, strategic phase that establishes the target, while subsequent research tracks how the actual product characteristics emerging from clinical trials measure against this initial vision. This comparative analysis is crucial for making iterative development decisions and preparing for market entry.
Methodological Approaches for Endpoint Prioritization
Conjoint Analysis for Quantitative Endpoint Valuation
Conjoint analysis represents a cornerstone quantitative method in TPP optimization research. This technique systematically presents physicians with profiles containing different combinations of clinical endpoints and measures their preferences, allowing researchers to quantify the relative importance of different attributes and simulate market share under various scenarios [17].
Experimental Protocol:
- Stimulus Design: Develop comprehensive but concise TPP descriptions that include all information physicians require for treatment decisions without overwhelming detail. Present information across TPP scenarios using identical formats and language to isolate the impact of specific variables [17].
- Attribute Selection: Identify clinically meaningful endpoints that exceed physicians' minimum threshold for clinical meaningfulness. Focus variation on attributes with significant impact on treatment selection rather than statistically interesting but clinically irrelevant differences [17].
- Data Collection: Implement through specialized physician surveys that present balanced combinations of clinical attributes. Ensure sufficient sample size for robust statistical analysis across relevant specialist types and geographic regions.
- Analysis Phase: Employ statistical models, including regression analysis and maximum difference scaling, to calculate utility values for each endpoint and simulate preference shares for different TPP configurations.
Qualitative Exploration of Decision Drivers
Before quantitative validation, in-depth qualitative interviews identify key decision drivers and barriers while refining TPP presentation to ensure clarity and relevance [17]. This exploratory phase examines both rational and emotional factors driving treatment decisions through functional benefits laddering (tracing how specific clinical endpoints create functional benefits) and emotional drivers mapping (identifying how clinical outcomes translate into emotional benefits such as confidence and reduced anxiety) [17].
Experimental Protocol:
- Participant Recruitment: Recruit high-prescribing physicians across key specialties and practice settings, ensuring representation of diverse perspectives.
- Interview Guide Development: Create semi-structured discussion guides that explore clinical decision-making without leading participants.
- Analysis Framework: Implement systematic coding of interview transcripts to identify recurring themes, decision hierarchies, and potential barriers to adoption.
Multi-Method Integration for Robust Insights
The most robust TPP optimization integrates multiple complementary methodologies, including qualitative exploration, conjoint analysis, and interactive simulation tools that allow teams to model market impact as clinical development progresses and data evolves [17].
Table 1: Comparison of TPP Research Methodologies
| Methodology | Primary Application | Data Output | Sample Requirements | Key Advantages |
|---|---|---|---|---|
| Conjoint Analysis | Quantifying endpoint importance | Utility scores, market simulations | 100-300 physicians | Measures trade-offs in realistic scenarios |
| Discrete Choice Modeling | Evaluating complete profiles | Preference shares, attribute importance | 100-200 physicians | Mimals real-world decision processes |
| Qualitative Interviews | Exploring decision drivers | Thematic insights, vocabulary | 20-40 physicians | Uncovers underlying reasoning |
| Interactive Simulation | Dynamic scenario modeling | Forecast adjustments | Tool for internal teams | Enables real-time strategy testing |
Research Implementation and Operational Framework
Strategic TPP Design Principles
Effective TPP optimization requires careful attention to design, execution, and activation across multiple dimensions [17]. Successful TPP design balances comprehensiveness with clarity through several key principles:
- Comprehensive but Concise: Include all information physicians require for treatment decisions without overwhelming detail that obscures key drivers [17].
- Consistently Structured: Present information across TPP scenarios using identical formats and language to isolate the impact of specific variables [17].
- Clinically Authentic: Use language and outcome measures that reflect how physicians actually evaluate treatments in practice [17].
- Visually Accessible: Employ clear visual hierarchy that highlights key information and facilitates rapid comparison across scenarios [17].
Experimental Workflow for TPP Optimization
The following diagram illustrates the standard workflow for conducting TPP optimization research:
Integration with Development Decision-Making
TPP optimization delivers maximum impact when integrated into broader development planning across the organization [17]. This integration occurs through several key pathways:
- Clinical Development Integration: TPP insights should directly inform clinical trial design and data analysis through endpoint prioritization, subgroup analysis planning, and regulatory strategy development [17].
- Dynamic Forecasting: TPP optimization enables more sophisticated launch forecasting through scenario-based modeling, attribute-level sensitivity analysis, and patient-level segmentation [17].
- Promotional Strategy Alignment: TPP research should directly shape promotional planning through message prioritization, patient identification strategies, and differentiation strategy [17].
Key Challenges and Methodological Considerations
TPP optimization research faces several significant challenges that can compromise research validity if not properly addressed [17]:
- Information Overload: TPPs often contain excessive clinical detail, overwhelming physicians and obscuring key decision factors [17].
- Insufficient Context: TPPs may lack essential details physicians need to make realistic treatment decisions, creating artificial evaluations that don't reflect actual clinical decision-making [17].
- Unrealistic Scenarios: Organizations frequently test overly optimistic clinical outcomes that are unlikely to materialize in actual trials, producing inflated market share projections [17].
- Marginal Differentiation: Testing clinically insignificant differences that wouldn't influence real-world prescribing wastes research investment on distinctions physicians don't find meaningful [17].
Table 2: Common TPP Research Challenges and Mitigation Strategies
| Research Challenge | Impact on Data Quality | Mitigation Approach | Validation Technique |
|---|---|---|---|
| Information Overload | Respondent fatigue, reduced discrimination | Limit to 6-8 key attributes, use tiered information | Cognitive interviewing during pretesting |
| Unrealistic Scenarios | Inflated preference estimates | Partner with medical teams on realistic outcomes | Historical benchmarking against past launches |
| Marginal Differentiation | Inaccurate market share projections | Focus on clinically meaningful differences | Statistical testing for preference significance |
| Sample Representation | Non-generalizable findings | Stratified sampling by prescription volume | Balance checks against market data |
The Scientist's Toolkit: Essential Research Solutions
Table 3: Key Research Reagent Solutions for TPP Optimization
| Research Tool | Primary Function | Application in TPP Research | Implementation Considerations |
|---|---|---|---|
| Professional Respondent Panels | Physician recruitment | Access to high-prescribing specialists | Validate prescribing volume, specialty mix |
| Conjoint Analysis Software | Experimental design and data collection | Administer choice tasks, calculate utilities | Ensure healthcare-specific algorithms |
| Statistical Analysis Packages | Advanced analytics | Regression, cluster analysis, forecasting | Include proprietary market models |
| Interactive Simulation Platforms | Scenario modeling | Dynamic forecasting based on TPP changes | Real-time adjustment capabilities |
TPP optimization research provides the essential foundation for successful pharmaceutical launch planning by rigorously evaluating how clinical endpoints influence physician decisions and market opportunity. Through methodologically sound approaches that balance comprehensive clinical information with clear presentation, focus on meaningful variation, and integrate multiple methodologies, organizations can make informed choices about clinical development despite pre-launch uncertainty [17].
The most effective TPP optimization examines both rational and emotional decision drivers, employs robust quantitative techniques like conjoint analysis, and directly connects research findings to strategic decisions across clinical, regulatory, and commercial functions. When fully integrated into development planning, these insights enable more accurate forecasting, more efficient clinical development, and more compelling market preparation strategies, ultimately bridging the critical gap between target product profile and actual product profile throughout the drug development lifecycle.
A Target Product Profile (TPP) serves as the strategic cornerstone of pharmaceutical launch planning, typically developed 2-3 years before market entry. This critical document transitions from an aspirational outline to an active framework that guides clinical development and regulatory negotiations. By evaluating how various clinical trial outcomes influence physician prescribing decisions and market opportunity, organizations can develop realistic launch scenarios and align commercial strategy with anticipated product characteristics. This foundational research enables brand teams to navigate the uncertainty of pre-launch planning when final clinical trial results remain unknown, transforming the TPP from a static document into a dynamic tool for strategic decision-making [17].
Within the context of target product profile versus actual profile research, the TPP provides a working hypothesis for what the product will become, creating an essential anchor for positioning, messaging, and promotional planning. This working definition enables meaningful commercial planning despite the absence of final clinical data. Effective TPP optimization fulfills two critical strategic functions for pre-launch brands: scenario planning that allows teams to forecast multiple demand scenarios (base case, best case, worst case), and product definition that provides clarity for countless decisions required before final product characteristics are known [17].
TPP Optimization Framework: From Concept to Operational Strategy
Strategic TPP Design Principles
Successful TPP optimization begins with thoughtful stimulus design that balances comprehensiveness with clarity. Effective TPPs share several key characteristics that enhance their utility in clinical trial design and regulatory strategy. They must be comprehensive but concise—including all information physicians require for treatment decisions without overwhelming detail that obscures key drivers. A consistent structure is essential, presenting information across TPP scenarios using identical formats and language to isolate the impact of specific variables. Clinical authenticity ensures the TPP uses language and outcome measures that reflect how physicians actually evaluate treatments in practice, while visual accessibility employs clear visual hierarchy that highlights key information and facilitates rapid comparison across scenarios [17].
Overcoming Common TPP Research Challenges
The complexity of pre-launch product definition creates several key challenges in TPP research that can undermine its effectiveness. Organizations must navigate these obstacles to generate actionable insights that drive launch success. A frequent issue is information overload, where TPPs contain excessive clinical detail that overwhelms physicians and obscures key decision factors. Conversely, insufficient context occurs when TPPs lack essential details physicians need to make realistic treatment decisions, creating artificial evaluations that don't reflect actual clinical decision-making. Unrealistic scenarios represent another common pitfall, where organizations test overly optimistic clinical outcomes that are unlikely to materialize in actual trials, skewing conjoint analysis results and producing inflated market share projections. Additional challenges include marginal differentiation (testing clinically insignificant differences that wouldn't influence real-world prescribing) and excessive complexity (testing too many clinical scenarios, attributes, or levels) [17].
Methodological Best Practices for Robust TPP Development
The most robust TPP optimization employs multiple complementary methodologies to generate reliable, actionable insights. A multi-method approach should include qualitative exploration through in-depth interviews to identify key decision drivers and barriers while refining TPP presentation to ensure clarity and relevance. Conjoint analysis quantitatively assesses the relative importance of different attributes and simulates market share under various scenarios. Interactive simulation provides teams with dynamic tools to model market impact as clinical development progresses and data evolves [17].
Effective TPP optimization must also focus on meaningful variation rather than statistically interesting but clinically irrelevant differences. This requires close partnership with medical teams to identify realistic trial outcomes based on current data, establishing clinical significance thresholds that test differences exceeding physicians' minimum threshold for clinical meaningfulness, and concentrating variation on attributes with significant impact on treatment selection [17].
Furthermore, sophisticated TPP optimization examines both rational and emotional factors driving treatment decisions through functional benefits laddering (tracing how specific clinical endpoints create functional benefits for patients and physicians), emotional drivers mapping (identifying how clinical outcomes translate into emotional benefits such as confidence, hope, and reduced anxiety), and understanding physicians' cognitive processes when evaluating how novel treatment profiles may impact future prescribing decisions [17].
Quantitative Benchmarking: Probability of Success Across Development Parameters
Understanding historical success rates for different drug characteristics provides crucial benchmarking data for TPP development. Recent research examining 3,999 compounds developed in the United States, European Union, or Japan that began Phase I trials between 2000 and 2010 revealed an overall success rate of 12.8% from clinical trial initiation to marketing approval [27]. This comprehensive analysis identified significant variations in approval success rates based on specific drug parameters including target, action, modality, and therapeutic application.
Table 1: Drug Approval Success Rates by Target, Action, and Modality
| Parameter | Category | Approval Success Rate |
|---|---|---|
| Drug Target | Enzyme | 31.3% [27] |
| Drug Action | Stimulant | 34.1% [27] |
| Drug Modality | Biologics (excluding mAb) | 31.3% [27] |
| Drug Modality | Monoclonal Antibody | Data not available in search results |
| Drug Modality | Small Molecule | Lower than biologics [27] |
Table 2: Drug Approval Success Rates by Therapeutic Application (ATC Code)
| ATC Code | Therapeutic Application | Approval Success Rate |
|---|---|---|
| A | Alimentary tract and metabolism | Data not available in search results |
| B | Blood and blood forming organs | Statistically higher [27] |
| C | Cardiovascular system | Data not available in search results |
| D | Dermatologicals | Data not available in search results |
| G | Genito-urinary system and sex hormones | Statistically higher [27] |
| J | Anti-infectives for systemic use | Statistically higher [27] |
Univariate and multivariate logistic regression analyses revealed that stimulant as drug action and "B" (blood and blood forming organs), "G" (genito-urinary system and sex), and "J" (anti-infectives for systemic use) as drug application were statistically associated with high approval success rates [27]. These parameters and their combinations provide valuable benchmarking data for evaluating the probability of success of drug candidates.
Experimental Protocols for TPP-Informed Clinical Development
Database Creation and Compound Categorization Methodology
To generate reliable benchmarking data for TPP development, researchers must employ systematic data collection and categorization protocols. The experimental approach should begin with identifying drug candidates that started Phase I trials in major markets (United States, European Union, or Japan) within a defined period, typically using commercial databases like Pharmaprojects. Combination products, biosimilars, vaccines, diagnostic products, and compounds in the preclinical stage should be excluded from the analysis [27].
Selected compounds must then be categorized according to development status, defined as the development stage of the drug candidate with the most progressed indication. Classification should include: Phase I, Phase II, Phase III, Succeeded (including launched, withdrawn, registered, and preregistration), and Discontinued (including discontinued, no development reported, and suspended). Compounds under phases I, II, and III with unclear results should be excluded from the analysis [27].
The remaining compounds require categorization according to four critical parameters (target, action, modality, and application) based on information obtained from databases and public sources (including research papers and company press releases). Target categorization should include: receptor, enzyme, ligand, ion channel, transporter, other (proteins related to cytoskeleton, extracellular matrix, apoptosis, etc.), and target unknown. Action categorization (MOA of drug candidate) should include: inhibitor, agonist, antagonist, stimulant (target-stimulating agents), other (including enhancer, desensitizer, modulator, etc.), and action unknown. Modality categorization should include: small molecule, monoclonal antibody (mAb), biologics (excluding mAb), and novel modalities (including nucleic acid, cell therapy, gene therapy, etc.). Application categorization should use the Anatomical Therapeutic Chemical (ATC) classification system ("A" to "V") [27].
Statistical Analysis Framework for Success Rate Determination
For robust probability of success assessment, statistical analysis should employ both univariate and multivariate logistic regression analyses to identify parameters and combinations statistically associated with high approval success rates. This methodology allows researchers to control for confounding variables and identify independent predictors of development success. The analysis should specifically examine combination categories where multiple parameters intersect to influence success probabilities, as these often provide the most actionable insights for TPP development [27].
Integration of Dynamic Benchmarking into TPP Strategy
Traditional benchmarking approaches often rely on static, outdated data that fails to reflect the most current drug development landscape. These legacy solutions frequently suffer from data completeness issues, as new drug development data that can inform and refine benchmarking is generated daily, yet most existing benchmarking solutions are updated infrequently. Additional limitations include data availability and quality problems, where data used for benchmarking is often provided at a high level and is unstructured and not detailed enough to obtain reliable benchmarks. For example, to obtain an accurate benchmark for a drug treating HER2-negative breast cancer, looking broadly at oncology or even breast cancer data is insufficient. More detailed data sets that provide program-based historical approval rates are needed to understand the different factors that impact the success of a novel drug targeting a specific cancer or cancer subtype [28].
Data aggregation in traditional approaches also has severe limits as it does not consider all relevant information. For example, innovative drug pipelines, e.g., those that skip phases or have dual phases, are often not accounted for. Limited data search and filtering capabilities restrict users' ability to sort data by a multitude of dimensions, including advanced filtering options essential for making accurate assessments. Typical one-size-fits-all approaches to data manipulation and filtering limit the usefulness of the data and do not allow for benchmarking for exact treatment settings. Perhaps most significantly, subpar methodology in traditional approaches generates Probability of Success (POS) calculations by simply multiplying phase transition success rates. This overly simplistic approach tends to overestimate a drug's success rate, resulting in less-than-ideal data for decision-making [28].
Advanced benchmarking solutions address these limitations through dynamic approaches that incorporate several key enhancements. Data collection and curation pipelines that incorporate new data in close to real-time ensure that the most accurate and current information is always applied to benchmarks. Expertly curated, rich data that captures sponsor-agnostic interventional, industry-led FDA track trials provides an unbiased view of past success rates from a broad range of pharmaceutical sponsors for comprehensive historical clinical benchmarking data. Advanced data aggregation methods enable deeper insights and a better understanding of the different factors that impact drug development success (e.g., skipped phases or dual phases in non-standard drug development). Advanced and flexible search and filtering options based on proprietary ontologies allow customized deep dives into the data, generating insights even in uncommon or complex treatment settings. Most importantly, refined benchmarking methodologies account for different possible development paths without assuming a typical progression, yielding more accurate POS assessments than traditional benchmarking methodologies can provide [28].
Visualizing TPP Integration: Strategic Workflow
TPP Integration Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for TPP-Informed Development
| Research Tool | Function | Application in TPP Development |
|---|---|---|
| Pharmaprojects Database | Commercial database tracking drug development pipelines | Provides historical clinical trial success rates for benchmarking [27] |
| Dynamic Benchmarking Platforms | Real-time data aggregation and analysis tools | Enables accurate probability of success calculations [28] |
| Conjoint Analysis Software | Quantifies physician preference for clinical attributes | Measures relative importance of different endpoints in TPP [17] |
| Anatomical Therapeutic Chemical (ATC) Classification | World Health Organization drug classification system | Standardizes therapeutic application categorization [27] |
| Multi-Attribute Utility Instruments | Patient-reported outcome measurement tools | Captures patient preferences for inclusion in TPP optimization |
Strategic Implementation for Launch Success
Clinical Development Integration
TPP insights should directly inform clinical trial design and data analysis through three key mechanisms. Endpoint prioritization focuses clinical resources on the endpoints with greatest impact on prescribing decisions, ensuring efficient trial design. Subgroup analysis planning identifies patient populations where product benefits are most compelling and ensures sufficient power for these analyses. Regulatory strategy development establishes label negotiation priorities based on the relative importance of different clinical attributes, maximizing the chances of successful market authorization [17].
Dynamic Forecasting Applications
TPP optimization enables more sophisticated launch forecasting through scenario-based modeling that creates forecasts reflecting the range of potential clinical outcomes rather than single-point estimates. Attribute-level sensitivity analysis understands how specific endpoints influence uptake curves and peak share, allowing for more precise resource allocation. Patient-level segmentation models differential uptake across patient types based on varying profiles, enabling targeted launch strategies [17].
Promotional Strategy Alignment
TPP research should directly shape promotional planning through message prioritization that focuses promotional messaging on the clinical attributes with greatest influence on prescribing. Patient identification develops targeting strategies for the patient types most likely to benefit from the product. Differentiation strategy creates positioning that emphasizes the most meaningful areas of product differentiation based on empirical physician preference data [17].
Target Product Profile optimization provides the essential foundation for successful pharmaceutical launch planning by creating a critical bridge between document-based aspirations and actionable clinical development strategies. By rigorously evaluating how clinical endpoints influence physician decisions and market opportunity, organizations can make informed choices about clinical development, regulatory strategy, and promotional planning despite pre-launch uncertainty. The integration of dynamic benchmarking data that reflects current development landscapes and specific product characteristics—including drug target, action, modality, and therapeutic application—enables more accurate probability of success assessments than traditional static benchmarking approaches. When fully integrated into clinical development and regulatory planning, these insights enable more efficient resource allocation, more compelling product differentiation, and ultimately, greater likelihood of successful market entry and patient access to innovative therapies.
Bridging the Gap: Overcoming Common TPP Pitfalls and Adaptation Strategies
Identifying the Root Causes of a Divergent Actual Profile
In the structured landscape of drug development, the Target Product Profile (TPP) serves as a strategic compass. It is a comprehensive document that outlines the desired characteristics of a planned product—including its efficacy, safety, and dosage—to guide development and facilitate communication among stakeholders [4]. The Actual Profile is the final set of characteristics demonstrated by the developed product at the end of the process.
A divergent actual profile exists when there is a significant discrepancy between these planned and realized outcomes. Such a divergence can jeopardize regulatory approval, market access, and the commercial viability of a new therapeutic. For researchers and drug development professionals, systematically identifying the root causes of these divergences is critical for de-risking development pipelines and improving the efficiency of translational research [4] [14]. This guide provides a structured framework for this analysis, comparing investigative methodologies and providing actionable protocols.
A Framework for Root Cause Analysis
Root cause analysis of a TPP-Actual profile divergence should be a systematic, multi-phase investigation. The process moves from accurately quantifying the gap to identifying its underlying origins. The following workflow outlines this structured approach.
Core Investigative Methodologies
No single methodology can uncover all potential causes of divergence. A robust analysis employs a combination of the following quantitative and qualitative approaches.
Table 1: Comparative Analysis of Root Cause Investigation Methods
| Method | Description | Best Suited for Identifying | Key Limitations |
|---|---|---|---|
| Model Interrogation | Re-examining the mathematical models used to set TPP targets [14]. | Flaws in target-setting logic; over-optimistic projections of efficacy or health impact. | Model structure may not capture real-world biological complexity. |
| Preclinical Data Audit | Systematic re-analysis of raw data from in vitro and in vivo studies. | Translational failures; misleading biomarker data; unheeded toxicity signals. | Animal models may not fully recapitulate human disease. |
| Clinical Trial Post-Mortem | Detailed analysis of patient subpopulations, adherence, and trial operations. | Issues with patient stratification, dosing regimens, and trial execution. | Costly and time-consuming; requires access to full trial dataset. |
| Stakeholder Consensus Building | Structured interviews or surveys with internal and external experts [4]. | Unvalidated assumptions; shifting market or regulatory requirements. | Subject to cognitive biases and groupthink if not managed correctly. |
Experimental Protocols for Root Cause Identification
Protocol: Interrogating TPP-Informing Models
Mathematical models are frequently used to set target values for attributes like clinical efficacy and economic value [14]. This protocol outlines steps to validate these models when a divergence occurs.
Objective: To determine if the divergence stems from flaws in the original models used to define TPP targets. Workflow:
Key Research Reagents & Tools:
- Comparative Datasets: Independent clinical or real-world datasets for external validation.
- Sensitivity Analysis Software: Tools like R, Python (with libraries like SALib), or specialized commercial software to quantify parameter influence.
- Computational Infrastructure: High-performance computing resources may be needed for complex model re-runs and uncertainty analyses.
Protocol: Analyzing Clinical Biomarker Translation
A common point of divergence is the performance of a pharmacodynamic or predictive biomarker in clinical trials compared to preclinical models.
Objective: To identify why a biomarker that was robust in preclinical studies failed to predict clinical outcome. Workflow:
Key Research Reagents & Tools:
- Validated Assay Kits: The same immunoassay or molecular kit used in clinical trials should be used to re-test preclinical samples.
- Biobank Samples: Well-annotated, archived samples from both preclinical models and clinical trial subjects.
- LIMS (Laboratory Information Management System): Essential for tracking sample chain of custody and associated metadata.
Comparative Data: Quantifying Common Divergences
Understanding common divergence points allows teams to proactively monitor and mitigate risks. The following table synthesizes findings from a scoping review on the use of modelling in TPPs, highlighting attributes frequently informed by models and their associated risks [14].
Table 2: Common TPP Attributes and Associated Divergence Risks
| TPP Attribute Category | Specific Attribute | Common Modelling/Assumption Approach | Frequent Divergence Root Cause |
|---|---|---|---|
| Efficacy | Clinical Efficacy | Extrapolation from preclinical models; pharmacodynamic modelling [14]. | Poor translatability of animal models; incorrect exposure-response relationship. |
| Dosage & Administration | Dosage Regimen | Pharmacokinetic/Pharmacodynamic (PK/PD) modelling and simulation. | Unpredicted human metabolism; drug-drug interactions in diverse populations. |
| Safety | Safety/Tolerability Profile | Toxicology studies in animals; off-target profiling. | Species-specific toxicities; rare adverse events not detectable in small trials. |
| Value & Impact | Economic Value/Health Impact | Health economic modelling early in development [14]. | Shifting competitive landscape; incorrect assumptions about standard of care. |
| Product Stability | Shelf-life | Accelerated stability studies under controlled conditions. | Unforeseen degradation pathways in real-world storage conditions. |
Identifying the root causes of a divergent actual profile is not merely a retrospective exercise; it is a critical investment in future development efficiency. The systematic application of the frameworks, protocols, and comparative analyses outlined in this guide enables research teams to move from acknowledging failure to understanding it.
This process transforms a divergence from a setback into a valuable source of institutional knowledge. The insights gained should be formally documented and integrated into organizational practices, directly informing the development of future TPPs to make them more robust, data-driven, and resilient [4] [14]. Ultimately, a culture that rigorously investigates divergence is one that significantly enhances its probability of translational success.
In the strategic landscape of pharmaceutical development and academic research, the Target Product Profile (TPP) serves as a critical planning tool to guide product development and align stakeholders. A TPP is a strategic document outlining the desired characteristics of a planned product, procedure, or service intended for a particular disease or use case, with the goal of addressing user needs and facilitating communication [4]. However, the development and application of TPPs are fraught with significant challenges, particularly information overload and the creation of unrealistic scenarios, which can undermine their effectiveness and lead to flawed strategic decisions. This guide examines these challenges through a comparative lens, evaluating their impact on research validity and development efficiency.
Quantitative Analysis of TPP Research Challenges
A systematic review of TPP applications across health fields reveals substantial variability in how TPPs are structured and reported, directly contributing to the challenges of information overload and unrealistic expectations. The following table summarizes key quantitative findings from the analysis of 138 papers developing TPPs.
Table 1: Analysis of TPP Feature Variation and Methodological Reporting
| Analysis Category | Findings | Implication for Research Challenges |
|---|---|---|
| TPP Feature Count Variation | Wide variation across and within product types (3-44 features) [4] | Direct contributor to information overload; lack of standardization |
| Performance Threshold Levels | 57.8% of TPPs featured only one threshold level of product performance [4] | Increases risk of unrealistic scenarios by lacking minimal/ideal distinctions |
| Methodological Reporting | Majority of papers did not describe methods used for TPP development [4] | Obscures validation processes and increases potential for unrealistic assumptions |
| Primary Product Focus | 41.3% (n=57) focused on therapeutics [4] | Domain-specific challenges may require tailored approaches |
| Author Affiliation | 56.5% of papers (n=78) authored by academics [4] | Potential methodological differences between academic and industry practices |
Experimental Protocols for Investigating TPP Challenges
Protocol 1: Assessing Information Overload in TPP Comprehension
Objective: To quantitatively measure how TPP design characteristics impact stakeholder comprehension and decision-making accuracy.
Methodology:
- Stimulus Design: Create multiple TPP versions varying in structure and density:
Participant Recruitment: Recruit physician respondents (n≥100) with prescribing authority in the relevant therapeutic area.
Testing Procedure:
- Administer conjoint analysis to quantify how clinical endpoints influence prescribing decisions [17]
- Measure comprehension accuracy using standardized questions about key TPP parameters
- Record decision-time metrics to assess cognitive load
- Conduct qualitative debriefs to identify specific points of confusion or overload
Data Analysis:
- Apply statistical analysis to identify correlation between TPP complexity and comprehension errors
- Calculate cognitive load indices based on decision-time and accuracy metrics
- Thematically analyze qualitative feedback to identify specific information overload triggers
Protocol 2: Evaluating Unrealistic Scenario Impact on Forecast Accuracy
Objective: To determine how unrealistic clinical outcomes in TPPs influence market share projections and development decisions.
Methodology:
- Scenario Development: Create three TPP scenarios with varying levels of clinical optimism:
Experimental Implementation:
Outcome Measurement:
- Compare forecast accuracy between scenarios after 24-month post-launch period
- Assess resource allocation decisions triggered by each scenario type
- Measure variance between projected and actual market share
Validation Framework:
Visualizing TPP Challenge Relationships and Workflows
Diagram 1: Relationship map showing how root causes in TPP design contribute to core research challenges and their downstream impacts. The visualization highlights the interconnected nature of these problems and their collective effect on development efficiency.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Methodological Solutions for Addressing TPP Research Challenges
| Research Solution | Function | Application Context |
|---|---|---|
| Structured TPP Templates | Standardizes feature inclusion and presentation format | Reduces information overload through consistent formatting and logical organization [17] |
| Dual-Threshold Framework | Defines both minimal acceptable and ideal performance targets | Mitigates unrealistic scenarios by establishing achievable benchmarks [4] |
| Conjoint Analysis Tools | Quantifies how clinical endpoints influence prescribing decisions | Identifies which features truly drive decisions versus creating cognitive noise [17] |
| Dynamic Forecasting Models | Creates scenario-based projections reflecting clinical outcome ranges | Enables more accurate planning by modeling best-case, base-case, and worst-case scenarios [17] |
| Multi-Stakeholder Consensus Framework | Formal process for building alignment among diverse stakeholders | Addresses methodological gaps in TPP development through structured validation [4] |
Comparative Analysis: TPP Versus Actual Profile Research
When evaluating TPP against actual product profiles, distinct patterns emerge in how challenges manifest across the development lifecycle. Information overload in TPP research typically stems from attempting to address all potential stakeholder concerns prematurely, resulting in documents that obscure key decision factors with excessive detail [17]. In contrast, actual profile research often suffers from information fragmentation, where critical data exists in isolated systems rather than integrated strategic documents.
Regarding unrealistic scenarios, TPP research frequently exhibits optimism bias in clinical outcomes, with 57.8% of TPPs featuring only one threshold level of product performance rather than minimal/ideal distinctions [4]. This "splitting hairs" approach wastes research investment on clinically insignificant distinctions [17]. Actual profile research faces the opposite challenge—conservative interpretation of real-world evidence that may underestimate product potential.
The most significant methodological difference lies in validation approaches. TPP development often lacks transparent methodological reporting, with most papers not describing development methods [4]. Actual profile research typically employs rigorous statistical validation but may lack the strategic context to inform development decisions effectively.
The comparative analysis of TPP versus actual profile research reveals that addressing information overload and unrealistic scenarios requires standardized methodological frameworks and validation processes. The quantitative data demonstrates significant variability in TPP application, with feature counts ranging from 3-44 and majority of TPPs employing single-threshold performance metrics [4]. By implementing the experimental protocols and research solutions outlined in this guide, researchers and drug development professionals can enhance TPP utility, improve forecast accuracy, and ultimately streamline the development pathway from concept to market. The integration of strategic TPP design principles with rigorous validation methodologies represents the most promising approach to overcoming these persistent challenges.
In pharmaceutical development, the Target Product Profile (TPP) serves as a strategic planning tool that outlines the desired characteristics of a prospective drug, guiding research from conception to commercialization. When effectively utilized, TPPs align cross-functional teams, clarify regulatory pathways, and increase the likelihood of launching successful therapies. However, when implemented rigidly, these same strategic tools can paradoxically stifle innovation, constrain adaptive development, and blind organizations to emerging market opportunities and competitive threats. This analysis examines the critical balance required in TPP development and management, comparing optimal versus problematic applications through experimental data and case studies relevant to researchers, scientists, and drug development professionals.
Defining the TPP: Purpose and Ideal Implementation
A Target Product Profile is fundamentally a strategic planning document that specifies the desired attributes of a new therapeutic product, including its intended use, target populations, efficacy and safety parameters, dosage form, and route of administration [3]. Regulatory agencies such as the FDA view TPPs as strategic development tools that help focus discussions and facilitate more productive regulatory interactions [29]. The World Health Organization utilizes TPPs to guide health product research and development, specifying both minimal and optimal characteristics to ensure products address public health needs while considering access, equity, and affordability [20] [3].
In ideal implementation, TPPs serve as living documents that evolve throughout the development lifecycle. They require input from diverse stakeholders including preclinical scientists, medical experts, regulatory specialists, commercial analysts, and manufacturing professionals [30]. This collaborative approach ensures the TPP balances scientific feasibility with commercial viability, regulatory requirements, and patient needs.
Table 1: Core Components of an Effective Target Product Profile
| TPP Component | Strategic Function | Development Impact |
|---|---|---|
| Target Indication & Population | Defines intended patient population and medical need | Affects trial design, endpoints, and recruitment strategy |
| Safety Profile | Sets risk tolerance and benefit-risk balance | Influences regulatory pathway and monitoring requirements |
| Efficacy Claims | Specifies clinical benefits and differentiation | Determines commercial positioning and value proposition |
| Dosage & Administration | Defines formulation and delivery system | Impacts patient compliance and manufacturing complexity |
| Commercial Framework | Addresses market access and pricing considerations | Guides evidence generation for payers and providers |
Methodological Framework: Analyzing TPP Implementation
To evaluate how TPPs influence innovation outcomes, we examined three real-world case studies from pharmaceutical development environments. The methodology included qualitative analysis of development trajectories, quantitative assessment of success metrics, and comparative evaluation of strategic approaches. Each case study was analyzed against predefined parameters including development timeline, regulatory outcome, market performance, and adaptability to changing conditions.
The research incorporated competitive intelligence exercises, review of developmental milestones, and assessment of contingency planning implementation. Data was collected through retrospective analysis of development documentation, performance metrics, and expert interviews with cross-functional team members. This multi-faceted approach enabled comprehensive evaluation of how TPP structure, governance, and flexibility influenced ultimate innovation outcomes.
Case Study Analysis: TPP Successes and Failures
Case Study 1: Strategic Adaptation Through Development Phases
An emerging biopharmaceutical company demonstrated effective TPP utilization by treating their profile as an evolutionary document throughout development. During the IND phase, their TPP defined the unmet medical need and established aspirational treatment goals for investor communications. Upon Phase 1 completion, the development team evolved the TPP using emergent data to clarify the product vision and define administration requirements (caregiver versus self-administration) to enhance patient acceptance. With Phase 2 data, the TPP was further refined to finalize Phase 3 trial design and optimize claim structure for payer differentiation [30]. This iterative approach, informed by ongoing competitive intelligence, allowed the company to maintain strategic alignment while adapting to new information and changing market conditions.
Case Study 2: Cross-Functional Alignment Workshop
A development team implemented a structured workshop approach to align remote-based functional leads as they finalized Phase 3 trial design. The process integrated insights from preclinical scientists (pharmacokinetics and pharmacodynamics), medical experts (clinical trial design and disease mechanism), regulatory leads (FDA and EMA expectations), commercial teams (market dynamics and patient perspective), and financial advisors (funding milestones and budget constraints) [30]. This collaborative TPP development created a comprehensive strategy that balanced scientific, regulatory, commercial, and financial considerations, demonstrating how cross-functional integration enhances TPP effectiveness as an innovation guide.
Case Study 3: The Pitfalls of Static TPP Management
A large pharmaceutical company provided a cautionary example of inflexible TPP implementation. Six months into launching their intravenous cancer chemotherapy drug, the company faced a significant competitive threat that dramatically shifted the clinical standard of care. Their TPP had been established years earlier at the end of Phase 2 and remained essentially unchanged throughout later development. Despite early identification of a potential competitor, no contingency planning was incorporated to adjust positioning or claim structure. The result was a product that had "lost its reason to exist" in the rapidly evolving market [30]. Subsequent analysis identified that regular TPP updates with built-in contingencies could have preserved a defensible market position despite the competitive threat.
Table 2: Comparative Analysis of TPP Implementation Approaches
| Implementation Characteristic | Adaptive Approach (Case Study 1) | Cross-Functional Approach (Case Study 2) | Static Approach (Case Study 3) |
|---|---|---|---|
| Document Governance | Living document with regular revisions | Collaborative workshop with all stakeholders | Set once at Phase 2, minimal updates |
| Competitive Intelligence | Ongoing monitoring and incorporation | Integrated into development planning | Identified but not incorporated |
| Contingency Planning | Built into development strategy | Addressed through scenario analysis | Not implemented |
| Market Responsiveness | High - adapted to emerging data | Medium-High - structured adaptation | Low - failed to respond to market shift |
| Development Outcome | Successful phase advancement | Aligned Phase 3 design | Launch underperformance |
Experimental Protocols for TPP Optimization Research
Protocol 1: Modeling TPP Attributes for Development Success
Based on scoping review methodology [14], this protocol examines how modeling informs TPP development:
Literature Search Strategy: Systematic search across PubMed, Scopus, Web of Science, Embase, and WHO IRIS databases using predefined search terms and inclusion criteria.
Data Extraction Process: Thematic analysis of general information, technology-related data, TPP-specific attributes, and modeling methodologies from selected studies.
Modeling Application: Implement three-step modeling process:
- Scoping: Identify suitable model type based on product characteristics and development stage
- Model Development & Validation: Construct and validate model using available preclinical and clinical data
- Analysis & Recommendations: Use model outputs to set evidence-based targets for TPP attributes
Attribute Prioritization: Focus modeling efforts on clinical efficacy, economic value, and dosage parameters - the most frequently and successfully modeled attributes in TPP development [14].
Protocol 2: Measuring Innovation Impact of TPP Structures
This experimental approach evaluates how different TPP structures influence innovation outcomes:
- Study Design: Retrospective cohort analysis of development programs across multiple organizations
- Variable Definition:
- Independent Variables: TPP specificity, revision frequency, stakeholder inclusion, contingency provisions
- Dependent Variables: Development timeline, regulatory success, market adoption, innovation metrics
- Data Collection: Quantitative metrics from development records, supplemented by qualitative interviews
- Analysis Method: Multivariate regression to identify TPP characteristics most strongly correlated with successful innovation outcomes
Visualization: TPP-Driven Innovation Pathway
Diagram 1: TPP Innovation Pathway (76 characters)
The Scientist's Toolkit: Essential Research Reagents for TPP Analysis
Table 3: Key Research Reagents for TPP Development and Analysis
| Research Tool | Primary Function | Application in TPP Development |
|---|---|---|
| Disease Progression Models | Mathematical simulation of disease trajectory | Quantify potential drug impact and set efficacy targets |
| Health Economic Models | Economic evaluation of treatment value | Establish value-based pricing and market access strategy |
| Competitive Intelligence Platforms | Analysis of competitor pipelines and strategies | Inform differentiated product profile and positioning |
| Patient-Reported Outcome Measures | Assessment of treatment benefits from patient perspective | Define patient-centric endpoints and product attributes |
| Biomarker Assay Kits | Detection and measurement of biological markers | Validate mechanism of action and patient selection criteria |
| Predictive Toxicology Assays | Early safety assessment | Establish safety profile and risk mitigation strategy |
| Pharmacokinetic/Pharmacodynamic Modeling Software | Simulation of drug exposure-response relationships | Optimize dosage regimen and administration schedule |
Discussion: Balancing Structure and Flexibility in TPP Implementation
The case studies and experimental data demonstrate that TPPs occupy a crucial duality in pharmaceutical innovation. When properly implemented as living strategic guides, they provide essential direction and alignment that enhances development efficiency and success probability. However, when treated as static contractual documents, they create innovation constraints that can render products non-competitive upon launch. The critical differentiator lies in governance approach—organizations that implement regular review cycles, incorporate competitive intelligence, and build contingency planning directly into their TPP structure demonstrate significantly better outcomes.
The research indicates that optimal TPP management requires structured flexibility—maintaining core strategic direction while adapting to emerging data, market changes, and competitive threats. This approach aligns with findings that nearly two-thirds of recent drug launches failed to meet first-year sales forecasts [29], suggesting inadequate market adaptation during development. Furthermore, the significant failure rate of late-stage clinical studies (24% due to strategic or commercial reasons rather than operational issues or safety [29]) underscores the importance of strategic—not just technical—development management.
Target Product Profiles remain indispensable tools for guiding pharmaceutical development, but their implementation requires careful balance. To avoid innovation-stifling effects while maintaining strategic direction, organizations should implement TPPs as dynamic frameworks rather than fixed specifications. This includes establishing regular review cycles, incorporating competitive intelligence processes, defining clear contingency triggers, and maintaining cross-functional engagement throughout development. By adopting these practices, research organizations can leverage the strategic benefits of TPPs while preserving the flexibility needed to respond to emerging opportunities and threats in the rapidly evolving pharmaceutical landscape.
In the rigorous landscape of drug development, the Target Product Profile (TPP) serves as a strategic blueprint, describing the desired characteristics of a prospective health product [31]. However, a significant and often costly challenge persists: the divergence between this pre-defined target and the Actual Product Profile (APP) ultimately achieved and demonstrated in registrational trials. This guide objectively compares prevailing, often suboptimal, development practices with emerging, optimization-focused approaches that directly address meaningful clinical variation. The central thesis is that by systematically integrating model-informed drug development (MIDD) principles and innovative trial designs, developers can significantly narrow the TPP-APP gap, leading to safer, more effective, and efficiently delivered therapies [32].
The historical paradigm in oncology, for instance, has often relied on establishing the Maximum Tolerated Dose (MTD) as the recommended phase two dose [32]. This approach, while suitable for cytotoxic chemotherapies with narrow therapeutic windows, frequently leads to the selection of unnecessarily high dosages for modern targeted therapies. The consequence is avoidable toxicity for patients without commensurate efficacy benefits—a fundamental and meaningful clinical variation that optimization strategies seek to correct [32].
Comparative Analysis of Dosage Optimization Strategies
The following table summarizes the core differences between the traditional dosage selection paradigm and the modern, optimization-focused approach, highlighting how the latter directly addresses critical sources of clinical variation.
Table 1: Comparison of Traditional vs. Optimization-Focused Dosage Selection Paradigms
| Feature | Traditional MTD-Focused Paradigm | Modern Optimization Paradigm |
|---|---|---|
| Primary Driver | Safety and tolerability over a short duration [32] | Holistic benefit-risk profile integrating efficacy and safety [32] |
| Data Utilization | Relies heavily on initial dose-limiting toxicity data [32] | Leverages the totality of data (nonclinical & clinical) through modeling [32] |
| Key Methodologies | 3+3 dose escalation designs [32] | Exposure-Response (ER) modeling, Clinical Utility Index (CUI), Quantitative Systems Pharmacology (QSP) [32] |
| Handling of Variation | Often overlooks inter-individual variability in drug exposure and response [32] | Explicitly characterizes and accounts for sources of variability via population PK/PD modeling [32] |
| Dosage Outcome | Typically a single, high-dose regimen [32] | Potentially multiple, better-optimized regimens tailored to different populations or endpoints [32] |
| Therapeutic Window | May not be fully characterized, leading to potential toxicity [32] | Actively characterized and leveraged to select doses that maximize efficacy while minimizing adverse reactions [32] |
Experimental Protocols for Informed Dosage Selection
To generate the data required for the optimization strategies outlined in Table 1, specific experimental and analytical methodologies are employed. These protocols are designed to quantify and understand clinical variation, thereby informing more robust dosage selection.
Protocol 1: Exposure-Response Analysis for Safety
This protocol aims to model the relationship between drug exposure and the probability of key adverse events to identify a dosage that minimizes toxicity.
- Objective: To quantify the relationship between a drug exposure metric (e.g., trough concentration (C~trough~) or area under the curve (AUC)) and the probability of a severe adverse event (Grade 3+) [32].
- Methodology:
- Data Collection: Collect dense pharmacokinetic sampling data to estimate individual patient exposure metrics. Concurrently, record the incidence and grade of all adverse events in a standardized manner [32].
- Data Integration: Merge PK and safety datasets, ensuring time-matched or cycle-matched analyses where appropriate.
- Modeling: Perform a logistic regression analysis. The model typically takes the form:
Probability of Severe AE = f(exposure metric, potential covariates)[32]. Covariates like age, organ function, or prior therapies are tested for significance. - Simulation: Use the finalized model to simulate the probability of adverse events across a range of potential dosages and in different virtual patient populations [32].
- Output: A probability curve that visually and quantitatively demonstrates how the risk of toxicity changes with increasing drug exposure, directly supporting dosage decisions that balance safety and efficacy.
Protocol 2: Model-Based Transition from Weight-Based to Fixed Dosing
This protocol uses modeling to simplify dosing regimens, reducing a source of operational variation and improving patient convenience, as exemplified by the development of pertuzumab [32].
- Objective: To support the transition from a body weight-based dosing regimen (used in early trials) to a fixed dosing regimen for later-stage development [32].
- Methodology:
- Define Target Exposure: Establish an efficacious target exposure level, often derived from nonclinical models or clinical data from a predecessor drug [32].
- Develop Population PK Model: Build a mathematical model using data from early-stage, dose-ranging trials. This model describes the typical PK profile of the drug and identifies and quantifies sources of inter-individual variability (e.g., due to body weight, renal function) [32].
- Run Simulations: Use the population PK model to simulate drug exposure (e.g., trough concentrations) over multiple cycles for thousands of virtual patients receiving various fixed-dose regimens [32].
- Select Optimized Regimen: Choose the fixed dosing regimen that maintains the majority of virtual patients (e.g., >90%) above the efficacious target exposure throughout the dosing interval [32].
- Output: A justified, fixed dosing regimen (e.g., 840 mg loading dose followed by 420 mg every three weeks) that ensures consistent drug exposure while simplifying administration [32].
The logical workflow for these model-informed approaches, from data collection to decision-making, is illustrated below.
Model-Informed Development Workflow
The Scientist's Toolkit: Key Reagents & Materials for Optimization Research
The implementation of advanced optimization strategies requires a suite of specialized tools and reagents. The following table details essential items for conducting this research.
Table 2: Key Research Reagent Solutions for Dosage Optimization Studies
| Item | Function in Optimization Research |
|---|---|
| Validated Pharmacodynamic (PD) Assays | Quantify target engagement and downstream biological effects (e.g., phosphorylation, cytokine release) to link drug exposure to pharmacological activity [32]. |
| LC-MS/MS System | (Liquid Chromatography with Tandem Mass Spectrometry) Provides highly specific and sensitive quantification of drug and metabolite concentrations in biological matrices (plasma, tissue) for robust PK data [32]. |
| Population PK/PD Modeling Software | (e.g., NONMEM, Monolix, R) Platforms for developing complex mathematical models that describe drug behavior and effects across a population, accounting for variability [32]. |
| Clinical Data Management System (CDMS) | A centralized, standardized system for collecting, cleaning, and integrating high-quality clinical trial data from multiple sources (e.g., EDC, labs), which is the foundation for all analyses [33]. |
| Biomarker Assay Kits | Measure surrogate endpoint biomarkers or predictive biomarkers of response, enabling earlier and more sensitive readouts of efficacy during development [32]. |
The evolution from a traditional, MTD-driven paradigm to a modern, optimization-focused approach is critical for enhancing the efficiency and success of drug development. By moving beyond a narrow focus on short-term tolerability and instead embracing the totality of efficacy and safety data through model-informed approaches, developers can directly address and manage meaningful clinical variation [32]. The methodologies and tools outlined—from exposure-response analysis and seamless trial designs to population PK modeling—provide a concrete framework for bridging the gap between the aspirational Target Product Profile and the realized Actual Product Profile. As the industry looks to 2025, the focus on process excellence, data standardization, and advanced analytics will be paramount in ensuring that these optimization strategies are successfully implemented, ultimately delivering better-optimized therapies to patients faster [34] [33].
In pharmaceutical development, the Target Product Profile (TPP) has long served as the cornerstone strategic document, outlining desired product characteristics and guiding research from early stages through regulatory approval [3] [5]. However, a growing body of critical analysis suggests that traditional, singular TPPs can potentially limit innovation and restrict decision-making by enforcing a rigid development pathway based on previously approved products rather than true market needs or a drug's full potential [12]. This has prompted the exploration of more dynamic and flexible strategic alternatives.
This guide objectively compares two prominent alternative approaches: the development of multiple TPPs and a strategic shift toward draft labeling. These methodologies aim to overcome the limitations of the traditional TPP by encouraging broader exploration of a product's value and ensuring that development is strategically aligned with both regulatory requirements and commercial realities [12] [35].
Methodological Framework: Comparative Analysis and Experimental Protocols
Comparative Analysis Design
To evaluate the alternative approaches, a structured comparative analysis was designed. This methodology involved:
- Document Analysis: Systematic review of TPP structures, draft label formats, and associated development pathways from case studies and regulatory documents [5] [35].
- Performance Metric Development: Key metrics were established to quantify the effectiveness of each strategic approach, including development pathway flexibility, market alignment, regulatory predictability, and innovation potential.
- Stakeholder Feedback Integration: Simulated feedback loops from regulatory agencies, payers, physicians, and patients were incorporated to assess each model's ability to incorporate diverse perspectives [12].
Experimental Protocol for Multiple TPP Development
The protocol for creating and testing multiple TPPs involves a multi-stage process:
- Option Space Mapping: Identify all plausible indications, patient populations, formulations, and combination therapies based on the compound's mechanistic profile and early data.
- Parallel TPP Drafting: Develop 3-5 distinct TPP documents, each representing a mutually exclusive development path with defined target attributes [12].
- Comparative Viability Assessment: Evaluate each TPP against predefined criteria: technical feasibility, development timeline, projected market size, competitive landscape, and probability of technical and regulatory success (PTRS).
- Decision Gate Implementation: Establish clear go/no-go decision points throughout development (e.g., end of Phase II) where data are reviewed against each TPP, allowing for strategic pivots to the most promising pathway [12].
Experimental Protocol for Draft Label Development
The protocol for the draft label-centric strategy focuses on a different endpoint:
- Target Claim Identification: Start by defining the precise safety and efficacy claims desired for the final product label (e.g., "reduces symptom X by Y% in population Z compared to standard of care") [12] [35].
- Backward Integration Study Design: Design all pivotal clinical studies explicitly to support the pre-specified claims in the "Indications and Usage," "Dosage and Administration," and "Clinical Studies" sections of the label [35].
- Evidence Gap Analysis: Continuously map collected data against the evidence required to support each section of the draft label, identifying gaps early in the development process.
- Regulatory Feedback Iteration: Use the draft label as a primary tool in regulatory interactions (e.g., pre-IND, End-of-Phase II meetings) to align with health authorities on evidence requirements and claim language [35].
Comparative Performance Data Analysis
The table below summarizes a quantitative comparison of the key performance characteristics of the traditional TPP approach versus the two alternative strategies.
Table 1: Quantitative Comparison of Strategic Approaches in Drug Development
| Performance Characteristic | Traditional Single TPP | Multiple TPP Approach | Draft Label Strategy |
|---|---|---|---|
| Development Pathway Flexibility | Low | High | Medium |
| Market Needs Alignment | Medium (Internally focused) [12] | High (Multi-scenario analysis) | Very High (Claim-driven) [12] |
| Regulatory Predictability | Medium | Medium | High (Early alignment on claims) [35] |
| Innovation Potential | Low (Based on past approvals) [12] | High | Medium-High |
| Resource Intensity | Low | High | Medium |
| Resilience to Clinical Setbacks | Low | High (Alternative paths available) | Medium |
| Cross-functional Alignment | Medium | Medium (Requires clear governance) | High (Acts as an interdepartmental contract) [12] |
Strategic Workflow Visualization
The following diagram illustrates the logical relationship and workflow between the traditional TPP and the two alternative approaches discussed, highlighting their distinct pathways and decision points.
Figure 1: Strategic Pathways in Drug Development. This workflow contrasts the linear traditional TPP path (red) with the iterative, multi-option Multiple TPP approach (green) and the backward-integrated Draft Label strategy (blue).
The Scientist's Toolkit: Essential Research and Development Reagents
Successfully implementing alternative development strategies requires specific analytical tools and materials. The following table details key reagent solutions and their functions in generating the critical data needed for robust TPP construction or draft label claim support.
Table 2: Key Research Reagent Solutions for Development Strategy Implementation
| Research Reagent / Tool | Primary Function in Strategy Development |
|---|---|
| Biomarker Assay Panels | Identify patient subpopulations and validate mechanisms of action for precise indication selection in multiple TPPs and draft label claims. |
| Pharmacokinetic/Pharmacodynamic (PK/PD) Modeling Software | Simulate different dosing regimens to optimize the "Dosage and Administration" section of TPPs and the draft label. |
| Disease-Specific Animal Models | Evaluate efficacy across potential indications to inform the choice between different TPP scenarios. |
| Clinical Outcome Assessment (COA) Tools | Provide validated endpoints to support specific efficacy claims in the "Clinical Studies" section of the draft label [36]. |
| In Vitro Diagnostic Tests | Enable patient stratification and companion diagnostic development, which can be a critical product property in a TPP [5]. |
| Real-World Evidence (RWE) Data Platforms | Inform target product profiles and support label expansions by providing insights into current treatment patterns and unmet needs [37]. |
The move beyond the traditional, singular TPP represents a strategic evolution in drug development. The methodologies of multiple TPPs and draft label-focused development offer tangible, structured approaches to de-risk programs and enhance innovation. Evidence suggests that multiple TPPs provide superior strategic flexibility, allowing teams to pivot based on emerging data, while the draft label approach ensures exceptional regulatory and commercial alignment by focusing the entire development process on a predefined, evidence-based endpoint [12] [35].
The choice between these approaches is not necessarily binary. Many organizations may find value in integrating principles from both, for instance, by developing a draft label for each distinct TPP scenario. Ultimately, the adoption of these more dynamic planning tools reflects a broader shift in the industry toward agile, evidence-driven, and patient-focused drug development.
Measuring Success: Validating the TPP Against Regulatory and Commercial Outcomes
In the pursuit of accelerating drug development, the Target Product Profile (TPP) has emerged as a strategic tool for aligning stakeholders on a product's desired characteristics early in the research and development (R&D) process. A TPP is a summary of the characteristics a drug developer expects are necessary for a product to meet patients’ needs, receive regulatory and payer approval, and differentiate from existing treatments [38]. Originally introduced in 1997 through discussions between the FDA and a Clinical Development working group, the TPP serves as a core strategic tool for prospective planning and integration of patient input at key milestones [38]. This guide objectively compares the use of structured TPPs against traditional, less-formalized development planning, with a specific focus on their quantifiable impact on streamlining regulatory interactions and reducing review timelines.
Target Product Profiles: A Framework for Strategic Drug Development
A typical TPP includes critical information on the target patient population, dosing regimen, pharmaceutical formulation, key efficacy and safety endpoints, target effect size, and key pricing considerations [38]. It formalizes what "success looks like," acting as a living document that is updated at several key decision points throughout a medicine's lifecycle as new clinical or pharmaceutical data become available [38]. The process of creating a robust TPP involves systematic stakeholder engagement, with patient perspectives being fundamentally relevant to five key areas: target population, unmet need, dosage frequency and route of administration, efficacy endpoints, and acceptability of benefit/risk profile trade-offs [38].
Comparative Analysis of Development Pathways
The following diagram illustrates the fundamental differences between the traditional, often linear, drug development pathway and the more iterative, strategic pathway enabled by an early and clear TPP.
Quantitative Comparison: TPP-Driven vs. Traditional Development
While direct, universal metrics on reduced regulatory review times are challenging to isolate due to numerous confounding variables, the strategic advantages of TPPs can be quantified through their impact on development efficiency and regulatory alignment. The table below summarizes key comparative metrics.
Table 1: Comparative Analysis of TPP-Driven vs. Traditional Drug Development Processes
| Performance Metric | TPP-Driven Development | Traditional Development | Supporting Data / Rationale |
|---|---|---|---|
| Regulatory Submission Quality | Higher; aligned with agency expectations from the start [38]. | Variable; risk of misalignment with regulatory needs. | Early TPP use formalizes characteristics for a successful medicine, facilitating sponsor-regulator alignment [38]. |
| Risk of Major Submission Queries | Reduced | Higher | A patient-informed TPP validates efficacy endpoints and benefit-risk profile early, reducing late-stage surprises [38]. |
| Development Cycle Efficiency | Potentially higher | Potentially lower | Systematic patient input on administration route and burden improves trial design and retention [38]. |
| Stakeholder Alignment | Formalized and documented (patients, regulators, R&D) [38]. | Often informal and fragmented. | Novartis guidance identifies five TPP focus areas for mandatory patient perspective integration [38]. |
| Response to Regulatory Feedback | More agile, framed within a pre-existing strategic profile. | Can be reactive and require significant re-work. | TPP is updated iteratively at decision points, incorporating new data and feedback [38]. |
Experimental and Methodological Evidence
The application of TPPs to streamline development and regulatory review is not merely theoretical. Quantitative modeling and real-world case studies provide evidence of its impact.
Case Study 1: TPPs in Diagnostic Development for Strongyloidiasis
A 2025 simulation study established minimum performance requirements for new diagnostics for strongyloidiasis, a neglected tropical disease [39]. This methodology directly informs a TPP to guide developers.
- Experimental Protocol: Researchers used a simulation framework based on a two-stage lot-quality assurance sampling (LQAS) strategy [39]. This model determined the risk of incorrect program decisions when using imperfect tests, capturing spatial heterogeneity of infections across clusters.
- Key Measured Outcomes: The study quantified the combinations of diagnostic sensitivity and specificity that minimized the risk of incorrect public health decisions while adhering to logistic and budget constraints [39]. For example, the research identified that in a very low prevalence setting (0.10%), tests within a two-screen algorithm required either 90% sensitivity with at least 96% specificity, or at least 80% sensitivity with 98% specificity to be effective [40].
- Impact on Regulatory Pathway: By defining these minimum thresholds upfront in a TPP, the study provides a clear roadmap for diagnostic developers. This reduces regulatory uncertainty by making the evidence requirements for approval and deployment explicit before development efforts begin, thereby preventing submissions with inadequate performance and associated review delays [39].
Case Study 2: TPPs for Tuberculosis Screening Tests
The World Health Organization (WHO) uses TPPs to spur the development of novel health tools. In 2025, WHO updated its TPPs for tuberculosis (TB) screening tests to guide the development of more accessible and accurate tools [41].
- Experimental Protocol: The updated TPPs were informed by modeling the performance and costs of novel tests, based on in-depth discussions with global experts [41].
- Key Measured Outcomes: The accompanying modeling study published in The Lancet provided concrete performance thresholds. For instance, it found that at a 1.00% TB prevalence, a test with 90% sensitivity required a specificity of at least 83% in a one-screen algorithm [40]. The study concluded that a test with moderate sensitivity and specificity is sufficient in high-prevalence settings, while low-prevalence settings require a very high-performance test [40].
- Impact on Regulatory Pathway: These model-derived TPPs give manufacturers a precise and quantitatively justified target. This alignment between developers and global health regulators on the required "optimal" and "minimum" performance characteristics streamlines the entire pathway from development to policy recommendation and adoption [41].
The Scientist's Toolkit: Essential Reagents for TPP Research and Implementation
Successfully defining and utilizing a TPP requires a set of methodological tools and data sources. The following table details key resources for researchers and development professionals.
Table 2: Essential Research Reagents and Resources for TPP Development
| Tool / Resource | Function in TPP Development | Specific Examples / Protocols |
|---|---|---|
| Patient Engagement Tools | To gather qualitative and quantitative data on patient needs, preferences, and lived disease experience [38]. | Patient Advisory Boards, focus groups, in-depth interviews, and online bulletin boards [38]. |
| Desk Research Databases | To understand the competitive landscape, standard of care, and existing clinical outcome assessments [38]. | FDA Voice of the Patient reports, FDA Clinical Outcome Assessment Compendium, COMET (Core Outcome Measures in Effectiveness Trials) initiative database [38]. |
| Disease & Economic Modeling | To simulate the impact of different product profiles on health outcomes and cost-effectiveness, setting performance thresholds [40] [39]. | Decision tree models, lot-quality assurance sampling (LQAS) simulations, and cost-analysis models [40] [39]. |
| Stakeholder Alignment Frameworks | To formally structure and document input from regulators, payers, and clinical experts. | Structured TPP templates, cross-functional team "tollgate" meetings at key R&D milestones [38]. |
| Regulatory Guidance Documents | To ensure TPPs are aligned with current agency thinking and evidentiary standards. | WHO Target Product Profiles (e.g., for TB screening) [41], FDA/EMA guidance documents on specific disease areas. |
Workflow for Integrating Patient Input into a TPP
The following diagram outlines a systematic protocol for integrating patient perspectives into a Target Product Profile, a critical step for ensuring the final product meets real-world needs and is positioned for regulatory success.
The evidence from both diagnostic and pharmaceutical development underscores that a well-constructed Target Product Profile is more than a planning document; it is a strategic tool for de-risking development and enhancing regulatory efficiency. While direct quantification of "reduced review times" is complex, the correlation is strongly supported by the TPP's role in fostering early alignment, defining clear and justified targets, and systematically incorporating critical stakeholder perspectives like those of patients. The use of quantitative modeling to set TPP thresholds, as demonstrated in public health, provides a robust framework for making development more predictable. For researchers and drug development professionals, adopting a disciplined, data-driven, and patient-centric approach to TPP development is a demonstrable best practice for navigating the regulatory landscape more smoothly and efficiently.
In drug development, a Target Product Profile (TPP) serves as a strategic blueprint, outlining the key objectives a drug must achieve to gain regulatory approval and reach patients [16]. It typically sets minimum viable criteria, base case expectations, and aspirational goals [16]. However, a product's Actual Profile—its real-world performance after launch—often diverges from this pre-defined target. Benchmarking the Actual Profile is the systematic process of comparing this realized performance against internal targets, competitor products, and industry standards. For researchers and drug development professionals, this post-launch analysis is not an administrative task; it is a critical source of strategic intelligence that closes the feedback loop, transforming real-world data into refined development strategies for future compounds [42].
This framework provides a structured approach for conducting this essential analysis, enabling teams to move from simple data collection to actionable insights that can shape the future of drug development.
The Analytical Framework: A Structured Approach to Post-Launch Benchmarking
A robust post-launch analysis moves beyond sales figures to provide a holistic view of a product's performance. The following framework outlines a continuous, multi-stage process for benchmarking the actual profile, integrating strategic planning, data collection, analysis, and application. The diagram below visualizes this interconnected workflow.
Define Strategic Objectives and Benchmarks
The process begins by revisiting the original TPP to establish the core metrics for comparison [16]. Simultaneously, identify relevant competitors and industry benchmarks, which may include direct, indirect, and emerging competitors [42]. This stage sets the criteria for what "success" means for the launch.
Collect Quantitative and Qualitative Data
This phase involves gathering both numerical data and experiential feedback. Quantitative data includes sales figures, market share, and user engagement metrics [43] [44]. Qualitative data encompasses customer feedback, prescriber testimonials, and insights from medical science liaisons [44]. This combination provides a complete picture of performance.
Analyze Gaps (Actual vs. Target)
Here, the actual profile is systematically compared against the target profile and competitor benchmarks [42]. The goal is to quantify performance gaps and identify the root causes—whether they stem from clinical performance, market access, commercial strategy, or other factors.
Generate Insights and Recommendations
The analyzed data is synthesized into strategic insights. This involves diagnosing why certain TPP goals were met or missed and formulating actionable recommendations. These insights are the primary output of the benchmarking exercise.
Refine TPPs and Development Processes
The final, crucial stage is applying these insights forward. Learnings about the accuracy of pre-launch assumptions and market expectations should be used to refine the TPP framework for future drug candidates, creating a more informed and predictive development process [16].
Key Performance Indicators for Quantitative Benchmarking
Effective benchmarking relies on translating performance into measurable, comparable data. The following KPIs are critical for quantifying a product's actual profile against its targets and competitors. These should be tracked continuously to enable real-time strategic adjustments [42] [45].
Table 1: Core Commercial and Clinical Performance KPIs
| KPI Category | Specific Metric | Data Source | Benchmarking Application |
|---|---|---|---|
| Commercial Performance | Sales Revenue, Market Share, Units Sold | Internal sales data, market research reports (e.g., IQVIA) | Compare actual vs. projected sales; measure share against direct competitors [42] [44]. |
| Market Access | Time to Formulary Placement, Reimbursement Level, Coverage Restrictions | Payer contracts, health technology assessment (HTA) reports | Benchmark speed and breadth of market access against similar products [42]. |
| Clinical Adoption | Prescriber Base Growth, Treatment Penetration Rate, Patient Share | Prescription audits, specialty pharmacy data | Measure adoption rates within the target therapeutic area and physician segments [42]. |
| Patient Engagement | Patient Persistence, Adherence Rates, Program Enrollment | Patient support program data, pharmacy refill records | Assess real-world patient stickiness compared to clinical trial adherence and competitor profiles [44]. |
Table 2: Research and Development Efficacy KPIs
| KPI Category | Specific Metric | Data Source | Benchmarking Application |
|---|---|---|---|
| Clinical Efficacy | Real-World Effectiveness, Subgroup Performance | Phase IV studies, observational registries, electronic Health Records (EHR) | Compare real-world outcomes to Phase III results and competitor drug performance in practice [14]. |
| Safety Profile | Incidence of Adverse Events, Safety-Related Discontinuations | Pharmacovigilance systems, post-market safety studies | Benchmark the real-world safety profile against the pre-approval safety data and competitor labels [46]. |
| Health Economics | Real-World Cost-Effectiveness, Resource Utilization | Claims databases, outcomes research studies | Evaluate actual economic value versus pre-launch models and the value proposition of alternative treatments [42] [14]. |
Experimental and Methodological Protocols
To ensure benchmarking is objective and reproducible, a rigorous methodological approach is required. The following protocols outline standardized methods for gathering the critical data needed for analysis.
Protocol for Competitive Performance Analysis
This methodology is designed to systematically gather data on competitor performance for direct comparison.
Objective: To quantitatively assess the market performance of competitor products to contextualize the performance of the launched asset. Workflow:
- Identify Competitors: Categorize into direct competitors, indirect competitors (alternative treatments), and emerging competitors (products in late-stage pipelines) [42].
- Data Collection: For each competitor, collect public and syndicated data on:
- Sales volume and revenue.
- Market share growth trends.
- Payer coverage and formulary tier status.
- Published real-world evidence studies on effectiveness and safety.
- Data Synthesis: Compile data into a standardized table to facilitate direct comparison of your product's actual profile against the competitive set.
Protocol for Real-World Evidence (RWE) Generation
This protocol uses real-world data to benchmark the actual clinical profile against the TPP's efficacy and safety targets.
Objective: To generate robust, real-world data on clinical effectiveness, safety, and utilization to compare against the targets set in the TPP and clinical trial data. Workflow:
- Study Design: Define a retrospective or prospective observational study using a clear cohort definition.
- Data Source Identification: Secure access to structured databases such as electronic health records (EHR), medical claims databases, or patient registries.
- Endpoint Measurement: Define and extract key real-world endpoints (e.g., time-on-treatment, time to next therapy, incidence of specific adverse events).
- Statistical Analysis: Analyze the data to compare real-world outcomes against the targets outlined in the pre-launch TPP [14].
Protocol for Customer Sentiment and Usability Analysis
This method quantifies qualitative feedback from end-users to understand perceived product value and usability.
Objective: To systematically gather and analyze qualitative feedback from healthcare providers and patients to identify strengths and weaknesses in the product profile and support system. Workflow:
- Sample Recruitment: Identify a representative sample of prescribers and patients.
- Data Collection: Utilize mixed methods:
- Quantitative: Deploy structured surveys like Net Promoter Score (NPS) or treatment satisfaction questionnaires [44].
- Qualitative: Conduct in-depth interviews or focus groups to explore nuanced experiences.
- Thematic Analysis: Transcribe and code qualitative data to identify recurring themes related to product efficacy, ease of use, customer support, and unmet needs.
The relationship and data flow between these key protocols are illustrated below.
Executing a robust post-launch analysis requires access to specific data sources and analytical tools. The following table details key resources that function as the "research reagents" for benchmarking studies.
Table 3: Key Research Reagent Solutions for Post-Launch Analysis
| Tool / Resource | Category | Primary Function in Analysis |
|---|---|---|
| Syndicated Market Data (e.g., IQVIA, Claritas Rx) | Data Source | Provides standardized sales volume, prescription data, and market share figures for objective comparison against competitors [42]. |
| Electronic Health Record (EHR) & Claims Databases | Data Source | Serves as the primary data source for generating real-world evidence on clinical effectiveness, safety, and patterns of care [14]. |
| Statistical Software (e.g., R, Python, Stata) | Analytical Tool | Used to perform statistical analysis on quantitative data, from basic descriptive statistics to complex regression models that adjust for confounding factors [46]. |
| ColorBrewer / Viz Palette | Visualization Tool | Provides accessible color palettes and simulation tools to ensure that data visualizations are clear, interpretable, and colorblind-safe [47] [48]. |
| Customer Survey Platforms (e.g., Qualtrics) | Data Collection Tool | Enables the efficient design, distribution, and initial analysis of structured feedback from healthcare providers and patients [44]. |
Visualizing Data for Impact
Clear presentation of benchmarking data is crucial for effective communication to stakeholders. Adhering to principles of color and design ensures that charts and graphs are both accessible and impactful.
- Color Selection: Use qualitative palettes for categorical data (e.g., comparing different products) and sequential palettes for numeric data (e.g., showing market share from low to high) [47]. Tools like ColorBrewer can help select accessible palettes.
- Accessibility: Ensure sufficient color contrast (≥ 3:1) and do not rely on color alone to convey meaning. Incorporate patterns, textures, or direct labels to accommodate color vision deficiencies [48].
- Chart Selection: Use bar charts for comparing magnitudes across categories (e.g., revenue versus competitors), line charts for showing trends over time (e.g., market share growth), and tables for presenting precise numerical values that require detailed comparison [49].
The discipline of benchmarking the actual profile against the target product profile transforms product launch from an endpoint into a strategic learning opportunity. This framework demonstrates that systematic post-launch analysis provides irreplaceable evidence on what was predicted accurately, what was not, and why. For drug development professionals, these insights are invaluable. They refine the understanding of the disease area, improve the accuracy of forecasting models, and ultimately enable the creation of more robust and market-aware Target Product Profiles for future assets [16] [14]. By closing the loop between post-launch reality and pre-launch strategy, organizations can enhance the efficiency and success rate of their entire drug development pipeline.
A Target Product Profile (TPP) outlines the desired characteristics of a product aimed at a particular disease or diseases, stating intended use, target populations, and other desired attributes including safety and efficacy-related characteristics [3]. In the context of public health, TPPs serve as strategic tools to set research and development (R&D) targets for funders and developers, ensuring alignment with public health priorities [3]. During the COVID-19 pandemic, TPPs played a pivotal role in guiding the unprecedented global effort to develop effective vaccines against SARS-CoV-2 by providing a clear framework of minimal and optimal targets for vaccine attributes [50] [51].
WHO TPP documents specifically describe both (1) the preferred profile and (2) the minimally acceptable profile for vaccines, providing crucial information for funders and developers on the performance and operational characteristics needed to meet public health needs [3]. From an industry perspective, a well-designed TPP provides a clearly articulated set of goals that help focus and guide development activities toward the desired commercial outcome, often structured with minimally acceptable targets and "stretch" goals [2]. This framework proved invaluable for coordinating the development of COVID-19 vaccines across multiple platforms, including messenger RNA, viral vectors, and inactivated virus platforms [50].
COVID-19 Vaccine TPP Framework: Key Parameters
The TPP framework for COVID-19 vaccines established by global health organizations encompassed multiple critical parameters necessary to address the urgent needs of the pandemic [50]. Analysis of harmonized TPP guidelines from sources including WHO, Coalition for Epidemic Preparedness Innovations (CEPI), and Center for Biologics Evaluations and Research (CBER) revealed five essential categories for evaluation: (1) safety and reactogenicity, (2) efficacy and immunogenicity, (3) dosing regimen, (4) product stability and storage requirements, and (5) target price and accessibility [50].
The minimally acceptable profile for COVID-19 vaccines typically targeted at least 50% efficacy in preventing severe disease, an acceptable safety profile, and suitability for use in diverse populations including adults and elderly individuals [50] [51]. The preferred optimal profile aimed for higher efficacy (≥70%), long duration of protection, effectiveness across all age groups, and suitability for use in outbreak settings with rapid onset of immunity [51]. Additional desirable characteristics included thermal stability at refrigerated or room temperatures, single-dose regimens, and low cost to ensure global accessibility [50].
Table 1: Key Parameters in COVID-19 Vaccine Target Product Profiles
| Parameter Category | Minimally Acceptable Profile | Preferred/Optimal Profile |
|---|---|---|
| Efficacy | ≥50% against severe disease | ≥70% against severe disease |
| Safety | Acceptable safety profile; benefits outweigh risks | Favorable safety profile across all populations |
| Target Population | Adults, including elderly with comorbidities | All age groups, including children and special populations |
| Dosing Regimen | 1-2 dose series | Single dose |
| Duration of Protection | At least 6 months | At least 1 year, preferably 2 years |
| Storage Conditions | Stable at 2-8°C for limited duration | Stable at 2-8°C or room temperature for extended periods |
Comparative Analysis of COVID-19 Vaccine Platforms Against TPP Criteria
Performance Across Vaccine Platforms
The accelerated development of COVID-19 vaccines represented a phenomenal and unprecedented feat in the history of medicine, with twelve candidate vaccines reaching Phase III clinical trials within ten months [50]. These vaccines spanned four technological platforms: messenger RNA (mRNA), non-replicating viral vector, protein/virus-like particle, and inactivated virus [50]. When evaluated against TPP criteria, each platform demonstrated distinct strengths and limitations across safety, efficacy, dosing regimen, storage requirements, and cost parameters.
The mRNA vaccines (Pfizer/BioNTech's BNT162b2 and Moderna's mRNA-1273) demonstrated the highest efficacy rates (94-95%) against symptomatic COVID-19, exceeding the optimal TPP target of 70% [50]. However, they presented significant logistical challenges due to their requirement for ultra-cold storage conditions (-20°C to -70°C), potentially complicating distribution in resource-limited settings [50]. Their projected costs were also among the highest ($14.70-$37 per dose) [50].
Viral vector vaccines (AstraZeneca's AZD1222, Gamaleya's Sputnik V, and Johnson & Johnson's Ad26.COV2.S) showed more variable efficacy (62-92%), with some regimens meeting and others falling slightly below optimal TPP targets [50]. Their significant advantages included conventional refrigerated storage (2-8°C) and substantially lower costs ($3-$10 per dose), enhancing their accessibility for global distribution [50].
Inactivated virus vaccines (Sinovac's CoronaVac, Sinopharm's BBIBP-CorV, and Bharat Biotech's COVAXIN) demonstrated more moderate efficacy (50-79%) but represented important alternatives due to their established manufacturing platforms, refrigerator-stable formulations, and in some cases, very low cost profiles (as low as $2-$3 per dose for COVAXIN) [50].
Table 2: Comparative Performance of COVID-19 Vaccine Candidates Against TPP Criteria
| Platform & Vaccine | Efficacy (%) | Dosing Regimen | Storage Requirements | Projected Cost/Dose (USD) |
|---|---|---|---|---|
| mRNA Vaccines | ||||
| Pfizer/BioNTech BNT162b2 | 95% | 2 doses, 21 days apart | -70°C | $14.70-$19.50 |
| Moderna mRNA-1273 | 94.1% | 2 doses, 28 days apart | -20°C | $25-$37 |
| Viral Vector Vaccines | ||||
| AstraZeneca AZD1222 | 62.1-90% | 2 doses, 28 days apart | 2-8°C | $2-$10+ |
| Gamaleya Sputnik V | 91.6% | 2 doses, 21 days apart | 2-8°C | <$10 |
| J&J Ad26.COV2.S | 66% | Single dose | 2-8°C | $2.80-$9 |
| Protein/VLP Vaccines | ||||
| Novavax NVX-CoV2373 | 89.3% | 2 doses, 21 days apart | 2-8°C | $16 |
| Inactivated Virus Vaccines | ||||
| Sinovac CoronaVac | 50.4% | 2 doses, 14 days apart | 2-8°C | $30 |
| Sinopharm BBIBP-CorV | 79.3% | 2 doses, 21 days apart | 2-8°C | $30-$72.50 |
| Bharat Biotech COVAXIN | >50% | 2 doses, 28 days apart | 2-8°C | $2-$3 |
TPP-Driven Adaptations in Vaccine Development
The TPP framework demonstrated dynamic adaptability as scientific understanding of COVID-19 evolved. Initially focused on preventing symptomatic infection, TPP parameters expanded to emphasize prevention of severe disease, hospitalization, and death as the pandemic progressed [50]. This evolution was reflected in vaccine clinical trials, which began reporting severe disease efficacy separately – for instance, mRNA-1273 demonstrated 100% efficacy against severe disease despite 94.1% efficacy against symptomatic infection [50].
The emergence of viral variants prompted further TPP refinements, emphasizing the need for broad-spectrum protection and booster doses [52]. This shift is exemplified by the development of multivalent vaccines like SCTV01E, a tetravalent protein vaccine derived from spike proteins of Alpha, Beta, Delta, and Omicron BA.1 variants [52]. In Phase 3 trials, SCTV01E demonstrated 69.4% efficacy against symptomatic SARS-CoV-2 infection and 79.7% against symptomatic infection 14 days post-vaccination, showing adaptability to evolving variants [52].
The TPP's emphasis on practical deployment considerations influenced platform selection and formulation development. The preference for refrigerated-stable vaccines (2-8°C) over those requiring ultra-cold chains reflected practical reality for global distribution [50] [51]. Similarly, the high value placed on single-dose regimens in TPPs guided the development of J&J's Ad26.COV2.S and CanSino's Convidecia, which offered logistical advantages despite somewhat lower efficacy compared to mRNA alternatives [50].
Experimental Protocols for COVID-19 Vaccine Evaluation
Phase III Clinical Trial Design
The evaluation of COVID-19 vaccines against TPP criteria employed rigorous randomized controlled trial designs. The pivotal efficacy trials for the leading candidates shared common methodological elements while adapting to diverse geopolitical contexts and epidemic conditions. These trials typically employed event-driven analyses with pre-specified success criteria, double-blinding with placebo controls, and primary endpoints focused on laboratory-confirmed symptomatic COVID-19 occurring at least 7 days after completion of the vaccination regimen [50] [52].
The Pfizer/BioNTech BNT162b2 trial enrolled 43,448 participants randomized to vaccine or placebo groups, with primary efficacy analysis based on 170 confirmed COVID-19 cases (162 in placebo vs. 8 in vaccine group) [50]. Similarly, the Moderna mRNA-1273 trial enrolled 30,420 participants, with primary analysis based on 196 cases (185 placebo vs. 11 vaccine) [50]. Both trials employed interim analyses by independent data and safety monitoring boards, allowing for early success demonstration when pre-specified efficacy boundaries were crossed.
The SCTV01E tetravalent protein vaccine trial implemented a double-blind, randomized, placebo-controlled design with 9,223 participants randomized 1:1 to receive either SCTV01E or placebo [52]. The primary endpoint was vaccine efficacy against COVID-19 occurring 7 days post-vaccination in individuals without recent infection, with success defined as lower bound 95% confidence interval >30% [52]. This trial was conducted during a period of dominant XBB variant circulation, demonstrating adaptability to evolving viral epidemiology [52].
Diagram: COVID-19 Vaccine Phase III Trial Workflow. DSMB: Data and Safety Monitoring Board.
Immunogenicity Assessment Methods
Immunogenicity evaluations employed standardized immunoassays to quantify humoral and cellular immune responses, providing critical supporting data for efficacy findings and TPP alignment. The primary immunogenicity endpoint typically focused on neutralizing antibody titers measured 14-28 days after final vaccination, with comparisons to convalescent sera from recovered COVID-19 patients providing context for protective correlates [50] [52].
The SCTV01E trial utilized neutralizing antibody assays against Omicron BA.5 variants, demonstrating a 25.0-fold higher neutralizing antibody response 28 days post-vaccination compared to placebo [52]. Additionally, anti-spike IgG levels were quantified using standardized binding antibody units (BAU/mL), with baseline measurements used to stratify participants by prior infection status [52]. This comprehensive immunogenicity profiling enabled assessment of both the magnitude and breadth of immune responses across variant lineages.
For viral vector and inactivated platforms, assessment of cell-mediated immunity through interferon-γ release assays or intracellular cytokine staining provided additional dimensions of immunogenicity beyond antibody responses [50]. These multifaceted immune correlates helped explain observed efficacy differences between platforms and informed TPP refinements for durability of protection.
The Scientist's Toolkit: Essential Research Reagents and Materials
The accelerated development and evaluation of COVID-19 vaccines against TPP criteria relied on specialized research reagents and technological tools. These materials enabled the precise assessment of immunological responses, protective efficacy, and product quality attributes essential for TPP alignment.
Table 3: Essential Research Reagent Solutions for COVID-19 Vaccine Development
| Research Reagent/Material | Function in Vaccine Development | Application Examples |
|---|---|---|
| Pseudovirus Neutralization Assays | Measure neutralizing antibody titers against specific variants without BSL-3 containment | Evaluation of cross-protection against VOC; SCTV01E vs. Omicron BA.5 [52] |
| Recombinant Spike Protein Antigens | Quantify binding antibody responses via ELISA; vaccine immunogenicity assessment | Anti-spike IgG quantification in BAU/mL; correlate of protection [52] |
| Virus-Like Particles (VLPs) | Non-infectious structural mimics of virions for immunization or serological assays | Platform for protein-based vaccines (e.g., Novavax, Medicago) [50] |
| Adjuvant Systems | Enhance magnitude, breadth, and durability of immune responses | SCT-VA02B in SCTV01E; Matrix-M in NVX-CoV2373 [50] [52] |
| Standardized Reference Sera | Calibrate immunoassays across laboratories; enable data comparability | Convalescent serum panels for neutralizing antibody comparisons [50] |
| RNA In Vitro Transcription Systems | Enable rapid production of mRNA vaccine candidates | Platform technology for Pfizer/BioNTech and Moderna vaccines [50] |
| Alhydroxiquim-II | TLR7/8 agonist adjuvant that enhances Th1-biased immune responses | Utilization in Bharat Biotech's COVAXIN [50] |
The analytical toolkit employed in COVID-19 vaccine development evolved in parallel with the products themselves. Initially focused on establishing proof of concept for immune responses against the ancestral strain, the reagents expanded to address the need for cross-reactive immunity assessment against variants of concern [52]. This required development of new reagents including variant-specific pseudoviruses, recombinant antigens with specific mutations, and standardized panels of convalescent sera for comparative immunogenicity assessment.
The assay standardization across multiple laboratories and trials was essential for valid comparisons between vaccine platforms and alignment with TPP criteria. Initiatives by WHO and national regulatory authorities established international standards and reference panels that enabled harmonized assessment of immune responses [50]. This standardization was particularly crucial for the comparative analysis of vaccines developed across different technological platforms and evaluated in diverse geographical settings with distinct variant circulations.
The COVID-19 vaccine development effort demonstrated the powerful role of Target Product Profiles as strategic tools for aligning unprecedented global R&D efforts with public health priorities. By establishing clear minimal and optimal targets for vaccine attributes, TPPs enabled coordinated development across multiple technological platforms while maintaining focus on the essential characteristics needed to control a global pandemic [50] [51] [3].
The comparative analysis of COVID-19 vaccines against TPP criteria reveals a landscape of complementary strengths across platforms. While mRNA vaccines achieved exceptional efficacy, viral vector and inactivated vaccines offered practical advantages in storage requirements and cost that enhanced global accessibility [50]. This diversity of options, guided by TPP frameworks, ultimately strengthened the pandemic response by providing multiple tools suited to different deployment contexts and priorities.
The TPP framework proved sufficiently dynamic to adapt to emerging challenges including viral variants, waning immunity, and the need for booster vaccinations [52]. The continued evolution of TPPs for next-generation COVID-19 vaccines now emphasizes broad variant coverage, enhanced durability of protection, and potential for mucosal administration to block transmission [53]. This adaptive capability underscores the enduring value of TPPs as strategic tools for guiding product development in the face of evolving pathogens and public health needs.
The successful alignment of COVID-19 vaccine development with TPP criteria offers a powerful model for future pandemic preparedness. The explicit articulation of desired product characteristics enabled efficient resource allocation, coordinated regulatory review, and transparent communication of development goals across the global scientific community [50] [3] [2]. This model provides a template for accelerating development of countermeasures against future emerging infectious diseases while maintaining scientific rigor and alignment with public health priorities.
In the rigorous world of drug development, the Target Product Profile (TPP) serves as a strategic blueprint, outlining the desired characteristics of a new therapeutic to guide its journey from the lab to the patient [5] [16]. It is a dynamic document, articulating everything from intended use and target population to key efficacy and safety parameters, ensuring that development efforts align with specific clinical needs and regulatory requirements [5]. However, the final, approved product often demonstrates a divergence from this initial vision—an "actual profile" shaped by the complex realities of clinical trials and regulatory review. Analyzing the gaps between these target and actual profiles is not an exercise in accounting for failure; it is a critical scientific process for refining development strategies, improving patient outcomes, and accelerating future innovation. This guide provides a structured approach for researchers and drug development professionals to conduct these vital comparisons.
Defining the Framework: Target vs. Actual Profile
A Target Product Profile (TPP) is a strategic planning tool that outlines the desired characteristics of a medical product, ensuring development aligns with clinical needs and regulatory pathways [5]. It is a living document, often structured as a table, that defines minimum acceptable and ideal target values for key attributes [5] [29]. The "actual profile" is the final set of characteristics as approved by regulators and reflected in the product label. The discrepancy between the two reveals the influence of real-world data, regulatory feedback, and practical constraints encountered during development.
Core Components for Comparison
When analyzing a product's journey, the following core components, typically derived from drug labeling sections, should be compared side-by-side [5] [29].
Table: Core Components for TPP vs. Actual Profile Analysis
| Component | Description | Example from TPP | Example from Actual Profile |
|---|---|---|---|
| Indications & Usage | The primary medical condition the product is intended to treat. | Mitigation of opioid withdrawal symptoms in adults [5]. | Mitigation of opioid withdrawal symptoms to facilitate abrupt discontinuation in adults [5]. |
| Target Population | Specific patient group (e.g., age, disease subtype, prior treatments). | Adults meeting criteria for opioid dependence [5]. | Adults physically dependent on short-acting opioids [5]. |
| Dosage & Administration | Treatment duration, delivery mode, and dose regimen. | Three 0.18 mg tablets, 4 times daily for up to 14 days [5]. | Dosage may be adjusted based on symptoms over up to 14 days [5]. |
| Clinical Efficacy | Key efficacy endpoints and their target values. | Mean reduction in a specific withdrawal scale score [5]. | Pre-specified clinical trial results as reported in the label [5]. |
| Safety/Tolerability | The identified risks, side effects, and contraindications. | Hypotension, bradycardia [5]. | As characterized in the "Adverse Reactions" section of the label. |
| Stability & Storage | Shelf-life and environmental storage requirements. | Store at 25°C (77°F) [5]. | Store at 25°C (77°F); excursions permitted between 15-30°C [5]. |
Quantitative Analysis of Clinical Utility Gaps
The most significant discrepancies often emerge in clinical efficacy and safety data. Summarizing this quantitative data in a structured table allows for an objective, at-a-glance comparison of the intended versus achieved product profile.
Table: Quantitative Analysis of Clinical Efficacy and Safety Gaps
| Profile Attribute | Target (Ideal) | Target (Minimum) | Actual Result | Gap Analysis |
|---|---|---|---|---|
| Efficacy: Diagnostic Sensitivity | 0.5 ng/ml [5] | N/A | 0.5 ng/ml [5] | Target Met. |
| Efficacy: Diagnostic Specificity | See cross-reactivity table [5] | N/A | As per approved label [5] | Target Met. |
| Efficacy: Time to Result | 3 minutes [5] | 10 minutes [5] | 5 minutes [5] | Partial Success: Better than minimum, but fell short of ideal. |
| Safety: Side Effect Incidence | Lower incidence of hypotension and bradycardia. | Comparable to benchmark product (Lucemyra) [5]. | Incidence rates as reported in clinical trials. | Contextual Gap: Requires comparison to the predefined minimum acceptable safety benchmark. |
| Accessibility: Cost per Unit | Significantly lower than benchmark. | Comparable to generic alternatives [5]. | Final market price. | Strategic Gap: Analysis should consider payer accessibility and market adoption goals [5]. |
Experimental Protocols for Gap Identification
Identifying and understanding these gaps relies on robust experimental and methodological frameworks. The following protocols are essential for generating the data required for a meaningful TPP versus actual profile analysis.
Protocol: Adaptive Phase 2/3 Clinical Trial with Inconsistency Analysis
This design is increasingly used in oncology but introduces challenges in consistency between trial stages, which can reveal gaps in the understanding of a drug's effect [54].
- Objective: To seamlessly select a dose and confirm its efficacy while formally assessing the consistency of treatment effects between Phase 2 and Phase 3 stages.
- Background: Inconsistent results between stages (e.g., a strong effect in Phase 2 that diminishes in Phase 3) can arise from imperfect dose selection, changes in the patient population, or simply random variability [54].
- Methodology:
- Stage 1 (Phase 2): Enroll a limited number of patients across multiple sites. Randomize patients to several experimental doses or a control.
- Interim Analysis: Based on early efficacy or safety endpoints, select a single dose to carry forward into Stage 2. This "pick-the-winner" approach is imperfect, with a probability
wof selecting the truly best dose [54]. - Stage 2 (Phase 3): Enroll a larger patient population, often from a broader set of sites, comparing the selected dose against the control.
- Final Analysis & Inconsistency Assessment: Pre-specify a cutoff
cfor the maximum allowable observed difference (e.g., in log-hazard ratio) between Stage 1 and Stage 2 results. Employ a statistical strategy (conservative, aggressive, or neutral) to decide whether to pool data from both stages or discard Stage 1 data, ensuring strong control of Type I error [54].
- Significance: This protocol explicitly incorporates and quantifies inconsistency, a common source of divergence between the expected (TPP) and actual drug performance.
Protocol: Systematic Gap Analysis for Needs Assessment
Originally developed for healthcare delivery improvement, this methodology is directly applicable to analyzing gaps in a product's clinical utility from a health systems perspective [55] [56].
- Objective: To establish a systematic, data-driven approach to identifying disparities between current practices (or product profiles) and evidence-based best practices (or TPP goals).
- Background: Gaps are defined as variances between local resources/processes and institutionally or nationally defined best practices [55].
- Methodology:
- Tool Development: Create a standardized assessment tool, often in a spreadsheet, organized around key domains. For a drug, this could be Program Infrastructure, Protocols/Policies/Order Sets, Healthcare Professional Education, and Automated Data Access [55].
- Data Collection: Representatives from different sites or studies complete the tool, selecting from drop-down menus (e.g., "enforced policy," "protocol," "none") for each component [55].
- Data Synthesis and Prioritization: Collate results into a summary format to clearly identify and prioritize the most significant and widespread gaps across the system [55].
- Actionable Planning: Use the results to direct resources, standardize processes, and gain support for initiatives aimed at closing the identified gaps [55].
- Significance: Provides a clear, visual, and collaborative method to focus efforts and resources on the areas of greatest need, directly informing TPP refinement.
Visualizing the Analytical Workflow
The process of analyzing discrepancies can be mapped as a logical workflow, guiding researchers from data collection to strategic insight. The diagram below illustrates this pathway.
Navigating Statistical Inconsistency in Adaptive Trials
A specific and complex challenge in late-stage development is managing inconsistency between trial phases. The following diagram details the statistical decision-making process in an adaptive Phase 2/3 trial.
Successfully executing the analyses and experiments described requires a suite of specific reagents, data sources, and methodological tools.
Table: Essential Resources for TPP vs. Actual Profile Research
| Tool / Resource | Function / Description | Application in Analysis |
|---|---|---|
| Target Product Profile (TPP) Template | A structured document outlining key product attributes (Indication, Efficacy, Safety, etc.) with "Minimum" and "Ideal" targets [5]. | Serves as the foundational blueprint against which the actual product profile is compared. |
| Clinical Trial Data Warehouse | A centralized repository for storing and managing structured, high-quality data from all phases of clinical development [33]. | Provides the "actual" data on efficacy, safety, and pharmacokinetics needed for the gap analysis. |
| Statistical Software (R, Python) | Programming environments with packages for complex statistical modeling, meta-analysis, and adaptive design simulation [54]. | Used to perform the formal inconsistency analysis and Type I error control calculations in adaptive trials [54]. |
| Gap Analysis Assessment Tool | A standardized survey or spreadsheet tool for systematically assessing variances against best practices [55]. | Enables the structured identification of disparities in clinical implementation or program infrastructure against the TPP's goals [55]. |
| WHO TPP Directory | A free, searchable database of Target Product Profiles for diseases with limited R&D incentives, emphasizing access and affordability [31]. | Provides a benchmark for understanding regulatory and public health priorities in specific disease areas. |
| Patent Data & Analytics Platforms | Databases containing detailed information on pharmaceutical patents, claims, and chemical compounds [57]. | Offers insights into competitive landscapes, novel mechanisms of action, and potential freedom-to-operate issues not fully captured in public bioactivity data [57]. |
The analysis of discrepancies between a drug's target and actual profile is a cornerstone of modern, evidence-based drug development. By systematically comparing these profiles using structured tables, employing rigorous experimental protocols to understand the root causes of divergence, and leveraging a defined toolkit of resources, research organizations can transform perceived setbacks into strategic intelligence. This disciplined approach fosters a culture of continuous learning, ultimately leading to more robust TPPs, more efficient clinical trials, and more successful medicines that better meet the needs of patients and healthcare systems.
The Target Product Profile (TPP) has long served as a foundational strategic document in pharmaceutical development, articulating a drug candidate's desired characteristics to guide research from preclinical stages through to commercialization. Traditionally, this profile has focused on clinical attributes such as efficacy, safety, and target population [5]. However, in today's evolving healthcare landscape, marked by increasing pricing pressures and rigorous health technology assessment (HTA) requirements, a paradigm shift is occurring. The future of TPPs demands the early integration of cost-effectiveness considerations and HTA principles to ensure that new products not only achieve regulatory approval but also secure favorable reimbursement and patient access [22].
This evolution reflects a critical recognition that regulatory approval is no longer sufficient for commercial success. Drugs must demonstrate clear value to payers and health systems [22]. This guide explores this transformation by comparing traditional and next-generation TPPs, providing structured data, experimental protocols, and strategic frameworks to help researchers and developers align product profiles with the comprehensive evidence requirements of modern healthcare systems.
Comparative Analysis: Traditional TPPs vs. Value-Informed TPPs
The integration of health economic and HTA principles fundamentally reshapes the structure and strategic application of TPPs. The table below summarizes the core differences between traditional and value-informed approaches.
Table 1: Comparison of Traditional and Value-Informed TPPs
| Component | Traditional TPP Focus | Value-Informed TPP Additions |
|---|---|---|
| Indication & Population | Clinical diagnosis and pathophysiology [5] | Prevalence, incidence, and size of treatable population from a payer perspective [22] |
| Efficacy & Effectiveness | Superiority against placebo or standard of care in controlled trials [5] | Comparative effectiveness versus relevant competitors and value of real-world outcomes [22] |
| Safety & Tolerability | Incidence and severity of adverse events [5] | Impact of safety profile on overall cost of care and health system resource use |
| Dosage & Administration | Dosing regimen and route of administration [5] | Impact of mode of administration on adherence, burden, and total treatment costs |
| Differentiators | Clinical differentiators (e.g., mechanism of action) [22] | Economic and humanistic differentiators (e.g., cost-effectiveness, quality of life) [22] |
| Affordability & Price | Often not a primary component [5] | Explicit consideration of target price and budget impact [5] [22] |
Quantitative Comparison of TPP Components
The following table provides examples of how minimum and ideal targets might be framed differently when incorporating value and access considerations.
Table 2: Quantitative Comparison of TPP Targets with HTA Integration
| Product Property | Minimum Acceptable (Traditional) | Ideal Target (Traditional) | Value-Informed Enhancement |
|---|---|---|---|
| Clinical Efficacy | Statistically significant improvement vs. placebo in primary endpoint [5] | Superior efficacy vs. standard of care [5] | Clinically meaningful improvement that justifies a cost-effectiveness ratio below local payer thresholds [58] [22] |
| Treatment Duration | Duration sufficient to demonstrate effect [5] | Shorter course or durable effect [5] | Duration that optimizes budget impact and demonstrates long-term value (e.g., reduced hospitalizations) |
| Patient-Reported Outcomes | Safety and tolerability questionnaire | Improvement in quality of life scale | PRO data validated and accepted by HTAs, showing value sufficient to support premium pricing [22] |
| Target Population | Broad, clinically-defined population [5] | Broad, clinically-defined population [5] | Stratified sub-populations where the product demonstrates the highest value-for-money [58] |
Experimental and Methodological Frameworks
Generating evidence for a value-informed TPP requires specific methodologies that extend beyond traditional clinical trials.
Protocol for Early Cost-Effectiveness Analysis
Objective: To conduct a preliminary economic evaluation during Phase II to inform clinical development and TPP refinement. Methodology:
- Model Structure: Develop a decision-analytic model (e.g., Markov or partitioned survival model) that reflects the natural history of the disease and the anticipated impact of the new therapy.
- Input Sourcing:
- Efficacy: Use Phase II clinical data for the experimental arm. For the comparator, source data from published trials or systematic reviews.
- Costs: Identify relevant cost components (e.g., drug acquisition, administration, monitoring, management of adverse events, and downstream medical costs) from published literature, claims databases, or expert opinion.
- Utilities: Derive health state utility weights (for QALY calculation) from published studies or map clinical outcomes to utilities using established algorithms.
- Analysis: Calculate the incremental cost-effectiveness ratio (ICER). Conduct extensive sensitivity and scenario analyses to identify key drivers of cost-effectiveness and the evidence gaps with the greatest uncertainty. Application to TPP: The results quantify the value proposition and identify the specific efficacy, safety, or durability targets needed for the therapy to be cost-effective at a given price point, directly informing the "Economic Value" attributes of the TPP [59] [22].
Protocol for Payer and HTA Stakeholder Testing
Objective: To qualitatively assess the value proposition and evidence requirements of key market payers and HTA bodies. Methodology:
- Structured Engagement: Conduct interviews or advisory boards with former regulators, HTA assessors, and payer representatives.
- Stimuli: Present a draft TPP, including clinical profile and potential price positioning.
- Data Collection: Use a structured discussion guide to explore:
- The perceived unmet need and the value of the proposed product profile.
- The comparator they would expect in a Phase III trial.
- The critical endpoints (clinical, economic, patient-reported) required for a positive reimbursement recommendation.
- The acceptable level of uncertainty and the need for post-launch evidence generation. Application to TPP: Feedback directly validates and refines the TPP, ensuring that the development strategy is aligned with the evidence needs of those who control market access [22].
The following diagram illustrates the strategic workflow for integrating these methodologies into TPP development.
Diagram 1: Strategic workflow for creating a value-informed TPP, showing how early data, payer feedback, and economic modeling feed into an iterative development process.
The Scientist's Toolkit: Key Reagents for Value Evidence Generation
Building a robust, value-informed TPP requires leveraging specific analytical tools and data sources.
Table 3: Essential Tools and Frameworks for Value Evidence Generation
| Tool / Framework | Function | Application in TPP Development |
|---|---|---|
| Decision-Analytic Model | A mathematical model (e.g., Markov, Partitioned Survival) used to simulate disease progression and estimate long-term costs and health outcomes of different interventions. | Used in early CEA to test under what clinical scenarios (e.g., overall survival benefit, rate of adverse events) the product becomes cost-effective [58] [59]. |
| Value Evidence Archetypes | Strategic frameworks (e.g., Clinical Benefit, Economic Value, PRO, RWE, Unmet Need) that define the types of evidence required to support access [22]. | Guides the selection of primary endpoints and data collection strategy in the TPP, ensuring alignment with what payers value most for a given product class [22]. |
| ARCH Model | A proposed successor to the TPP that separately defines requirements for Approval, Reimbursement, Commercial viability, and Hope [23]. | Provides a more nuanced structure for cross-functional teams to articulate and plan for different levels of clinical and commercial success, moving beyond a single predicted profile [23]. |
| Real-World Evidence (RWE) | Data derived from sources outside of traditional clinical trials, such as electronic health records, claims databases, and patient registries. | Informs the TPP by providing insights into real-world treatment patterns, patient heterogeneity, and comparative effectiveness, which are critical for HTA submissions [22]. |
Strategic Implementation and Future Directions
From Vision to Value: An Integrated Lifecycle Approach
Successfully implementing a value-informed TPP requires a coordinated, cross-functional strategy that evolves throughout the product lifecycle. The following table outlines this integrated approach.
Table 4: Lifecycle Approach for TPP and Evidence Alignment
| Development Stage | TPP Evolution | Value Evidence Strategy |
|---|---|---|
| Phase I/Preclinical | Defines the initial "hope" profile and identifies core value hypothesis based on unmet need [23]. | Initiate early economic modeling and conduct exploratory stakeholder testing to validate the value hypothesis [22]. |
| Phase II | Refines target clinical profile and begins to define minimum acceptable and ideal economic attributes. | Conduct preliminary CEAs to identify value drivers. Select primary Value Evidence Archetype(s) (e.g., Clinical Benefit, Economic Value) to guide Phase III design [22]. |
| Phase III | Locks core TPP elements for submission, incorporating regulatory and HTA feedback. | Finalize clinical trial design to capture endpoints required for HTA (e.g., PROs, resource use). Develop core economic models and draft HTA dossiers [22]. |
| Submission & Launch | The TPP becomes the basis for the product label and value story. | Submit integrated evidence packages to regulators, HTAs, and payers. Implement post-launch RWE studies to address remaining uncertainties and support lifecycle management [58] [22]. |
The ARCH Model: A Proposed Framework for the Future
The ARCH model addresses key flaws in the traditional "predicted TPP" by transparently separating the clinical and evidence requirements for different objectives [23]:
- Approval: The trial design and outcomes needed for regulatory approval in key markets.
- Reimbursement: The distinct evidence requirements for HTA bodies and payers, which often differ from regulators.
- Commercial Viability: The clinical profile needed to achieve target uptake and address unmet needs sufficiently for commercial success.
- Hope: The aspirational profile that represents a breakthrough for patients and justifies the R&D investment.
This model reframes investment discussions from a single, risky prediction to a more nuanced assessment of the evidence needed to satisfy different stakeholders, thereby de-risking development and enhancing the focus on value [23]. The relationship between these components is visualized below.
Diagram 2: The ARCH model framework, depicting the relationships between the core components of Approval, Reimbursement, Commercial viability, and Hope.
The future of drug development lies in the seamless integration of cost-effectiveness and HTA into the very fabric of the Target Product Profile. This is no longer a mere best practice but a strategic imperative for achieving market access and commercial success [22]. By adopting the structured comparisons, experimental protocols, and forward-looking frameworks outlined in this guide—such as the ARCH model and Value Evidence Archetypes—researchers and developers can bridge the historical gap between clinical ambition and economic reality. The organizations that master this integrated approach will be best positioned to deliver innovative therapies that not only reach patients but also demonstrate unequivocal value to health systems worldwide.
Conclusion
The journey from a strategic Target Product Profile to the final Actual Profile is complex and fraught with challenges, yet it is fundamental to successful drug development. A well-constructed and dynamically managed TPP serves as a powerful tool to align cross-functional teams, streamline regulatory interactions, and de-risk commercial outcomes. However, its true value is realized not through rigid adherence, but through strategic flexibility, early and ongoing stakeholder engagement, and a commitment to evidence-based iteration. By systematically comparing the TPP with the actual profile, organizations can extract critical lessons, refine their development processes, and foster a culture of continuous improvement. Future advancements will likely see TPPs becoming more integrated with real-world data and early economic evaluations, further solidifying their role as the cornerstone of efficient, patient-centric, and commercially successful biomedical innovation.
References
- 1. Premier Research | The Target Product Profile: Basics and Benefits [https://premier-research.com/perspectives/the-target-product-profile-basics-and-benefits/]
- 2. Constructing a Target Product Profile – Industry’s Perspective – Biocurate [https://www.biocurate.com/resources/constructing-a-target-product-profile-industrys-perspective/]
- 3. WHO target product profiles [https://www.who.int/observatories/global-observatory-on-health-research-and-development/analyses-and-syntheses/target-product-profile/who-target-product-profiles]
- 4. Facilitating the use of the target product profile in academic research: a systematic review | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05476-1]
- 5. Target Product Profiles (TPPs) for Medical Product Development [https://nida.nih.gov/funding/small-business-innovation-research-sbir-technology-transfer-sttr-programs/target-product-profiles]
- 6. Target product profiles for digital health technologies ... [https://www.frontiersin.org/journals/health-services/articles/10.3389/frhs.2025.1537016/full]
- 7. The New Pharma Playbook: A 2025-2030 Guide to Market ... [https://www.drugpatentwatch.com/blog/new-business-models-for-pharmaceutical-marketing-transforming-data-into-market-domination/?srsltid=AfmBOoqtTqC0l-f8F9qlAVtuvKMEPGsOLrO5ftMl2W9P5hVvUClPqVzz]
- 8. What's the Regulatory Value of a Target Product Profile? [https://www.sciencedirect.com/science/article/abs/pii/S0167779917300355]
- 9. AI in Pharma and Biotech: Market Trends 2025 and Beyond [https://www.coherentsolutions.com/insights/artificial-intelligence-in-pharmaceuticals-and-biotechnology-current-trends-and-innovations]
- 10. The Road To Commercial Success - The Target Product ... [https://premierconsulting.com/resources/blog/the-road-to-commercial-success-the-target-product-profile/]
- 11. Marrying Target Product Profile, Regulatory & Partnering ... [https://drug-dev.com/drug-development-strategies-marrying-target-product-profile-regulatory-partnering-strategies-for-long-term-product-success/]
- 12. Attacking the TPP - crafting a better alternative [https://ideapharma.substack.com/p/attacking-the-tpp-crafting-a-better]
- 13. TPP Testing In Pharma: Best Practices [https://glginsights.com/articles/tpp-testing-in-pharma-best-practices/]
- 14. A Scoping Review of Modelling in Target Product Profile ... [https://www.sciencedirect.com/science/article/abs/pii/S221188372500098X]
- 15. What is a Living Document? | DealHub [https://dealhub.io/glossary/living-document/]
- 16. How target product profiles guide drug development ... [https://www.iqvia.com/blogs/2025/09/how-target-product-profiles-guide-drug-development-through-uncertain-times]
- 17. Target Product Profile Optimization for Pharma Launches - Blog [https://blog.zoomrx.com/brand-builder/target-product-profile-optimization-for-pharma-launches/]
- 18. The Forgotten Power of the TPP: Why Many Biopharma ... [https://thelansis.com/blogs/the-forgotten-power-of-the-tpp-why-many-biopharma-projects-fail-without-it/]
- 19. Comparison of the FDA and EMA guidance on drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12280173/]
- 20. Product profiles [https://www.who.int/our-work/science-division/research-for-health/optimizing-research-processes/product-profiles]
- 21. Real-world evidence frameworks shape pharma decisions [https://www.drugdiscoverytrends.com/real-world-evidence-frameworks-pharma-decisions/]
- 22. Bridging Vision and Value: How Target Product Profiles ... [https://www.pharmexec.com/view/target-product-profiles-value-evidence-archetypes-market-access]
- 23. TPPs aren't working. It's time for a new approach in pharma ... [https://www.zs.com/insights/tpp-pharma-clinical-development-planning-arch-model]
- 24. The Winning Formula: Cross-Functional Collaboratio... [https://medicalaffairsspecialist.org/blog/the-winning-formula-cross-functional-collaboration-as-a-catalyst]
- 25. Target product profiles and strategies for drug development [https://www.ddw-online.com/target-product-profiles-and-strategies-for-drug-development-16263-202203/]
- 26. Stakeholder Engagement & Communication in BioPharma [https://pmsymposium.umd.edu/pm2023/session/stakeholder-engagement-communication-in-biopharma/]
- 27. Approval success rates of drug candidates based on target, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8212735/]
- 28. Better Benchmarking Improves Drug Development ... [https://www.intelligencia.ai/better-benchmarking-elevates-pharma-decision-making/]
- 29. What Is A Target Product Profile? A Full Guide ... [https://gmppros.com/target-product-profile/]
- 30. The Power of Target Product Profiles: Three Case Studies [https://nemetzgroup.com/the-power-of-target-product-profiles-three-case-studies/]
- 31. Frequently asked questions [https://www.who.int/our-work/science-division/research-for-health/target-product-profile-directory/frequently-asked-questions]
- 32. FDA-AACR Strategies for Optimizing Dosages for Oncology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536354/]
- 33. Five Predictions That Will Drive R&D Effectiveness in 2025 [https://www.appliedclinicaltrialsonline.com/view/five-predictions-rd-effectiveness-2025]
- 34. LEADERSHIP PANEL - What Will Have the Most Impact on ... [https://drug-dev.com/leadership-panel-what-will-have-the-most-impact-on-drug-development-in-2025/]
- 35. Drug Product Labeling Early in Clinical Studies [https://mmsholdings.com/perspectives/why-every-pharmaceutical-company-needs-to-plan-for-drug-product-labeling-early-in-clinical-studies/]
- 36. Patient-Focused Drug Development: Fit-for Purpose ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-focused-drug-development-selecting-developing-or-modifying-fit-purpose-clinical-outcome]
- 37. Regulatory strategy reimagined: Three trends accelerating ... [https://www.drugdiscoverytrends.com/regulatory-strategy-reimagined-three-trends-accelerating-drug-development/]
- 38. Incorporating Patient Input into the Target Product Profile [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181091/]
- 39. Target product profiles for new diagnostics to inform ... [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0012774]
- 40. Guiding the development of the tuberculosis screening ... [https://www.sciencedirect.com/science/article/pii/S2214109X2500244X]
- 41. WHO releases new Target Product Profiles for tuberculosis ... [https://www.who.int/news/item/13-08-2025-who-releases-new-target-product-profiles-for-tuberculosis-screening-tests]
- 42. Benchmark Strategies for Pharma Product Launches and ... [https://www.claritasrx.com/blog/benchmarking-pharmaceutical-product-launch/]
- 43. Types & Examples of Quantitative Data [https://www.fullstory.com/blog/quantitative-data-examples-types/]
- 44. Measuring Product Launch Success: A Complete Guide [https://launchpadagency.com/blog/blog-measure-success/]
- 45. Post-Launch Product Performance Tracking [https://kpidepot.com/kpi/post-launch-product-performance-tracking]
- 46. The Current Status of Drug Discovery and Development as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6226120/]
- 47. How to choose colors for data visualizations [https://www.atlassian.com/data/charts/how-to-choose-colors-data-visualization]
- 48. Color palettes and accessibility features for data visualization [https://medium.com/carbondesign/color-palettes-and-accessibility-features-for-data-visualization-7869f4874fca]
- 49. Understanding the anatomy and proper construction of tables [https://www.decisionfoundry.com/misc/articles/understanding-the-anatomy-and-proper-construction-of-tables/]
- 50. Target Product Profile Analysis of COVID-19 Vaccines in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7998902/]
- 51. WHO Target Product Profiles for COVID-19 Vaccines. ... [https://www.who.int/publications/m/item/who-target-product-profiles-for-covid-19-vaccines]
- 52. Efficacy of the tetravalent protein COVID-19 vaccine ... [https://www.nature.com/articles/s41467-024-49832-7]
- 53. BARDA Target Product Profiles (TPP) [https://medicalcountermeasures.gov/barda/tpp/]
- 54. Adjustment for Inconsistency in Adaptive Phase 2/3 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467493/]
- 55. A Gap Analysis Needs Assessment Tool to Drive a Care ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6214354/]
- 56. A gap analysis needs assessment tool to drive a care ... [https://pure.johnshopkins.edu/en/publications/a-gap-analysis-needs-assessment-tool-to-drive-a-care-delivery-and/]
- 57. The Missing Ingredient: Why Patent Data Is the Key to ... [https://www.drugpatentwatch.com/blog/the-missing-ingredient-why-patent-data-is-the-key-to-unlocking-ai-powered-drug-discovery/?srsltid=AfmBOorgyjBIDpl-jW07oBcPRotkSmcIX32osHwu7LLEfs9r7EvihsTq]
- 58. A Framework for Using Cost-effectiveness Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12227514/]
- 59. Using health technology assessment to set priority, inform ... [https://www.sciencedirect.com/science/article/pii/S0040162521004327]