Strategic Prodrug Design and Formulation: Enhancing Solubility, Permeability, and Targeted Delivery
This article provides a comprehensive overview of modern prodrug strategies for researchers and drug development professionals.
Strategic Prodrug Design and Formulation: Enhancing Solubility, Permeability, and Targeted Delivery
Abstract
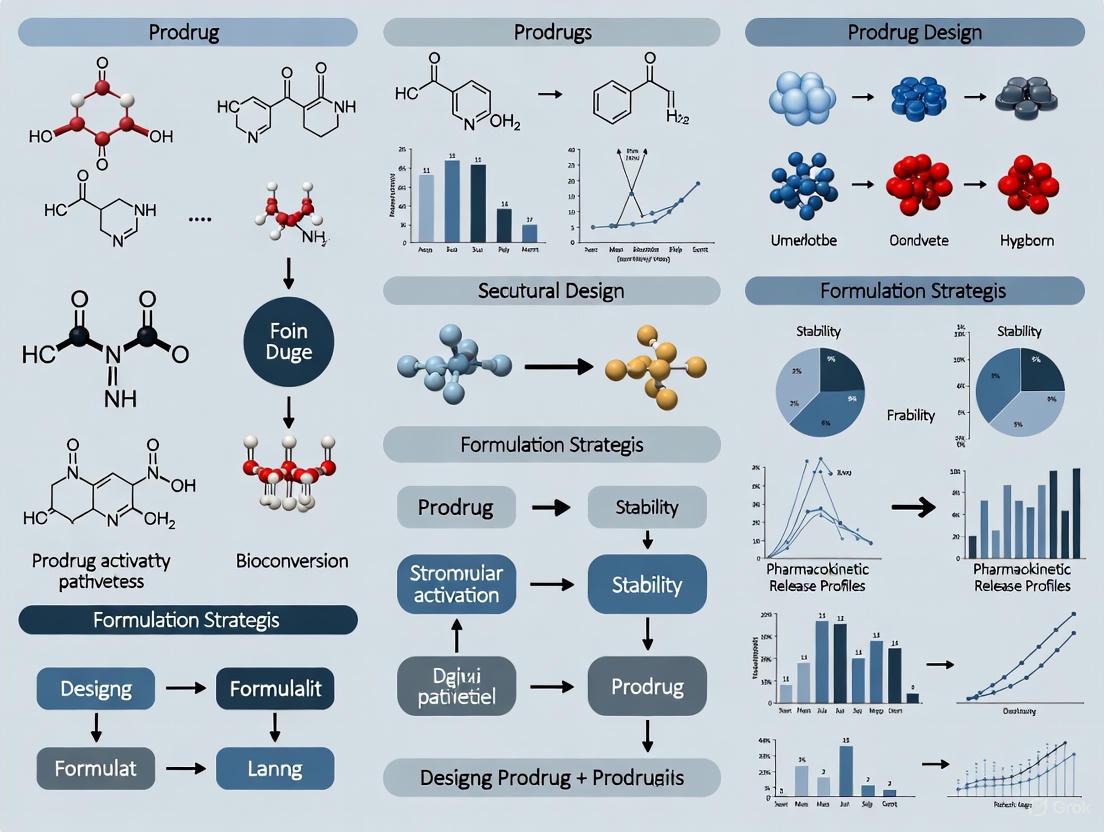
This article provides a comprehensive overview of modern prodrug strategies for researchers and drug development professionals. It explores the foundational principles of prodrug design, detailing how chemical modifications transform inactive compounds into active drugs to overcome key development challenges. The scope includes methodological approaches for enhancing solubility and permeability, practical troubleshooting for common formulation hurdles, and current validation techniques. By synthesizing recent advancements and real-world applications, this resource aims to equip scientists with the knowledge to leverage prodrug technology for optimizing pharmacokinetic properties and achieving targeted therapeutic delivery.
Prodrug Fundamentals: Principles, Classifications, and Key Objectives in Modern Drug Development
A prodrug is a pharmacologically inactive compound that is metabolized within the body to release an active drug substance [1] [2]. This strategic approach is employed to overcome various barriers in drug delivery, such as poor solubility, low permeability, rapid metabolism, or significant side effects [3] [4]. The design of prodrugs allows for the optimization of a drug's absorption, distribution, metabolism, and excretion (ADME) properties, ultimately enhancing its therapeutic efficacy and safety profile [3].
Frequently Asked Questions (FAQs)
1. What are the main types of prodrugs? Prodrugs are primarily classified into two major types based on their site of activation [1]:
- Type I Prodrugs are bioactivated inside cells (intracellularly). Examples include anti-viral nucleoside analogs and lipid-lowering statins.
- Type II Prodrugs are bioactivated outside cells (extracellularly), such as in digestive fluids or the circulatory system. Salicin and certain antibody-directed enzyme prodrugs (ADEPT) used in chemotherapy are examples. Some prodrugs can belong to multiple subtypes, known as "Mixed-Type" prodrugs, which are bioactivated at multiple sites in parallel or sequential steps [1].
2. Why use a prodrug instead of the active drug? The prodrug strategy offers several key advantages [3] [4]:
- Improve Bioavailability: Enhancing the drug's absorption and the amount that reaches the systemic circulation.
- Enhance Solubility: Making a poorly water-soluble drug more soluble for better formulation and absorption.
- Increase Site-Specificity: Targeting the drug to a specific organ, tissue, or cell type to reduce off-target effects.
- Minimize Side Effects: Reducing toxicity, irritation, or unpleasant taste/orodor of the parent drug.
- Overcome Rapid Metabolism: Protecting the drug from being deactivated too quickly before it can exert its effect.
3. What are common functional groups used in prodrug design? Common bioreversible functional groups and their activating mechanisms include [4]:
- Esters and Carbonates: Activated by ubiquitous enzymes called esterases and carboxylesterases.
- Phosphates and Phosphonates: Cleaved by phosphatases to improve water solubility.
- Carbamates and Amides: Cleaved by esterases or peptidases.
- Oximes and Imines: Susceptible to chemical hydrolysis.
4. What challenges are associated with prodrug development? Despite their benefits, prodrug development faces several challenges [5] [4]:
- Variable Activation: Inefficient or inconsistent activation due to inter-individual variability in enzyme expression or activity.
- Formulation Stability: Potential for chemical instability of the prodrug or its degradation products.
- Toxic Metabolites: The promoiety (carrier group) released during activation could be toxic.
- Premature Activation: The prodrug might convert to the active drug before reaching its target site.
Troubleshooting Common Experimental Issues
Problem 1: Inconsistent or Inefficient Prodrug Activation
Potential Cause: Inter-individual variability in the expression or activity of the enzyme responsible for prodrug activation (e.g., due to genetic polymorphisms) [4]. Solution Strategies:
- Enzyme Activity Profiling: Characterize the specific enzyme(s) responsible for activation (e.g., carboxylesterases, phosphatases, cytochrome P450 enzymes) using in vitro assays with human liver microsomes, recombinant enzymes, or target cell lysates [3].
- Linker Optimization: If the prodrug is carrier-linked, explore different linker chemistries that are substrates for enzymes with less variable expression [6] [7].
- Consider Bioprecursor Prodrugs: Design bioprecursor prodrugs that are activated by multiple or more ubiquitous metabolic pathways to reduce reliance on a single enzyme [4].
Problem 2: Poor Aqueous Solubility of the Prodrug
Potential Cause: The prodrug itself, despite design intentions, may have inadequate solubility for in vitro testing or formulation [5] [8]. Solution Strategies:
- Ionizable Promoieties: Incorporate highly ionizable groups, such as phosphate or amino acids, which can increase aqueous solubility by orders of magnitude [8] [4]. For example, phosphate ester prodrugs like fosphenytoin show dramatically improved solubility over their parent drugs [8].
- Formulation Aids: Employ advanced formulation techniques such as the creation of nano-suspensions or the use of lipid-based delivery systems to enhance solubility [9].
- Solid Dispersions: Develop solid dispersions where the prodrug is dispersed within a hydrophilic polymer matrix to improve dissolution rate [9].
Problem 3: Chemical Instability of the Prodrug in Formulation
Potential Cause: The linker between the drug and the promoiety may be chemically unstable under storage conditions (e.g., susceptible to hydrolysis or oxidation) [5]. Solution Strategies:
- Linker Modification: Synthesize prodrug analogs with altered linkers that provide better chemical stability while maintaining efficient enzymatic cleavage [7]. For instance, a more sterically hindered ester may hydrolyze slower.
- Control Microenvironment: Use lyophilization (freeze-drying), adjust the pH of liquid formulations, or incorporate stabilizers like antioxidants to improve shelf-life [5] [9].
- Packaging Innovations: Utilize specialized packaging materials that provide barriers to moisture and oxygen [9].
Problem 4: Unexpected Toxicity or Off-Target Effects
Potential Cause: Premature release of the active drug in non-target tissues, or toxicity from the promoiety released upon activation [4]. Solution Strategies:
- Tissue-Targeted Design: Develop prodrugs that are activated by enzymes specifically overexpressed at the target site (e.g., tumor-specific enzymes for chemotherapy prodrugs) [3] [4].
- Stimuli-Responsive Linkers: Design linkers that are cleaved by unique stimuli in the target microenvironment, such as low pH (tumors, lysosomes) or high reactive oxygen species (ROS) levels [7] [4].
- Promoiety Selection: Evaluate the safety profile of different promoieties during the early design phase to select one with minimal toxicity [4].
Experimental Protocols for Prodrug Research
Protocol 1: Assessing Enzymatic Activation Kinetics
Objective: To determine the rate of conversion of a prodrug to its active metabolite by specific enzymes. Materials:
- Purified prodrug compound
- Source of enzyme (e.g., recombinant enzyme, liver microsomes, plasma, target cell lysate)
- Appropriate buffer (e.g., phosphate-buffered saline, pH 7.4)
- Water bath or incubator
- HPLC or LC-MS system for analysis
Methodology:
- Incubation Preparation: Prepare a solution of the prodrug in a suitable buffer. Pre-warm the solution in a water bath at 37°C.
- Initiate Reaction: Add the enzyme preparation to the pre-warmed prodrug solution to start the reaction. Include a negative control without the enzyme.
- Sampling: At predetermined time intervals (e.g., 0, 5, 15, 30, 60, 120 minutes), withdraw an aliquot from the incubation mixture.
- Reaction Termination: Immediately mix the aliquot with an equal volume of an organic solvent (e.g., acetonitrile) to denature the proteins and stop the reaction.
- Analysis: Centrifuge the samples to remove precipitated proteins. Analyze the supernatant using HPLC or LC-MS to quantify the remaining prodrug and the appearance of the active drug.
- Data Analysis: Plot the concentration of the active drug over time. Calculate the activation rate constant (k) or the half-life of conversion.
Protocol 2: Evaluating Solubility and Permeability
Objective: To measure the improvements in aqueous solubility and intestinal permeability afforded by the prodrug design. Materials:
- Prodrug and parent drug compounds
- Shaking water bath
- Caco-2 cell line (for permeability studies)
- Transwell plates
- HPLC system
Methodology:
- Aqueous Solubility:
- Add an excess amount of the prodrug to a vial containing a suitable aqueous buffer (e.g., pH 6.8 phosphate buffer to simulate intestinal fluid).
- Shake the vial in a water bath at 37°C for 24-48 hours to reach equilibrium.
- Filter or centrifuge the solution to remove undissolved material.
- Dilute the supernatant and analyze the drug concentration using HPLC. Compare with the solubility of the parent drug.
- Permeability (Caco-2 Model):
- Culture Caco-2 cells on semi-permeable membranes in Transwell plates until they form a confluent monolayer.
- Add the prodrug dissolved in buffer to the donor compartment (apical side for oral absorption studies).
- Incubate at 37°C. Sample from the receiver compartment (basolateral side) at regular intervals.
- Analyze samples by HPLC to determine the apparent permeability coefficient (Papp). A higher Papp value indicates better permeability.
Quantitative Data on Prodrug Performance
The following table summarizes how prodrug strategies have successfully improved the solubility of various parent drugs [8].
Table 1: Examples of Solubility Enhancement via Prodrug Design
| Parent Drug | Prodrug | Solubility of Parent Drug (mg/mL) | Solubility of Prodrug (mg/mL) |
|---|---|---|---|
| Phenytoin | Phenytoin Phosphate | 0.02 | 142 |
| Clindamycin | Clindamycin-2-PO4 | 0.2 | 150 |
| Chloramphenicol | Chloramphenicol Succinate Sodium | 2.5 | 500 |
| Paclitaxel | PEG-Paclitaxel | 0.025 | 666 |
Research Reagent Solutions
This table lists key reagents and materials essential for prodrug research and development.
Table 2: Essential Research Reagents for Prodrug Experiments
| Reagent/Material | Function in Prodrug Research |
|---|---|
| Carboxylesterases | Key enzymes for hydrolyzing ester-based prodrugs; used in in vitro activation studies [4]. |
| Liver Microsomes | Subcellular fractions containing cytochrome P450 enzymes and other metabolizing enzymes; used to study oxidative activation and metabolic stability [4]. |
| Caco-2 Cell Line | A model of the human intestinal epithelium; critical for assessing prodrug permeability and absorption potential [4]. |
| Alkaline Phosphatase | Enzyme used to study the activation of phosphate-containing prodrugs [8]. |
| HPMA Copolymer | A polymer used in the synthesis of polymer-drug conjugates and in Polymer-Directed Enzyme Prodrug Therapy (PDEPT) [8]. |
| Stimuli-Responsive Linkers | Linkers designed to break under specific conditions (e.g., low pH, high ROS); used to create targeted prodrugs [7]. |
Prodrug Activation and Pharmacokinetics
The diagram below illustrates the basic pharmacokinetic pathway of a prodrug after administration, leading to the release of the active drug and its subsequent elimination [10].
Rational Prodrug Design Workflow
This flowchart outlines a logical workflow for the rational design and evaluation of a prodrug, from identifying the problem to selecting an optimal candidate [3] [4].
Frequently Asked Questions (FAQs)
1. What is a prodrug and what is its primary purpose in drug development? A prodrug is a biologically inactive or minimally active compound that undergoes enzymatic or chemical transformation within the body to release the active parent drug [11] [3]. The primary purpose is to optimize the physicochemical, biopharmaceutical, and pharmacokinetic properties of drugs, thereby overcoming challenges related to poor solubility, low permeability, high toxicity, and inadequate site-specificity [11] [12] [3]. It is a versatile strategy to improve drug delivery and therapeutic outcomes.
2. When should a researcher consider the prodrug approach for a lead compound? The prodrug approach should be considered when a pharmacologically active lead compound exhibits undesirable properties that hinder its clinical or commercial development. Key indicators include:
- Poor aqueous solubility, leading to formulation challenges and low bioavailability [11] [13].
- Low permeability, resulting in insufficient absorption and failure to reach intracellular targets [12] [13].
- Systemic toxicity or lack of target selectivity, particularly for chemotherapeutic agents [14] [15].
- Rapid pre-systemic metabolism, which shortens the drug's half-life and reduces exposure [3] [16].
3. What are the common functional groups and enzymes involved in prodrug activation? Common bioreversible functional groups used to link a drug to a carrier include esters, amides, carbonates, carbamates, and phosphates [11] [16]. These are typically activated by hydrolytic enzymes such as:
- Esterases: Found in plasma, liver, and other tissues, they are frequently targeted for hydrolyzing ester-based prodrugs [16].
- Phosphatases: Activate phosphate prodrugs [3].
- Peptidases and Proteases: Activate prodrugs designed with amino acid or peptide linkers, such as Valacyclovir, which is activated by human valacyclovirase [11] [3].
- Nitroreductases: Can activate nitroaromatic prodrugs, as seen in hypoxia-activated prodrugs [17].
- Cytochrome P450 enzymes: Often involved in the activation of bioprecursor prodrugs via oxidation or reduction reactions [16].
4. What are the major formulation challenges associated with prodrug development? Formulating prodrugs presents unique challenges, including:
- Chemical Instability: The drug-promoiety linker may be unstable, leading to premature degradation during storage or before reaching the target site [5].
- Reactive Degradation By-products: Degradation can generate reactive intermediates that may cause secondary degradation pathways or pose toxicity risks [5].
- Altered Solid-State Properties: The prodrug may exhibit different crystallinity, polymorphism, or hygroscopicity compared to the parent drug, complicating solid dosage form development [5].
- Solubility of Degradants: The aqueous solubility of the prodrug's degradation products must be considered to avoid precipitation in formulations [5].
Troubleshooting Guides
Issue 1: Poor Aqueous Solubility of Lead Compound
Problem: Your active pharmaceutical ingredient (API) has unacceptably low aqueous solubility, leading to poor dissolution and low oral bioavailability.
Solution: Design a water-soluble prodrug by attaching a hydrophilic promotety.
- Recommended Strategy: Synthesize phosphate ester or amino acid ester prodrugs. These groups significantly enhance aqueous solubility [11].
- Experimental Validation Protocol:
- Synthesis: Conjugate a phosphate group or an amino acid (e.g., valine, glycine) to the API via a biodegradable ester or other suitable linker [11].
- Solubility Measurement:
- Prepare a saturated solution of the prodrug in a suitable aqueous buffer (e.g., pH 7.4 phosphate buffer).
- Shake the mixture for a predetermined time (e.g., 24 hours) at a constant temperature (e.g., 37°C).
- Filter the solution through a 0.45 μm membrane filter.
- Analyze the concentration of the dissolved prodrug in the filtrate using a validated UV-Vis spectrophotometric or HPLC method [11].
- Chemical Stability Assessment:
Table 1: Examples of Prodrugs for Solubility Enhancement
| Parent Drug (Issue) | Prodrug Strategy | Resulting Improvement | Reference |
|---|---|---|---|
| Palmarumycin CP1 (High lipophilicity) | Glycyl ester derivative | >7-fold increase in water solubility | [11] |
| Oleanolic Acid (Solubility: 0.0012 μg/mL) | l-Valine ethylene-glycol-linked diester | Solubility >25 μg/mL; Increased oral bioavailability in rats | [11] |
| MSX-2 (A2A antagonist, low solubility) | Phosphate prodrug | Water solubility of 9.0 mg/mL | [11] |
| Antiviral Cf1743 (Low solubility) | Dipeptide prodrug (Val, Asn, Lys, Asp) | 4000-fold greater solubility; 7-15-fold greater bioavailability | [11] |
Issue 2: Low Permeability and Oral Absorption
Problem: Your API is sufficiently soluble but fails to cross biological membranes effectively, resulting in low oral absorption.
Solution: Design a prodrug to increase lipophilicity or to be recognized by active influx transporters.
- Recommended Strategy:
- Esterification: For drugs with carboxylic acid groups, create simple alkyl esters (e.g., ethyl ester) to enhance passive permeability [13].
- Transporter Targeting: For drugs with suitable handles, design prodrugs that are substrates for intestinal uptake transporters, such as the human peptide transporter 1 (hPEPT1), using amino acid or dipeptide promoieties [12] [3] [13].
- Experimental Validation Protocol:
- Lipophilicity Assessment:
- Determine the apparent partition coefficient (Log P) or distribution coefficient (Log D) at pH 7.4 for the prodrug and parent drug using the shake-flask method and n-octanol/water buffer systems.
- Analyze the samples by HPLC-UV to calculate the concentration in each phase. An increase in Log P/Log D indicates enhanced lipophilicity [12].
- Permeability Screening (In Vitro):
- Use Caco-2 or MDCK cell monolayers grown on permeable transwell supports.
- Add the prodrug to the donor compartment (e.g., apical side for oral absorption studies) and measure its appearance in the receiver compartment over time.
- Calculate the apparent permeability coefficient (Papp). A higher Papp for the prodrug compared to the parent API indicates improved permeability [12] [13].
- Transporter Interaction Studies:
- Perform the Caco-2 permeability assay in the presence and absence of a specific transporter inhibitor (e.g., glycylsarcosine for hPEPT1).
- A significant reduction in the Papp of the prodrug in the presence of the inhibitor confirms transporter-mediated uptake [13].
- Lipophilicity Assessment:
Table 2: Prodrug Strategies to Overcome Poor Permeability
| Parent Drug (BCS Class) | Prodrug Strategy | Mechanism of Improvement | Key Outcome |
|---|---|---|---|
| Acyclovir (Class III/IV) | Valacyclovir | hPEPT1 transporter-mediated absorption | 3-5 fold increase in bioavailability [3] |
| SNX-2112 (Low solubility/permeability) | SNX-5422 (Glycine derivative) | Increased solubility and lipophilicity (pKa tuning) | Bioavailability increased from ~40% to ~80% in mice [13] |
| Melagatran (Low permeability) | Ximelagatran (N-hydroxyamidine) | Reduced basicity (pKa ~5) enhancing passive diffusion | Bioavailability increased from 6% to 20% in humans [13] |
| Tricin (Flavonoid) | Alanine-Glutamic acid dipeptide prodrug | Targeting hPEPT1 transporter | 45-fold greater exposure in rats [13] |
Issue 3: Off-Target Toxicity and Lack of Selectivity
Problem: Your API is potent but causes systemic side effects due to a lack of specificity for its intended target, such as in cancer therapy.
Solution: Design a prodrug that remains inactive until it reaches the target site, where a unique trigger (e.g., enzyme, pH, light) catalyzes its activation.
- Recommended Strategies:
- Enzyme-Activated Prodrugs: Leverage enzymes overexpressed in target tissues (e.g., glutathione S-transferases, β-lyases, or nitroreductases in some tumors) [14] [17].
- Hypoxia-Activated Prodrugs (HAPs): Utilize the hypoxic environment of solid tumors for selective activation via nitroreduction [17].
- Bioorthogonal Activation: Use external triggers like near-infrared (NIR) light to activate prodrugs containing photolabile linkers (e.g., thioketal) [15].
- Experimental Validation Protocol:
- In Vitro Selectivity and Potency:
- Activation Kinetics:
- In Vivo Efficacy and Toxicity:
- Administer the prodrug and the parent API to animal models (e.g., tumor-bearing mice) at equimolar doses.
- Evaluate efficacy by measuring tumor growth inhibition.
- Assess toxicity by monitoring body weight, organ histology, and biomarkers (e.g., gastrointestinal toxicity). A successful prodrug will show similar or better efficacy with significantly reduced toxicity [14] [15].
Experimental Protocols for Key Assays
Protocol 1: Determining Apparent Permeability (Papp) in Caco-2 Cells
Objective: To evaluate the ability of a prodrug to cross intestinal epithelial cell barriers and assess the involvement of active transporters.
Materials:
- Caco-2 cell line
- Transwell plates (e.g., 12-well, 0.4 μm pore size)
- Transport buffer (e.g., HBSS with 10 mM HEPES, pH 7.4)
- Test compounds (Prodrug and parent drug)
- Transporter inhibitors (e.g., Glycylsarcosine for hPEPT1)
- HPLC system with UV or MS detection
Method:
- Cell Culture: Seed Caco-2 cells on transwell inserts at a high density and culture for 21 days to allow full differentiation and expression of transport proteins. Confirm monolayer integrity by measuring transepithelial electrical resistance (TEER > 300 Ω×cm²).
- Experiment Setup: Pre-wash the monolayers with transport buffer. Add the test compound to the donor compartment (e.g., apical for A-to-B transport). Add fresh buffer to the receiver compartment (basolateral).
- Sampling: Incubate at 37°C with gentle shaking. Collect samples from the receiver compartment at regular intervals (e.g., 30, 60, 90, 120 min) and replace with fresh buffer.
- Analysis: Quantify the compound concentration in all samples using HPLC.
- Calculation: Calculate the Papp (cm/s) using the formula: Papp = (dQ/dt) / (A × C₀), where dQ/dt is the flux rate (mol/s), A is the membrane surface area (cm²), and C₀ is the initial donor concentration (mol/mL) [12] [13].
Protocol 2: Evaluating Enzymatic Prodrug Activation
Objective: To demonstrate and quantify the conversion of a prodrug to its active parent drug by a specific enzyme.
Materials:
- Purified enzyme (e.g., esterase, phosphatase, nitroreductase) or target cell/tissue lysate
- Prodrug solution
- Appropriate incubation buffer (e.g., phosphate buffer, pH 7.4)
- Co-factors (e.g., NADPH for nitroreductases)
- Water bath or incubator shaker (37°C)
- HPLC or LC-MS system
Method:
- Incubation: Prepare a solution of the prodrug in the incubation buffer. Add the enzyme or lysate to initiate the reaction. Include a control without the enzyme.
- Time Course: Incubate the mixture at 37°C. Withdraw aliquots at predetermined time points (e.g., 0, 5, 15, 30, 60 min) and immediately quench the reaction (e.g., by adding ice-cold acetonitrile or acid).
- Sample Preparation: Centrifuge the quenched samples to precipitate proteins. Collect the supernatant for analysis.
- Analysis: Inject the supernatants into the HPLC/LC-MS system to separate and quantify the remaining prodrug and the generated parent drug.
- Data Analysis: Plot the concentration of the parent drug versus time. Calculate the activation half-life and the Michaelis-Menten parameters (Km and Vmax) if using a purified enzyme system [14] [16] [17].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Prodrug Research and Development
| Reagent / Material | Function in Prodrug Research | Example Application |
|---|---|---|
| Caco-2 Cell Line | An in vitro model of the human intestinal epithelium to assess permeability and transporter involvement. | Screening prodrug permeability and confirming hPEPT1-mediated uptake [12] [13]. |
| Esterases (e.g., from porcine liver) | Hydrolytic enzymes used to study the activation kinetics of ester-based prodrugs. | Evaluating the conversion of valine-ester prodrugs to their parent drugs [11] [16]. |
| Diboron Reagents (e.g., B2(OH)4) | Bioorthogonal reducing agents used in conjunction with organocatalysts for controlled prodrug activation. | Activating nitroaromatic prodrugs in cellular and animal models [17]. |
| 4,4'-Bipyridine | An organocatalyst that mediates bioorthogonal nitro-reduction with diboron reagents. | Enabling metal-free, controlled activation of prodrugs in biological systems [17]. |
| Specific Transporter Inhibitors | Pharmacological tools to confirm the role of specific influx transporters in prodrug uptake. | Using glycylsarcosine to inhibit hPEPT1 and validate transporter-targeted design [13]. |
Workflow and Pathway Visualizations
Prodrug Optimization Workflow
Prodrug Activation Pathway
Frequently Asked Questions
Q1: What are the fundamental differences between carrier-linked prodrugs and bioprecursors?
Carrier-linked prodrugs consist of an active parent drug covalently linked to a carrier group (or promoiety) through a biodegradable linkage such as an ester or amide bond [18] [11]. The carrier is typically chosen to modify the drug's physicochemical properties. In contrast, bioprecursor prodrugs do not contain a carrier group but are inactive molecules that undergo molecular modification via metabolic reactions (often redox or conjugation reactions) to generate the active drug [18] [11]. They are essentially substrates for metabolic enzymes.
Q2: How does the Type I/II classification system relate to these structural classifications?
The Type I/II system classifies prodrugs based on their site of activation, whereas carrier-linked and bioprecursor are structural classifications. A single structural class can often fall into either activation type, as shown in the table below [19].
Table 1: Interrelationship Between Prodrug Classification Systems
| Activation Site / Structural Type | Carrier-Linked Prodrug | Bioprecursor Prodrug |
|---|---|---|
| Type I: Intracellular Activation | Levodopa (L-DOPA) [4] | Codeine (converted to morphine by CYP2D6) [19] [20] |
| Type II: Extracellular Activation | Valacyclovir (activated in intestine/liver) [3] [19] | Sulfasalazine (activated by gut bacteria) [20] |
Q3: What are the most common functional groups used in designing carrier-linked prodrugs?
Ester bonds are the most prevalent, accounting for over 50% of marketed prodrugs [18]. Other common functional groups include carbonates, carbamates, amides, and phosphates. The choice of group depends on the desired hydrolysis rate, stability, and the enzyme responsible for activation [18] [4].
Table 2: Common Functional Groups in Carrier-Linked Prodrugs
| Functional Group | Key Feature | Example Prodrug (Active Drug) |
|---|---|---|
| Ester | Hydrolyzed by ubiquitous esterases; most common approach [18]. | Oseltamivir (Oseltamivir carboxylate) [18] [4] |
| Phosphate/Ester | Greatly enhances water solubility; activated by phosphatases [18] [4]. | Fosphenytoin (Phenytoin) [18] |
| Amide | More stable than esters; can be designed for transporter targeting [18]. | LY544344 (LY35470) [18] |
| Carbamate | Stable against hydrolysis; often used for sustained release [4]. | Irinotecan (SN-38) [19] [4] |
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent or Incomplete Prodrug Activation
Potential Cause: Variability in enzyme expression or activity. Enzymes like carboxylesterases, phosphatases, and cytochrome P450 isoforms can have significant inter-individual variability due to genetics, drug interactions, or disease states [4].
Solution:
- Characterize Enzyme Kinetics: Determine the Michaelis-Menten constants (Km and Vmax) for the enzymatic conversion of your prodrug using in vitro systems (e.g., liver microsomes, human plasma, or specific recombinant enzymes) [18].
- Use Genotyped Tissues/Enzymes: If a polymorphic enzyme (e.g., CYP2D6 or CYP2C19) is involved, use characterized enzyme sources to understand the impact of genetics on activation rate [19].
- Validate In Vitro-In Vivo Correlation (IVIVC): Ensure your chosen in vitro activation system reliably predicts in vivo behavior.
Experimental Protocol: Assessing Metabolic Stability and Activation in Plasma
Objective: To evaluate the in vitro stability and conversion rate of a prodrug in plasma, which contains various hydrolytic enzymes.
Materials:
- Prodrug compound
- Blank plasma (from relevant species, e.g., rat, human)
- Incubation buffer (e.g., phosphate-buffered saline, PBS)
- Precipitation agent (e.g., acetonitrile with internal standard)
- Water bath or incubator (maintained at 37°C)
- Centrifuge
- Analytical instrument (e.g., LC-MS/MS)
Method:
- Preparation: Pre-warm plasma in a water bath at 37°C for 10 minutes. Prepare a stock solution of the prodrug in a suitable solvent (e.g., DMSO), then dilute in pre-warmed buffer.
- Incubation: Initiate the reaction by mixing the prodrug solution with plasma to achieve a final concentration relevant to your study (e.g., 1 µM). Vortex immediately.
- Sampling: At predetermined time points (e.g., 0, 5, 15, 30, 60, 120 minutes), withdraw an aliquot (e.g., 50 µL) and immediately mix with a cold precipitation agent (e.g., 150 µL acetonitrile) to stop the reaction.
- Processing: Centrifuge the samples (e.g., 13,000 rpm for 10 minutes) to precipitate proteins. Transfer the clear supernatant to vials for analysis.
- Analysis: Quantify the concentrations of the remaining prodrug and the formed active drug using a validated analytical method (e.g., LC-MS/MS).
Interpretation: Plot the decline of prodrug and the appearance of the active drug over time. Calculate the half-life (t~1/2~) of the prodrug and the conversion rate.
Challenge 2: Poor Aqueous Solubility of the Parent Drug Leading to Formulation Difficulties
Solution: Implement a water-solubilizing promoiety strategy. Common groups include phosphate esters, amino acids, and polyethylene glycol (PEG) chains [18] [11].
Experimental Protocol: Kinetic Aqueous Solubility Assay
Objective: To compare the aqueous solubility of a parent drug and its prodrug derivative.
Materials:
- Test compounds (Parent drug and prodrug)
- Aqueous buffer (e.g., PBS at pH 7.4)
- Thermostated shaker or bath (37°C)
- Centrifuge and filter plates (e.g., 0.45 µm pore size)
- Analytical instrument (e.g., HPLC-UV)
Method:
- Saturation: Add an excess of solid compound to a known volume of buffer in a vial. Shake vigorously for 24 hours at 37°C to achieve equilibrium.
- Separation: Centrifuge the samples or pass them through a pre-warmed filter plate to separate the undissolved solid from the saturated solution.
- Quantification: Dilute the clear supernatant appropriately and analyze the concentration of the dissolved compound using a validated HPLC-UV method. A standard curve of the compound in a known solvent is required for quantification.
Interpretation: The concentration measured in the saturated solution is the kinetic solubility. A successful solubilizing prodrug will show a significant (e.g., 10 to 1000-fold) increase in solubility compared to the parent drug [11].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Prodrug Metabolism and Analysis Studies
| Reagent / Material | Function in Prodrug Research |
|---|---|
| Liver Microsomes (Human/Rat) | Contains cytochrome P450 enzymes and other Phase I metabolizing enzymes; used to study oxidative activation of bioprecursors [4]. |
| Recombinant Enzymes (e.g., hCE1, hCE2) | Specific carboxylesterases for characterizing ester-based prodrug activation kinetics and enzyme specificity [18]. |
| Caco-2 Cell Line | A model of human intestinal permeability; used to assess carrier-linked prodrug absorption and transporter involvement [3]. |
| Plasma (Various Species) | Source of hydrolytic enzymes (esterases, phosphatases) for evaluating the stability and activation of prodrugs in systemic circulation [18]. |
| Specific Chemical Inhibitors | Inhibitors for enzymes like CYP450s or esterases to confirm the metabolic pathway responsible for prodrug activation [4]. |
Prodrugs, defined as biologically inactive compounds that undergo conversion into active pharmaceuticals within the body, have evolved from a serendipitous discovery to a cornerstone of rational drug design [3] [21]. This strategy is instrumental in overcoming common drug development hurdles, such as poor solubility, inadequate permeability, and suboptimal pharmacokinetics [22] [12]. For researchers and drug development professionals, understanding the prevalence and impact of prodrugs is crucial for guiding molecular optimization processes. This technical resource provides a data-driven analysis of the prodrug market, supported by experimental insights and troubleshooting guides relevant to prodrug design and formulation research.
Quantitative Analysis of Prodrug Approvals
The prodrug approach represents a significant and growing segment of the pharmaceutical market. The quantitative data below underscores its substantial impact.
Table 1: Prevalence of Prodrugs in FDA-Approved New Molecular Entities [22] [23] [24]
| Time Period | Total FDA-Approved Small Molecule NMEs | Number of Prodrugs | Percentage of Prodrugs |
|---|---|---|---|
| 2008 - 2018 | ~249 | At least 30 | ~12% |
| 2012 - 2022 | Information Missing | Information Missing | ~13% |
| 2015 | 32 | 7 | ~20% |
| 2010 - 2014 | 127 | 13 | ~10.2% |
Table 2: Global Prodrug Research Activity (2014-2024) [22] [25]
| Research Activity Metric | Annual Average (Last Decade) | Recent Peak (2023) |
|---|---|---|
| Global Patent Applications | > 4,800 | 5,730 |
| Scientific Publications | ~ 1,261 | Information Missing |
Overall, it is estimated that approximately 10% of all commercially available medicines worldwide are prodrugs [3] [21] [24]. The therapeutic areas dominating recent clinical trials for prodrugs include cancer (35%), central nervous system disorders (16%), and antiviral therapies (14%) [22] [25].
FAQs & Troubleshooting Guides for Prodrug Research
FAQ 1: What are the primary strategic goals when designing a prodrug?
The prodrug strategy is employed to achieve several key objectives [12] [3]:
- Enhancing Bioavailability: This is the most common goal, primarily achieved by improving a drug's solubility and membrane permeability. A review of prodrug design goals found that 59% were aimed at enhancing bioavailability, with 35% targeting permeability and 15% targeting solubility improvements [12].
- Achieving Site-Specific Targeting: Modern prodrugs can be designed to exploit specific enzymes or transporters that are overexpressed in target tissues, such as tumors or sites of inflammation, thereby reducing systemic toxicity [3].
- Overcoming Rapid Metabolism: Chemical moieties like carbamates and amides can be used to shield a drug from extensive first-pass metabolism, thereby increasing its systemic exposure [22].
- Reducing Toxicity and Side Effects: By masking the active drug until it reaches the site of action, prodrugs can minimize off-target effects and improve patient tolerability [3] [21].
FAQ 2: Which functional groups are most commonly used in prodrug clinical trials and why?
The selection of a promoiety is guided by the desired pharmacokinetic profile, particularly the kinetics of enzymatic hydrolysis.
Table 3: Common Promoieties in Prodrugs (2014-2024 Clinical Trials) [22]
| Promoiety | Prevalence in Clinical Trials | Hydrolysis Kinetics & Key Applications |
|---|---|---|
| Ester | 27% | Rapid hydrolysis; widely used to improve lipophilicity and absorption. |
| Phosphate | 27% | Rapid hydrolysis; primarily used to enhance aqueous solubility. |
| Amide | 12% | Slower, more stable hydrolysis; useful for moderating rapid metabolism. |
| Carbamate | 6% | Slower, more stable hydrolysis; useful for moderating rapid metabolism. |
| Salts | 8% | Not a promoiety per se, but used with prodrugs to improve solubility and crystallinity. |
Troubleshooting Guide: Addressing Inconsistent Activation of Ester-Based Prodrugs
Problem: An ester prodrug demonstrates excellent in vitro permeability but shows variable and low efficacy in in vivo models, suggesting inconsistent activation.
Investigation and Solutions:
- Potential Cause 1: Enzyme Polymorphism. The activating enzyme (e.g., carboxylesterase) may have genetic polymorphisms leading to variable expression or activity across a population [23] [21].
- Solution: Conduct in vitro metabolism studies using human hepatocytes from multiple donors. During early development, perform pharmacogenomic screening to identify susceptible populations.
- Potential Cause 2: Drug-Drug Interactions (DDIs). Coadministered drugs may inhibit the enzymes required for prodrug activation.
- Solution: A classic example is the interaction between clopidogrel (prodrug) and omeprazole, which inhibits the CYP2C19 enzyme required for activation [21]. During preclinical development, screen for DDIs using recombinant enzymes and human liver microsomes.
- Potential Cause 3: Saturation of Activation Pathway. The enzymatic conversion may be saturable at higher doses, leading to non-linear pharmacokinetics.
- Solution: Perform dose-ranging studies in animal models to characterize the saturation kinetics and adjust the dosing regimen accordingly.
FAQ 3: How is permeability assessed during prodrug development?
Permeability is a critical parameter for prodrug success. Researchers use a combination of methods to evaluate it [12]:
- In Silico Methods: Computational models use filters like the "Rule of Five" and calculate parameters like logP (partition coefficient) to predict permeability during early-stage design [12].
- In Vitro Models: Cell-based assays, particularly Caco-2 cell monolayers, are the gold standard for determining the apparent permeability coefficient (Papp) of a prodrug candidate.
- Ex Vivo and In Situ Methods: Techniques like gut sacs and intestinal perfusion provide more physiologically relevant data on effective permeation (Peff).
Diagram: Workflow for Evaluating Prodrug Permeability
The Scientist's Toolkit: Key Research Reagents & Materials
Table 4: Essential Reagents for Prodrug Research and Development
| Reagent / Material | Function in Prodrug R&D |
|---|---|
| Caco-2 Cell Line | An immortalized cell line from human colon adenocarcinoma used as an in vitro model of the human intestinal mucosa to assess permeability and transport mechanisms [12]. |
| Human Hepatocytes | Primary liver cells used to study first-pass metabolism and enzymatic activation (or deactivation) of prodrug candidates, crucial for predicting in vivo performance [23]. |
| Recombinant Metabolic Enzymes (e.g., CYP450 isoforms, CES1/2) | Used to identify the specific enzymes responsible for prodrug activation, enabling screening for polymorphisms and potential drug-drug interactions [21]. |
| Specific Transporter-Expressing Cell Lines (e.g., hPEPT1, OATP) | Engineered cell lines that overexpress specific uptake transporters. They are vital for developing targeted prodrugs that utilize carrier-mediated transport, like valacyclovir [3]. |
| Simulated Biological Fluids (e.g., SGF, SIF) | Used in dissolution testing to evaluate the chemical stability and release profile of the prodrug in various regions of the gastrointestinal tract. |
Case Study: Mechanism of Valacyclovir Activation
Valacyclovir is a successful prodrug of acyclovir, designed to overcome poor oral bioavailability.
Diagram: Mechanism of Valacyclovir Activation and Targeting
Experimental Insight: The high bioavailability of valacyclovir is achieved through a "double-targeted" approach [3]:
- Transporter-Mediated Absorption: The prodrug is efficiently absorbed across the intestinal epithelium by the human peptide transporter 1 (hPEPT1).
- Enzyme-Mediated Activation: Once inside the cell, it is rapidly hydrolyzed by the enzyme human valacyclovirase to release acyclovir.
This case highlights the importance of considering both transport and enzymatic activation pathways in the rational design of modern prodrugs.
Design and Application: Chemical Strategies and Real-World Case Studies
FAQs and Troubleshooting Guides
Fischer Esterification
Q: My Fischer esterification reaction is yielding very little product. What could be the cause and how can I improve the yield?
A: The Fischer esterification is an equilibrium reaction, and low yields are often due to the equilibrium favoring the starting materials. To drive the reaction toward ester formation:
- Use a large excess of your alcohol reactant. One study showed that increasing the ethanol to acetic acid ratio from 1:1 to 10:1 improved the ester yield from 65% to 97% [26].
- Remove water from the reaction mixture as it forms. Employ a Dean-Stark trap, which allows for the continuous azeotropic removal of water, preventing the reverse hydrolysis reaction and shifting the equilibrium [26] [27].
- Ensure you are using a strong acid catalyst like concentrated sulfuric acid or toluenesulfonic acid (TsOH) [26] [27].
Q: Can I use phenolic alcohols or tertiary alcohols in a Fischer esterification?
A: This is a significant limitation of the method.
- Phenol esters are difficult to form because phenol is a weaker nucleophile compared to typical alcohols, a problem exacerbated in acidic conditions [27].
- Tertiary alcohols are generally not suitable because they readily undergo dehydration to alkenes under the strong acidic conditions required for the reaction [27]. For both scenarios, alternative strategies such as using more reactive acid chlorides or carboxylate salts with alkyl halides are recommended [27].
Phosphorylation
Q: I am performing an enzymatic phosphorylation of an oligonucleotide using T4 Polynucleotide Kinase (PNK) and getting few or no transformants. What should I troubleshoot?
A: This is a common issue in molecular biology workflows. The causes and solutions are summarized in the table below [28].
| Problem | Cause | Solution |
|---|---|---|
| Inefficient Phosphorylation | Impurities in DNA substrate (salt, phosphate, ammonium ions) inhibiting the kinase. | Purify the DNA substrate prior to the phosphorylation reaction. |
| Blunt or 5' recessed DNA ends. | Heat the DNA substrate with buffer for 10 minutes at 70°C, then rapidly chill on ice before adding ATP and enzyme. | |
| Missing ATP. | Add ATP to a final concentration of 1 mM. Alternatively, use T4 DNA Ligase Buffer which contains ATP. |
Q: When mapping protein phosphorylation sites with mass spectrometry (MS), I have low coverage and can't locate the precise modified residue. How can I improve my results?
A: Phosphorylation site mapping by MS has several inherent challenges. Key strategies to overcome them include [29]:
- Use Multiple Proteases: Trypsin is the most common protease, but it may not generate ideal peptides from all protein regions. Using a second enzyme like GluC or chymotrypsin can dramatically improve sequence coverage.
- Account for Low Stoichiometry: The detected phosphorylation may be at a very low level and not biologically relevant. Employ quantitative MS methods (e.g., SILAC, isobaric tags) to measure phosphorylation stoichiometry and focus on sites that change under relevant conditions.
- Address Ambiguous Site Localization: When phosphorylation sites are close together, MS/MS spectra may not have enough information to pinpoint the exact residue. Use scoring algorithms like the Ascore to statistically evaluate site-assignment confidence.
Carrier-Linkage for Prodrugs
Q: What are the key considerations when designing a water-soluble carrier-linked prodrug?
A: An ideal prodrug should balance stability and activation [11]:
- Promoter Stability: The prodrug must be stable enough to survive absorption but must efficiently release the active drug at the target site.
- Aqueous Solubility: The carrier (e.g., phosphate group, amino acid) should significantly improve the parent drug's water solubility.
- Targeted Activation: The linker should be designed for enzymatic cleavage at the site of action. For example, using a dipeptide carrier that is a substrate for dipeptidyl-peptidase IV (DPPIV) can facilitate activation in specific tissues [11].
Q: Which chemical carriers are most effective for improving water solubility?
A: Ester-linked carriers, particularly phosphate groups and amino acids, are highly effective. The table below summarizes successful examples from recent research.
| Parent Drug (Issue) | Prodrug Carrier | Solubility Improvement & Key Outcomes | Citation |
|---|---|---|---|
| MSX-2 (Low solubility) | L-Valine ester | Solubility: 7.3 mg/mL (vs. less soluble parent). Stable in solution, rapid enzyme-triggered release. | [11] |
| Cf1743 (Low solubility & bioavailability) | Dipeptide ester (Valine-based) | Solubility: >4000-fold increase. Bioavailability: 7-15 fold higher than parent drug. | [11] |
| Oleanolic Acid (Low solubility & bioavailability) | L-Valine-ethylene glycol diester | Solubility: Increased from 0.0012 µg/mL to >25 µg/mL. Enhanced oral bioavailability in rats. | [11] |
| Palmarumycin CP1 (High lipophilicity) | Glycine ester | Solubility: >7 times more soluble in water than parent drug. | [11] |
Experimental Protocols
Detailed Protocol: Standard Fischer Esterification
This protocol describes the synthesis of an ester from a carboxylic acid and a primary or secondary alcohol using an acid catalyst [26] [27].
Reagent Solutions:
- Carboxylic Acid Substrate
- Alcohol (e.g., ethanol, methanol) - used in excess as solvent
- Acid Catalyst - concentrated sulfuric acid (H₂SO₄) or p-toluenesulfonic acid (TsOH)
- Saturated Sodium Bicarbonate (NaHCO₃) solution
- Anhydrous Salt - e.g., magnesium sulfate (MgSO₄) or sodium sulfate (Na₂SO₄)
- Extraction Solvents - Diethyl ether or ethyl acetate, and brine
Methodology:
- Reaction Setup: In a round-bottom flask, combine the carboxylic acid (1.0 equivalent) with a large excess of the alcohol (e.g., 10-100 equivalents). Slowly add a catalytic amount of concentrated sulfuric acid (e.g., 0.1 equivalents) while stirring.
- Reflux: Attach a reflux condenser and heat the mixture to reflux for 1-8 hours. For higher yields: Use a Dean-Stark trap in place of the condenser to remove water azeotropically.
- Reaction Work-up: After cooling, carefully neutralize the mixture by adding a saturated sodium bicarbonate solution slowly until CO₂ evolution ceases and the aqueous layer is basic.
- Extraction: Transfer the mixture to a separatory funnel. Extract the ester from the aqueous layer with an organic solvent (e.g., diethyl ether, 3 x 15 mL). Wash the combined organic layers with brine to remove residual water.
- Drying and Concentration: Dry the organic layer over an anhydrous salt like MgSO₄. Filter off the solid and concentrate the filtrate under reduced pressure using a rotary evaporator to obtain the crude ester.
- Purification: Purify the crude product by distillation or column chromatography as needed.
Detailed Protocol: Mapping Phosphorylation Sites by Mass Spectrometry
This workflow outlines the key steps for identifying serine, threonine, or tyrosine phosphorylation on a protein of interest [29].
Reagent Solutions:
- Purified Protein of Interest
- Protease - Trypsin (most common), Lys-C, GluC, or Chymotrypsin
- Liquid Chromatography-Tandem Mass Spectrometer (LC-MS/MS)
- Phosphopeptide Enrichment Resins - e.g., TiO₂, IMAC, Phos-Tag
- Lysis/Wash Buffers - Suitable for the protein and protease
- Stable Isotope Labels (for quantification) - SILAC amino acids or chemical tags (e.g., iTRAQ, TMT)
Methodology:
- Protein Digestion: Denature and digest the purified protein with a sequence-specific protease (e.g., trypsin) to generate a mixture of peptides.
- Phosphopeptide Enrichment (Optional but Recommended): To reduce sample complexity and increase sensitivity, enrich the peptide mixture for phosphopeptides using affinity resins like titanium dioxide (TiO₂) or immobilized metal affinity chromatography (IMAC).
- LC-MS/MS Analysis: Separate the peptides using nano-liquid chromatography and analyze them by tandem mass spectrometry. The instrument will measure the mass of intact peptides (MS1) and then fragment selected ions to obtain sequence data (MS2).
- Database Search and Site Localization: Use search algorithms (e.g., MaxQuant, SEQUEST) to match the experimental MS/MS spectra against theoretical spectra from a protein database, accounting for potential phosphorylation. Apply localization scoring algorithms (e.g., Ascore) to assign the specific modified residue with a confidence score.
- Validation (Crucial): Confirm the functional relevance of identified sites by mutating the phosphorylated residue (e.g., to alanine) and assessing the functional or phenotypic consequences in a biological assay.
Signaling Pathways and Workflow Visualizations
Prodrug Activation via Enzyme-Triggered Hydrolysis
This diagram illustrates the general mechanism for a carrier-linked bipartite prodrug, where an enzyme cleaves the carrier group to release the active drug.
Phosphorylation Site Mapping Workflow
This flowchart outlines the core steps for identifying protein phosphorylation sites using mass spectrometry.
Fischer Esterification Mechanism
This diagram details the step-by-step mechanism (PADPED) for the acid-catalyzed esterification of a carboxylic acid.
The Scientist's Toolkit: Research Reagent Solutions
This table details essential reagents used in the featured chemical techniques and their primary functions in a research setting.
| Reagent / Enzyme | Primary Function in Research | Key Application Context |
|---|---|---|
| T4 Polynucleotide Kinase (PNK) | Catalyzes the transfer of a phosphate group from ATP to the 5' terminus of DNA/RNA. | Phosphorylation of oligonucleotides for molecular biology techniques like ligation and labeling [28]. |
| Trypsin / Lys-C | Proteases that cleave proteins at specific amino acid residues (C-terminal to Lys/Arg) to generate peptides for MS analysis. | Protein digestion for bottom-up proteomics and phosphorylation site mapping [29]. |
| Acid Catalysts (H₂SO₄, TsOH) | Protonate the carbonyl oxygen of a carboxylic acid, making it more electrophilic and catalyzing the reaction with an alcohol. | Fischer esterification reaction to form ester bonds [26] [27]. |
| Dipeptidyl-peptidase IV (DPPIV) | A cell-surface enzyme that cleaves dipeptides from the N-terminus of proteins. Used as a target for activation. | Designed cleavage of dipeptide-linked prodrugs for targeted drug release, e.g., in leukocytes [11]. |
| Dean-Stark Apparatus | A laboratory technique for the continuous removal of water from a reaction mixture via azeotropic distillation. | Driving equilibrium in reversible reactions like Fischer esterification toward product formation [26]. |
| Stable Isotope Tags (SILAC, iTRAQ) | Allow for accurate relative quantification of peptides/proteins between different samples by mass spectrometry. | Determining phosphorylation stoichiometry and identifying dynamically regulated phosphorylation sites [29]. |
Enhancing Membrane Permeability and Oral Bioavailability
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary biological barriers that limit oral drug bioavailability? Oral drug bioavailability is primarily limited by a series of physiological barriers within the gastrointestinal tract (GIT). These can be categorized as follows [30]:
- Anatomical Factors: The GIT has varying environments from the stomach to the colon. The stomach's strong acidic environment (pH 1.0–2.5) can degrade acid-labile drugs, while the small intestine, despite its large surface area, contains pancreatic enzymes and bile salts that can inactivate certain compounds. The colon has a complex microbiome that can metabolize drugs [30].
- Biochemical Barriers: This includes the pH gradient throughout the GIT and the presence of digestive enzymes that can break down drugs, particularly proteins and peptides [30].
- Physiological Barriers: The intestinal epithelium is a phospholipid bilayer that favors the absorption of lipophilic molecules and restricts hydrophilic and large molecules. Furthermore, a dynamic mucus layer covers the epithelium, which can trap foreign particles and prevent direct contact with the absorptive surface [30].
FAQ 2: How does the prodrug strategy improve oral bioavailability? The prodrug strategy involves the chemical modification of an active drug into an inactive derivative that undergoes conversion to the active parent compound within the body. This approach is used to overcome a range of limitations [3] [31] [32]:
- Improving Solubility and Permeability: By attaching promoieties, a prodrug can enhance the drug's water solubility or its lipophilicity, thereby improving dissolution or passive diffusion across the intestinal membrane.
- Overcoming First-Pass Metabolism: Prodrugs can be designed to be resistant to metabolic enzymes in the gut and liver, ensuring more intact drug reaches the systemic circulation.
- Enabling Targeted Delivery: Modern prodrugs can be engineered to target specific enzymes or transporters in the intestinal membrane (e.g., the hPEPT1 transporter for valacyclovir), which can enhance absorption and enable site-specific release [3].
FAQ 3: What formulation strategies can enhance the bioavailability of poorly water-soluble drugs? For compounds with poor aqueous solubility, which is a common challenge in drug discovery, several formulation strategies can be employed [33] [30] [34]:
- Lipid and Surfactant-Based Systems: Self-emulsifying drug delivery systems (SEDDS) and liposomes can enhance solubility and absorption by facilitating drug transport via the lymphatic system, bypassing first-pass metabolism.
- Nanoparticulate Formulations: Drug nanoparticles, nanoemulsions, and other nanocarriers can dramatically increase the surface area for dissolution, protect the drug from the harsh GIT environment, and improve absorption.
- Solid Dispersions: Dispersing a poorly soluble drug in a hydrophilic polymer carrier can create a supersaturated solution in the GIT, significantly driving absorption.
Troubleshooting Guides
Problem: Poor Absorption Due to Low Permeability
Potential Causes and Solutions:
| Potential Cause | Diagnostic Experiments | Proposed Solution | Key Reagents/Tools |
|---|---|---|---|
| Inherently low passive diffusion | - Caco-2 assay: Measures transport of the compound across a model of the intestinal epithelium. [34]- PAMPA (Parallel Artificial Membrane Permeation Assay): A high-throughput screen for passive permeability. [34] [35] | - Prodrug design: Incorporate lipophilic promoieties (e.g., ester chains) to increase log P. [3] [32]- Permeation enhancers: Use excipients like surfactants, fatty acids, or glycerides (use with caution due to potential for epithelial damage). [33] [32] | - Caco-2 cell lines- PAMPA plates & artificial membranes- Prodrug synthesis reagents (e.g., acyl chlorides for esterification) |
| Substrate for efflux transporters (e.g., P-gp) | - Bidirectional Caco-2 assay: Asymmetric transport indicates efflux activity. [34] | - Chemical modification: Alter the drug structure to avoid recognition by efflux transporters.- Co-administration with efflux inhibitors (though this has clinical safety implications). | - Known efflux transporter substrates/inhibitors (e.g., Verapamil for P-gp) |
| Metabolic instability in the gut wall | - Incubation with intestinal homogenates or specific enzymes (e.g., esterases) and measure parent compound loss over time. [34] | - Prodrug approach: Design a prodrug that is resistant to gut enzymes but cleaved in systemic circulation or the target tissue (e.g., tenofovir alafenamide). [3] | - Intestinal S9 fractions or specific purified enzymes (e.g., carboxylesterases) |
Problem: Poor Bioavailability Due to Low Solubility/Dissolution Rate
Potential Causes and Solutions:
| Potential Cause | Diagnostic Experiments | Proposed Solution | Key Reagents/Tools |
|---|---|---|---|
| High crystallinity & low aqueous solubility | - Equilibrium solubility measurement in biorelevant media (e.g., FaSSIF, FeSSIF). [34] | - Particle size reduction (e.g., nanomilling) to increase surface area. [34]- Solid dispersions with polymers like HPMC or PVP to create amorphous drug. [34]- Lipid-based formulations (e.g., SEDDS) to maintain drug in a solubilized state. [33] [34] | - Biorelevant media powders (FaSSIF/FeSSIF)- Polymers for dispersion (HPMC, PVP, Soluplus)- Lipids & surfactants (e.g., Gelucire, Labrasol) |
| Poor dissolution in GI pH range | - Dissolution testing across a pH gradient (1.2 to 7.4). [30] | - Salt formation to improve dissolution at specific pH.- Prodrug approach: Attach a hydrophilic ionizable group (e.g., phosphate) to enhance water solubility. [3] [31] | - USP dissolution apparatus- pH adjustment solutions |
Problem: Extensive Presystemic (First-Pass) Metabolism
Potential Causes and Solutions:
| Potential Cause | Diagnostic Experiments | Proposed Solution | Key Reagents/Tools |
|---|---|---|---|
| Cytochrome P450 (CYP) metabolism in the liver | - Metabolic stability assay in liver microsomes or hepatocytes. [34] | - Prodrug design: Create a structure that is not a substrate for the metabolizing enzyme but releases the active drug after absorption.- Chemical modification: Block or substitute the metabolic soft spot on the molecule. | - Liver microsomes (human/rat)- NADPH regenerating system |
| Enzymatic hydrolysis in the gut lumen | - Stability assessment in simulated intestinal fluid or with pancreatic enzymes. [30] | - Enteric coating: A formulation strategy to protect the drug from stomach acid and intestinal enzymes until it reaches the absorption site.- Prodrug: Mask susceptible functional groups (e.g., esters) to prevent enzymatic recognition. [3] | - Simulated intestinal fluids- Pancreatin |
Experimental Protocols for Key Assays
Protocol 1: Assessing Passive Membrane Permeability using PAMPA
Principle: The Parallel Artificial Membrane Permeation Assay (PAMPA) is a high-throughput, non-cell-based model used to predict passive transcellular permeability by measuring the rate of drug diffusion across a lipid-infused artificial membrane [34] [35].
Procedure:
- Membrane Preparation: A hydrophobic filter membrane is coated with a solution of phospholipids (e.g., phosphatidylcholine) in an organic solvent to form an artificial lipid layer. The solvent is allowed to evaporate completely.
- Plate Assembly: The donor plate (containing the compound solution) is placed over the acceptor plate, which contains a blank buffer solution (e.g., PBS at pH 7.4), so that the artificial membrane is between them.
- Dosing and Incubation: A solution of the test compound (typically 50-100 µM) in a physiologically relevant buffer (e.g., pH 6.5 for small intestine) is added to the donor well. The assembly is incubated for a set period (e.g., 2-16 hours) at room temperature without agitation.
- Sample Analysis: After incubation, the concentration of the compound in both the donor and acceptor compartments is quantified using a suitable analytical method (e.g., UV spectroscopy, HPLC).
- Data Calculation: The permeability coefficient (Pe) is calculated using the following formula, where CA(t) is the concentration in the acceptor well at time t, CD is the concentration in the donor well at time zero, VD and VA are the volumes of the donor and acceptor wells, A is the filter area, and t is the incubation time.
Protocol 2: Evaluating Metabolic Stability in Liver Microsomes
Principle: This assay determines the intrinsic metabolic stability of a drug candidate by incubating it with liver microsomes, which contain cytochrome P450 enzymes, and measuring the disappearance of the parent compound over time [34].
Procedure:
- Incubation Preparation: Prepare a reaction mixture containing:
- 0.1 M Phosphate Buffer (pH 7.4)
- Liver Microsomes (e.g., 0.5 mg/mL protein concentration)
- Test Compound (typically 1 µM)
- Pre-Incubation: Allow the mixture to equilibrate for 5 minutes in a water bath at 37°C.
- Reaction Initiation: Start the reaction by adding an NADPH regenerating system (provides the cofactors essential for CYP enzyme activity).
- Sampling: At predetermined time points (e.g., 0, 5, 15, 30, 45, 60 minutes), withdraw an aliquot of the incubation mixture and quench it with an equal volume of ice-cold acetonitrile containing an internal standard to stop the reaction.
- Sample Analysis: Centrifuge the quenched samples to precipitate proteins. Analyze the supernatant using LC-MS/MS to quantify the remaining parent drug.
- Data Analysis: Plot the natural logarithm of the percent parent remaining versus time. The slope of the linear regression is the apparent first-order elimination rate constant (k), from which the in vitro half-life (t1/2 = 0.693/k) and intrinsic clearance (CLint = k / microsomal protein concentration) can be calculated.
Visualization of Key Concepts
Diagram 1: Pathways for Oral Drug Absorption and Key Barriers
Title: Oral drug absorption pathway and key barriers limiting bioavailability.
Diagram 2: Strategic Solutions to Overcome Bioavailability Barriers
Title: Formulation and prodrug strategies to overcome bioavailability barriers.
The Scientist's Toolkit: Research Reagent Solutions
| Category | Item/Reagent | Function in Experiment | Key Considerations |
|---|---|---|---|
| Permeability Assessment | Caco-2 Cell Lines | In vitro model of the human intestinal epithelium for predicting drug absorption and efflux. [34] | Requires long culture time (21 days) to fully differentiate. |
| PAMPA Plates & Lipid Membranes | High-throughput tool for screening passive permeability potential. [34] [35] | Does not account for active transport or efflux mechanisms. | |
| Solubility & Dissolution | Biorelevant Media (FaSSIF/FeSSIF) | Simulates the composition and surface activity of fasted and fed state intestinal fluids for realistic solubility measurements. [34] | More predictive than simple aqueous buffers. |
| USP Dissolution Apparatus | Standardized equipment for measuring the rate and extent of drug release from a dosage form. [30] | Critical for quality control and formulation development. | |
| Metabolic Stability | Liver Microsomes & Hepatocytes | Subcellular fraction or whole cells containing metabolic enzymes (CYPs, UGTs) for in vitro stability and clearance studies. [34] | Cryopreserved hepatocytes offer a more complete metabolic profile than microsomes. |
| NADPH Regenerating System | Provides essential cofactors for Cytochrome P450 enzyme activity in microsomal incubations. [34] | Essential for initiating and maintaining metabolic reactions. | |
| Prodrug Synthesis | Activated Promoieties (e.g., acyl chlorides, phosphorochloridates) | Chemically reactive compounds used to attach lipophilic or hydrophilic groups to a parent drug molecule. [3] [32] | Requires careful selection to ensure efficient in vivo cleavage. |
| Formulation Enablers | Lipid Excipients (e.g., Medium Chain Triglycerides) | Key components of lipid-based drug delivery systems that enhance solubilization and lymphatic transport. [33] [34] | Compatibility with capsules (e.g., gelatin) must be checked. |
| Polymers for Amorphous Solid Dispersions (e.g., HPMC, PVP) | Inhibit drug recrystallization and maintain supersaturation in the GI tract to drive absorption. [34] | Drug-polymer miscibility is critical for physical stability. |
A critical challenge in modern drug development is overcoming poor cellular permeability, which can render otherwise potent therapeutic compounds ineffective. For drugs targeting intracellular pathways, such as those used against viruses and cancers, the ability to cross cell membranes is non-negotiable. The prodrug strategy has emerged as a powerful solution to this problem, wherein a biologically inactive derivative of a drug undergoes enzymatic or chemical transformation within the body to release the active parent compound [12] [16]. This approach is particularly valuable for optimizing biopharmaceutical and pharmacokinetic parameters while mitigating adverse effects [12].
Statistical evidence underscores the importance of this strategy: approximately 13% of drugs approved by the U.S. Food and Drug Administration (FDA) between 2012 and 2022 were prodrugs [12]. A recent analysis identified around 95 distinct design goals for prodrugs, with approximately 59% aimed at enhancing bioavailability, primarily through improvements in permeability (35%) and solubility (15%) [12]. This case study examines how permeability-driven design principles are applied to develop effective antiviral and anticancer prodrugs, providing a technical framework for researchers in the field.
Theoretical Foundations: Membrane Permeability and the Prodrug Approach
Mechanisms of Membrane Permeability
For small molecule drugs to reach intracellular targets, they must traverse biological membranes through one of two primary mechanisms:
Passive Transport: This energy-independent process occurs through diffusion, driven by a concentration gradient. Key molecular properties influencing passive diffusion include [12]:
- Polarity: Lower polarity generally enhances permeability.
- Molecular Weight: Smaller molecules diffuse more readily.
- Lipophilicity: Higher lipophilicity (within optimal limits) improves membrane partitioning.
Active Transport: This energy-dependent process is facilitated by specific transporter proteins (e.g., ATP-binding cassette transporters) that utilize energy (such as ATP hydrolysis) to move compounds across membranes [12]. Unlike passive diffusion, active transport can exhibit saturation kinetics due to the finite number of available transporter proteins [12].
The Biopharmaceutics Classification System (BCS)
The BCS provides a valuable framework for categorizing drugs based on their solubility and permeability characteristics [12]. Understanding a drug's BCS class is fundamental to identifying the need for a prodrug strategy.
Table 1: Biopharmaceutics Classification System (BCS) and Drug Examples
| Class | Solubility | Permeability | Examples of Drugs |
|---|---|---|---|
| I | High | High | Acyclovir, Captopril, Abacavir |
| II | Low | High | Atorvastatin, Diclofenac, Ciprofloxacin |
| III | High | Low | Cimetidine, Atenolol, Amoxicillin |
| IV | Low | Low | Furosemide, Chlorthalidone, Methotrexate |
Adapted from [12]
Prodrug strategies are particularly beneficial for BCS Class III (high solubility, low permeability) and Class IV (low solubility, low permeability) compounds, aiming to transition them toward a more favorable Class I profile.
The Role of Efflux Transporters
A significant barrier to drug permeability, especially in specialized tissues like the blood-brain barrier and in cancer cells, is the overexpression of ATP-binding cassette (ABC) efflux transporters. Key players include [36] [37] [38]:
- P-glycoprotein (P-gp/ABCB1): A broad-spectrum efflux pump that significantly limits the intracellular accumulation and tissue penetration of many anticancer and antiviral drugs [37] [39].
- Breast Cancer Resistance Protein (BCRP/ABCG2): Another major efflux transporter with overlapping substrate specificity to P-gp, contributing to multidrug resistance [36] [40].
- Multidrug Resistance-Associated Protein 1 (MRP1/ABCC1): Transports a range of conjugated anions and chemotherapeutic agents [36].
Prodrug design can incorporate structural features that avoid recognition by these efflux pumps, thereby improving intracellular drug concentrations.
Figure 1: Logic Flow of Permeability-Driven Prodrug Design. This diagram outlines the strategic approach to overcoming poor drug permeability through prodrug engineering.
Antiviral Prodrug Case Studies
Remdesivir: A Multi-Stage Prodrug for Enhanced Cellular Uptake
Remdesivir is a broad-spectrum antiviral nucleotide analog that exemplifies sophisticated prodrug design to overcome the significant permeability challenges associated with charged nucleotide analogs [41].
- Mechanism of Action: The active form of Remdesivir, a triphosphate nucleoside analog, inhibits viral RNA polymerase. However, the polar phosphate groups prevent efficient cellular uptake.
- Prodrug Strategy: Remdesivir is administered as a phosphoramidate prodrug. This design masks the charged phosphate groups with lipophilic aromatic substituents and amino acid esters, dramatically increasing its lipophilicity and membrane permeability [41].
- Activation Pathway: Intracellular activation is a multi-step process involving ester cleavage followed by spontaneous cyclization and hydrolysis to release the nucleoside monophosphate, which is subsequently phosphorylated to the active triphosphate form.
Table 2: Key Properties and Design Features of Antiviral Prodrugs
| Prodrug Name | Active Drug | Primary Permeability Challenge | Prodrug Strategy | Enzymes Involved in Activation |
|---|---|---|---|---|
| Remdesivir | Nucleoside Triphosphate | High polarity of phosphate groups | Phosphoramidate derivatization | Esterases, Carboxylesterases (CES) [41] |
| Favipiravir | Ribofuranosyltriphosphate | Low membrane permeability | Administered as a ribonucleoside prodrug | Hypoxanthine-guanine phosphoribosyltransferase (HGPRT) [41] |
| Valacyclovir | Acyclovir | Low oral bioavailability (20%) | L-valyl esterification | Enzyme: Valacyclovirase (Branched-chain amino acid transferase) [12] |
| AZT (Zidovudine) | AZT-monophosphate | Efflux by P-gp and ABCG2 | Dimerization to create transporter inhibitors [40] | N/A (Used to inhibit efflux, not as a prodrug) |
AZT Dimer Inhibitors: Blocking Efflux to Enhance Permeability
While not a prodrug itself, the modification of Azidothymidine (AZT) illustrates a creative approach to overcoming transporter-mediated permeability barriers. AZT, an antiretroviral, is a substrate for both P-gp and ABCG2 efflux transporters at the blood-brain barrier, limiting its CNS penetration [40].
- Design Strategy: Researchers synthesized a series of AZT homodimers linked by methylene chains of varying lengths [40].
- Mechanism: These dimers do not function as conventional prodrugs. Instead, they act as dual inhibitors of P-gp and ABCG2. By simultaneously blocking both major efflux transporters, they increase the brain penetration of co-administered AZT and other antiretroviral therapeutics [40].
- Key Finding: Dimer potency was found to be dependent on the tether length, with longer linkers (e.g., AZT-C12) showing superior inhibitory activity against both transporters [40].
Anticancer Prodrug Case Studies
Capecitabine: Tumor-Selective Activation and Permeability
Capecitabine is an oral fluoropyrimidine carbamate prodrug that showcases the application of permeability design for both enhanced absorption and targeted activation [16].
- Mechanism of Action: The active drug, 5-fluorouracil (5-FU), is a pyrimidine analog with antineoplastic activity. However, 5-FU itself has variable oral absorption and significant toxicity.
- Prodrug Strategy: Capecitabine is designed with high oral bioavailability. Its lipophilic nature allows for efficient passive absorption from the gastrointestinal tract [16].
- Activation Pathway: Activation is a three-enzyme, tumor-selective process:
- Liver: Carboxylesterase (CES) hydrolyzes capecitabine to 5'-deoxy-5-fluorocytidine (5'-DFCR).
- Liver and Tumors: Cytidine deaminase converts 5'-DFCR to 5'-deoxy-5-fluorouridine (5'-DFUR).
- Tumors: Thymidine phosphorylase (dThdPase), an enzyme often highly concentrated in tumor tissues, converts 5'-DFUR to the active 5-FU. This selective activation maximizes efficacy in the tumor while minimizing systemic exposure [16].
Taxanes and Overcoming ABCB1-Mediated Resistance
Taxanes like docetaxel (DTX) and cabazitaxel (CBZ) are cornerstone treatments for castration-resistant prostate cancer (CRPC). A major mechanism of resistance is the overexpression of the ABCB1 (P-gp) efflux transporter, which actively pumps taxanes out of cancer cells [39].
- The Problem: Acquired resistance in CRPC cell lines (e.g., RC4-2B) is strongly linked to increased ABCB1 expression, conferring cross-resistance to both DTX and CBZ [39].
- Experimental Solution: Research demonstrates that this resistance can be overcome by:
- Using Specific ABCB1 Inhibitors: Elacridar, a potent ABCB1 inhibitor, can reverse taxane resistance in vitro, confirming the transporter's role [39].
- Switching to Non-Substrate Chemotherapeutics: DNA-damaging agents like Camptothecin (CPT) and Cytarabine (Ara-C) were found to be equally cytotoxic against both parental and ABCB1-overexpressing resistant cells, as they are not effluxed by ABCB1 [39]. This provides a viable treatment strategy for taxane-resistant CRPC.
The Scientist's Toolkit: Essential Reagents and Methodologies
Table 3: Research Reagent Solutions for Prodrug Permeability Studies
| Reagent / Assay | Function / Purpose | Key Application in Prodrug Research |
|---|---|---|
| Caco-2 Cell Model | In vitro model of human intestinal permeability | Predicts oral absorption potential of prodrug candidates [12]. |
| MDCK or MDCK-II Cells | Canine kidney epithelial cells; often transfected with human transporters (e.g., MDR1-MDCKII) | Specifically assesses interaction with and efflux by P-gp and other ABC transporters [12]. |
| P-gp/ABCB1 Inhibitors(e.g., Elacridar, Verapamil, Zosuquidar) | Pharmacologically block P-gp efflux activity | Used to confirm P-gp-mediated efflux of a parent drug and to validate that a prodrug evades this transporter [39]. |
| Parallel Artificial Membrane Permeability Assay (PAMPA) | High-throughput measure of passive transmembrane diffusion | Screens prodrug libraries for improved passive permeability independent of active transporters [12]. |
| Carboxylesterases (CES)(e.g., from porcine liver) | Hydrolyze ester and amide-based prodrugs | In vitro evaluation of enzymatic conversion rates for ester-based prodrugs like capecitabine [16]. |
| ATPase Assay | Measures ATP hydrolysis by ABC transporters | Determines if a prodrug candidate is a substrate or inhibitor of transporters like P-gp [38]. |
Core Experimental Protocols
Protocol 1: Assessing Permeability in MDR1-MDCKII Cell Monolayers
Purpose: To evaluate whether a prodrug is a substrate for the human P-gp efflux transporter [12].
Method:
- Cell Culture: Grow MDR1-MDCKII cells on transparent filter supports until they form a confluent, polarized monolayer with tight junctions.
- Transport Experiment: Add the prodrug candidate to either the apical (A) or basolateral (B) compartment in a suitable buffer (e.g., HBSS).
- Perform bidirectional transport: A→B and B→A.
- Include a control group with a known P-gp inhibitor (e.g., 10 µM Elacridar).
- Incubation and Sampling: Incubate at 37°C with gentle shaking. Collect samples from the receiver compartment at predetermined time points (e.g., 30, 60, 90, 120 min) and analyze drug concentration using HPLC or LC-MS/MS.
- Data Analysis:
- Calculate the Apparent Permeability Coefficient (Papp) for each direction.
- Determine the Efflux Ratio: ER = Papp (B→A) / Papp (A→B).
- Interpretation: An ER ≥ 2 that is significantly reduced (e.g., by ≥50%) in the presence of a P-gp inhibitor suggests the compound is a P-gp substrate.
Protocol 2: In Vitro Prodrug Activation Kinetics
Purpose: To quantify the rate of conversion of a prodrug to its active parent molecule by specific enzymes [16].
Method:
- Incubation Setup: Prepare incubation mixtures containing the prodrug, appropriate enzyme source (e.g., liver microsomes, recombinant esterases, or target cell lysates), and buffer (e.g., phosphate buffer, pH 7.4).
- Time Course Experiment: Initiate the reaction by adding the enzyme source and incubate at 37°C. Aliquot samples at multiple time points (e.g., 0, 5, 15, 30, 60 min).
- Reaction Termination: Stop the reaction immediately by adding an equal volume of an organic solvent like acetonitrile (which also precipitates proteins).
- Analysis: Centrifuge the samples and analyze the supernatant using a validated analytical method (e.g., HPLC-UV) to quantify the disappearance of the prodrug and the appearance of the active drug.
- Data Analysis: Plot the concentration of the active drug over time and calculate the activation velocity (e.g., pmol/min/mg protein) and half-life of conversion.
Technical Support Center: Troubleshooting Guides and FAQs
FAQ 1: Permeability and Prodrug Design
Q: My lead compound has excellent in vitro potency but poor cellular permeability. When should I consider a prodrug approach? A: A prodrug strategy is strongly indicated when:
- Your compound falls into BCS Class III or IV [12].
- It contains highly polar, ionizable groups (e.g., phosphates, carboxylates) that limit passive diffusion.
- It is a confirmed substrate for efflux transporters like P-gp or BCRP, leading to low intracellular concentrations or poor tissue penetration (e.g., across the BBB) [37] [39].
- In vitro-to-in vivo efficacy correlations fail due to insufficient cellular uptake.
Q: How can I design a prodrug to evade efflux by P-glycoprotein? A: Strategies include:
- Structural Masking: Modify the functional groups that are recognized by P-gp. For example, esterification of hydrogen-bond donors can reduce transporter affinity.
- Increase Lipophilicity: Enhance passive diffusion to such an extent that it simply overwhelms the efflux capacity, though this must be balanced with solubility requirements.
- Molecular Size/Shape Alteration: P-gp has a large, flexible binding pocket; sometimes, subtle changes in steric bulk can eliminate recognition without compromising target activity [40] [38].
FAQ 2: Experimental and Analytical Challenges
Q: My prodrug shows excellent permeability in Caco-2 assays, but in vivo efficacy is low. What could be the reason? A: This discrepancy can arise from several factors:
- Insufficient Metabolic Activation: The prodrug may not be efficiently converted to the active drug in the target tissue. Check the expression levels of the required activating enzymes in vivo.
- Rapid Systemic Clearance: The prodrug itself may be cleared (e.g., by hepatic metabolism or renal excretion) before it reaches the target site or has time to be activated.
- Off-Target Activation: Activation may occur prematurely in plasma or non-target tissues, leading to degradation of the active drug before it reaches the site of action.
Q: How do I determine the optimal linker for a carrier-linked prodrug? A: Linker selection is empirical but should be guided by:
- Cleavage Mechanism: Choose a linker that is stable in circulation but efficiently cleaved by the enzyme present at the target site (e.g., a peptide linker for tumor-associated proteases, or an ester linker for carboxylesterases).
- Steric Hindrance: The linker should not sterically block the interaction of the active drug with its target upon release.
- Physicochemical Properties: The linker must confer the desired solubility and lipophilicity to the entire prodrug molecule. A systematic evaluation of linker lengths and chemistries, as seen in the AZT dimer study, is often necessary [40].
Troubleshooting Table: Common Issues in Prodrug Development
Table 4: Troubleshooting Guide for Prodrug Experiments
| Problem | Potential Causes | Suggested Solutions |
|---|---|---|
| Low Prodrug Conversion Rate | 1. Poor substrate specificity for the activating enzyme.2. Low enzyme expression/activity in the test system.3. Prodrug chemical stability is too high. | 1. Redesign the promoiety to better match the enzyme's natural substrate (e.g., use a different amino acid ester for esterases).2. Use a more physiologically relevant enzyme source (e.g., human liver S9 fractions vs. recombinant enzymes).3. Incorporate a more labile linker (e.g., a different ester type) [16]. |
| Prodrug is itself a substrate for efflux transporters | The added carrier/promoiety contains structural elements recognized by P-gp/BCRP. | 1. Synthesize analogs with minor structural modifications to the carrier.2. Investigate if the prodrug is a weaker substrate than the parent drug. A reduction in efflux ratio is still a win.3. Consider a bioprecursor strategy that does not use a carrier group [40]. |
| Rapid Pre-systemic Metabolism | The prodrug is hydrolyzed in the gut lumen or by first-pass liver metabolism before reaching systemic circulation. | 1. Increase the steric bulk around the labile bond to slow down enzymatic hydrolysis.2. Switch to an enzyme substrate that is not highly expressed in the gut/liver (e.g., target a phosphatase instead of an esterase). |
| High Cytotoxicity of the Prodrug itself | The carrier molecule or linker may have inherent toxicity. | 1. Test the cytotoxicity of the linker/carrier molecule alone.2. Design a new prodrug using a different, biologically inert carrier (e.g., PEG, sugar derivatives). |
Figure 2: Mechanism of ABC Efflux Transporter-Mediated Drug Resistance. Transporter proteins like P-gp and BCRP utilize ATP hydrolysis to pump substrate drugs and prodrugs out of the cell, reducing intracellular concentration. A key goal of prodrug design is to evade this recognition.
Troubleshooting Guides
Issue 1: Low or No PLA2-Mediated Activation of Prodrug
Problem: The phospholipid-based prodrug shows insufficient or no drug release upon exposure to phospholipase A2 (PLA2), preventing site-specific activation at the target tissue [42] [43].
Solution:
- Verify Conjugation Position: Confirm that the active drug moiety is conjugated to the sn-2 position of the phospholipid glyceride backbone. Conjugation to the phosphate group or the sn-1 position is designed to avoid PLA2 hydrolysis and will not result in enzyme-triggered release [42] [44].
- Check Linker Design: The linker between the phospholipid and the drug can significantly impact PLA2 susceptibility. Bulky or charged linkers near the sn-2 ester bond can cause steric hindrance, blocking the enzyme's active site. Consider using shorter or more flexible linkers [42] [43].
- Characterize Aggregation State: PLA2 activity requires the prodrug to form specific aggregates, such as mixed micelles or bilayers, that the enzyme can recognize. Use dynamic light scattering (DLS) or cryo-electron microscopy to confirm the formation of biorelevant aggregates. The prodrug should have surface properties and aggregation performance similar to natural phospholipids [42] [44].
Experimental Protocol: Assessing PLA2-Mediated Activation In Vitro
- Preparation: Dissolve the PL-prodrug in a suitable buffer (e.g., Tris-HCl, pH 8.0) containing calcium chloride (CaCl₂, typically 5-10 mM), which is a cofactor for many PLA2 enzymes [43].
- Aggregate Formation: Sonicate or extrude the solution to form uniform liposomes or micelles.
- Reaction Setup: Incubate the prodrug aggregates with a defined activity unit of the target PLA2 enzyme (e.g., secretory PLA2) at 37°C.
- Control Setup: Run a parallel control without the enzyme.
- Sample Analysis: At predetermined time intervals, quench the reaction and analyze samples using High-Performance Liquid Chromatography (HPLC) or LC-MS to quantify the release of the free drug and the lysophospholipid byproduct [42].
- Data Calculation: Calculate the percentage of prodrug hydrolyzed over time to determine the activation kinetics.
Issue 2: Inefficient Lymphatic Targeting After Oral Administration
Problem: The phospholipid-based prodrug fails to utilize the intestinal lymphatic system for transport, limiting its ability to bypass first-pass metabolism [43] [45].
Solution:
- Confirm Lipophilicity: Ensure the prodrug meets the prerequisite lipophilicity for lymphatic transport, typically requiring a log P value greater than 5 and high solubility in triglycerides (>50 mg/g) [42] [43].
- Co-administer with Lipids: Administer the prodrug with a long-chain triglyceride (LCT)-based lipid vehicle (e.g., oleic acid, soybean oil). LCTs stimulate chylomicron synthesis, which is essential for the packaging and transport of lipophilic compounds into the lymph [43].
- Validate Metabolic Pathway: The prodrug must be absorbed into the enterocyte and incorporated into the nascent chylomicron. Conduct cell-based assays (e.g., using Caco-2 cells) or in situ intestinal perfusion models to confirm the prodrug's association with lipoproteins [43].
Issue 3: Lack of Correlation Between Computational Predictions and Experimental Results
Problem: Molecular docking simulations predict good binding and activation of the PL-prodrug by PLA2, but experimental results show poor hydrolysis [42] [44].
Solution:
- Upgrade Simulation Method: Molecular docking alone has low accuracy (~20%). Employ more physics-based computational methods, such as Molecular Dynamics (MD) simulations or Free Energy Perturbation (FEP) methods, which account for the flexibility of the enzyme, solvation effects, and provide more accurate binding affinity predictions ( ~80% accuracy) [42].
- Simulate the Membrane Environment: Perform MD simulations with the prodrug placed in a lipid bilayer membrane, as PLA2 activation occurs at a lipid-water interface. This provides critical information on the prodrug's orientation and accessibility to the enzyme [42].
Experimental Protocol: Molecular Dynamics Simulation for Prodrug Optimization
- System Building: Construct a model of the PLA2 enzyme and a lipid bilayer containing the PL-prodrug molecule using software like CHARMM-GUI.
- Solvation and Ionization: Place the system in a water box and add ions to simulate physiological conditions.
- Energy Minimization: Run an energy minimization step to remove any steric clashes.
- Equilibration: Gradually heat the system and run a short simulation under constant temperature and pressure (NPT ensemble) to stabilize the system.
- Production Run: Perform a multi-nanosecond MD simulation to observe the interactions and stability of the prodrug within the membrane and its binding pose with PLA2.
- Analysis: Analyze the root-mean-square deviation (RMSD), hydrogen bonding, and free energy of binding (e.g., using MM-PBSA) to evaluate the complex's stability and affinity [42].
Issue 4: Prodrug Instability in Formulation or During Circulation
Problem: The prodrug undergoes premature, non-specific hydrolysis in the gastrointestinal tract or systemic circulation before reaching the target site [43].
Solution:
- Phosphate Group Conjugation: If premature hydrolysis by PLA2 is a problem, reconjugate the drug to the phosphate group of the phospholipid instead of the sn-2 position. This design avoids PLA2-mediated activation and allows the prodrug to join different metabolic pathways [42] [44].
- Probe Chemical Stability: Perform stability studies under various pH conditions (simulating GI tract pH range) and in biological matrices like plasma to identify the primary degradation pathway. Reformulate with stabilizing excipients based on the findings [43].
Frequently Asked Questions (FAQs)
Q1: What are the key structural considerations when designing a phospholipid-based prodrug? A: The conjugation strategy is paramount. There are three main approaches [42] [43]:
- sn-2 conjugation: Targets PLA2-mediated activation for site-specific drug release in diseased tissues overexpressing the enzyme (e.g., tumors, inflamed areas).
- Phosphate group conjugation: Avoids PLA2 hydrolysis, can enhance blood-brain barrier permeability, and may help overcome multidrug resistance.
- sn-1 conjugation: Used in specific applications like pro-anticancer ether lipids (ProAELs).
Q2: How can computational modeling guide the design of PL-based prodrugs? A: Computational methods can significantly reduce experimental burden by [42] [44]:
- Molecular Docking: Providing a fast, initial screen of potential binding poses of the prodrug in the PLA2 active site.
- Molecular Dynamics (MD) Simulations: Revealing the stability of the prodrug-enzyme complex in a biorelevant (membrane) environment over time and identifying key interaction residues.
- Free Energy Perturbation (FEP): Calculating binding free energies with high accuracy to predict the affinity of PLA2 for different prodrug structures and rank-order design candidates.
Q3: What are the primary advantages of using phospholipid-based prodrugs? A: The main advantages include [43] [45] [44]:
- Integration into physiological lipid pathways, enabling lymphatic transport (bypassing first-pass metabolism) and improved oral bioavailability.
- Enzyme-triggered site-specific activation, enhancing therapeutic efficacy and reducing off-target side effects.
- Improved pharmacokinetic profiles due to increased lipophilicity and altered distribution.
- Potential to cross the blood-brain barrier and overcome multidrug resistance.
Q4: Our prodrug is successfully taken up by target cells but shows low efficacy. What could be the cause? A: This could be due to inefficient intracellular drug release. After cellular uptake (e.g., via endocytosis), the prodrug may be trafficked to lysosomes or other compartments where the activating enzyme (e.g., PLA2) is not present or active. Consider investigating the intracellular fate of the prodrug and whether the linker is cleaved by intracellular enzymes. Incorporating linkers sensitive to intracellular hydrolases or cathepsins may be a potential solution.
Data Presentation
Table 1: Comparison of Computational Methods for PL-Prodrug Optimization
| Method | Key Principle | Typical Simulation Time | Accuracy (vs. Experimental) | Best Use Case |
|---|---|---|---|---|
| Molecular Docking | Predicts binding pose and score of a ligand in a protein's active site. | Minutes to Hours | Low (~20%) [42] | Initial, high-throughput screening of prodrug variants. |
| Molecular Dynamics (MD) | Simulates physical movements of atoms and molecules over time in a defined environment. | Days to Weeks | Medium to High [42] | Assessing prodrug stability in membranes, understanding enzyme-binding interactions. |
| Free Energy Perturbation (FEP) | Calculates free energy differences between similar molecules by alchemically transforming one into another. | Weeks | High (~80%) [42] | Accurately predicting relative binding affinities for lead optimization. |
Table 2: Key Research Reagent Solutions for PL-Prodrug Development
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Phospholipase A2 (PLA2) | Enzyme for in vitro activation studies of sn-2 conjugated prodrugs [42] [43]. | Use secretory PLA2 (sPLA2) for targeting inflammatory and cancerous tissues. Requires Ca²⁺ as a cofactor. |
| Long-Chain Triglycerides (LCT) | Lipid vehicle (e.g., soybean oil) for oral administration to stimulate chylomicron production and lymphatic transport [43]. | Superior to Medium-Chain Triglycerides (MCT) for promoting lymphatic uptake of lipophilic prodrugs. |
| Lysophospholipid | Starting material for synthesizing prodrugs conjugated at the sn-2 position [43]. | The protecting group strategy on the linker is critical for a successful conjugation reaction. |
| Molecular Modeling Software (e.g., GROMACS, SCHRÖDINGER) | Platform for running MD simulations and FEP calculations to predict PLA2 affinity and guide rational design [42]. | More accurate than docking but requires significant computational resources and expertise. |
Signaling Pathways and Workflows
Diagram: Phospholipid Prodrug Activation Pathway
Diagram: Computational Optimization Workflow
Navigating Development Challenges: From Predictive Modeling to Clinical Translation
Troubleshooting Guide & FAQs
Frequently Asked Questions
Q1: What are the primary causes of unpredictable conversion kinetics for prodrugs in vivo?
Unpredictable conversion kinetics most often arise from complex interplay between a prodrug's chemical design and the biological system. Key factors include:
- Variable Enzyme Levels: The expression and activity of converting enzymes (e.g., carboxylesterases, cytochrome P450s, phosphatases) can vary significantly between individuals, organs, and disease states [46] [47]. A prodrug designed to be activated by a specific enzyme may convert too rapidly, too slowly, or not at all if the enzyme profile is not as anticipated.
- Saturation of Enzymatic Pathways: High prodrug doses can saturate the converting enzymes, leading to non-linear pharmacokinetics where increases in dose do not result in proportional increases in active drug exposure [46].
- Chemical Instability: The prodrug linkage may be unstable in the gastrointestinal tract or systemic circulation, leading to premature release of the active drug and potential for local toxicity or degradation before reaching the site of action [11].
- Influence of Efflux Transporters: Efflux transporters like P-glycoprotein can limit the intestinal absorption of a prodrug, reducing its bioavailability and the amount available for conversion [46].
Q2: How does metabolic variability impact prodrug performance, and how can I account for it during design?
Metabolic variability is a major source of inter-individual differences in prodrug efficacy and safety [47] [48]. This variability stems from:
- Genetic Polymorphisms: Genetic variations in drug-metabolizing enzymes (e.g., CYP450 isozymes, UGTs) can create subpopulations of "poor metabolizers" or "ultra-rapid metabolizers," leading to toxic drug accumulation or sub-therapeutic levels, respectively [47] [48].
- Drug-Drug Interactions (DDIs): Co-administered drugs can induce or inhibit the enzymes responsible for prodrug activation. For example, a strong CYP3A4 inhibitor could drastically reduce the activation of a prodrug reliant on that pathway [47].
- Pathophysiological Conditions: Liver or kidney disease can impair metabolic capacity and drug clearance, altering the conversion and exposure profiles of both the prodrug and the active metabolite [48].
To account for this during design:
- Conduct Thorough In Vitro Profiling: Use human liver microsomes, recombinant enzymes, and hepatocytes from multiple donors to identify all major metabolic pathways and assess inter-donor variability early in development [47].
- Utilize Pharmacogenomic Data: If a prodrug is reliant on a specific enzyme with known polymorphisms, screen chemical analogs to see if activation can be re-routed through a less variable pathway [47].
- Perform Physiologically Based Pharmacokinetic (PBPK) Modeling: Incorporate data on enzyme abundance, genetic variability, and potential DDIs into PBPK models to simulate and predict population-level pharmacokinetics before clinical trials [47].
Q3: My prodrug has excellent in vitro solubility, but oral absorption in preclinical models is low. What could be going wrong?
This common pitfall often points to issues occurring after administration. Key areas to investigate are:
- Poor Permeability: The prodrug itself may have poor permeability across intestinal membranes, despite good solubility [46] [11].
- Premature Hydrolysis: The prodrug may be chemically or enzymatically hydrolyzed in the gut lumen by digestive enzymes or gut bacteria, releasing the active parent drug which may have poor absorption properties [46] [11].
- Insufficient Enzymatic Conversion at the Absorption Site: For prodrugs designed to be activated at the brush-border membrane (e.g., by enzymes like peptidases), the local enzyme activity may be insufficient to generate enough permeable drug for absorption [46].
Q4: What experimental strategies can I use to identify a "metabolic soft spot" in my prodrug candidate?
A "metabolic soft spot" is a site on the molecule that is particularly susceptible to enzymatic degradation, leading to high clearance and short half-life [47]. To identify it:
- In Vitro Incubations: Incubate the prodrug with liver microsomes or hepatocytes from humans and preclinical species and use LC-MS to identify the structures of the major metabolites [47].
- Reaction Phenotyping: Use specific chemical inhibitors or recombinant enzymes to pinpoint which individual enzyme (e.g., CYP3A4, UGT1A1) is primarily responsible for the metabolism [47].
- Structural Modification (Blocking the Soft Spot): Once identified, the soft spot can be blocked using strategies like introducing a stable bioisostere (e.g., replacing a labile benzylic methyl group with a -CF3 group) or adding steric hindrance to shield the site from enzymatic attack [47].
Key Experimental Protocols
Protocol 1: Assessing Metabolic Lability and Identifying Soft Spots
Objective: To determine the metabolic stability of a prodrug and identify its major sites of metabolism.
Materials:
- Test System: Pooled human liver microsomes (HLM) or cryopreserved human hepatocytes.
- Co-factors: NADPH regenerating system (for microsomes) or appropriate cell culture media (for hepatocytes).
- Analytical Instrumentation: LC-MS/MS system.
Method:
- Incubation: Prepare incubation mixtures containing the test system (e.g., 0.5 mg/mL HLM protein), magnesium chloride, and the prodrug (e.g., 1 µM). Pre-incubate for 5 minutes at 37°C.
- Initiate Reaction: Start the reaction by adding the NADPH regenerating system.
- Time Points: At predetermined time points (e.g., 0, 5, 15, 30, 60 minutes), remove an aliquot of the incubation mixture and quench it with an equal volume of ice-cold acetonitrile.
- Sample Analysis: Centrifuge the quenched samples, analyze the supernatant by LC-MS/MS to determine the parent prodrug concentration remaining over time.
- Metabolite Identification: Use high-resolution MS to perform metabolite profiling on the samples, identifying metabolites based on their mass shifts relative to the parent compound.
Data Analysis:
- Plot the natural log of the percent parent remaining versus time. The slope of the linear phase is used to calculate the in vitro half-life (t1/2) and intrinsic clearance (Clint) [47].
- The structures of the most abundant metabolites indicate the location of metabolic soft spots.
Protocol 2: Evaluating Enzymatic Conversion of a Prodrug to its Active Parent
Objective: To confirm and quantify the release of the active parent drug from the prodrug by specific enzymes.
Materials:
- Recombinant Enzymes: Commercially available recombinant human enzymes (e.g., CES1, CES2, CYP450s).
- Specific Substrates and Inhibitors: Positive control substrates and selective inhibitors for the enzymes of interest.
- Analytical Instrumentation: HPLC-UV or LC-MS/MS.
Method:
- Enzyme-Specific Incubation: Incubate the prodrug with individual recombinant enzymes under optimal buffer and temperature conditions.
- Time Course: Take time-points over a defined period (e.g., up to 2 hours).
- Reaction Quenching: Quench reactions with a solvent that denatures the enzyme (e.g., acetonitrile or methanol with acetic acid).
- Quantification: Centrifuge the samples and analyze the supernatant to quantify the formation of the active parent drug using a calibrated analytical method.
Data Analysis:
- Calculate the rate of parent drug formation (e.g., pmol/min/pmol enzyme).
- Compare conversion rates across different enzymes to identify the primary activator.
- Use chemical inhibitors in HLM incubations to confirm the contribution of a specific enzyme to the overall activation.
Table 1: Common Functional Groups in Prodrugs and Associated Conversion Risks
| Functional Group | Common Use | Conversion Mechanism | Potential Risks & Variability Sources |
|---|---|---|---|
| Ester | Improve permeability, mask polar groups | Hydrolysis by carboxylesterases, paraoxonases, cholinesterases [46] | Polymorphisms in CES1/CES2; enzyme levels vary by tissue and disease state [46] [47]. |
| Phosphate | Enhance water solubility | Hydrolysis by alkaline phosphatases [46] [49] | High phosphatase activity in gut can cause premature release; variability in tissue phosphatase levels [46]. |
| Peptide | Target specific transporters (e.g., PepT1) or enzymes | Hydrolysis by peptidases (e.g., DPP-IV) [11] | Expression of peptidases and transporters can vary, leading to unpredictable absorption [11]. |
| N-hydroxy / Amidoxime | Cytochrome P450-activated prodrug | Reduction by CYP450 enzymes or soluble enzymes [46] | Subject to significant CYP450 polymorphism and drug-drug interactions, leading to high variability [46] [47]. |
Table 2: Strategies to Overcome Common Prodrug Pitfalls
| Pitfall | Design Strategy | Example |
|---|---|---|
| High Metabolic Clearance (Soft Spot) | Block the soft spot with halogenation, deuteration, or bioisosteric replacement [47]. | Replacing a labile benzylic C-H bond with a C-F bond to reduce CYP-mediated oxidation [47]. |
| Poor Aqueous Solubility | Introduce ionizable, water-solubilizing promoiety (e.g., phosphate, amino acid) [11] [49]. | Fosfluconazole (phosphate ester of fluconazole) for intravenous administration [49]. |
| Variable Enzymatic Activation | Design for activation by ubiquitous enzymes or multiple redundant pathways. | Valacyclovir (valyl ester) is activated by esterases and also recognized by the intestinal oligopeptide transporter PepT1, improving and stabilizing absorption [11]. |
| Premature Hydrolysis in GI Tract | Use a linker or promoiety that is stable at acidic pH and resistant to digestive enzymes [46]. | Employing a double-ester prodrug (e.g., pivampicillin) which requires sequential enzymatic hydrolysis for activation [46]. |
Visual Workflows and Pathways
Diagram Title: Prodrug In Vivo Pathways and Pitfalls
Diagram Title: Metabolic Soft Spot Identification Workflow
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Prodrug Metabolism and Kinetics Studies
| Reagent / Material | Function in Experimental Design |
|---|---|
| Pooled Human Liver Microsomes (HLM) | Provides a broad representation of human drug-metabolizing enzymes (CYPs, UGTs, esterases) for initial metabolic stability screening [47]. |
| Cryopreserved Human Hepatocytes | Offers a more physiologically relevant in vitro system containing full complement of enzymes and transporters; used for more advanced clearance and metabolite ID studies [47]. |
| Recombinant Human Enzymes | Allows for reaction phenotyping to pinpoint the specific enzyme (e.g., CYP3A4, CES2) responsible for prodrug activation or degradation [47]. |
| Specific Enzyme Inhibitors | Used in HLM incubations to chemically knockout a specific enzyme's activity, confirming its role in metabolism (e.g., Ketoconazole for CYP3A4, Bis-p-nitrophenyl phosphate for esterases) [47]. |
| NADPH Regenerating System | Essential co-factor for reactions catalyzed by cytochrome P450 enzymes in liver microsomal incubations [47]. |
| Caco-2 Cell Line | A model of human intestinal permeability used to assess prodrug absorption and potential for transporter-mediated influx/efflux [46]. |
| Plasma (Human & Preclinical) | Used to assess the chemical and enzymatic stability of the prodrug in the bloodstream, predicting potential for premature hydrolysis [46]. |
Within the broader thesis on strategies for prodrug design and formulation, the integration of computational tools represents a paradigm shift. Traditional prodrug development, often reliant on extensive laboratory experimentation, is being transformed by in silico models and machine learning (ML). These technologies enable researchers to predict and optimize key parameters—such as permeability, stability, and synthesizability—before a compound is ever synthesized, accelerating the development of effective prodrugs while mitigating risks and costs [50] [12]. This technical support center is designed to help researchers navigate the practical application of these powerful tools.
Core Concepts: FAQs on Computational Prodrug Design
FAQ 1: What are the primary applications of machine learning in prodrug optimization?
ML is deployed across multiple stages of the prodrug optimization workflow. Key applications include:
- Predicting Permeability and Absorption: ML models, particularly supervised learning, analyze molecular structures to forecast a prodrug's ability to cross biological membranes, a critical factor for bioavailability [51] [12].
- De Novo Molecular Design: Generative AI can design entirely novel prodrug structures in silico, optimizing for specific properties like stability, solubility, and low toxicity [52] [53].
- Virtual Screening: AI-powered tools can rapidly screen vast virtual libraries of candidate compounds, prioritizing those most likely to succeed for synthesis and testing [54] [52].
- Predicting ADMET Properties: Models can forecast the Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) profiles of candidate prodrugs, helping to eliminate problematic compounds early [52].
FAQ 2: What is the difference between a "multi-target" prodrug and a "promiscuous" drug, and how can computational tools help design the former?
This is a key concept in rational polypharmacology. A multi-target drug is strategically designed to interact with a pre-defined set of molecular targets to achieve a synergistic therapeutic effect for complex diseases. In contrast, a promiscuous drug exhibits a lack of specificity, binding to a wide range of unintended targets, which often leads to off-target effects and toxicity [55].
Computational tools, particularly Graph Neural Networks (GNNs) and multi-task learning frameworks, are essential for distinguishing between these outcomes. They can model complex interactions across biological networks, allowing researchers to deliberately design a prodrug's target spectrum to contribute to the desired therapeutic outcome while minimizing undesirable off-target binding [55].
FAQ 3: What are the most common data-related challenges when training ML models for prodrug design?
Successful ML projects require high-quality data, which is often a significant hurdle.
- Lack of Data & Imbalanced Datasets: Some benchmark datasets for drug-target interaction contain very few drug molecules, making it difficult to train robust models. Furthermore, the ratio of active to inactive drug responses can be highly imbalanced (e.g., 1:41) [56].
- Data Quality and Heterogeneity: Data from chemical structures, biological assays, and clinical trials come in different formats. Harmonizing them into a unified format for model training is complex and time-consuming [52].
- Data Bias: If training data over-represents a specific demographic or chemical space, the resulting model's predictions may not generalize well to other populations, leading to biased outcomes [56].
Troubleshooting Common Experimental Issues
Issue: Generated prodrug structures are theoretically promising but cannot be synthesized.
- Potential Cause: Generative AI models often explore molecular structures beyond their training data. A small change in a functional group can create a structure that requires an impossibly complex or nonsensical synthetic pathway [56].
- Solution:
- Implement a Synthetic Accessibility Filter: Integrate a scoring system that evaluates the synthetic feasibility of generated structures as a core part of your generative workflow. One study noted that after applying such a filter, only 6 reasonable molecules were selected from 40 candidate structures generated by a deep learning model [56].
- Use Reaction-Aware Generative Models: Employ advanced generative models that are constrained by known chemical reactions and rules. For instance, the "Magnet" system from Iambic Therapeutics uses reaction-aware models to ensure generated molecules are synthetically accessible [53].
Issue: Model performs well on training data but poorly on new, real-world data.
- Potential Cause: This is often due to distribution shift, where the deployment data differs statistically from the training data. For example, a model trained on gene expression from brain tissue may fail when predicting for bone tissue [56].
- Solution:
- Improve Data Curation: Ensure your training dataset is as diverse and representative as possible of the real-world contexts in which the model will be applied.
- Employ Transfer Learning: Fine-tune a pre-trained model on a smaller, targeted dataset that is specific to your new experimental context (e.g., a specific tissue type) [56].
- Quantify Uncertainty: Implement methods that allow the model to express its confidence in a prediction. This alerts users to avoid relying on predictions where the model is likely to be wrong [56].
Issue: The "black box" nature of a complex ML model makes its predictions difficult to trust and interpret.
- Potential Cause: Many deep learning models, such as deep neural networks, are inherently complex and their decision-making processes are not easily understood [52].
- Solution:
- Adopt Explainable AI (XAI) Techniques: Use tools like SHAP (SHapley Additive exPlanations) or LIME (Local Interpretable Model-agnostic Explanations) to interpret individual predictions and understand which molecular features the model deems important [56].
- Prioritize Interpretable Models: Where predictive accuracy allows, use more interpretable models like Random Forests or decision trees, which can provide insight into the decision-making process.
Experimental Protocols & Workflows
Protocol: An Integrated Workflow for Prodrug Permeability Prediction
This protocol outlines a standard methodology for assessing prodrug permeability using a combination of in silico and in vitro methods [12].
1. In Silico Pre-Screening
- Objective: To rapidly screen large virtual libraries of candidate prodrugs and prioritize compounds for further testing.
- Methodology:
- Calculate key molecular descriptors such as the logarithm of the octanol/water partition coefficient (logP), molecular weight, and the number of hydrogen bond donors and acceptors.
- Apply the "Rule of Five" (Lipinski's Rule) as an initial filter to identify compounds with a higher probability of good permeability.
- Use Machine Learning models (e.g., supervised learning or graph neural networks) trained on historical permeability data to predict apparent permeability coefficients (Papp) for the candidate compounds [51] [55].
2. In Vitro Validation
- Objective: To experimentally confirm the permeability predictions from the in silico models.
- Methodology:
- Use cell-based assays such as Caco-2 (human colon adenocarcinoma) cell monolayers.
- The candidate prodrug is applied to the donor compartment, and the amount that appears in the receptor compartment over time is measured.
- Calculate the Apparent Permeability Coefficient (Papp) to quantify the permeability rate.
3. Data Integration and Model Refinement
- Objective: To create a feedback loop that improves the accuracy of your predictive models.
- Methodology: The experimentally derived Papp values are fed back into the ML training dataset, retraining and refining the model for future prediction cycles.
The following workflow diagram illustrates this iterative, design-make-test-analyze (DMTA) cycle, which is central to modern computational prodrug discovery.
Protocol: Generative AI for Prodrug Design and Formulation Optimization
This protocol describes how generative AI can be used to create novel prodrug molecules or optimize formulation structures, as demonstrated in recent research [57].
1. Exemplar Data Collection
- Objective: To provide a foundational dataset for the AI model to learn from.
- Methodology: Collect high-quality images or structural data of existing, sub-optimal formulations or known active drug molecules. For formulation science, this could be microscopy images showing the spatial arrangement of ingredients [57].
2. Model Training and Conditional Generation
- Objective: To train a generative model that can create new, optimized digital structures.
- Methodology:
- Use a Generative Adversarial Network (GAN) architecture, such as a Continuous-Conditional GAN (ccGAN), which is effective for generating 3D structures from limited exemplar data [57].
- Train the model with "conditional control" parameters, such as target drug loading, desired particle size, or specific molecular properties (e.g., logP). This steers the generation process toward structures with user-specified attributes [57].
3. In Silico Analysis and Optimization
- Objective: To digitally test and optimize the AI-generated structures without costly physical experimentation.
- Methodology:
- Analyze the generated digital structures for Critical Quality Attributes (CQAs) like predicted porosity, dissolution rate, or permeability.
- Use optimization algorithms to select the digital prodrug or formulation structure that best meets the target profile.
4. Synthesis and Physical Validation
- Objective: To confirm that the digitally optimized design performs as expected in the real world.
- Methodology: Synthesize the top-ranking prodrug candidate or manufacture the optimized formulation and validate its performance through standard in vitro or in vivo assays.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential computational tools, data sources, and algorithms that form the modern toolkit for computational prodrug optimization.
Table 1: Essential Research Reagents & Tools for Computational Prodrug Optimization
| Tool/Resource Name | Type | Function in Prodrug Research |
|---|---|---|
| Molecular Fingerprints (e.g., ECFP) [52] [55] | Molecular Representation | Encodes chemical structures into compact numerical formats (bit vectors) for similarity searching and machine learning applications. |
| Graph Neural Networks (GNNs) [52] [55] | Machine Learning Algorithm | Excels at learning from molecular graphs and biological networks, capturing dependencies in non-Euclidean structures for tasks like property prediction. |
| Generative Adversarial Networks (GANs) [53] [57] | Generative AI Algorithm | Generates novel, synthetically accessible molecular structures or formulation morphologies optimized for specific properties. |
| AlphaFold / NeuralPLexer [50] [53] | Protein Structure Prediction | Predicts the 3D structure of target proteins or ligand-protein complexes, enabling structure-based prodrug design. |
| DrugBank / ChEMBL [55] | Bioactivity Database | Provides curated data on drug-target interactions, chemical structures, and bioactivity, essential for training and validating ML models. |
| SwissADME / ADMETlab [54] [50] | In Silico Prediction Tool | Predicts ADMET properties, solubility, and drug-likeness of candidate prodrugs to prioritize synthesis. |
| Caco-2 Cell Model [12] | In Vitro Assay System | A gold-standard cell-based assay for experimentally determining the apparent permeability (Papp) of prodrug candidates. |
Advanced Workflow: Multi-Target Prodrug Discovery
For complex diseases, designing a prodrug that effectively engages multiple intentional targets requires a systems-level approach. The following diagram maps the integrated computational and experimental workflow for this advanced strategy.
Foundational Concepts: Lipinski's Rule of Five
What is Lipinski's Rule of Five and why is it critical for oral drug development?
Lipinski's Rule of Five is a set of guidelines established by Christopher A. Lipinski in 1997 that predicts the oral bioavailability of pharmaceutical candidates based on their chemical properties. It states that an orally active drug should not violate more than one of the following four criteria [58]:
- Molecular weight less than 500 daltons
- LogP (partition coefficient) below 5, indicating favorable lipophilicity
- No more than 5 hydrogen bond donors (NH and OH groups)
- No more than 10 hydrogen bond acceptors (O and N atoms)
The importance of this rule in drug discovery lies in its ability to streamline the development process by eliminating compounds less likely to succeed as oral treatments. Current statistics indicate that approximately 16% of oral medications violate at least one of these criteria, with only 6% failing two or more, highlighting the rule's effectiveness in identifying viable candidates. Medications adhering to these guidelines demonstrate a correlation with favorable pharmacokinetic characteristics, with an average Quantitative Estimate of Drug-likeness (QED) of 0.766 for approved oral formulations [58].
What quantitative evidence supports the Rule of Five's predictive power?
Table 1: Rule of Five Compliance Statistics in Drug Development
| Metric | Value | Significance |
|---|---|---|
| Oral medications violating ≥1 criterion | 16% | Substantial majority comply |
| Oral medications violating ≥2 criteria | 6% | Multiple violations rare |
| Average QED for approved oral formulations | 0.766 | High correlation between compliance & favorable PK |
| Molecular weight range for most drug-like molecules | 160-480 g/mol | Optimal range for bioavailability |
| LogP range for drug-like molecules | -0.4 to 5.6 | Ideal balance of hydrophilicity/lipophilicity |
Advanced Strategies Beyond the Rule of Five
How can we effectively design drugs that fall beyond Rule of Five constraints?
Oral drugs exist far beyond the Rule of Five (bRo5) space, particularly for challenging targets. Analysis of drugs and clinical candidates with molecular weight >500 Da reveals several successful strategies [59]:
- Structural modifications: Intramolecular hydrogen bonding and macrocyclization help improve bioavailability of larger compounds
- Formulation optimization: Higher doses and advanced formulations can enhance oral bioavailability
- Natural product inspiration: Natural products and structure-based design from peptidic leads are key sources for oral bRo5 drugs
- Alternative administration routes: Development of parenteral drugs in parallel to oral formulations expands therapeutic options
Research indicates that natural products and semisynthetic natural product drugs constitute over one-third of all marketed small-molecule drugs, and only 51% of FDA-approved small-molecule drugs are both used orally and comply with the Rule of Five [60].
What role does prodrug design play in optimizing absorption and permeability?
Prodrug design represents a versatile, powerful method to enhance drug permeation by increasing lipophilicity or improving aqueous solubility. The majority of prodrugs are used clinically with these aims, and this approach can be integrated into the iterative process of lead optimization rather than employed as a post-hoc approach [61].
Table 2: Prodrug Design Strategies for Improved Absorption
| Strategy | Mechanism | Examples |
|---|---|---|
| Improved aqueous solubility | Enhance dissolution rate | Phosphate esters |
| Increased lipophilicity | Facilitate membrane permeation | Ester prodrugs |
| Transporter-mediated absorption | Utilize biological transport systems | Valacyclovir |
| Site-specific delivery | Target specific tissues or organs | Colon-targeted prodrugs |
| Co-drugs (mutual prodrugs) | Combine two active substances | l-DOPA-entacapone |
There are three primary objectives in prodrug design [16]:
- Pharmaceutical: Improving solubility, chemical stability, organoleptic properties, and reducing irritation
- Pharmacokinetic: Enhancement of ADME properties (absorption, distribution, metabolism, excretion)
- Pharmacodynamical: Reduced toxicity, improved therapeutic index, creation of co-drugs
Experimental Protocols for Absorption and Permeability Assessment
What are the key methodological approaches for predicting intestinal absorption?
Figure 1: Experimental workflow for assessing drug permeability.
Protocol 1: Caco-2 Cell Permeability Assay
The Caco-2 cell line simulates the human intestinal epithelium and represents a gold standard for permeability prediction [62].
Materials Required:
- Caco-2 human colorectal adenocarcinoma cells
- DMEM culture medium with fetal bovine serum
- Transwell inserts (0.4-3.0 μm pore size)
- Test compound and analytical equipment (HPLC, LC-MS)
- Transport buffer (HBSS or PBS)
Procedure:
- Culture Caco-2 cells on permeable filters for 21 days to allow full differentiation
- Confirm monolayer integrity by measuring transepithelial electrical resistance (TEER)
- Add test compound to donor compartment (apical for A-B transport, basal for B-A transport)
- Sample from receiver compartment at predetermined time points (typically 30-120 minutes)
- Analyze samples using appropriate analytical methods to determine compound concentration
- Calculate apparent permeability (Papp) using the formula: Papp = (dQ/dt) × (1/(A × C0)) where dQ/dt is the transport rate, A is the filter surface area, and C0 is the initial concentration
Performance Considerations: The Caco-2 model provides excellent prediction of human intestinal absorption but requires extended cultivation time (21 days) and lacks a mucosal layer. Co-culture with mucin-producing HT29-MTX cells can better replicate the human intestinal environment [62].
Protocol 2: Parallel Artificial Membrane Permeability Assay (PAMPA)
PAMPA is a cell-free high-throughput tool that predicts passive transcellular permeability [63].
Materials Required:
- Multi-well filter plates
- Artificial membrane lipids (typically lecithin in dodecane)
- Donor and acceptor plates
- Test compound and UV-compatible plates
- UV plate reader
Procedure:
- Prepare artificial membrane by coating filter with lipid solution
- Add test compound dissolved in buffer to donor compartment
- Fill acceptor compartment with buffer
- Incubate for 2-16 hours under controlled conditions
- Measure compound concentration in both compartments using UV spectroscopy
- Calculate permeability based on the rate of compound appearance in the acceptor compartment
Advantages: PAMPA is robust, reproducible, and suitable for high-throughput screening. It specifically measures passive permeability without the complicating factors of active transport [63].
Troubleshooting Common Experimental Issues
Why might a Rule of Five-compliant compound still exhibit poor permeability?
Despite computational compliance, several experimental factors can affect actual permeability:
Problem: Inconsistent Caco-2 Model Performance
- Cause: Variations in cell passage number, culture conditions, or insufficient differentiation time
- Solution: Standardize passage range (30-50), monitor TEER values (>300 Ω·cm²), and extend differentiation time to 21+ days
- Prevention: Implement quality control checks including marker compounds (e.g., high permeability metoprolol, low permeability atenolol)
Problem: Poor Correlation Between PAMPA and Cellular Models
- Cause: PAMPA only detects passive transcellular permeability while cell models include paracellular and active transport components
- Solution: Use both systems complementarily - PAMPA for passive permeability screening and Caco-2 for comprehensive absorption prediction
- Advanced Approach: Employ biomimetic barriers like Phospholipid Vesicle-based Permeation Assay (PVPA) for improved predictability [63]
Problem: Unexpectedly Low Permeability for Rule of Five-Compliant Compounds
- Cause: Undetected efflux transport (e.g., P-glycoprotein interaction) or metabolism during absorption
- Solution: Conduct bidirectional transport assays with and without efflux inhibitors; incorporate gut metabolism studies
- Alternative Approach: Consider prodrug design to circumvent efflux or metabolism issues [16]
How can we resolve discrepancies between computational predictions and experimental results?
Problem: Overestimation of Absorption by Rule of Five
- Context: The Rule of Five provides initial prioritization but doesn't guarantee absorption
- Investigation Steps:
- Verify compound stability in gastrointestinal pH conditions
- Assess solubility and dissolution rate in biologically relevant media
- Evaluate metabolism in intestinal homogenates or hepatocytes
- Test for P-glycoprotein and other efflux transporter substrates
- Resolution: Integrate additional in silico models including PBPK simulations and advanced QSAR approaches [64]
Research Reagent Solutions Toolkit
Table 3: Essential Materials for Absorption and Permeability Studies
| Reagent/System | Function | Application Notes |
|---|---|---|
| Caco-2 cell line | Model human intestinal epithelium | Requires 21-day differentiation; monitor TEER |
| MDCK cells | Alternative renal epithelial model | Faster growth (7-10 days) but different transporter expression |
| PAMPA plates | High-throughput passive permeability screening | Ideal for early discovery; limited to transcellular pathway |
| Permeapad | Biomimetic phospholipid barrier | Suitable for combined dissolution/permeation studies |
| Transport buffers (HBSS) | Physiological simulation during transport assays | Can be modified with pH gradients to simulate GI conditions |
| Efflux transporter inhibitors | Identify P-gp/BCRP-mediated transport | Use verapamil (P-gp inhibitor) or Ko143 (BCRP inhibitor) |
| TEER measurement system | Monitor cell monolayer integrity | Essential quality control for cell-based models |
| LC-MS/MS systems | Quantitative analysis of compound permeability | Provides sensitivity and specificity for low permeability compounds |
Emerging Technologies and Future Directions
How is artificial intelligence transforming absorption prediction?
AI-integrated QSAR modeling represents a revolutionary advancement in predicting absorption and permeability [64]:
- Advanced Algorithms: Machine learning (Random Forests, SVM) and deep learning (graph neural networks) capture complex structure-permeability relationships beyond traditional linear models
- Enhanced Descriptors: 4D descriptors accounting for conformational flexibility and quantum chemical descriptors provide more realistic molecular representations
- Integration with Complementary Methods: Molecular docking and dynamics simulations offer structural insights into ligand-target interactions
- ADMET Prediction: Comprehensive absorption, distribution, metabolism, excretion, and toxicity profiling early in discovery
The Random Forest algorithm is particularly valuable in QSAR modeling due to its robustness, built-in feature selection, and ability to handle noisy data. Feature importance ranking methods like SHAP (SHapley Additive exPlanations) allow researchers to understand which molecular descriptors most influence permeability predictions [64].
What novel experimental systems are addressing current limitations?
Emerging three-dimensional models provide greater physiological relevance [62]:
- Organ-on-a-chip systems: Microfluidic devices that replicate intestinal tissue complexity and flow dynamics
- Induced pluripotent stem cell (iPSC) models: Human-derived intestinal epithelial cells with patient-specific characteristics
- Cell spheroids: Three-dimensional structures that better mimic tissue architecture
- Advanced co-culture systems: Incorporation of mucus-producing cells, immune cells, and microbiota for comprehensive absorption assessment
These systems address critical limitations of traditional models, including the absence of mucosal layers, flow dynamics, and cellular heterogeneity present in human intestine, potentially improving the predictive accuracy of absorption studies [62].
Assessing Efficacy: Analytical Methods, Permeability Models, and Comparative Analysis
Prodrugs are biologically inactive derivatives of active pharmaceutical compounds, designed to overcome various pharmaceutical and pharmacological barriers, such as poor solubility, limited bioavailability, and undesirable side effects. The crucial step in successful prodrug design is its efficient activation to release the active parent drug at the desired site of action. This technical support center provides comprehensive troubleshooting guidance for researchers validating prodrug performance across experimental models, framed within the broader context of strategies for prodrug design and formulation research.
Validating prodrug performance requires an integrated approach utilizing in silico (computational), in vitro (cell-free and cell-based), and in vivo (animal model) systems. Each model offers specific advantages and presents unique challenges. This guide addresses common experimental issues through targeted FAQs and troubleshooting protocols, supported by quantitative data comparisons and standardized methodologies essential for drug development professionals.
Troubleshooting Guides: Addressing Common Experimental Challenges
Stability and Metabolic Conversion Issues
Problem: Poor correlation between in vitro and in vivo prodrug stability data.
Prodrug stability correlations can vary significantly across different experimental systems. The table below summarizes observed correlation strengths from systematic studies:
Table 1: Correlation of Prodrug Stability Between Experimental Models
| Tissue Type | Comparison System | Correlation Strength (r²) | Slope Range | Reference |
|---|---|---|---|---|
| Human Small Bowel | Caco-2 Cell Homogenate | 0.79 - 0.98 | 1.0 - 1.3 | [65] |
| Human Pancreas | AsPC-1 & Capan-2 Cell Homogenates | 0.58 - 0.79 | 0.5 - 0.8 | [65] |
| Human Liver | Human Liver Microsomes | 0.07 - 0.24 | 1.3 - 1.9 | [65] |
Troubleshooting Guide:
Issue: Weak liver stability correlation
- Potential Cause: Species differences in metabolic enzymes between human liver microsomes and tissue homogenates.
- Solution: Utilize humanized liver mouse models (e.g., Hu-URG mice) which have demonstrated excellent correlation (r = 0.98) for ester prodrugs [66]. Validate with multiple donor microsome preparations to account for human variability.
Issue: Inconsistent enzymatic conversion rates
- Potential Cause: Enzyme activity loss in prepared homogenates or microsomes.
- Solution: Standardize enzyme activity assays using reference substrates. Include positive controls in every experiment. Use fresh tissue preparations and validate freezing-thawing cycles [65].
Issue: Unpredictable activation kinetics
- Potential Cause: Insufficient characterization of activating enzymes.
- Solution: Perform comprehensive reaction phenotyping using chemical inhibitors, recombinant enzymes, and antibody inhibition studies to identify primary enzymes responsible for prodrug conversion [66].
Experimental Protocol: Prodrug Stability in Tissue Homogenates
- Preparation: Homogenize tissues (e.g., pancreas, liver, small intestine) in appropriate buffer (50-100 mg tissue/mL). Prepare cell homogenates from cultured cells (Caco-2, AsPC-1, Capan-2) at similar protein concentrations [65].
- Incubation: Add prodrug to homogenate (final concentration 10-100 µM) and incubate at 37°C.
- Sampling: Withdraw aliquots at predetermined time points (e.g., 0, 5, 15, 30, 60, 120 min).
- Analysis: Terminate reaction with organic solvent, centrifuge, and analyze supernatant using HPLC or LC-MS.
- Calculation: Determine half-life (t½) from logarithmic concentration-time plots.
In Silico Prediction Challenges
Problem: Computational models fail to accurately predict experimental results.
Table 2: Performance of In Silico Methods for Prodrug Development
| Computational Method | Prediction Accuracy | Computational Cost | Best Use Cases | Limitations |
|---|---|---|---|---|
| Molecular Docking | ~20% | Low | Initial screening, binding pose prediction | Limited database, poor pose choice [67] [44] |
| Molecular Dynamics (MD) | ~80% | High | Enzyme-substrate binding, linker optimization | Time-consuming, requires expertise [67] [44] |
| Free Energy Perturbation (FEP) | High (~80%) | Very High | Binding affinity predictions | Complex setup, resource-intensive [44] |
| Quantum Mechanics/Molecular Mechanics (QM/MM) | High | High | Chemical reaction mechanisms | Limited system size [67] |
Troubleshooting Guide:
Issue: Poor docking accuracy
- Potential Cause: Wrong choice of docking pose or incorrect binding site identification.
- Solution: Use multiple docking algorithms and cross-validate results. Perform molecular dynamics simulations to confirm docking pose stability [44].
Issue: Mismatch between predicted and experimental intrinsic dissolution rates (IDR)
- Potential Cause: Inaccurate force field parameters or insufficient simulation time.
- Solution: Combine different computational approaches. For example, use DDDPlus for dissolution predictions alongside experimental validation. For psilocybin, in silico IDR predictions showed correct trends but varying absolute values compared to experimental data [68].
Issue: Inability to predict metabolic activation
- Potential Cause: Lack of enzyme structural data or insufficient conformational sampling.
- Solution: Apply MD simulations to study enzyme dynamics. For CYP450 enzymes, MD simulations have successfully elucidated mechanisms of amino acid replacement that influence prodrug metabolism and regioselectivity [67].
Experimental Protocol: Molecular Dynamics for Prodrug Activation
- System Setup: Obtain protein structure from PDB. Prepare prodrug structure using quantum mechanics calculations.
- Solvation: Solvate the system in a water box (e.g., TIP3P water molecules) with appropriate counterions.
- Equilibration: Perform energy minimization followed by gradual heating to 310K and equilibration at 1 atm pressure.
- Production Run: Conduct MD simulation for sufficient time (typically 100-200 ns) to observe relevant conformational changes.
- Analysis: Analyze root mean square deviation (RMSD), binding free energies, and interaction patterns [67].
In Vivo Translation Difficulties
Problem: Promising in vitro results fail to translate to in vivo efficacy.
Troubleshooting Guide:
Issue: Species-specific metabolism differences
- Potential Cause: Differential expression or activity of activating enzymes between species.
- Solution: Use humanized animal models. For ester prodrug HD56, humanized liver mice successfully addressed species differences and provided excellent in vivo-in vitro correlation (r = 0.98) [66].
Issue: Incorrect dosing regimen
- Potential Cause: Lack of preliminary pharmacokinetic data.
- Solution: Perform dose-range finding studies and preliminary PK evaluation before efficacy experiments. Estimate appropriate dosing schedules to achieve therapeutic concentrations while avoiding toxicity [69].
Issue: Poor bioavailability despite good permeability
- Potential Cause: Pre-systemic metabolism or efflux transport.
- Solution: Investigate bidirectional transport in Caco-2 or LLC-PK1 cells overexpressing transporters like MDR1. Identify major metabolic pathways using recombinant enzymes and chemical inhibitors [66].
Experimental Protocol: In Vivo Efficacy Study Design
- Model Selection: Choose appropriate tumor models (subcutaneous, orthotopic, metastatic) based on research questions [69].
- Randomization: Randomize animals based on tumor volume and body weight once tumors are palpable to remove bias.
- Dosing: Administer prodrug via clinical route. Include appropriate controls (standard-of-care, unformulated drug, vehicle, unloaded nanoparticle) [69].
- Monitoring: Measure tumor volume and body weight regularly. Use Kaplan-Meier analysis for survival data.
- Sample Size: Calculate using statistical power analysis. For tumor volume data: n = 1 + 2C × (s/d)² where s is standard deviation, d is anticipated difference, and C is 7.85 [69].
Essential Research Reagent Solutions
Table 3: Key Research Reagents for Prodrug Development
| Reagent / Model | Function in Prodrug Development | Application Examples |
|---|---|---|
| Caco-2 Cell Homogenate | Predicts stability in human small intestine | Correlation with small bowel stability (r² = 0.79-0.98) [65] |
| Human Liver Microsomes | Assess hepatic metabolism and stability | Weak correlation with liver tissue (r² = 0.07-0.24) [65] |
| Humanized Liver Mice (Hu-URG) | In vivo model for human-specific metabolism | Ester prodrug evaluation (r = 0.98 correlation) [66] |
| Carboxylesterase Enzymes | Key enzymes for ester prodrug activation | Reaction phenotyping [66] |
| Molecular Dynamics Software | Predict enzyme-substrate interactions and binding | PLA2-mediated prodrug activation optimization [44] |
| PAMPA Assays | Preliminary permeability screening | Biopharmaceutics Classification System categorization [68] |
Frequently Asked Questions (FAQs)
Q1: What is the most reliable in vitro system for predicting intestinal stability of amino acid/dipeptide prodrugs? Caco-2 cell homogenates show excellent correlation (r² = 0.79-0.98) with human small bowel tissue homogenate for floxuridine prodrug stability. The slope of 1.0-1.3 indicates highly comparable degradation rates between these systems [65].
Q2: How can we address the poor correlation between human liver microsomes and liver tissue for prodrug stability? The weak correlation (r² = 0.07-0.24) suggests significant limitations in using liver microsomes alone. Supplement with hepatocytes, tissue slices, or transition to humanized liver mouse models which have demonstrated excellent correlation (r = 0.98) for ester prodrugs [65] [66].
Q3: Which in silico method provides the best balance of accuracy and computational efficiency for prodrug design? While molecular docking is fast, its accuracy is low (~20%). Molecular dynamics simulations offer significantly better accuracy (~80%) and can guide linker optimization in phospholipid-based prodrugs, making them a valuable investment for critical design decisions [67] [44].
Q4: What controls are essential for in vivo efficacy studies of nanoformulated prodrugs? Include standard-of-care treatment, free (unformulated) drug control, vehicle control, and unloaded nanoparticle control. If the formulation has a targeting ligand, include an untargeted version. Dose cytotoxic formulations at equivalent and equitoxic MTD doses [69].
Q5: How can we mimic subcutaneous prodrug conversion in vitro? Incorporate active enzymes into artificial extracellular matrix systems. The SCISSOR platform has successfully conserved biorelevant enzymatic activity for studying subcutaneous prodrug formulations by adding relevant enzymes to the testing medium [70].
Visual Workflows for Prodrug Validation
Comprehensive Prodrug Validation Cascade
The following diagram illustrates the integrated approach to prodrug validation, highlighting the key steps and decision points in the experimental cascade:
Computational Methods Hierarchy
This diagram illustrates the relationship between different computational methods used in prodrug design, showing their relative accuracy and computational complexity:
Effective validation of prodrug performance requires careful model selection and interpretation of data across the development pipeline. The troubleshooting guides and FAQs presented here address common challenges in predicting stability, metabolic conversion, and in vivo translation. By implementing these standardized protocols and understanding the limitations of each model system, researchers can accelerate prodrug development and improve prediction accuracy from experimental systems to clinical outcomes.
BCS and Prodrugs: A Troubleshooting FAQ
1. How can the BCS framework guide the initial design of a prodrug?
The BCS classifies drug substances based on their aqueous solubility and intestinal permeability into four categories, which helps identify the primary absorption barrier for a parent drug and informs the strategic goal of a prodrug approach [71] [72]. For a BCS Class II drug (low solubility, high permeability), the prodrug strategy should primarily aim to enhance solubility. Conversely, for a BCS Class III drug (high solubility, low permeability), the design should focus on improving permeability, often by increasing the molecule's lipophilicity to facilitate passive diffusion [12] [4].
2. Our prodrug shows excellent in vitro solubility/permeability, but in vivo performance is poor. What could be happening?
This is a common challenge often related to the kinetics of prodrug activation [73]. The prodrug may not be efficiently converted to the active parent drug in the gastrointestinal (GI) lumen or at the absorption site. The absorption of many prodrugs is highly dependent on in vivo conversion kinetics by enzymes such as esterases, phosphatases, or other hydrolases. Incomplete conversion due to inter-individual variability in enzyme activity or expression can lead to insufficient exposure to the active moiety [3] [16] [73]. We recommend using more predictive in vitro models like dissolution/permeation (D/P) systems that can simultaneously simulate dynamic dissolution, permeation, and conversion processes [73].
3. How can we establish clinically relevant dissolution specifications (CRDS) for a BCS Class IV prodrug?
For challenging compounds like BCS Class IV prodrugs (low solubility, low permeability), establishing a CRDS requires moving beyond traditional pharmacopoeial methods [73]. A robust framework involves:
- Using Biorelevant Media: Employ dissolution media that mimic the dynamic conditions of the GI tract (e.g., FaSSIF/FeSSIF) to account for the impact of bile salts and lipids on solubility and dissolution [73].
- Integrating Permeation: Utilize a dissolution/permeation (D/P) system to dynamically assess the interplay between drug dissolution and absorption [73].
- Leveraging Modeling: Apply Physiologically Based Biopharmaceutics Modeling (PBBM) to integrate in vitro data and establish a dissolution "safe space" that ensures bioequivalence [73].
4. What are the critical stability considerations when formulating a prodrug?
Prodrugs can present unique stability challenges that differ from the parent drug [5]. Key issues include:
- Linker Instability: The chemical linker (e.g., ester, carbonate) between the drug and promoiety can be susceptible to hydrolysis or other degradation pathways in the solid state or in solution, leading to formation of the active drug or other degradants prematurely [5].
- Reactive Degradants: Degradation of the prodrug may generate reactive intermediates that can initiate secondary degradation pathways or interact with excipients [5].
- Solid-State Properties: Prodrug formation can disrupt the solid-state crystallinity of the parent drug, leading to issues with polymorphism, which can affect physical stability and dissolution [5].
Essential Experimental Protocols for Prodrug Assessment
Protocol 1: Determining BCS Classification for a Prodrug
Objective: To experimentally determine the solubility and permeability of a prodrug for accurate BCS classification [71] [12].
Materials:
- Prodrug compound
- USP buffer solutions (pH 1.0 to 6.8)
- Shaking water bath
- HPLC system with UV detector
- Caco-2 cell line or parallel artificial membrane permeability assay (PAMPA) kit
- Transport buffer (e.g., Hanks' Balanced Salt Solution, HBSS)
Method: A. Solubility Determination:
- Prepare a saturated solution of the prodrug in each buffer pH by adding an excess amount to the medium.
- Equilibrate in a shaking water bath at 37°C for a minimum of 24 hours.
- Filter the solution through a 0.45 µm membrane filter.
- Analyze the filtrate using a validated HPLC-UV method to determine the equilibrium concentration.
- A drug is considered highly soluble if the highest single therapeutic dose dissolves in 250 mL or less of aqueous medium across the pH range of 1.0–6.8 [71] [72].
B. Permeability Assessment (Using Caco-2 Model):
- Culture Caco-2 cells on semi-permeable membranes until they form a confluent, differentiated monolayer (typically 21 days).
- Add the prodrug to the donor compartment (e.g., apical for intestinal absorption studies) in transport buffer.
- Incubate at 37°C and sample from the receiver compartment at predetermined time points.
- Analyze samples by HPLC to determine the prodrug concentration.
- Calculate the apparent permeability coefficient (Papp). A prodrug is typically considered highly permeable if its human intestinal absorption extent is ≥85% [71] [12]. This is often correlated with Papp values from validated cell models.
Protocol 2: Integrated Dissolution/Permeation System for Prodrugs
Objective: To simultaneously evaluate the dissolution and permeation behavior of a prodrug formulation under biorelevant conditions, providing a more predictive assessment of in vivo performance [73].
Materials:
- Dissolution/Perfusion (D/P) system (e.g., using chambers with artificial membranes)
- Biorelevant media (FaSSIF for fasted state, FeSSIF for fed state)
- Peristaltic pumps
- HPLC system
Method:
- Media Preparation: Prepare the donor (dissolution) compartment with a volume of biorelevant medium (e.g., FaSSIF, pH 6.5) and maintain at 37°C.
- Sample Loading: Introduce the prodrug formulation (e.g., powder or intact tablet) into the donor chamber.
- Permeation Simulation: The acceptor (permeation) compartment contains a pH-buffered solution and is separated from the donor compartment by a permeable membrane that mimics the intestinal barrier.
- Dynamic Sampling: Using a peristaltic pump, the dissolved drug in the donor compartment is circulated to contact the membrane, and samples are collected from both donor and acceptor compartments over time.
- Analysis: Quantify the concentrations of both the prodrug and the active parent drug in all samples using HPLC. This allows you to profile the dissolution, conversion, and permeation kinetics simultaneously [73].
Diagram 1: Integrated dissolution/permeation system workflow for prodrug assessment.
Research Reagent Solutions Toolkit
Table 1: Essential reagents and materials for prodrug assessment experiments.
| Reagent/Material | Function in Experiment | Key Considerations |
|---|---|---|
| Biorelevant Media (FaSSIF/FeSSIF) | Simulates fasted and fed state intestinal fluids for dissolution testing [73]. | Critical for predicting food effects and supersaturation potential. |
| Caco-2 Cell Line | A standard in vitro model for predicting human intestinal permeability [12]. | Requires long culture time (21 days); expresses various transporters and enzymes. |
| Artificial Membranes (PAMPA) | Used in permeability screening; models passive diffusion [12]. | Faster and lower cost than cell-based models but lacks transporter and metabolic activity. |
| Esterases / Phosphatases | Enzymes used to study the enzymatic conversion kinetics of prodrugs [3] [16]. | Enzyme source and concentration should be selected to reflect the target tissue (e.g., intestinal vs. hepatic). |
| LC-MS/MS System | For quantitative analysis of prodrug and parent drug in complex matrices [73]. | Essential for discerning the prodrug from its active metabolite and degradation products. |
Advanced Troubleshooting: Addressing Complex Scenarios
5. How can we assess the risk of bioequivalence failure for a prodrug product?
Bioequivalence risk is high for prodrugs, especially those classified as BCS Class IV or those exhibiting high variability [73]. Mitigation involves:
- Identify Critical Variables: Focus on parameters that most impact absorption: particle size (affecting dissolution rate), conversion enzyme variability, and food effects [73].
- Define a "Safe Space": Use PBBM to establish a range of dissolution profiles (e.g., in biorelevant media) that are bioequivalent. Formulations whose dissolution falls within this "safe space" have a low risk of bioequivalence failure [73].
- Control Conversion Kinetics: Ensure that excipients in the formulation do not inhibit or excessively accelerate the enzymatic conversion of the prodrug.
6. What modern in silico tools can support prodrug design and permeability prediction?
In silico methods are valuable in early development to prioritize promising candidates [12].
- Computational LogP Predictors: Tools like ALOGP and KLOGP estimate the lipophilicity of the prodrug, a key driver of passive permeability [12].
- Molecular Dynamics (MD) Simulations: Can simulate the permeation of the prodrug molecule through a lipid bilayer, providing an estimated permeability coefficient (Pe) [12].
- Rule-Based Filters: Applying the "Rule of Five" can provide an initial alert for potential permeability or absorption problems—molecules with more than 5 H-bond donors, 10 H-bond acceptors, a molecular weight >500, and LogP >5 often show poor permeability [12].
Table 2: Troubleshooting common experimental discrepancies in prodrug development.
| Observation | Potential Root Cause | Investigative Action |
|---|---|---|
| Low apparent permeability in Caco-2 assay | Prodrug is a substrate for efflux transporters (e.g., P-glycoprotein). | Conduct transport assays with and without efflux transporter inhibitors (e.g., GF120918). |
| Unexpected degradation products in dissolution media | Chemical instability of the prodrug linker at specific pH values [5]. | Perform forced degradation studies across a pH range (1-8) to identify stable formulation conditions. |
| Poor in vitro-in vivo correlation (IVIVC) | In vitro test does not capture key in vivo processes (e.g., luminal metabolism, supersaturation) [73]. | Adopt a more complex in vitro model, such as a D/P system with biorelevant media and enzyme supplementation [73]. |
In modern drug development, overcoming challenges related to a compound's solubility, permeability, and stability is paramount for achieving therapeutic efficacy. Two fundamental approaches to addressing these challenges are conventional formulations and prodrug design. Conventional formulations involve pharmaceutical technologies that modify the drug's delivery system without altering its chemical structure, while prodrug strategies employ chemical modification to create biologically inactive precursors that undergo conversion to the active drug within the body [74]. This analysis compares these strategies within the context of modern drug development, providing researchers with a technical framework for selecting the optimal approach for their specific experimental challenges.
The prodrug approach represents a versatile strategy for optimizing biopharmaceutical and pharmacokinetic parameters. Prodrugs are compounds with reduced or no biological activity that, through enzymatic or chemical processes, release the active parent drug in vivo [12]. Notably, approximately 13% of drugs approved by the U.S. Food and Drug Administration (FDA) between 2012 and 2022 were prodrugs, underscoring the importance of this strategy in addressing drug development challenges [12].
Table 1: Fundamental Characteristics of Formulation Strategies
| Feature | Conventional Formulations | Prodrug Strategy |
|---|---|---|
| Chemical Structure | Unmodified active pharmaceutical ingredient (API) | Chemically modified bio-reversible derivative of API |
| Mechanism of Action | Physical/mechanical modification of drug delivery | Enzymatic or chemical conversion to active metabolite |
| Primary Applications | Addressing solubility, stability, palatability | Enhancing permeability, bioavailability, targeted delivery |
| Development Timeline | Often shorter development cycles | Can involve more complex chemical synthesis and validation |
| Regulatory Considerations | Well-established pathways | Requires demonstration of conversion efficacy and safety of promotety |
Troubleshooting Guide: Common Experimental Challenges
FAQ: How do I address poor aqueous solubility of my lead compound?
Challenge: Insufficient aqueous solubility is one of the most prevalent issues in drug development, affecting approximately 40% of marketed drugs and up to 75% of compounds in development [12]. This often results in low bioavailability and limited therapeutic application.
Conventional Formulation Solutions:
- Solid Dispersions: Disperse the API within a hydrophilic matrix to improve dissolution characteristics [9].
- Nanocrystal Technology: Reduce API particle size to the nanoscale (nanosuspensions) to significantly increase surface area and enhance dissolution rate [9].
- Lipid-Based Systems: Utilize lipid excipients to solubilize lipophilic compounds and enhance gastrointestinal absorption [12] [9].
- Cyclodextrin Complexation: Form inclusion complexes with cyclodextrins to mask hydrophobic regions of drug molecules and improve apparent solubility [12].
Prodrug Strategy Solutions:
- Salt Formation: Create phosphate, sulfate, or other water-soluble salt forms of ionizable functional groups to dramatically enhance aqueous solubility [25]. For example, morpholinyl-based prodrugs of cannabidiol demonstrated up to 24-fold better solubility than the parent compound [25].
- PEGylation: Conjugate with polyethylene glycol (PEG) to create amphiphilic prodrugs with improved solubilization characteristics [25].
- Amino Acid Conjugation: Link hydrophobic drugs to amino acids (e.g., valine) to create water-soluble prodrugs that can leverage active transport mechanisms [25].
FAQ: What approaches can enhance membrane permeability?
Challenge: Low membrane permeability prevents otherwise effective compounds from reaching intracellular targets or achieving adequate systemic exposure, particularly for Biopharmaceutical Classification System (BCS) Class III and IV drugs [12].
Conventional Formulation Solutions:
- Permeation Enhancers: Incorporate excipients that temporarily disrupt epithelial tight junctions or fluidize membrane structures [75].
- Nanocarrier Systems: Utilize lipid nanoparticles, polymeric nanoparticles, or micelles that can facilitate transport across biological barriers through various pathways [75].
- Ionic Liquid Forms: Transform acidic or basic APIs into ionic liquids that demonstrate significantly enhanced dissolution rates and transepithelial transport—one study showed a 700-fold faster dissolution rate and approximately three times higher transport compared to a prodrug approach [76].
Prodrug Strategy Solutions:
- Lipophilicity Enhancement: Temporarily mask polar functional groups (e.g., hydroxyl, carboxyl) with non-polar promoieties to increase logP and facilitate passive diffusion [12] [74]. A study analyzing prodrug design goals found that approximately 35% of applications aimed to enhance permeability through this mechanism [12].
- Carrier-Mediated Transport Targeting: Design prodrugs that are substrates for specific transporters (e.g., peptide transporters, nucleoside transporters) to enable active uptake processes [74]. Valacyclovir, the L-valyl ester prodrug of acyclovir, utilizes the peptide transporter PEPT1 to achieve 3-5 times higher bioavailability than the parent drug [74].
Table 2: Permeability Enhancement Strategies Comparison
| Strategy | Mechanism | Experimental Considerations |
|---|---|---|
| Chemical Permeation Enhancers | Temporary membrane disruption | Potential for local toxicity; concentration-dependent effects |
| Nanocarrier Systems | Alternative transport pathways | Complex manufacturing; characterization of particle size and distribution |
| Ionic Liquid Forms | Improved dissolution and supersaturation | Limited database of GRAS counterions; long-term toxicity assessment |
| Prodrug Lipophilicity Enhancement | Increased passive diffusion | Must balance lipophilicity to avoid solubility limitations |
| Targeted Prodrug Transport | Exploitation of endogenous transporters | Species differences in transporter expression; potential for saturation |
FAQ: How can I mitigate chemical instability and degradation?
Challenge: Chemical degradation of the API in formulation or during storage compromises therapeutic efficacy and can generate potentially toxic degradation products.
Conventional Formulation Solutions:
- Lyophilization: Remove water to prevent hydrolysis-driven degradation pathways for moisture-sensitive compounds [5].
- Antioxidant Incorporation: Add reducing agents (e.g., ascorbic acid, BHT) to the formulation to protect against oxidative degradation [9].
- Protective Packaging: Use specialized packaging materials (e.g, amber glass, blister packs with desiccants) to shield the product from light, oxygen, and moisture [9].
- pH Adjustment: Optimize the pH of liquid formulations to stabilize compounds susceptible to acid- or base-catalyzed degradation [5].
Prodrug Strategy Solutions:
- Stable Linker Design: Incorporate chemically stable linkers (e.g., carbamates, amides) between the drug and promoiety that resist degradation until enzymatic activation in vivo [5] [16].
- Bioprecursor Approach: Design prodrugs that are not simple derivatives but require molecular transformation (e.g., oxidation, reduction) to generate the active drug, often exhibiting superior stability profiles [16].
Experimental Protocols for Prodrug Evaluation
Protocol: Permeability Assessment for Prodrug Candidates
Purpose: To evaluate and compare the membrane permeability of prodrug candidates against the parent drug using established in vitro models.
Materials:
- Caco-2 Cell Monolayers: Human colon adenocarcinoma cell line model of intestinal absorption (citation:1] [76]
- Transwell/Permeability Support Systems: Multi-well plates with permeable membrane inserts
- Transport Buffer: Hanks' Balanced Salt Solution (HBSS) with appropriate pH adjustment
- LC-MS/MS System: For quantitative analysis of drug and prodrug concentrations
Procedure:
- Culture Caco-2 cells on permeable supports for 21 days until full differentiation and tight junction formation.
- Confirm monolayer integrity by measuring transepithelial electrical resistance (TEER) values >300 Ω·cm².
- Prepare prodrug and parent drug solutions in transport buffer at physiologically relevant concentrations.
- Apply drug solutions to the donor compartment (apical for absorption studies).
- Sample from the receiver compartment at predetermined timepoints (e.g., 30, 60, 90, 120 minutes).
- Analyze samples using LC-MS/MS to quantify drug/prodrug concentrations.
- Calculate apparent permeability (Papp) using the formula: Papp = (dQ/dt) / (A × C₀), where dQ/dt is the transport rate, A is the membrane surface area, and C₀ is the initial donor concentration.
Troubleshooting Tip: If prodrug instability is observed during the assay, add esterase inhibitors to the transport buffer to distinguish between inherent permeability and permeability following conversion to parent drug.
Protocol: Kinetic Evaluation of Enzymatic Prodrug Conversion
Purpose: To determine the conversion kinetics of prodrug to active drug in biological matrices.
Materials:
- Biological Matrices: Human plasma, liver microsomes, S9 fractions, or specific enzyme solutions
- Enzyme-Specific Substrates/Inhibitors: For reaction phenotyping (e.g., eserine for cholinesterases, BNPP for carboxylesterases)
- Analytical Instrumentation: HPLC-UV or LC-MS/MS system with appropriate detection capabilities
- Incubation System: Water bath or thermal block maintained at 37°C
Procedure:
- Prepare prodrug solution in appropriate buffer at concentrations relevant to expected therapeutic levels.
- Pre-incubate biological matrix at 37°C for 5 minutes.
- Initiate reaction by adding prodrug solution to the matrix.
- Aliquot samples at predetermined timepoints (e.g., 0, 5, 15, 30, 60, 120 minutes).
- Immediately quench reactions with organic solvent (e.g., acetonitrile with internal standard).
- Centrifuge to precipitate proteins and analyze supernatant for both prodrug and active drug concentrations.
- Plot concentration versus time and calculate conversion half-life (t₁/₂) and other kinetic parameters.
Diagram 1: Prodrug Activation and Metabolic Pathways. For therapeutic efficacy, the activation rate constant (k_bio) must exceed both the elimination rate of the prodrug (k_el1) and the elimination rate of the active drug (k_el2).
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Prodrug Formulation Studies
| Reagent/Category | Function/Application | Specific Examples |
|---|---|---|
| In Vitro Permeability Models | Prediction of intestinal absorption potential | Caco-2 cells, MDCK cells, PAMPA assay system [12] |
| Metabolic Enzyme Systems | Evaluation of prodrug activation kinetics | Carboxylesterases, phosphatase enzymes, cytochrome P450 isoforms [16] |
| Analytical Standards | Quantification of prodrug and active drug | LC-MS/MS internal standards, stable isotope-labeled compounds |
| Chemical Promoieties | Prodrug synthesis and optimization | Amino acids (valine, isoleucine), phosphate esters, lipid conjugates [25] [74] |
| Computational Tools | In silico prediction of properties | LogP calculators, molecular dynamics simulations, machine learning algorithms [12] |
Diagram 2: Formulation Strategy Selection Workflow
The selection between conventional formulation approaches and prodrug strategies depends on the specific physicochemical and biopharmaceutical limitations of the active compound. Conventional formulations offer practical solutions for solubility and stability challenges without chemical synthesis, while prodrug strategies provide more fundamental solutions to permeability and targeting issues through chemical modification. The growing percentage of FDA-approved prodrugs (approximately 13% between 2012-2022) demonstrates the increasing importance of this approach in modern pharmaceutical development [12]. Researchers should consider a systematic evaluation beginning with conventional approaches for simpler challenges, progressing to prodrug strategies when more sophisticated solutions are required for bioavailability, targeting, or metabolic stability limitations.
Proteolysis-targeting chimeras (PROTACs) represent a revolutionary therapeutic modality with the potential to degrade disease-causing proteins that have historically been considered "undruggable" by traditional small-molecule inhibitors [77]. These heterobifunctional molecules operate by recruiting E3 ubiquitin ligases to facilitate the ubiquitination and subsequent proteasomal degradation of target proteins through an event-driven, catalytic mechanism [78]. Despite their considerable promise, the clinical translation of PROTACs faces significant pharmacological challenges, primarily stemming from their inherently large molecular weight and excessive polar surface area, which often result in poor membrane permeability, suboptimal bioavailability, and inadequate pharmacokinetic profiles [79] [77].
The prodrug approach has emerged as a powerful strategy to overcome these limitations, enabling spatiotemporally controlled protein degradation with enhanced specificity and reduced systemic toxicity [78] [80]. By designing PROTACs as inactive precursors that undergo selective activation at the target site through specific stimuli, researchers can mitigate off-target effects while improving drug-like properties [81]. This paradigm shift from traditional active compounds to stimulus-activated prodrugs represents a significant advancement in the field of targeted protein degradation, particularly for complex molecules that violate conventional drug-likeness rules such as Lipinski's Rule of Five [79] [12].
This technical resource center provides comprehensive guidance on implementing prodrug strategies for PROTACs and other complex molecules, featuring troubleshooting guides, experimental protocols, and practical solutions to common challenges encountered during research and development.
Troubleshooting Guide: Common Challenges in PROTAC Prodrug Development
Table 1: Troubleshooting Common PROTAC Prodrug Challenges
| Challenge | Potential Causes | Solutions & Optimization Strategies |
|---|---|---|
| Poor Cellular Permeability | High molecular weight (>800 Da), excessive polar surface area, violation of Lipinski's Rule of Five [79] | • Implement prodrug strategy with lipophilic promoteties [12]• Optimize linker length and hydrophobicity [79]• Reduce molecular weight through smaller ligands [79] |
| Insufficient Solubility | High lipophilicity, strong intermolecular interactions, crystalline solid state [5] [79] | • Formulate with phosphate or sulfate promoteties to enhance aqueous solubility [3]• Employ nanocarrier systems (liposomes, polymers) [78] [79]• Develop lipid-based formulations [5] |
| Premature Activation | Chemical instability in physiological buffers, enzymatic cleavage in non-target tissues [5] | • Optimize linker chemistry for enhanced stability [5]• Design stimuli-responsive linkers activated only by specific tumor microenvironment cues [81] [77] |
| Inadequate Target Engagement | Insufficient prodrug-to-active conversion, suboptimal ternary complex formation, "hook effect" [77] | • Validate enzyme expression in target tissues [3]• Optimize stimuli-responsive elements (light wavelength, enzyme substrates) [78]• Fine-tune administration dosage to mitigate hook effect [77] |
| Systemic Toxicity | "On-target but off-tissue" protein degradation, non-selective E3 ligase expression [78] [77] | • Develop tissue-specific targeting approaches [77]• Implement spatiotemporally controlled activation (light, ultrasound) [81] [78] |
Table 2: Assessment Methods for PROTAC Prodrug Permeability and Solubility
| Parameter | Experimental Methods | Key Considerations |
|---|---|---|
| Permeability | • PAMPA assay• Caco-2 cell models• MDCK cell monolayers [12] | • Correlate apparent permeability (Papp) with in vivo data• Assess transporter involvement through inhibition studies [12] |
| Solubility | • Shake-flask method• Thermodynamic solubility measurement• Fed-state simulated intestinal fluid screening [79] | • Evaluate in both aqueous and biorelevant media• Monitor solid-state form changes [5] |
| Activation Kinetics | • In vitro plasma stability assay• Cell lysate incubation• Tissue homogenate studies [3] | • Compare activation rates across different biological matrices• Identify specific enzymes responsible for conversion [3] |
| Membrane Permeability Prediction | • In silico logP calculations• Molecular dynamics simulations• Machine learning algorithms [12] | • Apply "rule of five" as preliminary filter• Consider beyond-rule-of-five exceptions for complex molecules [12] |
Frequently Asked Questions (FAQs)
Q1: What specific physicochemical properties of PROTACs make them particularly suitable for prodrug approaches?
PROTACs typically exhibit molecular weights exceeding 800 Da, high polar surface area (>200 Ų), and multiple hydrogen bond donors and acceptors, leading to poor membrane permeability and limited oral bioavailability [79] [77]. Their bipartite structure, comprising target protein ligands and E3 ligase recruiters connected by linkers, provides multiple sites for chemical modification through prodrug design [78]. Additionally, the catalytic mechanism of PROTACs means that even modest improvements in delivery efficiency can yield significant therapeutic benefits, making prodrug strategies particularly valuable [77].
Q2: How do stimulus-responsive PROTAC prodrugs achieve spatial and temporal control of protein degradation?
Stimulus-responsive PROTAC prodrugs incorporate cleavable masking groups that are removed by specific endogenous or exogenous stimuli, enabling precise activation at the target site [81]. For example:
- Photoactivatable PROTACs contain photocleavable groups (e.g., DMNB) that are removed upon UV or near-infrared irradiation, allowing spatiotemporal control with millimeter precision [78].
- Enzyme-activated PROTACs are designed with substrates for enzymes overexpressed in target tissues (e.g., phospholipase A2 in inflamed tissues) [3].
- Redox-responsive PROTACs leverage differential glutathione levels in tumor microenvironments for selective activation [77].
These approaches minimize off-target degradation and systemic toxicity by maintaining the PROTAC in an inactive state until reaching the desired site of action [81] [78].
Q3: What are the key considerations when selecting a promoiety for PROTAC prodrugs?
The selection of an appropriate promoiety depends on the specific limitation being addressed:
- For enhancing permeability: Lipophilic promotieties (alkyl, aryl chains) can reduce polarity and improve membrane crossing, but must be balanced against potential solubility reduction [12].
- For improving solubility: Hydrophilic groups (phosphate esters, sulfate esters) can significantly enhance aqueous solubility [3].
- For targeted activation: Enzyme-specific substrates or stimuli-labile linkers (e.g., thioketone bonds for singlet oxygen cleavage) enable site-selective activation [78]. Critical considerations include the efficiency of cleavage at the target site, the physicochemical properties of the released promoiety, and the potential biological activity of the promoiety itself [5].
Q4: What formulation challenges are unique to PROTAC prodrugs compared to traditional small molecules?
PROTAC prodrugs present distinct formulation challenges due to their complex structure and chemical properties [5] [79]:
- Chemical stability: The drug-promoiety linker may be susceptible to hydrolysis or enzymatic cleavage during storage, requiring specialized pharmaceutical development [5].
- Degradation products: Reactive intermediates formed during promoiety cleavage may cause secondary degradation pathways or interact with excipients [5].
- Polymorphism: Prodrug solid-state properties often differ from the parent drug, potentially affecting dissolution and bioavailability [5].
- Nanocarrier compatibility: When utilizing nanoparticle delivery systems, compatibility between the PROTAC prodrug and carrier materials must be carefully optimized [81] [79].
Experimental Protocols: Key Methodologies for PROTAC Prodrug Evaluation
Protocol: Assessing Cellular Permeability and Uptake of PROTAC Prodrugs
Principle: This protocol evaluates the membrane permeability and cellular uptake of PROTAC prodrugs using Caco-2 cell monolayers, a well-established model of intestinal absorption [12].
Reagents and Materials:
- Caco-2 cells (HTB-37, ATCC)
- DMEM culture medium with 10% FBS, 1% non-essential amino acids, and 1% penicillin-streptomycin
- Transport buffer: HBSS with 25 mM glucose and 10 mM HEPES, pH 7.4
- PROTAC prodrug and reference compounds
- LC-MS/MS system for analytical quantification
Procedure:
- Culture Caco-2 cells on collagen-coated Transwell inserts (3.0 μm pore size, 24-well format) for 21-28 days until transepithelial electrical resistance (TEER) values exceed 400 Ω·cm².
- Pre-incubate monolayers with transport buffer for 30 minutes at 37°C.
- Apply PROTAC prodrug solution (typically 10-100 μM in transport buffer) to the donor compartment (apical for A-B transport, basolateral for B-A transport).
- Incubate at 37°C with gentle shaking. At predetermined time points (30, 60, 90, 120 minutes), sample from the receiver compartment.
- Analyze samples using LC-MS/MS to quantify drug concentrations.
- Calculate apparent permeability (Papp) using the formula: Papp = (dQ/dt) / (A × C₀), where dQ/dt is the transport rate, A is the membrane area, and C₀ is the initial donor concentration.
Troubleshooting Tips:
- Include control compounds with known high (e.g., metoprolol) and low (e.g., atenolol) permeability to validate assay performance.
- Monitor TEER values before and after experiments to ensure monolayer integrity.
- Assess potential efflux transport involvement by including inhibitors like verapamil (for P-gp) or Ko143 (for BCRP) [12].
Protocol: Evaluating Enzymatic Activation of PROTAC Prodrugs
Principle: This method determines the conversion rate of PROTAC prodrugs to their active forms in biological matrices, providing critical insights for targeted activation strategies [3].
Reagents and Materials:
- Target enzyme or enzyme source (recombinant enzyme, tissue homogenates, cell lysates)
- Appropriate reaction buffer optimized for the specific enzyme
- Protease inhibitor cocktail (for non-protease enzymes)
- Stopping solution (typically organic solvent like acetonitrile with internal standard)
- UPLC-MS/MS system for analysis
Procedure:
- Prepare enzyme solution in appropriate buffer at physiologically relevant concentration.
- Pre-incubate enzyme solution at 37°C for 5 minutes.
- Initiate reaction by adding PROTAC prodrug solution (final concentration typically 1-50 μM).
- At predetermined time points (0, 5, 15, 30, 60, 120 minutes), withdraw aliquots and mix with stopping solution to denature enzymes and precipitate proteins.
- Centrifuge samples at 14,000 × g for 10 minutes and collect supernatant for analysis.
- Analyze samples by UPLC-MS/MS to quantify both prodrug and active PROTAC concentrations.
- Calculate conversion kinetics using appropriate models (e.g., first-order, Michaelis-Menten).
Troubleshooting Tips:
- Include controls without enzyme to account for chemical degradation.
- For tissue homogenates, normalize protein concentration across samples.
- Validate analytical method to ensure no interference from enzyme matrix or degradation products.
Research Reagent Solutions: Essential Tools for PROTAC Prodrug Development
Table 3: Key Research Reagents for PROTAC Prodrug Development
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| E3 Ligase Ligands | Thalidomide (CRBN), VHL ligands, MDM2 ligands [78] [77] | Recruit endogenous ubiquitin ligase machinery for target protein degradation |
| Photoactivatable Groups | Nitroveratryloxycarbonyl (NVOC), Dimethoxybenzoin (DMNB) [78] | Enable light-controlled PROTAC activation with spatial and temporal precision |
| Enzyme-Sensitive Linkers | Phospholipid-based linkers, peptide substrates, glucuronide conjugates [3] [77] | Provide selective activation in target tissues expressing specific enzymes |
| Permeability Enhancement Groups | Alkyl esters, carbonates, lipophilic amino acid esters (valyl, isoleucyl) [12] | Improve membrane penetration through increased lipophilicity |
| Solubility-Enhancing Promoieties | Phosphate esters, sulfate esters, polyethylene glycol (PEG) chains [3] | Address aqueous solubility limitations for improved formulation |
| Nanocarrier Systems | Liposomes, polymeric nanoparticles, albumin conjugates [78] [79] | Enhance delivery efficiency through passive or active targeting strategies |
Diagnostic Diagrams: PROTAC Prodrug Mechanisms and Assessment
PROTAC Prodrug Activation Mechanisms
Diagram 1: PROTAC Prodrug Activation and Catalytic Cycle. This workflow illustrates the sequential activation and mechanism of stimulus-responsive PROTAC prodrugs, highlighting their recyclable nature.
PROTAC Prodrug Permeability Assessment Methods
Diagram 2: Comprehensive Permeability Assessment Strategy for PROTAC Prodrugs. This diagram outlines the multi-faceted approach for evaluating membrane permeability across computational, cellular, tissue, and whole-animal models.
Conclusion
Prodrug design remains a powerful and versatile strategy in the modern drug development arsenal, effectively addressing pervasive challenges of solubility, permeability, and targeted delivery. By integrating foundational principles with advanced methodological approaches—including computational modeling and novel phospholipid-based systems—researchers can systematically overcome development hurdles. The future of prodrug technology is intrinsically linked to the adoption of machine learning for predictive design and its application to next-generation therapeutic modalities like PROTACs. Continued innovation in this field promises to yield more effective, safer, and highly targeted therapies, solidifying the prodrug approach as a cornerstone of strategic pharmaceutical development.
References
- 1. Prodrug [https://en.wikipedia.org/wiki/Prodrug]
- 2. What Is a Prodrug? How Prodrugs Work, Examples, and ... [https://www.goodrx.com/drugs/medication-basics/what-is-a-prodrug?srsltid=AfmBOoq_UUUjqNPZiO7uH00j0y1ozmexZinhFw-A4uNC6QtXDI5TyTPt]
- 3. Prodrugs for Improved Drug Delivery: Lessons Learned ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7692606/]
- 4. 7.3 Prodrug design - Medicinal Chemistry [https://fiveable.me/medicinal-chemistry/unit-7/prodrug-design/study-guide/N1RYoPkbPMc2R6E4]
- 5. Formulation Challenges of Prodrugs [https://link.springer.com/chapter/10.1007/978-0-387-49785-3_30]
- 6. Challenges and Strategies in Prodrug Design [https://sciensage.info/index.php/JASR/article/view/2430]
- 7. Prodrug-based drug delivery systems [https://pubmed.ncbi.nlm.nih.gov/41165835/]
- 8. Prodrug - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/chemistry/prodrug]
- 9. Challenges in Drug Formulation: Solving Complex Problems [https://www.scitechnol.com/peer-review/challenges-in-drug-formulation-solving-complex-problems-TpjZ.php?article_id=24047]
- 10. Understanding the pharmacokinetics of prodrug and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6989223/]
- 11. The Prodrug Approach: A Successful Tool for Improving Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6273601/]
- 12. Prodrug Approach as a Strategy to Enhance Drug Permeability [https://pmc.ncbi.nlm.nih.gov/articles/PMC11946379/]
- 13. the role of prodrugs for oral drug delivery [https://www.sciencedirect.com/science/article/abs/pii/S1740674912000200]
- 14. Toxicity mechanism-based prodrugs: Glutathione ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6800212/]
- 15. Tumor-targeted metabolic inhibitor prodrug labelled with ... [https://www.sciencedirect.com/science/article/pii/S2211383523004173]
- 16. Strategies in the designing of prodrugs, taking into account ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523417300764]
- 17. Prodrug activation by 4,4'-bipyridine-mediated aromatic ... [https://www.nature.com/articles/s41467-024-52604-y]
- 18. Prodrug Approaches for Improved DMPK Characteristics ... [https://dmpkservice.wuxiapptec.com/articles/62-prodrug-approaches-for-improved-dmpk-characteristics-and-their-preclinical-study-considerations/]
- 19. What Is a Prodrug? How Prodrugs Work, Examples, and ... [https://www.goodrx.com/drugs/medication-basics/what-is-a-prodrug?srsltid=AfmBOoqaI9gWm9LmGdfzq1zIAmbuj-RB6IwlfbiRiisZQ4Hg9FS91eRs]
- 20. Prodrug [https://pharmacologycanada.org/Prodrug]
- 21. What Is a Prodrug? How Prodrugs Work, Examples, and ... [https://www.goodrx.com/drugs/medication-basics/what-is-a-prodrug?srsltid=AfmBOopxFQvcmanZ5ezkEfLeYxCAtmSMfq9NRzcBVLmgtiHy1_sMmyXK]
- 22. Current Trends in Clinical Trials of Prodrugs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11859331/]
- 23. Newly Developed Prodrugs and Prodrugs in Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC7070911/]
- 24. Prodrugs – Recent approvals and a glimpse of the pipeline [https://www.sciencedirect.com/science/article/abs/pii/S0928098717304463]
- 25. Current Trends in Clinical Trials of Prodrugs [https://www.mdpi.com/1424-8247/18/2/210]
- 26. Fischer Esterification - Carboxylic Acid to Ester Under ... [https://www.masterorganicchemistry.com/2022/11/16/fischer-esterification/]
- 27. Fischer Esterification [https://www.chemistrysteps.com/fischer-esterification/]
- 28. Troubleshooting Guide for Phosphorylation [https://www.neb.com/en-us/tools-and-resources/troubleshooting-guides/troubleshooting-guide-for-phosphorylation?srsltid=AfmBOooYvvKwK2EVvPmswov_RWCs89wvEIpGpN3dnOWJ1Qb7-r4eWtXr]
- 29. Mapping and analysis of phosphorylation sites: a quick guide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3583658/]
- 30. Advances in Oral Drug Delivery Systems: Challenges and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9960885/]
- 31. Prodrugs as empowering tools in drug discovery and ... [https://pubs.rsc.org/en/content/articlelanding/2024/cs/d2cs00957a]
- 32. Prodrug approach: An overview of recent cases [https://www.sciencedirect.com/science/article/abs/pii/S0223523416309321]
- 33. Novel formulation strategies for improving oral ... [https://pubmed.ncbi.nlm.nih.gov/8254497/]
- 34. Review Optimizing Oral Bioavailability in Drug Discovery [https://www.sciencedirect.com/science/article/abs/pii/S0022354916418915]
- 35. How Conformationally Flexible Cyclic Peptides Enter and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9969412/]
- 36. Revisiting strategies to target ABC transporter-mediated drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533758/]
- 37. P-glycoprotein [https://en.wikipedia.org/wiki/P-glycoprotein]
- 38. A review on dynamics of permeability-glycoprotein in efflux ... [https://www.frontiersin.org/journals/drug-discovery/articles/10.3389/fddsv.2024.1363364/full]
- 39. Overcoming ABCB1 mediated multidrug resistance in ... [https://www.nature.com/articles/s41419-024-06949-3]
- 40. Dual inhibitors of the human blood-brain barrier drug efflux ... [https://www.sciencedirect.com/science/article/abs/pii/S0968089617313536]
- 41. Interactions of Potential Anti-COVID-19 Compounds with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7827085/]
- 42. Molecular Modeling-Guided Design of Phospholipid-Based Prodrugs - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6538990/]
- 43. Prospects and Challenges of Phospholipid-Based Prodrugs [https://pmc.ncbi.nlm.nih.gov/articles/PMC6321354/]
- 44. Molecular Modeling-Guided Design of Phospholipid-Based ... [https://www.mdpi.com/1422-0067/20/9/2210]
- 45. Lipidic prodrug approach for improved oral drug delivery and therapy - PubMed [https://pubmed.ncbi.nlm.nih.gov/30320896/]
- 46. Prodrugs: design and clinical applications | Nature Reviews Drug Discovery [https://www.nature.com/articles/nrd2468]
- 47. Drug metabolism in drug discovery and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6146880/]
- 48. Drug Metabolism: Understanding the Fate of Medications in ... [https://www.openaccessjournals.com/articles/drug-metabolism-understanding-the-fate-of-medications-in-the-body-16654.html]
- 49. The expanding role of prodrugs in contemporary drug design and development | Nature Reviews Drug Discovery [https://www.nature.com/articles/nrd.2018.46]
- 50. In Silico Research Is Rewriting the Rules of Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12070237/]
- 51. Machine Learning in Drug Discovery Market 2025 Trends [https://www.towardshealthcare.com/insights/machine-learning-in-drug-discovery-market-sizing]
- 52. The Role of AI in Drug Development in 2025 [https://digitalhealth.folio3.com/blog/role-of-ai-in-drug-development/]
- 53. Beyond Legacy Tools: Defining Modern AI Drug Discovery ... [https://www.biopharmatrend.com/business-intelligence/what-is-ai-drug-discovery/]
- 54. Top 5 Drug Discovery Trends 2025 Driving Breakthroughs [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/drug-discovery-trends-2025/]
- 55. Machine Learning for Multi-Target Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473769/]
- 56. Questions you should ask AI-based drug discovery ... [https://medium.com/data-science/questions-you-should-ask-ai-based-drug-discovery-companies-78c5a011c915]
- 57. In silico formulation optimization and particle engineering ... [https://www.nature.com/articles/s41467-024-54011-9]
- 58. Mastering Lipinski's Rule of Five for Drug Discovery Success [https://www.bioaccessla.com/blog/mastering-lipinskis-rule-of-five-for-drug-discovery-success]
- 59. Oral Druggable Space beyond the Rule of 5: Insights from ... [https://www.sciencedirect.com/science/article/pii/S1074552114002890]
- 60. Drug discovery beyond the 'rule-of-five' [https://pubmed.ncbi.nlm.nih.gov/18035532/]
- 61. Prodrug design to improve pharmacokinetic and drug ... [https://pubmed.ncbi.nlm.nih.gov/20858214/]
- 62. Advancements in techniques for analyzing cell permeability [https://www.sciencedirect.com/science/article/pii/S2405844025022236]
- 63. Drug permeability profiling using cell-free permeation tools [https://www.sciencedirect.com/science/article/pii/S0928098718301751]
- 64. AI-Integrated QSAR Modeling for Enhanced Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525248/]
- 65. The Correlation of Prodrug Stability in Between Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3580045/]
- 66. Article Species-specific in vivo exposure assessment and ... [https://www.sciencedirect.com/science/article/pii/S0090955625090580]
- 67. Computational Simulations to Guide Enzyme-Mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7279318/]
- 68. Assessing the utility of in silico tools in early drug ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224723011577]
- 69. Guide to NCL In Vivo Studies: Efficacy, Pharmacokinetics ... [https://www.ncbi.nlm.nih.gov/books/NBK604930/]
- 70. Subcutaneous prodrug formulations in vitro [https://www.pion-inc.com/blog/testing-prodrugs-in-vitro]
- 71. Emerging Role of Biopharmaceutical Classification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9780568/]
- 72. Biopharmaceutics Classification System [https://en.wikipedia.org/wiki/Biopharmaceutics_Classification_System]
- 73. Integration of a dissolution/permeation system with ... [https://www.sciencedirect.com/science/article/abs/pii/S0939641125002346]
- 74. Prodrugs: Harnessing chemical modifications for improved ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224723009553]
- 75. Recent Development of Nanomaterials for Transdermal Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10136181/]
- 76. Ionic liquid versus prodrug strategy to address formulation challenges [https://pubmed.ncbi.nlm.nih.gov/25534684/]
- 77. New-generation advanced PROTACs as potential therapeutic ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02024-9]
- 78. Prodrug Strategy for PROTACs: High Efficiency and Low ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12177783/]
- 79. Developmental Challenges of PROTACs [https://labtesting.wuxiapptec.com/2025/05/01/6-strategies-to-overcome-protacs-developmental-challenges/]
- 80. for Prodrug : High Efficiency and Low Toxicity Strategy PROTACs [https://pubmed.ncbi.nlm.nih.gov/40547641/]
- 81. Emerging Strategies in Smart Nano- PROTAC for Stimuli-Responsive... [https://www.sciopen.com/article/10.26599/NBE.2025.9290128]