Overcoming Poor Metabolic Stability in Drug Discovery: Strategies, Assays, and Future Directions
Poor metabolic stability remains a major cause of failure in drug development, leading to unfavorable pharmacokinetics, low bioavailability, and rapid clearance.
Overcoming Poor Metabolic Stability in Drug Discovery: Strategies, Assays, and Future Directions
Abstract
Poor metabolic stability remains a major cause of failure in drug development, leading to unfavorable pharmacokinetics, low bioavailability, and rapid clearance. This article provides a comprehensive guide for researchers and drug development professionals on navigating these challenges. It covers the foundational principles of drug metabolism, details the core in vitro assays—from liver microsomes to hepatocytes—used to assess metabolic stability, and presents practical strategies for lead optimization through structural modification. Furthermore, it addresses troubleshooting common pitfalls, explores advanced predictive models, including machine learning, and emphasizes the importance of cross-species and in vitro-in vivo correlation for successful candidate selection and translation to human outcomes.
Understanding Metabolic Stability: Why It's a Critical Gatekeeper in Drug Development
Defining Metabolic Stability and Its Impact on Pharmacokinetics
For researchers in drug development, metabolic stability is not just a biochemical concept but a critical determinant of a compound's success. It refers to a drug candidate's susceptibility to biotransformation by the body's metabolic enzymes, primarily in the liver [1] [2]. This property directly impacts key pharmacokinetic (PK) parameters, including half-life ((t_{1/2})), clearance, and oral bioavailability [1] [3]. A compound with poor metabolic stability is rapidly broken down, often failing to achieve and maintain the systemic exposure necessary for therapeutic efficacy [2]. This guide provides troubleshooting support for the in vitro assays that are foundational to optimizing metabolic stability early in the discovery process.
Frequently Asked Questions (FAQs)
1. What is metabolic stability and why is it a primary concern in lead optimization? Metabolic stability measures how resistant a compound is to enzymatic breakdown. It is a primary concern because it dictates the duration and intensity of a drug's pharmacological action [1] [2]. A metabolically unstable compound will have a short half-life and high clearance, leading to low systemic exposure and poor bioavailability [3]. This often necessitates frequent or high dosing, which can inconvenience patients and increase the risk of side effects [2]. Optimizing stability during lead optimization is therefore crucial for selecting candidates with a higher probability of in vivo success.
2. Our lead compound shows high intrinsic clearance in liver microsomes. What are the first investigative steps? High intrinsic clearance indicates rapid metabolic degradation. The first step is to identify the soft spots—the specific parts of the molecule undergoing metabolism. This involves Metabolite Identification (MetID) studies [4]. Incubate your compound with liver microsomes (or hepatocytes) and use LC-MS/MS to identify the structures of the major metabolites. Understanding the chemical transformation (e.g., hydroxylation, dealkylation) provides direct clues for rational structural modification to block these vulnerable sites [4].
3. We observe a significant discrepancy between in vitro metabolic stability and in vivo clearance. What are the common causes? This is a frequent challenge in PK scaling. Common causes include:
- Ignoring Extrahepatic Metabolism: Liver-focused assays may miss metabolism in other organs like the intestine, lung, or kidney [5]. Consider running stability assays with subcellular fractions from these tissues.
- Overlooking Non-Microsomal Enzymes: Liver microsomes are rich in Cytochrome P450 (CYP) enzymes but contain fewer Phase II enzymes. The contribution of cytosolic enzymes like aldehyde oxidase (AO) may be significant for your compound [5]. Confirmatory assays in liver cytosol or S9 fractions are recommended.
- Poor Prediction of Transport: In vitro systems may not fully replicate the complex interplay between drug-metabolizing enzymes and transporters (e.g., P-glycoprotein), which can greatly influence hepatic uptake and clearance in vivo [1].
4. When should we use hepatocytes over liver microsomes for stability assessment? The choice depends on the metabolic pathway of interest. Liver microsomes are ideal for a focused study on Phase I metabolism, particularly CYP450-mediated reactions [5]. Hepatocytes, being intact cells, contain a full complement of both Phase I and Phase II enzymes (e.g., UGTs, SULTs) and more closely mimic the physiological environment of the liver [5]. Use hepatocytes when you need a comprehensive view of a compound's metabolic fate or when microsomal data does not correlate well with in vivo observations.
5. How can we rapidly screen a large compound library for metabolic stability? Traditional LC-MS/MS methods can be a bottleneck for large libraries. Consider a high-throughput, single time-point substrate depletion assay in 96- or 384-well format, where the percent of parent compound remaining after a short incubation (e.g., 15-30 minutes) is measured [6]. This approach efficiently classifies compounds as stable or unstable for prioritization. Emerging technologies like the Metabolizing Enzyme Stability Assay Plate (MesaPlate) also offer a fluorescence-based method to quantify metabolic stability by tracking NADPH and oxygen depletion, which can offer higher throughput [7].
Troubleshooting Common Experimental Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| Unexpectedly High Compound Remaining | - Loss of enzyme activity due to improper storage/thawing.- Inadequate cofactor concentration. | - Confirm microsomes/hepatocytes are stored at ≤ -70°C and thawed on ice.- Verify fresh preparation of NADPH regenerating system. |
| High Variability Between Replicates | - Inconsistent protein concentration across wells.- Poor solubility of the test compound leading to precipitation. | - Pipette enzymes and cofactors carefully; pre-mix reagents where possible.- Ensure compound is soluble in incubation buffer; consider minimal, uniform DMSO concentration (<0.1-1%). |
| No Depletion in Microsomes, but Rapid Loss in Hepatocytes | - Metabolism is primarily driven by Phase II enzymes or cytosolic enzymes (e.g., AO). | - Follow up with assays in liver cytosol or S9 fractions to identify the involved pathway [5]. |
| Poor Correlation with In Vivo PK | - In vitro system misses key elements (e.g., transporters, extrahepatic metabolism). | - Perform reaction phenotyping to identify specific enzymes involved [4].- Investigate stability in extrahepatic tissue preparations [5]. |
Essential Experimental Protocols and Data Interpretation
Standard Liver Microsomal Stability Assay
This is the workhorse assay for initial metabolic stability screening [8] [6].
Detailed Methodology:
- Incubation System: The typical 100 µL incubation mixture contains:
- 0.5 - 1.0 mg/mL liver microsomal protein (rat, dog, human) [8] [6].
- 1.0 µM test compound (final concentration) [6].
- NADPH Regenerating System: 0.650 mM NADP+, 1.65 mM Glucose-6-phosphate, 1.65 mM MgCl₂, and 0.2 unit/mL Glucose-6-phosphate dehydrogenase [6].
- 100 mM Potassium Phosphate Buffer, pH 7.4 [6].
- Procedure:
- Pre-incubate the mixture (without NADPH) for 5 minutes at 37°C.
- Initiate the reaction by adding the NADPH regenerating system.
- At predetermined time points (e.g., 0, 5, 15, 30, 45 minutes), withdraw an aliquot and quench the reaction with a chilled organic solvent (e.g., acetonitrile) containing an internal standard.
- Centrifuge to precipitate proteins and analyze the supernatant using LC-MS/MS to quantify the remaining parent compound [6].
- Data Analysis: The natural logarithm of the percent remaining is plotted against time. The slope of the linear phase is used to calculate the in vitro half-life ((t{1/2})) and intrinsic clearance ((CL{int})) using the following equations [8]:
- (t_{1/2} = \frac{0.693}{k}) where (k) is the elimination rate constant (-slope).
- (CL{int} = \frac{0.693}{t{1/2}} \times \frac{\text{mL incubation}}{\text{mg microsomal protein}})
Quantitative Comparison of Metabolic Stability Assays
The table below summarizes the applications and components of key in vitro systems.
| Assay System | Key Enzymes Covered | Primary Application | Data Output |
|---|---|---|---|
| Liver Microsomes [5] | CYP450s, FMO, UGTs | Focused assessment of Phase I oxidative metabolism. | In vitro (t{1/2}), (CL{int}) |
| Liver S9 Fraction [5] | CYP450s, UGTs, SULTs, GSTs | Broader profile of both Phase I and Phase II metabolism. | In vitro (t{1/2}), (CL{int}) |
| Hepatocytes [5] | Full spectrum of Phase I and II enzymes | Most physiologically relevant system for overall hepatic clearance. | In vitro (t{1/2}), (CL{int}) |
| Liver Cytosol [5] | Aldehyde Oxidase (AO), GSTs, etc. | Identification of non-microsomal, cytosolic enzyme metabolism. | In vitro (t{1/2}), (CL{int}) |
Inter-Species Differences in Metabolic Stability
Data from a study on a PDE5 inhibitor candidate (NHPPC) highlights the importance of cross-species assessment [8].
| Species | % Remaining after 60 min | Intrinsic Clearance (mL/min/mg protein) |
|---|---|---|
| Rat | 42.8% | 0.0233 |
| Dog | 0.8% | 0.1204 |
| Human | 42.0% | 0.0214 |
Interpretation: In this case, the dog was a poor predictor of human metabolic stability, as it metabolized the compound much more rapidly. The rat model showed a clearance rate much closer to that of humans [8]. This underscores the need for careful species selection when extrapolating in vitro data to predict human PK.
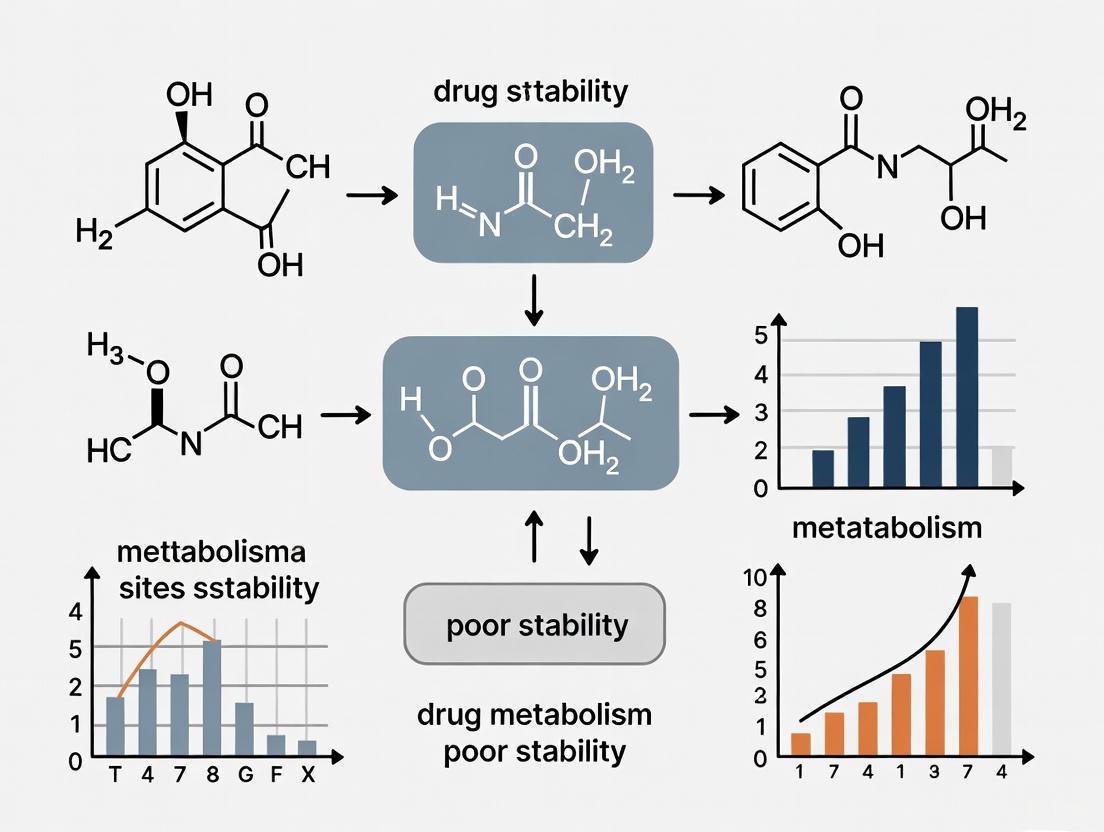
Experimental Workflow and Pathway Visualization
Metabolic Stability Assay Selection Pathway
This diagram outlines a logical decision pathway for selecting the appropriate metabolic stability assay based on research objectives.
In Vitro to In Vivo Prediction Workflow
This workflow charts the process of generating in vitro metabolic stability data and leveraging it to predict in vivo pharmacokinetic outcomes.
The Scientist's Toolkit: Key Research Reagents and Materials
| Reagent / Material | Function in Metabolic Stability Assays |
|---|---|
| Liver Microsomes [8] [6] | Subcellular fractions containing membrane-bound enzymes (CYP450s, UGTs) for assessing Phase I metabolism. |
| Cryopreserved Hepatocytes [5] | Intact liver cells containing a full suite of metabolic enzymes, providing the most physiologically relevant in vitro system. |
| NADPH Regenerating System [8] [6] | Provides a continuous supply of NADPH, the essential cofactor for CYP450-mediated oxidative reactions. |
| Potassium Phosphate Buffer (pH 7.4) [8] [6] | Maintains a physiologically relevant pH for the enzymatic reactions during incubation. |
| LC-MS/MS System [8] [4] | The gold-standard analytical platform for sensitive and specific quantification of parent compound depletion and metabolite identification. |
| Specific Chemical Inhibitors [4] | Used in reaction phenotyping to inhibit specific CYP450 enzymes (e.g., ketoconazole for CYP3A4) to identify metabolic pathways. |
FAQs: Understanding Metabolic Stability
What is metabolic stability and why is it a primary cause of clinical failure?
Metabolic stability refers to a drug candidate's susceptibility to biotransformation (breakdown) by the body's metabolic enzymes [2]. It is a critical determinant of a drug's pharmacokinetic profile, influencing how long a therapeutic remains active and at what concentration it reaches its target site [2] [1].
Poor metabolic stability is a major contributor to the high failure rate in clinical drug development. Analyses show that 40-50% of clinical failures are due to a lack of clinical efficacy, while 30% are due to unmanageable toxicity [9]. Both outcomes are directly linked to inadequate metabolic stability. A drug that is metabolized too quickly may not reach its target in sufficient concentrations to be effective, while a drug that forms reactive or toxic metabolites can cause serious safety issues [9] [2].
What are the key in vitro systems used to assess metabolic stability?
Researchers use several in vitro systems to predict a compound's metabolic fate. The table below summarizes the most common ones and their applications [5].
| In Vitro System | Components | Primary Metabolic Functions Assessed |
|---|---|---|
| Liver Microsomes | Subcellular fractions rich in membrane-bound enzymes [5] | Phase I metabolism (e.g., Cytochrome P450 (CYP) enzymes, FMO) [5] |
| Liver S9 Fraction | Contains both microsomal and cytosolic components [5] | Phase I and some Phase II metabolism (e.g., CYP, UGT, SULT) [5] |
| Hepatocytes | Whole liver cells [5] | Full complement of hepatic oxidative, reductive, and conjugative enzymes; considered the most physiologically relevant system [10] [5] |
| Liver Cytosol | Cytoplasmic fraction of liver cells [5] | Specific Phase II pathways and cytosolic enzymes (e.g., Aldehyde Oxidase) [5] |
Why do compounds with excellent target potency often fail in the clinic due to metabolism?
A primary reason is the historical overemphasis on Structure-Activity Relationship (SAR)—optimizing for high potency and specificity against the intended target—while underemphasizing Structure–Tissue Exposure/Selectivity Relationship (STR) [9]. A molecule can be perfectly designed to hit its target but fail if it is rapidly cleared from the systemic circulation or if it accumulates in vital organs, leading to toxicity [9]. The modern approach, termed Structure–Tissue Exposure/Selectivity–Activity Relationship (STAR), advocates for balancing potency with tissue exposure and selectivity to select candidates with a higher probability of clinical success [9].
What are "low-turnover" drugs and what special challenges do they present?
Low-turnover drugs are compounds that are metabolized very slowly [10]. A significant and growing proportion of drug candidates (up to 30% in some reports) fall into this category [10].
The core challenge is that standard metabolic stability assays have limited incubation times (e.g., ~1 hour for liver microsomes, ~4 hours for hepatocytes) due to the loss of enzyme activity [10]. For a slowly metabolized compound, there may be no detectable substrate depletion within this short window, making it impossible to calculate a reliable intrinsic clearance value [10]. This forces researchers to report a "less-than" value, which is not useful for differentiating between late-stage candidates or for predicting human pharmacokinetics with confidence [10].
Troubleshooting Guides for Common Scenarios
Scenario 1: In Vitro to In Vivo Translation - Poor Correlation Between Assays and Animal Models
Problem: Your compound shows favorable metabolic stability in human liver microsomes, but in vivo animal studies reveal rapid clearance and poor bioavailability.
Troubleshooting Steps:
- Verify the Model System: Liver microsomes primarily contain phase I oxidative enzymes. If your compound is cleared via non-microsomal pathways (e.g., by Aldehyde Oxidase in the cytosol) or through Phase II conjugation, the microsomal data will be misleading [5]. Action: Move to a more complete system, such as hepatocytes, which contain the full suite of hepatic metabolic enzymes [10] [5].
- Account for Extrahepatic Metabolism: The liver is the primary site of metabolism, but other organs can contribute significantly. Action: Conduct stability assays using subcellular fractions from other tissues, such as the intestine, lung, or kidney, to identify non-hepatic clearance routes [5] [11].
- Challenge the Animal Model: There are known physiological and metabolic differences between animals and humans, leading to weak correlations in bioavailability [11]. Action: Use allometric scaling from animal data with caution. Supplement your data with advanced human-relevant models, such as hepatocyte coculture systems (e.g., HepatoPac) or fluidically-linked multi-organ chips (e.g., gut-liver systems) that better simulate human first-pass metabolism [10] [11].
Scenario 2: The "Low-Turnover" Compound - Unable to Measure Intrinsic Clearance
Problem: Your promising candidate shows negligible depletion in standard human liver microsome and hepatocyte assays, preventing you from ranking it against other compounds or predicting its human half-life.
Troubleshooting Steps:
- Extend the Incubation Time: Standard hepatocyte suspension assays are limited to a few hours. Action: Employ specialized, longer-lived model systems:
- Hepatocyte Relay Method: The test compound is sequentially incubated with fresh hepatocytes over multiple days (e.g., 4 hours per day for up to 5 days), maintaining enzyme activity and allowing for measurable depletion of low-turnover drugs [10].
- Hepatocyte Coculture Systems (e.g., HepatoPac): These systems use hepatocytes cocultured with stromal cells to maintain metabolic function and stability for weeks, enabling accurate clearance measurements for even the most stable compounds [10].
- Shift to Metabolite Identification: If parent depletion is too slow to measure, focus on the products. Action: Use the extended incubation systems above to identify and quantify key metabolites. This reveals the primary clearance pathways and provides kinetic data (Vmax, Km) if authentic metabolite standards are available [10].
- Consider Alternative Clearance Pathways: The compound may be cleared predominantly by non-metabolic routes. Action: Investigate biliary and renal excretion pathways in relevant in vitro and in vivo models to build a complete picture of elimination [1].
Scenario 3: High Metabolic Lability - Rapid Clearance in All Systems
Problem: Your lead compound is rapidly degraded in all metabolic stability assays, indicating a very short projected half-life in humans.
Troubleshooting Steps:
- Identify the Metabolic Soft Spot: Action: Incubate the compound with liver microsomes or hepatocytes and use LC-MS/MS to identify the major metabolites. The structure of these metabolites will reveal which part of the molecule is vulnerable (e.g., a specific ester, methyl group, or aromatic ring) [2].
- Employ Structural Modification: Action: Use medicinal chemistry to block the identified soft spot. Common strategies include:
- Introducing metabolically stable moieties (e.g., replacing a hydrogen with a fluorine or deuterium) [2].
- Blocking labile functional groups (e.g., cyclizing a chain, changing a substituent) [2].
- Reducing lipophilicity (cLogP) to potentially make the compound a less favorable substrate for metabolic enzymes [12].
- Explore a Prodrug Strategy: If the rapid metabolism is due to poor solubility or permeability, a prodrug may be the solution. Action: Design a prodrug—an inactive derivative that is rapidly converted to the active parent drug in the body. This can improve oral absorption and bypass first-pass metabolism, effectively enhancing metabolic stability for the active moiety [2].
Quantitative Data on Clinical Failure and Metabolic Stability Assays
Primary Reasons for Clinical Attrition of Drug Candidates
The following data summarizes why drug candidates fail in clinical trials, with issues related to metabolism being a primary contributor to efficacy and toxicity failures [9].
| Reason for Failure | Proportion of Failures |
|---|---|
| Lack of Clinical Efficacy | 40% - 50% |
| Unmanageable Toxicity | ~30% |
| Poor Drug-Like Properties (e.g., PK, solubility) | 10% - 15% |
| Lack of Commercial Needs / Poor Strategic Planning | ~10% |
Key Parameters and Desired Profiles in Metabolic Stability Assessment
When profiling compounds, researchers measure specific parameters to assess their viability. The table below outlines common metrics and their desired values for a promising oral drug candidate [9].
| Pharmacokinetic Parameter | Description | Preferred Profile for a Lead Candidate |
|---|---|---|
| Microsomal Stability (t₁/₂) | Time for parent drug concentration to reduce by half in liver microsomes | > 45-60 minutes [9] |
| Hepatocyte Stability | Measured intrinsic clearance from hepatocyte incubations | Low clearance value (enables differentiation for low-turnover drugs) [10] |
| Bioavailability (F) | Fraction of administered drug that reaches systemic circulation | > 30% [9] |
| Half-Life (t₁/₂) | Time for drug concentration in plasma to reduce by half | > 4-6 hours (to support once- or twice-daily dosing) [9] |
| Volume of Distribution (V) | Theoretical volume in which a drug is distributed | Context-dependent; influences half-life along with clearance |
Experimental Protocols for Key Metabolic Stability Assays
Protocol 1: Metabolic Stability Assay Using Liver Microsomes
Objective: To determine the in vitro intrinsic clearance of a test compound via Phase I metabolism.
Materials:
- Test compound
- Human or animal liver microsomes
- NADPH (cofactor)
- Potassium phosphate buffer (pH 7.4)
- Magnesium chloride (MgCl₂)
- Acetonitrile (for termination)
- LC-MS/MS system for analysis
Method:
- Preparation: Pre-incubate liver microsomes (e.g., 0.5 mg/mL protein concentration) with test compound (e.g., 1 µM) in potassium phosphate buffer (100 mM, pH 7.4) containing MgCl₂ (3 mM) for 5 minutes at 37°C.
- Initiation: Start the reaction by adding NADPH (1 mM final concentration).
- Time Points: At predetermined time points (e.g., 0, 5, 15, 30, 45, 60 minutes), remove an aliquot of the incubation mixture and quench it with a cold volume of acetonitrile to precipitate proteins and stop the reaction.
- Analysis: Centrifuge the quenched samples, dilute the supernatant, and analyze the concentration of the parent compound remaining using LC-MS/MS.
- Data Calculation: Plot the natural logarithm of the parent compound's peak area versus time. The slope of the linear regression is the depletion rate constant (k). Intrinsic clearance (Cl₍ᵢₙₜ₎) is calculated as: Cl₍ᵢₙₜ₎ = k / (microsomal protein concentration).
Protocol 2: High-Throughput Metabolic Stability Screening with Automated Assessment
Objective: To screen a large number of compounds for metabolic stability with high efficiency and automated data quality control [12].
Materials:
- All materials from Protocol 1
- Ultra-Performance Liquid Chromatography (UPLC) system coupled to a tandem mass spectrometer (UPLC/MS/MS)
- Automated liquid handler
- Custom software for data processing (e.g., Visual Basic program)
Method:
- Cassette Grouping: To increase throughput, compounds are pooled (cassetted) for analysis. A smart pooling strategy is used, grouping compounds based on their calculated Log D (c Log D₃.₀) values, as this parameter correlates well with chromatographic retention time. This minimizes the risk of peak co-elution and ion suppression [12].
- Discrete Incubation: Compounds are incubated discretely (individually) with liver microsomes and NADPH, as described in Protocol 1.
- Post-Incubation Pooling: After incubation, samples from different compounds (within the same c Log D group) are pooled into a single cassette for analysis.
- UPLC/MS/MS Analysis: The cassette samples are analyzed using a fast, high-resolution UPLC/MS/MS method.
- Automated QC and Re-analysis: A key feature of this workflow is automated data assessment. If the data for a compound in the cassette does not meet pre-defined quality criteria (e.g., poor peak shape, low signal), the system automatically triggers a re-analysis of the original discrete sample. This ensures data quality is maintained despite the high-throughput nature of the screen [12].
The Scientist's Toolkit: Essential Research Reagents and Materials
| Tool / Reagent | Function in Metabolic Stability Research |
|---|---|
| Cryopreserved Hepatocytes | Gold-standard cell-based system containing a full complement of human metabolic enzymes for predicting in vivo clearance [10] [5]. |
| Liver Microsomes | Subcellular fractions used for high-throughput screening of Phase I metabolic lability, particularly Cytochrome P450-mediated metabolism [5]. |
| NADPH | Essential cofactor required for the catalytic cycle of Cytochrome P450 enzymes; used to initiate metabolic reactions in vitro [7]. |
| MesaPlate | A fluorescence-based assay plate that quantifies metabolic stability by measuring NADPH and oxygen depletion rates, offering an alternative to LC-MS/MS [7]. |
| Superoxide Dismutase & Catalase | Antioxidant enzymes added to incubation systems to simplify reaction kinetics by eliminating reactive oxygen species, enabling accurate calculation of substrate depletion [7]. |
| 1-Aminobenzotriazole | A broad-spectrum, mechanism-based inhibitor of Cytochrome P450 enzymes, used in reaction phenotyping to confirm CYP-mediated metabolism [7]. |
Experimental Workflows and Conceptual Frameworks
Workflow for High-Throughput Metabolic Stability Screening
The following diagram illustrates an automated, quality-controlled workflow for efficiently screening large compound libraries.
The STAR Framework for Candidate Selection
This diagram outlines the Structure–Tissue Exposure/Selectivity–Activity Relationship (STAR) matrix, a modern approach for classifying drug candidates to improve clinical success rates [9].
Frequently Asked Questions
What is the primary functional difference between Phase I and Phase II metabolism? Phase I reactions (e.g., oxidation, hydrolysis) primarily introduce or expose a functional group (-OH, -NH2, -COOH) to a molecule, often resulting in a modest increase in hydrophilicity and sometimes activating prodrugs or creating toxic intermediates [13] [14] [15]. Phase II reactions (conjugation) attach an endogenous, polar molecule (e.g., glucuronic acid, sulfate) to these groups, which typically significantly increases water solubility, inactivates the drug, and prepares it for excretion [13] [16] [14].
A common misconception is that Phase I must always precede Phase II. Is this accurate? No. While Phase I often provides a functional group for subsequent Phase II conjugation, many drugs bypass Phase I entirely if they already possess a suitable functional group (-OH, -NH2) and undergo direct Phase II metabolism [14] [15].
What does it mean if my compound shows rapid depletion in a human liver microsome (HLM) assay? A short half-life (t1/2) and high intrinsic clearance (CLint) in HLM assays indicate high metabolic instability [17] [18]. This often predicts low oral bioavailability and a short in vivo half-life, as the compound is extensively metabolized by the liver before it can reach its site of action [17].
How can I determine if a metabolite is pharmacologically active or toxic? Metabolites must be synthesized or isolated and then tested in relevant pharmacological and toxicological assays. In vitro studies using recombinant enzymes or specific enzyme inhibitors can help identify which enzyme system is responsible for producing the metabolite of interest [13] [19].
Why is metabolic stability a key parameter in early drug discovery? Compounds with poor metabolic stability are likely to have low bioavailability, short duration of action, and high inter-individual variability. Optimizing metabolic stability helps ensure adequate drug exposure for therapeutic efficacy and reduces the risk of failure in later, more costly development stages [18].
Our lab is new to oligonucleotide therapeutics. How does their metabolism differ from small molecules? Oligonucleotide metabolism differs significantly. They are primarily metabolized by nucleases (exo- and endo-nucleases) that cleave phosphodiester bonds, rather than the CYP450 system. Metabolites are typically chain-shortened sequences. Analysis requires specialized techniques like ion-pairing LC-MS to handle their high polarity and negative charge [20].
Troubleshooting Common Experimental Challenges
| Challenge | Possible Cause | Suggested Solution |
|---|---|---|
| Unexpectedly High Metabolic Stability | Lack of Phase II metabolism in microsomal system; Nonspecific binding to labware [18]. | Supplement HLMs with alamethicin and UDPGA for glucuronidation. Use coated plates or include bovine serum albumin (BSA) [18]. |
| In Vitro-In Vivo Correlation Failure | In vitro system lacks extrahepatic metabolism; Ignores transporter effects (Phase III) [14] [19]. | Use hepatocytes over microsomes; Incorporate transporter inhibition studies. |
| Inability to Identify Metabolites | Low metabolite abundance; Poor ionization; Complex matrix interference [17]. | Use high-resolution mass spectrometry (HRMS); Apply modern data mining software; Compare samples from matrix blanks. |
| High Variability in Replicate Samples | Compound instability in matrix; Inconsistent protein precipitation; Inadequate incubation temperature control [18]. | Ensure immediate sample processing; Validate sample extraction recovery; Use pre-warmed incubators and buffers. |
| Unexpectedly Low Metabolite Formation | Cofactor depletion; Enzyme inhibition by test compound; Incorrect pH of incubation buffer [13]. | Use fresh/replenished cofactors; Test for enzyme inhibition; Verify buffer pH and composition. |
Core Enzyme Systems at a Glance
Table 1: Key Characteristics of Major Phase I and Phase II Drug Metabolizing Enzymes
| Phase | Enzyme Family | Core Reaction | Primary Site | Key Cofactor(s) | Functional Outcome |
|---|---|---|---|---|---|
| Phase I | Cytochrome P450 (CYP) [14] | Oxidation, Reduction | Liver (ER) | NADPH, O2 | Introduces polar groups, can activate prodrugs or create reactive metabolites [13] [14]. |
| Phase I | Flavin-Containing Monooxygenase (FMO) [18] | Oxidation | Liver (ER) | NADPH, O2 | Oxidizes nucleophilic heteroatoms (N, S, P). |
| Phase II | UDP-glucuronosyltransferases (UGTs) [16] [14] | Glucuronidation | Liver, GI, Kidney | UDPGA | Major conjugation pathway; significantly increases hydrophilicity and targets compounds for biliary or renal excretion [13] [16]. |
| Phase II | Sulfotransferases (SULTs) [16] | Sulfation | Liver, GI, Platelets | PAPS | High-affinity, low-capacity conjugation; can be overwhelmed, leading to shunt to other pathways. |
| Phase II | Glutathione S-transferases (GSTs) [13] [16] | Glutathione Conjugation | Liver, Kidney | Glutathione (GSH) | Crucial detoxification of electrophilic compounds; protects against oxidative stress [13]. |
| Phase II | N-Acetyltransferases (NATs) [16] [14] | Acetylation | Liver, RBCs | Acetyl-CoA | Subject to genetic polymorphism (fast vs. slow acetylators), impacting drug toxicity and efficacy [14]. |
Table 2: Quantitative Metabolic Stability Parameters from a Model Study on Violacein [17]
| System | Half-life (t1/2, min) | In Vitro CLint (µL/min/mg) | In Vivo CLint (mL/min/kg) | Interpretation |
|---|---|---|---|---|
| Rat Liver Microsomes (RLMs) | 36 | 38.4 | 93.7 | Rapid elimination; low stability in this species. |
| Mouse Liver Microsomes (MLMs) | 81 | 17.0 | 67.0 | Moderate stability. |
| Human Liver Microsomes (HLMs) | 216 | 6.4 | 6.6 | Slowest elimination; highest stability, favorable for human dosing. |
Detailed Experimental Protocol: Metabolic Stability Assay in Liver Microsomes
This protocol is used to determine the in vitro half-life (t1/2) and intrinsic clearance (CLint) of a new chemical entity, assessing its susceptibility to Phase I and combined Phase I/II metabolism [18].
1. Principle The test compound is incubated with liver microsomes (human or animal) in the presence of cofactors. The depletion of the parent compound over time is monitored using Liquid Chromatography-Mass Spectrometry (LC-MS/MS). The rate of disappearance is used to calculate metabolic stability parameters [17] [18].
2. Materials and Reagents Table 3: Research Reagent Solutions for Metabolic Stability Assays
| Reagent / Material | Function / Explanation |
|---|---|
| Pooled Human/Rat/Mouse Liver Microsomes | Source of drug-metabolizing enzymes (CYPs, UGTs). |
| NADPH Regenerating System | Provides a constant supply of NADPH, essential for CYP450-mediated Phase I oxidation [13]. |
| UDPGA (Uridine 5'-diphosphoglucuronic acid) | Cofactor for UGT-mediated glucuronidation (Phase II) [18]. |
| Alamethicin | Pore-forming peptide that permeabilizes microsomal membranes, allowing UDPGA access to the active site of UGT enzymes [18]. |
| Magnesium Chloride (MgCl2) | Cofactor for various enzymatic reactions. |
| Potassium Phosphate Buffer | Provides a stable physiological pH for the incubation. |
| LC-MS/MS System with Autosampler | For quantitative analysis of parent compound depletion. |
3. Procedure
- Preparation:
- Prepare a 1 mg/mL stock solution of the test compound in an appropriate solvent (e.g., DMSO).
- Thaw microsomes on ice and prepare all cofactor solutions in ice-cold potassium phosphate buffer.
- Incubation Setup (Two Conditions):
- Condition A (Phase I only): Microsomes (0.5 mg/mL) + NADPH Regenerating System + Test Compound (1 µM).
- Condition B (Phase I + II): Microsomes (0.5 mg/mL) + Alamethicin (25 µg/mL) → pre-incubate on ice for 15 minutes. Then add NADPH Regenerating System + UDPGA (2-5 mM) + Test Compound (1 µM) [18].
- Initiation and Time Points:
- Pre-warm the incubation mixtures at 37°C for 5 minutes.
- Start the reaction by adding the NADPH Regenerating System (for Condition A) or the test compound (for Condition B).
- At predetermined time points (e.g., 0, 5, 15, 30, 45, 60 minutes), withdraw an aliquot and quench the reaction with an equal volume of ice-cold acetonitrile containing an internal standard.
- Sample Analysis:
- Centrifuge the quenched samples to precipitate proteins.
- Analyze the supernatant by LC-MS/MS to measure the peak area of the parent compound at each time point.
4. Data Analysis
- Plot the natural logarithm (ln) of the parent compound's remaining percentage against time.
- The slope of the linear regression (k) is the elimination rate constant.
- Calculate the in vitro half-life: t1/2 = 0.693 / k.
- Calculate intrinsic clearance: CLint, in vitro = k / [microsomal protein concentration].
Experimental Workflow and Metabolic Pathways
The following diagrams illustrate the core concepts of the metabolic pathway and the experimental workflow for the stability assay.
Diagram 1: Drug Metabolism and Excretion Pathway
Diagram 2: Metabolic Stability Assay Workflow
FAQs: Understanding the Fundamentals
What is the first-pass effect, and why is it critical for oral drug development? The first-pass effect (also known as first-pass metabolism or presystemic metabolism) is a phenomenon where a drug undergoes metabolic processing at a specific location in the body, leading to a reduction in the concentration of the active drug before it reaches the systemic circulation or its site of action [21] [22]. This effect is most prominent for orally administered drugs, as the liver is the primary site of this metabolism. After absorption from the digestive system, a drug enters the hepatic portal system and is carried via the portal vein to the liver, where it can be extensively metabolized before it is distributed to the rest of the body [21]. For drugs with high first-pass extraction, this can drastically reduce their oral bioavailability, meaning only a small fraction of the administered dose reaches the bloodstream to exert its therapeutic effect [21].
Which organs and enzymes are primarily responsible for first-pass metabolism? While the liver is the major site of first-pass metabolism due to its high concentration of metabolizing enzymes, extraction can also occur in other locations, including the gut wall, lungs, and vasculature [21] [22]. The four primary systems affecting the first-pass effect are:
- Enzymes of the gastrointestinal lumen
- Gastrointestinal wall enzymes
- Bacterial enzymes
- Hepatic enzymes [21]
The cytochrome P450 (CYP) enzyme family, particularly CYP3A4, plays a crucial role in the first-pass metabolism of many drugs, significantly impacting their bioavailability [21] [23]. Importantly, significant levels of CYP3A4 and CYP2D6 are also present in the intestinal brush border, contributing to pre-systemic metabolism before the drug even reaches the liver [23].
How do metabolic stability and clearance relate to the first-pass effect? Metabolic stability refers to a compound's susceptibility to biotransformation and is a key determinant of its pharmacokinetic profile, including bioavailability and half-life [1] [2]. A drug with low metabolic stability is rapidly broken down, which often correlates with a high hepatic extraction ratio and significant first-pass effect [2]. Conversely, designing drugs with low clearance (high metabolic stability) is a common goal to prolong half-life and reduce dosing frequency [24]. However, accurately predicting human clearance for low-clearance compounds presents technical challenges, as they may show minimal turnover in standard in vitro assays, leading to overestimation of human clearance and half-life [24].
What is the clinical significance of the first-pass effect for patient dosing? Drugs that undergo considerable first-pass metabolism, such as morphine, propranolol, and nitroglycerin, often require much larger oral doses compared to their intravenous dosages to achieve a similar therapeutic effect [21] [22]. This can lead to complex dosing regimens and high inter-patient variability in drug response, as the extent of first-pass metabolism can be influenced by individual differences in enzyme expression, genetics, age, disease state (particularly liver disease), and concurrent use of other medications that inhibit or induce metabolizing enzymes [21] [23] [22].
Troubleshooting Guides
Challenge: Poor Oral Bioavailability Due to High First-Pass Metabolism
Problem: Your drug candidate shows excellent in vitro potency but has unacceptably low oral bioavailability in preclinical models, suspected to be due to extensive first-pass metabolism.
Investigation and Diagnosis:
Confirm the Site of Metabolism: Determine if metabolism occurs in the gut wall, the liver, or both.
- Method: Conduct comparative in vitro assays using human liver microsomes, human intestinal microsomes, and suspended hepatocytes from both liver and intestine [21] [24]. The hepatocyte relay method can be particularly useful for low-clearance compounds [24].
- Interpretation: Significant metabolism in intestinal microsomes points to a gut wall component, while metabolism primarily in liver preparations indicates hepatic first-pass.
Identify the Enzymes Involved:
- Method: Perform reaction phenotyping using specific chemical inhibitors or antibodies against individual CYP enzymes (e.g., CYP3A4, CYP2D6) or recombinant human enzymes [23] [24].
- Interpretation: If CYP3A4 is identified as the primary enzyme, you can anticipate potential drug-drug interactions and variability [23].
Solutions and Mitigation Strategies:
Employ a Prodrug Strategy: Design a prodrug that is resistant to first-pass metabolism but converts to the active parent drug in the systemic circulation. This can dramatically improve bioavailability [21] [2].
Modify the Administration Route: Bypass the first-pass effect entirely by using alternative routes of administration.
- Parenteral (IV, IM): Achieves 100% bioavailability [25].
- Sublingual/Buccal: Allows direct absorption into systemic circulation, as used for nitroglycerin [21] [22].
- Rectal: Partially bypasses first-pass metabolism [21].
- Transdermal/Inhalational: Delivers drug directly to the systemic circulation [21].
Utilize Enzyme Inhibition: Co-administer a low dose of a metabolic enzyme inhibitor. A clinical example is the combination of dextromethorphan with quinidine, where quinidine inhibits CYP2D6-mediated metabolism of dextromethorphan, thereby increasing its systemic exposure [22].
Optimize Chemical Structure: Use structure-activity relationship (SAR) studies to modify the molecular structure, making it less susceptible to metabolic degradation. This can involve altering functional groups or incorporating metabolically stable moieties [26] [2].
Challenge: Accurately Predicting Low Human Clearance
Problem: Your compound shows minimal turnover in standard metabolic stability assays, making it difficult to predict its human half-life and optimal dosing regimen.
Investigation and Diagnosis:
Use Advanced In Vitro Models: Standard human liver microsomal or hepatocyte assays have a lower limit of detection for intrinsic clearance (CL~int~) [24]. To address this:
- Method: Implement the Hepatocyte Relay Method. This involves transferring the supernatant of a test compound incubation after several hours to freshly thawed hepatocytes, repeating this process to achieve a cumulative incubation time of 20 hours or more [24].
- Interpretation: This method extends the measurable range of CL~int~ and has shown good correlation with in vivo intrinsic clearance in humans and preclinical species [24].
Apply Time-Dependent Modeling: For very low-clearance compounds, data from prolonged incubations can be fitted to biphasic kinetic models to account for potential loss of enzyme activity over time, providing more accurate clearance estimates [24].
Solutions and Mitigation Strategies:
- Increase Assay Sensitivity: Increase hepatocyte density in the incubation (e.g., from 0.5 million cells/mL to 1.0 million cells/mL) to effectively lower the limit of CL~int~ measurement [24].
- Leverage Physiologically Based Pharmacokinetic (PBPK) Modeling: Use in vitro clearance data from sensitive assays to build PBPK models that can simulate and predict human pharmacokinetics, including half-life and bioavailability, even for low-clearance compounds [21] [26].
Experimental Protocols for Key Assays
Protocol: Hepatocyte Relay Assay for Low-Clearance Compounds
Purpose: To accurately determine the intrinsic clearance and identify metabolites for compounds with low metabolic turnover [24].
Workflow:
The following diagram illustrates the sequential process of the hepatocyte relay assay.
Materials:
- Research Reagent Solutions:
- Cryopreserved Human Hepatocytes: Pooled from multiple donors for consistency [24].
- Incubation Media: Williams' Medium E or similar, supplemented with necessary cofactors.
- NADPH Regenerating System: Provides essential cofactor for CYP450 enzyme activity.
- Stopping Solution: Acetonitrile or methanol with internal standard to terminate the reaction.
- LC-MS/MS System: For quantitative analysis of parent drug and metabolite identification [24].
Procedure:
- Initial Incubation: Thaw hepatocytes and incubate with the test compound (1 µM) at a density of 0.5-1.0 million cells/mL for 4 hours at 37°C.
- First Relay: Centrifuge the incubation mixture. Transfer the supernatant to a fresh vial containing newly thawed, viable hepatocytes. Incubate for another 4 hours.
- Subsequent Relays: Repeat step 2 as needed (typically 3-5 relays) to achieve a cumulative incubation time (e.g., 20 hours).
- Sample Analysis: At each relay time point, collect samples, precipitate protein with stopping solution, and analyze by LC-MS/MS to monitor parent compound depletion and metabolite formation.
- Data Analysis: Calculate intrinsic clearance (CL~int~) from the parent depletion profile over the cumulative incubation time.
Protocol: Reaction Phenotyping using Chemical Inhibitors
Purpose: To identify the specific cytochrome P450 enzyme(s) responsible for metabolizing a drug candidate [23] [24].
Materials:
- Research Reagent Solutions:
- Human Liver Microsomes (HLM) or cDNA-Expressed CYP Enzymes: Source of metabolic enzymes.
- Selective Chemical Inhibitors: e.g., Ketoconazole (CYP3A4), Quinidine (CYP2D6), Furafylline (CYP1A2) [23].
- NADPH Regenerating System.
- LC-MS/MS System.
Procedure:
- Set up Incubations: Incubate the test compound with HLM in the presence and absence of selective CYP inhibitors. Include control incubations without inhibitors and without NADPH.
- Run Parallel Incubations: Use cDNA-expressed individual CYP enzymes to directly confirm which enzyme can metabolize the drug.
- Quantify Metabolite Formation: Measure the rate of formation of the primary metabolite(s) in each incubation.
- Data Analysis: A significant reduction (>80%) in metabolite formation in the presence of a specific inhibitor (or with a specific cDNA-expressed CYP) identifies the major enzyme responsible for the metabolic pathway.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and their applications in studying hepatic first-pass metabolism.
| Reagent / Material | Function / Application in Research |
|---|---|
| Cryopreserved Hepatocytes | Gold-standard in vitro system for predicting hepatic clearance and metabolite profiling; maintains full complement of hepatic enzymes and transporters [24]. |
| Human Liver Microsomes (HLM) | Subcellular fraction containing membrane-bound CYP enzymes; used for high-throughput metabolic stability screening and reaction phenotyping [1] [24]. |
| cDNA-Expressed CYP Enzymes | Recombinantly expressed individual human CYPs; used to definitively identify which specific enzyme metabolizes a drug candidate [24]. |
| Selective Chemical Inhibitors | Compounds that inhibit specific CYP enzymes (e.g., ketoconazole for CYP3A4); essential for reaction phenotyping studies [23] [24]. |
| NADPH Regenerating System | Supplies NADPH, the essential cofactor for CYP450-mediated oxidative metabolism, in sustained in vitro incubations [24]. |
Key Data for Common Drugs and Strategies
The following table summarizes the first-pass effect and mitigation strategies for several well-known drugs.
| Drug | Therapeutic Class | First-Pass Effect & Bioavailability (F%) | Clinical Mitigation Strategy |
|---|---|---|---|
| Propranolol [21] [22] | Beta-blocker | Extensive first-pass metabolism; oral dose >> IV dose. | Administer high oral doses; monitor blood concentrations [22]. |
| Nitroglycerin [21] [22] | Anti-anginal | Extensive hepatic first-pass metabolism; very low F% if swallowed. | Administer sublingually to bypass first-pass effect [21] [22]. |
| Morphine [22] | Opioid analgesic | Considerable first-pass metabolism. | Use larger oral doses compared to parenteral routes. |
| Remdesivir [21] | Antiviral | Trapped in liver after oral administration; negligible systemic availability. | Administer via IV infusion to bypass first-pass metabolism entirely [21]. |
| Dextromethorphan [22] | Antitussive / Neurologic | Significant first-pass bioinactivation by CYP2D6. | Co-administer with quinidine (CYP2D6 inhibitor) to boost systemic levels [22]. |
| Saquinavir [23] | Protease Inhibitor | Substrate for CYP3A4 and P-gp; low oral bioavailability. | Co-administer with low-dose ritonavir (CYP3A4 inhibitor) to boost bioavailability. |
Visualizing the First-Pass Effect Journey
The diagram below illustrates the journey of an orally administered drug and the sites where first-pass metabolism can occur, significantly reducing the amount of active drug reaching the systemic circulation.
FAQs and Troubleshooting Guides
FAQ 1: What is the fundamental difference between Intrinsic Clearance (CLint) and Hepatic Clearance (CLH)?
Answer: CLint and CLH describe different aspects of drug elimination. Intrinsic Clearance (CLint) is a theoretical measure of the innate metabolic capacity of the liver enzymes for a drug, independent of external factors like blood flow or protein binding. It represents the volume of blood (containing a saturating drug concentration) that the liver can completely clear of drug per unit time [27].
In contrast, Hepatic Clearance (CLH) is the actual volume of blood cleared of the drug per unit time as it passes through the liver. It is the clinically observable clearance that determines systemic drug levels. CLH is a function of liver blood flow (QH), the fraction of unbound drug in the blood (fuB), and the intrinsic clearance (CLint), as described by the well-stirred model [28] [29]:
CLH = (QH • fuB • CLint) / (QH + fuB • CLint)
The relationship means that CLH for a drug can never exceed liver blood flow, whereas CLint can be much higher [27].
FAQ 2: Why do my in vitro predictions of human hepatic clearance systematically underpredict the in vivo observed values?
Answer: Systematic underprediction is a well-documented challenge in In Vitro-In Vivo Extrapolation (IVIVE). Several key factors contribute to this error [30]:
- Clearance-Dependent Error: The error is often not uniform. Studies have found that underprediction tends to be more pronounced for compounds with high in vivo intrinsic clearance. This is attributed to limitations in current in vitro systems, such as the loss of enzymatic activity over long incubations, permeability limitations, and the impact of the unstirred water layer [30].
- Limitations of In Vitro Systems: Simple in vitro systems like microsomes lack the full complement of enzymes and transporters present in intact hepatocytes. Even hepatocytes, which contain both Phase I and Phase II enzymes, may not fully replicate the in vivo liver environment over time [30] [31].
- Experimental Artifacts: Issues such as depletion of endogenous cofactors, non-specific binding to incubation apparatus, and inaccuracies in measuring the fraction of unbound drug can all lead to an underestimation of the true clearance [30] [1].
Troubleshooting Guide:
- For Low Clearance Compounds: If compound disappearance is less than 20% over the assay duration, the result may be unreliable due to analytical variability. Consider using specialized assays with longer incubation times (e.g., co-culture systems with 72-hour incubations) to achieve greater sensitivity [31].
- For High Clearance Compounds: Be aware that predictions for high-extraction-ratio compounds are particularly prone to error, with in vitro models often failing to correctly identify them as such [30].
- Use Pooled Donors: To mitigate problems associated with inter-individual variability in human metabolism, use cryopreserved hepatocytes pooled from a minimum of three different donors [31].
- Adopt a Holistic Approach: Supplement traditional in vitro assays with more advanced models, such as microphysiological systems (organ-on-a-chip) that fluidically link gut and liver models, or use physiological-based pharmacokinetic (PBPK) modeling to integrate various data sources for a more accurate prediction [11].
FAQ 3: When should I use microsomes versus hepatocytes for metabolic stability assays?
Answer: The choice depends on the stage of your drug discovery project and the metabolic information you need.
- Liver Microsomes: are subcellular fractions containing a high concentration of Phase I enzymes, particularly cytochrome P450s (CYPs). They are ideal for primary, high-throughput screening early in discovery to rapidly rank compounds for metabolic stability and identify CYP-mediated metabolism [30] [5].
- Hepatocytes: are intact liver cells containing the full complement of both Phase I and Phase II enzymes and transporters. They provide a more physiologically relevant model and are best used as a secondary screen on favorable compounds from the primary screen. Hepatocytes are essential for identifying non-CYP metabolism, transporter effects, and comprehensive metabolite profiling [31] [5].
Interpreting Discrepancies: If a compound is more stable in hepatocytes than in microsomes, it may indicate poor cellular permeability or that it is a substrate for efflux transporters. Conversely, if a compound is less stable in hepatocytes, it likely undergoes significant Phase II metabolism (e.g., glucuronidation, sulfation) [31].
Experimental Protocols
Protocol 1: Determining Intrinsic Clearance Using Hepatocyte Stability Assay
This protocol measures the in vitro intrinsic clearance of a test compound by monitoring its disappearance in a suspension of cryopreserved hepatocytes [31].
1. Key Research Reagent Solutions
| Item | Function |
|---|---|
| Cryopreserved Hepatocytes | Species-specific liver cells containing full complement of Phase I and Phase II metabolizing enzymes and transporters. |
| Incubation Buffer | Physiologically compatible medium (e.g., Krebs-Henseleit buffer) to maintain cell viability and function. |
| Test Compound | The drug candidate of interest, typically prepared as a stock solution in DMSO or buffer. |
| Acetonitrile (ACN) | Organic solvent used to terminate the metabolic reaction at each time point and precipitate proteins. |
| Liquid Chromatography-Mass Spectrometry/Mass Spectrometry (LC-MS/MS) | Analytical platform for sensitive and specific quantification of the test compound in the presence of biological matrix. |
2. Methodology
- Thaw and Viability Check: Rapidly thaw cryopreserved hepatocytes (pooled from multiple donors is recommended) and assess cell viability using trypan blue exclusion. Proceed only if viability exceeds a certain threshold (e.g., 80%).
- Incubation Setup: Dilute the hepatocytes to a standard density (e.g., 1 million cells/mL) in incubation buffer pre-warmed to 37°C. Add the test compound to initiate the reaction. A typical final DMSO concentration should be ≤0.1-1%.
- Sample Collection: Immediately remove an aliquot (t=0) and quench it in an equal volume of ice-cold acetonitrile. Repeat this process at predetermined time points (e.g., 5, 15, 30, 60, 120 minutes).
- Sample Analysis: Centrifuge the quenched samples to pellet precipitated proteins and cells. Analyze the supernatant using LC-MS/MS to determine the peak area ratio of the test compound to an internal standard.
- Data Calculation:
- Plot the natural logarithm (ln) of the peak area ratio versus time.
- The gradient of the linear regression line is the elimination rate constant (k).
- Calculate the in vitro half-life:
t₁/₂ = 0.693 / k - Calculate the intrinsic clearance:
CLint (μL/min/million cells) = (V * 0.693) / t₁/₂where V is the incubation volume per million cells (μL/10⁶ cells) [31].
Protocol 2: In Vitro-In Vivo Extrapolation (IVIVE) of Hepatic Clearance
This protocol describes how to scale the in vitro intrinsic clearance from hepatocytes to a predicted in vivo hepatic clearance using the well-stirred model [31].
1. Methodology
- Obtain In Vitro CLint: Determine the in vitro intrinsic clearance (CLint, vitro) in μL/min/million cells using the hepatocyte stability assay described in Protocol 1.
- Scale to In Vivo CLint: Convert the in vitro value to a predicted in vivo intrinsic clearance using species-specific scaling factors (SF), which are based on hepatocellularity (number of hepatocytes per gram of liver) and liver weight [31].
CLint, vivo (mL/min/kg) = [CLint, vitro (μL/min/million cells) * SF] / 100 - Apply the Well-Stirred Model: Input the scaled CLint, vivo into the well-stirred model equation to predict the in vivo hepatic clearance (CLH) [30] [31] [28]:
CLH = (QH • fuB • CLint, vivo) / (QH + fuB • CLint, vivo)Where:QH= Liver blood flow (species-specific, e.g., ~20.7 mL/min/kg for human [30]).fuB= Fraction of drug unbound in blood.CLint, vivo= Scaled in vivo intrinsic clearance.
2. Data Interpretation and Classification
Predicted clearance values can be categorized based on the hepatic extraction ratio (E = CLH / QH) [31]. The following table provides a generalized classification using physiologically based scaling factors, which often results in a significant underprediction trend as noted in the troubleshooting guide [30].
Table: Hepatic Clearance Classification and Prediction Accuracy
| Hepatic Extraction Ratio (E) | Clearance Category | Typical In Vivo CLH (Human) | % within 2-fold (Human Hepatocytes) [30] | % within 2-fold (Human Microsomes) [30] |
|---|---|---|---|---|
| E < 0.3 | Low | < ~6 mL/min/kg | 34.6% | Data not specified |
| 0.3 ≤ E ≤ 0.7 | Intermediate | ~6 - 14 mL/min/kg | 35.7% | Data not specified |
| E > 0.7 | High | > ~14 mL/min/kg | 11.1% | Data not specified |
Relationship Between Key Parameters
The parameters Intrinsic Clearance (CLint), Half-life (t₁/₂), and Hepatic Extraction (E) are fundamentally interconnected in determining a drug's pharmacokinetic profile.
Table: Interrelationship of Key Pharmacokinetic Parameters
| Parameter | Definition | Direct Determinants | Impact on Drug Profile |
|---|---|---|---|
| Intrinsic Clearance (CLint) | Innate ability of liver enzymes to clear drug without flow limitations. | Enzyme affinity (Km) and capacity (Vmax). | Governs potential for metabolism; high CLint suggests susceptibility to enzyme induction/inhibition. |
| Hepatic Extraction Ratio (E) | Fraction of drug removed from blood in a single liver pass. | Liver blood flow (QH), protein binding (fuB), and CLint. | Determines oral bioavailability (F = 1 - E) and sensitivity to changes in blood flow and binding. |
| Half-life (t₁/₂) | Time for drug concentration in plasma to reduce by 50%. | Volume of Distribution (Vd) and Total Clearance (CL). | Dictates dosing frequency and time to reach steady state. |
The following diagram illustrates the logical and mathematical relationships between these parameters, showing how in vitro data is scaled and used to predict in vivo outcomes.
A Practical Guide to Metabolic Stability Assays: From Microsomes to Hepatocytes
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: Why is there a significant difference in metabolic stability between human and mouse liver microsomes for my compound?
Answer: Interspecies differences are common and arise from variations in enzyme expression levels and isoform composition between humans and mice. [32] These enzymatic variations, rather than physicochemical properties like LogD or AlogP, are the primary drivers of differing metabolic rates. [32]
- Troubleshooting Tip: If your compound shows high species-specific variability, use caution when extrapolating animal data to predicted human outcomes. Incorporate metabolic stability assays from multiple species early in the lead optimization phase.
FAQ 2: My negative control shows unexpected substrate depletion. What could be wrong?
Answer: Unexpected activity in negative controls typically points to issues with the assay system.
- Troubleshooting Checklist:
- Verify NADPH Omission: Ensure the NADPH Regenerating System was truly omitted from the negative control reaction. Even trace amounts can cause activity. [33]
- Check Microsome Vitality: Avoid repeated freeze-thaw cycles of microsomes, as this can compromise enzymatic activity. Do not thaw microsomes at room temperature; always thaw slowly on ice. [33]
- Assess Solvent Inhibition: Confirm that the final concentration of organic solvent (e.g., from the test article stock solution) is kept below 1% to avoid inhibiting CYP activities. [33]
FAQ 3: The data from my single-point assay is inconsistent. How can I improve reliability?
Answer: Inconsistency often stems from non-optimized, non-initial rate conditions.
- Solution: Ensure you are measuring the reaction under initial rate conditions, where less than 15% of the substrate is consumed. [33] This may require separate optimization of:
- Microsomal protein concentration
- Test article concentration
- Incubation times [33]
FAQ 4: How can I predict metabolic stability computationally to guide my compound design?
Answer: In silico models have become powerful tools for prediction. You can use publicly available models or build your own.
- Public Resources: The ADME@NCATS portal offers open-source models trained on large internal datasets (e.g., >7,000 compounds for HLM stability), achieving accuracies exceeding 80%. [34]
- Advanced Methods: State-of-the-art models like MetaboGNN use Graph Neural Networks (GNNs) and Graph Contrastive Learning to predict stability directly from molecular structures and can identify key molecular fragments associated with stability, offering valuable insights for chemists during lead optimization. [32]
Experimental Protocols & Data
Standard Protocol for Liver Microsomal Stability Assay
The following table outlines a general procedure for measuring NADPH-dependent metabolic stability in liver microsomes using the substrate depletion method. [33] [34]
| Step | Parameter | Details & Critical Points |
|---|---|---|
| 1 | Reaction Setup | Prepare a 190 µL incubation mixture containing: 183 µL of 100 mM Phosphate Buffer (pH 7.4), 2 µL of 100X Test Article (in solvent, keep final organic solvent <1%), and 5 µL of 20 mg/mL Liver Microsomes. [33] |
| 2 | Pre-incubation | Pre-incubate the mixture (microsomes, buffer, test article) for 5 minutes in a 37°C water bath with gentle agitation. [33] |
| 3 | Reaction Initiation | Initiate the metabolic reaction by adding 10 µL of 20 mM NADPH Regenerating Solution. For negative controls, omit NADPH or use heat-inactivated microsomes. [33] [34] |
| 4 | Incubation | Incubate at 37°C for a predetermined time (e.g., up to 60 min). Use multiple time points (e.g., 0, 5, 10, 15, 30, 60 min) for multi-point assays to determine half-life (t1/2). [34] |
| 5 | Reaction Termination | Terminate the reaction by adding 200 µL of cold organic solvent (e.g., Acetonitrile or Ethyl Acetate). Vortex thoroughly. [33] |
| 6 | Sample Processing | Centrifuge samples at ~3000 rpm for 5-20 minutes to pellet protein. Transfer the supernatant for analysis. [33] [34] |
| 7 | Analysis | Analyze samples using LC-MS/MS to quantify the percentage of the parent compound remaining at each time point. [32] [34] |
Quantitative Data from Key Studies
The table below summarizes metabolic stability data and model performances from recent research, providing benchmarks for your own work.
| Study / Model | Dataset Size | Key Metric | Result / Performance | Application Note |
|---|---|---|---|---|
| MetaboGNN (2025) [32] | 3,981 compounds | Root Mean Square Error (RMSE) | HLM: 27.86, MLM: 27.91 (% parent remaining) | Top-performing model from a recent challenge; incorporates interspecies differences. |
| NCATS HLM Model (2024) [34] | 6,648 compounds | Prediction Accuracy | >80% balanced accuracy | Publicly available model on ADME@NCATS portal; leverages cross-species data. |
| NCATS RLM Model (2020) [6] | ~20,216 compounds | Classification (Stable/Unstable) | t1/2 cutoff: 30 min | High-throughput data used to build robust QSAR models for rat metabolic stability. |
Workflow Visualization
Liver Microsomal Assay Workflow
The Scientist's Toolkit: Research Reagent Solutions
This table details the essential materials and reagents required for a standard liver microsomal stability assay. [33] [6] [34]
| Reagent / Material | Function / Purpose in the Assay |
|---|---|
| Liver Microsomes (HLM, MLM, RLM) | Source of metabolic enzymes (CYPs, FMOs, UGTs). The subcellular fraction containing the endoplasmic reticulum where Phase I metabolism occurs. [33] |
| NADPH Regenerating System | Critical cofactor system to provide a continuous supply of NADPH, which is essential for CYP and FMO enzyme activity. [33] [6] |
| Phosphate Buffer (pH 7.4) | Provides a physiologically relevant pH environment for the enzymatic reactions. [33] |
| Test Article / Compound | The drug candidate or chemical entity whose metabolic stability is being assessed. |
| Organic Solvent (ACN, MeOH, EtOAc) | Used to prepare compound stock solutions and to terminate the metabolic reaction by denaturing proteins. [33] [6] |
| Alamethicin / MgCl₂ / UDPGA | Required for assessing UGT (Uridine glucuronosyltransferase) activity. Alamethicin is a pore-forming agent that facilitates cofactor access to UGT enzymes inside microsomal vesicles. [33] |
| Control Compounds (e.g., Buspirone, Propranolol) | Compounds with well-characterized metabolic profiles are used as assay controls to ensure system functionality and reliability. [6] [34] |
Technical Support Center
Troubleshooting Guides & FAQs
Q1: Our metabolic stability results show high variability between replicates. What could be the cause and how can we resolve this?
- Potential Cause: Inconsistent hepatocyte viability or improper handling leading to degraded enzyme activity.
- Troubleshooting Steps:
- Verify Hepatocyte Quality: Confirm viability is >85% using trypan blue exclusion before starting the assay. Do not use thawed hepatocytes if viability is low [35].
- Check Preparation Consistency: Ensure the cell suspension is homogenous before each aliquot. Use an automated liquid handler to minimize pipetting error [35].
- Review Incubation Conditions: Confirm that the temperature is consistently maintained at 37°C and that the incubation platform provides uniform agitation.
- Solution: Implement a strict quality control checkpoint for cell viability and use automation for all sample preparation steps.
Q2: We are detecting unexpected or novel metabolites in our assay. How should we proceed?
- Potential Cause: This may indicate a previously unknown metabolic pathway, which is a key advantage of using integrated hepatocyte assays [35].
- Troubleshooting Steps:
- Confirm the Finding: Reproduce the result with a fresh aliquot of test compound and hepatocytes to rule out a preparation error.
- Increase Data Scrutiny: Use high-resolution mass spectrometry to accurately determine the elemental composition of the novel metabolite [35].
- Cross-Check Literature: Investigate if this metabolic pathway has been reported in other species or in published literature for similar compounds.
- Solution: Document the finding thoroughly. This novel information is critical for understanding the complete metabolic profile of your compound and should be factored into lead optimization strategies [2].
Q3: The calculated intrinsic clearance (CLint) from our hepatocyte assay does not correlate well with in vivo data. What are the common pitfalls?
- Potential Cause: The assay conditions may not adequately capture all metabolic processes, or scaling factors may be incorrect [1].
- Troubleshooting Steps:
- Review Protein Binding: Check if the in vitro incubation medium contains appropriate protein levels, as unbound fraction differences can significantly impact clearance predictions [1].
- Evaluate Metabolite Stability: Ensure that primary metabolites are not undergoing further biotransformation during the assay, which can skew parent depletion rates.
- Assess Enzyme Kinetics: Verify that the hepatocyte concentration and incubation time are within the linear range for metabolite formation and parent depletion.
- Solution: Incorporate physiological scaling factors that account for protein binding and use retrospective analysis to refine in vitro-in vivo correlation (IVIVC) models for your chemical series [1].
Q4: The automated data analysis software is misclassifying a metabolite. How can we improve the accuracy?
- Potential Cause: The software's metabolite prediction algorithm may lack specific parameters for your compound's unique chemical structure.
- Troubleshooting Steps:
- Manual Verification: Manually inspect the chromatographic peaks and mass spectra to confirm the software's assignment.
- Adjust Parameters: Modify the software's settings for expected biotransformations (e.g., add a less common metabolic reaction like dioxygenation) based on your compound's likely metabolic soft spots [35].
- Use Control Compounds: Run a set of control compounds with well-characterized metabolic pathways to validate the software's performance under your specific conditions [35].
- Solution: Do not rely solely on automated data processing. Always include a step for expert manual review and curation of the metabolite profile.
Quantitative Data Tables
Table 1: Key Parameters for a Standardized Integrated Hepatocyte Stability Assay
| Parameter | Specification | Purpose & Rationale |
|---|---|---|
| Hepatocyte Viability | >85% | Ensures robust enzymatic activity for both Phase I and Phase II metabolism [35]. |
| Cell Density | 0.5 - 1.0 x 10^6 cells/mL | Maintains physiological enzyme ratios and linear reaction kinetics [35]. |
| Test Compound Concentration | 1 µM | Minimizes potential for enzyme saturation and non-physiological kinetics [35] [1]. |
| Incubation Time | 0 - 120 minutes | Allows for accurate measurement of parent depletion and metabolite formation over time [35]. |
| Sample Collection Timepoints | 0, 15, 30, 60, 120 min | Enables calculation of half-life (t1/2) and intrinsic clearance (CLint) [35]. |
Table 2: Example Metabolic Stability Data of Control Compounds in Human Hepatocytes
| Control Compound | Major Metabolic Route(s) | Half-life (t1/2, min) | Intrinsic Clearance (CLint, µL/min/million cells) |
|---|---|---|---|
| Verapamil | N-dealkylation (CYP3A4) | Short (< 30) | High (> 50) |
| Diazepam | C3-hydroxylation, N-demethylation (CYP3A4/2C19) | Medium (30 - 90) | Medium (10 - 50) |
| Acetaminophen | Glucuronidation, Sulfation (UGT, SULT) | Long (> 90) | Low (< 10) |
Note: The data above is representative. Actual values should be established internally for validation purposes [35].
Experimental Protocols
Methodology: Integrated Hepatocyte Stability Assay for Metabolic Stability and Metabolite Profiling
This protocol outlines the simultaneous assessment of metabolic stability and metabolite identification using cryopreserved hepatocytes in a 96-well format [35].
Part 1: Automated Sample Preparation and Incubation
- Thaw Hepatocytes: Rapidly thaw cryopreserved hepatocytes in a 37°C water bath. Dilute the cells in pre-warmed incubation media (e.g., Williams' E medium).
- Determine Viability: Mix an aliquot of cells with trypan blue and count using a hemocytometer or automated cell counter. Proceed only if viability exceeds 85%.
- Prepare Incubation Mix: Adjust hepatocyte density to 1 million cells/mL in incubation media. Pre-incubate the cell suspension at 37°C with gentle agitation for 10 minutes.
- Initiate Reaction: Add the test compound (from a 100x stock in DMSO) to the hepatocyte suspension to achieve a final concentration of 1 µM. Use an automated liquid handler for precision and to start multiple timepoints simultaneously [35].
- Terminate Reaction: At predetermined timepoints (e.g., 0, 15, 30, 60, 120 min), transfer an aliquot of the incubation mixture to a stopping solution (e.g., acetonitrile containing an internal standard) to precipitate proteins and halt enzymatic activity.
Part 2: LC-HRMS Analysis for Parent and Metabolite Monitoring
- Sample Analysis: Centrifuge the stopped reaction samples to remove precipitated protein. Inject the supernatant onto a Liquid Chromatography-High Resolution Mass Spectrometry (LC-HRMS) system.
- Chromatography: Use a reversed-phase C18 column with a gradient elution of water and acetonitrile (both containing 0.1% formic acid) to separate the parent compound and its metabolites.
- Mass Spectrometry: Operate the HRMS in data-dependent acquisition (DDA) mode. Use a full-scan MS survey to monitor parent compound depletion, followed by MS/MS scans on the most intense ions to obtain structural information for metabolite identification [35].
Part 3 & 4: Automated Data Analysis and Reporting
- Stability Assessment: Process the parent compound peak area versus time data using automated software to calculate the depletion half-life (t1/2) and intrinsic clearance (CLint).
- Metabolite Profiling: Use streamlined batch-processing software to identify metabolites based on accurate mass shifts, isotope patterns, and MS/MS fragmentation patterns compared to the parent compound [35].
Workflow and Pathway Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Hepatocyte Stability Assays
| Item | Function & Rationale |
|---|---|
| Cryopreserved Hepatocytes | Biologically relevant in vitro system containing the full complement of Phase I and Phase II metabolic enzymes, providing a holistic view of drug metabolism [35] [19]. |
| Williams' E Medium | A complex cell culture medium designed to maintain hepatocyte function and viability during the incubation period. |
| Liquid Chromatography-High Resolution Mass Spectrometry (LC-HRMS) | Enables simultaneous quantitative analysis of parent drug depletion and qualitative identification of metabolite structures based on accurate mass measurement [35]. |
| Automated Liquid Handling System | Improves assay precision and throughput by reducing manual pipetting errors and ensuring consistent sample preparation across multiple timepoints and compounds [35]. |
| Control Compounds (e.g., Verapamil, Diazepam) | Used to validate assay performance. These have well-characterized metabolic rates and pathways, serving as benchmarks for system suitability [35]. |
| Data Processing Software | Automated tools for batch-processing HRMS data to calculate metabolic stability parameters and generate metabolite profiles, significantly accelerating data analysis [35]. |
In the pursuit of overcoming poor metabolic stability in drug candidates, understanding specific metabolic pathways is crucial. Liver subcellular fractions, namely S9 and cytosol, are invaluable in vitro tools that provide a focused view of metabolic processes, particularly those mediated by cytosolic enzymes like aldehyde oxidase (AO) and various conjugation pathways [5]. These systems enable researchers to deconstruct the liver's metabolic capacity, offering a high-throughput, cost-effective means to identify soft spots and guide structure-activity relationship (SAR) campaigns early in lead optimization [36] [37].
The liver S9 fraction is the supernatant obtained after the first centrifugation (9,000 x g) of a liver homogenate [36]. It contains both microsomal (endoplasmic reticulum) and cytosolic enzymes, providing a broad spectrum of both Phase I and Phase II metabolic activities [36] [37]. In contrast, the liver cytosol is the soluble fraction obtained after further high-speed centrifugation (typically 105,000 x g) of the S9 fraction, and it contains exclusively soluble cytosolic enzymes, but no microsomal enzymes [38] [5].
Table 1: Core Characteristics of Metabolic Stability Systems
| Feature | Liver S9 Fraction | Liver Cytosol | Liver Microsomes | Hepatocytes |
|---|---|---|---|---|
| Enzyme Composition | Both microsomal & cytosolic enzymes [36] [37] | Only cytosolic enzymes [38] [5] | Only microsomal enzymes [36] | Full cellular complement of enzymes & transporters [36] |
| Key Enzymes Present | CYPs, UGTs, AO, SULTs, GSTs [36] [5] | AO, SULTs, GSTs, Xanthine Oxidase [36] [5] | CYPs, UGTs, FMOs [36] | All hepatic Phase I & II enzymes [36] |
| Cofactor Requirements | Requires exogenous cofactors (e.g., NADPH, UDPGA, PAPS) [36] [37] | Requires cofactors for specific reactions (e.g., PAPS for SULT) [38] | Requires exogenous cofactors (e.g., NADPH for CYPs) [36] | Contains endogenous cofactors; more physiologically relevant [36] |
| Primary Use in Stability Screening | Comprehensive Phase I & II metabolism; identifying AO involvement [36] [37] | Specific assessment of cytosolic enzyme metabolism (e.g., AO) [5] | Primary assessment of Phase I, CYP-mediated metabolism [36] | Gold standard for overall hepatic clearance; full metabolic profile [36] |
Experimental Protocols
Standard Liver S9 Stability Assay Protocol
This protocol is designed to measure the intrinsic clearance of a test compound using liver S9 fraction.
Incubation Conditions:
- Test System: Human or rat liver S9 fraction (gender-pooled) [36].
- Protein Concentration: Must be optimized; S9 fractions have an inherent dilution of enzymes compared to microsomes [36].
- Incubation Temperature: 37°C [37].
- Substrate Concentration: Typically 1-3 µM [36] [37].
- Cofactors: Supplement with relevant cofactors based on the metabolic pathways under investigation [37]:
- NADPH-regenerating system: For Phase I oxidative metabolism.
- Uridine 5'-diphospho-α-D-glucuronic acid (UDPGA): For glucuronidation.
- 3'-Phosphoadenosine-5'-phosphosulfate (PAPS): For sulfation.
- Reduced Glutathione (GSH): For trapping reactive metabolites or GST-mediated conjugation.
- Reaction Termination: Using ice-cold acetonitrile or methanol at predetermined time points (e.g., 0, 15, 30, 45 minutes) [37].
Sample Analysis:
- Following centrifugation, the supernatant is analyzed via Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) to monitor the disappearance of the parent compound over time [36] [37].
- Data is quantified by plotting the natural logarithm of the peak area ratio (compound/internal standard) against time.
Data Calculation:
- The elimination rate constant (k) is determined from the slope of the depletion curve.
- In vitro half-life (t1/2) and intrinsic clearance (CLint) are calculated using the following equations [37]:
- Half-life, t1/2 (min) = ln(2) / k
- Intrinsic Clearance, CLint (µL/min/mg protein) = (Incubation Volume / Protein) × (0.693 / t1/2)
Controls:
- Positive Controls: Include compounds like midazolam (for Phase I metabolism) and 7-hydroxycoumarin (for direct Phase II metabolism) to validate system activity [37].
- Negative Controls: Incubations without cofactors are essential to reveal chemical instability or non-cofactor dependent degradation [37].
Liver Cytosol Stability Assay for Aldehyde Oxidase (AO)
This protocol specifically targets the assessment of AO-mediated metabolism.
Incubation Conditions:
- Test System: Human liver cytosol [38] [5].
- Buffer: Appropriate physiological buffer (e.g., phosphate buffer, pH 7.4).
- Substrate Concentration: 1-3 µM.
- Cofactors: AO contains an embedded molybdopterin cofactor (MoCo), flavin adenine dinucleotide (FAD), and two iron-sulfur clusters, and does not require exogenous cofactors to be added to cytosol or S9 [38]. This is a key differentiator from CYP enzymes.
- Inhibitor: To confirm AO-specific metabolism, a selective AO inhibitor such as hydralazine can be included in parallel incubations [38].
Sample Analysis and Data Calculation:
- The process for termination, analysis, and calculation of CLint is identical to the S9 assay described above.
Troubleshooting FAQs
FAQ 1: My compound shows rapid depletion in hepatocytes but is stable in microsomes. What could be the reason and how can I investigate further?
- Problem: This discrepancy strongly suggests metabolism by non-microsomal, cytosolic enzymes [36] [5]. Microsomes contain only endoplasmic reticulum enzymes (mainly CYPs and UGTs), while hepatocytes contain the full enzyme complement.
- Solution:
- Run a Liver S9 Assay: The S9 fraction contains cytosolic enzymes. If your compound is depleted in S9 even without NADPH, it indicates a significant role for cytosolic, non-CYP enzymes [36].
- Run a Liver Cytosol Assay: Follow up with a specific cytosol stability test to directly confirm and quantify metabolism by cytosolic enzymes like AO [5].
- Use Chemical Inhibitors: In the S9 or cytosol system, include specific enzyme inhibitors. For example, use hydralazine to inhibit AO and observe if the depletion rate decreases, confirming AO's involvement [38].
FAQ 2: I am getting inconsistent results with my AO inhibition studies in S9 fraction when also running a GSH-trapping experiment. What might be interfering?
- Problem: This is a known experimental pitiability. The presence of reduced glutathione (GSH) can interfere with the inhibitory activity of hydralazine [38]. GSH is a nucleophile and can react directly with hydralazine, reducing its effective concentration and its ability to inhibit AO.
- Solution:
- Decouple the Experiments: Avoid addressing multiple research questions in a single incubation. Run separate experiments—one for GSH trapping of reactive metabolites and another for AO inhibition phenotyping [38].
- Consider Inhibitor Properties: Understand the time-dependent nature of your inhibitor. Hydralazine's interaction with GSH could have been predicted by considering its chemical reactivity and mechanism of inhibition [38].
FAQ 3: How do I determine if the metabolic instability observed in S9 is due to Phase I or Phase II metabolism?
- Problem: The S9 system is a composite of multiple enzyme classes, and the initial screen may not pinpoint the primary route of metabolism.
- Solution: This is resolved by designing incubations with specific cofactor combinations.
- Incubation with NADPH only: Supports CYP-mediated Phase I metabolism.
- Incubation with UDPGA/PAPS only: Supports direct Phase II conjugation (glucuronidation/sulfation) without prior Phase I metabolism.
- Incubation with NADPH + UDPGA/PAPS: Supports sequential metabolism (Phase I followed by Phase II).
Table 2: Interpreting Metabolic Pathways via Cofactor Dependence in S9
| Cofactor Condition | Observed Metabolism | Interpretation | Example Compound Behavior |
|---|---|---|---|
| NADPH only | Yes | Metabolism is primarily via Phase I enzymes (e.g., CYPs). | Midazolam, Testosterone [37] |
| UDPGA/PAPS only | Yes | Compound is a direct substrate for Phase II conjugation enzymes. | 7-Hydroxycoumarin [37] |
| NADPH + UDPGA/PAPS | Enhanced metabolism vs. single cofactor | Compound undergoes sequential metabolism (Phase I then Phase II). | Midazolam (1'-hydroxylation then glucuronidation) [37] |
| No Cofactors | Yes | Indicates chemical instability or metabolism by enzymes not requiring standard cofactors (e.g., hydrolases). | N/A |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for S9 and Cytosol Stability Assays
| Reagent / Material | Function / Description | Key Considerations |
|---|---|---|
| Liver S9 Fraction | Supernatant of liver homogenate containing microsomal & cytosolic enzymes [36]. | Available as species- and gender-pooled for representative data; ensure lot-to-lot consistency via enzyme activity checks (e.g., 7-EC O-deethylase activity) [36]. |
| Liver Cytosol | Soluble fraction containing cytosolic enzymes (AO, SULTs, etc.) [38] [5]. | Used to specifically investigate cytosolic metabolism; confirm absence of microsomal contamination if needed. |
| NADPH Regenerating System | Provides a constant supply of NADPH, the essential cofactor for CYP450 enzymes [36]. | Critical for maintaining Phase I metabolic activity throughout the incubation. |
| UDPGA | Cofactor for uridine 5'-diphospho-glucuronosyltransferase (UGT)-mediated glucuronidation [36] [37]. | Used to assess direct glucuronidation or sequential metabolism. |
| PAPS | Cofactor for sulfotransferase (SULT)-mediated sulfation [37]. | Used to assess sulfation pathways. |
| Reduced Glutathione (GSH) | Trapping agent for electrophilic reactive metabolites; cofactor for GST-mediated conjugation [38]. | Can interfere with some inhibitors (e.g., hydralazine); use strategically [38]. |
| Aldehyde Oxidase (AO) Inhibitor (e.g., Hydralazine) | Selective inhibitor used to confirm the involvement of AO in a compound's metabolism [38]. | Be aware of potential interactions with other assay components like GSH. Time-dependent inhibitor. [38]. |
| Positive Control Compounds | Midazolam: for Phase I/CYP3A4 activity. 7-Hydroxycoumarin: for direct Phase II conjugation [37]. | Essential for validating the metabolic competency of each batch of S9 or cytosol. |
In the broader thesis of overcoming poor metabolic stability, investigating extrahepatic metabolism is a crucial frontier. While the liver is the primary site of drug metabolism, extrahepatic tissues including the intestine, lung, and kidney possess significant metabolic capacity that can profoundly influence a drug's bioavailability, efficacy, and toxicity profile [39]. Ignoring these pathways during research can lead to unexpected clinical failures, as compounds stable in liver-based assays may be rapidly inactivated in other tissues, or conversely, transformed into active or toxic metabolites [40]. A comprehensive ADME (Absorption, Distribution, Metabolism, and Excretion) strategy must therefore integrate assessments beyond hepatic stability to build a complete picture of a drug's fate in the body. This guide provides detailed troubleshooting and methodological support for researchers establishing these vital extrahepatic metabolic stability assays.
Experimental Protocols for Key Extrahepatic Tissues
General Workflow for Tissue-Specific Metabolic Stability Assays
The following diagram illustrates the core experimental workflow for assessing metabolic stability in extrahepatic tissues, which is foundational to the protocols described in this section.
Protocol: Metabolic Stability in Intestinal Microsomes or S9 Fractions
Objective: To evaluate the contribution of intestinal metabolism to a compound's first-pass effect, which can significantly reduce oral bioavailability [39].
Detailed Methodology:
- Tissue Preparation: Use human or preclinical species' intestinal microsomes or S9 fractions. The S9 fraction is often preferred for intestinal assays as it contains both phase I and phase II enzymes [40].
- Incubation Conditions:
- Prepare a 1 mg/mL microsomal protein concentration or a 0.5-1 mg/mL S9 protein concentration in a suitable buffer (e.g., potassium phosphate buffer, pH 7.4).
- Add the test compound at a final concentration of 1-10 µM.
- For S9 fractions, include necessary cofactors for both phase I and II metabolism: an NADPH regenerating system (for Phase I) and UDPGA (for glucuronidation) and/or PAPS (for sulfation).
- Pre-incubate the mixture for 5 minutes at 37°C.
- Reaction Initiation and Quenching: Start the reaction by adding the NADPH regenerating system. At predetermined time points (e.g., 0, 5, 15, 30, 60 minutes), withdraw an aliquot (e.g., 50 µL) and quench it with a 2X volume of ice-cold acetonitrile containing an internal standard.
- Sample Analysis: Centrifuge the quenched samples, and analyze the supernatant using UHPLC-MS/MS to quantify the remaining parent drug over time [41].
- Data Analysis: Determine the in vitro half-life (t1/2) and intrinsic clearance (Clint) using standard kinetic models.
Protocol: Metabolic Stability in Lung Tissue Preparations
Objective: To assess pulmonary first-pass metabolism, which is critical for inhaled therapeutics and can also influence systemically administered drugs [39].
Detailed Methodology:
- Tissue Preparation: Use lung microsomes or S9 fractions. The lung contains various CYP enzymes (e.g., CYP2B, CYP2E1, CYP3A) and a high level of flavin-containing monooxygenases (FMOs) [40].
- Incubation Conditions:
- The incubation setup is similar to the intestinal protocol, with a protein concentration of 0.5-1 mg/mL.
- Include an NADPH regenerating system. Consider adding FMO-specific cofactors if relevant.
- Reaction and Analysis: Follow the same quenching, centrifugation, and UHPLC-MS/MS analysis steps as for the intestinal protocol [41].
- Data Analysis: Calculate the degradation half-life of the parent compound to estimate the lung's metabolic capacity.
Protocol: Metabolic Stability in Renal Tissue Preparations
Objective: To evaluate metabolism in the kidney, a key organ for drug elimination that expresses enzymes like CYP4A11, UGTs, and sulfotransferases (SULTs) [39].
Detailed Methodology:
- Tissue Preparation: Use kidney microsomes (for CYP-mediated metabolism) or cytosol (for SULT-mediated metabolism).
- Incubation Conditions:
- For microsomal incubations, use a protein concentration of 0.5-1 mg/mL with an NADPH regenerating system.
- For cytosolic incubations (to assess SULT activity), use a potassium phosphate buffer and include the cofactor PAPS.
- Reaction and Analysis: The process for reaction quenching, sample processing, and LC-MS/MS analysis is consistent with the other tissue protocols [41].
- Data Analysis: Calculate the intrinsic clearance specific to the enzymatic pathway being tested.
Data Presentation: Quantitative Comparison of Metabolic Systems
The following tables summarize key quantitative parameters and controls for different experimental systems used in extrahepatic metabolism studies.
Table 1: Key Parameters for In Vitro Extrahepatic Metabolic Stability Assays
| Parameter | Typical Range (Microsomes/S9) | Key Considerations | Reference Method |
|---|---|---|---|
| Protein Concentration | 0.5 - 1.0 mg/mL | Too high can cause non-specific binding; too low can miss slow metabolism. | Bradford / BCA Assay |
| Incubation Volume | 50 - 200 µL | Must be feasible for multiple time-point sampling. | N/A |
| Substrate Concentration | 1 - 10 µM | Should be well below Km to ensure first-order kinetics. | Stock solution in DMSO/ACN |
| Incubation Time | 0 - 60/120 min | Must include T=0 to establish initial concentration. | Pre-defined time points |
| Half-life (t1/2) | Calculated from slope (k) | In vitro t1/2 = ln(2) / k | Linear regression of Ln(% remaining) vs. time |
| Intrinsic Clearance (Clint) | Calculated | Clint = (0.693 / in vitro t1/2) * (Incubation Volume / Protein Amount) | Derived from t1/2 |
Table 2: Recommended Controls for Extrahepatic Stability Assays
| Control Type | Purpose | Expected Outcome | Interpretation of Deviation |
|---|---|---|---|
| Negative Control (No Cofactor) | Identify non-enzymatic degradation. | Minimal parent loss. | Significant parent loss indicates chemical instability. |
| Positive Control (Tissue-Specific) | Verify metabolic activity of the tissue preparation. | Rapid metabolism of control compound. | Low activity indicates issue with tissue quality/viability. |
| Zero-Time Point Control | Establish baseline parent concentration. | 100% parent compound. | N/A |
| Blank Matrix Control | Assess MS interference from matrix. | No interfering peaks. | Interference requires method adjustment. |
Troubleshooting Common Experimental Challenges
FAQ 1: Our positive control is not metabolizing, indicating low enzyme activity across all tissue types. What could be wrong?
- Solution: This suggests a systemic issue with the assay conditions.
- Verify Cofactor Integrity: Prepare fresh NADPH regenerating system and UDPGA/PAPS solutions. These cofactors are unstable and can degrade upon repeated freeze-thaw cycles or if stored improperly.
- Check Protein Quality and Storage: Ensure the microsomal/S9 preparations have been stored at -80°C and have not undergone multiple freeze-thaw cycles. Use fresh aliquots for each experiment.
- Confirm Protein Concentration: Re-measure the protein concentration to ensure it is within the recommended range.
- Check Incubation Temperature: Verify that the water bath or incubator is maintaining a steady 37°C.
FAQ 2: We observe high variability and poor reproducibility between replicates in our kidney cytosolic assay. How can we improve consistency?
- Solution: This often relates to sample handling and reaction uniformity.
- Thorough Mixing: After adding the cofactor (PAPS for cytosolic assays) to initiate the reaction, vortex the incubation mixture thoroughly and immediately to ensure a uniform reaction start.
- Low-Binding Labware: Peptides and some small molecules can adsorb to plastic surfaces. Use low-binding tubes and tips throughout the assay to minimize sample loss [42].
- Pre-incubation Temperature Equilibration: Ensure all reagents, including the buffer, tissue matrix, and test compound, are fully pre-warmed to 37°C before mixing to start the reaction.
FAQ 3: The parent compound disappearance in lung S9 is very rapid, and we cannot accurately determine the initial rate. How can we adapt the protocol?
- Solution: For rapidly metabolized compounds, modify the incubation parameters to capture the initial linear phase of metabolism.
- Shorten Time Points: Use very short initial time points (e.g., 0, 1, 2.5, 5, 7.5, 10 minutes).
- Reduce Enzyme Concentration: Lower the protein concentration (e.g., to 0.1-0.2 mg/mL) to slow down the reaction rate.
- Decrease Temperature: Perform the incubation at a lower temperature (e.g., 25°C) as a preliminary screen to rank compounds, though this will not provide physiologically relevant Clint values.
FAQ 4: We suspect the formation of unstable metabolites that are degrading in our analytical system, leading to confusing data. How can we investigate this?
- Solution: This is a known challenge, as initial metabolites can be rapidly transformed and not fully captured in vitro [41].
- Stabilize Samples Immediately: Quench samples directly into a stabilization agent. For example, citric acid and sodium sulfite were used successfully to stabilize R14 in pharmacokinetic samples [41].
- Use High-Resolution MS: Employ UHPLC-QTOF MS/MS for metabolite identification. This allows you to detect and characterize transient metabolites based on accurate mass, even without a reference standard [41] [43].
- Trapping Experiments: Consider conducting specific trapping experiments (e.g., with glutathione for reactive metabolites) to intercept and identify unstable intermediates.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Extrahepatic Metabolism Studies
| Reagent / Material | Function in Experiment | Key Considerations for Use |
|---|---|---|
| Tissue Microsomes/S9 | Source of metabolic enzymes from intestine, lung, or kidney. | Confirm species, tissue source, and protein concentration. Avoid repeated freeze-thaw cycles. |
| NADPH Regenerating System | Provides essential cofactor for CYP450 and other Phase I oxidation reactions. | Prepare fresh for each experiment for optimal activity. |
| UDPGA (Uridine 5'-diphosphoglucuronic acid) | Essential cofactor for UGT-mediated glucuronidation (Phase II). | Temperature-sensitive; aliquot and store at -80°C. |
| PAPS (3'-Phosphoadenosine-5'-phosphosulfate) | Essential cofactor for SULT-mediated sulfation (Phase II). | Also temperature-sensitive; prepare fresh from stable salts if possible. |
| Low-Binding Tips & Tubes | Minimizes non-specific adsorption of test compounds to plastic surfaces. | Critical for peptides and lipophilic compounds to ensure accurate recovery [42]. |
| Potassium Phosphate Buffer (pH 7.4) | Provides a physiologically relevant pH environment for the incubation. | Filter sterilize and check pH at incubation temperature (37°C). |
| Stable Isotope-Labeled Internal Standards | Normalizes analytical variability during LC-MS/MS analysis. | Ideal for correcting for sample preparation losses and matrix effects. |
Troubleshooting Guides and FAQs
Common Experimental Issues & Solutions
Problem: High Background Signal
| Possible Source | Recommended Test or Action |
|---|---|
| Insufficient washing | Increase number of washes; add a 30-second soak step between washes; ensure plates are drained completely after washing [44] [45]. |
| Contaminated buffers | Prepare fresh buffers immediately before use [45]. |
| Plate sealers reused | Use a fresh, clean plate sealer for each incubation step to prevent cross-contamination [44] [45]. |
| Substrate exposed to light | Protect substrate solution from light by storing it in a dark place and limiting exposure during the assay [44]. |
Problem: Weak or No Signal
| Possible Source | Recommended Test or Action |
|---|---|
| Reagents not at room temperature | Allow all reagents to sit on the bench for 15-20 minutes at the start of the assay to reach room temperature [44]. |
| Incorrect reagent preparation | Check protocol and calculations; ensure reagents were added in the proper order and prepared to the correct dilution [44] [45]. |
| Expired reagents | Confirm all reagents are within their expiration dates; do not use expired materials [44]. |
| Incorrect plate reader wavelength | Verify the plate reader is set to the correct wavelength/filter for the substrate being used [44]. |
| Capture antibody did not bind to plate | If coating your own plate, ensure you are using an ELISA plate (not a tissue culture plate) and dilute the antibody in PBS [44] [45]. |
Problem: Poor Replicate Data (High Well-to-Well Variation)
| Possible Source | Recommended Test or Action |
|---|---|
| Insufficient or uneven washing | Check that all ports of an automatic plate washer are clean; add a soak step and rotate the plate halfway through washing [45]. |
| Uneven plate coating | Ensure consistent coating and blocking volumes; verify the quality of the assay plate [45]. |
| Improper use of plate sealers | Always use a fresh plate sealer for each incubation step [45]. |
| Wells scratched during pipetting | Use caution when dispensing and aspirating; calibrate automated washers so tips do not touch the well bottom [44]. |
Problem: Poor Assay-to-Assay Reproducibility
| Possible Source | Recommended Test or Action |
|---|---|
| Variations in incubation temperature | Adhere strictly to the recommended incubation temperature; avoid areas with environmental fluctuations [44] [45]. |
| Inconsistent protocol execution | Follow the same protocol meticulously from run to run; avoid modifications [45]. |
| Improper reagent handling | Ensure all reagents are at room temperature before pipetting unless instructed otherwise [45]. |
| Incorrect standard curve dilutions | Double-check calculations and pipetting technique when preparing standard curves [44] [45]. |
Problem: Edge Effects (Uneven staining at plate periphery)
| Possible Source | Recommended Test or Action |
|---|---|
| Uneven temperature across plate | Completely seal the plate during incubations; if using an incubator, place the plate in the center [44] [45]. |
| Evaporation | Always use a plate sealer during incubations to prevent evaporation [44]. |
| Stacked plates | Avoid stacking plates during incubation steps [44]. |
Addressing Low Metabolic Stability & Clearance
FAQ: How can we obtain reliable data for low-clearance compounds in early discovery?
Low-clearance compounds (showing no significant turnover in standard hepatocyte assays) pose a challenge as they can lead to an overprediction of human clearance and an underprediction of half-life [24]. The Hepatocyte Relay Method was developed to address this [24].
Detailed Protocol: Hepatocyte Relay for Low-Clearance Compounds [24]
- Initial Incubation: Incubate the test compound with freshly thawed cryopreserved hepatocytes (e.g., 0.5 million cells/mL) for 4 hours.
- First Relay: After 4 hours, centrifuge the incubation plate and transfer the supernatant to a new plate containing a fresh batch of thawed hepatocytes. Incubate for another 4 hours.
- Subsequent Relays: Repeat the relay process multiple times (e.g., 5 times) to achieve a cumulative incubation time of 20 hours or more while maintaining enzyme competency.
- Sample Analysis: Determine parent compound consumption at each time point using LC-MS/MS to calculate a more accurate intrinsic clearance (CL~int~).
- Data Application: Use the refined CL~int~ data for better in vitro-in vivo correlation (IVIVC), dose projection, and metabolite identification.
FAQ: What strategies can enhance the bioavailability of small-molecule drugs with poor metabolic stability?
Overcoming poor oral bioavailability requires a multi-faceted approach addressing solubility, permeability, and metabolic stability [3].
Experimental Strategies for Bioavailability Optimization [3]
- Solubility Enhancement:
- Method: Salt formation, cocrystallization, amorphous solid dispersions, and particle size reduction (nanonization).
- Protocol: For amorphous solid dispersions, dissolve the drug and polymer carrier in a common solvent, then use spray drying or hot-melt extrusion to create a solid dispersion. Characterize using DSC and PXRD to confirm the amorphous state.
- Lipophilicity Optimization:
- Method: Use medicinal chemistry to optimize the logarithm of the partition coefficient (logP) to a favorable range (typically 1-3) to balance membrane permeability and aqueous solubility. The metric of Ligand-Lipophilicity Efficiency (LLE) is useful here.
- Structural Modification:
- Method: Employ prodrug approaches to mask metabolically labile functional groups, making the parent compound inert until it reaches the systemic circulation.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function |
|---|---|
| ELISA Plate | A specialized microplate with high protein-binding capacity to ensure effective capture antibody coating [44] [45]. |
| Cryopreserved Pooled Hepatocytes | Metabolically competent cells from multiple donors, used in standard metabolic stability assays and the hepatocyte relay method to predict human clearance [24]. |
| LanthaScreen TR-FRET Reagents | Assay kits utilizing time-resolved Förster resonance energy transfer (TR-FRET), ideal for high-throughput screening of kinase targets; using the correct emission filters is critical [46]. |
| Amorphous Solid Dispersion Polymers | Inert polymer carriers (e.g., HPMC-AS, PVP-VA) used to create solid dispersions that enhance the apparent solubility and dissolution rate of poorly soluble compounds [3]. |
| Microplate Washer | Automated instrument for consistent and efficient aspiration and dispensing of wash buffer, crucial for reducing background and variability in plate-based assays [47]. |
| Automated Liquid Handler | (e.g., Microlab STARlet) Executes precise dispensing of reagents or samples via multichannel heads, increasing throughput and reproducibility [47]. |
Workflow Diagrams
▷ Automated ELISA Workcell
▷ Hepatocyte Relay Method
▷ Bioavailability Optimization Pathways
Lead Optimization and Troubleshooting: Strategies to Block Metabolic Soft Spots
FAQs: Addressing Common Experimental Challenges
1. What are metabolic "soft spots" and why is identifying them crucial in drug discovery?
Metabolic soft spots are the specific sites on a drug molecule that are most susceptible to enzymatic modification or degradation. Identifying them is crucial because fast metabolism can lead to poor bioavailability, rapid clearance from the body, and significant drug-drug interactions [48]. Pinpointing these sites allows medicinal chemists to design more stable drug candidates by making targeted structural modifications, thereby optimizing the pharmacokinetic properties of lead compounds [49].
2. My metabolic soft-spot identification (MSSID) assay generates too many secondary metabolites, complicating the analysis. How can I simplify the metabolite profile?
This is a common challenge when using fixed, long incubation times for rapidly metabolized compounds. The solution is to use a single, variable incubation time tailored to the predetermined metabolic stability (half-life, t₁/₂) of each test compound. The goal is to aim for only 20-40% parent compound disappearance, which typically generates one or a few primary metabolites as the major products, minimizing the formation of complex secondary metabolites [48]. For example:
- For a high-clearance compound like saquinavir (t₁/₂ = 2.6 min), use a short incubation of ~4 minutes.
- For a low-clearance compound like mirtazapine (t₁/₂ = 165 min), a longer incubation of ~60 minutes is appropriate [48].
3. How can I obtain more confident metabolite identifications when my compounds are not in spectral libraries?
Confidence in metabolite identification can be significantly improved by using stable isotope labeling or online chemical labeling techniques.
- Stable Isotope Labeling (e.g., TLEMMA): Using precursors labeled with different stable isotopes (e.g., ²H, ¹³C) creates a distinctive isotopic pattern in the mass spectrometer. This pattern helps to unambiguously trace the precursor into its metabolites and drastically reduces the number of false structural candidates—by over 99% compared to unlabeled samples when using a triple-labeling approach [50].
- Online Chemical Labeling (e.g., MCheM): This method uses post-column derivatization reactions to probe for specific functional groups (e.g., amines, electrophiles, carbonyls) in metabolites. The reactivity information serves as an orthogonal data source, which, when integrated with MS/MS data, substantially improves the accuracy of in silico annotation tools [51].
4. Are there non-chromatographic methods for a rapid, high-throughput initial assessment of metabolic stability?
Yes, fluorescence-based methods like the Metabolizing Enzyme Stability Assay Plate (MesaPlate) have been developed as an alternative to LC-MS/MS. This approach quantifies the depletion rates of universal cofactors in the cytochrome P450 reaction (NADPH and oxygen) using fluorescence. When combined with antioxidant enzymes to simplify the reaction kinetics, these depletion rates can be used to accurately calculate the rate of substrate oxidation. This method is well-suited for high-throughput screening due to its lower cost and parallel analysis capabilities, though it is primarily applicable to P450-mediated metabolism [7].
5. What are the key types of metabolites that should raise safety flags during identification?
During metabolite profiling, you should pay special attention to four types of metabolites [52]:
- Active Metabolites: Those that exert a pharmacological effect similar to the parent drug, which can complicate the dose-response relationship.
- Reactive Metabolites: Electrophilic species that can covalently bind to proteins or DNA, potentially leading to toxicity.
- Disproportionate Human Metabolites: Metabolites with exposures in humans that are substantially higher (>10% of total drug-related exposure) than in the animal species used in toxicology studies.
- Unique Human Metabolites: Metabolites detected in humans but absent in animal models. Both disproportionate and unique human metabolites may require additional, costly safety testing.
Troubleshooting Guides
Issue 1: Poor-Quality MS/MS Spectra for Low-Abundance Metabolites
Problem: Low-abundance metabolites yield poor-quality MS/MS spectra, making structural elucidation difficult.
Solution: Optimize Data Acquisition with Generic Methods and Advanced Data Mining
- Implement Generic DDA Methods: Use generic, data-dependent acquisition (DDA) methods on high-resolution mass spectrometers (e.g., Q-TOF, Qtrap) that are not pre-optimized for the parent compound. These methods can continuously acquire high-quality MS/MS spectra for all ions above a certain threshold, capturing data for metabolites as they elute [48].
- Employ Advanced Data Mining: Use data processing techniques post-acquisition to find metabolite signals. These include:
- Mass Defect Filter (MDF): Filters data based on the small mass difference between the parent and metabolites.
- Neutral Loss Filter (NLF): Looks for common fragments lost from the parent ion.
- Product Ion Filter (PIF): Searches for characteristic product ions.
- Background Subtraction: Automatically subtracts spectra from control samples [48] [53].
- Leverage Ion Identity Networking: For chemical labeling workflows (like MCheM), use software that can correlate a precursor ion with its derivatization products based on co-elution, consolidating this information to enhance downstream annotation [51].
Issue 2: Discrepancies Between In Vitro and In Vivo Metabolic Clearance
Problem: The intrinsic clearance (CLint) calculated from in vitro systems (e.g., human liver microsomes) does not accurately predict in vivo clearance.
Solution: Understand and Account for the Limitations of In Vitro Systems Consider these common causes for discrepancy and adjust your experimental design or interpretation accordingly [49]:
| Potential Cause of Discrepancy | Impact on Predicted CLint | Mitigation Strategy |
|---|---|---|
| Extrahepatic Metabolism | Underprediction of in vivo CLint | Consider using additional systems (e.g., intestinal S9 fractions) if extrahepatic metabolism is suspected. |
| Active Transport | Over- or under-estimation depending on influx/efflux | Use intact hepatocyte models, which retain some transport functions, in addition to microsomes. |
| Lack of Equilibrium | In vivo CLint lower than in vitro CLint | This is a system limitation; use scaling factors derived from validation with known compounds. |
| Inter-individual Variability | Unreliable or highly variable data | Use pooled human liver microsomes or hepatocytes from multiple donors to average out variability. |
Issue 3: Inefficient Workflow for High-Throughput Soft-Spot Analysis
Problem: The standard MSSID workflow is too slow to keep pace with lead optimization.
Solution: Adopt an Integrated, High-Throughput Workflow Streamline the process from incubation to reporting with these steps [48]:
- Pre-determine Metabolic Stability: First, run a quick metabolic stability assay to establish the half-life (t₁/₂) for each compound.
- Variable Time Incubation: Incubate compounds at low concentration (e.g., 3-5 µM) in human liver microsomes for a single, variable time point based on their t₁/₂ to achieve 20-40% parent loss.
- LC/UV/MS Analysis: Analyze samples using an LC system coupled to both a photodiode array (PDA/UV) detector and a high-resolution mass spectrometer.
- Utilize LC/UV for Quantitation: Use the UV chromatogram (which is more quantitative and less susceptible to ionization differences than MS) to estimate the relative abundances of the major metabolites.
- Focus MS Efforts: Direct your MS/MS structural characterization efforts only on the one or two most abundant primary metabolites identified by UV.
The following workflow diagram illustrates this efficient process:
Experimental Protocols & Technical Data
Detailed Protocol: MSSID Assay with Single Variable Incubation Time
This protocol is designed for high-throughput soft-spot identification using human liver microsomes (HLM) [48].
Key Reagent Solutions:
- Human Liver Microsomes (HLM): Source of metabolic enzymes. Pooled from multiple donors is recommended to average variability.
- NADPH Regenerating System: Provides essential cofactors for cytochrome P450 enzymes.
- Compounds: Test compounds and positive controls (e.g., dextromethorphan, midazolam).
- Stop Solution: Typically an organic solvent like acetonitrile or methanol to quench the reaction.
- Incubation Buffer: Potassium phosphate buffer (pH 7.4).
Procedure:
- Pre-incubation: Mix the test compound (final concentration 3-5 µM) with HLM (e.g., 0.5-1.0 mg/mL protein concentration) in incubation buffer. Pre-warm the mixture for ~5-10 minutes.
- Initiate Reaction: Start the metabolic reaction by adding the NADPH regenerating system.
- Incubate: Allow the reaction to proceed for a single, predetermined time (see table below for guidance) in a shaking water bath at 37°C.
- Quench: At the end of the incubation period, add a stop solution (e.g., cold acetonitrile) to denature enzymes and halt the reaction.
- Sample Preparation: Centrifuge the quenched samples to precipitate proteins. Transfer the supernatant for LC-MS analysis.
- Analysis: Analyze the samples using LC-UV/MS with a generic data-dependent MS/MS acquisition method.
Incubation Time Guidance Based on Metabolic Stability:
| Metabolic Stability Category | Half-life (t₁/₂) Example | Target Parent Loss | Suggested Incubation Time |
|---|---|---|---|
| High Clearance | 1 - 5 min (e.g., Saquinavir) | 20-40% | 1 - 5 min |
| Medium Clearance | 5 - 15 min (e.g., Verapamil) | 20-40% | 5 - 15 min |
| Low Clearance | >60 min (e.g., Mirtazapine) | 20-40% | 30 - 60 min |
Comparison of Advanced Metabolite Identification Techniques
For challenging identification tasks, advanced techniques can be employed. The table below summarizes two powerful approaches.
| Technique | Key Principle | Key Advantage | Typical Application |
|---|---|---|---|
| TLEMMA [50] | Uses triple stable isotope-labeled precursors (e.g., ¹³C, ²H, ¹⁵N). | Reduces false candidate structures by >99% vs. unlabeled; enables precise network mapping. | De novo identification and reconstruction of metabolic pathways. |
| Multiplexed Chemical Metabolomics (MCheM) [51] | Employs online, post-column derivatization reactions to probe functional groups. | Provides orthogonal structural data (e.g., "contains a primary amine"), improving annotation rankings. | Functional group discovery and enhancing confidence in MS/MS-based annotation. |
The workflow for integrating orthogonal data from techniques like MCheM is shown below:
The strategic incorporation of halogen atoms, particularly fluorine and chlorine, into drug candidates is a cornerstone of modern medicinal chemistry for overcoming poor metabolic stability. This approach functions primarily by sterically blocking oxidative metabolic hotspots on a molecule, thereby increasing its half-life and improving its pharmacokinetic profile. A survey of FDA approvals in 2021 underscores the critical role of this strategy, revealing that 14 of the 50 new chemical entities contained halogen atoms, with fluorine appearing in eight drugs and chlorine in four, highlighting their prevalence in successful drug development campaigns [54].
The effectiveness of halogens stems from their unique physicochemical properties. Fluorine, the most electronegative element, and chlorine, which occupies an intermediate position in the halogen series, can be used to block susceptible sites of metabolism through a combination of steric bulk and electronic effects. When installed on aromatic rings or aliphatic carbons, these atoms can directly impede the approach and catalytic activity of cytochrome P450 enzymes and other oxidative systems, preventing the formation of metabolically labile positions and enhancing the stability of the drug candidate [55] [54].
Scientific Foundation: Mechanisms of Blocking Oxidation
How Halogens Sterically and Electronically Block Metabolism
The incorporation of halogen atoms serves as a strategic defense against oxidative metabolism through two primary, interconnected mechanisms:
- Steric Shielding: The halogen atom, with its significant van der Waals radius, creates a physical barrier that sterically hinders the approach of oxidative enzymes to vulnerable C-H bonds, particularly at benzylic, allylic, or aromatic positions. For instance, replacing a hydrogen (van der Waals radius of ~1.20 Å) with a fluorine (radius of ~1.47 Å) or a larger chlorine atom introduces greater steric congestion at the site of metabolism [54].
- Electronic Deactivation: The strong electron-withdrawing nature of halogens, especially fluorine, can decrease the electron density of adjacent C-H bonds. This electronic effect makes hydrogen atom abstraction by metal-oxo species in enzyme active sites (a common oxidative mechanism) more difficult, thereby reducing the rate of oxidation [55].
A common and elegant application is the blockade of benzylic positions, which are highly susceptible to oxidation. Replacing a benzylic CH2 group with an oxygen atom or, more commonly, introducing a halogen atom onto the benzylic carbon, can dramatically enhance metabolic stability [55].
Comparative Physicochemical Properties of Key Halogens
The choice of halogen is critical, as each imparts distinct properties that influence both the metabolic stability and the overall drug-like character of the molecule. The table below summarizes the key attributes of fluorine and chlorine, the two most frequently used halogens in drug design.
Table 1: Key Properties of Fluorine and Chlorine in Drug Design
| Property | Fluorine | Chlorine | Impact on Drug Design |
|---|---|---|---|
| Electronegativity (Pauling) | 4.0 (Highest) | 3.2 | Fluorine strongly withdraws electron density, lowering the pKa of neighboring functional groups [54]. |
| Van der Waals Radius (Å) | ~1.47 | ~1.75 | Chlorine provides greater steric bulk for blocking metabolic sites [54]. |
| C-X Bond Strength | Very High (e.g., C-F ~485 kJ/mol) | High (C-Cl ~327 kJ/mol) | C-F bonds are highly stable and resistant to metabolic cleavage [54]. |
| Common Role in Metabolism | Metabolic Blockade, Modulating Lipophilicity | Metabolic Blockade, Bioisostere for Methyl Group | Chlorine is often used as a bioisosteric replacement for a methyl group to alter in vivo metabolism [54]. |
| Halogen Bonding Potential | Weak | Good acceptor | Chlorine can form favorable halogen bonds with target proteins [54]. |
Troubleshooting Guide: FAQs on Halogen Incorporation
FAQ 1: Why did the incorporation of a halogen fail to improve the metabolic stability of my compound in human liver microsomes?
Answer: Several factors could be at play. First, the halogen may not have been placed at the correct metabolic soft spot. It is essential to first identify the primary site of oxidation through metabolite identification (MetID) studies before initiating a blocking strategy. Second, the introduction of the halogen might have inadvertently created a new metabolic soft spot elsewhere in the molecule by shifting the molecule's electronic profile. Third, the metabolism may be proceeding via a pathway that is not susceptible to steric blocking, such as conjugation (Phase II metabolism). Finally, the halogen itself could be subject to metabolic displacement if it is on an activated aromatic system.
FAQ 2: How do I choose between fluorine and chlorine for blocking a specific site?
Answer: The choice is a trade-off. Fluorine is often preferred due to its small size and superior ability to form strong, stable bonds with carbon, making it resistant to metabolic cleavage. Its high electronegativity is excellent for electronic deactivation. Chlorine, being larger, provides greater steric hindrance and is a better halogen bond acceptor, which can be beneficial for target affinity. However, its larger size can sometimes lead to undesirable steric clashes with the target protein, reducing potency. A chlorine atom is also more metabolically labile than fluorine in certain contexts. The decision should be guided by empirical testing of both options in parallel, assessing both metabolic stability and potency.
FAQ 3: What are the potential downsides or risks of using halogen atoms in my drug candidate?
Answer: While highly beneficial, halogen incorporation carries risks. A key risk is a loss of target potency if the halogen introduces unfavorable steric clashes or electronic effects at the binding site. It can also unfavorably alter the lipophilicity (log P/D) of the molecule, potentially reducing aqueous solubility or increasing off-target binding. In rare cases, certain halogenated compounds can be susceptible to bioactivation, forming reactive metabolites. It is crucial to monitor for this during lead optimization. Furthermore, the synthetic chemistry for introducing halogens, particularly fluorine in complex electronic environments, can be challenging and costly.
FAQ 4: My halogenated compound shows improved microsomal stability, but poor aqueous solubility. What can I do?
Answer: This is a common challenge, as halogens often increase molecular lipophilicity. To address this, consider fine-tuning the rest of the molecule to counterbalance the lipophilicity increase. This can be achieved by introducing hydrophilic functional groups (e.g., polar heterocycles, amines, alcohols) or ionizable centers in other parts of the molecule. Alternatively, formulation strategies, such as the use of amorphous solid dispersions or complexing agents, can be explored in later development stages to overcome solubility limitations.
Essential Experimental Protocols
Protocol 1: Forced Degradation Study to Probe Oxidative Susceptibility
Purpose: To identify the intrinsic oxidative susceptibility and potential degradation pathways of a drug substance under stressed conditions, informing where halogen incorporation might be most effective [56] [57].
Materials:
- Drug Substance: High-purity compound.
- Oxidizing Agents: 3% w/v Hydrogen peroxide (H₂O₂), 0.2% w/v Azobisisobutyronitrile (AIBN) for radical initiation.
- Solvents: High-Performance Liquid Chromatography (HPLC)-grade water, acetonitrile.
- Buffers: 0.05 M Phosphate buffer, pH 3.0, 7.0, and 9.0.
- Equipment: HPLC system with Diode Array Detector (DAD) coupled to a Mass Spectrometer (LC-MS/MS), controlled temperature bath or oven.
Methodology:
- Solution Preparation: Prepare separate solutions of the drug substance (e.g., 1 mg/mL) in the following conditions:
- Acidic Oxidative: Phosphate buffer pH 3.0 + 3% H₂O₂
- Neutral Oxidative: Phosphate buffer pH 7.0 + 3% H₂O₂
- Basic Oxidative: Phosphate buffer pH 9.0 + 3% H₂O₂
- Radical Mediated: Ethanol/water mixture + 0.2% AIBN
- Incubation: Incubate all solutions in a controlled temperature bath or oven at 40°C and 60°C. Withdraw samples at 0, 1, 3, 7, and 14 days.
- Analysis: Quench the reactions if necessary (e.g., with methionine for peroxide) and analyze by LC-MS/MS.
- Data Interpretation: Monitor the disappearance of the parent drug and the emergence of degradation products. Use high-resolution mass spectrometry to elucidate the structure of major degradants, pinpointing the most labile sites for oxidative attack.
Protocol 2: Metabolic Stability Assessment in Liver Microsomes
Purpose: To quantitatively evaluate the improvement in metabolic stability of a halogenated compound compared to its non-halogenated parent.
Materials:
- Test Compounds: Non-halogenated lead and halogenated analog.
- Biological Matrix: Pooled human or rat liver microsomes (e.g., 0.5 mg/mL protein concentration).
- Cofactor: 1 mM NADPH regenerating system.
- Buffers: 0.1 M Phosphate Buffered Saline (PBS), pH 7.4.
- Quenching Solvent: Ice-cold acetonitrile with internal standard.
- Equipment: Liquid handling robot, shaking water bath, LC-MS/MS system.
Methodology:
- Incubation: Pre-incubate microsomes with test compound (1 µM) in PBS at 37°C for 5 minutes. Initiate the reaction by adding the NADPH regenerating system. Run parallel control incubations without NADPH.
- Time Points: Withdraw aliquots at specific time points (e.g., 0, 5, 15, 30, 45, 60 minutes) and quench immediately with ice-cold acetonitrile.
- Sample Analysis: Centrifuge the quenched samples to precipitate proteins. Analyze the supernatant by LC-MS/MS to determine the peak area ratio of parent compound to internal standard over time.
- Data Analysis: Plot the natural logarithm of the parent compound concentration remaining versus time. The slope of the linear phase is the elimination rate constant (k). Calculate the in vitro half-life (t₁/₂ = 0.693/k) and intrinsic clearance (CLint). A longer half-life and lower clearance for the halogenated analog indicate successful metabolic blocking.
Diagram 1: Experimental Workflow for Halogen-Based Stabilization. This flowchart outlines the key steps from identifying a metabolic soft spot to evaluating the success of a halogen incorporation strategy.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents and Materials for Metabolism Blocking Studies
| Reagent / Material | Function / Purpose | Example Use Case |
|---|---|---|
| Pooled Liver Microsomes (Human/Rat) | In vitro system for predicting hepatic metabolic clearance and identifying metabolites. | Assessing intrinsic clearance and metabolic pathway shifts after halogenation [55]. |
| NADPH Regenerating System | Provides essential cofactors for cytochrome P450 enzyme activity. | Essential for all metabolic stability incubations with liver microsomes or hepatocytes. |
| Hydrogen Peroxide (H₂O₂) | Oxidizing agent for forced degradation studies. | Stressing the drug substance to model oxidative degradation pathways [56]. |
| LC-HRMS / MS-MS System | Separation, detection, and structural elucidation of drugs and their metabolites/degradants. | Identifying sites of oxidation and confirming structure of halogenated analogs [56]. |
| Selectfluor Reagent | Electrophilic fluorine source ("F⁺") for fluorination of electron-rich systems. | Synthesizing fluorinated analogs for metabolic blocking [54]. |
In modern drug discovery, overcoming poor metabolic stability is a critical hurdle that directly impacts a compound's efficacy, safety, and eventual clinical success. Metabolic instability leads to rapid clearance from the body, resulting in insufficient exposure at the target site and poor bioavailability. Two fundamental strategies employed to address this challenge are reducing lipophilicity and blocking metabolically labile groups. While reducing lipophilicity (measured as LogD₇.₄) is a common approach to decrease metabolic clearance, this strategy alone often proves insufficient without simultaneously addressing specific vulnerable sites on the molecule where biotransformation occurs. This technical support guide examines the interplay between these strategies through real-world case studies and provides troubleshooting advice for researchers navigating these complex optimization campaigns.
Theoretical Framework: Why Lipophilicity Reduction Alone Often Fails
The Lipophilicity-Half-Life Paradox
A comprehensive analysis of pharmacokinetic data reveals a surprising relationship between lipophilicity and half-life that often challenges conventional medicinal chemistry wisdom.
Table 1: Relationship Between Lipophilicity and Pharmacokinetic Parameters in Neutral Compounds
| LogD₇.₄ Range | Impact on Clearance (CLu) | Impact on Volume of Distribution (Vd,ss,u) | Net Effect on Half-Life |
|---|---|---|---|
| <1 | Low | Low | Variable |
| 1-2.5 | Moderate increase | Moderate increase | Minimal change |
| 2.5-4 | Significant increase | Significant increase | Minimal or negative impact |
| >4 | High | High | Often reduced |
Data from Genentech's internal dataset of 4,767 neutral compounds with rat pharmacokinetic data demonstrates that both clearance and volume of distribution tend to increase similarly with lipophilicity, resulting in minimal net effect on half-life [58]. This explains why simply lowering LogD without addressing specific metabolic soft spots frequently fails to improve half-life meaningfully.
Key Principles for Successful Optimization
- Clearance-Volume Interplay: Hepatic clearance and volume of distribution are often correlated properties similarly affected by lipophilicity [58].
- Metabolic Soft-Spot Focus: Successful half-life extension requires targeted modification of specific structural features prone to metabolism, not just global lipophilicity reduction [58].
- Multiparameter Optimization: Effective metabolic stability improvement must balance potency, selectivity, and other drug-like properties rather than focusing solely on single parameters [26].
Essential Research Reagent Solutions
Table 2: Key Experimental Systems for Metabolic Stability Assessment
| Research Reagent | Metabolic Enzyme Coverage | Primary Applications | Advantages |
|---|---|---|---|
| Liver Microsomes | Phase I (CYP450, FMO) | Intrinsic clearance measurement, metabolite identification | Cost-effective, standardized protocols [5] |
| Liver S9 Fraction | Phase I & II (UGT, SULT, GST) | Comprehensive metabolic stability assessment | Broader enzyme coverage than microsomes [5] [59] |
| Hepatocytes | Full hepatic metabolism complement | Physiologically relevant stability assessment | Maintain cellular integrity and cofactors [5] |
| Liver Cytosol | Cytosolic enzymes (AO, GST) | Specific non-microsomal metabolic pathway evaluation | Targeted assessment of cytosolic metabolism [5] |
| Recombinant CYP Enzymes | Individual CYP isoforms | Enzyme-specific metabolic pathway identification | Precise reaction phenotyping [7] |
Experimental Protocols for Metabolic Stability Assessment
High-Throughput Metabolic Stability Screening Using MesaPlate Technology
The Metabolizing Enzyme Stability Assay Plate (MesaPlate) provides a fluorescence-based alternative to traditional LC-MS methods for rapid metabolic stability screening [7].
Protocol Steps:
- Reaction Setup: Incubate test compounds with P450 enzymes (Baculosomes or human liver microsomes) in the presence of superoxide dismutase and catalase
- Cofactor Monitoring: Simultaneously measure NADPH and oxygen depletion rates using intrinsic NADPH fluorescence and commercial oxygen probes
- Rate Calculation: Apply simplified rate equation to calculate substrate depletion from cofactor consumption rates
- Data Analysis: Determine Michaelis-Menten parameters (Kₘ, kcat) from substrate concentration-dependent depletion rates
Troubleshooting FAQ:
- Q: How does this method handle fluorescent compounds that may interfere with detection? A: Spectral contributions from overlapping fluorophores can be distinguished using well-established techniques, making the method suitable for most compounds [7].
- Q: What validation has been performed for this method? A: The method has been validated against traditional chromatographic assays for multiple CYP isoforms including CYP3A4, CYP2C9, and CYP2D6, showing excellent correlation [7].
Human Liver S9 Fraction Metabolic Stability Assay
This protocol assesses comprehensive metabolic stability through both Phase I and II metabolism pathways [59].
Detailed Methodology:
- Incubation Preparation:
- Prepare human liver S9 fraction (0.5-1 mg/mL protein concentration)
- Add NADPH-regenerating system (for Phase I) and UDPGA (for Phase II glucuronidation)
- Include test compound at relevant concentrations (typically 1-10 μM)
Reaction Conditions:
- Incubate at 37°C in appropriate buffer (e.g., phosphate buffer, pH 7.4)
- Use shaking platform to ensure proper mixing
- Aliquot samples at predetermined time points (0, 5, 15, 30, 60 minutes)
Reaction Termination:
- Add ice-cold acetonitrile (2:1 v/v) to precipitate proteins
- Centrifuge at high speed (e.g., 14,000 × g for 10 minutes)
- Collect supernatant for analysis
Analytical Assessment:
Data Interpretation:
- Plot natural logarithm of remaining compound versus time
- Calculate half-life from slope of linear regression: t₁/₂ = ln(2)/k
- Determine intrinsic clearance: CLᵢₙₜ = (0.693/t₁/₂) × (incubation volume/protein amount)
Case Studies in Metabolic Stability Optimization
Case Study 1: 17β-HSD2 Inhibitors for Osteoporosis Treatment
This case demonstrates systematic optimization of metabolic stability while maintaining target potency [59].
Initial Challenge: Lead compounds exhibited excellent 17β-HSD2 inhibitory potency but poor metabolic stability with half-lives of 4-38 minutes in human liver S9 fraction.
Metabolic Soft-Spot Identification:
- Primary metabolism occurred on thiophene ring and methoxy substituents
- Demethylation of methoxy groups generated phenolic metabolites
- Thiophene oxidation led to reactive intermediates
Optimization Strategy:
- Blocking Labile Groups: Replaced metabolically vulnerable methoxy groups with halogens or cyclic constraints
- Heterocycle Replacement: Substituted thiophene with furan rings to alter electron distribution
- Steric Shielding: Introduced strategically positioned substituents to block enzymatic access to labile sites
Key Structural Modifications and Outcomes:
Table 3: Metabolic Stability Optimization of 17β-HSD2 Inhibitors
| Compound | Core Structure | Key Modifications | Human S9 Half-Life (min) | 17β-HSD2 IC₅₀ (nM) |
|---|---|---|---|---|
| 1 | Thiophene | Unoptimized lead | 4 | 25 |
| 2 | Thiophene | Partial optimization | 38 | 41 |
| 12 | Thiophene | Halogen substitution | >120 | 132 |
| 31 | Furan | Heterocycle replacement | 95 | 35 |
| 40 | Thiophene | Multiple blocking groups | >120 | 58 |
Successful Outcome: Compound 12 achieved significantly improved metabolic stability (half-life >120 minutes) while maintaining acceptable potency (IC₅₀ = 132 nM), representing a promising preclinical candidate [59].
Case Study 2: Strategic Use of Halogen Substitution
Analysis of matched molecular pairs provides statistical validation of effective metabolic stability transformations.
Table 4: Success Rates of Different Transformation Strategies for Half-Life Improvement
| Transformation Strategy | Probability of T₁/₂ Improvement | Typical Lipophilicity Change (ΔLogD₇.₄) |
|---|---|---|
| Improve metabolic stability without decreasing lipophilicity | 82% | Neutral to positive |
| General metabolic stability improvement | 67% | Variable |
| Decrease lipophilicity alone | 30% | Negative |
Most Effective Transformations:
- Hydrogen to Halogen Substitution: Increased metabolic stability despite increased lipophilicity
- Methyl to Fluorine Replacement: Simultaneously decreased lipophilicity and improved metabolic stability
- Cyclization Strategies: Created conformational constraints that blocked enzymatic access
A notable example from published literature demonstrates substitution of a metabolically labile methyl group with fluorine, reducing lipophilicity while considerably improving metabolic stability and extending half-life in rats from 3.5 to 220 hours [58].
Troubleshooting Guide: Common Experimental Challenges
FAQ 1: Why did reducing lipophilicity not improve my compound's half-life as expected?
Problem: This common issue typically arises from the interconnected nature of clearance and volume of distribution. Solution:
- Perform matched molecular pair analysis to identify transformations that improve metabolic stability without necessarily decreasing lipophilicity [58]
- Focus on addressing specific metabolic soft spots identified through metabolite identification studies
- Consider strategic introduction of halogens or cyclic constraints rather than simply adding polar groups
FAQ 2: How can I efficiently identify metabolic soft spots in my lead series?
Problem: Traditional metabolite identification requires extensive resource investment. Solution:
- Implement rapid microsomal stability screening with high-flow-rate extraction and capillary LC-MS for faster analysis [60]
- Use solid-phase extraction-MS as a higher-throughput alternative to HPLC-MS [61]
- Apply fluorescence-based methods like MesaPlate for initial high-throughput screening [7]
FAQ 3: What analytical approaches can accelerate metabolic stability assessment?
Problem: LC-MS analysis creates bottlenecks in high-throughput screening. Solution:
- Implement solid-phase extraction-MS methods reducing analysis time from 2.5 minutes to 24 seconds per sample [61]
- Apply high-flow-rate extraction coupled to capillary LC-MS for simultaneous high sensitivity and throughput [60]
- Utilize fluorescence-based methods avoiding chromatography entirely for rapid screening [7]
Visualization of Optimization Strategies
Figure 1: Strategic workflow for optimizing metabolic stability, demonstrating the superiority of combined approaches over lipophilicity reduction alone.
Successful optimization of metabolic stability requires moving beyond simplistic lipophilicity reduction to targeted strategies that address specific metabolic vulnerabilities. The case studies presented demonstrate that blocking labile groups through strategic structural modifications—including halogen substitution, heterocycle replacement, and steric shielding—provides more reliable half-life improvement than global lipophilicity reduction alone. Emerging technologies including high-throughput fluorescence-based screening methods, advanced analytical techniques, and computational prediction tools are accelerating this optimization process. By adopting these systematic approaches and learning from successful case studies, researchers can more effectively navigate the complex challenge of metabolic stability optimization in drug development.
Addressing Vendor-Related Variability in Liver Microsomes and Reagents
Why is vendor-related variability a critical issue in metabolic stability studies?
Vendor-related variability is a critical issue because inconsistent reagent quality can directly compromise the reliability of your metabolic stability data, leading to flawed predictions of a drug's in vivo performance. This can mislead lead optimization efforts and contribute to costly late-stage failures [62] [63].
Discrepancies between vendor products can create a significant disconnect between in vitro results and in vivo outcomes. One study documented an "Event" where lead compounds showed high stability in Tier I and Tier II assays using one vendor's rat liver microsomes (RLMs), but then exhibited rapid clearance in subsequent rat pharmacokinetic studies. Metabolite identification (Met ID) studies traced the discrepancy to the microsome vendor; the original vendor's RLMs produced 10–30-fold lower amounts of a key oxidative metabolite compared to a different vendor's RLMs [62].
How can I systematically identify vendor-related variability in my experiments?
A systematic approach involves monitoring for unexpected results and conducting direct comparative experiments. The workflow below outlines the key steps for identifying and diagnosing potential vendor-related issues.
Key steps in the diagnostic workflow include:
- Check for Experimental Disconnects: The primary red flag is a compound that performs well in metabolic stability assays (e.g., long half-life) but shows rapid clearance in in vivo pharmacokinetic studies [62].
- Conduct Side-by-Side Comparison: Incubate your test compounds with liver microsomes or other critical reagents from different vendors under identical experimental conditions [62] [63].
- Perform Metabolite Identification (Met ID): This is a crucial step. As the case study revealed, the "Event" compounds generated a major oxidative metabolite in one vendor's microsomes that was only present in trace amounts in another's. Use UPLC-MS/MS analysis to characterize and compare metabolite profiles across vendors [62].
- Analyze for Significant Differences: Look for statistically significant differences in key parameters like half-life (t₁/₂), intrinsic clearance (CLᵢₙₜ), and metabolite formation [62].
What quantitative impact can vendor choice have on metabolic stability data?
Vendor choice can significantly alter the metabolic stability classification of compounds. An analysis of Tier I (single-point) and Tier II (multi-point) metabolic stability data revealed that the frequency of substantial discrepancies increases when different vendors are used for the two tiers [62].
The table below summarizes the frequency of half-life (t₁/₂) differences when comparing data generated using microsomes from the same vendor versus different vendors.
| Comparison Scenario | Vendor Relationship | % Compounds with >2-fold t¹/² difference | % Compounds with >3-fold t¹/² difference |
|---|---|---|---|
| Tier I vs. Tier II (Pre-Event) | Same Vendor (Corning vs. Corning) | 9.5% | 3.4% |
| Tier I vs. Tier II (Post-Event) | Different Vendors (Corning vs. Xenotech) | 12.5% | 5.4% |
Source: Adapted from PMC10840824 [62].
What is a verified experimental protocol to assess vendor variability?
This detailed multi-point metabolic stability assay protocol is designed to systematically compare different lots or vendors of liver microsomes.
Detailed Methodology for Multi-Point Metabolic Stability Assay [62]:
- Test System: Liver microsomes (e.g., from vendors like Corning-Gentest or Xenotech). The microsomal lot number, species, and donor pool should be meticulously documented.
- Incubation Conditions:
- Microsomal Protein Concentration: 0.5 - 1 mg/mL.
- Compound Concentration: Typically 1-10 µM.
- Cofactor: NADPH regeneration system.
- Buffer: 100 mM phosphate buffer, pH 7.4.
- Temperature: 37°C.
- Time Points: 0, 5, 10, 15, 30, and 60 minutes.
- Reaction Termination: The reaction is stopped by transferring an aliquot of the incubation mixture into a pre-prepared volume of ice-cold acetonitrile containing an internal standard.
- Sample Analysis: Centrifuge the quenched samples and analyze the supernatant using LC-MS/MS to determine the percent remaining of the parent compound over time.
- Data Analysis: The natural logarithm of the percent remaining is plotted against time. The slope of the linear regression is used to calculate the in vitro half-life (t₁/₂ = -0.693/slope) and intrinsic clearance [62] [63].
What are the essential reagents and materials for these experiments?
A successful experiment requires carefully selected and managed critical reagents. The following table lists key materials and their functions.
Research Reagent Solutions
| Reagent/Material | Function & Importance | Management Considerations |
|---|---|---|
| Liver Microsomes | Enzyme source for metabolic reactions; the primary source of vendor variability. | Document vendor, species, lot number, and donor pool. Conduct side-by-side comparisons for critical projects [62] [63]. |
| NADPH Regeneration System | Provides essential cofactors for cytochrome P450 enzyme activity. | Use a consistent, high-quality source and preparation method to avoid introducing variability from this critical component. |
| Test Compound | The drug candidate being evaluated for metabolic stability. | Purity and stability of the compound must be verified, as these can also impact results. |
| Analytical Standards | Pure compounds used for calibration and quantification in LC-MS/MS. | Essential for generating reliable and reproducible quantitative data [64]. |
| Capture Antibodies | Used in immunocapture assays or LC-MS for specific analyte isolation. | Classified as critical reagents; require careful lifecycle management and bridging studies during lot changes [65] [64]. |
What is the best practice strategy for managing critical reagents?
A proactive and documented strategy is essential for managing all critical reagents, including liver microsomes, throughout the drug development lifecycle [65] [64]. The following workflow outlines a robust management procedure.
Core components of this strategy include:
- Characterization and Documentation: Thoroughly document the source, identity, concentration, and functional characteristics (e.g., binding affinity) of all critical reagents [64].
- Establish a Stable Supply: Procure or produce critical reagents in sufficient quantity, preferably for the entire lifespan of a clinical study, to minimize lot changes [64].
- Plan for Lot Changes: Implement a "bridging testing" protocol. When a new lot is introduced, conduct a minimum of three validation runs to compare its performance against the original lot. If assay performance is altered, full or partial re-validation may be required [65].
- Monitor Stability and Expiry: Define initial stability claims based on experimental data. Any extension of a reagent's expiry date should be a data-driven decision [65] [64].
Core Concepts: The Principles of Holistic DMPK Optimization
Why is a holistic approach critical in modern drug discovery?
Modern small molecule drug discovery has never been as exciting—or bewildering—as it is today. While the goal of identifying a safe and efficacious drug has not changed, the process has become increasingly complex over the past 30 years. Success in contemporary drug discovery hinges on using multiple drug design approaches for multi-parameter optimization (MPO) based on the goal and stage of the drug discovery program [66].
Holistic Drug Design (HDD) is defined as the strategic use of orthogonal, complementary, or synergistic drug design approaches for MPO. This approach recognizes that optimizing metabolic stability in isolation is insufficient; it must be balanced with other critical properties including solubility, permeability, potency, and selectivity [66]. When DMPK scientists, biologists, pharmacologists, and medicinal chemists collaborate through in vitro, in vivo, and in silico methods, they achieve three distinct goals:
- Identify and progress drug candidates with the best overall drug-like profiles
- Remove the most toxic drugs from the portfolio prior to human interaction
- Establish a clear and translational risk profile to enable clinical trial designs [67]
What are the key DMPK properties that must be balanced with metabolic stability?
The table below summarizes the core DMPK properties that must be optimized alongside metabolic stability:
Table 1: Key DMPK Properties in Holistic Optimization
| Property | Impact on Drug Performance | Optimal Range/Risk |
|---|---|---|
| Metabolic Stability | Determines elimination rate, half-life, and bioavailability [68] | Low stability → rapid clearance, short half-life [67] |
| Solubility | Affects absorption and bioavailability; poor solubility can cause inaccurate biological data [3] | High solubility needed for adequate dissolution [3] |
| Permeability | Influences absorption through biological membranes; affected by lipophilicity [69] [3] | Balanced permeability needed for adequate absorption [69] |
| Lipophilicity (LogP/LogD) | Impacts membrane permeability, solubility, and metabolism; high lipophilicity can increase metabolic clearance [3] [70] | Optimal range: LogP 1-3 (general), 2-4 (CNS drugs) [3] |
| Plasma Protein Binding | Determines free, pharmacologically active drug fraction [69] | High binding reduces free drug concentration [69] |
| Transporter Interactions | Influences distribution and excretion via influx/efflux transporters [69] | P-gp efflux can limit bioavailability [69] |
Experimental Protocols: Integrated Methodologies for Holistic Assessment
What does a fully integrated DMPK screening workflow look like?
AstraZeneca has developed an integrated and automated assay panel (DMPK Wave 1) that provides weekly data on lipophilicity, solubility, human plasma protein binding, and metabolic stability in both rat hepatocytes and human liver microsomes [71]. This robust screening strategy runs on a weekly basis and enables optimization of structure-activity relationships in parallel with DMPK properties to allow efficient and informed decision making.
Table 2: Comprehensive DMPK Assay Panel Specifications
| Assay Type | Biological System/Technique | Key Parameters Measured | Throughput Capacity |
|---|---|---|---|
| Metabolic Stability | Human liver microsomes, rat hepatocytes [71] [68] | Half-life, intrinsic clearance [68] | 200,000+ compounds per year [68] |
| Solubility | Aqueous buffer systems [71] | Kinetic and thermodynamic solubility [71] | High-throughput, 96-well format [71] |
| Lipophilicity | 1-Octanol/water partitioning [71] | LogD at pH 7.4 [71] | Fully automated [71] |
| Plasma Protein Binding | Human plasma [71] | Free fraction determination [71] | Ultraperformance LC-MS/MS readout [71] |
| Permeability | Caco-2 cells, PAMPA [69] | Apparent permeability, efflux ratio [69] | High-throughput compatible [69] |
How is metabolic stability properly evaluated in vitro?
Metabolic stability assays are a set of in vitro tests used to evaluate the elimination rate of a drug candidate metabolized by enzymes in the body. These assays are designed to evaluate the potential of a drug candidate to be metabolized into active, inactive, or toxic metabolites, which can have implications for its efficacy and safety [68].
Protocol: Liver Microsomal Stability Assay
- Biological Matrix: Liver microsomes obtained from liver tissue homogenates by differential centrifugation [68]
- Key Enzymes Present: Rich in various metabolic enzymes, especially CYP450 enzymes [68]
- Incubation Conditions: Compound incubated with liver microsomes and NADPH cofactor at 37°C [68]
- Time Points: Multiple time points (e.g., 0, 5, 15, 30, 45, 60 minutes) [68]
- Analysis: LC-MS/MS measurement of parent compound remaining at each time point [71]
- Parameters Calculated: Half-life (T½) and intrinsic clearance (CLint) [68]
Protocol: Hepatocyte Stability Assay
- Biological Matrix: Fresh or cryopreserved hepatocytes [68]
- Key Advantage: Maintains complete cellular structure with more complete metabolic enzyme system and coenzyme factors [68]
- Incubation Conditions: Compound incubated with viable hepatocytes in suspension [68]
- Time Points: Multiple time points similar to microsomal assay [68]
- Analysis: LC-MS/MS measurement of parent compound depletion [71]
- Special Applications: For slowly metabolized compounds, relay method using hepatocytes in suspension or plated hepatocyte culture method [68]
Troubleshooting Guides: Addressing Common Experimental Challenges
FAQ: Why are metabolic stability results different between liver microsomes and hepatocytes?
This is one of the most frequently encountered questions in metabolic stability assessment. The differences stem from fundamental biological distinctions between the test systems:
Table 3: Troubleshooting Metabolic Stability Discrepancies
| Issue/Observation | Potential Causes | Recommended Solutions |
|---|---|---|
| Compound metabolizes faster in liver microsomes than hepatocytes | 1. Poor membrane permeability limiting cellular uptake [68]2. Compound is an efflux transporter substrate [68]3. Differences in enzyme abundances | 1. Assess permeability in parallel [69]2. Include transporter inhibition studies [69]3. Use both systems for complete picture |
| Compound metabolizes faster in hepatocytes than liver microsomes | Significant non-CYP mediated metabolism (e.g., AO, MAO, UGT) [68] | 1. Identify specific non-CYP enzymes involved [68]2. Use recombinant enzymes for specific phenotyping [68] |
| CYP3A4 substrates show higher clearance in microsomes | Higher relative CYP3A4 activity in microsomal preps [68] | Use hepatocyte data for more physiologically relevant prediction [68] |
| No significant metabolism in either system | Compound is metabolically stable or uses unexpected clearance pathways [68] | 1. Use relay method or plated hepatocytes [68]2. Investigate alternative clearance mechanisms |
FAQ: How do we resolve conflicts between metabolic stability and other DMPK properties?
This represents a core challenge in holistic DMPK optimization. The following troubleshooting guide addresses common property conflicts:
Scenario: Good metabolic stability but poor solubility
Scenario: Good solubility but poor metabolic stability
- Root Cause: Structural features that are metabolic soft spots [70]
- Solutions:
Scenario: Good permeability but high efflux transporter liability
- Root Cause: Compound is substrate for efflux transporters like P-gp [69]
- Solutions:
The Scientist's Toolkit: Essential Research Reagent Solutions
What are the key biological reagents and systems for integrated DMPK assessment?
Table 4: Essential Research Reagents for Holistic DMPK Assessment
| Reagent/System | Function and Application | Key Considerations |
|---|---|---|
| Liver Microsomes | Contains CYP450 and some phase II enzymes; ideal for initial metabolic stability screening [68] | Cost-effective, easy to store, but incomplete enzyme representation [68] |
| Hepatocytes (Suspension) | Maintain complete cellular structure with full metabolic enzyme complement; more physiologically relevant [68] | More expensive, shorter viability; detects both CYP and non-CYP metabolism [68] |
| Plated Hepatocytes | Used for slowly metabolized compounds and transporter studies [68] | Longer-term studies, more physiologically relevant for uptake [68] |
| Recombinant Enzymes | Identify specific enzyme contributions to metabolism [68] | Phenotyping and reaction mapping [68] |
| Caco-2 Cells | Model for intestinal permeability and efflux transporter assessment [69] | Predicts human absorption, time-consuming assay [69] |
| Human Plasma | Plasma protein binding studies to determine free drug fraction [69] [71] | Critical for correlating in vitro potency with in vivo exposure [69] |
How do we select the right in vitro system for non-CYP metabolism assessment?
For compounds suspected to have significant non-CYP mediated metabolism, the appropriate matrix should be selected according to the type of metabolic enzymes in the presence or absence of an inhibitor. Stability experiments can also be performed using recombinant enzymes [68].
Table 5: Non-CYP Enzyme Assessment Tools
| Enzyme | Tissue Location | Cofactor Requirement | Recommended Inhibitor |
|---|---|---|---|
| Aldehyde Oxidase (AO) | Liver, lung, kidney, small intestine [68] | No cofactor [68] | Hydralazine [68] |
| Xanthine Oxidase (XO) | Liver, heart, lung, adipose, mammary gland [68] | No cofactor [68] | Febuxostat [68] |
| Aldo-Keto Reductase (AKR) | Liver, kidney, brain, blood [68] | NAD+, NADP+ [68] | Valproic acid [68] |
| Flavin Monooxygenase (FMO) | Kidney, intestine, fetal liver (FMO1); liver, lung, kidney (FMO3) [68] | NADPH [68] | Methimazole [68] |
| Monoamine Oxidase (MAO) | Liver, placenta, brain [68] | No cofactor [68] | Moclobemide (MAO-A), Deprenyl (MAO-B) [68] |
Advanced Integration: Leveraging In Silico and AI Approaches
How can computational approaches enhance holistic DMPK optimization?
Advances in computational modeling, machine learning, and AI have made in silico studies an increasingly powerful part of the DMPK toolbox. These approaches leverage existing data to predict ADME and toxicity profiles virtually, reducing the need for extensive wet-lab testing [69].
Key Computational Applications:
- Virtual Screening: Compounds with favorable predicted PK properties can be prioritized for experimental evaluation [69]
- Predictive Modeling: Physiologically-based pharmacokinetic (PBPK) models combine in vitro and in vivo data to predict human pharmacokinetics and dosing strategies [69]
- Risk Filtering: In silico tools help eliminate high-risk candidates before costly experimental studies are initiated [69]
- Deep Learning Generative Models: Used in late-stage MPO efforts to simultaneously optimize multiple parameters including primary activity, off-target effects, and ADME properties [66]
One case study demonstrated the successful application of a deep learning generative model to optimize eleven different objectives simultaneously: one primary activity assay, six off-target activity assays, and four ADME-related assays [66]. This approach highlights how modern AI methodologies can dramatically accelerate the multi-parameter optimization process that is fundamental to holistic DMPK.
What is the strategic framework for implementing holistic DMPK optimization?
Successful integration of metabolic stability with other DMPK properties requires a strategic framework throughout the drug discovery pipeline:
Early-Stage MPO Efforts (beginning with a validated hit):
- Center on expanding chemical space and increasing profiling data [66]
- Often rely more on probabilistic approaches, individual parameters, and general principles [66]
- Focus on identifying issues detrimental to developing a drug and assessing feasibility for MPO [66]
Late-Stage MPO Efforts (starting with an advanced lead):
- Center on focusing chemical space and optimizing profiles [66]
- Often rely more on rational approaches, composite metrics, and data analyses [66]
- Follow a "predict first" paradigm using high-quality chemical series-specific data [66]
The most successful implementations occur when DMPK insights are strategically integrated from the earliest stages, allowing DMPK experts to contribute to lead optimization and help prioritize compounds based on metabolic stability, permeability, and potential liabilities [69]. With timely feedback loops between DMPK scientists and medicinal chemists, teams can avoid unnecessary iterations and accelerate the identification of viable clinical candidates [69].
From In Vitro Data to In Vivo Success: Correlation, Prediction, and Translation
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Why does IVIVE commonly lead to systematic underprediction of in vivo hepatic clearance?
Systematic underprediction is a widely recognized challenge in IVIVE. Several factors contribute to this discrepancy [30]:
- Limitations of In Vitro Systems: Current in vitro systems (e.g., microsomes, hepatocytes) lack the full physiological environment of the liver. Issues such as the loss of enzymatic activity over time, depletion of endogenous cofactors, permeability limitations, and rate-limiting diffusion through an unstirred water layer can reduce the measured in vitro activity, particularly for high-clearance compounds [30].
- Transporter Effects: In vivo, hepatic clearance is influenced by uptake and efflux transporters. Conventional microsomal preparations do not include transporters, and while hepatocytes do, their activity may not fully replicate the in vivo situation. BDDCS Class 2 drugs (low solubility, high metabolism) are especially prone to inaccurate predictions due to these transporter effects [73].
- Binding Considerations: Inaccuracies in measuring the fraction unbound in blood (
fu,B) or in incubations (fu,inc) can introduce significant error. The interplay between protein binding, transporters, and enzymes is complex and difficult to model accurately in vitro [30] [73].
Q2: What are the specific challenges with predicting clearance for low-extraction-ratio compounds?
Measuring low clearance in vitro is experimentally challenging [30]:
- Low Turnover: Compounds with very low intrinsic clearance (
CLint) may show minimal degradation over standard incubation times (e.g., 1 hour for microsomes, 4-6 hours for hepatocytes). This leads to large uncertainty in the measured clearance value and subsequent dose predictions [30]. - Experimental Sensitivity: The analytical methods may lack the sensitivity to accurately quantify the small amount of parent compound depleted over the incubation period. Newer methods like the hepatocyte relay method or cultured hepatocyte systems have been developed to extend incubation times and better address this error [30].
Q3: How does species selection impact the accuracy of scaling for human predictions?
Interspecies scaling is complicated by physiological and molecular differences [74]:
- Species-Specific Metabolism: Enzymatic activity and substrate specificity can vary significantly between species. A compound may be a good substrate for an enzyme in one species but not in another.
- Differences in Protein Binding: The binding rate of drugs to plasma proteins can vary across species, likely due to different relative concentrations of plasma proteins in the blood. This can significantly affect the free fraction of drug available for metabolism and lead to inaccurate predictions if not properly accounted for [74].
Q4: Can in silico and AI models improve IVIVE predictions?
Yes, artificial intelligence (AI) and machine learning are emerging as powerful tools to address IVIVE challenges [75] [3]:
- Metabolic Stability Prediction: AI competitions, like the JUMP AI 2023, have focused on developing models to predict the metabolic stability of compounds from their chemical structures, using large datasets of human and mouse liver microsomal stability data [75].
- Early-Stage Prioritization: These in silico models allow for the rapid screening of large compound libraries during early drug discovery, helping to prioritize molecules with favorable metabolic stability profiles before synthesis and in vitro testing [3].
Troubleshooting Common Experimental Issues
| Problem Area | Specific Issue | Potential Root Cause(s) | Recommended Solution(s) |
|---|---|---|---|
| Systematic Error | Consistent underprediction of in vivo clearance [30] | Limitations of in vitro systems (e.g., cofactor depletion, loss of activity); Ignored transporter effects [30] [73] | Use empirical scaling factors cautiously; Consider more complex models (e.g., incorporating uptake); Use hepatocytes over microsomes for transporter-substrate drugs [30] |
| Low Clearance Compounds | High uncertainty in measured CLint [30] |
Low compound turnover within standard incubation times; Declining enzyme activity/viability [30] | Extend incubation times; Use specialized methods (e.g., hepatocyte relay); Increase analytical sensitivity [30] |
| High Clearance Compounds | Underprediction of clearance; Failure to identify high ER compounds [30] | Permeability limitation; Diffusional barriers (unstirred water layer); Cofactor depletion [30] | Use assay systems with higher metabolic capacity; Consider including binding terms correctly [30] |
| Data Variability | High variability between replicates or donors [30] | Donor variability in human tissue; Cryopreservation issues (though studies show minimal impact) [30] | Use pooled donor microsomes/hepatocytes; Ensure consistent cell viability and preparation protocols [30] |
| Protein Binding | Poor prediction despite good CLint correlation [73] |
Inaccurate measurement of fu,B or fu,inc; Species differences in plasma protein binding [74] [73] |
Re-evaluate protein binding assay conditions; Verify species-specific binding differences [73] |
Key Experimental Protocols
Standard Protocol for Determining Intrinsic Clearance in Liver Microsomes
This protocol outlines the methodology for measuring the metabolic stability of a compound using pooled human liver microsomes, a common high-throughput system in early drug discovery [75].
Principle: The compound is incubated with liver microsomes in the presence of an NADPH-regenerating system. The depletion of the parent compound over time is measured, and the in vitro intrinsic clearance (CLint, in vitro) is calculated from the observed half-life.
Materials:
- Research Reagent Solutions: See the dedicated "Scientist's Toolkit" section below for a complete list.
- Equipment: Thermostated incubator (37°C), liquid chromatography-mass spectrometry (LC-MS/MS) system, centrifuge.
Procedure:
- Preparation of Reaction Mixture:
- Prepare a master reaction mix containing 0.1 M phosphate buffer (pH 7.4), and an NADPH-regenerating system.
- Pre-warm the master mix to 37°C.
- Add pooled human liver microsomes (e.g., 0.5 mg/mL final protein concentration) to the master mix.
- Initiation of Reaction:
- Add the test compound (final concentration typically 1-2 µM) to the reaction mixture to start the incubation [75].
- Immediately after adding the compound, take an aliquot (time = 0 min).
- Incubation and Sampling:
- Incubate the reaction mixture at 37°C with gentle shaking.
- Withdraw aliquots at predetermined time points (e.g., 5, 15, 30, 45, 60 minutes).
- Terminate the reaction in each aliquot immediately by transferring it to a tube containing ice-cold acetonitrile [75].
- Sample Analysis:
- Centrifuge the terminated samples to precipitate proteins.
- Analyze the supernatant using LC-MS/MS to determine the concentration of the parent compound remaining at each time point.
- Data Analysis:
- Plot the natural logarithm (ln) of the parent compound concentration remaining versus time.
- Calculate the elimination rate constant (k, in min⁻¹) from the slope of the linear regression line.
- Calculate the in vitro half-life: ( t_{1/2} = \frac{0.693}{k} ).
- Calculate the in vitro intrinsic clearance: ( CL{int, in~vitro} = \frac{0.693}{t{1/2}} \times \frac{\text{mL incubation}}{\text{mg microsomal protein}} ).
Workflow for Scaling In Vitro Data to In Vivo Hepatic Clearance
This workflow describes the steps to extrapolate the measured in vitro intrinsic clearance to an in vivo human hepatic clearance value using the well-stirred model, the most commonly used model of hepatic disposition [30].
Principle: The scaled in vivo intrinsic clearance is calculated using physiological scaling factors. This value is then input into the well-stirred model of hepatic disposition, along with liver blood flow and relevant binding terms, to predict in vivo hepatic clearance.
Procedure:
- Scale to In Vivo Intrinsic Clearance:
- Convert the in vitro
CLintto an in vivo value using scaling factors. - For microsomes:
CLint, vivo = CLint, vitro × Microsomal Protein per Gram Liver × Liver Weight - For hepatocytes:
CLint, vivo = CLint, vitro × Hepatocytes per Gram Liver × Liver Weight
- Convert the in vitro
- Apply the Well-Stirred Model:
Data Presentation and Analysis
The following table compiles data from a large-scale evaluation of IVIVE prediction accuracy, highlighting the performance across different systems and extraction ratio ranges [30].
| System | Clearance Category (Extraction Ratio) | Root Mean Squared Error (RMSE) | % of Predictions Within 2-Fold of Observed |
|---|---|---|---|
| Human Hepatocytes | All | 6.6 | 30.7% |
| Low ER (<30%) | 2.9 | 34.6% | |
| Intermediate ER (30-70%) | 6.7 | 35.7% | |
| High ER (>70%) | 12.0 | 11.1% | |
| Human Microsomes | All | 6.4 | Not Specified |
| Low ER (<30%) | 3.0 | Slightly increased across ER ranges | |
| Intermediate ER (30-70%) | 6.6 | Slightly increased across ER ranges | |
| High ER (>70%) | 10.0 | Slightly increased across ER ranges |
Analysis of Prediction Accuracy by BDDCS Class
This table summarizes the performance of IVIVE based on the Biopharmaceutics Drug Disposition Classification System (BDDCS), which helps anticipate the influence of transporters on drug disposition [73]. The weighted average of inaccurate predictions (falling more than 2-fold outside in vivo values) was 66.5% across all systems and classes [73].
| BDDCS Class | Key Characteristics | Weighted Average of Inaccurate Predictions | Average Fold Error (AFE) Tendency |
|---|---|---|---|
| Class 1 | High solubility, high permeability; Minimal transporter effects [73]. | 62.3% | Variable, but generally lower bias than Class 2 [73]. |
| Class 2 | Low solubility, high permeability; Transporter effects likely in gut and liver [73]. | 81.9% | Often shows higher bias, indicating more severe underprediction [73]. |
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material | Function in the Experiment | Key Considerations |
|---|---|---|
| Pooled Human Liver Microsomes (HLM) | Subcellular fraction containing cytochrome P450 and other drug-metabolizing enzymes; primary source for metabolic activity in vitro [75]. | Use pools from multiple donors to mitigate individual variability. Confirm protein concentration and activity. |
| Cryopreserved Human Hepatocytes | Intact cells containing a full complement of drug-metabolizing enzymes and transporters; considered more physiologically relevant than microsomes [30]. | Assess viability upon thawing. Requires specific plating/media for suspended or cultured formats. |
| NADPH Regenerating System | Supplies a constant source of NADPH, the essential cofactor for oxidative metabolism by P450 enzymes. | Critical for maintaining metabolic activity during long incubations. Can be prepared from individual components or purchased as a kit. |
| Phosphate Buffer (pH 7.4) | Provides a physiologically relevant pH environment for the metabolic incubation. | Concentration typically 0.1 M. Must be sterile if using hepatocytes. |
| LC-MS/MS System | Analytical platform used to separate (chromatography) and detect (mass spectrometry) the parent compound with high sensitivity and specificity [75]. | Essential for accurately quantifying low levels of compound depletion, especially for low-clearance molecules. |
Navigating Species Differences in Drug Metabolism for Human PK Prediction
Frequently Asked Questions (FAQs)
FAQ 1: Why do animal models often fail to accurately predict human metabolic clearance? Animal models frequently fail to predict human outcomes due to significant species differences in the composition, expression, and catalytic activities of drug-metabolizing enzymes. While some cytochrome P450 (CYP) enzymes like CYP2E1 show good cross-species conservation, other major enzyme families like CYP1A, CYP2C, CYP2D, and CYP3A exhibit appreciable interspecies differences in their catalytic activities. These variations can lead to different metabolic rates and pathways between animals and humans, making extrapolation challenging [76].
FAQ 2: What are the most common metabolic stability issues encountered in drug discovery? The most common metabolic stability issues include short in vitro half-lives in liver microsomes or hepatocytes, often resulting from oxidative metabolism by CYP enzymes or Phase II conjugation reactions. For instance, in the development of 17β-HSD2 inhibitors, initial lead compounds exhibited unacceptably short half-lives of only 4-38 minutes in human liver S9 fractions, necessitating structural optimization to improve metabolic stability [59].
FAQ 3: Which animal species is most predictive for human CYP-mediated metabolism? No single animal species is universally predictive for all aspects of human CYP-mediated metabolism. Selection should be based on the specific CYP enzymes involved in a compound's metabolism. For example, cynomolgus monkeys (cyno) often show closer metabolic similarity to humans for certain pathways, but each species has distinct advantages and limitations. The most relevant species should be chosen based on preliminary in vitro interspecies comparison data [76] [77].
FAQ 4: How can I improve the metabolic stability of a lead compound with good target potency? Several structure-based strategies can improve metabolic stability while maintaining potency:
- Deuterium Incorporation: Replacing hydrogen with deuterium at metabolically labile sites can leverage the kinetic isotope effect to slow metabolic cleavage without altering biological activity, as successfully demonstrated with HCV inhibitor BMT-052 [77].
- Metabolic Soft Spot Identification: Use metabolite identification studies to pinpoint vulnerable molecular regions and guide structural modifications [59].
- Minor Structural Modifications: Transposing methyl groups or introducing small steric hindrances can block metabolic sites without significantly affecting target binding [77].
FAQ 5: What in vitro tools are available for predicting human hepatic clearance? Multiple complementary in vitro systems are available, each with distinct advantages and limitations [78]:
| Model System | Key Advantages | Primary Limitations | Best Applications |
|---|---|---|---|
| Primary Human Hepatocytes | High physiological relevance; contains full complement of metabolic enzymes and transporters | Donor variability; limited lifespan; requires cell culture maintenance | Comprehensive DMPK studies; transporter assays; long-term toxicity |
| Human Liver Microsomes | Enriched in Phase I/II enzymes; cost-effective; easy to use | Lacks cellular context and transporters; non-viable | High-throughput metabolic stability screening; CYP inhibition studies |
| Permeabilized Hepatocytes (MetMax) | Direct enzyme access; stable; no culture maintenance; retains subcellular structures | Lacks functional transporters; non-viable | High-throughput Phase I/II metabolism studies; intrinsic clearance |
Troubleshooting Common Experimental Challenges
Challenge 1: Discrepancies Between In Vitro Metabolic Stability and In Vivo Clearance
Problem: Compounds showing good metabolic stability in liver microsomes demonstrate unexpectedly high clearance in animal models.
Root Cause: This discrepancy often arises from extrahepatic metabolism, transporter-mediated clearance, or poor prediction of biliary excretion [79].
Solution:
- Use Integrated Hepatocyte Systems: Supplement microsomal data with intact hepatocyte studies that contain both phase I and II enzymes [78].
- Evaluate Transporter Effects: Assess potential for uptake transporter-mediated clearance using sandwich-cultured hepatocytes or transporter-transfected cell lines [79].
- Include Cofactor Supplementation: For specialized models like permeabilized hepatocytes, ensure adequate cofactor supplementation (NADPH, UDPGA) to maintain metabolic activity [78].
Experimental Protocol: Integrated Metabolic Stability Assessment
Challenge 2: Inaccurate Human PK Projection from Preclinical Data
Problem: Allometric scaling of animal PK data produces poor predictions of human clearance and volume of distribution.
Root Cause: Simple allometric scaling often fails due to species differences in protein binding, metabolic pathways, and transporter expression [80].
Solution:
- Apply Correction Methods: Use protein binding-corrected intercept methods or Rule of Exponents instead of simple allometric scaling [80].
- Leverage IVIVE-PBPK Integration: Combine in vitro-in vivo extrapolation (IVIVE) with physiologically based pharmacokinetic (PBPK) modeling for more mechanistic predictions [80].
- Species-Specific Scaling: For early discovery, use single-species scaling from most relevant species based on in vitro metabolism comparison [80].
Quantitative Prediction Methods for Human Clearance (CL) and Volume of Distribution (Vss):
| Method | Formula | Application Context |
|---|---|---|
| Simple Allometric Scaling (SAS) | CL = a × (BW)^b | Basic screening; requires data from ≥2 species |
| Rule of Exponents (ROE) | If 0.71 < b ≤ 1: CL × MLP = a × (BW)^b | Improved accuracy for specific exponent ranges |
| Fraction Unbound Corrected Intercept (FCIM) | CLhuman = 33.35 × (a/Rfu)^0.770 | Accounts for species differences in plasma protein binding |
| Single-Species Scaling (SSS) | CLhuman/fu,human = CLrat/fu,rat × (70/0.25)^0.75 | Early discovery with limited species data |
| Øie-Tozer Model (Vss) | Vss = Vp + (fup × Ve) + [(1-fup) × RE/I × Vp] + Vr × fup/fut | Mechanistic prediction of volume of distribution |
Challenge 3: Optimizing Metabolic Stability Without Compromising Target Potency
Problem: Structural modifications to improve metabolic stability frequently reduce potency against the therapeutic target.
Root Cause: Many structural features contributing to target binding may also represent metabolic soft spots [59].
Solution:
- Deuterium Incorporation Strategy: As demonstrated with BMT-052, strategic deuterium replacement at metabolic soft spots can improve stability while maintaining antiviral activity [77].
- Metabolic Switching Prevention: Avoid multiple simultaneous structural changes that can cause "metabolic switching" where new metabolic pathways emerge [59].
- Balanced Property Optimization: Focus on maintaining optimal lipophilicity (logP 1-3) while addressing specific metabolic liabilities [3].
Experimental Protocol: Metabolic Stability Optimization Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Core In Vitro Metabolism Tools:
| Research Reagent | Function & Application | Key Considerations |
|---|---|---|
| Human Liver Microsomes (HLM) | Contains Phase I oxidative enzymes and some Phase II conjugation enzymes; used for metabolic stability screening and metabolite profiling | Lot-to-lot variability; ensure adequate CYP activity characterization; supplement with NADPH for oxidation reactions [78] |
| Cryopreserved Human Hepatocytes | Gold standard for physiologically relevant metabolism studies; contains full complement of hepatic enzymes and transporters | Donor variability considerations; requires proper thawing and viability assessment; pooled donors recommended for screening [78] |
| Permeabilized Hepatocytes (MetMax) | Combined benefits of microsomes and hepatocytes; direct access to intracellular enzymes without transporter limitations | Ideal for high-throughput screening; stable frozen format; no culture maintenance required [78] |
| Transporter-Transfected Cell Lines | Assessment of uptake (OATP, OAT, OCT) and efflux (P-gp, BCRP) transporter interactions | Key for ECCS Class 3A/4 compounds; identify transporter-mediated clearance mechanisms [79] |
| Recombinant CYP Enzymes | Reaction phenotyping to identify specific CYP enzymes responsible for metabolism | Essential for DDI risk assessment; use with specific probe substrates and inhibitors [76] |
Analytical & Supporting Tools:
| Research Reagent | Function & Application | Key Considerations |
|---|---|---|
| NADPH Regenerating System | Essential cofactor for CYP-mediated oxidation reactions in microsomal and hepatocyte incubations | Maintain linear reaction conditions; prevent cofactor depletion during longer incubations [59] |
| UDPGA Cofactor | Cofactor for UGT-mediated glucuronidation reactions | Critical for comprehensive Phase II metabolism assessment; often overlooked in early screening [78] |
| LC-MS/MS Systems | Quantitative analysis of parent compound depletion and metabolite identification | High sensitivity required for low-clearance compounds; enable structural characterization of metabolites [59] |
| Protein Binding Assay Kits | Determination of fraction unbound in plasma and incubation matrices | Critical for IVIVE corrections; species differences in binding affect scaling accuracy [80] |
The Role of Computational Models and Machine Learning in Metabolic Stability Prediction
## Frequently Asked Questions (FAQs)
FAQ 1: What are the main limitations of current computational models for metabolic stability prediction, and how are modern approaches addressing them?
Current models, particularly traditional atom-centric Graph Neural Networks (GNNs), often provide incomplete molecular modeling by disregarding bond-level topological features and lack reliable uncertainty quantification, which is critical for assessing prediction confidence in a research setting. Modern frameworks like TrustworthyMS directly address these issues through a novel contrastive learning architecture. They incorporate a molecular graph topology remapping mechanism that synchronizes atom-bond interactions, capturing both localized electronic effects and global conformational constraints. Furthermore, they integrate uncertainty modeling via Beta-Binomial uncertainty quantification, enabling simultaneous prediction and confidence calibration under epistemic uncertainty. For traditional quantitative structure-activity relationship (QSAR) models, a key limitation is the poor quantitative prediction of in vivo clearance from in vitro data, often due to missing or uncertain components in scaling equations [81] [1].
FAQ 2: How can I account for interspecies differences (e.g., human vs. mouse) when building a predictive model for metabolic stability?
Interspecies differences arise from variations in enzyme expression levels and isoform composition, leading to significant metabolic variability for the same compound. To account for this, integrate interspecies differences directly into the model's learning objective. The MetaboGNN framework demonstrates that incorporating the metabolic stability difference between human liver microsomes (HLM) and mouse liver microsomes (MLM) as a dedicated multi-task learning component significantly enhances predictive accuracy. This approach allows the model to explicitly learn and capture patterns related to species-specific enzymatic variations, moving beyond parallel predictions for each species. Note that interspecies differences in metabolic stability (HLM–MLM) show negligible correlation with physicochemical properties like LogD and AlogP, indicating these differences stem primarily from enzymatic variations rather than membrane permeability [82].
FAQ 3: What strategies can I use to improve the metabolic stability of a lead compound based on in-silico predictions?
Computational models can guide specific structural modifications to enhance metabolic stability. Key strategies include:
- Reducing Lipophilicity: Lowering the overall lipophilicity (logP/logD) of a structure can reduce its affinity for metabolizing enzymes, which typically have lipophilic binding sites. This can be achieved by introducing polar functional groups [55].
- Blocking Metabolically Labile Groups: Identify and block sites vulnerable to metabolism, particularly to oxidation (e.g., benzylic or allylic positions). This can be done by introducing a halogen atom or replacing a carbon atom with a metabolically stable isostere like oxygen [55].
- Modifying Labile Functional Groups: Replace functional groups prone to hydrolysis (e.g., esters) with more stable bioisosteres (e.g., amides). Similarly, target functional groups that undergo rapid Phase II conjugation for modification [55].
FAQ 4: Which machine learning models have shown superior performance in recent metabolic stability prediction tasks?
Recent studies and competitions indicate that advanced neural network and ensemble learning models deliver state-of-the-art performance.
- Graph Neural Networks (GNNs) with Contrastive Learning: Models like MetaboGNN and TrustworthyMS, which use GNNs pretrained with graph contrastive learning (GCL), demonstrate superior predictive performance. They are particularly effective at learning robust molecular representations from limited data [81] [82].
- Gradient Boosting (GB): In frameworks predicting related metabolic conditions, Gradient Boosting has been shown to achieve low error rates and robust predictive capability [83].
- Convolutional Neural Networks (CNNs): CNNs can also achieve high specificity and accuracy, though they may require larger sample sizes and offer less inherent interpretability compared to traditional models [83].
FAQ 5: Why is uncertainty quantification important in metabolic stability prediction, and how is it implemented?
Uncertainty quantification is crucial because it provides a measure of confidence in the model's predictions, helping researchers prioritize compounds for costly experimental validation and make more reliable go/no-go decisions. An implementation is demonstrated by the TrustworthyMS framework, which uses Beta-Binomial uncertainty quantification. This method allows the model to calibrate its predictions and quantify epistemic uncertainty (uncertainty due to the model itself), making the output more trustworthy for critical research and development applications [81].
### Key Experiment: MetaboGNN Workflow for Liver Metabolic Stability Prediction
1. Objective To develop a robust predictive model for liver metabolic stability in human and mouse liver microsomes using Graph Neural Networks and Graph Contrastive Learning, explicitly incorporating interspecies differences to enhance accuracy and provide mechanistic insights.
2. Materials and Data
- Dataset: High-quality dataset from the 2023 South Korea Data Challenge for Drug Discovery.
- Compounds: 3,981 compounds with measured metabolic stability data.
- Training/Test Split: 3,498 training molecules, 483 test molecules.
- Key Features: SMILES structures, AlogP, number of hydrogen donors/acceptors.
- Stability Measurement: Liver microsomal stability (HLM and MLM) measured as the percentage of the parent compound remaining after a 30-min incubation via LC–MS/MS [82].
3. Methodology
- Step 1: Data Preprocessing and Exploratory Analysis
- Represent molecular structures as graphs.
- Analyze data distributions using Kernel Density Estimation (KDE) plots.
- Visualize the chemical space using Principal Component Analysis (PCA) on Morgan fingerprints.
- Calculate the interspecies difference metric:
HLM–MLM(% remaining). - Compute Pearson correlation coefficients among all features and stability values.
Step 2: Model Architecture and Pretraining
- Base Model: Implement a Graph Neural Network (GNN) to process molecular graphs.
- Pretraining: Employ Graph Contrastive Learning (GCL) as a self-supervised pretraining strategy. This enhances model generalizability by learning robust, transferable graph-level representations from the molecular structure data alone.
- Learning Objective: Incorporate a multi-task learning component where the model simultaneously predicts HLM stability, MLM stability, and the interspecies difference (HLM–MLM).
Step 3: Model Training and Evaluation
- Training: Train the model on the training set using the multi-task objective.
- Evaluation Metric: Use Root Mean Square Error (RMSE) for HLM and MLM predictions. The overall score is calculated as:
Score = 0.5 × RMSE(HLM) + 0.5 × RMSE(MLM). - Interpretation: Use attention-based analysis within the GNN to identify key molecular fragments associated with high or low metabolic stability.
4. Results and Performance The MetaboGNN model achieved state-of-the-art performance:
- RMSE for HLM: 27.91
- RMSE for MLM: 27.86 The model successfully identified LogD and AlogP as highly correlated with microsomal stability. The attention mechanism provided chemically meaningful insights by highlighting substructures that influence metabolic stability [82].
### Performance Comparison of Machine Learning Models
The following table summarizes the performance of various machine learning models as reported in recent literature for predicting metabolic stability and related metabolic syndrome (MetS) parameters.
Table 1: Performance Metrics of Machine Learning Models in Metabolic Stability and MetS Prediction
| Model / Framework | Application Context | Key Performance Metrics | Noteworthy Features / Top Predictors |
|---|---|---|---|
| TrustworthyMS [81] | Metabolic Stability Prediction | Outperformed state-of-the-art methods in predictive performance. | Uncertainty-aware; dual-view contrastive learning; topology-bond alignment. |
| MetaboGNN [82] | Liver Microsomal Stability (HLM & MLM) | RMSE (HLM): 27.91; RMSE (MLM): 27.86. | GNN with GCL; incorporates interspecies differences; provides fragment analysis. |
| Gradient Boosting (GB) [83] | Metabolic Syndrome (MetS) Prediction | Specificity: 77%; Lowest Error Rate: 27%. | Robust predictive capability; handles structured clinical data well. |
| Convolutional Neural Network (CNN) [83] | Metabolic Syndrome (MetS) Prediction | Specificity: 83%. | High accuracy, but requires larger sample sizes; less interpretable. |
| Support Vector Machine (SVM) [83] | Metabolic Syndrome (MetS) Prediction | Sensitivity: 0.774; Specificity: 0.74; Accuracy: 0.757. | Effective for classification tasks with structured data. |
| Random Forest (RF) [83] | Metabolic Syndrome (MetS) Prediction | Sensitivity: 0.97; Specificity: 0.99 (in a separate study). | High interpretability; provides feature importance (e.g., hs-CRP, ALT, sex). |
### The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Computational Tools for Metabolic Stability Research
| Item / Reagent | Function / Application in Research |
|---|---|
| Human & Mouse Liver Microsomes (HLM/MLM) | In vitro systems containing cytochrome P450 and other enzymes to simulate hepatic Phase I metabolism and assess intrinsic clearance [1] [82]. |
| Liquid Chromatography with Tandem Mass Spectrometry (LC-MS/MS) | Analytical method for quantifying the percentage of parent compound remaining after incubation with microsomes, providing the primary data for model training [82]. |
| Graph Neural Network (GNN) Frameworks | Core computational architecture (e.g., MetaboGNN) for representing molecules as graphs and learning from structural relationships to predict stability [81] [82]. |
| Graph Contrastive Learning (GCL) | A self-supervised pretraining strategy used to learn robust, generalizable molecular representations from limited data, enhancing model performance [82]. |
| SHAP (SHapley Additive exPlanations) | A framework for interpreting model predictions, identifying the most influential biomarkers (e.g., hs-CRP, bilirubin, ALT) and structural features [83]. |
| Physiologically Based Pharmacokinetic (PBPK) Modeling | A modeling technique that incorporates physiological parameters (e.g., organ weight, blood flow) and ontogeny to scale in vitro clearance to in vivo human contexts [84]. |
### Troubleshooting Common Experimental Challenges
Issue 1: Poor Correlation Between In Vitro Metabolic Stability Predictions and In Vivo Results
- Potential Cause: The scaling equations used to convert in vitro intrinsic clearance (
CLint) to *in vivo` hepatic clearance may be missing critical components. Old assumptions, such as the liver being the principal site of first-pass metabolism, are often oversimplified. New knowledge regarding the relationship between drug transporters and metabolizing enzymes may not be incorporated [1]. - Solution:
- Revise Scaling Assumptions: Update in vitro-in vivo correlation (IVIVC) models to include factors like extra-hepatic metabolism and transporter effects.
- Use PBPK Models: Implement a Physiologically Based Pharmacokinetic (PBPK) modeling approach. These models incorporate physiological parameters (e.g., organ weights, blood flows) and, crucially, can account for ontogeny (the maturation of organ function, especially in paediatric populations) and other patient-specific factors to provide a more accurate scaling framework [84].
Issue 2: Machine Learning Model Performs Well on Training Data but Poorly on New Compound Classes
- Potential Cause: The model is overfitting to the specific structural patterns in the training data and lacks generalizable molecular representations. This is common with limited dataset sizes.
- Solution: Employ Graph Contrastive Learning (GCL) as a pretraining step. GCL is a self-supervised method that learns by encouraging the model to produce similar representations for different augmented "views" of the same molecule while pushing apart representations of different molecules. This technique helps the model learn intrinsic structural features that are robust and transferable, improving performance on new, unseen compounds [82].
Issue 3: Difficulty in Interpreting Which Molecular Substructure is Causing Low Metabolic Stability
- Potential Cause: Many powerful models, particularly deep learning networks, operate as "black boxes," making it difficult to extract chemically meaningful insights.
- Solution: Utilize models with built-in interpretability features. Frameworks like MetaboGNN use attention mechanisms that assign importance weights to different atoms or bonds in the molecular graph. These weights can be visualized to identify fragments associated with stabilizing or destabilizing effects, directly guiding chemists in structural optimization [82]. Additionally, apply post-hoc interpretation tools like SHAP analysis to determine the contribution of specific features (e.g.,
LogD,hs-CRP,ALT) to the final prediction [83].
Issue 4: Model Predictions Lack a Measure of Confidence, Leading to Costly Experimental Dead-Ends
- Potential Cause: Standard regression or classification models output a single value without any indication of the prediction's reliability.
- Solution: Implement models with integrated uncertainty quantification. The TrustworthyMS framework, for example, uses Beta-Binomial uncertainty quantification to estimate epistemic uncertainty. This provides a confidence level for each prediction, allowing researchers to prioritize the testing of compounds where the model is highly certain and to treat low-confidence predictions with more caution [81].
FAQs on Assay Selection and Troubleshooting
Q1: What are the key differences between using hepatocytes and liver microsomes for metabolic stability studies?
Hepatocytes are a more physiologically complete model as they contain both Phase I and Phase II enzymes with their natural cofactors, providing a full metabolic profile. However, they are sensitive to freezing and incubation conditions, which can impact data reliability. Liver microsomes, while robust and cost-effective, are a subcellular fraction that primarily contain Phase I and UGT (UDP-glucuronosyltransferase) enzymes. They are ideal for high-throughput screening but do not reflect metabolism via pathways like sulphation, potentially leading to an underestimation of stability for compounds metabolized by these routes [85].
Q2: My Western blot has a high background. What are the most common causes and solutions?
High background is a common issue often traced to antibody concentration, blocking efficiency, or washing steps. The table below summarizes the primary causes and solutions [86].
| Possible Cause | Solution |
|---|---|
| Antibody concentration too high | Optimize and decrease antibody concentration; use a dot-blot test [86]. |
| Insufficient blocking | Optimize the choice of blocking buffer; increase blocking time; use compatible agents like BSA or skim milk [86]. |
| Insufficient washing | Increase the number and volume of washes; add a detergent like 0.05% Tween-20 to the wash buffer [86]. |
| Non-specific antibody cross-reactivity | Run a secondary antibody-only control; switch blocking agents if cross-reactivity is suspected [86]. |
Q3: What are the main challenges when developing bioanalytical methods for peptides, and how can they be overcome?
Peptide therapeutics present unique challenges, including low in vivo concentrations, poor stability, and non-specific adsorption. To overcome low concentrations, develop ultra-sensitive LC-MS/MS assays and use stable isotope-labeled internal standards. To address poor stability, immediately stabilize samples with protease inhibitors upon collection and optimize storage conditions. To mitigate non-specific adsorption, use low-binding labware and validate recovery rates at every step of the analytical process [42].
Q4: What troubleshooting steps should I take if my Bradford assay shows inconsistent results or low absorbance?
Inconsistent results often stem from pipetting errors or variations in reagent lots. For low absorbance, check the following [87]:
- Low Molecular Weight: The Bradford assay has a detection limit of ~3,000-5,000 Daltons. For smaller peptides, use an alternative assay like BCA.
- Interfering Substances: Detergents or alkaline conditions in your sample buffer can interfere. Dilute your sample or dialyze it to remove interferents.
- Reagent Quality: Use fresh, properly stored Bradford reagent and ensure it is at room temperature before use.
- Wavelength: Confirm that absorbance is measured at the correct wavelength of 595 nm.
Troubleshooting Guides for Common Assay Systems
Metabolic Stability Assays
This guide helps diagnose and resolve common problems encountered in metabolic stability studies using liver microsomes or hepatocytes.
| Problem | Possible Cause | Solution |
|---|---|---|
| Underestimation of Clearance | Use of liver microsomes for a compound primarily metabolized via sulphation [85]. | Use fresh hepatocytes, which contain a full complement of Phase II enzymes [85]. |
| Poor Correlation with In Vivo Data | Ignoring interspecies differences in enzyme expression and isoform composition [32]. | Incorporate interspecies difference data early in screening; use in vitro-in vivo extrapolation (IVIVE) models [32]. |
| High Variability in Replicate Data | Degradation of metabolizing system (e.g., hepatocytes) due to improper handling or storage [85]. | Ensure consistent and proper thawing/hepatocyte handling; use fresh or properly preserved reagents [85]. |
Western Blot Assays
A guide for resolving issues related to signal and background in Western blotting.
| Problem | Possible Cause | Solution |
|---|---|---|
| Weak or No Signal | Insufficient protein transfer to membrane [86]. | Use Ponceau S stain to confirm efficient transfer; optimize transfer time and current [86]. |
| Too much antibody masking the antigen [86]. | Compare different blocking buffers (e.g., BSA instead of milk); reduce blocking time [86]. | |
| Presence of sodium azide in buffers with HRP-conjugated antibodies [86]. | Eliminate sodium azide from all buffers used with HRP systems [86]. | |
| Multiple Non-Specific Bands | Impure antibody or antibody concentration too high [88]. | Use an affinity-purified antibody; lower the concentration of the primary antibody [88]. |
| Cross-reactivity of the antibody with other proteins [86]. | Use a different blocking agent; test antibody specificity with a knockout cell line control [86]. |
ELISA Assays
Common problems and solutions for Enzyme-Linked Immunosorbent Assays (ELISA).
| Problem | Possible Cause | Solution |
|---|---|---|
| High Background | Insufficient washing, leading to unbound enzyme conjugate remaining on the plate [45]. | Increase the number of washes; add a 30-second soak step between washes [45]. |
| Too much signal reagent (e.g., streptavidin-HRP) [45]. | Check the dilution of the detection antibody or enzyme conjugate; titrate to find the optimal concentration [45]. | |
| Poor Duplicates | Uneven coating of the plate or insufficient washing [45]. | Ensure consistent pipetting technique; use an automatic plate washer and check for clogged ports [45]. |
| Plate sealers were reused, causing cross-contamination [45]. | Use a fresh plate sealer for every incubation step [45]. |
Experimental Protocols for Key Metabolic Stability Assays
Protocol 1: Metabolic Stability Screening Using Liver Microsomes
Objective: To determine the intrinsic clearance (CL~int~) of a drug candidate by measuring the depletion of the parent compound over time in liver microsomes [85].
Materials:
- Research Reagent Solutions:
- Liver Microsomes: Human or mouse liver microsomes (HLM/MLM), stored at -80°C [85].
- NADPH-Regenerating System: Provides a constant supply of NADPH, a crucial cofactor for cytochrome P450 enzymes [85].
- Ultra-Performance Liquid Chromatography with Tandem Mass Spectrometry (UPLC-MS/MS): For sensitive and specific quantification of the parent compound and its metabolites [32].
- Incubation Buffer: Typically a phosphate buffer at physiological pH (e.g., 100 mM potassium phosphate buffer, pH 7.4).
Methodology:
- Preparation: Thaw liver microsomes on ice. Prepare a working solution of the test compound in a suitable solvent (e.g., DMSO), ensuring the final solvent concentration is ≤1%.
- Incubation: In a 96-well plate, combine the following:
- Incubation buffer
- Liver microsomes (final protein concentration ~0.5-1 mg/mL)
- Test compound (final concentration ~1 µM)
- Initiation: Pre-incubate the mixture for 5-10 minutes at 37°C. Start the reaction by adding the NADPH-regenerating system.
- Time Points: At predetermined time points (e.g., 0, 5, 15, 30, 45 minutes), remove an aliquot of the incubation mixture and quench it with an equal volume of ice-cold acetonitrile containing an internal standard.
- Sample Analysis: Centrifuge the quenched samples to precipitate proteins. Analyze the supernatant using UPLC-MS/MS to measure the peak area of the parent compound.
- Data Analysis: Plot the natural logarithm of the parent compound concentration remaining versus time. The slope of the linear phase is used to calculate the half-life (t~1/2~) and intrinsic clearance (CL~int~).
Protocol 2: In Vitro-In Vivo Extrapolation (IVIVE) Using Hepatocytes
Objective: To extrapolate in vitro metabolic stability data from hepatocytes to predict in vivo hepatic clearance [85].
Materials:
- Research Reagent Solutions:
Methodology:
- Cell Preparation: Thaw cryopreserved hepatocytes rapidly and suspend them in pre-warmed Williams' Medium E. Assess cell viability (should be >80%).
- Incubation: Seed hepatocytes in collagen-coated plates or use them in suspension. Add the test compound and incubate at 37°C.
- Sampling: At designated time points, collect supernatant samples and quench with ice-cold organic solvent.
- Analysis: Process samples and analyze parent compound concentration via UPLC-MS/MS.
- IVIVE Modeling: Use the calculated in vitro half-life to scale and predict in vivo hepatic clearance using physiological scaling factors and models that account for protein binding and liver blood flow.
Data Presentation: Quantitative Comparisons of Assay Systems
Table 1: Strengths and Limitations of Key Metabolic Stability Assay Systems
This table provides a comparative overview of common in vitro models used to assess metabolic stability in drug discovery [85].
| Assay System | Key Strengths | Key Limitations | Primary Application |
|---|---|---|---|
| Liver Microsomes | Robust, cost-effective; ideal for high-throughput screening of P450 and UGT metabolism [85]. | Lacks full cellular context and non-microsomal enzymes (e.g., sulfotransferases) [85]. | Tier-1, high-throughput metabolic stability screening and reaction phenotyping [85]. |
| Hepatocytes | Contains full complement of Phase I and II enzymes; more physiologically relevant [85]. | Sensitive to handling and storage; more variable and costly than microsomes [85]. | Gold standard for comprehensive metabolic profiling and IVIVE [85]. |
| AI Prediction Models (e.g., MetaboGNN) | Fast, low-cost; can predict interspecies differences and highlight key metabolic fragments [32]. | Performance dependent on quality and size of training data; may not capture all metabolic pathways [32]. | Early-stage lead optimization and prioritization of compounds for synthesis and testing [32]. |
Workflow and Pathway Visualizations
Metabolic Stability Assay Workflow
AI-Driven Stability Prediction
The Scientist's Toolkit: Essential Research Reagents
| Item | Function in Metabolic Stability Research |
|---|---|
| Liver Microsomes | Subcellular fractions rich in cytochrome P450 enzymes; used for high-throughput, initial metabolic stability screening [85]. |
| Cryopreserved Hepatocytes | Intact liver cells containing a full suite of Phase I and Phase II metabolic enzymes; considered the gold standard for comprehensive metabolic profiling [85]. |
| NADPH-Regenerating System | Provides a continuous supply of nicotinamide adenine dinucleotide phosphate (NADPH), the essential electron donor for cytochrome P450-mediated oxidation reactions [85]. |
| LC-MS/MS System | The core analytical platform for sensitive and specific quantification of the parent drug and its metabolites in complex biological matrices [32]. |
| Stable Isotope-Labeled Internal Standards | Used in mass spectrometry to correct for matrix effects and variability in sample preparation, ensuring accurate and precise quantification [42]. |
| Graph Neural Networks (GNNs) | An advanced AI tool that models a molecule as a graph of atoms and bonds to predict properties like metabolic stability and identify susceptible structural fragments [32]. |
Integrating Metabolic Data into a Comprehensive ADME Package for Candidate Selection
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Our lead compound shows excellent in vitro potency but poor metabolic stability in liver microsome assays. What are the first steps we should take?
A1: Begin by investigating the mechanisms behind the rapid clearance.
- Identify Major Enzymes: Use recombinant CYP enzymes or chemical inhibitors (like ketoconazole for CYP3A4) in your stability assays to pinpoint which cytochrome P450 enzymes are primarily responsible for the metabolism [89].
- Metabolite Identification: Conduct metabolite identification studies to see which part of the molecule is being modified. This provides direct clues for medicinal chemistry to block or alter metabolically labile sites [90].
- Evaluate Structural Alerts: Look for common metabolic soft spots, such as unsubstituted aromatic rings, ester groups, or N-alkyl chains, and prioritize these for modification.
Q2: We are seeing a significant discrepancy between the metabolic stability in liver microsomes and in hepatocytes. Which result should we trust for human prediction?
A2: Hepatocytes generally provide a more physiologically relevant prediction.
- Mechanism: Hepatocytes contain the full complement of hepatic enzymes (both Phase I and Phase II) and can often reveal conjugative metabolism (like glucuronidation) that microsomes, which lack most transferases, will miss [69] [90].
- Action: If clearance is faster in hepatocytes, investigate Phase II metabolism pathways. If clearance is faster in microsomes, it may indicate a lack of co-factors for Phase II metabolism in your microsomal system. An integrated approach using both systems provides the most comprehensive picture [89].
Q3: Our compound has high permeability but low apparent oral bioavailability in rodent models. What are the likely culprits?
A3: This common issue suggests a problem after absorption.
- First-Pass Metabolism: The compound is likely undergoing extensive metabolism in the liver (hepatic first-pass) before reaching systemic circulation [90].
- Gut Metabolism: Check for CYP3A4 or other enzyme activity in the intestines, which can significantly reduce bioavailability for some compounds.
- Transporter Effects: Investigate efflux transporters like P-glycoprotein (P-gp) at the intestinal wall, which can actively pump the drug back into the gut lumen after absorption, reducing net absorption and increasing exposure to gut metabolizing enzymes [69] [89].
Q4: How can we use in vitro data to predict the potential for drug-drug interactions (DDIs) early on?
A4: Key in vitro assays are critical for DDI prediction.
- CYP Inhibition: Assess the compound's potential to reversibly inhibit major CYP enzymes (e.g., 1A2, 2C9, 2C19, 2D6, 3A4). A low IC50 value indicates a high risk for DDIs [91] [89].
- CYP Induction: Use human hepatocytes to test if the compound induces the expression of CYP enzymes, particularly CYP3A4 and CYP1A2. Induction can lead to increased metabolism of co-administered drugs, reducing their efficacy [89] [90].
- Time-Dependent Inhibition (TDI): Perform time- and NADPH-dependent inhibition assays to identify if your compound forms reactive metabolites that irreversibly inhibit CYPs, a significant clinical DDI risk [90].
Troubleshooting Common Experimental Issues
Issue 1: High Variability in Metabolic Stability Assay Results
- Potential Causes & Solutions:
- Cause: Inconsistent protein concentration or cell viability between assay runs.
- Solution: Standardize and meticulously document the protein concentration (for microsomes) or cell count and viability (for hepatocytes) for each experiment. Use fresh or properly stored (liquid nitrogen) hepatocytes.
- Cause: Compound precipitation or non-specific binding to labware.
- Solution: Check the solubility of your compound in the assay buffer. Use silanized or polypropylene labware to minimize binding, and include controls to account for any loss.
Issue 2: Poor Correlation Between In Vitro and In Vivo Clearance
- Potential Causes & Solutions:
- Cause: Neglecting extra-hepatic metabolism or tissue binding in predictions.
- Solution: Incorporate plasma protein binding and tissue binding data into your in vitro-in vivo extrapolation (IVIVE) models. Consider non-CYP clearance pathways [89].
- Cause: Incorrect scaling factors used in IVIVE.
- Solution: Ensure you are using species-specific and well-validated scaling factors (e.g., microsomal protein per gram of liver, hepatocellularity) for the translation [90].
Issue 3: Inconclusive Cytochrome P450 Inhibition Results
- Potential Causes & Solutions:
- Cause: The test compound is fluorescent or absorbs at the same wavelength as the assay's fluorescent probe substrate, causing interference.
- Solution: Switch to a different detection method, such as LC-MS/MS, which is more specific and less prone to analytical interference.
- Cause: The chosen probe substrate is not specific for the target CYP enzyme.
- Solution: Use well-established, selective probe substrates for each CYP enzyme as recommended by regulatory guidance (e.g., FDA DDI guidance).
The following table outlines core in vitro ADME assays, their objectives, and how to interpret results for candidate selection.
| Assay | Primary Objective | Key Parameters | Interpretation for Candidate Selection |
|---|---|---|---|
| Metabolic Stability (Liver Microsomes/Hepatocytes) [69] [90] | Determine the rate of compound disappearance. | Intrinsic Clearance (CLint), Half-life (t1/2). | Low CLint & long t1/2 suggest favorable metabolic stability and potential for less frequent dosing. |
| Cytochrome P450 Inhibition [69] [89] | Assess potential for drug-drug interactions. | IC50 (reversible), TDI parameters (kinact/KI). | High IC50 (low potency) and no TDI are desirable to minimize DDI risk. |
| Permeability (Caco-2, PAMPA) [69] [90] | Predict intestinal absorption and brain penetration. | Apparent Permeability (Papp). | High Papp suggests good absorption for oral drugs. |
| Plasma Protein Binding [69] [91] | Determine the fraction of unbound, pharmacologically active drug. | Fraction Unbound (fu). | A very high fraction bound (>99%) may limit tissue distribution and necessitate higher doses. |
| Transporter Interactions (e.g., P-gp) [69] [89] | Evaluate involvement of uptake/efflux transporters. | Efflux Ratio (ER). | A high ER may indicate poor absorption or limited brain penetration due to efflux. |
Detailed Experimental Protocols
Protocol 1: Metabolic Stability Assay in Liver Microsomes
1. Objective: To determine the in vitro half-life and intrinsic clearance of a test compound in a specified species' liver microsomes.
2. Materials:
- Research Reagents & Solutions:
- Liver Microsomes: Pooled from human or preclinical species (e.g., mouse, rat, dog). Stored at -80°C [90].
- NADPH Regenerating System: Solution A (NADP+, Glucose-6-phosphate) and Solution B (Glucose-6-phosphate Dehydrogenase) or a single pre-made solution.
- Compound Stock Solution: Test compound dissolved in DMSO (e.g., 10 mM).
- Potassium Phosphate Buffer: 0.1 M, pH 7.4, containing 3.3 mM MgCl₂.
- Stop Solution: Acetonitrile with internal standard for LC-MS/MS analysis.
3. Methodology: 1. Pre-incubation: Prepare the incubation mixture containing liver microsomes (e.g., 0.5 mg/mL protein concentration) and test compound (e.g., 1 µM) in potassium phosphate buffer. Pre-incubate for 5 minutes at 37°C. 2. Initiate Reaction: Start the reaction by adding the NADPH Regenerating System. 3. Time Points: At predetermined time points (e.g., 0, 5, 15, 30, 45 minutes), remove an aliquot of the incubation mixture and quench it with ice-cold stop solution. 4. Sample Analysis: Centrifuge the quenched samples to precipitate proteins. Analyze the supernatant using LC-MS/MS to determine the peak area ratio (compound/internal standard) over time. 5. Data Analysis: Plot the natural logarithm of the remaining compound percentage versus time. The slope of the linear regression is -k (elimination rate constant). Calculate in vitro half-life as t1/2 = 0.693 / k and scale to intrinsic clearance (CLint).
Protocol 2: Caco-2 Permeability Assay
1. Objective: To assess the intestinal absorption potential and efflux transporter liability of a test compound.
2. Materials:
- Research Reagents & Solutions:
- Caco-2 Cell Monolayers: Grown on Transwell inserts for 21-25 days to fully differentiate and form tight junctions [69] [90].
- Transport Buffer: Hanks' Balanced Salt Solution (HBSS) with 10 mM HEPES, pH 7.4.
- Test Compound: Prepared in transport buffer at a relevant concentration (e.g., 10 µM).
- Lucifer Yellow: A paracellular marker to validate monolayer integrity.
- Known Substrates/Inhibitors: e.g., Digoxin (P-gp substrate) and GF120918 (P-gp inhibitor) for control experiments.
3. Methodology: 1. Monolayer Integrity Check: Measure the Transepithelial Electrical Resistance (TEER) of the cell monolayers before and after the experiment. Accept only monolayers with TEER values above a certain threshold (e.g., >300 Ω·cm²). 2. Bidirectional Transport: * A-to-B (Apical to Basolateral): Add compound to the apical chamber and sample from the basolateral chamber over time. * B-to-A (Basolateral to Apical): Add compound to the basolateral chamber and sample from the apical chamber over time. 3. Sample Analysis: Analyze samples using LC-MS/MS to determine compound concentration. 4. Data Analysis: Calculate the apparent permeability (Papp) in both directions. The Efflux Ratio (ER) is Papp (B-to-A) / Papp (A-to-B). An ER >> 2 suggests the compound is a substrate for an efflux transporter like P-gp.
Experimental Workflows and Pathways
Diagram: Strategy for Optimizing Metabolic Stability
Diagram: Integrated ADME Screening Cascade
Conclusion
Overcoming poor metabolic stability is not a single-step task but a continuous, integrated process throughout drug discovery. A deep foundational understanding, combined with the strategic application of a suite of in vitro assays, allows for the effective identification and optimization of metabolic soft spots. Proactive troubleshooting and an awareness of technical pitfalls, such as reagent variability, are essential for generating reliable data. Ultimately, the successful translation of in vitro metabolic stability data to predict human pharmacokinetics hinges on robust scaling methods and an understanding of species differences. The future of metabolic stability assessment lies in the increased adoption of high-throughput automation, more sophisticated in vitro models, and the powerful predictive capabilities of uncertainty-aware machine learning models, which together promise to de-risk development and accelerate the delivery of safer, more effective therapeutics to patients.
References
- 1. Metabolic stability for drug discovery and development [https://pubmed.ncbi.nlm.nih.gov/12793837/]
- 2. What is the importance of metabolic stability in drug design? [https://synapse.patsnap.com/article/what-is-the-importance-of-metabolic-stability-in-drug-design]
- 3. Overcoming Challenges in Small-Molecule Drug ... [https://www.mdpi.com/1422-0067/25/23/13121]
- 4. Drug Metabolism and Pharmacokinetics [https://www.bcm.edu/research/atc-core-labs/nmr-and-drug-metabolism-core/facility-and-services/drug-metabolism-and-pharmacokinetics]
- 5. Metabolic Stability in Drug Development: 5 Assays [https://labtesting.wuxiapptec.com/2023/10/09/metabolic-stability-drug-development-assays/]
- 6. Retrospective assessment of rat liver microsomal stability ... [https://www.nature.com/articles/s41598-020-77327-0]
- 7. Rapid and Quantitative Measurement of Metabolic Stability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3179854/]
- 8. Pharmacokinetic, metabolic stability, plasma protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6567057/]
- 9. Why 90% of clinical drug development fails and how to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9293739/]
- 10. Low-Turnover Drug Molecules: A Current Challenge for ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624102310]
- 11. Addressing 6 Major Challenges in ADME Drug Development [https://cn-bio.com/6-challenges-in-adme-drug-development/]
- 12. A high throughput metabolic stability screening workflow ... [https://www.sciencedirect.com/science/article/abs/pii/S0021967310000464]
- 13. Drug metabolism [https://en.wikipedia.org/wiki/Drug_metabolism]
- 14. Biochemistry, Biotransformation - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK544353/]
- 15. Phase I and Phase II biotransformation reactions [https://derangedphysiology.com/main/cicm-primary-exam/pharmacokinetics/Chapter-3355/phase-i-and-phase-ii-biotransformation-reactions]
- 16. Phase II drug metabolizing enzymes [https://pubmed.ncbi.nlm.nih.gov/20668491/]
- 17. Evaluation of Violacein Metabolic Stability and Metabolite ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114947/]
- 18. The influence of phase II enzymes on in vitro half-life ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X20317422]
- 19. Drug Metabolism - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK442023/]
- 20. Overcoming the Challenges of Metabolite Identification and ... [https://dmpkservice.wuxiapptec.com/blogs/66-overcoming-the-challenges-of-metabolite-identification-and-profiling-for-developing-oligonucleotides/]
- 21. First pass effect - Wikipedia [https://en.wikipedia.org/wiki/First_pass_effect]
- 22. First-Pass Effect - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK551679/]
- 23. First Pass Effect - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/first-pass-effect]
- 24. Addressing the Challenges of Low Clearance in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4365098/]
- 25. Drug Absorption - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK557405/]
- 26. Overcoming Challenges in Small-Molecule Drug Bioavailability [https://pmc.ncbi.nlm.nih.gov/articles/PMC11642056/]
- 27. Intrinsic clearance – An ABC of PK/PD [https://pressbooks.openeducationalberta.ca/abcofpkpd/chapter/clint/]
- 28. Why the well-stirred model is still used even though it is not ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295219302801]
- 29. Hepatic Clearance – Pharmacokinetics [https://sepia2.unil.ch/pharmacology/parameters/hepaticclearance/]
- 30. In vitro-in vivo extrapolation and hepatic clearance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7325626/]
- 31. Hepatocyte Stability | Cyprotex ADME-Tox Solutions [https://www.evotec.com/solutions/drug-discovery-preclinical-development/cyprotex-adme-tox-solutions/adme-pk/drug-metabolism/hepatocyte-stability]
- 32. MetaboGNN: predicting liver metabolic stability with graph ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409945/]
- 33. Thawing and Incubating Human and Animal Liver ... [https://www.thermofisher.com/us/en/home/references/protocols/drug-discovery/adme-tox-protocols/microsomes-protocol.html]
- 34. Developing Robust Human Liver Microsomal Stability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11510424/]
- 35. An Integrated Hepatocyte Stability Assay for Simultaneous ... [https://pubmed.ncbi.nlm.nih.gov/38438166/]
- 36. Efficiency in Drug Discovery: Liver S9 Fraction Assay As a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5405623/]
- 37. S9 Stability | Cyprotex ADME-Tox Solutions [https://www.evotec.com/solutions/drug-discovery-preclinical-development/cyprotex-adme-tox-solutions/adme-pk/drug-metabolism/s9-stability]
- 38. Case Study 11: Considerations for Enzyme Mapping ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9147050/]
- 39. Metabolic Stability Assays [https://labtesting.wuxiapptec.com/dmpk-services/metabolic-stability-assays/]
- 40. Considerations for Improving Metabolism Predictions for In ... [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2022.894569/full]
- 41. Drug Metabolism and Pharmacokinetic Evaluation of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389022/]
- 42. How to Overcome 9 Key Peptide Drug Development ... [https://labtesting.wuxiapptec.com/2025/10/10/how-to-overcome-9-key-peptide-drug-development-challenges/]
- 43. HyperPhS: a pharmacophore-guided multimodal ... [https://pubmed.ncbi.nlm.nih.gov/40981510/]
- 44. ELISA Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/elisa-troubleshooting-guide.html]
- 45. Troubleshooting Guide: ELISA [https://www.rndsystems.com/resources/troubleshooting-guide-elisa-development]
- 46. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 47. Lab Automation for High - Throughput Plate-Based Assays [https://www.moleculardevices.com/service-support/lab-automation-solutions/lab-automation-for-high-throughput-plate-based-assays]
- 48. High-Throughput Metabolic Soft-Spot Identification in Liver ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9693510/]
- 49. Metabolic Stability [https://www.pharmafocusasia.com/articles/metabolic-stability]
- 50. Triple labeling of metabolites for metabolome analysis ... [https://pubmed.ncbi.nlm.nih.gov/40633218/]
- 51. Enhancing tandem mass spectrometry-based metabolite ... [https://www.nature.com/articles/s41467-025-61240-z]
- 52. What Are Metabolite Profiling & Identification Studies? [https://labtesting.wuxiapptec.com/2023/03/30/what-are-metabolite-profiling-identification-studies/]
- 53. Drug Metabolite Profiling and Identification by High- ... [https://www.sciencedirect.com/science/article/pii/S0021925819485311]
- 54. New Halogen-Containing Drugs Approved by FDA in 2021 [https://pmc.ncbi.nlm.nih.gov/articles/PMC8912053/]
- 55. Improving the decision-making process in the structural ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644604032805]
- 56. Oxidation of Drugs during Drug Product Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC8876153/]
- 57. Oxidation of Drugs during Drug Product Development [https://www.pharmaexcipients.com/news/oxidation-drugs-during-development/]
- 58. Why Decreasing Lipophilicity Alone Is Often Not a Reliable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6004569/]
- 59. Metabolic stability optimization and metabolite ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523414008794]
- 60. Analysis of microsomal metabolic stability using high-flow ... [https://www.sciencedirect.com/science/article/abs/pii/S1570023204002831]
- 61. Solid phase extraction as a faster alternative to HPLC [https://pubmed.ncbi.nlm.nih.gov/17094126/]
- 62. Consideration of Vendor-Related Differences in Hepatic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10840824/]
- 63. Optimization of a Higher Throughput Microsomal Stability ... [https://www.sciencedirect.com/science/article/pii/S2472630322002126]
- 64. Ligand Binding Assay Critical Reagents and Their Stability [https://pmc.ncbi.nlm.nih.gov/articles/PMC4012044/]
- 65. Managing critical reagents through drug development [https://www.drugdiscoverytrends.com/managing-critical-reagents-through-drug-development/]
- 66. Holistic drug design for multiparameter optimization in ... [https://www.sciencedirect.com/science/article/abs/pii/S0960894X21002298]
- 67. How DMPK Lead Optimization Mitigates Risk and ... [https://labtesting.wuxiapptec.com/2021/05/12/how-dmpk-lead-optimization-mitigates-risk-and-conserves-resources/]
- 68. Metabolic Stability Study [https://dmpkservice.wuxiapptec.com/metabolic.html]
- 69. Integrating DMPK Early in Drug Development: A Strategic ... [https://blog.crownbio.com/integrating-dmpk-early-in-drug-development-a-strategic-imperative-for-success]
- 70. Strategies to Optimize Drug Half-Life in Lead Candidate ... [https://pubmed.ncbi.nlm.nih.gov/30675823/]
- 71. A Fully Integrated Assay Panel for Early Drug Metabolism and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7567642/]
- 72. Metabolic dysfunction over a life course key to healthy ageing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12185620/]
- 73. Hepatic Clearance Predictions from In Vitro–In Vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11024986/]
- 74. Interspecies and in vitro‐in vivo scaling for quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9931436/]
- 75. The first South Korean data challenge for drug discovery using ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-01047-8]
- 76. Species differences between mouse, rat, dog, monkey and ... [https://pubmed.ncbi.nlm.nih.gov/17125407/]
- 77. The Discovery of BMT-052, a Pan-genotypic HCV NS5B ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5512134/]
- 78. Overcoming In Vitro Liver Metabolism Screening ... [https://dls.com/resources/overcoming-in-vitro-liver-metabolism-screening-limitations-with-permeabilized-human-hepatocytes/]
- 79. Navigating Transporter Sciences in Pharmacokinetics ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624055417]
- 80. More Accurate Prediction of Human Pharmacokinetic ... [https://dmpkservice.wuxiapptec.com/articles/438-more-accurate-prediction-of-human-pharmacokinetic-parameters-for-small-molecule-compounds-methods-models-and-applications/]
- 81. Uncertainty-Aware Metabolic Stability Prediction with Dual ... [https://arxiv.org/abs/2506.00936]
- 82. MetaboGNN: predicting liver metabolic stability with graph ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-01089-y]
- 83. A machine learning-based framework for predicting ... [https://www.nature.com/articles/s41598-025-06723-1]
- 84. Modelling and simulation: questions and answers [https://www.ema.europa.eu/en/human-regulatory-overview/research-and-development/scientific-guidelines/clinical-pharmacology-pharmacokinetics/modelling-simulation-questions-answers]
- 85. Metabolic Stability In Drug Metabolism: IVIVE Models [https://www.pharmaron.com/knowledge-center/metabolic-stability-drug-metabolism/]
- 86. Western Blot Troubleshooting Guide [https://www.bosterbio.com/protocol-and-troubleshooting/western-blot-troubleshooting?srsltid=AfmBOoqXwQiqlrh5CF9OQINAa3yttvP9kU-0BMLZhU0PDfJhwPCJ6y65]
- 87. Bradford Assay Troubleshooting Guide Common Errors ... [https://go.zageno.com/blog/bradford-assay-troubleshooting]
- 88. Western Blot Antibody Troubleshooting [https://www.genscript.com/Western-Blot-Antibody-Troubleshooting.html]
- 89. In Vitro ADME [https://www.jubilantbiosys.com/services/in-vitro-adme/]
- 90. In Vitro ADME Studies: Laying the Foundation for ... [https://www.infinixbio.com/blog/in-vitro-adme-studies-laying-the-foundation-for-preclinical-success/]
- 91. ADME & In Vitro Toxicology [https://southernresearch.org/cro-service/adme-tox/]