In Silico Pharmacokinetic Prediction: Integrating AI, PBPK, and Machine Learning for Modern Drug Development
This article provides a comprehensive overview of the basic principles and advanced applications of in silico pharmacokinetic (PK) prediction for researchers and drug development professionals.
In Silico Pharmacokinetic Prediction: Integrating AI, PBPK, and Machine Learning for Modern Drug Development
Abstract
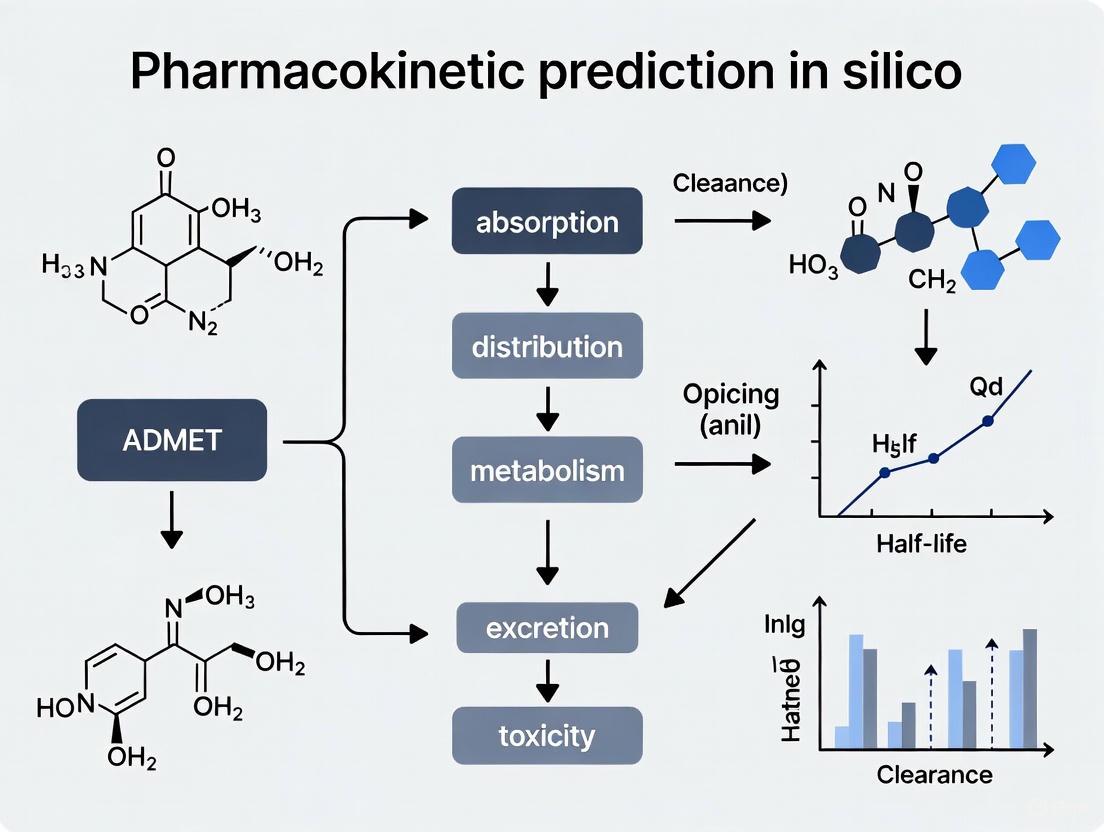
This article provides a comprehensive overview of the basic principles and advanced applications of in silico pharmacokinetic (PK) prediction for researchers and drug development professionals. It explores the foundational concepts of physiologically-based pharmacokinetic (PBPK) modeling and its integration with artificial intelligence (AI) and machine learning (ML). The scope spans from core methodologies like quantitative structure-activity relationship (QSAR) and PBPK modeling to their practical application in predicting absorption, distribution, metabolism, and excretion (ADME) properties. It addresses key challenges such as model complexity, parameter uncertainty, and computational efficiency, while also covering validation frameworks and comparative analyses of different modeling approaches. The content highlights how these in silico tools enable more efficient, cost-effective, and ethical drug development from discovery through clinical stages.
The Core Principles of In Silico Pharmacokinetics: From Physiological Concepts to AI Integration
Physiologically-based pharmacokinetic (PBPK) modeling is a mechanistic, mathematical technique for predicting the absorption, distribution, metabolism, and excretion (ADME) of chemical substances in humans and other animal species [1]. Unlike classical compartmental pharmacokinetic models, which use empirical fitting to plasma concentration data, PBPK models incorporate prior knowledge of human or animal physiology and the physicochemical properties of a drug to achieve a mechanistic representation within biological systems [2] [3]. This allows for a priori simulation of drug concentration-time profiles not only in plasma but also at specific sites of action, which are often difficult or impossible to measure experimentally [2].
The fundamental principle of PBPK modeling, introduced as early as the 1920s and formally described by Teorell in 1937, is to divide the body into physiologically relevant compartments corresponding to actual organs and tissues [4] [5] [6]. These compartments are interconnected by the circulatory system and characterized by physiological parameters such as blood-flow rates, tissue volumes, and permeability, creating an integrated system that mirrors the anatomy and physiology of the organism [2] [1] [3]. PBPK modeling represents a "middle-out" approach, combining elements of both data-driven "top-down" and mechanistic "bottom-up" strategies, and has become an indispensable tool in drug development, regulatory review, and health risk assessment [6] [7].
Core Principles and Model Structure
Fundamental Concepts and Historical Context
PBPK modeling is grounded in the principle that the mammalian body can be represented as an interconnected system of physiological compartments. A whole-body PBPK model explicitly represents organs most relevant to ADME processes, typically including heart, lung, brain, stomach, gut, liver, kidney, adipose tissue, muscle, and skin [2] [4]. These tissues are linked by arterial and venous blood pools, with each organ characterized by its specific blood-flow rate, volume, and partition coefficients [2].
The development of PBPK modeling began with seminal work by Bischoff, Brown, and Dedrick in the 1960s and 1970s, followed by influential publications on styrene and methylene chloride in the 1980s that expanded its application in toxicology and risk assessment [3]. The approach has flourished in recent decades, facilitated by increased computational power and the development of specialized software platforms, with now over 700 publications related to PBPK modeling across industrial chemicals, pharmaceuticals, and environmental pollutants [3].
Mathematical Foundation
PBPK models operate on mass balance principles, where the rate of change of drug quantity in each compartment is described by differential equations that account for all transport and metabolic processes [4] [3]. For a generic tissue compartment i, the basic mass balance equation under perfusion-limited kinetics is:
dQ_i/dt = F_i * (C_art - Q_i/(P_i * V_i)) [1]
Where:
dQ_i/dt= rate of change of drug quantity in compartmentiF_i= blood flow rate to compartmentiC_art= drug concentration in arterial bloodP_i= tissue-to-blood partition coefficientV_i= volume of compartmenti
The liver compartment typically has a more complex equation that accounts for input from the hepatic artery and portal vein (from intestinal and splenic circulation) [1]:
dQ_l/dt = F_a * C_art + F_g * (Q_g/(P_g * V_g)) + F_pn * (Q_pn/(P_pn * V_pn)) - (F_a + F_g + F_pn) * (Q_l/(P_l * V_l))
These differential equations for all compartments form a system that is solved numerically to simulate concentration-time profiles throughout the body [4].
Diagram: Structure of a Whole-Body PBPK Model
The following diagram illustrates the compartmental structure and circulatory connections of a typical whole-body PBPK model:
Diagram Title: Whole-Body PBPK Model Structure
This diagram shows the fundamental structure where organs are connected in parallel between arterial and venous blood pools, with the liver receiving additional input from the gastrointestinal tract via the portal vein [4] [1]. The lung compartment closes the circulatory loop.
Critical PBPK Model Parameters
PBPK model parameters can be categorized into three main groups: organism-specific physiological parameters, drug-specific properties, and administration protocol specifications [2].
Physiological Parameters
Physiological parameters describe the anatomy and physiology of the organism being modeled and are typically obtained from established literature compilations [2] [3]. These parameters are largely independent of the specific drug being studied.
Table 1: Key Physiological Parameters in PBPK Models
| Parameter Type | Examples | Source |
|---|---|---|
| Organ volumes | Liver volume, kidney volume, brain volume | Biological data compilations [3] |
| Blood flow rates | Cardiac output, hepatic blood flow, renal blood flow | Physiological literature [3] |
| Tissue composition | Water, lipid, protein content in various tissues | Experimental measurements [4] |
| Expression levels | Enzyme and transporter expression in different tissues | Proteomic/transcriptomic data [2] |
| Biometric data | Body weight, height, age, organ size relationships | Population databases [5] |
For special populations (e.g., pediatric, geriatric, or diseased populations), these physiological parameters are adjusted to reflect population-specific anatomical and physiological differences [2] [6].
Drug-Specific Parameters
Drug-specific parameters characterize the physicochemical and biological properties of the compound being modeled and can be further divided into two subcategories.
Table 2: Essential Drug-Specific Parameters for PBPK Modeling
| Parameter Category | Specific Parameters | Determination Methods |
|---|---|---|
| Physicochemical properties (independent of organism) | Molecular weight, lipophilicity (log P), acid dissociation constant (pKa), solubility | Experimental measurement or in silico prediction [2] [8] |
| Drug-biological system interaction properties | Fraction unbound in plasma (fu), blood-to-plasma ratio (B/P), tissue-plasma partition coefficients, membrane permeability, metabolic parameters (Km, Vmax), transport parameters | In vitro experiments, in vitro-in vivo extrapolation (IVIVE), quantitative structure-property relationships [2] [9] |
For tissue distribution, partition coefficients are frequently calculated using established distribution models that predict the equilibrium distribution between plasma and tissues based on drug physicochemical properties and tissue composition [2]. Passive processes like membrane permeation can often be predicted from fundamental properties, while active processes (metabolism, transport) typically require specific experimental data [2] [4].
The PBPK Modeling Workflow
Model Building Process
Building a PBPK model follows a systematic workflow that integrates information from multiple sources. The process can be summarized in several key stages:
Problem Identification and Literature Evaluation: Define the purpose of the model and conduct a thorough review of existing literature on the drug and relevant physiology [3].
Parameter Acquisition and Estimation: Gather the three essential parameter sets: physiological parameters (ventilation rates, cardiac output, organ volumes), thermodynamic parameters (tissue partition coefficients), and biochemical parameters (Km, Vmax for metabolism) [3].
Model Implementation: Construct the mathematical model using mass balance differential equations for each compartment, representing the interconnected physiological system [3].
Model Verification and Validation: Compare simulations with experimental pharmacokinetic data to assess model performance, then validate with additional independent data sets [3] [5].
Model Application: Use the validated model for its intended application, such as predicting exposure in special populations, evaluating drug-drug interactions, or supporting regulatory submissions [2] [9].
A recent example demonstrating this workflow is the development of a PBPK model for fexofenadine, which commenced with a comprehensive literature review to collect pertinent pharmacokinetic data, followed by model construction using PK-Sim software, and subsequent extrapolation to special populations including chronic kidney disease patients and pediatrics [5].
Diagram: PBPK Model Development Workflow
The following flowchart illustrates the systematic approach to PBPK model development:
Diagram Title: PBPK Model Development Workflow
This workflow highlights the iterative nature of PBPK model development, where discrepancies between simulations and experimental data may require parameter refinement or structural model adjustments [2] [3].
Key Applications in Drug Development
PBPK modeling has become an integral tool throughout the drug development continuum, with applications spanning from early discovery through clinical development and regulatory submission.
Table 3: Key Applications of PBPK Modeling in Pharmaceutical Research and Development
| Application Area | Specific Use Cases | Impact and Significance |
|---|---|---|
| First-in-Human (FIH) Predictions | Prediction of human pharmacokinetics from preclinical data, dose selection for first clinical trials [9] | Reduces uncertainty in initial human studies, helps establish safe starting doses [9] |
| Special Population Extrapolations | Pediatric extrapolations, patients with hepatic or renal impairment, elderly populations [2] [6] | Supports dose adjustments for populations where clinical trials are ethically or practically challenging [5] [6] |
| Drug-Drug Interaction (DDI) Assessment | Evaluation of enzyme inhibition/induction, transporter-mediated interactions [2] [7] | Identifies and quantifies DDI risks, informs contraindications and dose adjustments [2] |
| Formulation Development | Evaluation of different formulations, food effect predictions, absorption assessment [9] [6] | Guides formulation strategy to optimize bioavailability and product performance [6] |
| Regulatory Submissions | Support for labeling claims, pediatric study plans, DDI assessments [6] [7] | Provides mechanistic evidence to regulatory agencies, increasingly expected in submissions [6] |
According to a systematic review of PBPK publications between 2008-2014, the most common applications were drug-drug interaction studies (28%), interindividual variability and general clinical pharmacokinetics predictions (23%), absorption kinetics (12%), and age-related changes in pharmacokinetics (10%) [7]. For FDA regulatory filings, models were primarily used for DDI predictions (60%), pediatrics (21%), and absorption predictions (6%) [7].
Research Tools and Software Platforms
The implementation of complex PBPK models has been greatly facilitated by the development of specialized software platforms that integrate physiological databases and implement PBPK modeling approaches [2]. These tools have made PBPK modeling more accessible to researchers without requiring extensive programming or mathematical expertise.
Table 4: Key Software Platforms for PBPK Modeling
| Software Platform | Vendor/Developer | Key Features and Applications |
|---|---|---|
| GastroPlus | Simulations Plus | Comprehensive PBPK platform with absorption and dissolution modeling; offers training courses including "Introduction to PBPK Modeling" [2] [10] |
| Simcyp Simulator | Certara | Population-based PBPK platform with extensive library of virtual populations; used for DDI and special population modeling [2] [8] |
| PK-Sim | Bayer Technology Services/Open Systems Pharmacology | Whole-body PBPK modeling integrated with MoBi for multiscale systems pharmacology; used in recent fexofenadine PBPK study [2] [4] [5] |
| ADMET Predictor | Simulations Plus | QSAR-based property prediction software that can be used in conjunction with PBPK platforms to estimate parameters for new chemical entities [8] |
These platforms typically include extensive physiological databases covering multiple species, populations, and age groups, which are combined with compound-specific information to parameterize whole-body PBPK models [2]. Many also incorporate systems for in vitro-in vivo extrapolation (IVIVE) to predict clearance from enzyme and transporter kinetics [9].
Experimental Protocols for PBPK Modeling
Parameter Estimation Protocol
A critical step in PBPK model development is the acquisition and estimation of necessary parameters. The following protocol outlines a systematic approach:
Physiological Parameter Collection:
- Source species-specific physiological parameters (organ volumes, blood flows) from established databases such as those provided by the International Life Sciences Institute (ILSI) [3].
- For special populations, collect age-dependent or disease-specific physiological changes from literature (e.g., reduced renal function in chronic kidney disease) [5] [6].
Drug-Specific Parameter Determination:
- Measure or obtain from literature fundamental physicochemical properties: molecular weight, lipophilicity (log P), acid dissociation constants (pKa), and solubility [2] [8].
- Determine plasma protein binding (fraction unbound) using equilibrium dialysis or ultrafiltration [9].
- Calculate tissue:plasma partition coefficients using established distribution models (e.g., Poulin and Rodgers, Berezhkovskiy) implemented in PBPK software [2].
- For metabolism parameters, conduct in vitro metabolism studies using human liver microsomes, hepatocytes, or recombinant enzymes to obtain Km and Vmax values, then scale using IVIVE [9].
Sensitivity Analysis:
- Perform sensitivity analysis to identify parameters with the greatest influence on key model outputs (e.g., AUC, Cmax) [6].
- Prioritize experimental verification of high-sensitivity parameters.
Model Verification and Validation Protocol
Establishing model credibility requires rigorous verification and validation:
Model Verification:
- Compare model predictions with observed plasma concentration-time data from clinical studies [3] [5].
- Use visual predictive checks to assess overlap between simulated and observed concentration-time profiles [5].
- Calculate quantitative metrics such as observed-to-predicted ratios (RObs/Pre), average fold error (AFE), and absolute average fold error (AAFE) with a common acceptance criterion of within two-fold error [5].
External Validation:
PBPK modeling represents a fundamental advancement in pharmacokinetic prediction, shifting from empirical descriptive approaches to mechanistic, physiology-based frameworks. By explicitly representing the anatomical and physiological structure of the body, PBPK models provide a powerful platform for predicting drug concentrations not only in plasma but also at specific sites of action, enabling more informed decisions throughout drug discovery and development [2] [4].
The strength of PBPK modeling lies in its ability to integrate diverse data types—from in vitro assays to clinical observations—into a unified mechanistic framework that supports extrapolation to novel clinical scenarios [2] [6]. This capability is particularly valuable for addressing challenges in special populations where clinical trials may be ethically or practically challenging, such as pediatric patients, pregnant women, or individuals with organ impairment [5] [6].
As PBPK modeling continues to evolve, it is increasingly integrated with pharmacodynamic models to form comprehensive PBPK/PD models that can predict both drug exposure and response [2]. Furthermore, the incorporation of population variability and Bayesian statistical methods enhances the utility of PBPK models for personalized medicine approaches, moving closer to the goal of delivering the "right drug at the right dose" for individual patients [6] [7]. With ongoing advancements in computational power, physiological knowledge, and biochemical characterization of drugs, PBPK modeling is positioned to play an increasingly central role in silico pharmacokinetic research and model-informed drug development.
Pharmacokinetics (PK) is the study of how the body interacts with administered substances for the entire duration of exposure, focusing on the processes of absorption, distribution, metabolism, and excretion (ADME) [11]. These four parameters fundamentally influence the drug levels and kinetics of drug exposure to tissues, thereby determining the compound's pharmacological activity and performance as a drug [12]. In the context of modern drug development, understanding ADME is critical for predicting the systemic exposure of a drug over time, which directly informs dosage regimen design to ensure that the majority of patients achieve a therapeutic exposure range without intolerable side effects [13].
The integration of in silico (computational) research methods has revolutionized the evaluation of ADME properties early in the drug discovery pipeline. These approaches offer a compelling advantage by eliminating the need for physical samples and laboratory facilities, providing rapid and cost-effective alternatives to expensive and time-consuming experimental testing [14]. For researchers and drug development professionals, pharmacokinetic prediction models are indispensable tools for prioritizing lead compounds, forecasting human pharmacokinetics, and reducing late-stage attrition due to suboptimal drug-like properties.
The ADME Process: A Detailed Technical Examination
Absorption
Definition and Importance: Absorption is the process that brings a drug from its site of administration into the systemic circulation [11]. This stage critically determines the drug's bioavailability, which is defined as the fraction of the administered drug that reaches the systemic circulation in an active form [15]. The rate and extent of absorption directly affect the speed and concentration at which a drug arrives at its desired location of effect [11].
Key Mechanisms and Factors: The absorption process involves liberation, the process by which the drug is released from its pharmaceutical dosage form, which is especially critical for oral medications [11]. A primary consideration for orally administered drugs is the first-pass effect, where the drug is metabolized in the liver or gut wall before it reaches the systemic circulation, significantly reducing its bioavailability [11] [16]. Factors influencing drug absorption include:
- Route of administration (e.g., oral, intravenous, transdermal) [11] [16]
- Chemical properties of the drug (e.g., solubility, stability) [15]
- Formulation characteristics [13]
- Drug-food and drug-drug interactions [15] [13]
- Patient-specific factors such as gastric pH and emptying time [16]
Routes of Administration and Bioavailability:
| Route of Administration | Bioavailability | Key Characteristics | First-Pass Effect |
|---|---|---|---|
| Intravenous (IV) | 100% [11] [15] | Direct delivery into systemic circulation; rapid onset [11] | Avoided [16] |
| Oral (PO) | Variable; often <100% [11] [15] | Convenient; subject to GI environment and hepatic metabolism [11] [16] | Yes [11] [16] |
| Intramuscular (IM) | High | Absorption depends on blood flow to the muscle [11] | Avoided [16] |
| Subcutaneous (SC) | High | Slower absorption than IM [16] | Avoided [16] |
| Transdermal | Variable | Slow, steady drug delivery; bypasses liver [16] | Avoided [16] |
| Inhalation | Variable | Rapid delivery via lungs; large surface area for absorption [16] | Avoided [16] |
Distribution
Definition and Importance: After a drug is absorbed, it is distributed throughout the body into various tissues and organs [15]. Distribution describes the reversible transfer of a drug between different compartments and is crucial because it affects how much drug ends up at the active sites, thereby influencing both efficacy and toxicity [15] [12].
Key Parameters and Concepts:
- Volume of Distribution (Vd): A fundamental PK parameter defined as the amount of drug in the body divided by the plasma drug concentration [11]. It is a theoretical volume that describes the dissemination of a drug throughout the body's compartments. A low Vd indicates the drug is largely confined to the plasma, while a high Vd suggests extensive distribution into tissues [11].
- Protein Binding: Drugs can bind to plasma proteins (e.g., albumin), rendering them pharmacologically inactive while bound [13]. Only the free, unbound drug can act at receptor sites, be distributed into tissues, or be eliminated [11] [13]. Changes in protein binding (e.g., due to disease or drug interactions) can significantly alter the drug's effect and potential for toxicity [11].
- Barriers to Distribution: Natural barriers, such as the blood-brain barrier, can prevent certain drugs from reaching their target sites. Drugs with characteristics like high lipophilicity, small size, and low molecular weight are better able to cross this barrier [15].
Diagram 1: Drug Distribution and Protein Binding. This graph illustrates the equilibrium between free and protein-bound drug in plasma, and the movement of free drug to tissue compartments and receptor sites to exert a pharmacological effect.
Metabolism
Definition and Importance: Drug metabolism is the process of chemically altering drug molecules to create new compounds called metabolites [13]. This process is primarily a deactivation mechanism, converting lipophilic drugs into more water-soluble compounds to facilitate their excretion, though it can also activate prodrugs [11] [15].
Primary Pathways and Enzymes: The majority of small-molecule drug metabolism occurs in the liver via enzyme systems, with the cytochrome P450 (CYP450) family being the most prominent, responsible for metabolizing 70-80% of all drugs in clinical use [15].
- Phase I Reactions: Involve functionalization reactions such as oxidation, reduction, and hydrolysis. These reactions, often mediated by CYP450 enzymes, typically introduce or expose a functional group, making the drug more polar [11] [13].
- Phase II Reactions: Conjugation reactions (e.g., glucuronidation, sulfation) that attach an endogenous molecule to the drug or its Phase I metabolite. This usually increases water solubility substantially and inactivates the drug, facilitating biliary or renal excretion [11] [13].
Factors Influencing Metabolism:
- Genetics: Genetic polymorphisms can result in individuals being classified as poor metabolizers (PMs) or ultra-rapid metabolizers (UMs), leading to significant variability in drug exposure and response [15].
- Drug-Drug Interactions: Concomitant medications can inhibit or induce metabolic enzymes, leading to clinically significant interactions [15].
- Age: Liver function is reduced in the elderly and immature in newborns, requiring special dosing considerations [15] [16].
- Organ Impairment: Liver disease can profoundly impair drug metabolism [13].
Excretion
Definition and Importance: Excretion is the process by which the drug and its metabolites are eliminated from the body [11]. This process, along with metabolism, determines the duration and intensity of a drug's action [12].
Routes and Mechanisms of Excretion:
- Renal Excretion: The kidneys are the most important organs for excretion [12]. Renal clearance involves three main mechanisms: glomerular filtration of unbound drug, active secretion by transporters in the tubules, and passive reabsorption [11] [12].
- Biliary/Fecal Excretion: Some drugs and their metabolites are excreted into the bile and then into the feces [12].
- Other Routes: Excretion can also occur via the lungs (e.g., anesthetic gases), sweat, and breast milk [12].
Key Pharmacokinetic Parameters of Elimination:
- Clearance (CL): Defined as the ratio of a drug's elimination rate to the plasma drug concentration. It is a critical parameter for determining the maintenance dose rate [11].
- Half-Life (t½): The time required for the plasma concentration of a drug to decrease by 50%. It is directly proportional to the volume of distribution and inversely proportional to clearance (t½ = 0.693 × Vd / Clearance) [11]. A drug is generally considered eliminated after four to five half-lives [11].
- Drug Kinetics: Most drugs follow first-order kinetics, where the rate of elimination is proportional to the drug concentration. Some drugs, like phenytoin and alcohol, follow zero-order kinetics at high concentrations, where the elimination rate is constant and independent of concentration due to enzyme saturation [11].
Quantitative Pharmacokinetic Parameters
A critical component of pharmacokinetic prediction is the quantification of key parameters that define the ADME profile of a drug. These values are essential for building robust in silico models and making accurate predictions of human pharmacokinetics.
Table 2: Key Quantitative PK Parameters and Their Applications
| Parameter | Symbol | Definition | Formula/Description | Clinical/Research Application |
|---|---|---|---|---|
| Bioavailability | F | Fraction of administered dose that reaches systemic circulation [11] | F = (AUCoral / AUCIV) * (DoseIV / Doseoral) [11] | Determines equivalent dosing between routes [11] |
| Area Under the Curve | AUC | Total drug exposure over time [11] | Integral of plasma concentration-time curve [11] | Used to calculate bioavailability and clearance [11] |
| Volume of Distribution | Vd | Apparent volume into which a drug distributes [11] | Vd = Amount of drug in body / Plasma drug concentration [11] | Predicts loading dose; indicates extent of tissue distribution [11] |
| Clearance | CL | Volume of plasma cleared of drug per unit time [11] | CL = Elimination rate / Plasma concentration [11] | Determines maintenance dose rate [11] |
| Half-Life | t½ | Time for plasma concentration to reduce by 50% [11] | t½ = (0.693 * Vd) / CL [11] | Predicts time to steady-state and time for drug elimination [11] |
4In SilicoADME Prediction: Methods and Protocols
Computational ADME prediction has become an integral part of drug discovery, helping to identify potential liabilities early and optimize lead compounds [14]. A variety of in silico methods are employed, ranging from fundamental quantitative structure-activity relationship (QSAR) models to complex physiological simulations.
Predominant Computational Methods
- Quantitative Structure-Activity Relationship (QSAR): This method uses statistical modeling to relate a drug's molecular descriptors or structural properties to its biological activity or ADME properties [14] [12]. It is widely used for high-throughput virtual screening.
- Physiologically Based Pharmacokinetic (PBPK) Modeling: PBPK models simulate the concentration-time profile of a drug in different tissues by incorporating physiological parameters (e.g., organ sizes, blood flows), tissue composition, and drug-specific properties [14]. These models are powerful for predicting human PK, exploring drug-drug interactions (DDIs), and supporting regulatory submissions [17].
- Molecular Docking: This technique predicts the preferred orientation of a small molecule (drug) when bound to a target macromolecule (e.g., a CYP enzyme or transporter) [14]. It helps in understanding and predicting metabolic stability and transporter-mediated DDIs.
- Molecular Dynamics (MD) Simulations: MD simulations provide atomic-level detail of the motions and interactions of a drug with its environment over time, offering insights into binding affinities and reaction mechanisms relevant to metabolism [14].
Diagram 2: In Silico ADME Prediction Workflow. This flowchart outlines the primary computational approaches used to predict ADME properties from a compound's molecular structure, leading to data-driven lead optimization.
Experimental Protocols forIn VitroADME Assay
The development and validation of in silico models rely heavily on high-quality experimental data from standardized in vitro assays. The following protocols represent core methodologies for characterizing ADME properties.
Protocol 1: Metabolic Stability Assay Using Liver Microsomes
Objective: To determine the intrinsic metabolic clearance of a drug candidate by measuring its degradation rate in liver microsomes.
Materials:
- Test compound (e.g., drug candidate)
- Liver microsomes (human or relevant species) - source of CYP450 enzymes [17]
- NADPH-regenerating system - cofactor for CYP450 reactions
- Phosphate buffer (e.g., 0.1 M, pH 7.4)
- Stop solution (e.g., acetonitrile with internal standard)
- LC-MS/MS system for analytical quantification
Procedure:
- Incubation Preparation: Prepare incubation mixtures containing liver microsomes (e.g., 0.5 mg/mL protein) and the test compound (e.g., 1 µM) in phosphate buffer. Pre-incubate for 5 minutes at 37°C.
- Reaction Initiation: Start the reaction by adding the NADPH-regenerating system.
- Time Course Sampling: At predetermined time points (e.g., 0, 5, 15, 30, 60 minutes), remove aliquots from the incubation mixture and transfer them to a plate containing the stop solution to denature proteins and terminate the reaction.
- Sample Analysis: Centrifuge the stopped samples to precipitate proteins. Analyze the supernatant using LC-MS/MS to determine the remaining concentration of the parent compound over time.
- Data Analysis: Plot the natural logarithm of the parent compound concentration remaining versus time. The slope of the linear phase is the elimination rate constant (k). Intrinsic clearance (CLint) is calculated as CLint = k / (microsomal protein concentration).
Protocol 2: Caco-2 Permeability Assay for Predicting Absorption
Objective: To assess the intestinal permeability and potential for oral absorption of a drug candidate using a human colon adenocarcinoma cell line (Caco-2).
Materials:
- Caco-2 cell line
- Transwell plates (e.g., 12-well format with polycarbonate membranes)
- Dulbecco's Modified Eagle Medium (DMEM) with fetal bovine serum (FBS)
- Hanks' Balanced Salt Solution (HBSS) with HEPES buffer (pH 7.4)
- Test compound
- LC-MS/MS system for analytical quantification
Procedure:
- Cell Culture: Seed Caco-2 cells onto Transwell membranes at a high density and culture for 21-28 days to allow for differentiation and formation of a confluent monolayer. Monitor transepithelial electrical resistance (TEER) to confirm monolayer integrity.
- Experiment Setup: On the day of the experiment, wash the cell monolayers with pre-warmed HBSS. Add the test compound to the donor compartment (apical for A→B transport, basolateral for B→A transport). Fill the receiver compartment with blank HBSS.
- Incubation and Sampling: Incubate the plates at 37°C with gentle shaking. Sample from the receiver compartment at regular intervals (e.g., 30, 60, 90, 120 minutes) and replace with fresh pre-warmed HBSS.
- Sample Analysis: Quantify the concentration of the test compound in the receiver samples using LC-MS/MS.
- Data Analysis: Calculate the apparent permeability coefficient (Papp) using the formula: Papp = (dQ/dt) / (A * C0), where dQ/dt is the transport rate, A is the surface area of the membrane, and C0 is the initial donor concentration.
Table 3: Key Research Reagent Solutions for ADME Studies
| Reagent/Resource | Function in ADME Research | Application Example |
|---|---|---|
| Recombinant CYP Enzymes | Individual human cytochrome P450 isoforms for reaction phenotyping and DDI studies. | Identifying which specific CYP enzyme is responsible for metabolizing a drug candidate [15]. |
| Cryopreserved Hepatocytes | Intact liver cells containing full complement of phase I and II metabolic enzymes; used for more physiologically relevant metabolism studies. | Assessing metabolic stability and metabolite identification [17]. |
| Transfected Cell Lines | Cell lines overexpressing specific transporters (e.g., P-gp, BCRP, OATP). | Evaluating potential for transporter-mediated drug-drug interactions and permeability [17]. |
| Plasma Proteins | Human serum albumin (HSA) and alpha-1-acid glycoprotein (AAG) for protein binding studies. | Determining the fraction of drug that is unbound and pharmacologically active using assays like equilibrium dialysis [11] [13]. |
| PBPK Software Platforms | Commercial software (e.g., GastroPlus, Simcyp, PK-Sim) for simulating ADME in virtual populations. | Predicting human pharmacokinetics, food effects, and DDI potential prior to first-in-human studies [17] [14]. |
| Radiolabeled Compounds | Drug molecules labeled with isotopes (e.g., ¹⁴C, ³H) to track the fate of the drug and its metabolites. | Conducting definitive human ADME studies to elucidate mass balance and metabolic pathways [17]. |
Data Visualization and Model Communication in Pharmacokinetics
Effective communication of complex pharmacokinetic data and model outcomes is essential for informing drug development decisions. Visualization techniques transform numerical data into intuitive graphics, facilitating pattern recognition and timely decision-making [18].
Key Visualization Techniques:
- Line Graphs: The standard for depicting changes in drug concentration over time, allowing for the visualization of absorption and elimination profiles and the determination of parameters like half-life and Tmax [18].
- Visual Predictive Checks (VPCs): A graphical qualification tool where percentiles of observed data are overlaid with confidence intervals of the corresponding percentiles from model-based simulations. This assesses how well a population PK model captures the central tendency and variability of the data [19].
- Box-and-Whisker Plots: Useful for comparing the distribution of PK parameters (e.g., AUC, Cmax) across different patient populations, dose groups, or formulations [18].
- Interactive Visualization: Advanced software tools allow for interactive exploration of models, enabling project teams to ask "what-if" questions in real-time (e.g., "What is the impact of a higher dose or a different dosing interval?") and see the simulated outcomes immediately, thereby streamlining the decision-making process [19] [20].
The thorough understanding of Absorption, Distribution, Metabolism, and Excretion (ADME) processes forms the bedrock of pharmacokinetic science. For today's researchers and drug development professionals, the integration of robust in vitro and in vivo experimental data with sophisticated in silico prediction models is no longer optional but a necessity for efficient and successful drug development. The quantitative parameters derived from ADME studies directly enable the design of safe and effective dosing regimens, while computational tools like PBPK modeling and QSAR provide a powerful means to anticipate and overcome ADME-related challenges earlier in the pipeline. As these computational methods continue to evolve, their role in de-risking drug development and enabling truly predictive pharmacokinetics will only become more pronounced, ultimately accelerating the delivery of new therapies to patients.
The Role of Quantitative Structure-Activity Relationship (QSAR) in Early Parameter Estimation
Quantitative Structure-Activity Relationship (QSAR) modeling represents a fundamental computational approach in modern drug discovery and development, enabling the prediction of biological activity, pharmacokinetic properties, and toxicity of compounds directly from their molecular structures. These methodologies have become indispensable tools for early parameter estimation, particularly within the broader context of silico pharmacokinetic prediction research. By establishing mathematical relationships between molecular descriptors and experimentally determined biological endpoints, QSAR models allow researchers to prioritize promising candidate molecules, reduce reliance on costly and time-consuming experimental assays, and adhere to the principles of the 3Rs (Replacement, Reduction, and Refinement) in animal testing [21] [22].
The evolution of QSAR has progressed from traditional linear regression models based on simple physicochemical properties to sophisticated machine learning and deep learning algorithms that leverage vast chemical databases and complex molecular descriptors [23] [24]. This technical guide explores the core methodologies, applications, and emerging trends in QSAR modeling, with a specific focus on its critical role in predicting key pharmacokinetic parameters during the early stages of drug development. By providing researchers with a comprehensive framework for implementing these computational approaches, this whitepaper aims to support the development of more efficient and predictive drug discovery pipelines.
Fundamental QSAR Methodologies in Pharmacokinetic Prediction
Molecular Descriptors and Feature Selection
The foundation of any robust QSAR model lies in the careful selection and computation of molecular descriptors that numerically represent structural and physicochemical properties of compounds. These descriptors can be broadly categorized into several classes:
- Constitutional descriptors: Basic molecular properties including molecular weight, number of atoms, bonds, or rings [25]
- Topological descriptors: Graph-based representations encoding molecular connectivity patterns
- Geometrical descriptors: Parameters derived from the three-dimensional structure of molecules
- Electronic descriptors: Quantities representing electronic distribution such as dipole moment, polar surface area (PSA), and highest occupied molecular orbital (HOMO) or lowest unoccupied molecular orbital (LUMO) energies [25]
- Quantum chemical descriptors: Properties calculated using quantum mechanical methods
Feature selection techniques are critically important for developing predictive and interpretable QSAR models. Methods such as Genetic Function Approximation (GFA), permutation importance analysis in random forest, and stepwise regression help identify the most relevant descriptors while reducing the risk of overfitting [24] [26]. For instance, in a QSAR study on acetylcholinesterase inhibitors, polar surface area, dipole moment, and molecular weight were identified as the key structural properties governing inhibitory activity [25].
Statistical Modeling Approaches
QSAR modeling employs a diverse range of statistical and machine learning algorithms to establish quantitative relationships between molecular descriptors and biological activities:
- Multiple Linear Regression (MLR): Creates linear models based on descriptor-activity relationships, providing easily interpretable equations [25]
- Multiple Non-Linear Regression (MNLR): Captures non-linear relationships in the data
- Artificial Neural Networks (ANN): Powerful pattern recognition algorithms capable of modeling complex non-linear relationships [27]
- Random Forest: Ensemble learning method that constructs multiple decision trees and aggregates their predictions [24]
- Support Vector Machines (SVM): Effective for classification and regression tasks in high-dimensional spaces
- Deep Learning (DL): Advanced neural network architectures that can automatically learn relevant features from raw molecular data or images [24]
The selection of an appropriate modeling technique depends on the dataset characteristics, the complexity of the structure-activity relationship, and the desired balance between model interpretability and predictive power.
Experimental Protocols for QSAR Model Development
Standard QSAR Modeling Workflow
A robust QSAR modeling protocol involves several critical steps to ensure predictive reliability and regulatory acceptance:
Data Collection and Curation: Compile a structurally diverse set of compounds with reliable experimental biological activity data (e.g., IC50, EC50, clearance values). The dataset should encompass sufficient chemical diversity to represent the intended application domain [27] [24].
Chemical Structure Representation and Optimization: Generate accurate 2D or 3D molecular structures using software such as Chem3D or Gaussian. Perform geometry optimization using molecular mechanics (MM2) or quantum chemical methods (e.g., B3LYP/6-31G(d)) to obtain energetically stable conformations [27].
Molecular Descriptor Calculation: Compute comprehensive descriptor sets using specialized software packages including Molecular Operating Environment (MOE), alvaDesc, or ADMET Predictor. The number of calculated descriptors often ranges from hundreds to thousands per compound [24].
Dataset Division: Split the dataset into training and test sets using appropriate methods such as Kennard-Stone algorithm, random selection, or k-means clustering. Typically, 70-80% of compounds are allocated for model training, while the remaining 20-30% are reserved for external validation [27] [24].
Model Construction and Internal Validation: Develop QSAR models using selected algorithms on the training set. Perform internal validation using techniques such as leave-one-out (LOO) or leave-many-out (LMO) cross-validation to assess model robustness [27] [25].
External Validation and Applicability Domain Assessment: Evaluate the predictive performance of the finalized model on the external test set. Define the model's applicability domain to identify compounds for which predictions are reliable [25].
Advanced Protocol: DeepSnap-Deep Learning Integration
Recent advances have introduced innovative protocols such as the DeepSnap-Deep Learning (DeepSnap-DL) approach for improved prediction of challenging pharmacokinetic parameters like clearance:
Compound Image Generation: Capture multiple 2D snapshots of chemical structures from different rotational angles (e.g., 65°, 85°, 105°, and 145°) using DeepSnap software [24].
Deep Learning Model Configuration: Implement convolutional neural networks (CNNs) with optimized hyperparameters including learning rate (typically ranging from 0.0000001 to 0.001) and maximum epoch conditions (15-300) [24].
Model Selection and Validation: Identify the optimal model configuration based on validation set performance metrics, particularly area under the curve (AUC) values. For clearance prediction, the best performance was observed at 145° with a maximum epoch of 300 and learning rate of 0.000001 [24].
Ensemble Model Development: Combine predictions from conventional machine learning (using molecular descriptors) and DeepSnap-DL approaches by averaging predicted probabilities or implementing consensus strategies to significantly enhance predictive performance [24].
QSAR Applications in Key Pharmacokinetic Parameter Estimation
Prediction of Plasma Concentration-Time Profiles
The application of QSAR modeling has expanded beyond predicting individual pharmacokinetic parameters to forecasting complete plasma concentration-time profiles. A novel approach involves implicitly integrating deep neural networks with compartmental pharmacokinetic models, enabling direct prediction of concentration curves from chemical structures and in vitro/in silico ADME features [21].
In a comprehensive study utilizing 1,162 compounds across 30 projects, this integrated approach demonstrated significantly improved prediction accuracy compared to methods explicitly using PK parameters. The model achieved median R² values of 0.530-0.673 for intravenous administration and 0.119-0.432 for oral administration in 5-fold cross-validation, outperforming traditional techniques [21]. The methodology employed Integrated Gradients to elucidate feature attributions and their temporal dynamics, providing insights consistent with established pharmacokinetic principles [21].
Clearance Prediction Using Advanced Modeling Techniques
Clearance represents one of the most critical and challenging pharmacokinetic parameters to predict. Recent research has addressed this challenge through innovative modeling strategies:
Table 1: Performance Comparison of Clearance Prediction Models
| Model Type | Dataset Size | Algorithm | AUC | Accuracy | Key Features |
|---|---|---|---|---|---|
| Conventional ML | 1,545 compounds | Random Forest | 0.883 | 0.825 | 100 molecular descriptors selected by permutation importance [24] |
| DeepSnap-DL | 1,545 compounds | Deep Learning | 0.905 | 0.832 | Compound images from multiple angles [24] |
| Ensemble Model | 1,545 compounds | RF + DeepSnap-DL | 0.943 | 0.874 | Mean of predicted probabilities from both models [24] |
| Consensus Model | 1,545 compounds | RF + DeepSnap-DL | 0.958 | 0.959 | Agreement between classifications [24] |
The ensemble approach, which combines conventional machine learning with DeepSnap-DL, demonstrated particularly strong performance, highlighting the value of integrating multiple modeling paradigms for challenging prediction targets [24].
Integrated QSAR-PBPK Modeling Frameworks
The integration of QSAR with physiologically based pharmacokinetic (PBPK) modeling represents a significant advancement in predictive pharmacokinetics. This hybrid approach enables the prediction of tissue distribution and concentration-time profiles for compounds with limited experimental data [28].
A recent application of this framework focused on 34 fentanyl analogs, addressing the significant public health threat posed by these emerging new psychoactive substances. The QSAR-PBPK workflow involved:
Parameter Prediction: Using QSAR models within ADMET Predictor software to estimate critical PBPK input parameters including logD, pKa, and unbound fraction in plasma [28].
Model Validation: Validating the framework using intravenous β-hydroxythiofentanyl in rats, with all predicted PK parameters (AUC₀–t, Vss, T₁/₂) falling within a 2-fold range of experimental values [28].
Tissue Distribution Prediction: Simulating plasma and tissue distribution (including brain and heart) for 34 human fentanyl analogs, identifying eight compounds with brain/plasma ratios >1.2 (compared to fentanyl's ratio of 1.0), indicating higher CNS penetration and abuse potential [28].
This integrated approach demonstrated superior accuracy for predicting human volume of distribution compared to traditional interspecies extrapolation methods (error <1.5-fold vs. >3-fold), providing a scalable strategy for pharmacokinetic evaluation of poorly characterized compounds [28].
Quantitative Performance Data
Table 2: QSAR Model Performance Across Different Pharmacokinetic Applications
| Application Area | Endpoint | Dataset Size | Model Type | Performance Metrics |
|---|---|---|---|---|
| Plasma Concentration Profiles | IV administration | 1,162 compounds | DNN + 2-compartment model | R² = 0.530-0.673 (5-fold CV) [21] |
| Plasma Concentration Profiles | Oral administration | 1,162 compounds | DNN + 2-compartment model | R² = 0.119-0.432 (5-fold CV) [21] |
| Rat Clearance Prediction | Classification (High/Low CL) | 1,545 compounds | Ensemble (RF + DeepSnap-DL) | AUC = 0.943, Accuracy = 0.874 [24] |
| Acetylcholinesterase Inhibition | pIC50 | 48 compounds | Multiple Linear Regression | R² = 0.701, Q²CV = 0.638, R²test = 0.76 [25] |
| Fentanyl Analog PBPK | Volume of Distribution | 34 compounds | QSAR-PBPK | Error <1.5-fold vs. clinical data [28] |
Visualization of QSAR Workflows
Table 3: Essential Computational Tools for QSAR-Based Pharmacokinetic Prediction
| Tool/Resource | Type | Primary Function | Application in PK Parameter Estimation |
|---|---|---|---|
| ADMET Predictor | Software | Molecular descriptor calculation and ADMET prediction | Predicts critical PBPK input parameters (logD, pKa, Fup) [28] |
| GastroPlus | Software | PBPK modeling and simulation | Integrates QSAR-predicted parameters for whole-body PK simulation [28] |
| Molecular Operating Environment (MOE) | Software | Molecular modeling and descriptor calculation | Calculates comprehensive sets of molecular descriptors for QSAR [24] |
| alvaDesc | Software | Molecular descriptor calculation | Generates 2D/3D molecular descriptors for model development [24] |
| DataRobot | Platform | Automated machine learning | Builds and optimizes multiple prediction models for PK parameters [24] |
| DeepSnap | Software | Compound image generation | Creates 2D molecular images for deep learning approaches [24] |
| Gaussian | Software | Quantum chemical calculations | Computes electronic properties and optimizes molecular geometry [27] |
| National Cancer Institute (NCI) Database | Database | Chemical compound repository | Source of potential inhibitors for virtual screening [26] |
| PubChem Database | Database | Chemical structure and bioactivity | Provides structural information for compounds [28] |
QSAR modeling has evolved from a supplementary tool to a central methodology in early pharmacokinetic parameter estimation, enabling researchers to make informed decisions during the critical early stages of drug discovery. The integration of advanced machine learning techniques, novel molecular representations such as compound images, and hybrid modeling approaches like QSAR-PBPK frameworks has significantly enhanced the predictive accuracy and applicability of these computational methods. As the field continues to advance, driven by growing datasets, improved algorithms, and increased computational power, QSAR approaches are poised to become even more indispensable in the development of efficient, predictive, and translatable drug discovery pipelines. The ongoing challenge remains in the continual validation and refinement of these models to ensure their reliability and regulatory acceptance across diverse chemical domains and biological systems.
In the landscape of modern drug discovery, the ability to accurately predict a compound's pharmacokinetic (PK) profile—its journey through absorption, distribution, metabolism, and excretion (ADME) within a living organism—is paramount for both efficacy and safety. In silico modeling has emerged as a cornerstone technology, enabling researchers to simulate biological systems computationally, thereby reducing reliance on extensive animal experimentation and accelerating development timelines [29]. These models span a spectrum from descriptive, top-down approaches to mechanistic, bottom-up representations of physiology. Among these, compartmental modeling serves as a fundamental framework, representing the body as a set of interconnected, homogeneous chambers between which drugs transit [30]. However, a significant challenge persists in bridging the output of these models with true physiological relevance, ensuring that predictions accurately reflect the complex, spatially heterogeneous, and dynamically regulated environment of a biological system. This guide details the principles of compartmental modeling and explores advanced computational strategies that enhance the biological fidelity of in silico PK predictions, framing them within the broader thesis of establishing robust, predictive pharmacokinetics in early-stage research.
Foundations of Compartmental Modeling
Compartmental models are composed of sets of interconnected mixing chambers or "stirred tanks," where each compartment is considered homogeneous and instantly mixed, with a uniform concentration of the substance being modeled [30]. The state variables are typically concentrations or molar amounts of chemical species, and the processes that move these species between compartments—such as chemical reactions, transmembrane transport, and binding—are generally treated using first-order rate equations.
Core Principles and Mathematical Formalism
The fundamental simplicity of representing systems via ordinary differential equations (ODEs) makes compartmental models computationally tractable. A generic mass balance for a drug in a compartment yields the equation:
dA_i/dt = Input - Output + Σ_j k_ji A_j - Σ_j k_ij A_i - k_el_i A_i
Where:
A_iis the amount of drug in compartmenti.k_ijandk_jiare the first-order rate constants for transfer between compartmentsiandj.k_el_iis the elimination rate constant from compartmenti.
While these models have a reputation for being descriptive "black boxes," they can be refined to incorporate realistic mechanistic features through more sophisticated kinetics [30]. In pharmacokinetics, compartments represent homogeneous pools of particular solutes, with inputs and outputs defined as flows or solute fluxes. The primary output is the concentration-time curve, which describes how long a drug remains available in the body and guides dosage regimen design [30].
Table 1: Common Compartmental Model Structures in Pharmacokinetics
| Model Structure | Description | Typical Use Case |
|---|---|---|
| One-Compartment | Body is represented as a single, uniformly mixed pool. | Initial, simplistic estimation of PK parameters. |
| Two-Compartment | Body is divided into a central compartment (e.g., plasma) and one peripheral compartment (e.g., tissues). | Characterizing drugs with a distinct distribution phase. |
| Multi-Compartment | Extension to multiple peripheral compartments with different distribution characteristics. | Modeling complex distribution patterns, e.g., into fat, bone, or specific organs. |
| Mammillary Model | A central compartment connected to multiple peripheral compartments, but no connections between peripherals. | Most common structure for PK analysis. |
| Catenary Model | Compartments connected in a linear chain. | Representing sequential processes, like absorption. |
Enhancing Physiological Relevance with Advanced Modeling
While traditional compartmental models are powerful, their assumption of homogeneity limits their physiological accuracy. To bridge this gap, several advanced modeling frameworks have been developed.
From Compartmental to Physiologically-Based Pharmacokinetic (PBPK) Modeling
Physiologically Based Pharmacokinetic (PBPK) modeling represents a significant leap towards physiological relevance. Instead of abstract compartments, PBPK models explicitly represent individual organs and tissues, interconnected by the circulatory system. Each organ has a physiologically realistic volume, blood flow rate, and can be characterized by tissue-to-plasma partition coefficients [31]. This allows for a mechanistic representation of ADME processes. The application of PBPK modeling in biopharmaceutics (PBBM) is increasingly used to establish a link between in vitro drug product performance and in vivo outcomes, helping to construct a bioequivalence safe space and set clinically relevant drug product specifications [31].
The Emergence of Machine Learning in PK Prediction
A novel paradigm is the direct prediction of PK profiles using machine learning (ML). One framework demonstrates that a rat's plasma concentration versus time profile can be predicted using molecular structure as the sole input [29]. This approach first predicts key ADME properties (like clearance and volume of distribution) from the compound's structure and then uses these as inputs to a second ML model that predicts the full PK profile, mitigating the need for animal experimentation in early stages [29]. For tested compounds, this method achieved an average mean absolute percentage error of less than 150%, providing a valuable tool for virtual PK analysis [29].
Hybrid and Multi-Scale Modeling
The future lies in multi-scale models that integrate different modeling philosophies. A PBPK model can serve as a scaffold for physiological realism, while ML algorithms can be used to predict difficult-to-measure input parameters directly from chemical structure [29] [32]. Furthermore, agent-based models (ABMs) can simulate localized tissue environments, representing individual cells or groups of cells and their interactions. For instance, an ABM of neural tube closure functionalizes cell signals and biomechanics to render a dynamic representation of the developmental process, predicting the nature and probability of defects from perturbations [33]. Integrating such fine-grained, dynamic models into a PBPK framework represents the cutting edge of physiological relevance.
Experimental Protocols and Methodologies
Protocol: Developing a Machine Learning Framework for PK Profile Prediction
This protocol is adapted from a study that predicted rat PK profiles from molecular structure [29].
Data Curation:
- Collect a dataset of molecular structures (represented as SMILES strings) with corresponding in vivo PK parameters (Clearance - CL, Volume of distribution - Vdss) and full concentration-time (PK profile) data.
- Preprocess SMILES strings: Strip salts, convert to canonical forms, and standardize.
- Represent molecules as numerical features using RDKit, generating either molecular fingerprints (e.g., 2048-bit Morgan fingerprint) or 200+ molecular descriptors (e.g., QED, TPSA, hydrogen bond donors/acceptors).
Feature and Model Selection:
- Perform exhaustive feature selection to identify the optimal input parameters (e.g., CL and Vdss alone, or combined with descriptors/fingerprints).
- Split the dataset into a training set (e.g., 85% of compounds) and a held-out test set (e.g., 15%).
- Train multiple ML algorithms (e.g., Random Forest, XGBoost, Support Vector Regressor) to predict the PK profile, using predicted CL, predicted Vdss, and time points as inputs. Use k-fold cross-validation on the training set for model selection and hyperparameter tuning.
Model Validation and Performance Assessment:
- Validate the final model on the test set.
- Assess performance using metrics such as Root Mean Square Error (RMSE), Mean Absolute Percentage Error (MAPE), and the coefficient of determination (R²).
- Compare predicted and observed values for key PK metrics like C~max~ (peak concentration) and AUC~24h~ (Area Under the Curve up to 24 hours).
Figure 1: ML-based PK Prediction Workflow. A two-stage ML framework for predicting pharmacokinetic profiles directly from molecular structure.
Protocol: Building and Validating a PBBM for Clinically Relevant Specifications
This protocol outlines the steps for developing a Physiologically Based Biopharmaceutics Model (PBBM) for drug product development [31].
System Characterization:
- Drug Substance: Gather key physicochemical properties (solubility, pKa, logP, permeability, diffusivity).
- Physiology: Define the relevant human physiology (gastrointestinal fluid volumes, pH, bile salt levels, motility, transit times).
- Drug Product: Characterize the formulation, including dissolution profile under physiologically relevant conditions.
Model Construction:
- Select a robust PBPK platform (e.g., GastroPlus, Simcyp, PK-Sim).
- Populate the model with the collected drug, physiological, and formulation data.
- Integrate a dissolution model to link the formulation's performance to the in vivo environment.
Model Verification and Application:
- Verify the model by comparing its predictions against observed human PK data (e.g., from a clinical study).
- Use the verified model to construct a bioequivalence safe space, which defines the boundaries of dissolution profiles that will not lead to clinically significant differences in exposure.
- Apply the model to set clinically relevant dissolution specifications and to support regulatory submissions for biowaivers or formulation changes.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Computational and Data Resources for In Silico PK Modeling
| Tool/Resource | Type | Function and Application |
|---|---|---|
| JSim | Software Platform | Open-source modeling system for solving ODEs and PDEs; used for general-purpose computational physiology, including compartmental modeling [30]. |
| Berkeley Madonna | Software Platform | A general-purpose ODE solver used for modeling physiological systems and dynamical systems [30]. |
| Simcyp Simulator | PBPK Software | A leading platform for PBPK modeling and simulation, widely used in the pharmaceutical industry for predicting human PK and drug-drug interactions. |
| RDKit | Cheminformatics Library | Open-source toolkit for cheminformatics; used to convert SMILES strings into molecular descriptors and fingerprints for ML-based ADME prediction [29]. |
| Database of Essential Genes (DEG) | Database | A resource used in comparative genomics to identify genes essential for pathogen survival, aiding in therapeutic target discovery [34]. |
| UniProt | Database | A comprehensive resource for protein sequence and functional information, used for retrieving and comparing protein sequences [34]. |
| Leadscope Model Applier | QSAR Software | Provides predictive QSAR modeling for toxicology outcomes, supporting early risk assessments in drug discovery [35]. |
Visualization of Complex Biological Systems
To accurately model a biological process, one must first conceptualize its key components and their interactions. The following diagram outlines the core network involved in a specific morphogenetic process, neural tube closure, demonstrating how models can be built from known biology.
Figure 2: Agent-Based Model of Neural Tube Closure. A dynamic systems model showing how perturbations in signals and biomechanics can lead to defects [33].
The journey from simple, descriptive compartmental models to sophisticated, physiologically relevant simulations represents a paradigm shift in pharmacokinetic prediction. The integration of PBPK modeling provides a mechanistic framework that closely mirrors human physiology, while the advent of machine learning offers a powerful, data-driven approach to bypass early experimental bottlenecks. The ultimate bridge between in silico predictions and biological systems is being built through multi-scale, hybrid models that leverage the strengths of each approach. As these computational techniques continue to evolve, underscored by rigorous validation and a deep understanding of biology, they will increasingly enable researchers to make actionable predictions earlier in the drug design process. This will not only expedite development and reduce costs but also pave the way for more effective and safer therapeutics, fulfilling the core promise of in silico research.
Pharmacokinetic (PK) modeling, the quantitative study of how drugs are absorbed, distributed, metabolized, and excreted (ADME) in the body, has long been a cornerstone of drug development. Traditional PK modeling approaches, particularly nonlinear mixed-effects (NLME) modeling using established tools like NONMEM, have provided the fundamental framework for understanding drug behavior across populations. However, the increasing complexity of modern therapeutic modalities—from highly potent molecules with narrow therapeutic indices to complex biologic and nanoparticle formulations—has exposed the limitations of traditional methods. These challenges include handling massive parameter spaces, accounting for high inter-patient variability, and modeling non-linear kinetics from sparse clinical data.
The integration of artificial intelligence (AI) and machine learning (ML) presents a paradigm shift, enhancing the efficiency, predictive accuracy, and scope of traditional PK modeling. AI/ML methodologies are not merely replacing established techniques but are creating powerful hybrid systems that combine mechanistic understanding with data-driven pattern recognition. This transformation is enabling more robust Model-Informed Drug Development (MIDD), accelerating the path from candidate selection to regulatory approval, and paving the way for truly personalized medicine. This technical guide explores the core principles, methodologies, and applications of AI in PK modeling, providing researchers and drug development professionals with a comprehensive overview of this rapidly evolving landscape.
Performance Comparison: AI/ML vs. Traditional PK Modeling
A comparative analysis of AI-based and traditional PK modeling approaches reveals distinct performance advantages and optimal use cases for each methodology. The table below summarizes key findings from recent studies evaluating these approaches on both simulated and real-world clinical datasets.
Table 1: Comparative Performance of Traditional vs. AI/ML PK Modeling Approaches
| Modeling Approach | Key Characteristics | Performance Metrics | Best-Suited Applications |
|---|---|---|---|
| Traditional NLME (e.g., NONMEM) | Gold standard; mechanistic; highly interpretable; sequential model building [36] | Established benchmark; can struggle with complex, high-dimensional parameter landscapes [37] | Standard small molecules; scenarios with strong prior mechanistic knowledge |
| Machine Learning (ML) Models | Data-driven; handles complex patterns; multiple algorithms tested (e.g., Random Forest) [36] [38] | Often outperforms NONMEM; RMSE and MAE improvements vary by model and data [36] | Early screening of large compound libraries; analysis of high-dimensional data |
| Deep Learning (DL) Models | Complex neural networks; automatic feature extraction [36] | Strong performance, particularly with large datasets [36] | Modeling complex biologics (mAbs, nanoparticles); integrating diverse data types (e.g., imaging, -omics) |
| Neural ODEs | Combines neural networks with differential equations; balances flexibility and explainability [36] [39] | Provides strong performance and explainability, especially with large datasets [36] | Systems with complex, non-linear dynamics where some mechanistic understanding exists |
| Hybrid Mechanistic-AI | Integrates PBPK/PopPK with AI components; adds AI pattern recognition to known biology [40] | Enhances predictive power while maintaining scientific plausibility and regulatory trust [40] | Optimizing drug formulations; predicting API behavior with complex safety profiles |
Core AI/ML Methodologies and Experimental Protocols in PK Modeling
Automated Population PK Model Development
The labor-intensive, sequential process of traditional population PK (PopPK) model development is a prime target for automation. A 2025 study demonstrated an automated "out-of-the-box" approach for PopPK model development using the pyDarwin library [38].
- Objective: To automatically identify optimal PopPK model structures for drugs with extravascular administration, minimizing manual effort and timeline while ensuring model quality and biological plausibility [38].
- Experimental Workflow:
- Define Model Search Space: A generic search space of >12,000 unique PopPK model structures was constructed, covering various compartmental models, absorption mechanisms (first-order, zero-order, transit compartments), and elimination patterns [38].
- Implement Penalty Function: A dual-term penalty function was designed to automate model selection:
- Akaike Information Criterion (AIC) Term: Penalizes model overparameterization to ensure parsimony.
- Biological Plausibility Term: Penalizes abnormal parameter values (e.g., high relative standard errors, unrealistic inter-subject variability, high shrinkage) that expert modelers would reject [38].
- Execute Optimization: A combination of Bayesian optimization with a random forest surrogate and an exhaustive local search was used to efficiently navigate the vast model space, evaluating fewer than 2.6% of potential models on average [38].
- Key Findings: The automated approach reliably identified model structures comparable to or better than expert-developed models across four clinical and one synthetic dataset. For the synthetic ribociclib dataset, it recovered the exact true data-generation model. The average runtime was under 48 hours, significantly accelerating the model development cycle [38].
The following diagram illustrates the automated PopPK model development workflow.
Enhancing Physiologically-Based Pharmacokinetics (PBPK) with AI
PBPK modeling offers a mechanistic framework for predicting drug disposition but is often constrained by a large number of uncertain parameters. AI/ML techniques are being applied to address these limitations [41] [42].
- AI for Parameter Estimation and Uncertainty Quantification: ML algorithms, particularly Gaussian Process Emulators, can be trained on a limited set of PBPK simulations to create a rapid surrogate model. This surrogate can be used for global sensitivity analysis (e.g., using Latin Hypercube Sampling) to identify the most influential parameters, thereby reducing the effective dimensionality of the problem and focusing experimental resources [42].
- Addressing Data Gaps with QSAR and Deep Learning: For parameters difficult to measure experimentally, Quantitative Structure-Activity Relationship (QSAR) models powered by deep learning can predict ADME properties directly from a compound's chemical structure, informing and refining PBPK models earlier in the development process [41] [40].
Neural Ordinary Differential Equations (Neural ODEs)
A particularly innovative architecture bridging mechanistic and AI-driven modeling is the Neural ODE. This model uses a neural network to parameterize the derivative of the system's state, which is then integrated using an ODE solver [36] [39]. This approach inherently respects the temporal continuity of PK processes and can learn dynamics from irregularly sampled data, offering a powerful tool for modeling complex, non-linear PK profiles where traditional compartmental models may be insufficient [36].
The Scientist's Toolkit: Essential Reagents for AI-Enhanced PK Research
Implementing AI-driven PK modeling requires a suite of computational tools and platforms. The table below details key software and libraries that form the modern PK scientist's toolkit.
Table 2: Essential Research Reagent Solutions for AI-Enhanced PK Modeling
| Tool Name | Type | Primary Function in AI/PK Workflow |
|---|---|---|
| NONMEM | Software | Industry-standard for NLME modeling; often used as the engine for model fitting in automated workflows [38]. |
| pyDarwin | Python Library | Specialized library for automated PopPK model development and selection using advanced optimization algorithms [38]. |
| MonolixSuite | Software Suite | Provides an integrated environment for PK/PD modeling, with increasing integration of ML-assisted features for model selection and diagnostics [40]. |
| Neural ODEs | Modeling Architecture | Available in deep learning frameworks (PyTorch, TensorFlow); used for creating flexible hybrid models that combine neural networks with ODE systems [36] [39]. |
| PBPK Platforms | Software (e.g., GastroPlus, Simcyp) | Mechanistic PBPK simulators that can be augmented with AI/ML for parameter estimation, sensitivity analysis, and uncertainty quantification [41] [42]. |
| SciBERT / BioBERT | NLP Model | Pre-trained language models for mining biomedical literature to extract drug-disease relationships and PK parameters [43]. |
Applications and Implementation in Drug Development
Key Application Areas
- Early-Stage Discovery and ADMET Prediction: AI/ML models can rapidly predict a full suite of ADME and toxicity properties directly from chemical structure, enabling virtual screening of vast compound libraries to de-risk candidates before significant investment [40]. For instance, ML models can predict the pharmacokinetic profile of small molecule drugs based solely on their molecular structure, providing high-throughput screening with minimal wet lab data [44].
- Optimizing Clinical Development: In clinical stages, ML-based models analyze sparse patient data to efficiently identify covariates (e.g., age, renal function, genetics) that contribute to variability in drug response. This leads to more robust population PK models and better-informed dosing strategies for special populations [40]. AI tools have also been developed to predict nonspecific treatment response in placebo-controlled trials, improving trial design and analysis [44].
- Model-Informed Precision Dosing (MIPD): AI facilitates a shift towards personalized medicine by enabling the development of models that predict individual drug exposure and response. Architectures like recurrent neural networks (RNNs) and Neural ODEs can handle irregular and sparse data from clinical settings, supporting the implementation of adaptive dosing regimens tailored to individual patient constraints [39].
Implementation Workflow
The diagram below outlines a synergistic workflow that integrates traditional and AI-driven approaches throughout the drug development lifecycle.
Challenges and Future Directions
Despite its promise, the integration of AI into PK modeling faces several hurdles. The "black box" nature of some complex ML models can lack the transparency required for regulatory acceptance and scientific confidence [39] [40]. There is a critical need for large, high-quality, and well-curated datasets to train reliable models, as limited or biased data can lead to poor generalizability [40]. Furthermore, establishing "good machine learning practice" and standardized validation frameworks is essential for building trust with regulators [40].
The future evolution of AI in PK modeling will likely focus on explainable AI (XAI) to demystify model predictions and hybrid systems that deeply integrate mechanistic science with AI's pattern recognition capabilities [40]. As these models become more robust, they will advance in silico clinical trial simulation, allowing researchers to forecast outcomes under different scenarios and optimize trial protocols before enrolling patients [40]. Ultimately, the field is moving towards leveraging AI to integrate vast, patient-specific datasets—from genomics to real-world data—to enable accurate predictions of an individual's unique response to a drug, paving the way for optimized personalized treatments [39] [40].
The transformation of traditional PK modeling by AI and machine learning is well underway, moving from theoretical potential to tangible applications across the drug development continuum. By automating labor-intensive processes, uncovering complex patterns in high-dimensional data, and creating hybrid models that are both predictive and interpretable, AI is augmenting the capabilities of pharmacometricians and clinical pharmacologists. This synergy between mechanistic understanding and data-driven insight is creating a more efficient, robust, and predictive framework for pharmacokinetics. For researchers and drug development professionals, embracing this evolving landscape is no longer optional but essential to accelerating the delivery of new and personalized therapies to patients.
Methodologies in Action: PBPK, QSP, and AI-Driven Workflows for PK/PD Prediction
Physiologically based pharmacokinetic (PBPK) modeling represents a advanced mathematical framework that revolutionizes how researchers predict the absorption, distribution, metabolism, and excretion (ADME) of synthetic or natural chemical substances in humans and other animal species [1]. Unlike classical pharmacokinetic (PK) models that conceptualize the body as a system of abstract mathematical compartments with parameters lacking direct physiological referents, PBPK modeling is structured upon a mechanism-driven paradigm [45] [46]. This approach represents the body as a network of physiological compartments corresponding to specific organs and tissues (e.g., liver, kidney, brain) interconnected by blood circulation, integrating system-specific physiological parameters with drug-specific properties [46]. This fundamental difference provides PBPK models with remarkable extrapolation capability, enabling researchers to not only describe observed pharmacokinetic data but also quantitatively predict systemic and tissue-specific drug exposure under untested physiological or pathological conditions [46].
The historical development of PBPK modeling dates back to 1937 when the first pharmacokinetic model described in the scientific literature was essentially a PBPK model [1]. However, the complexity of these early models led to a shift toward simpler compartmental approaches until the advent of computers and numerical integration algorithms in the early 1970s renewed interest in physiological models [1]. Over the past decade, PBPK modeling has gained significant traction in regulatory settings, with the number of publications involving PBPK modeling increasing dramatically [45]. Between 2020 and 2024, among 245 FDA-approved new drugs, 65 NDAs/BLAs (26.5%) submitted PBPK models as pivotal evidence, demonstrating their growing importance in drug development [46].
PBPK Model Structure and Mathematical Framework
Fundamental Architectural Components
PBPK models are constructed using a multi-compartment architecture where each compartment represents a specific organ or tissue with physiological relevance. A typical whole-body PBPK model includes key compartments such as adipose, bone, brain, gut, heart, kidney, liver, lung, muscle, skin, and spleen [45] [47]. These compartments are interconnected through the circulating blood system, with flow rates that parallel the actual physiological structure of the body [45]. Each compartment is characterized by organ-specific parameters including tissue volumes, blood flow rates, and tissue-to-blood partition coefficients (Kp values) that determine how drugs distribute between blood and tissues [47].
The mathematical foundation of PBPK modeling relies on mass balance differential equations that describe the rate of change of drug quantity in each compartment. For a generic compartment i, the differential equation for the quantity Qi of substance is represented as:
dQidt=Fi(Cart−QiPiVi)
where Fi is blood flow, Cart is incoming arterial blood concentration, Pi is the tissue over blood partition coefficient, and Vi is the volume of compartment i [1]. This equation illustrates how the rate of drug accumulation in a tissue is governed by blood flow delivering the drug and the equilibrium distribution between tissue and blood.
Tissue Distribution Models
The distribution of drugs into tissues can be rate-limited by either perfusion or permeability, leading to two primary modeling approaches [45] [1]:
Perfusion rate-limited kinetics: Applies when tissue membranes present no significant barrier to diffusion, typically for small lipophilic molecules where blood flow becomes the limiting factor. This model assumes that at steady state, the total drug concentration in the tissue is in equilibrium with the total drug concentration in the circulation as determined by the drug-specific Kp value [45].
Permeability rate-limited kinetics: Occurs for larger polar molecules where permeability across the cell membrane becomes the limiting process. In this case, tissues are divided into intracellular and extracellular spaces separated by a cell membrane that acts as a diffusional barrier [45].
Most generic PBPK models assume perfusion rate-limited kinetics, with the liver and kidney being the primary sites of clearance [45]. The following diagram illustrates the structure of a comprehensive PBPK model and the workflow for its development:
Building a PBPK Model: Parameters and Workflow
Data Requirements and Parameterization
Building a robust PBPK model requires the integration of three fundamental categories of parameters [47]:
Organism parameters: Species- and population-specific physiological properties including organ volumes, blood flow rates, tissue compositions, and plasma protein levels. These parameters are available from standardized databases and scientific literature for various species and special populations.
Drug parameters: Fundamental physicochemical properties of the drug compound itself, including molecular weight, lipophilicity (logP/logD), solubility, pKa values, and permeability. These parameters are independent of the organism.
Drug-biological interaction parameters: Properties describing the interaction between the drug and biological systems, including fraction unbound in plasma (fu), tissue-plasma partition coefficients (Kp), and parameters related to metabolic enzymes and transporters.
The PBPK modeling workflow encompasses five distinct phases [47]:
- Model architecture definition: Identifying relevant anatomical compartments based on the ADME processes and target tissues.
- System-specific data collection: Gathering physiological parameters for the target species or population.
- Compound-specific data integration: Incorporating drug-specific parameters from in vitro assays or computational predictions.
- Model calibration and validation: Refining the model using available in vivo PK data and validating with independent datasets.
- Model application: Utilizing the validated model for simulation and prediction under various conditions.
Parameter Estimation Methods
Key to PBPK model parameterization is the estimation of tissue-plasma partition coefficients (Kp values), for which several approaches exist [45] [28]:
- In vitro to in vivo extrapolation (IVIVE): Uses data from in vitro systems as surrogates for in vivo reactions relevant to ADME processes.
- Quantitative Structure-Activity Relationship (QSAR) predictions: Leverages computational models to predict parameters like logD, pKa, and fraction unbound from chemical structure.
- Experimental measurement: Direct determination through specialized in vitro assays or in vivo studies.
Recent advances have demonstrated that QSAR-predicted Kp values can significantly improve model accuracy compared to traditional interspecies extrapolation methods. In human fentanyl models, QSAR-predicted Kp reduced the error in volume of distribution (Vss) prediction from >3-fold to <1.5-fold [28].
Predicting Tissue Drug Concentrations
Methodological Approaches and Challenges
Predicting tissue drug concentrations represents one of the most valuable applications of PBPK modeling, particularly for drugs whose targets are located outside the vasculature. Unlike plasma concentrations, which are readily measurable, tissue concentrations are often clinically inaccessible, creating a critical need for predictive methods [48]. PBPK models address this challenge by leveraging their physiological structure to simulate drug distribution to various tissues and organs.
The accuracy of PBPK-predicted tissue concentrations varies significantly across different tissues and drug compounds. A comprehensive study evaluating PBPK-predicted concentrations of beta-lactam antibiotics in adipose, bone, and muscle tissues revealed that predicted total tissue concentrations were less accurate (AFE: 0.68, AAFE: 1.89) than concurrent plasma concentration predictions (AFE: 1.14, AAFE: 1.50) [48]. Similarly, predictions of unbound interstitial fluid (uISF) concentrations showed even greater discrepancies (AFE: 1.52, AAFE: 2.32), with a tendency toward overprediction [48].
Quantitative Assessment of Prediction Accuracy
Extensive research has been conducted to evaluate the performance of PBPK models in predicting tissue concentrations. The table below summarizes key findings from recent studies assessing the prediction accuracy for various tissues and drug classes:
Table 1: Accuracy of PBPK-Predicted Tissue Concentrations Across Studies
| Tissue Type | Drug Class | Performance Metrics | Key Findings | Reference |
|---|---|---|---|---|
| Plasma | Beta-lactam antibiotics | AFE: 1.14, AAFE: 1.50 | Fairly accurate predictions for plasma concentrations | [48] |
| Total tissue | Beta-lactam antibiotics | AFE: 0.68, AAFE: 1.89 | Slight underprediction trend, within threefold range | [48] |
| unbound ISF | Beta-lactam antibiotics | AFE: 1.52, AAFE: 2.32 | Overprediction tendency, some outside threefold range | [48] |
| Brain tissue | Fentanyl analogs | Brain/plasma ratio >1.2 for 8 analogs | Identified high CNS penetration risk compounds | [28] |
| Multiple organs | 34 fentanyl analogs | Parameters within 1.3-1.7 fold | QSAR-PBPK framework enabled rapid prediction | [28] |
The conceptual workflow below illustrates the process of predicting tissue concentrations and the associated challenges:
Model Validation and Performance Assessment
Establishing Model Credibility
Robust validation is essential for establishing PBPK model credibility, particularly when models are intended for regulatory submissions or clinical decision support. Regulatory agencies generally request that PBPK model performance be assessed against observed outcomes of representative in vivo PK studies [49]. The validation process typically involves multiple approaches, beginning with visual checks of predicted versus observed concentration-time profiles, followed by quantitative assessment of key pharmacokinetic parameters including area under the curve (AUC), maximum concentration (Cmax), and half-life (t1/2) [49].
A significant challenge in PBPK model validation is the establishment of standardized acceptance criteria. The most commonly applied criterion in scientific literature has been the "twofold" criterion, where models are accepted when predicting PK parameters within twofold of observed clinical data [49]. However, this approach has been criticized for its wide range and failure to account for the inherent randomness of experimental data, particularly in small datasets [49].
Advanced Statistical Approaches
Recent methodological advances have proposed more robust statistical approaches for PBPK model validation. One promising method involves constructing a confidence interval (CI) for the predicted-to-observed geometric mean ratio (GMR) of relevant PK parameters, with predefined acceptance boundaries [49]. This approach is analogous to bioequivalence testing procedures, where the entire CI must fall within predefined boundaries (typically [0.8, 1.25]) for model acceptance [49].
This method offers several advantages over traditional approaches:
- Incorporation of variance: Accounts for the inherent randomness in observed data
- Robustness: Reduces the likelihood of accepting models merely by chance
- Flexibility: Can be applied with either individual observations or aggregate data
- Regulatory alignment: Aligns with established bioequivalence standards
The validation approach must be tailored to the model's context of use (COU), with more stringent requirements for high-impact applications such as direct clinical dosing recommendations [49]. For models used in early drug discovery, less rigorous validation may be acceptable, while regulatory submissions and clinical decision support demand comprehensive validation.
Regulatory Applications and Current Trends
PBPK in Drug Development and Regulatory Review
PBPK modeling has become increasingly integrated into drug development and regulatory evaluation processes. Analysis of recent FDA submissions reveals that oncology drugs account for the highest proportion (42%) of PBPK applications, followed by rare diseases (12%), central nervous system disorders (11%), and autoimmune diseases (6%) [46]. The predominant application domain is the quantitative prediction of drug-drug interactions (DDIs), representing 81.9% of all instances, with enzyme-mediated interactions (primarily CYP3A4) accounting for the majority (53.4%) [46].
Beyond DDI assessment, PBPK modeling is extensively applied to special population dosing, including patients with organ impairment (7.0%) and pediatric populations (2.6%) [46]. In these challenging populations, PBPK models virtualize pharmacokinetic profiles by incorporating population-specific physiological parameters, providing crucial support for designing initial dosing regimens where large-scale clinical trials are ethically or practically challenging [46].
Emerging Applications and Future Directions
The application of PBPK modeling continues to expand into novel areas, including:
Gene therapies and mRNA therapeutics: PBPK modeling is emerging as a MIDD approach to support clinical trial design, dose selection, and predicting PK/PD for advanced therapy medicinal products [50].
Dietary phytochemicals: PBPK modeling is particularly well-suited for natural products characterized by intricate material composition and limited clinical data [47].
Animal-free risk assessment: The development of modeling uncertainty factors (MUF) enables the use of PBPK models in risk assessment without traditional animal data, with proposed MUFs of 10 for AUC and 6 for Cmax based on the 97.5th percentile of prediction accuracy [51].
Looking forward, the integration of PBPK modeling with artificial intelligence (AI) and multi-omics data is poised to unprecedentedly enhance predictive accuracy, providing critical insights for precision medicine and global regulatory strategies [46].
Table 2: Essential Research Reagents and Computational Tools for PBPK Modeling
| Tool Category | Specific Tools/Resources | Key Function | Application Context |
|---|---|---|---|
| PBPK Software Platforms | Simcyp Simulator (Certara) | Population-based PBPK/PD modeling | DDI prediction, pediatric and special population modeling [47] [46] |
| GastroPlus (Simulations Plus) | Physiology-based biopharmaceutics modeling | Oral absorption, formulation development [47] | |
| PK-Sim (Open Systems Pharmacology) | Whole-body PBPK modeling | Open-source platform for multi-species PBPK [47] | |
| Parameter Estimation Tools | ADMET Predictor | QSAR-based property prediction | Prediction of physicochemical and ADME properties [28] |
| IVIVE methodologies | In vitro to in vivo extrapolation | Translation of in vitro assay data to in vivo parameters [45] | |
| Experimental Systems | Primary hepatocytes, liver microsomes | Metabolic clearance assessment | Measurement of intrinsic clearance and enzyme kinetics [52] |
| Transfected cell systems | Transporter activity assessment | Evaluation of uptake and efflux transporter interactions [48] | |
| Tissue homogenates | Partition coefficient measurement | Experimental determination of Kp values [28] | |
| Validation Resources | Clinical PK databases | Model verification | Comparison of predictions with observed human data [49] |
| Bioequivalence statistical packages | Model performance assessment | Implementation of confidence interval approaches [49] |
PBPK modeling represents a powerful, mechanistic framework that has transformed the landscape of pharmacokinetic prediction in silico research. By integrating physiological parameters with drug-specific properties, PBPK models enable researchers to simulate and predict drug concentrations not only in plasma but also at specific tissue sites, providing invaluable insights for drug development, particularly for compounds with tissue-specific targets or complex distribution patterns. While challenges remain in accurately predicting tissue concentrations, ongoing advances in model structure, parameter estimation, and validation methodologies continue to enhance the reliability and applicability of these tools across an expanding range of scenarios, from conventional small molecules to novel therapeutic modalities like gene therapies and natural products.
Integrating Machine Learning for ADME Parameter Prediction from Molecular Structure
The accurate prediction of a drug's Absorption, Distribution, Metabolism, and Excretion (ADME) properties represents a critical challenge in pharmaceutical research and development. Suboptimal ADME characteristics remain a primary reason for late-stage drug candidate attrition, resulting in significant financial losses and delays in therapeutic development [53] [54]. Traditional methods for predicting pharmacokinetic parameters, including in vitro to in vivo extrapolation and physiologically based pharmacokinetic (PBPK) modeling, often require extensive experimental data and time-consuming parameter calibration [53]. Over the past decade, machine learning (ML) has emerged as a transformative approach for predicting ADME and physicochemical properties from molecular structure, offering the potential to accelerate drug discovery pipelines and reduce reliance on animal studies [53] [55] [56].
The foundational principles of pharmacokinetics have traditionally been described by the ADME acronym, which encompasses how a drug moves through and is processed by the body [57] [13]. Pharmacokinetics (PK) specifically studies how a drug moves throughout the body, while pharmacodynamics (PD) describes what the drug does to the body—the pharmacological response that occurs when the drug reaches its site of action [13]. The ABCD framework (Administration, Bioavailability, Clearance, Distribution) provides an alternative perspective that aligns more closely with clinical pharmacokinetics by focusing on the active drug moiety in the body through space and time [57]. Within this context, in silico prediction of ADME parameters enables researchers to prioritize lead compounds with desirable pharmacokinetic properties earlier in the discovery process, before synthesis and experimental testing [56] [54].
Fundamental ADME Principles and Prediction Challenges
Core ADME Processes and Their Clinical Significance
ADME describes the complex interplay of physiological processes that determine a drug's systemic exposure and duration of action:
Absorption: The process by which a drug enters the systemic circulation from its site of administration. For orally administered drugs, this involves passage through the gastrointestinal wall and potential first-pass metabolism in the liver, resulting in reduced bioavailability compared to intravenous administration (100% bioavailability) [13]. Key parameters include permeability and solubility, often predicted through computational models of Caco-2 permeability and aqueous solubility.
Distribution: The reversible transfer of a drug between systemic circulation and various tissues and organs. This process is quantified by the volume of distribution (Vd), which describes the extent to which a drug distributes into tissues versus remaining in plasma [13]. Distribution is influenced by factors such as plasma protein binding, tissue permeability, and blood flow.
Metabolism: The enzymatic conversion of a drug into metabolites, primarily occurring in the liver through Phase I (functionalization) and Phase II (conjugation) reactions [13]. Cytochrome P450 (CYP) enzymes are responsible for metabolizing a large percentage of commonly used drugs, and predictions of metabolic stability and drug-drug interactions are crucial for assessing candidate viability.
Excretion: The irreversible loss of chemically unchanged drug from the body, primarily through renal or biliary pathways [13]. Clearance (CL) quantifies the rate of drug removal from the systemic circulation and is a critical determinant of dosing regimen and half-life.
Data Challenges in ADME Prediction
The development of robust ML models for ADME prediction faces several significant challenges related to data quality and availability:
Limited data accessibility: Unlike binding affinity data derived from high-throughput in vitro experiments, ADME data are largely obtained from in vivo studies using animal models or clinical trials, making them costly and labor-intensive to generate [55]. This has historically kept ADME datasets proprietary to pharmaceutical companies, with only limited public data available.
Data heterogeneity: Significant distributional misalignments and inconsistent property annotations exist between different data sources, such as between gold-standard datasets and popular benchmarks like Therapeutic Data Commons (TDC) [55]. These discrepancies arise from differences in experimental conditions, protocols, and chemical space coverage, introducing noise that can degrade model performance.
Molecular complexity: Natural products and beyond Rule-of-Five (bRo5) compounds present additional challenges due to their structural complexity, increased molecular weight, and unique physicochemical properties that deviate from conventional drug-like chemical space [58] [54].
Recent research has demonstrated that naive integration of heterogeneous ADME datasets without addressing distributional inconsistencies often decreases predictive performance rather than improving it, highlighting the need for systematic data consistency assessment prior to modeling [55].
Machine Learning Approaches for ADME Prediction
Algorithm Selection and Model Architectures
Multiple ML approaches have been successfully applied to ADME prediction, each with distinct strengths and applications:
Long Short-Term Memory (LSTM) Networks: LSTM-based ML frameworks have demonstrated strong performance in predicting concentration-time (C-t) profiles following intravenous drug administration. These models use ADME and physicochemical (ADMEP) descriptors with dose information as inputs, achieving R² values of 0.75 across all C-t profiles, with 77.8% of Cmax, 55.6% of clearance, and 61.1% of volume of distribution predictions within a 2-fold error range [53].
Random Forest Regression: Ensemble methods like Random Forest have shown excellent performance for specific ADME endpoints, achieving r² = 0.8410 and RMSE = 0.1112 for LD₅₀ (lethal dose) prediction in toxicity studies [59]. The method's robustness to outliers and ability to handle high-dimensional data make it suitable for various ADME classification and regression tasks.
Comparative ML Approaches: Recent systematic comparisons of various approaches that integrate ML models with empiric or mechanistic PK models show that pure ML, compartmental modeling with ML, and PBPK with ML approaches yield PK profile predictions of comparable accuracy across large datasets of over 1000 small molecules [56].
The following workflow illustrates the typical machine learning pipeline for ADME prediction:
Input Representations and Feature Engineering
The performance of ML models for ADME prediction heavily depends on the molecular representation strategy:
Extended-Connectivity Fingerprints (ECFP): Circular topological fingerprints that capture molecular substructures and patterns, commonly used with tree-based models and neural networks [55].
Physicochemical Descriptors: Traditional molecular descriptors including LogP (lipophilicity), molecular weight, hydrogen bond donors/acceptors, polar surface area, and rotatable bonds [59] [58].
Quantum Chemical Descriptors: Electronic properties, orbital energies, and partial charges derived from quantum mechanical calculations, though these are computationally intensive and less frequently used in high-throughput screening [54].
Recent studies have demonstrated that integrating ADME and physicochemical descriptors (ADMEP) with dose information provides sufficient information for accurate prediction of human PK profiles, achieving performance comparable to traditional PK prediction models [53].
Experimental Protocols and Implementation
Protocol: LSTM-Based PK Profile Prediction
The following detailed methodology is adapted from recent research on LSTM-based prediction of human PK profiles [53]:
Data Collection and Preprocessing
- Compound Selection: Curate a dataset of 40 drugs for training and 18 for testing, with concentration-time data simulated from published PK models to ensure consistency.
- Descriptor Calculation: Generate ADME and physicochemical descriptors using computational platforms such as ADMETlab 3.0. Key descriptors include LogP, LogS, molecular weight, hydrogen bond donors/acceptors, and topological polar surface area.
- Data Standardization: Apply z-score normalization to continuous variables and one-hot encoding to categorical variables to ensure optimal model performance.
Model Training and Validation
- Architecture Configuration: Implement a stacked LSTM architecture with 128 hidden units, followed by two fully connected layers with 64 and 16 neurons respectively. Include dropout layers (rate=0.2) to prevent overfitting.
- Training Protocol: Train models using Adam optimizer with learning rate of 0.001 and batch size of 32. Use mean squared error (MSE) as the loss function for continuous parameters and binary cross-entropy for classification tasks.
- Validation Strategy: Employ 5-fold cross-validation with stratified sampling to ensure representative distribution of chemical classes in each fold. Hold out a completely independent test set for final evaluation.
Performance Metrics and Evaluation
- Quantitative Metrics: Calculate R² values across all C-t profiles, with additional evaluation of the percentage of predictions within 2-fold error for key parameters (Cmax, clearance, volume of distribution).
- Statistical Analysis: Perform correlation analysis between input dose level, ADMEP descriptors, and prediction accuracy to identify factors influencing model performance.
Protocol: Random Forest for Toxicity Prediction
This protocol outlines the methodology for predicting toxicity parameters using Random Forest regression [59]:
Data Preparation
- Dataset Curation: Collect 58 organic compounds with experimentally determined LD₅₀ values from reliable sources.
- Descriptor Calculation: Compute physicochemical properties including LogP, LogS, Caco-2 permeability, CYP450 interactions, and hERG inhibition using SwissADME and PreADMET platforms.
- Data Analysis: Perform Pearson correlation, Principal Component Analysis (PCA), hierarchical clustering, and cosine similarity network construction to identify key trends and relationships in the data.
Model Development
- Algorithm Implementation: Train Random Forest regression models using scikit-learn with 500 decision trees and maximum depth of 30. Use mean decrease impurity for feature importance calculation.
- Cross-Validation: Apply five-fold cross-validation to assess model robustness and prevent overfitting. Use different random splits to ensure generalizability.
- Hyperparameter Tuning: Optimize critical parameters including number of trees, maximum depth, and minimum samples per leaf using grid search with 3-fold cross-validation.
The following table summarizes key quantitative performance metrics reported in recent studies:
Table 1: Performance Metrics of Machine Learning Models for ADME Prediction
| Prediction Task | ML Algorithm | Performance Metrics | Dataset Size | Reference |
|---|---|---|---|---|
| Human PK Profiles (IV) | LSTM Network | R²=0.75 for C-t profiles; 77.8% of Cmax, 55.6% of CL, 61.1% of Vss within 2-fold error | 40 training, 18 test | [53] |
| LD₅₀ Prediction | Random Forest | r²=0.8410; RMSE=0.1112 | 58 compounds | [59] |
| LogP Prediction | GALAS Algorithm | 80% within 0.5 log units; 96% within 1 log unit | >1000 new compounds added to training set | [58] |
| Solubility (LogS7.4) | GALAS Algorithm | 68% within 0.5 log units; 91% within 1 log unit | >2000 new compounds added to training set | [58] |
Data Management and Quality Assessment
Data Consistency Assessment Framework
The reliability of ML models for ADME prediction depends heavily on data quality and consistency. Recent research has highlighted significant misalignments between public ADME datasets, necessitating systematic assessment before model development [55]. The AssayInspector package has been developed specifically to address these challenges by providing:
- Distribution Analysis: Statistical comparison of endpoint distributions using two-sample Kolmogorov-Smirnov tests for regression tasks and Chi-square tests for classification tasks.
- Chemical Space Visualization: UMAP projection to identify coverage gaps and applicability domain boundaries across integrated datasets.
- Outlier Detection: Identification of experimental outliers, batch effects, and conflicting annotations for shared compounds across different data sources.
Implementation of rigorous data consistency assessment has been shown to prevent performance degradation that often occurs with naive dataset integration, particularly for critical ADME parameters such as half-life and clearance [55].
Dataset Integration Strategies
Effective integration of heterogeneous ADME data requires careful consideration of several factors:
- Experimental Protocol Alignment: Identification of consistent experimental conditions (e.g., pH, temperature, assay type) that significantly impact measured values.
- Applicability Domain Assessment: Evaluation of chemical space coverage to identify regions where predictions may be unreliable due to sparse training data.
- Annotation Standardization: Harmonization of conflicting property annotations for compounds appearing in multiple datasets through expert curation or consensus approaches.
The AssayInspector tool generates comprehensive insight reports with alerts and recommendations to guide data cleaning and preprocessing, supporting assessment of dataset compatibility before finalizing training data [55].
Research Reagent Solutions
Table 2: Essential Computational Tools for ADME Prediction
| Tool/Platform | Type | Primary Function | Key Features |
|---|---|---|---|
| ADMETlab 3.0 | Web Platform | ADME/Tox Prediction | Calculates key ADME descriptors; integrates gold-standard datasets [53] [55] |
| SwissADME | Web Tool | ADME Property Calculation | Computes physicochemical descriptors, pharmacokinetics, drug-likeness [59] |
| PreADMET | Desktop Application | ADME Prediction | Predicts Caco-2 permeability, CYP450 interactions, hERG inhibition [59] |
| AssayInspector | Python Package | Data Consistency Assessment | Identifies dataset misalignments, outliers, batch effects [55] |
| RDKit | Cheminformatics Library | Molecular Featurization | Generates molecular descriptors and fingerprints for ML [55] |
| ADME Suite | Commercial Software | Property Prediction | GALAS algorithms for LogP, solubility with expanded training sets [58] |
Advanced Integration and Workflow Systems
The increasing complexity of ML-based ADME prediction has driven development of integrated workflow systems that streamline model development and deployment:
Playbook Workflow Builder (PWB): A web-based platform for dynamically constructing and executing bioinformatics workflows using semantically annotated API endpoints and data visualization tools [60]. PWB enables researchers to build reproducible ADME prediction pipelines without extensive programming expertise.
Knowledge Resolution Graph (KRG): A network organizing well-documented APIs into an integrative system of microservices, where nodes represent semantic types (genes, drugs, metabolites) and edges represent operations performed by various tools [60]. This framework supports complex data analyses that draw knowledge from multiple resources.
These integrated systems facilitate the combination of ML-based ADME predictions with complementary data types, such as genomics and transcriptomics, enabling more comprehensive candidate evaluation in the context of individual patient characteristics and disease states [60].
The following diagram illustrates the data consistency assessment process essential for reliable model development:
Machine learning has fundamentally transformed the paradigm of ADME parameter prediction from molecular structure, enabling more efficient prioritization of drug candidates with desirable pharmacokinetic properties prior to synthesis. The integration of LSTM networks, Random Forest, and other ML approaches with traditional PK modeling has demonstrated performance comparable to established methods while reducing experimental costs and animal use [53] [56]. However, challenges remain in data quality, standardization, and interpretability that must be addressed through continued methodological advancement.
Future developments in ML-based ADME prediction will likely focus on several key areas: (1) improved handling of complex molecular classes such as natural products and beyond Rule-of-Five compounds; (2) enhanced model interpretability through explainable AI techniques; (3) integration of multiscale data from genomics, proteomics, and metabolomics to enable personalized pharmacokinetic predictions; and (4) development of federated learning approaches that allow model training across distributed datasets while maintaining data privacy [55] [60]. As these technologies mature, they will increasingly support the development of safer and more effective therapeutics with optimized pharmacokinetic profiles.
The integration of artificial intelligence (AI) with physiologically based pharmacokinetic (PBPK) modeling represents a transformative advancement in silico drug discovery research. This AI-PBPK approach provides a mechanistic framework for predicting the complex in vivo journey of drug candidates—from absorption to distribution, metabolism, and excretion (ADME)—by incorporating substance-specific properties with mammalian physiology [4]. This case study examines the development and application of an AI-PBPK model to optimize the selection of aldosterone synthase inhibitors (ASIs), a promising class of therapeutics for conditions like resistant hypertension driven by aldosterone excess [61] [62].
The traditional drug discovery pipeline is often protracted and resource-intensive, particularly when experimental determination of pharmacokinetic/pharmacodynamic (PK/PD) properties is required for numerous candidate compounds [61]. Classical PBPK models, while well-established, require comprehensive molecule-specific parameters that are often unavailable during early discovery stages [61] [45]. The emergence of AI and machine learning (ML) techniques addresses this limitation by enabling the prediction of critical ADME parameters directly from a compound's structural formula, thereby accelerating the identification of promising drug candidates [42] [63]. This case study exemplifies how this integrated computational methodology is applied to overcome specific challenges in ASI development, particularly the critical issue of enzymatic selectivity.
Scientific and Therapeutic Background
Aldosterone Synthase Inhibition as a Therapeutic Target
Aldosterone, a mineralocorticoid hormone, plays a pivotal role in regulating fluid balance, blood pressure, and cardiac remodeling through its action on the renin-angiotensin-aldosterone system (RAAS) [62]. Despite the use of RAAS-blocking drugs like angiotensin-converting enzyme inhibitors and mineralocorticoid receptor antagonists (MRAs), many patients experience 'aldosterone escape'—a paradoxical chronic elevation of circulating aldosterone levels that leads to treatment failure and adverse outcomes [62].
ASIs offer a novel therapeutic strategy by targeting the source of aldosterone production. They selectively inhibit cytochrome P450 11B2 (CYP11B2), the enzyme catalyzing the final and rate-limiting step of aldosterone biosynthesis in the adrenal cortex [61] [62]. By reducing pathological aldosterone levels at their origin, ASIs potentially circumvent limitations of MRAs, including the risk of hyperkalaemia and the counterregulatory increase in aldosterone secretion [61] [62].
The Selectivity Challenge
A significant hurdle in ASI development lies in achieving selective inhibition of aldosterone synthase over its closely related enzyme, 11β-hydroxylase (CYP11B1). CYP11B1, expressed in the adrenal zona fasciculata, facilitates the synthesis of cortisol, a critical glucocorticoid hormone [61]. The two enzymes share 95% sequence homology and have identical enzymatic active sites, making selective inhibition exceptionally challenging [62]. Off-target inhibition of cortisol synthesis can lead to serious side effects, necessitating a careful screening for compounds with high potency against CYP11B2 and minimal activity against CYP11B1 [61]. The ratio of a drug's IC50 (half-maximal inhibitory concentration) toward 11β-hydroxylase to that toward AS defines its selectivity index (SI), a crucial parameter for candidate optimization [61].
Model Development: Principles and Architecture
Foundations of PBPK Modeling
PBPK modeling is a mechanistic approach that describes the pharmacokinetics of a substance by dividing the body into physiologically relevant compartments (e.g., organs and tissues), connected by the circulating blood system [45] [4]. A system of mass balance differential equations is established for each compartment, which is solved numerically to simulate drug concentration-time profiles in various tissues and plasma [4].
The model parameterization incorporates:
- System-Specific Parameters: Physiological information independent of the drug, including organ volumes, blood flow rates, and tissue composition (e.g., water, lipid, and protein content) [45] [4]. These can be defined for different populations or species.
- Drug-Specific Parameters: Physicochemical properties of the substance (e.g., molecular weight, lipophilicity, protein binding) and parameters related to active processes (e.g., enzyme kinetics, transporter affinities) [4]. These are used to predict passive processes like tissue permeation and partition coefficients.
PBPK models can simulate the complete ADME process:
- Absorption: For oral administration, this involves modeling dissolution, stability, and permeability across the intestinal wall [4].
- Distribution: The process of a drug moving from systemic circulation into tissues, which can be perfusion-rate-limited (for small lipophilic molecules) or permeability-rate-limited (for larger, polar molecules) [45].
- Metabolism: Biotransformation, primarily in the liver but also in extrahepatic tissues, modeled using enzyme kinetic parameters [4].
- Excretion: Removal of the drug and its metabolites, typically via renal or biliary routes [4].
Integration of Artificial Intelligence
The AI-PBPK model developed for ASIs integrates machine learning (ML) and deep learning (DL) with a classical PBPK framework on a web-based platform, the B2O Simulator [61] [64]. This integration addresses a key limitation of classical PBPK models: their dependence on extensive in vitro data for molecule-specific parameters, which are scarce in early drug discovery [61] [42].
The AI/ML component predicts critical ADME parameters and physicochemical properties required for the PBPK model directly from the compound's structural formula or SMILES code [61]. This capability allows for the high-throughput screening of virtual compounds, prioritizing the most promising candidates for synthesis and experimental testing, thereby reducing reliance on resource-intensive in vitro assays [42] [63].
The following diagram illustrates the conceptual workflow of an AI-PBPK model, showing how AI-predicted parameters feed into the mechanistic PBPK framework.
Experimental Methodology
The study employed a structured workflow comprising four key phases to ensure model robustness and predictive accuracy [61] [64]:
- Model Construction: An initial PBPK model structure was established, and the AI component was configured to predict necessary parameters for ASIs.
- Calibration: Baxdrostat, the ASI with the most extensive published clinical data, was selected as the model compound. The model's predictions for Baxdrostat's PK parameters were compared against clinical trial data, and key model parameters were adjusted to improve fit [61].
- Validation: The calibrated model was externally validated using publicly available clinical PK data from two other ASIs: Dexfadrostat and Lorundrostat. This step assessed the model's generalizability and predictive performance for compounds within the same class [61].
- Simulation: The validated model was finally applied to predict the PK profiles of all five compounds under investigation, including BI689648 and the control compound LCI699 (Osilodrostat), an 11β-hydroxylase inhibitor [61].
Diagram Title: AI-PBPK Modeling Workflow for ASIs
Data Acquisition and Compound Selection
A comprehensive literature search was conducted using PubMed, Google Scholar, and ClinicalTrials.gov with keywords such as "aldosterone synthase inhibitor," "CYP11B2," and specific compound names (e.g., "CIN-107," "MLS-101") [61] [64]. This identified five key compounds for analysis. The associated PK/PD data were extracted from published literature or official company websites. The structural formulae and SMILES codes for all compounds were sourced from PubChem [61].
Table 1: Aldosterone Synthase Inhibitors Selected for AI-PBPK Modeling
| Compound | Alias | Developing Company | Highest R&D Status | Primary Target |
|---|---|---|---|---|
| Baxdrostat | CIN-107, RO-6836191 | CinCor, AstraZeneca PLC | Phase 3 | Aldosterone Synthase (CYP11B2) |
| Dexfadrostat | DP-13, (R)-Fadrozole | Damian Pharma | Phase 2 | Aldosterone Synthase (CYP11B2) |
| Lorundrostat | MLS-101 | Mineralys Therapeutics | Phase 2 | Aldosterone Synthase (CYP11B2) |
| BI 689648 | Not Specified | Boehringer Ingelheim | Not Specified | Aldosterone Synthase (CYP11B2) |
| LCI699 | Osilodrostat | Novartis | Approved (Cushing's) | 11β-Hydroxylase (CYP11B1) |
Pharmacodynamic (PD) Model
The pharmacodynamic properties, specifically the inhibition of aldosterone synthase and 11β-hydroxylase, were predicted using an adaptation of Macdougall's nonlinear model, a standard for dose-response analysis [61]. The workflow involved:
- Calculating the free plasma drug concentration from the PK profiles predicted by the PBPK model.
- Inputting the free concentration into the PD model to predict the enzyme inhibition rate.
- Determining the half-maximal inhibitory concentration (IC50) for each compound against both CYP11B2 and CYP11B1.
- Calculating the Selectivity Index (SI) as follows: SI = IC50 (CYP11B1) / IC50 (CYP11B2). A higher SI indicates greater selectivity for the target aldosterone synthase over 11β-hydroxylase [61].
Key Findings and Model Outputs
The primary output of the AI-PBPK simulation is the prediction of pharmacokinetic parameters and plasma concentration-time profiles for the investigated ASIs. Subsequently, the PD model utilizes these PK outputs to estimate critical efficacy and selectivity metrics.
Table 2: Key Pharmacokinetic and Pharmacodynamic Parameters of Aldosterone Synthase Inhibitors
| Compound | Predicted Cmax (ng/mL) | Predicted AUC (ng·h/mL) | Predicted Half-Life (h) | CYP11B2 IC50 (nM) | CYP11B1 IC50 (nM) | Selectivity Index (SI) |
|---|---|---|---|---|---|---|
| Baxdrostat | Model-derived | Model-derived | Model-derived | Model-derived | Model-derived | Model-derived |
| Dexfadrostat | Model-derived | Model-derived | Model-derived | Model-derived | Model-derived | Model-derived |
| Lorundrostat | Model-derived | Model-derived | Model-derived | Model-derived | Model-derived | Model-derived |
| BI 689648 | Model-derived | Model-derived | Model-derived | Model-derived | Model-derived | Model-derived |
| LCI699 (Control) | Model-derived | Model-derived | Model-derived | High (CYP11B1 inhibitor) | Low | <1 |
Note: Specific numerical values for the predicted parameters are reported in the original research article [61]. The table structure above highlights the key metrics that were simulated and compared.
The study demonstrated that the PK/PD properties of an ASI could be inferred from its structural formula within a certain error range [61]. The model successfully differentiated the selectivity profiles of the various ASIs, providing a quantitative basis for selecting lead compounds with an optimal balance of high potency against CYP11B2 and minimal off-target activity on CYP11B1. While occasional discordance between predictions and experimental observations was noted, the overall agreement confirmed the model's applicability for early-stage screening and optimization [61].
The development and application of AI-PBPK models, as demonstrated in this case study, rely on a suite of computational and data resources.
Table 3: Essential Research Reagents and Computational Tools for AI-PBPK Modeling
| Tool/Resource | Type | Primary Function | Application in ASI Case Study |
|---|---|---|---|
| B2O Simulator | Software Platform | Integrated AI-PBPK modeling platform | Core environment for model development, calibration, and simulation [61]. |
| GastroPlus | PBPK Software | Predicts absorption, PK, and pharmacodynamics | Referenced as a platform requiring comprehensive input parameters [61]. |
| Simcyp Simulator | PBPK Software | Population-based PBPK modeling and simulation | Referenced as a platform for simulating drug behavior across populations [61]. |
| SwissADME | Web Tool | Predicts ADME parameters and physicochemical properties | Example of an AI-based tool for predicting key input parameters [61]. |
| ADMETlab 3.0 | Web Tool | Predicts ADMET properties from molecular structure | Used to generate in silico ADME parameters for the PBPK model [61]. |
| PubChem | Database | Repository of chemical molecules and their properties | Source of structural formulae and SMILES codes for the five ASI compounds [61]. |
| ClinicalTrials.gov | Database | Registry and results database of clinical studies | Source of published clinical trial data for model calibration and validation [61]. |
This case study illustrates the powerful synergy between mechanistic PBPK modeling and data-driven AI prediction in modern drug discovery. The developed AI-PBPK model provides a robust in silico framework for predicting the PK/PD properties and selectivity of aldosterone synthase inhibitors directly from their molecular structures. This approach significantly de-risks the early stages of drug development by enabling the virtual screening and optimization of candidate compounds, thereby reducing the need for costly and time-consuming experimental screens.
While further validation and refinement are needed to enhance the model's predictive accuracy and generalizability, the methodology demonstrates broad potential. It can be extended to other therapeutic classes to facilitate drug safety assessment, efficacy prediction, and ultimately, the personalization of therapies [61] [42]. The integration of AI into PBPK modeling represents a paradigm shift in pharmacokinetic prediction, moving the industry closer to a fully computational drug discovery model.
In silico pharmacokinetic (PK) prediction has become a cornerstone of modern drug development, enabling researchers to simulate the absorption, distribution, metabolism, and excretion (ADME) of compounds in virtual human populations. These computational approaches have evolved from predicting basic PK parameters in standard adult populations to addressing complex challenges involving special populations, intricate drug-drug interactions (DDIs), and the unique disposition characteristics of biological products. The expansion into these areas is critical for ensuring drug safety and efficacy across the diverse patient populations encountered in real-world clinical practice, particularly given the frequent under-representation of children, elderly, pregnant women, and medically complex patients in clinical trials [65]. This technical guide explores the advanced applications of in silico PK modeling, focusing on three expanding frontiers: special population simulations, DDI prediction, and the modeling of biologics, framed within the broader thesis of advancing basic principles of pharmacokinetic prediction in silico research.
Special Populations: Addressing Variability in Drug Disposition
Special populations present unique physiological characteristics that significantly alter drug pharmacokinetics compared to healthy adults. Physiologically based pharmacokinetic (PBPK) modeling and artificial intelligence (AI) approaches have emerged as powerful tools to address these challenges by creating virtual populations that reflect physiological and pathophysiological variability [65].
Table 1: Virtual Populations in PBPK Modeling for Special Populations
| Population Category | Key Physiological Considerations | Representative Applications | Modeling Software Capabilities |
|---|---|---|---|
| Pediatrics | Ontogeny of metabolizing enzymes, organ size, body composition, renal function | Midazolam (CYP3A4 substrate), paracetamol, theophylline from neonates to adolescents [65] | Simcyp PBPK Simulator, PK-Sim |
| Geriatrics | Reduced hepatic/renal function, altered body composition, polypharmacy | Morphine, furosemide, simvastatin in patients aged 65-100 years [65] | Simcyp PBPK Simulator |
| Pregnancy | Increased plasma volume, renal blood flow, altered CYP activity (e.g., induced CYP3A4, CYP2C9, CYP2A6) | Cefazolin, cefuroxime across pregnancy trimesters [65] | Simcyp PBPK Simulator |
| Hepatic Impairment | Reduced metabolic capacity, altered plasma binding, portal-systemic shunting | Bosentan, repaglinide, valsartan in mild, moderate, and severe impairment [65] | Simcyp PBPK Simulator, GI-Sim |
| Renal Impairment | Reduced glomerular filtration, tubular secretion, altered non-renal clearance | Adefovir, oseltamivir carboxylate, sitagliptin across renal function stages [65] | Simcyp PBPK Simulator |
| Obesity | Altered tissue volumes, blood flows, cardiac output, enzyme expression | Midazolam, clindamycin, dolutegravir in children and adults with obesity [65] | Simcyp PBPK Simulator |
Experimental Protocols for Special Population Modeling
Protocol 1: Developing a PBPK Model for a Pediatric Population
- Data Collection: Gather physiological parameters (organ weights, blood flows, tissue composition) specific to pediatric age bands (preterm neonates to adolescents) from literature sources and specialized databases [65].
- Enzyme/Transporter Ontogeny: Incorporate established mathematical functions describing the maturation of drug-metabolizing enzymes (e.g., CYPs, UGTs) and transporters across developmental stages [65].
- Model Verification: Verify the model using drugs with well-understood PK in pediatric populations (e.g., midazolam for CYP3A4 ontogeny) before applying it to new chemical entities [65].
- Simulation and Validation: Simulate drug exposure in virtual pediatric cohorts and compare predictions against available clinical data to validate the model's predictive performance [8].
Protocol 2: Generating a Virtual Geriatric Population
- Parameter Definition: Define age-dependent physiological changes, including reduced hepatic and renal function, decreased cardiac output, and altered body composition, using population-based data [65].
- Incorporating Comorbidities and Polypharmacy: Account for common disease states (e.g., renal impairment) and likelihood of concomitant medications that may cause DDIs [65].
- Sensitivity Analysis: Perform sensitivity analyses to identify the physiological parameters with the greatest impact on drug exposure in the elderly [65].
- Clinical Translation: Apply the model to simulate clinical trials in geriatric virtual populations to inform dosing recommendations for this demographic [65].
Figure 1: PBPK Workflow for Special Populations. This diagram illustrates the systematic approach to developing and verifying PBPK models for special populations, from base model establishment to clinical output generation.
Drug-Drug Interactions: Predicting Metabolic Complexities
DDIs remain a major cause of adverse drug reactions and product withdrawals. In silico approaches provide powerful methodologies for predicting metabolic DDIs, particularly those mediated by cytochrome P450 (CYP) enzymes, which are responsible for the metabolism of a majority of marketed drugs [66] [67].
Table 2: Key CYP450 Enzymes in Drug-Drug Interactions
| CYP Enzyme | Approximate Contribution to Drug Metabolism | Example Substrate Drugs | Example Inhibitors | Example Inducers |
|---|---|---|---|---|
| CYP3A4 | 30-40% of total CYP protein [67] | Alfentanil, budesonide, colchicine [68] | Clarithromycin, cobicistat [68] | Carbamazepine, enzalutamide [68] |
| CYP2D6 | ~20% of drugs [67] | Atomoxetine, desipramine, dextromethorphan [68] | Bupropion, cinacalcet [68] | - |
| CYP2C9 | ~15% of drugs [67] | Celecoxib, S-warfarin [68] | Fluconazole, fluvastatin [68] | Aprepitant, dabrafenib [68] |
| CYP2C19 | ~10% of drugs [67] | Diazepam, clopidogrel [68] | Fluconazole, fluoxetine [68] | Apalutamide, enzalutamide [68] |
| CYP1A2 | ~5% of drugs [67] | Alosetron, caffeine, clozapine [68] | Ciprofloxacin, fluvoxamine [68] | - |
| CYP2B6 | ~5% of drugs [67] | Bupropion, efavirenz [68] | - | Efavirenz [68] |
Experimental Protocols for DDI Prediction
Protocol 1: In Silico Prediction Using Structure-Activity Relationship (SAR) Models
- Training Set Creation: Compile a dataset of known DDIs from sources like DrugBank and the Fujitsu ADME Database, focusing on specific CYP isoforms (e.g., 2345 pairs for CYP1A2, 2B6, 2C19, 2C8, 2C9, 2D6, 3A4) [69].
- Descriptor Calculation: Calculate PoSMNA (Pairs of Substances Multilevel Neighborhoods of Atoms) descriptors based on the structural formulas of the compound pairs [69].
- Model Building: Apply the PASS (Prediction of Activity Spectra for Substances) software, which uses a naïve Bayes classifier, to create SAR models for DDI prediction [69].
- Prediction and Validation: Input structural formulas of new drug pairs to predict potential DDIs, presented as probabilities Pa ("to be active") and Pi ("to be inactive"). Validate model accuracy using leave-one-out cross-validation (reported average accuracy ~0.92) [69].
Protocol 2: Machine Learning-Based CYP Substrate Classification
- Data Curation: Collect and curate a comprehensive dataset of substrates and non-substrates for key CYP450 isoforms from multiple authenticated sources (e.g., DrugBank, SuperCYP, FDA tables), ensuring each compound has a verified PubChem CID and consistent classification across at least two independent sources [66].
- Model Development: Employ Graph Convolutional Networks (GCN) that directly convert molecular structures into graphical representations (atoms as nodes, bonds as edges) to build classification models [66].
- Model Optimization: Utilize advanced techniques such as Bayesian optimization and SMILES enumeration to enhance model robustness and performance [66].
- Performance Evaluation: Evaluate model performance on external testing sets using metrics such as the Matthews correlation coefficient (ranging from 0.51 for CYP2C19 to 0.72 for CYP1A2 in benchmark studies) [66].
Figure 2: Metabolic DDI Mechanism. This diagram illustrates the fundamental mechanism of metabolism-mediated drug-drug interactions, where a precipitant drug alters the enzyme activity, thereby affecting the metabolism of a victim drug.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for In Silico Pharmacokinetic Research
| Tool Category | Specific Tool/Resource | Function and Application |
|---|---|---|
| PBPK Modeling Platforms | Simcyp Simulator [8] | Industry-standard platform for PBPK modeling and simulation; includes built-in virtual populations for special populations and DDI prediction. |
| ADME Prediction Software | ADMET Predictor [8] | Predicts key ADME parameters (e.g., Log P, fu, B/P, Peff, CYP Km/Vmax) used to build and inform PBPK models. |
| CYP450 Interaction Databases | FDA Table of Substrates/Inhibitors [68] | Authoritative resource listing drugs and other substances that interact with CYP enzymes and transporter systems. |
| Curated CYP450 Interaction Dataset [66] | Comprehensively curated dataset of substrates and non-substrates for six major CYP450 isoforms; used for training machine learning models. | |
| Specialized Prediction Tools | PASS (Prediction of Activity Spectra for Substances) [69] | Predicts diverse biological activities, including DDIs for pairs of molecules, based on structural formulas using MNA descriptors. |
| Data Sources for Model Building | DrugBank [66] [69] | Comprehensive database containing drug, drug target, and drug interaction information used for training set creation. |
| PubChem [66] | Public repository of chemical compounds providing unique CIDs used for compound verification and standardization across datasets. |
Integration of Approaches and Future Perspectives
The true power of modern in silico PK prediction lies in the integration of complementary approaches. PBPK models parameterized with AI-predicted ADME properties and informed by comprehensive DDI databases represent a robust framework for addressing complex research questions [65] [70] [8]. For instance, a protocol for a new chemical entity might involve predicting its ADME properties using software like ADMET Predictor, incorporating these parameters into a PBPK platform like Simcyp, and then simulating its exposure in a virtual geriatric population with polypharmacy to assess DDI risks before first-in-human trials [8]. This integrated approach is particularly valuable for biologics, where large-molecule disposition characteristics can be simulated using PBPK models adapted for monoclonal antibodies and other protein therapeutics, though this remains a specialized and advancing field [71].
Future directions in this field include the increased incorporation of real-world data (RWD) to refine virtual population models, the development of more sophisticated quantitative systems pharmacology/toxicology (QSP/QST) models that integrate PK with complex physiological responses, and the application of generative AI for molecular design and trial optimization [65] [70]. Furthermore, international regulatory harmonization, evidenced by guidelines like ICH M12 on drug interaction studies, continues to shape the standards for model qualification and application, ensuring that in silico predictions become ever more reliable and impactful in the drug development pipeline [72].
The development of new therapeutic agents is a complex, costly, and time-intensive endeavor. In recent years, virtual populations (VPs) and in silico clinical trials (ISCTs) have emerged as transformative mathematical modeling techniques that are reshaping the drug development landscape [73]. These computational approaches integrate mathematical models to explore patient heterogeneity and its impact on therapeutic outcomes, serving as a bridge between standard-of-care approaches designed around the "average patient" and fully personalized therapy [73]. The fundamental premise involves creating computational representations of patient populations with assigned physiological, genetic, and demographic characteristics that reflect real-world variability. These virtual cohorts are then exposed to simulated drug interventions, allowing researchers to predict pharmacokinetic and pharmacodynamic responses across diverse demographic groups.
Regulatory agencies increasingly encourage the use of computer modeling and simulation (CM&S) approaches to optimize randomized clinical trials, reducing both time requirements and financial costs while improving the conclusiveness of outcomes [74]. The MID3 guidelines (Model-Informed Drug Discovery and Development) established by regulatory bodies in collaboration with the pharmaceutical industry provide a quantitative framework for predicting and extrapolating model conclusions, categorizing them based on their potential impact on clinical or commercial decision-making [74]. Virtual clinical trials represent a paradigm shift in pharmacometric analysis, enabling researchers to refine dose projections for new drugs, study inter-patient variability in treatment response, stratify patient populations to identify responders versus non-responders, and assess potential drug combinations or alternate treatment regimens before initiating costly human trials [73].
Methodological Framework for Virtual Clinical Trials
Core Components of Virtual Clinical Trials
The implementation of a virtual clinical trial requires the integration of several computational components, each serving a distinct purpose in the simulation pipeline. The structure follows a systematic process that begins with model design and culminates in data analysis, with multiple iterative steps in between [73].
Virtual Population Generation: Virtual patients are created with specific demographic, physiological, and pathophysiological characteristics based on real-world clinical data or published literature values. The VP generation process typically incorporates variability in key parameters such as age, sex, body weight, organ function, genetic polymorphisms, and disease status to reflect population heterogeneity [74] [75].
Pharmacokinetic (PK) Modeling: PK models describe what the body does to the drug, capturing the processes of absorption, distribution, metabolism, and excretion. These models are typically described using compartment-based approaches that track drug movement from initial administration compartments into various body regions before eventual clearance [73].
Pharmacodynamic (PD) Modeling: PD models characterize what the drug does to the body, predicting the physiological response to drug exposure. These models establish relationships between drug concentrations at target sites and the resulting therapeutic and adverse effects [73].
Trial Simulation Execution: The virtual population is exposed to simulated drug interventions according to predefined dosing regimens, and the resulting PK/PD profiles are generated for each virtual patient. This step involves numerically solving systems of equations that constitute the mathematical model [76].
Output Analysis: Simulated outcomes are analyzed using statistical methods and artificial intelligence approaches to identify patterns, relationships, and significant effects across the virtual population [74].
Workflow for Virtual Clinical Trial Implementation
The development and execution of an in silico clinical trial follows a structured, iterative workflow that ensures the reliability and relevance of the simulated outcomes. This process is inherently cyclical, with steps being revisited as needed to refine models and interpretations [73].
Figure 1: Iterative workflow for designing and implementing an in silico clinical trial
Virtual Population Generation Techniques
The generation of virtual populations represents a critical step in the ISCT workflow, as the composition of the virtual cohort directly influences the generalizability of simulation results. Multiple approaches exist for VP generation, each with distinct advantages and limitations.
Physiologically-Based Virtual Populations: These VPs are generated using physiological parameters such as body weight, age, organ size, blood flow rates, and enzyme expression levels. The parameters are typically drawn from population distributions reported in the literature or from real-world demographic databases [74] [77].
Covariate-Based Virtual Populations: This approach incorporates specific covariates known to influence drug pharmacokinetics or pharmacodynamics, such as renal function, hepatic impairment, genetic polymorphisms in drug-metabolizing enzymes, or disease severity markers [75] [77].
Model-Calibrated Virtual Populations: In this method, virtual patients are generated by sampling from parameter distributions of previously developed physiological or pharmacokinetic models. The population is then calibrated to match specific clinical datasets through weighting or filtering techniques [78] [76].
The demographic and physiological characteristics of a virtual population developed for amikacin dosing optimization in neonates exemplifies the detailed parameterization required for clinically meaningful simulations [77]:
Table 1: Virtual Population Characteristics for Neonatal Amikacin Dosing Optimization
| Characteristic | Value/Range | Data Source |
|---|---|---|
| Post-menstrual age | 30-35 weeks | Real-world demographic data (n=1563) |
| Post-natal age | 0-14 days | Real-world demographic data (n=1563) |
| Birth weight | Median: 2.3 kg | Real-world demographic data (n=1563) |
| Renal function | Matched to post-natal age | Population pharmacokinetic model |
Applications to Dosing Strategy Optimization
Oral Anticancer Drugs: Food Effect Evaluation
Clinical trial simulations have been successfully applied to evaluate the effect of food on exposure to oral anticancer agents, a critical consideration for dosing optimization. A simulation study investigating abiraterone and nilotinib demonstrated the power of virtual trials to quantify food effects and between-occasion variability [79].
The study design involved simulating virtual patients with fasting-state population PK parameters derived from published literature. A one-compartment model with first-order absorption and elimination was implemented, with between-individual variability incorporated for oral clearance (CL/F) and volume of distribution (Vd/F). Patients were randomly assigned food intake conditions for each simulated dose, with food effects implemented as reductions in CL/F and Vd/F based on clinical observations—92% and 85% reductions for abiraterone with high-fat meals, and an 18% reduction in apparent clearance for nilotinib with light meals [79].
The virtual trials demonstrated that the study design could detect food effects as a statistically significant covariate on oral clearance for both abiraterone and nilotinib, with percent bias and precision of the food covariate below 20%. The approach accurately captured individual level exposures with less than 5% and 20% bias and precision for individual clearance estimates, demonstrating the utility of virtual trials for identifying conditions affecting drug exposure [79].
Table 2: Food Effect Simulation Results for Oral Anticancer Agents
| Parameter | Abiraterone | Nilotinib |
|---|---|---|
| Food effect on CL/F | 92% reduction | 18% reduction |
| Food effect on Vd/F | 85% reduction | Not reported |
| Bias in individual CL/F | <5% | <20% |
| Precision in individual CL/F | <20% | <20% |
| Between-occasion variability | <30% bias and precision | <30% bias and precision |
Immuno-Oncology Agents: Extended Interval Dosing
Virtual clinical trials have enabled the re-optimization of dosing regimens for immuno-oncology agents, particularly monoclonal antibody therapies such as atezolizumab, an anti-PD-L1 antibody. Traditional dosing regimens for many immunotherapies maintain drug concentrations far exceeding therapeutically required levels, potentially increasing toxicity without enhancing efficacy [80] [75].
A virtual clinical trial was conducted to identify extended-interval dosing regimens for atezolizumab that could maintain therapeutic efficacy while reducing exposure burden. The simulation utilized a population PK model incorporating time-dependent clearance and covariates including albumin, tumor burden, sex, body weight, age, and anti-drug antibody status [75]. A virtual population of 1000 patients was generated with demographic characteristics reflecting typical oncology populations.
The simulation identified 840 mg every 6 weeks (q6w) as an optimal extended-interval regimen that maintained trough concentrations above the target threshold of 6 μg/mL in >99% of virtual patients. This regimen significantly reduced steady-state AUC compared to standard dosing, potentially flattening the exposure-response relationship for adverse events of special interest (AESI) while maintaining efficacy [75]. The approach demonstrates how virtual trials can optimize dosing strategies to improve therapeutic indices.
Pediatric and Neonatal Populations: Dose Standardization
Perhaps one of the most valuable applications of virtual clinical trials is in pediatric and neonatal therapeutics, where ethical and practical constraints limit clinical trial possibilities. A pharmacometric study using virtual populations addressed amikacin dosing standardization in neonates, a population with rapidly changing physiology that significantly impacts drug pharmacokinetics [77].
Researchers applied a two-compartment population pharmacokinetic model to real-world demographic data from 1563 neonates. The model incorporated amikacin clearance dependence on birth weight and post-natal age. Simulations revealed that in neonates with post-menstrual age of 30-35 weeks and post-natal age of 0-14 days, target trough concentrations (<5 mg/L) were achieved in only 59% of patients with the current 15 mg/kg every 24 hours regimen, compared to 79-99% in other neonatal subpopulations [77].
The virtual trial simulations demonstrated that extending the dosing interval to ≥36 hours in this vulnerable subpopulation increased the frequency of target trough attainment to >80%, providing a scientific rationale for dose optimization without subjecting neonates to potentially toxic drug exposures [77]. This application highlights the power of virtual populations to address dosing challenges in special populations where clinical trial data is scarce.
Pulmonary Arterial Hypertension: Combination Therapy Optimization
Virtual clinical trials have been applied to optimize dosing regimens for complex diseases requiring combination therapy, such as pulmonary arterial hypertension (PAH). A quantitative systems pharmacology (QSP) model of PAH pathophysiology and pharmacology was used to predict changes in pulmonary vascular resistance and six-minute walk distance in response to oral treprostinil [78].
The model incorporated multiple pathways involved in PAH, including endothelin-1, nitric oxide/cyclic GMP, and prostacyclin signaling. A virtual population was generated that spanned the range of clinical observations, with virtual patient-specific weights calibrated to match outcomes from previous clinical trials. The model was then used to simulate a virtual clinical trial of the FREEDOM-EV study, which evaluated treprostinil in combination with background therapies [78].
The virtual trial accurately predicted the time course of clinical response, with probabilities of clinical significance matching observed trial outcomes at multiple time points. The model further identified that patients with lower endogenous endothelin-1 production and higher initial numbers of smooth muscle cells—characteristics more prevalent in severe PAH—showed differential responses to therapy, enabling patient stratification for optimized treatment approaches [78].
Technical Implementation and Research Reagents
Essential Computational Tools and Platforms
The implementation of virtual clinical trials requires specialized software tools and computational platforms that enable model development, parameter estimation, and large-scale simulation. The following table summarizes key research "reagents" in the computational domain:
Table 3: Essential Computational Tools for Virtual Clinical Trials
| Tool Category | Specific Examples | Application in Virtual Trials |
|---|---|---|
| PK/PD Modeling Platforms | NONMEM, Monolix, Phoenix NLME | Population parameter estimation, virtual population generation |
| Physiological Simulation | GastroPlus, Simcyp, PK-Sim | Physiologically-based pharmacokinetic modeling |
| Systems Pharmacology | MATLAB, R, Python with specialized libraries | QSP model development and simulation |
| Clinical Trial Simulation | Trial Simulator, East, nQuery | Design and power analysis for virtual trials |
| Data Analysis & Visualization | R, Python, Spotfire | Analysis of virtual trial outputs |
Virtual Population Generation and Validation
The process of generating and validating virtual populations follows a structured methodology to ensure physiological and clinical relevance:
Figure 2: Virtual population generation and validation workflow
The validation step is particularly crucial, as it ensures that the virtual population accurately reflects the target clinical population. This typically involves comparing the distributions of key demographic, physiological, and disease characteristics between the virtual population and real-world clinical cohorts [73] [74]. For example, in a virtual trial comparing lisdexamfetamine and methylphenidate for ADHD, virtual populations were generated with close agreement to reference populations from clinical trials, with matching demographic and comorbidity parameters [74].
Machine Learning and Emulation Techniques
Recent advances in machine learning have enabled the development of emulation techniques that accelerate virtual population inference, particularly for computationally expensive quantitative systems pharmacology models. The process involves creating surrogate models that approximate the input-output relationships of complex mechanistic models, dramatically reducing computational time [76].
The emulation process typically follows these steps:
- Training Data Generation: The original QSP model is executed thousands of times across the biologically plausible parameter space to generate tumor growth inhibition profiles.
- Surrogate Model Training: Machine learning algorithms (random forests, neural networks, Gaussian processes) are trained to predict model outputs from parameter inputs.
- Model Validation: The surrogate model's predictions are compared against the original model to ensure accuracy.
- Virtual Population Inference: The surrogate model enables rapid screening of millions of virtual patients to identify parameter sets that match clinical observations [76].
This approach has been successfully applied to infer virtual populations for immuno-oncology QSP models, achieving significant acceleration (up to 1000-fold) in virtual population inference while maintaining congruence with clinical tumor size distributions [76].
Emerging Trends and Methodological Advances
The field of virtual clinical trials continues to evolve, with several emerging trends shaping its future trajectory. Machine learning integration is becoming increasingly sophisticated, moving beyond emulation to active learning approaches that optimize virtual population generation and trial design [76]. Multi-scale modeling approaches that integrate molecular, cellular, tissue, and organism-level processes are expanding the mechanistic depth of virtual trials, particularly in complex disease areas like oncology [78] [76]. The incorporation of real-world data from electronic health records, wearable devices, and genomic databases is enhancing the physiological relevance of virtual populations, enabling more precise extrapolation to clinical settings [77].
Regulatory acceptance of virtual trial methodologies continues to grow, with the FDA's Project Optimus initiative emphasizing model-informed dose optimization in oncology [73] [75]. This regulatory alignment, coupled with advancing computational capabilities, suggests that virtual populations and clinical trial simulations will play an increasingly central role in drug development strategies across demographic subgroups.
Virtual populations and clinical trial simulations represent a paradigm shift in pharmacometric analysis, providing powerful tools for optimizing dosing strategies across diverse demographic groups. These approaches enable researchers to explore drug exposure-response relationships in vulnerable populations that are often excluded from traditional clinical trials, including neonates, pediatric patients, and those with organ impairment or complex comorbidities. Through case studies in oncology, infectious disease, and pulmonary hypertension, virtual trials have demonstrated their capacity to identify optimized dosing regimens that balance efficacy and toxicity while accounting for intrinsic and extrinsic factors affecting drug pharmacokinetics.
As computational methods continue to advance and regulatory acceptance grows, virtual clinical trials are poised to become an integral component of drug development strategies, helping to bridge the gap between population-level prescribing and personalized medicine. The systematic implementation of these approaches, following established workflows for virtual population generation, model validation, and trial simulation, offers a robust methodology for informing dosing decisions across the demographic spectrum.
Overcoming In Silico Hurdles: Managing Complexity, Data Gaps, and Computational Efficiency
Addressing Parameter Uncertainty and Limited Data Availability in Complex Models
In silico pharmacokinetic (PK) prediction aims to characterize the fate of drugs within the body using mathematical models. A fundamental challenge in this endeavor is dealing with the dual constraints of parameter uncertainty—imperfect knowledge of model parameters—and limited data availability, which is especially prevalent in specific patient populations and during early drug discovery. Parameter uncertainty arises from the inherent randomness in data, model simplifications, and the complex, often unobservable, nature of physiological processes. Ignoring this uncertainty can lead to biased parameter estimates, overconfident predictions, and ultimately, suboptimal or even unsafe dosing regimens in model-informed precision dosing (MIPD) [81] [82]. This guide details the core principles and methodologies for quantifying and addressing these uncertainties to enhance the reliability of PK predictions.
Quantifying Parameter Uncertainty: Foundational Methods
The first step in managing uncertainty is its robust quantification. Several established statistical methods are employed in pharmacometric analyses to measure the precision of parameter estimates.
Likelihood-Based Confidence Intervals
After obtaining parameter estimates by maximizing the likelihood function, the uncertainty around these estimates can be visualized as confidence regions in parameter space. The linearization method approximates these regions as ellipsoids but can distort their true shape. The more computationally intensive nonlinear method does not rely on this linearity assumption and can produce more accurate, non-elliptical confidence regions, providing a better representation of parameter uncertainty, particularly with limited data [81].
Covariance Matrix and Relative Standard Errors
Population modeling software typically outputs a covariance matrix upon successful model estimation. The diagonals of this matrix represent the variance of each parameter estimate. The Relative Standard Error (RSE), calculated as the standard error divided by the parameter estimate, is a key metric of estimation precision. As a rule of thumb, RSEs below 20-30% are often considered acceptable, though this is context-dependent. High RSEs indicate poor identifiability of a parameter, often due to insufficient data or an over-parameterized model [82].
Information Criteria for Model Comparison
When comparing models with different complexities, the Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) are used to balance goodness-of-fit against the number of parameters. These criteria help guard against overfitting, which can inflate parameter certainty by modeling noise rather than the underlying process. A lower AIC or BIC suggests a better-balanced model. Differences in BIC greater than 10 provide "very strong" evidence in favor of the model with the lower BIC [83].
Table 1: Key Metrics for Quantifying Parameter Uncertainty
| Metric | Description | Interpretation |
|---|---|---|
| Relative Standard Error (RSE) | (Standard Error / Parameter Estimate) × 100% | Lower percentage indicates higher precision. Values <20-30% are often desirable. |
| Akaike Information Criterion (AIC) | -2×log(Likelihood) + 2×(number of parameters) | Used for comparing non-nested models. A lower value indicates a better trade-off between fit and complexity. |
| Bayesian Information Criterion (BIC) | -2×log(Likelihood) + log(N)×(number of parameters) | Similar to AIC but with a stronger penalty for parameters. Better for identifying the true model. |
| Likelihood Ratio Test (LRT) | Difference in -2×log(Likelihood) between nested models | A significant p-value (e.g., <0.05) indicates the more complex model provides a significantly better fit. |
Methodologies for Sparse and Limited Data
Data limitations are a reality in many PK studies, especially for rare diseases, pediatric populations, and neglected tropical diseases (NTDs). Specific modeling approaches are designed to handle these scenarios effectively.
Population Pharmacokinetic (PopPK) Modeling with Nonlinear Mixed-Effects
PopPK models are the standard approach for analyzing sparse, unbalanced data collected from a population of individuals. Unlike traditional methods that require dense sampling from each subject, PopPK uses nonlinear mixed-effects models to simultaneously estimate fixed effects (population typical parameters) and random effects (inter-individual variability, residual error). This allows for the pooling of information across all individuals, meaning that a few observations from many subjects can yield robust population parameter estimates [83].
Maximum Likelihood Principle and Model Discrimination
When multiple candidate models are plausible given the available data, the maximum likelihood principle is used for discrimination. The method calculates the probability of observing the data for a given model and its parameters. The model with the highest maximum likelihood is preferred. Likelihood ratios are used to compare models; a ratio of 100 denotes a strong preference for one model over another. If the existing data is insufficient for clear discrimination, the models can be used to design new experiments that maximize the difference in predicted outcomes, thereby efficiently generating the most informative new data [81].
Integration of Real-World Data (RWD) and Virtual Populations
For populations underrepresented in clinical trials (e.g., children, pregnant women, patients with organ impairment), virtual populations can be constructed. These are simulated cohorts that reflect the physiological and pathophysiological characteristics of the target group. When used as inputs into mechanistic models like Physiologically-Based Pharmacokinetic (PBPK) models, they enable the prediction of drug exposure and response in these specific populations, helping to bridge the data gap. The integration of Real-World Data (RWD) from electronic health records and patient registries further refines these models [65].
Table 2: Modeling Approaches for Data-Rich and Data-Limited Scenarios
| Approach | Best For | Key Advantage | Example Application |
|---|---|---|---|
| Non-Compartmental Analysis (NCA) | Rich, dense data from traditional trials. | Simplicity; model-independent. | Early-phase clinical trials with intensive sampling. |
| Population PK (PopPK) | Sparse, unbalanced data from diverse populations. | Leverages all available data; quantifies variability. | Dosing optimization in pediatric or critically ill patients. |
| Physiologically-Based PK (PBPK) | Extrapolation to untested populations/scenarios. | Mechanistic; incorporates physiology and system data. | Predicting drug-drug interactions or the impact of organ impairment. |
| AI-Integrated PBPK | Early drug discovery with minimal compound-specific data. | Uses molecular structure to predict ADME parameters. | Screening lead compounds for promising PK/PD properties [61]. |
A Practical Protocol for Incorporating Parameter Uncertainty in Simulations
To ensure model-based simulations reflect real-world uncertainty, it is critical to propagate parameter uncertainty into the predictions. The following protocol, utilizing R and the mrgsolve package, outlines how to achieve this using the covariance matrix from a PopPK model [82].
Objective: To simulate concentration-time profiles that account for the uncertainty in the model's parameter estimates, producing confidence intervals around the predictions.
Required Software & Reagents:
- Software: R programming environment, NONMEM (or other PopPK software),
mrgsolvepackage for R,dplyr,MASS. - Input Files: Final parameter estimates (e.g.,
.extfile from NONMEM), Covariance matrix (e.g.,.covfile from NONMEM), Model file (.cppfor mrgsolve).
Methodology:
- Extract Parameter Estimates and Covariance Matrix: Import the final parameter estimates (from the
.extfile where ITERATION == -1E9) and the covariance matrix (from the.covfile) into R. - Simulate New Parameter Sets: Use the
mvrnorm()function from theMASSpackage to generate a large number (e.g., 1000) of new parameter sets. This function samples from a multivariate normal distribution defined by the vector of parameter estimates (themuargument) and the covariance matrix (theSigmaargument). - Remove Non-Physiological Values: Check for and remove any simulated parameter sets that contain negative values, as these are not physiologically plausible for most PK parameters (e.g., volume, clearance).
- Perform PK Simulations with Each Parameter Set: For each of the
nsimparameter sets, run a simulation using your PK model (e.g., inmrgsolve) to predict concentration-time profiles. - Summarize the Results: Calculate summary statistics (e.g., median, 5th, and 95th percentiles) from the ensemble of all simulations at each time point. This generates the confidence interval around the typical population prediction.
Advanced and Emerging Approaches
The field is evolving to incorporate more sophisticated computational techniques to tackle uncertainty and data sparsity.
Bayesian Methods
Bayesian statistics offer a powerful framework for handling uncertainty by treating model parameters as probability distributions. Prior knowledge about parameters (the "prior") is updated with experimental data to form a "posterior" distribution. This is particularly useful for incorporating information from previous studies or physiological principles. The SIMUSOLV software package, for instance, uses Bayesian methods to represent confidence regions without the assumptions required by methods based on the F statistic [81].
Artificial Intelligence and Machine Learning
AI and ML are being integrated into PK modeling to address complex challenges. Machine learning can analyze large datasets to identify non-obvious patterns and covariate relationships that influence PK/PD. In early discovery, AI-PBPK models can predict a compound's absorption, distribution, metabolism, and excretion (ADME) parameters directly from its structural formula, providing critical early insights when no experimental data exists. ML tools are also being used to automate model evaluation tasks, such as assessing goodness-of-fit [84] [61].
Forecasting Accuracy for Model Evaluation
When evaluating models for clinical use in MIPD, it is essential to assess their forecasting accuracy—how well they predict future drug concentrations—rather than just how well they fit existing data. This involves an iterative process where a model is fitted to early therapeutic drug monitoring (TDM) samples and then used to predict subsequent TDM levels. This "fit-for-purpose" analysis provides the best estimate of a model's real-world performance and helps identify models that may be overfitting the historical data [85].
The Scientist's Toolkit: Essential Research Reagents and Software
Table 3: Key Tools for Addressing PK Modeling Uncertainty
| Tool / Reagent | Category | Function in Addressing Uncertainty |
|---|---|---|
| NONMEM | Software | Industry-standard for PopPK model development and parameter estimation; outputs covariance matrix for uncertainty analysis [83]. |
| R / mrgsolve | Software | Open-source environment for statistical computing and PK simulation; used to propagate parameter uncertainty and visualize confidence intervals [82]. |
| SIMUSOLV | Software | Provides sophisticated algorithms for parameter estimation, model discrimination, and confidence region calculation using both linear and nonlinear methods [81]. |
| PBPK Platforms (GastroPlus, Simcyp) | Software | Mechanistic modeling platforms that incorporate virtual populations to assess variability and uncertainty in untested scenarios [65] [61]. |
| SwissADME / PreADMET | Web Tool | Predicts key ADME and physicochemical properties in silico, providing initial parameter estimates when experimental data is limited [59]. |
| Covariance Matrix | Data Output | Quantifies the uncertainty and correlation of estimated parameters; essential for realistic simulation of parameter uncertainty [82]. |
| Virtual Patient Populations | Modeling Construct | Digitally generated cohorts representing specific demographics or disease states, used to explore variability and extrapolate when clinical data is scarce [65]. |
Effectively addressing parameter uncertainty and limited data is not merely a statistical exercise but a fundamental requirement for producing robust, reliable, and clinically useful pharmacokinetic predictions. By systematically quantifying uncertainty through RSEs and confidence regions, employing population modeling techniques for sparse data, rigorously evaluating models based on forecasting performance, and leveraging emerging AI methodologies, researchers can make informed decisions even in the face of uncertainty. Integrating these principles into the model-building workflow ensures that in silico predictions more accurately reflect real-world complexities, thereby de-risking drug development and optimizing therapeutic regimens.
Strategies for Managing Rapidly Compounding Model Complexity and Large Parameter Spaces
Framed within the context of advancing the basic principles of pharmacokinetic (PK) prediction in in silico research, this guide addresses the critical challenge of managing escalating model complexity. As computational models evolve from simple equations to intricate systems integrating physiological, drug-specific, and patient-level data, the associated parameter spaces expand rapidly. This compounding complexity threatens both the interpretability and computational tractability of models essential for drug development. Herein, we detail strategies to navigate this landscape, ensuring robust, predictive, and efficient modeling.
Foundational Principles in Pharmacokinetic Modeling
Pharmacokinetic prediction aims to forecast the time course of a drug's absorption, distribution, metabolism, and excretion (ADME) within the body. The fundamental principles of this field are increasingly embodied in complex computational frameworks.
Physiologically Based Pharmacokinetic (PBPK) Modeling is a cornerstone of modern in silico research. These models use systems of differential equations to represent the body as a network of tissue compartments, predicting drug concentration in plasma and tissues over time by integrating drug-specific physicochemical properties with human physiological parameters [65] [61]. They are particularly valuable for simulating the impact of intrinsic (e.g., age, genetics, organ impairment) and extrinsic (e.g., drug-drug interactions) factors on PK profiles, enabling extrapolation to understudied populations [65].
Quantitative Systems Pharmacology/Toxicology (QSP/QST) extends these principles by integrating systems biology with PK and pharmacodynamic (PD) models. This allows for the evaluation of drug effects within complex biological networks, moving beyond mere exposure to understand the full scope of drug action and potential adverse effects, such as drug-induced liver injury (DILI) [65] [86].
The emergence of Artificial Intelligence and Machine Learning (AI/ML) has introduced a paradigm shift. ML models can now predict ADME properties directly from chemical structures, while more advanced hybrid approaches, such as AI-PBPK models, leverage machine learning to generate key input parameters for classical PBPK models from molecular structures. This integration addresses the critical bottleneck of data scarcity in early drug discovery [61] [56].
Core Strategies for Managing Complexity and Parameter Spaces
Effectively managing the interplay between model complexity and large parameter spaces requires a multi-faceted approach. The strategies below are essential for maintaining model performance, interpretability, and computational feasibility.
Parameter Importance and Hierarchical Analysis
A critical first step is to recognize that not all parameters contribute equally to a model's output. Identifying the most influential parameters allows researchers to focus their optimization efforts and simplify models without significant loss of predictive power.
- Sloppy Parameter Analysis: This mathematical technique, applied to complex cognitive models, reveals that many parameters have minimal impact on model performance. The dynamics are often governed by a small subset of "stiff" parameters, while the majority are "sloppy," forming an exponential hierarchy of sensitivity. This analysis makes the behavior of complex models more tractable and prevents overfitting by highlighting which parameters require precise tuning [87].
- Importance Evaluation and Hierarchical Stratification: In industrial applications, a method involving correlation analysis between process parameters and quality indicators can be used to rank parameters by importance. Subsequently, parameters are divided into hierarchical groups (e.g., primary, secondary) based on this ranking. Optimization then proceeds progressively, starting with the most important parameters and using their optimized values as constants when optimizing the next tier. This multi-level progressive strategy significantly reduces computational resource consumption and iteration numbers compared to global optimization methods [88].
Efficient Optimization Algorithms for Large-Scale Experiments
For high-dimensional parameter spaces, manual tuning is impractical. Automated hyperparameter optimization (HPO) strategies are indispensable.
Table 1: Key Hyperparameter Optimization Algorithms
| Algorithm | Core Principle | Advantages in PK/PD Context | Example Tools |
|---|---|---|---|
| Bayesian Optimization [89] | Builds a probabilistic surrogate model of the objective function to guide the search for optimal parameters. | Highly effective when model evaluation is computationally expensive (e.g., a single PBPK simulation). | Neptune, Scikit-optimize (BayesSearchCV) |
| Hyperband [89] | A bandit-based approach that uses successive halving to aggressively early-stop poorly performing configurations. | Efficiently allocates computational budget by quickly discarding non-viable drug candidates or parameter sets. | Ray Tune |
| Population-Based Training (PBT) [89] | Trains multiple models in parallel, allowing them to "compete" and exploit each other's promising hyperparameters. | Adapts hyperparameters during training; useful for exploring diverse parameter combinations in QSP models. | DeepHyper |
| Improved Particle Swarm Optimization (PSO) [88] | A metaheuristic inspired by social behavior, where a population of particles moves through the parameter space toward the best solution. | Effective for complex, non-linear optimization problems common in process industries; can be enhanced for faster convergence. | Custom Implementations |
Integration of AI/ML with Mechanistic Models
A powerful strategy to manage complexity is to combine the predictive power of data-driven AI/ML with the physiological realism of mechanistic models.
- AI-PBPK Modeling: This hybrid approach uses machine learning to predict key ADME parameters and physicochemical properties directly from a compound's structural formula (e.g., its SMILES code). These predicted parameters then serve as inputs for a classical PBPK model, which simulates the full PK profile. This method is especially valuable at the drug discovery stage where experimental ADME data are limited, allowing for the in silico screening of numerous candidate compounds [61].
- Comparative ML Approaches: Studies systematically compare ML models that predict complete plasma concentration-time profiles. These can be purely empirical (non-mechanistic), integrated with compartmental models, or combined with PBPK models. Evidence suggests that these approaches can yield PK profile predictions of comparable accuracy, enabling the prioritization of drug candidates with desirable PK properties prior to chemical synthesis [56].
Parameter-Efficient Fine-Tuning (PEFT) for Large Models
With the increasing adoption of large-scale foundation models, including in scientific domains, PEFT has become a crucial strategy. PEFT involves adapting a pre-trained model to a specific task by adjusting only a small subset of its parameters, dramatically reducing the computational cost and risk of overfitting compared to full fine-tuning [90]. While more common in natural language processing, this principle is highly relevant for leveraging large, pre-trained AI models in pharmacoinformatics.
Experimental Protocols and Workflows
Implementing the above strategies requires structured experimental protocols. The following workflows provide a blueprint for effective model development and parameter optimization in PK/PD research.
Protocol for AI-PBPK Model Development and Application
This protocol outlines the steps for building and applying a hybrid AI-PBPK model for early drug candidate screening [61].
Model Construction:
- Step 1 - Input: Feed the compound's structural formula (e.g., SMILES code) into a machine learning module.
- Step 2 - AI Prediction: The ML module predicts key ADME parameters and physicochemical properties (e.g., Log P, permeability, CYP450 interactions).
- Step 3 - PBPK Simulation: Input the ML-predicted parameters into a PBPK model to simulate the drug's PK profile (plasma concentration over time).
Model Calibration and Validation:
- Calibration: Select a model compound with substantial available clinical data (e.g., Baxdrostat). Compare predictions with clinical data and adjust key parameters to improve accuracy.
- Validation: Perform external validation using clinical PK data from other, related compounds (e.g., Dexfadrostat, Lorundrostat) to assess the model's general predictive performance.
Pharmacodynamic (PD) Prediction:
- Calculate the free plasma drug concentration from the predicted PK profile.
- Construct a PD model (e.g., an Emax model) to predict the inhibitory effect on molecular targets based on the free drug concentration, enabling the estimation of efficacy and selectivity [61].
AI-PBPK-PD Workflow
Protocol for Multi-Level Progressive Parameter Optimization
This protocol is designed to manage high-dimensional parameter spaces by focusing computational resources strategically [88].
Parameter Importance Ranking:
- Perform a correlation analysis (e.g., using Pearson correlation or Random Forest feature importance) between all available process parameters and the key quality indicators (e.g., AUC, Cmax, clearance).
- Rank the parameters based on their calculated importance.
Parameter Hierarchical Division:
- Divide the sorted parameters into distinct hierarchical levels (e.g., Level 1: Top 20% most important; Level 2: Next 30%; Level 3: Remaining 50%).
Progressive Modeling and Optimization:
- Level 1 Optimization: Establish a nonlinear mapping (e.g., using a neural network) between the Level 1 parameters and the output. Use an improved optimization algorithm (e.g., Particle Swarm Optimization) to find the optimal combination of only these parameters.
- Level 2 Optimization: Fix the optimized Level 1 parameters as constants. Then, build a new model that includes the Level 2 parameters. Optimize this new set.
- Level N Optimization: Repeat this process, progressively incorporating less important parameters, using the optimized values from all previous levels as constants.
Multi-Level Optimization Process
Table 2: Key Computational Tools for PK/PD Modeling and Optimization
| Tool / Resource | Type | Function in Research |
|---|---|---|
| SwissADME [59] [61] | Web Tool | Predicts key ADME and physicochemical properties (e.g., Log P, Log S, CYP450 interactions) from a compound's structure. |
| PreADMET [59] | Web Tool | Provides in silico ADMET prediction modules, including BBB penetration and Caco-2 permeability. |
| Simcyp Simulator [61] | PBPK Platform | A industry-standard platform for PBPK modeling and simulation, capable of generating virtual populations. |
| GastroPlus [61] | PBPK Platform | A comprehensive simulation software for modeling drug absorption, pharmacokinetics, and pharmacodynamics. |
| Optuna [89] [91] | HPO Framework | An automated hyperparameter optimization software framework, particularly suited for machine learning and large-scale models. |
| Ray Tune [89] | HPO Library | A Python library for scalable experiment execution and hyperparameter tuning, supporting algorithms like Hyperband. |
| PyRx [59] | Molecular Docking Tool | Software for virtual screening and molecular docking, used to predict binding affinities to target proteins. |
| B2O Simulator [61] | AI-PBPK Platform | An example of a web-based platform integrating ML and PBPK models for PK/PD prediction from molecular structure. |
The complexity of models in in silico pharmacokinetics will continue to compound with the integration of multi-scale data and sophisticated AI. The strategies outlined—focusing on parameter importance analysis, employing efficient optimization algorithms like Bayesian Optimization and Hyperband, leveraging hybrid AI-PBPK frameworks, and adopting progressive optimization methodologies—provide a robust defense against the intractability of large parameter spaces. By systematically applying these strategies, researchers can enhance the predictive power, transparency, and efficiency of their computational models, thereby accelerating the journey from drug discovery to clinical application.
In silico pharmacology uses computational methods to study the behavior of pharmaceutical compounds within the body. For population pharmacokinetics (PopPK), which aims to understand drug absorption, distribution, metabolism, and excretion (ADME) across diverse patient populations, these methods are particularly transformative [92]. PopPK analysis is typically conducted using non-linear mixed-effects (NLME) models that characterize drug concentration-time profiles across individuals, accounting for both fixed effects (population averages) and random effects (inter-individual variability) [38].
Traditional PopPK model development relies on a manual, sequential approach where modelers start with simple structures and progressively add complexity [38] [37]. This process is not only time-consuming and labor-intensive but also prone to identifying local optima rather than globally optimal model structures [93]. The automation of this process through machine learning (ML) represents a paradigm shift, enabling more efficient, reproducible, and comprehensive model development while addressing the challenges of patient variability and complex drug behaviors [38] [37].
The Machine Learning Revolution in PopPK
Core Challenges in Traditional PopPK Modeling
Traditional PopPK model development is characterized by several significant limitations that machine learning approaches aim to address:
- Sequential Nature: Conventional methods use a greedy stepwise approach, building models sequentially by adding one feature at a time, which can miss critical interactions between model components [37].
- Limited Exploration: The vast parameter space, especially for extravascular drugs with complex absorption behavior, cannot be thoroughly explored manually due to time constraints between data availability and regulatory events [38] [93].
- Local Optima Trapping: Sequential searches often identify local rather than global minima, resulting in non-optimal structure selection [38] [93].
- Reproducibility Issues: The trade-off between model fit and biological plausibility is weighted by individual preference, leading to variation in model selection and reproducibility challenges [38].
Machine Learning Solutions
Machine learning addresses these challenges through several key capabilities:
- Non-Sequential Exploration: ML algorithms can simultaneously evaluate numerous model configurations, capturing critical interactions between features that might be missed when added sequentially [37].
- Global Optimization: Advanced search algorithms such as Bayesian optimization with random forest surrogates or genetic algorithms can explore the entire model space more comprehensively, avoiding local minima [38] [37].
- Automated Evaluation: ML tools automatically assess goodness of fit, model robustness, and parsimony by applying specific penalty functions that form fitness scores, reducing manual intervention [37].
Technical Framework for Automated PopPK
Systematic Workflow for Automated PopPK Development
The implementation of machine learning for automated PopPK follows a structured workflow that integrates computational methods with pharmacological expertise.
Model Search Space Design
A critical component of automated PopPK is the definition of a comprehensive model search space. Recent research has demonstrated that a single model space containing >12,000 unique PopPK model structures can effectively characterize diverse extravascular drugs without requiring customization for each dataset [38] [93]. This model space typically includes 17 distinct structural features encompassing:
- Various absorption mechanisms (first-order with lag-time, distributed delay functions)
- Distribution characteristics (1, 2, or 3-compartment models)
- Elimination patterns (linear and non-linear, capacity-limited)
- Statistical models for inter-individual variability
- Residual error models [38] [93]
Optimization Algorithms and Search Strategies
Multiple optimization approaches have been successfully applied to PopPK automation:
- Genetic Algorithms: Inspired by natural selection, these algorithms evolve model populations through selection, crossover, and mutation operations to identify optimal structures [37].
- Bayesian Optimization with Random Forest Surrogates: This approach builds probabilistic models of the objective function to direct the search toward promising regions of the model space [38] [93].
- Hybrid Global-Local Search: Combining global search algorithms with exhaustive local search provides robustness against local minima while refining promising candidates [38].
Comparative analysis has demonstrated that hybrid approaches evaluating fewer than 2.6% of models in the search space can identify optimal structures in less than 48 hours on average (using 40-CPU, 40 GB environment) [38].
Fitness Functions and Penalty Design
The fitness function is crucial for guiding the search toward biologically plausible models. Modern implementations use composite functions that balance multiple objectives:
- Goodness of Fit: Typically measured by the NONMEM objective function value (OFV) [93].
- Model Parsimony: An Akaike information criterion (AIC) penalty prevents overparameterization [38].
- Parameter Plausibility: Custom penalties discourage abnormal parameter values, such as high relative standard errors, implausible inter-subject variability, or excessive shrinkage [38] [93].
Ablation experiments have demonstrated that including the parameter plausibility penalty is essential for preventing the selection of models with abnormal parameter values across diverse datasets [93].
Performance Evaluation and Validation
Quantitative Performance Metrics
Automated PopPK approaches have been rigorously evaluated against traditional methods using both synthetic and clinical datasets.
Table 1: Performance Comparison of Automated vs. Manual PopPK Development
| Metric | Traditional Approach | ML-Automated Approach | Improvement |
|---|---|---|---|
| Development Time | Weeks to months | <48 hours on average | >80% reduction [38] |
| Model Space Coverage | Limited subset (<5%) | Comprehensive (<3% evaluated) | More exhaustive exploration [38] |
| Structural Feature Matching | Reference standard | 15/17 features on average | High concordance [93] |
| OFV Improvement | Baseline | ~5% reduction | Statistically significant [93] |
| Reproducibility | Analyst-dependent | High across repeated runs | More systematic [38] |
Case Study Validations
Several case studies demonstrate the effectiveness of automated PopPK approaches:
- Synthetic Ribociclib Dataset: The automated approach correctly identified the exact true data-generation model used to create the synthetic dataset [38].
- Clinical Datasets (Osimertinib, Olaparib, Tezepelumab, Camizestrant): Automatically discovered model structures were comparable to manually developed expert models, with some cases showing improved fit (5% OFV reduction) [38] [93].
- Vancomycin Clearance Prediction in Adults: A hybrid approach combining PopPK with XGBoost machine learning demonstrated improved prediction of vancomycin clearance compared to PopPK alone, with more than four-fifths of subjects showing improved predictions [94].
Implementation Toolkit for Automated PopPK
Essential Research Reagents and Computational Tools
Successful implementation of automated PopPK requires specific tools and methodologies that form the researcher's toolkit.
Table 2: Essential Research Reagents and Tools for Automated PopPK
| Tool Category | Specific Solution | Function/Application |
|---|---|---|
| Modeling Software | NONMEM [38] [93] | Gold-standard software for NLME modeling and parameter estimation |
| Automation Framework | pyDarwin [38] [93] | Machine learning-enhanced automated model selection toolbox |
| Search Algorithms | Bayesian Optimization with Random Forest Surrogate [38] | Global search strategy for navigating complex model spaces |
| Fitness Evaluation | Custom Penalty Function [38] [93] | Balances model fit with biological plausibility and parsimony |
| Data Processing | R or Python with specialized libraries [29] [94] | Data preparation, visualization, and post-processing |
| Validation Tools | Visual Predictive Checks, Bootstrap Methods [38] | Model validation and performance assessment |
Integration with Broader In Silico Pharmacology
Automated PopPK exists within a broader ecosystem of in silico approaches that enhance drug discovery and development:
- QSAR and Molecular Descriptors: Quantitative Structure-Activity Relationship models predict ADME properties using molecular descriptors and machine learning algorithms such as neural networks and support vector machines [92].
- Physiologically-Based Pharmacokinetic (PBPK) Modeling: ML can enhance PBPK models by optimizing parameter estimation and improving predictive accuracy [29] [95].
- Hybrid ML-PK Approaches: Combining traditional PK models with machine learning, such as using ML to predict individual clearance based on patient factors, enhances prediction accuracy [39] [94].
The integration of machine learning into PopPK represents a significant advancement in pharmacometrics. Current research demonstrates that a single, well-designed model space and penalty function can generalize across diverse drugs, suggesting that a minimal set of model spaces could characterize most compounds [38]. Future developments will likely focus on expanding these approaches to more complex scenarios, including drug-drug interactions, metabolite characterization, and combination therapies.
While automation accelerates model development, the role of the analyst remains crucial for defining appropriate model spaces, formulating hypotheses, and evaluating final models for biological plausibility [37]. The synergy between human expertise and machine learning capabilities creates a powerful paradigm for advancing pharmacokinetic research.
As these technologies mature, they promise to make PopPK analysis more accessible, reproducible, and efficient – ultimately accelerating drug development and improving patient care through more precise dosing strategies. The adoption of automatic model search can potentially free pharmacometricians from repetitive tasks, improve model quality, and speed up PopPK analysis across the entire drug development pipeline [38] [93].
Within the framework of basic principles of pharmacokinetic prediction, in silico research aims to translate biological understanding into quantitative mathematical models. Physiologically Based Pharmacokinetic (PBPK) modeling serves as a cornerstone of this approach, using mechanistic frameworks to simulate the absorption, distribution, metabolism, and excretion (ADME) of compounds in living organisms [96] [97]. A critical, yet often overlooked, aspect of PBPK model development is the computational implementation strategy. Researchers must choose between creating a stand-alone model, built specifically for a single compound or purpose, and utilizing a model template, a pre-defined superstructure designed to implement many different chemical-specific models [98]. This technical guide provides an in-depth analysis of these two implementation pathways, focusing on their impact on computational efficiency, development workflow, and overall utility in drug research and development.
The choice between template and stand-alone implementation is not merely a programming preference; it directly influences model performance, reviewability, and application scope. As PBPK models see increased use in regulatory submissions for drug-drug interactions and dose selection in special populations [99] [100], understanding these computational trade-offs becomes essential for scientists and drug development professionals.
Core Principles: Template and Stand-Alone PBPK Models
Defining Stand-Alone PBPK Implementations
A stand-alone PBPK model is a custom-built implementation, typically comprising a system of ordinary differential equations (ODEs) that is specifically tailored to a single compound or a narrow class of compounds. Its structure includes only the compartments and biochemical processes relevant to its immediate purpose, such as specific metabolic pathways or tissue distributions for a particular drug [98]. This focused nature often allows for highly optimized code, as it avoids the computational overhead of calculating unused variables or evaluating irrelevant logical conditions.
Defining PBPK Model Templates
A PBPK model template is a single model "superstructure" that incorporates equations and logic found in a wide array of PBPK models [98]. It is designed for flexibility, containing multiple tissue compartments and modeling options that exceed the needs of any single application. To implement a specific model, users "map" their desired structure onto the template by activating relevant features and setting unused parameters to zero, effectively switching off unneeded compartments and pathways. While this approach offers significant advantages in standardization and human efficiency, it inherently involves evaluating expressions for many quantities that are not used in the final simulation for a given chemical.
Quantitative Comparison: Computational Performance Analysis
Experimental Design for Timing Comparisons
To systematically evaluate the performance disparity between implementation strategies, rigorous timing experiments are essential. The following methodology, derived from a foundational study, provides a framework for such comparisons [98]:
- Model Selection: Employ well-established PBPK models for specific compounds, such as dichloromethane (DCM) and chloroform (CF), for which both template and stand-alone implementations have been previously verified. These models should represent a range of structural complexities.
- Implementation Preparation: Create a template-based implementation by mapping the chosen model onto the superstructure. Develop a separate, dedicated stand-alone implementation of the same model logic using the same underlying programming language or platform.
- Exposure Scenarios: Conduct simulations across multiple exposure scenarios (e.g., constant continuous oral, periodic oral, constant continuous inhalation, and periodic inhalation) to ensure results are not scenario-dependent.
- Timing Measurement: For each experiment, execute multiple simulation runs and measure the computational time required, ensuring consistent hardware and software environments to allow for direct comparison.
- Validation: Prior to timing comparisons, verify that both implementations produce nearly identical results (e.g., within a numerical tolerance of 10–6) to ensure functional equivalence [98].
Key Findings on Computational Speed
Experiments comparing PBPK model template implementations against stand-alone implementations have yielded consistent, quantifiable results. The table below summarizes the primary factors influencing computational time identified through these studies.
Table 1: Factors Influencing Computational Time in PBPK Simulations
| Factor | Impact on Computational Time | Experimental Finding |
|---|---|---|
| Model Implementation Type | Primary | Simulations with PBPK model template implementations generally require more time than stand-alone implementations [98]. |
| Treatment of Body Weight | High | Treating body weight and dependent quantities as constant parameters (fixed) instead of time-varying can result in a 30% time savings [98]. |
| Number of State Variables | High | Decreasing the number of state variables by 36% led to a 20–35% decrease in computational time [98]. |
| Number of Output Variables | Low | The number of output variables calculated did not have a large impact on simulation time [98]. |
| Implementation Language | Contextual | Interpreted languages (R, Python) offer easier model development; compiled languages (C, Fortran) provide faster simulations. A hybrid approach (e.g., R with MCSim) balances both [98]. |
The general finding is that template implementations incur a computational overhead. However, this cost must be weighed against the significant benefits templates provide, including reduced human time in model development and streamlined quality assurance (QA) review processes, as the template's core structure and code undergo a rigorous QA only once [98].
Optimization Strategies for Enhanced Computational Efficiency
Model Structure Optimization
Optimizing the fundamental structure of a PBPK model is one of the most effective ways to improve computational performance.
- Compartment Lumping: Combining tissue compartments with similar perfusion and partition characteristics ("lumping") can dramatically reduce the number of differential equations. One study demonstrated that reducing equations from 100 to 16 achieved an 11-fold improvement in simulation speed [98].
- Minimize State Variables: As shown in Table 1, a direct reduction in the number of state variables leads to a nearly proportional decrease in computational time. Design models with the minimal set of state variables necessary to answer the research question.
- Fix Constant Parameters: Avoid recalculating parameters that are constant over the simulation timeframe. Explicitly treating parameters like body weight and their dependent physiological quantities as fixed, rather than time-varying, can yield immediate and significant time savings [98].
Implementation and Workflow Optimization
Beyond the model structure, choices in implementation and workflow can also yield efficiency gains.
- Leverage Compiled Code: For large-scale simulations like Monte Carlo analyses, which may involve hundreds of thousands of runs, the use of compiled code is critical. Utilizing platforms like MCSim, which translates a human-readable model definition into compiled C code, combines development convenience with execution speed [98].
- Template-Specific Tuning: When using a template, actively disable all unused features and compartments by setting their relevant parameters and blood flows to zero. This ensures the computational engine is not wasting cycles on irrelevant calculations.
- Strategic Workflow: The "middle-out" approach, which integrates bottom-up (from first principles) and top-down (from data) methodologies, is often employed to fine-tune model parameters and improve predictive performance without unnecessarily increasing complexity [97].
Success in PBPK modeling relies on a combination of software, data, and strategic approaches. The following table details key resources that constitute the modern PBPK modeler's toolkit.
Table 2: Essential Research Reagent Solutions for PBPK Modeling
| Tool Category | Specific Examples | Function and Application |
|---|---|---|
| Commercial PBPK Software | Simcyp Simulator, GastroPlus, PK-Sim | Provide integrated platforms with built-in physiological and population databases, streamlining model development, simulation, and application in areas like DDI prediction and oral absorption [101] [99] [97]. |
| Open-Source Platforms & Tools | PK-Sim (open-source), R/pharmacy packages, MCSim | Offer flexible, transparent, and cost-effective environments for model implementation, simulation, and parameter estimation, often supporting a hybrid compiled/interpreted workflow [98] [102] [97]. |
| Model Template Systems | US EPA PBPK Model Template | A pre-verified model superstructure that accelerates the development of chemical-specific models, reduces human time in model preparation, and simplifies the QA review process [98]. |
| Quality Assurance (QA) Protocols | FDA/EMA Guidance Documents, OECD Guidance No. 331 | Standardized procedures and reporting templates for model verification and validation, which are critical for building confidence in model predictions and for regulatory submissions [98] [103] [100]. |
| Advanced Integration Technologies | AI/ML (e.g., ANN, XGBoost), QSAR Models | Enhance PBPK model accuracy and scope by optimizing nanoparticle formulations, predicting hard-to-measure parameters, and simulating complex systems like tumor biodistribution [104]. |
Decision Framework and Future Directions
Selecting an Implementation Strategy
The choice between a template and a stand-alone PBPK implementation is not a simple binary decision but a strategic trade-off. The following diagram outlines the key decision points and their consequences in the model implementation workflow.
This decision pathway illustrates that the optimal choice is highly context-dependent. A template is advantageous for rapid deployment and when flexibility is prized, while a stand-alone model is superior for maximized computational performance in large-scale or resource-constrained applications.
Emerging Trends and Future Outlook
The field of PBPK modeling is dynamic, with several trends shaping its future:
- Integration with Artificial Intelligence: AI and machine learning are being integrated with PBPK models to optimize nanoparticle drug delivery, predict parameters, and enhance the accuracy of biodistribution forecasts, potentially reducing reliance on animal studies [104].
- Regulatory Acceptance and Standardization: PBPK modeling is now a established tool in regulatory science, with its use documented in over 25% of recent FDA new drug applications, primarily for DDI assessment and dosing in organ impairment [99]. Continued development of best practices and reporting standards is crucial for wider adoption.
- Addressing Implementation Challenges: Key challenges remain, including the need for expert model review, confidence in predictions for data-poor chemicals, and improving model transferability across platforms [105] [103] [100]. Future work on transparent, well-documented models and collaborative frameworks is essential to overcome these hurdles.
The decision between template and stand-alone PBPK implementation represents a fundamental trade-off between human efficiency and computational performance. Template-based approaches offer significant advantages in development speed, standardization, and ease of QA review, making them ideal for rapid prototyping and applications where model flexibility is key. In contrast, stand-alone implementations provide superior computational speed and minimalism, which is critical for large-scale parameter uncertainty and variability analyses. An understanding of the quantitative impacts of design choices—such as fixing constant parameters, reducing state variables, and strategically lumping compartments—enables researchers to optimize their workflows effectively. As the field advances, the integration of PBPK with AI and its growing role in regulatory decision-making will further elevate the importance of efficient, well-optimized computational workflows in silico pharmacokinetic research.
Mitigating Challenges in Modeling Novel Formulations and Complex Drug Delivery Systems
The development of novel drug delivery systems (DDS) represents a transformative frontier in pharmaceutical sciences, enabling targeted therapeutic delivery and enhanced treatment efficacy. However, accurately predicting the pharmacokinetic (PK) and pharmacodynamic (PD) behavior of these complex systems presents significant computational challenges. This whitepaper examines the primary obstacles in modeling advanced DDS—including nanocarriers, stimuli-responsive systems, and targeted delivery platforms—and outlines integrated computational strategies to overcome them. By leveraging artificial intelligence (AI), physiologically based pharmacokinetic (PBPK) modeling, and multiscale simulation approaches, researchers can accelerate the development of sophisticated drug delivery platforms while reducing reliance on extensive experimental testing. Within the broader context of in silico pharmacokinetic research, these methodologies provide a critical framework for optimizing formulation design and predicting clinical performance.
The evolution from conventional drug delivery to advanced drug delivery systems (ADDS) marks a paradigm shift in pharmaceutical development. These systems are engineered to release therapeutic agents at predetermined rates and target specific tissues or cell types, thereby enhancing drug stability, optimizing distribution, increasing target concentration, and reducing adverse reactions [106] [107]. The current landscape encompasses a diverse array of sophisticated platforms including nanoparticle-based carriers, molecularly imprinted polymers, sustained-release formulations, and drug-device combination products [108] [109].
As these delivery systems grow more complex, so do the challenges in predicting their in vivo behavior using computational models. Traditional pharmacokinetic modeling approaches often struggle to account for the unique properties of nanocarriers, targeted delivery mechanisms, and responsive release systems [110] [65]. This creates a critical need for advanced in silico methodologies that can accurately simulate the performance of novel formulations throughout the drug development pipeline. By addressing these modeling challenges, researchers can bridge the gap between formulation design and clinical performance, ultimately accelerating the translation of innovative drug delivery systems from benchtop to bedside.
Core Challenges in Modeling Complex Drug Delivery Systems
Biological Barrier Penetration and Tissue Heterogeneity
The human body presents numerous biological barriers that restrict drug delivery to target sites, with the blood-brain barrier (BBB) representing a particularly formidable challenge for central nervous system (CNS) therapeutics. This highly selective interface severely limits the passage of therapeutic agents from the bloodstream to the brain tissue [110]. Additionally, the tumor microenvironment exhibits unique characteristics such as heterogeneous vascularization, elevated interstitial pressure, and altered pH, which create substantial obstacles for uniform drug distribution [109]. These biological complexities are further compounded by individual patient factors including genetic variations, disease states, age-related physiological changes, and organ impairment, all of which significantly influence drug disposition and response [65].
Physicochemical Complexity of Formulations
Advanced drug delivery systems exhibit intricate physicochemical properties that challenge conventional modeling approaches. Nanoparticles, liposomes, and other nanocarriers possess dynamic characteristics—including size distribution, surface charge, encapsulation efficiency, and release kinetics—that evolve throughout the delivery process [108] [106]. Stimuli-responsive systems designed to release their payload in response to specific biological cues (e.g., pH, enzyme activity, or temperature) introduce additional complexity, as models must account for both spatial and temporal changes in the local microenvironment [109] [107]. Furthermore, the integration of drugs with medical devices, such as auto-injectors, microneedle patches, and implantable systems, creates combination products whose behavior depends on the intricate interplay between formulation and device performance [108] [111].
Analytical and Characterization Limitations
Comprehensive model development requires robust experimental data for validation, yet many advanced drug delivery systems present significant analytical challenges. Nanocarriers and modified proteins necessitate sophisticated characterization methods to determine critical quality attributes including particle size distribution, surface characteristics, drug loading efficiency, and release kinetics [108]. For complex generics, demonstrating bioequivalence often requires specialized studies that go beyond those needed for conventional drugs, particularly when the reference product contains complex active ingredients, formulations, or routes of delivery [111]. The inherent variability of biological systems, combined with the potential for immune responses to nanocarriers or viral vectors, introduces additional uncertainty that must be accounted for in predictive models [108] [110].
Table 1: Key Challenges in Modeling Advanced Drug Delivery Systems
| Challenge Category | Specific Challenges | Impact on Modeling |
|---|---|---|
| Biological Barriers | Blood-brain barrier, tumor microenvironment, patient-specific factors | Limits predictive accuracy for tissue distribution and target site concentrations |
| Formulation Complexity | Nanocarrier dynamics, stimuli-responsive behavior, drug-device integration | Requires multiscale, multi-mechanism modeling approaches |
| Analytical Limitations | Characterization of nanocarriers, demonstration of bioequivalence, immunogenicity | Creates gaps in validation data for model refinement |
Computational Modeling Approaches and Methodologies
AI-Enhanced Physiologically Based Pharmacokinetic (PBPK) Modeling
The integration of artificial intelligence with traditional PBPK modeling represents a groundbreaking approach for predicting the pharmacokinetic behavior of complex drug formulations. AI-PBPK models leverage machine learning (ML) and deep learning (DL) algorithms to predict critical absorption, distribution, metabolism, and excretion (ADME) parameters directly from a compound's structural formula, significantly enhancing the capability of classical PBPK models [61]. This integrated approach is particularly valuable during early drug discovery stages when experimental data are limited, as it enables researchers to screen potential candidate compounds more efficiently and prioritize the most promising candidates for further development [65] [61].
The implementation workflow for AI-PBPK modeling typically follows a structured process: (1) input of the compound's structural formula into the AI model to generate key ADME parameters and physicochemical properties; (2) utilization of these parameters in the PBPK model to predict pharmacokinetic profiles; and (3) development of a PD model to predict therapeutic effects based on plasma free drug concentrations [61]. This methodology was successfully applied in a recent study focusing on aldosterone synthase inhibitors, where the AI-PBPK model demonstrated good predictive accuracy for PK/PD properties, providing a valuable reference for early lead compound screening and optimization [61].
Nanocarrier and Targeted Delivery System Modeling
The modeling of nanocarrier-based drug delivery systems requires specialized approaches that account for their unique behavior in biological systems. For nanoparticle systems, key parameters include particle size, surface characteristics, ligand conjugation for active targeting, and drug release kinetics [108] [106]. Passive targeting mechanisms, such as the Enhanced Permeability and Retention (EPR) effect in tumor tissues, can be simulated using diffusion-based models that incorporate tissue permeability parameters [109]. Active targeting approaches, which utilize specific ligands to bind to target tissues, require more sophisticated models that account for receptor binding kinetics, internalization processes, and intracellular trafficking [109].
Stimuli-responsive systems necessitate models that incorporate environmental triggers such as pH, enzyme concentrations, or redox potential to accurately simulate drug release profiles [107]. For instance, pH-sensitive nanoparticles designed for tumor targeting require models that can simulate the pH gradient from blood circulation (pH 7.4) to the tumor microenvironment (pH 6.5-6.9) and further to endolysosomal compartments (pH 4.5-5.5) [107]. These multiscale models must integrate molecular-level interactions with tissue-level distribution patterns to provide comprehensive predictions of drug delivery efficiency.
Table 2: Modeling Parameters for Different Nanocarrier Systems
| Nanocarrier Type | Key Modeling Parameters | Special Considerations |
|---|---|---|
| Liposomes | Bilayer composition, size distribution, encapsulation efficiency, surface modification | Stability in circulation, interaction with plasma proteins, release kinetics |
| Polymeric Nanoparticles | Polymer degradation rate, drug-polymer interactions, porosity, erosion mechanisms | Controlled release profile, biodegradation products, potential inflammatory responses |
| Lipid Nanoparticles (LNPs) | Ionizable lipid composition, PEG-lipid content, nucleic acid encapsulation efficiency | Nucleic acid protection, endosomal escape efficiency, organ-selective targeting |
| Stimuli-Responsive Systems | Trigger sensitivity, response kinetics, environmental sensing mechanisms | Specificity for pathological conditions, off-target activation potential |
Integrated PBPK/PD Modeling for Special Populations
Virtual population modeling using PBPK approaches enables the prediction of drug behavior across diverse patient populations, addressing a critical challenge in drug development. These models can simulate physiological differences in pediatric and geriatric populations, pregnant women, and patients with organ impairment, providing valuable insights for personalized medicine approaches [65]. For instance, age-dependent decreases in hepatic and renal function can be incorporated into PBPK models to predict altered drug metabolism and excretion in older adults, while physiological changes during pregnancy can be modeled to optimize dosing regimens for pregnant patients [65].
The integration of real-world data (RWD) from electronic health records, patient registries, and patient-reported outcomes further enhances the predictive capability of these models by capturing the variability in comorbidities, concomitant medications, and treatment adherence that occurs in clinical practice [65]. Quantitative systems pharmacology/toxicology (QSP/QST) modeling builds upon PBPK foundations by incorporating additional layers of biological complexity, enabling the prediction of both therapeutic efficacy and potential adverse effects across different patient subpopulations [65].
Experimental Protocols and Validation Frameworks
Model Calibration and Validation Protocol
Establishing robust calibration and validation protocols is essential for ensuring the predictive accuracy of computational models for novel drug delivery systems. The recommended workflow begins with model construction using available compound data, followed by calibration through parameter adjustment based on comparison with experimental results [61]. External validation using independent datasets is then performed to assess model performance, with subsequent application to predict the behavior of new compounds or formulations [61].
A practical implementation of this protocol was demonstrated in a study of aldosterone synthase inhibitors, where Baxdrostat—the compound with the most extensive clinical data—was selected as the model drug for initial calibration [61]. The model was subsequently validated using clinical PK data from two additional ASIs (Dexfadrostat and Lorundrostat), with predictive performance assessed through comparison of simulated and observed pharmacokinetic profiles [61]. This systematic approach to model validation ensures reliability before application to novel compound evaluation.
Integrated In Silico-In Vitro Testing Framework
A tiered testing framework that integrates in silico predictions with targeted in vitro experiments provides a comprehensive strategy for model development and validation. This approach begins with computational prediction of critical formulation properties, followed by designed in vitro experiments to validate key parameters and refine the computational models [108] [106]. For nanoparticle systems, essential in vitro characterization includes particle size and distribution analysis, surface charge measurement, drug loading efficiency quantification, and release kinetics profiling under biologically relevant conditions [108].
For targeted delivery systems, in vitro binding assays using cell cultures expressing target receptors provide crucial data on ligand-receptor interaction kinetics, which can be incorporated into mechanistic models of targeted delivery [109]. Similarly, permeability assays across artificial or cell-based barriers (e.g., BBB models) yield quantitative data on barrier penetration potential that enhances the predictive accuracy of tissue distribution models [110]. This integrated framework maximizes efficiency by focusing experimental resources on parameters with the greatest impact on model accuracy and predictive power.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Modeling Complex Drug Delivery Systems
| Tool Category | Specific Tools/Platforms | Function and Application |
|---|---|---|
| Computational Modeling Platforms | GastroPlus, Simcyp Simulator, B2O Simulator | Provide integrated environments for PBPK modeling, population simulation, and formulation optimization |
| AI/ML Prediction Tools | ADMET-AI, SwissADME, pkCSM, ADMETlab 3.0 | Predict key ADMET parameters from molecular structure to inform PBPK models |
| Nanocarrier Formulation Materials | Ionizable lipids (for LNPs), PEGylated lipids, biodegradable polymers (PLGA, PLA), stimulus-responsive materials | Enable construction of advanced delivery systems with tailored properties |
| Characterization Assays | Particle size analyzers, HPLC/UPLC systems, surface plasmon resonance (SPR), in vitro release testing apparatus | Provide critical experimental data for model parameterization and validation |
| Biological Testing Systems | Cell-based barrier models (e.g., BBB models), 3D tumor spheroids, organ-on-a-chip devices | Generate biologically relevant data on barrier penetration and tissue distribution |
The successful modeling of novel formulations and complex drug delivery systems requires an integrated approach that combines advanced computational methodologies with targeted experimental validation. AI-enhanced PBPK modeling, virtual population simulations, and multiscale modeling techniques provide powerful tools for addressing the unique challenges presented by nanocarriers, targeted delivery systems, and stimuli-responsive formulations. As these computational approaches continue to evolve, they will play an increasingly vital role in accelerating the development of sophisticated drug delivery platforms, optimizing formulation design, and predicting clinical performance. By embracing these innovative modeling strategies within the broader framework of in silico pharmacokinetic research, pharmaceutical scientists can navigate the complexities of modern drug delivery with greater precision and efficiency, ultimately enabling the development of more effective and targeted therapeutic interventions.
Ensuring Predictive Power: Validation Frameworks and Comparative Analysis of In Silico Approaches
Best Practices for Model Calibration, Validation, and Regulatory Acceptance
In silico methodologies have become a central pillar of modern drug development, enabling researchers to simulate biological systems, predict pharmacokinetic (PK) and pharmacodynamic (PD) properties, and optimize therapeutic interventions. The U.S. Food and Drug Administration's (FDA) landmark decisions to phase out mandatory animal testing for many drug types and support alternative methods signal a paradigm shift toward computational evidence in regulatory science [112] [113]. This transition places increased importance on establishing rigorous frameworks for model calibration, validation, and regulatory acceptance, particularly for physiologically based pharmacokinetic (PBPK) and population PK (PopPK) models used in pharmacometric analyses.
Model-informed precision dosing (MIPD) leverages PopPK models, Bayesian estimation, and individual patient data to optimize dosing regimens, requiring exceptional model accuracy to ensure patient safety and therapeutic efficacy [114]. The foundation of reliable in silico research rests upon establishing model credibility through demonstrated calibration, comprehensive validation, and transparent documentation aligned with regulatory expectations.
Foundational Principles of Model Calibration
Calibration Concepts and Definitions
Calibration represents the process of adjusting model parameters to establish correlation between a model's predictions and observed experimental or clinical data. In computational modeling, calibration involves testing and adjusting model parameters to establish accuracy against known outcomes or reference standards [115] [116]. This process ensures the mathematical representation within the model faithfully reproduces biological reality.
Calibration verification means testing the model with materials of known values in the same manner as actual applications to assure the model accurately simulates systems throughout its intended operating range [115]. For PBPK models, this typically involves comparing predicted concentration-time profiles against observed clinical data across different dosing regimens.
Practical Calibration Methodologies
The calibration process requires carefully designed experiments using samples with assigned target values. For PK models, these may include control solutions with known concentrations, proficiency testing samples with target values, or specialized "linearity" materials with established reference points [115]. Clinical data from compounds with extensive clinical datasets, such as using Baxdrostat as a model compound for aldosterone synthase inhibitors, provides robust calibration benchmarks [61].
Graphical assessment represents a critical component of calibration evaluation. Researchers should plot simulated results on the y-axis against observed values on the x-axis, drawing a 45-degree line of identity for visual comparison [115]. Difference plots, displaying residuals (observed minus predicted values) against assigned values, offer enhanced visualization of agreement/disagreement patterns across the model's range.
Table 1: Statistical Measures for Calibration Assessment
| Metric | Calculation | Acceptance Criteria | Application Context |
|---|---|---|---|
| Prediction Error (PE) | (Predicted - Observed)/Observed × 100% | Mean PE < 30-40% [117] | PopPK model validation |
| Slope Comparison | Comparison to ideal slope of 1.00 | Ideal slope ± %TEa/100 [115] | Linear regression assessment |
| Absolute Average Fold Error (AAFE) | 10^(|Σ log(Predicted/Observed)|/n) | <2.0 for good prediction [61] | PBPK model performance |
Comprehensive Model Validation Strategies
Validation Framework and Principles
Model validation provides independent assessment of a model's accuracy, completeness, theoretical soundness, and fit for purpose [118]. A robust validation framework encompasses several dimensions: conceptual soundness, input verification, computational accuracy, and predictive performance. Validation is not a one-time event but an ongoing process throughout the model lifecycle.
For pharmacological models, validation ensures that virtual patient simulations accurately predict real-world drug behavior, a critical requirement when these models inform clinical decision-making through MIPD [114]. The reliability of output from precision dosing software depends heavily on the population PK model selected, making thorough validation essential for patient safety.
Input Validation and Verification
Input validation ensures all model parameters and data sources are accurate, traceable, and appropriate for the model's intended use. Leading practices emphasize rigorous input assessment through reconciliation with authoritative sources and verification against relevant benchmarks [118]. All inputs should undergo reasonableness checks, with heightened scrutiny on parameters that have changed since prior implementations.
For PBPK models, key input parameters include physiological characteristics (organ weights, blood flows, enzyme expression levels) and molecule-specific parameters (lipophilicity, protein binding, metabolic clearance). Machine learning approaches are increasingly used to predict ADME parameters from structural formulae when experimental data are limited [61]. These predicted parameters still require verification against any available experimental data.
Computational and Output Validation
Computational validation confirms the mathematical implementation accurately reflects the theoretical model structure. An independently developed first-principles model represents the gold standard for validating complex calculations [118]. For large-scale PBPK models, this may involve creating a simplified independent model that captures principal risk drivers without reproducing full complexity.
Output validation assesses the stability and reliability of model predictions under varying conditions. Techniques include:
- Sensitivity analysis: Measuring how output changes in response to input variations
- Stress testing: Evaluating model behavior under extreme conditions
- Back-testing: Comparing historical predictions to actual outcomes
- Dynamic validation: Comparing historical trends against projected results [118]
Table 2: Validation Techniques for Different Model Components
| Model Component | Primary Validation Methods | Performance Targets |
|---|---|---|
| Structural Model | Comparison to alternative structures, visual predictive checks, goodness-of-fit plots | Objective function value improvements, successful convergence |
| Covariate Effects | Stepwise covariate modeling, bootstrap evaluation, posterior predictive checks | Statistical significance (p<0.01 forward inclusion, p<0.001 backward elimination) |
| Error Models | Residual diagnostics, simulation-based evaluations | Absence of systematic bias, homoscedastic variance |
| Predictive Performance | Prediction-corrected visual predictive checks, normalized prediction distribution errors | <10% divergence from observed data distributions |
Regulatory Acceptance Framework
Evolving Regulatory Landscape
Regulatory agencies worldwide are establishing frameworks for evaluating computational models in drug development. The FDA's New Alternative Methods Program aims to spur adoption of alternative methods that can replace, reduce, and refine animal testing while improving predictivity of nonclinical testing [113]. The FDA's Modeling and Simulation Working Group, comprising nearly 200 scientists across FDA centers, works to advance regulatory science through computational approaches [113].
The concept of "qualification" allows alternative methods to be evaluated by FDA in advance for a specific context of use (COU) [113]. The qualified COU defines boundaries within which available data adequately justify use of the tool, similar to a drug's indications for use. This framework provides regulatory predictability for employing validated computational approaches.
Demonstrating Model Credibility
The FDA's draft guidance "Assessing the Credibility of Computational Modeling and Simulation in Medical Device Submissions" describes a risk-based framework for credibility assessment, which can be adapted for pharmacological models [113]. Key elements include:
- Context of Use Definition: Clearly specifying the model's purpose, scope, and application boundaries
- Model Verification: Ensuring computational implementation matches theoretical specifications
- Model Validation: Providing evidence the model accurately represents reality for the COU
- Uncertainty Quantification: Characterizing variability and uncertainty in model inputs and outputs
For PBPK models submitted to regulatory agencies, the European Medicines Agency recommends assessing model credibility through verification of coding, evaluation of input parameters, and comparison of simulated outcomes with clinical data not used for model development.
Experimental Protocols for Key Validation Experiments
PopPK Model Development and Validation Protocol
The development and validation of population pharmacokinetic models follows a structured approach, as demonstrated in a perioperative tacrolimus study after lung transplantation [117]:
Model Development Phase:
- Data Collection: Retrospectively collect rich or sparse PK samples from 200-300 patients, capturing relevant patient characteristics, genetic factors (e.g., CYP3A5 genotype), and clinical covariates
- Base Model Development: Use nonlinear mixed-effects modeling to develop a structural model (e.g., one-compartment with fixed absorption), identifying between-subject variability components
- Covariate Model Building: Apply stepwise covariate selection (p<0.01 for forward inclusion, p<0.001 for backward elimination) to identify significant relationships between patient factors and PK parameters
- Model Evaluation: Assess goodness-of-fit plots, parameter precision, and visual predictive checks
Model Validation Phase:
- Internal Validation: Apply bootstrap resampling (1000-2000 runs) to evaluate parameter stability
- External Validation: Apply developed model to an independent cohort of 100-150 patients
- Predictive Performance Assessment: Calculate prediction errors (PE) with acceptable performance demonstrated by mean PE of 30-40% and median PE of 5-10% [117]
- Clinical Application: Develop precision dosing algorithms based on final model to optimize target attainment
AI-PBPK Model Workflow Protocol
The integration of artificial intelligence with PBPK modeling represents an emerging approach for early drug discovery [61]:
Model Construction and Calibration:
- Platform Development: Establish web-based platform integrating machine learning and PBPK capabilities
- Model Compound Selection: Identify compound with extensive clinical data (e.g., Baxdrostat for ASIs) as calibration compound
- Parameter Prediction: Input structural formula into AI module to generate key ADME parameters and physicochemical properties
- Model Calibration: Compare initial PK predictions with published clinical data, adjusting key parameters to improve fit
Model Validation and Application:
- External Validation: Apply calibrated model to predict PK profiles for 2-3 additional compounds with available clinical data
- Performance Assessment: Evaluate predictive accuracy using geometric mean fold error metrics (target <2.0)
- PD Predictions: Develop Emax models to predict enzyme inhibition based on plasma free drug concentrations
- Selectivity Assessment: Calculate selectivity index (IC50 for off-target/IC50 for primary target) to optimize compound selection
AI-PBPK Model Development Workflow
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Computational Tools for In Silico Pharmacology
| Tool Category | Specific Examples | Function and Application | Regulatory Status |
|---|---|---|---|
| PBPK Platforms | GastroPlus, Simcyp Simulator, PK-Sim | Integrated PBPK modeling platforms for predicting drug disposition across populations | Accepted in regulatory submissions for specific contexts of use |
| ADMET Prediction Tools | SwissADME, pkCSM, ADMETlab 3.0 | AI-based prediction of absorption, distribution, metabolism, excretion, and toxicity parameters | Screening tools; require experimental verification for regulatory submissions |
| PopPK Software | NONMEM, Monolix, Pmetrics | Nonlinear mixed-effects modeling for population pharmacokinetic analysis | Industry standard for PopPK analysis in regulatory submissions |
| Clinical Data Sources | ClinicalTrials.gov, PubMed, Internal Databases | Sources of clinical PK/PD data for model calibration and validation | Variable quality; preferred sources have rigorous study designs |
| Reference Compounds | Baxdrostat, Tacrolimus, Midazolam | Well-characterized compounds with extensive clinical data for model verification | Suitable as calibration standards for specific metabolic pathways |
The evolving landscape of drug development demands increasingly sophisticated approaches to model calibration, validation, and regulatory strategy. As regulatory agencies phase out mandatory animal testing and embrace alternative methods, the importance of rigorous computational model evaluation has never been greater [112] [113]. Successful implementation of in silico approaches requires multidisciplinary expertise spanning pharmacology, computational biology, statistics, and regulatory science.
The fundamental principles outlined in this guide provide a framework for developing credible pharmacological models that can support critical decisions in drug discovery and development. By adopting rigorous calibration procedures, comprehensive validation strategies, and proactive regulatory engagement, researchers can accelerate the transition toward a future where in silico methodologies are fully integrated into the drug development paradigm. As the field advances, continued collaboration between industry, academia, and regulators will be essential to establish standardized benchmarks and ensure that computational approaches fulfill their potential to transform therapeutic development.
Pharmacokinetic (PK) modeling is a cornerstone of modern drug development, providing a quantitative framework to understand how drugs are absorbed, distributed, metabolized, and excreted (ADME) within the body. In silico PK research employs computational models to predict drug behavior, reducing reliance on costly and time-consuming clinical trials. The field has evolved three distinct yet complementary approaches: mechanistic Physiologically-Based Pharmacokinetic (PBPK) models, data-driven Population PK (PopPK) models, and the emerging paradigm of hybrid AI-PBPK models. Mechanistic PBPK models utilize a "bottom-up" approach, constructing mathematical representations of human physiology and drug-specific properties to simulate drug concentrations in various tissues and organs [2] [97]. These models incorporate known anatomical, physiological, and biochemical parameters—such as organ volumes, blood flow rates, and tissue composition—to create a physiologically realistic framework for predicting drug disposition [1]. In contrast, data-driven PopPK models employ a "top-down" methodology, using non-linear mixed-effects (NLME) modeling to identify structural models and quantify variability in drug exposure across populations from observed clinical data [38] [119]. These models characterize both fixed effects (population averages) and random effects (inter-individual variability) without necessarily incorporating mechanistic physiological details. The convergence of these approaches with artificial intelligence has given rise to hybrid AI-PBPK models, which integrate mechanistic principles with machine learning's pattern recognition capabilities to address limitations of both traditional methodologies [41] [120].
The following table summarizes the fundamental characteristics of these three modeling approaches:
Table 1: Fundamental Characteristics of PK Modeling Approaches
| Characteristic | Mechanistic PBPK | Data-Driven PopPK | Hybrid AI-PBPK |
|---|---|---|---|
| Primary Approach | Bottom-up, mechanism-based | Top-down, data-driven | Integrated middle-out |
| Core Foundation | Human physiology and drug properties | Statistical analysis of clinical data | Machine learning enhanced physiology |
| Data Requirements | In vitro drug data, physiological parameters | Rich clinical concentration-time data | Diverse datasets (preclinical, clinical, physicochemical) |
| Key Outputs | Tissue concentration-time profiles | Population parameter estimates, variability | Enhanced predictions with uncertainty quantification |
| Regulatory Acceptance | Well-established for specific applications [97] | Gold standard for population analysis [119] | Emerging, with growing recognition [120] |
Core Principles and Methodologies
Mechanistic PBPK Modeling
Theoretical Foundations and Model Structure
PBPK modeling is grounded in mass balance principles, representing the body as interconnected compartments corresponding to specific organs or tissues. Each compartment is characterized by physiological parameters including volume, blood flow rate, and tissue composition [1] [97]. The fundamental differential equation governing drug distribution in a perfusion-limited tissue compartment can be expressed as:
$$dQi/dt = Fi(C{art} - Qi/(Pi × Vi))$$
Where $Qi$ represents the quantity of drug in compartment *i*, $Fi$ is the blood flow rate, $C{art}$ is the arterial blood concentration, $Pi$ is the tissue-to-blood partition coefficient, and $V_i$ is the tissue volume [1]. This equation illustrates how drug accumulation in each tissue depends on the balance between arterial inflow and venous outflow. For more complex distribution patterns, especially for biologics and nanoparticles, additional processes must be considered, such as endocytosis, target-mediated drug disposition, and lymphatic transport [41].
Critical Model Assumptions
PBPK models operate under two primary assumptions regarding drug distribution. The perfusion-limited assumption applies when drug permeability across capillary membranes is high, making blood flow the rate-limiting step for distribution. This assumption typically holds for small lipophilic drugs [97]. In contrast, the permeability-limited assumption becomes relevant when drug movement across cellular membranes constitutes the rate-limiting step, which is common for large molecules, polar compounds, and nanoparticles [41] [97]. The selection between these assumptions significantly impacts model structure and parameterization, particularly for complex drug delivery systems.
Model Development Workflow
The construction of a PBPK model follows a systematic workflow comprising five distinct phases [97]. The initial phase involves defining the model architecture by selecting relevant anatomical compartments based on the drug's disposition characteristics and therapeutic target. The second phase entails gathering species- and population-specific physiological parameters from literature sources or specialized databases. The third phase integrates drug-specific parameters, including physicochemical properties (molecular weight, logP, pKa) and ADME characteristics (permeability, metabolic clearance, transporter interactions). The fourth phase involves model calibration and validation using available in vivo PK data, with adjustments made to improve predictive performance. The final phase applies the validated model for simulation purposes under various dosing regimens, populations, or physiological conditions.
Table 2: Key Parameters in PBPK Model Development
| Parameter Category | Specific Examples | Sources |
|---|---|---|
| Organism/System Parameters | Organ volumes, blood flow rates, tissue composition, enzyme/transporter expression levels | Physiological literature, specialized databases [2] |
| Drug-Specific Parameters | Molecular weight, lipophilicity (logP/logD), pKa, solubility, permeability | In vitro assays, pre-existing experimental data [2] |
| Drug-Biological Interaction Parameters | Fraction unbound (fu), tissue-plasma partition coefficients (Kp), metabolic clearance rates | In vitro-in vivo extrapolation (IVIVE), clinical data [97] |
Data-Driven Population PK Modeling
Theoretical Framework
Population PK (PopPK) modeling employs non-linear mixed-effects (NLME) methodology to characterize drug pharmacokinetics across diverse populations [38]. This approach simultaneously estimates population typical parameters (fixed effects), inter-individual variability (random effects), and residual unexplained variability. The fundamental structural model for a one-compartment PK model with first-order absorption and elimination can be expressed as:
$$C(t) = (Dose × F × ka)/(V × (ka - ke)) × (e^{-ke × t} - e^{-k_a × t})$$
Where $C(t)$ represents drug concentration at time $t$, $F$ is bioavailability, $ka$ is the absorption rate constant, $V$ is volume of distribution, and $ke$ is the elimination rate constant [38]. PopPK models extend this basic structure by incorporating inter-individual variability on key parameters, often assuming log-normal distributions.
Model Development Process
Traditional PopPK model development follows an iterative, hierarchical process beginning with structural model identification, followed by statistical model development, and culminating in covariate model building [38]. The process typically starts with simple one-compartment models and progressively increases complexity through comparison of objective function values and diagnostic plots. This sequential approach, while established, is labor-intensive and potentially susceptible to local minima convergence, prompting interest in automated methodologies [38].
Hybrid AI-PBPK Modeling
Integration Strategies
Hybrid AI-PBPK models represent a novel paradigm that combines mechanistic modeling with artificial intelligence techniques. The integration occurs at multiple levels: AI-assisted parameter estimation uses machine learning to predict critical PBPK parameters that are difficult to measure experimentally [41] [120]; model structure optimization employs AI algorithms to identify optimal model configurations from a vast search space [38]; and hybrid prediction frameworks combine mechanistic simulations with data-driven corrections to improve accuracy [120]. For instance, neural ordinary differential equations (NeuralODEs) can enhance traditional PBPK models by learning complex, data-driven dynamics not fully captured by physiological mechanisms alone [39].
Machine Learning Techniques
Various machine learning approaches have been successfully applied to PK modeling challenges. Tree-based models (e.g., random forests, gradient boosting) excel at handling complex, non-linear relationships between patient factors and drug exposure [119]. Neural networks, particularly recurrent architectures, effectively model temporal patterns in drug concentration profiles [39]. Bayesian machine learning integrates prior knowledge with observed data, providing natural uncertainty quantification [121]. These techniques address specific limitations of traditional approaches, such as handling irregular sampling times, incorporating high-dimensional covariates, and identifying complex interaction effects [39].
Experimental Protocols and Implementation
Protocol 1: Developing a Mechanistic PBPK Model
Model Construction and Parameterization
The development of a mechanistic PBPK model begins with defining the model structure based on the drug's properties and research objectives. For small molecules, a standard structure might include compartments for lung, liver, gut, kidney, heart, brain, muscle, adipose, and slowly perfused tissues [1]. Each compartment is parameterized with tissue-specific volume and blood flow values obtained from physiological literature. Drug-specific parameters including lipophilicity (logP), acid dissociation constant (pKa), molecular weight, and plasma protein binding are incorporated [2]. Tissue-plasma partition coefficients ($K_p$ values) can be estimated using established methods such as the Poulin and Rodgers or Berezhkovskiy approaches, which correlate tissue composition with drug physicochemical properties [2].
Model Verification and Validation
Verification ensures the model is implemented correctly, while validation assesses predictive performance against independent datasets [122]. The validation process should include both internal validation using data employed during model development and external validation with completely independent datasets. Acceptance criteria should be predefined based on the model's intended use, with common metrics including average fold error (AFE) and absolute average fold error (AAFE), where values ≤2.0 often indicate acceptable prediction accuracy [122].
Protocol 2: Implementing Population PK Analysis
Data Collection and Structural Model Identification
Population PK analysis requires rich PK data from multiple individuals, ideally with varying demographic and pathophysiological characteristics [38]. The initial step involves exploratory data analysis to identify potential relationships between patient factors and PK parameters. Structural model identification traditionally employs a stepwise approach, beginning with simple one-compartment models and progressively increasing complexity [38]. Modern automated approaches define a model search space encompassing various compartmental structures, absorption models, and elimination mechanisms, then use optimization algorithms to efficiently explore this space [38].
Covariate Model Building and Model Evaluation
Covariate analysis identifies patient factors that explain inter-individual variability in PK parameters. Stepwise forward inclusion/backward elimination remains common, though machine learning techniques increasingly assist in covariate selection [119]. Model evaluation employs both objective function changes for nested models and information criteria (AIC, BIC) for non-nested comparisons. Visual predictive checks and bootstrap analysis provide additional validation of model performance and robustness [38].
Protocol 3: Building a Hybrid AI-PBPK Model for Nanoparticles
AI-Based Parameter Prediction
A representative hybrid AI-PBPK approach for nanoparticles involves developing a quantitative structure-activity relationship (QSAR) model to predict critical PBPK parameters based on nanoparticle physicochemical properties [120]. The process begins with curating a comprehensive dataset of nanoparticle properties (size, surface charge, composition) and corresponding in vivo PK parameters. Machine learning algorithms such as random forests or deep neural networks are trained to predict parameters like cellular uptake rates and tumor delivery efficiency from physicochemical characteristics [120].
PBPK Model Integration and Validation
The AI-predicted parameters are integrated into a mechanistic PBPK model that accounts for nanoparticle-specific processes including mononuclear phagocyte system uptake, enhanced permeability and retention effect, and target-mediated disposition [120]. The hybrid model is validated by comparing simulated biodistribution profiles against experimental data not used in model training. Performance metrics like determination coefficient (R²) and root mean squared error (RMSE) quantify predictive accuracy, with values of R² ≥0.70 often indicating satisfactory performance for nanoparticle tumor delivery prediction [120].
Comparative Analysis and Applications
Performance Across Drug Modalities
The suitability of each modeling approach varies significantly across drug modalities. Small molecule drugs represent the most established application for all three approaches, with PBPK particularly valuable for predicting drug-drug interactions and PopPK for characterizing population variability [122]. Therapeutic proteins and monoclonal antibodies present unique challenges due to target-mediated drug disposition, FcRn recycling, and lymphatic transport, necessitating specialized PBPK models [41]. Nanoparticles and complex drug delivery systems benefit most from hybrid AI-PBPK approaches, which can capture complex relationships between physicochemical properties and in vivo behavior [120].
Applications in Drug Development
Table 3: Applications of PK Modeling Approaches in Drug Development
| Application Area | Mechanistic PBPK | Data-Driven PopPK | Hybrid AI-PBPK |
|---|---|---|---|
| First-in-Human Dose Prediction | Primary approach using IVIVE [121] | Supports starting dose selection [38] | Emerging application [120] |
| Special Populations | Extensively used for pediatrics, organ impairment [2] [97] | Used for covariate identification [38] | Potential for personalized dosing [39] |
| Formulation Optimization | Predicting food effects, absorption [97] | Limited application | Formulation-PK relationships [120] |
| Drug-Drug Interactions | Primary quantitative approach [122] [97] | Descriptive analysis | Enhanced prediction [41] |
Visualization of Modeling Approaches
Workflow Diagram: PBPK Model Development
Diagram Title: PBPK Model Development Workflow
Workflow Diagram: PopPK Model Development
Diagram Title: Population PK Model Development Workflow
Workflow Diagram: Hybrid AI-PBPK Integration
Diagram Title: Hybrid AI-PBPK Model Integration
Table 4: Essential Tools and Platforms for PK Modeling Research
| Tool Category | Specific Tools/Platforms | Key Functionality |
|---|---|---|
| Commercial PBPK Software | GastroPlus (Simulations Plus), Simcyp (Certara), PK-Sim (Bayer) [2] [97] | Integrated physiological databases, IVIVE capabilities, specialized modules for different applications |
| Open-Source Platforms | Open Systems Pharmacology, pyDarwin [38] | Flexible model development, algorithm implementation, collaborative development |
| Population PK Software | NONMEM, Monolix, Phoenix NLME [38] | NLME modeling, covariate analysis, model diagnostics and visualization |
| Machine Learning Libraries | Scikit-learn, TensorFlow, PyTorch [120] [119] | Implementation of ML algorithms, neural networks, automated feature selection |
| Specialized Databases | NCBI PMC, "Nano-Tumor Database" [120] | Literature access, curated experimental data for training ML models |
The comparative analysis of mechanistic PBPK, data-driven PopPK, and hybrid AI-PBPK models reveals a complementary landscape of in silico approaches for pharmacokinetic prediction. Mechanistic PBPK models provide physiological transparency and strong extrapolation capabilities, making them invaluable for first-in-human predictions, special populations, and drug-drug interactions. Data-driven PopPK models offer robust characterization of population variability and remain the standard for clinical trial analysis and dosing individualization. Hybrid AI-PBPK models represent the emerging frontier, addressing limitations of both approaches through enhanced parameter estimation, model optimization, and predictive accuracy, particularly for complex modalities like nanoparticles. The integration of artificial intelligence with mechanistic modeling represents a paradigm shift in pharmacokinetics, offering unprecedented opportunities to accelerate drug development, optimize therapeutic regimens, and advance personalized medicine. As these approaches continue to evolve and converge, they will undoubtedly reshape the landscape of in silico pharmacokinetic research and clinical pharmacology practice.
In silico pharmacokinetic prediction has become a cornerstone of modern drug discovery, offering the potential to reduce experimental costs and accelerate the identification of viable drug candidates. However, the reliability of these computational models depends critically on rigorous benchmarking practices that account for data quality, methodological appropriateness, and applicability domains. This technical review examines current benchmarking methodologies across key areas of pharmacokinetic prediction, highlighting systematic approaches for evaluating predictive accuracy from small molecules to therapeutic proteins. As pharmaceutical research increasingly embraces artificial intelligence and machine learning, establishing robust validation frameworks becomes paramount for translating computational predictions into successful therapeutic outcomes.
Foundational Concepts in Predictive Model Assessment
Core Performance Metrics and Validation Principles
Accurate assessment of predictive models requires multiple complementary metrics that capture different aspects of model performance. For regression tasks predicting continuous values (e.g., binding affinity, solubility), the root mean square error (RMSE) and coefficient of determination (R²) provide insights into prediction accuracy and variance explanation. For classification tasks (e.g., drug-target interaction prediction), precision, recall, F1-score, and ROC-AUC offer a comprehensive view of model capability across different decision thresholds.
Critical to meaningful benchmarking is external validation using completely independent datasets not seen during model training. Recent research emphasizes that models should be evaluated specifically within their applicability domain to ensure chemical space relevance [123]. Additionally, data consistency assessment (DCA) prior to modeling has been shown to be crucial, as dataset discrepancies can significantly degrade model performance [55].
Benchmarking Small Molecule Property Prediction
Data Quality Challenges and Integration Strategies
Small molecule pharmacokinetic prediction faces significant data challenges, particularly regarding data heterogeneity and distributional misalignments between different experimental sources. Analysis of public ADME datasets has revealed substantial misalignments and inconsistent property annotations between gold-standard and popular benchmark sources such as Therapeutic Data Commons (TDC) [55]. These discrepancies arise from differences in experimental conditions, measurement protocols, and chemical space coverage, introducing noise that compromises predictive accuracy.
The AssayInspector package has been developed specifically to address these challenges through systematic data consistency assessment prior to modeling. This model-agnostic tool leverages statistics, visualizations, and diagnostic summaries to identify outliers, batch effects, and discrepancies across datasets [55]. Importantly, research demonstrates that naive data integration or standardization often degrades performance rather than improving it, highlighting the necessity of rigorous data quality assessment before model training.
Performance Benchmarking of QSAR Tools
Comprehensive benchmarking of computational tools for predicting physicochemical and toxicokinetic properties reveals significant variation in performance across different chemical classes. A recent evaluation of twelve QSAR software tools across 41 validation datasets found that models for physicochemical properties (average R² = 0.717) generally outperformed those for toxicokinetic properties (average R² = 0.639 for regression) [123].
Table 1: Performance Benchmarking of QSAR Tools for Key Properties
| Property | Best Performing Tools | Performance Metrics | Chemical Space Coverage |
|---|---|---|---|
| LogP | OPERA | R² = 0.89-0.94 | Drugs, industrial chemicals |
| Solubility | OPERA, ADMET Predict | R² = 0.79-0.85 | Diverse organic compounds |
| Caco-2 Permeability | ADMET Predict | Balanced accuracy = 0.81-0.85 | Pharmaceutical compounds |
| hERG Inhibition | PreADMET, admetSAR | Balanced accuracy = 0.76-0.82 | Drug-like molecules |
The benchmarking emphasized that model performance is highly dependent on the chemical space being evaluated, with distinct performance patterns observed for drugs, industrial chemicals, and natural products [123]. Tools that provided applicability domain assessment, such as OPERA and ADMET Predict, demonstrated more reliable performance for real-world applications where chemical diversity is substantial.
Experimental Protocol for Small Molecule Benchmarking
A robust benchmarking protocol for small molecule property prediction should include:
Data Curation and Standardization: Implement automated curation pipelines using tools like RDKit to remove inorganic compounds, neutralize salts, and standardize chemical structures. Address experimental outliers through Z-score analysis (removing points with |Z| > 3) and resolve inconsistencies across datasets [123].
Chemical Space Characterization: Apply principal component analysis (PCA) on molecular fingerprints (e.g., FCFP with radius 2 folded to 1024 bits) to visualize dataset coverage relative to reference chemical spaces including approved drugs, industrial chemicals, and natural products [123].
Model Training with Applicability Domain: Implement appropriate applicability domain definitions using leverage and similarity approaches to identify reliable predictions.
Comprehensive Validation: Employ stratified splitting methods that maintain activity distribution and chemical diversity in training/test splits, followed by external validation on completely independent datasets.
Benchmarking Drug-Target Interaction Prediction
Methodological Comparisons and Performance Standards
Drug-target interaction (DTI) prediction represents a critical component of pharmacokinetic profiling, with both target-centric and ligand-centric approaches demonstrating complementary strengths. A systematic comparison of seven target prediction methods using a shared benchmark dataset of FDA-approved drugs revealed that MolTarPred emerged as the most effective method, particularly when using Morgan fingerprints with Tanimoto scores [124].
Table 2: Performance Comparison of DTI Prediction Methods
| Method | Approach | Key Features | Reported Performance |
|---|---|---|---|
| MolTarPred | Ligand-centric | 2D similarity using Morgan fingerprints | Highest effectiveness in benchmark |
| RF-QSAR | Target-centric | Random forest with ECFP4 fingerprints | AUC-ROC: 0.790-0.893 |
| BarlowDTI | Target-centric | Barlow Twins architecture | ROC-AUC: 0.9364 |
| GAN+RFC | Hybrid | GAN for data balancing, Random Forest | ROC-AUC: 0.9942 (Kd) |
| kNN-DTA | Hybrid | k-nearest neighbors with adaptive aggregation | RMSE: 0.684 (IC50) |
The benchmarking study highlighted that model optimization strategies, such as high-confidence filtering, involve important trade-offs. While filtering improves precision, it reduces recall, making it less ideal for drug repurposing applications where comprehensive target identification is prioritized [124].
Advanced Frameworks for Data Imbalance and Feature Engineering
Data imbalance presents a significant challenge in DTI prediction, where non-interacting pairs vastly outnumber interacting ones. A novel hybrid framework addressing this issue employs Generative Adversarial Networks (GANs) to create synthetic data for the minority class, effectively reducing false negatives [125]. When combined with comprehensive feature engineering using MACCS keys for structural drug features and amino acid/dipeptide compositions for target properties, this approach achieved remarkable performance metrics including accuracy of 97.46% and ROC-AUC of 99.42% on BindingDB-Kd dataset [125].
The framework's robustness was validated across diverse datasets (BindingDB-Kd, BindingDB-Ki, and BindingDB-IC50), demonstrating consistent performance with ROC-AUC values exceeding 97% across all datasets [125]. This scalability across different measurement types highlights the importance of dataset diversity in comprehensive benchmarking protocols.
Benchmarking for Therapeutic Proteins and Biologics
PBPK Modeling and Machine Learning Integration
For therapeutic proteins, particularly antibodies, physiologically-based pharmacokinetic (PBPK) modeling represents the gold standard for prediction, though it faces distinct challenges compared to small molecules. Therapeutic antibody PBPK models must account for complex biological processes including FcRn-mediated recycling, endosomal trafficking, and target-mediated drug disposition [41].
Recent advances have focused on integrating machine learning with PBPK modeling to address parameter uncertainty and model complexity. ML approaches show particular promise for parameter estimation, model learning, and uncertainty quantification in these complex systems [41]. For instance, ML-influenced PBPK models have demonstrated improved accuracy in predicting biodistribution in special populations where data are limited, such as pediatric and geriatric subjects [41].
Key Considerations for Biologics Benchmarking
Benchmarking predictive models for therapeutic proteins requires attention to several unique factors:
Species-Specific Parameters: Critical physiological parameters (e.g., FcRn expression levels, endocytosis rates) can vary significantly between species and even between individuals, requiring careful translation from preclinical models [41].
Target-Mediated Disposition: Accurate prediction requires quantifying target expression levels, binding kinetics, and internalization rates, which are often tissue-specific and disease-dependent [41].
Lymphatic Transport: For subcutaneous administration, models must account for lymphatic transport mechanisms, which differ significantly from vascular distribution [41].
The complexity of PBPK models for biologics is substantially higher than for small molecules, with a full physiological model potentially requiring hundreds of parameters when accounting for all relevant tissues and processes [41].
Table 3: Key Computational Resources for Pharmacokinetic Prediction Benchmarking
| Resource | Type | Primary Application | Key Features |
|---|---|---|---|
| AssayInspector | Python package | Data consistency assessment | Identifies dataset discrepancies, outliers, and batch effects |
| RDKit | Cheminformatics library | Chemical structure handling | Molecular descriptor calculation, fingerprint generation |
| ChEMBL Database | Bioactivity database | Model training and validation | Curated bioactivity data with confidence scores |
| OPERAv2.9 | QSAR tool suite | Physicochemical property prediction | Open-source models with applicability domain assessment |
| MolTarPred | Target prediction | Drug-target interaction | Ligand-centric approach using 2D similarity |
| BindingDB | Bioactivity database | DTI model validation | Binding affinity data (Kd, Ki, IC50) |
Integrated Workflow for Comprehensive Model Benchmarking
Robust benchmarking of predictive accuracy in pharmacokinetic modeling requires integrated strategies that address data quality, methodological appropriateness, and applicability domain considerations. The case studies presented demonstrate that while substantial progress has been made across different prediction domains, systematic challenges remain—particularly regarding data consistency, model transparency, and standardized evaluation protocols.
Future advancements will likely focus on automated data curation pipelines, standardized benchmarking datasets, and explainable AI approaches that provide insight into model decisions. Additionally, as the field moves toward more complex modeling of biologics and combination therapies, benchmarking frameworks must evolve to address the escalating parameter complexity and data requirements of these advanced systems. Through continued refinement of benchmarking methodologies, the field will enhance the reliability and translational impact of in silico pharmacokinetic prediction across the therapeutic development spectrum.
The Role of Real-World Data (RWD) in Validating and Refining In Silico Predictions
The paradigm of pharmacokinetic (PK) prediction has been fundamentally transformed by the integration of in silico modeling and real-world data (RWD). In silico approaches, including physiologically based pharmacokinetic (PBPK) modeling and population pharmacokinetic (popPK) modeling, provide powerful frameworks for predicting drug behavior through computational simulation [65] [84]. However, the true validation and refinement of these models increasingly depend on RWD acquired from electronic health records, patient registries, and standard clinical practice [65]. This convergence addresses a critical challenge in drug development: the limited participation of diverse patient populations (including children, elderly individuals, pregnant women, and people with comorbidities) in traditional clinical trials [65]. This technical guide examines the integral role of RWD in verifying and enhancing in silico predictions within the context of basic pharmacokinetic principles, providing methodologies and frameworks for researchers and drug development professionals.
The fundamental value proposition of this integration lies in creating a virtuous cycle of model improvement. Initially, in silico models generate predictions based on established physiological principles and in vitro data. Subsequently, RWD collected from diverse real-world settings provides an external validation dataset that either confirms model accuracy or reveals discrepancies stemming from unaccounted physiological variabilities or disease influences [9] [126]. This iterative process progressively enhances model robustness, ultimately supporting more reliable drug development decisions and personalized dosing recommendations across heterogeneous patient populations.
Foundations of In Silico Pharmacokinetic Modeling
Key Modeling Approaches
In silico pharmacokinetic prediction primarily employs two complementary modeling frameworks: mechanistic PBPK models and data-driven popPK models. Each approach possesses distinct characteristics, applications, and dependencies on RWD.
Table 1: Fundamental In Silico Pharmacokinetic Modeling Approaches
| Model Type | Core Principle | Primary Applications | RWD Integration |
|---|---|---|---|
| Physiologically Based Pharmacokinetic (PBPK) | Uses differential equation systems to simulate drug absorption, distribution, metabolism, and excretion based on physiological parameters [65] [9] | First-in-human dose prediction, drug-drug interaction assessment, toxicokinetic projection [9] | Validation of model predictions against real-world clinical observations; refinement of physiological parameters [9] |
| Population Pharmacokinetic (PopPK) | Employs nonlinear mixed-effects (NLME) models to characterize drug concentration-time profiles across individuals, accounting for fixed and random effects [127] [38] | Identification of covariate effects (e.g., age, weight, organ function); dose optimization across subpopulations [127] [126] | Direct incorporation of patient data from clinical practice; identification of new covariates influencing drug exposure [128] [126] |
| Quantitative Systems Pharmacology (QSP) | Models biological networks and drug-target interactions to predict pharmacological effects and clinical outcomes [65] [84] | Mechanism of action evaluation; biomarker identification; prediction of efficacy and safety [65] | Linking pharmacokinetic predictions to clinical outcomes observed in real-world settings [65] |
The Model-Refinement Cycle
The continuous improvement of in silico models follows an iterative cycle of prediction, validation, and refinement. RWD serves as the critical component that grounds computational predictions in clinical reality. This cycle begins with model pre-verification using preclinical data, proceeds to initial prediction for human pharmacokinetics, followed by confrontation with RWD, and culminates in model refinement to improve future predictions [9]. This process is particularly valuable for addressing population-specific pharmacokinetic variations that may not be adequately captured in controlled clinical trials, such as those related to extreme ages, multimorbidity, polypharmacy, or rare genetic variants [65] [127].
Methodological Framework for RWD-Enabled Model Validation
External Evaluation of Population Pharmacokinetic Models
The external validation of popPK models using RWD follows a standardized methodological sequence to quantitatively assess predictive performance. A recent study on dexmedetomidine exemplifies this approach, where five published popPK models were evaluated against prospective RWD from 102 children [128]. The protocol encompasses several critical stages:
Data Collection and Curation: RWD was collected through multicenter opportunistic sampling from children receiving dexmedetomidine per standard of care [128]. This included 168 plasma concentrations from patients aged 0.01 to 19.9 years. Critical data curation steps included:
- Sample Handling: Blood collection in EDTA-K₂ Microtainers with immediate plasma processing prior to freezing [128]
- Analytical Validation: Dexmedetomidine quantification using validated HPLC-tandem mass spectroscopy with accuracy and precision within FDA bioanalytical validation criteria (LLOQ: 5 pg/mL) [128]
- Outlier Management: Application of predefined censoring criteria for dosing rates (>6.5 μg/kg/hr) and observed concentrations (>5000 pg/mL) to exclude potentially erroneous values [128]
Predictive Performance Quantification: The predictive accuracy of published models was assessed through:
- Population Predictions (PRED): Generated using only demographic and dosing information from the external validation dataset [128]
- Individual Predictions (IPRED): Obtained through POSTHOC estimation of random effects based on individual covariates and observed concentrations [128]
- Statistical Metrics: Calculation of mean percent prediction errors comparing predicted and observed values, with results ranging from -1% to 120% for PRED and -24% to 60% for IPRED across different models [128]
This systematic evaluation revealed that models developed using similar 'real-world' data (e.g., the James et al. model) demonstrated superior generalizability compared to those derived from clinical trials with restrictive inclusion criteria [128]. This highlights how RWD can expose limitations in models developed from homogenous clinical trial populations when applied to more diverse real-world patient populations.
Virtual Patient-Driven PopPK Modeling
An emerging methodology leverages PBPK-derived virtual populations to establish popPK models subsequently validated with clinical RWD. This approach was demonstrated in salbutamol popPK modeling [126]:
Virtual Population Generation:
- Covariate Selection: Creation of virtual patients with variations in age (5, 10, 20, 30, 65 years), weight (based on BMI classification), race (American, Japanese, Chinese), and gender [126]
- PBPK Simulation: GastroPlus software (Version 9.8.3) simulated PK profiles following administration of 600 μg salbutamol via dry-powder inhaler [126]
- Parameter Estimation: ADMET Predictor (Version 10.4) estimated physicochemical and PK properties, including bioavailability (Fa, FDp, F), Cmax, Tmax, and AUC [126]
Model Development and Validation:
- Structural Model Identification: Two-compartment model with first-order absorption and linear elimination best fitted the virtual data based on diagnostic plots and selection criteria (AIC, BIC) [126]
- Covariate Modeling: Stepwise identification of significant covariate-parameter relationships, revealing impacts of age on clearance (Cl) and intercompartmental clearance (Q), gender on Cl and absorption rate (ka), race on Cl, and weight on peripheral volume (V2) [126]
- External Validation: Strong agreement between model-predicted and observed values from clinical patient data confirmed model validity [126]
This hybrid methodology addresses the chronic challenge of data scarcity in popPK modeling by leveraging synthetic data from PBPK models while maintaining clinical relevance through RWD validation [126].
Experimental Protocols for Key Applications
Protocol 1: External Evaluation of Existing PopPK Models with RWD
This protocol details the external evaluation of published popPK models using a real-world dataset, based on the dexmedetomidine validation study [128]:
Step 1: Literature Search and Model Selection
- Execute systematic literature search (PubMed, Google Scholar) using structured search terms
- Apply inclusion criteria focusing on demographic similarity to validation population and model completeness
- Recapture published model structures and parameter estimates into computational code (e.g., NONMEM)
Step 2: RWD Collection and Curation
- Establish multicenter observational study with standardized opportunistic sampling
- Implement validated bioanalytical methods meeting regulatory criteria for drug quantification
- Apply predefined data censoring rules to exclude physiologically implausible values
- Document all data processing decisions for audit trail
Step 3: Model Prediction and Comparison
- Generate population predictions (PRED) using only demographic and dosing data
- Calculate individualized predictions (IPRED) using POSTHOC estimation of random effects
- Compute quantitative metrics: mean percent prediction error for bias, root mean squared error for precision
- Perform visual predictive checks and goodness-of-fit plots
Step 4: Generalizability Assessment
- Rank models by predictive performance across the real-world population
- Identify specific subpopulations where models demonstrate inadequate performance
- Evaluate clinical impact of misprediction through exposure-safety/efficacy relationships
Protocol 2: PopPK Model Development Using PBPK-Derived Virtual Populations
This protocol outlines the development of popPK models using virtual patient data with subsequent RWD validation, following the salbutamol case study [126]:
Step 1: Virtual Population Design
- Define covariate distributions reflecting target patient population diversity
- Generate virtual patients using PBPK software (GastroPlus) with systematic variation of key covariates
- Simulate PK profiles using drug-specific parameters from prediction software (ADMET Predictor)
Step 2: Noncompartmental Analysis
- Perform initial PK analysis (PKAnalix) to establish baseline parameters
- Apply linear trapezoidal method for AUC calculation
- Determine elimination rate constant (λz) via linear regression of terminal phase
Step 3: Structural Model Development
- Test one-, two-, and three-compartment models with various absorption processes
- Implement estimation via maximum likelihood using SAEM algorithm (Monolix Suite)
- Select optimal structure using objective function value (OFV), AIC, and BIC
Step 4: Covariate Model Building
- Implement stepwise covariate model building using forward inclusion/backward elimination
- Evaluate physiological plausibility of identified covariate-parameter relationships
- Validate final model using visual predictive checks and bootstrap analysis
Step 5: External Validation with Clinical RWD
- Collect targeted clinical data from representative patient population
- Compare individual predicted versus observed concentrations
- Quantify prediction accuracy through mean absolute error and relative standard errors
Quantitative Assessment of RWD in Model Evaluation
The quantitative impact of RWD in validating in silico predictions can be assessed through multiple performance metrics. Recent research has specifically evaluated whether small real-world datasets provide sufficient power for model evaluation compared to large virtual datasets [129].
Table 2: Predictive Performance Metrics for Model Evaluation with RWD vs. Virtual Data
| Evaluation Metric | Clinical RWD (N=13) | Virtual Dataset (N=1000) | Interpretation |
|---|---|---|---|
| Population Bias (%) | -37.8% | -28.4% | Consistent model misspecification direction across dataset sizes |
| Individual Bias (%) | -21.4% | -13.9% | Reduced bias with individualization in both datasets |
| Population Imprecision (%) | 43.2% | 40.2% | Similar precision despite sample size difference |
| Individual Imprecision (%) | 31.3% | 18.1% | Improved precision with individualization, more pronounced in larger dataset |
| Statistical Comparison (p-value) | >0.05 (NS) | >0.05 (NS) | No significant difference in prediction error distributions |
This comparative analysis demonstrated that small clinical datasets (N=13) could detect model misspecification with similar effectiveness to large virtual datasets (N=1000), as evidenced by consistent bias direction, comparable imprecision metrics, and similar model misspecification patterns in goodness-of-fit plots and prediction-corrected visual predictive checks [129]. This finding has significant practical implications for model evaluation, suggesting that even limited RWD can provide meaningful validation insights when collected strategically.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful integration of RWD and in silico predictions requires specialized methodological tools and computational resources. The following table catalogues essential solutions referenced in recent literature:
Table 3: Essential Research Reagent Solutions for RWD-Enhanced In Silico Modeling
| Tool Category | Representative Solutions | Function | Application Example |
|---|---|---|---|
| PBPK Platforms | GastroPlus (Simulation Plus), Simcyp Simulator | Simulate drug disposition using physiological parameters; generate virtual populations [9] [126] | Prediction of human PK prior to first-in-human studies [9] |
| PopPK Software | NONMEM, Monolix Suite, NLME | Develop population models using nonlinear mixed-effects modeling [128] [38] | Identification of covariate effects on drug exposure [128] [126] |
| Machine Learning Automation | pyDaron, Genetic Algorithms | Automated popPK model structure identification and parameter estimation [38] | Reduced model development time from weeks to <48 hours [38] |
| Bioanalytical Assays | Validated HPLC-MS/MS methods | Quantify drug concentrations in biological matrices with high sensitivity and specificity [128] | Measurement of real-world drug concentrations for model validation [128] |
| Data Processing Tools | R (tidyverse, xpose4), Python (pandas) | Data formatting, exploration, visualization, and diagnostic testing [128] [127] | Generation of goodness-of-fit plots and visual predictive checks [128] |
Visualization of Workflows and Relationships
RWD Validation Workflow for In Silico Models
Virtual Patient PopPK Development and Validation
Challenges and Future Directions
Despite the demonstrated value of RWD in enhancing in silico predictions, several methodological challenges persist. Data quality and standardization remain significant concerns, as RWD originates from diverse sources with varying collection protocols and documentation completeness [127]. The representativeness of real-world populations presents both an opportunity and challenge, as models must account for broader physiological variability while avoiding overfitting to specific subpopulations [128] [127]. Additionally, regulatory acceptance of model-informed drug development approaches based on RWD requires further demonstration of robustness and predictive accuracy [127].
Future advancements will likely focus on increased automation through machine learning and artificial intelligence. Recent developments demonstrate automated popPK model building using frameworks like pyDarwin, which can identify optimal model structures in less than 48 hours while evaluating fewer than 2.6% of possible models in the search space [38]. The integration of generative AI for creating synthetic patient data and reinforcement learning for adaptive trial design represents the next frontier in this field [130] [38]. Furthermore, the emergence of large language models for analyzing unstructured clinical notes may unlock new dimensions of RWD for model refinement [130].
As these technologies mature, the role of RWD will expand beyond validation to active model building, enabling truly personalized pharmacokinetic predictions that account for the complex interplay of demographics, genetics, comorbidities, and concomitant medications observed in real-world practice [65] [127]. This progression will ultimately enhance the precision of drug therapy across diverse patient populations, moving beyond the limitations of traditional clinical trial data.
The integration of real-world data with in silico predictions represents a fundamental advancement in pharmacokinetic science. Through methodical external evaluation, virtual population modeling, and iterative refinement, RWD transforms computational predictions from theoretical exercises to clinically relevant tools. The methodologies and protocols outlined in this technical guide provide a framework for researchers to leverage this powerful combination, ultimately advancing more personalized and effective drug therapies. As artificial intelligence and automation technologies continue to evolve, the synergy between in silico modeling and real-world evidence will undoubtedly become increasingly central to drug development and precision medicine.
In silico research in pharmacokinetics aims to predict the complex behavior of drug compounds within the human body, encompassing absorption, distribution, metabolism, and excretion (ADME) processes. The reliability of these predictions directly impacts drug development timelines, resource allocation, and ultimately patient safety. Model evaluation therefore transcends mere technical exercise—it forms the foundation for credible, actionable scientific insights in drug development. Without rigorous assessment of predictive accuracy and robustness, computational models offer little value for critical decisions in the drug development pipeline.
The fundamental challenge in pharmacokinetic prediction lies in bridging multiple scales of complexity—from molecular interactions to whole-body physiological outcomes—while acknowledging and quantifying inevitable uncertainty. This whitepaper establishes a comprehensive framework for evaluating model performance within this context, providing researchers and drug development professionals with standardized methodologies to assess predictive accuracy and robustness, thereby enhancing the credibility and utility of in silico pharmacokinetic research.
Core Evaluation Metrics for Predictive Modeling
The selection of evaluation metrics must align with the specific modeling task—classification to categorize compounds (e.g., high vs. low permeability) or regression to predict continuous parameters (e.g., clearance rates, volume of distribution). No single metric provides a complete picture of model performance; a multifaceted approach is essential for a holistic assessment.
Metrics for Classification Models
Classification models in pharmacokinetics may be used to predict categorical outcomes such as a drug's likelihood of exhibiting high oral absorption or its potential for being a substrate of a specific metabolic enzyme. The following metrics, derived from the confusion matrix—a tabular visualization of model predictions against ground truth—are essential for evaluation [131] [132] [133].
Table 1: Core Evaluation Metrics for Classification Models
| Metric | Formula | Interpretation & Use Case in PK |
|---|---|---|
| Accuracy | (TP+TN)/(TP+TN+FP+FN) | Overall correctness. Best for balanced datasets where false positives and false negatives are equally important. |
| Precision | TP/(TP+FP) | Measures model's reliability when it predicts a positive class. Crucial when false positives are costly (e.g., incorrectly predicting a drug is non-toxic). |
| Recall (Sensitivity) | TP/(TP+FN) | Measures ability to identify all relevant positives. Vital when false negatives are costly (e.g., failing to flag a potentially hepatotoxic drug). |
| Specificity | TN/(TN+FP) | Measures ability to identify true negatives. Important for ruling out non-effectors (e.g., confirming a drug is not a CYP inhibitor). |
| F1-Score | 2 × (Precision×Recall)/(Precision+Recall) | Harmonic mean of precision and recall. Useful when seeking a balance between the two, especially with imbalanced datasets. |
| AUC-ROC | Area under the ROC curve | Measures the model's ability to distinguish between classes across all classification thresholds. A value of 1 indicates perfect separation. |
Beyond these core metrics, the Fβ-score provides flexibility, allowing researchers to assign relative importance (β times more) to recall over precision, which is valuable when the costs of false negatives and false positives are asymmetric [132]. Similarly, Cohen's Kappa and Matthews Correlation Coefficient (MCC) are insightful for imbalanced datasets, as they measure agreement between predictions and reality that accounts for chance [134].
Metrics for Regression Models
Regression tasks are central to pharmacokinetics, used for predicting continuous parameters like clearance (CL) and volume of distribution (Vss). These metrics quantify the error between predicted and observed values [131] [135] [136].
Table 2: Core Evaluation Metrics for Regression Models
| Metric | Formula | Interpretation & Use Case in PK |
|---|---|---|
| Mean Absolute Error (MAE) | (1/N) ∑⎮yj - ŷj⎮ | Average magnitude of error, robust to outliers. Interpreted in the original units of the parameter (e.g., L/h for clearance). |
| Mean Squared Error (MSE) | (1/N) ∑(yj - ŷj)² | Average of squared errors. Penalizes larger errors more heavily, useful when large errors are highly undesirable. |
| Root Mean Squared Error (RMSE) | √MSE | Square root of MSE. Interpretable in the original units of the data, but remains sensitive to outliers. |
| R-squared (R²) | 1 - [∑(yj - ŷj)² / ∑(y_j - ȳ)²] | Proportion of variance in the observed data that is explained by the model. Ranges from -∞ to 1, where 1 indicates perfect prediction. |
For models predicting parameters that span orders of magnitude (e.g., drug concentration), Root Mean Squared Logarithmic Error (RMSLE) can be preferable as it is less sensitive to outliers and penalizes underestimates more than overestimates [131].
Advanced Considerations for Robustness and Validation
Assessing Model Robustness
A model with high predictive accuracy on a static test set may still fail in real-world applications if it is not robust. Robustness refers to a model's ability to maintain stable performance when faced with perturbations, noise, or shifts in input data [137]. For pharmacokinetic models, such perturbations could arise from biological variability, differences in experimental protocols, or unanticipated drug-drug interactions.
The ISO/IEC TR 24029-1 standard provides a framework for assessing the robustness of neural networks, a concept applicable to many machine learning models. It categorizes perturbations and suggests evaluation strategies, including sensitivity analysis and stress testing under various conditions like data distribution shifts or adversarial inputs [137]. Key robustness metrics include measuring the change in accuracy or the stability of output confidence under these perturbed conditions.
Statistical Testing for Model Comparison
When comparing the performance of different models, it is not sufficient to merely observe differences in metric values; one must determine if these differences are statistically significant. Standard practice involves using a held-out test set to generate multiple performance estimates (e.g., via bootstrapping or cross-validation) [134].
Subsequently, statistical tests are applied to these estimates. For comparing two models, appropriate tests include the paired t-test (under normality assumptions) or the non-parametric Wilcoxon signed-rank test. For comparing multiple models, tests like repeated measures ANOVA or the Friedman test are recommended, followed by post-hoc analysis [134]. It is critical that the test set is never used for model training or threshold tuning, as this would invalidate the results and produce overly optimistic performance estimates [134].
Experimental Protocols for Model Evaluation
A standardized, rigorous experimental protocol is fundamental to generating credible and reproducible evaluation results.
Core Evaluation Workflow
The following workflow outlines the essential steps for a robust model evaluation, from initial data preparation to final performance reporting.
Protocol 1: Hold-Out Test Set Validation
This is the foundational protocol for evaluating a finalized model.
- Data Splitting: Randomly split the entire dataset into three parts: a training set (e.g., 70%), a validation set (e.g., 15%), and a held-out test set (e.g., 15%). The test set must be locked away and not used in any part of model training or tuning [134].
- Model Training & Tuning: Train the model on the training set. Use the validation set to tune hyperparameters, including the classification threshold. The optimal threshold might be chosen to maximize accuracy or Youden's index (Sensitivity + Specificity - 1) [134].
- Final Evaluation: Use the finalized model and the chosen threshold to make predictions on the held-out test set. Calculate all relevant evaluation metrics (from Tables 1 & 2) using these predictions.
- Robustness Check (Optional): Introduce controlled perturbations (e.g., noise, simulated biological variability) to the test set inputs and recalculate metrics to assess robustness [137].
Protocol 2: k-Fold Cross-Validation for Algorithm Selection
This protocol is preferred for smaller datasets or for comparing the general performance of different modeling algorithms.
- Data Preparation: Randomly shuffle the dataset and split it into k equally sized folds (common choices are k=5 or k=10).
- Iterative Training & Validation: For each unique fold
i(where i=1 to k):- Designate fold
ias the validation set. - Train the model on the remaining k-1 folds.
- Use the trained model to predict the held-out fold
iand calculate the desired metrics.
- Designate fold
- Performance Aggregation: Average the metric values obtained from the k iterations to produce a single, robust estimate of the model's performance. The standard deviation of these metrics can also be reported to indicate performance stability.
The following tools and resources are fundamental for conducting rigorous model evaluation in pharmacokinetic research.
Table 3: Key Research Reagent Solutions for Model Evaluation
| Tool / Resource | Function / Purpose | Application Example |
|---|---|---|
| Scikit-learn | A comprehensive open-source library for machine learning in Python. | Provides functions for calculating all standard metrics (accuracy, precision, MSE, R²), splitting datasets, and performing cross-validation [135]. |
| Physiologically Based Pharmacokinetic (PBPK) Modeling Software (e.g., GastroPlus) | A mechanism-driven framework to predict ADME by incorporating human physiology, drug properties, and trial design. | Used to simulate and predict human pharmacokinetics, allowing for the comparison of simulated vs. observed clinical data to validate the model [138]. |
| In vitro-in vivo extrapolation (IVIVE) | A methodology to translate data from in vitro experiments (e.g., metabolic clearance in human liver microsomes) into predictions of in vivo pharmacokinetic parameters [138]. | Used to predict human hepatic clearance (CL) and absorption rate constants (ka), forming the basis for many PBPK model inputs. |
| Allometric Scaling | A technique using anatomical and physiological similarities across species to extrapolate animal PK data to predict human PK parameters [138]. | Used to predict human clearance and volume of distribution from preclinical animal data, providing an initial estimate for first-in-human studies. |
| Neptune.ai | A platform for experiment tracking and model metadata management. | Logs, visualizes, and compares metrics from hundreds of model training and evaluation runs, ensuring reproducibility [136]. |
The rigorous evaluation of predictive models is a non-negotiable standard in modern, model-informed drug development. By systematically applying the appropriate metrics for classification and regression, adhering to robust experimental protocols that clearly separate training from testing data, and quantitatively assessing model robustness, researchers can build confidence in their in silico predictions. This disciplined approach to model evaluation ensures that computational insights are reliable, actionable, and capable of accelerating the development of safe and effective therapeutics.
Conclusion
In silico pharmacokinetic prediction represents a paradigm shift in modern drug development, integrating mechanistic PBPK modeling with advanced AI and machine learning to create more predictive, efficient workflows. The synthesis of these approaches allows researchers to navigate biological complexity, address data gaps, and generate reliable predictions from molecular structure to clinical outcome. As these technologies mature, they promise to further reduce reliance on traditional experimental models, accelerate development timelines, and enable more personalized therapeutic strategies. The future of PK prediction lies in the continued refinement of hybrid models, the expansion of virtual population simulations, and the deeper integration of real-world evidence, ultimately leading to safer, more effective medicines reaching patients faster.
References
- 1. Physiologically based pharmacokinetic modelling - Wikipedia [https://en.wikipedia.org/wiki/Physiologically_based_pharmacokinetic_modelling]
- 2. Applied Concepts in PBPK : How to Build a Modeling /PD PBPK ... Model [https://pmc.ncbi.nlm.nih.gov/articles/PMC5080648/]
- 3. Appendix C PBPK | Human Biomonitoring for Environmental... Modeling [https://nap.nationalacademies.org/read/11700/chapter/12]
- 4. Principles of PBPK | Open Systems Pharmacology Modeling [https://docs.open-systems-pharmacology.org/mechanistic-modeling-of-pharmacokinetics-and-dynamics/modeling-concepts/principles-of-pbpk-modeling]
- 5. predictive pharmacokinetic insights in humans [https://link.springer.com/article/10.1007/s44446-025-00024-4]
- 6. Physiologically-based Pharmacokinetic Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC5204363/]
- 7. PBPK Modeling and Simulation and Therapeutic Drug ... [https://www.mdpi.com/2227-9717/9/11/2087]
- 8. In Silico Prediction of Pharmacokinetic Profile for Human Oral ... [https://pubmed.ncbi.nlm.nih.gov/35171461/]
- 9. Real-world application of physiologically based ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624148556]
- 10. Courses - Simulations Plus [https://www.simulations-plus.com/courses/introduction-to-pbpk-modeling-bundle/]
- 11. Pharmacokinetics - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK557744/]
- 12. ADME [https://en.wikipedia.org/wiki/ADME]
- 13. Pharmacokinetics: Definition & Use in Drug Development [https://www.allucent.com/resources/blog/what-pharmacokinetics-and-adme]
- 14. In Silico ADME Methods Used in the Evaluation of Natural ... [https://pubmed.ncbi.nlm.nih.gov/40871023/]
- 15. Introduction to Pharmacokinetics: Four Steps in a Drug's ... [https://genomind.com/providers/introduction-to-pharmacokinetics-four-steps-in-a-drugs-journey-through-the-body/]
- 16. Chapter 1 Pharmacokinetics & Pharmacodynamics - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK595006/]
- 17. ADME Optimisation 2025 | Accelerate Drug Development [https://www.pharmaron.com/pharmaron-stories/adme-optimisation-2025/]
- 18. Interpreting PK analysis with data visualization [https://www.linkedin.com/pulse/interpreting-pk-analysis-data-visualization-algorics]
- 19. Visualization and Communication of Pharmacometric Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4055786/]
- 20. Pharmacokinetic Modeling and Visualization Tool [https://peytoncchen.github.io/PK-Visualization/]
- 21. Prediction of plasma concentration-time profiles in mice ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325004454]
- 22. Quantitative Structure-Activity Relationship (QSAR) [https://www.archivemarketresearch.com/reports/quantitative-structure-activity-relationship-qsar-45561]
- 23. How Quantitative Structure-Activity Relationship (QSAR) ... [https://www.linkedin.com/pulse/how-quantitative-structure-activity-relationship-qsar-ipvne/]
- 24. Prediction Model of Clearance by a Novel Quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8444299/]
- 25. An In Silico Study Based on QSAR and Molecular Docking ... [https://www.mdpi.com/1424-8247/17/7/830]
- 26. A comprehensive in-silico approach (pharmacophoric ... [https://www.sciencedirect.com/science/article/pii/S157018082500017X]
- 27. QSAR, molecular docking and ADMET properties in silico ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8282965/]
- 28. model validation, human pharmacokinetic prediction and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1692293/full]
- 29. Machine learning framework to predict pharmacokinetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11097621/]
- 30. Compartmental modeling in the analysis of biological systems [https://pubmed.ncbi.nlm.nih.gov/23007439/]
- 31. The Use of Physiologically Based Pharmacokinetic Analyses-in... [https://pubmed.ncbi.nlm.nih.gov/35585448/]
- 32. Actionable predictions of human pharmacokinetics at the ... [https://chemrxiv.org/engage/chemrxiv/article-details/65e5cb489138d23161a40164]
- 33. A computational dynamic systems model for in silico ... [https://www.sciencedirect.com/science/article/pii/S2666027X2400063X]
- 34. In silico Methods for Identification of Potential Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8616973/]
- 35. In Silico & Data Insights - Instem [https://www.instem.com/solutions/in-silico/]
- 36. A Comparative Analysis of NONMEM and AI-based Models ... [https://pubmed.ncbi.nlm.nih.gov/41254220/]
- 37. Machine Learning for PK/PD Modeling in Drug Development [https://www.certara.com/blog/machine-learning-for-pk-pd-modeling-in-drug-development/]
- 38. A machine learning approach to population ... [https://www.nature.com/articles/s43856-025-01054-8]
- 39. Pharmacology and artificial intelligence A new chapter in ... [https://www.sciencedirect.com/science/article/pii/S0040595725001088]
- 40. Overcoming PK/PD Modeling Challenges [https://www.pharmtech.com/view/overcoming-pk-pd-modeling-challenges]
- 41. Opportunities for machine learning and artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12573771/]
- 42. Opportunities for machine learning and artificial ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X25002017]
- 43. Advances in machine learning for optimizing ... [https://www.sciencedirect.com/science/article/pii/S1570164625000153]
- 44. Artificial Intelligence in Clinical and Translational Science [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580936/]
- 45. Basic Concepts in Physiologically Based Pharmacokinetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3828005/]
- 46. The Evolution and Future Directions of PBPK Modeling in ... [https://www.mdpi.com/1999-4923/17/11/1413]
- 47. Application of Physiologically-Based Pharmacokinetic (PBPK ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12334468/]
- 48. Predictive Performance of Physiologically Based ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624009681]
- 49. Using Confidence Intervals to Support ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10954928/]
- 50. Physiologically Based Pharmacokinetic Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541349/]
- 51. Investigating the uncertainty of prediction accuracy for ... [https://www.sciencedirect.com/science/article/pii/S0273230022001490]
- 52. High-performance PBPK model for predicting CYP3A4 ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1521068/full]
- 53. LSTM-Based Prediction of Human PK Profiles and Parameters for... [https://pubmed.ncbi.nlm.nih.gov/41147737/]
- 54. In Silico ADME Methods Used in the Evaluation of... | Preprints.org [https://www.preprints.org/manuscript/202501.2308/v1]
- 55. Enhancing molecular property prediction through data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574261/]
- 56. Predicting Pharmacokinetics in Rats Using Machine Learning [https://pubmed.ncbi.nlm.nih.gov/40091606/]
- 57. The ABCD of clinical pharmacokinetics - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4110820/]
- 58. New Features and Updates | ADME Suite Version 2025 [https://www.acdlabs.com/technical-support/current-software-versions/adme-suite/]
- 59. In silico evaluation of pharmacokinetic properties and ... [https://www.sciencedirect.com/science/article/pii/S1476927125002877]
- 60. Playbook workflow builder: Interactive construction of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11967941/]
- 61. Prediction of pharmacokinetic/pharmacodynamic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1578117/full]
- 62. The Emerging Role of Aldosterone Synthase Inhibitors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12400170/]
- 63. The future of pharmaceuticals: Artificial intelligence in drug ... [https://www.sciencedirect.com/science/article/pii/S2095177925000656]
- 64. Prediction of pharmacokinetic/pharmacodynamic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12066422/]
- 65. Leveraging In Silico and Artificial Intelligence Models to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180087/]
- 66. Curated CYP450 Interaction Dataset: Covering the Majority ... [https://www.nature.com/articles/s41597-025-05753-8]
- 67. A Review on New Frontiers in Drug-Drug Interaction ... [https://www.mdpi.com/1999-4923/17/6/747]
- 68. FDA's Examples of Drugs that Interact with CYP Enzymes ... [https://www.fda.gov/drugs/drug-interactions-labeling/healthcare-professionals-fdas-examples-drugs-interact-cyp-enzymes-and-transporter-systems]
- 69. In Silico Prediction of Drug–Drug Interactions Mediated by Cytochrome P450 Isoforms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8068971/]
- 70. Predictive Modelling in pharmacokinetics: from in-silico simulations to personalized medicine - PubMed [https://pubmed.ncbi.nlm.nih.gov/38480460/]
- 71. Pharmaceuticals | Special Issue : The Prediction of Pharmacokinetics/Pharmacodynamics Using In-Silico Modeling [https://www.mdpi.com/journal/pharmaceuticals/special_issues/Pharmacokinetics_Pharmacodynamics_Modeling]
- 72. [Advancing Drug Interaction Management Based on the ... [https://pubmed.ncbi.nlm.nih.gov/41183870/]
- 73. A practical guide for the generation of model-based virtual ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2023.1174647/full]
- 74. Methods to Develop an in silico Clinical Trial [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2021.741170/full]
- 75. In Silico Re-Optimization of Atezolizumab Dosing using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10175103/]
- 76. Emulation of Quantitative Systems Pharmacology models ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202323002177]
- 77. Pharmacometric in silico studies used to facilitate a ... [https://smw.ch/index.php/smw/article/view/3632]
- 78. Simulation of clinical trials of oral treprostinil in pulmonary ... [https://www.nature.com/articles/s41540-024-00481-y]
- 79. Clinical Trial Simulation to Evaluate Population ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4568821/]
- 80. Opportunities for using in silico‐based extended dosing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7444775/]
- 81. Dealing with Uncertainty in Pharmacokinetic Models Using ... [https://www.ncbi.nlm.nih.gov/books/NBK218074/]
- 82. Simulating your pharmacometric model with parameter ... [https://www.pmxsolutions.com/2019/01/31/how-to-simulate-your-pharmacometric-model-with-parameter-uncertainty/]
- 83. Introduction to Pharmacokinetic Modeling Methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3636497/]
- 84. Modeling Approaches for Determination of ... [https://www.biopharminternational.com/view/modeling-approaches-for-determination-of-pharmacokinetics-pharmacodynamics]
- 85. Pharmacokinetic Model Comparisons: How We Do It and Why ... [https://blog.insight-rx.com/resources/pharmacokinetic-model-comparisons-methods]
- 86. In Silico Pharmacokinetic and Pharmacodynamic (PK-PD) ... [https://www.mdpi.com/journal/pharmaceutics/special_issues/26SP16RBQI]
- 87. Understanding the complexity of computational models ... [https://www.sciencedirect.com/science/article/pii/S0749596X23000670]
- 88. Multi-Level Progressive Parameter Optimization Method for ... [https://www.mdpi.com/2227-9717/13/7/1993]
- 89. Hyperparameter Optimization at Scale: Strategies for Large ... [https://medium.com/@zhonghong9998/hyperparameter-optimization-at-scale-strategies-for-large-scale-experiments-8e59e1525c9a]
- 90. Parameter-Efficient Fine-Tuning for Large Models [https://arxiv.org/html/2403.14608v1]
- 91. How to formulate model parameter optimization strategy ... [https://www.tencentcloud.com/techpedia/121446]
- 92. In silico approaches which are used in pharmacy [https://japsonline.com/abstract.php?article_id=4213&sts=2]
- 93. Automating Population Pharmacokinetic Model ... [https://www.page-meeting.org/default.asp?abstract=10877]
- 94. Application of machine learning combined with population ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1352113/full]
- 95. The Trends and Future Prospective of In Silico Models from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10675155/]
- 96. Opportunities and challenges of physiologically based ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622001611]
- 97. Application of Physiologically-Based Pharmacokinetic ... [https://link.springer.com/article/10.1007/s40495-025-00427-w]
- 98. Comparing computational times for simulations when using ... [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2025.1518769/full]
- 99. The Evolution and Future Directions of PBPK Modeling in FDA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12655628/]
- 100. Applications, Challenges, and Outlook for PBPK Modeling ... [https://pubmed.ncbi.nlm.nih.gov/35552967/]
- 101. Optimization of Bottom‐Up PBPK Model Development in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631063/]
- 102. A PBPK modeling approach for personalized dose ... [https://www.nature.com/articles/s41598-025-03829-4]
- 103. The Perks and Drawbacks of Physiologically-Based ... [https://esmed.org/MRA/mra/article/view/2944]
- 104. Integrating artificial intelligence for design, optimization ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224725012080]
- 105. Challenges Associated With Applying Physiologically Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6084449/]
- 106. Novel Drug Delivery Systems: An Important Direction for Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11124876/]
- 107. Current advanced drug delivery systems: Challenges and ... [https://www.sciencedirect.com/science/article/pii/S1773224722006384]
- 108. Formulation Strategies, Tech Advances, Challenges, and ... [https://www.biopharminternational.com/view/formulation-strategies-tech-advances-challenges-and-considerations-in-novel-drug-delivery]
- 109. Advances in drug delivery systems, challenges and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10320272/]
- 110. Overcoming challenges in the design of drug delivery systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11703128/]
- 111. Overcoming Formulation Challenges in Generic Drug ... [https://www.drugpatentwatch.com/blog/overcoming-formulation-challenges-in-generic-drug-development/?srsltid=AfmBOoqqi9RbFlwv27kSYbxhech8z1lJp2lHkHYf2VCxMyoetH3WEMoj]
- 112. In Silico Research Is Rewriting the Rules of Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12070237/]
- 113. Implementing Alternative Methods [https://www.fda.gov/science-research/advancing-alternative-methods-fda/implementing-alternative-methods]
- 114. Tutorial on model selection and validation of model input into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10725261/]
- 115. Calibration Verification Criteria for Acceptable Performance [https://www.westgard.com/lessons/basic-method-validation/cal-verification-criteria.html]
- 116. Pharmaceutical Calibration Compliance Guide | Ensure GMP ... [https://ips-us.com/pharmaceutical-industry-calibration-compliance-a-complete-guide/]
- 117. Development and validation of a population ... [https://www.sciencedirect.com/science/article/pii/S2950133424000831]
- 118. Model Validation Best Practices [https://www.graemegroup.org/model-validation-best-practices/]
- 119. Methodological Techniques Used in Machine Learning to ... [https://pubmed.ncbi.nlm.nih.gov/40810920/]
- 120. An artificial intelligence-assisted physiologically-based ... [https://www.sciencedirect.com/science/article/pii/S0168365923004649]
- 121. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 122. Physiologically based pharmacokinetic modeling of small ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624148532]
- 123. Comprehensive benchmarking of computational tools for ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-024-00931-z]
- 124. A precise comparison of molecular target prediction methods [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d5dd00199d]
- 125. Predicting drug-target interactions using machine learning ... [https://www.nature.com/articles/s41598-025-03932-6]
- 126. Toward Personalized Salbutamol Therapy: Validating ... [https://www.mdpi.com/1999-4923/16/7/881]
- 127. Recommended approaches for integration of population ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11992666/]
- 128. Using Real-World Data to Externally Evaluate Population ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11286355/]
- 129. Population Pharmacokinetic Model Evaluation with a Small ... [https://pubmed.ncbi.nlm.nih.gov/40730936/]
- 130. Tech, ML and AI: Industry predictions for 2025 [https://www.ddw-online.com/tech-ml-and-ai-industry-predictions-for-2025-33318-202501/]
- 131. Evaluation Metrics in Machine Learning [https://www.geeksforgeeks.org/machine-learning/metrics-for-machine-learning-model/]
- 132. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 133. Classification: Accuracy, recall, precision, and related metrics [https://developers.google.com/machine-learning/crash-course/classification/accuracy-precision-recall]
- 134. Evaluation metrics and statistical tests for machine learning [https://www.nature.com/articles/s41598-024-56706-x]
- 135. AI指标数据分析:模型性能评估与数据处理方法 [https://www.dtstack.com/bbs/article/191790]
- 136. Performance Metrics in Machine Learning [Complete Guide] [https://neptune.ai/blog/performance-metrics-in-machine-learning-complete-guide]
- 137. ISO/IEC TR 24029-1:神经网络鲁棒性评估——概述 [https://sgsystemsglobal.com/zh-CN/%E8%AF%8D%E6%B1%87%E8%A1%A8/ISO-IEC-TR-24029-1-%E7%A5%9E%E7%BB%8F%E7%BD%91%E7%BB%9C%E7%9A%84%E9%B2%81%E6%A3%92%E6%80%A7/]
- 138. 小分子化合物人体药代动力学参数预测的方法及应用 [https://dmpkservice.wuxiapptec.com/cn/blogs/456-id/]