Strategic ADME Optimization in Lead Optimization: Accelerating Candidate Selection with Integrated Approaches
This article provides a comprehensive guide to ADME optimization in modern lead optimization, addressing the critical need to reduce late-stage attrition in drug development.
Strategic ADME Optimization in Lead Optimization: Accelerating Candidate Selection with Integrated Approaches
Abstract
This article provides a comprehensive guide to ADME optimization in modern lead optimization, addressing the critical need to reduce late-stage attrition in drug development. Tailored for researchers and drug development professionals, it explores the foundational principles of Absorption, Distribution, Metabolism, and Excretion (ADME), details cutting-edge in silico, in vitro, and in vivo methodologies, offers troubleshooting strategies for complex modalities like peptides and PROTACs, and validates integrated approaches that improve human translation. By synthesizing the latest advancements in AI-driven prediction, organ-on-a-chip technology, and strategic model integration, this resource aims to equip scientists with the knowledge to design more efficient and predictive ADME profiling workflows.
Understanding ADME Fundamentals: The Cornerstone of Successful Lead Optimization
Why ADME Properties are a Major Cause of Drug Attrition
Drug discovery and development is a lengthy, costly, and risky process, with estimates indicating that advancing a single drug candidate to market requires an average of 10-15 years, investments exceeding USD 1 billion, and failure rates exceeding 90% across all clinical phases [1] [2]. Within this high-attrition landscape, undesirable absorption, distribution, metabolism, and excretion (ADME) properties constitute a fundamental cause of failure for new molecular entities [3]. Historically, approximately 40% of all drug failures were directly attributable to ADME problems, prompting a paradigm shift toward earlier evaluation of these critical properties [4]. While this shift has reduced pharmacokinetic-related failures, ADME issues remain a significant contributor to candidate attrition, particularly when intertwined with toxicity concerns [3] [5].
The pharmaceutical industry has widely adopted the "fail early, fail cheap" strategy, recognizing that early assessment of ADME parameters during lead selection and optimization is crucial for identifying compounds with sufficient pharmacokinetic profiles to become viable efficacious drugs [6] [4]. This application note examines the quantitative impact of ADME properties on drug attrition, provides structured experimental protocols for key ADME assessments, and introduces advanced computational tools that are reshaping predictive strategies in modern drug development pipelines.
Quantitative Analysis of ADME-Related Attrition
Property Ranges and Attrition Risks
Table 1: Physicochemical Property Ranges Associated with Reduced Attrition Risk
| Property | Optimal Range | Attrition Risk When Suboptimal | Primary Impact |
|---|---|---|---|
| Molecular Weight | ≤500 g/mol | Increased permeability issues | Absorption, Distribution |
| logP (lipophilicity) | ≤5 | Poor solubility or excessive metabolism | Absorption, Metabolism |
| Hydrogen Bond Donors | ≤5 | Reduced membrane permeability | Absorption |
| Hydrogen Bond Acceptors | ≤10 | Reduced membrane permeability | Absorption |
| Polar Surface Area | <140 Ų | Compromised blood-brain barrier penetration | Distribution |
| Rotatable Bonds | ≤10 | Reduced oral bioavailability | Absorption |
General property rules for drugs may poorly reflect the subtle ADME differences required by indication-specific drug classes [1] [2]. For example, central nervous system (CNS) drugs generally exhibit more extreme profiles—being smaller, less polar, and more lipophilic—than non-CNS drugs to achieve adequate blood-brain barrier penetration [1].
Therapeutic Area Variability in ADME Profiles
Table 2: ADME Property Variability Across Major Therapeutic Classes (ATC Classification)
| ATC Class | Representative Drugs | Key ADME Characteristics | Attrition Risks |
|---|---|---|---|
| N (Nervous System) | 452 drugs | Lower MW, reduced PSA, increased lipophilicity | Narrow therapeutic windows, CNS toxicity |
| C (Cardiovascular) | 323 drugs | Moderate MW, balanced lipophilicity | Drug-drug interactions, variable clearance |
| J (Anti-infectives) | 298 drugs | Higher MW, complex structures | Tissue penetration challenges, metabolism issues |
| L (Antineoplastic) | 268 drugs | Wider property ranges | Complex toxicity profiles, narrow therapeutic index |
Analysis of marketed drugs across anatomical therapeutic chemical (ATC) classes reveals significant differences in property value distributions, highlighting the need for indication-specific ADME optimization strategies rather than universal property rules [1] [2].
Experimental Protocols for ADME Assessment
Protocol 1: Metabolic Stability Assessment Using Liver Microsomes
Purpose: To evaluate the metabolic stability of drug candidates using liver microsomes and predict in vivo clearance through in vitro-in vivo extrapolation (IVIVE) [6] [7].
Materials and Reagents:
- Test compound (10 mM stock solution in DMSO)
- Pooled species-specific liver microsomes (human/rat/mouse)
- NADPH-regenerating system
- Potassium phosphate buffer (0.1 M, pH 7.4)
- Methanol and acetonitrile (LC-MS grade)
- LC-MS/MS system with appropriate analytical column
Procedure:
- Prepare incubation mixture containing 0.5 mg/mL liver microsomes in potassium phosphate buffer
- Pre-incubate for 5 minutes at 37°C with gentle shaking
- Initiate reaction by adding NADPH-regenerating system
- Aliquot samples at predetermined time points (0, 5, 15, 30, 45, 60 minutes)
- Terminate reactions with ice-cold acetonitrile containing internal standard
- Centrifuge at high speed to remove precipitated proteins
- Analyze supernatant using LC-MS/MS to determine parent compound concentration
- Calculate half-life (t₁/₂) and intrinsic clearance (CLint) using first-order kinetics
Data Interpretation: Compounds with hepatic clearance >70% of liver blood flow are considered high-clearance, while those <30% are classified as low-clearance [6]. High clearance often correlates with poor oral bioavailability and increased attrition risk.
Protocol 2: Caco-2 Permeability and Efflux Assessment
Purpose: To predict human intestinal absorption and identify substrates for efflux transporters like P-glycoprotein [4] [1].
Materials and Reagents:
- Caco-2 cell line (passage 25-45)
- DMEM culture medium with supplements
- Transport buffer (HBSS-HEPES, pH 7.4)
- Test compound (100 μM)
- Lucifer yellow (integrity marker)
- LC-MS/MS system for quantification
Procedure:
- Culture Caco-2 cells on collagen-coated Transwell inserts for 21 days
- Validate monolayer integrity by measuring TEER (>300 Ω·cm²) and lucifer yellow flux
- Add test compound to donor compartment (apical for A→B, basolateral for B→A)
- Sample from receiver compartment at 30, 60, 90, and 120 minutes
- Analyze samples using LC-MS/MS to determine compound concentration
- Calculate apparent permeability (Papp) and efflux ratio (ER)
Data Interpretation: Papp (A→B) >10×10⁻⁶ cm/s indicates high permeability, while ER >2 suggests active efflux potentially limiting absorption [4]. High efflux ratios often predict food effects, drug-drug interactions, and variable exposure in humans.
Protocol 3: Plasma Protein Binding Determination
Purpose: To quantify the fraction of drug bound to plasma proteins, which influences volume of distribution, clearance, and free drug concentration [6] [1].
Materials and Reagents:
- Test compound
- Human or species-specific plasma
- Equilibrium dialysis device
- Dialysis membrane (12-14 kDa MWCO)
- Phosphate buffer (0.1 M, pH 7.4)
- LC-MS/MS system for analysis
Procedure:
- Add test compound to plasma side at therapeutically relevant concentration
- Assemble dialysis device with buffer on opposite side of membrane
- Incubate at 37°C for 4-6 hours with gentle rotation
- Sample from both plasma and buffer compartments
- Precipitate proteins in plasma samples with acetonitrile
- Analyze both sets of samples using LC-MS/MS
- Calculate fraction unbound (fu) and fraction bound (fb)
Data Interpretation: Compounds with >95% protein binding are considered highly bound, which can lead to variable free drug concentrations, altered pharmacokinetics, and potential drug-drug interactions through protein binding displacement [6].
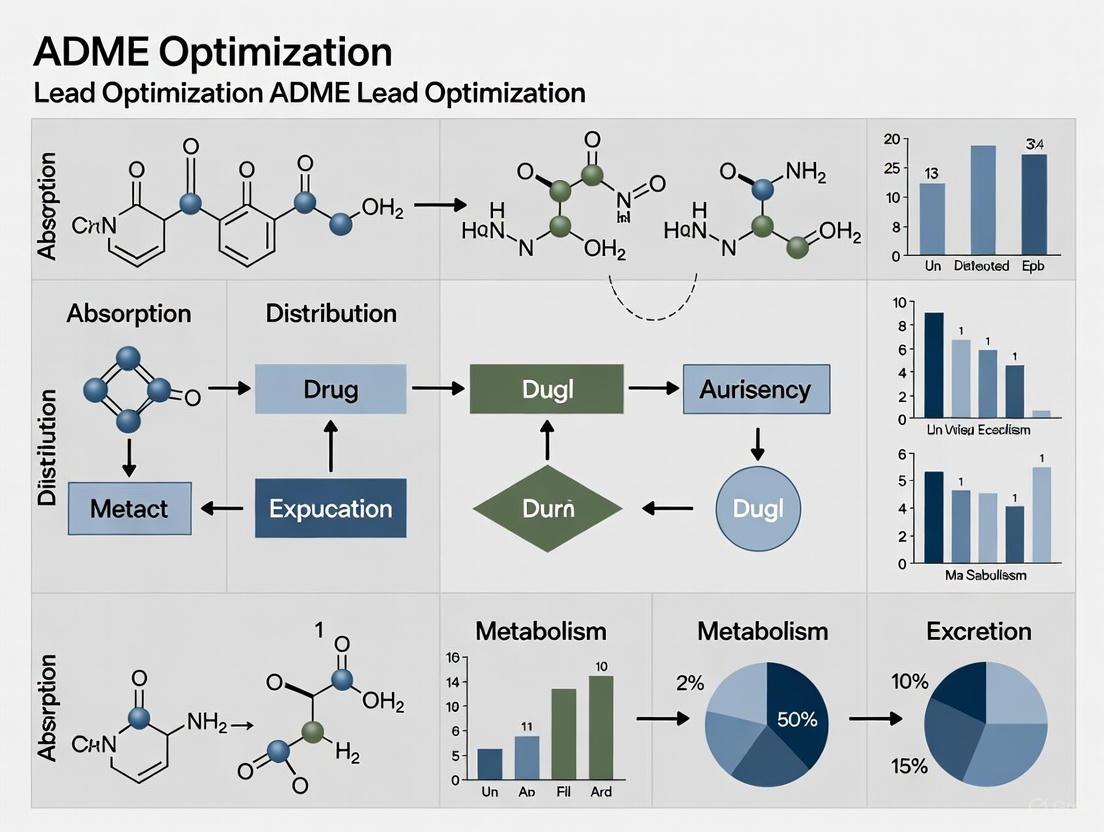
Visualization of ADME Assessment Workflows
Integrated ADME Screening Cascade
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for ADME Profiling
| Tool/Reagent | Function | Application in ADME Assessment |
|---|---|---|
| Pooled Liver Microsomes | Metabolic enzyme source | Intrinsic clearance determination, metabolite identification |
| Caco-2 Cell Line | Intestinal epithelium model | Permeability screening, efflux transporter assessment |
| Transfected Cell Lines | Specific transporter expression | Uptake/efflux transporter interaction studies |
| Human Hepatocytes | Integrated hepatic model | Phase I/II metabolism, enzyme induction potential |
| Equilibrium Dialysis Device | Binding measurement apparatus | Plasma protein binding determination |
| Accelerator Mass Spectrometry (AMS) | Ultra-sensitive detection | Human radiolabeled ADME studies, microdosing |
| PBPK Modeling Software | Physiological simulation | Human pharmacokinetic prediction, DDI risk assessment |
| SwissADME Web Tool | Free in silico screening | Rapid physicochemical and PK property estimation [8] |
Advanced tools like machine learning platforms and PBPK modeling software are increasingly integrated into ADME assessment workflows. These tools leverage large datasets of historical ADME properties to build predictive models that can guide chemical design and prioritize compounds for experimental testing [5] [9]. The SwissADME web tool provides free access to robust predictive models for physicochemical properties, pharmacokinetics, and drug-likeness, enabling researchers to rapidly evaluate key parameters for compound collections [8].
ADME properties remain a major cause of drug attrition due to their fundamental influence on drug exposure, target engagement, and ultimately therapeutic efficacy. The strategic integration of robust ADME assessment protocols—spanning in silico predictions, high-throughput in vitro assays, and targeted in vivo studies—into early discovery phases enables identification and mitigation of pharmacokinetic liabilities before costly late-stage development. The continuing evolution of computational approaches, particularly machine learning and AI-driven ADMET prediction platforms, promises to further transform this landscape by enhancing predictive accuracy and enabling more informed compound selection [5] [9]. By adopting these comprehensive assessment strategies and leveraging the specialized research tools outlined in this application note, drug development teams can significantly reduce attrition rates and advance candidates with optimized ADME profiles toward clinical success.
The optimization of Absorption, Distribution, Metabolism, and Excretion (ADME) properties represents a critical hurdle in modern drug discovery. The high-throughput screening of these properties has become the norm in the industry, largely to address historical trends where ADME issues contributed to more drug failures than efficacy or safety concerns in clinical trials [10]. At the heart of ADME optimization lie three fundamental physicochemical properties: lipophilicity (commonly measured as Log D), solubility, and permeability. These properties are deeply interconnected and form the basis for understanding a compound's pharmacological and pharmacokinetic fate after administration [11].
These core properties govern the drug's ability to be absorbed from the gastrointestinal tract, distribute to target tissues, and be metabolized and eliminated appropriately. With the realization of new techniques and refinement of existing ones, better projections for the pharmacokinetic properties of compounds in humans are now possible, shifting drug failure attributes more toward safety and efficacy properties [10]. The strategic assessment of these properties during lead optimization enables discovery teams to track project progress efficiently and provides a rationale for the types of studies needed at various stages of discovery [10]. This application note provides detailed protocols and benchmarks to guide researchers in the systematic evaluation of these essential properties.
Property Definitions and Strategic Significance
Lipophilicity (Log D) is the distribution coefficient of a compound between octanol and buffer at a specific pH, typically pH 7.4, accounting for both ionized and non-ionized forms [12] [13]. This parameter plays a crucial role in solubility, absorption, membrane penetration, plasma protein binding, distribution, and CYP450 interactions [13]. Aqueous solubility refers to the concentration of a dissolved compound in equilibrium with its solid form, which directly impacts bioavailability and absorption from the gastrointestinal tract [12] [13]. Permeability describes a compound's ability to cross biological membranes, a critical determinant for oral absorption and tissue distribution, often predicted through models like Caco-2, PAMPA, or computational descriptors [14] [15].
The interrelationship between these properties forms what is often described as the "Balance of Properties" in drug design. Lipophilicity directly influences both solubility and permeability—higher lipophilicity generally decreases aqueous solubility while increasing membrane permeability [12]. This inverse relationship creates a fundamental challenge in optimization, as improving one property often comes at the expense of another. Understanding these trade-offs is essential for effective lead optimization, requiring researchers to navigate a multi-parameter optimization space rather than focusing on individual properties in isolation.
Table 1: Optimal Ranges and Critical Benchmarks for Core Physicochemical Properties
| Property | Optimal Range | Strategic Significance | Key Risk Factors |
|---|---|---|---|
| Log D at pH 7.4 | 0-3 [12] | Best balance of solubility and permeability [12] | >5: Poor solubility, promiscuous binding, strong CYP450 interaction [12]; <0: Good solubility but poor permeability [12] |
| Aqueous Solubility | >50 μM (approximate guideline) | Ensures adequate dissolution for absorption [13] | Limits absorption from GI tract; affects reliability of other ADME assays [13] |
| Permeability (Caco-2 Papp) | >5 × 10⁻⁶ cm/s (high) | Indicator of good intestinal absorption [14] | Low permeability limits oral bioavailability; may require active transport [14] |
| Molecular Weight | ≤950 Da (for PROTACs) [15] | Impacts passive diffusion and solubility | Higher MW generally decreases absorption and permeability [15] |
| H-Bond Donors (HBD) | ≤3 (for PROTACs) [15] | Critical for membrane penetration | Increased HBD count typically reduces permeability [15] |
Visualizing the Interconnected Nature of ADME Properties
The following diagram illustrates how the three core physicochemical properties interrelate and collectively influence critical ADME outcomes:
Detailed Experimental Protocols and Methodologies
Lipophilicity (Log D) Measurement via Shake-Flask Method
The shake-flask method remains the gold standard for lipophilicity assessment, providing a direct measurement of distribution between octanol and aqueous phases [13].
Protocol Summary:
- Test Articles: Assayed in triplicate at a single concentration (typically 10 μM) [13]
- Partition Solvent: n-Octanol with buffer (typically phosphate buffer, pH 7.4) in a 1:1 ratio [13]
- Controls: Testosterone (high log D₇.₄ positive control), Tolbutamide (low log D₇.₄ negative control) [13]
- Procedure: Compound is dissolved in a solution with equal amounts of octanol and buffer, shaken for 3 hours, and then measured for the amount of compound in each phase [13]
- Analysis: LC/MS/MS measurement of parent compound in both phases [13]
- Calculation: Log D = log([compound]ₒcₜₐₙₒₗ / [compound]բᵤfғₑᵣ) [13]
- Compound Requirement: 1.0-2.0 mg [13]
Methodological Considerations: Recent advancements have improved the accuracy of Log D determination. A validation study demonstrated excellent correlation between automated and manual methods with the equation: Log DADW = 0.002(±0.008) + 1.011(±0.005)×Log Dmanual (N=179; r²=0.9960; standard error of estimate=0.1022) [12]. For ionizable compounds like propranolol, the use of universal buffer composed of acetic, phosphoric, and boric acids with NaOH helps maintain consistent pH conditions [12].
Thermodynamic Solubility Determination
Solubility assessment must distinguish between kinetic (apparent) and thermodynamic (equilibrium) solubility, with the latter being more predictive for in vivo performance.
Protocol Summary:
- Test Articles: Assayed in duplicate at a single concentration (typically 1 μM) [13]
- Buffer Systems: Phosphate buffered solution across a three-point pH range (5.0, 6.2, 7.4) to simulate gastrointestinal variation [13]
- Controls: Diclofenac (high solubility positive control), Dipyridamole (low solubility negative control) [13]
- Procedure: Compound is dissolved in buffer solutions at indicated pH values and allowed to reach thermodynamic equilibrium by incubating for 18 hours [13]
- Analysis: UV spectrophotometry measurement compared to fully saturated solution in 1-propanol [13]
- Compound Requirement: 1.0-2.0 mg [13]
Critical Considerations: The definition of solubility as "concentration of a dissolved compound in equilibrium with its solid" requires careful attention to multiple factors: the specific solid form (most stable vs. other forms), the solvent system (buffers vs. co-solvents), and equilibrium conditions (time and temperature) [12]. Solid particles are an integral part of the solubility assay and must be present for turbidity-based methods, though they represent artifacts in absorbance/elemental assays [12]. Identification of saturated solutions can be challenging, as visual inspection alone may be insufficient to distinguish between true saturation and suspension [12].
Permeability Assessment Using Caco-2 Transwell Assay
The Caco-2 cell model remains a cornerstone for in vitro permeability assessment, though method adaptations may be necessary for challenging compound classes.
Protocol Summary:
- Cell Culture: Caco-2 cells (TC7 clone) seeded at 125,000 cells per well in 24-well transwell plates and cultured for 14-21 days to form differentiated monolayers [15]
- Experimental Setup: Apparent permeability (Pₐₚₚ) determined from apical-to-basolateral (Pₐₚₚ,ₐբ) and basolateral-to-apical (Pₐₚₚ,բₐ) directions [15]
- Volumes: Apical compartment: 250 μL, basolateral compartment: 750 μL [15]
- Incubation: 2 hours at 37°C in 5% CO₂ and 100% humidity [15]
- Analysis: Samples from both compartments at t=0 and after 2 hours analyzed via UHPLC-MS/MS [15]
- Quality Control: Monolayer tightness controlled using melagatran as tightness marker [15]
Calculation Parameters:
- Apparent Permeability: Pₐₚₚ = (Δcᵣₑc/Δt × Vᵣₑc) / (c𝒹ₒₙ,₀ × A) where Δcᵣₑc/Δt is concentration change in receiver compartment over time, Vᵣₑc is receiver volume, c𝒹ₒₙ,₀ is initial donor concentration, and A is membrane surface area (0.33 cm²) [15]
- Mass Balance: Recovery = (amountᵣₑc,₂ₕ + amount𝒹ₒₙ,₂ₕ) / amount𝒹ₒₙ,₀ [15]
- Efflux Ratio: ER = Pₐₚₚ,բₐ / Pₐₚₚ,ₐբ [15]
- Passive Permeability: Geometric mean of Pₐₚₚ,ₐբ and Pₐₚₚ,բₐ used as Pₐₚₚ,ₚₐₛₛ [15]
Method Adaptation for Challenging Compounds: For problematic chemical classes such as PROTACs, several assay modifications have been explored:
- Serum Addition: HBSS buffer containing 10% FCS on both sides to reduce unspecific binding [15]
- pH Adjustment: Apical compartments adjusted to pH 6.5 instead of pH 7.4 to simulate intestinal conditions [15]
- Biorelevant Media: FaSSIF (Fasted State Simulated Intestinal Fluid) as apical buffer instead of HBSS [15]
- Mucin Layer: Addition of 50 mg/mL mucin on top of Caco-2 cells to simulate mucus barrier [15]
Advanced Applications and Specialized Approaches
Beyond Rule of 5 (bRo5) Space Considerations
Emerging modalities like Proteolysis-Targeting Chimeras (PROTACs) present unique challenges as they reside in the beyond Rule of 5 (bRo5) space with high molecular weight and lipophilicity [15]. For these compounds, standard small molecule methodologies may require adaptation, and surrogate permeability descriptors become increasingly valuable [15].
Table 2: Recommended Property Space for Oral PROTACs and Optimization Strategies
| Parameter | Recommended Boundary | Rationale | Experimental Considerations |
|---|---|---|---|
| Molecular Weight | ≤950 Da [15] | Impacts passive diffusion and solubility | Higher MW generally decreases absorption; synthesis feasibility |
| H-Bond Donors (HBD) | ≤3 [15] | Critical for membrane penetration | Reduced HBD count typically enhances permeability; shielding exposed HBDs is powerful optimization approach [15] |
| Rotatable Bonds | ≤12 [15] | Affects molecular flexibility | Lower count associated with improved permeability |
| Chromlog D | ≤7 [15] | Balance of solubility and permeability | High lipophilicity increases promiscuous binding and metabolic instability |
| Exposed Polar Surface Area (ePSA) | ≤170 Ų [15] | Surrogate for permeability assessment | Reduction through HBD shielding improves membrane penetration [15] |
Research indicates that for bRo5 compounds, the reduction of exposed polar surface area, particularly through shielding of hydrogen bond donors, represents a powerful approach to optimize permeability [15]. Additionally, standard small molecule-based methods for in vitro-in vivo extrapolation (IVIVE) of intrinsic clearance may systematically underpredict for PROTACs when using predicted fraction unbound in incubation (fᵤ,ᵢₙc), highlighting the need for experimentally determined values [15].
In Vitro-In Vivo Extrapolation and Prediction Tools
The transition from in vitro data to predicted in vivo consequences represents a critical paradigm shift in ADME optimization [16]. Rather than discussing raw assay data, forward-looking approaches focus on potential clinical problems that may surface during development, using suitable variables derived from assay data [16].
Computational Prediction Platforms: Several software platforms provide robust in silico prediction of ADME properties:
- ADMET Predictor PCB Module: Includes models for physicochemical property prediction using artificial neural network ensemble (ANNE) technology, including S+logP (ranked #1 in peer-reviewed comparisons), S+logD, multiprotic pKa, and various solubility predictions [17]
- ACD/ADME Suite: Provides structure-based calculations of pharmacokinetic properties including blood-brain barrier penetration, cytochrome P450 inhibition and substrate specificity, distribution, oral bioavailability, and passive absorption [14]
- BioSolveIT/Optibrium Platforms: Feature calculation of relevant ADME parameters including CYP2C9 pKi, CYP2D6 affinity, blood-brain barrier classification, HIA category, P-gp category, logD, logP, and logS [18]
These tools enable researchers to prioritize synthesis and experimental testing, conserving resources by filtering out compounds with unfavorable predicted parameters early in the design process [18].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Experimental Systems for ADME Profiling
| Tool/Reagent | Function and Application | Key Considerations |
|---|---|---|
| n-Octanol/Buffer Systems | Gold standard for Log D determination via shake-flask method [13] | Use universal buffer for ionizable compounds; maintain strict pH control [12] |
| Caco-2 Cell Line (TC7 clone) | In vitro model of intestinal permeability [15] | Requires 14-21 day differentiation; monitor tightness with reference compounds like melagatran [15] |
| Pooled Human Liver Microsomes | Metabolic stability assessment [13] | Batch-to-batch variability; use same lot for comparable results with bridging studies [13] |
| Simulated Intestinal Fluids (FaSSIF/FeSSIF) | Biorelevant solubility measurement [17] | Better predicts in vivo performance compared to simple aqueous buffers [17] |
| Cryopreserved Hepatocytes | Intrinsic clearance determination [15] | Maintain viability >70%; use species relevant to in vivo models [15] |
| Transwell Assay Systems | Permeability assessment with liquid handling automation [15] | Enable high-throughput screening; include mass balance calculations [15] |
Workflow Integration and Strategic Implementation
The following diagram outlines a recommended integrated workflow for the strategic implementation of these assays in lead optimization:
This workflow emphasizes the sequential yet interconnected nature of ADME screening, where compounds progress through a tiered testing cascade. Implementation of such systematic approaches follows the Discovery Assay by Stage (DABS) paradigm, which provides teams with rationale for study types during hit-to-lead, early and late lead optimization stages of discovery [10]. This framework has proven optimal for efficient resource utilization and helps discovery teams track compound and project progress systematically [10].
The systematic assessment of lipophilicity, solubility, and permeability represents a cornerstone of modern ADME optimization in drug discovery. Through the implementation of robust, well-characterized protocols for these fundamental properties—coupled with appropriate data interpretation and strategic decision-making—research teams can significantly de-risk the lead optimization process. The integration of experimental data with predictive computational models creates a powerful framework for compound design and selection, ultimately increasing the probability of identifying development candidates with favorable pharmacokinetic profiles. As the field continues to evolve with new modalities and technologies, these core principles remain essential for efficient navigation of the complex multi-parameter optimization space that defines successful drug discovery.
Within the context of a broader thesis on ADME optimization in lead optimization research, this document details the critical in vitro and in silico methodologies for profiling three fundamental parameters: metabolic stability, plasma protein binding, and clearance. The early and accurate assessment of these properties is crucial for streamlining drug development, as deficiencies in these areas are primary causes of failure in later-stage clinical trials [19] [20]. This guide provides detailed application notes and protocols to enable researchers to effectively integrate these assessments into the lead optimization cycle, supporting the design of candidates with a higher probability of success.
Core ADME Parameters: Significance and Experimental Assessment
The following section outlines the key parameters, their impact on the drug discovery process, and the standard experimental protocols used for their determination.
Metabolic Stability
Significance: Metabolic stability refers to the susceptibility of a compound to enzymatic modification, primarily by hepatic enzymes. It directly impacts a drug's half-life and oral bioavailability. A compound with low metabolic stability is rapidly cleared, which may necessitate frequent dosing to maintain therapeutic exposure [21] [22]. During lead optimization, the goal is to identify metabolically soft spots to guide structural modifications that improve stability without compromising potency.
Experimental Protocol: Intrinsic Clearance (CL~int~) Assay using Human Liver Microsomes (HLM) or Hepatocytes
- Principle: This assay measures the depletion of the test compound over time when incubated with metabolically active systems (HLM or suspended hepatocytes) to estimate its intrinsic metabolic clearance [21].
- Materials:
- Test compound (typically 1 µM final concentration)
- Pooled Human Liver Microsomes (0.5 mg/mL protein) or Cryopreserved Human Hepatocytes (0.5-1.0 million cells/mL)
- NADPH-regenerating system (for HLM) or appropriate nutrient medium (for hepatocytes)
- Potassium phosphate buffer (100 mM, pH 7.4)
- Stop solution (e.g., acetonitrile with internal standard)
- Water bath or incubator shaker (37°C)
- LC-MS/MS system for bioanalysis
- Procedure:
- Pre-incubation: Prepare the incubation mixture containing the liver microsomes/hepatocytes and test compound in buffer. Pre-incubate for 5 minutes at 37°C with gentle shaking.
- Initiation: Start the reaction by adding the NADPH-regenerating system (for HLM) or by dispensing the hepatocyte mixture.
- Time-point Sampling: Aliquot the reaction mixture (e.g., 50 µL) at multiple time points (e.g., 0, 5, 15, 30, 45, 60 minutes) into a plate containing the stop solution to precipitate proteins and terminate the reaction.
- Sample Analysis: Centrifuge the plates to remove precipitated protein. Analyze the supernatant using LC-MS/MS to determine the peak area ratio (compound/internal standard) at each time point.
- Data Analysis: Plot the natural logarithm of the remaining compound percentage against time. The slope of the linear regression is the disappearance rate constant (k). CL~int~ is calculated as follows:
- For microsomes: ( CL{int} (\mu L/min/mg) = k (min^{-1}) / \text{Microsomal Protein Concentration} (mg/mL) \times 1000 )
- For hepatocytes: ( CL{int} (\mu L/min/10^6 \text{ cells}) = k (min^{-1}) / \text{Cell Concentration} (10^6 \text{ cells}/mL) \times 1000 )
Table 1: Key Assays for Metabolic Stability and Protein Binding
| Parameter | Assay System | Key Output(s) | Data Application |
|---|---|---|---|
| Metabolic Stability [21] | Human Liver Microsomes (HLM) | Intrinsic Clearance (CL~int~) | Scaling to predict human hepatic clearance. |
| Cryopreserved Human Hepatocytes | Intrinsic Clearance (CL~int~) | Provides a more physiologically complete system (including non-CYP enzymes). | |
| Plasma Protein Binding [22] | Equilibrium Dialysis (ED) | Fraction Unbound (f~u~) | Considered the "gold standard" method. |
| Ultrafiltration (UF) | Fraction Unbound (f~u~) | Faster but prone to compound binding to membrane. | |
| Ultracentrifugation (UC) | Fraction Unbound (f~u~) | Suitable for high molecular weight or unstable compounds. |
Plasma Protein Binding
Significance: Plasma protein binding (PPB) measures the extent to which a drug binds to proteins in the blood, primarily albumin and alpha-1-acid glycoprotein. The unbound fraction (f~u~) is the pharmacologically active moiety, as only unbound drug can diffuse to its site of action or be metabolized [22]. A high degree of binding (>99%) can limit a drug's efficacy, influence its volume of distribution, and potentially lead to drug-drug interactions through protein binding displacement.
Experimental Protocol: Determination of Fraction Unbound (f~u~) by Equilibrium Dialysis
- Principle: Equilibrium dialysis separates a plasma compartment from a buffer compartment using a semi-permeable membrane. At equilibrium, the unbound drug concentration is equal in both chambers, allowing for the calculation of f~u~ [22].
- Materials:
- Test compound
- Human plasma (fresh or frozen)
- Buffer (e.g., 100 mM phosphate buffer, pH 7.4)
- Equilibrium dialysis device (e.g., 96-well format) with a molecular weight cutoff membrane (e.g., 12-14 kDa)
- Thermostated incubator (37°C)
- LC-MS/MS system for bioanalysis
- Procedure:
- Preparation: Spike the test compound into human plasma to achieve a therapeutic relevant concentration (e.g., 1-5 µM). Add buffer to the opposing chamber.
- Dialysis: Assemble the dialysis device and place it in an incubator at 37°C with gentle agitation for a predetermined time (typically 4-6 hours) to reach equilibrium.
- Post-dialysis Sampling: After dialysis, collect aliquots from both the plasma and buffer chambers.
- Sample Analysis: The buffer sample represents the unbound drug concentration (C~u~). The plasma sample represents the total drug concentration (C~total~). Analyze both sets of samples using LC-MS/MS. Note: For the plasma sample, a "blank" buffer should be used for dilution to match the matrix of the buffer chamber sample.
- Data Analysis: Calculate the fraction unbound: ( fu = Cu / C_{total} ). The result is often expressed as a percentage: % Unbound = f~u~ × 100.
Clearance
Significance: Clearance (CL) is the volume of plasma from which a drug is completely removed per unit of time. It is a critical parameter that determines the dosing regimen and steady-state concentrations of a drug. The goal during lead optimization is to identify compounds with a clearance profile that supports the desired dosing frequency, typically low clearance for once-daily oral dosing [21].
Experimental Protocol: In Vitro-In Vivo Extrapolation (IVIVE) of Human Hepatic Clearance
- Principle: This is a predictive approach that uses in vitro intrinsic clearance data from HLM or hepatocytes, scaled up to the whole organ level using physiological scaling factors, to predict in vivo human hepatic clearance (CL~H~) [21].
- Materials:
- Experimentally determined CL~int~ from HLM or hepatocytes (from Section 2.1 protocol)
- Scaling factors: Microsomal yield (e.g., 40 mg microsomal protein per gram liver) or Hepatocyte yield (e.g., 120 million cells per gram liver)
- Human liver weight (e.g., 20 g liver per kg body weight)
- Human hepatic blood flow (Q~H~), e.g., 20 mL/min/kg
- Procedure & Data Analysis:
- Scale-up: Convert the in vitro CL~int~ to a value representative of the whole human liver.
- For microsomes: ( CL{int, liver} (mL/min/kg) = CL{int} (\mu L/min/mg) \times \text{Liver Weight} (g \text{ liver}/kg \text{ body weight}) \times \text{Microsomal Yield} (mg \text{ protein}/g \text{ liver}) / 1000 )
- For hepatocytes: ( CL{int, liver} (mL/min/kg) = CL{int} (\mu L/min/10^6 \text{ cells}) \times \text{Liver Weight} (g \text{ liver}/kg \text{ body weight}) \times \text{Hepatocyte Yield} (10^6 \text{ cells}/g \text{ liver}) / 1000 )
- Model Application: Apply the scaled CL~int, liver~ to a physiological model of hepatic clearance, such as the "well-stirred" model, which also incorporates plasma protein binding data (f~u~) and blood-to-plasma ratio (B/P): ( CLH = \frac{ QH \times fu \times CL{int, liver} }{ QH + (fu \times CL_{int, liver}) } ) This predicted CL~H~ can be compared to known clinical values for desirable drugs to assess the viability of the lead compound.
- Scale-up: Convert the in vitro CL~int~ to a value representative of the whole human liver.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for ADME Assays
| Reagent / Material | Function in ADME Testing |
|---|---|
| Human Liver Microsomes (HLM) [21] | A subcellular fraction containing cytochrome P450 (CYP) and other drug-metabolizing enzymes; used for high-throughput metabolic stability and metabolite profiling. |
| Cryopreserved Human Hepatocytes [21] [7] | Intact liver cells that provide a more physiologically relevant system, containing the full complement of hepatic metabolizing enzymes and transporters. |
| NADPH-Regenerating System | Provides a continuous supply of NADPH, a crucial cofactor for CYP-mediated oxidation reactions in metabolic stability assays. |
| Equilibrium Dialysis Devices [22] | The preferred platform for determining plasma protein binding, allowing for gentle separation of protein-bound and unbound drug fractions at physiological temperature. |
| LC-MS/MS System | The core analytical technology for the sensitive and specific quantification of drugs and their metabolites in complex biological matrices like plasma, buffer, and incubation mixtures. |
Integrated Workflows and Predictive Modeling in Modern ADME Science
The traditional assay-based approach is increasingly being complemented and enhanced by computational models, creating a more efficient and insightful workflow.
The Evolving Role of In Silico ADME Modeling
In silico models for ADME prediction allow for the virtual screening of compound libraries before synthesis, enabling a "fail early, fail cheap" strategy [20]. Early models based on quantitative structure-activity relationships (QSARs) have evolved with the advent of artificial intelligence and machine learning (AI/ML). Modern graph neural networks (GNNs) that use multitask learning can simultaneously predict multiple ADME parameters, sharing information across tasks to improve performance even with limited data for any single endpoint [19]. Furthermore, these models can be made explainable, highlighting which structural features in a molecule contribute positively or negatively to a predicted ADME property, thus providing direct feedback to medicinal chemists for structural optimization [19].
Integration with Physiologically-Based Pharmacokinetic (PBPK) Modeling
Data from the in vitro assays described above serve as critical inputs for PBPK modeling. PBPK models are mathematical frameworks that simulate the absorption, distribution, metabolism, and excretion of a compound in the whole organism based on its physicochemical properties and in vitro data [7] [20]. These models are used to:
- Predict human pharmacokinetics prior to first-in-human studies.
- Assess the risk of drug-drug interactions (DDIs) by simulating the impact of enzyme inhibitors or inducers.
- Support regulatory submissions, as highlighted by the ICH M12 guideline on drug interaction studies [7].
The following diagram illustrates the integrated cycle of in vitro data generation, in silico modeling, and lead optimization.
Integrated ADME Optimization Workflow
The rigorous assessment of metabolic stability, plasma protein binding, and clearance is non-negotiable in modern lead optimization. By implementing the standardized experimental protocols detailed in this document and leveraging the growing power of in silico and PBPK modeling approaches, research teams can make data-driven decisions. This integrated strategy enables the systematic design of drug candidates with a higher likelihood of possessing desirable pharmacokinetic profiles, thereby reducing late-stage attrition and accelerating the development of new medicines.
The landscape of drug discovery has expanded beyond traditional small molecules to include advanced modalities such as peptides, proteolysis-targeting chimeras (PROTACs), and other large molecules. These modalities offer unique therapeutic advantages, including the ability to target previously "undruggable" pathways, yet they present distinct absorption, distribution, metabolism, and excretion (ADME) challenges during lead optimization [23] [24]. Peptides bridge the gap between small molecules and biologics, offering high specificity and affinity but typically suffering from poor permeability and metabolic instability [25] [26]. PROTACs, as heterobifunctional degraders, operate catalytically to eliminate target proteins but reside in the beyond-rule-of-5 (bRo5) chemical space, creating unique optimization hurdles [23] [15]. Successfully advancing these candidates requires tailored ADME strategies that address their specific physicochemical properties and in vivo behaviors. This application note details specialized protocols and considerations for optimizing the ADME properties of peptides and PROTACs within lead optimization research programs.
Peptide Therapeutics: ADME Profiling and Optimization
Core ADME Challenges and Optimization Strategies
Natural peptides typically exhibit poor ADME properties, including rapid clearance, short half-life, low permeability, and sometimes low solubility [25]. Most have less than 1% oral bioavailability due to enzymatic degradation in the gastrointestinal tract and low permeability across cell membranes [25] [26]. Unmodified peptides also tend to have short half-lives (often minutes) resulting from extensive proteolysis and rapid renal clearance, typically limiting them to extracellular targets [25].
Table 1: Peptide ADME Challenges and Corresponding Optimization Strategies
| ADME Challenge | Impact on Pharmacokinetics | Optimization Strategies |
|---|---|---|
| Metabolic Instability | Short in vivo half-life, requiring frequent dosing or infusion [25] | Cyclization, D-amino acid substitution, PEGylation, lipidation [26] |
| Low Permeability | Poor oral bioavailability, limiting administration routes [25] | Strategic truncation, peptidomimetics, use of permeation enhancers [27] [26] |
| Rapid Renal Clearance | Short circulation time, especially for peptides <25 kDa [26] | PEGylation to increase hydrodynamic radius, albumin binding through lipidation [26] |
| Enzymatic Degradation | Low oral bioavailability, significant first-pass metabolism [26] | N- and C-terminal capping, incorporation of unnatural amino acids [27] |
Structural modification strategies have proven effective in addressing these inherent peptide challenges. Case studies demonstrate that cyclization eliminates free N- and C-termini, protecting against exopeptidase attack as seen with Cyclosporin A [26]. Similarly, D-amino acid substitution disrupts protease recognition, enhancing metabolic stability in drugs like Leuprolide [26]. Pharmacokinetic profiles can be further refined through PEGylation, which increases hydrodynamic radius to reduce renal clearance, and lipidation (e.g., fatty acid modification) that enhances albumin binding for extended half-lives, successfully employed in Liraglutide and Semaglutide [26].
Experimental Protocols for Peptide ADME Profiling
A systematic, tiered framework for in vitro ADME profiling is crucial for guiding rational peptide design. The following protocol outlines a comprehensive approach used to elucidate structure-ADME relationships [26].
Protocol 1: Tiered In Vitro ADME Profiling for Peptides
Objective: To comprehensively evaluate the key ADME properties of peptide candidates and identify major liabilities during lead optimization.
Materials:
- Test Compounds: Peptide candidates (0.5-2.0 mg required per assay) [13]
- Simulated Biological Fluids: Simulated Gastric Fluid (FaSSGF) and Simulated Intestinal Fluid (FaSSIF) with and without digestive enzymes [26]
- Metabolic Matrices: Plasma (across multiple species), liver S9 fractions, intestinal S9 fractions, kidney microsomes, and lysosomes [26]
- Permeability System: Caco-2 cell monolayers, low-binding tips and plates, transport buffer with/without permeation enhancers (e.g., Sodium Caprate) [25] [26]
- Analytical Instrumentation: UHPLC-MS/MS system for quantification [26]
Procedure:
Solubility and Biorelevant Stability Assessment:
- Determine thermodynamic solubility in phosphate buffer at pH 7.4 (and other relevant pH values) [13].
- Incubate peptides (typically at 1-10 µM) in FaSSGF and FaSSIF, both with and without digestive enzymes [26].
- Sample at predetermined time points and analyze by UHPLC-MS/MS to quantify remaining parent peptide.
- Data Analysis: Calculate % of parent peptide remaining over time to determine degradation half-life in each medium.
Metabolic Stability Analysis:
- Incubate peptides with various biological matrices: plasma, liver S9 fractions, intestinal S9 fractions, kidney microsomes, and lysosomes [26].
- Use a liquid handling platform for consistency. For plasma stability, incubate at 37°C and take aliquots at T0, 30, 60, 120, and 180 minutes.
- Quench reactions with acetonitrile containing internal standard, centrifuge, and analyze supernatant via UHPLC-MS/MS.
- Data Analysis: Determine degradation half-life in each matrix. Note significant interspecies variability in plasma stability is common [26].
Permeability Assessment:
- Culture Caco-2 cells (TC7 clone) on transwell filters for 14-21 days to form confluent monolayers [15].
- Prior to experiment, wash monolayers with transport buffer (e.g., HBSS).
- Add peptide to donor compartment (apical for A→B, basolateral for B→A). To minimize nonspecific binding, use low-binding tips and plates, and consider adding BSA (0.5-1%) to the receiver wells [25].
- For studies with permeation enhancers, add compounds like Sodium Caprate (C10) to the apical compartment [26].
- Sample from both donor and receiver compartments at T0 and after 2 hours of incubation at 37°C [15].
- Analyze samples via UHPLC-MS/MS.
- Data Analysis: Calculate apparent permeability (Papp) and efflux ratio. Most peptides show low permeability, though effects of enhancers are compound-dependent [26].
The following workflow visualizes this multi-tiered profiling approach:
Research Reagent Solutions for Peptide ADME
Table 2: Key Reagents for Peptide ADME Assays
| Research Reagent | Function in ADME Profiling | Application Notes |
|---|---|---|
| Simulated Gastric/Intestinal Fluids (FaSSGF/FaSSIF) | Assess solubility and enzymatic stability in biorelevant conditions [26] | Use both with and without digestive enzymes to differentiate chemical and enzymatic degradation. |
| Multi-Species Plasma | Evaluate metabolic stability and interspecies differences [26] | Human, mouse, rat, and dog plasma are typical. Significant variability is often observed. |
| Tissue S9 Fractions & Microsomes | Characterize extra-hepatic metabolism (e.g., liver, intestine, kidney) [26] | Kidney microsomes can be critical for peptides like GLP-1 analogs that show faster degradation there. |
| Caco-2 Cell Line | Model passive transcellular and paracellular permeability [25] | Expresses human intestinal transporters (e.g., PEPT1); requires 14-21 day culture for differentiation. |
| Low-Binding Tips & Plates | Minimize nonspecific binding during assays [25] | Essential for obtaining accurate recovery and reliable quantitative results. |
| Permeation Enhancers (e.g., C10) | Investigate strategies to improve membrane permeability [26] | Effects are compound-dependent and require careful optimization. |
PROTACs: ADME Profiling and Optimization
Core ADME Challenges and Optimization Strategies
PROTACs are heterobifunctional molecules comprising a target protein-binding ligand, an E3 ubiquitin ligase-binding ligand, and a connecting linker [23]. Their large size (often MW >800 Da), high lipophilicity, and excessive hydrogen bonding capacity place them firmly in the bRo5 space, creating predictable ADME challenges [15]. Key issues include low solubility, poor permeability, and a high propensity for nonspecific binding that can confound in vitro assays [15]. Unlike traditional small molecules, PROTACs act catalytically, meaning they are released after degrading their target protein to engage in multiple cycles, which allows them to be effective at lower doses despite suboptimal PK parameters [23].
Table 3: PROTAC ADME Challenges and Corresponding Optimization Strategies
| ADME Challenge | Impact on Pharmacokinetics | Optimization Strategies |
|---|---|---|
| Low Permeability | Limits oral absorption and cellular uptake [15] | Reduce H-bond donors (≤3), control MW (≤950 Da), reduce rotatable bonds (≤12), shield HBDs [15] |
| Poor Solubility | Limits absorption, causes unreliable assay results [15] | Optimize linker composition and length, incorporate solubilizing groups, salt formation |
| Nonspecific Binding | Leads to low assay recovery, confounds in vitro data [15] | Add serum proteins (e.g., FCS, BSA) to assays, use low-binding labware [15] |
| Variable Clearance | Difficult to extrapolate from in vitro to in vivo [15] | Use experimentally determined fraction unbound (fu,inc) for IVIVE, not predicted values [15] |
Recent research has established preferred physicochemical property spaces for oral PROTACs to guide optimization. These include limiting H-bond donors (HBDs) to ≤3, molecular weight to ≤950 Da, and rotatable bonds to ≤12 [15]. Notably, reducing solvent-exposed HBDs to ≤2 is a particularly powerful strategy for optimizing permeability, sometimes allowing other parameters (MW, Chromlog D) to be pushed slightly higher [15]. The reduction of exposed polar surface area (ePSA), often through strategic shielding of HBDs, also significantly enhances permeability [15].
Experimental Protocols for PROTAC ADME Profiling
Standard small molecule ADME assays often require adaptation for PROTACs due to their bRo5 properties. The following protocol outlines a tailored discovery assay cascade.
Protocol 2: Tailored In Vitro ADME Profiling for PROTACs
Objective: To reliably characterize the ADME properties of PROTAC candidates, accounting for their unique challenges like nonspecific binding and low solubility.
Materials:
- Test Compounds: PROTAC candidates
- Modified Assay Buffers: HBSS with 10% Fetal Calf Serum (FCS) or 0.25-0.5% BSA [15]
- Permeability Systems: Caco-2 cell monolayers or surrogate systems for ePSA determination [15]
- Metabolic Systems: Cryopreserved hepatocytes (multiple species) in suspension [15]
- Analytical Instrumentation: UHPLC-MS/MS system for quantification [15]
Procedure:
Solubility and Nonspecific Binding Assessment:
- Perform kinetic solubility assays in physiologically relevant buffers.
- To assess nonspecific binding, compare compound recovery in standard buffer versus buffer supplemented with 10% FCS or BSA [15].
- Data Analysis: Low recovery (<50%) in standard buffer that improves with serum addition indicates significant nonspecific binding.
Permeability Assessment (Modified Caco-2):
- Culture Caco-2 cells as described in Protocol 1.
- Modify the standard transwell assay by adding 10% FCS to both apical and basolateral compartments to reduce nonspecific binding and improve recovery [15].
- Alternative approach: Use surrogate methods like exposed Polar Surface Area (ePSA) determination as a permeability prognosticator [15] [23].
- Data Analysis: Calculate Papp. Note that for PROTACs, the Caco-2 assay may not be predictive for absorption, so focus on molecular descriptors (MW, HBD count) for prioritization [15].
Metabolic Stability in Hepatocytes:
- Use cryopreserved hepatocytes (e.g., mouse, human) in suspension. Ensure viability is >70% via trypan blue staining [15].
- Incubate compounds (1 µM final) with hepatocytes at a density of 0.2 × 10^6 cells/mL in Krebs-Henseleit buffer (pH 7.4) at 37°C [15].
- Take aliquots at time points (e.g., 0, 10, 20, 40, 60, 90 min), quench with ACN containing internal standard, and analyze via UHPLC-MS/MS.
- Data Analysis: Determine intrinsic clearance (CLint). For IVIVE, use experimentally determined fraction unbound in incubation (fu,inc), as standard prediction methods (e.g., Kilford equation) are unsuitable for PROTACs and lead to systematic under-prediction [15].
The tailored ADME strategy for PROTACs emphasizes early frontloading of in vivo studies and the use of specific surrogate descriptors for permeability, as illustrated below:
Research Reagent Solutions for PROTAC ADME
Table 4: Key Reagents for PROTAC ADME Assays
| Research Reagent | Function in ADME Profiling | Application Notes |
|---|---|---|
| Serum Proteins (FCS, BSA) | Reduce nonspecific binding in in vitro assays (e.g., Caco-2) [15] | Adding 10% FCS or 0.25-0.5% BSA to assay buffers can dramatically improve recovery. |
| Cryopreserved Hepatocytes | Determine intrinsic metabolic clearance (CLint) [15] | Use multiple species; require experimentally determined fu,inc for accurate IVIVE. |
| Caco-2 Cell Line | Assess passive permeability potential (with modifications) [15] | Standard assay may not be predictive for absorption; use serum-modified protocols. |
| Surface Plasmon Resonance (SPR) | Study ternary complex formation and binding kinetics [23] | Critical for confirming target engagement and understanding degradation efficiency. |
| Analytical UHPLC-MS/MS | Quantify parent compound in all in vitro and in vivo matrices [15] | Essential for dealing with complex molecules and potential metabolite interference. |
Integrating modality-specific ADME profiling during lead optimization is critical for advancing peptides and PROTACs through the drug development pipeline. For peptides, this involves a focus on mitigating metabolic instability and low permeability through strategic structural modifications and specialized in vitro assays. For PROTACs, success hinges on navigating the beyond-rule-of5 property space by controlling key molecular descriptors and adapting standard ADME assays to address unique challenges like nonspecific binding. Employing the detailed protocols, property guidelines, and reagent solutions outlined in this application note will enable researchers to de-risk the development of these advanced modalities, ultimately accelerating the delivery of novel therapeutics to patients.
The Impact of Transporters and Enzymes on Drug Disposition
Within the framework of ADME (Absorption, Distribution, Metabolism, and Excretion) optimization during lead optimization, understanding the intricate roles of drug-metabolizing enzymes and membrane transporters is paramount. These key regulators are closely linked to the pharmacokinetics (PK), efficacy, and safety profile of drug candidates [28]. The interplay between enzymes and transporters significantly influences a compound's disposition, including its inter-organ distribution and clearance in humans [28] [29]. Predicting these influences from in vitro data remains a central challenge in the drug discovery decision-making process [28]. This document provides detailed application notes and protocols to guide researchers in the experimental and strategic evaluation of these critical systems.
Core Concepts and Biological Significance
Key Players in Drug Disposition
Drug-Metabolizing Enzymes (DMEs), such as those from the cytochrome P450 (CYP) family (e.g., CYP3A4, CYP2D6) and UDP-glucuronosyltransferases (UGTs), catalyze the biochemical modification of drugs, leading to their activation or inactivation [30]. Membrane Transporters, including those from the ATP-binding cassette (ABC) superfamily (e.g., P-glycoprotein/P-gp) and the solute carrier (SLC) superfamily (e.g., OATP1B1), actively facilitate the movement of drugs across cellular barriers in tissues like the intestine, liver, kidney, and blood-brain barrier [29]. Their combined action controls virtually all physiological processes related to drug exposure [31].
Enzyme and Transporter Interactions
Interactions often involve a drug acting as an inhibitor, inducer, or substrate for an enzyme or transporter.
- Enzyme/Transporter Inhibition: A drug (inhibitor) decreases the activity of an enzyme or transporter, potentially leading to increased concentrations of a co-administered substrate drug. Inhibition can be reversible (competitive, uncompetitive, non-competitive, mixed) or irreversible (mechanism-based) [30] [32].
- Enzyme/Transporter Induction: A drug (inducer) increases the expression or activity of an enzyme or transporter, potentially leading to decreased concentrations of a co-administered substrate drug [30] [32].
- Pro-drug Activation: Some drugs are administered as inactive pro-drugs that require enzymatic conversion (e.g., by CYP2D6) to their active form. Inhibition of the activating enzyme can nullify the drug's efficacy [30].
The clinical significance of these interactions depends on factors such as the strength of inhibition/induction, the therapeutic index of the substrate drug, and the involvement of major versus minor metabolic pathways [30].
The diagram below illustrates the core concepts of how enzymes and transporters impact drug disposition at key physiological barriers.
Diagram: Role of Enzymes and Transporters in Drug Disposition. CYP enzymes (red) metabolize drugs, reducing bioavailability. P-gp (blue) effluxes drugs, limiting absorption and distribution. Uptake transporters (green) facilitate hepatic entry.
Quantitative Data and Kinetic Parameters
Approximate Half-Lives of Human Hepatic CYP Enzymes
The half-life of an enzyme is a critical parameter for predicting the time course of induction or irreversible inhibition, as recovery depends on the synthesis of new enzyme [30].
| CYP Enzyme | Median Turnover Half-Life (Hours) |
|---|---|
| CYP1A2 | 39 |
| CYP2C8 | 23 |
| CYP2C9 | 104 |
| CYP2C19 | 26 |
| CYP2D6 | 51 |
| CYP3A4 | 72 |
Table: Approximate median turnover half-lives of human hepatic CYP enzymes. Data sourced from [30].
Kinetic Modifications in Enzyme Inhibition
The following table summarizes the changes to Michaelis-Menten kinetic parameters under different types of reversible inhibition. [I] represents the free inhibitor concentration, and Kᵢ is the dissociation constant for the inhibitor-enzyme complex [32].
| Inhibition Type | Apparent Kₘ (Kₘ,ₐₚₚ) | Apparent Vₘₐₓ (Vₘₐₓ,ₐₚₚ) |
|---|---|---|
| Competitive | Kₘ × (1 + [I]/Kᵢ) | Unchanged (Vₘₐₓ) |
| Uncompetitive | Kₘ / (1 + [I]/Kᵢ) | Vₘₐₓ / (1 + [I]/Kᵢ) |
| Non-Competitive* | Kₘ | Vₘₐₓ / (1 + [I]/Kᵢ) |
| Mixed | Kₘ × (1 + [I]/Kᵢ) / (1 + [I]/αKᵢ) | Vₘₐₓ / (1 + [I]/αKᵢ) |
Table: Kinetic parameter changes under reversible inhibition. *Non-competitive inhibition is a special case of mixed inhibition where α=1 [32].
Experimental Protocols
Protocol: In Vitro Enzyme Phenotyping Using Chemical Inhibitors
Objective: To identify the specific CYP enzyme(s) responsible for the metabolism of a new chemical entity (NCE) in human liver microsomes (HLM).
Principle: Selective chemical inhibitors for specific CYP isoforms are co-incubated with the NCE in HLM. A significant reduction in metabolite formation in the presence of a particular inhibitor indicates the involvement of that CYP pathway [28].
Materials:
- Test system: Pooled human liver microsomes (e.g., 0.5 mg/mL protein)
- Test compound: NCE at a concentration ≤ Kₘ
- Co-factor: NADPH regenerating system
- Selective CYP inhibitors (see Reagent Solutions table)
- Stop solution: Acetonitrile with internal standard
- Analytical instrument: LC-MS/MS
Procedure:
- Preparation: Dilute HLM in a suitable buffer (e.g., 100 mM phosphate buffer, pH 7.4). Prepare a master mix containing HLM and the NADPH regenerating system.
- Pre-incubation: Aliquot the master mix into tubes. Add individual selective inhibitors or vehicle control (for uninhibited control) to respective tubes. Pre-incubate for 5 minutes at 37°C.
- Reaction Initiation: Start the reaction by adding the NCE substrate.
- Incubation: Incubate at 37°C for a linear, predetermined time (e.g., 10-60 minutes).
- Reaction Termination: Stop the reaction by adding a volume of ice-cold acetonitrile with internal standard.
- Sample Analysis: Centrifuge samples to precipitate protein. Analyze the supernatant using LC-MS/MS to quantify the metabolite formation rate.
- Data Analysis: Calculate the percentage of remaining activity relative to the uninhibited control. A reduction of >80% by a selective inhibitor is considered strong evidence for the involvement of that pathway.
Protocol: Assessment of P-gp Substrate Status (Caco-2 / MDR1-MDCK Assay)
Objective: To determine if an NCE is a substrate for the P-glycoprotein (P-gp) efflux transporter.
Principle: The bidirectional transport of the NCE is measured across a monolayer of cells expressing P-gp (e.g., Caco-2 or MDR1-MDCK). A net efflux ratio (NER) greater than 2 is indicative of active efflux by P-gp [29].
Materials:
- Cell model: Caco-2 or MDR1-MDCK cells grown on permeable filters
- Test compound: NCE (at two concentrations, one low and one high)
- Transport buffer: Hanks' Balanced Salt Solution (HBSS) with HEPES, pH 7.4
- Selective P-gp inhibitor (e.g., Zosuquidar, Verapamil)
- Analytical instrument: LC-MS/MS
Procedure:
- Cell Culture: Seed cells on permeable transwell inserts and culture for 21 days (Caco-2) or until a tight monolayer is formed (confirmed by TEER measurement).
- Experimental Design: Perform bidirectional transport studies:
- A-to-B (Apical to Basolateral): Add NCE to the apical chamber, measure appearance in basolateral chamber.
- B-to-A (Basolateral to Apical): Add NCE to the basolateral chamber, measure appearance in apical chamber.
- Conduct both directions in the absence and presence of a selective P-gp inhibitor.
- Incubation: Add transport buffer containing the NCE to the donor compartment and blank buffer to the receiver compartment. Incubate at 37°C with gentle shaking.
- Sampling: Take samples from the receiver compartment at multiple time points (e.g., 30, 60, 90, 120 min) and replace with fresh buffer.
- Sample Analysis: Analyze samples using LC-MS/MS to determine the concentration of the NCE.
- Data Analysis:
- Calculate the apparent permeability (Pₐₚₚ) in both directions.
- Determine the Efflux Ratio (ER) = Pₐₚₚ (B-to-A) / Pₐₚₚ (A-to-B).
- Determine the Net Efflux Ratio (NER) = ER (without inhibitor) / ER (with inhibitor).
- An ER ≥ 2 and a NER ≥ 2 suggests the NCE is a P-gp substrate.
The workflow for conducting these key in vitro assays is summarized below.
Diagram: Key In Vitro Assay Workflow. Parallel experimental pathways for enzyme phenotyping and transporter substrate identification to inform PBPK modeling and DDI risk assessment.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Tool | Function in Experiment |
|---|---|
| Pooled Human Liver Microsomes (HLM) | A mixed-gender pool of human liver microsomes containing a full complement of CYP and UGT enzymes for in vitro metabolic stability and phenotyping studies. |
| Recombinant CYP Enzymes (rCYP) | Individual CYP isoforms (e.g., rCYP3A4, rCYP2D6) expressed in a standardized system. Used to confirm the specific enzyme responsible for metabolizing a candidate drug. |
| Selective Chemical Inhibitors | Tool compounds that selectively inhibit specific CYP enzymes (e.g., Ketoconazole for CYP3A4, Quinidine for CYP2D6) to identify metabolic pathways in phenotyping studies [30]. |
| MDR1-MDCK II Cells | Madin-Darby Canine Kidney cells transfected with the human MDR1 gene, which encodes for P-gp. This model provides a robust system for assessing P-gp-mediated transport. |
| Caco-2 Cells | A human colon adenocarcinoma cell line that, upon differentiation, expresses a range of transporters, including P-gp. Commonly used for permeability and transporter studies. |
| NADPH Regenerating System | A biochemical system (e.g., NADP+, Glucose-6-Phosphate, G6PDH) that supplies the reducing equivalents (NADPH) required for CYP-mediated oxidative reactions. |
Advanced Applications and Future Perspectives
Integration with Physiologically Based Pharmacokinetic (PBPK) Modeling
In vitro data on enzyme inhibition/induction and transporter interactions are crucial for building PBPK models. These models integrate physicochemical properties of the drug, in vitro data, and human physiology to simulate and predict complex drug-drug interactions (DDIs) in vivo [33]. For instance, a PBPK model for encorafenib, which is metabolized by CYP3A4 and is a P-gp substrate, successfully predicted its DDIs with CYP3A4 inhibitors like posaconazole, thereby prospectively de-risking its clinical development [33]. The mathematical implementation of enzyme turnover and inhibition in such software is critical for accurate DDI prediction, particularly for time-dependent inactivation [32].
Emerging Technologies: Quantum Machine Learning for QSAR
The field of ADME science is beginning to explore advanced computational methods. Quantum Machine Learning (QML) is being investigated for Quantitative Structure-Activity Relationship (QSAR) prediction, which relates molecular structures to biological activity. Early research suggests that quantum-classical hybrid models can demonstrate superior generalization power, especially when data availability is limited or when working with a reduced number of molecular features [34]. This could potentially enhance the prediction of whether a new compound is likely to be a substrate or inhibitor of enzymes and transporters, thereby guiding more efficient lead optimization.
Modern ADME Toolbox: From High-Throughput Screening to AI-Driven Prediction
Within modern drug discovery, the optimization of absorption, distribution, metabolism, and excretion (ADME) properties is critical for reducing late-stage attrition due to unfavorable pharmacokinetics [35]. A tiered in vitro assay strategy provides a framework for efficiently balancing speed, resource allocation, and data quality during lead optimization. This approach enables research teams to make earlier, more informed decisions by initially employing rapid, lower-cost assays to prioritize compounds, followed by more definitive, resource-intensive studies on the most promising candidates [13] [36]. This application note details the implementation of a two-tiered ADME screening strategy, providing structured protocols, benchmarks, and visualization tools to integrate this efficient screening paradigm into the drug discovery workflow.
The Rationale for a Two-Tiered Screening Strategy
The fundamental principle of a two-tiered strategy is to align the experimental design with the specific decision-making needs at each stage of the research process [36]. In the early phases of lead optimization, the primary goal is to quickly eliminate compounds with suboptimal ADME properties, for which high-quality, rapid data is more valuable than exhaustive, submission-ready datasets. This strategy manages program risk and cost by front-loading efficient screening to focus resources on candidates with the highest probability of success.
- Tier 1 (Early Screening): Designed for high-throughput and rapid turnaround, Tier 1 assays provide preliminary data to guide chemistry efforts and select leads for advanced profiling. The objective is to identify critical ADME liabilities early, enabling prompt corrective action in the design cycle [13].
- Tier 2 (Definitive Profiling): This tier involves more comprehensive and rigorous assays that often adhere to higher quality standards, such as Good Laboratory Practice (GLP). The data generated is suitable for regulatory submissions, such as Investigational New Drug (IND) applications, and provides a robust dataset for candidate selection [36].
Table 1: Comparison of Tiered Study Objectives
| Parameter | Tier 1 (Basic Program) | Tier 2 (IND-Enabling Program) |
|---|---|---|
| Primary Goal | Early decision-making, inform definitive study design [36] | Generate IND submission-ready data [36] |
| Throughput | High | Medium to Low |
| Resource Level | Low cost, minimal compound use [13] | Higher cost, comprehensive |
| Data Output | Trends and rankings | High-quality, definitive endpoints |
| Report Format | Standard internal report | Comprehensive standard report or eCTD-ready format [36] |
Core Components of a Two-Tiered ADME Assay Panel
A well-designed tiered strategy focuses on key in vitro assays that predict critical in vivo pharmacokinetic outcomes. The following core assays form the foundation of this approach.
Metabolic Stability
Pharmacological Question Addressed: “How long will my parent compound remain circulating in plasma within the body?” [13]
This assay uses hepatic microsomes to provide an initial estimate of a compound's metabolic clearance.
- Tier 1 Protocol (Single Time Point): Metabolic stability is assessed at a single concentration (typically 10 µM) in human liver microsomes (0.5 mg/mL) over a 60-minute incubation. The result is reported as the percentage of parent compound metabolized at the final time point, allowing for rapid ranking of compounds [13].
- Tier 2 Protocol (Multi-Time Point): A more definitive assay incorporates multiple time points (e.g., 0, 15, 30, 45, 60 minutes) to determine the half-life (T½) and intrinsic clearance (CLint), providing superior data for in vitro-in vivo extrapolation (IVIVE) [13].
Permeability
Pharmacological Question Addressed: “Will my compound be absorbed?”
Cell-based models like Caco-2 or PAMPA (Parallel Artificial Membrane Permeability Assay) are used to predict intestinal absorption.
- Tier 1 Protocol (PAMPA): This non-cell-based assay offers high throughput and is ideal for early screening. It measures the apparent permeability (Papp) of a compound across an artificial membrane, providing a cost-effective initial assessment of passive permeability [6].
- Tier 2 Protocol (Caco-2): This cell-based model provides a more physiologically relevant assessment, as it can identify compounds that are substrates for efflux transporters (e.g., P-glycoprotein) in addition to measuring passive permeability, offering a more complete absorption profile [35].
Cytochrome P450 (CYP) Inhibition
Pharmacological Question Addressed: “What is the potential for my compound to cause drug-drug interactions (DDI)?”
This assay evaluates the ability of a new chemical entity to inhibit major CYP enzymes, a common cause of clinically significant DDIs.
- Tier 1 Protocol (Single Concentration): Compounds are screened at a single concentration (e.g., 10 µM) against key CYP enzymes (e.g., 3A4, 2D6). The result is reported as percent inhibition, allowing for the rapid flagging of potent inhibitors [36] [35].
- Tier 2 Protocol (IC50 Determination): For compounds showing significant inhibition in Tier 1, a multi-concentration assay is performed to determine the half-maximal inhibitory concentration (IC50), which is used for a more quantitative DDI risk assessment [36].
Table 2: Tiered Assay Benchmarks and Rules of Thumb
| Assay | Tier | Key Endpoint | Benchmark for Low Risk |
|---|---|---|---|
| Metabolic Stability [13] | 1 | % Metabolized (60 min) | < 30% |
| 2 | In Vitro T½ (min) | > 60 min | |
| Permeability (Caco-2) [35] | 2 | Apparent Permeability (Papp, x 10⁻⁶ cm/s) | > 10 |
| CYP Inhibition [36] | 1 | % Inhibition (@ 10 µM) | < 50% |
| 2 | IC50 (µM) | > 10 µM | |
| Solubility [13] | 1 | Amount Dissolved (µM) | > 100 µM |
Detailed Experimental Protocol: Tier 1 Metabolic Stability
The following is a standardized protocol for a Tier 1 metabolic stability assay using liver microsomes, a cornerstone of early ADME screening [13].
Reagents and Materials
Table 3: Research Reagent Solutions for Metabolic Stability
| Reagent/Material | Function in the Assay |
|---|---|
| Human Liver Microsomes (HLM) [13] | Subcellular fraction containing drug-metabolizing enzymes (CYPs, UGTs). |
| NADPH Regenerating System | Supplies NADPH, a crucial cofactor for cytochrome P450 enzyme activity. |
| Compounds for Testing | New chemical entities whose metabolic stability is being evaluated. |
| Positive Control (e.g., Testosterone) [13] | A compound with known metabolic activity to verify system functionality. |
| Potassium Phosphate Buffer (pH 7.4) | Provides a physiologically relevant pH environment for the incubation. |
| Methanol or Acetonitrile | Used to terminate the metabolic reaction and precipitate proteins. |
Step-by-Step Procedure
- Preparation of Reaction Cocktail: In a pre-warmed (37°C) tube, prepare the master reaction cocktail to achieve final incubation concentrations of 0.5 mg/mL HLM and test article at 10 µM in potassium phosphate buffer (pH 7.4) [13].
- Pre-incubation: Aliquot the reaction cocktail (e.g., 98 µL) into a 96-well plate. Pre-incubate the plate for 5-10 minutes in a shaking incubator at 37°C.
- Initiation of Reaction: Start the reaction by adding a pre-warmed NADPH regenerating system (e.g., 2 µL). For the T=0 control, add the NADPH solution to the negative control well after adding the quenching solvent (Step 4).
- Termination of Reaction: At the predetermined time point (T=60 minutes), quench the reaction by adding a volume of ice-cold acetonitrile containing internal standard that is at least equal to the reaction volume.
- Sample Analysis: Centrifuge the quenched plate at high speed (e.g., 4000 rpm for 15 minutes) to pellet precipitated protein. Transfer the supernatant to a new plate for analysis by LC-MS/MS.
- Data Calculation: Quantify the peak area of the parent compound in the T=60 min sample relative to the T=0 min control. Calculate the percentage of parent compound remaining:
(Peak Area T=60 / Peak Area T=0) * 100.
Implementing a Tiered Strategy: A Practical Scenario
The following scenario illustrates how a tiered approach can be applied to a real-world drug discovery program.
- Scenario A: A client is planning an IND submission and needs to design a Cytochrome P450 induction study. Being budget-sensitive, they want to ensure the study design is correct from the outset [36].
- Tier 1 Application: A Tier 1 induction study using a single, sensitive donor for CYP1A2, 2B6, and 3A4 is recommended. The mRNA data can help inform the full study design. If up-regulation is observed, it would be beneficial to include the CYP2Cs from the beginning, potentially saving weeks compared to a stepwise approach [36].
- Tier 2 Follow-up: Once the Tier 1 study confirms the induction pathway, a Tier 2 CYP induction study is initiated to provide the standard EC50/Emax endpoints required for the IND submission [36].
The adoption of a tiered in vitro assay strategy is a hallmark of an efficient and modern drug discovery organization. By implementing the structured two-tier approach outlined in this application note—utilizing rapid, high-throughput Tier 1 screens to triage compounds and conserve resources, followed by definitive Tier 2 studies to generate robust, submission-ready data—research teams can significantly accelerate lead optimization timelines. This paradigm ensures that critical ADME properties are characterized early, derisking the development pipeline and increasing the likelihood of advancing high-quality drug candidates into clinical development.
The optimization of Absorption, Distribution, Metabolism, and Excretion (ADME) properties is a critical determinant of success in drug discovery, particularly during the lead optimization phase. Poor ADME profiles remain a major cause of compound attrition in later development stages [37]. Traditional in vivo and in vitro ADME screening methods, while valuable, are often resource-intensive, time-consuming, and expensive [38] [27]. Consequently, the application of in silico prediction methods has become indispensable for prioritizing compound synthesis and guiding molecular design.
The field of in silico ADME prediction has evolved significantly, transitioning from simplified relationships based on physicochemical properties to sophisticated artificial intelligence (AI) and machine learning (ML) models [37]. Recent advances leverage techniques such as graph neural networks (GNNs), multitask learning, and explainable AI (XAI) to enhance predictive accuracy and provide insights into the structural features influencing ADME parameters [38] [19]. These approaches are increasingly used to bias medicinal chemistry toward more ideal regions of property space, thereby streamlining the optimization of lead compounds [39].
This application note details the latest methodologies and protocols in in silico ADME prediction, with a specific focus on AI- and GNN-based approaches. It provides a structured framework for their application within lead optimization research, supported by comparative performance data, detailed experimental protocols, and visualization of key workflows.
Computational Approaches in ADME Prediction
A variety of computational modeling approaches are employed for predicting ADME properties, broadly categorized into descriptor-based models and graph-based models [40].
Descriptor-Based Models
Descriptor-based models rely on hand-crafted molecular representations, such as molecular descriptors (e.g., molecular weight, lipophilicity, polar surface area) and fingerprints (e.g., Extended Connectivity Fingerprints, ECFP), as input features for machine learning algorithms [40]. These representations are used to establish Quantitative Structure-Activity Relationship (QSAR) models.
- Common Algorithms: Traditional machine learning algorithms used with these descriptors include Support Vector Machines (SVM), Random Forests (RF), and eXtreme Gradient Boosting (XGBoost) [40].
- Utility: These models are highly effective, with studies showing that descriptor-based models can often match or even surpass the predictive accuracy of more complex graph-based models, especially when using comprehensive sets of molecular descriptors and fingerprints [40]. They are also computationally efficient and highly interpretable using methods like SHAP (SHapley Additive exPlanations) [40].
Graph-Based Models
Graph-based models, particularly Graph Neural Networks (GNNs), represent a molecule natively as a graph, where atoms are nodes and bonds are edges. The GNN automatically learns task-specific molecular representations through a process of message passing and feature aggregation from the molecular graph, eliminating the need for pre-defined descriptors [38] [40].
- Common Architectures: Commonly used GNN architectures include Graph Convolutional Networks (GCN), Graph Attention Networks (GAT), Message Passing Neural Networks (MPNN), and Attentive FP [40].
- Advantages: The key advantage of GNNs is their ability to learn complex, non-linear structure-property relationships directly from the graph structure. Recent studies have successfully employed multitask learning with GNNs, where a single model is trained to predict multiple ADME endpoints simultaneously. This approach allows the model to share information across related tasks, improving predictive performance, especially on tasks with limited data [38] [19].
Table 1: Comparison of Common Machine Learning Approaches for ADME Prediction
| Model Type | Representative Algorithms | Molecular Representation | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Descriptor-Based | SVM, RF, XGBoost, DNN | Pre-calculated descriptors and fingerprints [40] | High computational efficiency, strong performance, excellent interpretability [40] | Dependent on choice and quality of descriptors [40] |
| Graph-Based | GCN, GAT, MPNN, Attentive FP | Molecular graph (atoms and bonds) [40] | Automates feature learning; captures complex structural relationships [38] [40] | Higher computational cost; "black box" nature, though explainability methods are emerging [38] [40] |
The following diagram illustrates the core workflow and logical relationship between these different modeling approaches in a typical in silico ADME pipeline.
Performance Data and Model Selection
The selection of an appropriate modeling approach depends heavily on the specific ADME endpoint, the available data, and the project's requirements for accuracy, interpretability, and speed. The table below summarizes the reported performance of various algorithms on benchmark ADME tasks, providing a guide for model selection.
Table 2: Reported Performance of Selected Algorithms on Benchmark ADME/T Tasks
| ADME Task | Dataset | Task Type | Best Performing Algorithm(s) | Reported Metric & Performance | Key Reference |
|---|---|---|---|---|---|
| Aqueous Solubility | ESOL | Regression | SVM (Descriptor-based) | R²: ~0.90 (Superior to GNN baselines) | [40] |
| FreeSolv | Regression | SVM (Descriptor-based) | R²: ~0.90 (Superior to GNN baselines) | [40] | |
| Lipophilicity | Lipop | Regression | SVM (Descriptor-based) | R²: ~0.75 (Superior to GNN baselines) | [40] |
| Blood-Brain Barrier Penetration | BBBP | Classification | RF, XGBoost (Descriptor-based); Attentive FP (GNN) | Reliable performance from both descriptor-based and graph-based models | [40] |
| HIV Inhibition | HIV | Classification | RF, XGBoost (Descriptor-based) | Reliable performance from descriptor-based models | [40] |
| Toxicity | Tox21, ToxCast | Multi-task Classification | Attentive FP (GNN) | Outstanding performance on multi-task benchmarks | [40] |
| General ADME Parameters | Multi-parameter | Multi-task Regression/Classification | Multitask GNN (with fine-tuning) | Highest performance for 7/10 parameters vs. conventional methods | [38] |
Key Insights from Performance Data
- Descriptor-based models like SVM, RF, and XGBoost are highly competitive, often outperforming GNNs on standard regression tasks and many classification tasks, while being far more computationally efficient [40].
- Graph-based models like Attentive FP and Multitask GNNs excel in specific scenarios, particularly for multi-task learning on larger datasets or complex endpoints like toxicity [40] [38].
- Multitask learning is a powerful strategy for improving prediction across multiple ADME parameters, as it allows information sharing between tasks, effectively increasing the usable sample size for model training [38].
Protocols forIn SilicoADME Modeling
This section provides detailed methodological protocols for developing and applying descriptor-based and graph-based in silico ADME models.
Protocol 1: Building a Descriptor-Based ADME Prediction Model
Application: Creating a high-performance, interpretable model for a specific ADME endpoint (e.g., metabolic stability, permeability) using traditional machine learning.
Materials and Reagents:
- Software: KNIME, Python/R with scikit-learn, RDKit, MOE (for descriptor calculation).
- Data: Curated dataset of compounds with experimentally measured ADME endpoint values.
Procedure:
- Data Curation and Preparation:
- Collect a dataset of chemical structures and corresponding experimental values for the target ADME property.
- Apply rigorous data cleaning: standardize structures, remove duplicates, and handle salts. Curate the dataset to ensure data quality and consistency [37].
- Divide the data into a training set (∼80%) and a hold-out test set (∼20%) using techniques such as Kennard-Stone or random stratification to ensure representative chemical space coverage.
Molecular Representation:
- Calculate a comprehensive set of molecular features. A recommended combination is:
- Normalize the resulting feature matrix to a common scale (e.g., zero mean and unit variance).
Model Training and Validation:
- Train multiple machine learning algorithms (e.g., SVM, RF, XGBoost) on the training set using 5- or 10-fold cross-validation.
- Optimize model hyperparameters via grid or random search within the cross-validation loop to prevent overfitting.
- Use the hold-out test set only for the final evaluation of the best-performing model.
Model Interpretation:
- Apply explainable AI techniques like SHAP (SHapley Additive exPlanations) to the trained model [40].
- Analyze the most important descriptors and structural features driving the predictions to gain insights for lead optimization.
Protocol 2: Building a Multitask Graph Neural Network for ADME Prediction
Application: Simultaneously predicting multiple ADME parameters to leverage shared information across tasks and improve overall predictive accuracy.
Materials and Reagents:
- Software: Python, Deep Learning frameworks (PyTorch, TensorFlow), Deep Graph Library (DGL) or PyTorch Geometric.
- Data: Curated dataset of compounds with experimental values for multiple (e.g., 10) ADME parameters.
Procedure:
- Data Preprocessing and Graph Construction:
- Curate and clean the dataset as in Protocol 1. Ensure alignment of compounds across different ADME tasks.
- Represent each molecule as a graph. For each atom (node), define a feature vector (e.g., atom type, degree, hybridization, valence). For each bond (edge), define a feature vector (e.g., bond type, conjugation) [40].
- Handle missing values in the multi-task labels appropriately (e.g., through masking in the loss function).
Multitask GNN Model Architecture:
- Implement a GNN architecture (e.g., GCN, GAT, or MPNN) as the base for learning molecular representations.
- The model should consist of:
- Graph Feature Learning Layers: Multiple GNN layers that perform message passing to learn atom-level embeddings.
- Readout/Global Pooling Layer: Aggregates the atom-level embeddings into a single, fixed-size molecular representation (e.g., using sum, mean, or attention-based pooling like in Attentive FP) [40].
- Task-Specific Prediction Heads: Multiple parallel fully connected layers, each taking the shared molecular representation as input and predicting a single ADME endpoint [38].
Model Training with Fine-Tuning:
- First, pre-train the model using a multitask learning objective, sharing the GNN layers across all tasks. This leverages correlations between different ADME properties [38].
- Subsequently, fine-tune the model for each specific task by taking the pre-trained shared layers and training only the corresponding task-specific head on data for that single task. This adapts the general model to specialized tasks [38].
- Use a combined loss function (e.g., mean squared error for regression, cross-entropy for classification) during multitask pre-training.
Explanation of Predictions:
- Apply post-hoc explainability methods such as the Integrated Gradients (IG) method [38] [19].
- IG attributes the prediction to the input features (atoms/bonds) by integrating the gradients along a path from a baseline input to the actual input. This allows for the visualization of which structural motifs in a lead compound contribute positively or negatively to the predicted ADME property, providing actionable guidance for chemists.
The workflow for the Multitask GNN protocol, from data preparation to explainable output, is visualized below.
The Scientist's Toolkit: Essential Research Reagents and Solutions
The successful implementation of the protocols above relies on a suite of software tools and databases. The following table details key resources for in silico ADME research.
Table 3: Key Research Reagent Solutions for In Silico ADME Prediction
| Tool Name | Type | Primary Function | Access | Key Application in Protocol |
|---|---|---|---|---|
| RDKit | Software Library | Cheminformatics and ML; descriptor calculation, fingerprint generation, and graph construction. | Open-Source | Fundamental for data preprocessing and feature calculation in both Protocols 1 & 2 [40]. |
| ADMET Predictor | Commercial Software | Comprehensive platform for predicting a wide range of ADMET properties using proprietary models. | Commercial License | Used for benchmarking or as a source of predicted values in early discovery [7]. |
| SwissADME | Web Server | Free tool for predicting pharmacokinetics, drug-likeness, and medicinal chemistry friendliness. | Free Web Tool | Rapid, initial profiling of compounds during early design phases [37]. |
| OCHEM | Online Platform | Web-based platform for building, sharing, and deploying QSAR/QSPR models. | Free & Open-Source | Useful for building and hosting descriptor-based models as in Protocol 1 [37]. |
| Deep Graph Library (DGL) | Software Library | A Python package for implementing graph neural networks. | Open-Source | Primary framework for building the GNN model in Protocol 2 [38]. |
| Attentive FP | GNN Model | A state-of-the-art GNN architecture specifically designed for molecular property prediction. | Open-Source | Can serve as the base GNN architecture in Protocol 2 [40]. |
The integration of advanced in silico methods, particularly AI and GNNs, into lead optimization workflows marks a significant leap forward in predictive ADME science. While traditional descriptor-based models remain powerful, accurate, and efficient for many tasks, graph-based models offer a compelling approach for multi-task learning and capturing complex structural relationships. The emerging emphasis on explainable AI (XAI) is critical for translating model predictions into actionable chemical guidance, thereby closing the loop between computational prediction and experimental chemistry. By adopting the structured protocols and tools outlined in this application note, researchers can more effectively leverage these technologies to accelerate the discovery of compounds with desirable pharmacokinetic profiles, ultimately increasing the efficiency and success rate of drug development.
Physiologically-Based Pharmacokinetic (PBPK) Modeling for Human Dose Prediction
Physiologically-based pharmacokinetic (PBPK) modeling is a mechanistic, dynamic modeling approach that has become an integral tool in drug discovery and development over the last decade [41]. This modeling technique predicts the pharmacokinetic (PK) behavior of drugs in humans using preclinical data by incorporating species-specific physiological parameters with drug-specific properties [41] [42]. Unlike classical compartmental PK modeling that employs a "top-down" approach, PBPK modeling typically adopts a "bottom-up" methodology to simulate drug concentrations within major physiological compartments, providing higher physiological realism [42]. The fundamental strength of PBPK modeling lies in its ability to explore the effects of various physiologic parameters—including age, ethnicity, disease status, and organ impairment—on human pharmacokinetics, thereby guiding dose and regimen selection while aiding drug-drug interaction risk assessment [41].
Within the context of ADME (Absorption, Distribution, Metabolism, and Excretion) optimization during lead optimization research, PBPK modeling serves as a critical decision-support tool. It enables researchers to predict human PK from preclinical data, thereby facilitating lead optimization and candidate evaluation [42]. By providing a quantitative framework to simulate drug behavior under various conditions, PBPK modeling helps identify key ADME liabilities early in the development process, allowing for strategic intervention and optimization of compound properties [7] [43]. This approach reduces the need for extensive animal studies and can potentially replace certain clinical trials, aligning with the 3Rs (replacement, reduction, and refinement) principles in research [41] [7].
Core Principles of PBPK Modeling
Model Structure and Composition
PBPK models are composed of compartments representing different physiological organs of the body, interconnected by the circulating blood system [41]. Each compartment is defined by tissue-specific volumes and blood flow rates that are specific to the species of interest [41]. A full PBPK model typically incorporates physiological compartments such as the liver, kidneys, gut, brain, lungs, heart, adipose tissue, muscle, and blood, with each organ characterized by its specific volume, blood flow, and partition coefficients [42].
The mathematical foundation of PBPK models relies on mass balance differential equations that describe drug movement between compartments [41] [42]. For non-eliminating tissues, the equation is:
Where:
- VT = tissue volume
- CT = drug concentration in tissue
- QT = blood flow to tissue
- CA = arterial drug concentration
- CVT = venous drug concentration from tissue [41]
For eliminating tissues (such as the liver), an additional term accounts for drug clearance:
Where CLint represents the intrinsic clearance of the compound [41].
Key Model Assumptions
PBPK modeling operates under two primary assumptions regarding drug distribution:
Perfusion-limited (flow-limited) assumption: Applies to small lipophilic molecules where blood flow to the tissue proves to be the rate-limiting step for distribution. In this case, drug movement is primarily constrained by the rate of blood delivery to tissues [41] [42].
Permeability-limited (diffusion-limited) assumption: Relevant for more hydrophilic and larger molecules where permeability across cell membranes becomes the rate-limiting process. This model is appropriate when cellular membrane penetration represents a significant barrier to distribution [41] [42].
The following diagram illustrates the fundamental structure and workflow of a PBPK model for human dose prediction:
Model Parameters
PBPK modeling integrates two distinct parameter categories to generate accurate predictions:
Table 1: Essential Parameters for PBPK Model Construction
| Parameter Category | Specific Parameters | Source |
|---|---|---|
| Drug-Dependent Parameters | Molecular weight, pKa, logP, solubility, permeability, plasma protein binding (fu), blood:plasma partitioning (B:P), intrinsic clearance (CLint), enzyme kinetic parameters (Vmax, Km) | In vitro assays, in silico predictions [41] |
| System-Dependent Parameters | Organ volumes, blood flow rates, tissue compositions, enzyme/transporter abundance, glomerular filtration rate, plasma protein levels | Literature data, compiled databases in PBPK platforms [41] [42] |
| Drug-Biological Interaction Parameters | Tissue-plasma partition coefficients (Kp), fraction unbound in tissues (fu,t), transporter activity | In vitro to in vivo extrapolation (IVIVE), clinical data [42] |
Experimental Protocols for PBPK Model Development
Parameter Acquisition andIn VitrotoIn VivoExtrapolation (IVIVE)
The development of a robust PBPK model begins with comprehensive parameter acquisition through standardized experimental protocols:
Physicochemical Property Characterization
- Solubility Measurement: Determine pH-dependent solubility in buffers ranging from pH 1.2 to 7.4 using shake-flask or potentiometric methods. Report values in µg/mL [41].
- Permeability Assessment: Utilize Caco-2 or MDCK cell monolayers in transwell systems. Measure apparent permeability (Papp) in 10−6 cm/s under standardized conditions [41].
- Lipophilicity Determination: Measure octanol:water partition coefficient (logP) and distribution coefficient (logD) at physiological pH using shake-flask or chromatographic methods [41] [42].
Plasma Protein Binding and Blood Partitioning
- Plasma Protein Binding: Determine fraction unbound (fu) using equilibrium dialysis or ultrafiltration in human plasma. Note attention to binding to alpha-1-acid glycoprotein (AGP) for basic compounds [41].
- Blood:Plasma Partitioning: Incubate drug with fresh human blood at 37°C, separate plasma, and measure concentration ratio between blood and plasma (B:P) [41].
Metabolic Stability and Enzyme Phenotyping
- Hepatic Clearance Estimation: incubate drug with human liver microsomes (0.5 mg/mL), S9 fractions, or hepatocytes (1 million cells/mL). Determine intrinsic clearance (CLint) from depletion half-life in µL/min/mg protein (microsomes/S9) or µL/min/million cells (hepatocytes) [41].
- Reaction Phenotyping: Determine percent contribution of specific enzymes (e.g., CYPs) using chemical inhibitors, recombinant enzymes, or correlation analysis. Report as fm (fraction metabolized) values [41].
- Enzyme Kinetics: For saturable metabolism, determine Vmax and Km using the same in vitro system where intrinsic clearance was determined [41].
Drug-Drug Interaction Potential
- Reversible Inhibition: Determine IC50 values against major CYP enzymes using human liver microsomes and probe substrates [41].
- Time-Dependent Inhibition: Assess mechanism-based inhibition by determining kinact and KI through pre-incubation experiments [41].
- Enzyme Induction: Evaluate CYP induction in cultured human hepatocytes from at least 3 donors. Report fold induction and EC50 values relative to positive controls [41].
Model Verification and Refinement Strategy
PBPK modeling typically employs a combined "bottom-up" and "middle-out" approach to create and refine models [41] [42]. The verification protocol follows these key stages:
Verification of intravenous disposition prediction in preclinical species: Assess appropriate tissue-plasma partition coefficient (Kp) prediction methodology and evaluate prediction accuracy considering physicochemical properties [41].
Verification of oral absorption prediction in preclinical species: Simulate absorption over a range of doses to further assess prediction accuracy and identify potential absorption limitations [41].
Simulation of disposition and absorption in humans: Use appropriate clearance and Kp prediction methods selected based on the preclinical verification step [41].
Model refinement with clinical data: Once clinical data become available, refine the mechanistic PBPK model using a "middle-out" approach and apply it prospectively to simulate unstudied scenarios [41].
The following workflow illustrates the integrated approach to PBPK model development and application:
PBPK Software and Research Tools
The advancement and implementation of PBPK modeling have been facilitated by dedicated software platforms that provide comprehensive built-in libraries, parameter estimation tools, and simulation modules.
Table 2: Common PBPK Modeling Software Platforms
| Software | Developer | Key Features | Typical Applications |
|---|---|---|---|
| GastroPlus | Simulations Plus | Specialized in modeling oral absorption and dissolution; integrates physiology-based biopharmaceutics modeling | Formulation development, absorption optimization, food effect prediction [42] [44] |
| Simcyp | Certara | Comprehensive population-based PBPK platform with extensive library of physiological parameters | DDI prediction, pediatric PK, special populations, regulatory submissions [41] [42] |
| PK-Sim | Open Systems Pharmacology | Open-source platform with whole-body PBPK modeling capabilities across species | Academic research, drug disposition prediction, cross-species extrapolation [42] [45] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for PBPK Modeling
| Reagent/Material | Function in PBPK Modeling | Application Context |
|---|---|---|
| Human Liver Microsomes | Provide cytochrome P450 and other drug-metabolizing enzymes for in vitro clearance and inhibition studies | Metabolic stability assessment, reaction phenotyping, DDI potential [41] [7] |
| Cryopreserved Human Hepatocytes | Contain complete hepatic metabolic system including Phase I/II enzymes and transporters; maintain enzyme induction response | Intrinsic clearance determination, enzyme induction studies, metabolite identification [41] [43] |
| Caco-2 Cell Lines | Model human intestinal permeability through differentiated colon carcinoma cells with enterocyte-like properties | Permeability classification, absorption prediction, transporter studies [41] |
| Recombinant CYP Enzymes | Individual cytochrome P450 isoforms expressed in heterologous systems for specific reaction phenotyping | Enzyme contribution (fm) determination, kinetic parameter estimation [41] |
| Equilibrium Dialysis Devices | Measure plasma protein binding through separation of protein-bound and unbound drug fractions | Fraction unbound (fu) determination for IVIVE [41] [7] |
| Accelerator Mass Spectrometry (AMS) | Ultra-sensitive detection of radiolabeled compounds for microdosing studies and metabolite profiling | Human ADME studies, absolute bioavailability, metabolite exposure [7] |
Applications in ADME Optimization and Lead Optimization
PBPK modeling provides critical insights throughout the lead optimization phase, enabling data-driven decisions that enhance compound selection and development strategy.
Human Pharmacokinetic Prediction
The primary application of PBPK modeling in lead optimization is predicting human PK parameters from preclinical data. Using a verified "bottom-up" approach, PBPK models can simulate human concentration-time profiles, enabling early identification of compounds with suboptimal exposure [41] [43]. This capability allows researchers to prioritize lead compounds with higher probability of success, focusing resources on candidates most likely to achieve therapeutic concentrations at the target site [43].
Case studies demonstrate successful application of PBPK models for human PK projection during discovery stages. These implementations typically involve preverification in preclinical species, application of empirical scalars when necessary in clearance prediction, in silico prediction of permeability, and exploration of aqueous and biorelevant solubility data to predict dissolution [43]. The integration of these elements within a PBPK framework provides a quantitative basis for candidate selection and human dose prediction.
Formulation Strategy and Developability Assessment
PBPK modeling supports formulation development by identifying key ADME liabilities and linking them to actionable formulation strategies [46]. Integrated with developability assessments, PBPK models guide technology selection, route-of-delivery evaluation, and absorption optimization from lead nomination through Phase I [46]. Using compound-specific physicochemical and ADME inputs, PBPK modeling characterizes drug behavior after dosing and predicts the impact of alternative formulations [46].
Specific applications include:
- Identification of absorption limitations: Discriminate between solubility-limited and permeability-limited absorption to guide formulation strategy [46].
- Bioperformance specification setting: Establish dissolution specifications using PBPK simulations to ensure product performance across the patient population [46].
- Enabling technology evaluation: Simulate the performance of lipid-based systems, amorphous solid dispersions, and modified-release designs to select the most appropriate technology for specific absorption challenges [46].
Special Population Extrapolations
PBPK modeling enables extrapolation of drug behavior to special populations where clinical trials may be challenging or unethical, such as pediatric patients or individuals with organ impairment [42] [44]. By incorporating population-specific physiological parameters, PBPK models can simulate PK in these groups, guiding dose adjustments and optimizing therapy.
A recent example demonstrates the application of PBPK modeling for linezolid in pediatric patients with renal impairment [44]. The model, developed and validated for both healthy adults and adults with renal impairment, was subsequently adapted for pediatric applications. After verification with clinical PK data, the PBPK model precisely predicted linezolid exposure in pediatric populations with varying degrees of renal impairment, encompassing weight- and age-associated PK variations [44]. Simulations revealed that pediatric populations with severe or end-stage renal impairment exhibited 1.21-fold and 1.28-fold elevations in AUC values, respectively, relative to healthy pediatric counterparts when administered equivalent 10 mg/kg doses [44]. This analysis supported dose optimization to 8 mg/kg every 8 hours for children with severe or end-stage renal impairment [44].
Drug-Drug Interaction (DDI) Assessment
PBPK modeling has become a mainstream approach for predicting and characterizing clinical drug interactions throughout the development process [47]. With advancements in commercially available PBPK software, PBPK DDI modeling is now routinely used from early drug discovery through late-stage development and often supports regulatory submissions [47].
The mechanistic nature of PBPK models allows for prediction of complex DDIs involving multiple inhibitory, inductive, or pathway interactions simultaneously [47]. These models can incorporate:
- Enzyme inhibition/induction kinetics
- Transporter-mediated interactions
- Time-dependent inhibition
- Simultaneous effects on multiple metabolic pathways
Recent publications highlight 209 PBPK DDI examples in 2023 alone, demonstrating the expanding role of this approach in characterizing DDI potential for therapeutic molecules [47]. This is particularly relevant given the increasing prevalence of polypharmacy in clinical settings [47].
Physiologically-based pharmacokinetic modeling represents a powerful, mechanistic approach to human dose prediction that has become integral to modern drug development. By integrating drug-specific properties with species- and population-specific physiological parameters, PBPK modeling provides a quantitative framework for predicting human pharmacokinetics, optimizing formulation strategy, assessing drug-drug interaction potential, and extrapolating to special populations. Within lead optimization research, PBPK modeling serves as a critical decision-support tool that enhances ADME optimization, enables prioritization of candidates with higher probability of success, and reduces development risks through data-driven predictions. As PBPK modeling continues to evolve with advancements in software platforms, incorporation of artificial intelligence and machine learning approaches, and refinement of model acceptance criteria, its role in accelerating drug development while ensuring patient safety is expected to expand further.
The lead optimization phase in drug discovery is pivotal for refining candidate compounds to improve their efficacy, safety, and pharmacokinetic profiles. Accurate prediction of human Absorption, Distribution, Metabolism, and Excretion (ADME) properties during this stage is critical, as pharmacokinetic issues account for approximately 16% of Phase I clinical trial failures [48] [49]. Traditional preclinical models, including static 2D in vitro assays and animal studies, often fail to accurately predict human outcomes due to their oversimplified physiology and interspecies differences [48] [50]. For instance, bioavailability correlations between common animal models and humans are notably weak (R²=0.25-0.37) [50].
Organ-on-a-Chip (OOC) and Microphysiological Systems (MPS) represent a paradigm shift, offering human-relevant, dynamic, and physiologically accurate models for ADME profiling. These microfluidic devices culture living human cells in 3D, perfused arrangements that mimic organ-level functions and tissue-tissue interfaces [51] [52]. By integrating multiple organ models, such as gut-liver systems, MPS enable the study of complex ADME processes in a holistic manner, providing a more reliable and human-predictive tool for lead optimization [48] [53].
Key Applications in ADME Optimization
Microphysiological Systems are being deployed to address specific challenges across the ADME spectrum. The table below summarizes their core applications in the context of lead optimization.
Table 1: Key Applications of MPS in ADME Lead Optimization
| Application Area | MPS Configuration | Key Advantage | Impact on Lead Optimization |
|---|---|---|---|
| Oral Bioavailability & First-Pass Metabolism | Gut-Liver MPS [48] [53] | Integrated intestinal absorption and hepatic metabolism in a single system. | Simultaneously determines fraction absorbed (Fa), gut extraction (Fg), and hepatic extraction (Fh) for accurate human bioavailability estimation [48]. |
| Metabolic Stability & Metabolite Identification | Liver-on-a-Chip [53] | Sustained, physiologically relevant CYP450 activity for weeks, enabling chronic dosing. | Identifies time-dependent inhibition, induction, and slow-forming metabolites early, de-risking candidates [53]. |
| Systemic Distribution & Multi-Organ Toxicity | Multi-Organ (e.g., 18-organ MPS) [53] | Measures drug and metabolite concentrations across multiple tissue compartments over time. | Informs PK/PD models and identifies organ-specific toxicity (e.g., DILI) by capturing systemic effects [53]. |
| Route-Specific Absorption | Lung-/Skin-Liver MPS [53] | Models barrier function and downstream metabolism for pulmonary/transdermal delivery. | Supports optimization of alternative administration routes beyond oral [53]. |
| Drug-Drug Interaction (DDI) Assessment | Gut-Liver MPS with primary cells [50] | Recapitulates human intestinal CYP metabolism often missing in Caco-2 models. | Improves DDI prediction for orally administered drugs by accounting for gut wall metabolism [50]. |
Experimental Protocol: Determining Oral Bioavailability Using a Gut-Liver MPS
This protocol details the use of a dual-organ Gut-Liver MPS, such as the CN Bio PhysioMimix platform, to estimate human oral bioavailability (F) during lead optimization [48].
Research Reagent Solutions and Essential Materials
Table 2: Essential Materials for Gut-Liver MPS Bioavailability Assay
| Item Name | Function/Description |
|---|---|
| PhysioMimix Bioavailability Assay Kit | An all-in-one kit containing the Gut/Liver MPS hardware, consumables, and assay protocols to recreate the dual-organ model [48]. |
| Primary Human Intestinal Epithelial Cells | Forms a polarized, differentiated intestinal barrier with relevant transporters and metabolic enzymes (e.g., CYPs) [50]. |
| Primary Human Hepatocytes | Provides physiologically relevant liver metabolism and clearance functions in a 3D microtissue format [48]. |
| Oxygen-Tolerant Co-culture Module | A specialized chip (e.g., polysulfone) that enables the co-culture of aerobic intestinal cells and anaerobic gut microbes [52]. |
| PhysioMimix Computational Modeling Tools | In silico tools for experimental design optimization and mechanistic modeling of pharmacokinetic parameters from MPS data [48] [54]. |
Step-by-Step Methodology
System Setup and Cell Seeding:
- Assemble the Gut-Liver MPS, typically consisting of two microfluidic chambers (gut and liver) separated by a porous, ECM-coated membrane and connected by microfluidic channels simulating blood flow [48] [52].
- Seed primary human intestinal epithelial cells (e.g., Caco-2 or primary colonocytes) onto the apical side of the membrane in the gut compartment. Culture under flow and cyclic mechanical strain (e.g., 10-15% stretch) to promote differentiation into villus-like structures and a functional barrier [52].
- Seed primary human hepatocytes into the liver compartment, where they self-aggregate into 3D microtissues under perfused flow, maintaining high metabolic function for several weeks [48] [53].
Tissue Validation and Compound Dosing:
- Prior to dosing, validate tissue viability and functionality. Confirm gut barrier integrity via transepithelial electrical resistance (TEER) and the presence of key transporters and CYPs. Assess liver functionality through albumin/urea production and CYP activity (e.g., midazolam 1'-hydroxylase activity) [48].
- Introduce the lead candidate compound(s) at a physiologically relevant concentration into the apical (gut lumen) inlet of the system to simulate oral administration [48].
Sample Collection and Analytical Monitoring:
- Collect effluent media from the "systemic" circulation outlet at multiple time points (e.g., over 72 hours) to establish a concentration-time profile for the parent drug and its metabolites [48].
- Analyze samples using standard analytical techniques such as LC-MS/MS to quantify the drug and its major metabolites [48] [7].
Data Analysis and Pharmacokinetic Modeling:
- Apply mechanistic computational models to the concentration-time data. These models, often based on Bayesian inference, are used to fit the data and extract key PK parameters [48] [54].
- The model outputs critical parameters such as apparent permeability (Papp), intrinsic hepatic clearance (CLint,liver), and intrinsic gut clearance (CLint,gut) [48].
- Calculate the components of oral bioavailability: the fraction absorbed (Fa), the fraction escaping gut metabolism (Fg), and the fraction escaping hepatic metabolism (Fh). The overall oral bioavailability (F) is the product: F = Fa × Fg × Fh [48].
Diagram 1: Gut-Liver MPS Experimental Workflow
Case Study: Midazolam Bioavailability Prediction
A peer-reviewed publication (Abbas et al., 2025) demonstrated the integrated workflow using midazolam, a well-characterized CYP3A4 substrate [48] [49].
- Experimental Summary: Midazolam was dosed into the gut compartment of the Gut-Liver MPS. Its concentration was monitored over 72 hours, showing absorption through the gut barrier, entry into the liver compartment, and extensive hepatic metabolism [48].
- Computational Modeling: A mathematical model was fitted to the experimental data, allowing the confident determination of key parameters: intrinsic hepatic clearance (CLint,liver), intrinsic gut clearance (CLint,gut), and apparent permeability (Papp) [48].
- Outcome: The model calculated the bioavailability components (Fa, Fg, Fh) for midazolam. The resulting prediction of its oral bioavailability fell within the clinically observed range in humans, validating the approach [48].
Integration with In Silico Tools and Future Outlook
The true power of MPS data is unlocked through integration with computational models. Data generated from MPS experiments are used to refine Physiologically Based Pharmacokinetic (PBPK) models, creating a synergistic loop that enhances human prediction [48] [53] [54]. This integration allows for:
- In vitro to in vivo extrapolation (IVIVE) to predict human pharmacokinetics [54].
- Simulation and optimization of MPS experiments in silico before wet-lab execution, saving time and resources [48].
- The development of "digital twins" for specific patient populations to explore the impact of physiology and genetics on drug exposure [53].
The regulatory landscape is increasingly favoring these human-relevant approaches. Initiatives like the US FDA's ISTAND pilot program, which accepted a Liver-Chip for qualification, and the FDA's plan to phase out animal testing requirements for some drug classes, are accelerating the adoption of MPS in formal drug development pipelines [53]. For lead optimization scientists, the strategic integration of MPS offers a path to more confident candidate selection, reduced attrition, and ultimately, safer and more effective medicines.
Drug Discovery Screening Workflow
The Role of Zebrafish as a Predictive In Vivo Model for Early ADME and Toxicity Screening
The integration of zebrafish into early drug discovery pipelines represents a significant advancement for ADME optimization and toxicity screening. This model serves as a powerful bridge between in vitro assays and mammalian in vivo studies, offering a unique combination of physiological relevance, medium-to-high throughput capacity, and cost-effectiveness [55] [56]. With approximately 70-82% of human disease-related genes having zebrafish orthologues and conserved ADME-related pathways, this vertebrate model provides critical functional insights into drug absorption, distribution, metabolism, and excretion within a whole-organism context during lead optimization [57] [58]. This application note details standardized protocols and strategic frameworks for leveraging zebrafish to derisk drug candidates, enhance prediction accuracy, and reduce attrition in preclinical development.
Lead optimization represents a critical decision-making phase where identified lead compounds are refined to improve their efficacy, pharmacokinetics, and safety profiles [57]. A primary objective during this stage is to establish favorable ADME characteristics while minimizing toxicological risks. Traditional approaches relying solely on in vitro systems often fail to account for complex systemic interactions, while mammalian in vivo studies are resource-intensive and low-throughput, creating a significant bottleneck in the drug discovery pipeline [56] [57].
The zebrafish model effectively addresses this gap by providing a whole-organism context with conserved vertebrate biology in a format amenable to larger-scale screening. Zebrafish embryos and larvae develop rapidly, with most organs, including a functional liver, kidney, digestive tract, and blood-brain barrier, fully formed by 5 days post-fertilization (dpf) [56] [57]. According to European Commission Directive 2010/63/EU, zebrafish are not regulated as animals until capable of independent feeding (around 120 hpf/5 dpf), facilitating their use in alignment with the 3Rs principles (Replacement, Reduction, and Refinement) [59] [56] [57].
Zebrafish Models for ADME and Toxicity Assessment: Core Advantages
Biological and Practical Relevance
- High Genetic Homology: Zebrafish share approximately 70-82% genetic homology with humans, including conservation of many drug-metabolizing enzymes such as cytochrome P450s and detoxification pathways [57] [58].
- Developmental Transparency: The optical transparency of embryos and larvae enables non-invasive, real-time observation of compound distribution, organ-specific effects, and developmental processes using fluorescent tagging techniques [55] [57].
- Scalability and Cost-Efficiency: A single pair can generate hundreds of embryos weekly, facilitating medium-to-high-throughput screening. Their small size allows housing in multiwell plates, significantly reducing compound requirements and costs compared to mammalian models [56] [60].
ADME-Specific Applications
Zebrafish provide a functional platform for evaluating key ADME parameters:
- Absorption: Capability to assess percutaneous, gastrointestinal, and gill absorption routes [59].
- Distribution: Real-time visualization of tissue penetration and blood-brain barrier permeability [57].
- Metabolism: Presence of conserved Phase I and II metabolic enzymes enables evaluation of metabolic stability and metabolite formation [57].
- Excretion: Functional renal and hepatic systems allow observation of clearance pathways [57].
Experimental Protocols and Standardized Methodologies
Zebrafish Husbandry and Ethical Considerations
Regulatory Framework Compliance
- Embryonic Stage Definition: Zebrafish are considered embryos until capable of independent feeding, typically at 120 hours post-fertilization (hpf) or 5 days post-fertilization (dpf) in European guidelines, and until 72 hpf/3 dpf (hatching) in some US guidelines [59] [56].
- Ethical Alignment: Research using zebrafish embryos <120 hpf aligns with 3Rs principles by replacing and reducing mammalian animal use [56] [57].
Husbandry Protocol
- Maintain adult zebrafish in recirculating systems at 28.5°C with a 14/10-hour light/dark cycle [56].
- Collect embryos through natural spawning, stage according to standard morphological criteria [60].
- Raise embryos in E3 embryo medium in incubators at 28.5°C until experimental use.
- Manually dechorionate embryos at 24-48 hpf if necessary for improved compound uptake [59].
General Compound Exposure and ADME Assessment Protocol
Compound Administration
- In-Water Dosing (Primary Method): Dilute test compounds directly in embryo medium, typically in 96-well or 48-well plates [56]. Suitable for high-throughput screening of compounds with good water solubility and absorption.
- Microinjection (Alternative Method): Inject compounds directly into the embryo's circulation, yolk, or specific tissues for poorly soluble compounds or precise dosing [59] [56].
ADME Evaluation Workflow
- Exposure Setup: Dispense 5-7 dpf larvae into multiwell plates (1 larva/well in 200-500 μL medium) [60].
- Compound Treatment: Add test compound at relevant concentrations (typically 1-100 μM range) alongside vehicle controls.
- Kinetic Sampling: Collect samples at multiple time points (e.g., 1, 6, 24 hours) for LC-MS/MS analysis to determine compound levels [56].
- Distribution Imaging: For fluorescent compounds, capture real-time images using fluorescence microscopy to visualize tissue distribution [57].
- Metabolite Profiling: Analyze samples for metabolite identification using mass spectrometry techniques [57].
Toxicity Screening Protocols
Comprehensive Toxicity Assessment (ZeGlobalTox Approach) This integrated protocol assesses multiple organ toxicities in the same larvae, reducing animal use and streamlining the pipeline [57].
Cardiotoxicity Screening
- Endpoint: Heart rate, rhythm, pericardial edema, circulation defects [60].
- Procedure:
- Expose 48-72 hpf embryos to test compounds for 24-48 hours.
- Anesthetize larvae with tricaine methane sulfonate.
- Quantify heart rate (beats/minute) under microscope at room temperature.
- Record arrhythmic events, pericardial area, and circulation quality.
- Validation: zERG potassium channel orthologue responds to QT-prolonging drugs, correlating with human cardiotoxicity concerns [60].
Hepatotoxicity Assessment
- Endpoint: Liver size, morphology, steatosis, necrosis [57].
- Procedure:
- Treat transgenic larvae (e.g., Tg(fabp10a:dsRed)) with compounds from 72-120 hpf.
- Fix larvae and stain with Oil Red O or similar lipophilic dyes for neutral lipids.
- Image livers using fluorescence and brightfield microscopy.
- Quantify liver size, intensity of steatosis staining, and morphological changes.
- Analysis: Compare treated groups to controls for significant increases in lipid accumulation indicative of steatosis [57].
Neurotoxicity Screening
- Endpoint: Behavioral changes, neuronal death, developmental defects [60].
- Procedure:
- Expose embryos from 24-120 hpf to test compounds.
- Assess locomotor activity using automated tracking systems.
- Score for touch response, spontaneous movement, and balance.
- Utilize transgenic lines (e.g., Tg(HuC:GFP)) to visualize neuronal integrity.
- Analysis: Quantify behavioral parameters and neuronal counts compared to controls.
Genotoxicity Evaluation
- Endpoint: Micronucleus formation, DNA damage [61].
- Procedure:
- Expose embryos to compounds during early development (24-72 hpf).
- Extract and stain erythrocytes from circulation.
- Score micronuclei frequency in peripheral blood cells.
- Apply comet assay to quantify DNA damage in specific tissues.
- Validation: Adapted from OECD Guideline 487, this model predicts carcinogenic potential [61].
Quantitative Data and Predictive Performance
Table 1: Comparative Toxicity Assessment of Doxorubicin Across Models
| Model System | Doxorubicin Dose | Key Toxicity Findings | Translational Correlation |
|---|---|---|---|
| Zebrafish Embryo-Larva | Varying concentrations | High doses: lethal effects; Low doses: sub-lethal effects, malformations, heart rate changes [60] | Predictive of human cardiotoxicity risk |
| Juvenile Mice | 5 weeks administration | Decline in cardiac systolic function, cardiomyocyte atrophy, myofiber disarray [60] | Direct correlation with human cardiac complications |
| Human Patients | 500 mg/m² cumulative | Cardiac complications in 4%-36% of treated patients [60] | Clinical outcome reference |
Table 2: Zebrafish Toxicity Screening Predictive Capacity
| Toxicity Type | Zebrafish Endpoint | Human Translation | Validation Level |
|---|---|---|---|
| Cardiotoxicity | Heart rate variability, zERG inhibition, pericardial edema | QT prolongation, arrhythmia risk, cardiomyopathy [60] | High correlation with clinical cardiotoxicity |
| Hepatotoxicity | Liver steatosis (fat accumulation), size reduction, necrosis | Drug-induced liver injury (DILI), hepatic steatosis [57] | Conserved pathophysiology |
| Neurotoxicity | Locomotor deficits, behavioral changes, neuronal cell death | Neurotoxic side effects, CNS toxicity [60] | Functional conservation |
| Developmental Toxicity | Teratogenic effects, organ malformations, growth retardation | Human teratogenic potential [60] | High predictivity for developmental liabilities |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Zebrafish ADME/Tox Screening
| Reagent/Resource | Function and Application | Specific Examples |
|---|---|---|
| Wild-type Strains | General toxicity and ADME screening | AB, Tübingen strains [56] |
| Transgenic Lines | Organ-specific visualization and assessment | Tg(fabp10a:dsRed) for liver, Tg(myl7:GFP) for heart, Tg(HuC:GFP) for neurons [57] [58] |
| Embryo Medium | Maintenance and compound dilution during experiments | E3 medium (5 mM NaCl, 0.17 mM KCl, 0.33 mM CaCl₂, 0.33 mM MgSO₄) [60] |
| Anesthetic Agents | Immobilization for imaging and precise assessment | Tricaine methane sulfonate (MS-222) [60] |
| Histological Stains | Tissue-specific staining and pathology detection | Oil Red O for lipids, acridine orange for apoptosis, o-dianisidine for erythrocytes [57] |
| Molecular Biology Kits | Gene expression analysis for mechanistic toxicology | RT-PCR kits for stress response markers (e.g., CYP450s, HSP70) [61] |
Integrated Workflow for Lead Optimization
Lead Optimization Screening Cascade
Zebrafish have firmly established their value as a predictive in vivo model for early ADME and toxicity screening within modern drug discovery pipelines. Their unique combination of physiological relevance, scalability, and compliance with 3Rs principles makes them particularly suited for the lead optimization stage, where critical decisions determine a compound's progression toward clinical development [56] [57]. The standardized protocols outlined in this application note provide a framework for generating robust, reproducible data that effectively bridges the gap between in vitro assays and mammalian testing.
Future advancements in zebrafish ADME/Tox screening will likely focus on improved quantification of plasma exposure levels, further characterization of drug-metabolizing enzyme conservation, and the development of more sophisticated disease models for targeted therapeutic areas [56]. As these refinements continue to enhance the model's predictive power, zebrafish are poised to play an increasingly central role in derisking drug candidates and improving the efficiency of the entire drug discovery process.
Solving Common ADME Challenges: Strategies for Poor Solubility, Permeability, and Rapid Metabolism
Overcoming the Weak Correlation Between Animal and Human Bioavailability
The oral bioavailability of a drug candidate is a pivotal parameter in lead optimization, directly influencing the dosing regimen and therapeutic potential. A core practice in preclinical development has been the use of animal data to forecast human bioavailability. However, an extensive analysis of 184 compounds from published literature has demonstrated that no strong or predictive correlations exist for all preclinical species, both individually and combined [62]. This weak correlation presents a significant risk, as it can lead to the wrong candidate selection, faulty dosing predictions for first-in-human studies, and ultimately, costly late-stage failures.
This application note provides a structured framework to overcome this challenge. By moving beyond simple, direct species-to-species extrapolation, we detail an integrated strategy that leverages in silico models, robust in vitro assays, and a mechanistic interpretation of in vivo pharmacokinetic (PK) data. The protocols herein are designed to be integrated into lead optimization research, enabling scientists to select compounds with the highest probability of demonstrating acceptable oral bioavailability in humans.
Integrated Strategy for Improved Bioavailability Prediction
A multi-faceted approach is required to de-risk the prediction of human oral bioavailability. The following workflow integrates complementary methodologies to build a holistic understanding of a compound's disposition, moving from simple predictions to complex, systems-wide models.
The following diagram illustrates this integrated, tiered strategy:
Experimental Protocols and Data Interpretation
This section provides detailed methodologies for key experiments that generate critical quantitative data for assessing absorption and metabolism properties.
TieredIn VitroADME Assessment
The following table summarizes the core in vitro assays recommended for early profiling, based on guidelines from the Assay Guidance Manual [13].
| Assay | Pharmacologic Question | Key Parameter(s) | Benchmark for Good Exposure | Protocol Summary |
|---|---|---|---|---|
| Lipophilicity [13] | Will the compound be stored in lipids or bind proteins? | Log D at pH 7.4 | Log D ~1-3 | "Shake-flask" method; compound dissolved in octanol/buffer (1:1), shaken 3 hours; LC-MS/MS measurement in each phase. |
| Aqueous Solubility [13] | What is the potential bioavailability? | Solubility (µM) at pH 7.4 | >50 µM | Compound incubated in buffer (pH 5.0, 6.2, 7.4) for 18 hours; UV spectrophotometry measurement vs. saturated propanol control. |
| Hepatic Microsome Stability [13] | How long will the parent compound circulate? | % Parent Remaining, Half-life (t½), Intrinsic Clearance (CL~int~) | <50% metabolized in 60 min | Compound incubated with liver microsomes (0.5 mg/mL) + NADPH; LC-MS/MS measurement of parent at t=0 and t=60 min. |
| Caco-2 Permeability [63] | Will the compound be absorbed in the intestine? | Apparent Permeability (P~app~) | P~app~ > 10 x 10⁻⁶ cm/s | Monolayers of Caco-2 cells grown on transwell inserts; compound added to donor well; concentration measured in receiver well over time. |
CriticalIn VivoPharmacokinetic Study Protocol
Objective: To determine absolute oral bioavailability and characterize the fundamental PK profile of a lead compound in a preclinical species (e.g., rat).
Study Design:
- Animals: Male Sprague-Dawley rats (n=3 per route of administration), cannulated.
- Formulation: Test compound in a standard vehicle (e.g., 10% DMSO, 40% PEG400, 50% PBS).
- Dosing:
- Intravenous (IV) Bolus: 1 mg/kg via the caudal vein.
- Oral Gavage (PO): 5 mg/kg via oral gavage.
- Serial Blood Sampling: Collect at pre-dose, 0.083 (IV only), 0.25, 0.5, 1, 2, 4, 6, 8, and 24 hours post-dose. Plasma is harvested via centrifugation.
- Bioanalysis: Plasma concentrations of the parent compound are quantified using a validated LC-MS/MS method.
Data Analysis:
- Non-Compartmental Analysis (NCA): Perform NCA using a validated software (e.g., Phoenix WinNonlin) to determine key PK parameters:
- AUC~0-inf~: Area under the plasma concentration-time curve from zero to infinity.
- C~max~: Maximum observed plasma concentration.
- t~max~: Time to reach C~max~.
- t~½~: Terminal elimination half-life.
- CL: Total body clearance.
- V~d~: Volume of distribution.
- Bioavailability (F) Calculation:
- F (%) = (AUC~PO~ / AUC~IV~) × (Dose~IV~ / Dose~PO~) × 100
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the described protocols relies on specific, validated reagents and models. The following table details key solutions [63] [13].
| Research Reagent / Material | Function in Bioavailability Assessment |
|---|---|
| Caco-2 Cell Line | A human colon adenocarcinoma cell line that, upon differentiation, forms a monolayer with tight junctions and expresses relevant transporters (e.g., P-gp). It is the gold-standard in vitro model for predicting human intestinal absorption. |
| Pooled Liver Microsomes | Subcellular fractions (typically human, rat, or dog) containing membrane-bound drug-metabolizing enzymes, including cytochrome P450s (CYPs). Used to assess metabolic stability and identify major metabolic pathways. |
| MDCK Cell Line | Madin-Darby Canine Kidney cells, often transfected with human transporters (e.g., MDR1). Used as an alternative, faster-growing model for permeability and transporter efflux studies. |
| Equilibrium Dialysis Device | A physical system (e.g., Teflon cells with semi-permeable membranes) used to separate protein-bound and unbound drug in plasma. This is critical for determining plasma protein binding and the free fraction of drug available for activity. |
| LC-MS/MS System | Liquid Chromatography coupled with Tandem Mass Spectrometry. The cornerstone analytical platform for the sensitive and specific quantification of drugs and their metabolites in complex biological matrices like plasma, urine, and bile. |
LeveragingIn Silicoand PBPK Modeling
To bridge the gap between preclinical data and human prediction, computational approaches are indispensable.
AI and Multitask Learning
Recent advances in in silico methods aim to overcome the limitations of small ADME datasets. Graph neural networks (GNNs) with multitask learning can predict multiple ADME parameters simultaneously, sharing information across tasks to improve accuracy [19]. Furthermore, explainable AI (XAI) techniques, such as Integrated Gradients (IG), can interpret the model's predictions and provide structural insights to guide chemists during lead optimization, highlighting which molecular features improve or worsen ADME properties [19].
Physiologically Based Pharmacokinetic (PBPK) Modeling
PBPK modeling represents the most advanced integrative approach. It incorporates in vitro data (e.g., permeability, metabolic clearance, protein binding) and compound physicochemical properties into a mathematical model that simulates the concentration-time profile in specific tissues and plasma [7].
The workflow for leveraging PBPK is as follows:
The power of PBPK lies in its ability to mechanistically extrapolate to humans by replacing the animal physiology with human physiology. This allows for the prediction of human oral absorption and bioavailability, the simulation of drug-drug interactions (DDI), and the impact of formulation, thereby de-risking the transition into clinical development [7].
The weak correlation between animal and human oral bioavailability is a well-documented reality in drug development [62]. However, this challenge can be effectively managed by adopting a holistic, mechanistic strategy that does not rely on direct extrapolation. By systematically integrating in silico predictions, robust in vitro ADME data, and carefully designed in vivo PK studies within a PBPK framework, researchers can significantly improve their ability to select lead compounds with a high probability of success in the clinic. This integrated approach transforms bioavailability assessment from a correlative gamble into a predictive science.
The optimization of Absorption, Distribution, Metabolism, and Excretion (ADME) properties represents a critical hurdle in modern drug discovery. Compounds with complex ADME characteristics can significantly challenge standard investigation methods, potentially derailing development programs if these properties are not adequately characterized and addressed. The implementation of integrated in vitro-in vivo-in silico strategies throughout the drug development process has proven effective in identifying and mitigating these risks while accelerating development timelines [64]. Risdiplam (Evrysdi), an orally bioavailable small molecule approved for the treatment of spinal muscular atrophy (SMA), serves as an exemplary case study of how sophisticated ADME characterization techniques can successfully navigate these challenges. This application note details the comprehensive ADME profiling strategies employed for risdiplam, providing researchers with validated protocols and frameworks applicable to other compounds presenting similar complex ADME properties.
Risdiplam Background and Therapeutic Significance
Risdiplam is the first approved, small-molecule survival of motor neuron 2 (SMN2) mRNA splicing modifier for the treatment of spinal muscular atrophy, a severe progressive neuromuscular disease caused by insufficient levels of functional SMN protein [64] [65]. Its mechanism of action involves binding to two sites in SMN2 pre-mRNA—the 5' splice site of intron 7 and the exonic splicing enhancer 2 of exon 7—thereby promoting inclusion of exon 7 during splicing and increasing production of functional SMN protein [65]. What makes risdiplam particularly noteworthy from an ADME perspective is its design to distribute into both the central nervous system and peripheral tissues while being amenable to oral administration, overcoming significant biological barriers that often limit therapeutic options for neurological disorders [66].
Table 1: Key Physicochemical and Pharmacokinetic Properties of Risdiplam
| Property | Value | Reference |
|---|---|---|
| Molecular Formula | C₂₂H₂₃N₇O | [65] |
| Molecular Weight | 401.474 g/mol | [65] |
| Protein Binding | ~89% (primarily to serum albumin) | [65] |
| Apparent Volume of Distribution (Vss) | 6.3 L/kg | [65] |
| Terminal Elimination Half-life | ~50 hours (healthy adults) | [65] |
| Oral Bioavailability | High (complete absorption) | [67] |
| Route of Elimination | Primarily hepatic metabolism | [67] [65] |
Key ADME Challenges and Profiling Strategies
The ADME characterization of risdiplam presented four primary challenges that required innovative methodological approaches beyond standard protocols. This section details these challenges and the corresponding experimental strategies implemented to address them.
Challenge 1: Predicting In Vivo Hepatic Clearance of a Low-Turnover Compound
Risdiplam is a low-turnover compound with low hepatic extraction (approximately 5%), making accurate prediction of its in vivo hepatic clearance particularly challenging using standard in vitro systems [64] [67]. Conventional hepatocyte and liver microsome assays often lack the sensitivity and physiological relevance needed for reliable extrapolation of low-clearance compounds.
Experimental Protocol 1: Hepatic Clearance Prediction
- Objective: To accurately predict the in vivo hepatic clearance of risdiplam by integrating data from multiple complementary systems.
- Materials:
- Cryopreserved human hepatocytes (pooled from at least 10 donors)
- Human liver microsomes (pooled from at least 50 donors)
- Williams' E medium with glutamine
- Risdiplam stock solution (10 mM in DMSO)
- Liquid chromatography-tandem mass spectrometry (LC-MS/MS) system
- Methodology:
- Hepatocyte Suspension Assay: Incubate risdiplam (1 µM) with human hepatocytes (0.5-1.0 million cells/mL) in Williams' E medium at 37°C under 5% CO₂.
- Liver Microsome Stability: Incubate risdiplam (1 µM) with human liver microsomes (0.5 mg protein/mL) in the presence of NADPH-regenerating system.
- Sample Collection: Withdraw samples at 0, 15, 30, 60, 90, and 120 minutes for hepatocyte assays and 0, 5, 15, 30, and 60 minutes for microsomal assays.
- Bioanalysis: Terminate reactions with acetonitrile containing internal standard. Determine risdiplam concentrations using a validated LC-MS/MS method.
- Data Analysis: Calculate intrinsic clearance (CLint) from the disappearance half-life (t₁/₂) using the following formula: CLint = (0.693 / t₁/₂) × (Volume of incubation / Number of cells or mg protein).
- In Vitro-In Vivo Extrapolation (IVIVE): Incorporate the observed in vitro CLint values into a physiologically based pharmacokinetic (PBPK) model that accounts for species-specific physiological parameters (liver blood flow, microsomal recovery, etc.).
- Key Consideration: For low-clearance compounds like risdiplam, the extended incubation duration (up to 4 hours) and use of pooled matrices from multiple donors are critical for obtaining reliable data.
Challenge 2: Elucidating Non-CYP450 Metabolic Pathways
Unlike most small-molecule drugs, risdiplam's metabolism is mediated primarily through a non-cytochrome P450 enzymatic pathway, specifically by flavin-containing monooxygenases (FMO1 and FMO3), with only minor contribution from CYP3A [64] [67] [65]. This required specialized approaches to identify the relevant enzymes and assess metabolite formation.
Experimental Protocol 2: Metabolism and Enzyme Phenotyping
- Objective: To identify the principal enzymes responsible for risdiplam metabolism and characterize the major circulating metabolites.
- Materials:
- Recombinant human FMO1, FMO3, CYP3A4, and other CYP enzymes
- Selective chemical inhibitors (e.g., itraconazole for CYP3A, methimazole for FMO)
- Human liver microsomes and hepatocytes
- Antibodies for enzyme inhibition
- LC-MS/MS system with high-resolution mass spectrometry capability
- Methodology:
- Reaction Phenotyping: Incubate risdiplam (1-10 µM) with individual recombinant human enzymes to identify which isoforms catalyze its metabolism.
- Chemical Inhibition: Incubate risdiplam with human liver microsomes in the presence and absence of selective enzyme inhibitors.
- Correlation Analysis: Incubate risdiplam with a panel of individual human liver microsomal samples with characterized enzyme activities and assess correlation between metabolite formation and specific enzyme activities.
- Metabolite Identification: Incubate risdiplam (10 µM) with human hepatocytes for 2-4 hours. Analyze samples using high-resolution LC-MS/MS to identify metabolite structures based on mass fragmentation patterns.
- Relative Activity Factor (RAF) Approach: Use RAF to scale the relative contribution of each enzyme pathway from recombinant systems to human liver microsomes.
- Key Findings: Application of this protocol confirmed that FMO3 mediates approximately 75% of risdiplam's metabolism, while CYP3A contributes approximately 20%, with the remaining 5% excreted renally as unchanged drug [67] [65]. The major circulating metabolite M1 was identified and found to be pharmacologically inactive [65].
Challenge 3: Tissue Distribution and CNS Penetration Assessment
As a treatment for a neuromuscular disease, risdiplam required thorough characterization of its distribution into both central nervous system and peripheral tissues, particularly its ability to bypass the blood-brain barrier.
Experimental Protocol 3: Tissue Distribution Profiling
- Objective: To quantify the extent of risdiplam distribution into central nervous system and peripheral tissues.
- Materials:
- Animal models (mice, rats, non-human primates)
- LC-MS/MS system
- In vitro transport assay kits (LLC-PK1, MDCKII cell lines)
- Quantitative whole-body autoradiography (QWBA) equipment
- Methodology:
- In Vitro Transport Assays: Conduct bidirectional transport assays using cell lines transfected with human MDR1 (multidrug resistance protein 1) and related transporters to assess whether risdiplam is a substrate for efflux transporters that would limit CNS penetration.
- In Vivo Tissue Distribution: Administer a single oral dose of risdiplam to animals and collect plasma, cerebrospinal fluid (CSF), brain, spinal cord, muscle, and other tissues at multiple time points.
- Sample Analysis: Homogenize tissues and analyze risdiplam concentrations using a validated LC-MS/MS method.
- Data Analysis: Calculate tissue-to-plasma ratios and determine the unbound partition coefficient (Kp,uu) for CNS compartments.
- Key Findings: These studies demonstrated that risdiplam distributes well into both CNS and peripheral tissues, with similar drug levels observed in plasma, muscle, and brain of preclinical species [66]. Critically, risdiplam was not a substrate for human MDR1, explaining its favorable CNS penetration [66]. The CSF-to-unbound plasma partition coefficient confirmed that risdiplam CSF levels reflected free compound concentration in plasma [66].
Challenge 4: Drug-Drug Interaction (DDI) Risk Assessment
The unique metabolic profile of risdiplam, being primarily cleared by FMO3 rather than CYP enzymes, necessitated a specialized approach to DDI risk assessment, particularly regarding potential interactions with CYP3A inhibitors/inducers and the impact of ontogeny on FMO3 activity in pediatric patients.
Experimental Protocol 4: DDI and Ontogeny Assessment
- Objective: To evaluate the DDI potential of risdiplam and assess the impact of ontogeny on its elimination in pediatric patients.
- Materials:
- Human liver microsomes and hepatocytes
- Selective CYP and FMO inhibitors/inducers
- Clinical data from healthy volunteers and patients
- PBPK modeling software
- Methodology:
- In Vitro Inhibition Screening: Incubate risdiplam with human liver microsomes in the presence of CYP-specific probe substrates to assess its potential to inhibit major CYP enzymes.
- Clinical DDI Study: Conduct a clinical study in healthy male volunteers using a two-period crossover design to evaluate the effect of the strong CYP3A inhibitor itraconazole on risdiplam pharmacokinetics [68].
- Mechanistic Population PK (Mech-PPK) Modeling: Integrate population PK and PBPK modeling approaches to estimate in vivo FMO3 ontogeny using data from subjects aged 2 months to 61 years [67].
- Simulation of Theoretical Substrates: Simulate DDI propensity for dual CYP3A-FMO3 substrates with varying metabolic fractions to extrapolate findings to other compounds.
- Key Findings: Itraconazole had only a minor effect on risdiplam plasma pharmacokinetics, confirming the low fraction metabolized by CYP3A [68]. Mech-PPK modeling revealed that FMO3 expression/activity is approximately threefold higher in children (peaking at age 2 years) compared to adults [67]. This informed dosing recommendations for pediatric patients and predicted comparable or decreased CYP3A-victim DDI propensity in children compared to adults for dual CYP3A-FMO3 substrates [67].
Table 2: Summary of Key ADME Challenges and Resolution Strategies for Risdiplam
| ADME Challenge | Standard Approach Limitations | Implemented Strategy | Key Outcome |
|---|---|---|---|
| Hepatic Clearance Prediction | Insensitive for low-turnover compounds | Integrated in vitro-in vivo-in silico approach with PBPK modeling | Accurate prediction of human clearance |
| Metabolic Pathway Identification | Bias toward CYP450 characterization | Comprehensive reaction phenotyping focusing on FMO pathways | Identification of FMO3 as primary clearance enzyme (75%) |
| Tissue Distribution | Limited CNS penetration for many compounds | In vitro transporter assays + in vivo tissue distribution studies | Confirmed favorable CNS and peripheral tissue distribution |
| DDI Risk Assessment | Focus on CYP-mediated interactions | Clinical DDI study + mechanistic modeling of FMO3 ontogeny | Low DDI risk and established pediatric dosing |
Visualization of Key Pathways and Workflows
Risdiplam ADME Characterization Workflow
Risdiplam Metabolic Pathways and DDI Risk
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Complex ADME Profiling
| Reagent/Assay System | Specific Example | Application in Risdiplam ADME | Functional Purpose |
|---|---|---|---|
| Cryopreserved Hepatocytes | Pooled human hepatocytes (≥10 donors) | Metabolic stability, metabolite profiling | Provides comprehensive phase I and II metabolic activity in physiologically relevant system |
| Recombinant Enzymes | Human FMO3, CYP3A4, other CYPs | Reaction phenotyping, enzyme kinetics | Identifies specific enzymes responsible for metabolism and their relative contributions |
| Transfected Cell Lines | LLC-PK1/MDCKII cells expressing human MDR1, BCRP | Transporter substrate and inhibition assays | Assesses potential for efflux transporter-limited distribution, particularly across blood-brain barrier |
| Selective Chemical Inhibitors | Itraconazole (CYP3A), methimazole (FMO) | Enzyme inhibition studies | Confirms involvement of specific metabolic pathways in in vitro systems |
| Human Liver Microsomes | Pooled from ≥50 donors | Intrinsic clearance determination, metabolic stability | Provides robust system for initial metabolic screening and clearance predictions |
| PBPK Modeling Software | GastroPlus, Simcyp Simulator | In vitro-in vivo extrapolation, DDI prediction, pediatric extrapolation | Integrates in vitro and physicochemical data to predict human PK and assess covariate effects |
Integrated Data Analysis and Application
The true power of the ADME characterization strategy employed for risdiplam lay in the integration of data across multiple experimental systems and the application of mechanistic modeling. The development of a robust PBPK model that incorporated in vitro clearance data, tissue distribution information, and the unique FMO3 ontogeny profile enabled accurate prediction of risdiplam pharmacokinetics across the diverse patient population, from infants to adults [64] [67]. This integrated approach verified that functional SMN protein increases measured in patient blood following risdiplam treatment reflected similar increases in functional SMN protein in the CNS, muscle, and other peripheral tissues [66], providing crucial validation of its mechanism of action across relevant tissue compartments.
Table 4: Critical ADME Parameters and Their Clinical Implications for Risdiplam
| ADME Parameter | Experimental Value | Clinical Implication | Impact on Development |
|---|---|---|---|
| Major Metabolic Pathway | FMO3 (75%), CYP3A (20%) | Low potential for CYP-mediated DDIs | Reduced need for extensive DDI screening studies |
| CNS Penetration | Kp,uu ~1, not an MDR1 substrate | Therapeutic concentrations achievable in CNS | Viable for treating neurological aspects of SMA |
| FMO3 Ontogeny | ~3x higher activity in children (peak at 2 years) | Higher clearance in pediatric patients | Informed age-based dosing strategies |
| Oral Bioavailability | High (>90%) with low hepatic extraction | Consistent exposure with once-daily dosing | Convenient outpatient administration |
| Elimination Half-life | ~50 hours (adults) | Suitable for once-daily dosing | Improved patient compliance |
The comprehensive ADME characterization of risdiplam exemplifies how innovative, integrated approaches can successfully address complex pharmacokinetic challenges throughout drug development. The case study demonstrates that for compounds presenting non-standard ADME properties—such as predominant metabolism by non-CYP450 enzymes, low hepatic clearance, or requirement for tissue-specific distribution—tailored experimental strategies combined with mechanistic modeling can effectively de-risk development and support regulatory approval. The protocols detailed in this application note provide a validated framework that researchers can adapt for other compounds with challenging ADME profiles, potentially accelerating their development while maintaining scientific rigor. The successful translation of these approaches for risdiplam, culminating in its approval for SMA patients across a wide age range, underscores the critical value of sophisticated ADME optimization in modern drug discovery.
Structural Modification Strategies to Improve Peptide Developability
Peptide therapeutics represent a rapidly growing class of pharmaceuticals, bridging the gap between small molecules and biologics, with over 80 FDA-approved compounds and a market exceeding $50 billion [26]. Despite their high specificity and potency, peptide drug development faces significant Absorption, Distribution, Metabolism, and Excretion (ADME) challenges that must be addressed during lead optimization [25] [26]. Natural peptides typically exhibit poor ADME properties, including rapid clearance, short half-life, low permeability, and sometimes low solubility [25]. Most peptides demonstrate less than 1% oral bioavailability due to enzymatic degradation in the gastrointestinal tract and limited permeability across cell membranes [25] [26]. Furthermore, unmodified peptides usually have short half-lives (e.g., minutes) resulting from extensive proteolysis in blood, kidneys, and liver, coupled with rapid renal clearance [25]. This application note details structural modification strategies and experimental protocols to overcome these challenges and improve peptide developability within lead optimization research.
Strategic Approaches to Peptide Optimization
Key Structural Modification Strategies
Multiple chemical modification strategies have been developed to address the inherent ADME limitations of peptide therapeutics. These approaches enhance metabolic stability, membrane permeability, and pharmacokinetic profiles while maintaining target binding affinity.
Table 1: Structural Modification Strategies for Peptide ADME Optimization
| Strategy | Mechanism of Action | ADME Benefits | Clinical Examples |
|---|---|---|---|
| Terminal Capping [69] | Acetylation (N-terminal) or amidation (C-terminal) | Reduces exopeptidase degradation; improves metabolic stability | Various research peptides |
| D-Amino Acid Substitution [26] [69] | Incorporates mirror-image amino acids | Disrupts protease recognition; enhances metabolic stability | Leuprolide [26] |
| Cyclization [26] [69] | Forms cyclic backbone via side-chain or terminal linkages | Eliminates N-/C-termini vulnerable to exopeptidases; improves stability & affinity | Cyclosporin A [26] |
| PEGylation [26] | Covalent attachment of polyethylene glycol chains | Increases hydrodynamic radius; reduces renal clearance & provides steric protection | PEGylated peptide drugs |
| Lipidation/Fatty Acid Modification [26] | Incorporation of fatty acid chains | Enhances albumin binding; slows release and extends half-life | Liraglutide, Semaglutide [26] |
| Backbone Modification [69] | N-methylation or α-methylation of amino acids | Reduces protease susceptibility and hydrogen bonding capacity | Various research peptides |
| Unnatural Amino Acid Incorporation [70] [69] | Substitution with synthetic amino acid analogs | Enhances proteolytic resistance and modulates physicochemical properties | Peptide drug candidates |
Residue-Specific Modification Guidance
Strategic modifications target specific amino acid residues to address metabolic soft spots while maintaining pharmacological activity.
Table 2: Residue-Specific Modification Approaches
| Residue Type | Modification Approaches | Key Considerations |
|---|---|---|
| N- & C-Termini [69] | N-terminal acetylation; C-terminal amidation; steric blocking | Protects against aminopeptidases and carboxypeptidases |
| Metabolically Unstable Residues [69] | Alanine scanning; D-amino acid substitution; unnatural amino acid analogs | Identify critical residues via SAR studies; replace labile residues |
| Cysteine (Cys) [71] | Conjugate addition with stabilized Michael acceptors; transition metal-catalyzed arylation | Low pKa (~8.3) and high nucleophilicity enable selective derivatization |
| Methionine (Met) [71] | Redox-Activated Chemical Tagging (ReACT) with oxaziridines | Alkylation under acidic conditions; formation of stable sulfimide conjugates |
| Tyrosine (Tyr) [71] | Ene-type reactions; diazonium couplings; Mannich-type condensations | Reactivity pH-dependent (phenol pKa ~10); diverse carbon-electrophile reactions |
| Tryptophan (Trp) [71] | Metal-catalyzed C-H functionalization; organoradical conjugation | Modifications often target indole C-2 position; metal-based methods prevalent |
Experimental Protocols for Peptide Optimization
Computational Optimization Protocol for Modified Peptides
The mPARCE protocol provides an iterative computational pipeline for optimizing peptide binding affinity through incorporation of non-natural amino acids (NNAAs) [70].
PROTOCOL 1: Computational Peptide Optimization Using mPARCE
Purpose: To optimize peptide binding affinity through single-point mutations using non-natural amino acids while improving developability properties.
Input Requirements:
- 3D structure of protein-peptide complex (PDB format recommended)
- Parameter files for natural and non-natural amino acids
- Structural or SAR guidance for mutation prioritization (optional)
Workflow Steps:
- Parameterization of Non-Natural Amino Acids:
- Curate list of NNAAs from databases (e.g., BIOLIP, Chemical Component Dictionary)
- Filter NNAAs by molecular weight (<300 Da recommended) and physicochemical properties
- Generate Rosetta parameter files using rdkit-to-params package and molfiletoparams_polymer.py
System Preparation:
- Protonate protein-peptide complex structure considering physiological pH
- Define mutation positions based on structural knowledge or alanine scanning data
Iterative Mutation and Sampling:
- Perform single-point mutations using Monte Carlo sampling
- Apply Backrub sampling method (20,000 trials recommended, kT=1)
- Generate multiple conformational states for each mutant
Binding Affinity Assessment:
- Calculate consensus score using multiple scoring functions (DLigand2, Vina, Cyscore, NNscore, Rosetta docking score, Rosetta relaxation score)
- Accept mutations when ≥4 scoring functions agree on favorable binding improvement
Candidate Prioritization:
- Rank accepted sequences by consensus score improvement
- Apply property-based filtering (hydrophobicity, charge, size)
- Select top candidates for experimental validation
Validation: Benchmark against known protein-peptide complexes with experimental affinity data [70].
In Vitro ADME Profiling Cascade for Peptides
A tiered experimental approach provides comprehensive ADME assessment during peptide lead optimization.
PROTOCOL 2: Tiered In Vitro ADME Profiling for Peptides
Purpose: To identify key ADME liabilities and guide rational peptide design through systematic in vitro testing.
Phase I: Preliminary Solubility and Stability
- Solubility Assessment:
- Measure equilibrium solubility in phosphate buffer (pH 7.4)
- Use low-binding plates and tips to minimize adsorption
- Quantify via HPLC-UV/MS with appropriate detection methods
- Biorelevant Gastrointestinal Stability:
- Incubate in simulated gastric fluid (FaSSGF) and intestinal fluid (FaSSIF)
- Include digestive enzymes (pepsin for gastric, pancreatin for intestinal)
- Sample at timepoints (0, 15, 30, 60, 120 min) and analyze by LC-MS
- Calculate half-life and percent remaining
Phase II: Metabolic Stability Profiling
- Plasma Stability:
- Incubate in multiple species plasma (human, rat, mouse, dog)
- Add protease inhibitors to control matrices as needed
- Use low-binding containers and consider adding BSA to maintain sink conditions
- Determine degradation half-life and identify metabolites
- Tissue Metabolic Stability:
- Test in liver S9 fractions, microsomes, and lysosomes
- Include intestinal S9 fractions and kidney microsomes
- Assess interspecies differences for human translation
- Identify metabolic soft spots for further stabilization
Phase III: Permeability Assessment
- Cellular Permeability:
- Utilize Caco-2 or MDCK cell monolayers
- Add protease inhibitors to cell media to minimize degradation
- Measure apparent permeability (Papp) in both directions (A-B, B-A)
- Calculate efflux ratio for transporter identification
- Permeation Enhancer Evaluation:
- Test compounds with permeation enhancers (e.g., Sodium Caprate)
- Optimize enhancer concentration for efficacy and toxicity balance
- Assess compound-specific enhancement effects
Data Integration: Develop structure-ADME relationships to guide further chemical optimization [26].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Peptide ADME Optimization
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Low-Binding Plates & Tips [25] | Minimize peptide adsorption to surfaces during assays | Essential for accurate quantification of low-concentration peptides |
| Protease Inhibitor Cocktails [25] | Inhibit enzymatic degradation during permeability and stability assays | May include aprotinin, AEBSF, bestatin; concentration optimization required |
| Simulated Gastric/Intestinal Fluids [26] | Evaluate digestive stability under physiologically relevant conditions | Include with/without digestive enzymes to assess specific liabilities |
| Caco-2 Cell Line [25] [26] | Assess intestinal permeability and transporter effects | Expresses human intestinal transporters (PEPT1, SMVT); 21-day differentiation |
| Bovine Serum Albumin (BSA) [25] | Create sink conditions in receiver wells; minimize nonspecific binding | Helps maintain peptide solubility and reduces surface adsorption |
| Rosetta Software Suite [70] | Computational peptide design and binding affinity prediction | Requires parameterization of non-natural amino acids; steep learning curve |
| SPR Chips (CM5) [27] | Direct measurement of target binding affinity and kinetics | Immobilize full-length target or specific binding domains separately |
| Transwell Filter Systems [25] | Permeability assessment in cell-based models | Pore size selection critical (0.4-3.0μm); collagen coating may be required |
| Human & Animal Matrices [26] | Metabolic stability assessment in biologically relevant systems | Include plasma, liver S9, kidney microsomes for comprehensive profiling |
| Permeation Enhancers (e.g., C10) [26] | Increase membrane permeability for challenging peptides | Effects are compound-dependent; require careful optimization |
Workflow Visualization
Diagram 1: Peptide ADME Optimization Workflow
Diagram 2: Tiered In Vitro ADME Profiling Cascade
Strategic structural modification combined with comprehensive ADME profiling enables researchers to overcome the inherent developability challenges of peptide therapeutics. The integration of computational design tools like mPARCE with tiered experimental testing cascades provides a systematic framework for peptide optimization. By applying terminal protection, cyclization, D-amino acid substitution, and other chemical strategies, researchers can significantly improve metabolic stability, permeability, and pharmacokinetic properties. The protocols and methodologies detailed in this application note offer a roadmap for advancing peptide leads into viable development candidates with optimized ADME characteristics, ultimately accelerating the discovery of effective peptide therapeutics for diverse disease areas.
Navigating Drug-Drug Interactions (DDI) and ICH M12 Guidance
The International Council for Harmonisation (ICH) M12 guideline on drug interaction studies represents a major advancement in global regulatory harmonization for evaluating drug-drug interactions (DDIs) during pharmaceutical development [72] [73]. Finalized in May 2024 and subsequently adopted by regulatory agencies including the FDA, EMA, and China's NMPA, this guideline provides consistent recommendations for the design, conduct, and interpretation of enzyme- or transporter-mediated pharmacokinetic DDI studies [74]. For researchers engaged in lead optimization, understanding and implementing ICH M12 is crucial for efficient ADME (Absorption, Distribution, Metabolism, and Excretion) optimization, as it establishes standardized frameworks for assessing DDI liability early in development, thereby reducing late-stage attrition due to unforeseen interaction risks [73] [10].
The guideline primarily addresses the development of small chemical molecules and provides limited consideration for biologics such as monoclonal antibodies and antibody-drug conjugates [72] [75]. A significant outcome of the harmonization process is the updated terminology, replacing previously used terms "victim" and "perpetrator" drugs with the more scientifically neutral "object drug" (substrate) and "precipitant drug" (inhibitor or inducer) to facilitate clearer global communication [75] [74]. The implementation of ICH M12 supersedes previous regional guidelines, including the EMA Guideline on the investigation of drug interactions, though some region-specific aspects regarding gastrointestinal interactions may be supplemented by additional documents [72] [76].
Key Updates in ICH M12 and Implications for Lead Optimization
Critical Technical Updates
ICH M12 introduces several substantive technical revisions that directly impact how ADME properties should be evaluated during lead optimization. These updates provide more precise criteria for translating in vitro findings to clinical DDI risk, enabling medicinal chemists to make better-informed decisions during structural optimization.
- Protein Binding Assessment: The guideline now explicitly allows the use of measured unbound fraction (fu) for highly protein-bound drugs (≥99.9%) in basic static models, provided validated assay methods are used [75] [74]. This enables more accurate DDI risk prediction for highly lipophilic compounds common in early discovery.
- Time-Dependent Inhibition (TDI) Methods: ICH M12 formally recognizes both dilution and non-dilution methods for TDI assessment [74]. Recent comparative studies indicate the non-dilution method may provide higher prediction accuracy with less microsome consumption, making it particularly valuable for high-throughput screening during lead optimization [74].
- Metabolite DDI Assessment: The guideline strengthens requirements for evaluating pharmacologically active metabolites, specifying that metabolites contributing ≥25% of parent AUC and ≥10% of total drug-related material in circulation should be assessed for enzyme inhibition potential [75] [74].
Comparison with Previous Regional Guidelines
Table 1: Key Differences Between ICH M12 and Previous Regional Guidelines
| Assessment Area | ICH M12 | Previous FDA Guideline | Previous EMA Guideline |
|---|---|---|---|
| Enzyme Phenotyping | Recommends using both HLM with inhibitors AND recombinant enzymes | Stated sponsors "should use both methods" | Less specific on methodological requirements |
| TDI Risk Threshold | Basic static model: R-value ≥1.1 (further evaluation); ≥1.25 (clinical study needed) | Different cutoff values | Different cutoff values |
| CYP Induction Concentration | 50× Cmax,u for basic mRNA approach | 50× Cmax,u | 50× Cmax,u |
| Transporter Cut-off Values | Harmonized values between previous FDA and EMA | Region-specific values | Region-specific values |
| Metabolite Assessment | Detailed criteria for when to assess metabolites | Less specific guidance | Less specific guidance |
Experimental Framework for Enzyme-Mediated DDI Assessment
The following section provides detailed protocols for evaluating enzyme-mediated DDIs during lead optimization, aligned with ICH M12 recommendations.
Enzyme Reaction Phenotyping
Objective: Identify specific cytochrome P450 (CYP) enzymes responsible for the metabolism of an investigational drug to predict potential DDIs when co-administered with inhibitors or inducers of these pathways [74].
Protocol:
Materials and Reagents:
- Test compound (10 mM stock solution in DMSO)
- Pooled human liver microsomes (HLM) (0.5 mg/mL final protein concentration)
- Selective chemical inhibitors: Furafylline (CYP1A2), Montelukast (CYP2C8), Sulfaphenazole (CYP2C9), (+)-N-3-Benzylnirvanol (CYP2C19), Quinidine (CYP2D6), Ketoconazole (CYP3A)
- NADPH regenerating system (1.3 mM NADP+, 3.3 mM glucose-6-phosphate, 0.4 U/mL glucose-6-phosphate dehydrogenase, 3.3 mM magnesium chloride)
- Recombinant CYP enzymes (rCYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6, 3A4)
- Stop solution: Acetonitrile with internal standard
- LC-MS/MS system for analysis
Experimental Procedure:
- Prepare incubation mixtures containing HLM (0.5 mg/mL) in 100 mM potassium phosphate buffer (pH 7.4)
- Add selective chemical inhibitors at established isoform-specific concentrations
- Pre-incubate for 5 minutes at 37°C
- Initiate reactions by adding NADPH regenerating system
- Incubate for appropriate time (typically 10-45 minutes) based on metabolic stability data
- Terminate reactions with ice-cold acetonitrile
- Centrifuge at 3000×g for 10 minutes and analyze supernatant by LC-MS/MS
- Conduct parallel incubations with recombinant CYP enzymes
Data Analysis:
- Calculate percentage inhibition for each chemical inhibitor compared to control
- Determine relative contribution of each rCYP enzyme to total metabolism
- Consider metabolism ≥25% of total by a single enzyme as clinically relevant
Decision Criteria:
- If CYP3A contributes ≥25% to total clearance, clinical DDI studies with strong CYP3A inhibitors/inducers are recommended
- For other CYPs (1A2, 2C9, 2C19, 2D6), clinical DDI studies are recommended if they contribute ≥25% to total clearance
Diagram 1: Enzyme Reaction Phenotyping Workflow
Cytochrome P450 Reversible Inhibition
Objective: Assess the potential of an investigational drug to reversibly inhibit major CYP enzymes, which could cause increased exposure of co-administered drugs metabolized by these pathways [13] [74].
Protocol:
Materials and Reagents:
- Test compound (serial dilutions in DMSO, final concentration typically 0.1-100 μM)
- Isoform-specific probe substrates: Phenacetin (CYP1A2), Bupropion (CYP2B6), Amodiaquine (CYP2C8), Diclofenac (CYP2C9), S-Mephenytoin (CYP2C19), Dextromethorphan (CYP2D6), Midazolam or Testosterone (CYP3A4)
- Pooled human liver microsomes (0.1-0.2 mg/mL final protein concentration)
- NADPH regenerating system
- LC-MS/MS system for metabolite quantification
Experimental Procedure:
- Prepare incubation mixtures containing HLM and test compound at various concentrations
- Pre-incubate for 5 minutes at 37°C
- Add isoform-specific probe substrate at concentration ≈ Km
- Initiate reaction with NADPH regenerating system
- Incubate for linear reaction time (typically 5-30 minutes)
- Terminate reactions with ice-cold acetonitrile
- Centrifuge and analyze metabolite formation by LC-MS/MS
Data Analysis:
- Plot percentage remaining enzyme activity versus test compound concentration
- Calculate IC50 values using nonlinear regression
- Determine Ki values using Cheng-Prusoff equation if reversible inhibition mode is established
- Calculate Cmax,u/Ki,u ratio using unbound Cmax
Decision Criteria:
- Cmax,u/Ki,u ≥ 0.02: Proceed to clinical DDI study
- 0.1 > Cmax,u/Ki,u ≥ 0.02: Consider PBPK modeling
- Cmax,u/Ki,u < 0.02: No clinical DDI study recommended
Table 2: CYP Reversible Inhibition Decision Criteria Based on ICH M12
| Cmax,u/Ki,u Ratio | Clinical DDI Recommendation | Required Action |
|---|---|---|
| < 0.02 | Low inhibition potential | No clinical DDI study needed |
| 0.02 - 0.1 | Moderate inhibition potential | Consider PBPK modeling to assess need for clinical study |
| ≥ 0.1 | High inhibition potential | Clinical DDI study recommended |
Time-Dependent Inhibition (TDI) Assessment
Objective: Evaluate whether an investigational drug causes irreversible or quasi-irreversible inhibition of CYP enzymes, which may lead to more profound and prolonged DDIs than reversible inhibition [74].
Protocol:
Materials and Reagents:
- Test compound (serial dilutions in DMSO)
- Pooled human liver microsomes
- NADPH regenerating system
- Isoform-specific probe substrates (as in reversible inhibition)
- Positive control TDI inhibitors: Furafylline (CYP1A2), Ticlopidine (CYP2B6, 2C19), Gemfibrozil 1-O-β-glucuronide (CYP2C8), Tienilic Acid (CYP2C9), Paroxetine (CYP2D6), Verapamil (CYP3A)
Experimental Procedure (Dilution Method):
- Primary incubation: HLM + test compound/control + NADPH (30 min)
- Dilute primary incubation 10-fold into secondary incubation containing probe substrate
- Incubate secondary mixture for predetermined linear time
- Terminate reaction and analyze metabolite formation
- Include control without NADPH to distinguish TDI from reversible inhibition
Experimental Procedure (Non-dilution Method):
- Pre-incubate HLM with test compound and NADPH for 30 minutes
- Add probe substrate directly without dilution
- Incubate for linear reaction time
- Terminate and analyze as above
Data Analysis:
- Calculate IC50 shift ratio: IC50 (-NADPH) / IC50 (+NADPH)
- Alternatively, determine TDI parameters Kinact and KI through kinetic modeling
- Calculate R-value using basic static model
Decision Criteria:
- IC50 shift ratio ≥ 1.5 or R-value ≥ 1.1: Proceed to further evaluation
- R-value ≥ 1.25: Usually requires a clinical DDI study
Research Reagent Solutions for DDI Assessment
Table 3: Essential Research Reagents for ICH M12-Compliant DDI Studies
| Reagent Category | Specific Examples | Function in DDI Assessment |
|---|---|---|
| Human Liver Microsomes | Pooled HLM (50-donor recommended) | Provides complete CYP enzyme system for metabolism and inhibition studies |
| Recombinant CYP Enzymes | rCYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6, 3A4 | Enzyme phenotyping to identify specific CYP isoforms involved in drug metabolism |
| Selective Chemical Inhibitors | Furafylline (CYP1A2), Quinidine (CYP2D6), Ketoconazole (CYP3A) | Selective inhibition of specific CYP isoforms in reaction phenotyping studies |
| Isoform-Specific Probe Substrates | Phenacetin (CYP1A2), Bupropion (CYP2B6), Diclofenac (CYP2C9), Midazolam (CYP3A) | Substrates with known metabolic pathways for enzyme inhibition assays |
| Positive Control Inhibitors/Inducers | Ketoconazole (CYP3A inhibition), Rifampin (CYP3A induction) | Assay validation and quality control |
| Transporter-Expressing Cells | OATP1B1/1B3, OCT2/MATE1, BCRP-transfected cell lines | Assessment of transporter-mediated DDIs |
| Cryopreserved Hepatocytes | Freshly isolated or plateable cryopreserved human hepatocytes | CYP induction studies and integrated metabolism assessment |
Integrated DDI Risk Assessment Strategy for Lead Optimization
Implementing a systematic DDI risk assessment strategy during lead optimization enables efficient identification and mitigation of interaction risks before candidate selection. The following workflow integrates ICH M12 recommendations into a practical framework for medicinal chemists and DMPK scientists.
Diagram 2: Integrated DDI Risk Assessment in Lead Optimization
Tiered Testing Approach
A tiered testing strategy ensures efficient resource allocation during lead optimization while comprehensively addressing ICH M12 requirements:
Tier 1 - Rapid Screening:
- Metabolic stability in liver microsomes
- CYP reversible inhibition at single high concentration (10 μM)
- High-throughput solubility and permeability assessment
Tier 2 - Mechanistic Studies:
- Enzyme reaction phenotyping for compounds with significant metabolism
- IC50 determination for compounds showing >50% inhibition in Tier 1
- TDI assessment for compounds with CYP3A, 1A2, or 2C19 metabolism/inhibition
Tier 3 - Comprehensive Profiling:
- CYP induction assessment in human hepatocytes
- Transporter inhibition and substrate studies
- Metabolite identification and DDI assessment
- PBPK model development for complex DDI predictions
Structural Modification Strategies to Mitigate DDI Risk
When DDI assessment identifies unacceptable interaction risks, the following structural modification strategies can be employed during lead optimization:
Reducing Metabolic CYP Liability:
- Introduce metabolically stable motifs to shift clearance from CYP-mediated oxidation to direct conjugation or non-CYP pathways
- Block sites of metabolism on aromatic rings through halogen substitution or steric hindrance
- Reduce lipophilicity (LogD) to decrease affinity for CYP active sites
Minimizing Enzyme Inhibition:
- Introduce ionizable groups to reduce lipophilicity and membrane permeability, decreasing access to CYP active sites
- Modify structural features known to confer mechanism-based inhibition (e.g., terminal acetylenes, methylenedioxyphenyl groups)
- Reduce planarity and molecular size to decrease tight binding to CYP enzymes
Managing Enzyme Induction:
- Avoid structural features known to activate pregnane X receptor (PXR), such as certain heterocycles with specific substitution patterns
- Reduce lipophilicity, as high LogD correlates with increased PXR activation potential
The implementation of ICH M12 provides a harmonized global framework for DDI assessment that should be integrated throughout the lead optimization process. By employing the experimental protocols and risk assessment strategies outlined in this document, researchers can systematically identify and mitigate DDI liabilities while optimizing ADME properties. The standardized criteria and updated methodological recommendations in ICH M12 enable more accurate prediction of clinical DDI risks from in vitro data, facilitating the selection of drug candidates with lower potential for clinically significant interactions. As the pharmaceutical industry continues to develop increasingly complex molecules, adherence to these harmonized guidelines will be essential for efficient global drug development.
Enhancing Oral Bioavailability for Challenging Modalities like PROTACs
Proteolysis-Targeting Chimeras (PROTACs) represent a groundbreaking class of heterobifunctional molecules that hijack the ubiquitin-proteasome system to induce targeted protein degradation [77] [78]. Unlike conventional small molecules that operate via an occupancy-driven mechanism, PROTACs function through an event-driven mechanism, catalyzing the destruction of target proteins without requiring sustained binding [77]. This unique mode of action provides significant advantages, including the ability to target proteins previously considered "undruggable" and exhibiting high potency at low concentrations due to their catalytic nature [77] [78].
Despite their therapeutic potential, PROTACs face substantial challenges in achieving oral bioavailability, primarily due to their physicochemical properties that place them firmly in the beyond-Rule-of-5 (bRo5) chemical space [77] [79]. The Lipinski Rule of Five (Ro5) guidelines suggest that compounds are more likely to have poor absorption or permeation when they exceed certain thresholds: molecular weight (MW) > 500 Da, calculated log P > 5, hydrogen bond donors (HBD) > 5, and hydrogen bond acceptors (HBA) > 10 [77]. Typical PROTACs exhibit molecular weights between 700-1200 Da, high polar surface area, numerous rotatable bonds, and poor aqueous solubility, creating multiple barriers to oral absorption including limited intestinal permeability, extensive first-pass metabolism, and formulation challenges [77] [15] [79].
Table 1: Physicochemical Property Guidelines for Orally Bioavailable PROTACs
| Property | Recommended Range for Oral PROTACs | Traditional Rule of 5 Limits |
|---|---|---|
| Molecular Weight | ≤ 950-1000 Da [15] | ≤ 500 Da |
| Hydrogen Bond Donors (HBD) | ≤ 2-3 [15] | ≤ 5 |
| Hydrogen Bond Acceptors (HBA) | ≤ 15 [15] | ≤ 10 |
| Rotatable Bonds | ≤ 12-14 [15] | ≤ 10 |
| Topological Polar Surface Area (TPSA) | ≤ 200 Ų [15] | Not specified |
| Chromatographic log D | ≤ 7 [15] | log P ≤ 5 |
Strategic Framework for Optimizing Oral Bioavailability
Molecular Design Strategies
Linker Optimization: The linker represents the most flexible component of PROTAC architecture and serves as a primary focus for optimization. Strategic modifications include changing linker length, altering anchor points, employing cyclic linkers, and reducing amide motifs to improve metabolic stability and cellular permeability [77] [78]. Research demonstrates that replacing PEG linkers with 1,4-disubstituted phenyl rings significantly enhances cellular permeability, while incorporating alkyl chains with basic nitrogen atoms can improve solubility [77].
E3 Ligase Selection: The choice of E3 ligase ligand profoundly influences PROTAC properties. CRBN-based PROTACs generally exhibit superior "oral drug-like" qualities compared to VHL-targeted counterparts due to their smaller molecular weight and more favorable physicochemical properties [77] [78]. The first PROTAC molecules to enter clinical trials (ARV-110 and ARV-471) both utilize CRBN E3 ligase, highlighting its preference for orally administered candidates [77] [78].
Intramolecular Hydrogen Bonding: Introducing intramolecular hydrogen bonds represents a sophisticated strategy to enhance membrane permeability by reducing effective molecular size and polarity [77] [78]. This approach facilitates the transformation of extended "strip-type" conformations into more compact "ball" forms that can transition between polar (aqueous environment) and non-polar (membrane environment) states, improving cellular uptake [77].
Prodrug Approaches and Formulation Strategies
Prodrug Strategy: Converting PROTACs to prodrugs through chemical modification of pharmacologically active compounds can dramatically improve oral bioavailability [77] [78]. For instance, adding lipophilic groups to CRBN ligands has demonstrated significant increases in bioavailability despite concerns about further increasing molecular weight [77]. This approach protects vulnerable functional groups from metabolism and enhances permeability through the gastrointestinal barrier.
Food Effect Utilization: Clinical protocols for advanced PROTAC candidates specify administration "with food" to leverage the enhanced solubility in fed-state intestinal conditions [77] [78]. The presence of food stimulates bile salt secretion, creating a biorelevant buffer (FeSSIF) that improves PROTAC solubility and dissolution, ultimately leading to better systemic exposure [77].
Table 2: Key Optimization Strategies for Oral PROTAC Development
| Strategy | Mechanism of Action | Experimental Evidence |
|---|---|---|
| Linker Optimization | Improves metabolic stability and cellular permeability | Replacing PEG with 1,4-disubstituted phenyl rings significantly improved cellular permeability [77] |
| CRBN E3 Ligase Selection | Reduces molecular weight and improves drug-like properties | CRBN-based PROTACs ARV-110 and ARV-471 advanced to clinical trials with oral administration [77] [78] |
| Intramolecular H-Bonding | Creates chameleonic properties that adapt to different environments | Transformation from strip-type to ball-type conformation improves membrane permeability [77] |
| Prodrug Approach | Enhates permeability and protects from metabolism | Adding lipophilic group to CRBN ligand increased bioavailability in experimental models [77] [78] |
| Administration with Food | Improves solubility via interaction with bile components | Phase I trials of ARV-110 and ARV-471 use "once daily with food" administration [77] |
Experimental Protocols for Assessing Oral Bioavailability
Permeability Assessment Protocols
Modified Caco-2 Transwell Assay: Traditional Caco-2 assays often require modification for accurate PROTAC assessment due to recovery issues from nonspecific binding [15].
- Cell Culture: Seed Caco-2 cells (TC7 clone) at 125,000 cells per well in 24-well transwell plates and culture for 14-21 days to form differentiated monolayers [15].
- Buffer Preparation: Prepare HBSS (Hanks' Balanced Salt Solution) with potential modifications including 10% FCS (fetal calf serum), FaSSIF (fasted state simulated intestinal fluid) in apical compartment, or pH adjustment to 6.5 to mimic intestinal conditions [15].
- Assay Procedure: Add test compound (1 µM final concentration) to donor compartment and incubate at 37°C in 5% CO₂ for 2 hours. Sample both donor and receiver compartments at t=0 and t=120 minutes [15].
- Permeability Calculation: Calculate apparent permeability (Pₐₚₚ) using the formula: Pₐₚₚ = (ΔCᵣₑ꜀/Δt × Vᵣₑ꜀) / (C𝒹ₒₙ,₀ × A), where ΔCᵣₑ꜀/Δt is the concentration change in receiver compartment, Vᵣₑ꜀ is receiver volume, C𝒹ₒₙ,₀ is initial donor concentration, and A is membrane surface area (0.33 cm²) [15].
- Quality Control: Determine mass balance (recovery) and monitor monolayer integrity using tightness markers like melagatran [15].
Exposed Polar Surface Area (ePSA) Determination: ePSA serves as a surrogate permeability measurement that correlates with passive diffusion capacity [15]. This method measures the dynamic polar surface area available for hydrogen bonding with solvents, with lower ePSA values generally indicating better membrane permeability.
Metabolic Stability Assessment
Hepatocyte Clearance Assay:
- Hepatocyte Preparation: Thaw cryopreserved hepatocytes (e.g., female CD-1 mouse) and determine viability (>70%) via trypan blue exclusion [15].
- Incubation Conditions: Incubate compounds (1 µM final concentration) with hepatocytes at 0.2 × 10⁶ cells/mL in Krebs-Henseleit buffer (pH 7.4) with ≤1% DMSO at 37°C under 5% CO₂ [15].
- Sampling Protocol: Collect aliquots in duplicate at 0, 10, 20, 40, 60, and 90 minutes and quench with two volumes of acetonitrile containing internal standard [15].
- Analysis: Quantify parent compound disappearance using UHPLC-MS/MS with calibration standards prepared in heat-inactivated hepatocytes [15].
- Data Interpretation: Calculate intrinsic clearance (CLᵢₙₜ) using half-life method and perform in vitro-in vivo extrapolation (IVIVE) using experimentally determined fraction unbound (fᵤ,ᵢₙ꜀) for accurate prediction [15].
Visualization of PROTAC Optimization Pathways
PROTAC Mechanism and Optimization Strategy
Experimental Workflow for PROTAC Optimization
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for PROTAC Bioavailability Studies
| Reagent/Assay System | Function in PROTAC Development | Application Notes |
|---|---|---|
| Caco-2 Cell Line (TC7 clone) | Model for intestinal permeability prediction | Requires 14-21 day differentiation; modified protocols with serum/FaSSIF improve recovery [15] |
| Cryopreserved Hepatocytes | Metabolic stability assessment | Mouse CD-1 hepatocytes common for preclinical studies; viability >70% required [15] |
| Biorelevant Media (FaSSIF/FeSSIF) | Solubility and dissolution testing | Fed-state simulated intestinal fluid (FeSSIF) particularly relevant for food effect studies [77] |
| Mucin from Porcine Stomach | Mucus penetration studies | Used at 50 mg/mL concentration to model gastrointestinal mucus barrier [15] |
| Transwell Plates (24-well) | Permeability assay format | 0.33 cm² membrane surface area; apical volume 250 µL, basolateral volume 750 µL [15] |
| UHPLC-MS/MS Systems | Bioanalytical quantification | Enables sensitive detection of PROTACs and metabolites in complex matrices [15] |
The development of orally bioavailable PROTACs requires careful navigation of their inherent bRo5 properties through strategic molecular design and rigorous experimental assessment. By implementing linker optimization, selective E3 ligase engagement, conformational control through intramolecular hydrogen bonding, and prodrug approaches, researchers can significantly improve the oral bioavailability of these promising therapeutic modalities. The experimental frameworks and optimization strategies outlined in this document provide a structured approach to advancing PROTAC candidates through the lead optimization process, with the ultimate goal of realizing their full clinical potential through oral administration.
Integrating and Validating ADME Data: From Model Systems to Human Translation
Benchmarks and Rules of Thumb for Candidate Selection
The selection of a robust development candidate is a critical milestone in the drug discovery pipeline, marking the transition from exploratory research to preclinical development. This process requires a meticulous balance between a compound's pharmacological activity and its absorption, distribution, metabolism, and excretion (ADME) properties. Problems with ADME properties remain a significant cause of clinical failure, underscoring the necessity of early and rigorous assessment [80]. The integration of ADME optimization throughout lead optimization research provides a strategic framework for selecting compounds with the highest probability of technical and clinical success, ultimately reducing attrition rates and accelerating the development of viable therapeutics [13] [81].
Modern drug discovery has been transformed by technological advancements, including the application of artificial intelligence (AI) and automation. Generative AI-driven platforms, such as that developed by Insilico Medicine, have demonstrated the potential to significantly compress discovery timelines, nominating developmental candidates in an average of approximately 13 months and synthesizing around 70 molecules per program [82]. Despite these technological shifts, the fundamental goal remains unchanged: to identify a compound with optimal drug-like properties, often guided by established principles like Lipinski's Rule of Five and its variants, which help predict oral activity [83]. This document provides a detailed overview of the key benchmarks, experimental protocols, and strategic tools essential for effective candidate selection within the context of ADME optimization.
Key Benchmarks for Candidate Selection
A data-driven approach to candidate selection relies on established benchmarks for critical physicochemical and pharmacokinetic parameters. These benchmarks serve as guideposts during lead optimization, helping researchers prioritize compounds and identify potential liabilities early in the process.
Table 1: Key Benchmarks for Candidate Selection in Lead Optimization
| Parameter | Target Benchmark | Rule of Thumb / Significance | Primary Reference |
|---|---|---|---|
| Lipophilicity (log D) | log D~7.4~ ~0 to 3 | Optimal lipophilicity for membrane permeability and solubility; high log D may increase metabolic clearance and toxicity risk. | [13] |
| Molecular Weight | ≤ 500 Da | One of Lipinski's Rule of Five criteria; lower molecular weight generally favors oral bioavailability. | [83] |
| Hydrogen Bond Donors | ≤ 5 | One of Lipinski's Rule of Five criteria; impacts membrane permeability and solubility. | [83] |
| Hydrogen Bond Acceptors | ≤ 10 | One of Lipinski's Rule of Five criteria; impacts membrane permeability and solubility. | [83] |
| Solubility | > 50-100 µM (at pH 7.4) | Ensures sufficient dissolution for absorption in the gastrointestinal tract. | [13] |
| Hepatic Microsome Stability (Human) | % Remaining > 50% (at 60 min) | Indicates metabolic stability; low stability suggests high clearance and short half-life in vivo. | [13] |
| Preclinical DC Nomination Timeline | ~9-18 months | AI-driven platforms have demonstrated the ability to nominate developmental candidates within this range. | [82] |
| Molecules Synthesized per Program | ~70-115 molecules | The number of molecules synthesized and screened to identify a developmental candidate. | [82] |
For programs aiming to develop orally administered drugs, adherence to Lipinski's Rule of Five is a widely used initial filter. It is important to note that these rules are a guideline, and exceptions exist, particularly for natural products and drugs that utilize active transport mechanisms [83]. Furthermore, the "Rule of Three" (molecular mass < 300, log P ≤ 3, HBD ≤ 3, HBA ≤ 3, rotatable bonds ≤ 3) is often applied to fragment-based screening libraries to ensure sufficient chemical space for optimization while maintaining drug-likeness [83].
Beyond these foundational rules, other metrics provide valuable insights. Veber's Rule suggests that compounds with 10 or fewer rotatable bonds and a polar surface area (PSA) no greater than 140 Ų are more likely to possess good oral bioavailability [83]. The Ghose Filter provides another set of criteria, including a molar refractivity from 40 to 130 and a molecular weight range of 180 to 480 [83].
Experimental Protocols for ADME Assessment
A tiered experimental approach is recommended for assessing ADME properties, starting with low-cost, high-throughput in vitro assays and progressing to more complex in vivo studies for promising leads. The following protocols outline key experiments for profiling a compound's ADME characteristics.
Lipophilicity (log D) Measurement via Shake-Flask Method
Pharmacological Question Addressed: "Will my parent compound be stored in lipid compartments, and how well will it bind to a target protein?" Lipophilicity is a critical physicochemical parameter that influences solubility, absorption, membrane penetration, plasma protein binding, and distribution [13].
Protocol:
- Assay Design: Test articles are assayed in triplicate at a single concentration (typically 10 µM).
- Partition System: A 1:1 volume ratio of n-octanol and aqueous buffer (typically phosphate buffer, pH 7.4) is used.
- Procedure: The compound is dissolved in the pre-saturated solvent system and shaken for 3 hours at room temperature to reach equilibrium.
- Analysis: The concentration of the parent compound in each phase is quantified using LC/MS/MS.
- Controls:
- Positive Control: Testosterone (high log D~7.4~ value)
- Negative Control: Tolbutamide (low log D~7.4~ value)
- Data Calculation: Log D~7.4~ is calculated as the log~10~ of the ratio of the compound concentration in the octanol phase to the concentration in the buffer phase [Log ([compound]~octanol~ / [compound]~buffer~)].
- Compound Requirement: 1.0 - 2.0 mg [13].
Kinetic Aqueous Solubility
Pharmacological Question Addressed: "What is the bioavailability of my compound?" Aqueous solubility is a key determinant of a compound's bioavailability, especially for orally administered drugs, as it limits the absorption from the gastrointestinal tract [13] [80].
Protocol:
- Assay Design: Test articles are assayed in duplicate at an initial concentration (typically 1 mM).
- Buffer System: Phosphate-buffered solutions across a physiologically relevant pH range (e.g., 5.0, 6.2, 7.4).
- Procedure: The compound is dissolved in the buffer and incubated for 18 hours with shaking to reach thermodynamic equilibrium.
- Analysis: The concentration of dissolved compound is measured by UV spectrophotometry.
- Controls:
- Positive Control: Diclofenac (high solubility)
- Negative Control: Dipyridamole (low solubility)
- Background Control: DMSO only
- Data Reporting: The amount of compound dissolved is reported in µM.
- Compound Requirement: 1.0 - 2.0 mg [13].
Hepatic Microsome Stability
Pharmacological Question Addressed: "How long will my parent compound remain circulating in plasma within the body?" This assay uses subcellular fractions of the liver to investigate Phase I metabolic stability, providing an early indicator of a compound's potential in vivo half-life and clearance [13] [80].
Protocol:
- Assay Design: Test articles are assayed in triplicate at a single concentration (typically 1-10 µM).
- Incubation System: Human or relevant species (e.g., rat, mouse) liver microsomes (0.5 mg/mL) in a NADPH-regenerating system.
- Time Points: Aliquots are quenched at t = 0 and t = 60 minutes (multiple time points can be used for kinetic analysis).
- Analysis: The percentage of the parent compound remaining at each time point is quantified using LC/MS/MS.
- Controls:
- Positive Control: A substrate with known high metabolic turnover (e.g., testosterone for CYP3A4).
- Negative Control: A duplicate incubation without NADPH to assess non-CYP450 metabolism.
- Data Reporting:
- % Parent Remaining at a single time point (e.g., 60 min).
- With multiple time points, the in vitro half-life (T~1/2~) and intrinsic clearance (CL~int~) can be calculated.
- Compound Requirement: 1.0 - 2.0 mg [13].
Figure 1: A tiered, iterative workflow for ADME and PK assessment during lead optimization, from initial in vitro profiling to development candidate selection. R.A.C.E. = Rapid Assessment of Compound Exposure; SPR = Structure-Property Relationship; SAR = Structure-Activity Relationship. Adapted from the Assay Guidance Manual [13].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful ADME optimization relies on a suite of well-characterized reagents, assays, and computational tools. The following table details key resources used in the field.
Table 2: Essential Research Reagent Solutions for ADME Assessment
| Tool / Reagent | Function in ADME Assessment | Application Context |
|---|---|---|
| Human Liver Microsomes | Subcellular fractions containing drug-metabolizing enzymes (e.g., CYPs); used to assess metabolic stability and identify metabolites. | Critical for in vitro hepatic microsome stability assays [13]. |
| PAMPA (Parallel Artificial Membrane Permeability Assay) | A non-cell-based high-throughput assay to model passive transcellular permeability. | Tier 1 screening for absorption potential; validated against marketed drugs [80]. |
| CM5 SPR Chips | Sensor chips for surface plasmon resonance (SPR) instruments; used to immobilize target proteins. | Enables binding affinity (K~D~) and kinetics (k~on~, k~off~) measurements for target engagement, as used in peptide optimization [27]. |
| Accelerator Mass Spectrometry (AMS) | Ultra-sensitive technology for quantifying radiolabeled compounds and metabolites at very low concentrations. | Used in human ADME studies and microdosing trials to track compound disposition with high precision [7]. |
| PBPK Modeling Software | Physiologically-based pharmacokinetic (PBPK) modeling and simulation software. | Bridges discovery and development by predicting human PK, absorption, distribution, and drug-drug interactions [7]. |
| ADME QSAR Models | Quantitative Structure-Activity Relationship models that predict ADME properties from chemical structure. | Early in silico screening for properties like solubility, permeability, and microsomal stability; publicly available via portals like ADME@NCATS [80]. |
| Multitask Graph Neural Networks | AI models capable of predicting multiple ADME parameters simultaneously, with explainability features. | Addresses data sparsity in ADME prediction and provides structural insights for lead optimization [19]. |
Emerging Technologies and Future Perspectives
The field of ADME optimization is being reshaped by the integration of advanced computational and analytical technologies. AI-driven platforms are demonstrating tangible improvements in the efficiency of drug discovery. For instance, Insilico Medicine's generative AI platform nominated 22 developmental candidates from 2021 to 2024, with an average timeline of approximately 13 months from project initiation, a significant acceleration compared to traditional methods that can take 2.5-4 years for the same stage [82].
The application of multitask graph neural networks for ADME prediction represents a significant AI advancement. These models can share information across multiple prediction tasks (e.g., 10 different ADME parameters), overcoming limitations posed by sparse data for any single endpoint. Furthermore, they incorporate explainability methods like Integrated Gradients (IG), which quantifies the contribution of each structural feature to the predicted ADME value, providing medicinal chemists with data-driven insights for rational molecular design [19].
Beyond AI, the adoption of 3Rs principles (Replacement, Reduction, and Refinement) is driving innovation in PK study design. This includes investment in miniaturization, microsampling techniques, and advanced analytics like Met-ID, which allow for the collection of high-quality PK data from fewer animals and with reduced compound requirements [7]. The ongoing harmonization of regulatory guidance, such as the ICH M12 guideline on drug-drug interaction studies, further streamlines the path from discovery to clinical development by providing a unified international framework for critical ADME assessments [7].
The successful translation of in vitro absorption, distribution, metabolism, and excretion (ADME) data to predict in vivo outcomes remains a critical challenge in drug development. Inadequate pharmacokinetic (PK) properties contribute significantly to late-stage failures, making early and accurate prediction essential for reducing attrition rates [84]. This application note details a structured framework and practical protocols for bridging this translational gap, enabling researchers to make more informed decisions during lead optimization.
The paradigm has evolved from simple correlation exercises to integrated in vitro-in vivo-in silico strategies that incorporate physiologically based pharmacokinetic (PBPK) modeling and quantitative systems pharmacology [64] [85]. When properly implemented, these approaches can significantly improve the prediction of human pharmacokinetics, guide dose selection, and reduce reliance on animal studies through the principles of the 3Rs (replacement, reduction, and refinement) [7] [85].
Core Principles of In Vitro to In Vivo Translation
Foundational Concepts
Translating in vitro ADME data requires understanding several key principles. Physicochemical properties including lipophilicity (log D), solubility, and permeability significantly influence absorption and distribution [86] [13]. Hepatic microsomal stability data provides insights into metabolic clearance, while plasma protein binding affects free drug concentration available for pharmacological activity [13] [87].
The critical link between in vitro assays and in vivo prediction involves extrapolation through mathematical modeling. Intrinsic clearance values from hepatocyte or microsomal stability assays can be scaled to predict in vivo hepatic clearance using physiological scaling factors [64]. For permeability, Caco-2 assays or PAMPA models help estimate intestinal absorption, which can be refined through PBPK modeling [84].
Strategic Framework
A successful translation strategy employs a multiparametric optimization approach that monitors several ADME properties simultaneously rather than in isolation [84]. The ADME-Space concept, which uses self-organizing maps based on predicted ADME behaviors, provides a visual framework for evaluating lead compounds across multiple properties [84].
Furthermore, implementing a learn-confirm cycle at the interface between in vitro and in vivo testing creates an iterative feedback loop that refines prediction models continuously [85]. This approach is less resource-intensive than traditional methods and facilitates more informed compound selection.
Experimental Protocols for In Vitro ADME Characterization
Lipophilicity Assessment (Log D7.4)
Protocol Objective: Determine the distribution coefficient at pH 7.4 to assess compound lipophilicity.
Materials:
- Test compound solution in DMSO (10 mM)
- n-Octanol (HPLC grade)
- Phosphate buffer (0.1 M, pH 7.4)
- LC-MS/MS system for analysis
Procedure:
- Prepare test compound at 10 μM final concentration in a 1:1 mixture of octanol and buffer.
- Vortex the mixture for 3 hours to ensure equilibrium partitioning.
- Centrifuge at 3,000 × g for 10 minutes to separate phases.
- Carefully collect both octanol and aqueous phases.
- Analyze compound concentration in each phase using LC-MS/MS.
- Calculate Log D7.4 using the formula: Log ([compound]octanol / [compound]buffer) [13].
Quality Control: Include testosterone (high Log D) and tolbutamide (low Log D) as controls to verify assay performance [13].
Hepatic Microsomal Stability
Protocol Objective: Evaluate metabolic stability in liver microsomes to predict intrinsic clearance.
Materials:
- Pooled species-specific liver microsomes (0.5 mg/mL)
- NADPH regeneration system
- Potassium phosphate buffer (0.1 M, pH 7.4)
- Test compounds (10 μM final concentration)
- Quenching solution (cold acetonitrile)
- LC-MS/MS system with automated optimization capability
Procedure:
- Pre-incubate microsomes with test compound in potassium phosphate buffer at 37°C for 5 minutes.
- Initiate reaction by adding NADPH solution (final concentration: 1 mM).
- Remove aliquots at designated time points (0, 15, 30, 45, 60, 90 minutes).
- Quench reactions with cold acetonitrile (3:1 ratio of acetonitrile to incubation volume).
- Centrifuge at 4,000 rpm for 10 minutes to precipitate proteins.
- Analyze supernatant by LC-MS/MS to determine parent compound remaining [88].
- Use software such as QuanOptimize to automate method development and data processing [88].
Data Analysis: Calculate half-life (t1/2) and intrinsic clearance (CLint) from the disappearance rate of parent compound.
Parallel Artificial Membrane Permeability Assay (PAMPA)
Protocol Objective: Assess passive transmembrane permeability.
Materials:
- PAMPA plate system
- Phospholipid solution (e.g., phosphatidylcholine in dodecane)
- Test compound (50-100 μM)
- Donor and acceptor plates
- UV plate reader or LC-MS/MS
Procedure:
- Apply phospholipid solution to membrane filter to create artificial membrane.
- Add test compound to donor compartment.
- Fill acceptor compartment with buffer.
- Incubate for 2-6 hours under controlled conditions.
- Analyze compound concentration in both compartments.
- Calculate apparent permeability (Papp) [84].
Quantitative Translation Approaches
In Vitro-In Vivo Extrapolation (IVIVE) of Clearance
Protocol Objective: Scale hepatic microsomal stability data to predict in vivo clearance.
Procedure:
- Determine in vitro intrinsic clearance (CLint, in vitro) from microsomal half-life: CLint, in vitro = (0.693 / t1/2) × (incubation volume / microsomal protein)
- Scale to predicted in vivo intrinsic clearance: CLint, in vivo = CLint, in vitro × microsomal protein per gram liver × liver weight
- Apply appropriate liver model (e.g., well-stirred model) to calculate hepatic clearance: CLH = (QH × CLint, in vivo × fu) / (QH + CLint, in vivo × fu) Where QH = hepatic blood flow, fu = fraction unbound in blood [64]
Physiologically Based Pharmacokinetic (PBPK) Modeling
Protocol Objective: Develop a PBPK model to simulate in vivo pharmacokinetics.
Procedure:
- Input Compound Parameters: Incorporate in vitro data including permeability, microsomal stability, plasma protein binding, and physicochemical properties.
- Define System Parameters: Include species-specific physiological parameters (organ weights, blood flows, tissue compositions).
- Model Construction: Implement using commercial PBPK software platforms.
- Verification and Refinement: Compare initial simulations with available in vivo data and refine parameters as needed [7].
- Simulation and Prediction: Run simulations for various dosing scenarios to predict exposure and inform dosing regimen design.
PBPK modeling serves as a powerful tool for bridging drug discovery and development by integrating in vitro data to predict human pharmacokinetics, understand distribution, optimize formulation, and assess drug-drug interaction potential [7].
Critical Data Interpretation and Benchmarking
ADME Property Benchmarks for Lead Optimization
Table 1: Key ADME Property Benchmarks for Lead Optimization during Drug Discovery
| ADME Parameter | Assay Type | Optimal Range | Interpretation | In Vivo Correlation |
|---|---|---|---|---|
| Lipophilicity | Log D7.4 | 1-3 | Balanced permeability/metabolic stability | High log D >3: increased metabolic clearance, low log D <1: poor permeability |
| Microsomal Stability | % remaining at 45 min | >50% | Low clearance | <50% remaining: high hepatic extraction ratio |
| Solubility | Kinetic solubility (pH 7.4) | >100 μM | Adequate for oral absorption | <10 μM: potential dissolution-limited absorption |
| Permeability | PAMPA or Caco-2 | Papp >10 × 10⁻⁶ cm/s | Good intestinal absorption | Papp <1 × 10⁻⁶ cm/s: poorly absorbed |
| Plasma Protein Binding | Equilibrium dialysis | fu >5% | Sufficient free fraction | fu <1%: restricted tissue distribution |
These benchmarks provide medicinal chemists with guidance for interpreting in vitro ADME data in the context of in vivo performance [13] [84]. The "Golden Triangle" visualization tool, which plots molecular weight against log D7.4, can further assist in simultaneously optimizing absorption and clearance [86].
Case Study: Risdiplam ADME Characterization
The development of risdiplam, an SMN2 mRNA splicing modifier for spinal muscular atrophy, exemplifies successful application of these principles. Risdiplam presented challenges including low turnover mediated through non-cytochrome P450 enzymatic pathways. Researchers employed a combination of in vitro and in vivo results to develop a robust PBPK model that successfully predicted human pharmacokinetics [64]. This case highlights how integrated approaches can address complex ADME properties that are difficult to investigate using standard methods.
Integrated Workflow for In Vitro to In Vivo Translation
The following diagram illustrates the comprehensive integrated strategy for translating in vitro ADME data to in vivo predictions:
Integrated ADME Translation Workflow
This integrated workflow demonstrates the continuous cycle of in vitro testing, modeling, in vivo verification, and model refinement that enables successful prediction of human pharmacokinetics [64] [7] [85].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Essential Research Reagent Solutions for ADME Studies
| Reagent/Technology | Function | Application Notes |
|---|---|---|
| Pooled Liver Microsomes | Metabolic stability assessment | Available from multiple species (human, rat, mouse); ensure consistent lot for comparable data [13] |
| NADPH Regeneration System | Cofactor for CYP450 enzymes | Critical for maintaining metabolic activity during incubation periods [88] |
| LC-MS/MS with Automation | Quantitative analysis of compounds | Enables high-throughput analysis; systems like Xevo TQ-S with QuanOptimize automate method development [88] |
| Equilibrium Dialysis Devices | Plasma protein binding measurement | Determine fraction unbound (fu) for clearance and distribution predictions [87] |
| Caco-2 Cell Lines | Intestinal permeability assessment | Model for predicting oral absorption and transporter effects [84] |
| PBPK Software Platforms | In vivo prediction from in vitro data | Implements physiological models to simulate pharmacokinetics [7] |
| Accelerator Mass Spectrometry (AMS) | Ultra-sensitive quantification in clinical studies | Enables human ADME studies with microdosing approaches [7] |
The translation of in vitro ADME data to in vivo outcomes requires a systematic, integrated approach that combines robust experimental protocols with appropriate modeling strategies. By implementing the frameworks and methods detailed in this application note, researchers can significantly improve their ability to predict human pharmacokinetics during lead optimization, ultimately reducing late-stage attrition and accelerating the development of viable drug candidates.
The continued evolution of in silico approaches, including artificial intelligence and multitask graph neural networks for ADME prediction, promises to further enhance these translation capabilities in the future [19]. However, regardless of technological advances, the fundamental principle remains: high-quality, well-designed in vitro data generated using standardized protocols forms the essential foundation for successful in vivo predictions.
Absorption, Distribution, Metabolism, and Excretion (ADME) properties are critical determinants of the success or failure of drug candidates, with poor ADME profiles representing a major cause of attrition in drug development [37]. The evaluation of these properties relies on three complementary methodological approaches: in silico (computational), in vitro (laboratory-based), and in vivo (whole organism) models. During lead optimization research, these models form an integrated framework for selecting compounds with desirable pharmacokinetic profiles and sufficient bioavailability to be viable efficacious drugs [13]. This review provides a comparative analysis of these approaches, highlighting their respective strengths, limitations, and strategic applications within modern drug discovery pipelines. We present standardized protocols and data interpretation guidelines to facilitate their effective implementation in lead optimization campaigns.
In Silico ADME Models
In silico ADME prediction involves the use of computational models to estimate pharmacokinetic properties based on a compound's chemical structure [37]. These tools have evolved from simplified relationships between ADME endpoints and physicochemical properties to sophisticated machine learning approaches, including support vector machines, random forests, and convolutional neural networks [37]. The primary application of in silico models in lead optimization is the virtual screening of vast compound libraries to prioritize candidates for synthesis and testing, thereby guiding structural design before chemical synthesis [37].
Key Methodologies and Protocols
Table 1: Common In Silico ADME Prediction Platforms and Their Applications
| Platform Name | Model Type | Key Predictable Parameters | Typical Applications in Lead Optimization |
|---|---|---|---|
| ADMET Predictor [37] | Commercial AI/ML platform | Multiple ADMET endpoints | Early screening of virtual compound libraries |
| SwissADME [37] | Free web tool | Physicochemical properties, drug-likeness | Academic research, preliminary screening |
| pkCSM [37] | Free web tool | Permeability, metabolism, toxicity | Student projects, initial compound prioritization |
| OCHEM [37] | Online modeling environment | Various ADME endpoints | Collaborative model building and validation |
| iD3-INST [37] | Academic platform | ADME profiles for academic drug discovery | Supporting translational academic research |
Protocol 1: Implementation of In Silico ADME Screening in Lead Optimization
- Objective: To prioritize lead compounds from virtual libraries based on predicted ADME properties.
- Input Requirements: Chemical structures in standardized format (e.g., SMILES, SDF).
- Procedure:
- Compound Enumeration: Generate virtual compound libraries around lead series.
- Descriptor Calculation: Compute molecular descriptors and fingerprints.
- Model Application: Submit structures to one or multiple prediction platforms.
- Data Integration: Compile predictions for key parameters (e.g., logP, solubility, metabolic stability).
- Multi-parameter Optimization: Rank compounds based on balanced ADME and potency predictions.
- Data Interpretation: Compounds falling within the following ranges generally exhibit favorable drug-like properties: logP = 1-3, molecular weight <500 g/mol, and high predicted metabolic stability [37] [13].
Strengths and Limitations
Strengths:
- High Throughput: Capable of screening thousands to millions of compounds rapidly [37].
- Low Cost: Minimal resources required compared to experimental approaches [37].
- Prefiltering Capability: Identifies promising candidates before chemical synthesis [37].
- Mechanistic Insight: Provides structure-property relationships to guide medicinal chemistry [89].
Limitations:
- Training Data Dependency: Model accuracy depends on the quality and diversity of underlying data [37].
- Limited Transparency: Some complex AI models function as "black boxes" [37].
- Extrapolation Risk: Predictions may be unreliable for novel chemotypes outside the model's training set [89].
- Quantitative Accuracy: Often insufficient for standalone decision-making, requiring experimental confirmation [89].
In Vitro ADME Models
In vitro models experimentally evaluate specific ADME processes under controlled laboratory conditions using subcellular fractions, cell cultures, or tissue preparations [13] [90]. These assays serve as crucial bridges between in silico predictions and in vivo testing, providing mechanistically informed data on compound behavior [13]. During lead optimization, they facilitate structure-activity relationship (SAR) and structure-property relationship (SPR) analyses, enabling the selection of compounds with the highest probability of success in preclinical development [13].
Key Methodologies and Protocols
Table 2: Key In Vitro ADME Assays and Their Applications in Lead Optimization
| Assay Type | Experimental System | Key Parameters Measured | Lead Optimization Application |
|---|---|---|---|
| Lipophilicity [13] | Shake-flask (octanol-water) | logP, logD | Understanding membrane permeation and distribution |
| Metabolic Stability [13] | Liver microsomes, hepatocytes | Intrinsic clearance, half-life | Ranking compounds by metabolic liability |
| Permeability [90] | Caco-2, MDCK cell monolayers | Apparent permeability (Papp) | Predicting intestinal absorption |
| Transporter Interactions [90] | MDCK-MDR1, transfected cells | Transporter substrate/inhibition potential | Assessing DDI risk and tissue distribution |
| Plasma Protein Binding [7] | Equilibrium dialysis, ultrafiltration | Fraction unbound (fu) | Estimating effective drug concentration |
| Solubility [13] | Kinetic and thermodynamic assays | Aqueous solubility at physiological pH | Guiding formulation development |
Protocol 2: Metabolic Stability Assessment Using Liver Microsomes
- Objective: To predict the metabolic clearance of lead compounds and identify metabolically labile structural motifs [13].
- Materials:
- Test compounds (1.0-2.0 mg)
- Pooled human liver microsomes (0.5 mg/mL)
- NADPH-regenerating system
- Phosphate buffer (pH 7.4)
- LC-MS/MS system for analysis
- Procedure:
- Incubation Preparation: Combine test compound (typically 1 μM), microsomes, and buffer.
- Pre-incubation: Equilibrate mixture at 37°C for 5 minutes.
- Reaction Initiation: Add NADPH-regenerating system.
- Time-point Sampling: Withdraw aliquots at t=0, 5, 15, 30, and 60 minutes.
- Reaction Termination: Add ice-cold acetonitrile to precipitate proteins.
- Sample Analysis: Quantify parent compound remaining using LC-MS/MS.
- Data Interpretation:
- Calculate half-life (t1/2) and intrinsic clearance (CLint).
- Benchmarks: Compounds with low CLint are preferred. High CLint indicates rapid metabolism, potentially requiring structural modification [13].
Protocol 3: Permeability Assessment Using Caco-2 Cell Monolayers
- Objective: To predict intestinal absorption and identify transporter-mediated efflux [90].
- Materials:
- Caco-2 cell monolayers (21-28 days post-seeding)
- Transport buffer (HBSS, pH 7.4)
- Test compound
- Transwell plates
- LC-MS/MS system for analysis
- Procedure:
- Monolayer Integrity Check: Measure transepithelial electrical resistance (TEER).
- Bidirectional Transport:
- A-B (Absorption): Add compound to apical chamber, sample from basolateral.
- B-A (Efflux): Add compound to basolateral chamber, sample from apical.
- Incubation: Maintain at 37°C with gentle agitation.
- Time-point Sampling: Collect samples at regular intervals up to 2 hours.
- Sample Analysis: Quantify compound concentration in receiver chambers.
- Data Interpretation:
- Calculate apparent permeability (Papp).
- Determine efflux ratio (B-A Papp / A-B Papp).
- Benchmarks: Papp > 10×10-6 cm/s suggests high permeability; efflux ratio >2 suggests potential P-gp substrate [90].
Figure 1: Sequential integration of ADME models in lead optimization.
Strengths and Limitations
Strengths:
- Mechanistic Insight: Enable isolation and study of specific ADME processes [90].
- Human Relevance: Human-derived tissues and cells provide human-specific metabolic information [13].
- Medium Throughput: Suitable for profiling dozens to hundreds of compounds [13].
- Reduced Ethical Concerns: Minimize animal use in early discovery stages [90].
Limitations:
- Limited Systemic Context: Cannot capture integrated physiology [90].
- Technical Variability: Inter-laboratory differences in assay conditions can affect data comparability [13].
- Compound Requirements: Need for purified compounds in sufficient quantities (typically 1-2 mg) [13].
- Simplified Biology: May oversimplify complex in vivo processes like tissue distribution [91].
In Vivo ADME Models
In vivo ADME studies involve administering compounds to live organisms, most commonly rodents, to characterize their comprehensive pharmacokinetic profiles [91]. These studies provide the most physiologically relevant data on drug absorption, distribution, metabolism, and excretion within the context of whole-body integrated physiology [91]. In lead optimization, in vivo studies are typically reserved for evaluating the most promising candidates that have successfully passed through in silico and in vitro screening filters [13].
Key Methodologies and Protocols
Protocol 4: Rapid Assessment of Compound Exposure (R.A.C.E.) in Rodents
- Objective: To obtain preliminary in vivo pharmacokinetic data for lead compound prioritization [13].
- Materials:
- Test compound
- Laboratory rodents (typically mice or rats)
- Formulation vehicle
- Blood collection equipment (microsampling techniques preferred)
- LC-MS/MS system for bioanalysis
- Procedure:
- Compound Administration: Administer test compound via intended route (e.g., oral gavage).
- Sparse Sampling: Collect blood samples at 3-4 strategic time points (e.g., 0.5, 2, 6, and 24 hours).
- Sample Processing: Separate plasma and store frozen until analysis.
- Bioanalysis: Quantify compound concentrations in plasma using LC-MS/MS.
- Data Analysis: Calculate key PK parameters (AUC, Cmax, t1/2).
- Data Interpretation: Compare exposure parameters across lead series to select compounds with desirable PK profiles for further development [13].
Protocol 5: Radiolabeled ADME Studies in Preclinical Species
- Objective: To comprehensively characterize the absorption, distribution, metabolism, and excretion of a lead candidate [91].
- Materials:
- 14C- or 3H-labeled test compound
- Preclinical species (rodent and non-rodent)
- Metabolic cages
- Scintillation counter
- Radio-HPLC or LC-AMS for metabolite profiling
- Procedure:
- Compound Administration: Administer radiolabeled compound.
- Sample Collection: Collect blood, plasma, urine, feces, and potentially tissues over time.
- Radioactivity Quantification: Measure total radioactivity in matrices.
- Metabolite Profiling and Identification: Characterize metabolite structures.
- Mass Balance Determination: Account for administered radioactivity.
- Data Interpretation: Provides comprehensive understanding of compound disposition, including absorption extent, metabolite identification, and excretion routes [91].
Strengths and Limitations
Strengths:
- Physiological Relevance: Captures integrated ADME processes in whole organisms [91].
- Complete PK Profiling: Provides definitive data on bioavailability, clearance, and half-life [13].
- Tissue Distribution Data: Enables understanding of target organ exposure [91].
- Metabolite Identification: Reveals complete metabolic pathways and potential active/toxic metabolites [91].
Limitations:
- Low Throughput: Resource-intensive, typically evaluating only a few compounds at a time [13].
- High Cost: Significant compound, animal, and technical resource requirements [91].
- Species Differences: Extrapolation from animals to humans remains challenging [92].
- Ethical Considerations: Involves animal use, requiring strong scientific justification [90].
Integrated Workflow for Lead Optimization
Strategic Integration of ADME Models
Successful lead optimization requires strategic integration of all three ADME model types in a hierarchical screening cascade [13]. This integrated approach maximizes efficiency by applying lower-cost, higher-throughput methods early in the process, reserving resource-intensive approaches for the most promising candidates.
Figure 2: Strengths and limitations of different ADME model types.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for ADME Studies
| Reagent/Material | Specific Examples | Primary Application | Function in ADME Assessment |
|---|---|---|---|
| Liver Microsomes [13] | Human, rat, mouse liver microsomes | Metabolic stability, metabolite identification | Source of cytochrome P450 and other drug-metabolizing enzymes |
| Hepatocytes [92] | Cryopreserved human hepatocytes | Hepatic clearance, enzyme induction | Physiologically relevant liver model with full complement of enzymes and transporters |
| Cell Lines [90] | Caco-2, MDCK, MDCK-MDR1, HT29-MTX | Permeability, transporter interactions | Models of intestinal absorption, blood-brain barrier penetration |
| Immobilized Artificial Membranes [93] | IAM HPLC columns | Membrane partitioning potential | Biomimetic chromatography for predicting cellular uptake |
| Plasma Proteins [13] | Human serum albumin, α1-acid glycoprotein | Plasma protein binding | Quantification of fraction unbound for correlation with efficacy |
| Radiolabeled Compounds [91] | 14C-, 3H-labeled drugs | Mass balance, metabolite profiling | Tracing drug and metabolites through biological systems |
The strategic integration of in silico, in vitro, and in vivo ADME models creates a powerful framework for lead optimization in modern drug discovery. In silico tools enable rapid triaging of virtual compounds, in vitro assays provide mechanistically informed data on specific ADME processes, and in vivo studies deliver definitive pharmacokinetic profiles in whole organisms. Contemporary trends, including the adoption of more complex cell models [7], organs-on-chips [90], and advanced PBPK modeling [92], continue to enhance the predictive power of these approaches. By understanding the distinct strengths and limitations of each model type and implementing them in a strategically integrated workflow, researchers can significantly improve the efficiency of lead optimization and increase the likelihood of developing successful therapeutic agents.
In modern drug development, the optimization of Absorption, Distribution, Metabolism, and Excretion (ADME) properties is critical for selecting viable drug candidates. The integration of in vitro assays, Physiologically Based Pharmacokinetic (PBPK) modeling, and clinical data creates a powerful framework for predicting human pharmacokinetics and optimizing lead compounds. This integrated "middle-out" approach combines the mechanistic understanding from in vitro data with the physiological relevance of in vivo observations, enabling more informed decision-making throughout the drug discovery pipeline [42]. This Application Note details the protocols and workflows for implementing such a strategy, with a specific focus on ADME optimization during lead optimization research.
Key In Vitro ADME Assays for PBPK Input
Early in vitro assessment provides the fundamental drug-specific parameters required for robust PBPK model construction. The following assays are essential for informing the model and establishing Structure-Property Relationships (SPR) [13] [94].
Table 1: Essential In Vitro ADME Assays for PBPK Modeling
| ADME Attribute | Assay Type | Protocol Summary | Key Outputs for PBPK |
|---|---|---|---|
| Absorption | Lipophilicity [13] | "Shake-flask" method with octanol and aqueous buffer (pH 7.4) at a 1:1 ratio; incubation for 3 hours; LC/MS/MS analysis. | Log D₇.₄ (Distribution coefficient) |
| Permeability [94] | PAMPA, Caco-2, or transfected cell lines (e.g., MDCKII); measurement of compound passage across cell monolayer. | Apparent Permeability (Papp) | |
| Transporter Interactions [94] | Cell systems overexpressing specific transporters (e.g., P-gp, BCRP, OATP); assessment of uptake/efflux. | Transporter affinity (Km, Vmax) | |
| Distribution | Protein Binding [94] | Equilibrium dialysis, ultrafiltration, or ultracentrifugation of compound in plasma or tissue homogenate. | Fraction Unbound (fu) |
| Blood-to-Plasma Ratio [94] | Incubation of compound with whole blood; comparison of concentration in blood vs. plasma. | Blood-to-Plasma Ratio (B/P) | |
| Metabolism | Hepatic Microsome Stability [13] | Incubation of compound (e.g., 10 µM) with liver microsomes (0.5 mg/mL) +/- NADPH cofactor; LC/MS/MS analysis at t=0 and t=60 min. | % Parent Remaining, Intrinsic Clearance (CLint) |
| Reaction Phenotyping [94] | Use of specific recombinant CYP/UGT enzymes or inhibitory antibodies to identify metabolizing enzymes. | Enzyme-specific CLint, Fraction Metabolized (fm) | |
| Cytochrome P450 Inhibition [94] | Incubation of CYP probe substrates with human liver microsomes in presence of test compound. | IC₅₀, Ki (Inhibition constant) |
Experimental Protocols
Protocol: Hepatic Microsomal Stability Assay
This protocol determines the metabolic stability of a drug candidate in liver microsomes, a key parameter for estimating hepatic clearance in PBPK models [13].
Materials:
- Test Article: Drug candidate (1.0 - 2.0 mg required)
- Matrix: Pooled human liver microsomes (commercially available, e.g., from Xenotech)
- Cofactor: NADPH-regenerating system
- Controls: Testosterone (positive control), NADPH-deficient well (negative control)
- Equipment: LC/MS/MS system
Method:
- Preparation: Pre-warm incubation mixtures containing 0.5 mg/mL liver microsomes and 10 µM test article in phosphate buffer.
- Initiation: Start the reaction by adding the NADPH-regenerating system.
- Incubation: Maintain the reaction at 37°C. Aliquot samples at pre-determined time points (e.g., t = 0, 5, 15, 30, 45, 60 minutes).
- Termination: Stop the reaction by transferring aliquots to an equal volume of ice-cold acetonitrile.
- Analysis: Centrifuge samples and analyze the supernatant via LC/MS/MS to quantify the remaining parent compound.
Data Analysis: Calculate the percentage of parent compound remaining at each time point. The half-life (t₁/₂) and intrinsic clearance (CLint) can be derived from the slope of the natural logarithm of concentration versus time.
Protocol: Permeability Assessment using PAMPA
The Parallel Artificial Membrane Permeability Assay (PAMPA) is a high-throughput tool for predicting passive, transcellular absorption [94].
Materials:
- Test Article: Drug candidate
- Membrane: Lipid-impregnated filter (e.g., with phosphatidylcholine)
- Buffer: Aqueous buffers at pH 5.0, 6.2, and 7.4
- Equipment: 96-well PAMPA plate, UV plate reader or LC/MS
Method:
- Assembly: Fill the donor wells with test compound solution. Fill the acceptor wells with blank buffer.
- Assembling: Place the artificial membrane on the donor plate and carefully place the acceptor plate on top.
- Incubation: Incubate the assembled PAMPA sandwich for a set period (e.g., 2-16 hours) at room temperature.
- Analysis: Quantify the concentration of the compound in both the donor and acceptor wells at the end of the incubation using UV spectrophotometry or LC/MS.
Data Analysis: Calculate the apparent permeability (Papp) using the formula derived from Fick's law of diffusion. Compare the value to benchmarks for high vs. low permeability.
Integrated PBPK Modeling Workflow
A PBPK model integrates data from in vitro assays and early in vivo studies to simulate drug disposition. The following diagram illustrates the workflow for building and applying a PBPK model using an integrated strategy.
Case Study: PBPK Modeling of a Nifedipine-IR and Grapefruit Juice Interaction
A study successfully linked in vitro dissolution and enzyme inhibition data to clinical plasma profiles using PBPK modeling for nifedipine, an immediate-release (IR) formulation [95].
Application:
- Objective: Simulate the pharmacokinetic impact of grapefruit juice (GFJ) ingestion, a known intestinal CYP3A4 inhibitor, on nifedipine exposure.
- Integrated Approach:
- In vitro dissolution tests were conducted in media simulating fasted and fed states to describe the formulation's in vivo dissolution [95].
- Literature data on CYP3A4 levels in the gut and GFJ's dual effect (CYP3A4 inhibition + delayed gastric emptying) were incorporated into a PBPK model [95].
- The model was calibrated and used to simulate plasma concentration-time profiles with and without GFJ.
- Outcome: The model accurately predicted the observed food-drug interaction. A 60% reduction in intestinal CYP3A4 levels yielded simulated nifedipine concentrations within 20% of the actual in vivo data, establishing a quantitative link between dissolution characteristics and clinical performance [95].
The Scientist's Toolkit: Essential Research Reagents & Software
Table 2: Key Research Reagent Solutions and Software Platforms
| Category | Item | Function & Application in Integrated Strategies |
|---|---|---|
| In Vitro Systems | Pooled Human Liver Microsomes/S9 [13] | Contains major drug-metabolizing enzymes (CYPs, UGTs, FMOs) for assessing metabolic stability and metabolite formation. |
| Recombinant CYP/UGT Enzymes [94] | Individual enzymes used for reaction phenotyping to identify which specific enzyme metabolizes a drug candidate. | |
| Transfected Cell Lines (e.g., MDR1-MDCKII) [94] | Cell lines overexpressing specific transporters (e.g., P-gp, BCRP) to study transporter-mediated uptake and efflux. | |
| Software Platforms | Simcyp Simulator [42] | A leading PBPK platform with extensive libraries for predicting DDIs, PK in special populations, and performing virtual bioequivalence trials. |
| GastroPlus [42] | Specializes in physiology-based biopharmaceutics modeling, integrating mechanistic oral absorption with PBPK. | |
| PK-Sim [42] | An open-source whole-body PBPK platform suitable for cross-species extrapolation and tissue distribution predictions. |
The integration of in vitro ADME data, PBPK modeling, and clinical PK results provides a mechanistic, efficient, and predictive framework for lead optimization. This synergistic strategy moves beyond empirical observations, allowing researchers to anticipate human pharmacokinetics, de-risk drug-drug interactions, and optimize formulations for specific populations. By adopting the detailed protocols and workflows outlined in this Application Note, drug development scientists can enhance the scientific rigor of their candidate selection and accelerate the journey of promising compounds to the clinic.
Lessons from Clinical Mass Balance Studies for Informed Preclinical Design
Human radiolabeled mass balance studies are a critical component of clinical pharmacology programs supporting the development of new investigational drugs [96]. These studies, often referred to as absorption, distribution, metabolism, and excretion (ADME) studies, characterize the disposition of the parent drug and its metabolites in the human body [96]. The primary objectives include elucidating overall pathways of metabolism and excretion, identifying and quantifying circulating metabolites, and determining the abundance of metabolites relative to parent drug exposure [96]. When undesirable pharmacokinetics and toxicity are significant reasons for drug development failure in costly late stages, the strategic application of clinical mass balance findings to preclinical design becomes paramount [3]. This application note outlines how insights derived from clinical mass balance studies can inform smarter preclinical design, ultimately reducing attrition rates in drug development through a "fail early, fail cheap" strategy [3].
Key Lessons from Clinical Mass Balance Studies
Limitations of Single-Dose Design and the Multiple-Dose Alternative
Traditional human mass balance studies typically employ a single-dose approach, which has inherent limitations because single-dose measurements may not accurately represent steady-state conditions, particularly for molecules with time-dependent pharmacokinetics or ADME characteristics [97]. This approach requires extended subject confinement (usually exceeding 10 days), adding participant burden and raising ethical concerns, especially in patient populations [97].
A novel study design implementing multiple fractional [14C]-microtracer doses addresses these challenges [97]. This approach was evaluated in a rat proof-of-concept study using [14C]GDC-0334, demonstrating robust assessment of circulating metabolite profiles and clearance pathways from steady-state samples alone [97]. This method eliminates the need for sample pooling, simplifies sample preparation, and enhances analysis using undiluted samples [97].
Table 1: Comparison of Single-Dose vs. Multiple-Dose Mass Balance Study Designs
| Parameter | Single-Dose Design | Multiple-Dose Design |
|---|---|---|
| Physiological Relevance | May not represent steady-state conditions | Enables true steady-state assessment |
| Subject Confinement | Usually >10 days | Minimized |
| Sample Processing | Requires pooling | Simplified, uses undiluted samples |
| Metabolite Profile | Single-timepoint snapshot | Comprehensive steady-state characterization |
| Regulatory Precedence | Traditional approach (97% of studies) [96] | Emerging approach with significant advantages |
Metabolite Identification and the "10% Threshold"
Clinical mass balance studies provide critical information for metabolite profiling in plasma, urine, and feces samples [96]. The ratio of plasma metabolite to parent drug and/or total drug-related exposure determines whether metabolites require further nonclinical safety evaluation [96]. The FDA's "Safety Testing of Drug Metabolites" guidance mandates identification and characterization of metabolites exceeding the "10% threshold" - human metabolites that comprise greater than 10% of the measured total exposure to drug and metabolites (usually based on group mean AUC) [98]. This threshold has profound implications for preclinical design, as toxicology coverage must be confirmed for all significant human metabolites [98].
Failure to adequately characterize major metabolites has led to regulatory actions, including refuse-to-file letters and complete response letters [96]. For example, inadequate characterization of a major active metabolite contributed to a refuse-to-file letter for ozanimod, while deficiencies in characterizing major metabolites of deutetrabenazine resulted in a complete response letter [96].
Clearance Pathways and Elimination Routes
Understanding routes of elimination and clearance mechanisms from clinical mass balance studies directly informs the need for additional specialized preclinical and clinical studies [98]. When a drug is excreted primarily in the urine and cleared via renal mechanisms, renal impairment studies become necessary [98]. Similarly, drugs cleared via hepatic mechanisms may require hepatic impairment studies [98]. Furthermore, metabolite pathways accounting for greater than 25% of drug clearance may need evaluation in drug-drug interaction studies with co-medications that can inhibit or induce those pathways [98].
Protocols for Preclinical ADME Assessment Informed by Clinical Insights
Two-Tiered Preclinical ADME Screening Approach
A systematic two-tiered approach to preclinical ADME assessment allows for efficient compound prioritization during lead optimization [13]. This strategy incorporates critical clinical mass balance considerations early in the development pipeline.
Table 2: Tiered Preclinical ADME Assessment Protocol
| Tier | Assays | Key Parameters | Informs Clinical Mass Balance |
|---|---|---|---|
| Tier 1: Early Screening | Lipophilicity, Solubility, Hepatic Microsome Stability | Log D7.4, solubility (μM), % metabolism | Predicts absorption and metabolic stability |
| Tier 2: Advanced Profiling | CYP inhibition/induction, Plasma Protein Binding, Permeability assays | IC50, % bound, apparent permeability | Anticipates drug interactions and distribution |
Detailed Experimental Protocols
Hepatic Microsome Stability Assay
Objective: Predict metabolic clearance of parent compound [13]
Protocol:
- Test system: Human liver microsomes (0.5 mg/mL) or other relevant species [13]
- Test article concentration: 10 μM (single concentration) or multiple concentrations for kinetic analysis [13]
- Time points: t = 0 and t = 60 minutes (single time point) or multiple time points for half-life determination [13]
- Controls: NADPH-deficient negative control; substrates with known activity as positive controls [13]
- Analysis: LC/MS/MS measurement of parent compound at specific time points [13]
- Output: % metabolism of test article (single time point); intrinsic clearance and half-life (multiple time points) [13]
- Compound requirement: 1.0-2.0 mg [13]
Informed Design Consideration: Species selection should align with toxicology studies to enable cross-species metabolite comparison, anticipating the clinical "10% threshold" requirement.
Lipophilicity Assessment
Objective: Determine distribution characteristics influencing membrane penetration and tissue distribution [13]
Protocol:
- Method: Shake-flask method with n-octanol and aqueous buffer (1:1 ratio) [13]
- Test article: Single concentration (typically 10 μM) in triplicate [13]
- Controls: Testosterone (high log D7.4); tolbutamide (low log D7.4) [13]
- Analysis: LC/MS/MS measurement of parent compound in each phase [13]
- Calculation: Log D7.4 = log([compound]octanol / [compound]buffer) [13]
- Compound requirement: 1.0-2.0 mg [13]
Informed Design Consideration: Lipophilicity data helps predict volume of distribution and potential for tissue accumulation observed in clinical QWBA studies.
Radiolabeling Strategy for Preclinical Mass Balance Studies
Objective: Enable comprehensive mass balance and tissue distribution assessment [98]
Protocol:
- Isotope selection: 14C preferred over 3H for metabolic stability [98]
- Label position: Place radiolabel on metabolically stable moiety to track through metabolic pathways [98]
- Synthesis timeline: Initiate 1-2 years before planned clinical mass balance study [98]
- Formulation: Develop GMP-quality radiolabeled formulation for clinical studies [98]
Informed Design Consideration: Early radiolabeling strategy facilitates both preclinical tissue distribution studies (QWBA) and future clinical mass balance studies.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Mass Balance-Informed Preclinical Studies
| Reagent/Resource | Function | Application in Preclinical Design |
|---|---|---|
| Liver Microsomes | Subcellular fractions containing drug-metabolizing enzymes (CYPs, FMOs, esterases) [13] | Metabolic stability assessment; metabolite identification |
| CYP-Specific Substrates & Inhibitors | Reaction phenotyping tools | Identification of enzymes responsible for metabolite formation |
| Radiolabeled Compounds ([14C], [3H]) | Tracing drug and metabolites through biological systems [98] | Mass balance, tissue distribution (QWBA), metabolite profiling |
| Specific Chemical Inhibitors | Enzyme inhibition studies | Reaction phenotyping to identify metabolizing enzymes |
| Recombinant CYP Enzymes | Individual cytochrome P450 activity assessment | Reaction phenotyping to identify specific metabolizing enzymes |
| Hepatocytes | Intact cellular metabolism model | Higher fidelity metabolism studies including non-CYP pathways |
Visualizing the Integration Pathway
Integration of Clinical Mass Balance Findings into Preclinical Strategy
The strategic application of clinical mass balance insights to preclinical design represents a powerful paradigm shift in drug development. By understanding the limitations of traditional single-dose mass balance studies, researchers can implement more physiologically relevant multiple-dose approaches in preclinical testing [97]. By anticipating the critical "10% threshold" for metabolite identification, comprehensive metabolite screening can be incorporated early in lead optimization [98]. By recognizing how clearance pathways inform specialized population studies, more predictive preclinical models of hepatic and renal clearance can be developed. This forward-and-back translation approach, where clinical findings directly inform preclinical strategy, ultimately enhances the efficiency and success rate of drug development programs, reducing late-stage attrition due to ADME issues.
Conclusion
Successful ADME optimization in lead optimization no longer relies on a single technology but demands an integrated, strategic approach that combines foundational science with innovative tools. The future points toward the earlier application of AI and machine learning for de-risking molecular design, the wider adoption of human-relevant models like organ-on-a-chip to overcome species disparities, and the use of PBPK modeling to synthesize diverse data streams for more accurate human prediction. By embracing these integrated workflows, researchers can significantly improve the selection of viable drug candidates, enhance R&D efficiency, and increase the likelihood of clinical success, ultimately accelerating the delivery of new therapies to patients.
References
- 1. Refined ADME Profiles for ATC Drug Classes [https://www.mdpi.com/1999-4923/17/3/308]
- 2. Refined ADME Profiles for ATC Drug Classes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944659/]
- 3. Frontiers | Computational Approaches in Preclinical Studies on Drug Discovery and Development [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2020.00726/full]
- 4. -Space: a new tool for medicinal chemists to explore ADME ... ADME [https://www.nature.com/articles/s41598-017-06692-0?error=cookies_not_supported&code=ba920eb4-a693-41a6-ad95-b9d318ffe08e]
- 5. Leveraging machine learning models in evaluating ADMET properties for drug discovery and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205928/]
- 6. In Vitro and In Vivo Assessment of ADME and PK Properties During... [https://pubmed.ncbi.nlm.nih.gov/26561695/]
- 7. ADME Optimisation 2025 | Accelerate Drug Development [https://www.pharmaron.com/pharmaron-stories/adme-optimisation-2025/]
- 8. SwissADME: a free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules | Scientific Reports [https://www.nature.com/articles/srep42717]
- 9. Bridging data and drug development: Machine learning approaches for next-generation ADMET prediction - PubMed [https://pubmed.ncbi.nlm.nih.gov/41052751/]
- 10. Strategy of utilizing in vitro and in vivo ADME tools for lead optimization and drug candidate selection - PubMed [https://pubmed.ncbi.nlm.nih.gov/16181128/]
- 11. and Their Dependence on ADME ... Properties Physicochemical [https://link.springer.com/chapter/10.1007/978-1-4419-5629-3_9]
- 12. PPT - A BIT OF ADME FOR EVERYONE: LogD, SOLUBILITY ... [https://www.slideserve.com/fathi/a-bit-of-adme-for-everyone-logd-solubility-permeability-and-the-universal-detection-system]
- 13. In Vitro and In Vivo Assessment of ADME and PK Properties During Lead Selection and Lead Optimization – Guidelines, Benchmarks and Rules of Thumb - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK326710/]
- 14. Pharmacokinetics Software | Predict ADME | ACD/Labs Properties [https://www.acdlabs.com/products/percepta-platform/adme-suite/]
- 15. In vitro and in vivo ADME of heterobifunctional degraders: a tailored... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11843253/]
- 16. How to report and discuss ADME data in medicinal chemistry publications: in vitro data or in vivo extrapolations? - PubMed [https://pubmed.ncbi.nlm.nih.gov/25826359/]
- 17. PCB Module: Accurate Physicochemical Property Predictions [https://www.simulations-plus.com/software/admetpredictor/physicochemical-biopharmaceutical/]
- 18. ADME Properties in Drug Discovery • BioSolveIT [https://www.biosolveit.de/drug-discovery-solutions/adme-properties-in-drug-discovery/]
- 19. Improving ADME Prediction with Multitask Graph Neural Networks and... [https://chemrxiv.org/engage/chemrxiv/article-details/68d60081f2aff16770a09ee9]
- 20. In silico ADME/T modelling for rational drug design | Quarterly Reviews of Biophysics | Cambridge Core [https://www.cambridge.org/core/journals/quarterly-reviews-of-biophysics/article/in-silico-admet-modelling-for-rational-drug-design/967D13A3BF04B9B46B692472CF800A74]
- 21. Use of intrinsic clearance for prediction of human hepatic clearance [https://pubmed.ncbi.nlm.nih.gov/20073997/]
- 22. Improved Assays and Predictive Tools for Drug Lead Optimization [https://www.genengnews.com/insights/improved-assays-and-predictive-tools-for-drug-lead-optimization/]
- 23. | Aurigene Pharmaceutical Services PROTAC [https://www.aurigeneservices.com/protac]
- 24. ADME of Biologics—What Have We Learned from Small Molecules? - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3385832/]
- 25. Strategic Approaches to Optimizing Peptide Properties - PMC ADME [https://pmc.ncbi.nlm.nih.gov/articles/PMC4287298/]
- 26. Unlocking the Potential of Peptide Therapeutics: A Conversation with... [https://www.linkedin.com/pulse/unlocking-potential-peptide-therapeutics-conversation-dr-haoqing-07nvc]
- 27. Driving success with peptide lead optimization [https://www.news-medical.net/whitepaper/20251009/Driving-success-with-peptide-lead-optimization-solutions.aspx]
- 28. In vitro ADME phenotyping in drug discovery: current challenges and... [https://pubmed.ncbi.nlm.nih.gov/15679175/]
- 29. Membrane transporters in drug development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3326076/]
- 30. Understanding enzyme or transporter -based drug interactions [https://www.sps.nhs.uk/articles/understanding-enzyme-or-transporter-based-drug-interactions/]
- 31. Methods of Measuring Enzyme Activity Ex vivo and In vivo - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6147230/]
- 32. Compounds: Defining Inhibition / Induction Processes | Open Systems... [https://docs.open-systems-pharmacology.org/v9/working-with-pk-sim/pk-sim-documentation/pk-sim-compounds-defining-inhibition-induction-processes]
- 33. Physiologically based pharmacokinetic modelling to predict drug-drug... [https://pubmed.ncbi.nlm.nih.gov/37609899/]
- 34. Enhancing Drug Discovery: Quantum Machine Learning for QSAR Prediction with Incomplete Data [https://arxiv.org/html/2501.13395]
- 35. Current status and future directions of high-throughput ADME screening in drug discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7322755/]
- 36. Tailored ADME solutions for specific research goals [https://www.news-medical.net/whitepaper/20241003/Exploring-tailored-ADME-solutions-for-specific-research-goals.aspx]
- 37. The Trends and Future Prospective of In Models from the... Silico [https://pmc.ncbi.nlm.nih.gov/articles/PMC10675155/]
- 38. Improving ADME Prediction with Multitask Graph Neural Networks and Assessing Explainability in Lead Optimization | Biological and Medicinal Chemistry | ChemRxiv | Cambridge Open Engage [https://chemrxiv.org/engage/chemrxiv/article-details/680aee7350018ac7c512f652]
- 39. In-silico ADME models: a general assessment of their utility in drug discovery applications - PubMed [https://pubmed.ncbi.nlm.nih.gov/21320065/]
- 40. Could graph neural networks learn better molecular representation for drug discovery? A comparison study of descriptor-based and graph-based models | Journal of Cheminformatics | Full Text [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-020-00479-8]
- 41. and simulation in drug research and development... PBPK modeling [https://pmc.ncbi.nlm.nih.gov/articles/PMC5125732/]
- 42. Application of Physiologically-Based Pharmacokinetic ( PBPK ) Model ... [https://link.springer.com/article/10.1007/s40495-025-00427-w]
- 43. Real-world application of physiologically based pharmacokinetic models in drug discovery - PubMed [https://pubmed.ncbi.nlm.nih.gov/39884820/]
- 44. Physiologically Based Pharmacokinetic Modeling and Dose ... [https://www.dovepress.com/physiologically-based-pharmacokinetic-modeling-and-dose-optimization-o-peer-reviewed-fulltext-article-DDDT]
- 45. Next-generation risk assessment: integrating in vitro data and... [https://repositorio.bc.ufg.br/items/ce6e3022-743f-4970-8a8f-7c4a598e54a8]
- 46. Events- Simulations Plus [https://www.simulations-plus.com/events/integrating-pbpk-modeling-and-developability-assessment-to-guide-early-phase-formulation-strategy/]
- 47. Utility of physiologically based pharmacokinetic modeling in predicting and characterizing clinical drug interactions - PubMed [https://pubmed.ncbi.nlm.nih.gov/39884811/]
- 48. Blog | Integrating in silico tools with Organ - on - a - chip | CN Bio [https://cn-bio.com/integrating-in-silico-tools-with-organ-on-a-chip-to-advance-adme-studies/]
- 49. Integrating In Silico Tools with Organ - on - a - chip to Advance ADME ... [https://www.linkedin.com/pulse/integrating-silico-tools-organ-on-a-chip-advance-adme-studies-cnbio-cosae]
- 50. 6 Challenges in ADME Drug Development - CN Bio [https://cn-bio.com/6-challenges-in-adme-drug-development/]
- 51. : Next Generation Microphysiological for... Systems Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC7546538/]
- 52. Organ-on-a-chip - Wikipedia [https://en.wikipedia.org/wiki/Organ-on-a-chip]
- 53. Human-on-a-Chip: How Multi-Organ Systems Are Changing ADME Studies [https://openmedscience.com/human-on-a-chip-how-multi-organ-systems-are-changing-adme-studies/]
- 54. CN Bio adds computational modeling capabilities to ADME services for... [https://www.news-medical.net/news/20250903/CN-Bio-adds-computational-modeling-capabilities-to-ADME-services-for-enhanced-bioavailability-profiling.aspx]
- 55. assays for In testing vivo zebrafish toxicity [https://pubmed.ncbi.nlm.nih.gov/15679177/]
- 56. Use of Zebrafish in Drug Discovery Toxicology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7162671/]
- 57. Lead Optimization and ADME with Prediction | ZeClinics Zebrafish [https://www.zeclinics.com/?p=11550]
- 58. for ischemic stroke using larvae and adult Drug ... screening zebrafish [https://labanimres.biomedcentral.com/articles/10.1186/s42826-024-00232-4]
- 59. Diving into drug - screening : zebrafish embryos as an in vivo platform... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11078164/]
- 60. for detecting Zebrafish and drugs efficacy as screening model toxicity [https://www.oaepublish.com/articles/2572-8180.2017.15]
- 61. Atoxigen - ADME Tox model of zebrafish in the embryo-larvae stage [https://atoxigen.com/en/our-services/predictive-toxicology/zebrafish/]
- 62. versus Animal oral drug human : do they bioavailability ? correlate [https://pubmed.ncbi.nlm.nih.gov/23988844/]
- 63. Testing & Analysis Services - BOC Sciences ADME [https://www.solutions.bocsci.com/adme-testing.html]
- 64. Addressing Today's Absorption, Distribution, Metabolism, and Excretion... [https://pubmed.ncbi.nlm.nih.gov/34620695/]
- 65. : Uses, Interactions, Mechanism of Action | DrugBank Online Risdiplam [https://go.drugbank.com/drugs/DB15305]
- 66. Risdiplam distributes and increases SMN protein in both the central nervous system and peripheral organs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6262736/]
- 67. Estimation of FMO3 Ontogeny by Mechanistic Population... [https://link.springer.com/article/10.1007/s40262-023-01241-7]
- 68. A phase 1 healthy male volunteer single escalating dose study of the... [https://pubmed.ncbi.nlm.nih.gov/30302786/]
- 69. A Comprehensive Review on Current Advances in Peptide Drug Development and Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6566176/]
- 70. Protocol for iterative optimization of modified peptides bound to protein targets - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9640467/]
- 71. Residue-Specific Peptide Modification: A Chemist’s Guide - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5792174/]
- 72. on drug interaction studies - Scientific guideline ICH M 12 [https://www.ema.europa.eu/en/ich-m12-drug-interaction-studies-scientific-guideline]
- 73. Studies: Summary of the Efforts to Achieve... ICH M 12 Drug Interaction [https://pubmed.ncbi.nlm.nih.gov/40108838/]
- 74. Guideline: 4 Key Updates and... - WuXi AppTec DMPK ICH M 12 [https://dmpkservice.wuxiapptec.com/articles/423-ich-m12-guideline-4-key-updates-and-reshaping-framework-for-enzyme-mediated-drug-drug-interaction-studies/]
- 75. Guidelines & Your ICH - M Package 12 Drug Drug Interaction [https://www.certara.com/blog/ich-m12-guidelines-and-your-drug-drug-interaction-package/]
- 76. EMA Implementation of ICH E6, M11 & M - ECA Academy 12 [https://www.gmp-compliance.org/gmp-news/ema-implementation-of-ich-e6-m11-m12]
- 77. 7 strategies to improve PROTACs ' oral - Drug... bioavailability [https://www.drugdiscoverytrends.com/7-strategies-to-improve-protacs-oral-bioavailability/]
- 78. How to Improve PROTACs ' Oral - WuXi AppTec DMPK Bioavailability [https://dmpkservice.wuxiapptec.com/blogs/16-how-to-improve-protacs-oral-bioavailability/]
- 79. Frontiers | Grand challenges in oral drug delivery [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1571982/full]
- 80. Validating ADME QSAR Models Using Marketed Drugs - PubMed [https://pubmed.ncbi.nlm.nih.gov/34176369/]
- 81. Small-Molecule Drug Discovery: Processes, Perspectives, Candidate ... [https://www.chromatographyonline.com/view/small-molecule-drug-discovery-processes-perspectives-candidate-selection-and-career-opportunities-for-analytical-chemists]
- 82. Insilico Medicine announces preclinical drug ... discovery benchmarks [https://www.news-medical.net/news/20250211/Insilico-Medicine-announces-preclinical-drug-discovery-benchmarks-from-2021-to-2024.aspx]
- 83. Lipinski's rule five - Wikipedia of [https://en.wikipedia.org/wiki/Lipinski%27s_rule_of_five]
- 84. ADME-Space: a new tool for medicinal chemists to explore ADME properties | Scientific Reports [https://www.nature.com/articles/s41598-017-06692-0]
- 85. Predicting In Vivo Efficacy from In Vitro Data: Quantitative Systems Pharmacology Modeling for an Epigenetic Modifier Drug in Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7070804/]
- 86. The graphical representation of ADME-related molecule properties for medicinal chemists - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1359644610008056]
- 87. Frontiers | An in and vitro Pharmacokinetic Study of... ADME in vivo [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2019.00120/full]
- 88. Analytical Solutions for High Throughput ADME Studies | Waters [https://www.waters.com/nextgen/us/en/library/application-notes/2024/analytical-solutions-for-high-throughput-adme-studies.html]
- 89. and In Prediction | SpringerLink Vitro In Silico ADME [https://link.springer.com/chapter/10.1007/978-3-319-99593-9_13]
- 90. Frontiers | In vitro technology and ADMET research in traditional Chinese medicine [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1605330/full]
- 91. Preclinical in vivo ADME studies in drug development: a critical review - PubMed [https://pubmed.ncbi.nlm.nih.gov/22248306/]
- 92. Recent advances in the translation of drug metabolism and pharmacokinetics science for drug discovery and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9214059/]
- 93. Combined shake-flask, chromatographic and in approaches for... silico [https://pubmed.ncbi.nlm.nih.gov/40462676/]
- 94. A Guide to In Vitro ADME Testing in Drug Development • WuXi AppTec Lab Testing Division [https://labtesting.wuxiapptec.com/2022/06/23/in-vitro-adme-testing-in-drug-developmenta-short-guide/]
- 95. Utilizing in and vitro tools to link PBPK characteristics to... ADME [https://pubmed.ncbi.nlm.nih.gov/23696038/]
- 96. Human radiolabeled mass studies supporting the FDA... balance [https://pmc.ncbi.nlm.nih.gov/articles/PMC9652429/]
- 97. Beyond single-dose human mass : minimizing subject... balance study [https://pubmed.ncbi.nlm.nih.gov/41145078/]
- 98. What is a Human Mass (ADME) Balance ? | Allucent Study [https://www.allucent.com/resources/blog/what-human-mass-balance-study]