From Lab to Real World: 7 Data-Centric Strategies to Boost AI Model Transferability in Drug Development
This article provides a strategic roadmap for researchers and drug development professionals to enhance the performance and reliability of AI/ML models when applied to real-world industry data.
From Lab to Real World: 7 Data-Centric Strategies to Boost AI Model Transferability in Drug Development
Abstract
This article provides a strategic roadmap for researchers and drug development professionals to enhance the performance and reliability of AI/ML models when applied to real-world industry data. Covering the full model lifecycle—from foundational data strategies and modern methodological approaches like Small Language Models (SLMs) and MLOps to troubleshooting for common deployment challenges and rigorous validation frameworks—it offers actionable insights to bridge the gap between experimental research and industrial application. Readers will learn how to implement a 'Fit-for-Purpose' modeling approach, leverage expert-in-the-loop evaluation, and navigate the technical and organizational hurdles critical for successful model transferability in biomedical research.
Laying the Groundwork: Understanding Data and Domain Challenges in Industrial AI
Troubleshooting Guide: Common Model Transferability Failures and Solutions
This guide addresses specific, high-stakes challenges you may encounter when transferring computational or experimental models from development to real-world industry applications.
1. Problem: My model, which had super-human clinical performance at its training site, performs substantially worse at new validation sites.
- Underlying Cause: This is a classic failure to transport, often resulting from differences in the multivariate data distribution between your training dataset and the application dataset at the new site [1]. This can be due to site-specific clinical practices, variations in disease prevalence, or differences in data collection protocols.
- Troubleshooting Steps:
- Audit Data Definitions: Meticulously verify that the prediction target and all input variables are defined identically between the original and new sites. A subtle difference in the sepsis label definition, for example, was a key reason for the performance drop of a commercial sepsis prediction model [1].
- Check for Information Leaks: Scrutinize your training data for information that would not be available at the time of prediction in a real-world setting. This includes data generated after the clinical event or using the full length of a hospital admission to construct negative instances [1].
- Quantify the Shift: Use metrics like the transfer ratio (( R^t{\mathrm{transfer}} = \frac{\text{Performance}{\mathrm{real}}}{\text{Performance}_{\mathrm{ideal}}} )) to measure the performance drop between your ideal (training) and real-world (application) environments [2].
2. Problem: A cell line model predicts drug response with high accuracy but fails to predict patient outcomes.
- Underlying Cause: This is a fundamental translational challenge. Cell line models are trained on in vitro data that lacks the complexity of the human body, including the immune system and tumor micro-environment [3]. A model perfect for one context may be learning noise or patterns irrelevant to human biology.
- Troubleshooting Steps:
- Systematic Pipeline Scan: Don't just optimize one part of your model. Systematically test different combinations of data preprocessing, feature selection, and algorithm choices. Research has shown that scanning thousands of pipeline combinations can reveal optimal, robust settings for patient data prediction [3].
- Incorporate Homogenization: Use batch-effect correction methods like Remove Unwanted Variation (RUV) or ComBat to bridge the genomic differences between in vitro cell line data and in vivo patient data [3].
- Validate Across Multiple Datasets: A model that performs perfectly on one patient dataset may fail on another. Always validate your translational model on multiple, independent patient cohorts to ensure its robustness and clinical relevance [3].
3. Problem: My model trained on synthetic or simulated data does not generalize to real-world data (the "sim-to-real" gap).
- Underlying Cause: The synthetic data does not fully capture the uncontrolled variability, noise, and complex distributional shifts present in real-world data [2].
- Troubleshooting Steps:
- Implement Hybrid Training: Combine synthetic pre-training with targeted fine-tuning on a modest set of real-world data. This leverages the scalability of synthetic data while anchoring the model in reality [2].
- Use Domain Randomization: During training, randomize parameters in your simulations (e.g., lighting, textures, noise levels). This teaches the model to learn invariances and become more robust to the variations it will encounter in real life [2].
- Apply Blockwise Transfer: For complex models like Graph Neural Networks (GNNs), use a blockwise transfer approach: freeze general low-level encodings learned from synthetic data, and only fine-tune the higher-level, task-specific layers with a small amount of real data. This can reduce error (MAPE) by up to 88% with minimal real data [2].
4. Problem: I need to adapt an existing model to a new context but have very limited local data.
- Underlying Cause: Developing a new model from scratch is not feasible, but a general model lacks local specificity.
- Troubleshooting Steps:
- Structured Model Adaptation: Follow a formal guideline for model adaptation [4]:
- Step 1: Revision & Design: Collaborate with domain experts to assess the general model's structure and identify which components (e.g., conditional probability tables in a Bayesian network) need adjustment for the new context.
- Step 2: Knowledge Acquisition: Gather all available information for the new context, including limited local data, peer-reviewed literature, and expert knowledge.
- Step 3: Parameterization: Use techniques like linguistic labels or scenario-based elicitation to formally incorporate expert knowledge and update the model's parameters for the new site [4].
- Structured Model Adaptation: Follow a formal guideline for model adaptation [4]:
Frequently Asked Questions (FAQs)
Q1: How does transfer learning differ from traditional machine learning in this context? A: Traditional machine learning trains a new model from scratch for every task, requiring large, labeled datasets. Transfer learning reuses a pre-trained model as a starting point for a new, related task. This leverages prior knowledge, significantly reducing computational resources, time, and the amount of data needed, which is crucial for drug development where real patient data can be scarce and expensive [5].
Q2: What is "negative transfer" and how can I avoid it? A: Negative transfer occurs when knowledge from a source task adversely affects performance on the target task. This typically happens when the source and target tasks are too dissimilar [5]. To avoid it, carefully evaluate the similarity between your original model's context and the new application context. Do not assume all tasks are transferable. Using hybrid modeling approaches that incorporate mechanistic knowledge can also make models more robust to such failures [6].
Q3: Are there specific modeling techniques that enhance transferability? A: Yes, hybrid modeling (or grey-box modeling) combines mechanistic understanding with data-driven approaches. For example, a hybrid model developed for a Chinese hamster ovary (CHO) cell bioprocess was successfully transferred from shake flask (300 mL) to a 15 L bioreactor scale (a 1:50 scale-up) with low error, demonstrating excellent transferability by leveraging known bioprocess mechanics [6]. Intensified Design of Experiments (iDoE), which introduces parameter shifts within a single experiment, can also provide more process information faster and build more robust models [6].
Q4: What are the ethical considerations in model transferability? A: Using pre-trained models raises questions about the origin, bias, and ethical use of the original training data. It is critical to ensure that models are transparent and that their use complies with ethical and legal standards. Furthermore, a model that fails to transport could lead to incorrect clinical decisions, highlighting the need for rigorous validation and transparency about a model's limitations and intended use case [5] [1].
Experimental Protocols for Enhancing Transferability
Protocol 1: Implementing a Hybrid Modeling and iDoE Workflow
This methodology reduces experimental burden while building transferable models for bioprocess development [6].
- Experimental Design: Define a design space with Critical Process Parameters (CPPs), such as cultivation temperature and feed glucose concentration, at multiple levels.
- Intensified DoE (iDoE) Execution: Perform experiments where intra-experimental shifts of CPPs are introduced. This characterizes multiple CPP combinations within one run, maximizing information output on cell rates (growth, consumption, formation).
- Data Collection: At a small scale (e.g., shake flasks), collect high-frequency data on process responses (e.g., viable cell concentration - VCC, product titer).
- Hybrid Model Building: Develop a model that integrates mechanistic equations (e.g., for cell growth) with data-driven components (e.g., artificial neural networks to model complex, non-linear relationships between CPPs and specific rates).
- Model Transfer and Validation: Apply the hybrid model, without re-calibration, to predict process outcomes at a larger scale (e.g., 15 L bioreactor). Validate model predictions (VCC, titer) against new experimental data from the larger scale using metrics like Normalized Root Mean Square Error (NRMSE).
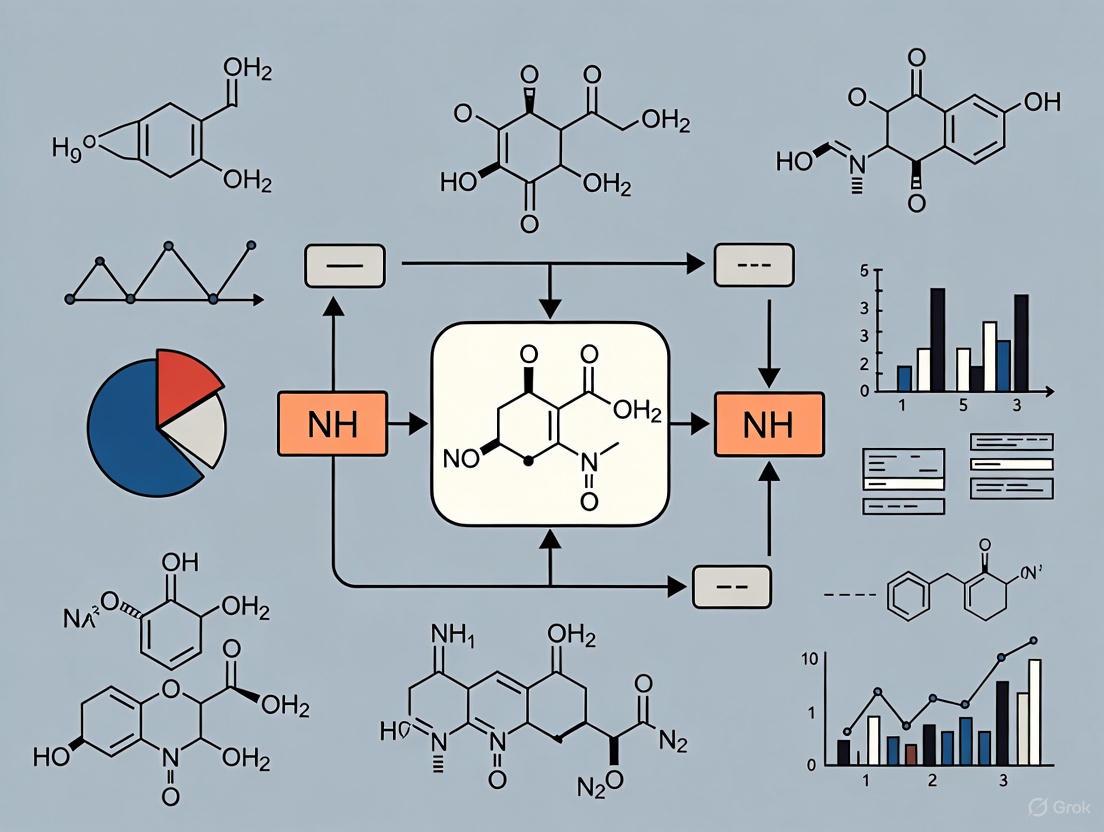
The workflow for this protocol is illustrated below:
Protocol 2: Systematic Pipeline Scanning for Translational Robustness
This protocol ensures models are robust across different patient datasets, moving beyond single-dataset optimization [3].
- Data Compilation: Gather relevant in vitro (e.g., cell line drug screening - GDSC) and in vivo (patient tumor) datasets.
- Pipeline Component Definition: Define multiple options for each step of the modeling pipeline:
- Cell Response Preprocessing: e.g., none, logarithm, power transform, k-means binarization.
- Homogenization/Batch Correction: e.g., none, RUV, ComBat, limma, YuGene.
- Feature Selection: e.g., all features, landmark genes, p-value filter.
- Feature Preprocessing: e.g., none, z-score, PCA.
- Algorithm: e.g., linear regression, lasso, elastic net, random forest (rf), SVM.
- Automated Pipeline Execution: Use a framework (e.g., the FORESEE R-package) to automatically train and evaluate models for all possible combinations of these components.
- Multi-Dataset Validation: Evaluate the performance (e.g., AUC of ROC) of every pipeline combination on multiple, independent patient datasets.
- Model Selection: Identify the pipeline that demonstrates consistently high performance across all validation datasets, rather than just performing best on one.
The following diagram maps the decision points in this systematic approach:
Quantitative Performance Data
The table below summarizes experimental results that demonstrate the impact of different strategies on model transferability.
Table 1: Quantifying Transferability in Experimental Models
| Model / Strategy | Source Context | Target Context | Performance Metric | Result | Key Insight |
|---|---|---|---|---|---|
| Hybrid Model with iDoE [6] | Shake Flask (300 mL) | 15 L Bioreactor (1:50 scale) | NRMSE (Viable Cell Density) | 10.92% | Combining mechanistic knowledge (hybrid) with information-rich data (iDoE) enables successful scale-up. |
| Hybrid Model with iDoE [6] | Shake Flask (300 mL) | 15 L Bioreactor (1:50 scale) | NRMSE (Product Titer) | 17.79% | |
| Systematic Pipeline Scan [3] | GDSC Cell Lines & Various Preprocessing | Breast Cancer Patients (GSE6434) | AUC of ROC | 0.986 (Best Pipeline) | Systematically testing modeling components, rather than relying on a single best practice, can yield near-perfect performance on a specific dataset. |
| Blockwise GNN Transfer [2] | Synthetic Network Data | Real-World Network Data | Mean Absolute Percentage Error (MAPE) | Reduction up to 88% | Transferring pre-trained model components and fine-tuning only specific layers with minimal real data dramatically improves performance. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Featured Experiments
| Research Reagent / Tool | Function / Explanation | Featured Use Case |
|---|---|---|
| CHO Cell Line | A recombinant mammalian cell line widely used for producing therapeutic proteins, such as monoclonal antibodies [6]. | Model organism for bioprocess development and scale-up studies [6]. |
| Chemically Defined Media (e.g., Dynamis AGT) | A cell culture medium with a known, consistent composition, ensuring process reproducibility and reducing variability in experimental outcomes [6]. | Provides a controlled nutritional environment for CHO cell cultivations in transferability studies [6]. |
| Feed Medium (e.g., CHO CD EfficientFeed) | A concentrated nutrient supplement added during the culture process to extend cell viability and increase protein production in fed-batch bioreactors [6]. | Used to manipulate Critical Process Parameters (CPPs) like glucose concentration in iDoE [6]. |
| RUV (Remove Unwanted Variation) | A computational homogenization method used to correct for non-biological technical differences between datasets, such as those from different labs or platforms [3]. | Bridges the batch-effect gap between in vitro cell line and in vivo patient genomic data in translational models [3]. |
| FORESEE R-Package | A software tool designed to systematically train and test different translational modeling pipelines, enabling unbiased benchmarking [3]. | Used for the systematic scan of 3,920 modeling pipelines to find robust predictors of patient drug response [3]. |
Troubleshooting Guide: Common Data Challenges in Pharma R&D
This guide addresses frequent data management problems encountered when moving from controlled research datasets to diverse, real-world data sources in pharmaceutical research and development.
Problem 1: How to Overcome Data Silos and Disorganization?
The Issue: Your organization's critical data is isolated across different departments, archives, and external partners, each with unique storage practices and naming conventions [7] [8]. This fragmentation makes it difficult to aggregate, analyze, and glean insights, ultimately slowing down research and drug discovery [7].
Solutions:
- Implement a Centralized Data Integration Platform: Use advanced platforms to consolidate data from multiple sources into a unified repository [9] [8].
- Adopt Interoperable Standards: Establish and enforce consistent data formats, nomenclature, and storage practices across the organization [7] [8].
- Encourage Cross-Functional Collaboration: Foster a culture of data sharing and break down territorial attitudes that lead to data being closely guarded [8].
Problem 2: How to Ensure Data Quality and Integrity in Multi-Source Data?
The Issue: Data sourced from myriad channels often suffers from inaccuracies, inconsistencies, and incompleteness. In an industry with high stakes, even minor discrepancies can profoundly impact drug efficacy, safety, and regulatory approvals [8].
Solutions:
- Employ Automated Data Validation: Implement robust data validation and verification processes to ensure accuracy and reliability [8].
- Utilize Data Governance Frameworks: Establish clear policies for data access, usage, and quality standards [9] [8].
- Leverage Specialized Tools: Use data management and analysis tools designed to enhance data quality and integrity [8]. For classification datasets, tools like
cleanlabcan automatically detect label issues across various data modalities [10].
Problem 3: How to Handle Massive Datasets with High Computational Demands?
The Issue: Pharma companies often work with petabytes of medical imaging and research data. Effectively working with databases of this scale requires massive computational resources, often requiring cloud-scale infrastructure and hybrid environments [7].
Solutions:
- Implement Elastic Scaling: Utilize modern tools and infrastructure that can elastically scale to fit research needs quickly and cost-effectively [7].
- Optimize Data Processing: For large datasets with limited memory, use batched processing methods. With
cleanlab, for instance, you can usefind_label_issues_batched()to control memory usage by adjusting thebatch_sizeparameter [10]. - Consider Rare Classes: For datasets with many classes, merge rare classes into a single "Other" category to improve processing efficiency without significantly affecting label error detection accuracy [10].
Problem 4: How to Maintain Compliance in Collaborative Environments?
The Issue: Research organizations must meet stringent regulatory requirements when using sensitive biomedical data, especially with the increase in remote work and far-flung collaborations. Data privacy regulations like HIPAA and GDPR set strict standards for data handling [7] [8].
Solutions:
- Centralize on Secure Platforms: Use shared, secure, and compliant platforms to keep projects moving while maintaining vigilance over sensitive information [7].
- Conduct Regular Security Audits: Perform frequent security audits and risk assessments to identify and address vulnerabilities [8].
- Implement Robust Cybersecurity Measures: Apply encryption, multi-factor authentication, and secure access controls to protect sensitive data [8].
Data Integration Methods Comparison
Table 1: Comparison of Data Integration Approaches for Multi-Source Data
| Method | Handled By | Data Cleaning | Source Requirements | Best Use Cases |
|---|---|---|---|---|
| Data Integration [11] | IT Teams | Before output | No same-source requirement | Comprehensive, systemic consolidation into standardized formats |
| Data Blending [11] | End Users | After output | No same-source requirement | Combining native data from multiple sources for specific analyses |
| Data Joining [11] | End Users | After output | Same source required | Combining datasets from the same system with overlapping columns |
Research Reagent Solutions: Data Management Tools
Table 2: Essential Solutions for Multi-Source Data Challenges
| Solution Type | Function | Example Applications |
|---|---|---|
| Centralized Data Warehouses [9] [11] | Consolidated repositories for structured data from multiple sources | Creating single source of truth for inventory levels, customer data |
| Data Lakes [9] [11] | Storage systems handling large volumes of structured and unstructured data | Combining diverse data types (EHR, lab systems, imaging) for comprehensive analysis |
| Entity Resolution Tools [12] | Identify and merge records referring to the same real-world entity | Resolving varying representations of the same entity across multiple data providers |
| Truth Discovery Systems [12] | Resolve attribute value conflicts by evaluating source reliability | Determining correct values when different sources provide conflicting information |
| Automated Data Cleansing Tools [10] | Detect and correct label issues, inconsistencies in datasets | Improving data quality for ML model training in classification tasks |
Experimental Protocols for Data Quality Assessment
Protocol 1: Entity Resolution for Multi-Source Data Integration
Objective: Resolve entity information overlapping across multiple data sources [12].
Methodology:
- Blocking: Divide records into blocks to avoid comparing every record with all others. Use standard blocking, sorted blocking, or token blocking techniques [12].
- Matching: Determine whether two representations refer to the same real-world entity using schema-aware or schema-agnostic methods [12].
- Knowledge Integration: Incorporate external knowledge bases, rules, or constraints to improve matching accuracy where applicable [12].
Entity Resolution Workflow
Protocol 2: Label Quality Assessment for Machine Learning Readiness
Objective: Detect and address label issues in classification datasets to improve model performance and transferability [10].
Methodology:
- Data Preparation: Format labels as integer-encoded values in the range {0,1,...,K-1} where K is the number of classes [10].
- Issue Detection: Use appropriate methods based on dataset size:
- Label Correction: For training data, auto-correct or manually review flagged issues. For test data, manually review flagged issues to ensure reliable evaluation [10].
Label Quality Assessment Process
Frequently Asked Questions
Effective integration requires a systematic approach [11]:
- Identify the need for combined data and relevant sources
- Extract data from sources in native format
- Transform data through normalization, removal of duplicates, and correction of inaccuracies
- Load data into analytics applications or business intelligence systems Automating as much of the cleansing process as possible is crucial for efficiency and enabling self-service data access [11].
What are the specific data quality issues in multi-source data compared to single-source data?
Multi-source data introduces three specific quality challenges [12]:
- Entity Information Overlapping: Different representations of the same entity across sources, requiring entity resolution
- Attribute Value Conflicts: Conflicting observations for the same attribute across different sources, requiring truth discovery
- Attribute Value Inconsistencies: Invalid or incomplete attribute values across different entities, requiring integrity constraints for detection and repair
How should we handle label errors in both training and test datasets?
For the most reliable model training and evaluation [10]:
- Merge training and test sets into one larger dataset
- Use cross-validation training to detect label issues across the combined dataset
- For training data: Auto-correcting labels is acceptable and should improve ML performance
- For test data: Manually fix labels via careful review of flagged issues to ensure evaluation reliability Tools like Cleanlab Studio can help efficiently fix label issues in large datasets [10].
What computational strategies work for large-scale data problems in drug discovery?
For petabyte-scale datasets common in pharmaceutical research [7]:
- Use hybrid environments combining cloud-scale resources with high-performance compute clusters
- Implement elastic scaling to quickly and cost-effectively meet fluctuating computational demands
- Employ batched processing for large datasets with limited memory, processing data in manageable chunks
- Consider algorithmic workflows that can be pipelined together, using the output of one process as input to the next
How can we boost model transferability from clean lab data to messy real-world data?
Enhancing model transferability requires [13] [14]:
- Data Augmentation: Using transformations in both spatial and frequency domains to increase data diversity
- Adversarial Training: Leveraging adversarial examples to reveal model weaknesses and enhance robustness
- Feature Perturbation: Strategically perturbing consistent features across modalities to improve generalization
- Multi-Domain Training: Incorporating data from various domains and conditions during model training
Troubleshooting Guides
Guide 1: Diagnosing Model Performance Decay in Production
Symptom: Your model's predictive accuracy or performance metrics are degrading over time, despite functioning correctly initially.
| Potential Cause | Diagnostic Check | Immediate Action | Long-term Solution |
|---|---|---|---|
| Gradual Concept Drift [15] | Monitor model accuracy or error rate over time using control charts [16]. | Retrain the model on the most recent data [17]. | Implement a continuous learning pipeline with periodic retraining [15]. |
| Sudden Concept Drift [15] | Use drift detection methods (e.g., DDM, ADWIN) to identify abrupt changes in data statistics [16]. | Trigger a model retraining alert and investigate external events (e.g., market changes, new regulations) [15]. | Develop a model rollback strategy to quickly revert to a previous stable version. |
| Data (Covariate) Shift [18] | Compare the distribution of input features in live data versus the training data (e.g., using Population Stability Index) [18]. | Evaluate if the model is still calibrated on the new input distribution [18]. | Employ domain adaptation techniques or source data from a more representative sample [5]. |
Guide 2: Addressing Data Integrity and Access Issues
Symptom: Inability to access, integrate, or trust the data needed for model training or inference.
| Potential Cause | Diagnostic Check | Immediate Action | Long-term Solution |
|---|---|---|---|
| Siloed or Disparate Data [19] | Audit the number and accessibility of data sources required for your research. | Use a centralized data platform to aggregate sources, if available [19]. | Advocate for and invest in integrated data infrastructure and shared data schemas [19]. |
| Data Quality Decay [16] | Check for "data corrosion," "data loss," or schema inconsistencies in incoming data [16]. | Implement data validation rules at the point of entry. | Establish robust data governance and quality monitoring frameworks. |
| Limited Data Availability [19] | Identify if required data is behind paywalls, has privacy restrictions, or simply doesn't exist [19]. | Explore alternative data sources or synthetic data generation. | Build partnerships for data sharing and advocate for open data initiatives where appropriate. |
Guide 3: Navigating the Regulatory and Ethical Landscape
Symptom: Projects are delayed or halted due to compliance issues, ethical concerns, or institutional barriers.
| Challenge Area | Key Questions for Self-Assessment | Risk Mitigation Strategy |
|---|---|---|
| Data Privacy & Security [20] | Have we obtained proper consent for data use? Are we compliant with regulations like HIPAA? [20] | Anonymize patient data and implement strict access controls [20]. |
| Algorithmic Bias & Fairness [19] | Does our training data represent the target population? Could the model yield unfair outcomes? | Use a centralized AI platform to reduce human selection bias and perform rigorous bias audits [19]. |
| Regulatory Hurdles [21] | Have we engaged with regulators early? Is our validation process rigorous and documented? | Proactively engage with regulatory bodies and design studies with regulatory requirements in mind. |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between concept drift and data drift?
A: Concept drift is a change in the underlying relationship between your input data (features) and the target variable you are predicting [15]. For example, the characteristics of a spam email change over time, even if the definition of "spam" does not. Data drift (or covariate shift) is a change in the distribution of the input features themselves, while the relationship to the target remains unchanged [18]. An example is your model seeing more users from a new geographic region than it was trained on [15].
Q2: How can I detect concept drift if I don't have immediate access to true labels in production?
A: While monitoring the actual model error rate is the most direct method, it's often not feasible due to label lag. In such cases, you can use proxy methods [15]:
- Prediction Drift: Monitor the distribution of the model's predictions. A significant shift can indicate concept drift [15].
- Data Drift: Analyze shifts in the input feature distributions, as concept drift often coincides with data drift [16] [15].
- Domain-specific Heuristics: Use business logic as a proxy. For instance, a sudden drop in the click-through rate for a recommendation model can signal performance decay [15].
Q3: Our model is performing well, but we are concerned about regulatory approval. What are key considerations for drug development research?
A: For healthcare and drug development, focus on:
- Transparency and Explainability: Be prepared to explain how your model works and why it makes certain predictions [20].
- Robust Validation: Go beyond standard accuracy metrics. Perform rigorous internal and external validation to ensure generalizability [20].
- Data Provenance: Maintain clear records of your data sources, how the data was processed, and any transformations applied [20].
- Ethical Data Sourcing: Ensure patient data is anonymized and used in compliance with all relevant regulations and with proper consent [20].
Q4: We have a small dataset for our specific task. How can we leverage transfer learning effectively while avoiding negative transfer?
A:
- Task Similarity is Key: Transfer learning works best when the source and target tasks are related [5]. Using a model trained on natural images for medical imaging is more likely to succeed than using one trained on text.
- Fine-Tuning: Don't just use the pre-trained model as a static feature extractor. Fine-tune the later layers of the model on your small, domain-specific dataset to adapt the learned features [5].
- Validate Rigorously: To avoid negative transfer (where the source knowledge harms performance), always validate the transferred model's performance on a held-out test set from your target domain and compare it to a baseline [5].
The following table summarizes key metrics and thresholds for common drift detection methods.
| Method Name | Type | Key Metric Monitored | Typical Thresholds/Actions |
|---|---|---|---|
| DDM (Drift Detection Method) | Online, Supervised | Model error rate | Warning level (e.g., error mean + 2σ), Drift level (e.g., error mean + 3σ) |
| EDDM (Early DDM) | Online, Supervised | Distance between classification errors | Tracks the average distance between errors; more robust to slow, gradual drift than DDM. |
| ADWIN (ADaptive WINdowing) | Windowing-based | Data distribution within a window | Dynamically adjusts window size to find a sub-window with different data statistics. |
| KSWIN (Kolmogorov-Smirnov WINdowing) | Windowing-based | Statistical distribution | Uses the KS test to compare the distribution of recent data against a reference window. |
Experimental Protocols
Protocol 1: Implementing a Concept Drift Detection Framework using ADWIN
Objective: To proactively detect concept drift in a live model using the Adaptive Windowing (ADWIN) algorithm.
Materials:
- A trained machine learning model in production.
- A stream of incoming feature data and, when available, ground truth labels.
- An implementation of the ADWIN algorithm (available in libraries like
scikit-multiflow).
Methodology:
- Initialization: Configure the ADWIN detector with a chosen significance level (e.g., δ=0.002) and a initial window size [16].
- Stream Processing: For each new data instance (or batch) that the model processes: a. Record the model's prediction and, if available, the true label to calculate the prediction error. b. Input the error value (or a relevant data statistic) into the ADWIN algorithm.
- Drift Detection: ADWIN maintains a window of recent data. It continuously checks whether the average of a sub-window of recent data differs significantly from the rest of the window.
- Alerting: If a significant change is detected, ADWIN triggers a drift alarm.
- Response: Upon alarm, initiate a pre-defined workflow: log the event, trigger model retraining on recent data, and/or alert the engineering team [16].
Diagram: ADWIN Drift Detection Workflow
Protocol 2: Evaluating Model Transferability with Domain Adaptation
Objective: To systematically assess and improve a model's performance when applied from a source domain (e.g., general patient population) to a target domain (e.g., a specific sub-population).
Materials:
- Labeled dataset from the source domain.
- (Possibly smaller) labeled dataset from the target domain for evaluation.
- A pre-trained model on the source domain.
Methodology:
- Baseline Performance: Evaluate the pre-trained source model directly on the held-out test set from the target domain. Record key performance metrics (e.g., AUC, F1-Score). This is your transferability baseline [5].
- Fine-Tuning: Take the pre-trained model and continue training (fine-tune) it on a small, labeled portion of the target domain data. Use techniques like a lower learning rate and/or freezing the initial layers to avoid catastrophic forgetting [5].
- Performance Comparison: Evaluate the fine-tuned model on the target domain test set. Compare the results to the baseline.
- Analysis: Calculate the performance delta. A significant improvement indicates successful transfer learning. If performance degrades, this may indicate "negative transfer," suggesting the domains are too dissimilar [5].
Diagram: Model Transferability Evaluation
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions for Robust ML Research
| Tool / Reagent | Function / Purpose | Example Use-Case |
|---|---|---|
| Evidently AI [15] | An open-source library for monitoring and debugging ML models. | Calculating prediction drift and data drift metrics in a production environment. |
| TensorFlow / PyTorch [5] | Core frameworks for building, training, and deploying ML models. | Implementing and fine-tuning pre-trained models for transfer learning tasks. |
| Hugging Face [5] | A platform hosting thousands of pre-trained models, primarily for NLP. | Quickly prototyping a text classification model by fine-tuning a pre-trained BERT model. |
| ADWIN Algorithm [16] | A drift detection algorithm that adaptively adjusts its window size. | Detecting gradual concept drift in a continuous data stream without pre-defining a window size. |
| Centralized Data Platform [19] | A unified system (e.g., AlphaSense, internal data lakes) to aggregate disparate data sources. | Solving the challenge of siloed content and ensuring a 360-degree view of research data. |
Troubleshooting Guide: Common Model Alignment and Transferability Issues
This guide addresses frequent challenges in applying the 'Fit-for-Purpose' mindset to model development for drug research.
| Problem Area | Common Symptoms | Potential Root Causes | Recommended Solutions |
|---|---|---|---|
| Negative Transfer | Model performs worse on the target task than training from scratch; poor generalization to new data [5]. | Source and target domains are too dissimilar; inadequate feature space overlap [5]. | Conduct thorough task & domain similarity analysis before transfer; use domain adaptation techniques [5]. |
| Data Scarcity | High variance in model performance; failure to converge on the target task [22]. | Limited labeled data for novel drug targets or rare diseases; costly and time-consuming experimental data generation [22]. | Leverage pre-trained models (PLMs) and self-supervised learning; employ data augmentation and synthetic data generation [22] [5]. |
| Model Misalignment with COU | Model behaves undesirably in specific contexts; violates regulatory or business guidelines [23]. | Lack of alignment to particular contextual regulations, social norms, or organizational values [23]. | Implement contextual alignment frameworks like Alignment Studio for fine-tuning on policy documents and specific regulations [23]. |
| Multi-Modal Fusion Challenges | Inability to leverage complementary data types (e.g., graph + sequence); model fails to capture complex interactions [22]. | Treating modalities separately; lack of effective cross-modal attention mechanisms [22]. | Implement advanced fusion modules like co-attention and paired multi-modal attention to capture cross-modal interactions [22]. |
| Overfitting on Small Datasets | High accuracy on training data but poor performance on validation/test data during fine-tuning [5]. | Fine-tuning a complex pre-trained model on a small, domain-specific dataset [5]. | Apply regularization (L1, L2, dropout); fine-tune only the last few layers; use progressive unfreezing of layers [5]. |
Frequently Asked Questions (FAQs)
Q1: How does the 'Fit-for-Purpose' model differ from traditional machine learning development? The 'Fit-for-Purpose' model, as a framework for Better Business, emphasizes that all building blocks of a project—Why (purpose), What (value proposition), Whom (stakeholders), Where (operational context), and How (operating practices)—must be coherently aligned [24]. In machine learning, this translates to ensuring that the model's design, data, and deployment environment are all intentionally aligned with the specific Context of Use, rather than just optimizing for a generic accuracy metric.
Q2: What is negative transfer and how can we avoid it in transfer learning? Negative transfer occurs when knowledge from a source task adversely affects performance on a related target task [5]. To avoid it:
- Analyze Domain Similarity: Carefully evaluate the relevance of the source model's pre-training data to your target domain [5].
- Validate First: Test the pre-trained model on a small, representative sample of your target data before committing to a full implementation [5].
- Use Transferability Metrics: Employ metrics to estimate performance before fine-tuning.
Q3: Our organization has specific guidelines (e.g., BCGs). How can we align a model to them? Aligning models to particular contextual regulations requires a principled approach. One method is an Alignment Studio architecture, which uses three components [23]:
- Framers: Process natural language policy documents to create fine-tuning data and scenarios.
- Instructors: Fine-tune the model using the generated data to instill the desired behaviors.
- Auditors: Use human and automated red-teaming to evaluate if the model has successfully learned the guidelines [23].
Q4: What strategies can improve the transferability of research findings to real-world industry settings? To enhance transferability, research should be designed for applicability in different contexts [25].
- Engage Stakeholders Early: Involve industry partners and end-users in the research process to ensure relevance and feasibility [25].
- Communicate Clearly: Share findings in an accessible manner for various audiences, not just academic peers [25].
- Conduct Multi-Site Trials: Perform pilot studies in multiple settings to test the robustness and adaptability of the model or method [25].
Q5: When should we consider using Small Language Models (SLMs) over Large Language Models (LLMs) in AI agents? For many industry applications, SLMs (models under ~10B parameters) are a strategic fit-for-purpose choice [26]. Consider SLMs when your tasks are narrow and repetitive (e.g., parsing commands, calling APIs, generating structured outputs), as they offer 10–30x lower inference cost and latency while matching the performance of last-generation LLMs on specific benchmarks [26].
Experimental Protocol: Implementing a 'Fit-for-Purpose' Multi-Modal Model
The following workflow details the methodology for frameworks like DrugLAMP, which integrates multiple data modalities for accurate and transferable Drug-Target Interaction (DTI) prediction [22].
Multi-Modal Model Workflow
1. Data Preparation & Input Modalities:
- Drug Data: Collect and preprocess molecular structures represented as SMILES strings and/or molecular graphs [22].
- Target Data: Collect and preprocess protein sequences and, if available, 3D protein structure or pocket information [22].
2. Feature Extraction with Pre-trained Models:
- Utilize Pre-trained Language Models (PLMs) to encode the sequential data (SMILES strings and protein sequences). This leverages the PLMs' ability to capture rich, contextual representations from vast unlabeled datasets [22].
- Use Graph Neural Networks (GNNs) or other feature extractors to process the molecular graph data [22].
3. Multi-Modal Fusion:
- Implement fusion modules to integrate the extracted features from different modalities. Key techniques include:
- Pocket-Guided Co-Attention (PGCA): Uses protein pocket information to guide the attention mechanism on drug features, focusing on the most relevant molecular substructures [22].
- Paired Multi-Modal Attention (PMMA): Enables effective cross-modal interactions between drug and protein features, allowing the model to learn complex, interdependent representations [22].
4. Contrastive Pre-training (2C2P Module):
- Perform contrastive compound-protein pre-training on large, unlabeled datasets. This step enhances the model's generalization and transferability by aligning features across modalities and conditions, which is crucial for predicting interactions for novel drugs or targets [22].
5. Supervised Fine-Tuning:
- Finally, fine-tune the entire model on a labeled DTI dataset for the specific prediction task (e.g., binding affinity classification). This adapts the generally pre-trained model to the precise "purpose" of the research question [22].
The Scientist's Toolkit: Key Research Reagents & Solutions
The following tools and frameworks are essential for building transferable, 'fit-for-purpose' models in computational drug discovery.
| Tool / Framework | Primary Function | Relevance to 'Fit-for-Purpose' & Transferability |
|---|---|---|
| Pre-trained Language Models (e.g., BERT, GPT) [5] | Provide powerful base models that have learned general representations from vast biological and chemical text/data. | Drastically reduce data and computational needs via transfer learning; can be fine-tuned for specific tasks like DTI prediction [22] [5]. |
| Multi-Modal Fusion Architectures [22] | Integrate diverse data types (e.g., graphs, sequences) into a unified model using attention mechanisms. | Critical for capturing the complex interactions in biology; enables models to leverage complementary information for more accurate predictions [22]. |
| Contrastive Learning Modules (e.g., 2C2P) [22] | Align representations from different modalities in a shared space using unlabeled data. | Enhances model generalization and robustness, key for transferability to novel drugs and targets where labeled data is scarce [22]. |
| Alignment Studio Framework [23] | A toolset for aligning LLM behavior to specific contextual regulations and business guidelines. | Ensures models are not just technically accurate but also operate within required ethical, legal, and organizational constraints [23]. |
| Small Language Models (SLMs) [26] | Provide a class of models under ~10B parameters optimized for specific, narrow tasks. | Offer a strategic "fit-for-purpose" solution for deployment in resource-constrained environments or for repetitive agentic tasks, balancing cost and performance [26]. |
Troubleshooting Guides
Guide 1: Resolving Model Instability in Pharmacometric Analyses
Problem: My pharmacometric model (e.g., PopPK, PKPD) fails to converge, produces biologically unreasonable parameter estimates, or yields different results with different initial estimates.
Explanation: Model instability is often a multifactorial issue, frequently stemming from a mismatch between model complexity and the information content of your data [27]. Diagnosing the root cause is essential for applying the correct solution.
Solution: Follow this structured workflow to identify and resolve stability issues [27].
Steps:
- Model Confirmation and Verification: Before investigating instability, ensure your model is an appropriate representation of the biological system (confirmation) and that your code is a faithful translation of the model schematic (verification) [27]. This step rules out coding errors as the source of instability.
- Assess Data Quality: Scrutinize your dataset for issues that can undermine stability, such as significant outliers, critical missing data, or errors in dosing and sampling records [27].
- Balance Model Complexity and Data Information: This is a common cause of instability [27].
- If the model is over-parameterized: Simplify the model structure. For example, a model expecting Target-Mediated Drug Disposition (TMDD) might need to be approximated with a simpler model (e.g., linear or time-varying clearance) if the data is insufficient to inform the full kinetic binding parameters [27].
- If the data is limited: Consider incorporating strong prior knowledge or leveraging a pre-existing, mechanistically sound "system-lens" model from the literature, ensuring it is fit-for-your-current-purpose [27].
- Evaluate Optimization Algorithm and Settings: Review your software's (e.g., NONMEM) optimization settings. The choice of algorithm, interaction method, and other numerical settings can significantly impact stability and may need adjustment for your specific model and data [27].
Guide 2: Managing Compressed Timelines for Regulatory Submissions
Problem: Our team needs to prepare a robust pharmacometric analysis for a regulatory submission (NDA/BLA) under an expedited timeline with limited resources.
Explanation: Regulatory agencies increasingly expect pharmacometric evidence, and managing this under compressed timelines is a common challenge [28]. Success hinges on efficient, cross-functional workflows and strategic planning.
Solution: Adopt a proactive, fit-for-purpose strategy to ensure submission readiness without compromising scientific rigor [28].
Steps:
- Early Regulatory Engagement: Proactively engage with agencies like the FDA or EMA to discuss your Model-Informed Drug Development (MIDD) strategy. Seek agreement on the Context of Use (COU) and the Model Analysis Plan (MAP) to minimize later objections [28] [29].
- Leverage Core Analyses Efficiently: Focus on fit-for-purpose population PK (PopPK) and exposure-response models to address critical questions on dose selection, variability, and benefit-risk, which are essential for labeling decisions [28].
- Streamline Operational Workflows: Utilize efficient software and platforms (e.g., R packages like
mrgsolvefor simulation) that support reproducible and flexible pharmacometric workflows to accelerate analysis time [30] [31]. - Communicate for Decision-Making: In decisional meetings, use a deductive approach: state your conclusion and recommendation first, followed by the supporting model results. This focuses the discussion on the actionable decision rather than the technical modeling details [32].
Frequently Asked Questions (FAQs)
Q1: What are the most critical skills for a pharmacometrician to influence drug development decisions? A pharmacometrician requires three key skill sets to be influential: technical skills (e.g., modeling, simulation), business skills (understanding drug development), and soft skills (especially effective communication) [32]. A survey found that 82% of professionals believe pharmacometricians, on average, lack strategic communication skills, highlighting a critical area for development [32].
Q2: How should I present pharmacometric results to an interdisciplinary team to maximize impact? Tailor your communication to your audience [32]. For interdisciplinary teams, use a deductive approach: start with the bottom-line recommendation, then provide the supporting evidence. Avoid deep technical details; instead, focus on how the analysis informs the specific decision at hand (e.g., "We recommend a 50 mg dose because the model predicts a 90% probability of achieving target exposure") [32].
Q3: What is the significance of the new ICH M15 guideline for MIDD? The ICH M15 draft guideline, released in late 2024, provides the first internationally harmonized framework for MIDD. It aims to align expectations between regulators and sponsors, support consistent regulatory decisions, and minimize errors in the acceptance of modeling and simulation evidence in drug labels [29]. It establishes a structured process with a clear taxonomy, including stages for Planning, Implementation, Evaluation, and Submission [29].
Q4: My model works for one software but fails in another. What could be the cause? This is a recognized symptom of model instability [27]. Differences in optimization algorithms, default numerical tolerances, or interaction methods between software platforms (e.g., NONMEM, Monolix, etc.) can produce different results when a model is poorly identified. Revisit the troubleshooting guide for model instability, paying close attention to the balance between model complexity and data information content [27].
The Scientist's Toolkit: Essential Research Reagents & Solutions
The table below lists key tools and methodologies used in modern pharmacometrics.
| Tool/Solution | Function & Application |
|---|---|
| Population PK/PD (PopPK/PD) Modeling [29] | A preeminent method using nonlinear mixed-effects models to characterize drug concentrations and variability in effects, and to perform clinical trial simulations. |
| Model-Informed Drug Development (MIDD) [29] | A framework that uses quantitative modeling to integrate data and prior knowledge to inform drug development and regulatory decisions. |
| mrgsolve [30] | An R package for pharmacokinetic-pharmacodynamic (PK/PD) model simulation. It is used to simulate drug behavior from a pre-defined model, aiding in trial design and dose selection. |
| RsNLME [31] | A suite of R packages supporting flexible and reproducible pharmacometric workflows for model building and execution. |
| Model Analysis Plan (MAP) [29] | A critical document in the ICH M15 framework that defines the introduction, objectives, data, and methods for a modeling exercise, ensuring alignment and clarity. |
| Credibility Assessment [29] | A framework (based on standards like ASME V&V 40) used to evaluate model relevance and adequacy, ensuring computational models are fit-for-purpose. |
Practical Methods and MIDD Tools for Enhanced Industrial Generalization
Leveraging Model-Informed Drug Development (MIDD) as a Strategic Framework
MIDD and Model Transferability: Core Concepts FAQ
Q1: What is Model-Informed Drug Development (MIDD) and how does it relate to model transferability?
A1: Model-Informed Drug Development (MIDD) is defined as a quantitative framework for prediction and extrapolation, centered on knowledge and inference generated from integrated models of compound, mechanism, and disease-level data. Its goal is to improve the quality, efficiency, and cost-effectiveness of decision-making [33]. Within this framework, model transferability refers to the ability of a model developed for one specific task or context—such as a pre-clinical model or a model for one patient population—to be effectively applied or adapted to a related but distinct context, such as a different disease population or a new drug candidate with a similar mechanism of action [5]. The strategic integration of transferability principles helps ensure that quantitative models remain valuable assets across a drug's lifecycle.
Q2: What are the primary business benefits of implementing a MIDD strategy with a focus on transferability?
A2: Adopting a MIDD strategy that emphasizes model transferability offers several key business and R&D benefits [33] [34]:
- Enhanced R&D Efficiency: It significantly shortens development cycle timelines and reduces discovery and trial costs by leveraging existing knowledge and models.
- Improved Decision-Making: It provides a structured, data-driven framework for evaluating safety and efficacy, thereby increasing the probability of technical and regulatory success.
- Cost Reduction: Companies like Pfizer and Merck & Co. have reported substantial cost savings—up to $100 million annually and $0.5 billion, respectively—attributed to the impact of MIDD on decision-making [33].
- Knowledge Preservation and Leverage: It creates reusable quantitative tools that can be applied across multiple drug programs, maximizing return on investment.
Q3: What are common pitfalls that hinder model transferability in MIDD, and how can they be avoided?
A3: A major challenge in transferring models is "negative transfer," which occurs when a model from a source task adversely affects performance on the target task because the domains are too dissimilar [5]. Other pitfalls include overfitting during fine-tuning on small datasets and the computational complexity of adapting large models [5]. To mitigate these risks:
- Conduct Rigorous Domain Analysis: Carefully evaluate the similarity between the source and target tasks (e.g., disease pathophysiology, patient demographics) before transfer [5] [35].
- Adopt a "Fit-for-Purpose" Mindset: Select and adapt models based on the specific "Question of Interest" and "Context of Use" for the new application, avoiding unnecessary complexity [34].
- Implement Robust Validation: Use techniques like cross-validation and external validation to ensure model performance generalizes to the new context.
Troubleshooting Guide: Common MIDD Implementation Challenges
Q1: My PK/PD model performs well in pre-clinical data but fails to predict early clinical outcomes. What should I check?
A1: This is a classic model transferability issue between pre-clinical and clinical phases. Follow this systematic troubleshooting protocol:
- Step 1: Verify Physiological Relevance. Check if your Physiologically-Based Pharmacokinetic (PBPK) model accurately reflects human (as opposed to animal) physiology and metabolic pathways. Ensure allometric scaling for dose prediction is appropriate [34].
- Step 2: Inter-species Differences. Re-evaluate assumptions about drug absorption, distribution, metabolism, and excretion (ADME). Key proteins like enzymes and transporters may have different expression and activity in humans.
- Step 3: Model Complexity. Determine if your model is either oversimplified (missing key mechanistic elements) or overly complex (leading to overfitting on pre-clinical data). A semi-mechanistic PK/PD approach might offer a better balance [34].
- Step 4: Data Quality and Recalibration. Use the limited early clinical (e.g., First-in-Human) data to recalibrate and refine the model, focusing on updating the most uncertain parameters.
Q2: How can I select the best pre-existing model from a repository ("model zoo") for my new, unlabeled clinical dataset?
A2: This is a common scenario in industry research where labeled data is scarce. Employ a source-free transferability assessment framework [36]:
- Step 1: Feature Extraction. Process a small, representative sample of your unlabeled target data through each candidate model in your repository to generate feature embeddings.
- Step 2: Create a Reference. Generate a task-agnostic reference embedding using an ensemble of Randomly Initialized Neural Networks (RINNs), which capture structural priors without training [36].
- Step 3: Similarity Analysis. Quantify the structural similarity between the embeddings from the candidate models and the RINN reference using a metric like Centered Kernel Alignment (CKA).
- Step 4: Model Ranking. Rank the candidate models based on their similarity scores. The model with the highest score is the most transferable to your new dataset and should be selected for fine-tuning or direct application [36].
Q3: Our quantitative systems pharmacology (QSP) model is not accepted by internal decision-makers for informing a clinical trial design. How can we improve stakeholder confidence?
A3: This is often a communication and validation issue, not a technical one.
- Action 1: Strengthen Context of Use (COU) Definition. Clearly and concisely document the specific question the model is intended to answer, its boundaries, and its limitations. This aligns with regulatory best practices [33] [34].
- Action 2: Demonstrate Predictive Performance. Present a retrospective analysis showing how the model accurately simulated or predicted outcomes from historical data within your organization.
- Action 3: Conduct Sensitivity and Uncertainty Analysis. Systematically identify and present the key model parameters that drive the outcomes and quantify the uncertainty in the predictions. This demonstrates a thorough understanding of the model's robustness.
- Action 4: Align with Regulatory Precedents. Cite successful examples of MIDD applications in regulatory submissions for similar drug classes or clinical questions [33] [37].
Detailed Experimental Protocols for Key MIDD Analyses
Protocol 1: Developing a "Fit-for-Purpose" Population PK/PD Model
Objective: To characterize the population pharmacokinetics and exposure-response relationship of a drug to inform dosing recommendations.
Materials & Methodology:
- Data: Rich or sparse drug concentration-time data and response (efficacy/safety) data from clinical trials.
- Software: Non-linear mixed-effects modeling software (e.g., NONMEM, Monolix, R).
- Structural Model Development: Identify the best-fitting structural PK model (e.g., one- or two-compartment) and PD model (e.g., Emax, linear) using standard goodness-of-fit plots and objective function value (OFV).
- Statistical Model Development: Identify and quantify sources of inter-individual variability (IIV) and inter-occasion variability (IOV) on model parameters. Model residual unexplained variability.
- Covariate Analysis: Identify patient-specific factors (e.g., weight, renal function, age) that explain a portion of the IIV. Use a stepwise forward inclusion/backward elimination procedure based on statistical significance (e.g., change in OFV).
- Model Validation: Validate the final model using:
- Bootstrap: Assess parameter precision and stability.
- Visual Predictive Check (VPC): Assess the model's ability to simulate data that matches the original dataset.
- Numerical Predictive Check (NPC): Quantify the difference between simulated and observed data.
Protocol 2: Conducting a Source-Free Model Transferability Assessment
Objective: To rank pre-trained models from a repository for their suitability on a new, unlabeled target dataset without access to source data.
Materials & Methodology:
- Inputs: A "model zoo" of pre-trained models; a small, unlabeled sample from the target domain.
- Software: Python with deep learning frameworks (e.g., PyTorch, TensorFlow).
- Embedding Extraction: For each candidate model
M_iin the zoo, forward-pass the target data sample and extract the feature embeddings from the model's penultimate layer. - Reference Embedding Generation: Create an ensemble of
KRandomly Initialized Neural Networks (RINNs) with the same architecture as the candidate models but with no training. Use this ensemble to extract a second set of embeddings from the same target data sample [36]. - Similarity Scoring: For each candidate model, compute the Minibatch-Centered Kernel Alignment (CKA) score between its embeddings and the RINN ensemble's embeddings. CKA measures the similarity of the representations.
- Model Selection: Rank all candidate models based on their CKA scores in descending order. The model with the highest
S_Escore is deemed the most transferable and is selected for the task [36].
Workflow Visualization
MIDD Strategy and Troubleshooting Workflow
Model Transferability Assessment Protocol
Table 1: Key Quantitative Tools and Methodologies in MIDD
| Tool / Methodology | Primary Function | Typical Context of Use |
|---|---|---|
| Physiologically-Based Pharmacokinetic (PBPK) Modeling [34] [37] | Mechanistic modeling to predict drug absorption, distribution, metabolism, and excretion (ADME) based on physiology and drug properties. | Predicting drug-drug interactions (DDIs); extrapolating to special populations (e.g., hepatic impairment); supporting generic drug bioequivalence. |
| Population PK (PPK) / Exposure-Response (ER) [34] | Quantifies and explains variability in drug exposure (PK) and its relationship to efficacy/safety outcomes (PD) across a patient population. | Optimizing dosing regimens; identifying sub-populations requiring dose adjustment; supporting label claims. |
| Quantitative Systems Pharmacology (QSP) [34] | Integrates systems biology and pharmacology to model drug effects on biological pathways and disease processes mechanistically. | Target validation; combination therapy strategy; understanding complex biological mechanisms; clinical trial simulation. |
| Model-Based Meta-Analysis (MBMA) [34] | Quantitative analysis of summary-level data from multiple clinical trials to understand drug class effects and competitive landscape. | Informing dose selection and trial endpoints; benchmarking a new drug's potential efficacy against standard of care. |
| Artificial Intelligence / Machine Learning (AI/ML) [34] | Analyzes large-scale datasets to predict compound properties, optimize molecules, identify biomarkers, and personalize dosing. | Drug discovery (e.g., QSAR); predicting ADME properties; analyzing real-world evidence (RWE). |
Foundations of Data-Centric AI
What is Data-Centric AI and how does it differ from model-centric approaches?
Answer: Data-Centric AI (DCAI) is a paradigm that shifts the focus from model architecture and hyperparameter tuning to systematically improving data quality and quantity [38]. Unlike the model-centric approach, which treats data as a static, fixed asset and optimizes the algorithm, DCAI treats data as a dynamic, core component to be engineered and optimized [39] [38].
The core difference is this: a model-centric team working with a fixed dataset might spend time adjusting neural network layers to improve accuracy from 95.0% to 95.5%. A data-centric team, holding the model architecture constant, would instead focus on improving the dataset itself—by correcting mislabeled examples, adding diverse data, or applying smart augmentations—to achieve a similar or greater performance boost that often transfers more reliably to real-world, industry data [38].
What are the core pillars of a Data-Centric AI development process?
Answer: The DCAI paradigm is structured around three interconnected pillars [38]:
- Training Data Development: The process of collecting and producing high-quality, rich data for model training. This involves data creation, collection, labeling, preparation, reduction, and augmentation.
- Inference Data Development: The generation of sophisticated evaluation sets that go beyond simple accuracy metrics. This aims to probe model capabilities like robustness, adaptability, and reasoning, using techniques like in-distribution and out-of-distribution evaluation.
- Data Maintenance: The ongoing process of maintaining data quality and reliability in dynamic environments. This includes data understanding, quality assurance, and efficient data storage and retrieval.
Troubleshooting Guides: Common Data-Centric AI Challenges
How do I fix a model that performs well on validation data but poorly on real-world industry data?
Problem: This is a classic sign of a model failing to transfer from a controlled research environment to a production setting. It often stems from a mismatch between your training data and the actual "inference data" encountered in the wild.
Solution: Implement a robust Inference Data Development strategy [38].
Action 1: Perform Out-of-Distribution (OOD) Evaluation
- Methodology: Systematically create test sets that differ from your training data. This can involve introducing noise, simulating domain shifts (e.g., different medical scanner types in healthcare), or using adversarial examples to test robustness.
- Protocol: From your main dataset, create a hold-out OOD test set that mirrors the conditions of your industry data as closely as possible. Benchmark your model's performance on this set to understand its failure modes.
Action 2: Identify and Calibrate Underrepresented Groups
- Methodology: Analyze your model's performance across different subgroups within your data. A common issue is that the training data does not adequately represent the full diversity of the target domain.
- Protocol: Use clustering or data profiling tools to identify latent subgroups. Then, actively source or synthesize data for these underrepresented groups to rebalance your training dataset, a process often called "data cartography."
The following workflow outlines the systematic process for diagnosing and resolving the disconnect between validation and real-world performance.
How can I resolve data quality issues that are causing technical debt and "data cascades"?
Problem: "Data cascades" are compounding events resulting from underlying data issues that cause negative, downstream effects, accumulating technical debt over time [38]. A Google study found that 92% of AI practitioners experienced this issue [38]. Common signs include inconsistent labels, missing values, and data that doesn't match the real-world distribution.
Solution: Institute a rigorous Data Quality Assurance framework during the Training Data Development and Data Maintenance phases [38].
Action 1: Implement Confident Learning for Label Quality
- Methodology: Use techniques like Confident Learning to algorithmically identify mislabeled examples in a dataset, regardless of the model or data type [38].
- Protocol: Apply an open-source Confident Learning library (e.g.,
cleanlab) to your dataset. It will output a list of potential label errors for your review and correction, significantly improving the cleanliness of your training labels.
Action 2: Establish Continuous Data Monitoring
- Methodology: Data quality is not a one-time task. Implement automated checks for data drift, schema changes, and anomaly detection in incoming data streams.
- Protocol: Define objective data quality metrics (e.g., accuracy, timeliness, consistency, completeness) and set up a dashboard to monitor these metrics over time. This is a core part of the Data Maintenance pillar [38].
The diagram below illustrates how small, unresolved data issues early in a project can compound into significant problems later, and how to intervene.
My model is exhibiting biased behavior. How can I address this from a data-centric perspective?
Problem: Bias in AI models often originates from biased or unrepresentative training data, leading to unfair outcomes in critical areas like patient stratification in drug development [40].
Solution: Proactively audit and curate your datasets to promote fairness and representation.
Action 1: Audit Data for Representational Gaps
- Methodology: Use data visualization and statistical tools to analyze the distribution of your data across sensitive or relevant attributes (e.g., age, gender, ethnicity, disease subtype).
- Protocol: Generate summary reports and visualizations showing the count and proportion of data points for each subgroup. This helps identify over- or under-represented cohorts.
Action 2: Apply Data-Centric Bias Mitigation Techniques
- Methodology: Instead of only using algorithmic debiasing, focus on improving the data itself. This can involve strategic data collection, augmentation of underrepresented groups, and re-weighting data samples.
- Protocol: For an underrepresented subgroup, employ data augmentation techniques specific to that domain (e.g., synthetic data generation) to increase its presence in the training set. Alternatively, use sampling strategies to ensure a more balanced batch composition during training.
Experimental Protocols & The Scientist's Toolkit
Detailed Methodology: Confident Learning for Label Error Detection
This protocol is used to identify and correct mislabeled examples in a dataset, a common issue in manually annotated biological data.
- Input: A dataset with features
Xand (noisy) labelss. - Cross-Validation: Train a classifier on
(X, s)usingk-foldcross-validation to generate out-of-sample predicted probabilitiesP. - Estimate Joint Distribution: Use
Pandsto compute the confident joint matrix, which estimates the joint distribution between the given (noisy) labels and the inferred (true) labels. - Find Label Errors: Identify the examples and their indices that are likely mislabeled based on the confident joint.
- Output: A boolean mask indicating which labels are likely erroneous, and a list of suggested alternative labels.
- Human-in-the-Loop Review: A domain expert (e.g., a biologist) reviews the suggested errors and makes the final correction, updating the dataset.
Detailed Methodology: Out-of-Distribution (OOD) Evaluation Set Creation
This protocol tests model robustness and prepares it for transfer to industry data.
- Define OOD Axes: Identify potential sources of distribution shift relevant to your domain (e.g., for histology images: different tissue staining protocols, scanners, or patient demographics).
- Data Sourcing: Actively source a new dataset that varies along one or more of these axes. This should be a separate dataset from your main training and validation sets.
- Annotation: Label this new OOD set with the same procedure as your main dataset to ensure label consistency.
- Benchmarking: Evaluate your trained model on this OOD set. Report performance metrics separately for the in-distribution (ID) test set and the OOD test set. A large performance gap indicates poor transferability and a need for data-centric improvements.
Research Reagent Solutions
The following table details key tools and conceptual "reagents" essential for implementing Data-Centric AI experiments.
| Research Reagent / Tool | Function in Data-Centric AI |
|---|---|
| Confident Learning Framework | Algorithmically identifies label errors in datasets by estimating the joint distribution of noisy and true labels, enabling high-quality data curation [38]. |
| Data Augmentation Libraries | Systematically increase the size and diversity of training data by applying label-preserving transformations, improving model robustness [38]. |
| Federated Learning Platforms | Enable model training across decentralized data sources without sharing raw data, addressing privacy concerns and expanding data access [40]. |
| Data Profiling & Visualization Tools | Provide statistical summaries and visualizations to understand data distributions, identify biases, and uncover representational gaps [38]. |
| Model Monitoring Dashboards | Track data drift and model performance metrics in real-time after deployment, a key component of the Data Maintenance pillar [38]. |
FAQ on Data-Centric AI for Research
We have limited data for a rare disease target. What data-centric techniques can help?
Answer: Data augmentation and synthetic data generation are key strategies within the Training Data Development pillar [38].
- Advanced Augmentation: Move beyond simple rotations and flips. Use domain-specific augmentations. For molecular data, this could be valid structural perturbations. For medical images, this could involve simulating different lighting or scanner artifacts.
- Synthetic Data Generation: Leverage generative models (e.g., VAEs, GANs, Diffusion Models) to create synthetic, labeled data samples that follow the distribution of your limited real data. This can artificially expand your dataset and improve model robustness.
- Transfer Learning with a Data-Centric Twist: Instead of just using a pre-trained model, use a pre-trained model to inform your data collection and augmentation strategy. Analyze which data points the model finds most confusing and prioritize collecting or generating more of that type of data.
How do we evaluate model success in a data-centric paradigm?
Answer: Move beyond a single aggregate accuracy metric on a static test set. The Inference Data Development pillar calls for a multi-faceted evaluation strategy [38]:
- Performance on Sliced Data: Report accuracy on semantically meaningful data slices (e.g., by patient subgroup, experimental batch, or disease severity).
- Robustness Metrics: Evaluate performance on OOD and adversarial test sets.
- Calibration: Measure how well the model's predicted probabilities match the true likelihood of correctness, which is critical for risk assessment in drug development.
- Fairness Audits: Use fairness metrics (e.g., demographic parity, equality of opportunity) across different subgroups.
How can we convince project stakeholders to invest in data-centric practices?
Answer: Frame the argument around risk mitigation, return on investment (ROI), and the critical goal of transferability to industry data.
- Cite Empirical Evidence: Reference studies like the one from Google which found that data cascades, which are preventable with DCAI, lead to significant technical debt and project failures [38].
- Run a Pilot Study: Demonstrate the value empirically. Take an existing model and, without changing its architecture, show how techniques like label cleaning or data augmentation can boost performance, especially on a test set designed to mimic real-world conditions.
- Highlight the Transferability Link: Emphasize that models trained on high-quality, diverse, and robust data are far more likely to work reliably when deployed in a real industry setting, such as a clinical research environment. This reduces the cost and time of post-deployment fixes.
Technical Support Center
Troubleshooting Guides
Guide 1: Addressing Accuracy Degradation After Pruning
Problem: A pruned model for molecular property prediction shows a significant drop in accuracy (e.g., >20% loss as noted in some studies [41]) compared to the original model.
Diagnosis: This is often caused by the aggressive removal of parameters critical for the model's task or insufficient fine-tuning after pruning.
Solution:
- Adopt an Iterative Pruning Strategy: Instead of removing a large percentage of parameters at once, progressively prune the model in smaller steps [42]. A recommended protocol is to prune ≤10% of the weights in a single cycle, followed by a short fine-tuning cycle, repeating until the target sparsity is reached [42] [43].
- Use a Calibrated Importance Metric: For transformer-based models in drug discovery, avoid simple magnitude-based pruning. Employ movement pruning, which considers both weight magnitude and the change in the loss function when a weight is dropped [42].
- Implement a Robust Fine-tuning Protocol: After pruning, fine-tune the model on your specific bioassay or molecular dataset. Use a lower learning rate (e.g., 1e-5) and a validation set to monitor for overfitting and ensure performance recovery [44].
Guide 2: Managing Performance Loss in Quantized Models for Molecular Dynamics
Problem: A quantized model used for molecular dynamics simulations or virtual screening exhibits unstable behavior or poor predictive performance.
Diagnosis: The loss of numerical precision from 32-bit floating points (FP32) to 8-bit integers (INT8) can introduce significant errors, especially in models not trained to handle lower precision [45] [41].
Solution:
- Switch to Quantization-Aware Training (QAT): If post-training quantization (PTQ) fails, integrate quantization simulations into the training loop. This allows the model to adapt to the lower precision, often preserving much higher accuracy [45] [43]. Frameworks like TensorFlow Lite and PyTorch provide QAT APIs.
- Apply Mixed-Precision Quantization: Do not quantize all layers uniformly. Identify sensitive layers (e.g., the final classification head) and keep them in higher precision (FP16 or FP32) while quantizing the rest of the model [43].
- Calibrate with a Representative Dataset: For PTQ, the calibration process is crucial. Use a diverse, task-specific subset of your data (e.g., a variety of molecular structures) to determine the optimal scaling factors for quantization [43].
Guide 3: Student Model Failing to Learn from Teacher in Distillation
Problem: In a knowledge distillation setup for a biomedical knowledge graph, the small student model does not converge or performs far worse than the teacher model.
Diagnosis: The performance gap may be too large, the student architecture may be inadequate, or the knowledge transfer method may be unsuitable for the task [46] [41].
Solution:
- Incorporate Intermediate Feature Matching: Move beyond simple output logit matching. Use feature-based distillation to align the intermediate representations (e.g., hidden layer activations) of the teacher and student models, providing richer learning signals [42] [44]. This has proven effective in graph-based distillation for drug repurposing [46].
- Adjust the Loss Weights: The total loss is often a weighted sum of the distillation loss and the standard cross-entropy loss with true labels. Experiment with the weighting factor (α) to balance learning from the teacher's soft labels and the ground-truth data [44].
- Validate the Student Model's Capacity: Ensure the student network has sufficient parameters and an appropriate architecture to capture the essential knowledge from the teacher. A student that is too small may be incapable of learning the task complexity.
Frequently Asked Questions (FAQs)
FAQ 1: Which compression technique is best for deploying a model on a limited-memory device at a clinical site?
For strict memory constraints, quantization is often the most effective single technique, as it can reduce model size by 75% or more by converting parameters from 32-bit to 8-bit precision [43]. For the smallest possible footprint, combine quantization with pruning to first reduce the number of parameters, then quantize the remaining weights [42] [41].
FAQ 2: Can these techniques be combined, and if so, what is the recommended order?
Yes, combining techniques typically yields the best results. A proven pipeline is:
- Knowledge Distillation: First, train a compact student model from a large teacher [42] [44].
- Pruning: Further compress the distilled student model by removing redundant parameters [42] [47].
- Quantization: Finally, reduce the numerical precision of the pruned model for deployment [42] [43]. This sequence builds efficiency incrementally while seeking to preserve task-specific accuracy.
FAQ 3: How can I quantitatively measure the efficiency gains from optimization?
Track these key metrics before and after optimization:
- Model Size: Reduction in disk space (MB/GB).
- Computational Complexity: Reduction in FLOPs (Floating Point Operations) or parameter count.
- Inference Speed: Latency reduction (milliseconds) on target hardware.
- Memory Usage: Lower peak RAM/VRAM consumption during inference.
- Energy Consumption: Measured in watts or joules; studies show compression can reduce energy use by 10-100x [42] [47].
FAQ 4: We have a proprietary model for toxicity prediction. Is it safe to apply these techniques?
Yes, these techniques modify the model's structure and numerical precision but do not typically expose the underlying training data. However, always validate the optimized model thoroughly on a comprehensive test set to ensure that critical predictive capabilities, especially for safety-critical tasks like toxicity prediction, have not been degraded [45].
Quantitative Data for Informed Decision-Making
Table 1: Performance and Efficiency Trade-offs of Compression Techniques on Transformer Models (Scientific Reports, 2025 [47])
| Model | Compression Technique | Accuracy (%) | F1-Score (%) | Energy Reduction (%) |
|---|---|---|---|---|
| BERT | Pruning + Distillation | 95.90 | 95.90 | 32.10 |
| DistilBERT | Pruning | 95.87 | 95.87 | -6.71* |
| ELECTRA | Pruning + Distillation | 95.92 | 95.92 | 23.93 |
| ALBERT | Quantization | 65.44 | 63.46 | 7.12 |
Note: The negative reduction for DistilBERT indicates an increase in energy use, highlighting that already-efficient models may not benefit from further compression.
Table 2: Comparative Analysis of Model Optimization Techniques
| Technique | Key Mechanism | Typical Model Size Reduction | Primary Use Case |
|---|---|---|---|
| Pruning | Removes unimportant weights or neurons [44] [41]. | Up to 40-60% [41] | Reducing computational complexity and inference latency. |
| Quantization | Lowers numerical precision of weights (e.g., FP32 to INT8) [45] [43]. | ~75% [43] | Drastically reducing memory footprint and power consumption. |
| Knowledge Distillation | Trains a small student model to mimic a large teacher [42] [46]. | 90-99% [42] | Creating a fundamentally smaller, faster architecture. |
Experimental Protocols
Protocol 1: Iterative Magnitude Pruning for a Predictive Model
This protocol is adapted from NVIDIA's workflow for pruning large language models, applicable to various deep learning models in drug discovery [44].
Objective: To reduce the size of a predictive model with minimal accuracy loss. Materials: Pre-trained model, training/validation dataset, hardware (e.g., GPU). Steps:
- Baseline Evaluation: Evaluate the original model on the validation set.
- Calibration: Run a small calibration dataset (e.g., 1024 samples) through the model to analyze weight magnitudes [44].
- Pruning Cycle:
- Identify and remove a small percentage (e.g., 10%) of weights with the smallest absolute values.
- Fine-tune the pruned model on the training data for a limited number of epochs with a reduced learning rate (e.g., 1/10 of the original) [44].
- Evaluation: Assess the pruned and fine-tuned model on the validation set.
- Iteration: Repeat steps 3-4 until the target sparsity or an unacceptable performance drop is reached.
Protocol 2: Knowledge Distillation for a Graph Neural Network
Based on a framework for drug repurposing, this protocol details how to transfer knowledge from a large teacher model to a compact student [46].
Objective: To create a compact student model that maintains high performance on a link prediction task in a biomedical knowledge graph. Materials: Trained teacher model, student model architecture, graph dataset (e.g., HetioNet). Steps:
- Teacher Outputs: Run the training data through the teacher model to generate soft target probabilities (logits) [44].
- Distillation Loss: Train the student model using a combined loss function:
- Feature-based Alignment (Optional): For enhanced performance, add a loss term that aligns intermediate feature maps between the teacher and student models [42] [46].
- Validation: Monitor the student's performance on a validation set independent of the teacher's training data.
Workflow and Pathway Visualizations
Model Optimization Decision Pathway
Knowledge Distillation Process Flow
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Tools and Frameworks for Model Optimization
| Tool / Framework | Type | Primary Function in Optimization | Application Example |
|---|---|---|---|
| TensorRT Model Optimizer (NVIDIA) [44] | Library | Provides pipelines for structured pruning and knowledge distillation of large models. | Pruning a 8B-parameter model down to 6B parameters for deployment [44]. |
| TensorFlow Lite / PyTorch Quantization [45] [43] | Library | Enables post-training quantization (PTQ) and quantization-aware training (QAT). | Deploying a virtual screening model on mobile devices with INT8 precision [45]. |
| CodeCarbon [47] | Utility | Tracks energy consumption and carbon emissions during model training and inference. | Quantifying the environmental benefit of using a compressed model for molecular dynamics [47]. |
| Optuna [43] | Framework | Automates hyperparameter optimization, crucial for fine-tuning after pruning or distillation. | Finding the optimal learning rate for fine-tuning a pruned toxicity predictor. |
| ONNX Runtime [45] [43] | Runtime | Provides a cross-platform environment for running quantized models with high performance. | Standardizing the deployment of an optimized model across different cloud and edge systems. |
The Rise of Small Language Models (SLMs) for Cost-Effective, Specialized Edge Deployment
SLM Technical Support Center
This support center provides practical guidance for researchers and scientists deploying Small Language Models (SLMs) in drug development environments. The content is framed within the broader thesis of enhancing model transferability to industrial research data.
Frequently Asked Questions (FAQs)
Q1: Why should our drug discovery team choose SLMs over larger models for our research? SLMs offer distinct advantages for the specialized, repetitive tasks common in pharmaceutical research [48] [49]:
- Cost Efficiency: Running an SLM can be 10x to 30x cheaper than a large frontier model, making advanced AI accessible for more projects and experiments [49].
- Operational Superiority: SLMs provide faster inference, lower GPU requirements, and the ability to be deployed on-edge, which is crucial for real-time analysis and preserving data privacy [50] [48].
- Specialization: SLMs can be finely tuned for specific tasks like intent classification, data extraction from lab reports, and generating structured outputs (e.g., JSON for tool calls), often matching or exceeding the accuracy of larger models on these narrow tasks [48] [49].
- Privacy and Compliance: On-device processing ensures sensitive research data, such as patient records or proprietary compound information, never leaves your secure environment, aiding compliance with regulations like HIPAA [51].
Q2: What are the most capable open-source SLMs available for research deployment in 2025? The field is evolving rapidly, but as of 2025, several models stand out for their balance of size and performance [50]:
| Model | Developer | Parameters | Core Strength | Ideal Use Case in Drug Development |
|---|---|---|---|---|
| Meta Llama 3.1 8B Instruct | Meta | 8 Billion | Industry-leading benchmark performance & multilingual support [50] | Analyzing diverse scientific literature and clinical data. |
| Qwen3-8B | Qwen | 8.2 Billion | Dual-mode reasoning & extensive 131K context window [50] | Processing long research documents and complex logical reasoning tasks. |
| GLM-4-9B-0414 | THUDM | 9 Billion | Code generation & function calling [50] | Automating data analysis scripts and integrating with lab instrumentation APIs. |
| NVIDIA Nemotron Nano 2 | NVIDIA | 9 Billion | High throughput (6x higher), low memory consumption [49] | High-volume, real-time data processing tasks on a single GPU. |
Q3: We have limited in-house data for a specific task. Can we still fine-tune an SLM effectively? Yes. Modern fine-tuning techniques like LoRA (Low-Rank Adaptation) or QLoRA are highly effective with small, high-quality datasets [48] [49]. Research indicates that with approximately 100 to several thousand curated examples, a well-tuned SLM can reach performance parity with a large LLM on specialized tasks [48]. The key is high-quality data curation and task-specific focus.
Q4: What is a "heterogeneous AI architecture" and how does it apply to our work? A heterogeneous architecture is a practical strategy that combines SLMs and LLMs, rather than relying on a single model for everything [49]. In this setup:
- SLMs act as efficient "workers," handling the vast majority of repetitive, predictable tasks like parsing commands, data extraction, and generating summaries [49].
- LLMs act as "consultants," reserved for situations that require broad, generalist knowledge, open-ended dialogue, or complex, multi-step problem-solving that cannot be easily decomposed [49]. This approach optimizes both cost and capability, ensuring you use the right tool for each job [49].
Troubleshooting Guides
Issue 1: Model Hallucinations or Inaccurate Outputs on Domain-Specific Data
- Problem: The SLM generates incorrect or nonsensical information when processing technical biomedical text or data.
- Solution:
- Fine-tune with Domain Data: Continue pre-training or fine-tune the SLM on a curated corpus of biomedical literature, clinical trial reports, and scientific papers relevant to your domain [52]. Models like BioGPT demonstrate the power of biomedical-specific training [52].
- Implement Retrieval-Augmented Generation (RAG): Ground the model's responses by connecting it to a vector database of verified, up-to-date internal knowledge bases (e.g., electronic lab notebooks, regulatory documents). This provides factual context for the model to draw from, reducing fabrications.
- Narrow the Task Scope: Re-cluster your usage data to ensure the SLM is being applied to a sufficiently narrow and well-defined task. Hallucinations often occur when a model's task is too vague or broad [48].
Issue 2: Slow Inference Speed on Edge Hardware
- Problem: The model's response time is too slow for real-time applications, even with a small model.
- Solution:
- Model Quantization: Convert the model's weights from 32-bit or 16-bit floating points to lower-precision formats like 8-bit integers (INT8) or even 4-bit (INT4). This drastically reduces memory footprint and increases inference speed.
- Model Compression: Apply techniques like pruning to remove redundant weights or neurons from the network that contribute little to the output.
- Hardware Check: Ensure your edge device has a compatible GPU (even a consumer-grade one) and that you are using optimized inference libraries like NVIDIA TensorRT.
Issue 3: High Fine-tuning Costs or Instability
- Problem: The process of fine-tuning the SLM is consuming too many computational resources or failing to converge.
- Solution:
- Use Parameter-Efficient Fine-Tuning (PEFT): Adopt methods like LoRA instead of full fine-tuning. LoRA freezes the pre-trained model weights and injects trainable rank-decomposition matrices into each layer of the Transformer architecture, reducing the number of trainable parameters by thousands of times [49].
- Curate Your Dataset: Focus on data quality over quantity. A smaller, clean, and well-labeled dataset is more effective for fine-tuning than a large, noisy one. Use the data curation and clustering process outlined in the experimental protocol below [48].
Experimental Protocols for SLM Implementation
This section provides a detailed, step-by-step methodology for transitioning from a generic LLM to a specialized SLM, based on industry research [48].
Protocol: A Five-Step Process for LLM-to-SLM Conversion
Objective: To systematically replace high-cost, general-purpose LLM calls with cost-effective, specialized SLMs for repetitive tasks in a research workflow.
Step-by-Step Methodology:
Secure Usage Data Collection:
- Action: Instrument your existing LLM-powered application to log all non-human-computer interaction (non-HCI) calls. Capture the prompts, the model's responses, and any tool usage.
- Data Security: Encrypt all logs at rest and in transit. Implement role-based access controls and strip any personally identifiable information (PII) or sensitive intellectual property immediately after collection to ensure compliance [48].
Data Curation and Filtering:
- Action: Automatically scan the collected logs to flag and remove any remaining sensitive content. Filter out failed or malformed prompts and responses.
- Outcome: The goal is to create a high-quality, sanitized dataset of 10,000 to 100,000 examples, which has been shown to be sufficient for fine-tuning SLMs on specific tasks [48]. Version this dataset for traceability.
Task Clustering and Pattern Identification:
- Action: Use unsupervised clustering algorithms (e.g., based on cosine similarity of sentence embeddings) on the curated prompts to identify natural groupings of repetitive tasks [48].
- Outcome: Research shows that fewer than 12 clusters often account for over 80% of all agent calls. Common clusters in research include "intent classification," "entity extraction from lab reports," and "JSON-formatted summarization" [48]. Validate these clusters by manual sampling.
SLM Selection and Evaluation:
- Action: Select 2-3 candidate SLMs (e.g., from the table in FAQ #2) based on license, size (aim for 1B-8B parameters), and general benchmark performance.
- Testing: Create a benchmark test set from your clustered tasks. Evaluate each candidate model on accuracy, token throughput (speed), and latency on your target hardware (e.g., a single A10 GPU). Choose the model that offers the best balance of performance and efficiency for your specific domain [48].
Specialized Training and Deployment:
- Action: Fine-tune the selected SLM for each identified task cluster using efficient methods like LoRA or QLoRA [49].
- Deployment: Deploy the fine-tuned models behind a feature flag or router. A/B test them against your original LLM baseline, monitoring for accuracy, latency, and cost savings. Use the data logging from Step 1 to continuously monitor for performance drift and identify new tasks for optimization [48].
The Scientist's Toolkit: Essential Research Reagents for SLM Deployment
This table details key software and hardware "reagents" required for successful SLM experimentation and deployment.
| Research Reagent | Category | Function & Explanation |
|---|---|---|
| NVIDIA NeMo | Software Framework | An end-to-end platform for curating data, customizing models, and managing the entire AI lifecycle. Essential for streamlining the fine-tuning and deployment process [49]. |
| LoRA / QLoRA | Fine-tuning Technique | Parameter-efficient fine-tuning methods that dramatically reduce computational costs and time by updating only a small subset of model parameters, making SLM specialization feasible for small teams [49]. |
| Sentence Transformers | Data Analysis Library | A Python library used to generate sentence embeddings, which is the foundational step for the task clustering described in Step 3 of the experimental protocol. |
| Consumer-Grade GPU (e.g., NVIDIA RTX 4090) | Hardware | Powerful enough to run inference and fine-tuning for many SLMs, enabling local development and prototyping without requiring large cloud compute budgets [49]. |
| Vector Database (e.g., Chroma, Weaviate) | Data Infrastructure | Stores and retrieves embeddings for implementing Retrieval-Augmented Generation (RAG), which is a critical technique for improving accuracy and reducing hallucinations in domain-specific applications. |
Hybrid Architecture for Model Orchestration
A hybrid architecture ensures that SLMs and LLMs are used optimally within a single system [49].
Implementing MLOps and LLMOps for Scalable, Production-Ready Model Management
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: For a new drug discovery project aiming to analyze structured assay data and also generate natural language summaries of findings, should we use MLOps, LLMOps, or both?
For this hybrid use case, a combined strategy is recommended. Use MLOps to manage the predictive models that process your structured assay data for tasks like toxicity prediction or compound affinity scoring [53]. Concurrently, use LLMOps to manage the large language model that generates the natural language summaries, ensuring coherent and accurate reporting [53] [54]. This approach allows you to leverage the precision of MLOps for numerical data and the linguistic capabilities of LLMOps for content generation.
Q2: Our fine-tuned LLM for scientific literature review is starting to produce factually incorrect summaries (hallucinations). What is the immediate troubleshooting protocol?
Your action plan should be:
- Audit your Retrieval-Augmented Generation (RAG) system: Check the retrieval component for failures. Ensure the vector database is returning relevant and accurate context from your knowledge base [55] [56].
- Evaluate prompt effectiveness: A poorly designed prompt can lead to hallucinations. Test and version different prompt strategies to guide the model toward more factual responses [55] [57].
- Review recent model or data changes: If you recently updated the model or its underlying data, roll back to a previous version to isolate the issue. Version control for prompts, models, and knowledge sources is critical [53] [55].
Q3: We are struggling with model performance degradation (model drift) after deploying a predictive biomarker identification model. Our current MLOps setup only monitors accuracy. What else should we track?
Accuracy alone is insufficient. Expand your monitoring to include:
- Data Drift: Monitor the statistical properties of the input data (feature distribution) to detect significant shifts from the training data [58] [54].
- Concept Drift: Monitor the relationship between the model's inputs and outputs, as this can change over time even if the input data distribution remains stable [56]. Implementing proactive alerts for these metrics will allow you to trigger model retraining before performance degrades critically [58].
Q4: How do we manage the high computational cost of running our LLM for generating patient cohort reports?
Cost management in LLMOps requires a multi-pronged approach:
- Optimize Prompts: Inefficient, lengthy prompts consume more tokens and drive up costs. Implement prompt engineering and optimization to reduce token usage [59] [56].
- Model Selection: Evaluate if a smaller, more specialized open-source model can perform the task at a lower inference cost compared to a large, general-purpose model [59] [55].
- Token Monitoring: Use specialized LLM monitoring tools to track token consumption across different processes and users, identifying areas for efficiency gains [55]. One source suggests that with an LLM Gateway, organizations can cut token spend by 30-50% without sacrificing performance [56].
Q5: What is the fundamental difference between versioning in MLOps and LLMOps?
In MLOps, versioning is predominantly focused on the model's code, the datasets used for training, and the model weights themselves [53]. In LLMOps, while model versioning is still important, the scope expands significantly. You must also version prompts, the knowledge bases (e.g., vector databases) used for retrieval, and the context provided to the model [53] [55]. A minor change in a prompt can drastically alter the model's output, making its versioning as crucial as code versioning [57].
Troubleshooting Guides
Scenario 1: LLM Hallucination and Factual Inaccuracy
| Step | Action | Diagnostic Tool/Metric | Expected Outcome |
|---|---|---|---|
| 1 | Verify Retrieval Quality | Check the top-k retrieved chunks from your vector database for relevance and accuracy. | Confirmation that the source data provided to the LLM is correct. |
| 2 | Improve Prompt Design | Implement and A/B test prompts with clear instructions to cite sources and state uncertainty. | Reduction in unsupported claims; increased citation of provided context. |
| 3 | Implement Output Guardrails | Use a model-based evaluator to score each generated response for factual accuracy against the source. | Automatic flagging or filtering of responses with low factual accuracy scores. |
Scenario 2: Traditional ML Model Performance Degradation (Drift)
| Step | Action | Diagnostic Tool/Metric | Expected Outcome |
|---|---|---|---|
| 1 | Detect Drift | Use statistical tests (e.g., PSI, KS) to monitor input feature distributions (data drift) and target variable relationships (concept drift). | Alerts triggered when drift metrics exceed a predefined threshold. |
| 2 | Isolate Root Cause | Analyze feature importance and correlation shifts to identify which features are causing the drift. | A shortlist of problematic features and potential data pipeline issues. |
| 3 | Retrain & Validate | Trigger automated model retraining with new data and validate performance on a hold-out set. | Restoration of model performance metrics (e.g., AUC, F1-score) to acceptable levels. |
Comparative Data Analysis
Table 1: MLOps vs. LLMOps Operational Characteristics
| Dimension | MLOps | LLMOps |
|---|---|---|
| Primary Use Cases | Prediction, scoring, classification, forecasting [53] | Conversation, reasoning, content generation, summarization [53] |
| Data Type | Structured, tabular data [53] [56] | Unstructured natural language, documents [53] [56] |
| Key Performance Metrics | Accuracy, AUC, F1-score, Precision, Recall [53] [59] | BLEU, ROUGE, Relevance, Helpfulness, Factual Accuracy [53] [59] |
| Primary Cost Center | Model training and retraining [59] [56] | Model inference (token usage) and serving [59] [56] |
| Versioning Focus | Model code, data, features, and weights [53] | Prompts, knowledge sources, context, and model [53] [55] |
| Common Risks | Data bias, model drift [53] [58] | Hallucinations, prompt injection, toxic output [53] [55] |
Table 2: Key Research Reagent Solutions for AI Model Management
| Tool Category | Example Solutions | Primary Function in Experiments |
|---|---|---|
| Experiment Tracking | MLflow, Weights & Biases, Comet ML [55] | Logs experiments, tracks hyperparameters, and compares different model and prompt versions. |
| Vector Databases | Pinecone, Weaviate, FAISS [53] [55] | Stores and retrieves embeddings for semantic search, a core component of RAG systems. |
| Prompt Management | LangSmith, PromptLayer [53] [60] | Versions, tests, and manages prompts to ensure consistency and optimize performance. |
| Orchestration & Deployment | Kubeflow, Ray, BentoML [53] [55] | Orchestrates complex ML/LLM workflows and provides robust model serving capabilities. |
| LLMOps Platforms | Arize AI, Whylabs [55] [60] | Specialized platforms for monitoring LLMs, detecting drift, hallucinations, and managing token cost. |
Experimental Protocols & Workflows
Protocol 1: Fine-Tuning an LLM with Parameter-Efficient Fine-Tuning (PEFT)
Objective: Adapt a general-purpose foundation LLM (e.g., LLaMA, Mistral) to a specialized domain (e.g., biomedical text) using limited computational resources.
Methodology:
- Model and Tokenizer Loading: Load a pre-trained model and its corresponding tokenizer from the Hugging Face Transformers library [55].
- PEFT Configuration: Define a Low-Rank Adaptation (LoRA) configuration. This specifies how the model will be adapted, typically by setting the rank
r, the LoRA alpha, and the target modules within the transformer architecture (e.g.,q_proj,v_proj) [55]. - Model Wrapping: Wrap the base model with the PEFT configuration using
get_peft_model. This creates a new model where only the LoRA parameters are trainable, drastically reducing the number of parameters that require updating [55]. - Training: Prepare a domain-specific dataset (e.g., PubMed abstracts), tokenize it, and train the PEFT model using a standard trainer (e.g., Hugging Face Trainer). The training will update only the small set of LoRA parameters [55].
Protocol 2: Implementing a Retrieval-Augmented Generation (RAG) System
Objective: Ground an LLM's responses in a private, up-to-date knowledge base to reduce hallucinations and improve factual accuracy.
Methodology:
- Knowledge Base Ingestion: Chunk internal documents (e.g., research papers, lab protocols) into manageable sections.
- Vectorization: Generate embeddings for each text chunk using an embedding model (e.g., all-MiniLM-L6-v2) and store them in a vector database [55] [56].
- Retrieval: For a user query, compute its embedding and perform a similarity search in the vector database to retrieve the most relevant text chunks.
- Synthesis: Construct a prompt that includes the user's query and the retrieved context, then send it to the LLM to generate a grounded, context-aware response [55] [56].
Workflow Visualizations
Diagram 1: Core MLOps Workflow for Predictive Models
Diagram 2: Core LLMOps Workflow for Language Models
Solving Real-World Hurdles: A Troubleshooting Guide for Deployment
Diagnosing and Mitigating Performance Degradation in Production
Frequently Asked Questions (FAQs)
Q1: What are the most common categories of performance issues I should investigate first? Performance issues can be broadly categorized to streamline troubleshooting. The three primary categories are:
- Frontend Issues: User-facing problems such as slow page loads, unresponsive interfaces, and slow data rendering.
- Backend Issues: Server-side problems including slow database queries, API timeouts, and delayed data processing.
- Infrastructure Issues: Problems related to the underlying environment, including network latency, server misconfigurations, and insufficient compute resources [61].
Q2: How can I determine if my model's performance degradation is due to data-related issues? A key factor is the generalization gap. If your model performs well on its original training or test data but poorly on new industry data, it often indicates a data shift or lack of transferability. This is common in drug discovery when models trained on standardized research datasets (e.g., GDSC) fail on real-world clinical data or new experimental batches due to differences in data distribution, experimental settings, or biological context [62] [63]. Conducting a thorough audit of the new data's properties (e.g., dose ranges, cell line origins, feature distributions) against the training data is a critical first diagnostic step [62].
Q3: What is a quick win to improve the performance of a data-heavy application? Limiting data retrieval is one of the most effective strategies. Instead of loading large datasets, show a manageable amount of data by default and provide users with robust search and filter capabilities. This reduces load on the database, network, and frontend, leading to significantly faster response times [64].
Q4: Why is transferability a major focus in computational drug discovery? In real-world drug discovery, researchers constantly work with newly discovered protein targets or newly developed drug compounds. Models that have only been tested on data they were trained on lack the generalizability required for these practical scenarios. Enhancing transferability is therefore fundamental for models to be useful in predicting interactions for novel drugs and targets, directly accelerating the drug discovery pipeline [22] [62].
Troubleshooting Guides
Guide 1: Diagnosing General Application Performance Issues
This guide outlines a systematic approach to identify common bottlenecks in production applications.
Step 1: Reproduce and Monitor Reproduce the performance issue in a staging environment that mirrors production as closely as possible. Use Application Performance Monitoring (APM) tools to get real-time visibility into server CPU, memory, database queries, and API response times [61].
Step 2: Isolate the Component Use monitoring data to isolate the problematic component. Check if the bottleneck is in the frontend, backend, or infrastructure.
Step 3: Analyze and Identify Root Cause
- For Database Bottlenecks: Identify slow-running queries using profiling tools. Look for missing indexes on frequently queried fields, a lack of pagination, or expensive operations like full table scans [61].
- For Inefficient Code: Use profiling tools to trace bottlenecks to specific functions or lines of code. Look for redundant operations, high-complexity algorithms (e.g., O(n²) loops), or memory leaks from unreleased object references [61].
- For Infrastructure Issues:
Step 4: Implement Mitigation
The workflow below summarizes the diagnostic process:
Guide 2: Mitigating Model Transferability Issues in Drug Discovery
This guide addresses the specific challenge of maintaining model performance when applying it to new, industry-grade data.
Step 1: Benchmark and Audit Performance Establish performance benchmarks on your original dataset. When introducing new data (e.g., from a different lab or clinical setting), run a performance audit to quantify the degradation. Track metrics like Root Mean Square Error (RMSE) and Pearson Correlation (PC) across different data segments [63].
Step 2: Identify the Source of Variability The degradation often stems from experimental variability between datasets. Key sources include:
- Dose-Response Settings: Differences in the number of doses, dose ranges, and dose-response matrices (e.g., 4x4 vs. 5x5) [62].
- Cell Line and Drug Overlap: Scarcity of overlapping compounds and cell lines between the training study and the new industrial data [62].
- Summary Metrics: Reliance on summary monotherapy measurements (e.g., IC50) which can have poor cross-dataset reproducibility [62].
Step 3: Apply Data Harmonization Techniques Harmonize data across different studies to improve model transferability.
- Curve Standardization: Normalize the complete dose-response curves instead of relying solely on summary metrics like IC50. This better captures the full pharmacodynamic profile [62].
- Use Transferable Features: Incorporate chemical structure-derived fingerprints (e.g., ECFP) and gene expression profiles, which are more consistent across studies than experimental summaries [62] [63].
Step 4: Leverage Advanced Modeling Strategies
- Transfer Learning: Use pre-trained models (e.g., ChemBERTa, GIN) on large-scale molecular datasets to learn robust drug representations. Fine-tune these models on your specific task to improve generalization, especially with limited labeled data [63].
- Multi-Modal Fusion: Integrate multiple representations of drugs (SMILES, molecular graphs, fingerprints) and cell lines (genetic mutations, expression data). Use attention-based fusion mechanisms (e.g., self-attention, cross-attention) to effectively combine these modalities and capture complex interactions [22] [63].
The following workflow illustrates a strategy for improving model transferability:
Quantitative Data and Experimental Protocols
Table 1: User Perception of Application Response Times
This table helps set performance targets by linking response times to user experience [64].
| Response Time | User Perception |
|---|---|
| 0–100 ms | Instantaneous |
| 100–300 ms | Slight perceptible delay |
| 300 ms–1 sec | Noticeable delay |
| 1–5 sec | Acceptable delay |
| 5–10 sec | Noticeable wait; attention may wander |
| 10 sec or more | Significant delay; may lead to abandonment |
Table 2: Reproducibility of Drug Combination Scores Across Studies
This data highlights the challenge of transferability, showing how key metrics can vary between experimental datasets [62].
| Score Type | Intra-Study Reproducibility (Pearson's r) | Inter-Study Reproducibility (Pearson's r) |
|---|---|---|
| CSS (Sensitivity) | 0.93 (O'Neil dataset) | 0.342 |
| S (Synergy) | 0.929 (O'Neil dataset) | 0.20 |
| Loewe (Synergy) | 0.938 (O'Neil dataset) | 0.25 |
| ZIP (Synergy) | 0.752 (O'Neil dataset) | 0.09 |
Table 3: Performance of TransCDR Model Under Different Scenarios
This table demonstrates the expected performance drop in "cold start" scenarios, which simulate real-world application on novel data [63].
| Scenario | Description | Performance (Pearson Correlation) |
|---|---|---|
| Warm Start | Predicting for known drugs & cell lines | 0.9362 ± 0.0014 |
| Cold Cell | Predicting for unseen cell line clusters | 0.8639 ± 0.0103 |
| Cold Drug | Predicting for unseen drugs | 0.5467 ± 0.1586 |
| Cold Scaffold | Predicting for drugs with novel scaffolds | 0.4816 ± 0.1433 |
Experimental Protocol: Cross-Study Validation for Model Generalizability
This protocol provides a methodology for rigorously testing a model's transferability to new data [62].
- Dataset Selection: Select multiple large-scale drug screening studies (e.g., ALMANAC, O'Neil, FORCINA).
- Data Preprocessing:
- Feature Extraction: For each drug, generate chemical structure-derived fingerprints. For each cell line, collect gene expression data (e.g., 273 essential cancer genes).
- Dose-Response Harmonization: Normalize the raw dose-response curves from different studies to a standard range to mitigate variability from differing experimental doses.
- Response Labeling: Calculate relevant response scores, such as Combination Sensitivity Score (CSS) or synergy scores (Bliss, Loewe, ZIP).
- Validation Strategy:
- Intra-Study Validation: Train a model (e.g., LightGBM) on a subset of a single dataset and test it on a held-out portion of the same dataset, ensuring no overlap in treatment-cell line combinations.
- Inter-Study Validation:
- "1 vs 1": Train a model on one full dataset and test it on another.
- "3 vs 1": Train a model on three combined datasets and test it on the remaining one.
- Performance Evaluation: Compare the model's performance (e.g., Pearson's correlation coefficient) between intra-study and inter-study validations. A significant drop in inter-study performance indicates poor transferability.
The Scientist's Toolkit: Essential Research Reagents & Solutions
This table lists essential data types and computational tools used in developing transferable models.
| Item | Function & Application |
|---|---|
| Chemical Fingerprints (ECFP) | A vector representation of a drug's molecular structure that is computationally efficient and facilitates comparison and prediction for novel compounds [62] [63]. |
| Pre-trained Language Models (ChemBERTa) | A transformer model pre-trained on vast corpora of SMILES strings. It can be fine-tuned for specific tasks like drug response prediction, improving performance especially with limited data [63]. |
| Graph Neural Networks (GIN) | A type of graph neural network effective at learning representations from molecular graphs. Pre-trained GIN models can capture rich structural information for downstream tasks [63]. |
| Public Drug Screening Datasets (GDSC, CCLE) | Large-scale databases providing drug sensitivity measurements for hundreds of cancer cell lines. Used as benchmark sources for training and validating predictive models [63]. |
| Dose-Response Curve Harmonization | A computational method to standardize dose-response data from different experimental settings, which is crucial for improving model performance across studies [62]. |
| Multi-Modal Fusion (Attention Mechanism) | A deep learning technique that integrates multiple data types (e.g., drug graphs, cell line mutations) by dynamically weighting the importance of each feature, enhancing predictive accuracy [22] [63]. |
Troubleshooting Guides
Guide 1: Diagnosing and Remedying Overfitting in Predictive Models
Problem: My model performs excellently on training data but poorly on unseen validation/test data, indicating poor generalization.
Diagnosis Steps:
- Monitor Performance Metrics: Track metrics like loss or accuracy on both training and a separate validation set throughout the training process. A growing gap between training and validation performance is a key indicator of overfitting [66] [67].
- Analyze Learning Curves: Plot training and validation loss against the number of training epochs. Overfitting is characterized by a continuous decrease in training loss while validation loss begins to increase after a certain point [66].
- Check Feature Importance: If using methods like Decision Trees, inspect the feature importance scores. High importance assigned to features known to be noise or irrelevant is a strong sign of overfitting [68].
Solutions:
- Apply Regularization: Introduce L1 (Lasso) or L2 (Ridge) regularization to the model's cost function. This penalizes overly complex models by pushing coefficient estimates towards zero, preventing them from taking extreme values based on noise [66] [67].
- Implement Early Stopping: Halt the training process when the validation loss stops decreasing for a predetermined number of epochs. The model at that point is likely to have the best generalization performance [66] [67].
- Simplify the Model: Reduce model complexity by using a model with fewer parameters (e.g., fewer layers or fewer units per layer in a neural network) [66] [67].
- Use Dropout: For neural networks, apply dropout during training. This technique randomly "drops" a subset of units in a layer, preventing complex co-adaptations and forcing the network to learn more robust features [66].
Guide 2: Addressing Poor Generalization to Unseen Drugs in DDI Models
Problem: My structure-based Drug-Drug Interaction (DDI) prediction model generalizes poorly to new, unseen drug compounds.
Diagnosis Steps:
- Evaluate with Rigorous Data Splits: Assess the model using a data splitting strategy (e.g., splitting by drug, not by interaction pairs) that ensures drugs in the test set are entirely absent from the training set. This simulates a real-world scenario and reveals true generalization capability [69].
- Analyze Per-Phenotype Performance: Instead of relying only on aggregated performance metrics, examine accuracy for individual DDI phenotypes. Performance is often uneven, and aggregated results can hide severe failures on rare but critical interactions [69].
Solutions:
- Employ Data Augmentation: Artificially expand your training dataset by creating modified versions of existing molecular data. This can help the model learn more invariant features and mitigate overfitting [66] [69].
- Leverage Transfer Learning: Start with a model pre-trained on a large, general molecular dataset. Then, fine-tune it on your specific, smaller DDI dataset. This allows the model to leverage general chemical knowledge without needing to learn everything from a limited dataset [70].
Frequently Asked Questions
FAQ 1: What is the fundamental trade-off between bias and variance, and how does it relate to overfitting?
The bias-variance tradeoff is a core concept in machine learning. Bias is the error from erroneous assumptions in the model; a high-bias model is too simple and underfits the data, failing to capture relevant patterns. Variance is the error from sensitivity to small fluctuations in the training set; a high-variance model is too complex and overfits, learning the noise in the data [67].
- High Bias (Underfitting): Model is too simple. Performs poorly on both training and test data [67].
- High Variance (Overfitting): Model is too complex. Performs well on training data but poorly on test data [67].
The goal is to find a balance where both bias and variance are minimized for optimal generalization [67].
FAQ 2: How can I control overfitting without changing my model's architecture or the learning rate and batch size?
You can use noise enhancement techniques. Deliberately introducing a controlled amount of noise during training can act as a regularizer. For example, adding noise to labels during gradient updates can suppress the model's tendency to memorize noisy labels, especially in low signal-to-noise ratio regimes, thereby improving generalization [71] [72]. This provides a way to increase the effective noise in SGD without altering the core hyperparameters.
FAQ 3: My dataset has a large amount of historical data with basic features and a small amount of recent data with new, predictive features. How can I build a robust model without discarding the large historical dataset?
A boosting-for-transfer approach can be effective [73].
- First, train a model (e.g., a Gradient Boosting Machine) on the large historical dataset using only the basic features.
- Then, use this model's errors on the smaller, newer dataset to compute weights for the samples, emphasizing the samples the first model got wrong.
- Finally, train a second model on the newer dataset (with all features) using these weights. The final prediction is the sum of the predictions from both models. This transfers knowledge from the large dataset while leveraging the new features [73].
FAQ 4: How does feature selection help prevent overfitting, and what are the risks?
Feature selection reduces the number of input features, which directly lowers model complexity and training time, helping to prevent overfitting [66] [68]. However, if the model is already overfitting, it can corrupt the feature selection process itself [68]. An overfit model can produce unstable feature importance rankings, cause you to discard genuinely relevant features, or select irrelevant features due to learned noise, ultimately leading to poor generalization [68]. Therefore, it is crucial to apply regularization and use robust validation schemes during the feature selection process.
| Technique | Category | Key Mechanism | Ideal Use Case | Considerations |
|---|---|---|---|---|
| L1/L2 Regularization [66] | Learning Algorithm | Adds penalty to loss function to constrain model coefficients. | Models with many features (high-dimensional data). | L1 can zero out weights, L2 shrinks them. |
| Dropout [66] | Model | Randomly drops units during training to prevent co-adaptation. | Deep Neural Networks of various architectures. | Increases training time; requires more epochs. |
| Early Stopping [66] | Model | Halts training when validation performance degrades. | Iterative models like NNs and GBDT; easy to implement. | Requires a validation set; need to save best model. |
| Data Augmentation [66] [69] | Data | Artificially increases training data via label-preserving transformations. | Image, text, and molecular data; limited data scenarios. | Must be relevant to the task and preserve label meaning. |
| Label Noise GD [72] | Learning Algorithm | Injects noise into labels during training for implicit regularization. | Data with low signal-to-noise ratio (SNR) or noisy labels. | Can improve generalization where standard SGD fails. |
| Transfer Learning [70] | Model/Domain | Leverages knowledge from a pre-trained model for a new, related task. | Small target datasets; availability of pre-trained models. | Risk of negative transfer if domains are too dissimilar. |
Table 2: Essential Research Reagent Solutions for Robust ML Experiments
| Reagent / Solution | Function in Experiment |
|---|---|
| Hold-Out Validation Set [66] | A subset of data not used for training, reserved to evaluate model performance and detect overfitting. |
| Pre-trained Models (e.g., VGG, BERT) [70] | Models previously trained on large datasets (e.g., ImageNet, Wikipedia) used as a starting point for transfer learning, saving time and resources. |
| K-Fold Cross-Validation [66] | A resampling procedure that provides a more robust estimate of model performance by using all data for both training and validation across multiple rounds. |
| Data Augmentation Pipeline [66] | A defined set of operations (e.g., rotation, flipping for images; synonym replacement for text) to systematically create expanded training datasets. |
| Feature Selection Algorithm [66] [68] | A method (e.g., filter, wrapper, embedded) to identify and retain the most relevant features, reducing dimensionality and model complexity. |
Methodologies and Workflows
Workflow 1: Protocol for Implementing Label Noise Gradient Descent
Objective: To improve the generalization of a neural network model on a dataset with a low signal-to-noise ratio or inherently noisy labels.
Methodology:
- Standard Training Baseline: Train your model using standard Gradient Descent (GD) or Stochastic Gradient Descent (SGD) on your dataset. Record the final test error.
- Label Noise Injection: Modify the training algorithm to introduce noise into the labels used for each gradient update. In its simplest form, for a batch of data with labels
y, a corrupted labely'can be generated (e.g., by randomly flipping a subset of labels with a given probability). - Noisy Label Training: Train the model using the same hyperparameters as the baseline, but now using the noisy labels
y'for the gradient calculation in each step. - Evaluation and Comparison: Evaluate the model trained with label noise on the same clean test set. Compare the test error with the baseline model.
Expected Outcome: In low-SNR regimes, the model trained with label noise GD should demonstrate a lower test error and better generalization by suppressing the memorization of the noisy labels, unlike standard GD which tends to overfit to the noise [72].
Workflow 2: Protocol for Transfer Learning via Fine-tuning
Objective: To achieve high performance on a specific target task with a relatively small dataset by leveraging a model pre-trained on a large, general source dataset.
Methodology:
- Base Model Selection: Choose a pre-trained model (e.g., VGG16 for images, BERT for NLP) that was trained on a large benchmark dataset for a related but broader task [70].
- Model Adaptation:
- Remove Top Layers: Remove the final classification/regression layers of the pre-trained model.
- Add New Layers: Add new, randomly initialized layers that are suited to the number of classes in your target task.
- Layer Freezing (Optional): Initially, freeze the weights of the earlier (pre-trained) layers. These layers capture general features (like edges or basic syntax). Train only the newly added top layers on your target dataset. This prevents overfitting to a small dataset by destroying the useful pre-trained features [70].
- Fine-Tuning: Unfreeze some or all of the pre-trained layers and continue training the entire model on your target dataset. Use a very low learning rate to make small, careful adjustments to the pre-trained weights, allowing them to adapt to the specifics of the new task without catastrophic forgetting [70].
Tackling Computational and Latency Constraints for Real-Time Applications
Technical Support Center
Troubleshooting Guides
Guide 1: Diagnosing and Resolving High Inference Latency
Problem: AI model responds too slowly for real-time drug discovery tasks like molecular docking or high-content screen analysis.
Investigation & Resolution:
| Step | Action | Expected Outcome |
|---|---|---|
| 1 | Check Time to First Byte (TTFB) and end-to-end latency using monitoring code [74]. | Identify if delay is in data transfer, pre-processing, or model inference. |
| 2 | Profile model inference speed using framework-specific tools. Is the model itself the bottleneck? [75] | Pinpoint whether the model's size or architecture is the primary cause. |
| 3 | If the model is too slow, apply model optimization techniques:- Quantization: Reduce numerical precision from 32-bit to 16-bit or 8-bit [43] [76].- Pruning: Remove redundant or low-importance weights from the network [43] [75]. | A significantly smaller, faster model with minimal accuracy loss [43]. |
| 4 | Evaluate hardware utilization. Ensure the system is using specialized accelerators like GPUs or TPUs effectively [75] [76]. | Higher computational throughput and lower latency. |
This workflow helps systematically isolate the source of latency, from data input to model output.
Guide 2: Addressing Data Pipeline Delays in Real-Time Analysis
Problem: System cannot ingest and pre-process high-volume sensor or imaging data (e.g., from high-content screens) fast enough for real-time model input.
Investigation & Resolution:
| Step | Action | Expected Outcome |
|---|---|---|
| 1 | Use asynchronous I/O operations to decouple data ingestion from processing [75]. | Pre-processing no longer blocks data acquisition, smoothing data flow. |
| 2 | Implement data caching for frequently accessed data or pre-processing results [75]. | Reduced time to fetch and transform repetitive data. |
| 3 | Introduce edge computing or edge processing to handle pre-processing closer to the data source [75] [76]. | Drastic reduction in network transmission delay and core system load. |
| 4 | Optimize data serialization; switch from JSON to formats like Protocol Buffers for smaller payloads [74]. | Faster data transfer between system components. |
This workflow parallelizes data handling and moves computation closer to the source to minimize delays.
Frequently Asked Questions (FAQs)
Q1: In the context of drug discovery, what is considered "low latency" for an AI model analyzing live cell imaging data?
A: While benchmarks vary by application, for real-time analysis of cellular responses, a latency of under 20 milliseconds is often required to keep pace with data generation and enable immediate feedback for adaptive experiments [74]. For slightly less time-critical tasks, such as analyzing batches of pre-recorded images for phenotypic screening, latencies of a few hundred milliseconds may be acceptable [74]. The key is to align latency targets with the specific experimental timeline.
Q2: We need to deploy a pre-trained generative model for molecular design on our local servers (on-premise) to ensure data privacy. How can we optimize it for faster inference without expensive new hardware?
A: You can employ several software- and model-focused techniques to boost performance on existing hardware [77]:
- Post-Training Quantization (PTQ): Convert your model's weights from 32-bit floating-point numbers to 16-bit or 8-bit integers. This can reduce model size and speed up inference significantly [43].
- Pruning: Systematically remove connections in the neural network that have minimal impact on the output, creating a sparser and faster model [43].
- Framework Optimization: Use inference-optimized runtimes like TensorRT or OpenVINO that are designed to maximize performance on your specific CPU or GPU architecture [43].
Q3: Our federated learning project across multiple research labs is slowed down by synchronizing large model updates. What strategies can help reduce this communication bottleneck?
A: Federated learning introduces unique latency challenges from synchronizing local models and handling non-IID data [78]. To mitigate this:
- Increase Local Epochs: Allow participant models to perform more training steps on their local data before submitting updates, reducing the frequency of communication [78].
- Use Compression: Apply compression techniques to the model updates before sending them over the network [75].
- Implement Advanced Aggregation: Consider asynchronous aggregation methods instead of waiting for all nodes, which can help if some nodes are significantly slower than others [78].
Q4: When optimizing a model for latency, how much accuracy loss is acceptable before it impacts the scientific validity of our results in target identification?
A: This is a critical question. The concept of "sufficient accuracy" is key [75]. A marginal reduction in prediction quality (e.g., a 1-2% drop in AUC) is often acceptable if it yields a dramatic latency benefit that enables real-time analysis or high-throughput screening that wasn't previously possible. The trade-off must be evaluated against the specific tolerance of your experimental workflow and downstream decision-making processes [75]. The goal is model efficacy in a real-world pipeline, not just standalone metric maximization.
The Scientist's Toolkit: Research Reagent Solutions
This table details key computational tools and platforms essential for implementing the low-latency strategies discussed.
| Tool / Solution | Function in Latency Constraint Research |
|---|---|
| OpenVINO Toolkit | Optimizes and deploys deep learning models for fast inference on Intel hardware, crucial for on-premise deployment [43]. |
| TensorRT | An SDK for high-performance deep learning inference on NVIDIA GPUs, using quantization and graph optimization to minimize latency [43]. |
| Edge TPU (Google) | An ASIC chip designed to run AI models at high speed on edge devices, enabling local, low-latency processing of sensor data [76]. |
| Optuna | An open-source hyperparameter optimization framework that automates the search for model configurations that balance accuracy and speed [43]. |
| Nuclera's eProtein Discovery System | An example of domain-specific integrated automation that accelerates protein expression from days to hours, representing a hardware-software solution to a key bottleneck [79]. |
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: What are the most common organizational hurdles when implementing Machine Learning (ML) in drug development research?
Organizations frequently face several interconnected hurdles, including:
- Lack of ML Expertise: A shortage of skilled and interdisciplinary workers creates hiring and retention challenges for drug companies [80].
- Resistance to Change: Organizational skepticism and slow acceptance can hinder the adoption of new computational approaches like ML and Model-Informed Drug Discovery and Development (MID3) [34] [81].
- Data Challenges: A lack of high-quality, machine-readable data, along with difficulties in accessing and sharing data due to costs, legal issues, and a lack of incentives, severely limits ML effectiveness [80].
- Regulatory Uncertainty: Uncertainty about how regulators will review ML algorithms used in drug development may limit investment and adoption in this field [80].
Q2: How can we demonstrate the value of ML to skeptical internal stakeholders to overcome resistance?
You can build your case by highlighting quantitative benefits demonstrated in the industry:
- Cost and Time Savings: Some companies have reported significant cost savings (e.g., $0.5 billion) and reductions in annual clinical trial budgets (e.g., $100 million) through the impact of advanced modeling and simulation, which includes ML approaches [33].
- Increased Success Rates: One major pharmaceutical company reported that systematic use of Model-Informed Drug Development (MIDD), a field that incorporates ML, saved an average of 10 months per development program [82].
- Discovery Acceleration: ML can screen more chemical compounds and zero in on promising drug candidates in less time than the current process, directly addressing the issue of lengthy 10-15 year development timelines [80] [83].
Q3: Our organization lacks in-house ML talent. What are some practical strategies to bridge this expertise gap?
Several policy and strategic options can address the human capital challenge [80]:
- Upskill Existing Staff: Create opportunities for current public and private sector workers to develop appropriate data science skills through targeted training programs.
- Promote Interdisciplinary Teams: Foster collaboration and communication between existing domain experts (e.g., biologists, chemists) and a small core of data scientists. This improves teamwork and leverages internal knowledge.
- Strategic Hiring: Focus on recruiting individuals with hybrid skills or demonstrated ability to work in cross-functional teams, rather than only seeking pure ML specialists.
Q4: What are the key data quality requirements for successful ML model transferability to industry settings?
For models to be reliable and transferable, your data should meet these criteria [80] [81]:
- High Quality: The data must be accurate, consistent, and well-annotated. ML models are highly sensitive to the quality of their training data.
- Standardized Formats: Implementing uniform standards for data and algorithms improves interoperability and allows researchers to combine different datasets more easily [80].
- Sufficient Quantity: ML requires large-scale biological, chemical, and clinical datasets for training and validation [84]. Techniques like data augmentation can be employed to generate more robust datasets [84].
Q5: How can we validate ML models to gain regulatory and internal confidence?
Validation is critical and can be approached through:
- Explainable AI (XAI): Using interpretable machine learning (IML) methods helps ensure algorithms remain explainable and transparent, which is vital for both internal trust and regulatory review [80] [84].
- Cross-Validation: This technique uses independent datasets to estimate the accuracy of ML algorithms and helps prevent overfitting or underfitting, common issues that compromise model reliability [81].
- Integration with Traditional Methods: Combining AI with traditional experimental methods and domain knowledge helps validate predictions and bridges the gap between computational and empirical research [84].
Troubleshooting Guides
Problem: Model predictions are inaccurate or do not generalize well to new data.
This is often a problem of model transferability, meaning the model fails when faced with real-world industry data different from its training data.
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Overfitting/Underfitting [81] | Perform cross-validation; check for high performance on training data but poor performance on test/validation data. | Increase the sample size of training data; apply regularization techniques; simplify model complexity if overfit. |
| Poor Data Quality [80] | Audit data sources for inconsistencies, missing values, and labeling errors. | Implement rigorous data curation and cleaning processes; establish uniform data standards. |
| Insufficient Data [80] | Evaluate the size and diversity of the training dataset relative to the problem's complexity. | Use data augmentation techniques to artificially expand the dataset [84]; explore transfer learning. |
| Lack of Domain Expertise | Review model assumptions and feature selection with a domain expert (e.g., a biologist or chemist). | Integrate domain knowledge into model design; foster collaboration between data scientists and domain experts. |
Problem: Encountering internal resistance from teams who distrust ML-based insights.
| Symptom | Underlying Issue | Mitigation Strategy |
|---|---|---|
| Stakeholders dismiss model outputs as a "black box." | Lack of transparency and explainability in the ML model. | Employ Explainable AI (XAI) and Interpretable ML (IML) methods to make model decisions understandable to humans [84]. |
| Preference for traditional methods and "the way it's always been done." | Resistance to change and organizational inertia [34]. | Start with small-scale pilot projects that demonstrate quick wins and clear value; showcase case studies from reputable sources [33] [82]. |
| Concerns about regulatory rejection. | Uncertainty about regulatory standards for ML in drug development [80]. | Proactively engage with regulatory science forums; advocate for internal investment in regulatory science expertise. |
Experimental Protocols & Data
Protocol for a Fit-for-Purpose ML Model in Drug Discovery
This protocol outlines a methodology for developing a robust ML model, aligning with the "fit-for-purpose" strategy for Model-Informed Drug Development (MID3) [34].
- Define the Question of Interest (QOI) and Context of Use (COU): Clearly articulate the specific problem the model is intended to solve (e.g., "Predict compound toxicity to prioritize in-vitro testing") and the context in which its predictions will be used [34].
- Data Curation and Standardization:
- Model Selection and Training:
- Model Validation and Interpretation:
- Integration and Iteration:
- Integrate model predictions with traditional experimental methods for validation [84].
- Establish a feedback loop where experimental results are used to continuously refine and update the ML model.
Quantitative Impact of Advanced Modeling in Pharma R&D
The table below summarizes documented benefits of integrating modeling and simulation, including ML, into pharmaceutical research and development.
| Metric | Impact Documented | Source / Context |
|---|---|---|
| Cost Savings | $0.5 billion | Impact on decision-making at Merck & Co./MSD [33] |
| Annual Clinical Trial Budget Reduction | $100 million | Pfizer's application of modeling & simulation [33] |
| Time Saved per Program | 10 months | Pfizer's systematic use of MIDD [82] |
| Clinical Trial Success Rate | 2.5x increase in positive proof-of-concept | AstraZeneca's use of mechanism-based biosimulation [82] |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key computational tools and methodologies used in modern, data-driven drug discovery.
| Tool / Solution | Function in Research |
|---|---|
| Generative Adversarial Network (GAN) [81] | An unsupervised deep learning model used to generate novel molecular structures with desired properties for drug discovery. |
| Quantitative Systems Pharmacology (QSP) [82] [34] | A mechanistic modeling approach that combines systems biology and pharmacology to predict drug effects across patient populations and explore combination therapies. |
| Physiologically Based Pharmacokinetic (PBPK) Modeling [82] [34] | A mechanistic approach that simulates how a drug moves through the body to predict drug-drug interactions and dosing in special populations. |
| Model-Based Meta-Analysis (MBMA) [82] | Uses highly curated clinical trial data to enable indirect comparison of drugs, supporting trial design and go/no-go decisions. |
| BERT Embeddings [85] | A Natural Language Processing (NLP) technique that provides nuanced contextual understanding of complex medical texts to enhance data extraction from literature. |
| Support Vector Machines & Deep Learning [81] | Supervised learning techniques applied to predict future outputs from biomedical data, such as classifying disease targets or predicting compound activity. |
Workflow Diagrams
ML Model Development and Implementation Workflow
Interdisciplinary Team Structure for ML Projects
FAQs: Navigating Model Trade-offs in Drug Discovery
1. Is the trade-off between model accuracy and interpretability unavoidable? Not always. While a common perception is that complex "black-box" models are necessary for high accuracy, this is not a strict rule. Research indicates that simpler, interpretable models can sometimes match or even outperform complex models, especially when data is limited or noise is present [86] [87]. Furthermore, techniques like automated feature engineering can create simpler models that retain the performance of their complex counterparts [87].
2. Why do my models perform well in internal validation but fail on external industry datasets? This is a classic problem of transferability, often caused by experimental variability between datasets [88]. Key factors include:
- Differing experimental settings: Variations in dosing regimens, assay types, and measurement techniques between studies [88] [89].
- Lack of data standards: The absence of standardized protocols in data generation leads to inconsistencies that models cannot generalize across [89].
- Non-overlapping biological contexts: Scarcity of overlapping cell lines and compounds between the training and target datasets [88].
3. What strategies can improve the transferability of models to new data? Several methodologies can enhance model robustness:
- Data Harmonization: Standardizing dose-response curves and other experimental readouts across different studies to create a consistent input space for models [88].
- Leveraging FAIR Data Principles: Ensuring data is Findable, Accessible, Interoperable, and Reusable improves data quality and model reliability [89] [90].
- Using Transferable Features: Prioritize features that are consistent across contexts, such as chemical structure-derived fingerprints and normalized pharmacodynamic properties, over summary metrics that are sensitive to experimental conditions [88] [91].
4. When should I prioritize an interpretable model over a high-accuracy black box? The choice depends on the context of use. Interpretable models are crucial in high-stakes applications such as:
- Credit scoring and lending decisions, where regulators require explanations for denials [92].
- Healthcare diagnostics, where doctors need to understand a model's reasoning to trust and verify its conclusions [92].
- Drug discovery, when you need to understand the relationship between a compound's structure and its biological activity to guide lead optimization [93].
5. How can I quantify the interpretability of a model? Interpretability can be quantified using frameworks like the Composite Interpretability (CI) score. This score combines expert assessments of a model's simplicity, transparency, and explainability with a quantitative measure of its complexity (e.g., number of parameters) to provide a comparative ranking [94].
The table below summarizes a quantitative comparison of different models based on such a framework.
Table 1: Model Interpretability-Accuracy Trade-off (Sample Benchmark)
| Model Type | Interpretability Score (CI) | Sample Accuracy (F1-Score) | Best Use Case |
|---|---|---|---|
| Logistic Regression (LR) | 0.22 | 0.75 | Inference; Understanding feature impacts [94] [93] |
| Naive Bayes (NB) | 0.35 | 0.72 | High-dimensional data with independent features [94] |
| Support Vector Machine (SVM) | 0.45 | 0.81 | Complex classification with clear margins [94] |
| Neural Network (NN) | 0.57 | 0.84 | Capturing complex, non-linear patterns [94] |
| BERT (Fine-tuned) | 1.00 | 0.89 | State-of-the-art NLP tasks where interpretability is not critical [94] |
Note: Scores are illustrative from a specific NLP use case (rating inference from reviews) and can vary based on application and data [94].
Troubleshooting Guides
Issue: Poor Model Generalization Across Drug Combination Studies
Problem: A model trained on one drug combination dataset (e.g., O'Neil) shows a significant drop in performance when applied to another dataset (e.g., ALMANAC), with synergy score correlations falling drastically [88].
Solution: Implement a Dose-Response Curve Harmonization Workflow.
This method addresses the root cause of variability: differences in experimental dose ranges and matrices [88].
Table 2: Research Reagent Solutions for Transferable Models
| Item / Reagent | Function in Experiment |
|---|---|
| Public Bioactivity Databases (e.g., ChEMBL, PubChem) | Provide large-scale, public data for pre-training models and establishing a broad applicability domain [91]. |
| Standardized Fingerprints (e.g., Chemical Structure) | Create a consistent, transferable representation of compounds that is independent of the original assay [88]. |
| FAIR Data Repository | A centralized system adhering to FAIR principles ensures that internal and external data are reusable and interoperable for model training [89] [90]. |
| LightGBM Framework | A gradient boosting framework known for high efficiency and performance on large tabular datasets, often used in benchmarking studies [88]. |
Experimental Protocol:
- Data Collection: Gather dose-response data from multiple source studies (e.g., ALMANAC, O'Neil, FORCINA) [88].
- Curve Normalization: Normalize the dose-axis of all monotherapy dose-response curves to a standardized range (e.g., 0 to 1) based on the tested dose range for each specific drug. This controls for differences in absolute dosage between studies [88].
- Response Imputation: Use interpolation or fitting to estimate drug response at a common set of predefined dose values across all studies. This creates a uniform input structure [88].
- Feature Engineering: Extract harmonized features from the standardized curves. These become the new, more robust input features for your machine learning model, replacing raw, study-specific summary metrics like IC50 [88].
- Model Training & Validation: Train your model (e.g., a LightGBM model) using these harmonized features. Validate performance using inter-study cross-validation, where the model is trained on a combination of three datasets and tested on the held-out fourth dataset [88].
The following workflow diagram illustrates this process:
Workflow for Data Harmonization
Issue: Choosing Between a Complex and a Simple Model
Problem: A deep neural network offers marginally higher accuracy than a logistic regression model, but the team cannot understand or trust its predictions for critical decisions.
Solution: Apply a "Simplify First" strategy and use model explanation techniques.
Experimental Protocol:
- Benchmark Simpler Models: First, establish a performance baseline using inherently interpretable models like logistic regression or decision trees on your problem [87].
- Quantify the Trade-off: Use a framework like the Composite Interpretability (CI) score to quantitatively compare the simplicity and performance of candidate models [94].
- Extract Features from Complex Models: If a complex model (e.g., a deep neural network) is needed for its performance, use it as a "supervisor." Employ techniques like SAFE (Surrogate Automatic Feature Engineering) to extract meaningful, interpretable features from the complex model's predictions or internal representations [87].
- Build a Glass-Box Surrogate: Train a simple, interpretable model (a "glass box") using the newly engineered features. This model can often achieve performance close to the complex black box while being fully understandable [87].
- Use Model-Agnostic Explainers: For the final model, apply tools like SHAP or LIME to generate post-hoc explanations for individual predictions, providing insight into the reasoning behind specific outcomes [92].
The logical flow for this simplification process is shown below:
Model Simplification Strategy
Ensuring Real-World Impact: Rigorous Evaluation and Benchmarking Frameworks
Frequently Asked Questions (FAQs)
Q1: My model has 95% accuracy, but it fails to detect critical rare events in production. Why is accuracy misleading me?
Accuracy can be highly deceptive for imbalanced datasets, which are common in industrial problems like fraud detection or equipment failure prediction [95] [96]. When one class vastly outnumbers the other (e.g., 99% good transactions vs. 1% fraud), a model that simply always predicts the majority class will achieve high accuracy but is practically useless [97]. For such cases, you must use metrics that focus on the positive class, such as the F1 Score or Precision-Recall AUC [98] [95].
Q2: When should I use AUC-ROC, and when should I use the F1 Score?
The choice depends on your business objective and the class balance of your data.
- Use AUC-ROC when you care equally about both the positive and negative classes and want a robust measure of your model's overall ranking capability [98]. It shows how well your model separates the two classes across all possible thresholds and is ideal for balanced problems [98] [96].
- Use the F1 Score when you are primarily concerned with the positive class and need a single metric that balances the trade-off between False Positives (FP) and False Negatives (FN) [98] [99]. It is the harmonic mean of Precision and Recall and is highly recommended for imbalanced classification problems [98].
Q3: What is the Kolmogorov-Smirnov (KS) statistic, and how is it used in industry?
The KS statistic is a measure of the degree of separation between the distributions of the positive and negative classes [100] [99]. It is calculated as the maximum distance between the cumulative distribution functions (CDFs) of the two classes [100] [101]. A higher KS value (closer to 1) indicates better separation. It is widely used in domains like risk management and banking because it is intuitive for business stakeholders and robust to data imbalance [100] [97]. It can also help determine the optimal classification threshold [96].
Q4: How do I choose the right threshold for my classification model?
There is no single "correct" threshold; it is a business decision that depends on the cost of False Positives versus False Negatives [98].
- If False Positives are costlier (e.g., in spam detection, where a legitimate email marked as spam is bad), you should increase the threshold to only classify a sample as positive when you are very confident. This increases Precision.
- If False Negatives are costlier (e.g., in cancer diagnosis, where missing a positive case is dangerous), you should lower the threshold to catch more positive cases. This increases Recall. You can use plots like the Precision-Recall curve or analyze metrics like the F1 score across thresholds to find a sweet spot that aligns with your business goals [98].
Troubleshooting Guides
Problem: Poor Performance on Imbalanced Industrial Data
Symptoms: High accuracy but unacceptable number of missed positive instances (high False Negatives) when the model is deployed on real-world, imbalanced data.
Solution Steps:
- Stop using Accuracy as your primary metric [95].
- Diagnose with the right metrics: Calculate the F1 Score, Precision, and Recall to get a true picture of your model's performance on the positive class [102] [95].
- Switch your evaluation curve: Use the Precision-Recall (PR) curve and calculate the PR AUC instead of relying solely on the ROC curve. The PR curve is more informative for imbalanced datasets as it focuses on the positive class and will clearly show if your performance is poor [98].
- Consider the KS Statistic: Evaluate the KS statistic to understand how well your model separates the two classes. A low KS score confirms the model's inability to distinguish between positives and negatives [100] [99].
Problem: Inconsistent Model Performance Between Validation and Production
Symptoms: The model showed strong AUC-ROC during validation but performs poorly on live, industry data.
Solution Steps:
- Check for data drift: The underlying data distribution in production may have changed since the model was trained. This is a common challenge for model transferability.
- Re-evaluate metric sensitivity: Remember that AUC-ROC can be overly optimistic on imbalanced data because the large number of True Negatives inflates the Specificity score [98]. Re-evaluate your model on a recent production sample using PR AUC, which is more sensitive to the performance on the positive class [98].
- Validate ranking power: Use the Kolmogorov-Smirnov (KS) test to verify that the model's predicted probabilities for the positive class are still ranked higher than those for the negative class in the new data [100] [101]. A significant drop in the KS statistic indicates a loss of separation power.
- Implement a robust validation protocol: Use k-fold cross-validation to reduce the variance of your performance estimate and ensure your model is not overfit to a particular validation split [103].
Metric Comparison & Selection Tables
Table 1: Core Binary Classification Metrics for Industrial Applications
| Metric | Formula | Interpretation | Ideal Value | Key Industrial Use Case |
|---|---|---|---|---|
| Accuracy | (TP+TN)/(TP+TN+FP+FN) | Overall correctness of predictions | 1.0 | Balanced problems where all classes are equally important [95] |
| Precision | TP/(TP+FP) | Proportion of correctly identified positives among all predicted positives | 1.0 | Fraud detection, where the cost of false alarms (FP) is high [102] [95] |
| Recall (Sensitivity) | TP/(TP+FN) | Proportion of actual positives correctly identified | 1.0 | Medical diagnosis or fault detection, where missing a positive (FN) is critical [102] [95] |
| F1 Score | 2 * (Precision * Recall)/(Precision + Recall) | Harmonic mean of Precision and Recall | 1.0 | General imbalanced classification; when a balance between FP and FN is needed [98] [99] |
| ROC AUC | Area under the ROC curve | Model's ability to rank a random positive higher than a random negative | 1.0 | Balanced problems; when overall ranking performance is key [98] [96] |
| PR AUC | Area under the Precision-Recall curve | Model's performance focused on the positive class | 1.0 | Highly imbalanced datasets; when the positive class is of primary interest [98] |
| KS Statistic | Max distance between positive and negative class CDFs | Degree of separation between the two classes | 1.0 | Credit scoring and risk modeling; to find the optimal threshold [100] [99] |
Table 2: Metric Selection Guide for Model Transferability Research
| Industrial Scenario | Primary Goal | Recommended Primary Metric | Recommended Supporting Metrics |
|---|---|---|---|
| Fraud / Defect Detection | Identify all true positives with minimal false alarms | F1 Score [98] | Precision, PR AUC, Lift Chart [99] |
| Medical Diagnosis / Predictive Maintenance | Minimize missed positive cases (False Negatives) | Recall [95] | F1 Score, PR AUC |
| Customer Churn Prediction | Prioritize and rank customers most likely to churn | ROC AUC [98] | Gain Chart, KS Statistic [99] |
| Credit Scoring | Effectively separate "good" from "bad" applicants | KS Statistic [100] [101] | Gini Coefficient, ROC AUC |
| Marketing Campaign Response | Identify the top deciles with the highest response rate | Lift / Gain Chart [99] | ROC AUC |
Experimental Protocols & Methodologies
Protocol 1: Evaluating a Classifier on an Imbalanced Dataset
Aim: To rigorously assess a binary classification model's performance and suitability for deployment on a highly imbalanced industrial dataset.
Research Reagent Solutions (Key Materials):
- Labeled Dataset: Should reflect real-world class imbalance.
- Probability Predictions: Output from a model like Logistic Regression or Random Forest, not just class labels [102].
- scikit-learn Library: Python library for computing metrics and plotting curves [98] [95].
- Visualization Tool: For generating PR and ROC curves.
Methodology:
- Data Preparation: Split data into training and test sets, preserving the imbalance in the test set.
- Model Training: Train the model on the training set.
- Generate Predictions: Obtain probability scores for the test set.
- Calculate Metrics:
- Visual Analysis:
- Interpretation: A high PR AUC and F1 Score, coupled with a high KS statistic, indicates a model that is robust and effective for the imbalanced industrial task, despite what the ROC AUC might suggest.
The following workflow summarizes the key decision points in this protocol:
Protocol 2: Finding the Optimal Classification Threshold
Aim: To systematically determine the classification threshold that optimizes for a specific business objective.
Methodology:
- Define Cost Function: Clearly articulate the business cost of a False Positive versus a False Negative.
- Generate Metrics Across Thresholds: For a range of thresholds (e.g., from 0.0 to 1.0), calculate the resulting Confusion Matrix, Precision, Recall, and F1 Score [98].
- Visualize Trade-offs:
- Select Threshold: Choose the threshold that either maximizes the F1 Score (for a balanced trade-off) or aligns with the predefined cost function (e.g., a threshold that ensures Recall is at least 95%).
The logical relationship between the threshold and key metrics is outlined below:
Implementing Expert-in-the-Loop Evaluation for Bias, Toxicity, and Factual Consistency
Frequently Asked Questions
Q1: What is the primary advantage of Expert-in-the-Loop (EITL) over a standard Human-in-the-Loop (HITL) for evaluation in high-stakes research?
EITL moves beyond general oversight to embed subject matter experts (e.g., senior clinicians, veteran researchers) directly into the design, training, and refinement of evaluation metrics. While HITL can provide modest performance gains (15–20%), EITL leverages deep domain knowledge to infuse context, define nuanced patterns, and weight critical variables, leading to reported efficiency gains of 40–65% and a tripling of ROI in some cases. It transforms experts from auditors into co-creators, scaling their wisdom across the entire evaluation pipeline. [104] [105]
Q2: Our automated metrics show high accuracy, but our model fails in real-world clinical scenarios. How can EITL address this?
This is a classic sign of evaluation fragmentation. A systematic review found that 95% of LLM evaluations in healthcare used accuracy as the primary metric, but only 5% used real patient care data for evaluation. [106] EITL addresses this by having experts design evaluation protocols that use real, complex patient data and assess critical, under-evaluated dimensions like fairness, bias, and toxicity (measured in only 15.8% of studies). [106] Experts ensure the evaluation reflects real-world clinical reasoning, not just exam-style question answering. [105] [106]
Q3: What are the key scalability challenges when implementing an EITL system, and how can we mitigate them?
The main challenge is the tension between scalability and specialization. Unlike HITL, which uses general annotators, EITL relies on scarce and costly domain experts. [104] Mitigation strategies include:
- Hybrid HITL/EITL Frameworks: Use HITL for scalable data labeling and EITL for high-precision validation of critical or ambiguous cases. [104]
- Tooling Investment: Implement robust expert annotation platforms and feedback orchestration systems to maximize expert efficiency. [104]
- Cost-Benefit Analysis: Weigh the operational cost of experts against the long-term value and risk mitigation in mission-critical systems where mistakes are expensive. [104]
Q4: Which evaluation metrics are most suitable for EITL to assess in the context of model transferability to industry data?
Experts are particularly well-suited to evaluate metrics that require nuanced, context-dependent judgment. While automated scores have value, expert judgment is irreplaceable for:
- Factual Correctness & Hallucination: Determining if an LLM output contains fake or made-up information against expert-known facts. [107]
- Answer Relevancy: Judging whether an output informatively and concisely addresses the specific industry problem. [107]
- Toxicity & Bias: Identifying harmful, offensive, or unfairly biased content that may be specific to a professional domain. [107]
- Contextual Relevancy (for RAG): Assessing if the retriever fetches the most relevant information for the generative model, which is crucial for knowledge-grounded tasks in research. [107]
Evaluation Landscape: Current Gaps and EITL Impact
The following table summarizes quantitative findings from a systematic review of LLM evaluations in healthcare, highlighting critical gaps that EITL methodologies are designed to address. [106]
| Evaluation Aspect | Current Coverage (from 519 studies) | EITL Enhancement Opportunity |
|---|---|---|
| Use of Real Patient Care Data | 5% | Experts can design and oversee evaluations using real-world, complex datasets to ensure clinical relevance. |
| Assessment of Fairness, Bias, and Toxicity | 15.8% | Domain experts are essential for identifying nuanced, context-specific biases and harmful outputs that automated systems miss. |
| Focus on Administrative Tasks | 0.2% (e.g., prescribing) | EITL can prioritize and validate performance on understudied but critical operational tasks. |
| Evaluation of Deployment Considerations | 4.6% | Experts can assess practical integration factors, robustness, and real-world performance decay. |
Experimental Protocol: Implementing an EITL Evaluation
This protocol provides a detailed methodology for integrating domain experts into the evaluation of bias, toxicity, and factual consistency.
1. Revision and Design Phase
- Objective: Finalize the evaluation criteria and adapt the model structure for the target domain.
- Steps:
- Assemble an Expert Panel: Collaborate with subject matter experts to assess the transferability of the chosen model or evaluation framework. [4]
- Define Evaluation Rubrics: Experts co-create detailed, domain-specific definitions for bias, toxicity, and factual consistency. For example, in drug development, "toxicity" could include specific types of misleading scientific claims.
- Revise Model Nodes/States: For structured models (e.g., Bayesian networks), experts review and adjust variables (nodes) and their relationships to reflect the target domain accurately. [4]
2. Knowledge Acquisition and Dataset Curation
- Objective: Gather all available information and create a benchmark dataset for evaluation.
- Steps:
- Identify Data Sources: Collate experimental data, peer-reviewed literature, gray literature, and expert knowledge for the study area. [4]
- Create Challenging Test Sets: Experts should help curate or synthesize evaluation datasets that contain edge cases, known ambiguities, and potential failure modes specific to the industry context. This ensures the model is not tested on simplistic or unrealistic data.
3. Expert-Centric Evaluation Execution
- Objective: Conduct a rigorous, multi-faceted evaluation of the model.
- Steps:
- Blinded Expert Rating: Provide experts with a randomized set of model inputs and outputs, stripped of identifying labels. Experts score the outputs based on the pre-defined rubrics using a Likert scale (e.g., 1-5 for factual consistency) or categorical labels (e.g., biased/unbiased). [108]
- LLM-as-a-Judge Calibration: In parallel, use an LLM-as-a-judge approach (e.g., with frameworks like G-Eval or Prometheus) to evaluate the same outputs. [109] [107] [110] The expert ratings serve as the ground truth for calibrating and validating the automated LLM judge.
- Discrepancy Analysis: Hold structured sessions where experts review cases where the model's output or the LLM judge's evaluation disagreed with human expert consensus. This is a critical step for refining both the model and the automated evaluation metrics. [107]
4. Iterative Model Refinement and Monitoring
- Objective: Use expert feedback for continuous model improvement.
- Steps:
- Incorporate Feedback: Use the expert-identified errors and biases to fine-tune the model or adjust its prompting strategy.
- Establish a Continuous EITL Loop: Implement a system where model outputs in production are periodically sampled and re-evaluated by experts, fueling a cycle of continuous learning and adaptation. [104]
EITL Evaluation Workflow
The following diagram visualizes the core feedback loop of an Expert-in-the-Loop evaluation system, illustrating how expert judgment is integrated to continuously assess and improve model performance.
The Scientist's Toolkit: Key Research Reagents
This table details essential "reagents" or components for setting up a robust EITL evaluation laboratory.
| Item / Solution | Function in EITL Evaluation |
|---|---|
| Domain Expert Panel | Provides the ground-truth judgments for bias, toxicity, and factual consistency. Their deep contextual knowledge is the primary reagent for validating model transferability. [104] [105] |
| Structured Evaluation Rubrics | Defines the specific, measurable criteria for each evaluated dimension (bias, etc.), ensuring consistent and reproducible scoring by both humans and automated systems. [107] |
| Challenging Benchmark Dataset | A curated set of inputs, including edge cases and domain-specific complexities, used to stress-test the model beyond generic performance. [110] |
| LLM-as-a-Judge Framework | An automated system (e.g., using Prometheus or custom prompts) that scales the evaluation process by mimicking expert judgment, once calibrated against the expert panel. [107] [110] |
| Feedback Orchestration Platform | Software tools that facilitate the efficient collection, management, and analysis of expert feedback, integrating it back into the model development lifecycle. [104] |
The following table summarizes the core attributes of the three AI data platform providers.
| Platform | Core Strengths | Specialized Domains | Key Evaluation & Annotation Features |
|---|---|---|---|
| iMerit [111] [112] | Expert-in-the-loop services, regulatory-grade workflows, custom solutions. | Pharmaceutical & Life Sciences [113], Medical AI [114], Autonomous Vehicles [111], LLM Red-Teaming [115] | RLHF, expert red-teaming, adversarial prompt generation, reasoning & factual consistency checks, retrieval-augmented generation (RAG) testing [112] [115]. |
| Scale AI [116] [112] | Broad data labeling services, large-scale operations, model benchmarking. | Autonomous Vehicles, E-commerce, Robotics [116] | Human-in-the-loop evaluation, benchmarking dashboards, pass/fail gating, annotation-based performance review [112]. |
| Encord [117] [118] [112] | Full-stack active learning platform, multimodal data support, data-centric AI tools. | Medical Imaging [117], Physical AI & Robotics [118], Sports AI [118], Logistics [118] | Automated data curation, error discovery, model evaluation workflows, quality scoring, performance heatmaps, embedding visualizations [116] [112]. |
Troubleshooting Guides and FAQs
This section addresses common challenges researchers face when integrating these platforms into their workflows for boosting model transferability to industrial and clinical data.
Data Quality and Annotation Consistency
Q1: During a drug compound image analysis project, our model's performance metrics are unstable. We suspect inconsistencies in the training data. How can we diagnose and fix this?
- Diagnosis: This is a classic symptom of low Inter-Rater Consistency (IRC), where human annotators disagree on labels, introducing noise that undermines model training and evaluation [119].
- Solution:
- Measure IRC: Use the platform's analytics to calculate annotator agreement metrics like Krippendorff's Alpha or Fleiss' Kappa [119]. A low score (e.g., below 0.7) confirms the issue.
- Audit Guidelines: Review and refine your annotation guidelines. Incorporate specific examples of edge cases relevant to your drug compound imagery [119].
- Implement Layered Review: For platforms like iMerit, activate a multi-step QA process. Have senior annotators or domain experts adjudicate disputed labels to establish a reliable ground truth [119] [114].
Q2: Our model performs well on internal benchmarks but fails on real-world, noisy data from clinical settings. How can we improve its transferability?
- Diagnosis: The model has overfitted to a clean, non-representative dataset and struggles with "edge cases" common in production environments.
- Solution: Use the platform's tools to proactively find and annotate these edge cases.
- Identify Failure Modes: With Encord, use its active learning toolkit to automatically curate datasets containing data points where your model is most uncertain or has previously made errors [116] [112].
- Targeted Augmentation: Use this curated set of challenging examples for targeted data augmentation and re-training, strengthening the model against real-world variability [116].
Model Evaluation and Benchmarking
Q3: We are fine-tuning a Large Language Model (LLM) to summarize clinical trial data, but automated metrics don't reflect the factual accuracy required for regulatory compliance. What is a more robust evaluation strategy?
- Diagnosis: Automated metrics (e.g., BLEU, ROUGE) often fail to capture factual consistency, clinical relevance, and the absence of harmful hallucinations.
- Solution: Implement a human-expert evaluation framework.
- Design Expert-led Evaluations: On a platform like iMerit, set up custom workflows for Reinforcement Learning from Human Feedback (RLHF) and red-teaming [112]. This involves:
- Factual Consistency Checks: Experts verify if summaries are grounded in the source trial data [112].
- Reasoning Evaluation: Assessing the logical coherence of the generated text [112].
- Adversarial Testing (Red-Teaming): Experts deliberately craft tricky prompts to try and induce hallucinations or unsafe outputs [115].
- Leverage Platform Templates: Use built-in evaluation templates for pairwise comparison, rating, and rubric-based reviews to ensure consistent and quantifiable expert feedback [112].
- Design Expert-led Evaluations: On a platform like iMerit, set up custom workflows for Reinforcement Learning from Human Feedback (RLHF) and red-teaming [112]. This involves:
Q4: How can we ensure our model evaluation process is audit-ready for regulatory submissions (e.g., to the FDA)?
- Diagnosis: Regulatory bodies require full traceability, proven consistency, and rigorous validation of the data and processes used to train and evaluate AI models.
- Solution: Choose a platform that embeds compliance into its core infrastructure.
- iMerit's Ango Hub offers GxP-ready workflows with built-in audit trails, structured metadata, and compliance with 21 CFR Part 11, HIPAA, and SOC 2 [113] [114]. Every annotation and evaluation step is logged, providing the necessary documentation for an audit.
- Encord provides robust security with label audit trails, encryption, and compliance with FDA, CE, and HIPAA regulations [117] [116].
Platform Integration and Workflow
Q5: Our team includes both in-house labelers and external contract annotators. How can we maintain quality and consistency across this hybrid workforce?
- Diagnosis: Without a centralized system, workflow fragmentation and inconsistent application of guidelines are common.
- Solution: Utilize the collaboration and project management features of your platform.
- Unified Workspace: Platforms like Labelbox and Encord provide a central hub for all annotators, ensuring everyone works from the same data and ontology [116] [120].
- Role-Based Access: Assign roles (e.g., Annotator, Reviewer, Admin) to control access and permissions. Implement QA workflows where senior team members review a subset of labels from all annotators [117] [114].
- Performance Analytics: Use built-in dashboards to track annotator performance metrics (e.g., agreement rates, throughput) and identify team members who may need retraining [117] [116].
Experimental Protocol for Evaluating Model Transferability
This protocol outlines a methodology for using these platforms to test and enhance how well a model transfers from research to industry data.
Objective
To quantitatively evaluate and improve a computer vision model's performance on real-world, domain-specific data, using platform tools for targeted data curation and expert evaluation.
Research Reagent Solutions
| Item | Function in the Experiment |
|---|---|
| iMerit Expert-in-the-Loop Services | Provides domain-expert annotators for creating high-quality ground truth and performing red-teaming/edge-case identification [112] [114]. |
| Encord Active Learning Toolkit | Automates the process of identifying the most valuable data points for labeling from a large, unlabeled corpus to improve model efficiency [116] [112]. |
| Scale AI Benchmarking Dashboard | Offers a centralized interface for tracking model performance across multiple dataset versions and evaluation runs [112]. |
| Adversarial Prompt Generation Framework | A systematic approach (e.g., using tools like PyRIT) for generating test cases that challenge model robustness and safety [115]. |
Step-by-Step Methodology
Phase 1: Baseline Establishment
- Initial Benchmark: Evaluate the pre-trained model on a held-out test set of high-quality, research-grade data. Record baseline metrics (e.g., mAP, Accuracy, F1-Score).
- Industry Data Test: Run the same model on a new, unlabeled dataset collected from the target industrial environment (e.g., clinical trial images, warehouse footage). The performance drop observed here quantifies the initial "transferability gap."
Phase 2: Targeted Data Curation
- Failure Analysis: Use a platform like Encord to run error analysis. The platform will use embedding visualizations and performance heatmaps to identify clusters of data where the model performs poorly [112].
- Active Learning Cycle:
- From the pool of industrial data, the platform's active learning system selects the most "informative" samples—those the model is most uncertain about [116].
- This curated batch is sent for labeling. For complex domains (e.g., medical, pharmaceutical), this labeling is performed by iMerit's domain experts to ensure high IRC and clinical accuracy [113] [114].
Phase 3: Expert Model Evaluation
- Edge Case Identification: Experts from iMerit analyze model outputs on the industrial data to identify new, previously unknown failure modes or edge cases [112].
- Red-Teaming: For LLM projects, experts conduct adversarial prompt generation to systematically probe for weaknesses like factual hallucinations or safety failures in the model's output [115].
Phase 4: Iterative Improvement & Final Validation
- Model Retraining: The model is fine-tuned on the newly labeled, high-value dataset from Phase 2.
- Final Evaluation: The retrained model is evaluated again on the original industrial data test set. Performance is compared against the baseline from Step 2. Expert evaluations from Phase 3 are used to qualitatively assess improvements in robustness and safety.
Workflow Visualization
The following diagram illustrates the core experimental workflow for improving model transferability.
Red-Teaming and Adversarial Testing to Uncover Edge Cases and Model Vulnerabilities
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: What is the core difference between traditional software penetration testing and AI red teaming?
AI red teaming focuses on exploiting cognitive and behavioral vulnerabilities unique to AI systems, such as prompt injection, model inversion, and reasoning flaws, rather than just traditional infrastructure or code weaknesses. It targets the model's decision boundaries, training data, and the agent's ability to be manipulated through its own tools and memory, which are absent in conventional applications [121].
Q2: Our model performs well on standard benchmarks. Why does it fail against simple adversarial prompts?
Standard benchmarks often measure performance on a held-out test set from the same data distribution as the training data. Adversarial prompts exploit the low-probability regions of your data distribution—the "edge cases" that are underrepresented in your training set but that an attacker will seek out. This creates a significant robustness gap between academic benchmarks and real-world performance [122].
Q3: What are the most effective prompt injection techniques we should test for in 2025?
Modern attacks are sophisticated and multi-faceted. The most effective techniques currently include [123]:
- Syntactic Anti-Classifiers: Replacing flagged words with detailed, descriptive synonyms to evade content filters.
- Encoding: Using simple encoding schemes like base64 or hexadecimal to obfuscate malicious instructions.
- End Sequences: Using fake prompt boundaries (e.g.,
</system>) to trick the model into ignoring prior instructions. - Language Blindspotting: Crafting prompts in languages underrepresented in the model's training data to bypass alignment safeguards.
Q4: How can we integrate continuous AI security testing into our existing MLOps pipeline?
Effective integration requires gated testing at multiple stages [121]:
- Development Phase: Implement automated adversarial testing during model training and validation.
- Staging Phase: Conduct comprehensive, human-led red teaming before any production deployment.
- Production Phase: Employ continuous monitoring and periodic security assessments on the live model.
Q5: How do we measure the success and ROI of our AI red teaming program?
Success should be measured with AI-specific metrics, not traditional security ones. Key Performance Indicators (KPIs) include [124] [121]:
- Reduction in Validated Attack Paths: The number of exploitable chains eliminated over time.
- Mean Time to Remediate (MTTR) AI Vulnerabilities: The speed of fixing identified issues.
- Vulnerability Coverage: The percentage of known AI-specific attack vectors you regularly test.
- Attack Success Rate Baseline: Establishing and then lowering the baseline rate of successful adversarial attacks against your models.
Troubleshooting Guides
Problem: Model is vulnerable to prompt injection and jailbreaks.
- Step 1: Identify the Attack Vector. Use an open-source tool like Garak or KnAIght to systematically test your model against a library of known jailbreak techniques, from "Grandma" attacks to DAN variants [125] [123].
- Step 2: Strengthen Input Validation. Implement input classifiers that detect not just keywords but also patterns of obfuscation, such as high-perplexity padding, encoded strings, and the use of fake prompt boundaries [123].
- Step 3: Implement Output Guardrails. Use a secondary model or a rule-based system to screen all model outputs for policy violations before they are delivered to the user. Cloud-native tools like AWS Bedrock Guardrails can be integrated for this purpose [121].
- Step 4: Adversarial Training. Fine-tune your model on examples of these jailbreaks where the correct behavior is to refuse the request. This teaches the model to recognize and resist such manipulations.
Problem: Model reveals sensitive data from its training set (Model Inversion).
- Step 1: Quantify the Risk. Use a framework like SecEval to run standardized benchmarks that attempt to reconstruct training data from model outputs. This helps establish a baseline risk profile [125].
- Step 2: Apply Differential Privacy. During training, use a differentially private stochastic gradient descent (DP-SGD) optimizer. This adds calibrated noise to the training process, making it mathematically difficult to determine if any specific data point was in the training set [122].
- Step 3: Limit Query Rates. For deployed models, especially those with API access, implement strict rate limiting and monitor for anomalous query patterns that suggest automated attempts to extract data [121].
Problem: AI agent can be manipulated to misuse its tools or pursue wrong goals.
- Step 1: Red Team for Goal Hijacking. Design tests where your team attempts to manipulate the agent's objective through conversation steering or context manipulation. For example, can a customer service agent be tricked into applying an unauthorized discount? [121]
- Step 2: Implement Strict Permission Controls. Apply the principle of least privilege to the agent's tool access. An agent that answers general questions should not have credentials to execute database writes or access sensitive financial systems [121].
- Step 3: Use Memory Sanitization. For agents with persistent memory, implement a process to scan and sanitize the memory context to prevent the persistence of malicious instructions across user sessions [121].
Experimental Protocols for Model Robustness
Protocol 1: Automated Adversarial Example Generation
Objective: To systematically generate inputs that fool the model into making incorrect predictions or outputs, thereby identifying blind spots in its decision boundaries.
Methodology:
- Tool Setup: Utilize an open-source framework like the Adversarial Robustness Toolbox (ART) or Garak [125] [121].
- Attack Selection: Choose a suite of attacks relevant to your data modality:
- For Image Models: Fast Gradient Sign Method (FGSM), Projected Gradient Descent (PGD).
- For LLMs: Apply automated prompt injection modules available in Garak, which test for vulnerabilities across multiple categories (e.g., prompt injection, data extraction).
- Execution: Run the selected attacks against your model in a controlled, sandboxed environment. The goal is to measure the attack's success rate and the magnitude of performance drop (e.g., accuracy decrease) on the adversarial examples compared to the clean test set.
- Analysis: Analyze the successful adversarial examples to identify common characteristics. Are they concentrated in a particular class or feature space? This analysis directly informs where your model's transferability to noisy, real-world "industry data" is weakest [122].
Protocol 2: LLM Red Teaming Engagement
Objective: To simulate a realistic attack on a deployed LLM or AI agent to uncover vulnerabilities that automated tools might miss.
Methodology:
- Planning & Scoping: Define the rules of engagement. Identify critical assets the model can access (e.g., databases, APIs) and set the objectives for the red team (e.g., "exfiltrate simulated PII data," "cause the agent to perform an unauthorized action") [126] [121].
- Reconnaissance: Perform open-source intelligence (OSINT) gathering on the deployed model. This includes studying its public documentation, testing its base responses, and understanding its system prompt limitations [126].
- Adversarial Execution: The red team executes a multi-stage attack campaign, emulating the MITRE ATT&CK for AI framework [124]. Techniques must include [121] [123]:
- Goal Hijacking: Using narrative injection and role-playing to divert the agent from its original task.
- Jailbreaking: Applying a combination of techniques like encoding, syntactic anti-classifiers, and end sequences to bypass refusal safeguards.
- Tool Misuse: Attempting to trick the agent into using its granted tools and permissions in an unintended, harmful way.
- Reporting & Debriefing: Document every successful attack path, the techniques used, and the potential business impact. This report is critical for the "blue team" (defenders) to prioritize remediation efforts, such as refining the model's prompts, adding safety filters, or reducing its permissions [126].
Workflow Visualization
The following diagram illustrates the continuous lifecycle for red-teaming and adversarial testing, integrating both automated and human-led components.
The Scientist's Toolkit: Research Reagent Solutions
This table details key tools and frameworks essential for conducting rigorous AI red teaming and adversarial testing.
| Tool/Framework Name | Type | Primary Function | Relevance to Industry Model Transferability |
|---|---|---|---|
| Garak [125] | Open-Source Tool | Automated vulnerability scanning for LLMs with 100+ attack modules. | Probes model robustness at scale, identifying edge cases before deployment to industry data. |
| Adversarial Robustness Toolbox (ART) [121] | Open-Source Framework | Generating adversarial examples for a wide range of model types (vision, text, etc.). | Measures and improves a model's resilience to noisy, real-world data distributions. |
| OpenAI Evals [125] | Evaluation Framework | Structured benchmarking of LLM behavior for safety, accuracy, and alignment. | Provides standardized metrics to track model performance and regression on critical tasks. |
| KnAIght [123] | Open-Source Tool | AI prompt obfuscator that applies multiple techniques (encoding, anti-classifiers) for testing. | Stress-tests the input sanitization and safety layers of production AI systems. |
| MITRE ATLAS [123] | Knowledge Base | A framework of adversary tactics and techniques tailored to AI systems. | Provides a common language and methodology for comprehensive threat modeling. |
Troubleshooting Guides & FAQs
This section addresses common challenges researchers face when building evidence for regulatory submissions to the FDA and EMA.
FAQ: How can we design a clinical development plan that satisfies both FDA and EMA requirements?
- Challenge: Aligning clinical trials with differing agency expectations on trial design, comparators, and data analysis.
- Solution: Engage with both agencies early via FDA pre-submission meetings and EMA Scientific Advice procedures to discuss and align on your development plan [127] [128]. Proactively address potential divergences, such as the EMA's greater emphasis on active comparators versus the FDA's traditional acceptance of placebo controls in certain contexts [128].
- Protocol Tip: For a unified global strategy, design clinical trials that incorporate agreed-upon endpoints, justified comparator arms, and a statistical analysis plan that controls for Type I error and demonstrates clinical meaningfulness [128].
FAQ: Our AI-based medical device shows promise in research. How do we demonstrate its clinical value for a regulatory submission?
- Challenge: Proving the real-world clinical value and transferability of an AI model beyond technical performance metrics.
- Solution: Employ a structured evaluation framework like the Model for ASsessing the value of AI (MAS-AI) [108] [129]. This tool helps decision-makers prioritize AI solutions by evaluating critical domains and process factors, ensuring the technology addresses a genuine clinical need.
- Validation Protocol: Implement a Delphi process with multidisciplinary stakeholders, including clinicians, patients, and methodologists, to rate the importance of various value domains (e.g., diagnostic accuracy, clinical impact, cost-effectiveness, organizational aspects, and patient aspects) on a Likert scale (e.g., 0-3). This confirms the face validity and transferability of your assessment across different healthcare settings [108].
FAQ: What is the most common reason for validation delays in regulatory submissions?
- Challenge: Submissions are rejected or delayed due to formatting errors and non-compliance with electronic submission standards.
- Solution: Both FDA and EMA require the Electronic Common Technical Document (eCTD) format for submissions [130] [131]. Use validated publishing software and the FDA Electronic Submissions Gateway (ESG) for transmission [130].
- Troubleshooting Checklist:
- Confirm all documents are in the correct eCTD structure (Modules 1-5).
- For the FDA, ensure the inclusion of a correctly completed FDA fillable form [130].
- For the EMA, ensure the Risk Management Plan follows EU templates and that Pediatric Investigation Plan requirements are met [128].
- Start early, as agencies like the EMA note that high submission volumes can impact validation timelines [132].
FAQ: We have a promising therapy for a rare disease. How can we navigate the differences in Orphan Drug designation between the FDA and EMA?
- Challenge: The criteria for Orphan Drug designation are similar but not identical between the agencies, which can impact development strategy.
- Solution: Understand the key differences in prevalence and the concept of "significant benefit." The EMA requires a demonstration of significant benefit over existing treatments, which can relate to improved clinical outcomes or ease of use [133].
- Evidence Strategy: For the EMA, prepare robust data comparing your product's potential benefits against any existing options. For both agencies, engage with their orphan drug designation programs early to seek guidance on your specific product and proposed development path [133].
Quantitative Data for Regulatory Submissions
The following tables summarize key quantitative data and criteria for FDA and EMA submissions.
Table 1: Key Performance Metrics from Model Validation Studies (MAS-AI)
| Metric | Result | Interpretation |
|---|---|---|
| Domain Face Validity | >70% of respondents (from Denmark, Canada, Italy) rated domains as moderately/highly important [108]. | Confirms the core domains of the MAS-AI framework are relevant across different countries. |
| Process Factor Importance | 87% to 93% of respondents rated the five process factors as moderately/highly important [108]. | Highlights critical factors beyond pure performance that impact AI implementation success. |
| Subtopic Validity Cut-off | All subtopics rated above 70% importance, except for five specific to Italy [108]. | Demonstrates the framework's general transferability while noting potential regional variations. |
Table 2: Comparison of FDA and EMA Regulatory Submission Requirements
| Aspect | U.S. Food and Drug Administration (FDA) | European Medicines Agency (EMA) |
|---|---|---|
| Standard Review Timeline | 10 months for NDA/BLA (Standard); 6 months (Priority Review) [128]. | ~12-15 months total from submission to EC authorization (210-day active assessment) [128]. |
| Expedited Pathways | Fast Track, Breakthrough Therapy, Accelerated Approval, Priority Review [128]. | Accelerated Assessment (150-day assessment), Conditional Approval [128]. |
| Orphan Drug Incentives | 7 years market exclusivity, tax credits, PDUFA fee waiver [133]. | 10 years market exclusivity (12 with PIP), fee reductions, protocol assistance [133]. |
| Pediatric Requirements | Pediatric Research Equity Act (PREA) - studies can be deferred post-approval [128]. | Pediatric Investigation Plan (PIP) - must be agreed upon before pivotal adult studies [128]. |
| Risk Management Plan | Risk Evaluation and Mitigation Strategy (REMS) when necessary [128]. | Risk Management Plan (RMP) required for all new marketing authorization applications [128]. |
Experimental Protocols for Evidence Generation
Protocol 1: Delphi Method for Stakeholder Consensus on Model Validity
This methodology is used to establish face validity and transferability for novel tools like AI models, as seen in the development of MAS-AI [108].
- Workshop Recruitment: Assemble a multidisciplinary sample of stakeholders. This should include decision-makers from hospitals/healthcare, patient partners, researchers, and technical experts [108].
- Rating Rounds: Present participants with the domains and subtopics of the evaluation model. Ask them to rate the importance of each item on a Likert scale (e.g., 0=Not important to 3=Highly important).
- Data Analysis: Calculate the percentage of respondents rating each domain and subtopic as "moderately" or "highly" important. A pre-defined cut-off (e.g., 70% agreement) confirms validity.
- Iteration: Conduct multiple rounds of rating and feedback to refine the model and achieve consensus.
Protocol 2: Requesting Parallel Scientific Advice from FDA and EMA
A proactive protocol to align evidence generation strategies with both major agencies simultaneously.
- Eligibility and Request: Determine if your product, especially for complex or innovative therapies, is suitable for parallel advice. Submit separate requests to both agencies, outlining the specific questions on clinical development, evidence needs, and trial design [127] [128].
- Agency Preparation: The FDA will assign internal review teams. The EMA's Scientific Advice Working Party (SAWP) will appoint two coordinators from national agencies, who form assessment teams [127].
- Joint Discussion: A joint meeting is typically held where both agencies and the sponsor discuss the development proposals. This is a critical forum to understand and reconcile differing perspectives.
- Consolidated Feedback: Both agencies will provide written feedback. While not legally binding, this advice is highly influential and should form the basis of a globally-aligned development plan [127].
Evidence Generation and Submission Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Regulatory Evidence Generation
| Item | Function in Evidence Generation |
|---|---|
| eCTD Publishing Software | Specialized software to compile, manage, and publish submission documents in the mandatory Electronic Common Technical Document (eCTD) format for FDA and EMA [131]. |
| Stakeholder Delphi Protocol | A structured methodology to gather and analyze input from diverse experts (clinicians, methodologists, patients) to establish the face validity and relevance of a model or assessment framework [108]. |
| Regulatory Intelligence Database | A continuously updated resource (software or service) that tracks the latest FDA guidances, EMA guidelines, and international harmonization (ICH) standards to ensure ongoing compliance. |
| Risk Management Plan (RMP) Template | A pre-formatted template, aligned with EMA requirements, for detailing safety specifications, pharmacovigilance activities, and risk minimization measures [128]. |
| FDA Fillable Forms | Specific administrative forms required by the FDA (e.g., Form FDA 356h) that must accompany eCTD submissions to enable automated processing and quicker access by reviewers [130]. |
Conclusion
Successfully transferring AI models from research environments to robust industry applications in drug development requires a holistic, 'Fit-for-Purpose' strategy. This synthesis of intent demonstrates that foundational data integrity, the application of specialized methodologies like MIDD and SLMs, proactive troubleshooting of deployment challenges, and rigorous, human-in-the-loop validation are not isolated tasks but interconnected pillars. The future of biomedical AI lies in creating transparent, explainable, and continuously learning systems that are deeply integrated into the drug development lifecycle—from early discovery to post-market surveillance. By adopting these data-centric strategies, researchers and drug development professionals can significantly accelerate the delivery of safe and effective therapies to patients, turning the promise of AI into tangible clinical impact.
References
- 1. Why do probabilistic clinical models fail to transport ... [https://www.nature.com/articles/s41746-024-01037-4]
- 2. Real-World Performance Transferability [https://www.emergentmind.com/topics/performance-transferability-to-real-world-data]
- 3. Methodological challenges in translational drug response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7192505/]
- 4. Guidelines for model adaptation: A study of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9353019/]
- 5. Transfer Learning For Model Transferability [https://www.meegle.com/en_us/topics/transfer-learning/transfer-learning-for-model-transferability]
- 6. Model Transferability and Reduced Experimental Burden ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8733703/]
- 7. 5 common data management problems affecting drug discovery [https://www.drugdiscoverytrends.com/5-common-data-management-problems-affecting-drug-discovery/]
- 8. Top three data management challenges impacting pharma ... [https://www.ontoforce.com/blog/top-three-data-management-challenges-impacting-pharma-rd]
- 9. Real-World Data Integration Examples: How Companies ... [https://mammoth.io/blog/real-world-data-integration-examples-how-companies-unified-their-data/]
- 10. FAQ - cleanlab [https://docs.cleanlab.ai/stable/tutorials/faq.html]
- 11. How to Integrate Data from Multiple Sources [https://www.oracle.com/analytics/integrating-data-multiple-data-sources/]
- 12. Multi-Source Data Repairing: A Comprehensive Survey [https://www.mdpi.com/2227-7390/11/10/2314]
- 13. Bag of Tricks to Boost Adversarial Transferability [https://arxiv.org/abs/2401.08734]
- 14. Boosting adversarial transferability in vision-language ... [https://www.nature.com/articles/s41598-025-91802-6]
- 15. What is concept drift in ML, and how to detect and address it [https://www.evidentlyai.com/ml-in-production/concept-drift]
- 16. Concept drift [https://en.wikipedia.org/wiki/Concept_drift]
- 17. A Gentle Introduction to Concept Drift in Machine Learning [https://www.machinelearningmastery.com/gentle-introduction-concept-drift-machine-learning/]
- 18. Data Shift in ML: Understanding Statistical Intuition [https://www.nannyml.com/blog/types-of-data-shift]
- 19. 7 Top Market Research Challenges (and How to Solve ... [https://www.alpha-sense.com/blog/trends/market-research-challenges/]
- 20. Challenges and opportunities of big data analytics in healthcare [https://pmc.ncbi.nlm.nih.gov/articles/PMC11080701/]
- 21. Why regulatory hurdles need to be overcome for clean ... [https://www.weforum.org/stories/2024/03/regulatory-hurdles-clean-energy-transition/]
- 22. Accurate and transferable drug–target interaction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11629708/]
- 23. Aligning Large Language Models to Particular Contextual ... [https://arxiv.org/html/2403.09704v1]
- 24. Is your organization fit for purpose? [https://elisabetlagerstedt.com/2022/04/20/is-your-organization-fit-for-purpose/]
- 25. Exploring the Transferability of Research Impact [https://researchfish.com/blog/research-characteristics-transferability/]
- 26. The Strategic Case for Small Language Models in AI Agents [https://medium.com/@adnanmasood/fit-for-purpose-the-strategic-case-for-small-language-models-in-ai-agents-da6d5532a93a]
- 27. A Pharmacometric Workflow for Resolving Model Instability in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521063/]
- 28. Navigating Regulatory Submissions with Pharmacometric ... [https://www.certara.com/webinar/delivering-on-deadline-navigating-regulatory-submissions-with-pharmacometrics-insights/]
- 29. Scoping review of the role of pharmacometrics in model ... [https://link.springer.com/article/10.1007/s10928-025-10005-8]
- 30. Pharmacometric simulation with mrgsolve [https://blog.djnavarro.net/posts/2023-08-14_mrgsolve/]
- 31. contentRsNLME [https://onlinehelp.certara.com/rsnlme/2.0/RsNLME_User_Guide/contentRsNLME/contentRsNLME.htm]
- 32. Communicating to Influence Drug Development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4846777/]
- 33. Good Practices in Model‐Informed Drug Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4809625/]
- 34. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 35. Exploring model transferability in ML-integrated RPL ... [https://www.sciencedirect.com/science/article/pii/S1570870524002373]
- 36. Source-Free Model Transferability Assessment for Smart ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12251657/]
- 37. Leveraging Quantitative Methods and Modeling to ... [https://www.fda.gov/drugs/news-events-human-drugs/leveraging-quantitative-methods-and-modeling-modernize-generic-drug-development-and-review-public]
- 38. Data-Centric AI | Journal of Intelligent Information Systems [https://link.springer.com/article/10.1007/s10844-024-00901-9]
- 39. Data Centric AI [https://neurips.cc/virtual/2021/workshop/21860]
- 40. 9 AI problems in 2025: Common challenges and solutions [https://lumenalta.com/insights/ai-problems-9-common-challenges-and-solutions]
- 41. Automated Pruning Framework for Large Language ... [https://www.mdpi.com/2673-2688/6/5/96]
- 42. How Pruning, Distillation, and PEFT Are Reshaping AI in ... [https://medium.com/@hs5492349/the-model-optimization-revolution-how-pruning-distillation-and-peft-are-reshaping-ai-in-2025-c9f79a9e7c2b]
- 43. AI Model Optimization Techniques for Enhanced ... [https://www.netguru.com/blog/ai-model-optimization]
- 44. Pruning and Distilling LLMs Using NVIDIA TensorRT ... [https://developer.nvidia.com/blog/pruning-and-distilling-llms-using-nvidia-tensorrt-model-optimizer/]
- 45. Quantization In Drug Discovery [https://www.meegle.com/en_us/topics/quantization/quantization-in-drug-discovery]
- 46. A graph-based knowledge distillation framework for drug ... [https://www.sciencedirect.com/science/article/pii/S0952197625027836]
- 47. Comparative analysis of model compression techniques for ... [https://www.nature.com/articles/s41598-025-07821-w]
- 48. NVIDIA Research Proves Small Language Models ... [https://galileo.ai/blog/small-language-models-nvidia]
- 49. How Small Language Models Are Key to Scalable Agentic AI [https://developer.nvidia.com/blog/how-small-language-models-are-key-to-scalable-agentic-ai/]
- 50. The Best Small LLMs For Edge Devices In 2025 [https://www.siliconflow.com/articles/en/best-small-llms-for-edge-devices]
- 51. Weekly ML Update: Small Language Models Rise In 2025 [https://bostoninstituteofanalytics.org/blog/weekly-wrap-up-25th-oct-1st-nov-how-small-language-models-slms-are-outperforming-giants-in-2025/]
- 52. Advancing drug discovery and development through GPT ... [https://www.sciencedirect.com/science/article/pii/S2666521225000365]
- 53. LLMOps vs MLOps: Comparison Table + 30 FAQs Answered [https://www.azilen.com/blog/llmops-vs-mlops/]
- 54. MLOps & LLMOps | Key Differences & Best Practices [https://xorbix.com/insights/from-mlops-to-llmops-managing-the-lifecycle-of-advanced-ai-models/]
- 55. Mastering LLMOps: Building Production-Ready Large ... [https://dev.to/vaib/mastering-llmops-building-production-ready-large-language-models-4idp]
- 56. LLMOps for AI Agents in Production: Monitoring, Testing, ... [https://onereach.ai/blog/llmops-for-ai-agents-in-production/]
- 57. “LLMOps is not MLOps… we learnt the hard way” [https://ai.plainenglish.io/llmops-is-not-mlops-we-learnt-the-hard-way-27cddc6343fc]
- 58. Top MLOps Challenges and How to Solve Them | Medium [https://chisoftware.medium.com/how-can-you-solve-the-most-common-mlops-challenges-insights-from-our-practice-a8324ef2e5d9]
- 59. What is LLMOps? Key Components & Differences to MLOPs [https://lakefs.io/blog/llmops/]
- 60. Top Platforms for LLMOps and Agent Orchestration in 2026 [https://www.askui.com/blog-posts/ai-deployment-llmops-orchestration]
- 61. 14 Common Application Performance Issues & How to Fix Them [https://middleware.io/blog/fix-application-performance-issues/]
- 62. Harmonizing across datasets to improve the transferability ... [https://www.nature.com/articles/s42003-023-04783-5]
- 63. TransCDR: a deep learning model for enhancing the ... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-024-02023-8]
- 64. Explore user experience strategies for mitigating ... [https://learn.microsoft.com/en-us/power-platform/architecture/key-concepts/performance/ux-strategies]
- 65. Common mitigation strategies - AWS Prescriptive Guidance [https://docs.aws.amazon.com/prescriptive-guidance/latest/resilience-analysis-framework/mitigation-strategies.html]
- 66. 8 Simple Techniques to Prevent Overfitting [https://towardsdatascience.com/8-simple-techniques-to-prevent-overfitting-4d443da2ef7d/]
- 67. ML | Underfitting and Overfitting [https://www.geeksforgeeks.org/machine-learning/underfitting-and-overfitting-in-machine-learning/]
- 68. How Overfitting Ruins Your Feature Selection - Hex [https://hex.tech/blog/overfitting-model-impact/]
- 69. On the robustness of generalization of drug–drug interaction ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-021-04398-9]
- 70. Using Transfer Learning to Boost Model Performance [https://www.kdnuggets.com/using-transfer-learning-to-boost-model-performance]
- 71. Improved generalization by noise enhancement [https://arxiv.org/abs/2009.13094]
- 72. Label Noise Gradient Descent Improves Generalization in ... [https://openreview.net/forum?id=PPazOk82Sq]
- 73. Boosting as a scheme for transfer learning [https://www.chrisstucchio.com/blog/2022/boosting_for_knowledge_transfer.html]
- 74. Low Latency: The Ultimate Guide for Real-Time ... [https://www.videosdk.live/developer-hub/webtransport/low-latency]
- 75. Real-time AI performance: latency challenges and ... [https://mitrix.io/blog/real-time-ai-performance-latency-challenges-and-optimization/]
- 76. Ultimate Guide to Latency Optimization for AI Systems [https://blog.naitive.cloud/ultimate-guide-to-latency-optimization-for-ai-systems/]
- 77. How to Optimize Networks for Peak Performance 2025 [https://re-solution.co.uk/how-to-optimize-networks-2025/]
- 78. Deep Learning 2025: Federated, Reinforcement, Transfer [https://www.solulab.com/ai-deep-learning-techniques/]
- 79. Inside ELRIG's Drug Discovery 2025 [https://www.drugtargetreview.com/article/190237/inside-elrigs-drug-discovery-2025/]
- 80. Benefits and Challenges of Machine Learning in Drug ... [https://www.gao.gov/products/gao-20-215sp]
- 81. Implementation of Machine Learning in Drug Development [https://proventainternational.com/bioinformatics-machine-learning-in-drug-development-article/]
- 82. Essentials of Model-informed Drug Development in Oncology [https://www.certara.com/blog/essentials-of-model-informed-drug-development-midd-top-down-vs-bottom-up-approaches/]
- 83. How data science can accelerate drug development [https://www.recipharm.com/resources/innovation-bottleneck]
- 84. The Role of AI in Drug Discovery: Challenges, Opportunities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10302890/]
- 85. Enhancing drug discovery and patient care through ... [https://www.sciencedirect.com/science/article/pii/S2472630324001201]
- 86. The Accuracy vs Interpretability Trade-off Is a Lie [https://medium.com/data-science/the-accuracy-vs-interpretability-trade-off-is-a-lie-0bf89c84f5b3]
- 87. Simpler is better: Lifting interpretability-performance trade ... [https://www.sciencedirect.com/science/article/pii/S016792362100066X]
- 88. Harmonizing across datasets to improve the transferability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10090076/]
- 89. Data standards in drug discovery: A long way to go [https://www.sciencedirect.com/science/article/abs/pii/S1359644624000047]
- 90. Boosting biopharma R&D with a next-gen tech stack [https://www.mckinsey.com/industries/life-sciences/our-insights/boosting-biopharma-r-and-d-performance-with-a-next-generation-technology-stack]
- 91. Industry-scale application and evaluation of deep learning for ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-020-00428-5]
- 92. The trade-off between model complexity and interpretability ... [https://milvus.io/ai-quick-reference/what-tradeoffs-exist-between-model-complexity-and-interpretability]
- 93. Understanding The Accuracy-Interpretability Trade-Off [https://towardsdatascience.com/accuracy-interpretability-trade-off-8d055ed2e445/]
- 94. Demystifying the Accuracy-Interpretability Trade-Off [https://arxiv.org/html/2503.07914v1]
- 95. Understanding F1 Score, Accuracy, ROC-AUC & PR- ... [https://www.deepchecks.com/f1-score-accuracy-roc-auc-and-pr-auc-metrics-for-models/]
- 96. Understanding these Key Model Evaluation Metrics is a ... [https://medium.com/@frankonyango.w/from-accuracy-to-kolmogorov-smirnov-understanding-and-calculating-model-evaluation-metrics-e84a87d8046e]
- 97. 7 methods to evaluate your classification models | by Jin [https://medium.com/analytics-vidhya/everything-you-need-about-evaluating-classification-models-dfb89c60e643]
- 98. F1 Score vs ROC AUC vs Accuracy vs PR AUC [https://neptune.ai/blog/f1-score-accuracy-roc-auc-pr-auc]
- 99. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 100. Evaluating classification models with Kolmogorov-Smirnov ... [https://towardsdatascience.com/evaluating-classification-models-with-kolmogorov-smirnov-ks-test-e211025f5573/]
- 101. ML Model Performance Evaluation: Gini Index, ROC-AUC ... [https://ginimachine.com/academia-post/ml-model-performance-evaluation/]
- 102. Model Evaluation Metrics in Machine Learning [https://www.datasource.ai/en/data-science-articles/model-evaluation-metrics-in-machine-learning]
- 103. Evaluating machine learning models-metrics and techniques [https://www.aiacceleratorinstitute.com/evaluating-machine-learning-models-metrics-and-techniques/]
- 104. Experts-in-the-Loop The Future of High-Precision AI Systems [https://www.nextwealth.com/blog/experts-in-the-loop-the-future-of-high-precision-ai-systems/]
- 105. Expert in the Loop: Why AI Needs Specialists, Not Just ... [https://medium.com/@ai_93276/expert-in-the-loop-why-ai-needs-specialists-not-just-humans-5797b6500654]
- 106. Testing and Evaluation of Health Care Applications of Large ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11480901/]
- 107. LLM Evaluation Metrics: The Ultimate LLM Evaluation Guide [https://www.confident-ai.com/blog/llm-evaluation-metrics-everything-you-need-for-llm-evaluation]
- 108. Validity and transferability of model for assessing the value ... [https://www.sciencedirect.com/science/article/pii/S1386505625003442]
- 109. Mastering LLM Techniques: Evaluation [https://developer.nvidia.com/blog/mastering-llm-techniques-evaluation/]
- 110. Large Language Model Evaluation: 10+ Metrics & Methods [https://research.aimultiple.com/large-language-model-evaluation/]
- 111. iMerit: Customer Case Studies for AI Use Cases [https://imerit.net/resources/case-studies/]
- 112. Top 7 Expert Service Providers for Model Evaluation in 2025 [https://imerit.net/resources/blog/top-7-expert-service-providers-for-model-evaluation-in-2025/]
- 113. Pharma & Life Sciences Ai Data Solutions [https://imerit.net/domains/medical-ai/pharmaceuticals-life-sciences/]
- 114. Top 5 Tools for Medical Data Annotation in AI Development [https://imerit.net/resources/blog/top-5-tools-for-medical-data-annotation-in-ai-development/]
- 115. Adversarial Prompt Generation: Building Safer AI with Human Oversight [https://imerit.net/resources/blog/adversarial-prompt-generation-building-safer-ai-with-human-in-the-loop-oversight/]
- 116. Alternatives: Why Scale Teams Choose AI AI Encord [https://encord.com/blog/scale-alternatives/]
- 117. 12 Best Data Labeling Companies [2025] [https://encord.com/blog/data-annotation-companies-for-computer-vision/]
- 118. Best Data Labeling Platforms for Each AI Use Case (2025) [https://encord.com/blog/best-data-labeling-platforms-for-each-ai-use-case/]
- 119. A Guide to Inter-rater Reliability and Annotator Agreement ... [https://imerit.net/resources/blog/human-vs-model-agreement-how-inter-rater-consistency-shapes-benchmark-reliability/]
- 120. 6 Best V7 Alternatives in 2025[Updated] [https://www.labellerr.com/blog/v7-alternatives/]
- 121. AI Security Testing: Protecting Models and Agents From ... [https://www.obsidiansecurity.com/blog/ai-security-testing]
- 122. A Systematic Review of Robustness in Deep Learning for ... [https://arxiv.org/abs/2112.00639]
- 123. The State of AI Red Teaming in 2025 & 2026 [https://whiteknightlabs.com/2025/11/04/the-state-of-ai-red-teaming-in-2025-2026/]
- 124. The Future of Security Testing: A 2025 Guide to Adversarial ... [https://www.breachlock.com/resources/blog/the-future-of-security-testing-a-2025-guide-to-adversarial-exposure-validation/]
- 125. Best Open Source LLM Red Teaming Tools (2025) [https://onsecurity.io/article/best-open-source-llm-red-teaming-tools-2025/]
- 126. Red Teaming in 2025: The Bleeding Edge of Security Testing [https://www.cycognito.com/learn/red-teaming/]
- 127. Scientific advice and protocol assistance [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-advice-protocol-assistance]
- 128. FDA vs EMA: Key Regulatory Differences for ... [https://lsacademy.com/en/fda-vs-ema-key-regulatory-differences-for-pharmaceuticals/]
- 129. Validity and transferability of Model for ASsessing the value ... [https://pubmed.ncbi.nlm.nih.gov/41092593/]
- 130. Electronic Regulatory Submission and Review [https://www.fda.gov/drugs/forms-submission-requirements/electronic-regulatory-submission-and-review]
- 131. A Guide to Regulatory Submissions in the US (FDA) & EU ... [https://kivo.io/news/a-regulatory-submissions-guide-for-the-us-fda-eu-ema]
- 132. Advice on end-of-year submission dates for type I variations in ... [https://www.ema.europa.eu/en/news/advice-end-year-submission-dates-type-i-variations-2025]
- 133. FDA and EMA Resources, Policies, and Programs ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK609376/]