Principles of Rational Drug Design: A Modern Framework for Targeted Therapeutics
This article provides a comprehensive overview of the principles and practices of Rational Drug Design (RDD), a systematic approach that leverages knowledge of biological targets to develop new medications.
Principles of Rational Drug Design: A Modern Framework for Targeted Therapeutics
Abstract
This article provides a comprehensive overview of the principles and practices of Rational Drug Design (RDD), a systematic approach that leverages knowledge of biological targets to develop new medications. Tailored for researchers, scientists, and drug development professionals, the content spans from foundational concepts and target identification to advanced computational methodologies like Structure-Based and Ligand-Based Drug Design. It further addresses critical challenges in optimization, the rigorous process of preclinical and clinical validation, and a comparative analysis with traditional discovery methods. By synthesizing current literature and recent technological advances, this guide serves as a resource for streamlining the drug discovery pipeline and developing safer, more effective therapeutics.
What is Rational Drug Design? Foundations and Core Concepts
Rational Drug Design (RDD) represents a fundamental shift from traditional, empirical drug discovery methods to a targeted, knowledge-driven approach. This methodology uses three-dimensional structural information about biological targets and computational technologies to design therapeutic agents with specific desired properties, moving beyond the trial-and-error paradigm that has long dominated pharmaceutical development [1]. The core principle of RDD is the strategic modification of functional chemical groups based on considerations of structure-activity relationships (SARs) to improve drug candidate effectiveness [1]. This approach has evolved significantly since its initial formalization in the 1950s, with landmark successes in the 1970s and 1980s including cholesterol-lowering lovastatin and antihypertensive captopril, which remain in clinical use today [1].
The contemporary landscape of drug discovery has been transformed by recent advancements in bioinformatics and cheminformatics, creating unprecedented opportunities for RDD [2]. Key techniques including structure- and ligand-based virtual screening, molecular dynamics simulations, and artificial intelligence-driven models now allow researchers to explore vast chemical spaces, investigate molecular interactions, predict binding affinity, and optimize drug candidates with remarkable accuracy and efficiency [2]. These computational methods complement experimental techniques by accelerating the identification of viable drug candidates and refining lead compounds, ultimately reducing the resource-intensive nature of drug discovery, which traditionally costs approximately USD 2.6 billion and takes over 12 years to bring a new therapeutic agent to market [1].
Core Principles and Methodologies of Rational Drug Design
The Conceptual Framework of RDD
Rational Drug Design operates on several foundational principles that distinguish it from traditional approaches. At its core, RDD relies on the concept that understanding the molecular basis of disease enables the deliberate design of interventions that specifically modulate pathological processes. This approach begins with identifying a biological target—such as DNA, RNA, or a specific protein—that plays a particular role in disease development [1]. The process then proceeds to identify hit compounds that can interact with the chosen biological target, followed by optimization of their chemical structures and drug properties to develop lead compounds [1].
The methodological ideal of RDD involves continuous reinforcement between theoretical insights into drug-receptor interactions and hands-on drug testing [1]. This iterative process depends heavily on molecular modeling used in conjunction with optimization cycles that rely on structure-activity relationships (SARs) to strategically modify functional chemical groups with the aim of improving drug candidate effectiveness [1]. The well-established method of bioisosteric replacement exemplifies this approach, involving finding the balance between maintaining desired biological activity and optimizing drug-related properties that influence efficacy, such as solubility, lipophilicity, stability, selectivity, non-toxicity, and absorption [1].
Key Computational Methods in Modern RDD
Modern RDD employs a sophisticated array of computational methods that have revolutionized early-stage drug discovery:
- Structure-Based Virtual Screening: This method uses three-dimensional structural information about biological targets to computationally screen large libraries of compounds for potential binding affinity and biological activity [2].
- Ligand-Based Virtual Screening: When structural information about the target is limited, this approach uses known active compounds to identify new candidates with similar properties [2].
- Molecular Dynamics Simulations: These simulations model the physical movements of atoms and molecules over time, providing insights into molecular interactions, binding mechanisms, and conformational changes [2].
- Pharmacophore Modeling: This technique identifies the essential spatial arrangement of molecular features necessary for biological activity, serving as a template for identifying or designing new active compounds [1].
- Artificial Intelligence-Driven Models: AI and machine learning algorithms now play an important role in predicting key properties such as binding affinity and toxicity, contributing to more informed decision-making early in the drug discovery process [2].
The Emergence of Informatics-Driven Approaches
A significant advancement in modern RDD is the concept of the "informacophore," which extends traditional pharmacophore models by incorporating data-driven insights derived not only from SARs but also from computed molecular descriptors, fingerprints, and machine-learned representations of chemical structure [1]. This fusion of structural chemistry with informatics enables a more systematic and bias-resistant strategy for scaffold modification and optimization. Unlike traditional pharmacophore models rooted in human-defined heuristics and chemical intuition, informacophores leverage the ability of machine learning algorithms to process vast amounts of information rapidly and accurately, identifying hidden patterns beyond human capacity [1].
The development of ultra-large, "make-on-demand" or "tangible" virtual libraries has significantly expanded the range of accessible drug candidate molecules, with suppliers like Enamine and OTAVA offering 65 and 55 billion novel make-on-demand molecules respectively [1]. To screen such vast chemical spaces, ultra-large-scale virtual screening for hit identification becomes essential, as direct empirical screening of billions of molecules is not feasible [1].
Table 1: Key Computational Methods in Rational Drug Design
| Method | Primary Function | Data Requirements | Applications |
|---|---|---|---|
| Structure-Based Virtual Screening | Identify compounds with binding affinity to target | 3D structure of biological target | Hit identification, lead optimization |
| Ligand-Based Virtual Screening | Identify compounds similar to known actives | Chemical structures of known active compounds | Hit expansion, scaffold hopping |
| Molecular Dynamics Simulations | Model molecular interactions over time | Atomic coordinates, force field parameters | Binding mechanism analysis, conformational sampling |
| Pharmacophore Modeling | Define essential features for biological activity | Active compounds, optionally target structure | Virtual screening, de novo design |
| AI/ML Models | Predict compound properties and activity | Large datasets of compounds with annotated properties | Property prediction, chemical space exploration |
Experimental Validation: Bridging In Silico Predictions and Therapeutic Reality
While computational tools and AI have revolutionized early-stage drug discovery, these in silico approaches represent only the starting point of a much broader experimental validation pipeline [1]. Theoretical predictions—including target binding affinities, selectivity, and potential off-target effects—must be rigorously confirmed through biological functional assays to establish real-world pharmacological relevance [1]. These assays, which include enzyme inhibition, cell viability, reporter gene expression, or pathway-specific readouts conducted in vitro or in vivo, offer quantitative, empirical insights into compound behavior within biological systems [1].
The critical data provided by biological functional assays validate or challenge AI-generated predictions and provide feedback into SAR studies, guiding medicinal chemists to design analogues with improved efficacy, selectivity, and safety [1]. This iterative feedback loop—spanning prediction, validation, and optimization—is central to the modern drug discovery process [1]. Advances in assay technologies, including high-content screening, phenotypic assays, and organoid or 3D culture systems, offer more physiologically relevant models that enhance translational relevance and better predict clinical success [1].
Several notable drug discovery case studies exemplify this synergy between computational prediction and experimental validation:
- Baricitinib: A repurposed JAK inhibitor identified by BenevolentAI's machine learning algorithm as a candidate for COVID-19, which required extensive in vitro and clinical validation to confirm its antiviral and anti-inflammatory effects, ultimately supporting its emergency use authorization [1].
- Halicin: A novel antibiotic discovered using a neural network trained on a dataset of molecules with known antibacterial properties; biological assays were crucial to confirming its broad-spectrum efficacy against multidrug-resistant pathogens in both in vitro and in vivo models [1].
- Vemurafenib: A BRAF inhibitor for melanoma initially identified via high-throughput in silico screening targeting the BRAF (V600E)-mutant kinase, with computational promise validated through cellular assays measuring ERK phosphorylation and tumor cell proliferation [1].
These cases underscore a fundamental principle in modern drug development: without biological functional assays, even the most promising computational leads remain hypothetical. Only through experimental validation is therapeutic potential confirmed, enabling medicinal chemists to make informed decisions in the iterative process of drug optimization [1].
Research Reagent Solutions for RDD Experimental Protocols
The experimental validation of computationally designed drug candidates requires specialized reagents and materials. The following table details essential research reagents and their applications in rational drug design workflows.
Table 2: Essential Research Reagents for Rational Drug Design Validation
| Reagent/Material | Function in RDD | Specific Application Examples |
|---|---|---|
| Ultra-Large Virtual Compound Libraries | Provide vast chemical space for virtual screening | Enamine (65 billion compounds), OTAVA (55 billion compounds) for hit identification [1] |
| Biological Functional Assays | Validate computational predictions empirically | Enzyme inhibition, cell viability, reporter gene expression assays [1] |
| High-Content Screening Systems | Enable multiparametric analysis of compound effects | Phenotypic screening, mechanism of action studies [1] |
| Organoid/3D Culture Systems | Provide physiologically relevant disease models | Enhanced translational prediction during preclinical validation [1] |
| ADMET Profiling Assays | Evaluate absorption, distribution, metabolism, excretion, and toxicity | In vitro and in vivo assessment of drug candidate properties [1] |
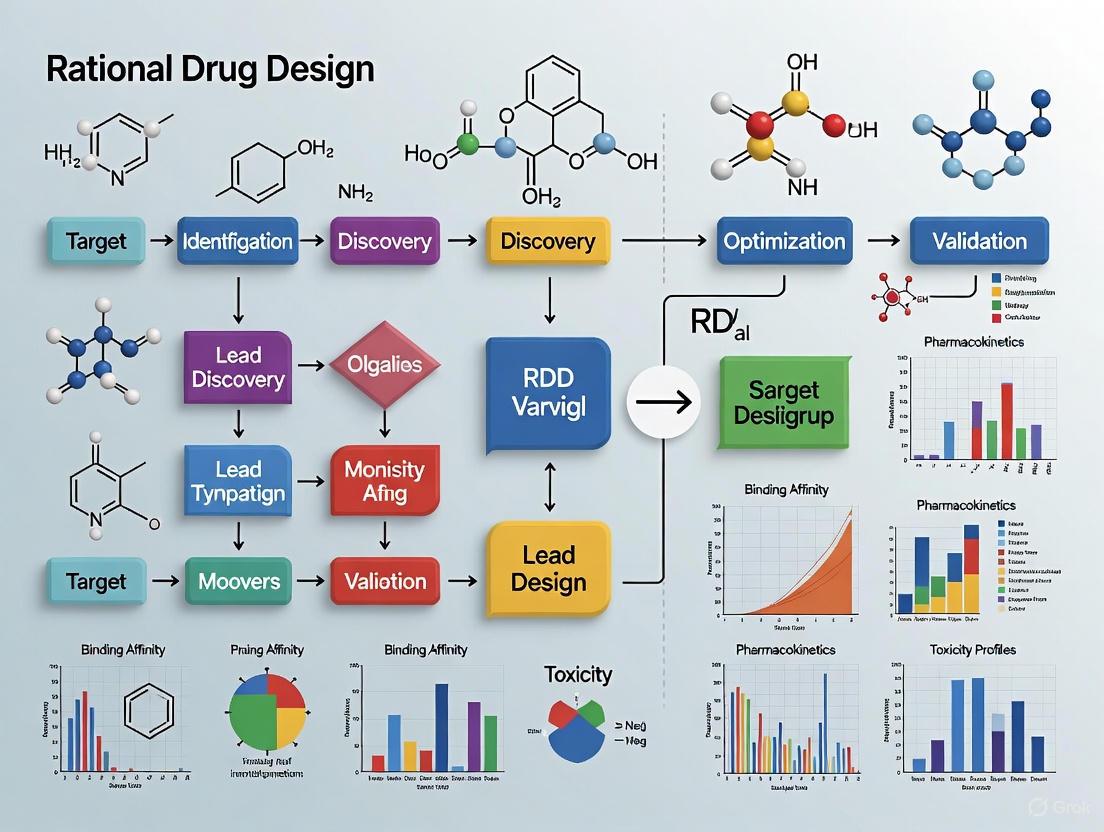
Visualization of RDD Workflows and Conceptual Frameworks
Rational Drug Design Methodology Workflow
Informatics-Driven Drug Discovery Paradigm
Rational Drug Design has evolved from its origins in theoretical drug-receptor interactions to become an informatics-driven discipline that systematically addresses the complexities of drug discovery. The integration of computational prediction with experimental validation creates a powerful framework for identifying and optimizing therapeutic agents, significantly advancing beyond traditional trial-and-error approaches. Despite these advancements, challenges remain in terms of accuracy, interpretability, and computational power requirements for current RDD methodologies [2].
The future of RDD lies in enhancing the synergy between computational and experimental approaches, with emerging technologies such as AI-driven models, structural bioinformatics, and advanced simulation techniques playing increasingly important roles [2]. As these methods continue to evolve, rational drug design is poised to further accelerate the drug development pipeline, reduce costs, and improve the success rate of bringing new therapeutics to market. The continued refinement of informacophore approaches and the expansion of accessible chemical spaces will likely drive innovations in targeted therapeutic development, ultimately enabling more precise and effective treatments for complex diseases.
In the field of modern pharmaceutical sciences, biological targets represent the foundational cornerstone upon which rational drug design (RDD) is built. These targets, predominantly proteins, enzymes, and receptors, are biomolecules within the body that specifically interact with drugs to regulate disease-related biological processes [3]. The identification and characterization of these targets form the most crucial and foundational step in drug discovery and development, largely determining the efficiency and success of pharmaceutical research [3] [4]. Rational drug design strategically exploits the detailed recognition and discrimination features associated with the specific arrangement of chemical groups in the active site of target macromolecules, enabling researchers to conceive new molecules that can optimally interact with these proteins to block or trigger specific biological actions [5].
Biological targets can be categorized based on their functions and mechanisms of action into several classes, including enzymes, receptors, ion channels, transport proteins, and nucleic acids [3]. The critical role these targets play in cellular signal transduction, metabolic pathways, and gene expression establishes their central position in drug discovery. The lock-and-key model, initially proposed by Emil Fischer in 1890, and its extension to the induced-fit theory by Daniel Koshland in 1958, provide conceptual frameworks for understanding how biological 'locks' (targets) possess unique stereochemical features that allow precise interaction with 'keys' (drug molecules) [5]. This molecular recognition process forms the fundamental basis of rational drug design, wherein both ligand and target may mutually adapt through conformational changes to achieve an optimal fit [5].
Table 1: Major Classes of Biological Targets in Drug Discovery
| Target Class | Key Characteristics | Therapeutic Significance | Example Targets |
|---|---|---|---|
| Enzymes | Catalyze biochemical reactions; often have well-defined active sites | Inhibition or activation modulates metabolic pathways | Kinases, Proteases, Polymerases |
| Receptors | Transmembrane or intracellular proteins that bind signaling molecules | Regulate cellular responses to hormones, neurotransmitters | GPCRs, Nuclear Receptors |
| Ion Channels | Gate flow of ions across cell membranes | Control electrical signaling and cellular homeostasis | Voltage-gated Na+ channels, GABA receptors |
| Transport Proteins | Facilitate movement of molecules across biological barriers | Affect drug distribution and nutrient uptake | Transporters for neurotransmitters, nutrients |
Principles of Rational Drug Design Approaches
Rational drug design represents a paradigm shift from traditional trial-and-error approaches to a methodical process grounded in structural and mechanistic understanding of target molecules. This approach proceeds through three fundamental steps: design of compounds that conform to specific structural requirements, synthesis of these molecules, and rigorous biological testing, with further rounds of refinement and optimization based on results [5]. The overarching goal of RDD is to lessen drug discovery duration and expenses through strategic narrowing of drug-like compounds in the discovery pipeline, addressing the prohibitive costs (2-3 billion dollars) and extended timelines (12-15 years) associated with traditional drug development [4].
Two primary methodologies dominate rational drug design: structure-based (receptor-based) and pharmacophore-based (ligand-based) approaches. Structure-based drug design (SBDD) directly exploits the three-dimensional structural information of the target protein, typically obtained through experimental methods like X-ray crystallography or NMR, or through computational approaches like homology modeling [4] [5]. This "direct" design approach allows researchers to visualize and utilize detailed 3D features of the active site, introducing appropriate functionalities in designed ligands to create favorable interactions [5]. The key steps in SBDD include preparation of the protein structure, identification of binding sites, ligand preparation, and docking with scoring functions to evaluate potential interactions [4].
In contrast, pharmacophore-based drug design serves as an indirect approach employed when the three-dimensional structure of the target protein is unavailable [5]. This method extracts critical information from the stereochemical and physicochemical features of known active molecules, generating hypotheses about ligand-receptor interactions through analysis of structural variations across compound series [5]. The strategy of "molecular mimicry" enables researchers to position the 3D relative location of structural elements recognized as necessary in active molecules into new chemical entities, facilitating the design of compounds that mimic natural substrates, hormones, or cofactors like ATP, dopamine, histamine, and estradiol [5]. When applied to peptides, this approach extends to "peptidomimetics," designing non-peptide molecules that mimic peptide functionality while overcoming developmental challenges associated with peptide-based drugs [5].
The ideal scenario in rational drug design involves synergistic integration of both structure-based and ligand-based approaches, where promising docked molecules designed through favorable interactions with the target protein are compared to active structures, and interesting mimics of active compounds are docked into the protein to assess convergent conclusions [5]. This synergy substantially accelerates the discovery process but depends critically on establishing correct binding modes of ligands within the target's active site [5].
Target Identification and Validation Strategies
The initial stages of drug discovery involve the precise identification and validation of disease-modifying biological targets, a process that has been revolutionized by advanced technologies and methodologies. Drug targets typically refer to biomolecules within the body that can specifically bind with drugs to regulate disease-related biological processes, while novel targets encompass biomolecules related to disease but not yet successfully targeted in clinical settings [3]. These novel targets include newly discovered unverified biomolecules, proteins recently associated with disease mechanisms, targets with mechanistic support but lacking known modulators, known targets repurposed for new indications, and synergistic or combinatorial targets with at least one unverified component [3]. Additionally, "undruggable" proteins—those characterized by flat functional interfaces lacking defined pockets for ligand interaction—represent a significant category of challenging targets [6].
Target identification has entered a new era with the integration of artificial intelligence and multi-omics technologies. AI-based approaches can be trained on large-scale biomedical datasets to perform data-driven, high-throughput analyses, integrating multimodal data such as gene expression profiles, protein-protein interaction networks, chemical structures, and biological pathways to perform comprehensive inference [3]. Genomics approaches leverage AI methods to mine multi-layered information including genome-wide variant effects, functional annotations, gene interactions, expression and regulation, epigenetic modifications, protein-DNA interactions, and gene-disease associations [3]. Single-cell omics technologies represent a cutting-edge advancement that enables resolution of genomic, transcriptomic, proteomic, and metabolomic profiles at the single-cell level, systematically characterizing cellular heterogeneity, identifying rare cell subsets, and dissecting dynamic cellular processes and spatial distributions [3].
Perturbation omics provides a critical causal reasoning foundation for target identification by introducing systematic perturbations and measuring global molecular responses [3]. This framework includes genetic-level perturbations (single-gene and multi-gene perturbations) and chemical-level perturbations (small molecules and diverse compound libraries), with AI techniques such as neural networks, graph neural networks, causal inference models, and generative models significantly enhancing analytical power to simulate interventions and reveal functional targets [3]. Structural biology AI models, including tools like AlphaFold for protein structure prediction, complement these approaches by providing atomic-level structural insights and dynamic conformational analyses essential for target identification [3].
Despite these technological advancements, target discovery still faces substantial challenges, including complex disease mechanisms involving multiple signaling pathways and gene networks, data complexity and integration challenges with heterogeneous and noisy omics data, target validation difficulties requiring substantial experimental efforts, and challenges in clinical translation where promising targets in vitro or in animal models may not translate into clinical efficacy [3].
Table 2: Key Databases and Tool Platforms for Target Identification
| Database Category | Primary Function | Representative Examples |
|---|---|---|
| Omics Databases | Provide large-scale cross-omics and cross-species data | Genomics, transcriptomics, proteomics databases [3] |
| Structure Databases | Archive 3D structural information of biological macromolecules | Protein Data Bank (PDB), structural classification databases [3] |
| Knowledge Bases | Construct multi-dimensional association networks of genes, diseases, and drugs | Disease-gene association databases, drug-target interaction databases [3] |
"Undruggable" Targets: Challenges and Innovative Solutions
A significant frontier in rational drug design involves tackling "undruggable" targets—proteins characterized by large, complex structures or functions that are difficult to interfere with using conventional drug design strategies [6]. These challenging targets typically lack defined hydrophobic pockets for ligand binding, instead featuring shallow, polar surfaces that resist traditional small-molecule interaction [6]. The term "undruggable" particularly applies to several protein classes: Small GTPases (including KRAS, HRAS, and NRAS), Phosphatases (both protein tyrosine phosphatases and protein serine/threonine phosphatases), Transcription factors (such as p53, Myc, estrogen receptor, and androgen receptor), specific Epigenetic targets, and certain Protein-Protein Interaction interfaces with flat interaction surfaces [6].
Among these, KRAS represents a paradigmatic example of historical "undruggability." As the most frequently mutated oncogene protein with varying mutation rates in different solid tumors, KRAS experienced prolonged clinical drug vacancy due to its shallow surface pocket with undesired polarity [6]. The protein alternates between inactive GDP-bound and active GTP-bound states, regulated by guanine nucleotide exchange factors and GTPase activating proteins [6]. The breakthrough came in 2021 with the FDA approval of sotorasib, a covalent KRASG12C inhibitor for non-small cell lung cancer, validating that targeting "undruggable" proteins is achievable through innovative approaches [6].
Several strategic frameworks have emerged to address these challenging targets:
Covalent Regulation: Covalent inhibitors bind to amino acid residues of target proteins through covalent bonds formed by mildly reactive functional groups, conferring additional affinity compared to non-covalent inhibitors [6]. These inhibitors offer advantages of sustained inhibition and longer residence time, as the covalently bound target remains continuously inhibited until protein degradation and regeneration [6]. This approach reduces dosage requirements, improves patient compliance, and can overcome some resistance mechanisms.
Targeted Protein Degradation (TPD): This groundbreaking advancement employs small molecules to tag undruggable proteins for degradation via the ubiquitin-proteasome system or autophagic-lysosomal system [7]. Unlike traditional inhibitors that aim to block protein activity, TPD technologies completely remove disease-associated proteins from the cellular environment, providing a novel therapeutic paradigm for conditions where conventional small molecules have fallen short [7]. Proteolysis Targeting Chimeras represent a prominent example of this approach.
Allosteric Inhibition: Rather than targeting traditional active sites, allosteric inhibitors bind to alternative, often less conserved sites on protein surfaces, inducing conformational changes that disrupt protein function [6]. This approach offers enhanced selectivity and the potential to overcome resistance mutations that affect active-site binding.
DNA-Encoded Libraries (DELs): This technology allows for high-throughput screening of vast chemical libraries by utilizing DNA as a unique identifier for each compound, facilitating simultaneous testing of millions of small molecules against biological targets [7]. DELs enable efficient exploration of chemical diversity and streamline identification of potential drug candidates for challenging targets.
Experimental and Computational Methodologies
The drug discovery pipeline employs a diverse array of experimental and computational methodologies to identify and validate biological targets and their modulators. Structure-based drug design relies heavily on techniques such as X-ray crystallography and nuclear magnetic resonance to elucidate the three-dimensional structures of target proteins [4]. These structural insights provide the foundation for molecular docking simulations, which computationally predict the binding orientation and affinity of small molecules within target binding sites [4]. Molecular dynamics simulations further extend these static pictures by modeling the dynamic behavior of protein-ligand complexes under physiological conditions, providing critical information about binding stability and conformational changes [3].
Advanced computational approaches have revolutionized target identification and validation. Computer-Aided Drug Design employs computational methods to predict the binding affinity of small molecules to specific targets, significantly reducing the time and resources required for experimental screening [7]. With advancements in artificial intelligence, CADD has become increasingly sophisticated, enabling researchers to simulate complex biological interactions and refine drug design more effectively [7]. AI-driven structure prediction tools, such as AlphaFold, generate static structural models that provide the basis for systematically annotating potential binding sites across proteomes [3]. These models serve as initial conformations for AI-enhanced molecular dynamics simulations, which extend simulation timescales while maintaining atomic resolution, enabling identification of cryptic binding pockets and characterization of allosteric regulation mechanisms [3].
Fragment-based drug discovery represents another powerful approach that leverages stochastic screening and structure-based design to identify small molecular fragments that bind weakly to target proteins, which are then optimized into high-affinity ligands [6]. Virtual screening complements this approach through in silico screening techniques premised on the lock-and-key model of drug-target compatibility, rapidly evaluating enormous chemical libraries against target structures [6]. Click chemistry has emerged as a transformative experimental methodology that streamlines the synthesis of diverse compound libraries through highly efficient and selective reactions, particularly the Cu-catalyzed azide-alkyne cycloaddition that selectively produces 1,4-disubstituted 1,2,3-triazoles under mild conditions [7]. This modular approach allows straightforward incorporation of various functional groups, facilitating optimization of lead compounds and enabling creation of complex structures from simple precursors [7].
The emerging paradigm of retro drug design represents a fundamental shift in computational approach. Unlike traditional forward approaches, RDD begins from multiple desired target properties and works backward to generate "qualified" compound structures [8]. This AI strategy utilizes traditional predictive models trained on experimental data for target properties, employing an atom typing-based molecular descriptor system, followed by Monte Carlo sampling to find solutions in the chemical space defined by the target properties, with deep learning models employed to decode molecular structures from these solutions [8].
Table 3: The Scientist's Toolkit: Essential Research Reagents and Platforms
| Tool Category | Specific Technologies | Research Applications |
|---|---|---|
| Structural Biology | X-ray crystallography, NMR spectroscopy, Cryo-EM | Protein structure determination, ligand binding analysis [4] |
| Computational Modeling | Molecular docking, Molecular dynamics simulations, AI-based structure prediction | Binding pose prediction, protein dynamics, binding affinity calculations [3] [4] |
| Compound Screening | DNA-encoded libraries (DELs), Fragment-based screening, High-throughput screening | Hit identification, lead compound discovery [7] [6] |
| Chemical Synthesis | Click chemistry, Combinatorial chemistry, Medicinal chemistry optimization | Compound library synthesis, lead optimization [7] |
| Omics Technologies | Genomics, Transcriptomics, Proteomics, Single-cell omics | Target identification, biomarker discovery, mechanism of action studies [3] |
| AI and Data Science | Machine learning models, Deep neural networks, Multi-modal AI integration | Predictive modeling, chemical space exploration, drug property optimization [3] [8] |
Biological targets—proteins, enzymes, and receptors—maintain their critical role as the foundation of rational drug design, with their identification and validation remaining the most crucial step in the drug discovery process. The field has witnessed remarkable progress in methodologies to approach these targets, from structure-based and ligand-based design to innovative strategies for previously "undruggable" targets. The integration of artificial intelligence and machine learning across all stages of target identification and validation represents a paradigm shift, enabling researchers to navigate the complex landscape of disease mechanisms with unprecedented precision and efficiency [3].
The future of biological target exploration in rational drug design will likely focus on several key areas. Multimodal AI approaches that integrate structural biology and systems biology will become increasingly important, combining atomic-resolution insights into target conformations with dynamic cellular data to reveal physiological relevance [3]. The convergence of advanced technologies such as targeted protein degradation, covalent inhibition strategies, and DNA-encoded libraries with traditional approaches will expand the druggable genome, potentially bringing challenging target classes like transcription factors and phosphatases into therapeutic reach [7] [6]. Furthermore, the growing emphasis on patient-specific variations and personalized medicine will drive need for better understanding of how individual genetic differences affect target vulnerability and drug response.
As these advancements continue to mature, the drug discovery pipeline is poised to become more efficient, predictive, and successful. The integration of large-scale omics data, real-world evidence, and sophisticated computational models will enable more informed decisions in target selection and validation, potentially reducing the high attrition rates that have long plagued pharmaceutical development. Through continued innovation and interdisciplinary collaboration, the field of rational drug design will strengthen its foundational principle: that a deep understanding of biological targets remains the most direct path to transformative therapies.
Rational Drug Design (RDD) represents a foundational shift in pharmaceutical development, moving from traditional trial-and-error approaches to a precise, scientific methodology based on the knowledge of a biological target and its role in disease [9]. This inventive process focuses on the design of molecules that are complementary in shape and charge to their biomolecular target, typically a protein or nucleic acid, to modulate its function and provide a therapeutic benefit [5] [9]. The core principle of RDD is the exploitation of the detailed recognition features associated with the specific arrangement of chemical groups in the active site of a target macromolecule, allowing researchers to conceive new molecules that can optimally interact with the protein to block or trigger a specific biological action [5].
The paradigm of rational drug design is often described as reverse pharmacology because it starts with the hypothesis that modulating a specific biological target will have therapeutic value, in contrast to phenotypic drug discovery which begins with observing a therapeutic effect and later identifying the target [9]. RDD integrates a vast array of scientific disciplines including molecular biology, bioinformatics, structural biology, and medicinal chemistry, aiming to make drug development more accurate, efficient, cost-effective, and time-saving [10]. This meticulous approach makes it possible to develop drugs with optimal safety and effectiveness, thereby transforming therapeutic strategies for combating diseases [10].
Core Principles of Rational Drug Design
Molecular Recognition and Binding Models
The theoretical foundation of rational drug design rests on the principles of molecular recognition—the specific interaction between two or more molecules through non-covalent bonding [5]. These precise recognition and discrimination processes form the basis of all biological organization and regulation.
Two fundamental models describe these interactions:
- Lock-and-Key Model: Proposed by Emil Fischer in 1890, this model suggests that a substrate (key) fits precisely into the active site of a macromolecule (lock), with the biological 'locks' possessing unique stereochemical features necessary for their function [5].
- Induced-Fit Model: Daniel Koshland's 1958 extension of Fischer's model accounts for the conformational changes that occur in both the ligand and target macromolecule during recognition, proposing that both parties mutually adapt through small structural adjustments until an optimal fit is achieved [5].
Approaches to Rational Drug Design
Rational drug design implementation follows two primary methodological approaches, often used synergistically:
Structure-Based Drug Design (SBDD): Also called receptor-based or direct drug design, this approach relies on knowledge of the three-dimensional structure of the biological target obtained through experimental methods such as X-ray crystallography, cryo-electron microscopy (cryo-EM), or NMR spectroscopy [5] [9] [11]. When an experimental structure is unavailable, researchers may create a homology model of the target based on the experimental structure of a related protein [9]. This approach allows medicinal chemists to design candidate drugs that are predicted to bind with high affinity and selectivity to the target using interactive graphics and computational analysis [9].
Ligand-Based Drug Design (LBDD): When the three-dimensional structure of the target protein is not available, researchers employ this indirect approach, which relies on knowledge of other molecules (ligands) that bind to the biological target of interest [5] [9]. These known active molecules are used to derive either a pharmacophore model (defining the minimum necessary structural characteristics a molecule must possess to bind to the target) or a Quantitative Structure-Activity Relationship (QSAR) model, which correlates calculated properties of molecules with their experimentally determined biological activity [9].
The most effective drug discovery projects typically exploit both approaches synergistically, using the structural knowledge from SBDD to guide modifications while leveraging the activity data from LBDD to validate design decisions [5].
Step-by-Step Rational Drug Design Process
Target Identification and Validation
The rational drug design process begins with the critical initial phase of identifying and validating a suitable biological target.
Target Identification involves pinpointing a specific biomolecule (typically a protein or nucleic acid) that plays a key role in the disease process [10] [12]. A "druggable" target must be accessible to the putative drug molecule and, upon binding, elicit a measurable biological response [12]. Various methods are employed for target identification:
- Genomics and Data Mining: Using bioinformatics approaches to analyze available biomedical data, including publications, patent information, gene expression data, and genetic associations to identify and prioritize potential disease targets [10] [12].
- Proteomics: Examining protein profiles in diseased cells to discover potential target molecules [10].
- Phenotypic Screening: Identifying disease-relevant targets through observation of phenotypic changes in cellular or animal models [12].
Target Validation establishes the relevance of the identified biological target in the disease context and confirms that its modulation will produce the desired therapeutic effect [10] [12]. Well-validated targets decrease the risks associated with subsequent drug discovery stages [10]. Key validation techniques include:
- Genetic Techniques: Gene knockout, knock-in, or RNA interference (RNAi) to modulate target expression and observe phenotypic consequences [10] [12].
- Antisense Technology: Using chemically modified oligonucleotides complementary to target mRNA to block synthesis of the encoded protein [12].
- Monoclonal Antibodies: Employing highly specific antibodies to neutralize target function, particularly for cell surface and secreted proteins [12].
- Chemical Genomics: Applying small tool molecules to functionally modulate potential targets in a systematic manner [12].
Table 1: Primary Methods for Target Identification and Validation
| Method Category | Specific Techniques | Key Applications | Considerations |
|---|---|---|---|
| Genomic Approaches | Data mining, genetic association studies, mRNA expression analysis | Identifying targets linked to disease through genetic evidence | Provides correlation but not always functional validation |
| Proteomic Methods | Protein profiling, mass spectroscopy, phage-display antibodies | Discovering proteins highly expressed in disease states | Directly identifies protein targets |
| Genetic Manipulation | Gene knockout, knock-in, RNAi, siRNA | Establishing causal relationship between target and disease | Can produce compensatory mechanisms; expensive and time-consuming |
| Biochemical Tools | Monoclonal antibodies, antisense oligonucleotides | Highly specific target modulation in physiological contexts | Antibodies limited to extracellular targets; oligonucleotides have delivery challenges |
Lead Discovery
Once a target is validated, the lead discovery phase focuses on identifying initial 'hit' compounds with promising characteristics that can potentially be developed into drug candidates [10]. These hit compounds are small molecules that demonstrate both the capacity to interact effectively with the validated drug target and the potential for structural modification to optimize efficacy, safety, and metabolic stability [10].
Multiple strategies are employed for lead discovery:
- High-Throughput Screening (HTS): This traditional method involves experimentally testing large libraries of compounds (often hundreds of thousands) for activity against the target using automated assays [10] [12].
- Virtual Screening: Using computational methods to discover new drug candidates by screening large compound libraries in silico [10] [9]. Molecular docking programs predict how small molecules in a library might bind to the target structure [9] [11].
- Fragment-Based Lead Discovery: Identifying smaller, less complex molecules that bind weakly to the drug target and then combining or growing them to produce a lead compound with higher affinity [10].
- Structure-Based Design: Using the three-dimensional structure of the biological target to find or design compounds that will interact with it [10].
Contemporary approaches are increasingly leveraging artificial intelligence and machine learning to accelerate this process. Recent work demonstrates that integrating pharmacophoric features with protein-ligand interaction data can boost hit enrichment rates by more than 50-fold compared to traditional methods [13].
Diagram 1: Lead Discovery Workflow in Rational Drug Design. This flowchart illustrates the primary pathways for identifying hit compounds depending on the availability of structural information for the biological target.
Lead Optimization
Lead optimization is a crucial phase where initial hit compounds are refined and enhanced to improve their drug-like properties while reducing undesirable characteristics [10]. This process aims to enhance the therapeutic index of potential drug candidates by improving attributes such as potency, selectivity, metabolic stability, and pharmacokinetic profiles while diminishing potential off-target effects and toxicity [10].
Key methods employed in lead optimization include:
- Molecular Modeling: Enables visual analysis and manipulation of lead compounds to understand their three-dimensional properties and interactions with the target [10].
- Quantitative Structure-Activity Relationship (QSAR) Studies: Uses statistical methods to correlate structural features of compounds with their biological activity, enabling prediction of properties for new analogs [10] [14] [15]. Modern QSAR incorporates machine learning algorithms and advanced molecular descriptors to improve predictive accuracy [14] [1].
- Bioisosteric Replacement: A method for strategically replacing certain functional groups in the lead compound with alternatives that have similar physicochemical properties, often without significantly altering the drug's biological activity [10] [1]. This approach helps maintain desired activity while optimizing other drug properties.
- Structure-Based Optimization: Using the three-dimensional structure of the target to guide specific modifications that enhance binding affinity and selectivity [9] [11].
The lead optimization process typically involves multiple iterative Design-Make-Test-Analyze (DMTA) cycles, where compounds are designed, synthesized, tested, and analyzed with each iteration informing the next design phase [13]. Advanced approaches are now compressing these traditionally lengthy cycles from months to weeks through AI-guided retrosynthesis and high-throughput experimentation [13].
Table 2: Key Methodologies in Lead Optimization
| Methodology | Primary Function | Technical Approaches | Output Metrics |
|---|---|---|---|
| Structure-Activity Relationship (SAR) | Elucidate how structural changes affect biological activity | Systematic analog synthesis, biological testing, pattern recognition | Identification of critical functional groups and structural elements |
| Quantitative Structure-Activity Relationship (QSAR) | Quantitatively predict biological activity from molecular structure | Statistical modeling, machine learning, molecular descriptor calculation | Predictive models for activity, selectivity, and ADMET properties |
| Molecular Docking | Predict binding orientation and affinity of ligands | High-throughput virtual screening, high-precision docking, ensemble docking | Binding poses, estimated binding energies, interaction patterns |
| Molecular Dynamics Simulations | Study ligand-receptor interactions under dynamic conditions | Unbiased MD, steered MD, umbrella sampling | Binding stability, conformational changes, transient interactions |
Experimental Validation and Preclinical Development
Before a candidate drug can progress to human trials, it must undergo rigorous experimental validation and preclinical assessment to establish both efficacy and safety [10].
Pharmacokinetics and Toxicity Studies evaluate how the body processes the drug candidate and its potential adverse effects [10]. Key aspects include:
- ADME Profiling: Assessment of Absorption, Distribution, Metabolism, and Excretion characteristics using a combination of in vitro, in vivo, and in silico methods [10] [9] [1].
- Toxicity Studies: Investigation of potential adverse effects through in vitro assays and animal studies [10].
Modern approaches increasingly employ physiologically relevant models such as high-content screening, phenotypic assays, and organoid or 3D culture systems to enhance translational relevance and better predict clinical success [1]. Techniques like Cellular Thermal Shift Assay (CETSA) have emerged as leading approaches for validating direct target engagement in intact cells and tissues, helping to close the gap between biochemical potency and cellular efficacy [13].
Preclinical Trials are conducted in controlled laboratory settings using in vitro methods (test tubes, cell cultures) and in vivo models (laboratory animals) [10]. These studies focus on two major aspects:
- Pharmacodynamics (PD): Studies the biological effects the drug has on the body [10].
- Pharmacokinetics (PK): Examines how the body processes the drug, covering absorption, distribution, metabolism, and excretion [10].
The data collected throughout these validation stages helps optimize final drug formulation, dosage, and administration route before progressing to clinical trials [10].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of rational drug design requires a comprehensive suite of specialized reagents, tools, and platforms. The following table details key resources essential for conducting RDD research.
Table 3: Essential Research Reagents and Tools for Rational Drug Design
| Category | Specific Tools/Reagents | Primary Function | Application Context |
|---|---|---|---|
| Structural Biology Tools | X-ray crystallography platforms, Cryo-EM, NMR spectroscopy | Determine 3D atomic structures of target proteins and protein-ligand complexes | Structure-based drug design, binding site identification, binding mode analysis |
| Virtual Screening Resources | Compound libraries (ZINC, ChEMBL), Commercial "make-on-demand" libraries (Enamine, OTAVA) | Provide vast chemical space for computational screening | Hit identification, lead discovery through virtual screening |
| Computational Software | Molecular docking programs (AutoDock, GOLD); MD software (AMBER, GROMACS); QSAR tools | Predict ligand-receptor interactions, binding affinity, and dynamic behavior | Structure-based design, binding mode prediction, ADMET property estimation |
| Target Engagement Assays | Cellular Thermal Shift Assay (CETSA), surface plasmon resonance (SPR) | Confirm direct binding of compounds to targets in physiologically relevant environments | Validation of target engagement, mechanism of action studies |
| Bioinformatics Databases | Genomic databases (GenBank), protein databases (PDB), gene expression databases | Provide essential biological data for target identification and validation | Target selection, pathway analysis, understanding disease biology |
| ADMET Screening Tools | Caco-2 cell models, liver microsomes, cytochrome P450 assays, hERG channel assays | Predict absorption, distribution, metabolism, excretion, and toxicity properties | Lead optimization, safety profiling, candidate selection |
Current Trends and Future Perspectives
The field of rational drug design continues to evolve rapidly, with several transformative trends shaping its future direction:
Artificial Intelligence and Machine Learning have evolved from disruptive concepts to foundational capabilities in modern drug R&D [13]. Machine learning models now routinely inform target prediction, compound prioritization, pharmacokinetic property estimation, and virtual screening strategies [13]. The emerging concept of the "informacophore" represents a paradigm shift, combining minimal chemical structures with computed molecular descriptors, fingerprints, and machine-learned representations to identify features essential for biological activity [1]. This approach reduces biased intuitive decisions and may accelerate discovery processes [1].
In Silico Screening has become a frontline tool in modern drug discovery [13]. Computational approaches like molecular docking, QSAR modeling, and ADMET prediction are now indispensable for triaging large compound libraries early in the pipeline, enabling prioritization of candidates based on predicted efficacy and developability [13]. These tools have become central to rational screening and decision support [13].
Hit-to-Lead Acceleration through AI and miniaturized chemistry is rapidly compressing traditional discovery timelines [13]. The integration of AI-guided retrosynthesis, scaffold enumeration, and high-throughput experimentation (HTE) enables rapid design-make-test-analyze (DMTA) cycles, reducing discovery timelines from months to weeks [13]. For example, deep graph networks were recently used to generate over 26,000 virtual analogs, resulting in sub-nanomolar inhibitors with a 4,500-fold potency improvement over initial hits [13].
Functional Target Engagement methodologies are addressing the critical need for physiologically relevant confirmation of drug-target interactions [13]. As molecular modalities diversify to include protein degraders, RNA-targeting agents, and covalent inhibitors, technologies like CETSA provide quantitative, system-level validation of direct binding in intact cells and tissues [13].
Integrated Cross-Disciplinary Pipelines are becoming standard in leading drug discovery organizations [13]. The convergence of expertise from computational chemistry, structural biology, pharmacology, and data science enables the development of predictive frameworks that combine molecular modeling, mechanistic assays, and translational insight [13]. This integration supports earlier, more confident decision-making and reduces late-stage surprises [13].
As these trends continue to mature, rational drug design is poised to become increasingly precise, efficient, and successful in delivering novel therapeutics to address unmet medical needs across a broad spectrum of diseases.
Diagram 2: Overview of the Rational Drug Design Pipeline from target identification to clinical trials, highlighting the sequential stages of the drug discovery and development process.
Contrasting Rational Design with Phenotypic Screening (Forward vs. Reverse Pharmacology)
The process of drug discovery has historically been dominated by two contrasting philosophical approaches: rational drug design and phenotypic screening. These methodologies represent fundamentally different paths to identifying and optimizing therapeutic compounds. Rational drug design, also known as reverse pharmacology or target-based drug discovery, begins with a hypothesis about a specific molecular target's role in disease [16] [17]. This approach leverages detailed knowledge of biological structures and mechanisms to deliberately design compounds that interact with predefined targets. In contrast, phenotypic screening, often termed forward pharmacology, employs a more empirical approach by observing compound effects on whole cells, tissues, or organisms without requiring prior understanding of specific molecular targets [18] [19]. The strategic choice between these paradigms has profound implications for research direction, resource allocation, and the nature of resulting therapeutics, forming a core consideration in pharmaceutical research and development.
The resurgence of phenotypic screening over the past decade, after being largely supplanted by target-based methods during the molecular biology revolution, highlights how these approaches exist in a dynamic balance [18]. Modern drug discovery recognizes that both strategies have distinct strengths and applications, with the most effective research portfolios often incorporating elements of both. This technical guide examines the principles, methodologies, and applications of both rational design and phenotypic screening, providing researchers with a comprehensive framework for selecting and implementing these approaches within contemporary drug discovery programs.
Theoretical Foundations and Definitions
Rational Drug Design (Reverse Pharmacology)
Rational drug design constitutes a target-centric approach where drug discovery begins with the identification and validation of a specific biological macromolecule (typically a protein) understood to play a critical role in a disease pathway [5]. The fundamental premise is that modulation of this target's activity will yield therapeutic benefits. This approach requires detailed structural knowledge of the target, often obtained through X-ray crystallography, nuclear magnetic resonance (NMR) spectroscopy, or cryo-electron microscopy [20] [5]. The design process exploits the three-dimensional arrangement of atoms in the target's binding site to conceive molecules that fit complementarily, similar to a key fitting into a lock, though modern interpretations account for mutual adaptability as described by the induced-fit theory [5].
Rational drug design encompasses two primary methodologies: receptor-based design (direct design) when the target structure is known, and pharmacophore-based design (indirect design) when structural information is limited to known active compounds [5]. The power of this approach lies in its systematic nature, allowing researchers to optimize compounds for specific parameters including binding affinity, selectivity, and drug-like properties through iterative design cycles. Rational design has been particularly successful for target classes with well-characterized binding sites and established structure-activity relationships, such as protein kinases and G-protein coupled receptors [20].
Phenotypic Screening (Forward Pharmacology)
Phenotypic screening represents a biology-first approach where compounds are evaluated based on their effects on disease-relevant phenotypes without requiring prior knowledge of specific molecular targets [18] [19]. This strategy acknowledges the incompletely understood complexity of biological systems and disease pathologies, allowing for the discovery of therapeutic effects that might be missed by more reductionist approaches. The philosophical foundation of phenotypic screening is that observing compound effects in realistic disease models can identify beneficial bioactivity regardless of the specific mechanism involved, with target identification (deconvolution) typically following initial compound discovery [19].
Modern phenotypic screening has evolved significantly from earlier observational approaches, now incorporating sophisticated cell-based models, high-content imaging, and transcriptomic profiling to quantify complex phenotypic changes [18] [19]. This approach is particularly valuable for addressing biological processes that involve multiple pathways or complex cellular interactions, where modulating a single target may be insufficient for therapeutic effect. Phenotypic screening has proven especially productive for identifying first-in-class medicines with novel mechanisms of action, expanding the druggable target space beyond what would be predicted from current biological understanding [18].
Historical Context and Evolution
The historical development of these approaches reveals a pendulum swing in pharmaceutical preferences. Traditional medicine and early drug discovery were inherently phenotypic, with remedies developed through observation of their effects on disease states [18] [21]. The isolation of morphine from opium in 1817 by Friedrich Sertürner marked the beginning of systematic compound isolation from natural sources, but still within a phenotypic framework [21]. The molecular biology revolution of the 1980s and the sequencing of the human genome in 2001 catalyzed a major shift toward target-based approaches, promising more efficient and predictable drug discovery [18].
A seminal analysis published in 2011 demonstrated that between 1999 and 2008, a majority of first-in-class drugs were discovered through phenotypic approaches rather than target-based methods [18] [19]. This surprising observation, coupled with declining productivity in pharmaceutical research, spurred a resurgence of interest in phenotypic screening, now augmented with modern tools and strategies [18]. Contemporary drug discovery recognizes both approaches as valuable, with the strategic choice depending on disease understanding, available tools, and program objectives.
Table 1: Key Characteristics of Rational Design and Phenotypic Screening
| Feature | Rational Drug Design | Phenotypic Screening |
|---|---|---|
| Starting Point | Defined molecular target | Disease-relevant phenotype |
| Knowledge Requirement | Target structure and function | Disease biology |
| Primary Screening Output | Target binding or inhibition | Phenotypic modification |
| Target Identification Timing | Before compound discovery | After compound discovery |
| Throughput Potential | High (with automated assays) | Variable (often medium) |
| Chemical Space Exploration | Focused on target-compatible compounds | Unrestricted |
| Success Rate for First-in-Class | Lower | Higher historically |
| Major Challenge | Target validation | Target deconvolution |
Methodological Approaches and Experimental Protocols
Rational Drug Design Methodologies
Structure-Based Drug Design
Structure-based drug design (SBDD) relies on three-dimensional structural information about the biological target, typically obtained through X-ray crystallography, NMR spectroscopy, or cryo-electron microscopy [20] [5]. The process begins with target selection and validation, establishing that modulation of the target will produce therapeutic effects. Once a structure is available, researchers identify potential binding sites and characterize their chemical and steric properties.
The core SBDD workflow involves:
- Binding site characterization - Identifying pockets and clefts on the target surface capable of binding small molecules
- Molecular docking - Computational screening of compound libraries to predict binding poses and affinities
- De novo ligand design - Creating novel molecular structures complementary to the binding site
- Structure-activity relationship (SAR) analysis - Iterative compound optimization based on structural data
Advanced SBDD incorporates molecular dynamics simulations to account for protein flexibility and solvation effects, providing more accurate predictions of binding thermodynamics [20] [2]. Fragment-based drug design (FBDD) represents a specialized SBDD approach that screens low molecular weight fragments (<250 Da) then elaborates or links them into higher-affinity compounds, reversing the traditional probability paradigm of high-throughput screening [20].
Ligand-Based Drug Design
When three-dimensional target structure is unavailable, ligand-based methods provide an alternative rational approach. These techniques utilize known active compounds to infer pharmacophore models - abstract representations of steric and electronic features necessary for molecular recognition [5]. The key methodologies include:
- Pharmacophore modeling - Identifying essential structural features and their spatial relationships
- Quantitative structure-activity relationship (QSAR) analysis - Establishing mathematical relationships between chemical descriptors and biological activity
- Molecular similarity analysis - Identifying novel compounds with structural similarity to known actives
- Scaffold hopping - Discovering novel chemotypes that maintain critical interaction capabilities
These approaches rely on the principle of molecular mimicry, where chemically distinct compounds produce similar biological effects through interaction with the same target [5]. Successful examples include ATP competitive kinase inhibitors that replicate hydrogen-bonding interactions of the natural substrate while improving drug-like properties.
Phenotypic Screening Methodologies
Cell-Based Phenotypic Assays
Modern phenotypic screening employs sophisticated cell-based models that recapitulate key aspects of disease biology. The development of these assays begins with careful model selection to ensure biological relevance and translational potential [19]. Key considerations include:
- Disease relevance - The model should capture critical aspects of the human disease pathology
- Assay robustness - Sufficient reproducibility for screening applications
- Scalability - Compatibility with medium- to high-throughput formats
- Readout relevance - Measured parameters should connect to clinical endpoints
Advanced phenotypic models include patient-derived cells, co-culture systems, 3D organoids, and induced pluripotent stem cell (iPSC)-derived cell types [19]. These systems better capture the cellular context and disease complexity than traditional immortalized cell lines. Readouts extend beyond simple viability to include high-content imaging of morphological changes, transcriptomic profiling, and functional measures such as contractility or electrical activity.
Phenotypic Screening Workflow
A comprehensive phenotypic screening campaign follows a structured workflow:
- Model development and validation - Establishing biologically relevant screening systems
- Primary screening - Testing compound libraries for phenotypic effects
- Hit validation - Confirming activity in secondary assays and counter-screens
- Lead optimization - Improving compound properties through medicinal chemistry
- Target deconvolution - Identifying mechanism of action and molecular targets
- Preclinical development - Advancing optimized leads toward clinical trials
The "rule of 3" for phenotypic screening suggests using at least three different assay systems with orthogonal readouts to triage hits and minimize artifacts [19]. This multi-faceted approach increases confidence that observed activities represent genuine therapeutic potential rather than assay-specific artifacts.
Target Deconvolution in Phenotypic Screening
Target deconvolution - identifying the molecular mechanism of action for phenotypically active compounds - represents one of the most significant challenges in phenotypic screening [18] [19]. Several experimental approaches have been developed for this purpose:
- Affinity purification - Using modified compound versions to capture interacting proteins
- Genetic approaches - CRISPR-based screens to identify genes that modify compound sensitivity
- Proteomic profiling - Assessing global protein expression or phosphorylation changes
- Transcriptomic profiling - Comparing gene expression signatures to reference databases
- Resistance generation - Selecting and characterizing resistant clones to identify targets
Each method has strengths and limitations, making a combination of approaches most effective for confident target identification. For some therapeutic applications, particularly when diseases are poorly understood, detailed mechanism of action may not be essential for initial development, allowing progression with partial mechanistic understanding [17].
Table 2: Essential Research Reagents for Rational Design and Phenotypic Screening
| Reagent Category | Specific Examples | Function in Research |
|---|---|---|
| Target Proteins | Recombinant purified proteins, membrane preparations | Enable binding assays and structural studies in rational design |
| Cell-Based Models | Immortalized cell lines, primary cells, iPSC-derived cells, co-culture systems | Provide biologically relevant screening platforms for phenotypic approaches |
| Compound Libraries | Diverse small molecules, targeted libraries, fragment collections, natural product extracts | Source of chemical starting points for both approaches |
| Detection Reagents | Fluorescent probes, antibodies, labeled substrates, biosensors | Enable quantification of binding, activity, or phenotypic changes |
| Genomic Tools | CRISPR libraries, RNAi collections, cDNA expression clones | Facilitate target validation and deconvolution |
| Animal Models | Genetically engineered mice, patient-derived xenografts, disease models | Provide in vivo validation of compound activity and mechanism |
Applications, Case Studies, and Clinical Impact
Success Stories from Rational Drug Design
Rational design approaches have produced numerous clinically important drugs, particularly for well-characterized target classes. Protein kinase inhibitors represent a standout success, with imatinib (Gleevec) for chronic myeloid leukemia serving as a paradigmatic example [20] [17]. Imatinib was designed to target the BCR-ABL fusion protein resulting from the Philadelphia chromosome, with co-crystal structures guiding optimization of binding affinity and selectivity [17]. Although initially regarded as selective for BCR-ABL, subsequent profiling revealed activity against other kinases including c-KIT and PDGFR, contributing to its efficacy in additional indications [18].
HIV antiretroviral therapies provide another compelling case for target-based approaches [17]. Early identification of key viral enzymes including reverse transcriptase, integrase, and protease enabled development of targeted inhibitors that form the backbone of combination antiretroviral therapy. The precision of this approach transformed HIV from a fatal diagnosis to a manageable chronic condition, demonstrating the power of targeting well-validated molecular mechanisms [17].
Structure-based design has been particularly impactful for optimizing drug properties beyond simple potency. Examples include enhancing selectivity to reduce off-target effects, improving metabolic stability to extend half-life, and reducing potential for drug-drug interactions. These applications highlight how rational approaches excel at refining compound profiles once initial activity has been established.
Success Stories from Phenotypic Screening
Phenotypic screening has demonstrated remarkable productivity for discovering first-in-class medicines, with analyses showing it has been the source of more first-in-class small molecules than target-based approaches [18] [19]. Notable examples include:
- Ivacaftor and correctors for cystic fibrosis - Discovered through screening for compounds that improve CFTR channel function in patient-derived cells, these agents work through novel mechanisms that would have been difficult to predict from target-based approaches [18].
- Risdiplam and branaplam for spinal muscular atrophy - Identified through phenotypic screens for compounds that modulate SMN2 pre-mRNA splicing, representing an unprecedented mechanism targeting the U1 snRNP complex [18].
- Artemisinin for malaria - Derived from traditional medicine and validated through phenotypic screening against Plasmodium parasites, demonstrating the value of phenotype-first approaches when molecular targets are poorly understood [21] [17].
- Lenalidomide and related immunomodulatory drugs - Although clinical effects were observed before mechanism understanding, these agents were later found to function through novel mechanisms involving Cereblon and targeted protein degradation [18].
These successes highlight how phenotypic approaches can expand the "druggable target space" to include unexpected cellular processes and novel mechanisms of action [18]. They demonstrate particular value when no attractive target is known or when project goals include discovering first-in-class medicines with differentiated mechanisms.
Strategic Integration in Drug Discovery Portfolios
The most productive drug discovery organizations strategically deploy both rational and phenotypic approaches based on project requirements and stage of development [19] [5]. Key considerations for approach selection include:
- Level of biological understanding - Well-understood pathways favor rational design; complex or poorly understood biology favors phenotypic screening
- Project goals - First-in-class discovery often benefits from phenotypic approaches; best-in-class optimization typically employs rational design
- Available tools and expertise - Model systems for phenotypic screening and structural tools for rational design
- Therapeutic area conventions - Established target classes versus novel biological space
- Resource constraints - Phenotypic screening often requires more specialized models; rational design demands structural biology capabilities
The concept of a "chain of translatability" emphasizes using disease-relevant models throughout discovery to enhance clinical success rates [19]. This framework encourages selection of approaches and models based on their ability to predict human therapeutic effects rather than purely technical considerations.
Current Challenges and Future Directions
Persistent Challenges in Rational Drug Design
Despite significant advances, rational drug design faces several persistent challenges. The accuracy of binding affinity predictions remains limited by difficulties in modeling solvation effects, entropy contributions, and protein flexibility [20] [2]. While structure-based methods can often predict binding modes correctly, reliable free energy calculations remain elusive, necessitating experimental confirmation of theoretical predictions.
Target validation represents another major challenge, as compounds designed against hypothesized targets may fail in clinical development if biological understanding is incomplete [17]. This has been particularly problematic in complex diseases like Alzheimer's, where numerous target-based approaches have failed despite strong scientific rationale [17]. The reductionist nature of target-based approaches may overlook compensatory mechanisms or systems-level properties that limit efficacy in intact organisms.
Additionally, rational design approaches can be constrained by limited chemical space exploration, as design efforts often focus on regions of chemical space perceived as compatible with the target binding site. This can potentially miss novel chemotypes or mechanisms that would not be predicted from current understanding.
Persistent Challenges in Phenotypic Screening
Phenotypic screening faces its own distinct set of challenges, with target deconvolution remaining particularly difficult [18] [19]. Even with modern tools like CRISPR screening and chemical proteomics, identifying the precise molecular targets responsible for phenotypic effects can be time-consuming and sometimes inconclusive. For some compounds with complex polypharmacology, the therapeutic effect may emerge from combined actions on multiple targets rather than a single entity [18].
Assay development for phenotypic screening requires careful balance between physiological relevance and practical screening considerations. Overly complex models may better capture disease biology but prove difficult to implement robustly, while simplified systems may miss critical aspects of pathology [19]. The validation of phenotypic models requires significant investment before screening can begin.
Additionally, hit optimization from phenotypic screens can be challenging without understanding the molecular target, as traditional structure-activity relationships may not apply when the mechanism is unknown. This can lead to empirical optimization cycles that prolong discovery timelines.
Technological Advances and Future Outlook
Both rational and phenotypic approaches are being transformed by new technologies that enhance their capabilities and address existing limitations. In rational design, artificial intelligence and machine learning are revolutionizing target identification, compound design, and property prediction [2]. These methods can integrate diverse data types to generate novel hypotheses and accelerate optimization cycles. Advances in structural biology, particularly cryo-electron microscopy, are providing high-resolution structures for previously intractable targets like membrane proteins and large complexes [20].
For phenotypic screening, innovations in stem cell biology, organ-on-a-chip technology, and high-content imaging are creating more physiologically relevant and information-rich screening platforms [19]. These systems better capture human disease biology, potentially improving translational success. Functional genomics tools like CRISPR screening enable systematic exploration of gene function alongside compound screening, potentially streamlining target deconvolution [18].
The future of drug discovery likely involves increased integration of approaches rather than exclusive commitment to one paradigm [5]. Strategies that combine phenotypic discovery with subsequent mechanistic elucidation, or that use structural information to guide optimization of phenotypically discovered hits, leverage the complementary strengths of both philosophies. As these methodologies continue to evolve and converge, they promise to enhance the efficiency and productivity of drug discovery, delivering innovative medicines for patients with diverse conditions.
Key Historical Milestones and Success Stories in Rational Drug Design
Rational Drug Design (RDD) represents a fundamental shift in pharmaceutical science from traditional empirical methods to a targeted approach based on understanding molecular interactions and disease mechanisms. Unlike earlier trial-and-error approaches, RDD utilizes detailed knowledge of biological targets and their three-dimensional structures to consciously engineer therapeutic compounds [22] [23]. This methodology has become the most advanced approach for drug discovery, employing a sophisticated arsenal of computational and experimental techniques to achieve its main goal: discovering effective, specific, non-toxic, and safe drugs [22]. The progression of RDD has been marked by significant theoretical advances and technological innovations that have systematically transformed how researchers identify and optimize lead compounds.
The foundation of rational drug design rests on the principle of molecular recognition—the precise interaction between a drug molecule and its biological target [5]. Early conceptual models have evolved from Emil Fischer's 1890 "lock-and-key" hypothesis, which viewed drug-receptor interactions as rigid complementarity, to Daniel Koshland's 1958 "induced-fit" theory, which recognized that both ligand and target undergo mutual conformational adaptations to achieve optimal binding [22] [5]. These fundamental principles underpin all modern rational drug design strategies and continue to guide the development of therapeutic interventions with increasing sophistication.
Historical Evolution of Rational Drug Design
The development of rational drug design has followed a trajectory marked by paradigm-shifting discoveries and methodological innovations. The table below chronicles the key historical milestones that have defined this evolving field.
Table 1: Key Historical Milestones in Rational Drug Design
| Time Period | Key Development | Theoretical/Methodological Advancement | Impact on Drug Discovery |
|---|---|---|---|
| Late 19th Century | Lock-and-Key Model (Emil Fischer) | Conceptualization of specific drug-receptor complementarity | Established foundation for understanding molecular recognition |
| 1950s | Induced-Fit Theory (Daniel Koshland) | Recognition of conformational flexibility in drug-receptor interactions | Provided more accurate model of binding dynamics |
| 1960s-1970s | Quantitative Structure-Activity Relationships (QSAR) | Systematic correlation of physicochemical properties with biological activity [24] | Introduced quantitative approaches to lead optimization |
| 1972 | Topliss Decision Tree | Non-mathematical scheme for aromatic substituent selection [24] | Streamlined analog synthesis through stepwise decision framework |
| 1970s-1980s | Structure-Based Drug Design | Direct utilization of 3D protein structures for ligand design [5] | Enabled targeted design complementary to binding sites |
| 1980s-Present | Molecular Modeling & Dynamics | Computational simulation of molecular behavior over time [22] | Provided insights into dynamic interactions and stability |
| 1990s-Present | High-Throughput Virtual Screening | Automated in silico screening of compound libraries [22] | Accelerated hit identification through computational methods |
| 2000s-Present | Artificial Intelligence in Drug Design | Implementation of machine learning for property prediction and de novo design [22] | Enhanced prediction accuracy and generated novel chemical entities |
The transformation of drug design from an artisanal practice to a rigorous science accelerated significantly in the mid-20th century. Early systematic approaches emerged with Corwin Hansch's pioneering work on Quantitative Structure-Activity Relationships (QSAR) in the 1960s, which established mathematical correlations between a molecule's physicochemical properties (such as hydrophobicity, electronic characteristics, and steric factors) and its biological activity [24]. This methodology represented a critical step toward predictive molecular design. The subsequent introduction of the Topliss Decision Tree in 1972 provided medicinal chemists with a practical, non-mathematical scheme for making systematic decisions about aromatic substituent selection, significantly improving the efficiency of analog synthesis during lead optimization [24].
The late 20th century witnessed another revolutionary advancement with the advent of structure-based drug design, enabled by progress in structural biology techniques like X-ray crystallography. This approach allowed researchers to directly visualize target structures and design molecules that complementarily fit into binding sites [5]. The ongoing integration of computational power, sophisticated algorithms, and artificial intelligence continues to refine these methodologies, progressively enhancing the precision and efficiency of the drug design process [22].
Fundamental Principles and Methodologies
Rational drug design operates through two primary methodological frameworks: structure-based drug design and ligand-based drug design. These approaches can be employed independently or synergistically, depending on the available information about the biological target and known active compounds.
Structure-Based Drug Design (SBDD)
Structure-based drug design, also referred to as receptor-based or direct drug design, relies on knowledge of the three-dimensional structure of the biological target obtained through experimental methods like X-ray crystallography or nuclear magnetic resonance (NMR), or through computational approaches like homology modeling [5] [4]. The fundamental premise of SBDD is designing ligand molecules that form optimal interactions—including hydrogen bonds, ionic interactions, and van der Waals forces—with specific residues in the target's binding pocket [5] [4]. This approach allows researchers to exploit the detailed recognition capabilities of the receptor site to create novel prototypes with desired pharmacological properties.
The SBDD process typically follows a systematic workflow: (1) preparation of the protein structure, (2) identification of binding sites in the protein of interest, (3) preparation of ligand libraries, and (4) docking and scoring of ligands to evaluate binding affinity and predict potential candidates [4]. Despite its powerful capabilities, SBDD faces several challenges, including accounting for target flexibility, appropriately handling water molecules in the binding site that may mediate interactions, and accurately modeling solvation effects that influence binding free energies [4].
Ligand-Based Drug Design (LBDD)
When the three-dimensional structure of the target protein is unavailable, ligand-based drug design (also called pharmacophore-based or indirect drug design) provides an alternative approach [5] [4]. This methodology deduces the structural requirements for biological activity by analyzing a set of known active and inactive compounds. Through techniques such as pharmacophore modeling and three-dimensional quantitative structure-activity relationship (3D QSAR) studies, researchers identify stereochemical and physicochemical features essential for target interaction, then design new chemical entities that mimic these critical characteristics [5] [4].
A key concept in LBDD is "molecular mimicry," where chemically diverse compounds are designed to share common spatial arrangements of functional groups that mediate binding to the target [5]. This approach has been successfully applied to mimic various biological structures, including ATP (for kinase inhibitors), dopamine (for CNS agents), histamine (for anti-allergic therapies), and steroid hormones (for endocrine therapies) [5]. When applied to peptides, this strategy evolves into the specialized field of "peptidomimetics," which aims to transform biologically active peptides into metabolically stable, bioavailable drug candidates [5].
Integrated Framework and Experimental Validation
The most effective drug discovery projects often combine both structure-based and ligand-based approaches, creating a synergistic framework that leverages all available information [5]. In this integrated model, promising molecules designed through one approach can be validated using the other—for instance, a compound identified through molecular mimicry can be docked into the protein structure to verify complementary interactions, or a molecule designed through SBDD can be compared to known active structures to assess consistency with established structure-activity relationships [5].
The following diagram illustrates the integrated workflow of rational drug design, highlighting the synergy between structure-based and ligand-based approaches:
Diagram 1: Integrated Rational Drug Design Workflow
Regardless of the design strategy employed, the rational drug design process follows an iterative cycle of compound design, chemical synthesis, and biological testing [5]. This iterative refinement allows researchers to progressively optimize lead compounds by improving their affinity, selectivity, and drug-like properties while reducing toxicity. Experimental validation remains essential throughout this process, with advanced biochemical assays and analytical techniques providing critical feedback to inform subsequent design cycles.
Success Stories in Rational Drug Design
Captopril: The First ACE Inhibitor
The development of Captopril represents a landmark achievement in rational drug design and the first angiotensin-converting enzyme (ACE) inhibitor to reach the market [25]. The project originated from the observation that victims of the Brazilian viper (Bothrops jararaca) experienced dramatic drops in blood pressure, which researchers traced to ACE-inhibiting peptides in the venom [25]. Initial research isolated teprotide, a potent nonapeptide inhibitor that demonstrated promising antihypertensive effects in clinical trials but suffered from poor oral bioavailability due to its peptide nature [25].
The critical breakthrough came when researchers David Cushman and Miguel Ondetti recognized that ACE was a zinc metalloprotease with mechanistic similarities to carboxypeptidase A, whose structure had been determined through X-ray crystallography [25]. Based on this insight, they constructed a conceptual model of the ACE active site and designed inhibitors that incorporated a zinc-binding group [25]. This rational approach led to the discovery of Captopril, which featured a novel thiol group that strongly coordinated the catalytic zinc ion, resulting in potency 1000-fold greater than their initial lead compound [25].
Table 2: Key Experimental Reagents and Techniques in Captopril Development
| Research Reagent/Technique | Function in Drug Discovery Process |
|---|---|
| Brazilian Viper Venom Peptides | Provided natural product templates for ACE inhibition |
| Radioimmunoassay for Angiotensin I/II | Enabled quantification of ACE activity in biological samples |
| Carboxypeptidase A X-ray Structure | Served as homology model for ACE active site |
| Zinc Chelating Agents (EDTA) | Confirmed metalloprotease nature of ACE |
| Benzylsuccinic Acid | Provided bi-product inhibitor concept for zinc metalloproteases |
| Succinyl Proline Derivatives | Initial synthetic leads for non-peptide ACE inhibitors |
| Thiol-Containing Analogs | Enhanced zinc binding affinity for increased potency |
The following diagram outlines the key experimental workflow and design strategy that led to the development of Captopril:
Diagram 2: Captopril Design Strategy and Discovery Timeline
Brivaracetam: SV2A Ligand Optimization
The development of Brivaracetam exemplifies rational optimization of pharmacodynamic activity at a defined molecular target [26]. The story began with the discovery that levetiracetam, the (S)-enantiomer of the ethyl analogue of piracetam, provided protection against seizures in animal models through stereospecific binding to a novel brain target [26]. Researchers subsequently identified this target as SV2A, a synaptic vesicle glycoprotein involved in modulating neurotransmitter release [26].
Using levetiracetam as a starting point, researchers systematically investigated substitutions on the pyrrolidine ring to enhance binding affinity to SV2A [26]. This rational optimization strategy identified the 4-n-propyl analogue, brivaracetam, which exhibited a 13-fold higher binding affinity compared to levetiracetam and a broadened spectrum of anticonvulsant activity in animal models [26]. Clinical trials confirmed that brivaracetam was efficacious and well-tolerated in treating partial onset seizures, validating SV2A as a viable target for antiepileptic therapy [26].
Imatinib: Targeted Cancer Therapy
Imatinib (Gleevec) stands as one of the most celebrated success stories of rational drug discovery, particularly in oncology [27]. The development of Imatinib began with the identification of the BCR-ABL fusion protein as the molecular driver of chronic myeloid leukemia (CML) [27]. Researchers at Novartis designed Imatinib as a small molecule that specifically inhibits the tyrosine kinase activity of BCR-ABL, effectively targeting the fundamental molecular abnormality in CML [27].
The rational design of Imatinib transformed CML from a fatal disease into a manageable condition, earning it the designation as a "magic bullet" for targeted cancer therapy [27]. This success demonstrated the power of targeting specific molecular pathways in cancer and established a new paradigm for oncology drug development, inspiring numerous subsequent targeted therapies.
Current Challenges and Future Perspectives
Despite significant advances, rational drug design continues to face several challenges. The complexity of human biology means that even well-targeted drugs can produce unforeseen effects, highlighting the limitations of our current understanding of biological systems [27]. Additionally, the high costs and extended timeframes required for drug development remain substantial hurdles, with the average new drug costing approximately $2.6 billion and requiring 12-15 years from discovery to market [22] [4]. The high attrition rate in drug development further complicates this picture, with only one compound typically reaching approval out of thousands initially synthesized and tested [22].
The future of rational drug design is being shaped by several transformative technologies. Artificial intelligence and machine learning are increasingly being applied to predict compound properties, identify novel targets, and even generate new molecular entities [22] [27]. Advances in structural biology, particularly cryo-electron microscopy, are providing unprecedented insights into protein structures and drug-target interactions [22]. The integration of genomic and proteomic data is enabling more personalized approaches to drug design, while high-throughput virtual screening continues to accelerate the identification of promising lead compounds [22] [5].
As these technologies mature, they promise to further enhance the precision and efficiency of rational drug design, potentially leading to more effective therapies for conditions that currently lack adequate treatment options. The ongoing evolution of rational drug design methodologies continues to solidify their position as the cornerstone of modern pharmaceutical development, offering hope for addressing unmet medical needs through scientifically-driven therapeutic innovation.
Computational Methods and Practical Applications in Modern RDD
Structure-Based Drug Design (SBDD) represents a paradigm shift in preclinical drug discovery, moving away from traditional high-throughput screening (HTS) methods toward a more rational approach grounded in detailed structural knowledge of biological targets [20]. Whereas HTS often generates hits that are difficult to optimize into viable drug candidates due to insufficient information about ligand-receptor interactions, SBDD directly addresses this gap by investigating the precise molecular interactions between ligands and their receptors [20]. This approach has become a cornerstone of modern pharmaceutical research, offering a rational framework for transforming initial hits into optimized drug candidates with enhanced potency and selectivity profiles [28].
The fundamental premise of SBDD relies on determining the three-dimensional atomic structure of pharmacologically relevant targets to guide the design and optimization of therapeutic compounds [29]. By leveraging detailed structural information, medicinal chemists can design molecules that complement the shape and chemical properties of a target's binding site, enabling more efficient and predictive drug development [20]. In the context of increasingly complex biological systems and rising demands for precision therapeutics, SBDD serves as a critical bridge between experimental techniques, computational modeling, and medicinal chemistry [28].
Key Structural Biology Techniques in SBDD
Experimental Methods for Structure Determination
The successful application of SBDD depends on high-resolution 3D structural information obtained through multiple complementary experimental techniques:
X-ray Crystallography has traditionally been the dominant method for structure determination in drug discovery. It provides high-resolution structures that clearly show atomic positions within protein-ligand complexes, allowing researchers to visualize binding interactions and guide compound optimization [28]. However, this technique faces significant limitations, including the low success rate of obtaining suitable crystals (only approximately 25% of successfully expressed and purified proteins yield crystals suitable for X-ray analysis) [28]. Additionally, X-ray crystallography is essentially "blind" to hydrogen information, cannot capture the dynamic behavior of complexes, and may miss approximately 20% of protein-bound waters that are critical for understanding binding thermodynamics [28].
Cryo-Electron Microscopy (Cryo-EM) has emerged as a powerful alternative that can generate structures of proteins in various conformational states without requiring crystallization [28]. This technique continues to push the resolution limits for complex targets that are difficult to crystallize, such as membrane proteins and large complexes [29]. Cryo-EM is particularly valuable for studying targets that resist crystallization, though it traditionally required larger protein sizes and faced resolution limitations compared to X-ray methods [28].
Nuclear Magnetic Resonance (NMR) Spectroscopy provides unique capabilities for studying protein-ligand interactions in solution under physiological conditions [28]. Unlike static snapshots from crystallography, NMR can elucidate dynamic behavior and capture multiple conformational states relevant to molecular recognition [28]. A significant advantage is NMR's ability to directly detect hydrogen bonding interactions through chemical shift analysis, providing crucial information about binding energetics [28]. This technique faces challenges with larger molecular systems but continues to expand its applicable range through technical advancements like TROSY-based experiments and dynamic nuclear polarization [28].
Integrative Approaches and Computational Methods
The evolving landscape of SBDD increasingly emphasizes integrative structural biology, combining multiple experimental techniques with computational approaches to overcome the limitations of individual methods [29]. This convergence is essential for unlocking complex targets and accelerating drug discovery [29].
Artificial Intelligence and Machine Learning have transformed structural biology, exemplified by AlphaFold2's Nobel Prize-winning achievements in protein structure prediction [29]. However, the true impact of AI-powered structure prediction depends on experimental validation through techniques like Cryo-EM, NMR, and X-ray crystallography [29]. Recent research indicates that current generative models for SBDD may suffer from either insufficient expressivity or excessive parameterization, highlighting the need for continued refinement of these computational approaches [30].
Molecular Docking and Virtual Screening serve as computational workhorses in SBDD, enabling researchers to rapidly screen large virtual compound libraries against target structures [20]. While docking programs have limitations in scoring function reliability across diverse chemical classes, they remain valuable tools when combined with experimental validation [20].
Table 1: Comparison of Major Structural Biology Techniques in SBDD
| Technique | Resolution Range | Sample Requirements | Key Advantages | Major Limitations |
|---|---|---|---|---|
| X-ray Crystallography | Atomic (0.5-2.5 Å) | High-quality crystals | High resolution; Direct electron density visualization | Difficult crystallization; Static snapshots; Misses hydrogen atoms |
| Cryo-EM | Near-atomic to low (>2 Å) | Purified protein (small amounts) | No crystallization needed; Captures multiple states | Traditionally required larger complexes; Lower resolution for some targets |
| NMR Spectroscopy | Atomic to residue level | Soluble, isotopically labeled protein | Solution-state conditions; Dynamics and hydrogen bonding | Molecular size limitations; Spectral complexity |
Experimental Protocols and Methodologies
NMR-Driven SBDD Workflow
A novel research strategy termed NMR-Driven Structure-Based Drug Design (NMR-SBDD) combines selective side-chain labeling with advanced computational tools to generate reliable protein-ligand structural ensembles [28]. The methodology involves several key steps:
Sample Preparation and Isotope Labeling: Proteins are expressed using 13C-amino acid precursors that selectively label specific side chains, simplifying NMR spectra and focusing on pharmacologically relevant regions [28]. This labeling strategy reduces spectral complexity while providing crucial atomic-level information about binding interactions.
Data Acquisition and Chemical Shift Analysis: NMR experiments focus on detecting 1H chemical shift perturbations that directly report on hydrogen-bonding interactions [28]. Protons with large downfield chemical shift values (higher ppm) typically serve as hydrogen bond donors in classical H-bonds, while upfield shifts indicate interactions with aromatic systems [28]. These measurements provide experimental validation of molecular interactions that are difficult to detect by other methods.
Structure Calculation and Ensemble Generation: NMR-derived constraints are integrated with computational methods to generate structural ensembles that represent the dynamic behavior of protein-ligand complexes in solution [28]. This approach captures conformational flexibility and multiple binding states that may be missed by single-conformation techniques.
Diagram 1: NMR-Driven SBDD Workflow. This process integrates experimental NMR data with computational modeling for structure-based drug design.
Cryo-EM Single Particle Analysis Workflow
For targets resistant to crystallization, Cryo-EM provides an alternative path to structure determination through single-particle analysis:
Sample Vitrification: The protein sample is rapidly frozen in thin ice layers, preserving native conformations without crystalline order requirements [29]. This flash-freezing process captures molecules in multiple functional states.
Data Collection and Image Processing: Automated imaging collects thousands of particle images, which undergo extensive computational processing including 2D classification, 3D reconstruction, and refinement [29]. Advanced detectors and software have dramatically improved the resolution achievable through this technique.
Model Building and Validation: The resulting electron density map enables atomic model building, followed by rigorous validation against experimental data [29]. For drug discovery applications, focus remains on binding pocket architecture and ligand density.
X-ray Crystallography Workflow for SBDD
Traditional crystallography remains a vital tool for SBDD, particularly through high-throughput soaking systems:
Crystal Growth and Optimization: Extensive screening identifies conditions that yield diffraction-quality crystals, often requiring optimization of protein constructs and crystallization conditions [28]. Engineering strategies may remove flexible regions that impede crystallization.
Ligand Soaking and Data Collection: Pre-formed crystals are soaked with ligand solutions, followed by rapid freezing and X-ray diffraction data collection [28]. This approach enables medium-to-high throughput structure determination of multiple protein-ligand complexes.
Electron Density Analysis and Refinement: Electron density maps reveal ligand positioning and protein conformational changes, guiding iterative compound design [28]. Omit maps help validate ligand placement and reduce model bias.
Research Reagent Solutions for SBDD
Successful implementation of SBDD relies on specialized reagents and tools that enable structural studies and compound optimization:
Table 2: Essential Research Reagents and Materials for SBDD
| Reagent/Material | Function in SBDD | Application Examples |
|---|---|---|
| Isotope-Labeled Amino Acids (13C, 15N) | Enables NMR signal assignment and interaction studies | Selective side-chain labeling for simplified spectra; Backbone labeling for structure determination [28] |
| Crystallization Screening Kits | Identifies conditions for crystal formation | Sparse matrix screens combining various buffers, salts, and precipitants [28] |
| Cryo-EM Grids | Sample support for vitrification | Ultra-thin carbon or gold grids with optimized hydrophobicity [29] |
| Protein Expression Systems | Production of pharmacologically relevant targets | Bacterial, insect, and mammalian systems with tags for purification [28] |
| Fragment Libraries | Starting points for drug discovery | Collections of low molecular weight compounds with high solubility and structural diversity [20] |
Technical Considerations and Implementation Challenges
Addressing Methodological Limitations
Each structural biology technique presents unique challenges that must be addressed through methodological innovations:
Crystallization Obstacles remain a significant bottleneck, with only approximately 25% of successfully expressed and purified proteins yielding diffraction-quality crystals [28]. Strategies to overcome this include construct optimization to remove flexible regions, crystallization chaperones to facilitate packing, and lipid cubic phase methods for membrane proteins [28].
Molecular Weight Limitations in NMR spectroscopy traditionally restricted studies to smaller proteins, but technical advancements like TROSY-based experiments and deep learning methods have extended the accessible range to larger complexes [28]. Integration with complementary techniques like cryo-EM further expands NMR's applicability to challenging systems [28].
Resolution and Throughput Challenges in cryo-EM continue to improve with direct electron detectors and enhanced computational processing [29]. While the technique still typically requires larger sample amounts than crystallography, ongoing developments are steadily reducing these requirements.
Thermodynamic Considerations in Binding Affinity
A fundamental challenge in SBDD involves the enthalpy-entropy compensation that occurs during ligand binding [28]. While structural information guides the optimization of favorable enthalpic interactions (hydrogen bonds, van der Waals contacts), these often come at the cost of conformational entropy as the ligand and protein become more rigid upon binding [28]. Additionally, the reorganization of water networks around the binding site significantly influences binding free energy, making predictions challenging [28].
NMR spectroscopy provides unique insights into these thermodynamic trade-offs by detecting hydrogen bonding interactions and observing dynamic processes across multiple timescales [28]. This information helps medicinal chemists balance the various contributions to binding affinity during compound optimization.
Structure-Based Drug Design represents a powerful framework within rational drug discovery that continues to evolve with technological advancements in structural biology [29]. The integration of multiple techniques—X-ray crystallography, Cryo-EM, and NMR spectroscopy—provides complementary insights that overcome the limitations of individual methods [28]. As the field progresses toward increasingly complex targets, including membrane proteins and dynamic systems, this integrative approach will be essential for advancing therapeutic development [29].
The future of SBDD lies in the seamless combination of experimental structural data with computational predictions and AI-driven approaches [29] [30]. While computational methods have made remarkable progress, their true impact depends on experimental validation through high-resolution structural techniques [29]. By leveraging the unique strengths of each methodology and acknowledging their respective limitations, researchers can continue to advance the frontiers of structure-based drug discovery and deliver innovative medicines to address unmet medical needs.
Rational Drug Design (RDD) represents a systematic, knowledge-driven approach to drug discovery that aims to identify and optimize novel therapeutic compounds based on an understanding of their molecular targets and biological interactions. Within this paradigm, Ligand-Based Drug Design (LBDD) has emerged as a fundamental methodology when three-dimensional structural information of the biological target is unavailable [4]. LBDD methodologies are particularly crucial for targeting membrane-associated proteins such as G protein-coupled receptors (GPCRs), ion channels, and transporters, which constitute over 50% of current drug targets but often resist structural characterization [31] [32]. By exploiting the known biological activities of existing ligands, LBDD enables researchers to establish critical structure-activity relationships (SARs) that guide the discovery and optimization of novel bioactive molecules without requiring direct structural knowledge of the target [31].
Two complementary computational approaches form the cornerstone of modern LBDD: pharmacophore modeling and Quantitative Structure-Activity Relationship (QSAR) analysis [4] [33]. Pharmacophore modeling identifies the essential spatial arrangement of molecular features necessary for biological activity, while QSAR establishes mathematical relationships between quantifiable molecular properties and biological responses [33] [34]. Together, these methodologies provide powerful tools for virtual screening, lead optimization, and the prediction of key pharmacological properties, significantly accelerating the drug discovery process and reducing its associated costs [32] [35]. This technical guide examines the fundamental principles, methodological workflows, and contemporary applications of these core LBDD techniques within the broader context of rational drug development.
Theoretical Foundations of Ligand-Based Drug Design
Key Principles and Assumptions
LBDD operates on several fundamental principles that enable drug discovery in the absence of target structural information. The primary assumption, known as the similarity-property principle, states that structurally similar molecules are likely to exhibit similar biological properties and activities [33]. This principle forms the basis for molecular similarity searching, where compounds sharing chemical or physicochemical features with known active molecules are prioritized for experimental testing [33]. A second critical concept is the pharmacophore hypothesis, which postulates that a specific three-dimensional arrangement of steric and electronic features is necessary for optimal molecular interactions with a target and subsequent biological activity [33] [34].
The theoretical framework of LBDD also incorporates several biochemical models of ligand-target interaction, including the traditional "lock-and-key" model and the more dynamic "induced-fit" and "conformational selection" hypotheses [31] [33]. These models acknowledge that biological activity depends not only on the static chemical structure of ligands but also on their dynamic conformational properties and how these influence receptor binding [31]. Understanding these relationships allows researchers to extract critical information from known active compounds to guide the design of novel therapeutic agents.
Molecular Representations in LBDD
The representation of molecular structure is fundamental to all LBDD approaches, with different dimensionality representations serving distinct purposes in the drug discovery pipeline:
1D Representations: Simplified line notations such as SMILES (Simplified Molecular Input Line Entry System) and molecular fingerprints enable fast storage, lookup, and comparison of molecular structures [31]. These representations are valuable for high-throughput screening and similarity searching in large chemical databases.
2D Representations: Molecular graphs where atoms represent nodes and bonds represent edges allow for the calculation of topological descriptors and constitutional properties [31]. These include molecular weight, molar refractivity, number of rotatable bonds, and hydrogen bond donor/acceptor counts, which are widely used in QSAR analysis [31] [33].
3D Representations: Atomic Cartesian coordinates enable the realistic modeling of molecular shape and the spatial arrangement of functional groups [31]. Three-dimensional representations are essential for pharmacophore modeling and for calculating steric and electrostatic properties that influence biological activity.
4D and Higher Representations: These incorporate molecular flexibility by considering ensembles of molecular conformations rather than single static structures [36] [31]. Such representations provide more realistic models of ligand behavior under physiological conditions and have been applied in advanced pharmacophore modeling and QSAR refinement.
Pharmacophore Modeling: Concepts and Methodologies
Fundamental Concepts and Definition
A pharmacophore is defined as "the essential geometric arrangement of molecular features necessary for biological activity" [33]. It represents an abstract pattern of functional groups that a molecule must possess to interact effectively with a specific biological target. The International Union of Pure and Applied Chemistry (IUPAC) formally defines a pharmacophore as "the ensemble of steric and electronic features that is necessary to ensure the optimal supramolecular interactions with a specific biological target and to trigger (or block) its biological response" [33].
Pharmacophore features typically include:
- Hydrogen bond donors and acceptors
- Hydrophobic regions
- Aromatic rings
- Positively and negatively ionizable groups
- Exclusion volumes (defining regions where atoms would cause steric clashes)
These features capture the key molecular interactions that mediate ligand binding, including hydrogen bonding, ionic interactions, van der Waals forces, and hydrophobic effects [4] [33].
Pharmacophore Model Development Workflow
The process of developing a pharmacophore model follows a systematic workflow that can be implemented using various computational tools and software platforms.
Ligand Preparation and Conformational Analysis
The initial step involves curating a set of known active compounds with diverse chemical structures but common biological activity [34]. These ligands undergo geometry optimization using computational methods such as Molecular Mechanics (MM) or Density Functional Theory (DFT) to identify their most stable low-energy conformations [31] [37]. For example, in the development of quinazolin-4(3H)-one derivatives as breast cancer inhibitors, geometry optimization was performed using DFT with B3LYP/6-31G* basis set to find the most stable conformers [37].
Conformational sampling then generates multiple plausible three-dimensional arrangements of each molecule to account for their flexibility when binding to the biological target [38] [31]. Advanced approaches like the Conformationally Sampled Pharmacophore (CSP) method systematically explore the conformational space accessible to ligands under physiological conditions, providing more comprehensive coverage of potential bioactive conformations [38].
Pharmacophore Hypothesis Generation and Validation
The core process of pharmacophore model development involves identifying common spatial arrangements of molecular features among the active ligands. Computational algorithms such as PharmaGist analyze multiple active compounds to detect shared three-dimensional patterns of chemical features [34]. The model generation process typically produces several candidate pharmacophore hypotheses, which must be rigorously evaluated based on their ability to:
- Discriminate between known active and inactive compounds
- Align active molecules with low root-mean-square deviation (RMSD)
- Exclude molecules that are structurally similar but biologically inactive
Statistical validation establishes the predictive power and robustness of the selected pharmacophore model before its application in virtual screening campaigns [34].
Applications in Virtual Screening and Lead Optimization
Validated pharmacophore models serve as search queries for screening large chemical databases such as ZINC, a publicly available repository containing millions of commercially available compounds [34]. Tools like ZINCPharmer enable rapid identification of molecules that match the essential pharmacophore features, significantly enriching the hit rate compared to random screening [34]. In the case study of dengue protease inhibitors, pharmacophore-based screening of the ZINC database identified promising candidates that were subsequently validated through QSAR analysis and molecular docking [34].
Beyond virtual screening, pharmacophore models provide valuable guidance for lead optimization by highlighting critical molecular features that contribute to biological activity. Medicinal chemists can use this information to design structural analogs with improved potency, selectivity, or drug-like properties while maintaining the essential pharmacophore elements required for target interaction [33].
Quantitative Structure-Activity Relationship (QSAR) Modeling
Historical Development and Fundamental Principles
QSAR modeling represents a cornerstone of computational chemistry that formally began in the early 1960s with the pioneering work of Hansch and Fujita, and Free and Wilson [33]. The fundamental principle underlying QSAR is that biological activity can be correlated with quantifiable molecular properties through mathematical relationships, enabling the prediction of activities for novel compounds [33].
The historical development of QSAR includes several landmark contributions:
- Meyer-Overton Theory (1899-1901): Early observations that the narcotic potency of anesthetics correlated with their lipid solubility [33]
- Hammett Equation (1930s): Introduced substituent constants (σ) to quantify electronic effects on reaction rates [33]
- Hansch Analysis (1960s): Extended Hammett's approach to biological systems by incorporating hydrophobic parameters (logP) [33]
- Free-Wilson Method (1960s): Developed additive models for the contributions of specific substituents to biological activity [33]
Modern QSAR continues to evolve with the integration of machine learning algorithms and complex molecular descriptors, but remains grounded in these fundamental principles.
Molecular Descriptors in QSAR
Molecular descriptors are numerical representations of chemical structures and properties that serve as the independent variables in QSAR models [36]. These descriptors can be categorized based on their dimensionality and the structural features they encode:
Table 1: Classification of Molecular Descriptors in QSAR Modeling
| Descriptor Type | Description | Examples | Applications |
|---|---|---|---|
| 1D Descriptors | Based on molecular composition and bulk properties | Molecular weight, atom counts | Preliminary screening, rule-based filters (e.g., Lipinski's Rule of Five) |
| 2D Descriptors | Derived from molecular topology and connectivity | Topological indices, connectivity indices, molecular fingerprints | Traditional QSAR, similarity searching, patent analysis |
| 3D Descriptors | Represent three-dimensional molecular geometry | Molecular surface area, volume, steric and electrostatic parameters | 3D-QSAR methods (CoMFA, CoMSIA), pharmacophore modeling |
| 4D Descriptors | Incorporate conformational flexibility | Ensemble properties from multiple conformations | Advanced pharmacophore modeling, QSAR refinement |
| Quantum Chemical Descriptors | Derived from electronic structure calculations | HOMO-LUMO energies, electrostatic potential, dipole moment | Modeling electronic effects, reaction mechanisms |
Contemporary QSAR implementations often utilize software tools such as PaDEL, DRAGON, and RDKit for descriptor calculation, generating hundreds to thousands of potential descriptors for each compound [36] [37]. This necessitates careful descriptor selection to avoid overfitting and to ensure model interpretability.
QSAR Model Development Workflow
The development of robust, predictive QSAR models follows a systematic process with critical validation steps at each stage.
Data Preparation and Descriptor Calculation
QSAR modeling begins with the assembly of a curated dataset of chemical structures with associated biological activities (typically expressed as IC₅₀, KI, or EC₅₀ values) [37]. These activity values are often converted to negative logarithmic scales (pIC₅₀ = -logIC₅₀) to normalize the distribution and linearize the relationship with free energy changes [34] [37]. Molecular structures undergo geometry optimization followed by comprehensive descriptor calculation using specialized software [37].
Dataset Division and Feature Selection
The compiled dataset is divided into training and test sets using algorithms such as the Kennard-Stone method, which ensures representative sampling of the chemical space [37]. The training set (typically 70-80% of the data) is used for model development, while the test set (20-30%) is reserved for external validation [37]. To address the "curse of dimensionality" that arises from having many more descriptors than compounds, feature selection techniques such as Genetic Algorithm (GA), Stepwise Regression, or LASSO (Least Absolute Shrinkage and Selection Operator) are employed to identify the most relevant descriptors [36] [37].
Model Building and Validation
Model development applies statistical and machine learning algorithms to establish mathematical relationships between the selected descriptors and biological activity:
- Classical Methods: Multiple Linear Regression (MLR), Partial Least Squares (PLS), Principal Component Regression (PCR) [36] [33]
- Machine Learning Approaches: Random Forests (RF), Support Vector Machines (SVM), k-Nearest Neighbors (kNN) [36]
- Advanced Techniques: Neural Networks, Gaussian Processes, Gene Expression Programming [36] [31]
Rigorous validation is essential to ensure model reliability and predictive power. Internal validation uses techniques such as leave-one-out (LOO) or leave-many-out (LMO) cross-validation to assess model robustness [37]. The cross-validated correlation coefficient (Q²) should exceed 0.5 for a model to be considered predictive [37]. External validation evaluates the model's performance on the previously unseen test set, with the predictive correlation coefficient (R²pred) providing the most stringent measure of model utility [37]. Additionally, Y-scrambling tests verify that the model is not the result of chance correlation by randomly permuting activity values and confirming that the resulting models show significantly worse performance [37].
Defining the Applicability Domain
The applicability domain (AD) of a QSAR model defines the chemical space within which the model provides reliable predictions [37]. This concept is critical for understanding the limitations of a model and avoiding extrapolation beyond its validated boundaries. The AD can be defined using various approaches, including:
- Range-based methods: Considering the minimum and maximum values of each descriptor in the training set
- Leverage approaches: Calculating the Mahalanobis distance or Hat index to identify influential compounds [37]
- Geometric methods: Mapping the distribution of training compounds in the descriptor space
Compounds falling outside the applicability domain should be treated with caution, as their predicted activities may be unreliable [37].
Integrated Computational Workflows in Modern Drug Discovery
Combining Pharmacophore Modeling and QSAR
The integration of pharmacophore modeling and QSAR creates a powerful synergistic workflow for drug discovery [34] [37]. A typical integrated approach might involve:
- Pharmacophore-based virtual screening to identify potential hit compounds from large databases [34]
- QSAR modeling to predict the activities of the screened compounds and prioritize the most promising candidates [34]
- Molecular docking to investigate potential binding modes and interactions with the target protein [34] [37]
- ADMET prediction to assess drug-likeness and pharmacokinetic properties [37]
This integrated strategy was successfully applied in the identification of dengue protease inhibitors, where pharmacophore screening of the ZINC database was followed by QSAR-based activity prediction and molecular docking validation [34].
Table 2: Key Computational Tools and Resources for LBDD
| Tool Category | Examples | Primary Function | Access |
|---|---|---|---|
| Pharmacophore Modeling | PharmaGist, ZINCPharmer, Catalyst | Pharmacophore hypothesis generation and screening | Web servers, Commercial software |
| Descriptor Calculation | PaDEL, DRAGON, RDKit | Calculation of molecular descriptors | Open-source, Commercial |
| QSAR Modeling | MATLAB, BuildQSAR, QSARINS | Model development and validation | Open-source, Commercial |
| Chemical Databases | ZINC, DrugBank, ChEMBL | Sources of chemical structures and bioactivity data | Publicly accessible |
| Molecular Docking | AutoDock, GOLD, Glide | Protein-ligand interaction modeling | Open-source, Commercial |
| ADMET Prediction | SwissADME, pkCSM, admetSAR | Prediction of pharmacokinetic properties | Web servers, Commercial packages |
Case Studies in LBDD Application
Anti-Breast Cancer Drug Discovery
QSAR modeling has been extensively applied in the discovery of novel anti-breast cancer agents. In one recent example, researchers developed a QSAR model for quinazolin-4(3H)-one derivatives targeting breast cancer [37]. The study utilized 35 compounds with known inhibitory activities (IC₅₀ values) against breast cancer cell lines. After geometry optimization using Density Functional Theory (DFT) with B3LYP/6-31G* basis set, molecular descriptors were calculated using PADEL software [37].
The optimal QSAR model demonstrated excellent statistical parameters (R² = 0.919, Q²cv = 0.819, R²pred = 0.791), indicating strong predictive capability [37]. The model was used to design seven novel quinazolin-4(3H)-one derivatives with predicted activities superior to both the template compound and the reference drug Doruxybucin [37]. Subsequent molecular docking studies against the epidermal growth factor receptor (EGFR) target (PDB ID: 2ITO) confirmed favorable binding interactions, and pharmacological property prediction suggested promising drug-like characteristics [37].
Dengue Protease Inhibitor Identification
Another compelling application combined pharmacophore modeling and QSAR for the identification of dengue virus NS2B-NS3 protease inhibitors [34]. Researchers developed a ligand-based pharmacophore model using known active compounds containing 4-Benzyloxy Phenyl Glycine residues [34]. This model was used to screen the ZINC database through ZINCPharmer, identifying compounds with similar pharmacophore features [34].
A separate 2D-QSAR model was developed using 80 reported protease inhibitors and validated using both internal and external validation methods [34]. This QSAR model was then employed to predict the activities of the compounds identified through pharmacophore screening. The integrated approach identified two promising candidates (ZINC36596404 and ZINC22973642) with predicted pIC₅₀ values of 6.477 and 7.872, respectively [34]. Molecular docking confirmed strong binding to the NS3 protease active site, and molecular dynamics simulations with MM-PBSA binding energy calculations further validated the stability of these interactions [34].
Emerging Trends and Future Perspectives
The field of LBDD continues to evolve with several emerging trends shaping its future development:
AI-Integrated QSAR Modeling: The integration of artificial intelligence, particularly deep learning approaches such as graph neural networks and SMILES-based transformers, is enhancing the predictive power and applicability of QSAR models [36]. These methods can capture complex nonlinear relationships in large chemical datasets, enabling more accurate activity predictions [36].
Hybrid Structure-Based and Ligand-Based Approaches: Combining LBDD with structure-based methods when partial structural information is available provides complementary insights [32] [35]. The Relaxed Complex Scheme incorporates molecular dynamics simulations to account for protein flexibility, potentially overcoming limitations of both pure structure-based and ligand-based approaches [32].
Advanced Pharmacophore Methods: Conformationally sampled pharmacophore approaches and ensemble-based pharmacophore models provide more realistic representations of ligand-receptor interactions by accounting for molecular flexibility [38] [36].
Public Databases and Cloud-Based Platforms: Increasing access to curated chemical and biological databases, combined with cloud-based computational platforms, is democratizing access to advanced LBDD tools and reducing barriers to entry [36].
As these trends continue to mature, LBDD methodologies are expected to play an increasingly central role in rational drug design, particularly for challenging targets where structural information remains limited. The integration of LBDD with experimental validation will continue to drive the discovery and optimization of novel therapeutic agents addressing unmet medical needs.
Computer-Aided Drug Design (CADD) has transitioned from a supplementary tool to a central component in modern drug discovery pipelines, offering a more efficient and cost-effective approach that complements traditional experimental techniques [39]. By leveraging computational power, researchers can predict drug candidate behavior, assess interactions with biological targets, and optimize pharmacokinetic properties before synthesis and experimental validation [39]. This paradigm is particularly crucial within the framework of Rational Drug Design (RDD), which relies on using the three-dimensional structural knowledge of biological targets to strategically design novel therapeutic agents [1]. The traditional drug discovery pipeline is notoriously time-consuming and expensive, with an average cost of $2.6 billion and a timeline exceeding 12 years from concept to market [1]. CADD methodologies, particularly virtual screening and molecular docking, directly address these bottlenecks by dramatically accelerating the initial identification and optimization of potential drug candidates, thereby streamlining the transition from hit identification to lead development [1] [35].
The conceptual foundation of modern, informatics-driven RDD is increasingly shaped by the "informacophore" concept [1]. This extends the traditional pharmacophore—which represents the spatial arrangement of chemical features essential for molecular recognition—by incorporating data-driven insights derived not only from structure-activity relationships (SAR) but also from computed molecular descriptors, fingerprints, and machine-learned representations of chemical structure [1]. This fusion of structural chemistry with informatics enables a more systematic and bias-resistant strategy for scaffold modification and optimization, acting as a key element in modern RDD strategies [1].
CADD approaches are broadly categorized into two main types: structure-based drug design (SBDD) and ligand-based drug design (LBDD) [35]. Molecular docking is a primary technique within SBDD, used when the three-dimensional structure of the target is known, typically through X-ray crystallography or cryo-electron microscopy [40] [35]. Virtual screening, on the other hand, is a preliminary computational tool used in both SBDD and LBDD to rapidly evaluate massive libraries of compounds for potential bioactivity, serving as a productive and cost-effective technology in the search for novel medicinal molecules [35].
Table 1: Core CADD Approaches in Rational Drug Design
| Approach | Description | Primary Applications | Key Techniques |
|---|---|---|---|
| Structure-Based Drug Design (SBDD) | Relies on the 3D structure of the biological target (e.g., a protein). | Hit identification, lead optimization, predicting binding modes. | Molecular Docking, Molecular Dynamics Simulations, Structure-Based Virtual Screening. |
| Ligand-Based Drug Design (LBDD) | Used when the target structure is unknown but active ligands are available. | Hit identification, lead optimization, toxicity prediction. | Quantitative Structure-Activity Relationship (QSAR), Pharmacophore Modeling, Ligand-Based Virtual Screening. |
Virtual Screening in Drug Discovery
Virtual screening (VS) is a computational methodology that employs sophisticated algorithms to sift through ultra-large chemical libraries—containing billions of molecules—to identify a subset of compounds with the highest potential to bind to a therapeutic target and elicit a desired biological effect [35]. This process is indispensable in the contemporary era of "make-on-demand" or "tangible" virtual libraries, such as those offered by Enamine (65 billion compounds) and OTAVA (55 billion compounds), where direct empirical screening of every molecule is physically and financially infeasible [1]. VS acts as a powerful filter, prioritizing compounds for subsequent experimental testing and significantly increasing the hit rate compared to traditional high-throughput screening (HTS) alone [35].
The workflow for virtual screening can be broadly classified into two distinct but complementary strategies: Ligand-Based VS and Structure-Based VS. The choice between them depends primarily on the available information about the target and known active compounds. The following diagram illustrates the decision-making workflow for selecting and executing a virtual screening strategy.
Ligand-Based Virtual Screening
Ligand-Based Virtual Screening (LBVS) is employed when the three-dimensional structure of the target is unknown or uncertain, but a set of molecules with confirmed activity against the target is available [35]. This approach operates on the principle of molecular similarity, which posits that structurally similar molecules are likely to exhibit similar biological activities. LBVS methods include:
- Pharmacophore Modeling: A pharmacophore represents the essential molecular features (e.g., hydrogen bond donors/acceptors, hydrophobic regions, aromatic rings, charged groups) and their spatial arrangement necessary for biological activity [41] [35]. LBVS uses this model as a 3D query to search databases for compounds that match the feature arrangement.
- Quantitative Structure-Activity Relationship (QSAR): QSAR is a chemometric method that constructs a mathematical model correlating quantitative descriptors of molecular structure (e.g., lipophilicity, polar surface area, molecular weight) with a known biological activity [35]. This model can then predict the activity of new, untested compounds from a virtual library [40] [35].
Structure-Based Virtual Screening
Structure-Based Virtual Screening (SBVS) requires the knowledge of the three-dimensional atomic structure of the target protein, often obtained from the Protein Data Bank (PDB) [40] [35]. This approach directly evaluates the potential for a ligand to bind within a specific site on the target, typically the active site. The core methodology of SBVS is molecular docking, which involves two main steps:
- Pose Prediction: Sampling possible orientations (poses) and conformations of the ligand within the binding site.
- Scoring: Ranking these poses using a scoring function to estimate the strength of the interaction (binding affinity) [35].
Molecular Docking: Methodologies and Protocols
Molecular docking is a cornerstone technique of SBDD that predicts the preferred orientation of a small molecule (ligand) when bound to its macromolecular target (receptor) [35]. The primary goal is to predict the binding pose and estimate the binding affinity, providing critical insights for lead optimization in rational drug design. A well-defined docking protocol, as exemplified in recent studies targeting SARS-CoV-2 Mpro, involves several sequential steps to ensure reliable and reproducible results [40].
Table 2: Key Research Reagents and Computational Tools in CADD
| Reagent / Software Tool | Type | Primary Function in CADD |
|---|---|---|
| Target Protein (e.g., Mpro, PDB: 7BE7) | Biological Macromolecule | The 3D structure serves as the target for docking and virtual screening simulations [40]. |
| Compound Libraries (e.g., Enamine, OTAVA) | Chemical Database | Ultra-large collections of "make-on-demand" molecules used as the source for virtual screening hits [1]. |
| Discovery Studio (DS) | Software Suite | Integrated platform for performing protein preparation, pharmacophore modeling, molecular docking, and analysis of results [40]. |
| BIOVIA Draw | Software Tool | Used for drawing and preparing 2D structures of compounds for QSAR and database building [40]. |
| AutoDock Vina / GOLD | Docking Engine | Algorithms that perform the conformational sampling and scoring of ligands within a protein binding site [35]. |
Experimental Protocol for Molecular Docking
The following protocol outlines a standard workflow for a molecular docking study, synthesizing methodologies from key search results [40] [35].
Step 1: Protein Target Preparation The process begins by obtaining the three-dimensional crystal structure of the target protein from the RCSB Protein Data Bank (e.g., PDB ID: 7BE7 for SARS-CoV-2 Mpro) [40]. Using software like Discovery Studio, the protein structure is "cleaned" by removing water molecules, co-crystallized native ligands, and any irrelevant ions. The protein is then prepared by adding hydrogen atoms, assigning partial charges (e.g., using a CHARMm force field), and defining protonation states of residues at biological pH [40].
Step 2: Ligand Database Preparation A library of compounds for docking is compiled from commercial or public databases (e.g., ZINC, PubChem). The 2D structures of these compounds are drawn or downloaded and converted into 3D models. Energy minimization is performed to optimize the geometry, and necessary chemical descriptors are calculated [40] [35].
Step 3: Docking Simulation and Analysis The preprocessed ligand library is docked into the defined binding site of the prepared protein using a docking program such as AutoDock Vina or a tool within Discovery Studio. The docking algorithm generates multiple putative binding poses for each ligand, which are then ranked based on a scoring function. The top-ranked compounds, such as ENA482732 in the Mpro study, are selected based on their docking scores and critical analysis of their non-bonding interactions (e.g., hydrogen bonds, hydrophobic contacts, pi-stacking) with the target [40]. The entire docking and virtual screening workflow, from preparation to hit identification, is summarized below.
Advanced Applications and Integrative Approaches
The true power of modern CADD is realized when virtual screening and molecular docking are integrated with other computational and experimental techniques, creating a synergistic cycle of prediction and validation. This integration is pivotal for addressing complex challenges in drug discovery.
Synergy with AI and Machine Learning: Machine learning (ML) is revolutionizing medicinal chemistry by identifying hidden patterns in ultra-large datasets beyond human capacity [1]. ML models can enhance virtual screening by improving the accuracy of scoring functions, predicting ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties early in the process, and even generating novel molecular structures with desired properties [39]. The informacophore concept is a prime example, where machine-learned representations of molecular structure are used to identify minimal features essential for bioactivity [1].
Addressing Drug Resistance and Multi-Target Design: CADD strategies are effectively employed to combat drug resistance. For instance, molecular docking and dynamics simulations have been used to identify second-generation inhibitors targeting mutant isocitrate dehydrogenase 1 (mIDH1) in acute myeloid leukemia, overcoming resistance to first-generation drugs [39]. Similarly, CADD enables the virtual screening of inhibitors that simultaneously bind multiple domains within a protein (e.g., PTK6) or interact with multiple therapeutic targets, potentially improving efficacy and reducing resistance [39].
Validation through Biological Functional Assays: Computational predictions must be rigorously confirmed through experimental validation. Biological functional assays—such as enzyme inhibition, cell viability, and high-content screening—provide the indispensable empirical backbone of the discovery process [1]. They offer quantitative insights into compound activity, potency, and mechanism of action, validating or challenging computational hypotheses and providing critical feedback to guide the next cycle of rational design [1]. Successful case studies like the repurposed JAK inhibitor Baricitinib for COVID-19 and the novel antibiotic Halicin underscore this principle; their computational promise was confirmed through extensive in vitro and in vivo functional assays [1].
Virtual screening and molecular docking stand as indispensable pillars of Computer-Aided Drug Design, firmly embedded within the rational drug design paradigm. By leveraging computational power to explore vast chemical spaces and predict molecular interactions at an atomic level, these methodologies dramatically accelerate the initial phases of drug discovery, reduce costs, and provide deep mechanistic insights. The continued evolution of these fields, particularly through integration with artificial intelligence and machine learning, promises to further enhance the precision, efficiency, and predictive power of drug discovery campaigns. However, the ultimate success of any computationally derived lead candidate remains dependent on a rigorous, iterative cycle of in silico prediction and experimental validation, ensuring that virtual promises translate into tangible therapeutic breakthroughs.
Rational Drug Design (RDD) represents a foundational paradigm in modern medicinal chemistry, exploiting detailed molecular recognition principles to systematically develop therapeutic agents. Unlike traditional empirical approaches, RDD employs a target-driven strategy that proceeds through three core steps: designing compounds conforming to specific structural requirements, synthesizing these molecules, and rigorously testing their biological activity [5]. This method fundamentally operates on the principle that understanding the three-dimensional arrangement of chemical groups in a target macromolecule's active site enables researchers to conceive new molecules that can optimally interact with the protein to either block or trigger a specific biological action [5]. Within this RDD framework, lead discovery serves as the critical gateway where initial candidate molecules are identified for further optimization, with High-Throughput Screening (HTS) and Fragment-Based Drug Discovery (FBDD) emerging as two premier strategies for this purpose.
The theoretical foundation of RDD rests on molecular recognition models, primarily the lock-and-key model proposed by Emil Fischer in 1890, where a substrate fits into the active site of a macromolecule with stereochemical precision, and the induced-fit theory developed by Daniel Koshland in 1958, which accounts for conformational changes in both ligand and target during recognition [5]. These principles enable two complementary RDD approaches: receptor-based drug design (utilizing known three-dimensional protein structures) and pharmacophore-based drug design (leveraging structural information from active molecules when the protein structure is unknown) [5]. The emergence of "informacophores" – minimal chemical structures combined with computed molecular descriptors, fingerprints, and machine-learned representations essential for biological activity – further exemplifies the evolution of RDD in the big data era, offering a more systematic and bias-resistant strategy for molecular optimization [1].
High-Throughput Screening (HTS) in Lead Discovery
Principles and Methodologies
High-Throughput Screening constitutes a paradigm of automated experimentation that enables the rapid testing of thousands to millions of chemical compounds for biological activity against therapeutic targets. HTS utilizes robotic automation, miniaturized assays, and parallel processing to execute large-scale experiments that would be impractical with manual methods [42] [43]. This approach has become indispensable in early-stage drug discovery, allowing researchers to quickly identify "hit" compounds with desired activity from vast chemical libraries [42]. The fundamental advantage of HTS lies in its massive scalability; where traditional methods might process dozens of samples, HTS can process thousands of compounds simultaneously, dramatically accelerating the hit identification phase [43].
The technological infrastructure enabling modern HTS encompasses several integrated components. Robotic automation systems handle physical tasks like sample preparation, liquid handling, and plate management, enabling thousands of daily experiments with minimal human intervention [43]. Microplate readers facilitate various detection modalities including absorbance and luminescence detection, while assay miniaturization through multiplex assays and plate replication boosts productivity by reducing reagent costs and space requirements [42]. Advanced data acquisition systems manage the enormous data volumes generated, with quality control procedures such as z-factor calculation ensuring data reliability and accuracy [42]. The implementation of positive controls in HTS ensures consistent and reliable results, while statistical analysis software and machine learning models aid in hit rate calculation and compound library screening [42].
Experimental Protocols and Workflow
A standardized HTS protocol follows a sequential workflow designed to maximize efficiency while maintaining scientific rigor:
Assay Development and Optimization: Prior to screening, researchers develop and validate a robust assay system that accurately measures the desired biological activity. This involves selecting appropriate detection methods (e.g., fluorescence, luminescence, absorbance), determining optimal reagent concentrations, and establishing controls. Assay miniaturization typically occurs in 384-well or 1536-well plates to maximize throughput [42].
Compound Library Management: Chemical libraries ranging from thousands to millions of compounds are prepared in dimethyl sulfoxide (DMSO) stocks and reformatted into screening-ready plates. Sample management systems ensure proper tracking, storage, and retrieval of compounds throughout the screening process [42].
Automated Screening Execution: Robotic systems transfer nanoliter to microliter volumes of compounds and reagents to assay plates in a predefined sequence. The process includes:
Data Acquisition and Analysis: Raw data is collected and processed through specialized software. Key steps include:
- Data normalization to correct for plate-based variations
- Hit identification using statistical thresholds (typically >3 standard deviations from mean)
- Quality assessment using metrics like z-factor (with values >0.5 indicating excellent assays) [42]
Hit Confirmation: Primary hits undergo retesting in dose-response formats to determine potency (IC₅₀/EC₅₀ values) and confirm activity [42].
The following diagram illustrates the core HTS workflow:
Quantitative Landscape and Applications
The HTS market continues to expand significantly, reflecting its entrenched position in drug discovery. Current projections estimate the global HTS market will reach USD 18.8 billion by 2029, growing at a compound annual growth rate (CAGR) of 10.6% from 2025-2029 [42]. North America dominates the market, accounting for approximately 50% of global growth, followed by Europe and the Asia-Pacific region [42]. The technology's applications span multiple domains, with target identification representing the largest application segment valued at USD 7.64 billion in 2023 [42].
Table 1: High-Throughput Screening Market Analysis and Applications
| Parameter | Value/Range | Context and Significance |
|---|---|---|
| Global Market Size (2029) | USD 18.8 billion | Projected market value during 2025-2029 period [42] |
| Growth Rate (CAGR) | 10.6% | Forecast period from 2025-2029 [42] |
| Market Dominance | North America (50%) | Accounts for half of global market growth [42] |
| Leading Application | Target Identification | Valued at USD 7.64 billion in 2023 [42] |
| Throughput Capacity | Thousands to 100,000+ compounds/day | Varies by automation level and assay complexity [42] [43] |
| Primary End-users | Pharmaceutical Companies | Largest revenue share, followed by academic institutes and CROs [42] |
| Key Technologies | Cell-based Assays, Ultra-HTS, Label-free | Major technological segments driving innovation [42] |
The implementation of HTS provides substantial operational advantages, with studies reporting 5-fold improvements in hit identification rates compared to traditional methods, and development timelines reduced by approximately 30% [42] [43]. The technology has evolved beyond simple binding assays to encompass complex phenotypic screening, high-content imaging, and 3D cell culture models that provide more physiologically relevant data [42] [44]. The continuing integration of artificial intelligence and machine learning further enhances screening efficiency by enabling better analysis of complex biological data and predictive modeling of compound efficacy [44].
Fragment-Based Drug Discovery (FBDD)
Principles and Methodologies
Fragment-Based Drug Discovery has emerged as a powerful complementary approach to HTS, particularly for tackling challenging targets with featureless or flat binding surfaces such as protein-protein interactions [45]. Instead of screening large, complex molecules, FBDD begins with very small chemical fragments (molecular weight typically <250 Da) that bind weakly but efficiently to discrete regions of the target [45] [46]. These fragments subsequently undergo systematic optimization through iterative structure-guided design to develop higher-affinity leads [46]. The fundamental premise of FBDD rests on the superior sampling of chemical space achievable with fragment libraries; while a typical HTS library of 10⁶ compounds samples only a minute fraction of possible drug-like molecules, a fragment library of 10³ compounds provides more efficient coverage of chemical space due to the fragments' simplicity and combinatorial potential [45].
The theoretical foundation of FBDD acknowledges that fragment binding efficiency often exceeds that of larger compounds when normalized by molecular weight, providing superior starting points for optimization [46]. This approach is particularly valuable for targeting the growing number of "difficult" drug targets, including those with flat, featureless binding surfaces that traditionally evade small-molecule intervention [45]. The success of FBDD is evidenced by its contribution to the drug development pipeline, with close to 70 drug candidates currently in clinical trials and at least 7 marketed medicines originating from fragment screens [45]. The methodology has evolved significantly over the past two decades, earning its place as a premier strategy for discovering new small molecule drug leads [45].
Experimental Protocols and Workflow
The FBDD workflow comprises distinct stages that transform weak fragment hits into potent lead compounds:
Fragment Library Design: Curating a collection of 500-5,000 fragments with emphasis on:
- Low molecular weight (<250 Da)
- High solubility (>1 mM in aqueous buffer)
- Structural simplicity with potential for synthetic elaboration
- Chemical diversity covering various scaffolds [45]
Primary Fragment Screening: Employing sensitive biophysical techniques to detect weak binding (typical Kd values 0.1-10 mM):
- Surface Plasmon Resonance (SPR) for binding kinetics and affinity
- Nuclear Magnetic Resonance (NMR) spectroscopy for structural information
- X-ray Crystallography for atomic-resolution binding modes
- Thermal Shift Assays for protein stabilization measurements [45]
Hit Validation and Characterization: Confirming binding through orthogonal methods and determining:
- Binding affinity (Kd) using dose-response measurements
- Ligand efficiency (LE = -RT ln(IC₅₀)/heavy atom count)
- Binding mode through co-crystallization when possible [45]
Fragment Optimization: Iterative structure-based design cycles including:
The following diagram illustrates the FBDD workflow:
Technological innovations continue to enhance FBDD efficiency. Recent advances include high-throughput SPR-based fragment screening over large target panels that can be completed in days rather than years, enabling rapid ligandability testing and general pocket finding [45]. This approach reveals fragment hit selectivity and allows affinity cluster mapping across many targets, helping identify selective fragments with favorable enthalpic contributions that possess more development potential [45]. Additionally, novel approaches leveraging avidity effects to stabilize weak fragment-protein interactions enable protein-binding fragments to be isolated from large libraries quickly and efficiently using only modest amounts of protein [45].
Case Studies and Success Metrics
FBDD has demonstrated remarkable success across diverse target classes, yielding clinical candidates and marketed drugs. Notable examples include:
Pan-RAS Inhibitors: The fragment-based discovery of novel, reversible pan-RAS inhibitors binding in the Switch I/II pocket. Through structure-enabled design, fragments were developed into a series of macrocyclic analogues that effect inhibition of the RAS/RAF interaction and downstream phosphorylation of ERK [45].
RIP2 Kinase Inhibitors: A fragment-based screening and design program leading to the discovery of pyrazolocarboxamides as novel inhibitors of receptor interacting protein 2 kinase (RIP2). Fragment evolution, robust crystallography, and structure-based design afforded advanced pyrazolocarboxamides with excellent biochemical and whole blood activity and improved kinase selectivity [45].
WRN Helicase Inhibitors: Identification and development of fragment-derived chemical matter in previously unknown allosteric sites of WRN, a key target for MSI-H or MMRd tumors. Fragment-based screening revealed a novel allosteric binding pocket in this dynamic helicase, enabling chemical progression of fragment hits [45].
STING Agonists: Optimization of a fragment hit yielding ABBV-973, a potent, pan-allele small molecule STING agonist for intravenous administration [45].
Table 2: Fragment-Based Drug Discovery Success Metrics and Applications
| Parameter | Value/Range | Context and Significance |
|---|---|---|
| Marketed Drugs | At least 7 | Approved medicines originating from fragment screens [45] |
| Clinical Candidates | ~70 drugs | Currently in clinical trials [45] |
| Target Classes | Kinases, Proteases, PPI targets, Helicases | Broad applicability across target types [45] |
| Typical Fragment Library Size | 500-5,000 compounds | Significantly smaller than HTS libraries [45] |
| Initial Fragment Affinity | 0.1-10 mM (Kd) | Very weak binding requiring sensitive detection [45] |
| Key Screening Methods | SPR, NMR, X-ray Crystallography | Sensitive biophysical techniques [45] |
| Special Strength | "Difficult" and flat binding sites | Particularly valuable for protein-protein interactions [45] |
The continued advancement of FBDD incorporates cutting-edge computational and screening methods, including covalent fragment strategies to unlock difficult-to-drug targets [45]. The integration of structural and computational tools has significantly enhanced FBDD efficiency, facilitating rational drug design and expanding the approach to novel modalities beyond traditional targets [46].
Comparative Analysis and Integration
Strategic Selection and Hybrid Approaches
While both HTS and FBDD serve the critical lead discovery function in drug development, their strategic applications differ significantly based on project requirements, target characteristics, and available resources. Understanding their complementary strengths enables research teams to deploy the most appropriate strategy or develop hybrid approaches that leverage the advantages of both methodologies.
Table 3: Strategic Comparison Between HTS and FBDD Approaches
| Parameter | High-Throughput Screening (HTS) | Fragment-Based Drug Discovery (FBDD) |
|---|---|---|
| Library Size | 10⁵-10⁷ compounds | 10²-10⁴ fragments |
| Compound Properties | Drug-like molecules (MW 300-500 Da) | Simple fragments (MW <250 Da) |
| Initial Affinity Range | nM-μM | μM-mM |
| Screening Methods | Biochemical/cell-based assays | Biophysical (SPR, NMR, X-ray) |
| Chemical Space Coverage | Limited but specific | Broad and efficient |
| Target Classes | Well-behaved soluble targets | Challenging targets (PPIs, allosteric sites) |
| Hit Rate | Typically 0.01-1% | Typically 0.1-10% |
| Optimization Path | Relatively straightforward | Requires significant structural guidance |
| Resource Requirements | High infrastructure investment | High expertise investment |
| Timeline | Rapid hit identification | Longer hit-to-lead process |
The synergy between HTS and FBDD is increasingly recognized as a powerful combination in modern drug discovery. HTS can identify potent starting points for well-behaved targets with established assay systems, while FBDD excels where HTS fails, particularly for challenging targets with featureless binding surfaces [45] [46]. Some organizations implement both approaches in parallel, using HTS for immediate lead generation while employing FBDD for longer-term pipeline development against more difficult targets.
The ideal integration occurs when information is available for both the target protein and active molecules, allowing receptor-based and ligand-based design to be developed independently yet synergistically [5]. In such scenarios, molecules designed through one approach can be validated through the other – for example, promising docked molecules designed with favorable target interactions can be compared to active structures, while interesting mimics of active compounds can be docked into the protein structure to assess convergent conclusions [5]. This synergistic integration creates a powerful feedback loop that substantially accelerates the discovery process.
The Scientist's Toolkit: Essential Research Reagents and Technologies
Successful implementation of HTS and FBDD requires specialized reagents, instruments, and computational resources. The following table details core components of the lead discovery toolkit:
Table 4: Essential Research Reagents and Technologies for Lead Discovery
| Category | Specific Tools/Reagents | Function and Application |
|---|---|---|
| HTS Automation | Robotic liquid handlers, plate readers, automated incubators | Enables high-volume screening with minimal manual intervention [42] [43] |
| FBDD Detection | SPR systems, NMR spectrometers, X-ray crystallography platforms | Detects weak fragment binding (μM-mM range) [45] |
| Compound Libraries | Diverse small molecule collections (HTS), fragment libraries (FBDD) | Source of chemical starting points for screening [1] [45] |
| Assay Technologies | Fluorescent/luminescent probes, cell-based reporter systems, biochemical kits | Measures biological activity and target engagement [42] |
| Specialized Reagents | Purified protein targets, cell lines, detection antibodies | Critical components for assay development [42] [45] |
| Data Analysis | Statistical software, machine learning algorithms, visualization tools | Processes large datasets and identifies valid hits [1] [42] |
| Structural Biology | Crystallization screens, homology modeling software | Provides atomic-level insights for structure-based design [45] [5] |
Emerging Technologies and Future Directions
The landscape of lead discovery continues to evolve with the integration of advanced computational methods, artificial intelligence, and novel screening paradigms. Artificial intelligence and machine learning are transforming both HTS and FBDD by enabling predictive modeling to identify promising candidates, automated image analysis, experimental design optimization, and advanced pattern recognition in complex datasets [43] [44]. GPU-accelerated computing platforms drive high-throughput research, with demonstrated capabilities to make genomic sequence alignment up to 50× faster than CPU-only methods, unlocking large-scale studies that were once impractical [43].
The emerging field of pharmacotranscriptomics-based drug screening (PTDS) represents a paradigm shift from traditional target-based and phenotype-based screening approaches [47]. PTDS detects gene expression changes following drug perturbation in cells on a large scale and analyzes the efficacy of drug-regulated gene sets, signaling pathways, and complex diseases by combining artificial intelligence [47]. This approach is particularly suitable for detecting complex drug efficacy profiles, as demonstrated in applications screening traditional Chinese medicine, and is categorized into microarray, targeted transcriptomics, and RNA-seq methodologies [47].
Covalent fragment approaches are expanding the chemical tractability of the human proteome, particularly for challenging targets that have resisted conventional drug discovery efforts [45]. Photoaffinity-based chemical proteomic strategies are being developed to broadly map ligandable sites on proteins directly in cells, advancing this information into useful chemical probes for targets playing critical roles in human health and disease [45]. Additionally, the integration of quantum chemistry methods like F-SAPT (Functional-group Symmetry-Adapted Perturbation Theory) provides unprecedented insight into protein-ligand interactions by quantifying both the strength and fundamental components of intermolecular interactions [45].
The ongoing maturation of these technologies within the framework of rational drug design promises to further accelerate lead discovery, enhance success rates, and expand the druggable genome. As computational and experimental methods continue to converge, the integration of HTS, FBDD, and emerging screening paradigms will undoubtedly shape the future of therapeutic development, offering powerful strategies to address increasingly challenging biological targets in human disease.
Rational Drug Design (RDD) represents a methodical approach to drug discovery that leverages the three-dimensional structural knowledge of biological targets to create novel therapeutic agents. This paradigm shift from traditional trial-and-error screening to structure-based design has dramatically accelerated pharmaceutical development, particularly in antiviral therapeutics. The development of Human Immunodeficiency Virus (HIV) protease inhibitors stands as a landmark achievement in RDD, demonstrating how precise atomic-level understanding of enzyme structure and function can yield life-saving medications [48]. These inhibitors have become cornerstone components of combination antiretroviral therapy (cART), transforming HIV/AIDS from a fatal diagnosis to a manageable chronic condition [49]. This whitepaper examines key case studies illustrating RDD principles applied to HIV protease inhibitors, details experimental methodologies, and explores emerging directions in the field, providing a comprehensive technical resource for drug development professionals.
HIV Protease: Structure, Function, and Therapeutic Significance
Biological Role and Structural Characteristics
HIV protease is an aspartic protease that is essential for viral replication. It functions as a C2-symmetric homodimer, with each monomer consisting of 99 amino acid residues. The catalytic site contains a conserved Asp-Thr-Gly sequence with two aspartic acid residues (Asp-25 and Asp-25') that are critical for proteolytic activity [48]. This enzyme is responsible for cleaving the viral Gag and Gag-Pol polyprotein precursors into mature functional proteins, including reverse transcriptase, protease itself, and integrase. Without this proteolytic processing, viral particles remain immature and non-infectious [50] [49].
The enzyme features a flexible flap region (residues 43-58) that covers the active site and undergoes significant conformational changes during substrate binding and catalysis. Molecular dynamics simulations have revealed that these flaps fluctuate between closed, semi-open, and wide-open conformations, with the semi-open state representing the thermodynamically favored conformation in the ligand-free enzyme [51]. This dynamic behavior is crucial for substrate access to the active site and represents an important consideration for inhibitor design.
RDD Target Rationale and Validation
HIV protease presents an ideal target for RDD approaches due to several key characteristics. Its well-defined active site allows for precise molecular interactions with designed inhibitors. The enzyme's essential role in the viral life cycle means that effective inhibition directly prevents viral replication. Additionally, as a viral enzyme with no direct human equivalent, inhibitors can achieve high specificity, minimizing off-target effects [48]. The validation of HIV protease as a drug target was confirmed through mutagenesis studies showing that mutations in the active site (e.g., G40E and G40R) produce non-infectious viral particles due to impaired proteolytic activity [51].
Table 1: Key Characteristics of HIV Protease as an RDD Target
| Characteristic | Significance for RDD |
|---|---|
| Homodimeric structure | Allows for symmetric inhibitor design |
| Conserved catalytic aspartates | Provides defined anchor points for inhibitor binding |
| Flexible flap region | Presents opportunity for allosteric inhibition strategies |
| High-resolution crystal structures available | Enables precise structure-based design |
| Essential for viral maturation | Target inhibition directly correlates with therapeutic effect |
Case Study 1: RDD-142 - A Darunavir Analog Precursor
Compound Profile and Repurposing Strategy
RDD-142 ((N-((2R,3S)-3-amino-2-hydroxy-4-phenylbutyl)-N-benzyl methoxybenzenesulfonamide)) represents an innovative application of RDD principles through drug repurposing strategy. This synthetic molecule is a precursor of the Darunavir analog, an established HIV-1 protease inhibitor, but was investigated for its potential application in hepatocellular carcinoma (HCC) treatment [52]. This case exemplifies the expanding applications of RDD beyond initial indications, leveraging established compounds against novel targets.
The compound was evaluated both as a free molecule and in liposomal formulation to enhance its pharmacokinetic profile. The liposomal formulation was developed using a simple, rapid, organic solvent-free procedure that generates stable nanoscale vesicles. PEGylated phospholipids were incorporated to prolong circulation time in the bloodstream, addressing common limitations of therapeutic molecules such as poor solubility and short half-life [52].
Mechanism of Action and Experimental Validation
RDD-142 exhibits a multi-mechanistic antiproliferative activity in hepatocellular carcinoma (HepG2) cells while preserving healthy immortalized human hepatocyte (IHH) cells. Mechanistic studies revealed that RDD-142 delays cancer cell proliferation by attenuating the ERK1/2 signaling pathway and concurrently activating autophagy through p62 up-regulation [52].
These effects were linked to RDD-142's inhibitory activity on the chymotrypsin-like subunit of the proteasome, which triggers an unfolded protein response (UPR)-mediated stress response. The cytostatic effect was demonstrated to be dose-dependent, with an IC50 value of 41.3 µM determined by xCELLigence real-time cell analysis after 24 hours of treatment. Cell cycle analysis revealed significant G2/M phase accumulation, with approximately 50% of cells blocked in this phase at 30 µM concentration [52].
Table 2: Experimental Characterization of RDD-142 Antiproliferative Activity
| Parameter | Method | Result |
|---|---|---|
| IC50 (HepG2) | xCELLigence real-time cell analysis | 41.3 µM (24h treatment) |
| IC50 (IHH) | xCELLigence real-time cell analysis | >100 µM (2.5x higher than HepG2) |
| Cell cycle disruption | Flow cytometry with PI staining | G2/M phase accumulation (50% at 30 µM) |
| Proteasome inhibition | Immunoblotting | Chymotrypsin-like subunit activity reduction |
| Pathway modulation | Western blot | ERK1/2 signaling attenuation; p62 up-regulation |
Formulation Optimization and Efficacy Enhancement
The liposomal formulation of RDD-142 demonstrated significant advantages over the free compound. Experimental results showed that the PEGylated liposomal formulation significantly enhanced intracellular intake and cytotoxic efficacy against HepG2 cells [52]. This formulation approach offers a successful strategy to reduce effective dosage and minimize adverse effects, addressing key challenges in oncology therapeutics.
The enhanced performance of the liposomal formulation underscores the importance of delivery system optimization in RDD, demonstrating that compound efficacy depends not only on target binding but also on pharmacokinetic properties. This case study illustrates how traditional RDD approaches can be augmented with formulation science to maximize therapeutic potential.
Case Study 2: Amprenavir - Structure-Based Design of a Protease Inhibitor
Design Strategy and Molecular Interactions
Amprenavir represents a classic success story in structure-based RDD of HIV protease inhibitors. The compound was designed as a potent and selective HIV-1 PR inhibitor with sub-nanomolar inhibition activity (Kᵢ = 0.6 nM) [50]. The design strategy employed transition state mimicry, where the peptide linkage (-NH-CO-) typically cleaved by the protease was replaced by a hydroxyethylen group (-CH₂-CH(OH)-) that the enzyme cannot cleave [48].
This peptidomimetic approach maintains binding affinity while conferring metabolic stability. Amprenavir features a core structure similar to saquinavir but incorporates different functional groups on both ends: a tetrahydrofuran carbamate group on one end and an isobutylphenyl sulfonamide with an added amide on the other [48]. This strategic design resulted in fewer chiral centers, simplifying synthesis and enhancing aqueous solubility, which subsequently improved oral bioavailability.
Ensemble Docking and Conformational Flexibility
The critical role of enzyme conformational flexibility in inhibitor binding was demonstrated through comprehensive ensemble docking studies. These investigations utilized multiple crystallographic structures of HIV-1 protease (52 distinct PDB structures) to account for target flexibility in predicting binding modes and energies [50].
The ensemble docking approach revealed that different protease conformations yielded varying interaction modes and binding energies with Amprenavir. Analysis demonstrated that the conformation of the receptor significantly affects the accuracy of docking results, highlighting the importance of considering protein dynamics in structure-based RDD [50]. The optimal induced fit was predicted for the conformation captured in PDB ID: 1HPV, providing atomic-level insights into the binding mechanism.
Experimental Validation and Binding Mode Analysis
Docking validation was performed by redocking the cognate ligand (Amprenavir) into the active site of various HIV-1 protease structures. The success of the docking method was confirmed by its ability to reproduce the original binding mode, with root mean square deviation (RMSD) values generally below 3.0 Å for most protease conformations [50].
The 2D interaction diagrams generated from these studies revealed an extensive network of hydrogen bonds and hydrophobic interactions stabilizing the inhibitor-enzyme complex. Specifically, Amprenavir forms critical hydrogen bonds with the catalytic aspartate residues (Asp-25 and Asp-25') and maintains multiple hydrophobic contacts with residues in the flap region and active site pocket [50]. These detailed interaction maps informed subsequent optimization efforts and contributed to the development of next-generation inhibitors.
Computational Methodologies in RDD
Molecular Dynamics Simulations of Protease Dynamics
Molecular dynamics (MD) simulations have provided crucial insights into the conformational flexibility of HIV protease and its implications for inhibitor design. Studies examining the protease in its free, inhibitor-bound (ritonavir), and antibody-bound forms have revealed that upon binding, the overall flexibility of the protease decreases, including the flap region and active site [51].
Simulations of the free wild-type protease demonstrated that the flap region fluctuates between closed, semi-open, open, and wide-open conformations, with flap tip distances (measured between Ile-50 Cα atoms) ranging from ~0.6 nm in closed states to >3.0 nm in wide-open states [51]. This dynamic behavior is essential for substrate access and product release. Upon inhibitor binding, the mean flap tip distance stabilizes at approximately 0.6 ± 0.1 nm, corresponding to the closed conformation, effectively restricting the open-close mechanism essential for proteolytic activity.
Allosteric Inhibition Strategies
MD simulations have also illuminated allosteric inhibition mechanisms through antibody binding and specific mutations. Studies of the monoclonal antibody F11.2.32, which binds to the epitope region (residues 36-46) of HIV protease, demonstrated that antibody binding reduces protease flexibility similarly to active-site inhibitors [51]. This allosteric inhibition strategy offers potential for addressing drug resistance, as the elbow region is less susceptible to mutations than the active site.
Analysis of protease mutants (G40E and G40R) with decreased enzymatic activity revealed that these mutations similarly rigidify the protease structure, restricting flap opening and decreasing overall residue flexibility [51]. These findings highlight the importance of dynamics in protease function and suggest that control of flexibility through allosteric modulators represents a promising approach for next-generation inhibitor design.
Diagram 1: HIV protease inhibition mechanisms showing both active-site and allosteric strategies converging on conformational restriction.
Experimental Protocols for Key RDD Methodologies
Ensemble Docking Protocol for HIV Protease Inhibitors
The ensemble docking approach provides a robust methodology for accounting for protein flexibility in structure-based drug design. The following protocol, adapted from studies with Amprenavir, offers a framework for comprehensive docking analyses [50]:
Structure Preparation: Retrieve multiple crystallographic structures of the target protein (HIV protease) from the Protein Data Bank. Both holo (ligand-bound) and apo (unliganded) structures should be included to capture conformational diversity.
Receptor Pre-processing: Prepare receptor PDB files using tools like AutoDock Tools and WHAT IF server. Add all hydrogen atoms properly, merge non-polar hydrogens into corresponding carbon atoms, and assign Kollman charges.
Ligand Preparation: Generate 3D structures of ligands using programs like CORINA. Assign Gasteiger charges, define torsional degrees of freedom, and identify rotatable bonds.
Grid Generation: Create a grid box (typically 60×60×60 points in x, y, and z directions) centered on the catalytic site of the protease structures to define the search space for docking simulations.
Docking Parameters: Employ Lamarckian genetic algorithm with 100 independent runs and 2.5×10⁷ maximum number of energy evaluations. Maintain other parameters at default values unless specified by specific requirements.
Cluster Analysis: Perform cluster analysis on docking results using a root mean square tolerance of 2.0 Å to identify predominant binding modes.
Interaction Analysis: Generate schematic 2D representations of ligand-receptor interactions using visualization tools like LIGPLOT to identify key molecular contacts.
Liposomal Formulation Protocol for Enhanced Delivery
The development of liposomal formulations for compounds like RDD-142 follows this optimized protocol [52]:
Lipid Film Formation: Dissolve PEGylated phospholipids (e.g., DSPE-PEG2000) with cholesterol in organic solvent in a round-bottom flask. Remove solvent under reduced pressure using a rotary evaporator to form a thin lipid film.
Hydration: Hydrate the lipid film with aqueous phase containing the drug molecule (e.g., RDD-142) in appropriate buffer above the phase transition temperature of the lipids.
Size Reduction: Subject the multilamellar vesicle suspension to extrusion through polycarbonate membranes with decreasing pore sizes (typically 400 nm, 200 nm, and 100 nm) using a lipid extruder to obtain unilamellar vesicles of desired size.
Purification: Separate unencapsulated drug from liposomal formulation using size exclusion chromatography or dialysis against suitable buffer.
Characterization: Determine particle size and size distribution by dynamic light scattering, zeta potential by laser Doppler anemometry, and encapsulation efficiency by HPLC analysis after disruption of liposomes with organic solvent.
Diagram 2: Integrated RDD workflow showing computational and experimental phases in HIV protease inhibitor development.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for HIV Protease RDD Studies
| Reagent/Material | Specifications | Application | Rationale |
|---|---|---|---|
| HIV-1 Protease | Recombinant, purified homodimer | Enzymatic assays, binding studies | Target protein for functional and structural studies |
| HepG2 Cells | Human hepatocellular carcinoma line | Cytotoxicity and proliferation assays | Model system for anticancer activity assessment |
| IHH Cells | Immortalized human hepatocytes | Selectivity and toxicity screening | Non-malignant control for specificity determination |
| PEGylated Lipids | DSPE-PEG2000, HSPC, cholesterol | Nanoparticle formulation | Enhanced drug delivery and pharmacokinetics |
| xCELLigence System | RTCA DP Instrument | Real-time cell proliferation monitoring | Label-free, dynamic assessment of cytostatic effects |
| AutoDock Software | Version 4.2 with ADT tools | Molecular docking simulations | Prediction of ligand-protein interactions and binding modes |
| Propidium Iodide | >94% purity by HPLC | Cell cycle analysis by flow cytometry | DNA staining for cell cycle phase distribution |
| Proteasome Activity Kit | Chymotrypsin-like subunit specific | Proteasome inhibition assays | Target engagement validation for RDD-142 |
Emerging Directions and Future Perspectives
Long-Acting Formulations and Novel Delivery Systems
Recent advances in RDD for HIV therapeutics have expanded beyond traditional small molecules to include long-acting formulations and innovative delivery strategies. The successful development of liposomal RDD-142 demonstrates how formulation science can enhance the therapeutic profile of existing compounds [52]. Similarly, clinical research on long-acting antiretrovirals like lenacapavir showcases the industry's movement toward extended-duration dosing regimens that improve adherence and patient outcomes [53].
The ongoing development of twice-yearly lenacapavir for pre-exposure prophylaxis (PrEP) and treatment, along with investigations into once-weekly oral combinations (e.g., islatravir and lenacapavir), represents the next frontier in HIV therapeutics [53]. These advances leverage RDD principles to optimize pharmacokinetic properties while maintaining potent antiviral activity.
Immunotherapeutic Approaches and Combination Strategies
Emerging research on anti-PD-1 inhibitors like budigalimab for HIV treatment illustrates the expanding scope of RDD to include immunomodulatory approaches [54]. Phase 1b studies have demonstrated that PD-1 blockade can enable durable viral control without antiretroviral therapy through reversal of T cell exhaustion and restoration of immune function [54].
Additionally, innovative combination approaches pairing broadly neutralizing antibodies (bNAbs) with long-acting antiretrovirals show promise as complete regimens with extended dosing intervals. Phase 2 studies of twice-yearly lenacapavir in combination with bNAbs (teropavimab and zinlirvimab) have maintained viral suppression out to 52 weeks and are progressing to Phase 3 clinical development [53].
The application of Rational Drug Design to HIV protease inhibitors has yielded remarkable successes that continue to evolve through innovative methodologies and expanding applications. The case studies of RDD-142 and Amprenavir demonstrate the power of structure-based approaches, both in repurposing existing compounds for new indications and in de novo design of targeted therapeutics. The integration of computational methods, including ensemble docking and molecular dynamics simulations, with experimental validation has created a robust framework for inhibitor development. As the field advances, emerging directions in long-acting formulations, immunotherapies, and combination regimens promise to further transform HIV treatment and potentially expand applications to other therapeutic areas. These developments underscore the enduring impact of RDD principles in addressing complex challenges in drug discovery and development.
Overcoming Challenges and Optimizing Drug Candidates in RDD
Addressing Target Flexibility and Solvation Effects in Molecular Modeling
In the paradigm of Rational Drug Design (RDD), the overarching goal is to accelerate the discovery of safe and effective therapeutics by leveraging structural and computational insights. A cornerstone of this approach is structure-based drug design (SBDD), which relies on the three-dimensional structure of a biological target to guide the development of novel ligands [55]. For decades, most SBDD and molecular modeling operated under a significant simplification: treating both the target protein and its surrounding environment as static, rigid entities. It is now widely recognized that this static view represents a major limitation, as proteins are inherently flexible systems that exist as an ensemble of interconverting conformations and function within a complex solvated environment [55] [56]. The inability to accurately model target flexibility and solvation effects has been a critical barrier in improving the success rate of computational predictions.
Target flexibility is essential for biological function, as seen in proteins like hemoglobin, which adopts distinct "tense" and "relaxed" states, and adenylate kinase, which undergoes large conformational changes in its "lids" during catalysis [55]. Similarly, solvation effects are not merely a background buffer but actively participate in binding and recognition. Water molecules mediate key interactions, and the displacement of unfavorable water from a binding pocket can be a major driver of binding affinity [57] [58]. Ignoring these phenomena leads to inaccurate predictions of ligand binding affinity and specificity, ultimately contributing to high attrition rates in later stages of drug development [55] [59]. This whitepaper details advanced computational methodologies that address these twin challenges, providing a technical guide for researchers aiming to incorporate dynamic and solvated realities into their RDD pipelines.
Theoretical Background and Key Concepts
The Spectrum of Protein Flexibility
Proteins can be classified based on their flexibility upon ligand binding. The technical literature generally recognizes three categories [55]:
- Rigid Proteins: Ligand binding induces only minor side-chain rearrangements. The Protein Data Bank (PDB) is artificially enriched with these structures due to the technical ease of their crystallization.
- Flexible Proteins: Ligand binding triggers large-scale movements around "hinge points" or active site loops, accompanied by significant side-chain motion.
- Intrinsically Unstable Proteins: These proteins lack a defined conformation until a ligand binds, a process known as "induced fit."
The fundamental paradigm for understanding flexible binding is the conformational selection model. This model posits that an unbound protein exists in a dynamic equilibrium of multiple conformations. A ligand does not "force" the protein into a new shape but selectively binds to and stabilizes a pre-existing, complementary conformation from this ensemble, shifting the equilibrium [55].
Classifying Solvation Models
Computational methods for handling solvation effects fall into two primary categories, each with distinct advantages and limitations, as summarized in the table below [60].
Table 1: Comparison of Implicit and Explicit Solvent Models
| Feature | Implicit Solvent Models | Explicit Solvent Models |
|---|---|---|
| Fundamental Approach | Treats solvent as a continuous, polarizable medium characterized by a dielectric constant (ε). | Treats individual solvent molecules (e.g., water) with their own coordinates and degrees of freedom. |
| Key Descriptors | Dielectric constant, surface tension, cavity creation energy. | Force fields (e.g., AMBER, CHARMM, TIP3P), atomistic charges, Lennard-Jones parameters. |
| Computational Cost | Relatively low; efficient for high-throughput screening and quantum mechanics calculations. | High; requires significant resources to simulate many solvent molecules and their interactions. |
| Strengths | Computationally efficient; provides a reasonable average description of bulk solvent effects. | Physically realistic; captures specific solute-solvent interactions (e.g., hydrogen bonding) and local solvent structure. |
| Weaknesses | Fails to capture specific solute-solvent interactions, hydrogen bonding, and local solvent density fluctuations. | Computationally demanding; limited sampling timescales; accuracy dependent on force field parameterization. |
Hybrid models, such as QM/MM (Quantum Mechanics/Molecular Mechanics) approaches, combine these two philosophies. In a typical QM/MM setup, the solute and a few key solvent molecules are treated with high-level quantum mechanics, while the bulk solvent is modeled either with explicit molecular mechanics or an implicit continuum, offering a balance between accuracy and computational cost [57] [61] [60].
Methodologies for Addressing Target Flexibility
Molecular Dynamics (MD) Simulations
Molecular Dynamics (MD) is a powerful computational technique that simulates the physical movements of atoms and molecules over time, based on classical Newtonian mechanics. By solving Newton's equations of motion for all atoms in the system, MD generates a "trajectory" that provides a movie-like view of the protein's motion, capturing its inherent flexibility and revealing rare, transient conformations [55] [61].
Protocol: Setting up and Running an MD Simulation for Conformational Sampling
- System Preparation: Obtain the initial protein structure from the PDB. Add missing hydrogen atoms and assign protonation states using tools like
pdb4amberorH++. Place the protein in a solvation box of explicit water molecules (e.g., TIP3P model) and add counterions to neutralize the system's charge. - Energy Minimization: Perform a series of energy minimization steps to remove any bad steric clashes introduced during the setup process. This is typically done using steepest descent and conjugate gradient algorithms.
- System Equilibration: Gradually heat the system from 0 K to the target temperature (e.g., 300 K) over 50-100 picoseconds (ps) under constant volume (NVT ensemble), applying restraints to the protein heavy atoms. Follow this with equilibration under constant pressure (NPT ensemble) for another 50-100 ps to adjust the solvent density.
- Production Run: Run an unrestrained simulation for tens to hundreds of nanoseconds (or even microseconds/milliseconds with specialized hardware). The length required depends on the conformational changes of interest. Integrate the equations of motion using algorithms like the leapfrog or velocity Verlet method with a time step of 1-2 femtoseconds. Control temperature and pressure using thermostats (e.g., Nosé-Hoover) and barostats (e.g., Parrinello-Rahman).
- Trajectory Analysis: Analyze the saved trajectory frames to identify key conformational states, calculate root-mean-square deviation (RMSD), root-mean-square fluctuation (RMSF), and other metrics. Tools like
cpptraj(AmberTools) orMDTrajare commonly used.
- System Preparation: Obtain the initial protein structure from the PDB. Add missing hydrogen atoms and assign protonation states using tools like
Advanced Sampling Techniques: Standard MD is often limited to relatively short timescales. To overcome high energetic barriers and sample rare events (like the opening of a cryptic pocket), enhanced sampling methods are employed:
- Gaussian Accelerated MD (GaMD): Adds a harmonic boost potential to the system's potential energy, smoothing the energy landscape and accelerating conformational transitions [58].
- Markov State Models (MSMs): Constructs a kinetic model from many short, distributed MD simulations, identifying long-timescale dynamics and metastable states [58].
The Relaxed Complex Scheme (RCS)
The Relaxed Complex Scheme (RCS) is a sophisticated computational strategy designed to discover ligands that bind to a range of a protein's naturally occurring conformational states, thereby explicitly accounting for target flexibility and "induced fit" effects [56].
Table 2: Key Phases of the Relaxed Complex Scheme
| Phase | Objective | Typical Methods & Tools |
|---|---|---|
| 1. Conformational Ensemble Generation | To create a diverse and representative set of protein conformations for docking. | Long-timescale MD simulations; enhanced sampling (GaMD); sampling from crystal structures. |
| 2. Molecular Docking | To screen a library of compounds against each snapshot in the conformational ensemble. | Docking software like AutoDock, DOCK, or Glide. |
| 3. Re-scoring with Advanced Free Energy Calculations | To improve the ranking of docked poses by providing more accurate binding affinity estimates. | MM/PBSA (Molecular Mechanics/Poisson-Boltzmann Surface Area) or MM/GBSA (Generalized Born Surface Area) using MD trajectories of the complex. |
The RCS is inspired by experimental methods like "SAR by NMR" and recognizes that high-affinity ligands may bind to low-population, transient conformations that are sampled during the protein's dynamics [56]. A variant, the Double-ligand RCS, can be used to identify two weak binders that can be linked into a single, high-affinity drug candidate, ensuring the chosen fragments can bind to the same protein conformation simultaneously [56].
Machine Learning and Integrated Approaches
The advent of machine learning (ML), particularly deep learning, has provided powerful new tools for predicting flexible binding sites. These methods can integrate diverse data types to identify pockets, including cryptic allosteric sites, that are difficult to find with traditional methods [58].
- Graph Neural Networks (GNNs): Models like GraphSite represent proteins as graphs where nodes are residues or atoms and edges represent spatial or chemical relationships. GNNs natively handle the non-Euclidean structure of proteins and can effectively learn the local chemical environments indicative of a binding site, even in flexible regions [58].
- Integrated and Ensemble Methods: Recognizing that no single method is universally superior, integrated platforms have been developed. The COACH server, for example, combines predictions from multiple independent algorithms (e.g., geometry-based, energy-based, and template-based) to generate a meta-prediction with superior accuracy and coverage [58].
Workflow for the Relaxed Complex Scheme
Methodologies for Addressing Solvation Effects
Implicit Solvent Models
Implicit solvent models, also known as continuum models, are a class of computational methods that replace explicit solvent molecules with a continuous polarizable medium. The solute is placed inside a molecular-shaped cavity, and the solvent's response to the solute's charge distribution is modeled mathematically [60]. The total solvation free energy (ΔGsolv) is typically decomposed into several components [60]: ΔGsolv = ΔGcavity + ΔGelectrostatic + ΔGdispersion + ΔGrepulsion
- Protocol: Performing a Geometry Optimization with an Implicit Solvent
- Select a Model: Choose an appropriate implicit solvent model for your calculation (e.g., PCM, SMD, or COSMO).
- Define the Cavity: The software will construct a cavity around the solute molecule based on a set of atomic radii (e.g., Bondi radii scaled by a factor like 1.1).
- Set Solvent Parameters: Specify the solvent's dielectric constant (e.g., ε = 78.4 for water) and other optional parameters like surface tension.
- Run the Calculation: For a geometry optimization or energy calculation at the quantum mechanical (QM) level (e.g., Density Functional Theory), the implicit solvent model is included as a perturbation to the Hamiltonian. The calculation iterates to self-consistency, where the solute's electron density and the solvent's reaction field are mutually polarized.
- Analysis: The output provides the total energy of the solvated system and often a breakdown of the solvation free energy components.
Explicit Solvent Simulations
Explicit solvent models treat each solvent molecule individually, using molecular mechanics force fields. This allows for a physically realistic representation of specific solute-solvent interactions, such as hydrogen bonding, and captures the dynamic nature of the solvation shell [61] [60].
- Protocol: Building a System for Explicit Solvent MD Simulation
- Solvate the Solute: Use a program like
tleap(AmberTools) orpackmolto immerse the pre-processed protein or solute into a box of explicit water molecules. Common water models include the 3-site TIP3P and SPC models, or more advanced polarizable models like AMOEBA. - Neutralize and Add Salt: Add a sufficient number of counterions (e.g., Na⁺ or Cl⁻) to neutralize the system's net charge. To mimic physiological conditions, additional salt ions can be added to a specific concentration (e.g., 150 mM NaCl).
- Apply Periodic Boundary Conditions (PBC): Replicate the simulation box in all three dimensions to create an infinite periodic system, effectively eliminating vacuum boundaries and mimicking a bulk solution.
- Handle Long-Range Electrostatics: Use a method like the Particle Mesh Ewald (PME) summation to accurately and efficiently calculate long-range electrostatic interactions under PBC.
- Solvate the Solute: Use a program like
Advanced Hybrid and Polarizable Methods
- QM/MM (Quantum Mechanics/Molecular Mechanics): This hybrid approach is particularly valuable for studying chemical reactions in solution or enzymatic catalysis. The system is partitioned into two regions [57] [61]:
- QM Region: The chemically active core (e.g., the ligand and key active site residues) is treated with quantum mechanics, allowing for bond breaking/forming and accurate electronic structure description.
- MM Region: The surrounding protein and solvent are treated with a molecular mechanics force field, providing computational efficiency. A key consideration is the embedding scheme. In electrostatic embedding, the point charges of the MM region polarize the electron density of the QM region, which is crucial for modeling mutual polarization [61].
- Polarizable Force Fields: Next-generation force fields like AMOEBA (Atomic Multipole Optimized Energetics for Biomolecular Applications) go beyond traditional fixed-charge models. They incorporate atomic multipoles and inducible dipoles, allowing the charge distribution of both the solute and solvent to respond to their changing environment [57] [60]. This is critical for accurately modeling phenomena like the solvatochromic shifts in UV-Vis spectra or the binding affinity of charged ligands [57].
Taxonomy of Computational Solvation Models
Integrated Workflow and The Scientist's Toolkit
Combining the methodologies for flexibility and solvation into a cohesive strategy is essential for robust RDD. A proposed integrated workflow is as follows:
- Target Assessment: Begin by analyzing the target protein for known flexibility (e.g., from literature or multiple PDB structures) and the expected role of water (e.g., conserved crystallographic waters).
- Ensemble Generation: Use MD simulations with an explicit solvent model (like TIP3P or AMOEBA) and enhanced sampling if needed, to generate a diverse conformational ensemble of the target.
- Binding Site Analysis: For key snapshots from the ensemble, perform druggability assessment using tools like SiteMap or FPocket, which can account for solvation properties like the thermodynamics of bound water (e.g., using WaterMap).
- Ensemble Docking: Screen a virtual library against the conformational ensemble using a docking program capable of incorporating some side-chain flexibility.
- Refinement and Scoring: Take the top-ranked poses from docking and subject them to more rigorous analysis. This can involve:
- Short MD simulations of the ligand-bound complex in explicit solvent.
- Re-scoring using MM/PBSA or MM/GBSA to estimate binding free energies.
- For critical candidates, use alchemical free energy perturbation (FEP) calculations for highly accurate affinity predictions.
Table 3: The Scientist's Toolkit for Modeling Flexibility and Solvation
| Tool Name | Category | Primary Function in RDD |
|---|---|---|
| AMBER | MD & Force Fields | Suite for MD simulations; includes force fields for proteins/nucleic acids and tools for MM/PBSA calculations. |
| AutoDock Vina | Molecular Docking | Program for flexible ligand docking into rigid or semi-flexible protein binding sites. |
| GROMACS | MD | High-performance MD simulation package, widely used for conformational sampling of biomolecules. |
| PCM | Implicit Solvation | An implicit solvent model implemented in many quantum chemistry packages (e.g., Gaussian, GAMESS) for QM calculations in solution. |
| AMOEBA | Polarizable Force Field | A polarizable force field for more accurate MD simulations of molecular interactions, including induction effects. |
| COACH | Binding Site Prediction | Meta-server that integrates multiple methods to predict ligand binding sites from protein structure. |
| SiteMap | Druggability Assessment | Tool for identifying and evaluating binding sites, including analysis of enclosure, hydrophobicity, and solvent thermodynamics. |
The integration of sophisticated methods for handling target flexibility and solvation effects marks a significant evolution in Rational Drug Design. Moving beyond the static, vacuum-like approximations of the past is no longer an option but a necessity for improving the predictive power of computational models. Techniques like the Relaxed Complex Scheme, long-timescale Molecular Dynamics, and advanced solvation models such as explicit solvent simulations and polarizable QM/MM approaches, provide a more physiologically realistic framework for understanding molecular recognition. As these methodologies continue to mature, augmented by machine learning and increased computational power, they promise to streamline the drug discovery pipeline, reduce late-stage attrition, and ultimately democratize the development of safer and more effective small-molecule therapeutics [59] [58]. The future of RDD lies in embracing the dynamic and solvated nature of biological systems.
Within the structured pipeline of modern drug discovery, lead optimization represents a critical stage dedicated to the systematic refinement of a biologically active "hit" compound into a promising preclinical drug candidate. This process is a cornerstone of rational drug design (RDD), a methodology that relies on a deep understanding of biological targets and their molecular interactions to guide development, contrasting with traditional trial-and-error approaches [62]. The primary objective of lead optimization is to transform a molecule that has demonstrated basic activity against a therapeutic target into one that possesses the enhanced potency, selectivity, and drug-like properties necessary for success in subsequent in vivo studies and, ultimately, in the clinic [63].
The transition from hit to lead involves meticulous chemical modification. A lead molecule, while active, is almost always flawed—it may suffer from instability in biological systems, inadequate binding affinity, or interaction with off-target proteins [63]. The goal of lead optimization is not to achieve molecular perfection but to balance multiple properties through iterative design, synthesis, and testing until a candidate emerges that is suitable for preclinical development [63]. This phase acts as both a filter and a builder, filtering out unstable or unsafe options to save resources downstream while building up a smaller set of robust drug candidates [63]. In the broader context of RDD, lead optimization is where computational predictions and structural insights are rigorously tested and translated into molecules with refined pharmacological profiles.
Core Strategies in Lead Optimization
The lead optimization process employs a suite of interdependent strategies aimed at improving the multifaceted profile of a compound. These strategies are executed through iterative cycles of design, synthesis, and biological testing.
Structure-Activity Relationship (SAR) Exploration
The foundation of lead optimization is the systematic exploration of the Structure-Activity Relationship (SAR). This involves making deliberate, minor chemical modifications—such as changing a functional group, modifying polarity, or optimizing size—to a lead compound's structure and analyzing how these changes affect its biological activity and physicochemical properties [63]. The insights gained from SAR studies guide medicinal chemists in understanding which parts of the molecule are essential for binding (the pharmacophore) and which can be altered to improve other characteristics. This empirical mapping is crucial for prioritizing which analogs to synthesize next and for informing scaffold-hopping techniques to generate novel chemical series with improved properties [64].
Optimization of Selectivity and ADMET Properties
Simultaneous with improving potency, a major focus is on enhancing a compound's selectivity and its Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) profile.
- Enhancing Selectivity: Selectivity ensures that a compound interacts specifically with its intended target and not with unrelated proteins, particularly those that are structurally similar. A lack of selectivity is a common source of off-target effects and toxicity. Profiling and counter-screening assays are used to test compounds against panels of related enzymes or receptors to confirm target specificity and rule out undesirable off-target activity [65].
- ADMET Optimization: Lead optimization aims to fix key ADMET shortcomings early in the process [63]. This includes:
- Absorption & Permeability: Optimizing properties for desired routes of administration, often focusing on oral bioavailability.
- Metabolic Stability: Assessing and improving a compound's resistance to degradation by metabolic enzymes (e.g., cytochrome P450s) to achieve a suitable half-life [64].
- Toxicity & Safety: Running early safety screens to minimize off-target effects and inherent toxicity [63].
A central challenge is that optimizing one property can negatively impact another. For instance, increasing molecular weight to improve potency might reduce solubility, or enhancing permeability by increasing lipophilicity could worsen metabolic stability [63]. This makes lead optimization a complex balancing act.
Technology and Tools Driving Modern Lead Optimization
The lead optimization process has been transformed by a powerful arsenal of technologies that enable more predictive and efficient candidate refinement.
Table 1: Key Technologies and Tools in Lead Optimization
| Technology Category | Specific Tools/Methods | Application in Lead Optimization |
|---|---|---|
| Computational Modeling | Molecular Docking, Molecular Dynamics Simulations, QSAR, Pharmacophore Modeling | Predicts binding modes, analyzes stability of ligand-target complexes, and forecasts activity/ADMET properties of analogs before synthesis [63] [2]. |
| Artificial Intelligence & Machine Learning | Deep Graph Networks, Support Vector Machines (SVMs), Random Forests (RFs) | Generates virtual analogs, predicts synthetic accessibility, prioritizes compounds based on multi-parameter optimization, and forecasts ADMET properties [13] [66]. |
| Biophysical & Structural Biology | X-ray Crystallography, Cryo-EM, NMR, Cellular Thermal Shift Assay (CETSA) | Determines 3D structure of target-ligand complexes to guide design; CETSA validates direct target engagement in physiologically relevant cellular environments [13] [63] [62]. |
| High-Throughput Experimentation | Automated Synthesis, Robotics, Microfluidic Systems | Accelerates the design-make-test-analyze (DMTA) cycle by enabling rapid synthesis and profiling of hundreds of analogs for activity and developability [63]. |
The integration of these tools creates a data-rich workflow. For example, AI can suggest novel synthetic routes or predict properties, computational models can prioritize the most promising candidates for synthesis, and automated platforms can then synthesize and test these compounds, generating high-quality data to feed back into the models for the next optimization cycle [63]. This synergistic use of technology is key to compressing traditional lead optimization timelines from years to months [13].
Experimental Protocols for Key Assays
Robust experimental protocols are vital for generating reliable data to guide optimization decisions. The following assays are central to evaluating compound performance during lead optimization.
Biochemical Potency and Mechanism of Action Assays
Objective: To measure the direct interaction of a compound with its purified target protein, determining its potency (e.g., IC50, Ki) and elucidating its mechanism of action (e.g., competitive, allosteric) [65].
Protocol:
- Assay Format: Employ homogeneous, "mix-and-read" biochemical assays (e.g., fluorescence polarization, TR-FRET, or radiometric assays) for high-throughput profiling. These formats minimize wash steps and complexity [65].
- Enzyme Kinetics: Incubate the target enzyme with a range of substrate concentrations in the presence of serially diluted test compounds. Include controls with a known inhibitor and a no-inhibitor baseline.
- Signal Detection: Use a plate reader to measure the fluorescence, luminescence, or absorbance signal corresponding to the enzymatic reaction product.
- Data Analysis: Plot reaction velocity against compound concentration to generate dose-response curves. Fit the data using non-linear regression to calculate IC50 values. To determine the mechanism of action, analyze the data using Lineweaver-Burk or other kinetic plots [65].
Cellular Target Engagement (CETSA)
Objective: To confirm that a compound engages with its intended target in a physiologically relevant cellular environment, bridging the gap between biochemical potency and cellular efficacy [13].
Protocol:
- Cell Treatment: Treat intact cells (or tissue samples) with the compound of interest or a vehicle control for a predetermined time.
- Heat Challenge: Subject the cell aliquots to a range of elevated temperatures (e.g., 50-65°C) to denature proteins. The binding of a ligand often stabilizes the target protein, increasing its thermal stability.
- Cell Lysis and Fractionation: Lyse the heat-challenged cells and separate the soluble (non-denatured) protein from the insoluble (denatured) aggregates by centrifugation.
- Protein Quantification: Quantify the amount of intact, soluble target protein in each sample using a specific detection method, such as Western blot or high-resolution mass spectrometry [13].
- Data Analysis: Plot the fraction of intact protein remaining soluble against the temperature for each treatment condition. A rightward shift in the melting curve (increased melting temperature, Tm) for the compound-treated sample indicates direct target engagement and stabilization [13].
In Vitro ADME Profiling
Objective: To evaluate key pharmacokinetic properties of lead compounds early in the optimization process [63] [64].
Protocol:
- Metabolic Stability (e.g., Microsomal Half-Life):
- Incubation: Incubate the test compound with liver microsomes (human or relevant species) in the presence of NADPH cofactor.
- Time Course Sampling: Remove aliquots of the reaction mixture at multiple time points (e.g., 0, 5, 15, 30, 60 minutes).
- Analysis: Stop the reaction and quantify the remaining parent compound using Liquid Chromatography-Mass Spectrometry (LC-MS/MS).
- Calculation: Plot the natural log of the parent compound concentration remaining versus time. The slope of the line is used to calculate the in vitro half-life.
- Permeability (e.g., Caco-2 Assay):
- Cell Culture: Grow a confluent monolayer of Caco-2 cells on a semi-permeable membrane in a transwell apparatus.
- Dosing: Add the test compound to the donor compartment (either apical or basolateral side).
- Sampling: Measure the appearance of the compound in the receiver compartment over time.
- Calculation: Determine the apparent permeability coefficient (Papp) and assess efflux ratios by comparing apical-to-basolateral and basolateral-to-apical transport.
Visualizing the Workflow and Cycle
The lead optimization process can be conceptualized as a structured workflow that feeds into an iterative cycle, as illustrated in the following diagrams.
Diagram 1: Lead Optimization High-Level Workflow. This chart outlines the key stages from hit confirmation to candidate selection or attrition, highlighting the critical role of SAR and ADMET profiling.
Diagram 2: The Design-Make-Test-Analyze (DMTA) Cycle. This iterative cycle is the engine of lead optimization, where data from each round informs the next design phase to progressively improve the compound series [63].
The Scientist's Toolkit: Essential Reagents and Materials
A successful lead optimization campaign relies on a suite of specialized reagents and platforms to generate high-quality, translatable data.
Table 2: Key Research Reagent Solutions for Lead Optimization
| Tool / Reagent | Function in Lead Optimization |
|---|---|
| Transcreener Assays | Homogeneous, high-throughput biochemical assays for measuring enzyme activity (e.g., kinases, GTPases). Ideal for primary screens and follow-up potency testing due to their simplicity and reliability [65]. |
| CETSA Kits | Kits configured for Cellular Thermal Shift Assays to provide quantitative, system-level validation of direct drug-target engagement in intact cells, bridging biochemical and cellular efficacy [13]. |
| Liver Microsomes | Subcellular fractions containing metabolic enzymes (CYPs, UGTs) used in high-throughput in vitro assays to predict metabolic stability and identify potential metabolites [63]. |
| Caco-2 Cell Line | A human colon adenocarcinoma cell line that, when differentiated, forms a polarized monolayer with enterocyte-like properties. It is the industry standard model for predicting intestinal absorption and permeability of oral drugs [63]. |
| DNA-Encoded Libraries (DEL) | Vast collections of small molecules, each tagged with a unique DNA barcode, enabling the screening of billions of compounds against a purified target to rapidly identify novel starting points for hit expansion [67]. |
| AI/ML Platforms (e.g., Chemistry42, StarDrop) | Software suites that leverage artificial intelligence and machine learning to de novo design molecules, predict ADMET properties, prioritize compounds, and guide multi-parameter optimization decisions [63] [66]. |
Challenges and Future Perspectives
Despite technological advances, lead optimization remains a complex, time-consuming, and resource-intensive phase in drug discovery [63]. Key challenges persist:
- Multivariate Optimization: The primary challenge is balancing numerous factors—potency, selectivity, solubility, metabolic stability, and safety—simultaneously, as improving one property often adversely affects another [63].
- Translational Gap: A significant number of compounds that are active in biochemical or simple cellular assays fail later due to poor bioavailability, unexpected toxicity, or off-target effects in more complex in vivo systems. Improving the predictive power of early assays is crucial [63].
- Data Integration and Quality: Reliable ADMET profiles and solid in vivo models are not always available, and missing or non-representative data can lead optimization efforts astray [63].
The future of lead optimization is being shaped by the deeper integration of AI and automation. AI tools are increasingly capable of highlighting the most promising synthetic directions and predicting in vivo outcomes with greater accuracy [63] [66]. When combined with automated synthesis and parallel testing, these technologies enable faster and more informed DMTA cycles. Furthermore, the growing use of multi-omics data and patient-derived models helps design compounds that are more clinically relevant from the outset, potentially reducing late-stage attrition [63]. As these tools and methodologies mature, the lead optimization process will continue to evolve from a partially empirical endeavor to a more predictive and efficient science, solidifying its role as the crucial bridge between a molecule's initial promise and its potential to become a life-saving therapeutic.
In the paradigm of Rational Drug Design (RDD), the primary objective is to invent new medications based on knowledge of a biological target, deliberately moving away from traditional trial-and-error approaches [4] [9]. A critical factor in the success of RDD is the simultaneous consideration of a compound's Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADME/Tox) profile early in the discovery process [68] [69]. Despite high affinity for their intended targets, many drug candidates fail in late-stage development due to poor pharmacokinetic or unacceptable safety profiles [9] [69]. Consequently, integrating ADME/Tox predictions has become a cornerstone of modern RDD, aiming to optimize these properties in tandem with therapeutic efficacy to reduce attrition rates and accelerate the development of safer, more effective drugs [4] [68].
This guide details the core principles, predictive methodologies, and experimental protocols essential for managing ADME/Tox properties within an RDD framework.
Core ADME/Tox Properties and Their Predictive Parameters
The following table summarizes the key properties and parameters that researchers must predict and optimize for a successful drug candidate.
Table 1: Key ADME/Tox Properties and Their Predictive Parameters in Rational Drug Design
| Property | Key Parameters to Predict | Influence on Drug Profile | Common Predictive Rules (e.g., Lipinski's Rule of 5) |
|---|---|---|---|
| Absorption | Bioavailability, Permeability (e.g., Caco-2, PAMPA), Aqueous Solubility, Efflux Transport [70] [71] [72] | Dictates the fraction of an administered dose that reaches systemic circulation [71]. | Violation of >1 rule may indicate poor absorption [69]. |
| Distribution | Volume of Distribution (Vd), Plasma Protein Binding (PPB), Blood-Brain Barrier (BBB) Penetration [70] [71] [72] | Determines the extent of drug spread throughout the body and access to the target site [70] [71]. | Rules often include thresholds for molecular size and lipophilicity [69]. |
| Metabolism | Metabolic Stability (e.g., half-life), CYP450 Enzyme Inhibition/Induction, Metabolite Identification [71] [73] [72] | Impacts the drug's duration of action and potential for drug-drug interactions [71]. | Structural alerts for metabolically labile sites or CYP inhibition [69]. |
| Excretion | Renal Clearance, Biliary Excretion [70] [71] [72] | Governs the rate at of drug removal from the body, affecting dosing frequency [71]. | Rules may flag compounds with high molecular weight for potential biliary excretion [69]. |
| Toxicity | Genotoxicity (e.g., Ames test), Hepatotoxicity, Cardiotoxicity, Cytotoxicity [74] [72] [69] | Identifies potential adverse effects and safety risks [72]. | Structural alerts for reactive functional groups known to cause toxicity [74] [69]. |
The journey of a drug through the body via these phases can be visualized as a sequential process.
Diagram 1: The ADME/Tox Journey of a Drug in the Body
Predictive Computational and In Silico Methodologies
Structure-Based and Ligand-Based Design
Rational drug design leverages two primary computational approaches. Structure-Based Drug Design (SBDD) relies on the three-dimensional structure of a biological target (e.g., from X-ray crystallography or NMR) to design molecules that are complementary in shape and charge to the binding site [4] [9]. Techniques include virtual screening of compound libraries and de novo ligand design. Key challenges include accounting for target flexibility and the role of water molecules [4]. Conversely, Ligand-Based Drug Design (LBDD) is employed when the 3D target structure is unknown but information about known active molecules is available. It uses techniques like Pharmacophore Modeling and Quantitative Structure-Activity Relationship (QSAR) to predict new active compounds [4] [9].
AI/ML and Integrated Risk Platforms
Modern Artificial Intelligence and Machine Learning (AI/ML) platforms can predict over 175 ADMET properties by training on large, high-quality datasets [69]. These platforms can predict properties such as solubility, metabolic stability, and various toxicity endpoints (e.g., Ames mutagenicity) in seconds [69]. These predictions can be synthesized into a unified ADMET Risk Score, which applies "soft" thresholds to a range of properties to provide a single metric for a compound's developability, helping prioritize lead compounds with a higher likelihood of success [69].
Essential Experimental Protocols and Assays
The following section details key experimental methodologies used to generate data for validating computational predictions and advancing drug candidates.
Absorption Assays
Objective: To evaluate a compound's ability to cross biological membranes and enter systemic circulation [73] [72].
- Parallel Artificial Membrane Permeability Assay (PAMPA):
- Principle: A non-cell-based, high-throughput assay that uses an artificial membrane infused in a lipid solution to mimic passive diffusion across the gastrointestinal tract [73].
- Protocol:
- Membrane Preparation: A filter in a 96-well plate is coated with a mixture of phospholipids to create an artificial membrane [73].
- Compound Incubation: A solution of the test compound is added to the donor compartment. The acceptor compartment contains a blank buffer, often at a different pH to create a physiological gradient [73].
- Incubation & Analysis: The plate is incubated (e.g., for 30 minutes) with stirring. Samples from both compartments are analyzed using a UV plate reader or LC-MS/MS [73].
- Data Calculation: Permeability (Pe) is calculated based on the compound's appearance rate in the acceptor compartment [73].
- Caco-2 Permeability Assay:
- Principle: A cell-based assay using a human colon adenocarcinoma cell line (Caco-2) that, upon differentiation, forms a monolayer resembling the intestinal epithelium. It models both passive transcellular/paracellular diffusion and active transporter effects [73] [72].
- Protocol:
- Cell Culture: Caco-2 cells are seeded and cultured on a semi-permeable filter in a transwell system until they form a confluent, differentiated monolayer (typically 21 days) [73].
- Transepithelial Transport: The test compound is added to either the apical (A) or basolateral (B) donor compartment. The receiver compartment is sampled over time [73].
- Analysis: Compound concentration in samples is quantified via LC-MS/MS. Apparent permeability (Papp) is calculated. Efflux ratio (Papp B-to-A / Papp A-to-B) indicates potential for active efflux (e.g., by P-glycoprotein) [73].
Metabolism Assays
Objective: To determine the metabolic stability of a compound and its potential for enzyme-mediated drug-drug interactions [73] [72].
- Metabolic Stability (Microsomal/Hepatocyte Incubation):
- Principle: Measures the rate of compound depletion upon incubation with liver microsomes (containing CYP450 enzymes) or hepatocytes (containing full suite of metabolic enzymes) [73] [72].
- Protocol:
- Incubation: Test compound is incubated with liver microsomes (or suspended hepatocytes) in the presence of NADPH cofactor at 37°C [73].
- Sampling: Aliquots are taken at multiple time points (e.g., 0, 5, 15, 30, 45 minutes) and the reaction is stopped by adding acetonitrile [73].
- Analysis: Samples are centrifuged, and the supernatant is analyzed by LC-MS/MS to determine the remaining parent compound concentration [73].
- Data Calculation: In vitro half-life (t1/2) and intrinsic clearance (CLint) are calculated from the depletion curve [73].
- Cytochrome P450 (CYP) Inhibition Assay:
- Principle: Assesses the ability of a test compound to inhibit a specific CYP enzyme (e.g., CYP3A4, CYP2D6), which is critical for predicting drug-drug interactions [73] [72].
- Protocol:
- Enzyme Reaction: A recombinant CYP enzyme or human liver microsomes are incubated with a probe substrate (known to be metabolized by the specific CYP) and the test compound at various concentrations [73].
- Metabolite Detection: The reaction is monitored by measuring the formation rate of the specific metabolite of the probe substrate, often using fluorescent or luminescent detection methods [73].
- Data Calculation: The IC50 value (concentration of test compound that inhibits 50% of enzyme activity) is determined from the dose-response curve [73].
Toxicity Assays
Objective: To identify potential adverse effects of a compound, including genetic damage, organ-specific toxicity, and general cell death [72].
- Ames Test (for Genotoxicity):
- Principle: Uses specific strains of Salmonella typhimurium and E. coli with mutated genes to detect reverse mutations induced by the test compound, indicating potential mutagenicity and carcinogenicity [74] [72].
- Protocol:
- Bacterial Strain Preparation: Selected tester strains are grown in culture [72].
- Incubation with Compound: Bacteria are incubated with the test compound, both with and without a metabolic activation system (rat liver S9 fraction), on a minimal glucose agar plate [72].
- Incubation and Counting: Plates are incubated for 48 hours, and the number of revertant colonies is counted. A significant increase in revertants compared to the vehicle control indicates a positive mutagenic response [74] [72].
- Hepatotoxicity Assays (e.g., using DILI Assay Kits):
- Principle: Assesses the potential of a drug to cause drug-induced liver injury (DILI) using advanced in vitro models like primary human hepatocytes or 3D organ-on-a-chip systems [68] [72].
- Protocol:
- Cell Seeding: Hepatocytes or liver-on-a-chip devices are prepared and stabilized [68].
- Compound Exposure: Cells are exposed to a range of concentrations of the test compound for a defined period (e.g., 24-72 hours) [68] [72].
- Endpoint Analysis: Multiple endpoints are measured, including cell viability (e.g., ATP content), intracellular glutathione depletion, and release of liver enzymes like ALT and AST [68] [72].
The workflow for an integrated ADME/Tox assessment, combining computational and experimental approaches, is outlined below.
Diagram 2: Integrated ADME/Tox Assessment Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Successful ADME/Tox profiling relies on a suite of specialized reagents and tools. The following table details essential materials used in the field.
Table 2: Essential Research Reagent Solutions for ADME/Tox Studies
| Reagent / Tool | Function in ADME/Tox Studies | Specific Application Example |
|---|---|---|
| Caco-2 Cell Line | A human epithelial colorectal adenocarcinoma cell line that differentiates to form a polarized monolayer with tight junctions, microvilli, and expresses relevant drug transporters. Used to predict human intestinal absorption [73] [72]. | Caco-2 permeability assay to determine apparent permeability (Papp) and assess active efflux [73]. |
| PAMPA Explorer Test System | A kit providing artificial membrane-coated plates and reagents for high-throughput, cell-free assessment of passive transcellular permeability [73]. | Early-stage screening of large compound libraries for passive absorption potential [73]. |
| Liver Microsomes (Human/Rat) | Subcellular fractions containing membrane-bound cytochrome P450 (CYP) and other drug-metabolizing enzymes, but lacking soluble enzymes. Used for metabolic stability and metabolite identification studies [73] [72]. | Determination of in vitro half-life (t1/2) and intrinsic clearance (CLint) [73]. |
| Cryopreserved Hepatocytes | Isolated, cryopreserved liver cells containing the full complement of hepatic metabolizing enzymes and transporters. Provide a more physiologically relevant model for metabolism than microsomes [73] [72]. | Studies of phase I/II metabolism, transporter-mediated uptake, and hepatotoxicity [72]. |
| pION µSOL Assay Kits | Kits designed to measure the kinetic solubility of compounds by monitoring absorbance changes, mimicking the pH environment of the gastrointestinal tract [73]. | Determination of compound solubility at various pH levels (pH-Mapping) to predict in vivo dissolution and absorption [73]. |
| Rapid Equilibrium Dialysis (RED) Device | A disposable 96-well plate format device used for semi-automated plasma protein binding studies via equilibrium dialysis [73]. | Determining the fraction of drug unbound (fu) in plasma, which influences distribution and efficacy [73]. |
| Ames Tester Strains | Specific strains of Salmonella typhimurium (e.g., TA98, TA100) and E. coli with defined mutations that make them sensitive to mutagenic agents [74] [72]. | In vitro assessment of a compound's potential to cause genetic mutations (genotoxicity) [72]. |
| PhysioMimix DILI Assay Kit | A commercial kit for use with organ-on-a-chip systems, providing a more predictive in vitro model for assessing drug-induced liver injury [68]. | Mechanistic investigation of human-relevant hepatotoxicity in a dynamic, multi-cellular microenvironment [68]. |
Emerging Technologies and Future Directions
The field of ADME/Tox prediction is rapidly evolving with several groundbreaking technologies.
- Organ-on-a-Chip (OOC) Systems: These microfluidic devices culture human cells in a way that mimics the 3D structure, mechanical forces, and biochemical microenvironment of human organs. For example, liver-on-a-chip models provide highly predictive data for drug-induced liver injury (DILI), a leading cause of drug failure and withdrawal [68].
- AI and Machine Learning: Advanced AI/ML models, such as Graph Neural Networks (GNNs), are being trained on massive chemical and biological datasets to achieve unprecedented accuracy in predicting ADME properties like solubility, metabolic pathways, and toxicity endpoints from molecular structure alone [68] [69].
- High-Throughput Screening (HTS) Automation: Fully integrated, automated robotic systems based on liquid handling platforms now allow for the rapid profiling of thousands of compounds against a battery of ADME/Tox assays (e.g., permeability, metabolic stability, plasma protein binding), dramatically accelerating early-stage decision-making [73] [68].
- Regulatory Harmonization: The recent introduction of the ICH M12 guideline aims to standardize the conduct of drug-drug interaction studies globally. This harmonization ensures data consistency and facilitates a more efficient drug development process across different regulatory regions [68].
Integrating ADME/Tox management into the core of Rational Drug Design is no longer an option but a necessity for developing successful therapeutics. By leveraging a synergistic combination of in silico predictions, high-throughput in vitro assays, and emerging technologies like organs-on-chips and AI, researchers can now identify and mitigate pharmacokinetic and safety liabilities earlier than ever before. This proactive, property-driven approach de-risks the drug development pipeline, saves significant time and resources, and ultimately paves the way for bringing safer and more effective medicines to patients.
Strategies for Mitigating Off-Target Interactions and Reducing Side Effects
Within the paradigm of rational drug design (RDD), the precise targeting of therapeutic agents to their intended biomolecular targets represents a fundamental objective. The RDD process inventively finds new medications based on knowledge of a biological target, designing molecules that are complementary in shape and charge to the biomolecular target with which they interact [9]. However, a significant impediment to therapeutic success remains the phenomenon of off-target interactions—where drugs or therapeutic modalities inadvertently interact with non-intended biological macromolecules, potentially leading to adverse effects and reduced therapeutic efficacy.
The pharmaceutical industry faces a persistent challenge with clinical attrition rates, with approximately 40-50% of clinical failures attributed to lack of clinical efficacy and 30% to unmanageable toxicity [75]. Such statistics underscore the critical importance of comprehensive off-target mitigation strategies throughout the drug discovery and development pipeline. This whitepaper examines current methodologies and emerging technologies for identifying, characterizing, and mitigating off-target interactions across multiple therapeutic modalities, with particular emphasis on their application within rational drug design frameworks.
Fundamental Principles of Off-Target Mitigation in Drug Design
The Rational Drug Design Framework
Rational drug design operates on the principle of leveraging detailed knowledge of biological targets to design interventions with maximal therapeutic effect and minimal adverse outcomes. This approach primarily encompasses two complementary methodologies: structure-based drug design and ligand-based drug design [4]. Structure-based drug design relies on three-dimensional structural information of the target protein, often obtained through X-ray crystallography or NMR spectroscopy, to design molecules with optimal binding characteristics [9]. Ligand-based approaches, conversely, utilize knowledge of molecules known to interact with the target of interest to derive pharmacophore models or quantitative structure-activity relationships (QSAR) when structural data is unavailable [76].
The lock-and-key model and its refinement, the induced-fit theory, provide conceptual frameworks for understanding molecular recognition in drug-target interactions [5]. These models illustrate how both ligand and target can undergo mutual conformational adjustments until an optimal fit is achieved, highlighting the complexity of predicting binding interactions.
Classification of Off-Target Interactions
Off-target interactions generally fall into two primary categories:
- Off-target pharmacology: Interactions with structurally related or unrelated biomolecules that share similar binding motifs or physicochemical affinity for the therapeutic agent.
- On-target toxicity: Adverse effects resulting from drug action at the intended target in non-diseased tissues or from undesirable modulation of the target's physiological function.
The Structure–Tissue Exposure/Selectivity–Activity Relationship (STAR) framework has been proposed to improve drug optimization by classifying drug candidates based on both potency/specificity and tissue exposure/selectivity [75]. This classification system enables more informed candidate selection and clinical dose planning:
Table 1: STAR Classification System for Drug Candidates
| Class | Specificity/Potency | Tissue Exposure/Selectivity | Clinical Dose | Efficacy/Toxicity Profile |
|---|---|---|---|---|
| I | High | High | Low | Superior efficacy/safety |
| II | High | Low | High | High efficacy with toxicity concerns |
| III | Adequate | High | Low | Good efficacy with manageable toxicity |
| IV | Low | Low | Variable | Inadequate efficacy/safety |
Mitigation Strategies for Small Molecule Therapeutics
Structure-Based Design Approaches
Structure-based drug design offers powerful tools for minimizing off-target interactions through precise molecular engineering. When the three-dimensional structure of the target protein is available, researchers can exploit detailed recognition features of the binding site to design ligands with optimized selectivity [5]. Key approaches include:
Receptor-based design utilizes the structural information to create direct interactions between the designed molecule and specific functional groups of the target protein [5]. This approach allows medicinal chemists to introduce appropriate functionalities in the ligand to strengthen binding to the intended target while reducing affinity for off-targets.
Homology modeling extends these capabilities when experimental structures are unavailable, enabling the construction of protein models based on related structures [9]. This approach is particularly valuable for assessing potential cross-reactivity with structurally related proteins.
Table 2: Experimental Protocols for Structure-Based Off-Target Mitigation
| Method | Protocol Description | Key Applications | Limitations |
|---|---|---|---|
| Virtual Screening | Computational docking of compound libraries against target structure | Identification of selective hits; prediction of off-target binding | Limited by scoring function accuracy; conformational flexibility |
| Binding Site Analysis | Comparative analysis of binding sites across related targets | Identification of selectivity determinants | May miss allosteric binding sites |
| Molecular Dynamics | Simulation of drug-target interactions over time | Assessment of binding stability; identification of key interactions | Computationally intensive; time-scale limitations |
Ligand-Based Design Approaches
When structural information for the target is limited, ligand-based design approaches provide valuable alternatives for optimizing selectivity. These methods leverage known active compounds to infer structural requirements for target binding while minimizing off-target interactions:
Pharmacophore modeling identifies the essential steric and electronic features necessary for molecular recognition at the target binding site [9]. By comparing pharmacophores across targets, researchers can design compounds that selectively match the intended target while discriminating against off-targets.
Quantitative Structure-Activity Relationship (QSAR) analysis correlates calculated molecular properties with biological activity to derive predictive models [76]. These models can be used to optimize both potency against the primary target and selectivity against antitargets.
Similarity-based methods utilize chemical fingerprints and similarity metrics (e.g., Tanimoto index) to identify compounds with desired selectivity profiles [76]. The underlying principle assumes that structurally similar compounds may share biological activities, allowing researchers to avoid structural motifs associated with off-target activity.
Structural Optimization and Property-Based Design
Strategic molecular modification represents a cornerstone of off-target mitigation in small molecule therapeutics. Several key approaches include:
Bioisosteric replacement involves substituting functional groups or atomic arrangements with others that have similar physicochemical properties but potentially improved selectivity profiles [4]. This approach can eliminate problematic structural features associated with off-target binding while maintaining target affinity.
Property-based design focuses on optimizing physicochemical properties to influence tissue distribution and exposure. The Rule of Five and related guidelines help maintain drug-like properties that balance permeability, solubility, and metabolic stability [75]. By controlling properties such as lipophilicity, molecular weight, and polar surface area, researchers can influence a compound's propensity to accumulate in tissues where off-target interactions may occur.
Stereochemical optimization leverages the differential binding of enantiomers to target proteins [4]. As enantiomers may interact differently with off-target proteins, careful selection of stereochemistry can enhance selectivity.
Advanced Therapeutic Modalities: CRISPR-Based Therapeutics
CRISPR-Cas9 Off-Target Mechanisms
The CRISPR-Cas9 system has emerged as a powerful genome editing technology with immense therapeutic potential. However, its application is challenged by off-target editing events where the Cas9 nuclease cleaves DNA at unintended genomic locations [77]. The mechanisms underlying these off-target effects include:
Mismatch tolerance in the guide RNA-DNA hybridization allows for stable binding even with imperfect complementarity [77]. The energetic compensation of the RNA-DNA hybrid can accommodate several base pair mismatches, particularly in the PAM-distal region.
Cellular environment factors such as elevated enzyme concentration, prolonged exposure, and chromatin accessibility can influence off-target rates [78]. The duration of Cas9 activity within cells directly correlates with the probability of off-target cleavage.
Mitigation Strategies for CRISPR Therapeutics
Several innovative approaches have been developed to enhance the precision of CRISPR-based gene editing:
Delivery Method Optimization: Modulating the persistence of CRISPR components in cells represents a fundamental strategy. Transitioning from plasmid DNA delivery (which can linger for days) to RNA delivery (degraded within 48 hours) or direct protein delivery (degraded within 24 hours) significantly reduces the window for off-target activity [78].
CRISPR Nickases: Engineering Cas9 to create single-strand breaks (nicks) rather than double-strand breaks requires two adjacent nicking events to generate a double-strand break [78]. This approach dramatically reduces off-target effects, as it requires simultaneous recognition by two guide RNAs at the same genomic locus.
High-Fidelity Cas9 Variants: Protein engineering approaches have generated enhanced specificity Cas9 variants through both rational and evolutionary methods:
Table 3: High-Fidelity Cas9 Variants and Their Development Methods
| Variant | Development Method | Key Mechanism | Specificity Improvement |
|---|---|---|---|
| eSpCas9 | Rational Mutagenesis | Weakened non-specific DNA binding | Significant reduction in off-target cleavage |
| Cas9-HF1 | Rational Mutagenesis | Modified DNA-binding domains | High on-target with minimal off-target |
| HiFi-Cas9 | Random Mutagenesis | Evolved specificity through screening | Maintains high on-target with reduced off-target |
| evoCas9 | Random Mutagenesis | Laboratory evolution for precision | Enhanced discrimination against mismatches |
Rational mutagenesis approaches involve targeted modifications to key amino acids in the DNA-binding domain to weaken non-specific interactions [78]. Random mutagenesis with screening utilizes high-throughput selection to identify variants with naturally enhanced specificity [78].
Emerging Modalities and Specialized Challenges
Targeted Protein Degradation
Targeted protein degradation (TPD) represents an emerging therapeutic paradigm with unique off-target considerations. Unlike traditional small molecules that modulate protein function, degraders facilitate the complete removal of target proteins from cells. The off-target risks in TPD include both functional off-target pharmacology and off-target protein degradation [79].
A case study examining hERG liability in a TPD compound demonstrated a comprehensive de-risking strategy [79]. Despite observed in vitro hERG inhibition, subsequent in vivo studies in dogs showed no ECG effects at the highest feasible dose levels. The investigative approach included:
- Cellular and tissue proteomics to identify off-target degradation
- Immunoblotting assays to confirm protein level changes
- Plasma and tissue exposure measurements to establish safety margins
- Integrated risk assessment comparing therapeutic and toxic exposure levels
This multi-faceted approach highlights the importance of moving beyond standard safety assays for novel modalities and developing tailored assessment strategies.
G Protein-Coupled Receptor (GPCR) Targeting
GPCRs represent important drug targets, accounting for approximately one-third of approved therapeutics [80]. Traditional GPCR drugs bind to the extracellular domain, often activating multiple signaling pathways (G proteins and β-arrestin) which can lead to side effects.
Recent research has revealed a novel approach to activating GPCRs through intracellular targeting [80]. A study on the parathyroid hormone type 1 receptor (PTH1R) demonstrated that a non-peptide message molecule (PCO371) binding to the intracellular region could activate G proteins without recruiting β-arrestin [80]. This approach achieved pathway-specific signaling, potentially reducing side effects while maintaining therapeutic efficacy.
Experimental Protocols for Off-Target Assessment
Comprehensive Profiling Assays
Rigorous experimental assessment of off-target interactions requires a multi-tiered approach:
Primary Pharmacological Profiling: Broad screening against panels of related targets (e.g., kinase panels, GPCR panels) provides initial assessment of selectivity [75]. This typically involves testing at a single concentration (often 10μM) against dozens to hundreds of targets.
Secondary Binding Assays: Quantitative determination of binding affinity (Ki or IC50) for potential off-targets identified in primary screening establishes selectivity ratios [75]. A minimum 10-fold selectivity window is generally preferred for progression candidates.
Functional Assays in Relevant Systems: Assessment of compound effects in cellular or tissue systems expressing potential off-targets provides physiological context [79]. These assays help identify functional consequences of off-target binding.
Specialized Methodologies for Advanced Modalities
CRISPR Off-Target Assessment:
- Guide-seq: Genome-wide method for identifying off-target sites by capturing double-strand break locations
- CIRCLE-seq: In vitro method using circularized genomic DNA to profile nuclease activity
- BLESS: Direct in situ capture of double-strand breaks with sequencing
Targeted Protein Degradation Profiling:
- Cellular proteomics: LC-MS/MS-based quantification of protein abundance changes across the proteome
- Thermal protein profiling: Monitoring protein thermal stability shifts to identify engaged targets
- Functional genomics: CRISPR-based screening to identify genetic dependencies and synthetic lethal interactions
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Key Research Reagent Solutions for Off-Target Assessment
| Reagent/Platform | Function | Application Context |
|---|---|---|
| High-Fidelity Cas9 | Engineered nuclease with enhanced specificity | CRISPR-based gene editing with reduced off-target effects |
| Selectivity Screening Panels | Pre-configured target panels for selectivity assessment | Small molecule off-target profiling (kinases, GPCRs, etc.) |
| Proteomics Platforms | LC-MS/MS systems for protein quantification | Identification of off-target degradation in TPD |
| Cryo-EM Infrastructure | High-resolution structure determination | Visualization of drug-target interactions for rational design |
| Chemical Similarity Tools | Algorithms for compound similarity searching | Ligand-based design and off-target prediction |
| hERG Assay Systems | In vitro prediction of cardiotoxicity potential | Early de-risking of cardiac liability |
| Polypharmacology Tools | Computational prediction of multi-target interactions | Systematic assessment of target promiscuity |
The mitigation of off-target interactions represents a multifaceted challenge that requires integrated approaches across the drug discovery pipeline. Successful strategies combine structural insights from target biology, computational predictions of interaction potential, empirical testing in relevant systems, and strategic optimization of therapeutic agents. The evolving landscape of therapeutic modalities—from small molecules to biologics to gene editing systems—demands continued innovation in off-target assessment and mitigation methodologies.
As rational drug design continues to advance, the integration of comprehensive off-target mitigation strategies will be essential for delivering safer, more effective therapeutics. The frameworks and methodologies outlined in this whitepaper provide a foundation for researchers to address these critical challenges in systematic and innovative ways, ultimately contributing to improved success rates in drug development and better outcomes for patients.
The Role of Multi-objective Optimization and Advanced Machine Learning Algorithms
The process of drug discovery is inherently multifaceted, requiring the simultaneous optimization of numerous molecular properties for a candidate to succeed. Rational Drug Design (RDD) has been transformed by the integration of multi-objective optimization (MultiOOP) and many-objective optimization (ManyOOP) frameworks, which systematically balance conflicting design goals. This technical guide explores how advanced machine learning (ML) algorithms, particularly deep generative models and evolutionary metaheuristics, enable the navigation of vast chemical spaces to design novel therapeutics. By framing drug design as a ManyOOP—involving objectives such as binding affinity, toxicity, and drug-likeness—researchers can identify optimal molecular candidates with precision and efficiency previously unattainable with traditional methods. This document provides a comprehensive overview of the core methodologies, experimental protocols, and computational tools driving this paradigm shift in pharmaceutical research.
Rational Drug Design (RDD) is a computational approach that aims to create novel drug candidates with predefined pharmacological properties from first principles. The core challenge lies in the necessity to satisfy multiple, often conflicting, objectives simultaneously. A drug candidate must demonstrate high binding affinity for its target, possess favorable pharmacokinetic properties ( Absorption, Distribution, Metabolism, Excretion, and Toxicity - ADMET), exhibit low toxicity, and maintain synthetic feasibility [81] [82]. Traditionally, these properties were optimized sequentially or through weighted-sum approaches, which often failed to capture the complex trade-offs between objectives.
Multi-objective optimization (MultiOOP) and many-objective optimization (ManyOOP, involving more than three objectives) provide a mathematical framework for this challenge [82]. In these paradigms, instead of a single optimal solution, algorithms identify a set of Pareto-optimal solutions. Each solution on the Pareto front represents a different trade-off, where improvement in one objective necessitates deterioration in another [82]. This is naturally aligned with the compromises required in drug design. The integration of advanced ML with MultiOOP has given rise to a powerful new class of RDD tools that can efficiently explore the immense chemical space (estimated at >10⁶⁰ molecules) and generate novel, optimized candidates [83] [81].
Foundational Concepts and Methodologies
Defining the Multi-objective Optimization Problem in Drug Design
In the context of RDD, a multi-objective optimization problem can be formally defined as shown in Equation 1 [82]: Minimize/Maximize ( F(m) = [f1(m), f2(m), ..., fk(m)]^T ) Subject to: ( gj(m) \leq 0, j=1,2,...,J; h_p(m) = 0, p=1,2,...,P )
Here, ( m ) represents a molecule within the molecular search space. The vector ( F(m) ) contains ( k ) objective functions (( fi )) representing the molecular properties to be optimized, such as binding energy or QED score. The functions ( gj ) and ( h_p ) represent inequality and equality constraints, respectively, which can include structural alerts, synthetic accessibility rules, or predefined scaffold requirements [84] [82].
Key Machine Learning Architectures for Molecular Optimization
Several deep learning architectures form the backbone of modern multi-objective molecular optimization frameworks:
- Variational Autoencoders (VAEs): These models map molecules into a continuous latent vector space, allowing for smooth interpolation and optimization. The ScafVAE framework, for instance, uses a scaffold-aware VAE to generate molecules by first assembling bond scaffolds and then decorating them with specific atom types, balancing novelty with chemical validity [83].
- Generative Adversarial Networks (GANs): GANs can generate novel molecular structures by learning the underlying data distribution of known drug-like molecules [81].
- Transformer-based Models: Adapted from natural language processing, Transformers treat molecular representations (like SELFIES or SMILES) as sequences. Models like ReLSO and FragNet use contrastive learning and regularization to create well-organized latent spaces suitable for optimization [85].
- Evolutionary Algorithms (EAs): EAs are population-based metaheuristics that evolve candidate molecules over multiple generations through selection, crossover, and mutation operations, guided by multi-objective fitness functions [82] [85]. Frameworks like CMOMO integrate EAs with deep learning for constrained multi-objective optimization [84].
Table 1: Key Machine Learning Architectures in Multi-objective Molecular Optimization
| Architecture | Core Principle | Key Advantages in Drug Design | Example Frameworks |
|---|---|---|---|
| Variational Autoencoder (VAE) | Encodes molecules to a continuous latent space; decodes latent vectors back to molecules. | Enables smooth property optimization and interpolation in latent space. | ScafVAE [83], CVAE [81] |
| Generative Adversarial Network (GAN) | Two neural networks (generator & discriminator) compete to generate realistic data. | Capable of generating highly novel molecular structures. | GAN [81] |
| Transformer | Uses self-attention mechanisms to process sequential molecular representations. | Superior sequence modeling; handles long-range dependencies in molecular graphs. | ReLSO, FragNet [85] |
| Evolutionary Algorithm (EA) | Population-based search inspired by natural selection. | Naturally suited for finding diverse Pareto-optimal solutions in a single run. | CMOMO [84], DEL [85] |
Experimental Protocols and Workflows
The integration of multi-objective optimization with ML for drug design follows a structured workflow. The diagram below outlines the key stages, from data preparation to candidate validation.
Protocol: Latent Space Optimization with Transformer-Based Models
This protocol details the methodology for integrating a latent Transformer model with many-objective metaheuristics, as demonstrated in recent studies [85].
Objective: To generate novel drug candidates with optimized binding affinity, ADMET properties, and drug-likeness scores.
Materials:
- Generative Model: A pre-trained latent Transformer autoencoder (e.g., ReLSO or FragNet) capable of encoding molecules to a continuous latent space and decoding vectors back to valid molecular structures (e.g., in SELFIES format).
- Property Prediction Tools: Software for predicting molecular properties (e.g., ADMET predictors, QED, Synthetic Accessibility Score - SAS).
- Docking Software: Tools for molecular docking to estimate binding affinity (e.g., AutoDock Vina).
- Optimization Algorithms: Many-objective metaheuristic algorithms (e.g., MOEA/DD, NSGA-III).
Procedure:
- Model Initialization and Validation:
- Initialize the pre-trained generative model. Validate its performance by assessing the reconstruction accuracy and the chemical validity of generated molecules.
- Example: In a comparative study, the ReLSO model demonstrated superior performance over FragNet in both reconstruction accuracy and latent space organization for molecular generation tasks [85].
Define Objectives and Constraints:
- Formally define the optimization problem. For a dual-target cancer drug with safety considerations, objectives may include:
- f₁: Minimize docking score to Target Protein A (e.g., GSK3β).
- f₂: Minimize docking score to Target Protein B.
- f₃: Maximize QED (drug-likeness).
- f₄: Minimize SAS (synthetic accessibility).
- f₅: Minimize predicted toxicity (e.g., hERG inhibition).
- Define any constraints, such as the presence or absence of specific chemical substructures [84].
- Formally define the optimization problem. For a dual-target cancer drug with safety considerations, objectives may include:
Population Initialization:
- Generate an initial population of molecules, often by encoding a set of known lead molecules or through random sampling in the latent space. Frameworks like CMOMO use a "Bank library" of high-property molecules similar to a lead compound to initialize the population [84].
Iterative Optimization Loop:
- For each generation of the metaheuristic algorithm (e.g., EA): a. Decode: Use the generative model's decoder to convert the population of latent vectors into molecular structures. b. Evaluate: Calculate all objective functions for each decoded molecule using the property prediction and docking tools. c. Select and Reproduce: Apply the metaheuristic's selection, crossover, and mutation operators to create a new population of latent vectors for the next generation. The Vector Fragmentation-based Evolutionary Reproduction (VFER) strategy can be used to enhance efficiency [84].
Termination and Analysis:
- Terminate the process after a predefined number of generations or upon convergence.
- The output is a Pareto front of non-dominated solutions, representing the best possible trade-offs between the objectives.
Protocol: Scaffold-Aware Generation with Variational Autoencoders
Objective: To generate novel, synthetically accessible molecules with multi-target activity using a scaffold-based generation approach.
Materials:
- ScafVAE Framework: A graph-based VAE with a bond scaffold-based decoder and a perplexity-inspired fragmentation encoder [83].
- Surrogate Prediction Models: Lightweight ML models trained on the latent space to predict molecular properties.
- Molecular Dynamics (MD) Simulation Software: For validating binding stability (e.g., GROMACS, AMBER).
Procedure:
- Pre-training: Pre-train the ScafVAE model on a large dataset of drug-like molecules (e.g., ChEMBL, ZINC) to learn meaningful molecular representations.
- Surrogate Model Augmentation: Augment the surrogate models using contrastive learning and molecular fingerprint reconstruction. This improves prediction accuracy for properties with scarce experimental data [83].
- Latent Space Exploration:
- Sample points from the Gaussian-distributed latent space.
- Use the surrogate models to predict properties and identify regions corresponding to desired multi-objective profiles.
- Conditional Decoding: The ScafVAE decoder generates molecules through a two-step process: a. Bond Scaffold Assembly: Assemble molecular graphs by specifying connected bonds without atom types. b. Atom Decoration: Iteratively assign atom types to the scaffold to produce a valid molecule. This approach expands the accessible chemical space while maintaining high validity [83].
- Experimental Validation: Select top candidates from the Pareto front for further in silico validation using MD simulations to confirm stable binding interactions with the target proteins [83].
The Scientist's Toolkit: Essential Research Reagents and Computational Solutions
Successful implementation of multi-objective optimization in RDD relies on a suite of computational tools and platforms.
Table 2: Key Research Reagent Solutions for Multi-objective Drug Design
| Tool/Resource | Type | Primary Function | Application in Workflow |
|---|---|---|---|
| ScafVAE [83] | Graph-based VAE | Scaffold-aware de novo molecular generation. | Core generative model for creating novel molecular structures. |
| ReLSO / FragNet [85] | Transformer Autoencoder | Molecular generation via a regularized latent space. | Provides a continuous latent space for optimization with SELFIES. |
| CMOMO [84] | Deep Evolutionary Framework | Constrained multi-objective molecular optimization. | Handles complex constraints and objectives during optimization. |
| RDKit | Cheminformatics Library | Handles molecular validity, descriptor calculation, and fingerprint generation. | Data pre-processing, validity checks, and feature generation. |
| AutoDock Vina | Docking Software | Predicts binding poses and affinities of ligands to protein targets. | Evaluates the primary efficacy objective (binding strength). |
| ADMET Predictor | QSAR/QSPR Software | Accurately predicts key pharmacokinetic and toxicity endpoints. | Evaluates critical safety and drug-likeness objectives. |
| GROMACS/AMBER | Molecular Dynamics Suite | Simulates the physical movements of atoms and molecules over time. | Validates the stability of binding interactions for top candidates. |
Discussion and Future Perspectives
The integration of multi-objective optimization with advanced ML represents a fundamental shift in RDD, moving from sequential, single-property optimization to a holistic, parallel assessment of a drug candidate's profile. Frameworks like ScafVAE and CMOMO demonstrate the practical feasibility of generating dual-target drug candidates with optimized properties against cancer resistance mechanisms [83] [84]. The shift from multi-objective (2-3 objectives) to many-objective (4+ objectives) optimization is critical, as it more accurately reflects the real-world complexity of drug design [82] [85]. Studies show that Pareto-based many-objective approaches outperform traditional scalarization methods, successfully identifying molecules that balance binding affinity, ADMET properties, and drug-likeness [85].
Future research will focus on improving the realism and scope of optimization. This includes better integration of synthetic accessibility constraints, more accurate and efficient surrogate models for complex properties, and the development of hybrid methods that combine the strengths of evolutionary algorithms with the representational power of deep generative models [84] [82]. As these methodologies mature, they promise to significantly accelerate the discovery of innovative, efficacious, and safe drug therapies.
Assessing Efficacy and Comparing RDD to Traditional Discovery
In the framework of Rational Drug Design (RDD), the validation pipeline represents a systematic, evidence-driven approach to translating theoretical drug candidates into clinically viable therapies. This pipeline establishes a rigorous, iterative process where computational predictions are progressively tested against biological reality, creating a feedback loop that continuously refines models and enhances predictive accuracy. The core principle of RDD involves using structural and mechanistic information to guide drug development deliberately, moving beyond random screening to targeted design. The validation pipeline operationalizes this principle by ensuring that each stage of development—from initial computational target identification through in vitro characterization and ultimate in vivo confirmation—is logically connected and empirically verified.
The fundamental sequence of this pipeline moves from in silico predictions (computer simulations and modeling), to in vitro testing (controlled laboratory experiments on cells or biomolecules), and finally to in vivo evaluation (studies in living organisms). This progression represents increasing biological complexity and clinical relevance, with each stage serving to validate or refute predictions from the previous stage. Modern drug development has witnessed the emergence of sophisticated "in vitro-in silico-in vivo" approaches that create quantitative relationships between these domains, enabling more reliable prediction of human pharmacokinetics and pharmacodynamics before embarking on costly clinical trials [86] [87].
Foundational Concepts and Definitions
The Triad of Validation Models
In Silico Models: Computational approaches that simulate biological processes, drug-target interactions, or physiological systems. These include molecular docking simulations, pharmacokinetic modeling, quantitative structure-activity relationship (QSAR) models, and machine learning algorithms trained on biological data. The primary advantage of in silico methods is their ability to rapidly screen thousands of potential compounds and generate hypotheses about biological activity with minimal resource expenditure [86] [88].
In Vitro Models: Laboratory-based experiments conducted with biological components outside their normal biological context (e.g., cell cultures, isolated proteins, tissue preparations). These models provide initial experimental verification of computational predictions under controlled conditions, allowing for precise manipulation of variables and high-throughput screening. Modern in vitro approaches include cell-based assays, 3D tissue cultures, organ-on-a-chip systems, and high-content screening platforms that generate quantitative data for refining in silico models [86].
In Vivo Models: Studies conducted in living organisms to evaluate drug effects in complex physiological systems. These models account for ADME (Absorption, Distribution, Metabolism, Excretion) properties, toxicity, and efficacy in integrated biological systems. Common models include rodents, zebrafish, and larger animals, with each providing different advantages for predicting human responses. In vivo validation represents the most clinically relevant pre-clinical assessment of drug candidates [86] [87].
Key Validation Metrics and Parameters
Throughout the validation pipeline, quantitative metrics establish the relationship between predictions and experimental outcomes. The following table summarizes critical validation parameters used at each stage:
Table 1: Key Validation Metrics Across the Drug Development Pipeline
| Validation Stage | Primary Metrics | Secondary Metrics | Interpretation Guidelines |
|---|---|---|---|
| In Silico | Predictive accuracy, Receiver Operating Characteristic (ROC) curves, Root Mean Square Error (RMSE) | Molecular docking scores, Binding affinity predictions, QSAR model coefficients | High sensitivity/specificity in cross-validation; concordance with known active/inactive compounds |
| In Vitro | IC₅₀/EC₅₀ values, Percentage inhibition at fixed concentration, Selectivity indices | Cell viability (MTT assay), Target engagement measurements, Kinetic parameters | Dose-response relationships; statistical significance (p<0.05); replication across biological repeats |
| In Vivo | Pharmacokinetic parameters (Cₘₐₓ, Tₘₐₓ, AUC, t₁/₂), Tumor growth inhibition, Survival benefit | Toxicity markers, Biomarker modulation, Pathological scoring | Correlation with human pharmacokinetics; establishment of therapeutic window; translational confidence |
The relationship between these validation stages is not linear but iterative, with data from later stages informing refinements of earlier models. This creates a continuous learning system that improves the predictive power of the entire pipeline over time.
Computational Foundations: In Silico Modeling Approaches
Pharmacokinetic and Pharmacodynamic Modeling
Physiologically Based Pharmacokinetic (PBPK) modeling represents a sophisticated in silico approach that simulates drug absorption, distribution, metabolism, and excretion based on physiological parameters and drug physicochemical properties. Software platforms like GastroPlus implement Advanced Compartmental Absorption and Transit (ACAT) models to simulate intravenous, gastrointestinal, ocular, nasal, and pulmonary absorption of molecules [86]. These tools use numerical integration of differential equations that coordinate well-characterized physical events resulting from diverse physicochemical and biologic phenomena.
For drug combination therapies, particularly relevant in complex diseases like cancer, compartmental PK models have been developed to predict in vivo performance. These models group tissues into compartments based on blood flow and drug binding characteristics, creating a simplified but powerful representation of drug disposition in the body. When coupled with effect data (e.g., percentage of cell growth inhibition over time), these models can predict tissue drug concentration-effect relationships, enabling the design and optimization of dosing regimens [86].
Table 2: Comparison of Major In Silico Modeling Platforms in Drug Development
| Software Platform | Primary Application | Key Features | Validation Requirements |
|---|---|---|---|
| GastroPlus | PBPK modeling and IVIVC | ACAT model for absorption simulation; PKPlus and PBPKPlus modules | Correlation between predicted and observed human pharmacokinetic parameters |
| STELLA | Compartmental PK modeling | Graphical representation of systems; uses Compartments, Flows, Converters; Euler's or Runge-Kutta integration methods | Agreement with in vitro data and prior in vivo PK profiles from literature |
| OHDSI Analytics Pipeline | Patient-level prediction modeling | Standardized approach for reliable development and validation; open-source software tools | Large-scale external validation across multiple databases and healthcare systems |
| PySpark MLlib | Machine learning at scale | Distributed data processing; DataFrame APIs; declarative transformations; built-in model tuning | Internal and external validation discrimination performance; calibration metrics |
Artificial Intelligence and Machine Learning Approaches
Machine learning platforms like PySpark MLlib provide infrastructure for building predictive models on massive datasets, addressing the scale demands of modern drug discovery. MLlib enables the creation of end-to-end machine learning pipelines that include feature engineering, model training, and distributed validation—critical for handling the high-dimensional data generated in omics approaches to drug target identification [88].
The OHDSI analytics pipeline demonstrates a standardized approach for reliable development and validation of prediction models, addressing common limitations in medical prediction models through phenotype validation, precise specification of the target population, and large-scale external validation [89]. This pipeline has been successfully applied to develop COVID-19 prognosis models using multiple machine learning methods (AdaBoost, random forest, gradient boosting machine, decision tree, L1-regularized logistic regression, and MLP neural network) validated across international databases containing over 65,000 hospitalizations [89].
Experimental Translation: From Computational Predictions to Laboratory Verification
In Vitro Validation Methodologies
In vitro validation provides the critical experimental bridge between computational predictions and biological systems. The following experimental protocols represent standardized approaches for validating in silico predictions:
Protocol 1: Cell Growth Inhibition Assay (MTT Assay)
- Purpose: To evaluate the inhibitory effects of drug candidates on cell proliferation, particularly for anticancer agents.
- Cell Culture: Maintain human cell lines (e.g., PNT-2, PC-3, A549) in RPMI-1640 medium supplemented with 10% fetal bovine serum at 37°C in a 5% CO₂ atmosphere. Subculture cells by trypsinization twice weekly [86].
- Drug Treatment: Prepare stock solutions of reference drugs (gemcitabine, 5-fluorouracil) and repurposed drugs (itraconazole, verapamil, tacrine) in DMSO. Dilute with culture medium prior to use. Include DMSO-only controls [86].
- Assay Procedure: Seed cells at optimal density (4 × 10⁴ cells/mL) in multi-well plates. After 24 hours, treat with drug concentrations based on in silico predictions. Incubate for predetermined time periods. Add MTT reagent and incubate for 4 hours. Solubilize formazan crystals with DMSO and measure absorbance at 570 nm [86].
- Data Analysis: Calculate percentage cell growth inhibition relative to untreated controls. Generate dose-response curves and determine IC₅₀ values using appropriate statistical software.
Protocol 2: Artificial Neural Networks (ANNs) for In Vitro-In Vivo Correlation
- Purpose: To establish quantitative relationships between in vitro drug release and in vivo absorption using nonlinear modeling approaches.
- Data Collection: Generate comprehensive in vitro dissolution data under various experimental conditions (different apparatus, dissolution media, pH values) [87].
- Network Architecture: Design a feedforward neural network with input nodes representing in vitro dissolution time points, hidden layers with nonlinear activation functions, and output nodes representing in vivo absorption parameters [87].
- Model Training: Employ backpropagation algorithms to minimize the difference between predicted and observed in vivo responses. Use cross-validation to prevent overfitting [87].
- Validation: Apply the trained ANN to predict in vivo performance from new in vitro data. Compare predictions with actual observed in vivo results to assess model accuracy [87].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for Validation Pipeline Experiments
| Reagent/Material | Function in Validation Pipeline | Application Examples | Technical Considerations |
|---|---|---|---|
| Human Cell Lines (PNT-2, PC-3, A549) | Provide biologically relevant systems for initial efficacy and toxicity testing | Cancer cell growth inhibition assays; target engagement verification | Maintain >90% viability; routinely check for contamination and authentication |
| Reference Compounds (Gemcitabine, 5-Fluorouracil) | Serve as positive controls and benchmark for new drug candidates | Establishing baseline activity for anticancer drug combinations | Prepare fresh stock solutions; optimize storage conditions (-20°C) |
| Repurposed Drug Library (Itraconazole, Verapamil, Tacrine) | Provide compounds with known safety profiles for combination therapies | Evaluating enhanced efficacy of anticancer drugs in combination | Consider solubility limitations (DMSO stock solutions) |
| MTT Reagent (3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) | Measure cell viability and proliferation as indicator of compound efficacy | Quantifying dose-response relationships in cell-based assays | Optimize cell density and incubation time; ensure complete solubilization |
| DMSO (Dimethyl Sulfoxide) | Universal solvent for compounds with low aqueous solubility | Preparing stock solutions of hydrophobic drug candidates | Use low concentrations (<0.1%) to avoid cellular toxicity |
Integrated Workflows: Case Studies in Validation Pipeline Implementation
Case Study 1: Anticancer Drug Combination Development
A comprehensive study demonstrated the implementation of a full validation pipeline for anticancer drug combinations. Researchers developed two-compartment PK models based on in vitro assay results with the goal of predicting in vivo performance of drug combinations in cancer therapy. Combinations of reference anticancer drugs (gemcitabine and 5-fluorouracil) with repurposed drugs (itraconazole, verapamil, or tacrine) were evaluated in vitro using prostate and lung cancer cell lines [86].
The in silico PK models were developed based on these in vitro results and human PK profiles from literature. The models predicted that itraconazole would be the most effective in combination with either reference anticancer drug, demonstrating itraconazole-dose dependent cell growth inhibition. The models further predicted increased efficacy with continued itraconazole administration (24-hour dosing interval), providing specific dosing regimen recommendations for future clinical testing [86].
This case study exemplifies the RDD principle of using computational models to extrapolate from limited experimental data to clinically relevant predictions, potentially accelerating the development of effective combination therapies while reducing the need for extensive animal testing.
Case Study 2: IVIVC for Modified-Release Formulations
In a nifedipine osmotic release tablet case study, researchers developed integrated in vitro-in silico-in vivo models using both mechanistic gastrointestinal simulation (GIS) and artificial neural networks (ANNs). The study aimed to establish predictive relationships between in vitro dissolution profiles and in vivo absorption [87].
Both GIS and ANN approaches demonstrated sensitivity to input kinetics represented by in vitro profiles obtained under various experimental conditions. The GIS model exhibited better generalization ability, providing excellent predictability for two dosage forms exhibiting different in vivo performance, while the ANN model showed higher prediction errors for the formulation with different release mechanisms [87]. This highlights how different in silico approaches may be successfully employed in model development, with relevant outcomes sensitive to the methodology employed.
Diagram 1: IVIVC Model Development Workflow
Analytical Framework: Data Management and Validation Metrics
Standardized Analytics Pipelines for Reliable Prediction
The Observational Health Data Sciences and Informatics (OHDSI) analytics pipeline provides a standardized approach for reliable development and validation of prediction models. This pipeline includes harmonization and quality control of originally heterogeneous observational databases, large-scale application of machine learning methods in a distributed data network, and transparent use of open-source software tools with publicly shared analytical code [89].
The implementation of this pipeline for predicting COVID-19 mortality risk demonstrated that following a standardized analytics pipeline can enable rapid development of reliable prediction models. The study compared six machine learning methods across multiple international databases, with L1-regularized logistic regression demonstrating superior calibration and discrimination performance compared to more complex algorithms [89]. This highlights the importance of rigorous validation over algorithmic complexity in predictive modeling for drug development.
Data Visualization Principles for Effective Communication
Effective communication of validation results requires appropriate data visualization strategies. The choice between tables and charts depends on the communication goals:
Tables are advantageous when readers need to extract specific information, precise numerical values, or ranks. They provide exact representation of numerical values essential for detailed comparisons and data lookup [90] [91].
Charts encode data values as position, length, size, or color, supporting readers when making comparisons, predictions, or perceiving patterns and trends [90].
For table design, three key principles enhance communication: (1) aid comparisons through appropriate alignment and formatting; (2) reduce visual clutter by eliminating unnecessary grid lines and repetition; and (3) increase readability through clear headers, highlighting of key results, and logical organization [90].
Diagram 2: Integrated Validation Pipeline Workflow
Emerging Trends and Future Directions
AI-Enabled Clinical Trials and Real-World Data Integration
By 2025, the integration of real-world data (RWD) is transforming clinical trial optimization, with RWD becoming central to how trials are designed, executed, and evaluated. Key trends include tokenization and privacy-preserving linkage to connect clinical trial data with electronic health records and claims data, AI-driven trial design and monitoring for real-time adaptation, and endpoint-driven design supported by RWD to enable risk-based monitoring strategies [92].
This evolution creates new opportunities for validating in silico predictions against large-scale human data, potentially accelerating the translation of computational insights into clinical applications. The embedding of RWD into every stage of drug development—from protocol development to post-market surveillance—promises to accelerate innovation while improving equity and outcomes [92].
Continuous Machine Learning for Adaptive Validation
The medical device sector is witnessing the emergence of continuous machine learning, with the first submissions for devices enabled by continuous ML anticipated in 2025. Unlike current "passive" ML approaches where products are locked down after training, continuous ML devices adapt as they are exposed to more patient data, enabling continuous learning during the device's operational life cycle to actively respond to patient needs [93].
This approach could revolutionize validation pipelines by creating self-improving models that continuously refine their predictions based on real-world clinical experience, ultimately leading to more accurate and personalized therapeutic interventions.
The validation pipeline from in silico predictions to in vitro and in vivo models represents a cornerstone of modern Rational Drug Design. By establishing rigorous, quantitative relationships between computational predictions and biological observations, this pipeline enables more efficient and predictive drug development. The case studies and methodologies presented demonstrate that successful implementation requires:
- Iterative refinement of models based on experimental feedback
- Standardized analytics pipelines to ensure reproducibility and reliability
- Appropriate validation metrics at each stage of the pipeline
- Integration of emerging technologies like AI and real-world data
- Effective communication of results through thoughtful data visualization
As drug development grows increasingly complex and resource-intensive, robust validation pipelines will become even more critical for translating theoretical advances into tangible patient benefits. The continued refinement of these approaches promises to enhance the efficiency, predictability, and success rates of the entire drug development enterprise.
Preclinical studies play a crucial role in the journey toward new drug discovery and development, assessing the safety, efficacy and potential side effects of a target compound or medical intervention before any testing takes place on humans [94]. Within the framework of Rational Drug Design (RDD), these studies provide the essential quantitative data that informs the deliberate, knowledge-driven design of therapeutic molecules, moving beyond traditional trial-and-error approaches [4] [95]. RDD exploits the detailed recognition and discrimination features that are associated with the specific arrangement of the chemical groups in the active site of a target macromolecule [5]. The overarching goal of preclinical assessment is to generate robust evidence on a compound's biological activity (pharmacodynamics) and its fate within the body (pharmacokinetics), thereby building the foundational rationale for proceeding to human trials and reducing costly late-stage failures [96] [94].
Preclinical Development within the Drug Development Pipeline
Drug development follows a structured process with five main stages: discovery, preclinical research, clinical research, regulatory review, and post-market monitoring [96]. Preclinical research serves as the critical bridge between initial drug discovery and clinical trials in humans. During this phase, promising candidates identified in discovery are tested in laboratory and animal studies to evaluate their biological activity, potential benefits, and safety [96]. A typical preclinical development program consists of several major segments, including the manufacture of the active pharmaceutical ingredient, preformulation and formulation, analytical method development, and comprehensive metabolism, pharmacokinetics, and toxicology studies [94]. The duration of this research can vary from several months to a few years, depending on the complexity of the medical intervention and specific regulatory requirements [94].
The Four Phases of Preclinical Research
Preclinical research is systematically organized into four distinct phases [94]:
- Phase 1: Basic Research: This initial phase involves studies to understand the underlying biology of a disease and identify potential drug targets—biological processes or pathways that play a role in a particular condition. This is followed by target validation to confirm the therapeutic effects of modulating the target.
- Phase 2: Drug Discovery and Candidate Nomination: Researchers focus on finding or designing molecules that can interact with the validated target. Potential therapeutic compounds, known as "hits," are tested, often in cellular disease models, and the most promising "drug candidate" is selected based on factors like potency, selectivity, and safety profile.
- Phase 3: Lead Optimization: Promising compounds, or "leads," are chemically modified to improve their performance. Scientists gather critical information on the safest and most effective doses and build a dosing strategy. This stage aims to arrive at the best possible drug candidate.
- Phase 4: Investigational New Drug (IND)-Enabling Studies: The most promising candidate undergoes advanced safety testing. Sponsors must also submit detailed information on drug manufacturing and proposed clinical trial plans to regulators (e.g., FDA, EMA). Approval of the IND application is required to proceed to human clinical trials.
Core Principles: Pharmacodynamics and Pharmacokinetics
The safety and efficacy assessment of a drug candidate during preclinical development rests on two fundamental pillars: pharmacodynamics (PD) and pharmacokinetics (PK). These two disciplines provide a holistic understanding of a drug's action and disposition [94].
Pharmacodynamics describes the relationship between the concentration of a drug at its site of action and the resulting biological effect (i.e., the dose response) [94]. It defines what the drug does to the body, encompassing therapeutic effects, mechanisms of action, and potential adverse events.
Pharmacokinetics describes the time course of drug movement through the body, governed by the processes of Absorption, Distribution, Metabolism, and Excretion (ADME) [94]. It defines what the body does to the drug, determining the drug's concentration-time profile in plasma and tissues.
The interplay between PK and PD is critical. Pharmacokinetic interactions occur when a drug affects the concentration of another co-administered drug, while pharmacodynamic interactions occur when a drug affects the actions of another drug without altering its concentration [94]. A comprehensive preclinical assessment integrates both to build a complete picture of a drug's profile.
Table 1: Key Physicochemical Properties Influencing PK/PD Profiles [4]
| Property | Description | Impact on PK/PD |
|---|---|---|
| Partition Coefficient | Measure of a drug's lipophilicity/hydrophilicity | Determines membrane permeability, distribution, and absorption. |
| Dissociation Constant (pKa) | The pH at which a molecule is 50% ionized. | Influences solubility and permeability, which vary with physiological pH. |
| Ionization Capacity | The ability of a molecule to gain or lose a proton. | Affects solubility, binding to receptors, and passive diffusion. |
| Complexation | The association of a drug with other components to form a complex. | Can alter solubility, dissolution rate, stability, and bioavailability. |
| Protein Binding | The extent to which a drug binds to plasma proteins. | Influences the volume of distribution and the amount of free, active drug. |
| Stereochemistry | The three-dimensional spatial arrangement of atoms in a molecule. | Different enantiomers can have vastly different pharmacological activities and PK profiles [4]. |
Experimental Methodologies and Protocols
Pharmacokinetic (PK) Studies: Assessing ADME
Objective: To quantitatively characterize the Absorption, Distribution, Metabolism, and Excretion of a new drug candidate. Core Protocol: A standard in vivo PK study involves administering the drug to animal models (e.g., rodents, canines) via the intended route (e.g., oral, intravenous) and collecting serial blood samples at predetermined time points. Tissue samples may also be collected post-mortem to assess distribution [94].
- Sample Collection and Analysis: Blood samples are processed to plasma, and tissues are homogenized. The concentration of the parent drug and its metabolites in these samples is quantified using validated bioanalytical methods, typically Liquid Chromatography with tandem Mass Spectrometry (LC-MS/MS).
- Data Analysis: Non-Compartmental Analysis (NCA) is a model-independent approach used to estimate primary PK parameters directly from the plasma concentration-time data [96]. These parameters are summarized in Table 2.
Table 2: Key Pharmacokinetic Parameters from Non-Compartmental Analysis
| Parameter | Unit | Description |
|---|---|---|
| C~max~ | Mass/Volume (e.g., ng/mL) | The maximum observed plasma concentration. |
| T~max~ | Time (e.g., h) | The time to reach C~max~. |
| AUC~0-t~ | Mass/Volume * Time (e.g., ng·h/mL) | The area under the plasma concentration-time curve from zero to the last measurable time point. |
| AUC~0-∞~ | Mass/Volume * Time (e.g., ng·h/mL) | The total area under the plasma concentration-time curve from zero to infinity. |
| t~1/2~ | Time (e.g., h) | The elimination half-life. |
| CL | Volume/Time (e.g., L/h) | The total body clearance of the drug. |
| V~d~ | Volume (e.g., L) | The apparent volume of distribution. |
Diagram 1: In Vivo Pharmacokinetic Study Workflow
Pharmacodynamic (PD) Studies: Assessing Efficacy and Safety
Objective: To evaluate the biological and therapeutic effects of the drug candidate and establish the relationship between dose (or exposure) and response. Core Protocol: PD studies are designed to measure a drug's efficacy and potential side effects in disease-relevant models. This includes:
- In Vitro Assays: Testing the drug on cell cultures to measure target engagement, functional responses (e.g., cAMP accumulation, calcium flux), and cell proliferation or death.
- In Vivo Efficacy Models: Employing animal models of human disease (e.g., xenograft models for oncology, transgenic models for neurology) to demonstrate therapeutic benefit. Animals are dosed with the candidate drug, and disease-relevant endpoints (e.g., tumor volume, biomarker levels, behavioral changes) are monitored over time.
- Safety Pharmacology and Toxicology: Conducting studies to identify potential adverse effects. This includes core battery tests for central nervous system, cardiovascular, and respiratory functions, as well as repeat-dose toxicology studies to identify target organ toxicity and determine a No Observed Adverse Effect Level (NOAEL) [94].
Integrated PK/PD Modeling
Objective: To mathematically relate the pharmacokinetic profile of a drug to the intensity of its pharmacodynamic response, thereby bridging exposure and effect. Methodology: A semi-mechanistic PK/PD modeling approach is often used, which combines empirical and mechanistic elements to characterize the complex, time-dependent relationship between drug concentration and effect [96]. This model-integrated evidence is a cornerstone of Model-Informed Drug Development (MIDD) [96]. The steps involve:
- Developing a population pharmacokinetic (PPK) model to describe the drug's time course and account for variability among individuals [96].
- Developing a PD model (e.g., Emax model) to describe the relationship between concentration at the effect site and the observed response.
- Linking the PK and PD models, often through a hypothetical effect compartment, to account for any temporal disconnect between plasma concentrations and the observed effect (hysteresis).
Diagram 2: Integrated PK/PD Modeling Relationship
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Preclinical PK/PD Studies
| Reagent / Material | Function / Application |
|---|---|
| Validated Bioanalytical Assay (e.g., LC-MS/MS) | Quantification of the parent drug and its metabolite concentrations in biological matrices (plasma, serum, tissues) with high specificity and sensitivity. |
| Cell-Based Reporter Assays | In vitro systems to measure target engagement and functional downstream effects, such as gene expression or second messenger activation. |
| Disease-Relevant Animal Models | In vivo systems (e.g., xenograft, transgenic, induced-disease) to evaluate the therapeutic efficacy and safety of the drug candidate in a complex biological context. |
| Specific Antibodies & ELISA Kits | Detection and quantification of protein biomarkers, drug targets, or indicators of pharmacological response and toxicity. |
| ADME-Tox Screening Platforms | High-throughput in vitro tools (e.g., Caco-2 cells for permeability, liver microsomes for metabolic stability) to early assessment of PK properties and toxicity risks. |
| Formulation Vehicles | Chemically compatible and physiologically tolerable solvents or carriers (e.g., aqueous buffers, suspensions with methylcellulose) for administering the drug to animals. |
Regulatory and Strategic Considerations
Preclinical studies must adhere to strict regulatory guidelines and ethical considerations. Regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) provide specific guidelines for preclinical study design, conduct, and reporting [94]. Compliance with Good Laboratory Practice (GLP) is required to ensure the quality, reliability, and integrity of the generated data [94].
The final stage of preclinical development involves IND-enabling studies. The results from these studies, along with detailed plans for clinical trials and drug manufacturing, are submitted to regulators. The FDA and other agencies then evaluate the intervention's potential risks and benefits before granting permission to proceed to human testing [94]. The application of Model-Informed Drug Development (MIDD) approaches, such as PBPK and quantitative systems pharmacology (QSP), in the preclinical phase can significantly optimize this process, improve quantitative risk estimates, and increase the probability of regulatory success [96].
The Role of Clinical Trials in Validating RDD-Derived Therapeutics
Rational Drug Design (RDD) represents a paradigm shift from traditional empirical drug discovery to a targeted approach based on structural biology and molecular understanding of disease mechanisms. This methodology begins with identifying a biological target critical to disease pathology and proceeds with designing molecules to interact with this target in a specific, predictable manner [1]. The process traditionally relies on structure-activity relationship (SAR) studies, where molecular modeling guides strategic chemical modifications to optimize a drug candidate's effectiveness [1]. While RDD has produced successful therapeutics like lovastatin and captopril, its ultimate validation depends on demonstrating safety and efficacy in human clinical trials [1].
The convergence of computational technologies with traditional RDD has accelerated the discovery phase, but these advances have simultaneously increased the importance of rigorous clinical validation. Modern RDD increasingly incorporates artificial intelligence and machine learning, leading to the emergence of the "informacophore" concept—a data-driven extension of the traditional pharmacophore that integrates computed molecular descriptors and machine-learned structural representations [1]. However, even the most sophisticated computational predictions require empirical validation through biological functional assays and, ultimately, controlled human trials [1]. This article examines the critical role of clinical trials in translating RDD-derived candidates from theoretical promise to approved therapeutics.
The RDD to Clinical Pipeline: Workflow and Key Transition Points
The pathway from initial target identification to clinically validated therapeutic involves multiple stages where computational predictions meet experimental validation. Figure 1 illustrates this integrated workflow, highlighting how clinical trials represent the culmination of the RDD process.
Figure 1. Integrated RDD to Clinical Pipeline. This workflow illustrates the transition from computational design to clinical validation, highlighting key decision points where experimental data informs subsequent development stages.
The transition from preclinical to clinical development represents a critical juncture for RDD-derived compounds. Sponsors must submit robust Chemistry, Manufacturing, and Control (CMC) information to regulatory authorities, demonstrating controlled production conditions with tests ensuring identity, purity, potency, and stability [97]. Additionally, comprehensive nonclinical data must address pharmacokinetics, pharmacodynamics, and toxicology profiles derived from in vitro systems and animal models [97]. This package supports filing an Investigational New Drug (IND) application in the United States or a Clinical Trial Application (CTA) in the European Union, permitting initial human trials [97].
Clinical Trial Methodologies for RDD-Derived Therapeutics
Phase I Trial Designs: Establishing Safety and Dosing
Phase I trials represent the first human application of a new drug and set the foundation for subsequent development. For RDD-derived therapeutics, these trials must balance ethical concerns against the need to establish safe dosing parameters [97]. The guiding principle is to avoid unnecessary patient exposure to subtherapeutic doses while preserving safety and maintaining rapid accrual [98].
Table 1: Comparison of Phase I Trial Designs for Establishing Recommended Phase II Dose
| Design Method | Key Characteristics | Advantages | Limitations | Application to RDD-Derived Therapeutics |
|---|---|---|---|---|
| Traditional 3+3 Design | Cohorts of 3 patients; dose escalation based on prespecified rules using dose-limiting toxicity (DLT) observations [98] | Simple implementation; familiar to clinical investigators; built-in safety pauses | Slow escalation; may expose many patients to subtherapeutic doses; does not incorporate pharmacokinetic data | Suitable for cytotoxic agents where toxicity and efficacy are dose-dependent |
| Model-Based Designs | Assigns patients and defines recommended dose based on statistical modeling of dose-toxicity relationship [98] | More efficient dose escalation; fewer patients at subtherapeutic doses; incorporates all available data | Complex implementation; requires statistical expertise; potential safety concerns without proper safeguards | Emerging utility for molecularly targeted therapies where maximum tolerated dose may not equal optimal biological dose |
| Accelerated Titration Designs | Rapid initial dose escalation with one patient per cohort until moderate toxicity observed [98] | Faster identification of therapeutic dose range; reduces number of patients at low doses | Increased risk of severe toxicity with rapid escalation; requires careful safety monitoring | Appropriate when preclinical data strongly predicts human toxicity profile |
| Pharmacologically Guided Dose Escalation (PGDE) | Uses animal pharmacokinetic data to predict human dose escalation [98] | Science-based escalation; potentially fewer dose levels needed | Relies on interspecies scaling assumptions; limited validation across drug classes | Valuable for RDD-derived compounds with well-characterized pharmacokinetic properties |
Trial endpoint selection has evolved significantly for RDD-derived therapies, especially molecularly targeted agents. While traditional Phase I oncology trials primarily used toxicity endpoints to establish a maximum tolerated dose (MTD), targeted therapies may achieve efficacy at doses below the MTD [98]. This has prompted inclusion of alternative endpoints such as:
- Optimal Biological Dose (OBD): Dose associated with prespecified effects on biomarkers like target inhibition in tumor or surrogate tissue [98]
- Pharmacodynamic endpoints: Measurement of drug effects on the body, including molecular correlates and imaging endpoints [98]
- Pharmacokinetic endpoints: Assessment of drug absorption, distribution, metabolism, and excretion [98]
Phase II/III Trial Considerations: Demonstrating Efficacy
Later-phase trials for RDD-derived therapeutics face unique challenges, particularly for rare diseases or molecularly defined subgroups. The FDA's Rare Disease Evidence Principles (RDEP) provide a framework for developing drugs for very small patient populations (generally fewer than 1,000 patients in the U.S.) with significant unmet medical needs [99]. This approach acknowledges that traditional clinical trial designs may be impractical or impossible in these contexts.
Under RDEP, approval may be based on one adequate and well-controlled study plus robust confirmatory evidence, which may include [99]:
- Strong mechanistic or biomarker evidence
- Evidence from relevant non-clinical models
- Clinical pharmacodynamic data
- Case reports, expanded access data, or natural history studies
Table 2: Efficacy Endpoints for RDD-Derived Therapeutics in Oncology
| Endpoint Category | Specific Endpoints | Application Context | Considerations for RDD-Derived Therapeutics |
|---|---|---|---|
| Survival Outcomes | Overall Survival (OS); Progression-Free Survival (PFS) [100] | Traditional efficacy endpoints for cytotoxic and targeted therapies | May be complemented by biomarker data to establish biological activity |
| Biomarker Endpoints | Minimal Residual Disease (MRD) negativity [100] | Hematologic malignancies; sensitive measure of treatment effect | Particularly relevant for targeted therapies with specific molecular targets |
| Clinical Response | Objective Response Rate (ORR); Complete Response (CR) [100] | Solid tumors and hematologic malignancies | Standard efficacy measure across trial phases |
| Patient-Reported Outcomes | Quality of Life measures; symptom burden | Context of overall risk-benefit assessment | Increasingly important for targeted therapies with chronic administration |
For RDD-derived therapeutics targeting specific molecular pathways in heterogeneous diseases, enrichment strategies and adaptive designs may be employed. The FDA guidance "Developing Targeted Therapies in Low-Frequency Molecular Subsets of a Disease" describes approaches for evaluating benefits and risks of targeted therapeutics within a clinically defined disease where some molecular alterations may occur at low frequencies [101].
Regulatory and Ethical Framework
Clinical trials of RDD-derived therapeutics operate within a rigorous ethical and regulatory framework designed to protect human subjects while facilitating drug development. The foundation of modern human medical experimentation rests on principles outlined in the Nuremberg Code and Good Clinical Practices (GCP) [97]. These principles include:
- Voluntary informed consent is absolutely essential
- Experiments must yield fruitful results for the good of society
- Risk should never exceed humanitarian importance of the problem solved
- Scientists must be prepared to terminate experiments if continuation risks injury, disability, or death [97]
Regulatory oversight involves multiple entities. In the United States, the FDA protects public health by ensuring the safety, efficacy, and security of human drugs, while Institutional Review Boards (IRBs) ensure protection of human subjects [97]. Similarly, the European Medicines Agency (EMA) harmonizes drug assessment and approval across Europe, with Ethics Committees (ECs) overseeing subject protection [97].
For rare diseases, regulatory science has evolved to address unique challenges. FDA guidance "Rare Diseases: Natural History Studies for Drug Development" emphasizes the value of understanding a disease's natural course to support drug development, particularly when traditional trials are not feasible [101]. Additionally, the "Rare Diseases: Early Drug Development and the Role of Pre-IND Meetings" guidance assists sponsors in planning more efficient pre-investigational new drug application meetings [101].
Case Study: CD38-Targeted Therapies for High-Risk Multiple Myeloma
The development of CD38-targeted therapies exemplifies successful clinical validation of RDD-derived therapeutics. Multiple myeloma patients with high-risk cytogenetic features face poor outcomes despite conventional treatments [100]. Rational design of CD38-targeting monoclonal antibodies like daratumumab represented a targeted approach for this malignancy.
A systematic review and meta-analysis of 18 randomized controlled trials evaluating new drug combinations for high-risk multiple myeloma demonstrated the significant impact of CD38-targeted therapies [100]. Figure 2 illustrates the key findings from this analysis regarding progression-free survival benefits.
Figure 2. Efficacy of CD38-Targeted Therapy in High-Risk Multiple Myeloma. This diagram summarizes key outcomes from a meta-analysis of CD38-based regimens in transplant-eligible patients, showing significant improvements in progression-free survival (PFS) and reductions in disease progression or death risk during both induction and maintenance therapy phases [100].
The clinical development of these therapies employed sophisticated trial methodologies appropriate for their targeted mechanism:
- Patient Selection: Focus on high-risk cytogenetic features defined by specific abnormalities (t(4;14), t(14;16), t(14;20), del(17p), 1q21+) [100]
- Endpoint Selection: Included traditional endpoints (PFS, OS) alongside biomarker endpoints (MRD negativity) [100]
- Combination Strategies: Evaluated CD38-targeted agents with established backbone therapies [100]
The success of CD38-targeted therapies demonstrates how clinical trials validate and refine RDD-derived approaches, ultimately confirming their therapeutic value in defined patient populations.
Table 3: Key Research Reagent Solutions for RDD and Clinical Validation
| Tool Category | Specific Tools/Assays | Function in RDD and Clinical Validation | Application Context |
|---|---|---|---|
| Target Engagement Assays | CETSA (Cellular Thermal Shift Assay) [13] | Validates direct drug-target interaction in intact cells and tissues; provides quantitative, system-level validation | Bridge between computational predictions and cellular efficacy; used in mechanism confirmation |
| Informatics Platforms | Molecular docking software (AutoDock); ADMET prediction tools (SwissADME) [13] | Virtual screening of compound libraries; prediction of drug-like properties prior to synthesis | Early-stage compound prioritization; reduces resource burden on wet-lab validation |
| Functional Assays | Enzyme inhibition assays; cell viability assays; pathway-specific reporter systems [1] | Provides quantitative empirical insights into compound behavior within biological systems | Confirmation of computational predictions; establishes real-world pharmacological relevance |
| Biomarker Assays | MRD detection methods; protein expression analysis; pharmacokinetic assays [98] [100] | Measures drug effects on biological systems; provides pharmacodynamic evidence of activity | Clinical trial endpoint selection; dose optimization for targeted therapies |
| Formulation Tools | Spray drying equipment; nasal cast models; inhalation device screening platforms [102] [103] | Enables development of optimal delivery systems for various administration routes | Critical for biologics and respiratory delivery; ensures stability and efficient delivery |
The field of clinical development for RDD-derived therapeutics continues to evolve, with several emerging trends shaping future approaches:
Artificial Intelligence Integration: AI has evolved from a disruptive concept to a foundational capability, informing target prediction, compound prioritization, and pharmacokinetic property estimation [13]. Recent work demonstrates that integrating pharmacophoric features with protein-ligand interaction data can boost hit enrichment rates by more than 50-fold compared to traditional methods [13].
Innovative Clinical Trial Designs: With the emergence of therapies for rare diseases and molecularly defined subsets, regulatory science is adapting. The FDA's Rare Disease Evidence Principles provide a pathway for developing treatments for very small patient populations using flexible evidence standards [99].
Advanced Delivery Systems: For biologics and complex therapeutics, formulation strategies are becoming increasingly sophisticated. Research into nasal powder delivery platforms and optimized dry powder inhalers demonstrates the importance of delivery system engineering for therapeutic effectiveness [103].
The validation of RDD-derived therapeutics through clinical trials represents a critical bridge between computational design and patient benefit. While RDD strategies have dramatically improved the efficiency of early drug discovery, clinical trials remain the indispensable mechanism for confirming therapeutic value, optimizing dosing, and establishing the risk-benefit profile in human populations. As computational methods grow more sophisticated, clinical trial methodologies must similarly evolve to efficiently validate targeted therapies, particularly for rare diseases and molecularly defined patient subsets. The continued synergy between rational design and rigorous clinical validation promises to accelerate the development of novel therapeutics for diseases with significant unmet needs.
Within the paradigm of rational drug design (RDD), the imperative to innovate is driven by a critical juncture in pharmaceutical research and development (R&D). Traditional R&D models, while responsible for historic medical breakthroughs, are now characterized by soaring costs and declining productivity. This paper presents a comparative analysis of emerging, data-driven RDD methodologies against traditional approaches, framing the findings within the broader thesis that RDD principles are essential for revitalizing the pharmaceutical pipeline. Faced with an impending patent cliff threatening $350 billion in revenue and development costs that can exceed $2.2 billion per new drug, the industry must adopt more efficient and predictive strategies [104]. RDD, leveraging computational power and chemoinformatic principles, represents a fundamental shift from serendipitous discovery to a targeted, knowledge-driven process, offering a path to improved success rates and enhanced R&D efficiency [105].
Defining the Methodologies: Traditional vs. Rational Drug Design
The distinction between traditional and rational drug design is foundational to understanding their relative performance.
Traditional Drug Discovery
The traditional approach, often termed phenotypic screening, is largely empirical. It begins with the observation of a desired biological effect in a complex cellular or whole-organism system without prior knowledge of the specific molecular target. This process involves the mass screening of vast libraries of compounds, either natural or synthetic, to identify "hits" that produce the target phenotype. Subsequent lead optimization is then a cyclical process of synthesizing and testing analog compounds to improve potency and pharmacokinetic properties. This method is historically significant but is inherently resource-intensive and time-consuming, with a low probability of success as it often proceeds without a clear understanding of the underlying mechanism of action [104] [105].
Rational Drug Design (RDD)
In contrast, Rational Drug Design is a target-centric methodology. It initiates with the identification and validation of a specific macromolecular target, typically a protein or nucleic acid, that plays a critical role in a disease pathway. The design process is guided by a deep understanding of the target's three-dimensional structure and its interaction with potential drug molecules. Core to RDD are chemoinformatic approaches that systematically explore the relationship between chemical structure and biological activity [105]. This includes:
- Structure-Based Design: Using the 3D structure of the target (from X-ray crystallography, NMR, or homology modeling) to design molecules that fit complementarily into the binding site.
- Ligand-Based Design: When the target structure is unknown, using known active ligands to develop a Pharmacophore model or Quantitative Structure-Activity Relationship (QSAR) to predict the activity of new compounds.
- Chemogenomics: Systematically studying the interaction of many small molecules with families of related targets to derive rules that can be applied to novel, uninvestigated targets [105].
Table 1: Core Principles of Traditional and Rational Drug Design Methodologies
| Feature | Traditional Drug Discovery | Rational Drug Design (RDD) |
|---|---|---|
| Starting Point | Phenotypic observation in complex systems | Defined molecular target & disease mechanism |
| Core Approach | Empirical screening & iterative optimization | Hypothesis-driven, structure-guided design |
| Data Utilization | Limited, focused on lead series | Extensive use of structural, genomic, & chemoinformatic data |
| Target Knowledge | Often unknown at outset | Prerequisite for initiation |
| Automation & AI | Limited to High-Throughput Screening (HTS) | Integral to virtual screening & de novo design |
Quantitative Comparison: Success Rates and Development Metrics
The theoretical advantages of RDD are borne out in key performance indicators across the drug development lifecycle. The industry faces a persistent attrition rate, with the success rate for Phase 1 drugs falling to just 6.7% in 2024, down from 10% a decade ago [104]. This high failure rate, particularly in late-stage clinical trials, is the primary driver of cost and inefficiency. While direct, study-for-study comparisons of RDD vs. traditional methods are complex, the aggregate data and specific case studies demonstrate RDD's impact.
A pivotal metric is the internal rate of return (IRR) for R&D investment. After plummeting to a trough of 1.5%, the average forecast IRR for the top 20 drugmakers rebounded to 5.9% in 2024 [104]. This recovery is heavily influenced by the success of "first-in-class" therapies developed through targeted approaches. Tellingly, if GLP-1 agonists (a class derived from rational target investigation) were excluded, the cohort's IRR would drop to 3.8%, underscoring that high-impact innovation driven by RDD principles is paramount for profitability [104].
Table 2: Comparative Analysis of Key R&D Performance Indicators
| Performance Indicator | Traditional / Industry Average | RDD-Enhanced Approach | Impact & Evidence |
|---|---|---|---|
| Phase 1 Success Rate | 6.7% (2024) [104] | Potential for improvement via better target validation | AI/ML models analyze vast datasets to identify promising candidates earlier, reducing late-stage attrition [104]. |
| Cost per New Drug | ~$2.2 - $2.6 Billion [104] | Potential for significant reduction | AI can slash development costs by identifying the most promising candidates early, minimizing wasted resources; potential industry savings estimated at up to $100B annually [104]. |
| Development Timeline | >100 months (Phase 1 to filing) [104] | Accelerated discovery & optimization | AI significantly speeds up the discovery process, from target identification to lead optimization [104]. |
| R&D IRR (excl. GLP-1) | 3.8% [104] | 5.9% (overall top 20 avg.) [104] | Highlights the superior financial return of focused, rational approaches to first-in-class therapies. |
| Molecular Analysis Speed | Slower, fingerprint-based similarity searches [106] | Faster, more accurate graph-based methods | Graph-based similarity searches using Maximum Common Subgraph (MCS) are more accurate than fingerprint-based methods, reducing false positives in virtual screening [106]. |
Experimental Protocols and Workflows
The quantitative benefits of RDD are realized through specific, rigorous experimental and computational protocols.
Protocol for a Traditional Phenotypic Screening Campaign
This protocol outlines the standard workflow for a discovery project based on phenotypic screening [104] [105].
- Assay Development: A cellular or organismal model that robustly recapitulates the disease phenotype is established and validated for high-throughput use.
- Library Screening: A diverse chemical library, often containing hundreds of thousands to millions of compounds, is screened against the assay in a High-Throughput Screening (HTS) operation.
- Hit Identification: Compounds that produce a statistically significant desired effect ("hits") are identified and confirmed in dose-response experiments.
- Lead Generation: Confirmed hits are evaluated for drug-likeness (e.g., using "Lipinski's Rule of Five"), and a chemical lead series is selected for optimization. The molecular target is often still unknown at this stage.
- Target Deconvolution: Efforts are made to identify the mechanism of action of the lead series, which can be a major bottleneck using techniques like affinity chromatography or genetic approaches.
- Iterative Optimization: Medicinal chemists synthesize analogs of the lead compound, which are tested in iterative cycles to improve potency, selectivity, and pharmacokinetic properties—a process often described as "make-test" [104].
Protocol for a Structure-Based Rational Drug Design Campaign
This protocol details a modern RDD workflow, emphasizing computational guidance [106] [105].
- Target Identification & Validation: A biomolecular target is selected based on genetic, proteomic, and clinical evidence of its critical role in the disease. AI and NLP can accelerate this by analyzing vast scientific literature and omics data [104].
- Structure Determination: The three-dimensional structure of the target, often with a bound native ligand, is determined via X-ray crystallography or Cryo-EM, or modeled via homology.
- Virtual Screening: Instead of physical HTS, computational docking of millions of purchasable compounds (e.g., from the ZINC database, containing over 750 million molecules) is performed against the target's binding site [106] [104].
- Hit Selection & Purchasing: A small subset (dozens to hundreds) of the top-ranking virtual hits is selected based on docking scores, interaction patterns, and predicted properties, and is then physically purchased for testing.
- Biochemical Assay: The purchased compounds are tested in a target-specific biochemical assay to confirm binding and functional activity, yielding a confirmed hit rate that is typically much higher than in traditional HTS.
- Structure-Guided Optimization: The 3D structures of the target bound to hit molecules are solved. Analogs are designed and optimized using graph-based methods and maximum common subgraph (MCS) analyses to explore chemical space and refine interactions, a more directed process than traditional iterative optimization [106].
Diagram 1: RDD Structure-Based Workflow
The Scientist's Toolkit: Essential Reagents and Solutions for RDD
The implementation of RDD relies on a suite of specialized computational and biological tools.
Table 3: Key Research Reagent Solutions for Rational Drug Design
| Tool / Reagent | Function / Description | Application in RDD |
|---|---|---|
| CHEMBL / PubChem | Public databases containing millions of bioactivity data points for molecules against protein targets [105]. | Target feasibility analysis, chemical starting point identification, model training for AI. |
| ZINC Database | A curated collection of over 750 million commercially available, "purchasable" compounds [106]. | Source of molecular structures for large-scale virtual screening campaigns. |
| Protein Data Bank (PDB) | Central repository for experimentally determined 3D structures of proteins, nucleic acids, and complexes [105]. | Source of structural data for target analysis, binding site definition, and structure-based design. |
| Scaffold Hunter | An open-source tool for visual analysis of chemical space based on molecular scaffolds [106]. | Navigation of structure-activity relationships, identification of novel chemotypes, and bioactivity data analysis. |
| Graph-Based Similarity Algorithms | Algorithms for computing molecular similarity based on Maximum Common Subgraph (MCS) rather than molecular fingerprints [106]. | More accurate molecular comparison and clustering, leading to fewer false positives in similarity searches. |
| AI/ML Models for QSAR | Machine learning models that predict biological activity based on quantitative structure-activity relationships [104] [105]. | Accelerated lead optimization and prediction of pharmacokinetic and toxicity properties. |
Visualization of Chemogenomic Data Analysis in RDD
Chemogenomics, a core component of modern RDD, involves the systematic mapping of chemical and target spaces. The following diagram illustrates the conceptual workflow and data structure for a chemogenomic analysis, which aims to fill the sparse compound-target interaction matrix by leveraging similarity in both ligand and target spaces [105].
Diagram 2: Chemogenomics Workflow
The comparative analysis unequivocally demonstrates that principles of Rational Drug Design are central to overcoming the profound efficiency challenges in pharmaceutical R&D. The data reveals that traditional methods, hampered by high attrition and cost, are becoming increasingly unsustainable. In contrast, RDD methodologies—powered by chemoinformatics, structural biology, and artificial intelligence—offer a transformative path forward. By enabling target-driven discovery, accelerated timelines, and more informed decision-making, RDD significantly de-risks the drug development process. The successful application of graph-based similarity searches, chemogenomic data mining, and AI-driven predictive models directly addresses the industry's need for higher success rates and improved R&D productivity. For researchers and drug development professionals, the integration of these rational principles is not merely an optimization of existing processes but a strategic imperative for delivering the next generation of innovative therapies in an increasingly challenging economic and scientific landscape.
Evaluating the Impact of RDD on Development Timelines and Costs
Rational Drug Design (RDD) represents a fundamental shift in the pharmaceutical industry, moving away from serendipitous discovery toward a targeted, knowledge-driven process of developing new medications. By definition, RDD is the inventive process of finding new medications based on knowledge of a biological target, designing molecules that are complementary in shape and charge to the biomolecular target with which they interact [9]. This approach stands in contrast to traditional phenotypic drug discovery, which relies on observing therapeutic effects without prior knowledge of the specific biological target [9].
The contemporary pharmaceutical landscape faces significant productivity challenges, making RDD increasingly critical. Currently, there are over 23,000 drug candidates in development, yet R&D productivity has been declining sharply. The success rate for Phase 1 drugs has plummeted to just 6.7% in 2024, compared to 10% a decade ago, while the internal rate of return for R&D investment has fallen to 4.1% – well below the cost of capital [107]. Within this challenging environment, RDD, particularly when augmented with artificial intelligence, offers a promising path forward by systematically reducing attrition rates and optimizing resource allocation throughout the drug development pipeline.
The Productivity Challenge in Pharmaceutical R&D
Current R&D Landscape and Economic Pressures
The biopharmaceutical industry is operating at unprecedented levels of R&D activity with over 10,000 drug candidates in various stages of clinical development [107]. This expansion is supported by substantial annual R&D investment exceeding $300 billion, supporting an industry revenue projected to grow at a 7.5% compound annual growth rate (CAGR), reaching $1.7 trillion by 2030 [107]. However, this robust top-line growth masks significant underlying pressures.
Despite increasing revenue projections, research budgets are not keeping pace with expansion. R&D margins are expected to decline significantly from 29% of total revenue down to 21% by the end of the decade [107]. This margin compression results from three intersecting factors: the shrinking commercial performance of the average new drug launch, rising costs per new drug approval, and increasing pipeline attrition rates that further drive up development costs.
Quantitative Analysis of Drug Development Efficiency
Table 1: Key Metrics Highlighting the Pharmaceutical R&D Productivity Challenge
| Metric | Current Value (2024-2025) | Historical Comparison | Impact on Development Costs |
|---|---|---|---|
| Phase 1 Success Rate | 6.7% | 10% a decade ago | Increases cost per approved drug due to high failure rate |
| R&D Internal Rate of Return | 4.1% | Well below cost of capital | Reduces available investment for innovative projects |
| R&D Margin | 21% (projected by 2030) | 29% previously | Constrains budget allocation for research activities |
| Annual R&D Spending | >$300 billion | Supporting 23,000 drug candidates | Increases financial burden with diminishing returns |
The data reveals a sector facing fundamental efficiency challenges. The declining success rate in early development phases is particularly concerning, as Phase 1 failures represent the earliest and traditionally least expensive points of attrition. When failure occurs this frequently in early stages, it increases the aggregate cost per approved drug substantially, as the expenses of both failed and successful candidates must be recouped through marketed products [107].
Fundamental Principles of Rational Drug Design
RDD operates on the principle of leveraging detailed knowledge of biological targets to design interventions with predictable effects. This approach encompasses several key methodologies:
Structure-Based Drug Design
Structure-based drug design (SBDD), also known as receptor-based or direct drug design, relies on knowledge of the three-dimensional structure of the biological target obtained through methods such as X-ray crystallography or NMR spectroscopy [9]. The process involves designing molecules that are complementary in shape and charge to the target's binding site [5]. When the three-dimensional structure of the target protein is known, this information can be directly exploited for the retrieval and design of new ligands that make favorable interactions with the active site [5]. This approach provides a visual framework for direct design of new molecular entities and allows researchers to rapidly assess the validity of possible solutions.
Ligand-Based Drug Design
When the three-dimensional structure of the target is unavailable, ligand-based drug design (also known as pharmacophore-based or indirect drug design) provides an alternative approach. This method relies on knowledge of other molecules that bind to the biological target of interest to derive a pharmacophore model [9]. A pharmacophore defines the minimum necessary structural characteristics a molecule must possess to bind to the target, enabling the design of new molecular entities through molecular mimicry – positioning 3D structural elements recognized in active molecules into new chemical entities [5]. This approach guides the discovery process by starting with known active compounds as templates rather than the protein structure itself.
Synergistic Integration of Approaches
The most effective RDD strategies integrate both structure-based and ligand-based approaches. When information is available for both the target protein and active molecules, the synergy between approaches can substantially accelerate discovery [5]. For example, when a promising molecule is designed through docking studies, it can be compared to known active structures for validation. Conversely, when an interesting molecular mimic is considered, it can be docked into the protein structure to verify complementary interactions. This integrated global approach aims to identify structural models that rationalize biological activities based on interactions with the 3D target structure [5].
Diagram 1: RDD Methodological Workflow illustrating structure-based and ligand-based approaches
Impact of RDD on Development Timelines and Costs
AI-Augmented RDD and Efficiency Gains
The integration of artificial intelligence with RDD methodologies represents the most significant advancement in pharmaceutical development efficiency. By 2025, it is estimated that 30% of new drugs will be discovered using AI, with demonstrated capabilities to reduce drug discovery timelines and costs by 25-50% in preclinical stages [108]. This acceleration stems from AI's ability to rapidly identify potential drug candidates, predict efficacy, and optimize patient selection for clinical trials based on key datasets and biomarkers.
AI-driven models serve as powerful tools for optimizing clinical trial designs by identifying drug characteristics, patient profiles, and sponsor factors to design trials that are more likely to succeed [107]. This data-driven approach ensures that every trial and potential participant counts, with studies designed as critical experiments with clear success or failure criteria rather than exploratory fact-finding missions [107]. The implementation of what industry leaders term "snackable AI" – AI used in day-to-day work – at scale improves decision-making patterns and augments human abilities without replacing employees [108].
Comparative Analysis: Traditional vs. RDD Approaches
Table 2: Impact of RDD and AI on Drug Development Efficiency
| Development Stage | Traditional Approach | RDD/AI-Augmented Approach | Efficiency Gain |
|---|---|---|---|
| Target Identification | 12-24 months | 3-6 months | 75% reduction in timeline |
| Lead Discovery | 24-36 months | 12-18 months | 50% reduction in timeline |
| Preclinical Development | 12-18 months | 6-12 months | 25-50% cost reduction |
| Clinical Trial Design | Historical controls & intuition | AI-optimized protocols | Higher success probability |
| Patient Recruitment | Broad inclusion criteria | Biomarker-targeted selection | Improved trial efficiency |
The efficiency gains demonstrated by AI-augmented RDD directly address the productivity crisis highlighted in Section 2. By reducing late-stage attrition through better target validation and compound selection, these approaches fundamentally improve the economics of pharmaceutical R&D. The ability to identify unsuccessful therapies earlier and shift resources away from them represents a fundamental competitive advantage in portfolio management [108].
Regulatory Pathway Optimization
RDD methodologies also enable more effective utilization of expedited regulatory pathways. In 2024, the FDA granted 24 accelerated approvals and label expansions, providing significant cost-saving opportunities for drug developers [107]. However, to qualify for accelerated approval, R&D timelines must adhere to the FDA's stringent confirmatory trial requirements, including target completion dates, evidence of "measurable progress," and proof that patient enrollment has already begun.
The case of Regeneron's CD20xCD3 bispecific antibody, which was rejected for accelerated approval due to failure to meet confirmatory trial criteria, illustrates the importance of balancing speed with rigorous evidence generation [107]. RDD approaches facilitate this balance by generating more robust early-stage data that supports both initial approval and confirmatory trial requirements.
Experimental Frameworks and Methodologies
Integrated RDD Experimental Protocol
Objective: To systematically identify and optimize lead compounds targeting a defined biological target using integrated rational drug design approaches.
Methodology:
Target Validation and Characterization
- Utilize genomic and proteomic data to confirm disease modification capability of selected target
- Express, purify, and characterize the target biomolecule (protein/nucleic acid)
- Develop robust binding and functional assays for compound screening
Structure-Based Design Arm
- Determine three-dimensional structure of target via X-ray crystallography or cryo-EM
- Identify and characterize binding sites through computational cavity detection
- Perform virtual screening of compound libraries using molecular docking
- Execute de novo ligand design focusing on complementary stereochemistry
Ligand-Based Design Arm
- Curate dataset of known active and inactive compounds from literature and patents
- Develop pharmacophore model defining essential structural features for activity
- Conduct Quantitative Structure-Activity Relationship (QSAR) analysis
- Design novel compounds using molecular mimicry principles
Integrated Lead Optimization
- Synthesize prioritized lead compounds from both approaches
- Evaluate binding affinity and functional activity in biochemical assays
- Assess selectivity against antitargets to minimize side effects
- Optimize drug-like properties (ADME-Tox) using predictive models
Experimental Validation
- Conduct in vitro and in vivo efficacy studies in disease-relevant models
- Perform preclinical toxicology and safety pharmacology assessment
- Advance optimized candidates to clinical development
Research Reagent Solutions
Table 3: Essential Research Reagents for RDD Experimental Protocols
| Reagent/Category | Function in RDD Process | Specific Application Examples |
|---|---|---|
| Protein Expression Systems | Production of purified biological targets for structural studies | Bacterial, insect, mammalian cell systems for recombinant protein production |
| Crystallization Screening Kits | Facilitate 3D structure determination of target proteins | Commercial sparse matrix screens for initial crystallization condition identification |
| Compound Libraries | Source of chemical starting points for screening | Diverse synthetic compounds, natural products, fragment libraries for virtual and HTS |
| Pharmacophore Modeling Software | Identification of essential structural features for bioactivity | Computer-aided molecular design platforms for 3D pharmacophore development |
| Molecular Dynamics Software | Simulation of binding interactions and conformational changes | Analysis of protein-ligand complex stability and residence times |
| ADME-Tox Prediction Platforms | Early assessment of drug-like properties | In silico prediction of metabolic stability, permeability, and toxicity liabilities |
Comparative Analysis of Development Pathways
Diagram 2: Development Pathway Efficiency comparison between approaches
Rational Drug Design represents a transformative approach to pharmaceutical development that directly addresses the sector's pressing productivity challenges. By leveraging precise knowledge of biological targets and their interactions with potential therapeutics, RDD enables more efficient resource allocation, reduced development timelines, and improved success rates across the drug development pipeline. The integration of artificial intelligence with traditional RDD methodologies further amplifies these benefits, potentially reducing preclinical discovery timelines and costs by 25-50% [108].
The documented decline in R&D productivity, characterized by Phase 1 success rates of just 6.7% and internal rates of return falling to 4.1%, underscores the critical need for more efficient approaches [107]. RDD addresses these challenges through target-driven discovery that minimizes late-stage attrition – the most significant cost driver in pharmaceutical development. Furthermore, the methodology supports more effective utilization of regulatory acceleration pathways by generating more robust early-stage data.
As the industry approaches the largest patent cliff in history, with an estimated $350 billion of revenue at risk between 2025 and 2029, the efficient replenishment of product portfolios becomes increasingly strategic [107]. Rational Drug Design, particularly when augmented with artificial intelligence and machine learning, provides a framework for rebuilding pipelines more efficiently and predictably. By combining more efficient R&D processes with strategic portfolio management and thoughtful trial design, pharmaceutical companies can not only survive the coming challenges but position themselves for sustained success in an increasingly competitive landscape [107].
Conclusion
Rational Drug Design represents a paradigm shift in pharmaceuticals, moving from serendipitous discovery to a deliberate, knowledge-driven process. By integrating foundational biology with advanced computational methods, RDD significantly enhances the efficiency and precision of developing new therapeutics. While challenges in predicting binding affinity, optimizing pharmacokinetics, and ensuring specificity remain, ongoing advancements in computational power, structural biology techniques like cryo-EM, and machine learning are rapidly expanding the frontiers of what is possible. The future of RDD lies in increasingly multidisciplinary approaches, incorporating genomics and proteomics data more deeply to create personalized medicines and tackle previously undruggable targets. This evolution promises to accelerate the delivery of safer, more effective treatments to patients, fundamentally shaping the future of biomedical research and clinical practice.
References
- 1. From Patterns to Pills: How Informatics Is Shaping Medicinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114992/]
- 2. Structural bioinformatics for rational drug design [https://www.sciencedirect.com/science/article/pii/S2475037925000159]
- 3. Artificial intelligence for drug target identification [https://www.sciencedirect.com/science/article/pii/S0065774325000028]
- 4. Fundamental considerations in drug design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9212230/]
- 5. Principles of Rational Drug Design [https://drugdesign.org/chapters/drug-design/]
- 6. Recent advances in targeting the “undruggable” proteins [https://www.nature.com/articles/s41392-023-01589-z]
- 7. New strategies to enhance the efficiency and precision of drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11850385/]
- 8. Retro Drug Design: From Target Properties to Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8132216/]
- 9. Drug design [https://en.wikipedia.org/wiki/Drug_design]
- 10. Understanding the Step-by-Step Process of Rational Drug ... [https://parssilico.com/blogs/90-step-by-step-process-of-rational-drug-design]
- 11. Structure-Based Drug Design [https://selvita.com/drug-discovery/small-molecules/expertise-areas/cadd/structure-based-drug-design]
- 12. Principles of early drug discovery - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3058157/]
- 13. Top 5 Drug Discovery Trends 2025 Driving Breakthroughs [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/drug-discovery-trends-2025/]
- 14. Development of quantitative structure-activity relationships ... [https://pubmed.ncbi.nlm.nih.gov/17168765/]
- 15. Rational drug design: How far have we come? [https://www.europeanpharmaceuticalreview.com/article/71221/rational-drug-design/]
- 16. Reverse pharmacology [https://en.wikipedia.org/wiki/Reverse_pharmacology]
- 17. Target Identification vs. Phenotypic Screening in Drug ... [https://pharmafeatures.com/strategic-dichotomy-target-identification-vs-phenotypic-screening-in-drug-discovery/]
- 18. Phenotypic Drug Discovery: Recent successes, lessons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9708951/]
- 19. Opportunities and challenges in phenotypic drug discovery [https://www.nature.com/articles/nrd.2017.111]
- 20. Current progress in Structure-Based Rational Drug Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3962124/]
- 21. Discovery and resupply of pharmacologically active plant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4748402/]
- 22. Drug Design—Past, Present, Future - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8911833/]
- 23. the emergence of rational drug design in ... [https://www.sciencedirect.com/science/article/abs/pii/S1369848605000488]
- 24. Rational drug design: How far have we come? [https://www.drugtargetreview.com/article/28498/rational-drug-design/]
- 25. Success Stories in Drug Discovery [https://drugdesign.org/chapters/success-stories-in-drug-discovery/]
- 26. Brivaracetam: a rational drug discovery success story - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2518467/]
- 27. Success story of Rational Drug Discovery [https://www.linkedin.com/pulse/success-story-rational-drug-discovery-dr-bandoo-chatale-bzlkf]
- 28. NMR-driven structure-based drug discovery by unveiling ... [https://www.nature.com/articles/s42004-025-01542-x]
- 29. Structure-Based Drug Design Summit: Home [https://structure-based-drug-design-summit.com/]
- 30. What Ails Generative Structure-based Drug Design [https://arxiv.org/html/2408.06050v1]
- 31. Computational ligand-based rational design: Role of ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3123535/]
- 32. Structure and dynamics in drug discovery [https://www.nature.com/articles/s44386-024-00001-2]
- 33. A (Comprehensive) Review of the Application of Quantitative Structure–Activity Relationship (QSAR) in the Prediction of New Compounds with Anti-Breast Cancer Activity [https://www.mdpi.com/2076-3417/15/3/1206]
- 34. Frontiers | Ligand-based pharmacophore modeling and QSAR approach to identify potential dengue protease inhibitors [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2023.1106128/full]
- 35. Virtual Screening, Molecular Docking and QSAR Studies in ... [https://jddtonline.info/index.php/jddt/article/view/4218]
- 36. AI-Integrated QSAR Modeling for Enhanced Drug Discovery: From Classical Approaches to Deep Learning and Structural Insight [https://www.mdpi.com/1422-0067/26/19/9384]
- 37. Ligand-based drug design of quinazolin-4(3H)-ones as breast cancer inhibitors using QSAR modeling, molecular docking, and pharmacological profiling | Journal of the Egyptian National Cancer Institute | Full Text [https://jenci.springeropen.com/articles/10.1186/s43046-023-00182-3]
- 38. Recent advances in ligand-based drug design: relevance and utility of the conformationally sampled pharmacophore approach - PubMed [https://pubmed.ncbi.nlm.nih.gov/20807187/]
- 39. Computer-Aided Drug Design and Drug Discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11946204/]
- 40. Computer-aided drug design for virtual-screening and active ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10661973/]
- 41. Computer-Aided Drug Design: QSAR, Molecular Docking ... [https://www.amazon.com/Computer-Aided-Drug-Design-Molecular-Pharmacophore/dp/3111434745]
- 42. High Throughput Screening (HTS) Market Size 2025-2029 [https://www.technavio.com/report/high-throughput-screening-market-industry-analysis]
- 43. How GPUs Can Accelerate High Throughput Screening ... [https://www.exxactcorp.com/blog/molecular-dynamics/how-gpus-can-accelerate-high-throughput-screening-research]
- 44. High Throughput Screening Market Market 2025: Artificial ... [https://www.linkedin.com/pulse/high-throughput-screening-market-2025-artificial-4x9vf/]
- 45. Fragment-Based Drug Discovery | April 15-16, 2025 [https://www.drugdiscoverychemistry.com/25/fragment-based-drug-discovery]
- 46. Fragment-Based Drug Design: From Then until Now, and ... [https://pubmed.ncbi.nlm.nih.gov/39992814/]
- 47. Advances in high-throughput drug screening based on ... [https://pubmed.ncbi.nlm.nih.gov/40945847/]
- 48. Discovery and development of HIV-protease inhibitors [https://en.wikipedia.org/wiki/Discovery_and_development_of_HIV-protease_inhibitors]
- 49. Development of Anti-HIV Therapeutics: From Conventional ... [https://www.mdpi.com/1424-8247/17/7/887]
- 50. A Case Study on a Potent HIV-1 Protease Inhibitor [https://pmc.ncbi.nlm.nih.gov/articles/PMC4518107/]
- 51. Inhibition of the activity of HIV-1 protease through antibody ... [https://www.nature.com/articles/s41598-020-62423-y]
- 52. The Synthetic Molecule RDD-142 Delays Cell Cycle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610667/]
- 53. Gilead Presents New HIV Research Data at EACS 2025 [https://www.gilead.com/news/news-details/2025/gilead-presents-new-hiv-research-data-at-eacs-2025--driving-scientific-innovation-in-treatment-and-prevention]
- 54. Budigalimab, an anti-PD-1 inhibitor, for people living with ... [https://www.nature.com/articles/s41591-025-03993-0]
- 55. Target Flexibility: An Emerging Consideration in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2701403/]
- 56. Review Target flexibility in molecular recognition [https://www.sciencedirect.com/science/article/abs/pii/S157096390500302X]
- 57. Modeling solvation effects on absorption and fluorescence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7878019/]
- 58. Computational methods revolutionize drug discovery by ... [https://www.eurekalert.org/news-releases/1105281]
- 59. Computational approaches streamlining drug discovery [https://www.nature.com/articles/s41586-023-05905-z]
- 60. Solvent model [https://en.wikipedia.org/wiki/Solvent_model]
- 61. 15.2 Explicit solvent models and QM/MM approaches [https://fiveable.me/computational-chemistry/unit-15/explicit-solvent-models-qmmm-approaches/study-guide/qTX1EJuvhy64u3Me]
- 62. Advancements in Rational Drug Design [https://www.longdom.org/open-access/advancements-in-rational-drug-design-strategies-and-applications-in-therapeutic-development-1102694.html]
- 63. Lead Optimization in Drug Discovery [https://chem-space.com/news/chemspace-lead-otimization]
- 64. Hit-To-Lead | Drug Discovery [https://www.sygnaturediscovery.com/drug-discovery/integrated-drug-discovery/hit-to-lead/]
- 65. Hit to Lead Assays: Accelerating Early Drug Discovery [https://bellbrooklabs.com/hit-to-lead-assays/?srsltid=AfmBOooOdqwPZMn7tfXWSOYaWmUYeZzUNzypAsGTOHHFcFKrfFaFm_mv]
- 66. Progress of AI-Driven Drug–Target Interaction Prediction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563295/]
- 67. Lead Generation Strategies | 11-12 November 2025 [https://www.drugdiscoverychemistry.com/europe/lead-generation-strategies]
- 68. Innovative Breakthroughs in ADME Toxicology: Paving the Way for Safer Drug Development - Cell4Pharma [https://cell4pharma.com/innovative-breakthroughs-in-adme-toxicology/]
- 69. ADMET Predictor® Modules [https://www.simulations-plus.com/software/admetpredictor/]
- 70. Chapter 1 Pharmacokinetics & Pharmacodynamics - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK595006/]
- 71. Introduction to Pharmacokinetics: Four Steps in a Drug's ... [https://genomind.com/providers/introduction-to-pharmacokinetics-four-steps-in-a-drugs-journey-through-the-body/]
- 72. A beginners guide to ADME Tox [https://www.cellgs.com/blog/a-beginners-guide-to-adme-tox.html]
- 73. Applications & Solutions - Drug Discovery - ADME/TOX [https://lifesciences.tecan.com/applications_and_solutions/drug_discovery/adme-tox]
- 74. New Features and Updates | Tox Suite Version 2025 [https://www.acdlabs.com/technical-support/current-software-versions/tox-suite/]
- 75. Why 90% of clinical drug development fails and how to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9293739/]
- 76. Quantitative Methods in System-Based Drug Discovery [https://www.intechopen.com/chapters/53186]
- 77. Off-target interactions in the CRISPR-Cas9 Machinery [https://pubmed.ncbi.nlm.nih.gov/40688512/]
- 78. Strategies to Avoid and Reduce Off-Target Effects [https://crisprmedicinenews.com/news/strategies-to-avoid-and-reduce-off-target-effects/]
- 79. Derisking strategy to mitigate off-target liability at hERG for ... [https://www.sciencedirect.com/science/article/pii/S1056871925002849]
- 80. New method of designing drugs without side effects [https://www.drugtargetreview.com/news/110167/new-method-of-designing-drugs-without-side-effects/]
- 81. Applications of Artificial Intelligence in Biotech Drug Discovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308071/]
- 82. Multi-and many-objective optimization: present and future ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2023.1288626/full]
- 83. Multi-objective drug design with a scaffold-aware variational ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d4sc08736d]
- 84. CMOMO: a deep multi-objective optimization framework for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12240737/]
- 85. Integrating transformers and many-objective optimization for ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-024-05822-6]
- 86. New In Vitro-In Silico Approach for the Prediction of In Vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8304213/]
- 87. In vitro – in silico – in vivo drug absorption model ... [https://www.sciencedirect.com/science/article/abs/pii/S0928098714002590]
- 88. Machine Learning at Scale: Why PySpark MLlib Still Wins ... [https://towardsai.net/p/artificial-intelligence/machine-learning-at-scale-why-pyspark-mllib-still-wins-in-2025]
- 89. A standardized analytics pipeline for reliable and rapid ... [https://www.sciencedirect.com/science/article/pii/S0169260721004685]
- 90. Design of tables for the presentation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10346464/]
- 91. Understanding the anatomy and proper construction of tables [https://www.decisionfoundry.com/misc/articles/understanding-the-anatomy-and-proper-construction-of-tables/]
- 92. How RWD is Transforming Clinical Trials in 2025 [https://www.linkedin.com/posts/patrick-saunders-hastings-45873b70_clinicaltrials-realworlddata-rwd-activity-7372272671193174016-vXfs]
- 93. 2025 R&D and Quality Predictions: Process Excellence ... [https://www.veeva.com/blog/2025-rd-and-quality-predictions-process-excellence-removes-barriers-speeds-connections/]
- 94. Preclinical Studies in Drug Development [https://www.ppd.com/what-is-a-cro/preclinical-studies-in-drug-development/]
- 95. Rational Drug Design - an overview [https://www.sciencedirect.com/topics/psychology/rational-drug-design]
- 96. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 97. Regulatory Affairs 101: Introduction to Investigational New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6662388/]
- 98. Dose Escalation Methods in Phase I Cancer Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC2684552/]
- 99. FDA Advances Rare Disease Drug Development with New ... [https://www.fda.gov/news-events/press-announcements/fda-advances-rare-disease-drug-development-new-evidence-principles]
- 100. The efficacy of new drug regimens in treating newly ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1575914/full]
- 101. Guidance Documents for Rare Disease Drug Development [https://www.fda.gov/drugs/guidances-drugs/guidance-documents-rare-disease-drug-development]
- 102. RDD Europe 2025: Connect with the Intertek team in Lisbon [https://www.intertek.com/pharmaceutical/events/respiratory-drug-delivery/]
- 103. RDD Europe 2025 [https://www.hovione.com/press-room/events/rdd-europe-2025]
- 104. Revitalizing the Pharmaceutical R&D Pipeline [https://www.drugpatentwatch.com/blog/reviving-an-rd-pipeline/?srsltid=AfmBOopgT-HH-dEOrOFJkZEyOV1CKGExK791g_CsW__aNGiffnXsdQZu]
- 105. Chemogenomic approaches to rational drug design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1978269/]
- 106. Graph-Based Methods for Rational Drug Design [https://link.springer.com/chapter/10.1007/978-3-031-21534-6_5]
- 107. Biopharma RD Faces Productivity And Attrition Challenges ... [https://www.clinicalleader.com/doc/biopharma-r-d-faces-productivity-and-attrition-challenges-in-2025-0001]
- 108. How 2025 can be a pivotal year of progress for pharma [https://www.weforum.org/stories/2025/01/2025-can-be-a-pivotal-year-of-progress-for-pharma/]