Target Product Profile (TPP): The Strategic Blueprint for Successful Drug Development
This article provides a comprehensive guide to Target Product Profiles (TPPs), a critical strategic planning tool in biomedical product development.
Target Product Profile (TPP): The Strategic Blueprint for Successful Drug Development
Abstract
This article provides a comprehensive guide to Target Product Profiles (TPPs), a critical strategic planning tool in biomedical product development. Tailored for researchers, scientists, and drug development professionals, it explores the foundational concepts of TPPs, outlines methodologies for their creation and application across diverse product types including gene therapies and digital health tools, addresses common challenges and optimization strategies, and examines their role in regulatory validation and comparative planning. By synthesizing current case studies and regulatory perspectives, this resource equips teams to effectively use TPPs as living documents that align development efforts with clinical needs, regulatory requirements, and commercial success.
What is a Target Product Profile? Defining the Strategic Blueprint
Core Definition and Purpose of a TPP
A Target Product Profile (TPP) is a strategic development tool that outlines the desired characteristics of a medical product, serving as a foundational document that aligns research and development activities with specific clinical needs and regulatory requirements. This technical guide examines the core definition, structural components, and methodological applications of TPPs within pharmaceutical and medical device development, providing researchers and development professionals with evidence-based frameworks for implementation. Through analysis of current literature and regulatory guidance, we demonstrate how TPPs facilitate stakeholder alignment, optimize resource allocation, and increase the probability of regulatory and commercial success by maintaining a consistent focus on target product attributes throughout the development lifecycle.
Core Definition and Concept
A Target Product Profile (TPP) is a strategic planning tool that summarizes the key attributes and desired characteristics of a prospective medical product. Fundamentally, it outlines what the product is intended to do, for whom, and how it will achieve these objectives within the constraints of regulatory pathways and market realities. According to the National Institute on Drug Abuse (NIDA), a TPP "guides the development of safe and effective medical products" by detailing "its intended use, target population, and key performance features, ensuring that efforts in research and development align with specific clinical needs and regulatory requirements" [1].
The World Health Organization (WHO) further clarifies that TPPs "state intended use, target populations and other desired attributes of products, including safety and efficacy-related characteristics" [2]. In industry practice, this strategic document serves as a dynamic blueprint that evolves throughout the development process, with the primary goal of keeping all stakeholders aligned toward a common endpoint [3]. The TPP concept has expanded beyond traditional pharmaceutical applications to include medical devices, diagnostic tests, vaccines, and other healthcare technologies, making it a versatile tool across the medical product development spectrum.
Historical Context and Evolution
The TPP framework was formally introduced by the U.S. Food and Drug Administration (FDA) in 2007 through the draft guidance "Target Product Profile — A Strategic Development Process Tool" [1]. This guidance established the TPP as "a format for a summary of a drug development program described in terms of labeling concepts" [4]. By focusing development activities on prospective labeling claims, the TPP methodology aimed to minimize late-stage failures and streamline regulatory discussions.
Over the past decade, the application of TPPs has expanded significantly beyond regulatory interactions to become central to strategic planning across the development lifecycle. Public health organizations, including WHO and the Biomedical Advanced Research and Development Authority (BARDA), now routinely develop TPPs to address priority health needs and guide product development for underserved populations [2] [5]. The framework has proven particularly valuable for aligning stakeholders around products targeting diseases with significant unmet medical needs, where traditional market mechanisms may fail to drive development [4].
The Strategic Importance of TPPs
Alignment of Stakeholder Objectives
TPPs serve as a central reference document that aligns diverse stakeholders throughout the development process. By explicitly defining product requirements early in development, TPPs create a shared vision among research teams, regulatory affairs, commercial functions, investors, and ultimately regulatory agencies [3]. This alignment is particularly crucial in academic research settings, where translation of discoveries to viable products often fails due to misalignment between scientific innovation and practical clinical needs [6].
The systematic use of TPPs facilitates effective communication between manufacturers and health authorities, providing a structured framework for discussing development plans and regulatory expectations [7]. This proactive alignment reduces the risk of costly late-stage development changes and increases the likelihood of regulatory approval by ensuring all stakeholders work toward consistently defined goals from the earliest development stages.
Risk Mitigation and Resource Optimization
In the current development landscape, characterized by funding constraints and increasing regulatory scrutiny, TPPs provide a structured approach to risk management. By defining minimum acceptable and ideal target criteria for critical product attributes, TPPs enable development teams to identify potential failure points early and make data-driven decisions about continuing, modifying, or terminating development programs [8]. This proactive risk assessment is particularly valuable for emerging biotech and small pharma companies that must navigate resource constraints while advancing promising candidates [3].
The resource optimization benefits of TPPs extend throughout the development lifecycle. A well-constructed TPP helps focus research efforts on collecting evidence specifically required to demonstrate that a product meets its predefined criteria, reducing wasteful diversion of resources to non-essential activities [1]. This efficient allocation of resources is especially critical in areas of unmet medical need, where development resources are often limited and must be deployed as effectively as possible [9].
Regulatory and Commercial Success
Recent industry analyses demonstrate the growing importance of TPPs in an increasingly challenging development environment. IQVIA notes that "the average first year sales for the 51 products launched in 2022 was only $65 million," excluding COVID products, with first-year sales "steadily declining over the past 5 years" [3]. Simultaneously, regulatory challenges have increased, with FDA complete response letters (CRLs) almost tripling since 2018 [10].
In this context, TPPs provide a strategic framework for navigating both regulatory and commercial challenges. By articulating "the unmet medical needs of patients, physicians, and payers," a well-constructed TPP helps position and differentiate a product for both regulatory success and market adoption [10]. The forward-looking nature of TPPs enables development teams to anticipate and address potential regulatory and commercial challenges before they derail development programs, increasing the probability of successful product launch and adoption.
Table 1: Strategic Benefits of Target Product Profiles in Medical Product Development
| Strategic Benefit | Impact on Development Process | Stakeholders Served |
|---|---|---|
| Stakeholder Alignment | Creates shared vision and terminology across functions | Research, Regulatory, Commercial, Investors |
| Risk Mitigation | Identifies failure points early; enables go/no-go decisions | Portfolio Managers, Development Teams |
| Resource Optimization | Focuses efforts on critical path activities | Resource-Limited Organizations, Academic Researchers |
| Regulatory Success | Facilitates communication with health authorities | Regulatory Affairs, Clinical Development |
| Commercial Viability | Ensures product addresses market needs | Commercial Teams, Investors, Payers |
Structural Components of a TPP
Core Elements and Attributes
The structure of a TPP typically organizes product attributes according to a logical framework that mirrors both development priorities and eventual product labeling. While specific elements vary by product type and development stage, certain core components appear consistently across high-quality TPPs. Based on analysis of multiple TPP frameworks from regulatory and public health organizations, the following elements represent the foundational architecture of a comprehensive TPP [1] [8] [5]:
- Indications and Usage: The specific disease or condition the product is intended to diagnose, treat, or prevent.
- Target Population: Demographic and clinical characteristics of the intended patient population.
- Dosage and Administration: Route of administration, dosage form, strength, and treatment regimen.
- Clinical Efficacy: Parameters and endpoints demonstrating therapeutic or diagnostic performance.
- Safety Profile: Adverse reactions, contraindications, warnings, and precautions.
- Pharmacology/Technical Properties: Mechanism of action, pharmacokinetics, or technical specifications.
- Product Stability and Storage: Shelf life, storage conditions, and handling requirements.
- Affordability and Accessibility: Cost considerations and availability for target populations.
These core elements provide the structural foundation upon which product-specific attributes are built, ensuring comprehensive coverage of factors critical to development success and eventual product utilization.
Performance Thresholds: Minimum Acceptable vs. Ideal Targets
A defining feature of effective TPPs is the specification of performance thresholds for each attribute. Most TPPs utilize at least two levels of target performance: a "minimum acceptable" threshold that represents the lowest performance level sufficient for product viability, and an "ideal" target that represents the optimal performance profile [1] [8]. This dual-threshold approach creates a development roadmap that clearly distinguishes between essential requirements and aspirational goals.
According to industry perspective, "Failure to meet the parameters defined as 'essential' will often mean termination of product development. Exceeding these parameters or meeting the 'ideal' profile will likely increase the value of the product" [8]. This tiered approach enables development teams to make strategic decisions about resource allocation and provides a clear framework for evaluating development progress against predefined benchmarks.
Table 2: Comparative TPP Structures Across Product Types
| Product Attribute Category | Pharmaceutical Products [1] | Medical Devices [1] | Diagnostic Tests [1] | Vaccines [5] |
|---|---|---|---|---|
| Intended Use | Indications and Usage | Intended Use/Indications for Use | Unmet Clinical Need/Intended Use | Indication for Use |
| Target Population | Target Population | Patient Population | Target User/Target Population | Target Population |
| Efficacy/Performance | Clinical Efficacy | Summary of Clinical Testing | Analytical Performance/Clinical Validity | Clinical Efficacy |
| Safety | Adverse Reactions | Safety Analysis/Risk for Health | Not Typically Specified | Safety/Reactogenicity |
| Dosage/Administration | Dosage and Administration, Delivery Mode | Treatment Duration | Time to Result, Sample Type | Dose Regimen, Route of Administration |
| Product Specifications | Dose Form, Strength | Summary of Technological Characteristics | Assay Design/Format, Sample Volume | Not Typically Specified |
| Stability/Storage | Product Stability and Storage | Not Typically Specified | Stability During Transport, Storage Conditions | Shelf Life, Storage Temperature |
| Cost Considerations | Affordability (Price) | Affordability (Price) | Affordability (Price) | Not Typically Specified |
TPP Development Methodology
Systematic Development Process
The development of a robust TPP requires a structured methodology that incorporates diverse perspectives and evidence-based decision making. A systematic review published in the Journal of Translational Medicine identified three distinct phases for TPP development: scoping, drafting, and consensus-building [6]. This methodological framework ensures that TPPs are grounded in comprehensive analysis and stakeholder input, increasing their utility throughout the development process.
The scoping phase involves comprehensive landscape analysis to understand current treatment options, unmet needs, and competitive environments. This includes literature review, analysis of existing product labels, and assessment of regulatory precedents [1] [8]. The drafting phase translates these insights into an initial TPP structure with defined attributes and target values. Finally, the consensus-building phase engages diverse stakeholders to refine the TPP and establish shared commitment to the development goals it defines [6] [4].
Stakeholder Engagement and Consensus Building
Effective TPP development requires systematic engagement of diverse stakeholders throughout the process. Renaissance Philanthropy emphasizes that "creating a TPP is a collaborative exercise" that should include "representatives from the following groups: researchers, industry, international public organizations, advocacy groups and associations, policy makers, laboratory experts, technical/funding agencies, implementers, modelers, economists, donors, and market experts" [4].
Consensus-building typically employs structured techniques including surveys scored on Likert scales, facilitated discussions focusing on areas of disagreement, and iterative refinement of proposed targets [4]. This process must balance the sometimes competing priorities of different stakeholder groups, particularly regarding tensions between ideal product characteristics and practical development constraints. The resulting consensus creates not only a technically sound TPP but also stakeholder buy-in critical to its effective implementation throughout the development lifecycle.
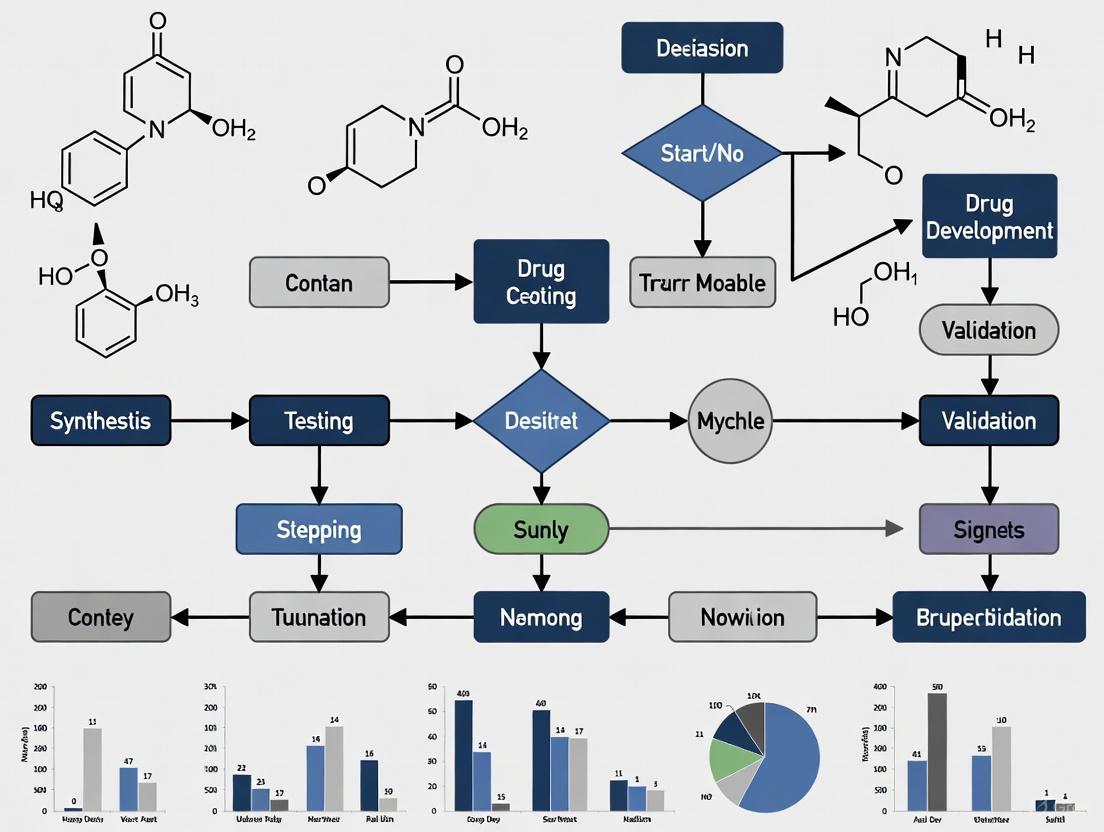
Diagram 1: TPP Development Workflow. This diagram illustrates the three-phase methodology for systematic TPP development, from initial scoping through final document completion.
TPPs in Practice: Implementation and Applications
Integration with Development Workflows
Successful TPP implementation requires deliberate integration into ongoing development workflows and decision-making processes. From an industry perspective, TPPs should function as "living documents" that are regularly updated as new data emerges and development contexts evolve [3]. This dynamic nature ensures that TPPs remain relevant and actionable throughout the typically long development lifecycle for medical products.
The utility of TPPs evolves throughout the development process. In early-stage development, TPPs help navigate high uncertainty and establish foundational goals with limited data. In late-stage development, they become more refined, integrating robust clinical data and commercial projections [3]. This evolutionary approach ensures that TPPs provide appropriate guidance at each development stage while maintaining consistency with the overarching product vision established early in the process.
Sector-Specific Applications
Pharmaceutical Development
In pharmaceutical development, TPPs are typically structured around eventual labeling concepts, with sections corresponding to prescribing information [1] [7]. This labeling-focused structure directly connects development activities to regulatory requirements, facilitating efficient agency interactions and alignment on evidence requirements. The drug development TPP comprehensively addresses clinical pharmacology, indications and usage, dosage and administration, safety considerations, and product stability [1].
Medical Devices and Diagnostics
For medical devices and diagnostic tests, TPPs emphasize technical performance characteristics, human factors, and usability considerations [1]. The diagnostic TPP framework includes attributes such as analytical performance, sample type, time to result, and ease of interpretation [1]. These product-specific attributes reflect the different evidentiary and usability requirements for non-pharmaceutical medical products while maintaining the core TPP function of aligning development with user needs.
Public Health and Global Health Applications
In public health contexts, TPPs serve to articulate priority product characteristics for funders and developers, with particular emphasis on accessibility and affordability for underserved populations [2] [9]. Organizations including WHO, Drugs for Neglected Diseases initiative (DNDi), and BARDA use TPPs to guide development of products addressing public health priorities, from neglected diseases to medical countermeasures for health security threats [2] [9] [5]. These TPPs explicitly consider implementation contexts and cost constraints that may not be prioritized in commercial development settings.
Diagram 2: TPP Stakeholder Alignment Framework. This diagram illustrates how the TPP serves as a central coordinating document that aligns both internal development functions and external stakeholders throughout the product development lifecycle.
The development and implementation of robust TPPs requires access to specific data resources and analytical tools. The following table summarizes key informational resources that support evidence-based TPP development.
Table 3: Essential Research Resources for TPP Development
| Resource Category | Specific Examples | Application in TPP Development | Access Considerations |
|---|---|---|---|
| Regulatory Guidelines | FDA TPP Draft Guidance (2007) [1] | Provides structural framework and regulatory expectations | Publicly available |
| Competitive Landscape Data | Approved product labels [8] | Establishes benchmarks for minimum acceptable and ideal targets | Publicly available through FDA databases |
| Clinical Endpoint Standards | FDA therapeutic area guidelines [8] | Informs selection of validated efficacy endpoints | Publicly available |
| Epidemiological Data | Disease incidence/prevalence studies [8] | Defines target population and quantifies unmet need | Varies by source; some proprietary |
| Stakeholder Input Frameworks | Consensus-building templates [4] | Supports structured engagement of diverse stakeholders | Adaptable from published methodologies |
| Performance Benchmarking Tools | Clinical trial databases [3] | Provides comparators for efficacy and safety targets | Mixed public/proprietary access |
The Target Product Profile represents a foundational strategic tool in medical product development, providing a structured framework for aligning diverse stakeholders around a shared product vision. By defining desired product characteristics early in development and maintaining this strategic focus throughout the development lifecycle, TPPs increase the efficiency and success probability of development programs across therapeutic areas and product types. The continued evolution of TPP methodologies, including potential integration of artificial intelligence and other advanced analytical techniques, promises to further enhance their utility in navigating the increasing complexities of medical product development [3]. As development challenges grow more complex, the disciplined approach embodied by rigorous TPP development and implementation will remain essential for translating scientific innovation into clinically meaningful products that address pressing patient needs.
A Target Product Profile (TPP) serves as a strategic blueprint that outlines the key objectives a drug or medical product must meet to gain regulatory approval and reach patients [3]. It embodies the crucial concept of "beginning with the goal in mind," providing a structured framework that guides the entire development process from initial discovery through clinical trials and regulatory submission [11]. Originally formalized by the US Food and Drug Administration (FDA) as a strategic development process tool, the TPP has evolved from a regulatory document into a comprehensive strategic asset that aligns scientific, regulatory, and commercial goals across the healthcare ecosystem [3] [11].
The fundamental purpose of a TPP is to create a shared definition of success across all functions involved in product development. It typically outlines three tiers of targets: minimum viable criteria for regulatory approval, base case expectations for performance, and aspirational goals that define true product differentiation and market success [3]. This multi-tiered approach allows development teams to navigate uncertainty while maintaining focus on core objectives, making it particularly valuable in today's complex and rapidly evolving pharmaceutical landscape where disruption has become the norm [3] [12].
Core Components and Structure of a TPP
A well-constructed TPP provides a comprehensive framework that captures both clinical and commercial considerations. While specific elements may vary by product type and development stage, the core components establish a common language and set of priorities across the organization.
Foundational Elements of a TPP
The structure of a TPP typically follows the logic of a future product label, ensuring alignment with regulatory requirements while addressing practical clinical use. The National Institute on Drug Abuse (NIDA) provides a standardized worksheet that exemplifies this structured approach, mapping key attributes from drug labeling to specific product properties [1].
Table 1: Core Components of a Pharmaceutical TPP
| Drug Label Attribute | Product Properties | Minimum Acceptable Results | Ideal Results |
|---|---|---|---|
| Indications and Usage | Primary Indication | Mitigation of opioid withdrawal symptoms | Complete cessation of withdrawal symptoms with improved retention in care |
| Indications and Usage; Clinical Studies | Target Population | Adults with opioid dependence | Adults and adolescents across multiple substance use disorders |
| Dosage and Administration | Treatment Duration | Up to 14 days | Single administration with sustained effect |
| Dosage and Administration | Delivery Mode | Oral | Long-acting injectable or implant |
| Dosage and Administration | Dose Regimen | Three tablets, four times daily | Once-daily dosing |
| Dosage Forms and Strengths | Dose Form | 0.18mg tablet | Multiple strength options for flexible dosing |
| Clinical Studies | Clinical Efficacy | Mean reduction in withdrawal scores | Significant improvement in treatment completion rates |
| Adverse Reactions | Risk/Side Effect | Manageable hypotension, bradycardia | No cardiovascular effects |
| How Supplied, Storage and Handling | Product Stability and Storage | Stable at 25°C (77°F) | Stable at ambient temperatures (10°C - 40°C) |
| Clinical Pharmacology | Mechanism of Action, Pharmacokinetics | Central alpha-2 adrenergic agonist | Novel mechanism with reduced side effect profile |
| Drug Interactions | Drug Interactions | Limited interaction with common therapies | No significant drug interactions |
| - | Affordability (Price) | Lower than existing branded options | Priced comparably to generic alternatives |
| - | Accessibility | Prescription requirement | Available in multiple care settings |
This structured approach ensures that every aspect of product development is guided by clear, measurable targets that balance what is scientifically achievable with what is clinically desirable and commercially viable [1].
TPP Applications Across Product Types
The TPP framework extends beyond traditional pharmaceuticals to encompass diverse medical products, including medical devices and diagnostic tests. The core principles remain consistent, while specific attributes are tailored to the technology and its intended use.
Table 2: TPP Adaptation Across Medical Product Types
| Product Type | Key TPP Considerations | Example Application |
|---|---|---|
| Pharmaceuticals | Efficacy, safety, dosing regimen, pharmacokinetics, drug interactions | Medication for opioid use disorder with improved safety profile [1] |
| Medical Devices | Intended use, technological characteristics, clinical performance, usability | Non-invasive transcranial stimulator for opioid withdrawal symptoms [1] |
| Diagnostic Tests | Analytical performance, clinical validity, ease of use, time to result | Rapid fentanyl test strip with high sensitivity and specificity [1] |
| Global Health Products | Stability in field conditions, cost, route of administration, training requirements | Treatments for neglected tropical diseases requiring minimal healthcare infrastructure [9] |
This adaptability demonstrates the TPP's utility as a universal strategic tool across the medical product development landscape, providing appropriate scaffolding for diverse technologies while maintaining a consistent development philosophy [1] [9].
The Evolution of TPP Strategy and Application
The application of TPPs has significantly evolved from a static regulatory exercise to a dynamic strategic process that shapes decision-making throughout the product lifecycle. This evolution reflects the increasing complexity of drug development and the need for more sophisticated approaches to manage risk and uncertainty.
From Regulatory Document to Strategic Compass
Initially, TPPs primarily served as communication tools with regulatory agencies, focusing on label requirements and approval criteria. However, the high failure rate of late-stage clinical trials for strategic rather than scientific reasons prompted a fundamental shift in TPP utilization [11]. Industry analysis revealed that nearly 24% of late-stage (Phase 2/3) clinical studies fail due to strategic or commercial issues rather than operational problems or product safety and efficacy [11].
This recognition transformed the TPP from a static document into what industry leaders now describe as a "strategic compass" or "North Star" that guides decision-making across the organization [3] [13]. This evolved approach requires:
- Cross-functional ownership involving R&D, commercial, market access, and manufacturing teams rather than siloed responsibility [13]
- Dynamic updating that incorporates emerging data and reflects changes in the external environment [3]
- Explicit linkage to decision gates that drive go/no-go choices rather than merely serving reporting functions [13]
The impact of this strategic approach is quantifiable. Data show that development programs that referenced a TPP in their New Drug Application (NDA) submission underwent a median review time that was 30 days shorter than those that did not. Furthermore, nearly 5% of NDAs approved between 2008 and 2015 that did not reference a formal TPP received an initial refuse-to-file notification, whereas none that referenced a formal TPP received that notification [11].
Expansion into Public Health and Global Access
Simultaneously, the TPP framework has expanded beyond commercial drug development to address global public health challenges. Organizations like the Drugs for Neglected Diseases Initiative (DNDi) have adapted TPPs to prioritize patient access and affordability in resource-limited settings [9].
This public health orientation introduces distinct priorities into the TPP development process:
- Affordability as a critical design constraint rather than an afterthought [9]
- Field suitability including stability in challenging environmental conditions and minimal training requirements [9]
- Access considerations that ensure products reach marginalized populations [1]
The evolution of the TPP reflects a broader recognition that technical success and commercial success are not synonymous, and that intentional design and strategic alignment from the earliest development stages are essential for products to achieve their intended public health impact [13] [9].
TPP Testing and Validation Methodologies
As TPPs have grown more strategic, so have the methodologies for testing and validating their assumptions. Quantitative TPP testing has emerged as a critical discipline for de-risking development decisions and aligning internal expectations with market realities.
Experimental Protocol for Quantitative TPP Testing
TPP testing employs structured market research methodologies to evaluate a product's potential value proposition with key stakeholders before significant development resources are committed. The process follows a systematic approach [14]:
- TPP Formatting: The first step involves translating the TPP into a short, optimized summary (typically one page) that groups clinical elements for clear communication. This format facilitates respondent understanding and maximizes feedback quality from healthcare professionals [14].
- Audience Identification: The appropriate expert population is selected based on the research objectives. This may include:
- Structured Data Collection: A series of streamlined and semi-standardized questions are administered to gather unbiased feedback on:
- Understandability of the product concept
- Credibility of the proposed claims
- Perceived differentiation from existing options
- Prescription/usage potential under various scenarios [14]
- Scenario Analysis: Multiple TPP versions (e.g., worst-case, base-case, best-case) are tested to evaluate how different clinical outcomes might impact market potential [14].
This methodology provides empirical data to inform portfolio prioritization, clinical development strategy, and commercial planning [14].
Application Across the Development Lifecycle
TPP testing provides value at multiple decision points throughout the product lifecycle, with the research focus evolving as the product advances [14]:
- Business Development & Licensing: Corporate strategy teams use TPP testing to evaluate external assets for acquisition or licensing, helping to size market opportunities and fact-check selling claims made by external companies [14].
- Early Drug Development: Teams responsible for internal innovation test different clinical scenarios for drugs in the early pipeline (preclinical through Phase 1) to inform prioritization strategies and quantify the risks and benefits of each scenario [14].
- Launch Preparation: Marketing and commercial teams use TPP testing for late-stage drugs (Phase 2 through pre-approval) to confirm and refine prescription assumptions, inform sales forecasts, and optimize launch strategies [14].
The following diagram illustrates the continuous TPP testing workflow throughout the drug development lifecycle:
Diagram: TPP Testing Workflow in Drug Development
Essential Research Reagents for TPP Development
Creating and testing a robust TPP requires both strategic frameworks and practical research tools. The following table details key methodological components and their functions in the TPP development and testing process.
Table 3: Research Reagents for TPP Development
| Research Component | Function | Application in TPP Process |
|---|---|---|
| Structured TPP Template | Standardized format for capturing product attributes | Ensures comprehensive consideration of all critical development criteria; facilitates cross-functional alignment [1] |
| Competitive Landscape Analysis | Assessment of existing and emerging treatments | Establishes benchmarking criteria; identifies differentiation opportunities and minimum acceptable targets [1] |
| Healthcare Professional Surveys | Quantitative assessment of clinical value proposition | Tests understandability, credibility, and prescription potential of TPP attributes with key prescribers [14] |
| Stakeholder Mapping Framework | Identification of relevant expert populations | Ensures appropriate audience selection for TPP testing across multiple specialties and decision-making roles [14] |
| Scenario Testing Models | Evaluation of multiple clinical outcome possibilities | Quantifies market potential under worst-case, base-case, and best-case clinical scenarios [14] |
| Regulatory Precedent Analysis | Review of previous regulatory decisions and guidance | Informs realistic minimum criteria for approval; identifies potential regulatory hurdles [3] |
These methodological "reagents" form a toolkit that enables systematic development and validation of TPP assumptions, transforming subjective hypotheses into data-driven strategies [14] [1].
Future Directions and Emerging Applications
The evolution of TPPs continues as new technologies and market dynamics create both challenges and opportunities for more sophisticated application of this strategic tool.
Artificial Intelligence in TPP Development
Artificial intelligence is beginning to play a transformative role in streamlining TPP creation and refinement. Current AI applications include [3]:
- Data Extraction: Mining insights from vast quantities of scientific and regulatory literature to inform TPP assumptions
- Template Generation: Creating first-draft TPP templates based on structured prompts and historical data
- Horizon Scanning: Identifying emerging changes in regulatory or therapeutic landscapes that might impact development strategies
The future potential lies in what industry experts term "agentic AI" – autonomous tools that could dynamically update TPPs or flag strategic shifts based on real-time data analysis [3]. However, significant challenges remain, including the reliance on publicly available data that skews toward successful trials and omits valuable insights from failed studies, as well as limited access to proprietary commercial data that limits AI's effectiveness in modeling market outcomes [3].
Evolving Regulatory and Market Landscape
The regulatory environment for pharmaceutical products continues to evolve, particularly in the United States where emerging policies are creating new considerations for TPP development [15] [12]. Recent developments include:
- Price Alignment Policies: Movement toward "Most-Favored-Nation" pricing that aligns US drug prices with the lowest prices paid by peer countries [15]
- Manufacturing Reshoring: Incentives and pressures to locate pharmaceutical manufacturing in the United States [15]
- Transparency Initiatives: Executive orders aimed at increasing competition and transparency in prescription drug markets [15]
These trends make contingency planning an increasingly critical component of TPP strategy. Development teams must consider not only current regulatory climates but also anticipate what approval and market access requirements might look like five to seven years in the future when their products reach the market [3] [12].
The Target Product Profile has evolved substantially from its origins as a regulatory document to become a central strategic tool guiding drug development across multiple domains. This evolution reflects the pharmaceutical industry's growing recognition that scientific excellence alone is insufficient to ensure that valuable medicines reach the patients who need them. The modern TPP serves as a dynamic strategic framework that aligns cross-functional teams, anticipates market realities, and adapts to emerging data throughout the development lifecycle.
As the industry faces ongoing disruption from technological advances, policy changes, and evolving market dynamics, the disciplined application of TPPs offers stability and strategic clarity [3]. By defining success from the outset and maintaining alignment across functions, organizations can navigate the inherent uncertainties of drug development with greater confidence and efficiency. The continued evolution of TPP practice – including the integration of artificial intelligence and more sophisticated testing methodologies – promises to further enhance their value in bridging the gap between scientific innovation and patient impact across both commercial and public health contexts.
Key Components of a Robust TPP Structure
A Target Product Profile (TPP) serves as a strategic development tool that outlines the desired characteristics of a planned medical product, procedure, or service. This strategic blueprint guides research and development by specifying key objectives a product must meet to gain regulatory approval and reach patients, ensuring alignment among stakeholders from the earliest development stages [3] [6]. In the context of academic research, TPPs facilitate communication with funders and align development strategies with prioritized public health needs, thereby increasing translational research efficiency [2] [6]. A well-structured TPP provides a clear vision for product development, enhances decision-making, minimizes risks, and increases the likelihood of successful regulatory approval and market adoption [1].
Core Components of a TPP
A robust TPP structure systematically outlines both the intended use and the specific performance characteristics required for a successful product. These components are typically organized in a table format that compares minimum acceptable criteria against ideal targets, providing a clear development roadmap [1].
Table 1: Fundamental TPP Components for a Pharmaceutical Product
| Drug Label Attribute | Product Property | Minimum Acceptable Results | Ideal Results |
|---|---|---|---|
| Indications and Usage | Primary Indication | Mitigation of opioid withdrawal symptoms | Broader indication for multiple substance use disorders |
| Indications and Usage; Clinical Studies | Target Population | Adults meeting criteria for opioid dependence | Expanded population including adolescents |
| Dosage and Administration | Treatment Duration | Up to 14 days | Longer maintenance therapy options |
| Dosage and Administration | Delivery Mode | Oral | Multiple delivery options (e.g., extended-release injection) |
| Dosage Forms and Strengths | Dose Form | 0.18mg tablet | Multiple strengths and formulations |
| Clinical Studies | Clinical Efficacy | Superior to placebo on validated clinical scales | Demonstrated superiority to existing standard of care |
| Adverse Reactions | Risk/Side Effect Profile | Acceptable safety profile with manageable side effects | Superior safety compared to existing treatments |
| How Supplied, Storage and Handling | Product Stability and Storage | Stable at 25°C (77°F) | Less restrictive storage conditions |
| Clinical Pharmacology | Mechanism of Action, Pharmacokinetics, Pharmacodynamics | Defined mechanism and half-life | Favorable pharmacokinetic profile supporting less frequent dosing |
| Drug Interactions | Drug Interactions | Minimal clinically significant interactions | No significant drug interactions |
| Affordability (Price) | Cost | Lower than existing branded alternatives | Cost-effective with high value-based reimbursement potential |
| Accessibility | Availability | Prescription basis | Over-the-counter or simplified prescribing process |
The structure emphasizes access, equity, and affordability as integral parts of the innovation process that must be considered at all development stages, not just after a product is created [2]. Many TPPs feature either one threshold level of product performance (56.5%) or two levels (minimum acceptable and ideal) to define product requirements [6].
TPP Applications Across Product Types
The TPP framework adapts to various medical product categories, including therapeutics, medical devices, and diagnostic tests, with specific components tailored to each product's technological and regulatory requirements.
Medical Devices
For medical devices, the TPP focuses on technological characteristics, clinical performance metrics, and usability factors that differ from pharmaceutical products.
Table 2: TPP Components for a Medical Device (Example: Opioid Withdrawal Device)
| Product Property | Benchmark Device (NET Recovery) | Minimum Acceptable Results | Ideal Results |
|---|---|---|---|
| Intended Use/Indications for Use | Non-invasive stimulator for opioid withdrawal symptoms in conjunction with standard medications | Stand-alone treatment for mild to moderate withdrawal symptoms | Broad spectrum use across multiple withdrawal syndromes |
| Patient Population | Patients aged 18+, diagnosed with OUD, with moderate COWS score | Expanded age range including older adolescents | No restrictions based on comorbidity profiles |
| Treatment Duration | 1 hour per day, not to exceed 7 days | Shorter daily treatment duration | Extended treatment duration without time limitations |
| Summary of Technological Characteristics | Electrical stimulation at auricular region | Multiple stimulation modalities with customizable parameters | Home-use capability with remote monitoring |
| Summary of Clinical Testing | 61.3% mean reduction in COWS score at 60 minutes | Statistically significant improvement over sham treatment | Superior efficacy compared to pharmacological approaches |
| Safety Analysis/Risk for Health | Risks consistent with predicate device | No serious adverse events | Superior safety profile to predicate device |
| Affordability (Price) | $600 - $1,500 | Lower price point with maintained efficacy | Cost-saving compared to standard treatment pathways |
| Accessibility | Prescription use | Simplified prescription process | Direct-to-consumer availability |
Diagnostic Tests
For diagnostic tests like the fentanyl urine test example, the TPP emphasizes analytical performance, ease of use, and practical implementation factors.
Table 3: TPP Components for a Diagnostic Test (Example: Fentanyl Urine Test)
| Product Property | Benchmark Test (InstaStrip Fentanyl Rapid Test) | Minimum Acceptable Results | Ideal Results |
|---|---|---|---|
| Unmet Clinical Need | Detection of fentanyl in urine | Detection of fentanyl and major analogs | Broad spectrum detection of synthetic opioids |
| Intended Use | Detection of fentanyl concentrations in urine >1 ng/ml | Quantitative results with defined cutoffs | Point-of-care quantitative monitoring |
| Target User | Adults 18 years and older | Minimal training required for accurate use | No specialized training required |
| Stability During Transport | +10°C - +30°C | +10°C - +30°C | +4°C - +40°C |
| Analytical Performance | Lateral flow immunoassay | Improved sensitivity and specificity | Novel detection methodology with superior performance |
| Sample Type | Urine | Multiple sample types (urine, saliva, blood) | Non-invasive sample collection |
| Time to Result | 5 minutes | 10 minutes | 3 minutes |
| Diagnostic Sensitivity | 0.5 ng/ml | 0.2 ng/ml | 0.1 ng/ml |
| Reproducibility | 0.98 | >0.95 | >0.99 |
| Test Size and Portability | 0.5'x 0.3'x 0.2' (box) | Smaller footprint | Discreet, pocket-sized design |
| Affordability (Price) | $2 per test strip | Lower cost per test | Significant cost reduction for mass screening |
Methodological Framework for TPP Development
The development of a robust TPP follows a systematic process that incorporates diverse stakeholder inputs and evolves throughout the product lifecycle.
Development Process
A systematic review of TPP methodologies identified that TPP development typically follows a structured approach, though most papers do not fully describe their methods [6]. Based on available evidence, the optimal development process includes three key phases:
- Identifying Unmet Needs: Comprehensive analysis of the current treatment landscape, existing alternatives, and precise definition of the clinical gap the product will address [1] [6].
- Initial Drafting: Creating the first TPP version with input from cross-functional experts, including clinical, regulatory, and commercial perspectives [6].
- Building Consensus: Engaging stakeholders to refine the TPP, ensuring alignment on minimum and ideal targets [6].
Stakeholder Engagement and Evolution
TPPs are dynamic documents that evolve throughout the drug development lifecycle. In early-stage development, TPPs help navigate high uncertainty and establish foundational goals, while in late-stage development, they integrate robust data and commercial projections [3]. Successful TPP development requires collaboration between stakeholders from academia, industry, and regulatory bodies, with tools like TPPs supporting communication and product development in academic settings as effectively as in industry [6].
Artificial intelligence is emerging as a valuable tool in TPP development, capable of extracting insights from scientific and regulatory literature, generating first-draft TPP templates, and assisting in horizon scanning to identify changes in regulatory or therapeutic landscapes [3].
Table 4: Essential Resources for TPP Development
| Resource Category | Specific Resource | Function in TPP Development |
|---|---|---|
| Regulatory Guidance | FDA TPP Guidance (2007) | Provides framework for structuring TPP content and regulatory expectations [1] |
| Therapeutic Landscape Analysis | Drug Labeling of Existing Products | Establishes benchmarks for minimum acceptable and ideal product profiles [1] |
| Stakeholder Engagement | Expert Interviews & Workshops | Facilitates consensus building on TPP features and performance thresholds [6] |
| Disease Area Context | WHO TPPs for Public Health Priorities | Aligns development with global health needs and identifies preferred product characteristics [2] |
| Technical References | Published TPP Examples in Literature | Provides templates and methodologies for TPP structure and development processes [6] |
| Analytical Tools | AI-Assisted Data Extraction | Streamlines TPP creation by analyzing scientific literature and identifying regulatory precedents [3] |
A robust TPP structure serves as the foundational strategic document that guides successful medical product development from concept to commercialization. By clearly defining minimum acceptable and ideal target profiles across key product characteristics—including indications, target population, efficacy, safety, delivery, stability, and affordability—the TPP aligns stakeholders and focuses development efforts. The dynamic nature of TPPs requires regular refinement as products advance through development stages and new data emerges. When properly implemented, this structured approach to TPP development significantly enhances decision-making, reduces development risks, and increases the likelihood of creating successful products that address genuine unmet medical needs.
A Target Product Profile (TPP) serves as a strategic planning tool that outlines the desired characteristics of a medical product, guiding its development from conception to commercialization. Fundamentally, a TPP defines the intended use, target population, and key attributes of a product, including safety and efficacy characteristics [2]. In the pharmaceutical industry, this document acts as a strategic blueprint, outlining minimum viable criteria for regulatory approval, base case expectations for performance, and aspirational goals that define true commercial and therapeutic success [3]. Rather than remaining a static document, the most effective TPPs are dynamic planning tools that evolve in response to emerging data, regulatory feedback, and shifting clinical landscapes. This living nature makes the TPP indispensable for aligning scientific, regulatory, and commercial objectives throughout the complex drug development lifecycle, ensuring every development decision is purposeful and data-driven [3].
The TPP as a Dynamic Development Tool
The Iterative Nature of TPP Development
The concept of a TPP as a living document emerges from its iterative application throughout the product development lifecycle. Industry leaders recommend adopting a circular development approach that begins with identifying the product's intended clinical application, followed by a development program guided by and ultimately returning to the intended clinical use [16]. This "bedside to bench and back again" methodology ensures preclinical efforts remain aligned with clinical objectives, avoiding wasted resources and streamlining overall development.
The utility and specificity of TPPs naturally evolve as a drug progresses through development stages. During early-stage development, TPPs help navigate high uncertainty and establish foundational goals with limited available data. As the program advances into late-stage development, TPPs become increasingly refined, integrating robust clinical data, validated biomarkers, and sophisticated commercial projections [3]. This evolutionary process requires continuous refinement based on new information, with many organizations shifting toward more integrated approaches where development and commercial teams collaborate throughout the lifecycle to ensure TPPs remain dynamically relevant to current development challenges and opportunities.
Practical Implementation of TPP Evolution
Implementing a living TPP requires structured processes for updates and cross-functional alignment. A well-structured TPP provides a clear strategic vision that enhances decision-making, minimizes development risks, and increases the likelihood of successful regulatory approval and market adoption [1]. To maintain this strategic relevance, development teams should establish regular review milestones tied to key development events—such as completion of Phase 1 studies, end-of-Phase 2 meetings, or pre-NDA/BLA submissions—where TPP assumptions are systematically re-evaluated against emerging data.
The dynamic nature of TPPs also provides essential support for contingency planning in uncertain regulatory and clinical environments. By encouraging holistic thinking about long-term regulatory and commercial goals, living TPPs enable sophisticated scenario planning based on evolving standards of care and regulatory expectations [3]. This forward-looking capability allows development teams to facilitate strategic pivots without losing sight of core objectives, particularly important when considering that approval requirements might significantly change over the typical 5-7 year development timeline for new therapeutic entities.
Quantitative Frameworks for Evolving TPPs
Structured TPP Worksheets for Pharmaceutical Development
Table 1: TPP Worksheet for a New Pharmacotherapeutic [1]
| Drug Label Attributes | Product Properties | Minimum Acceptable Results | Ideal Results |
|---|---|---|---|
| Indications and Usage | Primary Indication | To be defined based on clinical need | To be defined based on clinical need |
| Indications and Usage; Clinical Studies | Target Population | To be defined based on clinical need | To be defined based on clinical need |
| Dosage and Administration | Treatment Duration | To be defined based on clinical need | To be defined based on clinical need |
| Dosage and Administration | Delivery Mode | To be defined based on clinical need | To be defined based on clinical need |
| Dosage and Administration | Dose Regimen | To be defined based on clinical need | To be defined based on clinical need |
| Dosage Forms and Strengths | Dose Form | To be defined based on clinical need | To be defined based on clinical need |
| Clinical Studies | Clinical Efficacy | To be defined based on clinical need | To be defined based on clinical need |
| Adverse Reactions | Risk/Side Effect | To be defined based on clinical need | To be defined based on clinical need |
| How Supplied, Storage and Handling | Product Stability and Storage | To be defined based on clinical need | To be defined based on clinical need |
| Clinical Pharmacology | Mechanism of Action, Pharmacokinetics, Pharmacodynamics | To be defined based on clinical need | To be defined based on clinical need |
| Drug Interactions | Drug Interactions | To be defined based on clinical need | To be defined based on clinical need |
| N/A | Affordability (Price) | To be defined based on clinical need | To be defined based on clinical need |
| N/A | Accessibility | To be defined based on clinical need | To be defined based on clinical need |
Comparative TPP Analysis for Established Therapeutic Areas
Table 2: Benchmark TPP for Opioid Withdrawal Treatment [1]
| Product Properties | FDA-approved Medication: Lucemyra (lofexidine) | Minimum Acceptable Results | Ideal Results |
|---|---|---|---|
| Primary Indication | Mitigation of opioid withdrawal symptoms to facilitate abrupt opioid discontinuation in adults | To be defined based on clinical need | To be defined based on clinical need |
| Target Population | Adults meeting criteria for opioid dependence, physically dependent on short-acting opioids | To be defined based on clinical need | To be defined based on clinical need |
| Treatment Duration | Up to 14 days | To be defined based on clinical need | To be defined based on clinical need |
| Delivery Mode | Oral | To be defined based on clinical need | To be defined based on clinical need |
| Dose Regimen | Three 0.18 mg tablets taken orally 4 times daily at 5- to 6-hour intervals | To be defined based on clinical need | To be defined based on clinical need |
| Dose Form | 0.18 mg tablet | To to be defined based on clinical need | To be defined based on clinical need |
| Clinical Efficacy | Mean SOWS-Gossop total score on Days 1-5: 7.0 (placebo, 8.9); 49% completed 5-day treatment (placebo, 33%) | To be defined based on clinical need | To be defined based on clinical need |
| Risk/Side Effect | Hypotension, bradycardia, fainting | To be defined based on clinical need | To be defined based on clinical need |
| Product Stability and Storage | Store at 25°C (77°F) | To be defined based on clinical need | To be defined based on clinical need |
| Mechanism of Action | Central alpha-2 adrenergic agonist; half-life ~12 hours; bioavailability 72% | To be defined based on clinical need | To be defined based on clinical need |
| Drug Interactions | May reduce efficacy of oral naltrexone; may prolong QT interval with methadone | To be defined based on clinical need | To be defined based on clinical need |
| Affordability (Price) | ~$900 for brand, ~$300 for generic (36 tablets) | To be defined based on clinical need | To be defined based on clinical need |
| Accessibility | Prescription | To be defined based on clinical need | To be defined based on clinical need |
Experimental Protocols for TPP-Informed Development
Preclinical Model Selection and Validation
The development of a dynamic TPP directly informs the design of critical preclinical experiments. For cell therapy products, preclinical studies must be customized to support the feasibility of the proposed administration route, address the candidate product's specific therapeutic properties, and fully characterize potential safety concerns [16]. A well-constructed TPP guides preclinical model selection by defining key elements of the product's intended clinical use, including patient criteria, method and timing of administration, dose, and the product's expected mechanism of action.
The experimental workflow for TPP-informed preclinical development begins with appropriate model system selection. Investigators must identify model systems that most accurately recapitulate critical elements of their product's intended clinical use as defined in the TPP [16]. For cell therapy products, this typically involves:
- Exploring publicly available preclinical and clinical data to potentially cross-reference existing studies and reduce de novo testing requirements
- Evaluating in vitro systems for specific efficacy or safety data, particularly when product efficacy requires interaction with human-specific ligands or cells
- Conducting pilot in vivo studies to tailor disease models to specific testing needs, including calibration of injury/disease severity and preliminary dose escalation
- Seeking regulatory feedback early in development to confirm suitability of chosen preclinical models and ensure alignment with regulatory expectations
This systematic approach ensures that subsequent proof-of-concept efficacy and pivotal safety studies generate clinically meaningful data that effectively derisks transition to human trials.
Analytical Framework for TPP Refinement
The dynamic nature of TPPs requires systematic data integration throughout development. As new preclinical and clinical data emerge, development teams must implement structured processes for TPP refinement:
Figure 1: TPP Iterative Refinement Process
The analytical framework for TPP refinement incorporates both quantitative and qualitative assessments across multiple dimensions. Efficacy endpoints must be statistically powered to detect treatment-associated changes relative to appropriate control groups, while safety endpoints must characterize both short- and long-term biodistribution and toxicology profiles [16]. Additionally, the TPP refinement process should incorporate comparative effectiveness assessments against standard of care treatments, as these comparisons directly influence market adoption potential and therefore the product's commercial viability.
Table 3: Key Research Reagent Solutions for TPP-Informed Development
| Research Reagent | Function in TPP Development |
|---|---|
| Preclinical Disease Models | Provide biologically relevant systems for evaluating candidate therapeutic efficacy and safety; selection guided by TPP-defined clinical context [16]. |
| Biomarker Assays | Enable quantitative assessment of target engagement, mechanism of action, and treatment response; provide critical data for TPP refinement. |
| Analytical Standard References | Support method validation and ensure data quality for pivotal preclinical studies that inform TPP criteria. |
| Cell-Based Assay Systems | Facilitate in vitro assessment of product potency, particularly for biologics and cell therapies; generate data for TPP efficacy thresholds [16]. |
| Pharmacokinetic/Pharmacodynamic (PK/PD) Assays | Characterize drug exposure and response relationships; inform TPP sections on dosing regimen and therapeutic window. |
Emerging Technologies in TPP Development
Artificial Intelligence in TPP Lifecycle Management
The application of artificial intelligence is transforming TPP development and management. Current AI tools can extract insights from vast quantities of scientific and regulatory literature, generate first-draft TPP templates based on structured prompts, and assist in horizon scanning to identify changes in regulatory or therapeutic landscapes [3]. These capabilities are particularly valuable for maintaining the dynamic nature of TPPs, as AI systems can continuously monitor the external environment for developments that might necessitate TPP revisions.
The future of AI in TPP management points toward agentic AI systems capable of autonomously updating TPPs or flagging strategic shifts based on emerging data [3]. While current AI tools face limitations—including reliance on publicly available data that skews toward successful trials and limited access to proprietary commercial data—their potential to reduce the strategic planning burden on development teams is substantial. As these technologies mature, AI-enabled TPP management systems will likely become standard tools for maintaining the living document nature of target product profiles in an increasingly complex and fast-moving development environment.
Regulatory Integration and Strategy
A critical aspect of maintaining a dynamic TPP is effective regulatory integration. Regulatory strategy represents an essential component of TPP planning, particularly during periods of administrative change or regulatory uncertainty [3]. Development teams should leverage existing FDA resources and guidance documents, engage early and strategically with regulators (especially for complex or orphan indications), and focus on working within established guidance rather than attempting to circumvent it.
The living nature of TPPs facilitates more effective regulatory interactions by providing a structured framework for discussing development progress and strategic adaptations. By becoming well-versed in regulatory expectations and precedents, development teams can reduce internal decision-making delays and approach regulatory agencies with well-informed proposals that reflect both current development realities and evolving regulatory requirements [3]. This proactive regulatory approach ensures that the TPP remains not only an internal planning tool but also an effective communication vehicle for external stakeholders.
The dynamic nature of Target Product Profiles represents a fundamental evolution in pharmaceutical development strategy. By embracing the concept of the TPP as a living document, development teams can navigate the inherent uncertainties of drug development with greater agility and strategic clarity. The continuous refinement process—informed by emerging data, regulatory feedback, and market changes—ensures that TPPs remain relevant and valuable throughout the development lifecycle. As artificial intelligence tools advance and regulatory environments evolve, the living TPP will increasingly serve as the central nervous system of development programs, integrating cross-functional perspectives and enabling data-driven decision-making from discovery through commercialization.
The Critical Role of TPPs in Guiding Drug Development from Discovery to Market
A Target Product Profile (TPP) is a strategic planning tool that outlines the desired characteristics of a pharmaceutical product aimed at a particular disease or diseases. It summarizes the intended use, target populations, and desired attributes of a product, including safety and efficacy-related characteristics [2]. In the pharmaceutical industry, TPPs serve as internal planning tools that guide development toward achieving a product profile that meets the needs of patients, healthcare providers, and regulators while ensuring commercial viability [17] [14].
The concept of TPPs was first introduced in 1997 through discussions between the FDA and a Clinical Development working group to improve sponsor and FDA interactions [17]. Since then, TPPs have evolved to become central strategic documents that align research and development (R&D) activities with commercial objectives throughout the drug development lifecycle. By answering the question "what does success look like?", the TPP serves as a core strategic tool that aids prospective planning and integration of patient input at key milestones [17].
Modern pharmaceutical companies treat their TPP as a living document that evolves with new data and changing market conditions [18]. This dynamic approach ensures development remains aligned with both regulatory requirements and market needs from early discovery through commercial launch and beyond.
Core Components of a Target Product Profile
Fundamental Elements and Structure
A comprehensive TPP contains specific, target-oriented information across multiple domains of product characteristics. These components collectively define what constitutes a successful product in both clinical and commercial contexts.
Table 1: Core Components of an Effective Target Product Profile
| TPP Component | Primary Function | Development Impact |
|---|---|---|
| Target Indication | Defines specific patient population | Affects trial design and endpoint selection |
| Safety Profile | Sets acceptable risk tolerance | Influences regulatory pathway and monitoring requirements |
| Efficacy Claims | Specifies clinical benefits | Determines commercial positioning and differentiation |
| Dosage & Administration | Defines route, frequency, and formulation | Affects patient compliance and manufacturability |
| Quality Attributes | Sets purity, stability, and packaging standards | Guides manufacturing process and control strategy |
Successful TPPs address three fundamental areas that determine development success: the clinical value proposition, regulatory strategy, and commercial positioning [18]. Clinical specifications form the technical foundation, including dosing regimens, administration routes, patient populations, and safety requirements that guide trial design and regulatory submissions [18]. The commercial framework addresses pricing strategy, market access requirements, and competitive positioning based on the product's profile relative to existing treatments [14] [18].
WHO TPP Specifications and Public Health Alignment
In the context of public health, WHO TPPs serve to set R&D targets for funders and developers, with a focus on access, equity, and affordability as integral parts of the innovation process [2]. WHO TPP documents describe both the preferred and the minimally acceptable profiles for vaccines, therapeutics, diagnostics, or medical devices [2]. These profiles provide information for funders and developers on the performance and operational characteristics expected of products if they are to meet WHO's public health needs, ensuring that not-for-profit product development programs align with identified global health priorities [2].
TPPs Throughout the Drug Development Lifecycle
Stage-Specific Application and Evolution
TPPs serve different functions at various stages of the drug development process, with their focus areas evolving as products advance through the development pipeline.
Table 2: TPP Focus Areas Across Development Phases
| Development Phase | TPP Focus Areas | Key Decisions Informed |
|---|---|---|
| Preclinical | Target validation, preliminary safety profile | Lead compound selection, initial indication |
| Phase I/II | Dose range, early efficacy signals | Trial design optimization, go/no-go decisions |
| Phase III | Label claims, commercial positioning | Regulatory submission strategy, launch planning |
| Pre-launch | Market access, competitive differentiation | Pricing, reimbursement, commercial strategy |
The TPP is updated at several key decision points or "tollgates" in a medicine's lifecycle, and as necessary depending on what new clinical or pharmaceutical data become available [17]. This iterative approach ensures the TPP remains aligned with emerging evidence and changing market conditions throughout the development process.
TPP Testing and Validation Methodologies
Quantitative TPP testing with relevant audiences provides valuable insights on understandability, credibility, and prescription potential, guiding strategic decisions related to the product portfolio [14]. The methodology involves formatting TPP information into a short, optimized summary detailing key drug characteristics, typically presented as a one-page document with grouped clinical elements to facilitate respondent understanding and absorption of information [14].
TPP testing can be applied at multiple stages within the drug life cycle, with three common use cases:
- Market opportunity confirmation for business development and licensing (BD&L): Corporate strategy teams evaluate market potential of external assets to determine optimal opportunities for drug acquisition or licensing [14].
- New drug development or early drug testing: Teams responsible for internal innovation test different scenarios for drugs in the early pipeline (e.g., preclinical and phase 1) to inform prioritization strategy [14].
- Launch and commercial strategy preparation: Marketing and commercial teams fine-tune launch strategies for late-stage drugs (phase 2, phase 3, preapproval) by confirming and refining prescription/usage assumptions [14].
Regulatory Strategy and TPP Integration
Regulatory Pathway Selection
The TPP drives regulatory pathway selection and agency interaction strategy. Regulatory bodies like the FDA view TPPs as strategic development tools that help focus discussions and facilitate more productive regulatory meetings [18]. Early FDA engagement using the TPP can identify potential regulatory issues before they impact critical path activities, with pre-IND meetings and scientific advice sessions providing valuable feedback on TPP assumptions and development plans [18].
Table 3: Regulatory Pathways and TPP Requirements
| Regulatory Pathway | TPP Requirements | Timeline Benefits |
|---|---|---|
| Traditional NDA | Complete documentation for all claims | Standard 10-12 month review |
| 505(b)(2) Application | Bridging study rationale to reference product | 3-7 years vs 8-12 years for full development |
| Fast Track Designation | Demonstration of unmet medical need | Potential 6-18 month acceleration |
Companies developing 505(b)(2) drugs often reference competitor TPPs to identify differentiation opportunities and regulatory advantages, using this competitive intelligence to optimize pathway selection and development timelines [18].
Probability of Success Calculations
Probability of Success (PoS) represents a quantitative approach to support development decisions by quantifying the uncertainty of achieving desired TPP targets at key decision points [19]. In drug development, PoS can be defined as achieving the full TPP profile or can be more limited (i.e., achieving one or more specific elements of the profile) [19]. PoS is particularly valuable for decisions such as starting clinical development or moving from Phase II to Phase III, where it focuses on the probability of demonstrating efficacy in confirmatory trials [19].
Quantitative PoS approaches address the limitation of traditional power calculations that assume a fixed effect size, instead incorporating a range of possible effect sizes through a "design prior" that captures uncertainty in a probability distribution [19]. These methods can incorporate external data sources, including real-world data and historical clinical trial data, to optimize calculations of trial success probability and projected drug candidate value [19].
Patient Engagement in TPP Development
Systematic Integration of Patient Perspectives
As the experts on their own disease, patients bring invaluable perspectives to drug development which cannot be obtained by other means [17]. A systematic guidance framework for patient-focused TPP development identifies five focus areas where patient perspectives are fundamental [17]:
- Target population - Patient insights help refine inclusion/exclusion criteria
- Unmet medical need - Patient-lived experience defines disease burden
- Dosage frequency and route of administration - Practical treatment considerations
- Efficacy endpoints - Relevance of outcomes that matter most to patients
- Acceptability of benefit/risk profile trade-offs - Informed by patient preference studies
A guiding principle is to incorporate patient perspectives in a systematic process starting as early as possible in development [17]. This approach ensures the TPP reflects patient needs from the outset rather than attempting to incorporate them later in development.
Methodologies for Gathering Patient Input
Multiple tools are available for obtaining patient perspectives to inform TPP development, each with distinct strengths and applications:
- Desk research - Accessing existing knowledge through literature searches, FDA voice-of-the-patient reports, and databases of core outcome sets [17]
- Patient Advisory Boards/Councils - Continuous and regular exchange on topics of common interest [17]
- Focus groups with patients/caregivers - Qualitative group discussions moderated by independent facilitators [17]
- In-depth interviews - Intensive individual interviews to explore perspectives on specific concepts [17]
When engaging patient representatives, specific recommendations include using clear language, showing respect for patients' expertise, engaging with patient experts (patients with knowledge of their disease), and providing adequate context and background information [17]. These practices ensure productive collaboration between R&D organizations and patient communities.
Experimental Protocols and Research Methodology
TPP Testing Research Protocol
A standardized methodology for TPP testing involves specific experimental protocols to ensure valid, reliable results:
Protocol 1: Quantitative TPP Testing with Healthcare Professionals
- TPP Formatting: Format TPP information into a one-page document with grouped clinical elements to facilitate understanding [14]
- Participant Identification: Identify relevant healthcare professional populations based on treatment characteristics, considering multiple specialties for complex treatments [14]
- Survey Administration: Present TPP summary using streamlined, semi-standardized questions to gather clear, unbiased feedback [14]
- Data Collection: Assess understandability, credibility, and prescription potential through structured questionnaires [14]
- Analysis: Evaluate clinical and market potential across different scenarios (e.g., worst-case vs. base-case vs. best-case) [14]
This protocol supports various applications including market opportunity confirmation, new drug development prioritization, and launch strategy preparation [14].
Patient Engagement Research Protocol
Protocol 2: Systematic Integration of Patient Perspectives into TPP
Desk Research Phase:
Gap Analysis: Identify missing patient perspective information not available through desk research [17]
Direct Engagement:
Integration: Incorporate patient insights into the five key focus areas of the TPP [17]
This protocol emphasizes early and continuous engagement, beginning when a compound is in the preclinical phase [17].
Visualization of TPP in Drug Development
TPP Development and Integration Workflow
TPP Development Workflow: This diagram illustrates how the TPP evolves throughout the drug development process, incorporating new data and stakeholder input at key milestones.
Patient Engagement Framework in TPP Development
Patient Engagement Framework: This diagram shows the key areas where patient input directly shapes the TPP, divided into disease experience and product perspective factors.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Research Reagent Solutions for TPP-Informed Development
| Research Tool | Function in TPP Development | Application Context |
|---|---|---|
| Historical Clinical Trial Data | Provides comparator data for efficacy and safety targets | PoS calculations, endpoint selection [19] |
| Real-World Data (RWD) | Informs natural history, unmet needs, and target population | External control arms, disease burden assessment [19] |
| Patient Preference Studies | Quantifies benefit-risk trade-offs and treatment priorities | Defining acceptable safety profile, administration routes [17] |
| Clinical Outcome Assessments (COAs) | Measures outcomes meaningful to patients | Efficacy endpoint selection and validation [17] |
| Biomarker Assays | Provides early signals of efficacy and safety | Go/no-go decisions in early development [19] |
These tools enable the quantitative foundation necessary for evidence-based TPP development, supporting critical decisions throughout the drug development lifecycle. Historical clinical trial data and real-world evidence are particularly valuable for constructing design priors in Probability of Success calculations, especially when clinical endpoint data are not yet available from Phase II trials [19].
Target Product Profiles serve as strategic compasses guiding drug development from discovery through commercialization. By aligning R&D activities with patient needs, regulatory requirements, and commercial realities, TPPs increase development efficiency and enhance the likelihood of delivering meaningful treatments to patients. The integration of patient perspectives, quantitative decision tools like Probability of Success, and systematic testing methodologies strengthens TPPs as living documents that evolve with emerging evidence. As pharmaceutical development grows increasingly complex and competitive, robust TPP practices will continue to play a critical role in navigating the challenging pathway from concept to clinic, ultimately ensuring that new medicines address unmet medical needs while achieving sustainable commercial success.
Building and Implementing Your TPP: A Cross-Functional Guide
A Target Product Profile (TPP) serves as a strategic framework in therapeutic development, summarizing the key features of an intended commercial product [8]. From an industry perspective, a well-designed TPP provides a clearly articulated set of goals that help focus and guide development activities to reach the desired commercial outcome [8]. This document functions as a living planning tool, aligning research and development (R&D) teams, funders, and regulators around a common vision. In public health, organizations like the World Health Organization (WHO) use TPPs to set R&D targets for missing health products, emphasizing that access, equity, and affordability are integral parts of the innovation process [2].
Structuring a TPP around "minimally acceptable" and "ideal" targets creates a development pathway with clear decision gates. Failure to meet the parameters defined as "essential" will often mean termination of product development, while exceeding these parameters or meeting the "ideal" profile will likely increase the product's value [8]. This structured approach ensures that resources are allocated efficiently and that the final product addresses a defined unmet medical need.
Core Components of a TPP
A high-value TPP is constructed through careful consideration of several essential components. These elements collectively define the product's intended use, target population, and key differentiating characteristics. The following diagram illustrates the logical workflow for developing a TPP, from defining the strategic objective to finalizing the structured profile.
Defining the Target Population and Unmet Need
Precisely defining the target population is the foundational step in TPP construction. This involves identifying the specific cohort of patients for which there is an inadequate treatment, thereby establishing the unmet medical need [8]. A clearly defined patient population ensures clinical development is focused and viable.
Key considerations for this section include:
- Segmentation: Are there specific subsets of patients or diagnoses for which the program is targeted? [8]
- Epidemiology: What is the incidence and/or prevalence of the specific condition? [8]
- Quantification of Unmet Need: How is the unmet need measured? What proportion of patients are inadequately treated by this measure, and over what period? [8]
Establishing Efficacy and Safety Differentiation
The TPP must clearly define how the candidate product is differentiated from current treatment options or the standard of care. This differentiation is typically demonstrated through clear measures of efficacy and safety [8].
Efficacy Endpoints
- Validated Endpoints: Efficacy endpoints used in Phase III clinical trials should be defined and validated. Regulatory bodies like the FDA produce guidelines outlining expectations for specific indications [8].
- Objectively Defined Measures: Endpoints should be objectively defined with clear measures of success (e.g., delta with comparator and a definition of what constitutes a clinically meaningful improvement) [8].
- Endpoint Hierarchy: Consideration should be given to primary versus secondary endpoints, including the time an endpoint is measured, length of follow-up, and relapse rates [8].
Safety Endpoints
- Required Safety Profile: The TPP should define the required safety profile for the target product, demonstrating at least equivalence or differentiation from the safety profile of current treatments [8].
- Specific Adverse Effects: Specific adverse effects of current treatments should be defined (e.g., by incidence and severity), and the level of improvement or equivalence sought must be stated [8].
Administration, Dosage, and Commercial Considerations
How the target product will be administered and its positioning in the treatment landscape must be clearly defined [8]. This directly impacts patient compliance and commercial viability.
Critical factors to specify include:
- Purpose: Will the target product be used for treatment or prevention? [8]
- Therapy Type: Will it be a monotherapy or used in combination with other current treatments? [8]
- Route of Administration: What is the proposed route of administration (e.g., oral, intravenous)? [8]
- Dosage Regimen: What is the proposed dosage schedule, and will any titration be needed to reach an effective dose? [8]
Structuring Minimum vs. Ideal Targets
The core of a strategic TPP is the delineation between "minimally acceptable" and "ideal" targets. This dual-track approach provides a clear framework for decision-making throughout the development process. The minimally acceptable criteria represent the absolute requirements for product viability, while the ideal profile outlines attributes that would maximize the product's clinical impact and commercial value [8] [2]. The relationship and decision-making process between these target levels is shown in the following diagram.
Comparative Tables for TPP Components
The following tables provide a structured format for summarizing quantitative and qualitative targets across key TPP categories.
Table 1: Efficacy and Safety Targets
| Attribute | Minimum Acceptable Target | Ideal Target |
|---|---|---|
| Primary Efficacy Endpoint | Statistically significant improvement vs. placebo; non-inferior to standard of care. [8] | Superior to standard of care with a clinically meaningful delta; improvement on clinically relevant secondary endpoints. [8] |
| Effect Size | Meets pre-defined clinically meaningful threshold. | Exceeds pre-defined threshold with high statistical significance. |
| Safety Profile | Equivalent to standard of care; acceptable risk-benefit ratio. [8] | Superior to standard of care with significant reduction in specific adverse effects. [8] |
| Serious Adverse Events | Incidence within pre-defined acceptable range. | Incidence lower than standard of care. |
Table 2: Clinical Development and Commercial Targets
| Attribute | Minimum Acceptable Target | Ideal Target |
|---|---|---|
| Target Population | A defined patient segment with significant unmet need. [8] | Broad patient population with potential for label expansion. |
| Dosage Regimen | Once-daily dosing; minimal titration. [8] | Less frequent than daily dosing (e.g., weekly); no titration required. |
| Route of Administration | Acceptable route for inpatient/acute care. | Preferred route for outpatient/chronic care (e.g., oral over intravenous). [8] |
| Stability & Shelf Life | Meets regulatory requirements for distribution. | Room-temperature stability; long shelf life reducing supply chain costs. |
| Competitive Profile | Meets one key unmet need in a competitive landscape. | Differentiated on multiple axes (efficacy, safety, convenience). [8] |
Experimental Protocols for TPP Validation
The hypotheses and targets outlined in the TPP must be validated through rigorous experimentation. The following section details key methodological approaches.
In Vitro Efficacy and Mechanism of Action Studies
Objective: To demonstrate proof-of-concept and elucidate the biological mechanism of action of the therapeutic candidate against the intended target.
Detailed Protocol:
- Cell-Based Assays:
- Cell Line Selection: Use clinically relevant cell lines (primary cells or engineered cell lines expressing the target) and appropriate control cells.
- Dose-Response Curves: Treat cells with a range of compound concentrations (typically from nM to μM) to establish a dose-response relationship. Incubation times should reflect the proposed mechanism.
- Endpoint Measurement: Quantify activity using validated endpoints (e.g., ELISA for protein secretion, flow cytometry for surface markers, luciferase reporter assays for pathway activity). The half-maximal effective concentration (EC50) should be calculated.
- Positive/Negative Controls: Include a known inhibitor/agonist as a positive control and a vehicle as a negative control in all experiments.
- Target Engagement & Binding Assays:
- Surface Plasmon Resonance (SPR) or Bio-Layer Interferometry (BLI): Determine binding affinity (KD), association rate (kon), and dissociation rate (koff) of the candidate therapeutic to the purified target protein.
- Competitive Binding Assays: Use a labeled reference compound to assess whether the candidate binds to the same site as natural ligands or competitors.
In Vivo Efficacy and Tolerability Studies
Objective: To evaluate the efficacy and preliminary safety of the candidate in a physiologically relevant animal model.
Detailed Protocol:
- Animal Model Selection:
- Select a model that recapitulates key aspects of the human disease (e.g., genetically engineered models, xenograft models for oncology, or induced-disease models).
- Justify the species, strain, sex, and age of animals used.
- Study Design:
- Randomization: Animals are randomly assigned to treatment groups (e.g., vehicle control, positive control, multiple dose levels of candidate) to minimize bias.
- Dosing Regimen: The route of administration, formulation, and dosing frequency should mirror the proposed clinical plan as closely as possible. The study duration must be sufficient to see a meaningful effect.
- Efficacy Endpoints: Measure predefined, clinically translatable endpoints (e.g., tumor volume, biomarker levels, functional scores) at baseline and regularly throughout the study.
- Tolerability Monitoring: Record body weight, food consumption, and clinical signs daily. Conduct gross necropsy at endpoint and collect key organs for potential histopathological analysis.
Research Reagent Solutions and Essential Materials
Table 3: Key Research Reagents and Materials
| Item | Function in TPP Validation |
|---|---|
| Validated Cell Lines | Provide a biologically relevant system for initial in vitro proof-of-concept and mechanism of action studies. |
| Animal Disease Models | Enable the assessment of efficacy and pharmacokinetic/pharmacodynamic (PK/PD) relationships in a complex, living system. |
| Reference Standards | (e.g., competitor therapeutics) Serve as benchmarks for comparing the efficacy and potency of the candidate product. |
| Specific Antibodies & Assay Kits | Allow for the quantitative measurement of target engagement, pathway modulation, and biomarker levels in vitro and ex vivo. |
| Formulation Vehicles | Ensure the candidate therapeutic is stable, soluble, and bioavailable for administration in in vivo studies. |
Integrating the TPP into the Development Workflow
Once completed, a TPP helps articulate the value proposition of a potential product (e.g., how many lives will it save, how many complications will it avoid?) [8]. It is not a static document but should be revisited and refined at key milestones, such as before initiating IND-enabling studies or Phase III trials. Consideration of the competitive landscape (e.g., cost to treat) and where the product fits will help define the potential market share and market value [8].
In the regulatory context, TPPs are considered as tools to frame development in relation to submission of product dossiers [2]. A well-structured TPP, with its clear minimal and ideal targets, facilitates more transparent and efficient communication with regulatory agencies throughout the development process, ultimately helping to bring valuable new therapies to patients in need.
In the modern pharmaceutical landscape, a Target Product Profile (TPP) serves as a strategic development tool, outlining the desired characteristics of a product aimed at a particular disease or condition [20]. The development of a comprehensive TPP requires a multifaceted approach that transcends traditional functional silos. Cross-functional collaboration is not merely beneficial but essential for creating TPPs that are both scientifically rigorous and commercially viable. This collaboration brings together diverse expertise from across the organization to align on product vision, development strategy, and regulatory pathways, ultimately enhancing research efficiency and improving the likelihood of regulatory and commercial success [21] [20].
The complexity of modern pharmaceutical organizations, which have largely shifted from traditional hierarchical models to matrix structures, makes this collaboration both powerful and challenging [21]. When operating effectively, cross-functional teams drive innovation and accelerate decision-making. However, the same diversity that provides strength can also lead to communication breakdowns, conflicting priorities, and misaligned objectives if not managed deliberately [21]. In the context of TPP research, where the goal is to define a clear target for product development, this alignment becomes a strategic imperative that can determine a company's ability to bring new therapies to market and ultimately improve patient outcomes [21].
Core Principles of Effective Cross-Functional Collaboration
Establishing a Unified Vision and Shared Language
At the heart of successful cross-functional alignment is a clear, compelling vision that transcends individual departments or therapeutic areas [21]. This vision must articulate not just what the TPP aims to achieve, but why it matters in the broader context of the company's mission and the patients it serves. Leaders must craft a narrative that resonates across diverse teams, from research scientists to market access specialists, connecting the dots between the TPP initiative and the company's long-term goals [21].
One significant challenge in matrix organizations is the varying terminologies and metrics used across different functions [21]. R&D teams might focus on scientific milestones, while commercial teams prioritize market share and revenue forecasts. To align these diverse groups, it is crucial to establish a shared language around the TPP initiative, including common Key Performance Indicators (KPIs) that reflect the interdependent nature of the work [21]. For instance, a cross-functional metric might measure the time from target identification to first patient dosing, encompassing both R&D and clinical operations. By adopting shared metrics, teams are encouraged to think holistically about their contributions to the overall TPP development process.
Strategic Team Composition and Role Definition
Assembling the right team requires careful consideration of the necessary expertise, decision-making authority, and stakeholder representation. The complex reporting structures inherent in matrix organizations can create confusion about roles, responsibilities, and decision-making authority, particularly during periods of significant organizational change [21]. Clarifying these aspects from the outset is critical for TPP development, which requires input across the drug development lifecycle.
Table: Essential Cross-Functional Roles in TPP Development
| Functional Representative | Primary Contribution | Critical Input for TPP |
|---|---|---|
| Research & Discovery | Target validation, mechanism of action | Scientific feasibility, biomarker strategy |
| Clinical Development | Trial design, endpoint selection | Clinical efficacy/safety targets, dosing rationale |
| Regulatory Affairs | Regulatory requirements, submission strategy | Agency feedback, competitive labeling analysis |
| Medical Affairs | Clinical differentiation, KOL insights | Evidence generation plan, communication strategy |
| Commercial/Marketing | Market assessment, competitive intelligence | Target product profile, positioning, pricing considerations |
| Market Access | Reimbursement requirements, health technology assessment | Value proposition, health economic outcomes |
| Manufacturing | Production feasibility, scaling considerations | Formulation, delivery device, shelf-life targets |
Methodological Framework for Collaborative TPP Development
TPP Development Process and Workflow
The development of a Target Product Profile requires a systematic approach that incorporates diverse perspectives while maintaining strategic alignment. Based on analysis of TPP development methodologies, a structured process typically includes three key stages: scoping, drafting, and consensus-building [20]. The workflow below visualizes this collaborative process, highlighting key decision points and iterative refinement loops:
Experimental Protocols for Validating Collaboration Effectiveness
To ensure that cross-functional collaboration delivers measurable benefits to TPP development, teams should implement structured assessment protocols. The following methodologies provide quantitative and qualitative measures of collaboration effectiveness:
Protocol 1: Cross-Functional Alignment Assessment
- Objective: Measure the degree of alignment across functions on key TPP elements
- Methodology: Conduct anonymous surveys using Likert scales (1-5) to assess agreement on TPP characteristics including target product profile, clinical endpoints, regulatory strategy, and commercial viability
- Frequency: Administer at project initiation, after draft completion, and post-finalization
- Success Metrics: >80% agreement on essential TPP characteristics; <15% variance in importance ratings across functions
- Analysis: Calculate alignment scores for each TPP characteristic and identify areas requiring facilitated discussion
Protocol 2: Decision Velocity Tracking
- Objective: Quantify the impact of cross-functional collaboration on development efficiency
- Methodology: Document time from TPP draft circulation to final approval, tracking revisions and iterations
- Frequency: Monitor continuously throughout TPP development process
- Success Metrics: Reduction in decision cycles compared to historical benchmarks; <3 revision cycles for 90% of TPP elements
- Analysis: Compare current TPP development timelines with historical averages and identify process bottlenecks
Implementation Tools and Enabling Technologies
Research Reagent Solutions for Collaborative TPP Development
Effective cross-functional collaboration requires both conceptual frameworks and practical tools. The following table details essential resources that facilitate the TPP development process:
Table: Essential Tools for Collaborative TPP Development
| Tool Category | Specific Solution | Function in TPP Development |
|---|---|---|
| Collaboration Platforms | Shared document repositories, Version control systems | Enable real-time co-authoring, maintain single source of truth for TPP documents, track revision history |
| Decision Support Tools | Weighted decision matrix, Criteria rating scales | Facilitate objective evaluation of trade-offs between TPP characteristics, prioritize requirements based on multiple factors |
| Communication Interfaces | Cross-functional meeting templates, Structured feedback forms | Standardize communication protocols, ensure comprehensive input collection, document action items |
| Data Integration Systems | Unified data warehouses, API connections | Aggregate diverse data sources (clinical, commercial, regulatory), support evidence-based TPP decisions |
| Project Management Software | Gantt charts, Responsibility assignment matrices | Visualize TPP development timelines, clarify role-specific deliverables, track progress against milestones |
| AI-Powered Analytics | Predictive modeling tools, Natural language processing | Analyze competitive landscape, forecast development risks, extract insights from regulatory documents |
Cross-Functional Meeting Management Protocol
Regular, structured interactions are essential for maintaining alignment throughout TPP development. The following diagram outlines an effective meeting management workflow that ensures productive cross-functional engagement:
Quantitative Assessment of TPP Characteristics
Systematic analysis of existing TPPs reveals patterns in development focus areas and potential gaps. The following data, synthesized from a review of digital health technology TPPs, demonstrates the distribution of characteristics across key consideration clusters:
Table: Distribution of Characteristics in Digital Health TPPs (Based on Systematic Review of 14 TPPs) [20]
| Characteristic Cluster | Frequency of Reporting | Key Example Characteristics |
|---|---|---|
| Clinical Utility | 92% | Clinical performance targets, Intended use population, Clinical workflow integration |
| Clinical Validity | 86% | Analytical performance, Sensitivity/specificity targets, Positive/negative predictive values |
| Infrastructural Requirements | 78% | Hardware/software dependencies, Connectivity requirements, Interoperability standards |
| Regulatory Requirements | 64% | Regulatory classification, Quality management systems, Certification needs |
| Human Factors | 57% | Usability requirements, Training needs, User interface specifications |
| Unmet Clinical Need | 50% | Problem statement, Current standard of care limitations, Target outcome improvement |
| Cost Considerations | 43% | Target price point, Reimbursement strategy, Total cost of ownership |
| Environmental Impact | 14% | Sustainability requirements, Power consumption, Device disposal considerations |
This distribution highlights significant gaps in how consistently key considerations are addressed in TPP development, particularly regarding cost considerations and environmental impact, which were reported in less than half of the analyzed TPPs [20]. This inconsistency presents an opportunity for cross-functional teams to establish more comprehensive TPP development practices.
Assembling the right team for cross-functional collaboration in TPP research requires intentional leadership that combines clear vision-setting, shared metrics, empowered champions, enabling technology, and aligned incentives [21]. In the context of TPP development, successful cross-functional collaboration manifests as a comprehensive product profile that balances scientific innovation with practical commercial and regulatory considerations, ultimately serving as an effective demand signal to guide development [20].
The complexity of pharmaceutical matrix organizations necessitates a disciplined approach to collaboration, particularly for TPP development which sits at the intersection of multiple functional domains [21]. By implementing the structured methodologies, assessment protocols, and enabling tools outlined in this guide, organizations can create more agile, responsive teams capable of developing TPPs that not only meet regulatory requirements but also address genuine unmet patient needs efficiently and effectively.
Within the strategic framework of a Target Product Profile (TPP), the precise definition of critical parameters is not merely an administrative exercise but a foundational activity that guides successful drug development. A TPP serves as a strategic planning tool that outlines the desired characteristics of a medical product, ensuring that research and development efforts align with specific clinical needs and regulatory requirements [1]. This strategic document articulates the ideal attributes of a drug candidate, acting as a "north star" for cross-functional teams across clinical, regulatory, and commercial functions [22]. At the heart of a robust TPP are three interdependent pillars: patient population, dosing regimen, and efficacy thresholds. These parameters form the core of the value proposition for any new therapeutic, directly influencing trial design, regulatory strategy, and ultimately, market access and adoption. In today's evolving landscape, where regulatory approval alone is insufficient for commercial success, meticulously defining these parameters early in development is a strategic imperative for securing favorable reimbursement and ensuring timely patient access [22].
Defining the Target Patient Population
The target patient population is a critical parameter that specifies the precise group of individuals for whom a therapy is intended. This definition directly influences clinical trial design, regulatory pathway, labeling, and commercial strategy. A well-defined patient population should be based on clear demographic, clinical, and pathophysiological characteristics to ensure the therapy addresses a coherent medical need.
Key Considerations for Population Definition
When defining the target population, developers must balance scientific rationale with strategic commercial considerations. Key aspects include:
- Disease Severity and Stage: Specifying whether the therapy targets early-stage, late-stage, or acute manifestations of a disease.
- Previous Treatment History: Defining whether the population is treatment-naïve, has failed existing therapies, or is intolerant to standard of care.
- Biomarker Status: Identifying specific genetic, proteomic, or other biomarkers that predict treatment response.
- Age and Special Populations: Explicitly including or excluding pediatric, geriatric, pregnant, or other special populations based on pharmacological rationale.
Comparative Analysis: Patient Population in Practice
Table 1: Patient Population Specifications in Example TPPs
| Therapeutic Area | Target Population | Key Inclusion Criteria | Strategic Rationale |
|---|---|---|---|
| Opioid Use Disorder [1] | Adults meeting criteria for opioid dependence, physically dependent on short-acting opioids | Specific diagnosis, type of opioid dependency | Focuses on a well-defined, high-need population for a clear regulatory pathway |
| Anthrax Vaccine [5] | All adults and pediatrics >12 months for post-exposure prophylaxis | Age-based, exposure context | Aims for broad public health protection in an emergency scenario |
| Novel Inhaled COPD Therapy [22] | Patients with confirmed COPD, history of exacerbations | Disease severity, historical clinical events | Targets patients with significant unmet need and measurable outcomes |
Establishing the Dosing Regimen
The dosing regimen is a multi-faceted parameter encompassing the route of administration, dose strength, frequency, and treatment duration. This parameter profoundly impacts patient adherence, quality of life, manufacturability, and commercial viability. A well-designed dosing regimen balances pharmacological efficacy with practical usability.
Components of a Dosing Regimen
- Route of Administration: Choosing between oral, intravenous, subcutaneous, inhaled, or other routes based on drug properties, disease location, and patient convenience. Needle-free approaches are often preferred for vaccines [5].
- Dose Frequency: Determining whether the drug is administered daily, weekly, or less frequently, impacting the "burden of therapy."
- Treatment Duration: Defining a finite treatment period (e.g., 7-14 days for opioid withdrawal [1]) or chronic therapy based on the nature of the disease.
- Dose Formulation: Specifying tablets, capsules, liquids, or injectables, which affects stability, storage, and usability.
Experimental Protocols for Dosing Determination
Determining the optimal dosing regimen requires a structured, sequential experimental approach.
Phase 1: Dose Escalation & PK/PD Studies
- Objective: To assess safety, tolerability, and pharmacokinetics (PK) and determine a range of potentially active doses.
- Methodology: Single and multiple ascending dose (SAD/MAD) studies in healthy volunteers or patients.
- Key Endpoints: Maximum tolerated dose (MTD), dose-limiting toxicities (DLTs), C~max~, T~max~, AUC, half-life (t~1/2~), and preliminary pharmacodynamic (PD) effects.
- Analysis: Population PK modeling to understand inter-individual variability and covariates affecting drug exposure.
Phase 2: Dose-Ranging & Regimen Optimization
- Objective: To characterize the dose-response relationship for efficacy and safety and select the optimal dose(s) for Phase 3.
- Methodology: Randomized, controlled, parallel-group studies comparing multiple doses and/or frequencies against a control.
- Key Endpoints: Primary efficacy endpoint, safety profile, and exposure-response (ER) relationships across doses.
- Analysis: ER modeling to quantify the relationship between drug exposure (e.g., AUC) and clinical endpoints, informing the final dose selection.
Diagram 1: Experimental Workflow for Dosing Regimen Determination
Setting Efficacy Thresholds
Efficacy thresholds are pre-defined, quantitative targets that a drug must achieve to be considered successful. These thresholds are grounded in clinical meaningfulness and must be justified based on the standard of care, unmet need, and regulatory precedents. They are the definitive benchmarks against which the success of a development program is measured.
Defining Minimum, Base, and Aspirational Goals
A robust TPP defines a range of efficacy targets [3]:
- Minimum Acceptable Profile: The lowest level of efficacy required for regulatory approval and a viable commercial profile. This is the "go/no-go" threshold.
- Base Case Profile: The expected level of performance, typically informed by competitive benchmarks and realistic projections from earlier phase data.
- Aspirational Profile: The ideal outcome that would represent a significant clinical advance and ensure strong market uptake and premium pricing.
Quantitative Thresholds Across Therapeutic Areas
Table 2: Efficacy Thresholds in Published TPPs and Guidelines
| Product / Indication | Efficacy Endpoint | Minimum Acceptable | Ideal / Aspirational | Evidence Source |
|---|---|---|---|---|
| Anthrax Vaccine (PEP) [5] | Efficacy (inferred by immunogenicity) | >70% (lower bound 95% CI >40%) | N/S | Neutralizing antibody titers |
| Opioid Withdrawal Device [1] | Reduction in COWS Score | Significant reduction from baseline | 61.3% mean reduction at 60 min | Clinical Opiate Withdrawal Scale |
| Filovirus Vaccine [5] | Efficacy in preventing disease | >80% (or immunogenicity threshold) | Long-lasting protection (≥3 years) | Clinical trial or Animal Rule |
| Novel COPD Therapy (Hypothetical) [22] | Symptom relief, Reduced exacerbations | Statistically significant vs. SoC | Superior to SoC with compelling health economic benefit | Phase III RCT |
Methodologies for Establishing Efficacy Thresholds
Justifying efficacy thresholds requires a robust evidence-based approach.
- Systematic Literature Review & Meta-Analysis: Conduct a comprehensive review of existing clinical trials for standard of care and competitor products to establish the current range of treatment effects and identify an opportunity for differentiation.
- Benchmarking Against Regulatory Precedents: Analyze the efficacy data that supported the approval of recent therapies in the same class or indication, often available in FDA Advisory Committee Briefing Documents.
- Health Technology Assessment (HTA) Guidance Review: Consult guidelines from bodies like NICE, ICER, and HAS, which often specify the evidence thresholds required for positive reimbursement recommendations.
- Quantitative Decision Analysis: Use statistical modeling and simulation to understand the probability of technical success (PTS) for different threshold scenarios, informing risk-balanced choices.
The Scientist's Toolkit: Essential Reagents and Materials
The experimental work defining TPP parameters relies on a suite of specialized reagents and tools.
Table 3: Key Research Reagent Solutions for TPP Parameter Definition
| Reagent / Material | Primary Function | Application in TPP Development |
|---|---|---|
| Validated Biomarker Assays | Quantitatively measure specific biological molecules (e.g., proteins, DNA). | Patient stratification, PK/PD modeling, and as surrogate efficacy endpoints. |
| Reference Standards & Controls | Provide a known benchmark for assay calibration and validation. | Ensuring consistency and reproducibility of analytical and bioanalytical results across studies. |
| Cell-Based Assay Systems | Model disease biology and drug mechanism of action in vitro. | Preliminary efficacy screening and understanding the biological context of efficacy. |
| Animal Models of Disease | Recapitulate aspects of human disease for in vivo testing. | Establishing proof-of-concept and initial dose-ranging for efficacy and safety (e.g., Animal Rule for vaccines [5]). |
| Clinical Outcome Assessments (COAs) | Standardized tools (e.g., questionnaires, diaries) to measure patient-reported outcomes. | Defining patient-centric efficacy endpoints that are meaningful to patients, providers, and payers [22]. |
Integrated Strategy and Lifecycle Management
The individual parameters of population, dosing, and efficacy are not developed in isolation. They form a tightly interconnected strategic framework where a change in one directly impacts the others. Furthermore, a TPP is a dynamic document that must evolve with emerging clinical data, competitive landscape shifts, and evolving payer expectations [22] [3].
Diagram 2: Interrelationship of Core TPP Parameters
Aligning TPP with Value Evidence Archetypes
To ensure market access success, the TPP's clinical parameters must be aligned with a Value Evidence Archetype early in development [22]. This strategic framework defines the kind of evidence needed to convince payers and Health Technology Assessment (HTA) bodies of the product's value. For instance:
- A therapy targeting a Clinical Benefit Archetype must have its efficacy thresholds set to demonstrate clear superiority over the standard of care.
- A product following an Economic Value Archetype must have its dosing and efficacy parameters defined in a way that supports a compelling cost-effectiveness or budget impact model.
- A drug addressing an Unmet Need Archetype might have more flexibility on the magnitude of efficacy but will require robust evidence on the severity of the unmet need and patient-reported outcomes.
Engaging commercial, HEOR (Health Economics and Outcomes Research), and market access leaders during the TPP development phase is essential to ensure this alignment is achieved [22].
A Target Product Profile (TPP) is a strategic planning tool that outlines the desired characteristics of a medical product, guiding its development from conception to market. It serves as a strategic framework that aligns commercial and clinical workstreams by defining the intended use, target population, and key performance features early in the development process [1]. By establishing a clear vision of the final product, a TPP ensures that research and development efforts align with specific clinical needs and regulatory requirements, fostering stakeholder alignment and facilitating efficient resource allocation [1]. This strategic document is dynamic, continuously evolving with emerging data and insights to support informed decision-making at every development stage [1].
The value of a TPP has become increasingly critical in today's challenging development landscape. The use of TPPs is essential for managing the development equation of risk × cost × time = success [23]. However, an overwhelming number of Biologics License Applications (BLAs) and New Drug Applications (NDAs) do not reference a TPP in their regulatory negotiations [23]. Furthermore, with first-year sales for non-COVID products steadily declining over the past five years and FDA Complete Response Letters (CRLs) almost tripling since 2018, the TPP framework provides an iterative document that defines and aligns commercial, clinical, medical, manufacturing, and regulatory requirements, ultimately positioning and differentiating a product in the market [23].
Core Structure of a Target Product Profile
Foundational Components
A well-structured TPP outlines essential product characteristics in a format that maps key attributes to minimum acceptable and ideal targets. This structure is typically organized around a worksheet that captures the drug labeling sections or equivalent regulatory classifications, translating them into specific, measurable product properties [1]. The core components include:
- Indications and Usage: Defines the primary indication and intended use of the product.
- Target Population: Describes the specific patient population and any relevant subgroup considerations.
- Dosage and Administration: Details treatment duration, delivery mode, dose regimen, and dose form.
- Clinical Efficacy: Outlines key efficacy endpoints and performance metrics.
- Safety Profile: Specifies acceptable risks, side effects, and adverse reaction profiles.
- Product Stability and Storage: Defines requirements for shelf life and storage conditions.
- Affordability and Accessibility: Considers price points and access considerations for patients and healthcare systems [1].
This structured approach ensures that all critical aspects of product development are considered from the outset, providing a comprehensive framework for decision-making throughout the development lifecycle.
TPP Development Methodology
Developing a robust TPP requires a systematic approach that incorporates multiple perspectives and data sources. The methodology should encompass three key stages:
- Scoping: Initial assessment of the treatment landscape and identification of unmet medical needs.
- Drafting: Creation of the initial TPP document with minimum acceptable and ideal targets for each attribute.
- Consensus-Building: Engagement with key stakeholders to align on the final TPP content and targets [20].
This process should be informed by a comprehensive analysis of the current treatment landscape, including existing and emerging competitors. For example, when developing a medication for a specific condition, a thorough appraisal of existing FDA-approved treatments provides critical benchmarks for establishing minimum acceptable and ideal performance targets [1]. This comparative approach ensures the new proposed therapy meets or surpasses current standards, maximizing its potential for patients, providers, and payors while addressing unmet medical needs [1].
Table: Core Components of a Target Product Profile
| Drug Label Attribute | Product Property | Minimum Acceptable Results | Ideal Results |
|---|---|---|---|
| Indications and Usage | Primary Indication | Defined based on medical need | Defined based on medical need |
| Indications and Usage; Clinical Studies | Target Population | Defined based on medical need | Defined based on medical need |
| Dosage and Administration | Treatment Duration | Defined based on medical need | Defined based on medical need |
| Dosage and Administration | Delivery Mode | Defined based on medical need | Defined based on medical need |
| Clinical Studies | Clinical Efficacy | Defined based on standard of care | Superior to standard of care |
| Adverse Reactions | Risk/Side Effect | Acceptable risk-benefit profile | Superior safety profile |
| How Supplied, Storage and Handling | Product Stability and Storage | Defined based on requirements | Enhanced stability/convenience |
| Affordability (Price) | Cost | Competitive pricing | Cost-effective with premium value |
| Accessibility | Availability | Standard distribution | Broad, equitable access |
TPP Applications in Pharmaceutical Development
Strategic Framework for Drug Development
In pharmaceutical development, TPPs provide a strategic framework that guides the entire product lifecycle from early research to regulatory submission and commercialization. The TPP serves as a primary strategic framework that aligns commercial and clinical workstreams, enabling drug developers to manage the development equation of risk × cost × time = success [23]. By defining the needs of patients, physicians, and payers early in the process, a TPP helps ensure a commercially viable product with potentially higher valuation [23].
A well-constructed pharmaceutical TPP is informed by the FDA's Guidance for Industry and Review Staff: "Target Product Profile — A Strategic Development Process Tool" [1]. It systematically maps key attributes from future drug labeling sections to specific product properties, establishing both minimum acceptable results and ideal targets for each parameter. This approach creates a clear development pathway while maintaining flexibility to adapt to emerging data throughout the clinical development process.
Benchmarking Against Established Therapies
A critical function of the TPP in drug development is facilitating comparative analysis against existing therapies. For instance, when developing a new pharmacotherapy for opioid use disorder, a TPP can be constructed using an FDA-approved medication like Lucemyra (lofexidine) as a benchmark [1]. The key product properties for the reference product are extracted from its drug label, enabling developers to establish realistic targets for their own product across multiple dimensions, including efficacy, safety, dosing, and storage requirements [1].
This benchmarking process is particularly valuable for identifying opportunities for product differentiation and improvement. By carefully analyzing the properties of similar products, innovators can pinpoint areas for enhancement and develop a superior treatment that addresses limitations of current standards of care [1]. This might include improved efficacy profiles, reduced side effects, more convenient administration regimens, or better affordability and accessibility.
Table: Example Pharmaceutical TPP for Opioid Withdrawal Treatment
| Drug Label Attribute | Product Property | FDA-approved: Lucemyra | Minimum Acceptable | Ideal Target |
|---|---|---|---|---|
| Indications and Usage | Primary Indication | Mitigation of opioid withdrawal symptoms | Mitigation of opioid withdrawal symptoms | Mitigation of opioid withdrawal + craving reduction |
| Clinical Studies | Target Population | Adults dependent on short-acting opioids | Adults with opioid use disorder | Broad population including long-acting opioids |
| Dosage and Administration | Treatment Duration | Up to 14 days | 7-14 days | Up to 30 days |
| Dosage and Administration | Dose Regimen | 3 tablets, 4 times daily | 3-4 times daily | 1-2 times daily |
| Clinical Studies | Clinical Efficacy | Mean SOWS score: 7.0 vs placebo 8.9 | Non-inferior to Lucemyra | Superior efficacy on validated scales |
| Adverse Reactions | Risk/Side Effect | Hypotension, bradycardia, fainting | Comparable safety profile | Improved safety with fewer CV events |
| Affordability (Price) | Cost | ~$900 (brand); ~$300 (generic) | Competitive with generic | Premium value with superior outcomes |
TPP Applications in Medical Device Development
Adaptation for Device-Specific Considerations
Medical devices require specialized TPP frameworks that address their unique technological characteristics and regulatory pathways. While sharing the same strategic purpose as pharmaceutical TPPs, device TPPs incorporate distinct elements such as intended use statements, technological specifications, and usability requirements [1]. These profiles provide a structured approach to ensuring safety, efficacy, and usability while addressing the specific regulatory requirements for medical devices, which often follow different approval pathways such as the FDA's Premarket Notification (510(k)) process [1].
A device TPP must comprehensively describe the physical properties, performance specifications, and human factors considerations unique to medical technology. This includes detailed information about the device's components, accessories, software integration, and any required accessories [1]. The technological characteristics should be specified with sufficient detail to guide engineering development while maintaining alignment with clinical needs and user requirements.
Case Example: Neurostimulation Device
The adaptation of TPPs for medical devices is illustrated by the example of a neurostimulation device for opioid withdrawal symptoms. The NET Device, a non-invasive, battery-powered, portable, reusable, prescription device designed to provide bilateral, transcranial, transcutaneous, alternating current stimulation (tACS), serves as a benchmark in this case [1]. The TPP for such a device would include specific parameters such as:
- Intended Use: Clear description of the device's purpose and the context of use, including whether it is intended for use in conjunction with other therapies [1].
- Patient Population: Specific characteristics of the target patient population, including age range, diagnosis criteria, and severity assessment scales [1].
- Treatment Parameters: Detailed specifications regarding treatment duration, frequency, and intensity [1].
- Technological Characteristics: Description of the stimulation type, energy delivery mechanism, and technical specifications [1].
- Clinical Performance: Objective metrics for efficacy based on validated clinical assessment scales [1].
This structured approach ensures that device development remains focused on addressing clear clinical needs while satisfying regulatory requirements for safety and effectiveness.
Table: Example Medical Device TPP for Opioid Withdrawal
| Product Property | NET Recovery Device | Minimum Acceptable | Ideal Target |
|---|---|---|---|
| Intended Use / Indications | tACS for opioid withdrawal with standard medications | Non-invasive neuromodulation for opioid withdrawal | Standalone therapy for opioid withdrawal symptoms |
| Patient Population | Age 18+, OUD diagnosis, COWS score ≥ moderate | Age 18+, OUD, moderate-severe withdrawal | Broad population including mild-moderate symptoms |
| Treatment Duration | 1 hour/day, max 7 days | 30-60 min/day, 5-7 days | Flexible dosing based on symptom response |
| Technological Characteristics | Electrical stimulation at auricular region | Non-invasive electrical stimulation | Multiple stimulation modalities with targeting |
| Clinical Performance | 61.3% mean COWS reduction at 60 minutes | ≥40% COWS reduction | ≥70% COWS reduction with sustained effect |
| Safety Analysis/Risk | Consistent with predicate device | No serious device-related adverse events | Superior safety profile to predicate |
| Affordability (Price) | $600-$1,500 | Competitive with existing devices | Cost-saving compared to standard care |
TPP Applications in Digital Health Technologies
Emerging Framework for Digital Health
Digital Health Technologies (DHTs), including those incorporating artificial intelligence (AI), represent an emerging application area for TPPs where standardization is still evolving. DHTs promise improved healthcare access, efficiency, and quality, helping meet the growing mismatch between capacity and demand [20]. However, adoption remains limited, especially for AI, in part due to complex system requirements that extend beyond traditional medical product considerations [20]. TPPs offer a potential solution by providing a mechanism for health systems to "demand signal" to innovators, outlining the characteristics necessary for DHTs to be utilized in practice [20].
The development of TPPs for DHTs requires consideration of unique factors including software validation, algorithm performance, cybersecurity, interoperability, and usability across diverse user populations. A systematic review examining current DHT TPPs found limited standardization in development or contents, with limited transparency in reporting [20]. The review identified 248 different characteristics reported across 14 TPPs, which were consolidated to 33 key characteristics, highlighting the diversity of approaches in this emerging field [20].
Special Considerations for AI-Enabled Technologies
AI-enabled DHTs introduce additional complexities that must be addressed in target product profiles. These include requirements for algorithm transparency, training data documentation, performance drift monitoring, and adaptation protocols. The recent establishment of the FDA Digital Health Advisory Committee underscores the regulatory attention being paid to this category, with specific focus on topics such as "generative artificial intelligence-enabled digital mental health medical devices" [24].
A comprehensive TPP for an AI-enabled DHT should address both the digital components and the clinical integration requirements. Based on analysis of existing DHT TPPs, key considerations include:
- Clinical Workflow Integration: How the technology fits within existing clinical pathways and health system workflows.
- Data Governance: Protocols for data privacy, security, and management throughout the product lifecycle.
- Algorithm Performance: Specifications for sensitivity, specificity, and reliability across diverse populations.
- Interoperability: Compatibility with existing health information systems and standards.
- Implementation Requirements: Technical infrastructure, training needs, and support systems required for successful deployment [20].
The dynamic nature of AI technologies further complicates TPP development, as these products may evolve significantly through software updates and algorithm refinements after initial deployment, requiring flexible TPP frameworks that can accommodate iterative improvement while maintaining safety and efficacy standards.
Comparative Analysis Across Product Types
Regulatory and Development Pathway Variations
While TPPs serve the same strategic purpose across different product types, their implementation varies significantly based on regulatory pathways and development considerations. Pharmaceuticals, medical devices, and digital health technologies each face distinct regulatory frameworks, evidence requirements, and development challenges that influence TPP structure and content.
Pharmaceutical TPPs predominantly follow the structure proposed in the FDA's 2007 draft guidance, organized around future drug labeling concepts [1]. Medical device TPPs incorporate elements specific to device classification and regulatory pathways such as 510(k) or De Novo classification [1]. Digital health TPPs are the least standardized, with ongoing efforts to define appropriate frameworks and requirements for these technologies, particularly those incorporating AI [20].
These differences reflect the unique evidence needs and risk profiles associated with each product category. Pharmaceuticals typically require extensive clinical trials demonstrating safety and efficacy through statistically significant outcomes. Medical devices must demonstrate substantial equivalence to predicates or establish reasonable assurance of safety and effectiveness for new device types. Digital health technologies often require validation of analytical and clinical performance, with particular emphasis on usability and human factors engineering.
Commonalities in Strategic Application
Despite these differences, common strategic principles apply to TPP development across all product categories. All effective TPPs:
- Articulate Unmet Needs: Clearly define the clinical problem being addressed and the value proposition for patients, providers, and healthcare systems.
- Establish Target Claims: Specify the intended uses, indications, and performance claims sought for the product.
- Define Threshold and Target Profiles: Distinguish between minimum acceptable performance and ideal targets to guide development priorities and trade-off decisions.
- Inform Development Strategy: Guide resource allocation, study design, and evidence generation plans throughout the product development lifecycle.
- Facilitate Stakeholder Alignment: Create a shared vision across functional areas including research, clinical development, regulatory affairs, commercialization, and manufacturing.
The fundamental purpose of aligning development efforts with patient needs and regulatory requirements remains consistent across product types, even as the specific content and structure of TPPs adapt to address category-specific considerations.
Table: Comparative TPP Requirements Across Product Types
| Characteristic | Pharmaceuticals | Medical Devices | Digital Health Technologies |
|---|---|---|---|
| Primary Regulatory Focus | Safety and efficacy through controlled trials | Substantial equivalence or reasonable assurance of safety and effectiveness | Analytical and clinical validation, human factors, cybersecurity |
| Key Evidence Requirements | PK/PD data, phase 1-3 clinical trials | Engineering testing, bench studies, clinical performance data | Algorithm performance, usability testing, clinical utility studies |
| Typical Development Timeline | 10-15 years | 3-7 years | 1-3 years |
| Post-Market Requirements | Phase 4 studies, safety monitoring | Post-market surveillance, registry studies | Performance monitoring, software updates, cybersecurity patches |
| Unique TPP Considerations | Dosing regimen, drug interactions, pharmacokinetics | Technical specifications, usability, service requirements | Interoperability, data governance, algorithm transparency |
Experimental and Methodological Approaches
Research Reagent Solutions for Product Characterization
The development of medical products relies on specialized research reagents and methodologies for target identification and product characterization. These tools enable researchers to understand product interactions with biological systems and validate mechanisms of action. Key research reagents and their applications include:
- Quantitative Mass Spectrometry: Enables proteome-wide interaction studies of small therapeutic molecules and their target proteins, complementing phenotypic-based drug screens [25].
- Isobaric Tandem Mass Tags (TMTs): Used to multiplex samples and increase quantification precision in thermal proteome profiling (TPP) analysis by data-dependent acquisition (DDA) [25].
- Data-Independent Acquisition (DIA) Methods: Provides higher sensitivity and protein coverage with reduced costs and sample preparation steps compared to labeled quantification approaches [25].
- Thermal Proteome Profiling (TPP) Pipeline: A cost-effective alternative for thermal shift quantification that enables detection of target engagement with known inhibitors and downstream targets [25].
- Cellular Thermal Shift Assay: Evaluates drug target interactions in cells through thermal stability assessments [25].
These methodological approaches support the characterization of product-target interactions that inform TPP development by providing critical data on mechanism of action, selectivity, and potential off-target effects.
Visualization Methodologies for Complex Data Relationships
Graph visualization and network analysis techniques provide powerful methods for representing complex relationships in development data, particularly for understanding product interactions and development pathways. These visualization methodologies enable researchers to:
- Model Complex Relationships: Represent entities as nodes and connections as edges to reveal patterns and insights missed in traditional statistical analyses [26].
- Apply Layout Algorithms: Utilize force-directed, circular, or hierarchical layouts to create visually informative network visualizations based on network characteristics and research objectives [26].
- Implement Visual Encoding: Vary node size, color, edge thickness, and style to represent multiple data attributes simultaneously in multivariate network data [26].
- Create Interactive Visualizations: Enable zooming, panning, node selection, and filtering functionality to explore complex data structures and uncover hidden patterns [27].
These visualization approaches facilitate the analysis of complex biological networks, development pathways, and relationship structures that inform target product profile development across pharmaceutical, device, and digital health applications.
TPP Development and Integration Workflow
Target Product Profiles serve as essential strategic tools that guide medical product development across pharmaceuticals, devices, and digital health technologies. While each product category requires specific adaptations to address unique regulatory pathways and development considerations, the core TPP function of aligning development efforts with clinical needs and commercial requirements remains consistent. The dynamic nature of TPPs enables iterative refinement throughout the development process, incorporating emerging data and insights to optimize product success [1].
The increasing complexity of medical products, particularly with the emergence of AI-enabled digital health technologies, underscores the ongoing importance of robust TPP frameworks. As the development landscape evolves, TPPs will continue to provide critical strategic direction for managing risk, cost, and time while maximizing the potential for developing successful products that address unmet medical needs and improve patient outcomes [23]. Future developments in TPP methodology will likely focus on standardizing approaches for novel product categories while maintaining flexibility to accommodate innovative technologies and development paradigms.
The Target Product Profile (TPP) serves as a strategic compass throughout the complex journey of drug development, providing a prospective blueprint that aligns preclinical research, clinical trials, and manufacturing with regulatory and commercial objectives [28]. For Adeno-Associated Virus (AAV)-based gene therapies, which represent a transformative frontier in treating rare and monogenic diseases, the TPP is particularly vital [28]. These therapies often feature a one-time administration model, complex production processes, and extended therapeutic effects, making early strategic planning essential for success [28]. This paper explores the formulation and application of TPPs within AAV-based gene therapy development, using the National Institutes of Health (NIH) Platform Vector Gene Therapy (PaVe-GT) program as a primary case study. The insights and frameworks presented herein are designed to provide researchers, scientists, and drug development professionals with a structured methodology for advancing their own gene therapy programs.
TPP Fundamentals: Definition, Purpose, and Evolution
Definition and Key Components
A TPP is a living document that outlines a therapy's desired quality, safety, and efficacy characteristics to meet clinical needs and regulatory standards [28]. It functions as a roadmap for development teams, a communication tool across disciplines, and a benchmark for go/no-go decisions [28]. For AAV-based therapies, a well-constructed TPP directly informs key study parameters, including proof-of-concept efficacy in animal models, non-clinical safety assessments, bioanalytical assay development, and manufacturing processes [28].
The core components of a comprehensive TPP for an AAV-based therapy are summarized in the table below.
Table 1: Core Components of a TPP for an AAV-Based Gene Therapy
| Component | Description | Considerations for AAV Therapies |
|---|---|---|
| Disease Indication | The specific rare genetic condition the therapy aims to address [28]. | Balance feasible outcomes (e.g., biomarker improvement) with aspirational goals (e.g., long-term disease correction) [28]. |
| Target Population | The intended patient group for treatment [28]. | Often pediatric for early-onset conditions; requires careful risk-benefit assessment due to AAV's potential for prolonged activity and immunogenicity [28]. |
| Dosage and Administration | The physical form, route, and schedule of administration [28]. | Typically a single intravenous infusion; details format (e.g., pre-filled syringes) and reflects AAV's delivery logistics [28]. |
| Clinical Efficacy Endpoints | Measurable outcomes to demonstrate therapeutic effect [28]. | Include transgene expression, biomarker changes (e.g., metabolite reduction), survival benefit, and quality of life measures [28]. |
| Safety and Tolerability | Outline of expected adverse effects [28]. | Defines acceptable immune responses, off-target effects, and overall risk-benefit profile for a one-time administration [28]. |
| Drug Stability and Shelf Life | Storage requirements and product longevity [28]. | Critical for maintaining vector potency given AAV's sensitivity to environmental factors [28]. |
The TPP as a Dynamic Document
A TPP is not static; it evolves through development stages. In early research, it serves as a visionary foundation with aspirational goals. As proof-of-concept (POC) data emerges, the TPP integrates data-driven endpoints and detailed safety profiles. By the Investigational New Drug (IND) application stage, it solidifies into a comprehensive specification tailored to meet Good Manufacturing Practice (GMP) and clinical trial standards [28]. This iterative refinement process ensures the TPP remains a relevant and actionable guide.
Figure 1: TPP Evolution Through Development Stages
Case Study: The PaVe-GT Program and AAV9-hPCCA
The NIH's Platform Vector Gene Therapy (PaVe-GT) program is an initiative to develop AAV gene therapies for four rare, low-prevalence diseases using a platform-based approach [29] [30]. This strategy aims to incorporate efficiencies across preclinical and clinical development by applying similar processes, study designs, and regulatory pathways [30]. A multidisciplinary team of basic researchers, disease and drug development experts, and project managers assembles to strategize and execute the program [28]. The program is committed to publicly disseminating all scientific and regulatory learnings to inform and enable other gene therapy development initiatives [30].
TPP Formulation for AAV9-hPCCA
The PaVe-GT team developed a TPP for AAV9-hPCCA, a candidate designed to treat propionic acidemia (PA) caused by mutations in the PCCA gene [28]. PA is a rare organic acidemia affecting ~1 in 100,000, leading to metabolic crises and high childhood mortality [28]. The initial TPP, drafted prior to IND-enabling studies, was based on preclinical POC data from Pcca knockout mice showing prolonged survival and reduced disease biomarkers [28].
Table 2: Initial TPP for AAV9-hPCCA for Propionic Acidemia
| TPP Element | Desired (Optimal) Target | Minimum Acceptable Target |
|---|---|---|
| Indication & Usage | Treatment of PA due to PCCA deficiency; expression of PCCA transgene/protein; reduction of plasma 2-methylcitrate; prevention of metabolic decompensation [28]. | Treatment of PA due to PCCA deficiency [28]. |
| Patient Population | Pediatric patients (2-18 years old) [28]. | Pediatric patients [28]. |
| Dosage & Administration | Single intravenous infusion [28]. | Single intravenous infusion [28]. |
| Efficacy | Improved survival; subjective quality of life measures [28]. | Stabilization of disease progression; change in surrogate endpoints [28]. |
| Duration of Effect | Long-term, stable expression [28]. | Stable expression for at least 2 years [28]. |
| Safety | Well-tolerated [28]. | No serious adverse events; no systemic infusion reactions [28]. |
Regulatory Engagement: The INTERACT Meeting
After completing POC studies, the PaVe-GT team sought early FDA feedback through an INitial Targeted Engagement for Regulatory Advice on CBER/CDER ProducTs (INTERACT) meeting [29] [30]. This pre-IND meeting type is designed for early-stage feedback after POC completion [28]. The briefing package included:
- In Vivo POC Data: Survival and biomarker data from Pcca knockout mice, with supporting mRNA and protein expression results [28] [30].
- Toxicology Plan: Proposed study design for IND-enabling Good Laboratory Practice (GLP) toxicology [28].
- Clinical Synopsis: A first-in-human trial design for pediatric PA patients, with endpoints like 2-methylcitrate reduction [28].
- CMC Information: Preliminary data from a small-scale feasibility batch to guide scaling to GMP standards [28].
- Platform Strategy: Information on the overall platform approach [28].
This engagement allowed the team to refine the TPP and development strategy based on regulatory input before committing to more costly late-stage preclinical work.
Experimental and Methodological Frameworks
Key Experimental Protocols in AAV Therapy Development
Advancing an AAV therapy from concept to clinic requires a series of rigorous, sequential experiments designed to demonstrate biological plausibility, efficacy, and safety.
Table 3: Key Experimental Protocols for AAV-Based Gene Therapy Development
| Experimental Stage | Protocol Objectives | Key Methodologies |
|---|---|---|
| In Vitro Proof-of-Concept | Establish biological activity of the transgene; assess transduction efficiency [31]. | Cell culture of target cell types (e.g., HEK293T); immunofluorescence and Western blot for transgene expression; functional enzymatic assays [31]. |
| In Vivo Proof-of-Concept | Demonstrate efficacy in a disease-relevant model; identify biomarker changes [28] [30]. | Use of genetically engineered mouse models (e.g., Pcca KO); AAV administration via route (e.g., IV); survival analysis; biomarker quantification (e.g., LC-MS/MS for metabolites) [28] [31]. |
| Biodistribution & Expression Profiling | Determine vector distribution and transgene expression in target/non-target tissues [31]. | qPCR/ddPCR for vector genome quantification; scRNA-seq to identify transduced cell types and tropism; immunohistochemistry [31]. |
| IND-Enabling GLP Toxicology | Assess safety and tolerability; define a therapeutic index [28]. | Toxicology studies in relevant animal species; clinical pathology; histopathology; immunogenicity assessment [28]. |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for AAV Gene Therapy Development
| Reagent / Material | Function and Application |
|---|---|
| AAV Serotypes (e.g., AAV9) | The viral capsid that determines tissue tropism and transduction efficiency. AAV9 is widely used for its broad tropism, including liver and CNS [28] [31]. |
| Cell Lines (HEK293T) | Standard cell line for the production of recombinant AAV vectors via triple transfection [31]. |
| Animal Disease Models | Genetically modified mice (e.g., Pcca KO) or patient-derived xenografts to model human disease and test therapeutic efficacy [28] [31]. |
| hiPSC-Derived Models | Patient-derived induced pluripotent stem cells differentiated into target tissues (e.g., retinal organoids, hepatocytes) for human-relevant disease modeling and toxicity screening [31]. |
| scRNA-Seq Platforms | Technology to characterize cell-type-specific transcriptomes in tissues or organoids, confirming target engagement and uncovering mechanisms of action or toxicity [31]. |
| ELISA & NAb Assays | Critical for assessing immunogenicity; ELISA measures total anti-AAV antibodies, while NAb assays determine the titer that neutralizes transduction [32]. |
Workflow Visualization: From Concept to IND
The following diagram outlines the key stages and decision points in the preclinical development of an AAV-based gene therapy, highlighting the central role of the TPP.
Figure 2: AAV Therapy Preclinical Workflow and TPP Integration
The development of a robust Target Product Profile is a foundational activity for successfully navigating the intricate landscape of AAV-based gene therapy development. As demonstrated by the PaVe-GT case study, a dynamic TPP that evolves with emerging preclinical data serves as a critical strategic tool, fostering alignment across multidisciplinary teams and guiding regulatory interactions. The practice of early engagement with regulators, such as through an INTERACT meeting, provides invaluable feedback that de-risks the development path. For researchers and drug developers, adopting a disciplined approach to TPP creation and iteration—grounded in strong biological rationale and structured by the frameworks presented here—can significantly enhance the efficiency and probability of success in bringing transformative AAV gene therapies to patients in need.
Real-World TPP Evolution Through Clinical Development Stages
A Target Product Profile (TPP) is a strategic planning tool that outlines the desired characteristics of a medical product, guiding its development from conception to commercialization [1]. It serves as a living document that articulates the intended use, target population, and key performance features of a prospective product, ensuring alignment between research efforts and specific clinical needs and regulatory requirements [1]. In the contemporary pharmaceutical landscape, TPPs have become indispensable for navigating funding constraints, regulatory shifts, and evolving therapeutic priorities, particularly for emerging biotech and small pharma companies [3].
The fundamental purpose of a TPP is to provide strategic clarity throughout the drug development lifecycle. By defining critical attributes early in the process, a TPP fosters stakeholder alignment, facilitates efficient resource allocation, and increases the likelihood of developing a successful product that addresses unmet medical needs [1]. From a regulatory perspective, TPPs frame development in relation to submission requirements, while in public health contexts, they set research and development targets for funders and developers [2]. Well-constructed TPPs typically outline minimum viable criteria for regulatory approval, base case expectations for performance, and aspirational goals that define true commercial and clinical success [3].
TPP Structure and Core Components
Standardized TPP Framework
A comprehensive TPP follows a structured format that maps key attributes to developmental objectives. The U.S. Food and Drug Administration's guidance outlines a framework organized around drug labeling sections, with specifications for product properties, minimum acceptable results, and ideal targets [1]. This systematic approach ensures all critical aspects of product development are considered and quantified where possible.
Table 1: Core Components of a Target Product Profile
| Drug Label Attribute | Product Property | Minimum Acceptable | Ideal Target |
|---|---|---|---|
| Indications and Usage | Primary Indication | Specific medical condition | Broader indications or first-line treatment |
| Target Population | Demographic & clinical characteristics | Narrowly defined group | Expanded populations |
| Dosage and Administration | Treatment Duration, Delivery Mode, Dose Regimen | Minimally effective duration and frequency | Optimal patient convenience and adherence |
| Clinical Studies | Clinical Efficacy | Statistically significant improvement over placebo | Superior to standard of care |
| Adverse Reactions | Risk/Side Effect Profile | Acceptable risk-benefit ratio | Superior safety profile |
| How Supplied/Storage | Product Stability | Standard storage conditions | Room temperature stability, longer shelf life |
| - | Affordability | Cost-effective within healthcare system | Premium pricing justified by outcomes |
| - | Accessibility | Available in major markets | Broad global access |
This framework is adaptable across various product types, including pharmaceuticals, medical devices, and diagnostic tests, with modifications to address specific technological considerations [1]. For instance, medical device TPPs include elements such as intended use, patient population, technological characteristics, and clinical testing parameters [1].
Research Reagents and Essential Materials for TPP Development
The development and refinement of TPPs require specific analytical tools and resources to generate the necessary evidence base.
Table 2: Essential Research Reagents and Tools for TPP Development
| Research Tool | Function in TPP Development | Application Context |
|---|---|---|
| Competitive Landscape Analysis | Benchmarks against existing treatments | Informs minimum acceptable and ideal targets |
| Regulatory Database | Provides precedent for approval requirements | Shapes indications, safety, and efficacy criteria |
| Clinical Trial Design Software | Models trial parameters and outcomes | Optimizes study design elements in TPP |
| Health Economic Models | Projects cost-effectiveness and budget impact | Informs affordability and pricing parameters |
| Disease Progression Models | Quantifies natural history of disease | Sets clinically meaningful efficacy thresholds |
| Biomarker Assays | Measures pharmacodynamic effects | Supports mechanism of action and dosing rationale |
| Stability Testing Systems | Evaluates product shelf-life | Informs storage and handling specifications |
TPP Evolution Through Clinical Development Stages
Phase-Appropriate TPP Refinement
The utility and specificity of TPPs evolve significantly as a drug progresses through development phases. In early-stage development, TPPs help navigate high uncertainty and establish foundational goals with broader ranges for key parameters [3]. As products advance, TPPs become more refined, integrating robust data and commercial projections to create precise targets for late-phase development [3].
Table 3: TPP Evolution Across Clinical Development Stages
| Development Stage | TPP Characteristics | Primary Function | Level of Specificity |
|---|---|---|---|
| Discovery/Preclinical | High-level strategic vision | Guides candidate selection and initial investment | Broad ranges for most parameters |
| Phase I | Focus on safety, PK/PD, mechanism | Establishes proof of concept and initial dosing | Preliminary human data informs basic parameters |
| Phase II | Therapeutic concept validation | Determines feasibility of efficacy signals | Narrower ranges based on clinical data |
| Phase III | Refined, evidence-based profile | Supports regulatory approval and labeling | Precise targets supported by robust data |
| Registration/Launch | Finalized label and commercial profile | Guides market access and commercialization | Fixed targets aligned with approved label |
This evolutionary process reflects the continuous iteration between emerging data and strategic goals. The TPP serves as a dynamic document that is regularly updated to incorporate new information, ensuring development remains aligned with both scientific reality and market needs [1] [3].
Quantitative Assessment of Protocol Complexity
Recent methodologies have emerged to quantitatively assess protocol complexity, which directly impacts TPP execution. The Protocol Complexity Tool (PCT) provides a framework to objectively measure complexity across five domains: operational execution, regulatory oversight, patient burden, site burden, and study design [33]. This tool utilizes 26 multiple-choice questions scored on a 3-point scale (0=low complexity, 0.5=medium complexity, 1=high complexity) to generate domain complexity scores and a total complexity score between 0-5 [33].
Research has demonstrated that higher protocol complexity scores correlate significantly with operational challenges. Specifically, total complexity score positively correlates with time-to-site activation (rho=0.61; p=0.005) at 75% site activation and participant enrollment (rho=0.59; p=0.012) at 25% recruitment [33]. These findings underscore the importance of simplicity in protocol design to enhance executable TPPs.
Figure 1: TPP Evolution from Strategic to Operational Tool
Methodologies for TPP Development and Evaluation
TPP Construction Protocols
The development of a robust TPP follows a systematic methodology that integrates multiple data sources and stakeholder perspectives. The process typically begins with a comprehensive analysis of the current treatment landscape, including existing and emerging therapies [1]. This involves extracting key product properties from competitor labels, clinical study reports, and health technology assessments to establish baseline expectations.
A critical protocol for TPP construction involves the use of benchmarked target profiles, where established products serve as reference points for new developments. For instance, when developing a medication for opioid withdrawal, a TPP can be constructed using FDA-approved Lucemyra (lofexidine) as a benchmark, with key product properties extracted from its drug label to establish minimum acceptable and ideal targets [1]. This comparative approach ensures new therapies meet or surpass current standards while addressing unmet medical needs.
The analytical process involves:
- Stakeholder Alignment: Engaging cross-functional teams including clinical development, regulatory affairs, commercial operations, and patient representatives
- Competitive Profiling: Systematic assessment of competitor products across efficacy, safety, and convenience parameters
- Gap Analysis: Identification of unmet needs and differentiation opportunities
- Target Setting: Establishing minimum acceptable and ideal targets for each critical attribute
- Scenario Planning: Developing contingency plans for different development outcomes
Protocol Complexity Assessment Methodology
The Protocol Complexity Tool (PCT) provides a structured methodology for evaluating protocol complexity during TPP refinement [33]. The assessment involves:
Domain Evaluation:
- Study Design Complexity: Assesses endpoints, eligibility criteria, and statistical considerations
- Operational Execution: Evaluates procedures, site requirements, and data collection methods
- Regulatory Oversight: Examines reporting requirements and regulatory burden
- Patient Burden: Measures visit frequency, procedures, and participation demands
- Site Burden: Assesss resource requirements and operational complexity
Scoring Protocol: Each of the 26 questions is scored on a 3-point scale (0, 0.5, 1) with domain scores calculated as: [ \text{Domain Complexity Score} = \frac{\sum \text{Question Scores}}{\text{Number of Questions in Domain}} ]
The Total Complexity Score is derived from: [ \text{Total Complexity Score} = \sum \text{Domain Scores} ]
This methodology enables quantitative assessment of protocol complexity and identification of opportunities for simplification without compromising scientific objectives [33].
Figure 2: Protocol Complexity Assessment Workflow
Advanced Applications and Future Directions
Artificial Intelligence in TPP Development
Artificial intelligence is increasingly playing a role in streamlining TPP creation and refinement. Current AI applications include extracting insights from scientific and regulatory literature, generating first-draft TPP templates based on structured prompts, and horizon scanning to identify changes in regulatory or therapeutic landscapes [3]. These tools can process vast quantities of information to identify patterns and precedents that might escape manual review.
However, AI implementation faces significant challenges, including reliance on publicly available data that skews toward successful trials while omitting valuable insights from failed studies [3]. Additionally, commercial data is frequently redacted or proprietary, limiting AI's effectiveness in modeling market outcomes. The future potential lies in agentic AI – autonomous tools that dynamically update TPPs or flag strategic shifts as new information emerges [3].
Regulatory Strategy and TPP Alignment
Regulatory strategy constitutes a critical component of TPP planning throughout development stages. During periods of administrative change or regulatory uncertainty, companies should leverage existing FDA resources and guidance documents, engage early and strategically with regulators (particularly for complex or orphan indications), and focus on working within established guidance rather than attempting to circumvent it [3]. By becoming well-versed in regulatory expectations and precedents, developers can reduce internal decision-making delays and approach agencies with well-informed proposals.
The TPP serves as a foundational document for regulatory interactions, providing a structured framework for discussing development plans and alignment with regulatory expectations. A well-constructed TPP demonstrates sponsor understanding of development requirements and facilitates more productive regulatory dialogue.
Contingency Planning and Scenario Analysis
Modern TPP development incorporates contingency planning to address the shifting scrutiny on certain therapeutic areas and evolving standards of care. TPPs support this by encouraging holistic thinking about long-term regulatory and commercial goals, allowing for scenario planning based on evolving standards, and facilitating strategic pivots without losing sight of core objectives [3]. Forward-looking companies must consider not only current regulatory climates but also anticipate what approval requirements might look like five to seven years in the future when development programs near completion.
This approach recognizes that TPPs must be dynamic documents that can accommodate changing clinical landscapes, competitive environments, and regulatory expectations while maintaining focus on the core product vision and patient needs.
Overcoming TPP Challenges: From Static Documents to Strategic Assets
In the high-stakes landscape of pharmaceutical research and development, a Target Product Profile (TPP) serves as a critical strategic compass. A TPP outlines the desired characteristics of a target product for a particular disease, stating its intended use, target populations, and desired attributes, including safety and efficacy-related characteristics [2]. It acts as a foundational planning tool that guides development toward a product with optimal commercial and therapeutic potential. However, when a TPP becomes stagnant and fails to evolve with emerging data, it transforms from a strategic asset into a significant liability. An outdated TPP can misdirect a development program, leading to costly late-stage failures and compromising the delivery of much-needed therapies to patients. This technical guide examines the critical dangers of an outdated TPP and provides a framework for maintaining its relevance throughout the drug development lifecycle.
The Evolving Nature of Target Product Profiles
A TPP is not a static document created at the inception of a project and left unchanged. By its nature, it should be a dynamic and living document that integrates new knowledge. The World Health Organization (WHO) emphasizes that TPPs describe both the "preferred" and the "minimally acceptable" profiles for health products, establishing a range of acceptable outcomes that can be refined as new information becomes available [2].
In practice, TPP testing is applied at multiple stages of the drug life cycle to inform strategic decisions [14]:
- Market opportunity confirmation for Business Development & Licensing (BD&L)
- New drug development or early drug testing to inform prioritization strategy
- Launch and commercial strategy preparation for late-stage drugs
At each of these stages, new data must be fed back into the TPP to ensure it remains an accurate reflection of both the product's potential and the evolving market and regulatory landscape.
Quantifiable Consequences: The Impact of an Outdated TPP
The risks of an outdated TPP manifest in both direct financial costs and strategic missteps. The following table summarizes the key quantitative impacts and associated commercial risks.
Table 1: Financial and Strategic Impact of an Outdated TPP
| Impact Area | Financial Consequence | Strategic & Commercial Risk |
|---|---|---|
| Clinical Trial Design | Increased costs due to protocol amendments; need for additional trials to collect missed data [14] | Failed endpoints; inability to demonstrate meaningful value proposition to regulators or payers |
| Development Timeline | Significant project delays (months to years) while re-tooling development strategy [14] | Lost market opportunity; reduced patent-protected commercial life |
| Resource Allocation | Misallocation of ~$2.6 billion average cost for a successful FDA-approved drug [14] | Opportunity cost from pursuing suboptimal assets; portfolio inefficiencies |
| Market Perception | N/A | Damaged credibility with key opinion leaders (KOLs) and investors from unrealistic profiles [14] |
Critical Pitfalls in Practice
Misalignment with Clinical Reality
One of the most significant dangers occurs when a TPP remains anchored to early, optimistic preclinical hypotheses that are not borne out in clinical trials. If the TPP is not updated to reflect actual Phase 1 or 2 data, the subsequent clinical program is built on a flawed foundation. This misalignment can lead to selecting the wrong endpoints, inappropriate patient populations, or unrealistic dosing regimens, ultimately resulting in failed Phase 3 trials.
Ignoring the Evolving Competitive Landscape
The competitive environment for a new therapy can change dramatically over a multi-year development program. An outdated TPP that does not account for new competitor products, changing standard of care, or shifts in payer requirements dooms a product to commercial irrelevance upon launch. The TPP must be regularly stress-tested against the external market to ensure its value proposition remains differentiated and sustainable [14].
Overlooking Practical Deployment Constraints
A TPP crafted in a vacuum, without ongoing input from end-users, may define a product that is difficult to deploy in real-world settings. For example, a profile insisting on a frozen formulation may not be viable in regions with unreliable cold-chain infrastructure. Regular testing of the TPP with healthcare professionals, payers, and even patients is crucial to identify and address these practical constraints before they derail commercial success [14].
A Proactive Framework: Mitigating Risk Through Continuous TPP Validation
To avoid the pitfalls of an outdated TPP, a proactive, data-driven approach to TPP management is essential. The following workflow outlines a continuous validation cycle.
This process should be anchored by formal TPP testing, a market research methodology where the TPP summary is presented to an audience of experts—such as prescribing healthcare professionals, payers, or patient advocates—to gather unbiased feedback on its understandability, credibility, and potential [14]. The insights from this testing are the critical data that fuel the "Compare Data vs. TPP" and "Update TPP" steps in the workflow.
Experimental & Methodological Validation
Robust experimental design is the bedrock upon which a reliable TPP is built and updated. The following protocol exemplifies a detailed methodology for generating high-quality data on protein-ligand interactions, which can directly inform the "Pharmacology" and "Safety" sections of a TPP for a drug candidate.
Detailed Protocol: Membrane-Mimetic Thermal Proteome Profiling (MM-TPP)
Objective: To identify membrane protein targets and off-target interactions of small-molecule drug candidates in a native-like environment, providing critical data for TPP efficacy and safety profiles [34] [35].
Workflow Overview:
Step-by-Step Methodology:
Library Preparation:
- Isolate the membrane fraction from target tissue (e.g., mouse liver) or cell lines via differential centrifugation [35].
- Solubilize the membrane fraction using a mild detergent.
- Reconstitute the solubilized proteins into a Peptidisc library. The Peptidisc membrane mimetic stabilizes integral membrane proteins in a water-soluble, native-like state, preserving their interactomes and lipid allosteric modulators, which is a significant advantage over detergent-based methods [34] [35].
Ligand Treatment & Thermal Challenge:
- Divide the Peptidisc library into two aliquots.
- Treat one aliquot with the ligand/drug candidate of interest and the other with a control (e.g., ddH2O) [35].
- Subject each sample to a gradient of elevated temperatures (e.g., 51°C, 56°C, 61°C) for a short duration (3 minutes) to induce protein denaturation [35].
Sample Processing & Analysis:
- Remove denatured and aggregated proteins by ultracentrifugation [35].
- Digest the soluble proteins (those stabilized by ligand binding) in the supernatant and analyze them via Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) [34] [35].
- Identify proteins exhibiting significant thermal stabilization or destabilization in the treatment group compared to the control using established statistical methods (e.g., thresholding on fold-differences between triplicate groups) [35].
Key Advantages for TPP Validation:
- Detergent-Free: The Peptidisc system avoids detergent-induced artifacts, enabling a more physiologically relevant assessment of membrane protein interactions, which is crucial as these represent nearly two-thirds of druggable targets [35].
- Proteome-Wide Scope: Provides an unbiased, system-wide view of both on-target and off-target engagements, delivering critical data to refine the TPP's efficacy and safety sections [34].
- High Sensitivity: Capable of detecting interactions for proteins expressed at low endogenous levels, as demonstrated by the stabilization of the bacterial ABC transporter MsbA [35].
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and their functions for implementing the MM-TPP protocol, which can generate pivotal data to keep a TPP current.
Table 2: Essential Research Reagents for MM-TPP Experiments
| Reagent / Material | Function in the Experiment |
|---|---|
| Peptidisc Membrane Mimetic | A self-assembling scaffold that stabilizes integral membrane proteins in a water-soluble, native-like state, making them compatible with downstream MS analysis without denaturing detergents [34] [35]. |
| Membrane Fraction Library | A complex mixture of proteins isolated from the target tissue or cell line, serving as the physiologically relevant source for identifying drug-protein interactions [35]. |
| Ligand of Interest | The small-molecule drug candidate or metabolite whose protein targets and off-target effects are being mapped across the proteome [34]. |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | The analytical platform used to identify and quantify the proteins remaining soluble after heat denaturation, allowing for the detection of ligand-induced thermal stability shifts [34] [35]. |
In an industry where the average cost of bringing a new drug to market exceeds $2.6 billion [14], the dangers of an outdated TPP cannot be overstated. A stagnant TPP blindsides development teams to emerging clinical realities, evolving competition, and practical deployment barriers, leading to expensive late-stage failures and non-viable products. The strategic imperative is to treat the TPP not as a static document but as a dynamic, data-driven hypothesis that is continuously validated and refined. By embedding a culture of continuous TPP validation—supported by robust experimental data, regular stakeholder testing, and a formal process for updates—organizations can navigate the complexities of drug development with clarity, mitigate profound financial and clinical risks, and significantly enhance the probability of delivering successful new therapies to patients.
Integrating Competitive Intelligence and Landscape Analysis
In modern drug development, Target Product Profiles (TPPs) provide the strategic blueprint for product development, outlining desired characteristics, intended use, target population, and key performance features [1]. Competitive intelligence and landscape analysis serve as critical inputs that inform and refine this blueprint, ensuring development efforts align not only with clinical needs and regulatory pathways but also with market realities and competitive dynamics. This integration enables research teams to develop products that address unmet medical needs while achieving commercial success and differentiation.
A TPP functions as a dynamic strategic planning tool that outlines the desired "what" of a medical product, while competitive landscape analysis provides the "why" behind those strategic choices by contextualizing them within the current and future market environment [1]. This synergy is particularly crucial in therapeutic areas with intense competition or rapid technological advancement, where positioning against established and emerging alternatives can determine commercial viability.
Foundational Concepts
Target Product Profiles in Pharmaceutical Development
A Target Product Profile (TPP) is a strategic development process tool that guides the creation of safe and effective medical products by aligning stakeholder expectations and ensuring development activities remain focused on specific clinical needs and regulatory requirements [1]. The U.S. Food and Drug Administration (FDA) recognizes TPPs as valuable tools for structuring development discussions.
Key TPP components typically include [1]:
- Indications and Usage: Primary therapeutic applications
- Target Population: Specific patient demographics and characteristics
- Dosage and Administration: Treatment duration, delivery mode, and dose regimen
- Clinical Efficacy: Performance metrics and endpoints
- Safety Profile: Adverse reactions and risk-benefit considerations
- Product Specifications: Dosage forms, strengths, stability, and storage requirements
TPPs should be living documents that evolve throughout the development lifecycle, incorporating new data from clinical studies, regulatory feedback, and market changes to inform development decisions [1].
Competitive Intelligence and Landscape Analysis
Competitive intelligence involves the systematic gathering and analysis of information about competitors, markets, and future trends to anticipate moves and proactively plan strategies [36]. In pharmaceutical development, this encompasses several analytical dimensions:
- Market Analysis: Understanding company positioning within therapeutic areas
- Economic-Financial Analysis: Assessing competitors' economic health through public financial data
- Technological Analysis: Monitoring emerging technologies and innovations through patents and scientific literature [36]
- Clinical Development Analysis: Tracking competitors' pipeline assets and development progress
Competitive landscape analysis provides a point-in-time snapshot of the competitive environment, identifying both direct and indirect competitors while analyzing their market positions, strategies, strengths, and weaknesses [37]. This analysis moves beyond simple feature comparisons to understand the broader competitive context in which a product will launch.
Methodological Framework for Integration
Establishing the TPP Foundation Through Internal Assessment
Before engaging in external competitive analysis, research teams must first establish a comprehensive understanding of their own product's strategic positioning. This internal assessment forms the baseline against which competitive factors will be evaluated.
Key internal assessment components include [37]:
- Target Product Profile Core Elements: Documenting the preliminary TPP with minimum acceptable and ideal target profiles for each parameter [1]
- Development Capabilities Assessment: Evaluating internal R&D strengths, limitations, and resource constraints
- Strategic Objectives: Defining commercial goals, target market share, and positioning strategy
- Key Value Propositions: Identifying potential differentiated features and benefits from clinical and patient perspectives
This internal alignment ensures that competitive intelligence gathering remains focused on strategically relevant dimensions rather than becoming an undirected data collection exercise.
Competitive Landscape Mapping Methodology
A comprehensive competitive landscape analysis follows a structured approach to identify and categorize competitive threats across multiple dimensions relevant to pharmaceutical development.
Table: Competitive Categorization Framework for Pharmaceutical Products
| Competitor Type | Identification Methods | Impact Assessment | Strategic Implications |
|---|---|---|---|
| Direct Competitors | CRM data analysis, clinical trial registry review, conference proceedings | High - Compete for same patient population with similar mechanisms | Requires clear differentiation in TPP efficacy, safety, or administration parameters |
| Indirect Competitors | Win-loss interviews, churn analysis, treatment guideline review | Medium - Address same condition with different approaches | TPP should highlight advantages over alternative treatment paradigms |
| Emerging Threats | Patent monitoring, scientific publication tracking, investor presentations | Variable - May disrupt current standard of care | TPP may need to accommodate future market expectations and technological shifts |
| Adjacent Market Players | Pipeline analysis, company acquisition tracking, platform technology assessment | Long-term - Potential for expansion into therapeutic area | TPP should consider potential future competitive landscapes |
The process for comprehensive competitor identification includes [37]:
- Direct Competitor Identification: Analyzing CRM data to identify competitors appearing in early-stage discussions and clinical trial registries for similar therapeutic approaches [37]
- Indirect Competitor Identification: Conducting win-loss analysis and cannulation studies to understand why treatments are selected over others and what alternatives are considered [37]
- Emerging Threat Detection: Implementing systematic patent monitoring and scientific publication surveillance to identify novel technologies and early-stage developments [36]
- Adjacent Market Analysis: Evaluating companies with platform technologies or related therapeutic expertise that could expand into the target indication
Analytical Integration into TPP Development
The integration of competitive intelligence into TPP development occurs through systematic analysis of how competitive factors influence each TPP parameter. This ensures the final TPP represents a strategically informed balance between clinical needs, technical feasibility, and competitive differentiation.
Table: TPP Competitive Benchmarking Framework
| TPP Parameter | Competitive Benchmarking | Minimum Acceptable Profile | Ideal Target Profile | Competitive Differentiation |
|---|---|---|---|---|
| Primary Indication | Current standard of care indications | Mitigation of primary symptoms | Disease modification | Broader label or first-in-class mechanism |
| Target Population | Competitors' approved populations | Adults meeting diagnostic criteria | Including treatment-resistant subgroups | Larger addressable population or unmet need |
| Clinical Efficacy | Competitors' clinical data and labels | Non-inferiority to standard of care | Superior efficacy on key endpoints | Clinically meaningful improvement on primary endpoint |
| Dosage Regimen | Current administration requirements | Once daily oral dosing | Once weekly with reduced side effects | Significant improvement in convenience or adherence |
| Safety Profile | Competitors' black box warnings and contraindications | Manageable side effect profile | Cleaner safety than established therapies | Improved risk-benefit for vulnerable populations |
| Storage & Stability | Current cold chain requirements | Standard refrigeration | Room temperature stability | Distribution advantage in resource-limited settings |
This structured approach enables research teams to make evidence-based decisions when setting TPP parameters, ensuring the target profile represents a commercially viable and clinically differentiated product.
Technical Protocols for Competitive Intelligence
Patent Analysis Protocol
Objective: Systematically identify and analyze patent literature to anticipate competitive technological developments and freedom-to-operate considerations.
Materials:
- Patent database access (USPTO, EPO, WIPO)
- Patent analysis software or competitive intelligence platforms [36]
- Scientific literature databases (PubMed, Embase)
Methodology:
- Search Strategy Development
- Define search terms based on mechanism of action, therapeutic area, and key technological approaches
- Establish inclusion/exclusion criteria for relevant patent families
- Implement iterative search refinement based on initial results
Competitive Technological Analysis
- Identify assignees and analyze patent portfolios by company
- Map technological trajectories and innovation trends
- Assess strength and breadth of patent protection
- Estimate timeline to potential commercialization based on patent filing dates [36]
Strategic Integration
- Identify potential partnership opportunities based on complementary IP
- Highlight freedom-to-operate risks requiring design-around strategies
- Inform TPP development with emerging technological capabilities
Patents provide a forward-looking perspective, showcasing not only currently available technologies but also those that might be commercialized within a 3-5 year timeframe [36]. This predictive capability makes patent analysis particularly valuable for products in early development that will enter future competitive environments.
Clinical Development Landscape Analysis Protocol
Objective: Comprehensively map the clinical development landscape for a therapeutic area to contextualize TPP development parameters and timelines.
Materials:
- Clinical trial registries (ClinicalTrials.gov, EU Clinical Trials Register)
- Investor presentations and company pipeline updates
- Scientific conference proceedings and abstracts
- Regulatory database access
Methodology:
- Landscape Scoping
- Define therapeutic area and relevant mechanisms of action
- Identify companies with active development programs
- Categorize development candidates by phase and mechanism
Data Extraction and Organization
- Extract trial design elements, endpoints, and inclusion criteria
- Document reported efficacy and safety outcomes
- Track development timelines and regulatory interactions
Gap Analysis and Strategic Positioning
- Identify unmet needs and underserved patient populations
- Evaluate competitive efficacy and safety benchmarks
- Determine optimal positioning within treatment algorithms
This protocol enables evidence-based TPP parameter setting by establishing current competitive benchmarks and identifying opportunities for differentiation across clinical, regulatory, and commercial dimensions.
Data Visualization and Analysis Tools
Competitive Landscape Mapping Visualization
Effective visualization of competitive landscapes enables research teams to quickly comprehend complex market dynamics and communicate strategic insights to stakeholders.
Competitive Landscape Mapping
TPP Development Integration Workflow
The process of integrating competitive intelligence into TPP development follows a systematic workflow that transforms raw data into strategic insights.
TPP Development Integration Workflow
Table: Competitive Intelligence Research Toolkit
| Resource Category | Specific Resources | Application in TPP Development | Strategic Value |
|---|---|---|---|
| Patent Databases | USPTO, EPO, WIPO, commercial patent platforms | Monitoring competitor R&D directions and technological developments | Forward-looking view of competitive landscape (3-5 year horizon) [36] |
| Clinical Trial Registries | ClinicalTrials.gov, EU Clinical Trials Register | Tracking competitor development progress and trial design choices | Understanding efficacy benchmarks and development timelines |
| Scientific Literature Databases | PubMed, Embase, Web of Science | Accessing published clinical results and preclinical research | Evidence-based parameter setting for efficacy and safety profiles |
| Financial & Business Databases | SEC filings, investor presentations, annual reports | Assessing competitor resources and strategic priorities | Understanding competitive capacity and commitment to therapeutic area |
| Competitive Intelligence Platforms | Klue, Crayon, similar platforms | Aggregating and analyzing competitive data [37] | Efficient monitoring and analysis of multiple competitive dimensions |
| Protocol Repositories | Nature Protocols, Journal of Visualized Experiments, Springer Protocols [38] | Accessing established methodological approaches | Ensuring competitive benchmarking uses standardized methodologies |
Case Study Application: TB Diagnostic Development
The World Health Organization's approach to developing Target Product Profiles for tuberculosis screening tests demonstrates the practical application of competitive landscape analysis in TPP development [39]. The WHO TPP development process incorporated:
- Comprehensive Technology Assessment: Evaluation of existing and emerging screening technologies, including ultra-portable digital radiographic equipment and AI-powered interpretation software [39]
- Stakeholder Engagement: Extensive consultation with manufacturers, researchers, and healthcare providers to understand technological capabilities and clinical needs [39]
- Product-Agnostic Specifications: Development of performance characteristics that encompass all possible technological approaches rather than prescribing specific solutions [39]
This approach resulted in TPPs that spurred development of novel tools while accommodating rapid technological advancements in the screening landscape, demonstrating how integrated competitive and technological analysis can drive strategic product development.
The integration of competitive intelligence and landscape analysis into Target Product Profile development represents a strategic imperative in modern pharmaceutical development. This integrated approach ensures that TPPs balance clinical needs with market realities, creating development blueprints for products that are not only scientifically sound and clinically valuable but also commercially viable and competitively differentiated.
The methodologies and protocols outlined provide a framework for systematic competitive assessment and strategic integration, enabling research teams to make evidence-based decisions throughout the development lifecycle. By adopting these practices, organizations can enhance development efficiency, improve resource allocation, and increase the likelihood of regulatory and commercial success in an increasingly competitive healthcare landscape.
Maintaining TPP Relevance Through Iterative Updates
Within the broader context of Target Product Profile (TPP) research, maintaining document relevance through strategic iterative updates represents a critical success factor in modern drug development. A TPP serves as a strategic planning tool that outlines the desired characteristics of a medical product, including its intended use, target population, and key performance features, ensuring alignment with clinical needs and regulatory requirements [1]. This technical guide examines the imperative for dynamic TPP management, provides evidence-based methodologies for implementing iterative updates, and presents structured frameworks for maintaining TPP relevance throughout the product development lifecycle. By adopting a systematic approach to TPP iteration, development teams can enhance decision-making, minimize risks, and increase the likelihood of successful product approval and adoption in an evolving therapeutic landscape.
Defining the Target Product Profile
A Target Product Profile (TPP) is a strategic development tool that indicates the characteristics required in a product to meet a particular health need [40]. Fundamentally, a TPP outlines both minimal and optimal characteristics across multiple dimensions, serving as a strategic blueprint that outlines the key objectives a drug must meet to gain regulatory approval and reach patients [3]. This living document typically includes minimum viable criteria for approval, base case expectations for performance, and aspirational goals that define true success, providing clarity and direction throughout the development process [3].
The utility of TPPs changes significantly as a product progresses through development stages. In early-stage development, TPPs help navigate high uncertainty and establish foundational goals, while in late-stage development, they become more refined, integrating robust data and commercial projections [3]. This evolution underscores the fundamental necessity of treating TPPs as dynamic documents rather than static artifacts, requiring planned iteration to maintain strategic relevance as new data emerges and market conditions shift.
The Case for Iterative Updates
Traditional approaches to TPP development often suffer from rigidity that can stifle innovation and limit adaptability. Critics argue that singular, static TPPs tend to be designed from the organization's point of view rather than from the market in, failing to describe the target the product needs to hit to be commercially successful [41]. Furthermore, when TPPs are constantly updated without a structured approach, they risk becoming a constantly shifting goalpost or simply a description of the drug's current state rather than a true target to aim for [41].
A well-structured iterative process addresses these limitations by incorporating mechanisms for incorporating new data, stakeholder feedback, and market changes while maintaining strategic alignment. By adopting a dynamic approach to TPP management, development teams can better navigate the shifting scrutiny on certain therapeutic areas and anticipate what approval requirements might look like five to seven years in the future [3]. This proactive stance toward TPP maintenance represents a significant competitive advantage in an industry characterized by long development timelines and evolving regulatory standards.
Methodologies for Strategic TPP Iteration
Establishing the Iterative Framework
Implementing a successful TPP iteration process requires a structured methodology with clearly defined triggers, stakeholders, and decision gates. The foundational principle involves treating TPP development as a collaborative and consensus-based approach that explicitly considers the needs and preferences of end users, such as program managers and patients, as well as subject-specific experts [40]. This approach ensures that iterations incorporate diverse perspectives rather than reflecting isolated organizational priorities.
The iteration cycle should be governed by predetermined criteria that trigger formal review, including: (1) completion of major development milestones (e.g., Phase 1, 2, 3 trial results), (2) significant changes in the competitive landscape, (3) emerging regulatory guidance or precedent, (4) new patient preference data, and (5) substantive shifts in standard of care. At each review point, the core question remains whether the current TPP still represents a viable path to regulatory approval and commercial success given available information.
Table 1: TPP Iteration Triggers and Response Protocols
| Trigger Category | Specific Triggers | Recommended Response Protocol | Key Stakeholders for Review |
|---|---|---|---|
| Clinical Development Milestones | Completion of Phase 1, 2, 3 trials; New safety or efficacy data | Formal assessment of assumptions vs. results; Gap analysis | Clinical development, Biostatistics, Regulatory affairs |
| Competitive Landscape Shifts | New product approvals; Emerging clinical data on competitor products; Patent expirations | Comparative efficacy assessment; Market positioning review | Commercial strategy, Competitive intelligence, Medical affairs |
| Regulatory Environment Changes | New FDA guidance; Precedent decisions on similar products; Changes in regulatory standards | Impact assessment on development pathway; Labeling implications | Regulatory affairs, Quality assurance, Legal |
| Market & Access Evolution | Payer requirement changes; Healthcare policy shifts; Patient preference data | Target product profile adjustment; Value proposition refinement | Market access, Patient advocacy, Health economics |
Multi-TPP Approach for Strategic Flexibility
Rather than relying on a single TPP, leading organizations are adopting a multi-TPP approach that generates several prototypes, each representing a different potential development path for the drug [41]. These parallel TPPs encompass various indications, patient populations, formulations, and commercial strategies, creating a strategic portfolio of development options. This approach allows for comparative analysis, informed decision-making, and the ability to adapt to new information and insights throughout the development process [41].
The methodology for developing multiple TPP prototypes involves structured scenario planning that identifies critical uncertainties and maps them to potential development pathways. For each scenario, a dedicated TPP articulates the specific characteristics required for success under those conditions. This approach transforms the TPP from a singular hypothesis into a tested strategic framework, with clinical data used to validate or invalidate each potential path rather than simply progressing a predetermined development plan.
Multi-TPP Strategic Development Framework
Draft Label as an Iterative Tool
An emerging methodology involves using the draft label as an alternative or complement to the traditional TPP, creating a more concrete and commercially-oriented perspective [41]. The draft label serves as a tangible representation of the intended product claims and provides a clearer framework for development, effectively acting as a contract between departments that outlines the necessary studies, patient populations, and data required to achieve the desired product claims [41].
This approach offers distinct advantages for iterative management, as label language inherently requires precision and reflects the ultimate regulatory communication about a product's capabilities. By iterating on the draft label throughout development, teams maintain focus on the evidence required to support specific claims rather than abstract performance targets. This methodology also fosters cross-functional alignment, as the draft label explicitly defines what each department must deliver to achieve the desired product profile.
Data Integration and Analysis for Informed Iteration
Analytical Frameworks for TPP Refinement
Strategic TPP iteration requires systematic data integration from multiple sources to inform refinement decisions. ProteomicsDB's PTMNavigator represents an advanced analytical framework that enables researchers to overlay experimental data with pathway diagrams, providing approximately 3000 canonical pathways from manually curated databases [42]. This type of tool exemplifies the sophisticated analytical capabilities necessary for data-driven TPP refinement, allowing development teams to visualize how drug treatments result in a discernable flow of PTM-driven signaling and aid in proposing extensions to existing pathways [42].
The analytical process should incorporate both quantitative and qualitative data streams, including: (1) clinical results against predetermined endpoints, (2) competitive intelligence on recently approved products, (3) regulatory precedent decisions, (4) patient preference and usability data, and (5) commercial access considerations. Each data stream should have defined metrics and thresholds that trigger TPP review when variances exceed acceptable ranges.
Table 2: TPP Iteration Decision Matrix Based on Clinical Data
| Data Type | Analytical Method | Threshold for Minor TPP Refinement | Threshold for Major TPP Pivot | Recommended Action |
|---|---|---|---|---|
| Primary Efficacy Endpoint | Statistical comparison to TPP target | 10-20% variance from TPP target | >20% variance from TPP target | Revise efficacy thresholds; Consider new clinical trials |
| Safety Profile | Adverse event incidence vs. TPP limits | New low-frequency non-serious AE | New serious AE or high-frequency moderate AE | Modify risk-benefit assessment; Adjust safety specifications |
| Dosing & Administration | Comparative bioavailability; User testing | Alternative dosing schedule with equivalent efficacy | Significant administration challenges affecting adherence | Reformulate product; Redesign delivery system |
| Commercial Viability | Cost-of-goods analysis; Payer research | 10-15% higher cost than TPP target | >25% higher cost than TPP target | Process optimization; Identify alternative manufacturing |
Cross-Functional Data Integration
Effective TPP iteration requires integrated data analysis across traditionally siloed functions. Large pharma organizations often led TPP development primarily through commercial teams, but the industry is shifting toward a more integrated approach where development and commercial teams collaborate throughout the lifecycle [3]. This ensures that TPPs remain dynamic and relevant by incorporating diverse perspectives and data sources.
The methodology for cross-functional data integration should include regular interdisciplinary review sessions with standardized data presentation formats that enable apples-to-apples comparison across domains. Clinical data should be presented alongside commercial implications, manufacturing constraints considered alongside clinical preferences, and regulatory requirements evaluated in the context of patient needs. This integrated analysis reveals connections and trade-offs that might be missed in functional silos, leading to more robust TPP iterations.
Cross-Functional Data Integration for TPP Iteration
Implementation Protocol for Iterative TPP Management
Stakeholder Engagement and Governance
Successful implementation of iterative TPP management requires formal governance structures and stakeholder engagement protocols. The World Health Organization emphasizes that developing effective TPPs involves a collaborative and consensus-based approach that explicitly considers the needs and preferences of end users, such as program managers and patients, as well as subject-specific experts [40]. This engagement must be systematic rather than ad hoc, with clearly defined roles and responsibilities throughout the iteration process.
The recommended governance structure includes a cross-functional TPP steering committee with representation from clinical development, regulatory affairs, commercial strategy, manufacturing, and market access. This committee should meet quarterly to review TPP performance indicators and determine whether formal iteration is required. Additionally, the protocol should include mechanisms for gathering external stakeholder input, including key opinion leaders, patient advocates, and payers, with their feedback systematically incorporated into TPP refinement decisions.
Change Control and Version Management
As TPPs evolve through iterative updates, rigorous change control and version management become essential to maintain organizational alignment and regulatory integrity. Each TPP version should include documented rationale for changes, supporting data driving modifications, and assessment of impact on development plans and resource allocation. This disciplined approach prevents the TPP from becoming a constantly shifting goalpost that undermines development stability [41].
The change control protocol should require impact assessment across multiple dimensions: (1) clinical development plan adjustments, (2) regulatory strategy implications, (3) manufacturing and supply chain considerations, (4) commercial positioning changes, and (5) resource allocation consequences. Each iteration should be treated as a formal decision point with clear criteria for progression rather than a continuous adjustment, maintaining the TPP's role as a strategic anchor while allowing necessary evolution.
Table 3: TPP Version Control and Change Management Protocol
| Version Attribute | Documentation Requirement | Approval Workflow | Communication Protocol |
|---|---|---|---|
| Major Version Update | Comprehensive business case with data package; Impact assessment across all functions | Steering committee review; Executive leadership approval | All development functions; Investor relations (if public); Regulatory agencies (as required) |
| Minor Version Update | Summary of changes and rationale; Limited impact assessment | TPP owner approval; Functional head concurrence | Affected functions only; Development team notification |
| Administrative Update | Document of changes for clarity; No substantive impact | TPP owner approval | Development team notification; Document control system update |
| Competitive Response Update | Competitive intelligence assessment; Strategic response rationale | Commercial leadership approval; TPP steering committee review | Commercial and clinical functions; Market access team |
Implementing effective TPP iteration requires specialized tools and resources that enable data-driven decision making and strategic analysis. The following table details key research reagent solutions and methodological frameworks essential for maintaining TPP relevance throughout the development lifecycle.
Table 4: Essential Research Reagent Solutions for TPP Development
| Tool/Resource | Function in TPP Development | Application in Iterative Updates | Access Source |
|---|---|---|---|
| PTMNavigator | Interactive visualization of differentially regulated post-translational modifications in cellular signaling pathways [42] | Enables projection of PTM perturbation datasets onto pathway diagrams to trace signaling cascades and identify pivotal PTMs | ProteomicsDB platform (www.proteomicsdb.org/analytics/ptmNavigator) |
| Pathway Databases | Repository of ~3000 canonical pathways from KEGG and WikiPathways for pathway-centric analysis [42] | Provides contextual framework for interpreting experimental results against biological pathways during TPP refinement | KEGG, WikiPathways, and internal ProteomicsDB representations |
| Draft Label Framework | Alternative to traditional TPP that provides more concrete, commercially-oriented development target [41] | Serves as iterative tool that fosters cross-functional alignment and maintains focus on evidence required for specific claims | Internal development based on regulatory precedent |
| Multi-TPP Scenario Platform | Framework for developing multiple TPP prototypes representing different development paths [41] | Enables comparative analysis of development options and facilitates strategic pivots based on emerging data | Internal strategic planning process |
| Stakeholder Engagement Protocol | Structured methodology for gathering and incorporating feedback from patients, physicians, and payers [40] [41] | Ensures TPP iterations reflect evolving market needs and user preferences rather than solely internal perspectives | WHO TPP development guidelines and customer insight frameworks |
In an era of increasing disruption and uncertainty in drug development, maintaining TPP relevance through systematic iterative updates represents a critical competency for research organizations. By implementing structured methodologies for TPP iteration, development teams can enhance strategic alignment, respond to evolving data and market conditions, and increase the likelihood of regulatory and commercial success. The frameworks presented in this technical guide provide actionable approaches for treating TPPs as dynamic strategic tools rather than static documents, enabling organizations to navigate complexity while maintaining development focus. As the pharmaceutical landscape continues to evolve, the ability to effectively iterate TPPs will increasingly distinguish successful development programs from those that struggle to adapt.
Standardization Gaps in TPP Development and Reporting
A Target Product Profile (TPP) is a strategic planning tool that outlines the desired characteristics of a medical product, ensuring that research and development (R&D) efforts align with specific clinical needs and regulatory requirements [1]. Originally conceptualized in 1997 through FDA discussions, the TPP embodies the principle of "beginning with the goal in mind" [17] [11]. It serves as a strategic framework, a detailed regulatory document, a technical dossier, and a due diligence tool for investors and partners [11]. By defining attributes such as intended use, target population, key performance features, safety, efficacy, and affordability early in development, a TPP fosters stakeholder alignment, facilitates efficient resource allocation, and increases the likelihood of regulatory and commercial success [1].
The value of a well-constructed TPP is demonstrated by tangible outcomes. Data show that new drug applications (NDAs) which referenced a TPP had a median review time 30 days shorter than those that did not. Furthermore, nearly 5% of NDAs approved between 2008 and 2015 that lacked a formal TPP received an initial refuse-to-file notification, compared to none that referenced a TPP [11]. Despite their proven utility, the development and reporting of TPPs face significant standardization gaps, which this guide will explore in detail.
Core Components of a Target Product Profile
A comprehensive TPP outlines essential product characteristics across multiple dimensions. The following table summarizes the key components, informed by the FDA's guidance and illustrated with examples from the National Institute on Drug Abuse (NIDA) [1].
Table 1: Core Components of a Target Product Profile for a Pharmacotherapeutic
| Drug Label Attribute | Product Property | Minimum Acceptable Results | Ideal Results |
|---|---|---|---|
| Indications and Usage | Primary Indication | (e.g., Mitigation of opioid withdrawal symptoms) | (e.g., Broader indication for opioid use disorder management) |
| Indications and Usage; Clinical Studies | Target Population | (e.g., Adults with specific diagnosis) | (e.g., Wider population including adolescents) |
| Dosage and Administration | Treatment Duration, Delivery Mode, Dose Regimen | (e.g., Up to 14 days, Oral, Four times daily) | (e.g., Single injection, Longer duration) |
| Dosage Forms and Strengths | Dose Form | (e.g., 0.18mg tablet) | (e.g., Multiple strengths, Liquid formulation) |
| Clinical Studies | Clinical Efficacy | (e.g., Statistically significant improvement vs. placebo on primary endpoint) | (e.g., Superior efficacy versus standard of care) |
| Adverse Reactions | Risk/Side Effect Profile | (e.g., Acceptable, manageable side effects) | (e.g., Superior safety profile versus standard of care) |
| How Supplied, Storage and Handling | Product Stability and Storage | (e.g., Stable at room temperature for 1 year) | (e.g., Stable at extreme temperatures for longer shelf life) |
| Clinical Pharmacology | Mechanism of Action, Pharmacokinetics | (e.g., Defined mechanism, predictable PK) | (e.g., Novel mechanism, once-daily dosing) |
| Drug Interactions | Drug Interactions | (e.g., No major contraindications) | (e.g., No known interactions) |
| (Not from label) | Affordability (Price) | (e.g., Cost not exceeding X) | (e.g., Lower cost than standard of care) |
| (Not from label) | Accessibility | (e.g., Prescription use) | (e.g., Over-the-counter availability) |
This structured format ensures that all critical attributes are considered from the outset of development. The TPP is not static; it should be a "living document," continuously evolving with emerging data and insights [1]. This iterative nature is key to its effectiveness but also presents challenges for standardization.
Identifying Standardization Gaps in TPP Processes
The absence of universally accepted standards for TPP development and reporting leads to significant inconsistencies, reducing the tool's effectiveness and hindering collaboration. These gaps span methodological, stakeholder engagement, and reporting dimensions.
Methodological and Structural Gaps
A fundamental gap is the lack of a standardized structural framework. While core elements like indication and efficacy are commonly included, the depth and specificity of these sections vary widely. There is no consensus on mandatory versus optional fields, leading to TPPs of vastly different scopes and qualities [1] [43]. Furthermore, the definition of "minimum acceptable" versus "ideal" targets is often subjective. Without standardized criteria for these thresholds, TPPs can be easily manipulated to make a development program appear more viable than it is, undermining their value as a strategic and decision-making tool [1].
Stakeholder Engagement and Input Gaps
Perhaps the most critical gap is the inconsistent integration of the patient perspective. Patients are the experts on their own disease, yet a 2019 survey found that only two of eleven pharmaceutical companies engaged patient representatives in TPP development [17]. This represents a major missed opportunity to align product profiles with what patients truly value, such as route of administration, dosing frequency, and benefit-risk trade-offs. The methodology for gathering this input is also non-standardized, with varying use of tools like desk research, patient advisory boards, and focus groups [17]. This lack of a formal process for incorporating insights from payers and providers further limits the TPP's utility in forecasting market access and adoption [11].
Reporting and Implementation Gaps
In the regulatory context, the use of TPPs is inconsistent across different agencies and regions. The tool, while promoted by the FDA, is not commonly used in European regulatory contexts, creating a challenge for global development programs [43]. This inconsistency extends to the public health domain, where organizations like the WHO and non-profits like DNDi develop their own TPPs, which are not always well-aligned, creating potential confusion for developers [2]. Finally, a significant implementation gap exists in academia, where the "backwards" thinking of basic research often prevails over the "forwards" thinking required for efficient translation, contributing to an attrition rate greater than 90% [43].
The relationships between these gaps, the stakeholders involved, and the potential consequences are complex. The following diagram maps this landscape to illustrate the systemic nature of the standardization challenge.
Figure 1: Landscape of Standardization Gaps in TPP Development and Reporting. This diagram visualizes the key categories of gaps and their downstream consequences on product development.
Methodological Framework for Standardized TPP Development
To address the identified gaps, a systematic and standardized methodology is essential. The following workflow provides a structured, multi-phase approach to TPP development that integrates critical stakeholder input and maintains the TPP as a living document.
TPP Development Workflow
A standardized development process ensures consistency and comprehensiveness. The following diagram outlines a recommended workflow, from initial conceptualization through to final regulatory submission and lifecycle management.
Figure 2: Standardized Workflow for TPP Development and Lifecycle Management. This process emphasizes stakeholder engagement and iterative updates.
Integrating Patient Perspectives: A Standardized Protocol
Given its importance, the process for integrating patient input must be particularly rigorous. The following table details a standardized protocol for obtaining and incorporating patient experience data into the five key TPP focus areas where patient perspectives are fundamental [17].
Table 2: Protocol for Integrating Patient Input into TPP Development
| Focus Area | Key Questions for Patients | Recommended Engagement Tool | Output for TPP |
|---|---|---|---|
| Target Population | How is your disease experienced? What sub-groups are most in need? | Desk Research (FDA Voice of the Patient reports, social listening) | Refined patient segmentation and inclusion criteria. |
| Unmet Need & Therapy Aims | What are the most burdensome symptoms? What does a "good day" look like? | Focus Groups / In-depth Interviews | Prioritized list of clinical outcomes and quality of life goals. |
| Efficacy Endpoints | Are the proposed clinical trial endpoints meaningful to you? | Patient Advisory Boards / Cognitive Debriefing | Validated Clinical Outcome Assessments (COAs) and patient-relevant endpoints. |
| Dosage & Administration | What is the maximum tolerable dosing frequency? Preferred route (oral, injection, etc.)? | Quantitative Surveys / Discrete Choice Experiments | Target product profile for formulation, dosing frequency, and route of administration. |
| Benefit-Risk Trade-offs | What level of side effect is acceptable for a given efficacy benefit? | Patient Preference Studies | A quantified benefit-risk threshold to guide development and regulatory discussions. |
Execution Guidelines:
- Timeline: This process should begin in the preclinical phase and be iterated at key development milestones [17].
- Materials: Use clear, accessible language and provide adequate background context to patient representatives to facilitate productive discussions [17].
- Stakeholder Engagement: The process should be collaborative ("working with patients"), respectful of patient expertise, and managed by dedicated patient engagement professionals [17].
The Researcher's Toolkit: Essential Reagents for TPP Development
Developing a robust TPP requires leveraging specific analytical tools and data sources. The following table functions as a "researcher's toolkit," detailing essential resources for constructing a evidence-based TPP.
Table 3: Research Reagent Solutions for TPP Development
| Tool / Resource | Function in TPP Development | Source / Example |
|---|---|---|
| FDA Drug Labels | Provides the definitive structure and content requirements for the final product definition, serving as a template for the TPP. | FDA Purple Book or DailyMed [1] |
| Competitor Product Analysis | Informs the minimum acceptable and ideal targets by benchmarking against existing standard of care. | e.g., Using Lucemyra (lofexidine) as a benchmark for an opioid withdrawal therapy [1] |
| FDA Clinical Outcome Assessment (COA) Compendium | Identifies validated endpoints and patient-reported outcome (PRO) instruments that are acceptable to regulators. | FDA Website [17] |
| COMET Initiative Database | Provides access to Core Outcome Sets, which are standardized sets of outcomes that should be measured in clinical trials for a specific disease. | COMET Initiative Website [17] |
| WHO TPPs & PPCs | Informs public health priorities and desired product characteristics for diseases of global health importance. | WHO Global Observatory on Health R&D [2] |
| Health Technology Assessment (HTA) Body Reports | Provides insight into the evidence requirements and economic evaluation criteria of payers. | e.g., NICE (UK), IQWiG (Germany) [17] |
Addressing the standardization gaps in TPP development and reporting is not an academic exercise; it is a practical imperative for enhancing the efficiency and success rate of medical product development. The high attrition rate in translational research—exceeding 90%—can be mitigated by adopting the structured, forward-thinking approach that a well-constructed TPP facilitates [43]. The frameworks, protocols, and toolkits presented in this guide provide a roadmap for researchers and developers to create more robust, patient-centric, and commercially viable TPPs. By standardizing the processes for defining "minimum" and "ideal" targets, systematically integrating patient and payer perspectives, and maintaining the TPP as a dynamic, living document, organizations can de-risk development, accelerate regulatory approval, and ultimately increase the likelihood that new products will successfully meet the needs of patients and healthcare systems.
Strategies for Effective TPP Governance and Version Control
A Target Product Profile (TPP) is a strategic planning tool that outlines the desired characteristics of a target product, including its intended use, target populations, and key safety and efficacy-related characteristics [2]. It serves as a foundational document that guides drug development from discovery through regulatory approval and commercialization. Effective TPP governance establishes the framework of policies, procedures, and responsibilities for creating, maintaining, and approving TPPs throughout the product lifecycle. Simultaneously, systematic version control manages changes to this critical document, ensuring traceability, maintaining alignment across stakeholders, and supporting regulatory compliance. For researchers and drug development professionals, implementing robust strategies in these areas is essential for maintaining development efficiency, reducing costly missteps, and achieving strategic alignment across multidisciplinary teams.
Establishing a TPP Governance Framework
Core Governance Structure and Responsibilities
A robust TPP governance framework requires clearly defined structures and roles to ensure systematic development and oversight. The governance body should represent all critical functions involved in product development, creating a cross-functional team that can make informed decisions balancing scientific, regulatory, and commercial considerations [44] [17].
Table: Key Roles and Responsibilities in TPP Governance
| Role/Function | Primary Governance Responsibilities |
|---|---|
| Clinical Development | Leads TPP creation and updates; provides scientific and medical expertise on trial design and endpoints [44]. |
| Regulatory Affairs | Ensures TPP alignment with regulatory requirements and agency expectations; advises on approval pathways [3]. |
| Patient Engagement | Incorporates patient perspective on endpoints, burden of disease, and benefit-risk trade-offs [17]. |
| Commercial/Market Access | Defines target product characteristics needed for commercial success, reimbursement, and market differentiation [3]. |
| Governance Chair | Facilitates cross-functional alignment; manages TPP review and approval cycles; resolves conflicts. |
TPP Development and Review Lifecycle
The TPP is a dynamic document that evolves throughout the drug development lifecycle, with governance ensuring it remains relevant and aligned with emerging data and changing market conditions [3]. A phased approach to TPP development mirrors the drug development continuum, with specific objectives at each stage.
- Preclinical Phase: Initial TPP creation focuses on defining the minimum viable criteria for approval, based on understanding of disease area, unmet patient needs, and competitive landscape [3]. The governance team establishes core product attributes and identifies key uncertainties.
- Early Clinical Development: TPP refinement incorporates early human data, with updates focusing on base case expectations for product performance [3]. Patient engagement becomes critical at this stage to validate assumptions about target population, dosage frequency, and route of administration [17].
- Late-Stage Development: The TPP becomes more refined, integrating robust clinical data and detailed commercial projections [3]. Governance focus shifts to aspirational goals that define true product differentiation and success, while ensuring alignment with regulatory strategy.
The governance process should establish regular review milestones, with formal change control procedures to manage updates. These "tollgates" in a medicine's lifecycle ensure the patient perspective and other critical inputs are systematically integrated into TPP updates [17].
Diagram: TPP Development and Governance Lifecycle. This workflow illustrates the evolution of the TPP through development phases, with governance oversight and version control managing changes.
Version Control Implementation for TPPs
Version Control Strategies and Methodologies
Implementing systematic version control for TPPs requires selecting appropriate strategies that balance traceability with practical usability. While TPPs themselves are documents rather than software code, the principles of version control systems (VCS) used in software development can be effectively adapted for managing TPP revisions throughout their lifecycle [45].
Table: Version Control Strategies Adapted for TPP Management
| Strategy | Implementation for TPPs | Advantages | Disadvantages |
|---|---|---|---|
| URL/Path Versioning | Store different TPP versions in separate, clearly labeled folders or paths (e.g., /TPP/v1.0/, /TPP/v2.0/) [46]. |
High visibility of version in path; simple to understand and implement. | Can lead to repository clutter; requires manual organization. |
| Metadata Tagging | Use descriptive tags to mark commits as important (e.g., "v1.0-Regulatory-Submission") [45]. | Enables quick identification of significant versions; flexible implementation. | Relies on consistent tagging practices across team members. |
| Branching for Major Revisions | Create branches for significant TPP updates while maintaining stable main branch [45]. | Allows parallel development of major revisions; maintains stable version. | Adds complexity; requires clear merging protocols. |
For most organizations, a hybrid approach combining multiple strategies works best for TPP version control. Significant milestones (such as regulatory submissions or major protocol amendments) should be marked with clear tags, while a consistent folder structure maintains organizational clarity. The chosen system should integrate with existing document management platforms and align with organizational quality management systems.
Version Control System Selection and Workflow
Selecting the appropriate version control system for TPP management depends on organizational size, collaboration requirements, and integration needs with existing systems. For most life sciences organizations, distributed version control systems (DVCS) like Git offer significant advantages for managing complex documents like TPPs [45].
- Centralized vs. Distributed Systems: While centralized systems like Subversion (SVN) offer simplicity through a single repository, distributed systems like Git provide greater resilience and offline capability by giving each user a complete copy of the repository [45]. This is particularly valuable for global teams working across time zones.
- Branching Strategies: Implement either trunk-based development with small, frequent integrations to reduce merge conflicts, or GitFlow with multiple long-lived branches for larger teams with complex release cycles [45]. For TPP management, trunk-based development is generally preferred for its simplicity.
- Commit Hygiene: Enforce practices of small, atomic commits with clear messages that document the rationale for TPP changes [45]. This creates an auditable trail of decisions, which is crucial for regulatory compliance and knowledge transfer.
Diagram: TPP Version Control Branching Strategy. This workflow demonstrates how branching enables parallel development of TPP updates while maintaining a stable main version.
Quantitative Assessment of TPP Complexity and Change Impact
Protocol Complexity Tool (PCT) Methodology
The Protocol Complexity Tool (PCT) provides a structured methodology to objectively measure and manage complexity in clinical trial protocols, which directly impacts TPP governance and version control decisions [44]. Developed through a collaborative design process with cross-functional experts, the PCT assesses complexity across five critical domains that influence trial execution and success.
- Development Process: The PCT was developed between June 2021 and December 2022 by a taskforce of 20 cross-functional experts in clinical trial design and execution [44]. Using an agile development approach with five version releases, the tool incorporated over 450 comments to reach consensus.
- Scoring Methodology: The PCT comprises 26 multiple-choice questions across five domains, each scored on a 3-point scale (low complexity=0, medium complexity=0.5, high complexity=1) [44]. Domain scores are averaged, then summed to produce a Total Complexity Score (TCS) between 0 and 5.
- Domain Structure: The five domains assessed are: (1) Study Design, (2) Patient Burden, (3) Site Burden, (4) Regulatory Oversight, and (5) Operational Execution [44]. This comprehensive coverage ensures all aspects of protocol complexity are measured.
Table: PCT Domain Structure and Scoring Methodology
| Domain | Key Assessment Areas | Example Questions | Scoring Impact |
|---|---|---|---|
| Study Design | Endpoints, learning from previous studies, design complexity, sub-studies [44]. | Number of primary/secondary endpoints; validation of study design; analysis complexity. | High complexity in this domain increases operational risk and resource requirements. |
| Patient Burden | Visit frequency, procedures, travel requirements, data reporting [44]. | Frequency of clinic visits; complexity of patient-reported outcomes; procedure burden. | Affects recruitment rates, retention, and data quality. |
| Site Burden | Resource requirements, data management, monitoring intensity [44]. | Staffing requirements; data entry complexity; source data verification needs. | Impacts site activation timelines and overall trial costs. |
| Regulatory Oversight | Reporting requirements, committee oversight, safety monitoring [44]. | Number of regulatory agencies; safety reporting requirements; independent committee oversight. | Increases administrative burden and potential for delays. |
| Operational Execution | Drug supply chain, sample management, vendor coordination [44]. | Complexity of drug supply; sample shipping requirements; number of vendors. | Affects trial implementation timeline and budget. |
Correlation Between Complexity and Trial Performance
Quantitative analysis demonstrates significant correlations between protocol complexity and key trial performance indicators, providing critical data points for TPP governance decisions. Understanding these relationships enables evidence-based simplification of protocols during TPP development and version updates.
- Time-to-Site Activation: Research shows a statistically significant positive correlation between Total Complexity Score and time to reach 75% site activation (rho=0.61; p=0.005; n=19) [44]. Higher complexity protocols require longer setup timelines.
- Participant Enrollment: Similarly, a significant positive correlation exists between TCS and time to reach 25% participant recruitment (rho=0.59; p=0.012; n=17) [44]. More complex protocols enroll more slowly, impacting overall development timelines.
- Impact of PCT Application: Following PCT application and subsequent protocol simplification, the Total Complexity Score was reduced in 75% of trials (12 of 16 assessed), remained the same in 18.8% (3 trials), and increased in only 6.2% (1 trial) [44]. Complexity reduction was most notable in operational execution and site burden domains.
These quantitative relationships provide governance bodies with evidence to support protocol simplification decisions during TPP version updates, balancing scientific objectives with operational feasibility.
Research Reagent Solutions for TPP Development
Table: Essential Tools and Methods for TPP Development and Governance
| Tool/Resource | Function in TPP Process | Application Context |
|---|---|---|
| Protocol Complexity Tool (PCT) | Objectively measures protocol complexity across 5 domains and 26 criteria [44]. | Used during TPP development and updates to identify areas for simplification; supports evidence-based decision making. |
| Patient Advisory Boards/Councils | Structured forums for obtaining patient perspectives on key TPP elements [17]. | Used to validate assumptions about target population, endpoints, and benefit-risk trade-offs; provides qualitative insights. |
| Regulatory Guidance Databases | Source of current regulatory expectations and precedent information [3]. | Informs minimum viable product criteria and regulatory strategy; supports contingency planning. |
| Version Control Systems (e.g., Git) | Manages TPP revisions, branches, and merges; maintains audit trail [45]. | Provides infrastructure for collaborative TPP development; ensures traceability of changes across versions. |
| AI-Assisted Analysis Tools | Extracts insights from scientific literature and generates first-draft TPP templates [3]. | Supports horizon scanning and initial TPP drafting; helps identify shifts in regulatory or therapeutic landscapes. |
Effective TPP governance and version control are not administrative burdens but strategic imperatives in modern drug development. By implementing structured governance frameworks with clear cross-functional responsibilities, establishing systematic version control processes adapted from software development best practices, and utilizing quantitative assessment tools like the Protocol Complexity Tool, organizations can significantly enhance development efficiency and decision-making. These strategies ensure TPPs remain dynamic, evidence-based tools that align with evolving clinical data, regulatory requirements, and patient needs throughout the product lifecycle. As the pharmaceutical landscape grows increasingly complex, robust TPP management practices will continue to grow in importance for delivering successful products that address unmet medical needs.
Benchmarking and Validating TPPs for Regulatory and Commercial Success
In the strategic development of innovative drug and biological products, the Target Product Profile (TPP) serves as a crucial strategic planning tool that outlines the desired characteristics of a target product aimed at a particular disease. Framing development within the context of a TPP is considered a best practice for navigating the complex regulatory landscape of the U.S. Food and Drug Administration (FDA). For developers of novel therapies, particularly in the cell and gene therapy space, early engagement with the FDA through mechanisms like the INitial Targeted Engagement for Regulatory Advice on CBER/CDER ProducTs (INTERACT) meeting provides invaluable non-binding, informal feedback on early development challenges. This guide examines the strategic integration of TPP principles with FDA regulatory procedures, focusing on the operational aspects of INTERACT meetings to de-risk development and align product characteristics with regulatory expectations from the earliest stages.
Understanding Target Product Profiles (TPP) in Regulatory Context
A Target Product Profile (TPP) outlines the desired 'profile' or characteristics of a target product aimed at a particular disease or diseases [2]. TPPs state the intended use, target populations, and other desired attributes of products, including safety and efficacy-related characteristics. In the regulatory context, TPPs are considered as tools to frame development in relation to the submission of product dossiers [2].
The Strategic Role of TPPs in Drug Development
- Strategic Planning Tool: In industry, in-house TPPs are used as planning tools that guide development toward desired characteristics, serving as a strategic compass throughout the product lifecycle [2].
- Public Health Application: In the context of public health, TPPs set Research & Development (R&D) targets for funders and developers. WHO TPPs support the development of missing health products, keeping focus on public health priorities while recognizing that access, equity, and affordability are integral parts of the innovation process [2].
- Regulatory Alignment: A well-constructed TPP facilitates more efficient regulatory interactions by providing a clear framework for discussing development goals and methodologies with regulatory authorities like the FDA.
Table: Types of Target Product Profiles and Their Applications
| TPP Type | Primary Purpose | Key Characteristics | Typical Users |
|---|---|---|---|
| Corporate TPP | Internal strategic planning | Guides development toward commercially viable and technically feasible attributes | Industry sponsors, product developers |
| Regulatory TPP | Regulatory submission framework | Frames development in relation to regulatory requirements | Regulatory affairs professionals, clinical developers |
| WHO TPP | Public health priority setting | Describes preferred and minimally acceptable profiles for vaccines, therapeutics, diagnostics | Public health organizations, funders, non-profit developers |
The INTERACT meeting is a non-binding, informal, early-stage consultation designed to help drug developers navigate regulatory challenges during the pre-Investigational New Drug (pre-IND) phase [47]. The FDA provides targeted feedback on the development of innovative products, particularly those involving complex biologics or advanced manufacturing techniques [47].
Definition and Purpose of INTERACT Meetings
INTERACT (INitial Targeted Engagement for Regulatory Advice on CBER/CDER ProducTs) is a meeting available early in product development for sponsors of biologics, including cell and gene therapies [48] [49]. Unlike traditional Type B pre-IND meetings, INTERACT meetings are not for finalizing IND submissions but rather for resolving early scientific and regulatory uncertainties [47].
Key objectives of INTERACT meetings include [49]:
- Discussing issues critical to early product development
- Obtaining preliminary, informal consultation with CBER prior to a Pre-IND meeting
- Obtaining initial, nonbinding advice regarding CMC, pharmacology/toxicology, and/or clinical aspects of a development program
- Discussing new delivery devices, early product development, and/or pre-clinical proof-of-concept
- Identifying critical development issues or deficiencies to address before significant resources are invested
When to Request an INTERACT Meeting
The appropriate timing for an INTERACT meeting is when a sponsor has identified the investigational product to be evaluated in a clinical study and conducted some preliminary preclinical proof-of-concept studies with the intended investigational product but has not yet designed and conducted definitive toxicology studies [48].
Table: INTERACT Meeting Timing Considerations
| Appropriate Timing | Premature Requests | Overdue Requests |
|---|---|---|
| • Identified investigational product [48]• Preliminary preclinical proof-of-concept studies conducted [48]• Before definitive toxicology studies designed [48]• Early development phase with novel products | • No specified investigational product [48]• No preclinical proof-of-concept data [48]• No preliminary studies with intended clinical product [48] | • Completed proof-of-concept and some safety studies [48]• Ready to design definitive toxicology studies [48]• Defined manufacturing process for clinical studies [48]• Existing clinical data for same product/indication [48] |
INTERACT vs. Pre-IND Meetings: Strategic Applications
Understanding the distinction between INTERACT and Pre-IND meetings is crucial for selecting the appropriate regulatory pathway for early-stage development programs.
Key Distinctions and Strategic Applications
INTERACT Meeting Focus: INTERACT meetings are designed for sponsors with an identified novel product with unique safety profile challenges related to complex manufacturing technologies, innovative devices, or new testing methodologies [49]. The meeting provides a forum to discuss innovative technologies, product manufacturing, reagents, starting materials, critical product components, novel delivery device qualification, and complex software issues [49].
Pre-IND Meeting Focus: Pre-IND meetings are more appropriate for topics that fall under the CBER Advanced Technologies Team (CATT), product selection, previous regulatory advice on a similar product and indication, toxicology study design considerations for IND-enabling studies, and certain clinical study protocol design considerations [49].
Practical Implementation: Preparing for a Successful INTERACT Meeting
INTERACT Meeting Timelines and Requirements
The FDA has established specific timelines and requirements for INTERACT meetings to ensure efficient use of resources for both sponsors and the agency.
Table: INTERACT Meeting Timelines and Key Parameters
| Parameter | Requirement | Details and Considerations |
|---|---|---|
| OTP Response to Meeting Request | 21 calendar days [48] | From FDA receipt to decision to grant/deny |
| Meeting Scheduling | 75 calendar days [48] | From FDA receipt of request to meeting date |
| Meeting Package Submission | With meeting request [48] | Must accompany the initial submission |
| Meeting Length | 60 minutes [48] | Strict time allocation requires careful planning |
| OTP Preliminary Response | No later than 5 days before meeting [48] | Allows sponsor to prepare focused discussion |
| Sponsor Response to Preliminary | Before meeting [48] | Opportunity to identify key discussion points |
| Maximum Questions | 10 questions (inclusive of sub-questions) [48] | Questions must be targeted and specific |
| Package Page Limit | 50 pages [48] | Encourages concise, focused presentation |
INTERACT Meeting Package Content Requirements
A successful INTERACT meeting package must be comprehensive yet concise, providing sufficient background while focusing on specific, targeted questions.
Chemistry, Manufacturing, and Controls (CMC) Content
The CMC section of the INTERACT briefing package should provide [48]:
- A summary or high-level description of the product, its manufacturing process and the proposed characterization and lot release tests
- The sponsor's position and justification for all of the sponsor's questions
- References to published information related to the product, along with copies of the publications
Pharmacology/Toxicology Content
The pharmacology/toxicology section should provide [48]:
- A comprehensive summary of all preclinical (in vitro and in vivo) studies conducted thus far using the intended clinical product, and the results obtained
- A detailed discussion, with protocol outlines, regarding the additional preclinical proof-of-concept studies the sponsor thinks they need to conduct
- The sponsor's position and justification for all questions the sponsor poses
Clinical Content
In the context of an INTERACT, clinical comments are generally high-level recommendations regarding the overall clinical development program, and do not focus on details of a specific clinical protocol [48]. The INTERACT briefing package should describe [48]:
- The disease of interest
- Target study population
- Available natural history information/data on the condition
- Available treatment options for condition
- Brief outline of first-in-human study
The Scientist's Toolkit: INTERACT Meeting Preparation
Table: Essential Resources for INTERACT Meeting Preparation
| Resource Category | Specific Documents/Guidances | Purpose and Application |
|---|---|---|
| FDA Guidance Documents | Preclinical Assessment of Investigational Cellular and Gene Therapy Products [48] | Provides framework for preclinical testing strategies |
| FDA Procedural Documents | SOPP 8101.1: Regulatory Meetings with Sponsors and Applicants for Drugs and Biological Products [48] | outlines formal procedures for meeting requests and conduct |
| Clinical Development Guidance | Considerations for the Design of Early-Phase Clinical Trials of Cellular and Gene Therapy Products [48] | Informs early clinical trial design strategies |
| Internal Development Documents | Comprehensive TPP aligning with INTERACT questions | Ensures regulatory feedback aligns with overall product strategy |
Strategic Integration of TPP and INTERACT Meetings
Aligning TPP Development with INTERACT Strategy
The most successful INTERACT meetings occur when sponsors have developed a comprehensive TPP that clearly articulates the target product characteristics and have identified specific, targeted questions that address areas of uncertainty in achieving those characteristics. This alignment ensures that the feedback received during the INTERACT meeting directly supports the overall development strategy encapsulated in the TPP.
Best Practices for INTERACT Meeting Success
Based on FDA guidance and industry experience, several best practices maximize the value of INTERACT meetings [47] [49]:
- Focus on Key Questions: Clearly define specific, high-priority regulatory and scientific questions. Avoid broad or overly generic inquiries that cannot be adequately addressed in the limited meeting time [47].
- Provide Clear and Concise Data: Present preliminary findings in a well-structured format. Focus on what is essential for FDA review, avoiding voluminous packages that exceed the 50-page recommendation [48] [47].
- Engage with the Right Experts: Bring relevant scientific and regulatory experts to the meeting to discuss complex topics effectively, ensuring each participant understands their role in the discussion [47].
- Strategic Use of FDA Feedback: Since INTERACT meetings are non-binding, sponsors should incorporate FDA recommendations where applicable but remain flexible in their development approach, using the feedback to inform rather than dictate strategy [47].
The strategic integration of Target Product Profiles with early regulatory engagement through FDA INTERACT meetings represents a powerful approach to de-risking the development of novel therapies, particularly in the complex realm of cell and gene therapies. By establishing a clear TPP early in development and seeking targeted FDA feedback on specific challenges through the INTERACT mechanism, sponsors can identify potential regulatory hurdles before significant resources are invested, align development strategies with regulatory expectations, and ultimately accelerate the delivery of innovative treatments to patients in need. The non-binding, informal nature of INTERACT meetings provides a unique opportunity for open dialogue on scientific and regulatory challenges without the formal constraints of later-stage regulatory interactions, making it an invaluable tool in the strategic development of breakthrough therapies.
Using TPPs for Go/No-Go Decision Making and Portfolio Management
A Target Product Profile (TPP) serves as a strategic planning tool that outlines the desired characteristics of a medical product—including drugs, diagnostics, and devices—to address specific unmet clinical needs [1]. Fundamentally, a TPP embodies the concept of "beginning with the goal in mind," establishing key performance and operational specifications in advance to ensure development efforts remain aligned with predefined health objectives [50]. In the context of research and development (R&D) portfolio management, TPPs provide a critical framework for prioritizing projects, allocating resources efficiently, and making evidence-based go/no-go decisions throughout the development lifecycle.
The strategic value of TPPs extends beyond mere planning documents. They function as dynamic, living documents that can be refined as new clinical data and market insights emerge [50] [7]. For pharmaceutical companies, biotech firms, and public health organizations, TPPs create a shared vision across multidisciplinary teams, ensuring that research, clinical development, regulatory, and commercial functions work toward consistent endpoints. By clearly defining the minimal acceptable and ideal product attributes, TPPs enable objective assessment of a candidate's probability of technical and regulatory success (PTRS), forming the basis for strategic portfolio optimization [9].
The Anatomy of a Target Product Profile
Core Components and Structure
A comprehensive TPP systematically outlines the critical attributes required for a product's successful development and commercialization. While specific elements may vary by product type (therapeutic, diagnostic, or device), the fundamental structure remains consistent, organized around the intended product labeling and key performance characteristics [7] [1].
Table 1: Core Components of a Therapeutic Product TPP
| Drug Label Attribute | Product Property | Minimum Acceptable Result | Ideal Result |
|---|---|---|---|
| Indications and Usage | Primary Indication | Emergency medicine for acute stroke patients immediately on hospital arrival [51] | Emergency medicine for acute stroke patients in the community before hospital arrival [51] |
| Target Population | Patient Population | Adults with moderate to severe stroke [51] | Adults with moderate to severe stroke with concurrent use with tPA or replacement of tPA [51] |
| Dosage and Administration | Treatment Duration | Acute [51] | Acute [51] |
| Dosage and Administration | Delivery Mode | Intravenous (IV) [51] | Intravenous (IV) [51] |
| Dosage Forms and Strengths | Dosage Form | Solution in pre-filled syringes [51] | Solution in autoinjectors [51] |
| Clinical Studies | Clinical Efficacy | 20% more favorable vs. placebo on minimal/no disability at 30 days [51] | 30% more favorable vs. placebo on minimal/no disability at 30 days [51] |
| Adverse Reactions | Risk/Side Effect | Devoid of symptomatic intracranial hemorrhage [51] | Devoid of any symptomatic intracranial hemorrhage [51] |
For diagnostic tests, the TPP structure incorporates different attributes focused on analytical and clinical performance. The framework includes categories such as unmet clinical need, analytical performance, clinical validity, clinical utility, and human factors [50] [1].
Table 2: Core Components of a Diagnostic Test TPP
| Product Property | Minimum Acceptable Result | Ideal Result |
|---|---|---|
| Unmet Clinical Need | Detection of fentanyl in urine [1] | Detection of fentanyl in urine [1] |
| Intended Use | Detection of fentanyl concentrations in urine >1 ng/ml [1] | Detection of fentanyl concentrations in urine >1 ng/ml [1] |
| Target User | Adults 18+ and healthcare professionals [1] | Adults 18+ and healthcare professionals [1] |
| Stability During Transport | +10°C - +30°C [1] | +4°C - +40°C [1] |
| Time to Result | 10 minutes [1] | 3 minutes [1] |
| Diagnostic Sensitivity | 0.5 ng/ml [1] | 0.5 ng/ml [1] |
| Reproducibility | 0.98 [1] | 0.98 [1] |
Integrating Patient Perspectives
Modern TPP development increasingly emphasizes the integration of patient experience data to ensure products address meaningful endpoints and reduce development failures due to misalignment with patient needs. A 2025 guidance framework identified five focus areas where patient perspectives are fundamental [17]:
- Target population and disease heterogeneity
- Unmet medical needs and therapy aims
- Dosage frequency and route of administration
- Efficacy endpoints relevant to patients
- Acceptability of benefit/risk profile trade-offs
Systematic methodologies for gathering patient input include desk research, patient advisory boards, focus groups, and in-depth interviews [17]. This patient-focused approach ensures that TPPs reflect outcomes that matter most to the end-users, potentially improving clinical trial recruitment, retention, and ultimate market adoption.
TPP Development Methodology
A Structured Development Process
The development of a robust TPP follows a systematic, phased approach that transforms initial concepts into a refined strategic document. Research indicates that effective TPP development typically progresses through three core decision-making phases: scoping, drafting, and consensus-building [50].
TPP Development Workflow
The scoping phase establishes the foundational understanding of the disease area, current treatment landscape, and unmet needs through literature reviews and preliminary expert consultations [50] [1]. During the drafting phase, developers define specific target attributes, distinguishing between minimum acceptable and ideal characteristics based on competitive benchmarking and initial patient input [51] [1]. The consensus-building phase involves iterative review with multidisciplinary stakeholders—including clinical experts, regulatory specialists, commercial leads, and patient representatives—to ensure alignment and feasibility [50] [17].
Analytical Frameworks and Benchmarking
Effective TPP development requires rigorous analysis of the competitive landscape and standard of care (SoC). This involves creating detailed profiles of existing therapies, including their mechanisms of action, efficacy profiles, safety considerations, and pricing structures [1].
Table 3: Competitive Benchmarking for TPP Development
| Product Properties | FDA-Approved Medication: Lucemyra (lofexidine) | Minimum Acceptable Results | Ideal Results |
|---|---|---|---|
| Primary Indication | Mitigation of opioid withdrawal symptoms to facilitate abrupt opioid discontinuation in adults [1] | Mitigation of opioid withdrawal symptoms | Mitigation of opioid withdrawal symptoms with improved efficacy |
| Target Population | Adults with opioid dependence physically dependent on short-acting opioids [1] | Adults with opioid dependence | Broader patient population including long-acting opioid users |
| Treatment Duration | Up to 14 days [1] | Up to 14 days | Extended duration up to 30 days |
| Dose Regimen | Three 0.18 mg tablets taken orally 4 times daily [1] | Four times daily dosing | Reduced frequency (twice daily) |
| Clinical Efficacy | Mean SOWS-Gossop total score: 7.0 (placebo: 8.9); 49% completed treatment (placebo: 33%) [1] | Superior to placebo | Superior to active comparator |
| Risk/Side Effect | Hypotension, bradycardia, fainting [1] | Comparable safety profile | Improved safety profile |
| Affordability | $900 for brand, $300 for generic (36 tablets) [1] | Comparable pricing | Lower cost than generic |
Implementing TPPs for Go/No-Go Decisions
Decision Gates Throughout the Development Lifecycle
TPPs provide the objective criteria for stage-gate decision processes in pharmaceutical R&D. By establishing clear metrics at each development phase, organizations can systematically evaluate whether a program should proceed ("go"), require modifications ("hold"), or be terminated ("no-go").
Go/No-Go Decision Gates in Drug Development
Key decision gates typically align with major development milestones:
- Candidate Selection: Evaluating whether preliminary data meets minimal thresholds for efficacy and safety to warrant clinical development [1] [17].
- Proof-of-Concept: Assessing whether early clinical data demonstrates sufficient biological activity and acceptable safety to justify larger trials [1].
- Phase 3 Initiation: Determining whether efficacy and safety profiles suggest a high probability of regulatory success and differentiation from standard of care [1].
- Registration & Launch: Confirming that overall benefit-risk profile supports regulatory submission and potential commercialization [7] [1].
Quantitative Decision-Making Framework
Go/no-go decisions should be based on predefined quantitative thresholds derived from the TPP. These metrics enable objective assessment of development risks and progress.
Table 4: Quantitative Go/No-Go Criteria Based on TPP Targets
| Development Stage | TPP Attribute | Go Threshold | Hold/Modify Threshold | No-Go Threshold |
|---|---|---|---|---|
| Preclinical | Efficacy (in vivo models) | ≥70% response vs. control [51] | 40-69% response vs. control | <40% response vs. control |
| Preclinical | Safety (therapeutic index) | ≥10-fold margin [51] | 5-9 fold margin | <5-fold margin |
| Phase 1 | Maximum Tolerated Dose | ≥2x anticipated efficacious dose [1] | 1-2x anticipated efficacious dose | <1x anticipated efficacious dose |
| Phase 2 | Clinical Efficacy | ≥30% improvement vs. placebo (p<0.05) [51] | 20-29% improvement vs. placebo | <20% improvement vs. placebo |
| Phase 2 | Biomarker Response | ≥50% of patients show target engagement [1] | 30-49% show target engagement | <30% show target engagement |
| Phase 3 | Primary Endpoint | Statistically significant with clinically meaningful effect [51] | Statistically significant but minimal clinical effect | Fails statistical significance |
TPPs in Portfolio Management
Strategic Portfolio Optimization
In portfolio management, TPPs enable organizations to evaluate development programs against standardized criteria, facilitating comparative analysis and strategic resource allocation. By scoring programs against their TPP targets, portfolio managers can visualize the development pipeline and balance risk across therapeutic areas and development stages [9].
Table 5: Portfolio Scoring Matrix Using TPP Criteria
| Program | Therapeutic Area | Phase | Probability of Technical Success | Commercial Potential | Strategic Alignment | TPP Achievement Score | Portfolio Priority |
|---|---|---|---|---|---|---|---|
| Program A | Oncology | Phase 2 | 45% | High | High | 75% | Tier 1 |
| Program B | Neuroscience | Phase 1 | 25% | Medium | High | 60% | Tier 2 |
| Program C | Infectious Disease | Preclinical | 15% | High | Medium | 45% | Tier 3 |
| Program D | Cardiovascular | Phase 3 | 65% | Medium | Medium | 85% | Tier 1 |
| Program E | Rare Disease | Phase 2 | 35% | Low | High | 55% | Tier 2 |
Resource Allocation and Risk Management
TPPs facilitate transparent decision-making for resource allocation by quantifying development programs against strategic objectives. Portfolio managers can use TPP-derived metrics to balance high-risk/high-reward programs with lower-risk opportunities, ensuring sustainable R&D pipelines [9] [1].
The TPP Achievement Score is a quantitative metric reflecting a program's progress toward its target profile. This score can be calculated as a weighted average across key TPP attributes, with weights reflecting strategic priorities (e.g., efficacy weighted 40%, safety 30%, convenience 20%, cost 10%). Programs with consistently low TPP Achievement Scores across multiple milestones become candidates for termination or out-licensing, while high-scoring programs merit increased investment and accelerated development.
Public health organizations like the WHO and DNDi employ TPPs specifically to guide development of products for neglected diseases, prioritizing affordability, accessibility, and suitability for resource-limited settings [2] [9]. This approach ensures that portfolio decisions align with public health needs rather than purely commercial considerations.
Advanced Applications and Future Directions
Diagnostic Test TPPs
While traditionally associated with therapeutic products, TPPs are equally critical for diagnostic development. A systematic review of 44 medical test TPPs revealed that most focused on infectious disease diagnostics, with comprehensive frameworks addressing analytical performance, clinical validity, and clinical utility [50]. However, key outcomes like cost-effectiveness were frequently overlooked, presenting an opportunity for enhanced TPP methodologies [50].
Diagnostic TPPs must specify requirements for analytical sensitivity (detection limit), analytical specificity (cross-reactivity), clinical sensitivity (detection of true positives), and clinical specificity (detection of true negatives) [50] [1]. Additionally, operational characteristics such as time to result, storage conditions, and infrastructural requirements are particularly important for diagnostics deployed in resource-limited settings [50].
The Scientist's Toolkit: Essential Reagents and Methods
Table 6: Research Reagent Solutions for TPP-Informed Development
| Research Tool | Function in TPP Development | Application Context |
|---|---|---|
| Clinical Outcome Assessments (COAs) | Measure patient-reported efficacy endpoints | Validating clinically meaningful endpoints defined in TPP [17] |
| Biomarker Assays | Quantify target engagement and pharmacodynamic effects | Demonstrating proof of mechanism for go/no-go decisions [1] |
| Animal Disease Models | Evaluate preclinical efficacy | Establishing preliminary efficacy for candidate selection [51] |
| Toxicology Assays | Assess safety and therapeutic index | Establishing safety thresholds for clinical development [1] |
| Formulation Screening Tools | Optimize drug delivery and stability | Meeting TPP specifications for dosage form and stability [1] |
| Comparative Benchmarking Assays | Evaluate against standard of care | Establishing competitive profile for portfolio prioritization [1] |
Emerging Best Practices
Future TPP development will increasingly incorporate real-world evidence and patient preference studies to ensure commercial success beyond regulatory approval [17]. Advanced analytics, including machine learning algorithms applied to historical development data, may enhance the predictive accuracy of TPP targets and go/no-go criteria.
Organizations are also moving toward more dynamic TPP platforms that automatically update probability of success calculations as new internal and external data emerge. This living document approach ensures that portfolio decisions reflect the most current scientific and competitive landscape [50] [1] [17].
Target Product Profiles represent a paradigm shift from opportunity-driven development to strategic, evidence-based product planning. When rigorously developed and systematically implemented, TPPs provide the foundational framework for objective go/no-go decision-making and strategic portfolio management. By aligning cross-functional teams around standardized criteria and enabling quantitative assessment of development risks, TPPs enhance R&D productivity and increase the likelihood that innovative medical products will successfully reach patients in need. As the healthcare landscape evolves, TPP methodologies will continue to incorporate patient perspectives, real-world evidence, and advanced analytics to further improve their predictive power and strategic value.
Distinguishing TPPs from Target Candidate Profiles (TCPs)
In the complex and high-stakes landscape of pharmaceutical research and development, strategic planning tools are essential for guiding successful outcomes. Two such critical tools are the Target Product Profile (TPP) and the Target Candidate Profile (TCP), which serve distinct but complementary purposes throughout the drug development lifecycle. A TPP is a strategic planning tool that outlines the desired characteristics of a final marketed product, including its intended use, target population, and key performance and safety features [1]. It serves as a foundational document that aligns stakeholders on the specific goals for a medical product, whether it be a drug, device, or diagnostic test [2] [1]. Acting as a precursor to the TPP during the early discovery phase is the TCP, a profile maintained by discovery team leaders to guide the selection of optimal candidate molecules before significant development resources are committed [52].
Understanding the distinction between these documents is crucial for researchers, scientists, and drug development professionals. While the TPP describes the final commercial product, the TCP defines the ideal compound to be selected from discovery to progress into development. This distinction ensures that early research decisions are made with the ultimate product goals in mind, thereby increasing the likelihood of developing safe, effective, and commercially viable medical products that address unmet patient needs [9] [1].
Conceptual Foundations and Definitions
Target Product Profile (TPP)
A Target Product Profile (TPP) is a strategic planning tool that guides the development of safe and effective medical products by outlining the desired 'profile' or characteristics of a target product aimed at a particular disease or diseases [2] [1]. It represents a dynamic document that evolves with emerging data and insights, supporting informed decision-making at every stage of development [1]. The TPP states the intended use, target populations, and other desired attributes of products, including safety and efficacy-related characteristics [2]. In public health contexts, TPPs set research and development targets for funders and developers, with organizations like the World Health Organization (WHO) developing TPPs to support the creation of missing health products while focusing on public health priorities, access, equity, and affordability [2].
Target Candidate Profile (TCP)
The Target Candidate Profile (TCP) serves as the precursor to the TPP during the discovery phase and is maintained by discovery team leaders [52]. While detailed characteristics of TCPs from the search results are limited, the TCP essentially defines the ideal compound to be selected from discovery to progress into development. It establishes the minimum criteria that a candidate molecule must meet to be considered for further development, bridging the gap between early research discoveries and the formal product development planning encapsulated in the TPP. This critical tool ensures that only the most promising candidates with the highest likelihood of success advance into the resource-intensive development phases.
Key Differences Between TCP and TPP
The relationship between TCP and TPP represents a progression from candidate selection to product definition throughout the drug development continuum. The TCP is utilized early in the discovery phase to guide the selection of optimal candidate molecules, while the TPP becomes the primary planning tool as the candidate moves into development stages [52]. The following diagram illustrates this sequential relationship and key focus areas:
Figure 1: The Sequential Relationship Between TCP and TPP in Drug Development
Comparative Analysis of Attributes
The TCP and TPP differ significantly in their specific attributes, level of detail, and intended audiences. The table below summarizes these key distinctions:
Table 1: Comparative Analysis of TCP and TPP Attributes
| Attribute | Target Candidate Profile (TCP) | Target Product Profile (TPP) |
|---|---|---|
| Primary Focus | Defines ideal compound for development selection | Describes final commercial product characteristics [52] |
| Development Stage | Early discovery phase [52] | From First-In-Human (FIH) study through to approval [52] |
| Key Components | Molecular characteristics, preliminary efficacy, safety thresholds | Comprehensive label claims, dosage form, manufacturing, clinical efficacy, safety profile [9] [1] [52] |
| Level of Detail | Foundational compound requirements | Detailed commercial product specifications |
| Primary Audience | Discovery team leaders, research scientists [52] | Multidisciplinary teams, regulators, funders [2] [1] |
| Regulatory Status | Internal research document | Formal tool for regulatory alignment [1] [52] |
Strategic Functions in the Development Process
The TCP serves as a gatekeeping function, ensuring that only compounds with the highest potential for success advance into development. It establishes the go/no-go criteria for transitioning from discovery to development [52]. In contrast, the TPP serves as both a planning and alignment tool, guiding the entire development process and ensuring all stakeholders share a common vision of the target product. The TPP provides the foundation for regulatory strategy, clinical trial design, and commercial planning [1]. It is worth noting that the TPP is a living document that should be reviewed and updated throughout the drug development process, with initial approval typically required before the start of First-In-Human studies [52].
Core Components of a Target Product Profile
Comprehensive TPP Structure and Elements
A well-constructed Target Product Profile encompasses a comprehensive set of attributes that collectively define the target product. These elements span scientific, technical, clinical, and commercial considerations, providing a complete framework for development. Based on analysis of multiple sources, the following table presents the core components of a biopharmaceutical TPP:
Table 2: Core Components of a Comprehensive Target Product Profile
| Category | Component | Description | Examples from Reference TPPs |
|---|---|---|---|
| Product Definition | Indications & Usage | Targeted disease and population [9] [1] | Mitigation of opioid withdrawal symptoms in adults [1] |
| Mechanism of Action | How the product produces its effect [52] | Central alpha-2 adrenergic agonist [1] | |
| Clinical Attributes | Clinical Efficacy | Primary and secondary efficacy endpoints [1] [52] | Mean SOWS-Gossop total score improvement [1] |
| Safety & Tolerability | Expected safety outcomes and side effects [9] [1] | Hypotension, bradycardia [1] | |
| Contraindications | Known or expected contraindications [52] | Specific drug interactions [1] | |
| Dosage & Administration | Treatment Duration | Length of treatment [1] | Up to 14 days [1] |
| Delivery Mode & Dose Regimen | How and how often administered [9] [1] | Three 0.18 mg tablets taken orally 4 times daily [1] | |
| Dose Form | Physical form of the product [1] | 0.18 mg tablet [1] | |
| Technical Specifications | Product Stability & Storage | Shelf life and storage conditions [9] [1] | Store at 25°C (77°F) [1] |
| Target Manufacturing Profile | Formulation and delivery system [52] | Defined based on product type | |
| Commercial Considerations | Affordability | Price and cost considerations [9] [1] | $2 per test strip (diagnostics) [1] |
| Accessibility | How the product is accessed by patients [1] | Prescription basis [1] | |
| Commercial Landscape | Competitive environment at launch [52] | Analysis of existing treatments |
TPP Applications Across Medical Product Types
The TPP framework is adaptable across various medical product categories, including pharmaceuticals, medical devices, and diagnostic tests [1]. While the core concept remains consistent—defining the desired characteristics of a final product—specific components may vary based on product type. For medical devices, a TPP would include technological characteristics and clinical testing specifics [1]. For diagnostic tests, the TPP would encompass analytical performance characteristics such as diagnostic sensitivity, specificity, and time to result [1]. This adaptability makes the TPP a versatile tool for guiding development across the healthcare product spectrum.
Experimental Protocols for TPP Development
Methodology for Establishing a Target Product Profile
Developing a robust TPP requires a systematic approach that incorporates multiple data sources and stakeholder perspectives. The following workflow outlines the key methodological steps in constructing a comprehensive TPP:
Figure 2: TPP Development Methodology
Step 1: Analyze Unmet Need and Treatment Landscape Conduct a comprehensive analysis of the current treatment landscape, including existing and emerging therapies [1]. Identify gaps in current treatment options and specify the unmet medical need the product will address. For example, when developing a medication for opioid withdrawal, thoroughly evaluate existing options like lofexidine to establish a benchmark for the new product [1].
Step 2: Define Ideal Product Characteristics Outline the optimal attributes of the desired product across all relevant categories, including indications, target population, clinical efficacy, safety profile, dosage forms, and administration parameters [9] [1]. These ideal targets represent the best-case scenario for product performance and characteristics.
Step 3: Establish Minimum Acceptable Criteria Define the minimum acceptable thresholds for each product attribute that would still constitute a viable product [1]. These criteria establish the lower boundaries for product advancement and help guide go/no-go development decisions.
Step 4: Align with Regulatory Requirements Ensure that the TPP components align with regulatory expectations and guidelines [1] [52]. The FDA encourages using TPPs as tools to frame technical product details during advisory meetings [52].
Step 5: Document in TPP Format Organize the product characteristics using a standardized TPP structure, typically presented in a table format with columns for product properties, minimum acceptable results, and ideal results [1].
Step 6: Review and Update Throughout Development Treat the TPP as a dynamic document that evolves with emerging data and insights [1] [52]. Schedule regular reviews and updates at key development milestones to ensure continued relevance.
Research Reagent Solutions for TPP-Informed Discovery
The following table details essential research reagents and materials used in experimental approaches that generate data for TPP and TCP development:
Table 3: Key Research Reagent Solutions for Drug Target Identification
| Research Reagent/Material | Function | Application in Target Discovery |
|---|---|---|
| Tandem Mass Tag (TMT) Reagents | Multiplexed protein quantification using isobaric labels [53] | Thermal Proteome Profiling (TPP) for target deconvolution [53] |
| Data-Independent Acquisition (DIA) Reagents | Label-free quantitative proteomics with consistent quantitative performance [53] [54] | Proteome-wide screening of small molecule interactions [54] |
| Cellular Thermal Shift Assay (CETSA) Components | Measure protein-drug interactions through thermal stability [53] | Target engagement studies in cellular contexts [53] |
| Staurosporine | Broad kinase inhibitor used for benchmarking [54] | Positive control in chemical proteomic methods [54] |
| Solid Phase Extraction (SPE) Tips | Sample cleanup and fractionation prior to MS analysis [53] | Minimize ratio compression in TMT-based TPP experiments [53] |
The distinction between Target Candidate Profiles (TCPs) and Target Product Profiles (TPPs) represents a critical conceptual and practical framework in pharmaceutical development. The TCP serves as the discovery-phase precursor, defining the ideal compound characteristics and establishing criteria for advancement into development [52]. In contrast, the TPP provides a comprehensive strategic plan for the final commercial product, guiding development from first-in-human studies through regulatory approval and commercialization [1] [52]. This progression from candidate definition to product specification ensures that development efforts remain aligned with patient needs, regulatory requirements, and commercial realities throughout the complex drug development journey.
Proper implementation of both TCP and TPP frameworks significantly enhances decision-making, minimizes development risks, and increases the likelihood of successful product approval and adoption [1]. By clearly articulating target characteristics at each stage of development, these tools promote stakeholder alignment, facilitate efficient resource allocation, and ultimately contribute to the development of medical products that effectively address unmet patient needs [2] [1]. As dynamic documents that evolve with emerging data, both TCPs and TPPs represent living frameworks that adapt to new scientific insights throughout the therapeutic development process.
A Target Product Profile (TPP) is a strategic planning tool that outlines the desired characteristics of a medical product, guiding its development from conception to regulatory approval. It functions as a living document that specifies the intended use, target population, and key performance and safety features, ensuring that development efforts align with specific clinical needs and regulatory requirements [1]. By defining these attributes early, a TPP fosters stakeholder alignment, facilitates efficient resource allocation, and increases the likelihood of developing a successful product that addresses unmet medical needs [1]. This paper utilizes the development of Lucemyra (lofexidine), a non-opioid treatment for opioid withdrawal symptoms, as a case study to illustrate the practical application of TPPs in benchmarking against the standard of care and driving strategic decision-making in drug development.
TPP Framework and the Case of Opioid Withdrawal
The Critical Role of TPPs in Strategic Development
A well-constructed TPP provides a clear vision for product development, guiding regulatory strategy and commercial planning. For any new therapeutic, the TPP outlines essential product characteristics, typically organized in a table format that maps key attributes from the target drug labeling, alongside minimum acceptable and ideal results for each parameter [1]. This structured approach enhances decision-making, minimizes risks, and increases the likelihood of successful product approval and adoption by maintaining a consistent focus on the target profile throughout the development process [1]. The dynamic nature of the TPP allows it to evolve with emerging data and insights, supporting informed decision-making at every development stage.
The Treatment Landscape for Opioid Withdrawal Syndrome
Opioid Withdrawal Syndrome (OWS) is a significant, incapacitating complication of abrupt opioid discontinuation in opioid-dependent individuals. Symptoms commonly include anxiety, insomnia, tremors, pain, muscle spasms, and gastrointestinal upset [55]. The distress caused by OWS is particularly severe during the first several days after withdrawal of short-acting opioids, and the fear of these symptoms presents a substantial barrier to opioid discontinuation [55]. A major physiologic driver of OWS is central noradrenergic hyperactivity that results when opioids are abruptly discontinued in opioid-tolerant individuals [55]. Prior to Lucemyra's approval, treatment options were limited, creating a significant unmet medical need for effective, non-opioid therapies to manage withdrawal symptoms.
Lucemyra TPP: Efficacy and Clinical Protocol Benchmarking
Core Efficacy Endpoints and Clinical Trial Design
The TPP for Lucemyra established clear efficacy benchmarks centered on mitigating opioid withdrawal symptoms. The primary efficacy endpoint in its pivotal trials was the Short Opioid Withdrawal Scale of Gossop (SOWS-G), a 10-item, patient-reported outcome with a total score ranging from 0 to 30, where lower scores indicate less severe opioid withdrawal [55]. The SOWS-G items assess: feeling sick, stomach cramps, muscle spasms/twitching, feeling of coldness, heart pounding, muscular tension, aches and pains, yawning, runny eyes, and insomnia/problems sleeping [55]. The TPP specified that Lucemyra must demonstrate statistically significant improvement in SOWS-G scores compared to placebo.
Table 1: Lucemyra Clinical Trial Efficacy Results
| Study Parameter | Study 1 (7-day) | Study 1 (7-day) | Study 2 (5-day) |
|---|---|---|---|
| Treatment Group | Lofexidine 2.88 mg/day | Lofexidine 2.16 mg/day | Lofexidine 2.16 mg/day |
| Mean SOWS-G Score (Days 1-7/5) | 6.1 (SE: 0.35) | 6.5 (SE: 0.34) | 7.0 (SE: 0.44) |
| Placebo Comparison | 8.8 (SE: 0.47) | 8.8 (SE: 0.47) | 8.9 (SE: 0.48) |
| P-value | p < .0001 | p < .0001 | p = .0037 |
| Study Completion Rate | Significantly higher than placebo | Significantly higher than placebo | Significantly higher than placebo |
The clinical data demonstrated that Lucemyra met these efficacy targets. In Study 1, mean SOWS-G scores over Days 1-7 were 6.1 for lofexidine 2.88 mg/day and 6.5 for 2.16 mg/day, compared to 8.8 for placebo (p < .0001 for both) [55]. Similarly, in Study 2, the mean SOWS-G score was 7.0 for lofexidine 2.16 mg/day versus 8.9 for placebo (p = .0037) [55]. These reductions were clinically meaningful, as changes of 2–4 points in SOWS-G scores have been correlated with a clinically meaningful response [55].
Detailed Clinical Trial Methodology
The pivotal trials for Lucemyra were rigorous, multi-center, randomized, double-blind, and placebo-controlled studies conducted in the United States [55].
Study Participants: Both studies enrolled adults (≥18 years) with dependence on short-acting opioids, confirmed by a baseline score of ≥2 on the Objective Opiate Withdrawal Scale prior to randomization. Major exclusion criteria included use of methadone or buprenorphine in the past two weeks, unstable medical or psychiatric illness, and significant cardiovascular abnormalities [55].
Dosing Regimen: In Study 1, subjects were randomized 3:3:2 to lofexidine 2.16 mg/day (0.54 mg QID), lofexidine 2.88 mg/day (0.72 mg QID), or placebo for 7 days. Study 2 randomized subjects 1:1 to lofexidine 2.88 mg/day (0.72 mg QID) or placebo for 5 days [55]. Dosing occurred at 8 am, 1 pm, 6 pm, and 11 pm daily.
Supportive Medications: The protocols allowed specific supportive medications: guaifenesin, antacids, dioctyl sodium sulfosuccinate, psyllium hydrocolloid suspension, bismuth sulfate, acetaminophen, and zolpidem, with any additional medications requiring sponsor approval [55].
Assessment Schedule: SOWS-G was measured at baseline and daily 3.5 hours after the first morning dose. Vital signs were closely monitored pre- and post-dosing, and ECGs were acquired at scheduled intervals throughout the studies [55].
Comprehensive Safety and Tolerability Profile
Cardiovascular Safety Parameters
The TPP for Lucemyra clearly delineated expected safety parameters, particularly concerning cardiovascular effects. Clinical data confirmed these expectations, revealing a distinct safety profile that required careful management but was generally manageable in the controlled treatment setting.
Table 2: Lucemyra Safety Profile Based on Clinical Trials
| Safety Parameter | Incidence in Clinical Trials | Management Strategy |
|---|---|---|
| Orthostatic Hypotension | Up to 42% | Monitor blood pressure; advise slow position changes; maintain hydration |
| Bradycardia | Up to 32% | Monitor heart rate; ECG monitoring in at-risk patients |
| Hypotension | 30% | Regular BP monitoring; dose adjustment if needed |
| Dizziness | Up to 23% | Caution when operating machinery; slow position changes |
| Somnolence/Sedation | Up to 13% | Avoid driving or hazardous activities; avoid other CNS depressants |
| Dry Mouth | Up to 11% | Supportive care; sugar-free lozenges or gum |
| Insomnia | Up to 55% | Note: Also high in placebo group (48%) |
The most common adverse reactions observed with Lucemyra were orthostatic hypotension (up to 42%), bradycardia (up to 32%), hypotension (30%), dizziness (up to 23%), somnolence (up to 13%), sedation (up to 13%), and dry mouth (up to 11%) [56] [57]. Although insomnia was reported frequently (up to 55%), it's noteworthy that this symptom was also highly prevalent in the placebo group (48%), suggesting it may be partly related to opioid withdrawal itself rather than solely a medication side effect [56].
Pharmacological Mechanism and Safety Considerations
Lucemyra's mechanism of action as a central alpha-2 adrenergic receptor agonist directly informs its safety profile. By reducing the release of norepinephrine in the central nervous system, it suppresses the noradrenergic hyperactivity that drives opioid withdrawal symptoms [55] [57]. This same mechanism, however, contributes to its cardiovascular effects, as norepinephrine plays a key role in regulating blood pressure and heart rate.
Important safety considerations include the risk of QT prolongation, which was observed in cardiac electrophysiology studies, with maximum mean change from baseline QTcF of 14.4 milliseconds at 1.8 mg single doses in healthy volunteers [56]. This risk necessitates caution in patients with pre-existing cardiac conditions or those taking other QT-prolonging medications. Additionally, abrupt discontinuation of Lucemyra can lead to rebound hypertension, requiring gradual dose reduction over two to four days when stopping treatment [56] [57].
TPP-Based Benchmarking Against Standard of Care
Comparative Analysis with Existing Treatments
The development of Lucemyra's TPP involved systematic benchmarking against the existing treatment landscape, particularly FDA-approved Lucemyra (lofexidine) itself, which served as a key comparator [1]. This comparative approach ensured the new proposed therapy would meet or surpass current standards, maximizing its potential for patients, providers, and payors while addressing unmet medical needs.
Table 3: TPP Benchmarking - Lucemyra vs. Ideal Target Profile
| Product Properties | FDA-approved Lucemyra | Minimum Acceptable Target | Ideal Target |
|---|---|---|---|
| Primary Indication | Mitigation of opioid withdrawal symptoms to facilitate abrupt opioid discontinuation in adults | Mitigation of opioid withdrawal symptoms | Complete prevention of opioid withdrawal symptoms |
| Target Population | Adults with opioid dependence physically dependent on short-acting opioids | Adults with opioid dependence | All patients experiencing opioid withdrawal |
| Treatment Duration | Up to 14 days | Up to 14 days | Single administration or shorter course |
| Delivery Mode | Oral | Oral | Multiple formulation options |
| Dose Regimen | Three 0.18 mg tablets QID (5-6 hour intervals) | QID dosing | Once-daily dosing |
| Clinical Efficacy | SOWS-G: 7.0 vs placebo 8.9; 49% completion vs 33% placebo | Statistically significant improvement over placebo | Superior to all existing therapies |
| Safety Profile | Hypotension, bradycardia, fainting | Manageable cardiovascular effects | No cardiovascular effects |
| Price/Affordability | ~$900 (brand), ~$300 (generic) for 36 tablets | Comparable to existing therapies | Lower cost than existing options |
This benchmarking exercise revealed Lucemyra's advantages in providing a non-opioid, specifically targeted pharmacological approach to opioid withdrawal, with clinical trial evidence supporting its efficacy and a manageable safety profile when administered with appropriate monitoring [1]. The TPP framework also highlighted areas for potential improvement in future iterations, such as simplified dosing regimens and reduced cardiovascular side effects.
Commercial Strategy and Market Positioning
The commercial strategy for Lucemyra, as reflected in its TPP, emphasized both accessibility and appropriate use within a comprehensive treatment framework. Recent financial data demonstrates the commercial impact of this strategy, with BioCorRx, Inc. reporting $635,224 in revenue for Q3 2025 driven primarily by LUCEMYRA distribution, compared to $0 in the same quarter the previous year, indicating successful market penetration [58]. The company has described this revenue as "material and recurring, signaling a strengthening commercial foundation" [58].
The TPP specifically called for the medication to be available by prescription, with affordability considerations addressed through both brand and generic pricing strategies [1]. The product's positioning as part of a complete treatment program, including medical supervision and counseling, aligns with its FDA-approved indication and the understanding that medication-assisted withdrawal is most effective when embedded within a comprehensive addiction treatment approach [59] [58].
The Scientist's Toolkit: Key Research Reagents and Materials
Successful execution of the Lucemyra development program required specific research tools and assessment methodologies. The following table details key reagents and materials essential for conducting clinical research in opioid withdrawal and evaluating compounds like lofexidine.
Table 4: Essential Research Materials for Opioid Withdrawal Studies
| Research Tool | Function/Application | Specifications/Examples |
|---|---|---|
| Short Opioid Withdrawal Scale-Gossop (SOWS-G) | Patient-reported outcome measure for quantifying opioid withdrawal severity | 10-item scale; total score 0-30; lower scores indicate less severe withdrawal [55] |
| Objective Opiate Withdrawal Scale (OOWS) | Clinician-administered assessment of observable signs of opioid withdrawal | Used for patient qualification (score ≥2 required) [55] |
| Lofexidine HCl | Active pharmaceutical ingredient; alpha-2 adrenergic agonist | 0.18 mg oral tablets; QID dosing [55] [57] |
| Electrocardiogram (ECG) Monitoring | Assessment of cardiovascular safety, particularly QT interval | Scheduled intervals (Days 1, 2, 4, 7 in Study 1; daily in Study 2) [55] |
| Supportive Medications Package | Protocol-allowed concomitant medications for symptom management | Guaifenesin, antacids, dioctyl sodium sulfosuccinate, psyllium, bismuth sulfate, acetaminophen, zolpidem [55] |
| Blinded Study Drug Packaging | Maintenance of study blind and proper dosing | Matched placebo in blister cards; identical appearance to active drug [55] |
The case study of Lucemyra demonstrates the critical value of the Target Product Profile as a strategic tool in guiding drug development and benchmarking against standard of care. Through systematic definition of target characteristics across efficacy, safety, dosing, and commercial considerations, the TPP provided a structured framework that aligned stakeholder expectations and facilitated the successful development and regulatory approval of a needed treatment for opioid withdrawal syndrome. The application of this approach enabled developers to clearly establish Lucemyra's value proposition: a non-opioid treatment with proven efficacy in reducing withdrawal symptoms and improving treatment retention, albeit with a manageable cardiovascular safety profile requiring appropriate monitoring.
Future directions in this therapeutic area will likely build upon the TPP foundation established by Lucemyra. Development efforts are already underway for next-generation treatments, including BioCorRx's BICX104, a long-acting, sustained-release naltrexone implant candidate for opioid and alcohol use disorders [58]. Additionally, non-pharmacological approaches such as neurostimulation devices represent emerging alternatives, with devices like the NET Device (a transcutaneous alternating current stimulator) showing promise in reducing Clinical Opiate Withdrawal Scale scores when used alongside standard treatments [1]. These advancements continue to reflect the principles of TPP-driven development, wherein clear target product characteristics guide strategic decision-making and resource allocation throughout the drug development lifecycle.
TPPs as Tools for Investor Communication and Asset Valuation
In the contemporary drug development landscape, characterized by funding constraints and heightened regulatory scrutiny, the Target Product Profile (TPP) has evolved from a simple planning document into a critical strategic instrument for investor communication and asset valuation. This technical guide delineates the methodology for constructing TPPs that align scientific development with commercial imperatives, thereby enabling researchers and developers to articulate a clear value proposition to potential investors and partners. By serving as a dynamic strategic framework, a robust TPP aligns internal efforts across clinical, regulatory, and commercial functions, mitigates development risks, and enhances the likelihood of achieving a successful and valuable product launch [3] [23].
A Target Product Profile (TPP) is a strategic planning tool that outlines the desired characteristics of a medical product, including its intended use, target population, and key performance and safety features [1]. Fundamentally, it acts as a "strategic blueprint" that guides development from discovery through regulatory approval and commercial launch [3]. In the context of public health, WHO TPPs further emphasize that access, equity, and affordability are integral parts of the innovation process and must be considered at all stages, not just post-development [2].
For the purpose of investor communication, a TPP transitions from an internal document to an external-facing instrument. It demonstrates a development team's deep understanding of the disease area, the competitive landscape, and the precise unmet patient need their product aims to address. A well-crafted TPP signals strategic maturity and readiness to engage with stakeholders who can provide the capital and partnerships necessary to bring a drug to market [3]. In an era where investor scrutiny is high and first-year sales for newly launched products are steadily declining, a robust TPP is more important than ever to differentiate a product and justify its potential valuation [23].
The Role of TPPs in Investor Communication and Valuation
Establishing Strategic Clarity and Alignment
A TPP provides a "North Star" for drug development, offering clarity and direction in an environment of high uncertainty [3]. For investors, this translates to confidence that the development team has a clear, data-driven vision. The TPP aligns internal efforts across clinical, regulatory, and commercial functions, ensuring that every step in the development process is purposeful and directly contributes to the end goals defined by the needs of patients, physicians, and payers [3] [23]. This early alignment is crucial for developing a commercially viable product with a potentially higher valuation [23].
Mitigating Risk and Supporting Valuation
The drug development process is inherently risky, and investors require tools to accurately assess and mitigate these risks. A TPP directly addresses this by:
- Guiding Regulatory Strategy: A TPP frames development in relation to regulatory submission requirements [2]. By defining minimum acceptable and ideal targets for efficacy and safety, it helps developers engage early and strategically with regulators, reducing the risk of a Complete Response Letter (CRL), the incidence of which has almost tripled since 2018 [23].
- Enabling Contingency Planning: TPPs support holistic thinking about long-term regulatory and commercial goals, allowing for scenario planning based on evolving standards of care [3]. This flexibility facilitates strategic pivots without losing sight of core objectives, thereby de-risking the investment.
- Articulating the Value Proposition: By explicitly defining the product's differentiation from existing therapies—including potential improvements in efficacy, safety, accessibility, and affordability—the TPP makes a direct case for the product's market potential and its ability to secure favorable market access [1] [23].
The following diagram illustrates how a TPP integrates various development components to create a cohesive strategy that communicates value and de-risks the asset for investors.
Diagram 1: TPP as a Central Strategic Framework. This diagram shows how the TPP integrates core strategic components—scientific, regulatory, commercial, and clinical—to create a unified plan that effectively communicates asset value and de-risks development for investors.
Quantitative Benchmarks for Asset Valuation
From a valuation perspective, a TPP provides the concrete benchmarks against which developmental progress and potential commercial return can be measured. Investors assess these benchmarks to determine the asset's risk-profile and potential for success. The table below summarizes key quantitative indicators from the industry landscape that underscore the importance of rigorous TPP-driven planning.
Table 1: Quantitative Benchmarks Highlighting the Need for Robust TPPs
| Metric | Industry Benchmark | Implication for Asset Valuation |
|---|---|---|
| Average First-Year Sales (2022 Launches) | $65 million (excluding COVID products, a steady decline over 5 years) [23] | Highlights a challenging commercial environment; underscores the need for a TPP to define a compelling product profile that can achieve breakout success. |
| Prescription Fill Rate | 44% of all prescriptions are filled [23] | Emphasizes the critical importance of designing a TPP that incorporates payer and market access considerations from the outset. |
| FDA Complete Response Letters (CRLs) | Number has almost tripled since 2018 [23] | A robust TPP that aligns with regulatory expectations is a key tool for mitigating the risk of a CRL, which can significantly delay launch and diminish asset value. |
| BLAs/NDAs referencing a TPP | An "overwhelming number"...do not reference a TPP [23] | Represents a significant strategic gap; developers who employ a disciplined TPP process can differentiate their asset and present a more mature, de-risked opportunity to investors. |
Methodological Framework for Constructing an Investor-Focused TPP
Core Components and Structure
A robust, investor-grade TPP is structured around the key sections of a future drug label, translating them into a set of target product properties with clear, measurable goals. This structure ensures the document remains focused on the attributes that regulators, payers, and ultimately physicians and patients, will use to evaluate the product. The core methodology involves defining for each attribute both the minimum acceptable and ideal target [1] [3]. The minimum criteria represent the "minimum viable criteria for approval," while the ideal goals "define true success" from a commercial and clinical perspective [3].
Table 2: Core TPP Framework for a Novel Pharmacotherapeutic [1]
| Drug Label Attribute / Product Property | Minimum Acceptable Result | Ideal Result |
|---|---|---|
| Indications and Usage (Primary Indication) | Treatment of condition X in a refractory population. | First-line treatment for condition X; expansion into adjacent indications. |
| Target Population | Adults 18-65 with severe disease, confirmed by biomarker Y. | Adults and adolescents from age 12; includes patients with mild-moderate disease. |
| Clinical Efficacy (vs. Standard of Care) | Non-inferiority on primary endpoint (e.g., 20% improvement). | Superiority on primary endpoint (e.g., >30% improvement) and key secondary endpoints (e.g., quality of life). |
| Dosage and Administration (Treatment Duration) | 12-week treatment course. | 8-week treatment course or shorter. |
| Dosage and Administration (Dose Regimen) | Twice-daily oral dosing. | Once-daily oral dosing. |
| Adverse Reactions (Risk/Side Effect Profile) | Well-tolerated with manageable side effects; no black box warning. | Cleaner safety profile than competitor; no requirement for intensive monitoring. |
| How Supplied/Storage (Stability) | Stable for 24 months under refrigerated conditions (2-8°C). | Stable for 36 months at room temperature. |
| Affordability (Price) | Priced at a premium to standard therapy. | Cost-effective with a price supporting favorable reimbursement and high uptake. |
| Accessibility | Requires specialized distribution. | Broad distribution through retail pharmacies. |
Analytical Protocols: Benchmarking Against the Treatment Landscape
A critical methodological step in TPP development is a comprehensive analysis of the current treatment landscape. This involves identifying a key competitor or standard-of-care therapy and using its documented profile as a benchmark. This comparative approach ensures the new proposed therapy is designed to meet or surpass current standards, maximizing its potential for patients, providers, and payers [1].
Experimental Protocol: Competitive Benchmarking Analysis
- Identify Benchmark Product(s): Select one or more established or emerging therapies in the target indication. For example, when developing a medication for opioid withdrawal, Lucemyra (lofexidine) serves as a natural benchmark [1].
- Data Extraction: Systematically extract key product properties from the competitor's regulatory documents, such as the FDA-approved drug label or, for devices, the Premarket Notification (510(k)). Key data points include indicated population, efficacy endpoints from pivotal trials, safety profile, dosage regimen, and storage conditions [1].
- Populate Comparative TPP Table: Structure the TPP to directly compare the benchmark's performance against your product's minimum and ideal targets. This creates a powerful, visual representation of your product's potential competitive advantage.
- Gap Analysis and Strategic Insight: Analyze the gaps between the benchmark and your ideal profile. This analysis informs clinical trial design, positioning, and the core value story for investors.
Table 3: Applied TPP Benchmarking for a Novel Opioid Use Disorder Therapy [1]
| Product Property | FDA-Approved Benchmark: Lucemyra | Minimum Acceptable Result for New Therapy | Ideal Result for New Therapy |
|---|---|---|---|
| Primary Indication | Mitigation of opioid withdrawal symptoms to facilitate abrupt discontinuation. | Non-inferior to Lucemyra in mitigating withdrawal symptoms. | Superior to Lucemyra in supporting long-term abstinence, not just withdrawal management. |
| Target Population | Adults dependent on short-acting opioids. | Adults with opioid use disorder (OUD). | Adults and adolescents with OUD, including those on long-acting opioids. |
| Treatment Duration | Up to 14 days. | Up to 14 days. | Up to 6 months for relapse prevention. |
| Clinical Efficacy | Mean SOWS score: 7.0 (Placebo: 8.9); 49% completed 5-day treatment (Placebo: 33%). | Statistically significant improvement over placebo on primary endpoint. | Superior to Lucemyra in treatment retention and patient-reported outcomes. |
| Risk/Side Effect | Hypotension, bradycardia, fainting. | A different, more manageable side effect profile. | Improved cardiovascular safety profile compared to Lucemyra. |
| Dose Regimen | Three tablets, four times daily. | Twice-daily dosing. | Once-daily dosing. |
| Affordability (Price) | ~$900 for a 36-tablet bottle (brand). | Priced below the branded benchmark. | Cost-effective to payers, enabling unrestricted access. |
Advanced Applications: TPPs for Diverse Product Types
The utility of TPPs extends beyond small molecule drugs to biologics, medical devices, and diagnostics. The fundamental structure remains, but the key product properties are adapted to the relevant technology and regulatory pathway.
TPP for a Medical Device
For a medical device, the TPP focuses on intended use, technological characteristics, and clinical performance data required for regulatory clearance or approval.
Table 4: TPP Framework for a Medical Device for Opioid Withdrawal [1]
| Product Property | Benchmark Device (NET Recovery) | Minimum Acceptable Result | Ideal Result |
|---|---|---|---|
| Intended Use | Transcutaneous stimulation for opioid withdrawal symptoms used with standard medications. | Non-inferior reduction in withdrawal scores as an adjunct therapy. | Monotherapy for managing moderate withdrawal symptoms. |
| Patient Population | Patients aged 18+, with moderate COWS score. | Adults 18+ diagnosed with OUD. | Adults and adolescents 16+ with a broad range of COWS scores. |
| Clinical Performance | 61.3% mean reduction in COWS score at 60 minutes. | Statistically significant reduction in COWS score vs. sham control. | >70% mean reduction in COWS score, sustained for several hours. |
| Treatment Duration | 1 hour/day, up to 7 days. | 1 hour/day, up to 7 days. | 30 minutes/day, up to 14 days. |
| Safety Analysis / Risk | Risks consistent with predicate device; no major safety concerns in testing. | No Serious Adverse Events (SAEs) related to device use. | Superior safety profile compared to standard pharmacological treatments. |
| Affordability (Price) | $600 - $1,500 | Priced competitively within the benchmark range. | Lower cost than a full course of pharmacological therapy. |
The Role of AI and Dynamic TPP Management
Artificial Intelligence is emerging as a tool to streamline TPP creation and refinement. Current AI tools can extract insights from vast quantities of scientific and regulatory literature to generate first-draft TPP templates [3]. The future points toward "agentic AI" – autonomous tools that can dynamically update TPPs or flag strategic shifts in the regulatory or competitive landscape [3]. However, challenges remain, as AI often relies on publicly available data which skews toward successful trials and may lack insights from failed studies or proprietary commercial data [3]. The following diagram outlines a proposed workflow for integrating AI into the TPP lifecycle.
Diagram 2: AI-Augmented TPP Development Workflow. This diagram visualizes how AI can process diverse data inputs to generate draft TPPs, create scenario models, and provide continuous monitoring, making the TPP a dynamic rather than static document.
Constructing a robust TPP requires leveraging specific tools and resources. The following table details key "research reagent solutions" – in this context, foundational documents, datasets, and frameworks – that are essential for informing a credible and data-driven TPP.
Table 5: Essential Resources for TPP Development
| Resource / Tool | Function in TPP Development | Specific Application Example |
|---|---|---|
| FDA Drug Labels | Provides the definitive structure and content for the "Drug Label Attributes" column of a TPP and serves as a data source for benchmarking competitors [1]. | Used to extract the exact indications, dosing, efficacy data, and safety warnings for a benchmark product like Lucemyra [1]. |
| FDA Guidance Documents | Informs the "Regulatory Strategy" by outlining the agency's current thinking on clinical trial design endpoints and evidence requirements for specific disease areas [3]. | Referenced when defining "Minimum Acceptable" and "Ideal" results for the "Clinical Efficacy" section to ensure alignment with regulatory expectations. |
| Competitor 510(k) Summaries (Devices) | For medical devices, this public document provides detailed information on a predicate device's technological characteristics and clinical testing data for benchmarking [1]. | Used to populate the "Benchmark" column in a device TPP, as shown with the NET Recovery device [1]. |
| Market Analysis & Pricing Data | Informs the "Commercial" aspects of the TPP, specifically the "Affordability" and "Accessibility" rows, ensuring the product profile is commercially viable [1] [23]. | Used to set realistic price targets and to understand payer barriers, addressing the finding that 56% of prescriptions are not filled [23]. |
| Structured TPP Worksheets | Provides a pre-defined framework or template to ensure all critical sections of a TPP are considered, streamlining the development process [1]. | The worksheet from NIDA provides a proven structure that can be adapted for new therapeutic areas [1]. |
For researchers and scientists, mastering the development and use of a Target Product Profile is no longer optional but a critical component of translational science. A TPP is the fundamental document that bridges the gap between laboratory research and commercial reality. By providing a structured, dynamic, and strategic framework, a well-articulated TPP demonstrates to investors that a development team possesses not only scientific excellence but also the commercial acumen and strategic discipline necessary to navigate the complex journey from concept to clinic. It is the primary tool for de-risking an asset, aligning development with market needs, and ultimately, maximizing valuation and the potential for successful patient impact.
A Target Product Profile (TPP) is a strategic document that outlines the desired characteristics of a health product—such as a drug, vaccine, diagnostic, or medical device—aimed at addressing a particular disease or set of diseases [2]. In the context of public health, TPPs serve as critical planning tools that guide research and development (R&D) toward products that meet pressing global health needs. The World Health Organization (WHO) develops TPPs to support the creation of missing health products, maintaining a sharp focus on public health priorities [2]. Unlike industry TPPs that may prioritize commercial viability, WHO TPPs explicitly integrate considerations of access, equity, and affordability throughout the innovation process, not merely as afterthoughts once a product is developed [2] [60].
WHO TPPs function as strategic reference documents that align the preferences of WHO for product development in a specific area with the specific TPPs used by industry or funding entities [60]. They inform a diverse range of stakeholders, including product developers, regulatory agencies, procurement agencies, and funders, about R&D and public health priorities [2]. The primary objective is to facilitate the most expeditious development of products that address the most urgent and significant public health needs [60]. For diseases and conditions where there is no market or limited incentive for R&D, such as poverty-related neglected diseases or pathogens with pandemic potential, WHO TPPs provide essential guidance to direct resources and efforts toward the greatest unmet health needs [60] [40].
The WHO Framework for TPP Development
Key Components and Terminology
The WHO utilizes a structured framework for TPPs, defining specific components and employing standardized terminology to ensure clarity and consistency across different product types and disease areas.
Table 1: Key WHO Product Profile Definitions and Components
| Term | Definition | Purpose and Context |
|---|---|---|
| Target Product Profile (TPP) | A document stating minimal and optimal characteristics for a product [60] [40]. | Used when a product pipeline develops, allowing for specific targets and minimum performance criteria [60]. |
| Preferred Product Characteristics (PPC) | A strategic document describing an ideal product class, often at an early development stage [60]. | Provides strategic guidance and high-level considerations to stimulate innovation in a new area; does not specify minimal acceptable criteria [2] [60]. |
| Target Regimen Profile (TRP) | A profile used when several drugs would be used in a combination regimen [60]. | Guides the development of multi-drug therapies, ensuring compatibility and efficacy of the combined regimen. |
| Minimal Criteria | The lowest acceptable performance and operational characteristics for a product [2]. | Products are expected to meet all minimum criteria to be considered viable for the intended public health need. |
| Optimal Criteria | The desired, ideal characteristics for a product [2]. | Represents the aspirational goals for product development; meeting as many optimal criteria as possible is encouraged. |
A WHO TPP document typically describes the product's intended use, target populations, and other desired attributes, with a strong emphasis on safety and efficacy-related characteristics [2]. The "minimal" and "optimal" framework allows for necessary trade-offs between performance, cost, and operational characteristics to be considered during WHO policy formulation, making the criteria indicative rather than absolute in the final policy decision [61].
The WHO TPP Development Process
The development of a WHO TPP follows a standardized, consensus-driven protocol that incorporates diverse expertise and public input. The process is designed to be transparent, evidence-informed, and inclusive of multiple constituencies [61] [40].
Diagram 1: The Standard WHO TPP Development Workflow
The process involves several key stages:
Stakeholder Engagement and STDG Formation: WHO constitutes a Scientific TPP Development Group (STDG) comprising subject matter experts, public health specialists, country policymakers, donors, regulators, and civil society representatives [61]. This group is engaged throughout the development process and proposes the final TPP.
Evidence-Informed Drafting: A draft TPP is prepared. Increasingly, this includes evidence-based modeling to quantify trade-offs, such as between test accessibility and accuracy, complementing expert opinion with data-driven insights [61].
Delphi Consensus Process: The draft is subjected to a Delphi method survey distributed to all STDG members to reach agreement on the proposed characteristics [61]. This structured communication technique helps build consensus among experts.
Public Comment Period: The revised draft is made publicly available on the WHO platform for a defined period (e.g., one month) to solicit feedback from the global community [61] [40]. This ensures broader viewpoints, including from industry, are considered.
Finalization and Publication: Feedback from the public comment process is analyzed and discussed in a final stakeholder consultation. Consensus is reached on each characteristic, and the final TPP is published and added to the WHO's Target Product Profile Directory [61] [39].
TPPs in Action: A Tuberculosis Case Study
The development of TPPs for tuberculosis (TB) diagnostics provides a robust, real-world illustration of how WHO applies this framework to a major global health priority. In 2022, an estimated 10.6 million people fell ill with TB, highlighting the critical need for improved diagnostic tools [61].
Methodology for Updating the TB Detection TPP
The 2024 update to the WHO TPP for TB detection at peripheral levels followed the standard protocol with a specific emphasis on evidence-based modeling. The methodology was designed to explicitly quantify trade-offs between test access and accuracy for new diagnostics within the care cascades of high-burden countries like South Africa, India, and Kenya [61]. A simulation-based model provided outputs on acceptable accuracy estimates and costs, which were presented to the STDG to guide the final characteristics [61]. The consultation process was extensive, with a 84% response rate (49 of 58 people) to the Delphi-like survey and 205 consented respondents providing feedback during the public comment period [61].
Table 2: Key Operational Definitions for TB Diagnostic TPPs
| Test Category | Intended Healthcare Setting | Infrastructure & Skill Requirements | Example |
|---|---|---|---|
| Point of Care (PoC) | Health settings without laboratories [61]. | Instrument-free; no need for electricity, equipment, or cold chain; no special skills required [61]. | Lateral flow test (dipstick) [61]. |
| Near Point of Care | Health clinics without laboratories [61]. | Instrument-based, preferably battery-operated; basic technical skills (e.g., basic pipetting) required [61]. | Portable nucleic acid amplification test (NAAT) platform [61]. |
| Low Complexity Assays | Peripheral laboratories (e.g., microscopy centers) [61]. | Requires an instrument and basic laboratory infrastructure; can be operated by staff with basic technical skills [61]. | GeneXpert 10-color platform [61]. |
Research Reagent Solutions for TB Diagnostic Development
The experimental development and validation of TB diagnostics that meet TPP criteria rely on a suite of critical research reagents and materials.
Table 3: Essential Research Reagents for TB Diagnostic Development
| Research Reagent / Material | Function in Development and Validation |
|---|---|
| Clinical Specimens (Sputum) | The traditional sample matrix used for validating analytical and clinical performance against culture as a reference standard [61]. |
| Alternative Specimens (Tongue Swabs, Urine) | Non-sputum-based samples critical for evaluating tests intended for use in vulnerable populations or non-traditional settings, aligning with TPP goals of increased accessibility [61]. |
| Inactivated TB Antigens & Synthetic Oligonucleotides | Used as positive controls and calibrators in immunoassays and molecular tests (e.g., NAATs) to ensure assay reproducibility and robustness [61]. |
| Characterized Biobanks (from diverse populations) | Collections of well-defined clinical samples essential for conducting rigorous sensitivity and specificity studies across different demographic and geographic groups [61]. |
| Culture Reference Strains (DS & MDR-TB) | Essential for establishing the limit of detection (LoD) and for validating a test's ability to detect drug-resistant TB, a key optimal characteristic in TPPs [61]. |
The WHO TPP Directory: A Strategic Resource for Researchers
To centralize and harmonize global efforts, WHO maintains the Target Product Profile Directory (TPPD), a free-to-use online database [60] [40]. The TPPD is a searchable repository of TPPs, PPCs, and TRPs for medicines, vaccines, diagnostics, and medical equipment [60]. It was created in response to pandemics, which highlighted the urgent need for centralized information to guide and coordinate R&D for neglected diseases and populations [60] [40].
The directory allows researchers, funders, and developers to search and filter profiles by disease, product type, year of creation, author (WHO or non-WHO), and status (active or archived) [60]. A key feature is the distinction between WHO-authored profiles, which indicate a significant unmet health need and WHO's official preferences, and non-WHO profiles from Product Development Partnerships, commercial companies, and other organizations [60]. The directory emphasizes that inclusion of non-WHO profiles does not imply endorsement by WHO [60]. This resource enables high-level landscape analysis of R&D activity and promotes standardization in how desired health products are described [60] [40].
WHO Target Product Profiles are indispensable tools for validating and directing public health-oriented R&D. By clearly articulating minimal and optimal product characteristics through a transparent, consensus-based process, TPPs align the efforts of diverse stakeholders—from academic researchers to commercial manufacturers—toward the common goal of addressing the world's most pressing health challenges. The continuous refinement of TPPs, as demonstrated by the evidence-informed update for TB diagnostics, ensures they remain relevant in a dynamic technological landscape. For the research and development community, engagement with WHO TPPs, facilitated by resources like the TPP Directory, is not merely beneficial but essential for ensuring that scientific innovation translates into equitable, accessible, and high-impact health products for those most in need.
Conclusion
A well-constructed and diligently maintained Target Product Profile is far more than a regulatory checkbox; it is the strategic core of successful therapeutic development. By serving as a dynamic, cross-functional blueprint, the TPP aligns scientific innovation with clinical needs, regulatory pathways, and commercial realities throughout the product lifecycle. The key takeaways underscore that TPPs must evolve from static documents into living frameworks that incorporate competitive intelligence, adapt to emerging data, and facilitate critical decision-making. As biomedical innovation advances into novel modalities like gene therapies and AI-driven digital health tools, the principles of effective TPP development will become increasingly vital. Future success will depend on developing more standardized approaches for TPP creation while maintaining the flexibility needed to guide transformative treatments from bench to bedside efficiently and effectively.
References
- 1. Target Product Profiles (TPPs) for Medical Product Development [https://nida.nih.gov/funding/small-business-innovation-research-sbir-technology-transfer-sttr-programs/target-product-profiles]
- 2. WHO target product profiles [https://www.who.int/observatories/global-observatory-on-health-research-and-development/analyses-and-syntheses/target-product-profile/who-target-product-profiles]
- 3. How target product profiles guide drug development ... [https://www.iqvia.com/blogs/2025/09/how-target-product-profiles-guide-drug-development-through-uncertain-times]
- 4. Target Product Profiles [https://renaissancephilanthropy.org/playbooks/target-product-profile/]
- 5. BARDA Target Product Profiles (TPP) [https://medicalcountermeasures.gov/barda/tpp/]
- 6. Facilitating the use of the target product profile in academic ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05476-1]
- 7. What is Target Product Profile (TPP)? [https://www.freyrsolutions.com/what-is-target-product-profile-tpp]
- 8. Constructing a Target Product Profile – Industry's Perspective [https://www.biocurate.com/resources/constructing-a-target-product-profile-industrys-perspective/]
- 9. Target product profiles [https://dndi.org/research-and-development/target-product-profiles/]
- 10. 5 Reasons Why Building a Robust Target Product Profile is ... [https://premier-research.com/perspectives/5-reasons-why-building-a-robust-target-product-profile-is-essential/]
- 11. Premier Research | The Target : Basics and Benefits Product Profile [https://premier-research.com/perspectives/the-target-product-profile-basics-and-benefits/]
- 12. Next in pharma 2025: The future is now [https://www.pwc.com/us/en/industries/pharma-life-sciences/pharmaceutical-industry-trends.html]
- 13. The Forgotten Power of the TPP: Why Many Biopharma ... [https://thelansis.com/blogs/the-forgotten-power-of-the-tpp-why-many-biopharma-projects-fail-without-it/]
- 14. TPP Testing In Pharma: Best Practices [https://glginsights.com/articles/tpp-testing-in-pharma-best-practices/]
- 15. How US President Trump upended the pharma industry in ... [https://www.swissinfo.ch/eng/drug-pricing/timeline-how-us-president-trump-upended-the-pharma-industry-in-2025/90348148]
- 16. Best practices in preclinical development of cell therapy ... [https://www.darkhorseconsultinggroup.com/post/best-practices-in-preclinical-development-of-cell-therapy-products]
- 17. Incorporating Patient Input into the Target Product Profile [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181091/]
- 18. What Is A Target Product Profile? A Full Guide ... [https://gmppros.com/target-product-profile/]
- 19. On the Concepts, Methods, and Use of “Probability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11924160/]
- 20. Frontiers | Target for digital health technologies... product profiles [https://www.frontiersin.org/journals/health-services/articles/10.3389/frhs.2025.1537016/full]
- 21. Accelerating Change in Matrix Pharma Organizations [https://wlhconsulting.com/accelerating-change-in-matrix-pharma-organizations-the-critical-role-of-cross-functional-teams-in-2025/]
- 22. Bridging Vision and Value: How Target Product Profiles ... [https://www.pharmexec.com/view/target-product-profiles-value-evidence-archetypes-market-access]
- 23. 5 Essentials for Building a Robust Target Product Profile [https://premier-research.com/perspectives/5-essentials-for-building-a-robust-target-product-profile/]
- 24. FDA Digital Health Advisory Committee [https://www.fda.gov/medical-devices/digital-health-center-excellence/fda-digital-health-advisory-committee]
- 25. Comparison of Quantitative Mass Spectrometric Methods ... [https://pubmed.ncbi.nlm.nih.gov/37439223/]
- 26. 6.5 Network and graph visualizations [https://fiveable.me/reproducible-and-collaborative-statistical-data-science/unit-6/network-graph-visualizations/study-guide/l7ZZ7oTCKSJp7IEp]
- 27. Tutorial: A Beginner's Guide To Graph Data Visualization [https://cambridge-intelligence.com/a-beginners-guide-to-graph-visualization/]
- 28. Developing Target (TPPs) for Product -Based Profiles AAV Therapies [https://www.linkedin.com/pulse/developing-target-product-profiles-tpps-aav-based-iizpe]
- 29. Adeno-Associated Virus Gene Development: Early Planning... Therapy [https://pubmed.ncbi.nlm.nih.gov/39976996/]
- 30. Adeno-Associated Virus Gene Therapy Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC11971537/]
- 31. Recreating pathophysiology of CLN2 disease and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12432371/]
- 32. Immunogenicity of Novel AAV Capsids for Retinal Gene ... [https://www.mdpi.com/2073-4409/11/12/1881]
- 33. Development of a protocol complexity tool [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02652-9]
- 34. Membrane-mimetic thermal proteome profiling (MM-TPP) ... [https://elifesciences.org/articles/104549]
- 35. Membrane-mimetic thermal proteome profiling (MM-TPP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611261/]
- 36. How to Conduct a Competitive Intelligence Analysis [https://www.errequadro.ai/en/competitive-intelligence-analysis/]
- 37. How to Do a Competitive Landscape Analysis in 2025 - Klue [https://klue.com/blog/competitive-landscape-analysis-guide]
- 38. Research Protocols - Pharmaceutical Sciences ... - Guides [https://guides.lib.uiowa.edu/c.php?g=132196&p=1087496]
- 39. Target product profiles for tuberculosis screening tests [https://www.who.int/publications/i/item/9789240113572]
- 40. Target product profile directory [https://www.who.int/our-work/science-division/research-for-health/target-product-profile-directory]
- 41. Attacking the TPP - crafting a better alternative [https://www.linkedin.com/pulse/attacking-tpp-crafting-better-alternative-mike-rea-f5gde]
- 42. PTMNavigator: interactive visualization of differentially ... [https://www.nature.com/articles/s41467-024-55533-y]
- 43. Why should academia care about the Target Product Profile? [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05520-0]
- 44. Development of a protocol complexity tool - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395810/]
- 45. Version Control Systems (VCS) in 2025 [https://trio.dev/version-control-systems/]
- 46. Top 5 API Versioning Strategies (2025) [https://blog.dreamfactory.com/top-5-api-versioning-strategies-2025-dreamfactory]
- 47. FDA INTERACT Meetings: What You Need to Know [https://www.linkedin.com/pulse/fda-interact-meetings-what-you-need-know-meranda-parascandola-hjc5e]
- 48. OTP INTERACT Meetings [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/otp-interact-meetings]
- 49. FDA INTERACT Meetings: Early Interactions for Cell and ... [https://premier-research.com/perspectives/fda-interact-meetings-early-interactions-for-cell-and-gene-therapy-sponsors/]
- 50. Target Product Profiles for medical tests: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7212678/]
- 51. CREATE Bio Example: Target Product Profile (TPP) [https://www.ninds.nih.gov/current-research/research-funded-ninds/translational-research/create-bio/create-bio-application-support-library/create-bio-example-target-product-profile-tpp]
- 52. Know the Pharma Basics: Target Product Profile [https://redsneakersblog.com/2017/01/14/know-the-pharma-basics-target-product-profile/comment-page-1/]
- 53. Experimental and data analysis advances in thermal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10921035/]
- 54. Streamlined analysis of drug targets by proteome integral ... [https://www.nature.com/articles/s41467-024-53240-2]
- 55. Efficacy of lofexidine for mitigating opioid withdrawal symptoms [https://pmc.ncbi.nlm.nih.gov/articles/PMC6968526/]
- 56. Lucemyra Side Effects: Common, Severe, Long Term [https://www.drugs.com/sfx/lucemyra-side-effects.html]
- 57. Lucemyra (lofexidine) - Uses, Side Effects, and More [https://www.webmd.com/drugs/2/drug-175333/lucemyra-oral/details]
- 58. BioCorRx, Inc. Announces Q3 2025 Results [https://www.biocorrx.com/news-media/press-releases/detail/236/biocorrx-inc-announces-q3-2025-results-second-straight]
- 59. Lofexidine (oral route) - Side effects & dosage [https://www.mayoclinic.org/drugs-supplements/lofexidine-oral-route/description/drg-20443753]
- 60. Frequently asked questions [https://www.who.int/our-work/science-division/research-for-health/target-product-profile-directory/frequently-asked-questions]
- 61. WHO target product profile for TB detection at peripheral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12157113/]