Comparative Effectiveness Research in Pharmaceuticals: A Guide to Methods, Applications, and Future Directions
This article provides a comprehensive overview of Comparative Effectiveness Research (CER) in the pharmaceutical sector, tailored for researchers, scientists, and drug development professionals.
Comparative Effectiveness Research in Pharmaceuticals: A Guide to Methods, Applications, and Future Directions
Abstract
This article provides a comprehensive overview of Comparative Effectiveness Research (CER) in the pharmaceutical sector, tailored for researchers, scientists, and drug development professionals. It covers the foundational definition and purpose of CER, as defined by the Institute of Medicine, and explores its core question: which treatment works best, for whom, and under what circumstances. The content delves into the key methodological approaches, including randomized controlled trials, observational studies, and evidence synthesis, while addressing critical challenges such as selection bias and data quality. It also examines the validation of CER findings and the comparative reliability of different study designs, concluding with the implications of CER for improving drug development, informing regulatory and payer decisions, and advancing personalized medicine.
What is Comparative Effectiveness Research? Defining the Foundation for Better Drug Decisions
Comparative Effectiveness Research (CER) is defined by the Institute of Medicine (IOM) as “the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care” [1]. The fundamental purpose of CER is to assist consumers, clinicians, purchasers, and policy makers in making informed decisions that will improve health care at both the individual and population levels [2]. In the specific context of pharmaceutical research, this translates to direct comparisons of drug therapies against other available treatments—including other drugs, non-drug interventions, or surgical procedures—to determine which work best for specific types of patients and under what circumstances [1].
This methodology represents a crucial shift from traditional efficacy research, which asks whether a treatment can work under controlled conditions, toward a focus on how it does work in real-world clinical practice [2]. CER is inherently patient-centered, focusing on the outcomes that matter most to patients in their everyday lives, and forms the foundation for high-value healthcare by identifying the most effective interventions among available alternatives [2].
Core Methodologies for Evidence Generation
The IOM definition emphasizes two core activities: the generation of new comparative evidence and the synthesis of existing evidence. Several established methodological approaches fulfill these functions in pharmaceutical research.
Primary Evidence Generation Methods
Table 1: Core Methodologies for Primary Evidence Generation in Pharmaceutical CER
| Method | Key Features | Strengths | Limitations | Pharmaceutical Applications |
|---|---|---|---|---|
| Randomized Controlled Trials (RCTs) | Participants randomly assigned to treatment groups; differs only in exposure to study variable [1] | Gold standard for causal inference; minimizes confounding [1] | Expensive, time-consuming; may lack generalizability to real-world populations [1] | Head-to-head drug comparisons; establishing efficacy under controlled conditions |
| Observational Studies | Participants not randomized; treatment choices made by patients and physicians [1] | Assesses real-world effectiveness; faster and more cost-efficient; suitable for rare diseases [1] | Potential for selection bias; confounding by indication [1] | Post-market surveillance; effectiveness in subpopulations; long-term outcomes |
| Prospective Observational Studies | Outcomes studied after creation of study protocol; interventions can include medications [1] | Captures real-world practice patterns; can study diverse populations [1] | Still susceptible to unmeasured confounding [1] | Pragmatic trials; patient-centered outcomes research |
| Systematic Reviews | Critical assessment of all research studies on a particular clinical issue using specific criteria [1] | Comprehensive evidence synthesis; identifies consistency of effects across studies [1] | Limited by quality and availability of primary studies [1] | Summarizing body of evidence for drug class comparisons |
Each method contributes distinct evidence for pharmaceutical decision-making. While RCTs provide the most reliable evidence of causal effects, observational studies offer insights into how drugs perform across heterogeneous patient populations in routine care settings [1]. The choice among methods involves balancing scientific rigor with practical considerations including cost, timeline, and generalizability requirements.
Analytical Approaches for CER
Advanced analytical methods are essential for generating valid evidence from observational data, which frequently forms the basis of pharmaceutical CER.
Risk Adjustment: An actuarial tool that identifies a risk score for a patient based on conditions identified via claims or medical records. Prospective risk adjusters use historical claims data to predict future costs, while concurrent risk adjustment uses current medical claims to explain an individual's present costs. Both approaches help identify similar types of patients for comparative purposes [1].
Propensity Score Matching: This method calculates the conditional probability of receiving a treatment given several predictive variables. Patients in a treatment group are matched to control group patients based on their propensity score, enabling estimation of outcome differences between balanced patient groups. This approach helps control for treatment selection biases, including regional practice variations [1].
Evidence Synthesis Approaches
Evidence synthesis represents the second pillar of the IOM definition, systematically integrating findings across multiple studies to develop more reliable and generalizable conclusions about pharmaceutical effectiveness.
Systematic reviews employ rigorous, organized methods for locating, assembling, and evaluating a body of literature on a particular clinical topic using predetermined criteria [1]. When systematic reviews include quantitative pooling of data through meta-analysis, they can provide more precise estimates of treatment effects and examine potential effect modifiers across studies [1].
For pharmaceutical research, these synthesis approaches are particularly valuable for:
- Resolving uncertainty when individual studies report conflicting findings
- Increasing statistical power for subgroup analyses to identify which patients benefit most from specific treatments
- Assessing the consistency of drug effects across different patient populations and care settings
- Informing clinical guideline development and coverage decisions
Implementation and Methodological Considerations
Successfully implementing CER in pharmaceuticals requires careful attention to several methodological and practical considerations that affect the validity and utility of the generated evidence.
Pharmaceutical CER utilizes diverse data sources, each with distinct strengths and limitations:
Claims Data: Historically used for actuarial analyses, these data provide large sample sizes and real-world prescribing information but typically lack clinical detail such as lab results or patient-reported outcomes [1].
Electronic Health Records (EHRs): Contain richer clinical information including vital signs, diagnoses, and treatment responses, though data quality and completeness may vary across institutions [3].
Prospective Data Collection: Specifically designed for research purposes, offering more control over data quality and the ability to capture patient-centered outcomes directly [1].
Data governance represents a critical framework for managing organizational structures, policies, and fundamentals that ensure accurate and risk-free data. Proper data governance establishes standards, accountability, and responsibilities, ensuring that data use provides maximum value while managing handling costs and quality [4]. Throughout the pharmaceutical data lifecycle, this includes planning and designing, capturing and developing, organizing, storing and protecting, using, monitoring and reviewing, and eventually improving or disposing of data [4].
Addressing Bias and Confounding
Selection bias presents a particular challenge in pharmaceutical CER, especially when physicians prescribe one treatment over another based on disease severity or patient characteristics [1]. Beyond the statistical methods previously discussed, approaches to address this include:
- Sensitivity Analyses: Testing how robust findings are to different assumptions about unmeasured confounding
- Instrumental Variable Methods: Using factors associated with treatment choice but not directly with outcomes to estimate causal effects
- High-Dimensional Propensity Scoring: Leveraging the vast number of variables in healthcare databases to improve confounding adjustment
Ethical and Professional Standards
CER investigators must adhere to ethical guidelines throughout research planning, design, implementation, management, and reporting [4]. Key principles include:
- Maintaining independence and avoiding conflicts of interest that could inappropriately influence research findings [4]
- Respecting human rights and ensuring data protection and confidentiality [4]
- Considering gender, ethnicity, age, disability, and other relevant factors when designing and implementing studies [4]
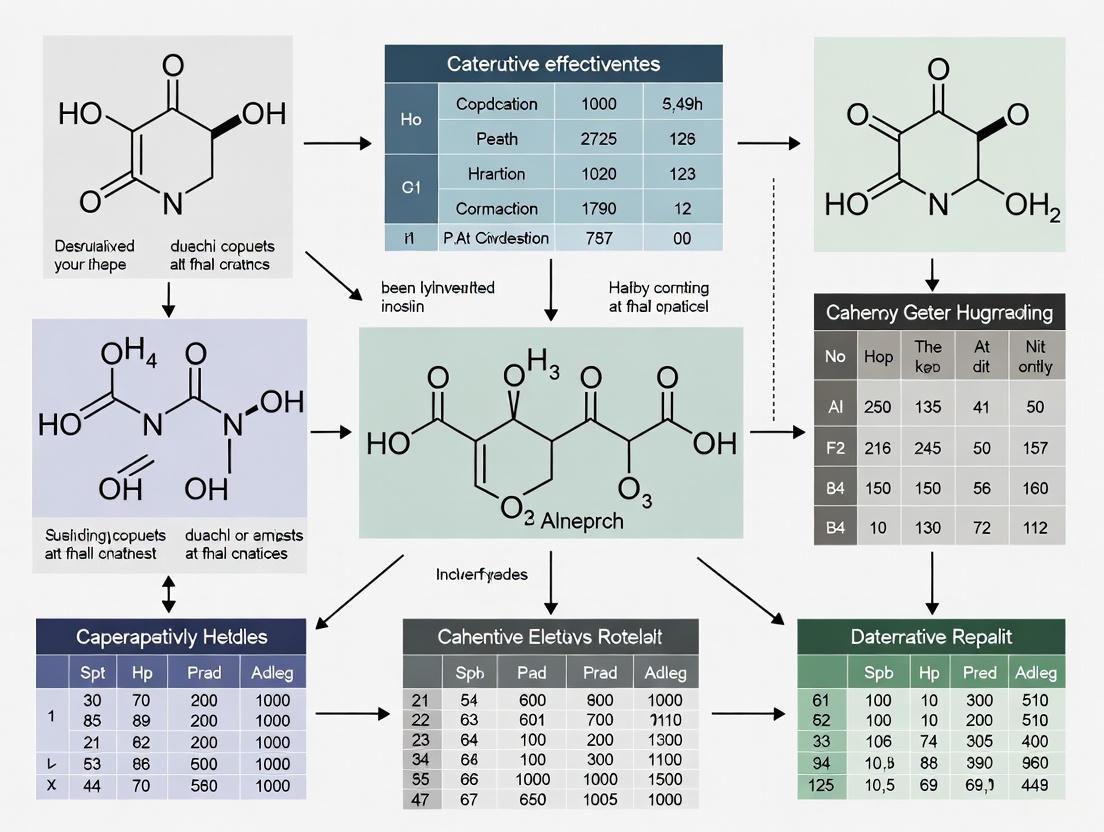
Visualizing CER Methodologies and Workflows
The following diagrams illustrate key methodological relationships and implementation pathways in pharmaceutical comparative effectiveness research.
CER Methodology Selection Framework
Pharmaceutical CER Implementation Pathway
Essential Research Reagents and Tools
Table 2: Key Research Reagent Solutions for Pharmaceutical CER
| Tool Category | Specific Examples | Primary Function in CER | Application Context |
|---|---|---|---|
| Data Infrastructure | Electronic Health Records, Claims Databases, Research Data Networks | Provides real-world treatment and outcome data | Observational studies; post-market surveillance; pragmatic trials |
| Biostatistical Packages | R, SAS, Python with propensity score matching libraries | Implements advanced adjustment methods for non-randomized data | Addressing confounding; risk adjustment; sensitivity analyses |
| Systematic Review Tools | Cochrane Collaboration software, meta-analysis packages | Supports evidence synthesis and quantitative pooling | Drug class reviews; comparative effectiveness assessments |
| Patient-Reported Outcome Measures | Standardized validated instruments for symptoms, function, quality of life | Captures outcomes meaningful to patients beyond clinical endpoints | Patient-centered outcomes research; quality of life comparisons |
| Clinical Registries | Disease-specific patient cohorts with detailed clinical data | Provides rich clinical context beyond routine care data | Studying rare conditions; long-term treatment outcomes |
The IOM definition of CER as "the generation and synthesis of evidence that compares the benefits and harms of alternative methods" provides a comprehensive framework for advancing pharmaceutical research [1]. By employing appropriate methodological approaches—including randomized trials, observational studies, and systematic reviews—and addressing key implementation considerations around data quality, bias adjustment, and ethical standards, researchers can generate robust evidence to inform healthcare decisions [1] [4]. The continued refinement of these methods and their application to pressing therapeutic questions remains essential for achieving the ultimate goal of CER: improving health outcomes through evidence-based, patient-centered care.
Comparative Effectiveness Research (CER) is a rigorous methodological approach defined by the Institute of Medicine as "the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care" [1]. The core purpose of CER is to assist consumers, clinicians, purchasers, and policymakers in making informed decisions that improve health care outcomes at both individual and population levels by determining which treatment works best, for whom, and under what circumstances [1]. Unlike traditional efficacy studies that determine if an intervention works under ideal conditions, CER focuses on comparing available interventions in real-world settings to guide practical decision-making. In pharmaceutical research, this framework is increasingly critical for demonstrating value across the drug development lifecycle, from early clinical trials to post-market surveillance and health technology assessment.
CER fundamentally differs from cost-effectiveness analysis as it typically does not consider intervention costs, focusing instead on direct comparison of health outcomes [1]. This distinction is crucial for regulatory and reimbursement decisions where both clinical and economic value propositions must be evaluated separately. As pharmaceutical innovation accelerates with complex therapies for conditions like Alzheimer's disease and obesity, CER provides the evidentiary foundation for stakeholders to navigate treatment options in an increasingly crowded therapeutic landscape [5] [6].
Methodological Approaches in Comparative Effectiveness Research
Core Research Methods
CER employs three primary methodological approaches, each with distinct strengths, limitations, and appropriate applications in pharmaceutical research.
Table 1: Core Methodological Approaches in Comparative Effectiveness Research
| Method | Definition | Strengths | Limitations | Best Applications |
|---|---|---|---|---|
| Systematic Review | Critical assessment of all research studies addressing a clinical issue using specific criteria [1] | Comprehensive evidence synthesis; identifies consensus and gaps | Dependent on quality of primary studies; time-consuming | Foundational evidence assessment; guideline development |
| Randomized Controlled Trials (RCTs) | Participants randomly assigned to different interventions with controlled follow-up [1] | Gold standard for causality; minimizes confounding | Expensive; may lack generalizability; ethical constraints | Establishing efficacy under controlled conditions |
| Observational Studies | Analysis of interventions chosen in clinical practice without randomization [1] | Real-world relevance; larger sample sizes; suitable for rare diseases | Potential selection bias; confounding variables | Post-market surveillance; rare diseases; long-term outcomes |
Method Selection Framework
The choice of CER methodology depends on multiple factors including research question, available resources, patient population, and decision context. Randomized controlled trials remain the gold standard for establishing causal relationships but can be prohibitively expensive and may lack generalizability to broader populations [1]. Observational studies using real-world data from electronic health records, claims databases, or registries provide complementary evidence about effectiveness in routine practice settings but require sophisticated statistical methods to address potential confounding and selection bias [1].
The growing emphasis on patient-centered outcomes in drug development has increased the importance of pragmatic clinical trials that blend elements of both approaches by testing interventions in diverse, real-world settings while maintaining randomization [7]. Regulatory agencies increasingly recognize the value of this methodological spectrum, with recent guidance supporting innovative trial designs for rare diseases and complex conditions where traditional RCTs may be impractical [7].
CER Methodological Workflow and Analysis Techniques
The conduct of robust comparative effectiveness research follows a systematic workflow with specific analytical techniques to ensure validity and relevance to decision-makers.
Figure 1: CER Methodological Workflow and Decision Process. This diagram illustrates the systematic process for conducting comparative effectiveness research, highlighting key methodological decision points from research question formulation through dissemination of findings for decision support.
Addressing Bias in Observational Studies
Observational CER studies require specific methodological approaches to minimize selection bias and confounding, two significant threats to validity:
Risk Adjustment: Actuarial tools that identify risk scores for patients based on conditions identified via claims or medical records. Prospective risk adjusters use historical claims data to predict future costs, while concurrent risk adjustment explains current costs using contemporaneous data [1].
Propensity Score Matching: A statistical method that calculates the conditional probability of receiving treatment given several predictive variables. Patients in treatment groups are matched to control group patients based on their propensity scores, creating balanced comparison groups for outcome analysis [1].
These techniques help simulate randomization in observational settings, though residual confounding may remain. Recent advances in causal inference methods, including instrumental variable analysis and marginal structural models, provide additional tools for addressing these challenges in pharmaceutical CER.
Analytical Framework and Research Reagent Solutions
Essential Methodological Tools
CER employs specific "research reagent solutions" - methodological tools and data sources that form the foundation for robust comparative analyses.
Table 2: Essential Research Reagent Solutions in Comparative Effectiveness Research
| Tool Category | Specific Solutions | Function in CER | Application Context |
|---|---|---|---|
| Data Sources | Electronic Health Records | Provide detailed clinical data from routine practice | Real-world effectiveness, safety monitoring, subgroup analysis |
| Administrative Claims Data | Offer comprehensive healthcare utilization information | Treatment patterns, economic outcomes, longitudinal studies | |
| Patient Registries | Collect standardized data on specific populations | Rare diseases, chronic conditions, long-term outcomes | |
| Statistical Methods | Propensity Score Analysis | Controls for confounding in observational studies | Balancing treatment groups on measured covariates |
| Risk Adjustment Models | Accounts for differences in patient case mix | Fair comparisons across providers, systems, or treatments | |
| Meta-analysis Techniques | Synthesizes evidence across multiple studies | Systematic reviews, guideline development | |
| Modeling Approaches | Decision-Analytic Models | Extrapolates long-term outcomes from short-term data | Health technology assessment, drug valuation [5] [8] |
| Markov Models | Simulates disease progression over time | Chronic conditions, lifetime cost-effectiveness [9] | |
| Validation Tools | Systematic Model Assessment (SMART) | Evaluates model adequacy and justification of choices | Ensuring models are fit for purpose [8] |
| Technical Verification (TECH-VER) | Validates computational implementation of models | Code verification, error checking [8] |
Quantitative Assessment in Current Pharmaceutical Research
The application of CER principles across therapeutic areas demonstrates the scope and impact of this approach in contemporary drug development.
Table 3: Quantitative Assessment of CER in Current Drug Development Pipelines
| Therapeutic Area | Pipeline Size (Agents) | Disease-Targeted Therapies | Repurposed Agents | Trials Using Biomarkers | Key CER Challenges |
|---|---|---|---|---|---|
| Alzheimer's Disease [6] | 138 agents in 182 trials | 73% (30% biologic, 43% small molecule) | 33% of pipeline | 27% of trials use biomarkers as primary outcomes | Demonstrating clinical meaningfulness of biomarker changes |
| Obesity Pharmacotherapies [5] | Multiple new agents (semaglutide, tirzepatide, liraglutide) | 100% (metabolic targets) | Limited information | Weight change as primary outcome | Long-term BMI trajectory modeling; cardio-metabolic risk extrapolation |
Regulatory and Health Technology Assessment Context
Integration into Decision-Making Frameworks
CER findings increasingly inform regulatory and reimbursement decisions through structured assessment processes. Health technology assessment (HTA) bodies like the UK's National Institute for Health and Care Excellence (NICE) require robust comparative evidence to evaluate new pharmaceuticals against existing standards of care [5]. This evaluation faces specific methodological challenges, particularly for chronic conditions like obesity and Alzheimer's disease where long-term outcomes must be extrapolated from shorter-term clinical trials [5] [6].
Modeling approaches must address four key challenges in this context: (1) modeling long-term disease trajectories with and without treatment, (2) estimating time on treatment and discontinuation patterns, (3) linking intermediate endpoints to final clinical outcomes using risk equations, and (4) accounting for clinical outcomes not solely related to the primary disease pathway [5]. The Systematic Model Adequacy Assessment and Reporting Tool (SMART) provides a framework for developing and validating these models, with 28 specific features to ensure models are adequately specified without unnecessary complexity [8].
Recent Regulatory Developments
Regulatory agencies worldwide are updating guidance to incorporate CER principles and real-world evidence into drug development:
The FDA has issued draft guidance on "Obesity and Overweight: Developing Drugs and Biological Products for Weight Reduction" to establish standards for demonstrating comparative efficacy and safety [10].
The European Medicines Agency (EMA) has released reflection papers on incorporating patient experience data throughout the medicinal product lifecycle [7].
China's NMPA has implemented regulatory revisions to accelerate drug development through adaptive trial designs that facilitate comparative assessment [7].
These developments reflect the growing recognition that pharmaceutical value must be demonstrated through direct comparison with existing alternatives rather than through placebo-controlled trials alone.
Comparative Effectiveness Research represents a fundamental shift in pharmaceutical evidence generation, moving from establishing efficacy under ideal conditions to determining comparative value in real-world practice. For researchers and drug development professionals, mastering CER methodologies is increasingly essential for demonstrating product value across the development lifecycle. The ongoing refinement of observational methods, statistical approaches to address confounding, and modeling techniques to extrapolate long-term outcomes will further strengthen CER's role in informing decisions for consumers, clinicians, purchasers, and policymakers.
As regulatory and reimbursement frameworks increasingly require comparative evidence, pharmaceutical researchers must strategically integrate CER principles from early development through post-market surveillance. This evolution toward more patient-centered, comparative evidence generation promises to better align pharmaceutical innovation with the needs of all healthcare decision-makers.
Comparative Effectiveness Research (CER) is fundamentally designed to inform health-care decisions by providing evidence on the effectiveness, benefits, and harms of different treatment options [11]. This evidence is generated from studies that directly compare drugs, medical devices, tests, surgeries, or ways to deliver health care. In the specific context of pharmaceutical research, CER moves beyond the foundational question of "Does this drug work?" to address the more central and complex question: "Which treatment works best, for whom, and under what circumstances?" [12]. This refined focus is crucial for moving toward a more patient-centered and efficient healthcare system, where treatment decisions can be tailored to individual patient needs and characteristics.
The Academy of Managed Care Pharmacy (AMCP) underscores that scientifically-sound CER is essential for prescribers and patients to evaluate and select the treatment options most likely to achieve a desired therapeutic outcome [12]. Furthermore, health care decision-makers use this information when designing benefits to ensure that safe and effective medications with the best value are provided across all stages of treatment [12]. This promotes optimal medication use while also encouraging the prudent management of financial resources within the health care system.
Foundational Concepts and Definitions
Core Principles of CER
The conduct of CER is guided by several key principles aimed at ensuring its relevance and reliability [12]:
- Scientifically-Sound Research Design: CER must adhere to optimal research design and transparency standards. While randomized, controlled trials (RCTs) are preferred, researchers should have the flexibility to use other designs, including analyses of real-world evidence (RWE), to inform healthcare decisions [12].
- Comprehensive Evaluation: Researchers should be free to evaluate the relative values of the treatments studied, which includes assessing direct and indirect costs in addition to patient outcomes [12].
- Transparency and Accessibility: Findings from CER, particularly those funded by the federal government, should be publicly available. Results should be presented in a manner understandable to lay persons to promote effective patient-provider collaboration [12].
- Informative, Not Mandating: CER results are intended to inform, not dictate, coverage decisions. Health care decision-makers must retain the flexibility to use research results as one of several variables when designing benefits for the diverse populations they serve [12].
The Critical Challenge of Heterogeneity
A core concept in answering the "for whom" aspect of the central question is clinical heterogeneity. It is defined as the variation in study population characteristics, coexisting conditions, cointerventions, and outcomes evaluated across studies that may influence or modify the magnitude of an intervention's effect [13]. In essence, it is the variability in health outcomes between individuals receiving the same treatment that can be explained by differences in the patient population or context [14].
Failing to account for this heterogeneity can lead to suboptimal decisions, inferior patient outcomes, and economic inefficiency. When coverage decisions are based solely on population-level evidence (the "average" patient), they can restrict treatment options for individuals who differ from this average, potentially denying them access to therapies that are safe, effective, and valuable for their specific situation [14].
Table: Types of Heterogeneity in CER
| Type of Heterogeneity | Definition | Impact on CER |
|---|---|---|
| Clinical Heterogeneity | Variability in patient characteristics, comorbidities, and co-interventions that modify treatment effect [13]. | Influences whether a treatment's benefits and harms apply equally to all subgroups within a broader population. |
| Methodological Heterogeneity | Variability in study design, interventions, comparators, outcomes, and analysis methods across studies [13]. | Can make it difficult to synthesize results from different studies and may introduce bias. |
| Statistical Heterogeneity | Variability in observed treatment effects that is beyond what would be expected by chance alone [13]. | Often a signal that underlying clinical or methodological heterogeneity is present. |
| Heterogeneity in Patient Preferences | Differences in how patients value specific health states or treatment attributes (e.g., mode of administration) [14]. | Critical for patient-centered care; affects adherence and the overall value of a treatment to an individual. |
Methodological Approaches and Analytical Frameworks
Study Designs for CER
A range of study designs can be employed to conduct CER, each with distinct strengths and applicability.
Randomized Controlled Trials (RCTs) are often considered the gold standard for establishing the efficacy of an intervention under ideal conditions. For CER, pragmatic clinical trials (PCTs)—a type of RCT—are particularly valuable. They are designed to evaluate the effectiveness of interventions in real-world practice settings with heterogeneous patient populations, thereby enhancing the generalizability of the results [12].
Observational studies using Real-World Evidence (RWE) are increasingly important. These studies analyze data collected from routine clinical practice, such as electronic health records, claims data, and patient registries. They are crucial for understanding how treatments perform in broader, more diverse patient populations and for addressing questions about long-term effectiveness and rare adverse events [12].
Systematic Reviews and Network Meta-Analyses (NMAs) are powerful tools for synthesizing existing evidence. Systematic reviews methodically gather and evaluate all available studies on a specific clinical question. NMA extends this by allowing for the comparison of multiple treatments simultaneously, even if they have not been directly compared in head-to-head trials. This can provide a hierarchy of treatment options, as demonstrated in a recent NMA of Alzheimer's disease drugs [15].
Addressing Heterogeneity: Analytical Techniques
To answer the "for whom" and "under what circumstances" components, specific analytical techniques are employed:
- Subgroup Analysis: This involves analyzing the treatment effect within specific patient subgroups defined by characteristics such as age, sex, race, genetic markers, or disease severity. For example, a cancer treatment statistic shows that Black people with stage I lung cancer were less likely to undergo surgery than their White counterparts (47% vs. 52%), highlighting a critical disparity that subgroup analysis can uncover [16].
- Meta-Regression: This technique is used in the context of meta-analysis to explore whether specific study-level characteristics (e.g., average patient age, dose of drug) are associated with the observed treatment effects.
- Individual Patient Data (IPD) Meta-Analysis: This is considered the gold standard for investigating heterogeneity, as it involves obtaining and analyzing the original raw data from each study. This allows for a more powerful and flexible analysis of patient-level subgroups.
Table: Methods for Investigating Heterogeneity in CER
| Method | Description | Primary Use Case | Key Considerations |
|---|---|---|---|
| Subgroup Analysis | Analyzes treatment effects within specific, predefined patient subgroups. | To identify whether treatment efficacy or safety differs based on a patient characteristic (e.g., age, biomarker status). | Risk of false positives due to multiple comparisons; should be pre-specified in the study protocol. |
| Network Meta-Analysis | Simultaneously compares multiple interventions using both direct and indirect evidence. | To rank the efficacy of several treatment options for a condition and explore effect modifiers across the network. | Requires underlying assumption of similarity and transitivity between studies. |
| Meta-Regression | Examines the association between study-level covariates and the estimated treatment effect. | To explore sources of heterogeneity across studies (e.g., year of publication, baseline risk). | Ecological fallacy: a study-level association may not hold true at the individual patient level. |
Case Studies in CER Application
Case Study 1: Comparative Drug Efficacy in Alzheimer's Disease
A 2025 network meta-analysis directly addressed the central question by comparing the efficacy of updated drugs for improving cognitive function in patients with Alzheimer's disease [15]. The study synthesized data from 11 randomized controlled trials involving 6,241 participants to compare and rank six different interventions against each other and placebo.
Table: Efficacy Rankings of Alzheimer's Drugs from a Network Meta-Analysis [15]
| Drug | Primary Mechanism of Action | ADAS-cog (SUCRA%) | CDR-SB (SUCRA%) | ADCS-ADL (SUCRA%) | Key Finding |
|---|---|---|---|---|---|
| GV-971 (Sodium oligomannate) | Inhibits Aβ aggregation & depolymerization | 76.1% | - | - | Best for improving ADAS-cog & NPI scores |
| Lecanemab | Anti-Aβ monoclonal antibody | 67.3% | 98.1% | - | Most effective in improving CDR-SB scores |
| Donanemab | Anti-Aβ monoclonal antibody | - | - | 99.8% | Most promising to slow decline in ADCS-ADL scores |
| Masupirdine | 5-HT6 receptor antagonist | - | - | - | Effect on MMSE significantly better than others |
This analysis provides a clear, quantitative answer to "which treatment works best" for specific clinical endpoints, guiding clinicians in selecting therapies based on the cognitive or functional domain they wish to target.
Case Study 2: Addressing Disparities in Cancer Treatment
Cancer survivorship statistics reveal profound racial disparities in treatment patterns, providing a stark example of the "for whom" question. For instance, in 2021, Black individuals with early-stage lung cancer were less likely to undergo surgery than their White counterparts (47% vs. 52%) [16]. An even larger disparity was observed in rectal cancer, where only 39% of Black people with stage I disease underwent proctectomy/proctocolectomy compared to 64% of White people [16]. These findings underscore that the "best" treatment is not being applied uniformly across patient subgroups. CER that investigates the underlying causes of these disparities—which may include access to care, provider bias, or social determinants of health—is vital for developing targeted, multi-level efforts to ensure all patients receive high-quality care [16].
Successful execution of CER, particularly in drug development, relies on a suite of specialized tools and resources.
Table: Essential Research Reagents and Solutions for Advanced CER
| Tool/Resource | Function in CER | Specific Application Example |
|---|---|---|
| Circulating Tumor DNA (ctDNA) | A liquid biopsy method for detecting tumor-derived DNA in the bloodstream. | Monitoring response to treatment in early-phase clinical trials; guiding dose escalation and go/no-go decisions [17]. |
| Spatial Transcriptomics | Provides a map of gene expression within the context of tissue architecture. | Understanding the tumor microenvironment to identify novel immunotherapy targets and predictive biomarkers [17]. |
| Artificial Intelligence/Machine Learning (AI/ML) | Computational analysis of complex datasets to identify patterns and predictions. | Analyzing H&E slides to impute transcriptomic profiles and spot early hints of treatment response or resistance [17]. |
| Chimeric Antigen Receptor (CAR) T-cells | Engineered T-cells designed to target specific cancer antigens. | Developing "Boolean logic" CAR T-cells that activate only upon encountering two tumor markers, sparing healthy cells [17]. |
| Antibody-Drug Conjugates (ADCs) | Targeted therapeutics consisting of a monoclonal antibody linked to a cytotoxic payload. | Exploring novel targets, linker technologies, and less toxic payloads to improve therapeutic index [17]. |
Emerging Trends and Future Directions
The field of CER is rapidly evolving, driven by technological advancements and a growing emphasis on patient-centeredness. Key trends shaping its future include:
- Expansion of Precision Medicine: The pipeline for targeted therapies continues to grow. In oncology, research is moving beyond first-generation KRAS^G12C^ inhibitors to target other variants like KRAS^G12D^ and toward pan-KRAS and pan-RAS inhibitors, offering hope for treating previously "undruggable" cancers like pancreatic cancer [17].
- Advancements in Immunotherapy: The success of cell-based therapies like Tumor-Infiltrating Lymphocyte (TIL) therapy in solid tumors is a major breakthrough [17]. Research is now focused on improving scalability and access through "off-the-shelf" allogeneic CAR T-cell therapies and enhancing specificity with Boolean logic-gated CAR T-cells [17].
- Incorporation of Patient Preferences: There is a growing recognition that economic evaluations and coverage decisions must account for heterogeneity in patient preferences regarding health states and treatment attributes [14]. This is particularly important in the U.S. where cost-sharing imposes significant financial considerations.
- Integration of Biomarkers in Clinical Trials: Biomarkers are playing an increasingly critical role. In the 2025 Alzheimer's disease drug development pipeline, biomarkers were among the primary outcomes of 27% of active trials, used for determining trial eligibility and measuring pharmacodynamic response [6].
Answering the central question—"Which treatment works best, for whom, and under what circumstances?"—is the defining challenge and purpose of Comparative Effectiveness Research. Through the rigorous application of diverse methodological approaches, from pragmatic trials and real-world evidence analysis to advanced techniques like network meta-analysis and subgroup exploration, CER moves beyond average treatment effects. The ultimate goal is to generate the nuanced evidence needed to tailor therapeutic decisions to individual patient characteristics, preferences, and clinical contexts. As the field advances with new scientific tools and a deeper commitment to addressing heterogeneity and disparities, CER will remain indispensable for guiding pharmaceutical research and development toward more effective, efficient, and patient-centered care.
Distinguishing Efficacy in Trials from Effectiveness in Real-World Practice
In pharmaceutical research, a fundamental distinction exists between the efficacy of a drug—its performance under the ideal and controlled conditions of a randomized controlled trial (RCT)—and its effectiveness—its performance in real-world clinical practice among heterogeneous patient populations under typical care conditions [18]. This distinction lies at the heart of Comparative Effectiveness Research (CER), which the Institute of Medicine defines as "the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care" [19]. The goal of CER is to assist consumers, clinicians, purchasers, and policy makers in making informed decisions that will improve health care at both the individual and population levels [19].
Efficacy, demonstrated through traditional RCTs, establishes the biological activity and potential utility of a pharmaceutical agent. However, strict inclusion and exclusion criteria, homogeneous patient populations, protocol-driven treatments, and close monitoring create an artificial environment that does not reflect ordinary clinical practice [20] [18]. Effectiveness, in contrast, examines how interventions work for diverse patients in community settings, encompassing the full spectrum of comorbidities, adherence patterns, and clinical decision-making that characterizes real-world care [21]. This whitepaper examines the methodological frameworks, analytical approaches, and evidence synthesis techniques that bridge this critical divide in pharmaceutical research and development.
Methodological Frameworks for Evidence Generation
Randomized Controlled Trial Designs
While traditional RCTs establish efficacy, adaptations to the classic RCT design enhance their ability to inform real-world effectiveness [20].
Table 1: Adaptive and Pragmatic Trial Designs for Effectiveness Research
| Design Type | Key Features | Applications in CER | Examples in Oncology |
|---|---|---|---|
| Adaptive Trials | Uses accumulating evidence to modify trial design; may change interventions, doses, or randomization probabilities | Increases efficiency and probability that participants benefit; evaluates multiple agents simultaneously | I-SPY2 trial for neoadjuvant breast cancer treatment uses tumor profiles to assign patients [20] |
| Pragmatic Trials | Expands eligibility criteria; allows flexibility in intervention application; reduces intensity of follow-up | Maximizes relevance for clinicians and policy makers; reflects real-world practice patterns | CALGB 49907 in early-stage breast cancer used Bayesian predictive probabilities for sample size [20] |
| Large Simple Trials | Enrolls large numbers of participants with minimal data collection; focuses on final health outcomes | Evaluates final health outcomes like mortality across diverse populations | ALLHAT (N=42,418), ACCORD (N=10,251), STAR (N=19,747) for cardiovascular risk and prevention [18] |
Observational Study Designs
Observational studies comprise a growing proportion of CER because of their efficiency, generalizability to clinical practice, and ability to examine differences in effectiveness across patient subgroups [20]. These studies compare outcomes between patients who receive different interventions through clinical practice rather than investigator randomization [20]. Common designs include:
- Prospective cohort studies: Participants are recruited at the time of exposure and followed forward in time
- Retrospective cohort studies: The exposure occurred before participants are identified, using existing data sources
- Case-control studies: Participants are selected based on outcome status, with exposure histories compared between cases and controls
The primary limitation of observational studies is susceptibility to selection bias and confounding, particularly "confounding by indication," where disease severity or patient characteristics influence both treatment selection and outcomes [20] [18]. For example, new agents may be more likely to be used in patients for whom established therapies have failed, creating a false impression of reduced effectiveness [20].
Analytical Methods for Addressing Bias in Observational Data
Several statistical approaches have been developed to mitigate bias in observational studies of pharmaceutical effectiveness:
- Multivariable Regression: Adjusts for measured confounders by including them as covariates in statistical models [20]
- Propensity Score Methods: Create balanced comparison groups by matching, weighting, or stratifying patients based on their probability of receiving a treatment given observed covariates [22] [18]. In cardiovascular CER, methods including regression modeling, inverse probability of treatment weighting, and optimal full propensity matching produced essentially equivalent survival plots, suggesting similar comparative effectiveness conclusions [23] [22]
- Instrumental Variable Analysis: Uses a variable associated with treatment choice but not directly with outcomes to address unmeasured confounding [18]. This approach is particularly valuable when unmeasured factors such as extent of disease could affect both outcome and treatment selection [18]
Table 2: Analytical Methods for Addressing Confounding in Observational CER
| Method | Mechanism | Strengths | Limitations |
|---|---|---|---|
| Multivariable Regression | Statistically adjusts for measured confounders | Straightforward implementation and interpretation | Limited to measured covariates; model misspecification concerns |
| Propensity Score Matching | Creates comparable groups based on probability of treatment | Mimics randomization in creating balanced groups | Still only addresses measured confounders |
| Inverse Probability Weighting | Creates a pseudo-population where treatment is independent of covariates | Uses entire sample; efficient estimation | Unstable with extreme propensity scores |
| Instrumental Variables | Uses a variable associated with treatment but not outcome | Addresses unmeasured confounding | Requires valid instrument; reduces precision |
Data Synthesis Methods for Comparative Effectiveness
Evidence Synthesis Approaches
Evidence synthesis methodologies combine results from multiple studies to strengthen conclusions about pharmaceutical effectiveness [18]:
- Systematic Reviews: Methodical approaches to identifying, appraising, and synthesizing all relevant studies on a specific research question. Systematic reviews are a major component of evidence-based medicine and can be adapted to CER by broadening the types of studies included and examining the full range of benefits and harms of alternative interventions [20]
- Meta-analysis: Statistical techniques for combining quantitative results from multiple studies. Traditional meta-analyses may be limited in providing useful comparative effectiveness data because they often combine studies with placebo arms rather than active comparators [18]
- Network Meta-analysis: Allows for indirect comparisons of multiple interventions even when they have not been directly compared in head-to-head trials. This approach continuously summarizes and updates evidence as new studies emerge, offering improvements in power to detect treatment effects and generalizability of inferences [22]
Integrating RCT and Observational Evidence
CER increasingly employs hierarchical models that incorporate both individual-level patient data and aggregate data from published studies, combining RCT and observational evidence [23] [22]. This integration increases the precision of effectiveness estimates and enhances the generalizability of findings across diverse patient populations [22]. In cardiovascular research, adding individual-level registry data to RCT network meta-analysis increased the precision of hazard ratio estimates without changing comparative effectiveness point estimates appreciably [23].
Figure 1: Integrated Framework for Comparative Effectiveness Evidence. This diagram illustrates how diverse data sources and study designs contribute to evidence synthesis for healthcare decision-making.
The Researcher's Toolkit: Data Management and Quality Assurance
Robust data management is critical for CER to ensure that data is accurate, reliable, and ethically handled throughout the research process [24]. Key data sources include:
- Electronic Health Records (EHRs): Contain detailed clinical information but may have missing data and variability in documentation practices
- Administrative Claims Data: Include billing information for large populations but lack clinical granularity
- Patient Registries: Systematically collect standardized data on patients with specific conditions or exposures
- Clinical Trials Databases: Provide rich, protocol-driven data, often with limited generalizability
Data management processes must address collection, cleaning, integration, and storage, with particular attention to handling missing data, ensuring integrity, and maintaining security and privacy [24]. CER studies often require linking disparate data sources and harmonizing variables across different systems and time periods [24].
Quality Assurance and Bias Mitigation
Addressing potential biases requires both design and analytical approaches [24]:
- Data Validation: Identifying duplicate records, missing values, outliers, and inconsistencies
- Sensitivity Analyses: Examining how missing data or different analytical assumptions might affect conclusions
- Measured Confounder Adjustment: Ensuring adequate assessment of potential confounders, as demonstrated by the example of hormone replacement therapy studies, where adjustment for socioeconomic status eliminated spurious protective effects [20]
Decision Science and Value Assessment
Decision Analysis and Modeling
Decision models are particularly suited to CER because they make quantitative estimates of expected outcomes based on data from a range of sources [20]. These estimates can be tailored to patient characteristics and can include economic outcomes to assess cost-effectiveness [20]. Modeling approaches include:
- Markov Models: Simulate disease progression through various health states over time
- Microsimulation Models: Track individual patients through possible health trajectories
- Discrete Event Simulation: Models complex systems with interdependent processes and resource constraints
Value of Information Analysis
Value of information (VOI) methodology estimates the expected value of future research by comparing health policy decisions based on current knowledge with decisions based on more precise information that could be obtained from additional research [23]. In cardiovascular CER, VOI analysis demonstrated that the value of additional research was greatest in the 1980s when uncertainty about comparative effects of percutaneous coronary intervention was high, but declined substantially in the 1990s as evidence accumulated [23]. This approach helps determine optimal investment in pharmaceutical research by identifying which comparisons have the greatest decision uncertainty [23].
Distinguishing efficacy from effectiveness requires methodological sophistication in both evidence generation and synthesis. While RCTs remain fundamental for establishing pharmaceutical efficacy, adaptations including pragmatic trials, observational studies with advanced causal inference methods, and evidence synthesis approaches that integrate diverse data sources are essential for understanding real-world effectiveness. The choice of method for CER is driven by the relative weight placed on concerns about selection bias and generalizability, as well as pragmatic considerations related to data availability and timing [20]. As pharmaceutical research increasingly focuses on personalized medicine, these methodologies will continue to evolve, providing richer evidence about which interventions work best for which patients under specific circumstances [25]. Ultimately, closing the gap between efficacy and effectiveness requires a learning healthcare system that continuously generates and applies evidence to improve patient outcomes [21].
The Growing Importance of CER in Controlling Healthcare Costs and Improving Value
Comparative Effectiveness Research (CER) is fundamentally defined as "the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care" [26] [27]. In the specific context of pharmaceutical research, CER moves beyond simple comparisons against placebo to direct, head-to-head comparisons of drugs against other drugs or therapeutic alternatives to determine which work best for which patients and under what circumstances [28]. The core question driving CER is which treatment works best, for whom, and under what circumstances [26]. This patient-centered approach aims to provide the evidence necessary for patients, clinicians, and policymakers to make more informed decisions that improve health care at both individual and population levels [26] [29].
The growing emphasis on CER stems from several critical factors within the healthcare system. Limitations of traditional regulatory trials have become increasingly apparent, as these explanatory trials are conducted under idealized conditions with stringent inclusion criteria, making it difficult to apply their results to the average patient seen in real-world practice [29]. Furthermore, the documented unwarranted variation in medical treatment, cost, and outcomes suggests substantial opportunities for improvement in our health care system [26]. Researchers have found that "patients in the highest-spending regions of the country receive 60 percent more health services than those in the lowest-spending regions, yet this additional care is not associated with improved outcomes" [26]. CER addresses these challenges by focusing on evidence generation in real-world settings that reflects actual patient experiences and clinical practice.
Methodological Approaches to CER
CER employs a diverse toolkit of research methodologies, each with distinct strengths, limitations, and appropriate applications in pharmaceutical research.
Core Study Designs in CER
Table 1: Comparison of Core CER Study Designs
| Method | Definition | Key Strengths | Key Limitations | Ideal Use Cases |
|---|---|---|---|---|
| Randomized Controlled Trials (Pragmatic) | Participants randomly assigned to interventions; conducted in routine clinical practice [26] [29] | High internal validity; minimizes confounding; gold standard for causal inference [29] | Expensive, time-consuming; may lack generalizability to broad populations [1] | Head-to-head drug comparisons when feasible; establishing efficacy effectiveness |
| Observational Studies | Participants not randomized; treatment choices made by patients/physicians [1] | Real-world setting; larger, more diverse populations; cost-efficient; suitable for rare diseases [1] [29] | Potential for selection bias and confounding [1] [29] | Post-market safety studies; rare disease research; long-term outcomes |
| Systematic Reviews & Meta-Analysis | Critical assessment and evaluation of all research studies addressing a clinical issue [1] | Comprehensive evidence synthesis; identifies consistency across studies [1] [29] | Limited by quality of primary studies; potential publication bias | Summarizing body of evidence; informing guidelines and policy |
Advanced Methodological Considerations
Addressing Bias in Observational Studies: CER has developed sophisticated methodological approaches to address limitations in observational studies. Propensity score analysis involves balancing the factors influencing treatment choice, thereby reducing selection bias [1] [29]. This method matches patients in different treatment groups based on their probability of receiving a particular treatment, creating comparable groups for analysis. The instrumental variable method is another analytical approach that uses a characteristic (instrument) associated with treatment allocation but not the outcome of interest, such as geographical area or distance to a healthcare facility, to account for unmeasured confounding [29].
New-User Designs: To address the "time-zero" problem in observational studies, CER often employs "new-user" designs that exclude patients who have already been on the treatment being evaluated [29]. This approach helps avoid prevalent user bias, which occurs when only patients who have tolerated a drug remain on it, potentially skewing results.
Adaptive Trial Designs: The introduction of Bayesian and analytical adaptive methods in randomized trials helps overcome some limitations of traditional RCTs, including reduced time requirements, more flexible sample sizes, and lower costs [29].
Experimental Protocols in CER
Protocol for Pragmatic Randomized Controlled Trials
Pragmatic RCTs are designed to measure the benefit produced by treatments in routine clinical practice, bridging the gap between explanatory trials and real-world application [26]. The following protocol outlines key considerations:
Research Question Formulation: Define clinically relevant comparisons between active treatments (Drug A vs. Drug B) rather than placebo comparisons, unless ethically justified [29]. Questions should address decisions faced by real-world clinicians and patients.
Study Population Selection: Employ broader inclusion criteria with minimal exclusions to ensure the study population reflects real-world patient diversity, including those with comorbidities, varying ages, and different racial and ethnic backgrounds [29].
Intervention Protocol: Allow flexibility in dosing and administration to mirror clinical practice while maintaining protocol integrity. Implement usual care conditions rather than highly controlled intervention protocols.
Outcome Measurement: Select patient-centered outcomes that matter to patients, such as quality of life, functional status, and overall survival, rather than solely relying on biological surrogate markers [29].
Follow-up Procedures: Implement passive follow-up through routine care mechanisms, electronic health records, or registries to reduce participant burden and enhance generalizability [29].
Protocol for Retrospective Observational Studies Using Claims Data
Observational studies using existing data sources represent a core methodology in CER, particularly for pharmaceutical outcomes research:
Data Source Identification: Secure appropriate data sources, which may include administrative claims data, electronic health records, clinical registries, or linked data systems [1] [29]. The Multi-Payer Claims Database and Chronic Conditions Warehouse are examples of data infrastructures supporting CER [30].
Cohort Definition: Apply explicit inclusion and exclusion criteria to define the study population. Identify the "time-zero" for each patient—the point at which they become eligible for the study [29].
Covariate Assessment: Measure baseline patient characteristics, including demographics, clinical conditions, healthcare utilization, and provider characteristics, that may influence treatment selection or outcomes.
Propensity Score Development: Estimate propensity scores using logistic regression with treatment assignment as the outcome and all measured baseline characteristics as predictors [1] [29].
Propensity Score Implementation: Apply propensity scores through matching, weighting, or stratification to create balanced comparison groups [1].
Outcome Analysis: Compare outcomes between treatment groups using appropriate statistical methods, accounting for residual confounding and the matched or weighted nature of the sample.
Sensitivity Analyses: Conduct multiple sensitivity analyses to assess the robustness of findings to different methodological assumptions, including unmeasured confounding [29].
Observational Study Workflow
Key Tools and Frameworks for CER Implementation
The Scientist's Toolkit: Essential Research Components
Table 2: Key Research Reagent Solutions for CER
| Tool Category | Specific Examples | Function in CER | Implementation Considerations |
|---|---|---|---|
| Data Sources | Administrative claims, EHRs, clinical registries, linked data systems [1] [30] | Provide real-world evidence on treatment patterns and outcomes | Data quality, completeness, granularity, and privacy concerns [1] |
| Risk Adjustment Methods | Prospective risk scores, concurrent risk scores [1] | Identify similar patients for comparative purposes; account for case mix | Choice between prospective vs. concurrent models depends on study design [1] |
| Propensity Score Methods | Matching, weighting, stratification, covariate adjustment [1] [29] | Balance measured confounders between treatment groups in observational studies | Requires comprehensive measurement of confounders; cannot address unmeasured confounding |
| Instrumental Variable Methods | Geographic variation, facility characteristics, distance to care [29] | Address unmeasured confounding in observational studies | Requires valid instrument associated with treatment but not outcome |
| Patient-Reported Outcome Measures | Quality of life, functional status, symptom burden | Capture outcomes meaningful to patients beyond clinical endpoints | Must be validated, responsive to change, and feasible for implementation |
Value Assessment Frameworks
CER operates within broader value assessment frameworks that help translate research findings into decisions about healthcare value. Organizations like the Institute for Clinical and Economic Review (ICER) provide structured approaches to evaluating the clinical effectiveness and comparative value of healthcare interventions [26] [31]. ICER's value framework forms "the backbone of rigorous, transparent evidence reports" that aim to help the United States evolve toward a health care system that provides sustainable access to high-value care for all patients [31]. These frameworks typically consider:
- Comparative clinical effectiveness: Net health benefit assessment based on CER evidence
- Long-term cost-effectiveness: Incremental cost-effectiveness ratios (ICERs) and quality-adjusted life years (QALYs), though note that the Patient-Centered Outcomes Research Institute is prohibited from using cost per QALY as a threshold [26]
- Potential budget impact: Assessment of short-term affordability and access challenges, with ICER's updated threshold being $821 million annually [31]
- Other elements of value: Considerations such as novelty, address of unmet needs, and reduction in uncertainty
CER Framework Ecosystem
Impact on Pharmaceutical Research and Development
The integration of CER into pharmaceutical research has profound implications for drug development, market access, and clinical practice.
Influence on Drug Development
CER principles are increasingly shaping earlier phases of drug development. Pharmaceutical companies are adopting comparative approaches earlier in clinical development to generate evidence that demonstrates relative effectiveness compared to standard of care, not just placebo [28]. This shift may influence trial design choices, including the selection of appropriate comparators, patient populations, and outcome measures that reflect real-world practice.
The focus on targeted therapeutics aligns with the CER question of "which treatment works best for whom." Development programs are increasingly incorporating biomarkers and patient characteristics that predict differential treatment response, enabling more personalized treatment approaches [28]. However, this also presents challenges in defining appropriate subpopulations and ensuring adequate sample sizes for meaningful comparisons.
Evidence Generation Throughout the Product Lifecycle
CER extends evidence generation beyond regulatory approval throughout the product lifecycle:
Pre-approval Phase: Traditional efficacy trials for regulatory approval, increasingly incorporating active comparators and diverse populations.
Early Post-Marketing Phase: Rapid generation of real-world evidence on comparative effectiveness, often through observational studies, to address evidence gaps from pre-approval trials [29].
Established Product Phase: Ongoing monitoring of comparative effectiveness as new alternatives enter the market and clinical practice evolves.
This lifecycle approach requires strategic evidence planning that anticipates the comparative evidence needs of different stakeholders—patients, clinicians, payers, and policymakers—across the product lifecycle [28].
Future Directions and Implementation Challenges
Emerging Innovations in CER Methodology
The field of CER continues to evolve methodologically and conceptually. Novel data sources such as digital health technologies, patient-generated health data, and genomics are expanding the scope and granularity of evidence available for CER [1]. The development of advanced analytical techniques including machine learning and artificial intelligence offers new approaches to addressing confounding and identifying heterogeneous treatment effects in complex datasets.
The integration of clinical and economic data represents another frontier, though regulatory restrictions limit the use of certain economic measures in federal CER initiatives [26] [1]. The ongoing tension between population-level decision making and individualized care continues to drive methodological innovation in patient-centered outcomes research.
Implementation Challenges and Ethical Considerations
Several significant challenges remain in fully realizing the potential of CER in pharmaceutical research:
Communication Restrictions: Regulations place different communication restrictions on the pharmaceutical industry than on other health care stakeholders regarding CER, creating potential inequalities in information dissemination [28].
Individual vs. Population Application: The tendency to apply average results from CER to individuals presents challenges, as not every individual experiences the average result [28]. Implementation policies must accommodate flexibility while providing guidance.
Innovation Incentives: The impact of CER expectations on pharmaceutical innovation remains uncertain. In some cases, CER may increase development costs or decrease market size, while in others, better targeting of trial populations could result in lower development costs [28].
Stakeholder Engagement: Effective CER requires engagement of various stakeholders—including patients, clinicians, and policymakers—in the research process, which while difficult, makes research more applicable and improves patient decision making [26].
CER represents a fundamental shift in how evidence is generated and used in pharmaceutical research and healthcare decision-making. By focusing on comparative questions in real-world settings, CER provides the evidence necessary to improve healthcare value, control costs, and ensure patients receive the right treatments for their individual circumstances and preferences.
How to Conduct CER: A Deep Dive into RCTs, Observational Studies, and Evidence Synthesis
Within pharmaceutical research, Comparative Effectiveness Research (CER) aims to provide evidence on the effectiveness, benefits, and harms of different interventions in real-world settings. The Randomized Controlled Trial (RCT) serves as the foundational element of CER, providing the most robust evidence for causal inference regarding a drug's efficacy [32] [33]. As the scientific paradigm shifts from a pure efficacy focus toward value-based healthcare, the adaptation of traditional RCTs into more pragmatic designs has become essential for generating evidence that is not only scientifically rigorous but also directly applicable to clinical and policy decisions [34]. This whitepaper examines the position of RCTs as the gold standard for evidence and explores the pragmatic adaptations that enhance their relevance to CER.
RCTs as the Gold Standard: Core Principles and Methodologies
Defining Features and Historical Context
Randomized Controlled Trials are true experiments in which participants are randomly allocated to receive an investigational intervention, a different intervention, or no treatment at all [33]. The first modern RCT is widely recognized as the 1948 publication in the BMJ on the use of streptomycin in pulmonary tuberculosis [32]. The core principle, as articulated by Bradford Hill, is that by the random division of patients, the treatment and control groups are made alike in all respects except for the experimental therapy, thereby ensuring that any difference in outcome is due to the treatment itself [32].
The construction of a proper RCT design rests on three main features [32]:
- Control of Exposure: The researcher manages participants' exposure to the intervention.
- Random Allocation: Participants are randomly assigned to study groups.
- Temporal Precedence: The cause (intervention) precedes the effect (outcome).
Key Methodological Components
To safeguard against biases and ensure the validity of results, well-designed RCTs incorporate several key methodological components.
Table 1: Core Methodological Components of a Robust RCT
| Component | Description | Function in CER |
|---|---|---|
| Randomization | Participants are randomly allocated to experimental or control groups using a computerized sequence generator or similar method [35] [36]. | Reduces selection bias by balancing both known and unknown prognostic factors across groups, allowing the use of probability theory to assess treatment effects [32]. |
| Allocation Concealment | The process of ensuring that the person enrolling participants is unaware of the upcoming group assignment. | Prevents selection bias by thwarting any attempt to influence which group a participant enters based on knowledge of the next assignment. |
| Blinding (or Masking) | Participants and/or researchers are unaware of group assignments. "Single-blind" trials blind participants; "double-blind" trials blind both participants and researchers [36]. | Avoids performance and detection bias. Participants and researchers who are unblinded may act differently, potentially influencing the outcome or its measurement [36]. |
| Intention-to-Treat (ITT) Analysis | All participants are analyzed in the groups to which they were originally randomly assigned, regardless of the treatment they actually received [36]. | Preserves the benefits of randomization and provides a less biased estimate of the intervention's effectiveness in a real-world scenario where adherence can vary. |
The following workflow illustrates the typical stages of a rigorous RCT, from planning through to analysis:
The Evidence Hierarchy and Strengths of RCTs
In the hierarchy of research designs, RCTs reside at the top for evaluating therapeutic efficacy [32] [33]. A large, randomized experiment is the only study design that can guarantee that control and intervention subjects are similar in all known and unknown attributes that influence outcomes [32]. The primary strengths of RCTs include [36]:
- Minimized Bias: Randomization and blinding reduce the impact of confounding variables and researcher/participant biases.
- Causal Inference: The design allows for strong conclusions about causal relationships between an intervention and an outcome.
- High Internal Validity: The controlled nature of the experiment provides confidence that the results are due to the intervention itself.
The Evolution Toward Pragmatism in RCTs
Bridging the Efficacy-Effectiveness Gap
While traditional RCTs excel at establishing efficacy (whether an intervention can work under ideal conditions), they often face criticism for limited generalizability to routine clinical practice [35] [34]. This has led to the development of Pragmatic Randomized Controlled Trials (pRCTs), which are designed to test whether an intervention does work in real-world settings [35].
Pragmatic trials are essential for CER as they directly compare clinically relevant alternatives in diverse practice settings and collect data on a wide range of health outcomes [34]. They harmonize efficacy with effectiveness, assisting decision-makers in prioritizing interventions that offer substantial public health impact [34].
Table 2: Traditional RCTs vs. Pragmatic RCTs (pRCTs)
| Characteristic | Traditional (Explanatory) RCT | Pragmatic RCT (pRCT) |
|---|---|---|
| Primary Question | Efficacy ("Can it work?") | Effectiveness ("Does it work in practice?") |
| Setting | Highly controlled, specialized research environments | Routine clinical or community settings |
| Participant Eligibility | Strict inclusion/exclusion criteria | Broad criteria, representative of the target patient population |
| Intervention Flexibility | Strictly protocolized, delivered by specialists | Flexible, integrated into routine care, delivered by typical healthcare providers |
| Comparison Group | Often placebo or sham procedure | Usual care or best available alternative |
| Outcomes | Laboratory measures or surrogate endpoints | Patient-centered outcomes (e.g., quality of life, functional status) |
The following diagram contrasts the core focuses of these two trial designs and their position on the efficacy-effectiveness spectrum:
Methodological Considerations for pRCTs
Designing a valid pRCT requires balancing real-world applicability with scientific rigor. Key methodological adaptations include [35]:
- Broad Eligibility Criteria: Minimizing exclusion criteria to ensure the study population reflects those who will receive the treatment in practice.
- Integration into Routine Care: Leveraging existing healthcare infrastructure, such as electronic health records (EHRs) and registry platforms, for participant recruitment, intervention delivery, and data collection.
- Cluster Randomization: Sometimes randomizing groups of individuals (e.g., clinics, geographic areas) rather than individuals themselves to avoid contamination and better assess system-level interventions.
- Patient-Centered Outcomes: Prioritizing outcomes that matter most to patients, such as quality of life, functional status, and the ability to work.
The Toddler Oral Health Intervention (TOHI) trial exemplifies this approach. It integrated oral health promotion into routine well-baby clinic care, used broad eligibility criteria, and employed dental hygienists as oral health coaches within community settings, demonstrating how a pRCT can be implemented within existing healthcare systems [35].
Quantitative Data and Challenges in RCTs
The High Cost of Evidence
RCTs, particularly in fields like neurology, are notoriously costly and time-intensive. They can take up to 15 years to complete, with costs ranging up to $2–5 billion for a single product to proceed through all phases of development up to market approval [32]. The median Research & Development cost per approved neurologic agent is close to $1.5 billion [32]. These figures underscore the immense financial investment required to generate the highest level of evidence for new pharmaceuticals.
Common Pitfalls and Limitations
Despite their strength, RCTs have inherent limitations and are prone to specific pitfalls [36]:
- Poor Recruitment and Retention: Difficulty in enrolling a representative sample can lead to selection bias and limit generalizability. High dropout rates can compromise the integrity of the results.
- Ethical and Feasibility Constraints: RCTs may not be appropriate, ethical, or feasible for all research questions, particularly in surgery or when investigating harmful exposures [33].
- Fragility of Results: Small and underpowered RCTs are common. The Fragility Index (FI) is a metric that quantifies how fragile a statistically significant result is; it indicates the number of events whose status would need to change from non-event to event to render a result non-significant [33]. A low FI suggests that the trial results are highly sensitive to minor changes in outcome data.
- Industry Sponsorship Bias: Approximately 70–80% of RCTs are industry-financed, which can create conflicts of interest and a bias toward publishing positive results [34].
Furthermore, the selection process in RCTs is rigorous. In some cases, such as recent trials on Alzheimer's disease, only about 15% of initially assessed patients may progress to the intention-to-treat analysis phase, raising questions about the applicability of results to the broader patient population seen in clinical practice [32].
The Scientist's Toolkit: Essential Reagents for RCTs
The successful execution of an RCT, whether traditional or pragmatic, relies on a suite of methodological and analytical "reagents."
Table 3: Key Research Reagent Solutions for RCTs
| Tool/Reagent | Category | Function in RCTs |
|---|---|---|
| Computerized Randomization Sequence | Methodology | Generates an unpredictable allocation sequence, forming the foundation for unbiased group comparison [35]. |
| CONSORT Guidelines | Reporting | A set of evidence-based guidelines (Consolidated Standards of Reporting Trials) to improve the quality and transparency of RCT reporting [32]. |
| Stratification Variables | Methodology | Variables (e.g., study site, disease severity) used during randomization to ensure balance between groups for known prognostic factors [35]. |
| Blinded Outcome Assessment | Methodology | Using independent assessors who are unaware of treatment allocation to measure outcomes, thereby reducing detection bias [35]. |
| Intention-to-Treat (ITT) Dataset | Data Analysis | A dataset where participants are analyzed in their originally assigned groups, preserving the benefits of randomization [36]. |
| Fragility Index (FI) | Statistical Analysis | A metric to assess the robustness of a statistically significant result, particularly useful for small trials with binary outcomes [33]. |
| Mixed Methods Integration | Analysis | Formal techniques (e.g., joint displays) for integrating quantitative trial data with qualitative data to explain variation in outcomes or understand implementation barriers [37]. |
The future of RCTs in pharmaceutical CER lies in the continued development and adoption of pragmatic methodologies. International collaborative networks, such as the PRIME-9 initiative across nine countries, are strengthening the pRCT concept by enabling the recruitment of larger, more diverse patient populations, sharing knowledge and resources, and overcoming ethical and regulatory barriers [34]. Furthermore, the integration of mixed methods—combining quantitative RCT data with qualitative research—holds great promise for generating deeper insights into why interventions work (or fail), for whom, and under what circumstances [37].
In conclusion, while the RCT remains the undisputed gold standard for establishing therapeutic efficacy, its evolution into more pragmatic and patient-centered designs is critical for answering the pressing questions of comparative effectiveness in real-world healthcare systems. For researchers and drug development professionals, mastering both the core principles of the traditional RCT and the adaptive strategies of the pRCT is essential for generating evidence that is not only scientifically rigorous but also meaningful for clinical practice and health policy.
In the evolving landscape of pharmaceutical research, Comparative Effectiveness Research (CER) has emerged as a crucial methodology for evaluating healthcare interventions. CER systematically evaluates and compares the benefits and harms of alternative healthcare interventions to inform real-world clinical and policy decisions [38]. Within this context, observational studies provide an indispensable framework for generating evidence about the effects of treatments, diagnostics, and prevention strategies as they are actually deployed in routine clinical practice.
Observational studies leveraging existing real-world data sources offer distinct advantages when randomized controlled trials (RCTs) are impractical, unethical, or insufficient for assessing long-term outcomes [39]. These studies allow for evaluations of interventions in real-world settings with large and representative populations, providing an important complement to RCTs [39]. They permit the study of clinical outcomes over periods longer than typically feasible in clinical trials, enabling observation of long-term impacts and unintended adverse events [39].
Table 1: Key Characteristics of Observational Studies in CER
| Characteristic | Description | Significance in Pharmaceutical Research |
|---|---|---|
| Data Source | Routine clinical care data, electronic health records, claims data, registries | Provides real-world evidence of drug performance in diverse populations |
| Intervention Comparison | Existing interventions representing current decisional dilemmas | Answers practical questions about which drug works best for specific patient subgroups |
| Time Horizon | Longer-term follow-up (often >5 years) | Captures long-term drug safety and effectiveness |
| Population Diversity | Broad, representative samples including elderly, comorbid patients | Enhances generalizability to real-world patient populations |
| Methodological Approach | State-of-the-art causal inference methods | Addresses confounding and selection bias inherent in non-randomized data |
Methodological Framework for Observational CER
Core Design Principles
Well-designed observational CER studies must articulate a clear comparative effectiveness question and leverage established data sources ready for patient-centered analysis [39]. The STROBE guidelines (Strengthening the Reporting of Observational Studies in Epidemiology) provide widely recognized standards for transparent reporting, though they focus primarily on completed studies rather than prespecifying analytical approaches [40].
Studies are expected to compare existing interventions that represent a current decisional dilemma and have robust evidence of efficacy or are currently in widespread use [39]. These may include clinical interventions (medications, diagnostic tests, procedures) and delivery system interventions (workforce technologies, healthcare service delivery designs) [39].
Statistical Analysis Plan for Observational Studies
A rigorous Statistical Analysis Plan (SAP) is fundamental to reducing questionable research practices and enhancing reproducibility in observational CER [40]. The SAP should be developed during initial research planning, ideally concurrently with the study protocol, and finalized before accessing or analyzing data [40].
Table 2: Essential Components of a Statistical Analysis Plan for Observational CER
| SAP Component | Description | Application in Pharmaceutical CER |
|---|---|---|
| Administrative Information | Study title, roles, responsibilities, version control | Ensures accountability and documentation |
| Background and Rationale | Context for the study, scientific justification | Explains the clinical dilemma and evidence gaps |
| Aims, Objectives, and Hypotheses | Clear research questions using PICO/PEO frameworks | Prevents HARKing (hypothesizing after results are known) |
| Study Methods | Data sources, inclusion/exclusion criteria, variable definitions | Ensures transparent patient selection and characterization |
| Statistical Analysis | Analytical approaches, confounding control, sensitivity analyses | Prespecifies causal inference methods to minimize bias |
The SAP template for observational studies promotes quality and rigor by prespecifying key aspects of the analysis, including study objectives, measures and variables, and analytical methods [40]. This approach helps reduce ad hoc analytic modifications and demonstrates avoidance of questionable research practices such as p-hacking [40].
Data Management and Presentation Standards
Variable Classification and Handling
Understanding data types is essential for proper analytical approach selection in observational studies. Variables are broadly classified as categorical (qualitative) or numerical (quantitative) [41]. Categorical variables include:
- Dichotomous variables: Two categories (e.g., sex, presence of skin cancer)
- Ordinal variables: Three or more categories with inherent order (e.g., Fitzpatrick skin classification)
- Nominal variables: Three or more categories without ordering (e.g., blood types) [41]
Numerical variables include:
- Discrete variables: Certain numerical values only (e.g., age in complete years)
- Continuous variables: Measured on a continuous scale (e.g., blood pressure, height) [41]
Variables measured on numerical scales are richer in information and should be preferred for statistical analyses, though they may be transformed into categorical variables for specific interpretive purposes [41].
Effective Data Presentation
Tables and graphs should be self-explanatory, understandable without requiring reference to the main text [41]. For categorical variables, frequency distributions should present both absolute counts and relative frequencies (percentages) [41].
Table 3: Standards for Data Presentation in Observational CER
| Element | Presentation Standard | Example |
|---|---|---|
| Categorical Variables | Absolute frequency (n) + Relative frequency (%) | 559 (23.16%) [41] |
| Numerical Variables | Appropriate summary statistics + distribution visualization | Mean ± SD or median (IQR) |
| Continuous Variables | Categorization with equal intervals when appropriate | Height categories: 1.55-1.61m, 1.61-1.67m, etc. [41] |
| Cumulative Frequencies | For ordered categorical or discrete numerical variables | "50.6% of subjects have up to 8 years of education" [41] |
Technical Implementation and Visualization Standards
Research Reagent Solutions for Observational CER
Table 4: Essential Methodological Tools for Observational CER
| Research Tool | Function | Application Context |
|---|---|---|
| Causal Inference Methods | Address confounding and selection bias | Comparative safety and effectiveness studies |
| Large-Scale Data Networks | Provide diverse, representative patient data | PCORnet, claims databases, EHR systems [39] |
| Statistical Software Platforms | Implement complex analytical models | R, Python, SAS for propensity score analysis |
| Data Linkage Systems | Integrate multiple data sources | Connecting pharmacy claims with clinical registries |
| SAP Templates | Pre-specify analytical approaches to reduce bias | Standardized protocols for observational studies [40] |
Analytical Workflow Visualization
The following diagram illustrates the core workflow for conducting observational studies in pharmaceutical CER:
Observational CER Workflow
Data Source Evaluation Framework
Data Source Assessment
Advancing Pharmaceutical Research Through Observational CER
Observational studies leveraging real-world data represent a powerful approach for generating evidence on pharmaceutical effectiveness in diverse patient populations. By applying rigorous methodological standards, including comprehensive statistical analysis plans, appropriate causal inference methods, and transparent reporting practices, researchers can provide trustworthy evidence for healthcare decision-making.
The growing emphasis on patient-centered outcomes and real-world evidence in regulatory and coverage decisions underscores the critical importance of well-designed observational CER. These studies complement RCTs by addressing questions about long-term effectiveness, safety in broader populations, and comparative performance in routine practice settings. Through continued methodological refinement and transparent conduct, observational studies will remain an essential component of the evidence generation ecosystem in pharmaceutical research.
In the realm of pharmaceuticals research, comparative effectiveness research (CER) serves a critical function by generating evidence to compare the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor clinical conditions [1]. The Institute of Medicine defines CER specifically to "assist consumers, clinicians, purchasers, and policy makers to make informed decisions that will improve health care at both the individual and population levels" [20]. Within this framework, systematic reviews and meta-analyses represent fundamental methodologies for evidence synthesis, providing structured, transparent, and reproducible approaches to summarizing existing research evidence. These formal synthesis methods enable researchers to determine which pharmaceutical interventions work best, for which patients, and under what circumstances—the core questions of CER [1].
The distinction between systematic reviews and meta-analyses is important conceptually, though the terms are often used together. A systematic review is a comprehensive, critical assessment and evaluation of all research studies that address a particular clinical issue using an organized method of locating, assembling, and evaluating a body of literature according to predetermined criteria [1]. A meta-analysis extends this process by applying statistical methods to quantitatively pool data from multiple studies, resulting in more precise effect estimates than individual studies can provide [42]. Together, these methodologies form the evidentiary foundation for informed decision-making in pharmaceutical development, reimbursement, and clinical practice.
Methodological Framework for Systematic Reviews
Foundational Principles and Reporting Standards
The conduct of high-quality systematic reviews rests upon several foundational principles: completeness (seeking to identify all relevant evidence), transparency (documenting all methods and decisions), rigor (applying methodological standards consistently), and reproducibility (enabling others to replicate the process). To standardize reporting, the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guideline provides an evidence-based minimum set of items for reporting systematic reviews [43]. The PRISMA 2020 statement, along with its various extensions, offers detailed guidance and examples for completely reporting why a review was done, what methods were used, and what results were found [44]. Adherence to these standards is particularly crucial in pharmaceutical CER, where conclusions may influence treatment guidelines and regulatory decisions.
The PRISMA framework encompasses several specialized extensions tailored to different review types, including PRISMA-P for protocols, PRISMA-NMA for network meta-analyses, PRISMA-DTA for diagnostic test accuracy studies, and PRISMA-ScR for scoping reviews [44]. This comprehensive guidance ensures that systematic reviews of pharmaceuticals address the unique methodological considerations inherent in comparing interventions across different patient populations and study designs.
The Systematic Review Workflow
The process of conducting a systematic review follows a structured sequence of stages, each with specific methodological requirements. The diagram below illustrates this workflow:
Figure 1: Systematic Review Workflow
Protocol Development
The initial stage involves developing a detailed review protocol that specifies the research question, inclusion and exclusion criteria, search strategy, and planned methods for analysis. The protocol should be registered in a publicly accessible repository to enhance transparency and reduce duplication of effort. The PRISMA-P extension provides specific guidance for protocol development [44].
Systematic Search
A comprehensive search strategy is developed to identify all potentially relevant studies. This typically involves searching multiple electronic databases (e.g., MEDLINE, Embase, Cochrane Central), clinical trial registries, and grey literature sources. The search strategy must balance sensitivity (retrieving all relevant studies) with specificity (excluding irrelevant studies) and should be documented with sufficient detail to permit replication.
Study Screening
Using predetermined eligibility criteria, identified records undergo a multistage screening process—typically title/abstract screening followed by full-text review. This process should involve at least two independent reviewers, with procedures for resolving disagreements [45].
Quality Appraisal
Included studies are critically appraised for methodological quality and risk of bias using established tools appropriate to the study design (e.g., Cochrane Risk of Bias tool for randomized trials, Newcastle-Ottawa Scale for observational studies). Quality assessment informs both the interpretation of results and, when appropriate, sensitivity analyses.
Data Extraction
Structured data extraction forms are used to collect relevant information from each included study. As noted in guidance from Ohio University, "A data extraction form is essentially a template, tailored to fit the needs of your review, that you will fill out for each included study" [46]. Standard extraction categories include study identification features, methods, participant characteristics, interventions, outcomes, and results [46].
Data Extraction and Management in Pharmaceutical CER
Designing Data Extraction Forms
The data extraction process requires careful planning and pilot testing to ensure consistency and completeness. Extraction forms should be tailored to the specific review question while capturing essential information about pharmaceutical interventions and their comparative effects. Key elements to extract include:
- Study identification: Author, year, citation, funding sources
- Methodology: Design (RCT, observational, etc.), duration, setting, country
- Participants: Sample size, demographic characteristics, diagnostic criteria, comorbidities
- Interventions: Drug name, dosage, regimen, administration route, comparators
- Outcomes: Primary and secondary endpoints, measurement timing, measurement instruments
- Results: Effect estimates, measures of variability, statistical methods [46]
At least two reviewers should extract data independently, with a process for resolving discrepancies through consensus or third-party adjudication [45]. Pilot testing the extraction form on a small sample of studies (typically 2-5) allows for refinement before full-scale implementation.
Data Extraction Tools
Various tools can facilitate the data extraction process, including:
Table 1: Data Extraction Tools for Systematic Reviews
| Tool Type | Examples | Advantages | Considerations |
|---|---|---|---|
| Spreadsheets | Microsoft Excel, Google Sheets | Flexible, accessible, familiar interface | May become cumbersome with large numbers of studies |
| Systematic review software | Covidence, RevMan, SRDR+ | Designed specifically for systematic reviews, collaboration features | Learning curve, potential cost barriers |
| Survey platforms | Qualtrics, REDCap | Structured data collection, validation features | May require customization for systematic review needs [46] |
The choice of tool depends on factors such as review complexity, team size, collaboration needs, and available resources. For pharmaceutical CER specifically, tools that can handle complex intervention details and multiple outcome measures are particularly valuable.
Data Synthesis Methodologies
Qualitative Synthesis Approaches
When studies are too heterogeneous in design, populations, interventions, or outcomes to permit statistical pooling, a narrative synthesis approach is used. This involves describing findings across studies, identifying patterns and relationships, and exploring differences in results. Effective narrative synthesis goes beyond simply summarizing individual studies to provide integrated analysis of how and why interventions work differently across contexts—a particularly important consideration in CER, where understanding variation in treatment effects is central to the research question [20].
Structured approaches to narrative synthesis include organizing studies by key characteristics (e.g., study design, patient population, intervention type), tabulating results to facilitate comparison, and using textual descriptions to explain similarities and differences in findings. For pharmaceutical CER, this might involve comparing results across different drug classes, patient subgroups, or treatment settings.
Quantitative Synthesis (Meta-Analysis)
When studies are sufficiently similar in design, population, intervention, and outcomes, meta-analysis provides a statistical method for combining results across studies to produce an overall quantitative estimate of effect. The decision to proceed with meta-analysis depends on assessments of clinical, methodological, and statistical heterogeneity [42].
Assessing Heterogeneity
Clinical heterogeneity refers to differences in patient populations, interventions, comparators, or outcomes across studies. Methodological heterogeneity involves differences in study design or risk of bias. Statistical heterogeneity reflects the degree of variation in effect estimates beyond what would be expected by chance alone, typically assessed using the I² statistic, which quantifies the percentage of total variation across studies due to heterogeneity rather than chance [42]. Conventional thresholds interpret I² values of 25%, 50%, and 75% as indicating low, moderate, and high heterogeneity, respectively.
Statistical Models for Meta-Analysis
The choice between fixed-effect and random-effects models depends on the nature of the included studies and the degree of heterogeneity:
Table 2: Meta-Analysis Models Based on Heterogeneity
| Heterogeneity Level | I² Value | Appropriate Model | Interpretation |
|---|---|---|---|
| Low heterogeneity | < 25% | Fixed-effect model | Assumes all studies are estimating an identical intervention effect |
| Moderate heterogeneity | 25% - 70% | Random-effects model | Assumes intervention effects follow a distribution across studies |
| Considerable heterogeneity | ≥ 70% | Narrative synthesis or subgroup analysis | Substantial variation suggests combining may be inappropriate [42] |
For dichotomous outcomes (e.g., mortality, response rates), relative risks or odds ratios are typically calculated. For continuous outcomes (e.g., blood pressure, quality of life scores), mean differences or standardized mean differences are used when different measurement scales are employed [42]. Meta-analyses are typically conducted using specialized software such as Cochrane Review Manager (RevMan), R packages like metafor, or Stata modules.
Advanced Meta-Analysis Techniques
Pharmaceutical CER often employs advanced meta-analytic methods to address complex evidence networks:
- Network meta-analysis: Allows simultaneous comparison of multiple interventions, including those not directly compared in head-to-head trials
- Meta-regression: Explores whether study characteristics (e.g., dose, patient age, study quality) explain heterogeneity in treatment effects
- Individual patient data (IPD) meta-analysis: Uses raw data from each participant in included studies, permitting more sophisticated subgroup analyses and standardized outcome definitions
These advanced techniques are particularly valuable for informing drug development and positioning decisions by providing comparative effectiveness evidence across the therapeutic landscape.
Comparative Effectiveness of Research Methods in Pharmaceuticals
Integrating Different Study Designs in CER
A distinctive feature of pharmaceutical CER is its consideration of evidence from diverse study designs, each with complementary strengths and limitations. The choice of method involves "the relative weight placed on concerns about selection bias and generalizability, as well as pragmatic concerns related to data availability and timing" [20].
Table 3: Comparison of Research Methods in Pharmaceutical CER
| Method | Key Features | Strengths | Limitations | Role in Pharmaceutical CER |
|---|---|---|---|---|
| Randomized Controlled Trials (RCTs) | Random assignment to interventions; controlled conditions | High internal validity; minimizes selection bias | Often restrictive enrollment; may lack generalizability; expensive and time-consuming | Gold standard for establishing efficacy; adaptive and pragmatic designs increase relevance [20] |
| Observational Studies | Natural variation in treatment patterns; real-world settings | Generalizability to clinical practice; efficient for large populations; examines subgroup differences | Susceptible to confounding and selection bias; limited for new interventions | Assesses effectiveness in real-world populations; examines long-term outcomes and rare adverse events [20] [47] |
| Systematic Reviews | Structured synthesis of existing evidence | Comprehensive summary of evidence; identifies consistency/inconsistency across studies | Dependent on quality and quantity of primary studies | Foundational for evidence-based decisions; identifies evidence gaps [1] |
| Meta-Analyses | Statistical pooling of results from multiple studies | Increased statistical power; more precise effect estimates | Potential for combining clinically heterogeneous studies | Provides quantitative summary of comparative effects; explores sources of heterogeneity [42] |
Concordance Between RCTs and Observational Studies
A critical methodological question in pharmaceutical CER concerns the concordance of treatment effects estimated by RCTs and observational studies. A 2021 systematic assessment of 30 systematic reviews across 7 therapeutic areas analyzed 74 pairs of pooled relative effect estimates from RCTs and observational studies [47]. The findings revealed:
- No statistically significant difference in relative effect estimates between RCTs and observational studies in 79.7% of comparisons
- Extreme differences (ratio < 0.7 or > 1.43) in 43.2% of pairs
- Statistically significant differences with estimates pointing in opposite directions in 17.6% of pairs [47]
These results suggest that while the majority of observational studies produce estimates similar to RCTs, substantial differences occur in a meaningful minority of cases. The sources of this variation—whether due to differences in patient populations, biases in observational study design, or analytical approaches—require careful consideration when interpreting evidence from different study designs [47].
Quality Assessment and Evidence Grading
Assessing Risk of Bias in Individual Studies
Critical appraisal of included studies is essential for interpreting results appropriately. Domain-based tools such as the Cochrane Risk of Bias tool for randomized trials assess potential biases across several dimensions: selection bias, performance bias, detection bias, attrition bias, and reporting bias. For observational studies, tools like the Newcastle-Ottawa Scale evaluate selection of participants, comparability of groups, and assessment of outcomes.
The GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach provides a systematic framework for rating the quality of evidence across studies for specific outcomes [42]. In the GRADE system:
- High quality: Further research is very unlikely to change confidence in the effect estimate
- Moderate quality: Further research is likely to have an important impact on confidence in the effect estimate
- Low quality: Further research is very likely to have an important impact on confidence in the effect estimate
- Very low quality: Any effect estimate is very uncertain [42]
GRADE assessments consider factors including risk of bias, inconsistency, indirectness, imprecision, and publication bias. For pharmaceutical CER, this structured approach to evaluating confidence in effect estimates is particularly valuable when making comparisons between interventions.
Special Considerations for Pharmaceutical Research
Data Synthesis Decision Pathway
The decision pathway for data synthesis in pharmaceutical systematic reviews involves multiple considerations, as illustrated below:
Figure 2: Data Synthesis Decision Pathway
Addressing Heterogeneity in Pharmaceutical Studies
In pharmaceutical systematic reviews, potential sources of heterogeneity requiring consideration include:
- Drug formulation and dosing: Differences in dosage forms, strengths, regimens
- Patient populations: Variations in disease severity, comorbidities, prior treatments
- Outcome definitions and measurement: Different endpoints, assessment methods, timing
- Study design features: Trial duration, blinding, comparator choices
When substantial heterogeneity is identified, approaches to address it include subgroup analysis, meta-regression, and sensitivity analysis. For CER, exploring sources of heterogeneity is particularly valuable as it may reveal which patient characteristics predict better response to specific pharmaceuticals.
The Scientist's Toolkit: Essential Materials for Systematic Reviews
Table 4: Essential Research Reagent Solutions for Systematic Reviews
| Tool Category | Specific Tools | Function | Application in Pharmaceutical CER |
|---|---|---|---|
| Literature Search | PubMed, Embase, Cochrane Central, ClinicalTrials.gov | Identify published and unpublished studies | Comprehensive identification of pharmaceutical trials and observational studies |
| Reference Management | EndNote, Zotero, Mendeley | Organize citations and PDFs; remove duplicates | Manage large volumes of references from multiple databases |
| Study Screening | Covidence, Rayyan, DistillerSR | Manage screening process; resolve conflicts | Efficient screening of large result sets using predetermined eligibility criteria |
| Data Extraction | Custom forms in Excel, SRDR+, Covidence | Extract structured data from included studies | Standardized extraction of drug, patient, outcome, and study design details |
| Quality Assessment | Cochrane RoB 2, Newcastle-Ottawa Scale, GRADEpro | Assess risk of bias and evidence quality | Evaluate methodological rigor of included pharmaceutical studies |
| Statistical Analysis | RevMan, R (metafor), Stata (metan) | Perform meta-analyses; create forest plots | Calculate pooled effect estimates for drug comparisons |
| Bias Assessment | Egger's test, funnel plots | Assess publication bias and small-study effects | Evaluate potential for biased evidence base in favor of new drugs |
Systematic reviews and meta-analyses provide indispensable methodologies for synthesizing evidence on pharmaceutical interventions within the framework of comparative effectiveness research. By employing rigorous, transparent, and systematic approaches to evidence synthesis, researchers can generate reliable answers to critical questions about which drugs work best, for which patients, and under what circumstances. The increasing sophistication of these methods—including network meta-analysis, individual patient data meta-analysis, and integration of real-world evidence—continues to enhance their value for drug development, regulatory decision-making, and clinical practice guidance. As pharmaceutical interventions grow more targeted and personalized, the role of systematic evidence synthesis in understanding heterogeneity of treatment effects will only increase in importance, ultimately supporting more effective and efficient patient care.
In pharmaceutical research, Comparative Effectiveness Research (CER) provides crucial evidence on the benefits and harms of available treatment strategies for real-world patients. A central challenge in CER is that treatment assignments are not random; they are influenced by patient characteristics, physician preferences, and clinical factors. These influences can introduce confounding bias, distorting the true relationship between a treatment and its outcomes. Propensity Scores (PS) and Instrumental Variables (IV) are two foundational methodological approaches developed to address this challenge, enabling researchers to draw more valid causal inferences from observational data. This technical guide examines both methodologies, their implementation, and their interplay within pharmaceutical CER, with detailed experimental protocols from recent case studies.
Propensity Score Methodology
Conceptual Foundation and Implementation
The propensity score is defined as the conditional probability of a patient receiving a specific treatment given their observed covariates [48]. In formal terms, for a patient with covariates ( X ), the propensity score is ( e(X) = Pr(T=1|X) ), where ( T=1 ) indicates treatment exposure. By balancing these observed covariates across treatment groups, PS aims to replicate the property of randomized experiments where treatment assignment is independent of patient baseline characteristics [48].
The implementation of propensity score analysis follows a structured five-step protocol [48]:
- Covariate Selection: Identify and specify the set of covariates to include. This set should encompass all known confounders—variables that predict both treatment assignment and the outcome. Crucially, covariates that are consequences of the treatment (mediators) should be excluded.
- PS Estimation: Typically using logistic regression, model treatment assignment as a function of the selected covariates. The predicted probabilities from this model constitute the propensity scores for all subjects.
- Matching: Create a matched cohort where treated and untreated subjects have similar or identical propensity scores. The nearest-neighbor within calipers method is common, where calipers of width 0.01 to 0.05 on the PS scale are used to ensure matches are sufficiently close.
- Balance Assessment: After matching, diagnostically check whether covariate distributions are balanced between treatment groups. Tools include visualizing the PS distribution overlap and calculating standardized differences, where a value below 10% is considered indicative of good balance.
- Effect Estimation: The final analysis estimates the treatment effect on the outcome using the matched cohort. For the average treatment effect on the treated (ATT), this can be calculated as ( \sum(y{exposed} - y{unexposed})/\text{number of matched pairs} ). Standard errors often require specialized methods like bootstrap resampling.
Case Study Protocol: Prostate Cancer Treatment Comparison
A recent CER study in metastatic castration-resistant prostate cancer (mCRPC) provides a robust example of PS application and a critical pitfall [49] [50].
- Objective: To compare the 36-month survival between patients initiating abiraterone acetate (n=2,442) versus docetaxel (n=1,213) using the French SNDS claims database.
- Design: A retrospective cohort study using 1:1 PS matching.
- Key Experimental Manipulation: The researchers computed PS using two different covariate assessment periods (CAPs):
- CAP 1: The 12 months leading up to and including the treatment initiation month [-12; 0 months].
- CAP 2: The 12 months leading up to, but excluding, the month immediately before treatment initiation [-12; -1 months].
- Findings: The choice of CAP profoundly influenced the study's efficiency and results, as summarized in Table 1.
Table 1: Impact of Covariate Assessment Period on PS Performance and Estimates
| Covariate Assessment Period (CAP) | Propensity Score (PS) Overlap (c-statistic) | Number of Matched Pairs | 36-Month Survival Difference (Abiraterone vs. Docetaxel) |
|---|---|---|---|
| [-12; 0 months] | 0.93 (Poor overlap) | 273 | Not meaningfully different |
| [-12; -1 months] | 0.81 (Improved overlap) | 765 | 38% vs. 28% (10 percentage point difference) |
The stark difference arose because the month immediately before treatment contained a procedure—implantable delivery systems—that was a near-perfect predictor of docetaxel use (59% vs. 1%) but unrelated to patient health status. This variable acted as a strong instrumental variable (IV), and its inclusion in the PS model led to biased effect estimation by creating non-overlapping subpopulations [49].
Instrumental Variable Methodology
Conceptual Foundation and Time-Varying Extensions
An instrumental variable is a source of exogenous variation that helps isolate the causal effect of a treatment on an outcome. For a variable ( Z ) to be a valid instrument, it must satisfy three core conditions [51]:
- Relevance: ( Z ) must be strongly associated with the treatment assignment ( T ).
- Exclusion Restriction: ( Z ) must affect the outcome ( Y ) only through its effect on ( T ) (i.e., no direct effect on ( Y )).
- Exchangeability: ( Z ) must be independent of unmeasured confounders of the ( T )-( Y ) relationship.
IV methods are particularly valuable for addressing unmeasured confounding, a limitation of PS approaches. Recent methodological advances have extended IV applications to time-varying treatments and confounders, which are common in pharmacoepidemiology [51].
A 2025 simulation study evaluated two IV approaches for time-varying settings [51]:
- IV-based G-estimation (IV-G): This method, from the class of g-methods, estimates a structural nested mean model to isolate the treatment effect. It was found to provide unbiased and precise estimates across various scenarios, including weak instruments and complex time-varying confounding.
- Inverse Probability Weighting (IPW): This approach re-weights subjects based on both their treatment and IV status over time. Its performance was reasonable with moderate or strong IVs but deteriorated with weak instruments.
Case Study Protocol: Rheumatoid Arthritis Biologics Comparison
- Objective: To estimate the effect of sustained Adalimumab use versus other biologics on quality-adjusted life years (QALYs) over 18 months in patients with Rheumatoid Arthritis [51].
- Data Source: US National Databank for Rheumatic Diseases (FORWARD), with 1,952 patients.
- Instrument: Time-varying physician preference, defined as the proportion of a physician's Adalimumab prescriptions in the preceding 6-month period. This exploits exogenous variation in prescribing habits.
- Method Application: Both IV-G and IPW were implemented. The IV-G approach involved modeling the treatment assignment at each time point as a function of the time-varying instrument and confounders, then using g-estimation to compute the causal effect of the sustained treatment strategy on the final QALY outcome.
- Finding: Both methods suggested no significant improvement in QALYs from Adalimumab compared to other biologics, but the IV-G estimation led to narrower confidence intervals, indicating higher precision [51].
The Scientist's Toolkit: Research Reagents and Materials
Table 2: Essential Components for Implementing PS and IV Analyses
| Component | Function in Analysis | Exemplar Instances from Case Studies |
|---|---|---|
| Longitudinal Healthcare Database | Provides real-world data on patient demographics, treatments, procedures, and outcomes over time. | French SNDS [49]; US FORWARD Databank [51] |
| Covariate Assessment Protocol | Defines the time window(s) for measuring confounders prior to treatment initiation. Critical for avoiding immortal time bias and IV inclusion in PS. | Pre-treatment CAPs of [-12; 0] vs. [-12; -1] months [49] |
| High-Dimensional Propensity Score (hdPS) | An algorithm that automates the selection of a large number of potential covariates from coded data (e.g., diagnosis/procedure codes) to improve confounding control. | Used in the mCRPC study to identify covariates from claims data [49]. |
| Instrumental Variable | A source of exogenous variation that mimics random assignment. Must be a strong predictor of treatment but not directly linked to the outcome. | Implantable delivery systems [49]; Time-varying physician preference [51] |
| Balance Diagnostics | Statistical and graphical tools to assess the success of PS matching in creating comparable groups. | Standardized differences; C-statistic; PS distribution histograms [49] [48] |
Integrated Workflows and Analytical Pathways
The following diagrams illustrate the core logical structures and analytical workflows for both PS and IV methods, highlighting key decision points and potential biases.
PS Analysis Workflow
IV Basic Causal Diagram
IV Exclusion Restriction Check
Propensity scores and instrumental variables are powerful but nuanced tools for causal inference in pharmaceutical comparative effectiveness research. PS methods are most effective for adjusting a wide array of measured confounders, but their validity can be compromised if the covariate set includes strong instruments, as demonstrated in the oncology case study. IV methods offer a robust approach to address unmeasured confounding, provided a valid and strong instrument can be identified. The emerging development of hybrid methods that combine PS weighting with dynamic borrowing techniques like the modified power prior further enriches the analytical arsenal, enabling the robust synthesis of trial and real-world data [52]. The choice between methods, or their combination, must be guided by a deep understanding of the clinical context, the underlying treatment assignment mechanism, and the specific sources of bias threatening the validity of the causal estimate.
Comparative Effectiveness Research (CER) is a foundational methodology in pharmaceuticals research, defined by the Institute of Medicine as "the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care" [29] [26] [1]. The central purpose of CER is to assist consumers, clinicians, purchasers, and policymakers in making informed decisions that improve health care at both individual and population levels [29]. Unlike traditional efficacy studies conducted for regulatory approval, which typically compare a treatment against placebo under ideal controlled conditions, CER focuses on comparing two or more active interventions in real-world settings to determine "which treatment works best, for whom, and under what circumstances" [26].
CER has gained prominence due to several limitations of the traditional clinical research paradigm. Explanatory randomized controlled trials (RCTs), while maintaining high internal validity through stringent inclusion criteria and controlled conditions, often prove difficult to implement in real-world practice [29]. These trials are frequently conducted with carefully selected patient populations that exclude older, sicker patients and those with comorbidities, potentially limiting the generalizability of results to the broader patient population seen in routine clinical practice [29]. Furthermore, the high costs and inefficiencies of traditional clinical trials have increased the economic burden on healthcare systems without always providing the comparative information needed by healthcare providers and patients [29]. CER addresses these limitations by generating evidence relevant to real-life clinical decision-making, ultimately aiming to involve both treating physicians and patients collaboratively in treatment decisions [29].
Core Methodologies in CER
The conduct of CER relies on multiple methodological approaches, each with distinct strengths and applications across the drug development lifecycle. The two primary categories of CER methodologies are experimental methods and observational studies, complemented by various evidence synthesis techniques [29].
Experimental Methods: Pragmatic Randomized Controlled Trials
Randomized Controlled Trials (RCTs) represent the benchmark design for clinical research and can be adapted for CER as pragmatic trials with modifications to their conduct and analysis [29]. While conventional explanatory RCTs are designed to determine whether an intervention can work under ideal conditions, pragmatic RCTs ask whether an intervention does work in routine clinical practice [29]. Key adaptations for pragmatic trials include:
- Broader Inclusion Criteria: Fewer exclusion criteria to enroll more representative patient populations [29]
- Patient-Centered Outcomes: Focus on outcomes that matter to patients in real-world settings rather than surrogate endpoints [29]
- Routine Care Follow-up: Patients may be passively followed through hospital registries and routine care mechanisms rather than intensive scheduled visits [29]
- Head-to-Head Comparisons: Direct comparison of active interventions rather than placebo-controlled designs [29]
- Novel Statistical Approaches: Incorporation of Bayesian and analytical adaptive methods to address limitations related to time, sample size, and cost [29]
Observational Studies
Observational methods are increasingly important in CER due to their applicability in routine clinical practice settings [29] [1]. These studies offer several advantages for comparative effectiveness questions:
- Heterogeneous Patient Populations: Involvement of diverse populations more representative of real-world patients [29]
- Large Sample Sizes: Ability to study large numbers of patients, facilitating research on rare diseases or outcomes [1]
- Real-World Setting: High external validity through evaluation in normal clinical practice environments [29]
- Cost Efficiency: Generally lower cost compared to RCTs [1]
- Multiple Comparisons: Capability to compare multiple regimens simultaneously [29]
Observational studies for CER can utilize various data sources, including clinical registries, electronic health records, administrative databases, and claims data [29] [53]. These studies may be prospective (following patients forward in time according to a study protocol) or retrospective (using existing data sources where both interventions and outcomes have already occurred) [1].
Table 1: Key Methodological Approaches in Comparative Effectiveness Research
| Method Type | Key Features | Primary Applications in CER | Key Limitations |
|---|---|---|---|
| Pragmatic RCTs [29] | Random assignment to interventions; conducted in routine practice settings; broader inclusion criteria | Head-to-head comparisons of active treatments; establishing effectiveness in real-world settings | Higher cost and time requirements compared to observational designs; may still have some selection bias |
| Prospective Observational Studies [1] | Participants not randomized; treatments chosen by patients/physicians; outcomes studied after protocol creation | Studying interventions where randomization is unethical or impractical; large-scale evidence generation | Potential for confounding by indication; requires robust statistical adjustment methods |
| Retrospective Observational Studies [1] | Uses existing data (claims, EHRs); both intervention and outcomes have occurred | Rapid, cost-effective evidence generation; studying rare outcomes or long-term effects | Data quality limitations; potential for unmeasured confounding; reliant on existing data elements |
| Systematic Reviews & Meta-Analysis [29] | Critical assessment and synthesis of existing research studies; may include quantitative pooling (meta-analysis) | Evidence synthesis; understanding consistency of effects across studies; informing clinical guidelines | Limited by quality and heterogeneity of primary studies; potential for publication bias |
Advanced Methodological Considerations
CER methodologies must address several challenges to ensure valid and reliable results. Confounding represents a particular concern in observational studies, where factors that influence both treatment assignment and outcomes can distort the true treatment effect [29]. Several statistical approaches have been developed to address these challenges:
Propensity Score Analysis: This method involves balancing factors influencing treatment choice by creating a single composite score that represents the probability of receiving a particular treatment given observed covariates [29] [1]. Patients in different treatment groups are then matched or stratified based on their propensity scores to create balanced comparison groups [1].
Instrumental Variable Methods: This approach uses a characteristic (instrument) that is associated with treatment allocation but not directly with the outcome of interest [29]. Potential instruments include geographical area, distance to healthcare facilities, or institutional characteristics [29]. This method helps address unmeasured confounding when valid instruments can be identified.
Risk Adjustment: An actuarial tool that identifies a risk score for a patient based on conditions identified via claims or medical records [1]. Risk adjustment can calibrate payments to health plans or identify similar types of patients for comparative purposes using either prospective (predicting future costs) or concurrent (explaining current costs) models [1].
"New-User" Design: This design for observational studies addresses selection bias and the "time-zero" aspect by excluding patients who have already been on the treatment being evaluated [29]. By comparing only new users of different interventions, this design reduces biases associated with treatment persistence and tolerance.
CER Application Across the Pharmaceutical Product Lifecycle
Comparative Effectiveness Research represents a continuous process that should be integrated throughout the entire pharmaceutical product lifecycle, from early clinical development through post-market surveillance. The systematic application of CER methodologies at each stage ensures that evidence generation addresses the needs of patients, clinicians, and policymakers for comparative information about treatment alternatives.
Clinical Development Phase
During clinical development, CER principles can be incorporated to establish comparative evidence foundations even before market approval:
Trial Design Considerations: Implement pragmatic elements in Phase III trials, including broader inclusion criteria, active comparator arms, and patient-centered outcome measures [29]. This approach helps bridge the "efficacy-effectiveness gap" between controlled trial results and real-world performance [53].
Stakeholder Engagement: Engage patients, caregivers, clinicians, and payers in endpoint selection and trial design to ensure research questions address outcomes that matter to decision-makers [54]. The Patient-Centered Outcomes Research Institute (PCORI) emphasizes that CER should be "patient-centered," focusing on outcomes that matter most to patients rather than solely on clinical metrics [54].
Comparative Evidence Generation: Design trials that directly compare new interventions against relevant alternatives rather than only placebo. This head-to-head evaluation produces evidence that helps patients and clinicians make decisions aligned with individual values, preferences, and life circumstances [54].
The following diagram illustrates the continuous integration of CER methodologies throughout the pharmaceutical product lifecycle:
Diagram: Integration of CER Methodologies Across Pharmaceutical Product Lifecycle
Post-Market Surveillance Phase
The post-market phase represents a critical period for CER generation, as real-world evidence accumulates from routine clinical use. The integration of post-market surveillance data into CER represents a continuous process that ensures ongoing evaluation of a product's comparative benefits and risks [55]. Key activities include:
Systematic Evidence Integration: Post-market surveillance regularly generates new data including safety reports, published literature, registry findings, and results from post-market clinical follow-up (PMCF) studies [55]. These data must be systematically evaluated for information that could change the assessment of the risk/benefit profile, clinical performance, and clinical safety of the product [55].
Active Safety Monitoring: Manufacturers should establish comprehensive post-market surveillance systems under their quality management systems based on a post-market surveillance plan [55]. Relevant data gathered through post-market surveillance, along with lessons learned from preventive and corrective actions, should be used to update technical documentation relating to risk assessment and clinical evaluation [55].
Benefit-Risk Assessment: A key objective of collecting post-market surveillance data is to ensure that the benefit-risk analysis remains relevant and accurate [55]. This includes documentation of:
- Nature, severity, number, and rate of harmful events
- Probability and duration of harmful events
- Totality of harmful events and their severity in aggregate [55]
Table 2: CER Data Sources and Applications in Post-Market Surveillance
| Data Source | CER Application | Methodological Considerations |
|---|---|---|
| Electronic Health Records (EHRs) [53] | Comparison of treatment effects in diverse patient populations; assessment of long-term outcomes | Data interoperability challenges; potential for unmeasured confounding; requires robust statistical adjustment |
| Disease Registries [29] | Evaluation of clinical outcomes in specific patient populations; comparison of multiple interventions | Selection bias in registry participation; data completeness variations; requires careful definition of time-zero |
| Claims Databases [1] | Assessment of resource utilization and costs; comparison of treatment patterns and outcomes | Limited clinical detail; potential for coding inaccuracies; informative censoring due to plan switching |
| Post-Market Clinical Follow-up (PMCF) [55] | Proactive collection of clinical data from routine use; updating of clinical evidence | Requirement for systematic methodology; integration with existing surveillance systems; sample size considerations |
| Patient-Reported Outcomes (PROs) [54] | Incorporation of patient perspectives on treatment benefits and harms; assessment of quality of life outcomes | Standardization of collection methods; response bias considerations; minimal important difference definitions |
Lifecycle Management Phase
Throughout the product lifecycle, CER informs strategic decisions regarding label expansions, clinical guidelines, and value demonstration:
Evidence Synthesis: Continuous updating of systematic reviews and meta-analyses to incorporate new comparative evidence as it emerges [29]. This includes both quantitative synthesis of clinical data and qualitative assessment of the overall body of evidence.
Guideline Development: CER findings increasingly form the basis of clinical practice guidelines as these results become part of the evidence base for recommended care pathways [29]. Guidelines based on robust comparative evidence help translate research findings into clinical practice.
Stakeholder Communication: Effective dissemination of CER findings to patients, clinicians, purchasers, and policymakers in formats that support informed decision-making [54]. PCORI emphasizes that research findings should be communicated in clear, understandable formats to ensure valuable information reaches those who can use it rather than remaining in academic journals [54].
The Scientist's Toolkit: Essential Reagents for CER
Implementing robust CER requires specific methodological tools and data resources. The following table details key "research reagent solutions" essential for conducting comparative effectiveness studies across the product lifecycle.
Table 3: Essential Research Reagents and Resources for Comparative Effectiveness Research
| Tool/Resource Category | Specific Examples | Function in CER |
|---|---|---|
| Data Resources [29] [1] [53] | Electronic Health Records (EHRs), Administrative Claims Databases, Disease Registries, Product Registries | Provide real-world data on treatment patterns, patient characteristics, and outcomes for observational CER studies |
| Statistical Methodologies [29] [1] | Propensity Score Analysis, Instrumental Variable Methods, Risk Adjustment Models, "New-User" Design | Address confounding and selection bias in non-randomized studies; improve validity of comparative effect estimates |
| Evidence Synthesis Frameworks [29] | Systematic Review Methodology, Meta-Analysis Techniques, Mixed Treatment Comparison Models | Synthesize evidence across multiple studies; provide comprehensive assessment of comparative benefits and harms |
| Stakeholder Engagement Platforms [56] [54] | Patient Advisory Panels, Clinical Investigator Networks, Stakeholder Feedback Mechanisms | Ensure research addresses questions relevant to patients and clinicians; improve applicability and uptake of findings |
| Outcome Measurement Tools [54] | Patient-Reported Outcome (PRO) Instruments, Quality of Life Measures, Functional Status Assessments | Capture outcomes that matter to patients beyond traditional clinical endpoints; support patient-centered CER |
Comparative Effectiveness Research represents a fundamental shift in how evidence is generated throughout the pharmaceutical product lifecycle. By focusing on direct comparison of alternative interventions in real-world settings, CER addresses critical questions about which treatments work best for specific patient populations and circumstances. The integration of CER methodologies—including pragmatic trials, observational studies, and evidence synthesis—across all stages from clinical development through post-market surveillance ensures that evidence generation keeps pace with the needs of patients, clinicians, and healthcare decision-makers.
The ongoing evolution of CER methodologies, particularly the refinement of approaches to address confounding in observational studies and the development of standardized frameworks for evidence synthesis, continues to strengthen the scientific rigor of comparative effectiveness assessments. Furthermore, the emphasis on stakeholder engagement throughout the research process helps ensure that CER addresses questions that are not only scientifically relevant but also personally meaningful to those facing healthcare decisions. As pharmaceutical research continues to advance, CER will play an increasingly vital role in translating therapeutic innovations into improved patient outcomes through informed clinical decision-making.
Navigating CER Challenges: Bias, Data Quality, and Evolving Methodologies
Mitigating Selection Bias and Confounding by Indication in Observational Studies
Comparative effectiveness research (CER) in pharmaceuticals aims to provide patients and physicians with evidence-based guidance on treatment decisions. A fundamental challenge in observational CER is ensuring validity by addressing two distinct phenomena: confounding bias and selection bias [57].
Confounding bias compromises internal validity, questioning whether an observed association truly reflects causation. It arises when factors that influence both treatment selection and the outcome are not adequately controlled [57]. In pharmaceutical research, this often manifests as confounding by indication, where the underlying disease severity or prognosis influences both the prescription of a specific drug and the subsequent outcome.
Selection bias compromises external validity, questioning whether results from a study sample are generalizable to the broader patient population of interest. It arises when the patients included in an analysis are not representative of the target population due to the study's selection mechanisms [57].
These biases are not only distinct in their consequences but also require different methodological approaches for mitigation. Erroneously using methods designed for one type of bias to address the other can lead to invalid results [57].
Formal Distinctions and Causal Structures
Understanding the distinct mechanisms of confounding and selection bias is a critical first step. The table below summarizes their core differences.
Table 1: Key Differences Between Confounding Bias and Selection Bias
| Aspect | Confounding Bias | Selection Bias |
|---|---|---|
| Core Problem | Unequal distribution of prognostic factors between treatment groups [57]. | Study sample is not representative of the target population [57]. |
| Validity Compromised | Internal Validity (causal inference) [57]. | External Validity (generalizability) [57]. |
| Primary Question | "Why did a patient receive one drug over another?" [57]. | "Why are some patients included in the analysis and others not?" [57]. |
| Typical Data Source | Arises from the treatment assignment mechanism [57]. | Arises from the selection mechanism into the study sample [57]. |
| Causal Graphical Rule | Paths between treatment and outcome are opened by common causes [58]. | Conditioning on a collider (often the selection variable itself) opens a spurious path [59]. |
Causal Diagrams Using Directed Acyclic Graphs (DAGs)
Directed Acyclic Graphs (DAGs) provide a powerful formalism for visualizing and identifying these biases. The following diagrams, created using DOT language, illustrate classic structures for confounding and selection bias. The color palette and contrast adhere to the specified guidelines to ensure clarity.
Confounding Bias DAG
The DAG above shows confounding bias. A common cause (L), such as disease severity, independently affects both the probability of receiving a specific treatment (A) and the outcome (Y). This creates a non-causal, back-door path (A ← L → Y) that must be blocked for unbiased effect estimation [58].
Selection Bias DAG
The DAG above illustrates selection bias. The selection variable (S), indicating inclusion in the study sample, is a common effect (collider) of both the treatment (A) and the outcome (Y). Conditioning on S (e.g., by analyzing only the selected sample) opens the non-causal path A → S ← Y, inducing a spurious association between treatment and outcome [59] [57].
Methodologies for Bias Mitigation
A Six-Step Process for Mitigating Confounding with DAGs
A structured, six-step process based on DAGs can guide researchers in selecting an appropriate set of covariates to minimize confounding bias [58].
- Step 1: Descendant Check. The covariates chosen to reduce bias should not be caused by the treatment (X). Adjusting for variables that are consequences of treatment can introduce bias [58].
- Step 2: Identify the Causal Effect. Define the total causal effect of interest (e.g., the effect of warming up on injury risk) [58].
- Step 3: List All Paths. List all paths between the treatment (X) and the outcome (Y) that are open (i.e., not blocked by colliders) [58].
- Step 4: Classify Paths. Classify each open path as causal (directed from X to Y) or non-causal (all others) [58].
- Step 5: Close Back-Door Paths. Identify a set of covariates that, when conditioned on, will block all non-causal paths without blocking any causal paths or opening new paths through colliders [58].
- Step 6: Check the Set. Verify that the set of covariates from Step 5 leaves no non-causal paths open and does not contain descendants of X [58].
Advanced Graphical Rules for Complex Selection Bias
While simple graphical rules exist, recent research highlights important cases they cannot address. These include situations where selection is a descendant of a collider of treatment and outcome, or where selection is affected by a mediator [60]. In such complex scenarios, more advanced methods are required.
Table 2: Advanced Methods for Addressing Selection Bias
| Method | Core Principle | Application Context |
|---|---|---|
| Inverse Probability Weighting (IPW) for Selection | Weights individuals in the selected sample by the inverse of their probability of being selected. This creates a pseudo-population that resembles the target population [60]. | Useful when external information on the covariates related to selection is available for the general population [60]. |
| g-Computation | A parametric method that involves modeling the outcome conditional on treatment and covariates, then averaging predictions over the target population's covariate distribution [60]. | Suitable for complex causal structures, including those where selection is affected by post-treatment variables like mediators [60]. |
| s-Recoverability Condition | A formal graphical condition stating that the sample distribution equals the target population distribution if the outcome (Y) and selection indicator (S) are d-separated by the treatment and covariates (X) [59]. | A diagnostic tool to check, based on the assumed DAG, whether selection bias can be theoretically corrected using the available data. |
The following workflow diagram integrates DAGs and these advanced methods into a coherent protocol for addressing bias.
Bias Mitigation Workflow
The Scientist's Toolkit: Essential Reagents for Causal Analysis
Table 3: Key Research Reagents and Tools for Causal Analysis
| Tool / Reagent | Function / Purpose |
|---|---|
| Causal DAG | A visual tool representing assumed causal relationships between variables; used to identify potential sources of confounding and selection bias [58] [57]. |
| d-separation | A graphical criterion used to read conditional independencies implied by a DAG; fundamental for determining minimally sufficient adjustment sets and detecting biases [59]. |
| Single-World Intervention Graphs (SWIGs) | An extension of DAGs that explicitly represents potential outcomes under intervention; useful for defining and identifying causal effects in complex settings, including mediation [60]. |
| Inverse Probability of Treatment Weighting (IPTW) | Creates a weighted pseudo-population where the distribution of confounders is balanced between treatment groups, mimicking randomization [60]. |
| Inverse Probability of Selection Weighting (IPSW) | Creates a weighted pseudo-population where the distribution of covariates in the sample resembles that of the target population, mitigating selection bias [60]. |
| g-computation Formula | A powerful estimation method that can handle complex causal structures, including time-varying confounding and mediation, by simulating potential outcomes [60]. |
| Software (e.g., dagitty, R packages) | dagitty is a user-friendly tool for drawing DAGs and deriving testable implications [59]. R packages like stdReg (for g-computation) and ipw (for weighting) implement these methods. |
Case Study: Applied Protocol for COVID-19 Surveillance
A study on estimating the COVID-19 cumulative infection rate in New York City demonstrates the practical utility of this approach in the presence of severe selection bias [59].
Experimental Protocol: Model-Based Bias Correction
- Primary Data Collection: Data was collected via surveys of Amazon Mechanical Turk (MTurk) crowd workers. The surveys queried subjects on household health status and demographic characteristics [59].
- Causal Model Construction: Researchers constructed a set of possible causal models (DAGs) of household infection and the survey selection mechanism. These models formally encoded different assumptions about how factors like age, geography, and symptoms influenced both infection risk and the likelihood of completing the survey [59].
- Model Ranking by Compatibility: Each causal model entailed specific statistical independencies (via d-separation) that could be tested against the collected survey data. The models were ranked based on their compatibility with the observed data [59].
- Effect Estimation: The most compatible causal model was used to estimate the cumulative infection rate for each survey period. This model-based approach corrected for the biased sample [59].
Results: Despite the crowdsourced sample being highly skewed toward younger individuals (a strong predictor of COVID-19 outcomes), the model-based approach recovered accurate estimates. The relative bias was only +3.8% and -1.9% from the reported cumulative infection rate for the two survey periods, respectively [59].
Mitigating selection bias and confounding is not merely a statistical exercise but a fundamental requirement for generating valid evidence from observational pharmaceutical research. A rigorous approach involves:
- Explicitly defining the study population and the selection mechanism [57].
- Using DAGs to formally articulate causal assumptions and identify potential biases [58] [59].
- Selecting appropriate statistical methods—such as g-computation or IPW—that are specifically designed to address the identified biases, particularly in complex scenarios that defy simple adjustments [60]. As CER continues to evolve, the adoption of these transparent and robust causal modeling methods will be critical for producing reliable evidence to guide drug development and clinical decision-making.
Overcoming Data Limitations in Claims and Electronic Health Records
Within pharmaceutical comparative effectiveness research (CER), the imperative to determine which treatments work best for which patients drives the extensive use of real-world data (RWD). Claims data and electronic health records (EHRs) constitute foundational sources of this RWD, yet their inherent limitations threaten the validity of research findings. This technical guide provides a structured framework for researchers to identify, assess, and mitigate these data challenges. We detail the specific characteristics, advantages, and pitfalls of both data sources, present methodologies for evaluating data quality, and propose advanced techniques for data linkage and bias adjustment. By adopting a proactive and rigorous approach to data handling, scientists can enhance the reliability of CER, thereby generating robust evidence to inform drug development and therapeutic decision-making.
Comparative effectiveness research (CER) is "the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care" [1]. In pharmaceuticals, CER moves beyond the idealized settings of randomized controlled trials (RCTs) to answer critical questions about how drugs perform in routine clinical practice across diverse patient populations [61]. While RCTs remain the gold standard for establishing efficacy, they are often costly, time-consuming, and lack generalizability to broader patient populations treated in real-world settings.
Observational studies using RWD have emerged as a vital strategy to produce meaningful comparisons of alternative treatment strategies more efficiently [61]. The two primary sources of RWD are:
- Claims Data: Generated when healthcare providers submit requests for payment to health plans, providing a record of interactions between patients, providers, and insurers [62].
- Electronic Health Records (EHRs): Digital documentation of patient health information generated throughout clinical care, including detailed clinical narratives, lab results, and vital signs [63] [64].
However, these data were originally designed for clinical care, billing, and administrative purposes—not research [65]. This fundamental distinction introduces significant limitations that researchers must overcome to ensure valid and reliable study outcomes.
A critical first step in designing robust CER is understanding the distinct strengths and limitations of claims and EHR data. The following tables provide a structured comparison to guide data source selection and study design.
Table 1: Core Characteristics and Strengths of Claims and EHR Data
| Characteristic | Claims Data | Electronic Health Records (EHRs) |
|---|---|---|
| Primary Purpose | Billing and reimbursement [62] | Clinical documentation and patient care [63] |
| Data Structure | Highly structured, standardized codes [62] | Mix of structured data and unstructured clinical notes [63] |
| Population Coverage | Excellent for insured populations, large sample sizes [66] | Limited to patients within a specific health system [65] |
| Longitudinality | Strong, tracks patient across providers and time [62] | Potentially fragmented across unconnected health systems [65] |
| Clinical Granularity | Limited to coded diagnoses and procedures [64] | Rich in clinical detail: lab results, vital signs, physician narratives [64] [67] |
| Cost Data | Comprehensive, includes reimbursed amounts [62] | Often limited or absent |
Table 2: Key Limitations and Data Quality Challenges
| Limitation | Claims Data | Electronic Health Records (EHRs) |
|---|---|---|
| Missing Data | Services not billed or uncovered; uninsured patients [66] | Care received outside the health system; incomplete documentation [63] [65] |
| Clinical Detail | Lacks lab results, disease severity, patient status [62] [66] | Available but often buried in unstructured notes [63] |
| Coding Accuracy | Diagnosis codes may reflect billing rather than clinical certainty [63] | Data entry errors; copy-paste inaccuracies; template-driven documentation [65] [67] |
| Representativeness | Excludes uninsured; biased by specific payer populations [62] | Over-represents sicker patients with more frequent encounters ("informed presence bias") [63] |
| Timeliness | Can lag weeks to months for closed claims [62] | More immediate, but requires extraction and processing [63] |
Methodological Framework for Data Quality Assessment
Experimental Protocol for EHR Data Validation
A retrospective review protocol can quantify the accuracy and completeness of EHR data elements against a verified source.
Aim: To assess the concordance of medication histories and medical problem lists between the EHR and a research-grade electronic data capture (EDC) system. Design: Retrospective chart review of subjects enrolled in clinical trials. Data Sources:
- EHR: The operational electronic health record system used in clinical care.
- EDC: The electronic data capture system used for the clinical trial, serving as the validated source of truth after Principal Investigator (PI) review and curation [68].
Methodology:
- Subject Selection: Recruit a cohort of patients from active clinical research studies.
- Data Extraction: For each subject, extract medication lists and medical problem lists from both the EHR and the EDC system at the time of trial screening.
- Blinded Review: A trained medical reviewer compares each data element (medication or medical problem) between the two sources.
- Categorization: Each element is classified into one of four categories:
- Concordant: Present and identical in both EHR and EDC.
- Incomplete: Not present in EHR, but present in EDC.
- Irrelevant: Present in EHR, but not present in EDC (e.g., duplicates, historical issues not relevant to current care).
- Inaccurate: Present in both but with discrepancies in dosage, timing, or diagnosis in the EHR [68].
Expected Outcome: A study employing this protocol found significant data discordance, with only 31.3% of medication records and 45.7% of medical problem records being fully concordant between the EHR and EDC [68]. This highlights the necessity of PI review and data curation before using EHR data for research.
Workflow for Claims and EHR Data Integration
Linking claims and EHR data leverages their complementary strengths, creating a more holistic dataset for CER. The following diagram illustrates a robust data integration workflow.
Diagram: Integrated Data Workflow for CER. This workflow demonstrates the process of combining claims and EHR data to create a more comprehensive dataset for analysis.
Advanced Techniques for Mitigating Biases and Errors
Addressing Information Bias
Information bias, including misclassification, arises when data inaccurately reflect the true patient status [63].
- For Unstructured EHR Data: Employ Natural Language Processing (NLP) and machine learning models to systematically extract and structure information from clinical narratives, such as physician notes and discharge summaries [63] [67]. This uncovers critical clinical context not available in claims data.
- For Both Data Sources: Implement quantitative data quality checks to assess missingness, implausible values (e.g., systolic blood pressure of 300 mmHg), and expected relationships between variables (e.g., diagnosis code and corresponding prescribed medication) [67].
- For Diagnosis Validation: Develop algorithmic phenotyping, where patients are classified as having a disease based on a combination of criteria (e.g., multiple diagnosis codes, specific medication prescriptions, and relevant lab results) rather than relying on a single ICD code [65].
Correcting for Selection Bias
Selection bias occurs when the study population does not represent the intended target population [63]. This is common in EHR-based studies where sicker patients or those with better access to care are over-represented.
- Propensity Score Methods: This is a powerful tool to address confounding by indication. The propensity score is the conditional probability of a patient receiving a specific treatment given their observed baseline characteristics [1]. Techniques include:
- Matching: Patients receiving Treatment A are matched to similar patients receiving Treatment B based on their propensity scores.
- Stratification: Dividing the study population into strata (e.g., quintiles) based on propensity scores and comparing outcomes within each stratum.
- Inverse Probability of Treatment Weighting (IPTW): Weighting patients by the inverse of their probability of receiving the treatment they actually received, creating a "pseudo-population" where treatment assignment is independent of measured confounders.
- Risk Adjustment: Use validated risk scores (e.g., based on comorbidities from claims or EHR data) to account for differences in baseline health status between comparison groups, ensuring fair comparisons of outcomes [1].
The following diagram illustrates the logical decision process for selecting appropriate bias mitigation strategies based on the data challenges present.
Diagram: Bias Mitigation Strategy Selection. A decision flow for choosing the most appropriate methodological technique to address specific data limitations.
The Researcher's Toolkit: Essential Reagents and Solutions
Table 3: Key Analytical Tools and Solutions for CER Data Challenges
| Tool / Solution | Category | Primary Function | Application Example |
|---|---|---|---|
| Natural Language Processing (NLP) | Software/Algorithm | Extracts structured information from unstructured clinical text [63]. | Identifying adverse drug reactions from physician progress notes not captured by ICD codes. |
| Propensity Score Software | Statistical Tool | Estimates and applies propensity scores for bias adjustment [1]. | Creating balanced cohorts to compare effectiveness of two diabetes drugs in observational data. |
| Common Data Models (CDMs) | Data Infrastructure | Standardizes data from disparate sources into a common format [67]. | Enabling scalable analytics across a distributed network of healthcare systems (e.g., PCORnet). |
| Data Quality Dashboards | Quality Assurance | Provides visualizations of data completeness, accuracy, and freshness over time [67]. | Auditing a new EHR data feed to ensure lab result values are within plausible ranges before study initiation. |
| Terminology Mappers | Vocabulary Tool | Maps local coding systems to standard terminologies (e.g., ICD-10 to SNOMED CT). | Harmonizing diagnosis codes from a claims database with problem list entries from an EHR for a unified patient cohort. |
Claims and EHR data are indispensable for advancing comparative effectiveness research in pharmaceuticals, offering real-world insights unattainable through clinical trials alone. However, their value is entirely dependent on a researcher's ability to navigate their profound limitations. Success requires a meticulous, multi-step approach: a deep understanding of each data source's genesis and quirks, rigorous validation and quality assessment protocols, and the application of sophisticated statistical and computational methods to mitigate bias and fill data gaps. By championing data quality, methodological transparency, and strategic data integration, researchers can transform flawed operational data into trustworthy evidence, ultimately guiding the development and use of safer, more effective pharmaceuticals for all patients.
The Role of Risk Adjustment and Propensity Scoring in Analytical Rigor
Comparative Effectiveness Research (CER) is defined by the Institute of Medicine as "the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care" [1]. In pharmaceutical research, CER plays a critical role in informing patients, clinicians, and policymakers about which treatments work best for which patients under specific circumstances [69]. Unlike efficacy studies conducted under ideal controlled conditions, CER aims to understand performance in real-world settings where patient heterogeneity, comorbidities, and varying treatment patterns introduce substantial confounding [18]. This confounding represents the fundamental analytical challenge in observational CER—systematic differences between patients receiving different treatments can create the illusion of causal relationships or obscure true treatment effects.
Risk adjustment and propensity scoring have emerged as essential methodological approaches to address this confounding in observational pharmaceutical studies. These techniques enable researchers to approximate the conditions of randomized controlled trials (RCTs) using observational data, thus balancing patient characteristics across treatment groups to permit more valid causal inference [70]. While RCTs remain the gold standard for establishing efficacy, they are often expensive, time-consuming, and may lack generalizability to real-world populations [18]. Furthermore, for many research questions, RCTs may be unethical, impractical, or underpowered for subgroup analyses, making well-conducted observational studies using proper adjustment methods increasingly valuable for pharmaceutical decision-making [69].
Foundational Concepts and Definitions
Core Methodologies for Addressing Confounding
Propensity Score (PS): The propensity score is defined as the probability of treatment assignment conditional on observed baseline covariates [70]. Formally, for a binary treatment T, observed covariates X, and propensity score e, this is represented as ei = Pr(Ti = 1|X_i). The propensity score is a balancing score, meaning that conditional on the propensity score, the distribution of observed baseline covariates is similar between treated and untreated subjects [70]. This property allows researchers to adjust for confounding by creating analysis strata where treated and control subjects have similar probabilities of receiving the treatment, thus mimicking random assignment with respect to the observed covariates.
Disease Risk Score (DRS): The disease risk score represents the predicted probability of the outcome conditional on confounders and being unexposed to the treatment of interest [71]. Formally, DRS can be expressed as P(Y = 1|T = 0,X), where Y denotes outcome, T denotes treatment, and X denotes confounders [71]. Unlike the propensity score, which models treatment assignment, the DRS models the outcome risk in the absence of treatment. This approach achieves "prognostic balance" by ensuring that the potential outcome under the reference condition is independent of covariates conditional on the DRS [72].
Risk Adjustment: Risk adjustment is an actuarial tool that identifies a risk score for a patient based on conditions identified via claims or medical records [1]. In CER, risk adjustment can be used to calibrate comparisons based on the relative health of patient populations. Risk adjustment models typically incorporate demographic information, diagnosis codes, medication use, and other clinical factors to create a comprehensive picture of patient health status at baseline, enabling fairer comparisons between treatment groups with different underlying risk profiles.
Conceptual Workflow for Addressing Confounding
The following diagram illustrates the fundamental logical relationship between confounding factors, methodological approaches, and causal inference in CER:
Comparative Analysis of Methodological Approaches
Performance Characteristics Under Different Scenarios
Table 1: Comparative Performance of Propensity Score vs. Disease Risk Score Methods
| Scenario Characteristic | Propensity Score (PS) Performance | Disease Risk Score (DRS) Performance | Key Evidence |
|---|---|---|---|
| Low Treatment Prevalence (<10%) | Higher estimation bias due to limited overlap between treatment groups | Lower bias, especially in nonlinear data structures [71] | Simulation studies show DRS outperforms PS when treatment prevalence drops below 0.1 [71] |
| Moderate-High Treatment Prevalence (10-50%) | Comparable or lower bias than DRS; better covariate balance [71] | Adequate performance but may be outperformed by PS in linear data scenarios [71] | PS demonstrated preferable performance in scenarios with treatment prevalence between 0.1-0.5 [71] |
| Data Structure | Performs well in linear or small sample data [71] | Superior in reducing bias under nonlinear and nonadditive data relationships [71] | DRS shows particular advantage when data contain interactions and nonlinear terms [71] |
| Sample Size | Effective across sample sizes but may struggle with rare treatments | Machine learning methods may extend applicability to large samples with complex data [71] | In small sample linear scenarios, PS maintains performance where DRS may not outperform [71] |
| Implementation Complexity | Requires careful balancing checks and may need additional matching techniques | Single score applicable across multiple exposure groups in complex scenarios [72] | DRS advantageous when comparing multiple exposure levels (e.g., vaccination status) [72] |
Practical Implementation Considerations
Propensity Score Applications: The primary strength of propensity scores lies in their ability to balance observed covariates across treatment groups, creating analysis datasets where treated and control subjects appear as if they were randomly assigned to treatment conditions [70]. This balancing property makes PS methods particularly valuable when researchers have comprehensive data on factors influencing treatment selection and wish to minimize confounding by those factors. The four main implementations of propensity scores in CER include: (1) matching on the propensity score, (2) stratification on the propensity score, (3) inverse probability of treatment weighting (IPTW) using the propensity score, and (4) covariate adjustment using the propensity score [70].
Disease Risk Score Applications: DRS methods excel in scenarios where the outcome is well-understood and can be accurately modeled based on baseline characteristics [71]. This approach is particularly advantageous when studying multiple exposure levels or complex treatment regimens, as a single DRS can be applied across all exposure groups rather than requiring separate models for each comparison [72]. For example, in COVID-19 vaccine effectiveness studies with multiple vaccination exposure categories, DRS methods significantly reduce computational complexity compared to propensity score approaches that require separate models for each dichotomous comparison [72].
Risk Adjustment Applications: Traditional risk adjustment serves as a foundational element in many observational studies, particularly those using healthcare claims data [1]. By quantifying patients' baseline health status, risk adjustment enables fairer comparisons between treatment groups that may differ systematically in their underlying prognosis. Risk adjustment is especially valuable when studying heterogeneous patient populations or when treatment selection is strongly influenced by disease severity or complexity.
Experimental Protocols and Implementation Guidelines
Propensity Score Estimation Protocol
Step 1: Model Specification
- Select covariates for inclusion based on theoretical relevance to treatment assignment and outcome
- Include all known confounders—variables that affect both treatment assignment and outcome
- Consider including instrumental variables that affect treatment but not outcome directly
- Exclude mediators that lie on the causal pathway between treatment and outcome
Step 2: Estimation Methods
- Logistic Regression: Traditional approach using maximum likelihood estimation
- Machine Learning Methods:
- LASSO (Least Absolute Shrinkage and Selection Operator): Performs well in linear settings with small sample sizes and common treatment prevalence [71]
- XgBoost: Outperforms other methods in nonlinear settings with large sample sizes and low treatment prevalence [71]
- Multilayer Perceptron (MLP): Captures complex nonlinear relationships but may require substantial data
Step 3: Balance Assessment
- Calculate absolute standardized mean differences (ASMD) for each covariate
- Target ASMD <0.1 after adjustment for adequate balance
- Use graphical diagnostics (e.g., love plots, distribution overlaps)
- Assess balance for higher-order terms and interactions if suspected
Step 4: Implementation for Effect Estimation
- Matching: 1:1 nearest neighbor matching without replacement with caliper of 0.2 standard deviations of the logit PS [71]
- Stratification: Divide into quintiles or other strata based on PS distribution
- Inverse Probability Weighting: Weight subjects by the inverse probability of receiving their actual treatment
- Covariate Adjustment: Include PS as a continuous covariate in outcome model
Disease Risk Score Estimation Protocol
Step 1: Model Specification
- Develop outcome prediction model using only control subjects (T=0)
- Include all prognostic factors for the outcome regardless of their relationship to treatment
- Consider nonlinear terms and interactions if clinically plausible
- Validate model performance using appropriate metrics (C-statistic, calibration)
Step 2: Score Application
- Apply the developed model to the entire study population
- Generate predicted probabilities for all subjects regardless of actual treatment
- Use these probabilities as the DRS for subsequent analyses
Step 3: Implementation for Effect Estimation
- Stratification: Create strata based on DRS distribution and analyze treatment effects within strata
- Covariate Adjustment: Include DRS as a continuous covariate in the outcome model
- Direct Adjustment: Model outcome as a function of treatment and DRS
Advanced Weighting Methods
Overlap Weighting Protocol: Overlap weighting represents an advanced approach that specifically targets the average treatment effect in the overlap population (ATO)—patients with clinical equipoise where treatment assignment is most uncertain [73]. This method produces bounded, stable weights and achieves exact mean covariate balance for patients with propensity scores near 0.5 [73].
Implementation Steps:
- Estimate propensity scores using preferred method
- Calculate weights as: wi = 1 - PSi for treated subjects and wi = PSi for control subjects
- Assess weight distribution and effective sample size
- Estimate treatment effects using weighted analyses
- Characterize the overlap population for appropriate interpretation
Table 2: Research Reagent Solutions for Confounding Adjustment
| Methodological Component | Essential Analytical Tools | Primary Function | Key Considerations |
|---|---|---|---|
| Data Preparation | Structured healthcare data (claims, EHR) | Provides baseline covariates, treatment assignments, and outcomes | Data quality issues, missing clinical variables, privacy concerns [1] |
| Statistical Software | R, Python, SAS, Stata | Implements estimation algorithms and balance diagnostics | Package selection affects method availability and ease of implementation |
| Propensity Score Estimation | Logistic regression, LASSO, XgBoost, MLP [71] | Models probability of treatment assignment | Machine learning methods may capture complex relationships but reduce interpretability |
| Balance Assessment | Standardized mean difference, variance ratios | Quantifies covariate balance between treatment groups | Should assess both first-order and higher-order terms for adequate balance |
| Effect Estimation | Regression models, weighting algorithms | Estimates treatment effects after confounding adjustment | Model specification should align with weighting/matching approach used |
Case Studies in Pharmaceutical Research
COVID-19 Treatment Comparisons
A 2025 simulation study investigated the performance of PS and DRS methods in scenarios with low treatment prevalence, motivated by early COVID-19 treatment patterns where emerging therapies had limited utilization [71]. The study examined 25 different scenarios varying in treatment prevalence (0.01-0.5), outcome risk, data complexity, and sample size. Findings demonstrated that DRS showed lower bias than PS when treatment prevalence dropped below 0.1, particularly in nonlinear data structures [71]. However, PS maintained comparable or better performance in scenarios with treatment prevalence between 0.1-0.5, regardless of outcome risk [71]. Machine learning methods for estimating both PS and DRS—particularly XgBoost and LASSO—outperformed traditional logistic regression in specific scenarios with complex data relationships [71].
Oncology Drug Effectiveness
A 2025 case study of pembrolizumab for advanced non-small cell lung cancer illustrates the practical challenges in real-world comparative effectiveness research [74]. This study highlighted how methodological decisions—including time period selection, biomarker adjustment, definition of therapeutic alternatives, and handling of treatment switching—substantially influenced survival estimates. Overall survival benefits of pembrolizumab therapies compared to alternatives varied from a non-significant difference to an improvement of 2.7 months depending on analytical choices [74]. The study utilized propensity score-based inverse probability weighting to adjust for confounding, demonstrating how these methods are deployed in complex oncology settings where randomization may not be feasible for all clinical questions.
Vaccine Effectiveness Studies
Research from the Virtual SARS-CoV-2, Influenza, and Other Respiratory Viruses Network (VISION) illustrates the application of DRS methods in complex multinomial exposure scenarios [72]. As COVID-19 vaccination schedules evolved to include multiple doses and booster timing considerations, researchers faced the challenge of comparing numerous exposure categories simultaneously. While propensity score methods would require separate models for each binary comparison, DRS approaches allowed researchers to calculate a single score applicable across all exposure groups [72]. Simulation studies demonstrated that while DRS-adjusted models performed adequately, multivariable models adjusting for covariates individually sometimes provided better performance in terms of coverage probability [72].
Analytical Workflow for Comparative Effectiveness Studies
The following diagram illustrates a comprehensive workflow for implementing confounding adjustment methods in pharmaceutical CER:
Discussion and Future Directions
The appropriate application of risk adjustment, propensity scoring, and disease risk scoring methods represents a critical component of methodological rigor in pharmaceutical comparative effectiveness research. Each approach offers distinct advantages and limitations, with performance highly dependent on specific study contexts including treatment prevalence, data structure, sample size, and research question [71]. The growing complexity of treatment regimens and the increasing importance of real-world evidence in regulatory and reimbursement decisions underscore the need for continued methodological refinement.
Future directions in this field include the development of more sophisticated machine learning approaches that can better capture complex relationships in high-dimensional data while maintaining interpretability [71]. Additionally, there is growing interest in methods that integrate both propensity-based and outcome-based approaches to leverage their complementary strengths. The emergence of novel weighting methods like overlap weighting highlights the importance of carefully defining the target population and estimand before selecting analytical methods [73]. As comparative effectiveness research continues to inform high-stakes decisions in pharmaceutical development and patient care, maintaining methodological rigor through appropriate confounding adjustment remains paramount.
Integrating Real-World Evidence (RWE) and Advanced Data Analytics
Comparative Effectiveness Research (CER) is defined as “the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat and monitor a clinical condition, or to improve the delivery of care” [69]. Its purpose is to assist consumers, clinicians, purchasers, and policy makers in making informed decisions that improve healthcare at both the individual and population level. CER plays a critical role in crafting clinical guidelines and reimbursement policies, providing essential information on how new drugs perform compared to existing treatments [69].
Real-World Evidence (RWE) is the clinical evidence regarding the usage and potential benefits or risks of a medical product derived from the analysis of Real-World Data (RWD) [75]. RWD encompasses data relating to patient health status and/or the delivery of healthcare routinely collected from a variety of sources, including electronic health records (EHRs), medical claims data, product or disease registries, and patient-generated data [75] [76]. Within the context of CER, RWE provides insights beyond those addressed by randomized controlled trials (RCTs) by demonstrating how therapeutic interventions perform in everyday clinical practice across diverse patient populations [77].
The integration of RWE into pharmaceutical research represents a paradigm shift, enabling a more nuanced understanding of a treatment's value throughout its lifecycle. While RCTs remain the gold standard for establishing efficacy under controlled conditions, they are often limited in their generalizability due to strict inclusion criteria and homogeneous patient populations [76]. RWE bridges this gap by providing clinically rich insights into what actually happens in routine practice, allowing researchers to assess comparative effectiveness across broader patient populations and over longer timeframes [69] [76].
Methodological Framework for RWE Generation
Defining the Research Question and Study Type
The foundation of any robust RWE study begins with a well-defined research question formulated within a specific conceptual framework. The research question should clearly specify the population, intervention, comparator, and outcomes (PICO) of interest [78]. A crucial early determination is whether the study is exploratory or a Hypothesis Evaluating Treatment Effectiveness (HETE) study [77].
- Exploratory Studies: Typically do not hypothesize a specific treatment effect or its magnitude. They serve as a first step to investigate possible treatment effectiveness and allow for process adjustments as investigators gain knowledge of the data.
- HETE Studies: Evaluate the presence or absence of a prespecified effect and/or its magnitude. These studies test a specific hypothesis in a specific population and require stricter procedural controls [77].
For HETE studies, researchers should publicly register their study protocol and analysis plan prior to conducting the analysis to enhance transparency and reduce concerns about "data dredging" or selective reporting [77].
Data Source Selection and Validation
Selecting appropriate data sources is critical for generating valid RWE. Different data sources offer complementary strengths, and often, multiple sources must be combined to create a comprehensive patient picture.
Table 1: Common Real-World Data Sources and Their Applications in CER
| Data Source | Primary Content | Strengths | Limitations | Common CER Applications |
|---|---|---|---|---|
| Electronic Health Records (EHRs) | Clinical data: patient demographics, comorbidities, treatment history, outcomes [76] | Clinically rich data, detailed clinical information | Variability in documentation quality, potential missing data | Comparative safety studies, treatment patterns, natural history studies |
| Medical Claims | Billing data: healthcare services utilization, prescribing patterns, costs [76] | Large population coverage, complete capture of billed services | Limited clinical detail, potential coding inaccuracies | Healthcare resource utilization, cost-effectiveness, treatment adherence |
| Disease Registries | Prospective, standardized data collection for specific diseases [76] | Disease-specific detailed data, systematically collected | Potential selection bias, may not be representative | Disease progression, long-term outcomes, comparative effectiveness |
| Patient-Reported Outcomes (PROs) | Data directly from patients: symptoms, quality of life, treatment experience [76] | Patient perspective, captures outcomes beyond clinical settings | Subject to recall bias, potential missing data | Patient-centered outcomes, quality of life comparisons, treatment satisfaction |
The process of transforming RWD into analyzable evidence requires several validation steps: defining which data elements can be collected from which RWD sources, establishing data capture arrangements, blending disparate data sources through probabilistic record matching algorithms, and validating supplemented data through editable electronic case report forms (eCRFs) [76].
Advanced Analytical Techniques for CER
Advanced analytics applied to RWD encompasses both explanatory modeling (focused on causal inference) and predictive modeling (focused on prediction accuracy), with the choice depending on the research question [79].
Table 2: Advanced Analytical Methods for RWE Generation
| Method Category | Primary Objective | Key Techniques | Typical CER Applications |
|---|---|---|---|
| Causal Inference Methods | Estimate treatment effects while accounting for confounding | Propensity score matching, inverse probability of treatment weighting, instrumental variables [79] | Head-to-head treatment comparisons, effectiveness in subpopulations |
| Machine Learning for Prediction | Identify patterns and predict outcomes | Ensemble methods (boosting, random forests), deep learning, natural language processing (NLP) [80] [79] | Patient stratification, disease progression modeling, adverse event prediction |
| Natural Language Processing (NLP) | Extract structured information from unstructured clinical notes | BERT embeddings, TF-IDF vectorization, named entity recognition [80] | Phenotype identification, comorbidity assessment, outcome ascertainment |
Machine learning approaches are particularly valuable for handling the complexity and high dimensionality of RWD. For example, NLP techniques like BERT embeddings can provide nuanced contextual understanding of complex medical texts, enabling researchers to extract valuable information from clinical notes at scale [80]. Similarly, ensemble methods can capture heterogeneous treatment effects across patient subgroups that might be missed by traditional statistical approaches [79].
Experimental Protocols and Workflows
Protocol for Retrospective Comparative Effectiveness Study
This protocol outlines a structured approach for conducting a retrospective cohort study using RWD to compare the effectiveness of two or more treatments.
1. Study Registration and Protocol Development
- Publicly register the study on a platform like ClinicalTrials.gov before initiating analysis
- Develop and post a detailed study protocol and statistical analysis plan (SAP)
- Clearly define the study as hypothesis-evaluating (HETE) [77]
2. Data Source Selection and Preparation
- Identify appropriate data sources (e.g., EHRs, claims, registries) based on the research question
- Assess data quality, completeness, and relevance for the target population
- Create a common data model or harmonize data structures across sources
- Implement data anonymization procedures where required [81]
3. Cohort Definition
- Apply explicit inclusion and exclusion criteria to define the study population
- Identify the exposure groups of interest (treatments being compared)
- Define the index date (start of follow-up) for each patient
- Ensure sufficient sample size through power calculations
4. Covariate and Outcome Definition
- Identify potential confounders and effect modifiers from available data
- Define primary and secondary outcomes using validated algorithms
- Address missing data through appropriate imputation methods
5. Analysis
- Implement propensity score methods or other causal inference approaches to balance covariates
- Estimate treatment effects using appropriate statistical models
- Conduct sensitivity analyses to assess robustness of findings
- Perform subgroup analyses if pre-specified [79]
Protocol for Hybrid RCT-RWE Study Design
This protocol combines elements of traditional randomized trials with RWD to enhance comparative effectiveness assessment.
1. Trial Design Phase
- Design a randomized controlled trial with pragmatic elements
- Define which outcomes will be collected through traditional methods versus RWD sources
- Establish linkages between trial data and RWD sources (EHRs, claims, registries)
- Obtain necessary consent and regulatory approvals for data linkage [81]
2. Data Collection Phase
- Collect trial-specific data per protocol
- Implement processes for regular extraction of RWD from linked sources
- Establish quality control procedures for both trial data and RWD
3. Data Integration and Harmonization
- Create an analytic dataset combining trial-collected data and RWD
- Resolve discrepancies between data sources through adjudication processes
- Apply common data models to ensure consistency
4. Analysis Phase
- Analyze trial outcomes using standard RCT methods
- Conduct supplementary analyses incorporating RWD elements
- Use RWD to assess long-term outcomes beyond the trial period
- Explore generalizability of findings to broader populations using RWD [69] [81]
The Novartis-Oxford collaboration exemplifies this approach, integrating clinical trial data from approximately 35,000 MS patients with imaging data and other RWD sources to identify disease phenotypes and predictors of progression [81].
Visualization of RWE Generation Workflow
The following diagram illustrates the end-to-end process for generating regulatory-grade real-world evidence:
RWE Generation Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Analytical Tools and Data Solutions for RWE Generation
| Tool Category | Specific Solutions | Function in RWE Generation | Application Examples |
|---|---|---|---|
| Data Cataloging | IQVIA Health Data Catalog (IHDC) [78] | Profiles 4,400+ health datasets using 250+ metadata descriptors to identify relevant data sources | Targeted searches for specific variables across multiple datasets |
| Common Data Models | OMOP, Sentinel Common Data Model [78] | Standardizes data structure and terminology across disparate sources to enable scalable analysis | Multi-database studies, reproducible analytics |
| NLP Platforms | BERT-based models, TF-IDF vectorization [80] | Extracts structured information from unstructured clinical notes for outcome and phenotype identification | Processing clinical notes to identify comorbidities or outcomes |
| Machine Learning Libraries | Scikit-learn, TensorFlow, PyTorch | Implements predictive modeling and causal inference methods for treatment effect estimation | Patient stratification, confounding control, outcome prediction |
| Visualization Tools | Tableau, R Shiny, Python Dash | Creates interactive dashboards to explore analytical results and communicate findings to stakeholders | Interactive treatment comparison displays for clinical teams |
| Study Registration Platforms | ClinicalTrials.gov, ENCePP [77] | Provides public registration of study protocols to enhance transparency and reduce bias | Registering HETE study designs before analysis |
Applications in Pharmaceutical Research and Development
Drug Development and Clinical Trial Optimization
RWE and advanced analytics are transforming drug development across the entire lifecycle:
Pre-trial Design: RWE informs study design by helping researchers identify potential patients and create appropriate inclusion/exclusion criteria [76]. For example, Novartis uses RWE to track patient responses to its drug Gilenya in multiple sclerosis trials, enabling rapid protocol adjustments based on real-time monitoring of MRIs and biomarkers [82].
Trial Recruitment: Advanced analytics can reduce recruitment times by identifying eligible patients through analysis of EHR data. AI-driven platforms have demonstrated potential to shorten development timelines from five years to 12-18 months while reducing costs by up to 40% [83].
External Control Arms: In cases where randomized control groups are not feasible, RWD can be used to create external control arms. For example, a study of ROS1+ non-small-cell lung cancer used electronic health record data from patients treated with crizotinib as a comparator for clinical trial data from patients treated with entrectinib [69].
Post-Marketing Surveillance and Comparative Safety
After drug approval, RWE plays a crucial role in ongoing safety monitoring and comparative effectiveness:
Pharmacovigilance: Machine learning algorithms enable continuous screening of real-world data for potential adverse events. The FDA's Sentinel System uses this approach to monitor drug performance in real-world environments, tracking patient outcomes and side effects in near real-time [82].
Benefit-Risk Assessment: RWE helps quantify the balance between therapeutic benefits and potential risks in diverse populations. For example, RWD was used to detect blood clots in a small percentage of patients receiving the Oxford/AstraZeneca COVID-19 vaccine, informing subsequent benefit-risk assessments by regulatory authorities [79].
Regulatory and HTA Submissions
Regulatory bodies and Health Technology Assessment (HTA) organizations are increasingly accepting RWE to support decision-making:
Label Expansions: RWE can support applications for new indications without requiring new clinical trials. The FDA's RWE Program specifically evaluates the use of RWD to support approval of new indications for already approved drugs [75].
HTA Submissions: RWE provides complementary evidence on comparative effectiveness in real-world populations, which is valuable for reimbursement decisions. HTA bodies use RWE to assess effectiveness in specific subpopulations and real-world clinical practice [69] [77].
Organizational Implementation Framework
Successfully integrating RWE and advanced analytics requires both technical capability and organizational adaptation. McKinsey estimates that over the next three to five years, an average top-20 pharma company could unlock more than $300 million annually by adopting advanced RWE analytics across its value chain [79].
Interdisciplinary Team Structure
Effective RWE generation requires collaboration across four distinct expert domains:
- Clinical Experts: Provide medical input on use case design and help interpret data patterns through the lens of clinical practice [79].
- Methods Experts: Ensure analytical rigor and statistical validity, bringing expertise in epidemiology, health outcomes, and biostatistics [79].
- Translators: Act as intermediaries between business stakeholders and technical teams, converting business requirements into analytical directives [79].
- Advanced Analytics Specialists: Build algorithms and data pipelines, with expertise in machine learning, statistics, and data engineering [79].
Bridging Analytical Cultures
Pharmaceutical companies must integrate two historically separate analytical cultures:
- Explanatory Modeling Culture: Focused on causal inference through methods like propensity scores, emphasizing statistical rigor and minimization of false discoveries [79].
- Predictive Modeling Culture: Focused on prediction accuracy using flexible models like ensemble methods, emphasizing performance on novel data [79].
The most successful organizations reason "back from impact" rather than "forward from methods," selecting approaches based on the specific evidentiary need rather than methodological preferences [79].
The integration of real-world evidence and advanced data analytics represents a transformative opportunity for comparative effectiveness research in pharmaceuticals. By leveraging diverse data sources and sophisticated analytical methods, researchers can generate evidence that complements traditional RCTs and provides insights into how treatments perform in real-world clinical practice.
The successful implementation of RWE programs requires careful attention to methodological rigor, transparent processes, and interdisciplinary collaboration. As regulatory and reimbursement bodies increasingly accept RWE, pharmaceutical companies that build robust RWE capabilities will be better positioned to demonstrate the value of their products and contribute to evidence-based healthcare decision-making.
The future of CER will undoubtedly involve greater integration of RWE throughout the drug development lifecycle, from early research through post-marketing surveillance. Continued advances in analytical methods, particularly in causal inference and machine learning, will further enhance the robustness and utility of RWE for informing treatment decisions and improving patient outcomes.
Comparative Effectiveness Research (CER) is a cornerstone of modern pharmaceutical research and health policy, defined as the conduct and synthesis of research that "identifies interventions most effective for specific patient groups" [84]. This evidence is crucial for informing the practices of healthcare providers and policymakers to make evidence-based resource allocation decisions [84]. In the pharmaceutical domain, CER provides essential insights into which drug therapies work best for which patients and under what conditions, enabling more precise and effective therapeutic interventions.
The emergence of artificial intelligence (AI) and machine learning (ML) represents a transformative force for CER methodologies. AI, particularly through sophisticated ML algorithms, is revolutionizing how researchers can analyze vast volumes of biological, chemical, and clinical data to generate more nuanced, rapid, and patient-centered evidence [85] [86]. This technological shift enables a fundamental move from traditional, linear research approaches to dynamic, predictive, and highly personalized evidence generation that can keep pace with the complex decision-making needs of modern pharmaceutical development and healthcare delivery.
The AI and ML Paradigm Shift in Pharmaceutical Research
Core AI/ML Concepts and Definitions
Artificial Intelligence in pharmaceutical research encompasses "technologies that simulate human intelligence to perform tasks such as learning, reasoning, and pattern recognition" [85]. Within this broad field, several specialized approaches have particular relevance for CER study design:
Machine Learning (ML): A subset of AI involving "algorithms with the ability to define their own rules based on input data without explicit programming" [85]. ML primarily operates through supervised methods (using labeled datasets to map inputs to known outputs), unsupervised methods (finding hidden structures in unlabeled data), and reinforcement learning (trial-and-error approach driven by decision-making within specific environments) [85].
Deep Learning (DL): A specialized subset of ML utilizing "artificial neural networks (ANN) inspired by the structure of the human brain" with layers of interconnected nodes capable of recognizing complex patterns in large datasets [85]. This approach has proven particularly valuable for molecular property prediction and clinical decision support.
Generative AI (GAI): Emerging AI capabilities that can design novel drug molecules from scratch, creating new possibilities for therapeutic intervention and comparison [87].
The Economic Imperative: Addressing the "$2 Billion Problem"
The traditional drug development pipeline faces a systemic crisis known as "Eroom's Law" - the paradoxical trend where the number of new drugs approved per billion dollars of R&D spending has been steadily decreasing despite revolutionary advances in technology [86]. This problem manifests in staggering metrics:
Table 1: The Economic Challenge of Traditional Drug Development
| Metric | Traditional Approach | AI-Enhanced Potential |
|---|---|---|
| Development Timeline | 10-15 years [86] | Significantly reduced [86] |
| Cost per New Drug | Exceeds $2.23 billion [86] | Substantial reduction possible [86] |
| Attrition Rate | 1 success per 20,000-30,000 compounds [86] | Improved success rates through better prediction [86] |
| Return on Investment | As low as 1.2% (2022) [86] | McKinsey estimates $110 billion annual value potential [86] |
AI and ML address this challenge by fundamentally rewiring the R&D engine, shifting from a process "reliant on serendipity, brute-force screening, and educated guesswork to one that is data-driven, predictive, and intelligent" [86]. This paradigm shift enables researchers to "slash years and billions of dollars from the development lifecycle" through more accurate prediction and reduced late-stage failures [86].
AI-Driven Transformations in CER Study Design
From Linear to Adaptive Study Architectures
Traditional comparative effectiveness studies typically follow a rigid, sequential pathway where "each stage must be largely completed before the next begins" [86]. This linear structure creates a system where "the cost of failure is maximized at the latest stages" and "information silos" prevent insights from late-stage trials from optimizing earlier research phases [86].
AI and ML enable a fundamental transformation to adaptive, integrated study designs that continuously learn from accumulating data. The following workflow illustrates this transformative approach:
Enhanced Patient Stratification and Subgroup Identification
ML algorithms excel at identifying complex, non-obvious patterns within multidimensional patient data that traditional statistical methods might overlook. This capability enables more precise patient stratification for CER studies, ensuring that comparative effectiveness is evaluated across clinically relevant subgroups rather than heterogeneous populations.
Random forest models, an ensemble ML method that "builds multiple decision trees and combines their outputs to improve prediction accuracy," have proven particularly effective for "classifying toxicity profiles and identifying potential biomarkers in preclinical research" [85]. These approaches allow researchers to move beyond simple demographic or clinical characteristics to identify subgroups based on complex molecular, genetic, and phenotypic signatures.
Drug-Target Interaction Prediction for Comparative Mechanistic Studies
Predicting drug-target interactions (DTI) represents a crucial application of AI that directly informs CER study design. DTI prediction "can significantly enhance speed, reduce costs, and screen potential drug design options before conducting actual experiments" [87]. This capability enables researchers to select more appropriate comparators and design more mechanistically informed studies.
The AI-driven DTI prediction process integrates multiple data modalities through sophisticated computational frameworks:
Integration of Qualitative Evidence with Quantitative Data
AI methodologies enable more sophisticated integration of qualitative evidence with traditional quantitative outcomes, addressing a critical need in comprehensive CER. As noted in recent research, "qualitative data are a key source of information, capturing people's beliefs, experiences, attitudes, behavior and interactions" that provide "context to decisions and richer information on stakeholder perspectives which are otherwise inaccessible through even the most robust quantitative assessments of clinical and cost-effectiveness" [88].
Natural language processing (NLP), a specialized AI domain, can systematically analyze qualitative data from "patient testimonies," "semi-structured interviews," and "focus groups" to identify themes and patterns that inform CER study endpoints and outcome measurement strategies [88]. This integration is particularly valuable for medical devices, digital health technologies, and rare disease treatments where "qualitative evidence can provide information on aspects not fully captured by available quantitative data" [88].
Experimental Protocols and Methodologies
AI-Enhanced Patient Recruitment and Trial Matching
Protocol Objective: Optimize patient recruitment and trial matching using ML algorithms to reduce recruitment timelines and improve population representativeness.
Methodology:
- Data Integration: Aggregate structured and unstructured data from electronic health records (EHRs), genomic databases, and patient-generated health data.
- Feature Engineering: Apply NLP to extract relevant clinical concepts from unstructured physician notes and patient narratives.
- Similarity Learning: Implement metric learning algorithms to identify patients with similar clinical profiles who may benefit from the interventions under comparison.
- Predictive Enrollment Modeling: Use time-to-event analysis with gradient boosting machines to forecast recruitment rates and identify potential bottlenecks.
- Dynamic Eligibility Optimization: Apply reinforcement learning to adjust eligibility criteria based on recruitment patterns while maintaining scientific validity.
Validation Approach: Compare recruitment efficiency (time to target enrollment, screen failure rates, population diversity metrics) against traditional methods using historical trial data through propensity score-matched analyses.
Predictive Analytics for Early Endpoint Detection
Protocol Objective: Utilize ML to identify surrogate endpoints and predict long-term outcomes from short-term data, reducing trial duration and cost.
Methodology:
- Multimodal Data Fusion: Integrate clinical, omics, digital biomarker, and real-world evidence data streams using neural network architectures.
- Temporal Pattern Recognition: Apply recurrent neural networks (RNNs) and long short-term memory (LSTM) networks to identify early signals predictive of long-term outcomes.
- Causal Inference Modeling: Implement double machine learning methods to estimate treatment effects while controlling for confounding variables.
- Endpoint Validation: Use bootstrapping and cross-validation techniques to assess the reliability of AI-identified surrogate endpoints against established clinical outcomes.
Implementation Considerations: Ensure regulatory alignment through early engagement with health technology assessment bodies regarding acceptable validation approaches for novel endpoints [88].
Synthetic Control Arm Development
Protocol Objective: Generate synthetic control arms using real-world data and historical trial information to reduce the number of patients receiving placebo or standard of care.
Methodology:
- Real-World Data Curation: Collect and harmonize structured EHR data, claims data, and registry information for the target patient population.
- Covariate Balance Optimization: Apply propensity score matching, entropy balancing, or genetic algorithms to create comparable groups.
- Outcome Prediction: Train models on historical control data to predict expected outcomes for the synthetic cohort.
- Bias Assessment: Implement quantitative bias analysis to evaluate potential residual confounding.
- Hybrid Design Implementation: Combine synthetic controls with concurrent controls in adaptive Bayesian designs to maintain statistical rigor while reducing sample size requirements.
Table 2: Key Research Reagent Solutions for AI-Enhanced CER
| Tool Category | Specific Solutions | Function in CER Study Design | Data Input Requirements |
|---|---|---|---|
| Drug-Target Interaction Prediction | TargetPredict [87], MT-DTI [87], Transformer-based Models [87] | Predicts molecular-level interactions between drug compounds and biological targets to inform mechanistic comparisons | Drug structures (SMILES), protein sequences/structures, known interaction databases |
| Clinical Trial Optimization Platforms | AI-Driven Patient Matching Algorithms, Predictive Enrollment Models | Enhances recruitment efficiency and population representativeness in comparative trials | Electronic health records, genomic data, patient-generated health data |
| Qualitative Data Analysis Tools | Natural Language Processing (NLP) for Patient Testimonies, Interview Transcript Analysis [88] | Systematically analyzes qualitative evidence on patient experiences and preferences to inform endpoint selection | Interview transcripts, focus group recordings, patient submission data |
| Real-World Evidence Integration | AI-Enhanced RWE Platforms, Causal Inference Models | Leverages real-world data to create synthetic control arms and enhance generalizability | EHRs, claims data, registries, patient-reported outcomes |
| Predictive Biomarker Discovery | Random Forest Classifiers [85], Neural Networks [85] | Identifies patient subgroups most likely to benefit from specific interventions | Omics data, clinical phenotypes, treatment response data |
Implementation Framework and Future Directions
Ethical and Regulatory Considerations
The integration of AI into CER introduces important ethical dimensions that researchers must address. As emphasized in recent literature, "it's never been more important to understand the ethics of AI in the workplace, especially if you're building ML models, training AI systems, or leveraging generative AI to support your own work" [89]. Specific considerations for CER include:
- Algorithmic Bias Mitigation: Implement rigorous testing for potential biases in AI systems that might disproportionately affect specific patient subgroups in comparative assessments.
- Transparency and Explainability: Develop methods to make AI-driven insights interpretable to regulators, clinicians, and patients, addressing the "black box" problem of complex algorithms [89].
- Regulatory Alignment: Engage early with health technology assessment bodies like NICE, which has developed real-world evidence frameworks that are evolving to incorporate AI-generated evidence [88].
Emerging Frontiers: Generative AI and Large Language Models
The advent of generative AI and large language models (LLMs) opens new possibilities for CER study design. Researchers are exploring "how to harness the powerful reasoning capabilities of large language models to integrate drug discovery tasks" [87]. Specific applications include:
- Automated Protocol Development: Using LLMs to generate comprehensive study protocols based on current methodological standards and regulatory requirements.
- Evidence Synthesis Acceleration: Applying transformer-based models to systematically review and synthesize existing comparative evidence across multiple data sources.
- Hypothesis Generation: Leveraging generative AI to identify novel comparative research questions from the extensive biomedical literature and real-world data.
Implementation Roadmap
Successful integration of AI into CER requires a structured approach:
- Skills Development: Build interdisciplinary teams with expertise in both CER methodology and AI implementation, potentially through specialized training programs [89] [90].
- Data Infrastructure Investment: Develop robust data governance frameworks and integration platforms to support the multimodal data requirements of AI algorithms.
- Iterative Validation: Establish continuous validation processes to assess and improve the performance of AI tools in real-world CER applications.
- Stakeholder Engagement: Implement comprehensive engagement strategies with patients, clinicians, and policymakers to ensure AI-enhanced CER addresses meaningful clinical questions and decision needs [88].
By embracing these transformative technologies while maintaining scientific rigor and ethical standards, CER researchers can develop more efficient, informative, and patient-centered comparative studies that accelerate the delivery of optimal therapies to the patients who need them most.
Validating CER Evidence: Comparing Methodologies and Building Confidence in Results
Within pharmaceutical comparative effectiveness research (CER), a fundamental question persists: how consistently do results from observational studies align with those from randomized controlled trials (RCTs)? This whitepaper synthesizes current evidence to address this question, presenting quantitative data on agreement rates, analyzing methodological protocols for valid comparison, and providing a research toolkit for the critical appraisal of both study designs. The analysis reveals that while broad agreement is common, significant discrepancies occur in a substantial minority of comparisons, driven largely by clinical heterogeneity and methodological biases rather than study design alone. For researchers and drug development professionals, this underscores the necessity of rigorous design and analytical techniques when generating and synthesizing real-world evidence and trial data.
Comparative Effectiveness Research (CER) is defined as the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care [12]. The central aim is to assist patients, clinicians, purchasers, and policy makers in making informed decisions that will improve health care at both the individual and population levels. CER is inherently patient-centered, focusing on outcomes that are important to patients, such as survival, quality of life, and functional status.
- Role of Study Designs: The evidence base for CER is built upon multiple study designs. Randomized Controlled Trials (RCTs) are traditionally considered the gold standard for establishing efficacy due to their experimental nature, designs that minimize bias, rigorous data quality, and analytical approaches supporting causal inference [91]. However, observational studies—which analyze data from real-world settings like electronic health records (EHRs), insurance claims, and registries—provide critical evidence on effectiveness in broader, more diverse patient populations and are indispensable for assessing long-term safety and outcomes in routine practice [91] [92].
The ongoing scientific and policy debate centers on the reliability of observational studies to estimate causal treatment effects comparable to those from RCTs. Understanding the frequency and causes of divergence is essential for the appropriate use of evidence in drug development and regulatory decision-making.
Quantitative Evidence: Meta-Epidemiological Comparisons
Large-scale meta-epidemiological studies have systematically quantified the agreement between observational studies and RCTs. The table below summarizes key findings from recent, high-quality analyses.
Table 1: Summary of Meta-Epidemiological Studies on RCT and Observational Study Agreement
| Study / Scope | Number of Pairs Analyzed | Agreement Metric | Key Finding | Notes |
|---|---|---|---|---|
| PMC8647453 (2021) [91]Various pharmaceuticals | 74 pairs from 29 systematic reviews | No statistically significant difference (based on 95% CI) | 79.7% of pairs showed no significant difference. | 43.2% of pairs showed an "extreme difference" (ratio < 0.7 or > 1.43); 17.6% had both significant difference and effects in opposite directions. |
| BMC Medicine (2022) [93]General medical research | 129 BoE* pairs from 64 systematic reviews | Ratio of Ratios (RoR) for binary outcomes | Pooled RoR = 1.04 (95% CI 0.97–1.11). | On average, no difference in pooled effect estimates. Considerable statistical heterogeneity was present. |
| BMC Medicine (2022) [93]Subgroup by PI/ECO-similarity | 37 "broadly similar" BoE pairs | Ratio of Ratios (RoR) for binary outcomes | High statistical heterogeneity and wide prediction intervals. | Clinical heterogeneity (PI/ECO-dissimilarities) and cohort study design were key drivers of variability. |
BoE: Body of Evidence
Interpretation of Quantitative Findings
The data presents a nuanced picture:
- Broad Agreement Exists: The finding that nearly 80% of comparisons show no statistically significant difference, coupled with a pooled Ratio of Ratios close to 1.0, indicates that observational studies often produce similar relative treatment effects to RCTs [91] [93].
- Significant Disagreement is Not Rare: Despite broad agreement, a non-trivial proportion of comparisons show clinically important discrepancies. The finding that over 40% of pairs had "extreme differences" and nearly 18% differed significantly and pointed in opposite directions highlights the potential for misleading conclusions from observational data in specific contexts [91].
- Heterogeneity is a Key Driver: The disagreement is not random. The BMC Medicine study identified that differences in Population, Intervention/Exposure, Comparison, and Outcome (PI/ECO) were a major source of variation. When the specific clinical questions addressed by the RCTs and observational studies were dissimilar, the statistical heterogeneity increased significantly, leading to less reliable and more divergent comparisons [93].
Methodological Protocols for Comparing Bodies of Evidence
To objectively assess the consistency between observational studies and RCTs, a rigorous, protocol-driven approach is required. The following workflow outlines the key stages in this process, from systematic identification to quantitative synthesis.
Figure 1: Methodological Workflow for Comparing RCT and Observational Study Evidence
Detailed Experimental and Analytical Methods
The stages in Figure 1 involve specific technical protocols:
Systematic Review Identification: Researchers conduct comprehensive searches in databases like PubMed and Embase for systematic reviews that contain pooled effect estimates from both RCTs and observational studies addressing the same clinical question [91] [93]. The search must be structured with explicit inclusion/exclusion criteria, focusing on specific therapeutic areas and outcomes.
Defining and Rating PI/ECO Similarity: This is a critical step for ensuring like-for-like comparison. Each PI/ECO domain is rated for similarity:
- Population: Are the patient groups "more or less identical," "similar but not identical," or only "broadly similar"?
- Intervention/Exposure: Is the pharmaceutical intervention and its delivery comparable?
- Comparator: Is the control or comparator group equivalent?
- Outcome: Are the efficacy/effectiveness or safety outcomes defined and measured identically? The overall similarity of a Body of Evidence (BoE) pair is classified according to the domain with the lowest degree of similarity [93]. This directly tests whether clinical heterogeneity explains divergence.
Data Extraction and Harmonization: For each BoE, researchers extract pooled relative effect estimates (e.g., Risk Ratio [RR], Hazard Ratio [HR], Odds Ratio [OR]) along with their 95% confidence intervals and measures of heterogeneity (e.g., I²). A key challenge is the harmonization of different effect measures. When necessary, conversion formulas are applied, for instance, converting an OR to a RR using an assumed control risk to ensure comparability [93].
Quantitative Synthesis - Calculating Agreement: The core analysis involves calculating the ratio of the relative effect estimate from observational studies over that from RCTs (Ratio of Ratios, RoR). A RoR of 1.0 indicates perfect agreement. A Monte Carlo simulation is often used to derive the 95% CI for this ratio, which determines statistical significance of any difference [91] [93]. Subgroup analyses are then performed to explore factors like PI/ECO-similarity, therapeutic area, and risk of bias.
The Scientist's Toolkit: Key Reagents and Methods for CER
For researchers designing or evaluating comparative effectiveness studies, the following "toolkit" comprises essential methodological concepts and analytical solutions.
Table 2: Research Reagent Solutions for Comparative Effectiveness Research
| Tool / Concept | Category | Function & Explanation |
|---|---|---|
| PI/ECO Framework | Study Design | A structured protocol to define the research question, ensuring that Population, Intervention/Exposure, Comparator, and Outcomes are precisely specified before study initiation. This is the foundational step for minimizing clinical heterogeneity. |
| New User Design | Study Design | An observational study design that identifies a cohort of patients who are newly starting a therapy. By defining a clear baseline, it helps mitigate biases like prevalent user bias, which can distort true treatment effects. |
| Propensity Score Methods | Statistical Analysis | A suite of techniques (matching, weighting, stratification) used to adjust for measured confounding in observational studies. They create a balanced pseudo-population where treatment groups are comparable on observed covariates. |
| Instrumental Variable (IV) Analysis | Statistical Analysis | A method to address unmeasured confounding by using a third variable (the instrument) that is correlated with the treatment assignment but not directly with the outcome. A powerful tool for causal inference in non-randomized data [94]. |
| Systematic Review with Meta-Analysis | Evidence Synthesis | A research method that identifies, appraises, and synthesizes all relevant studies on a specific question. Provides a more precise and reliable estimate of effect than any single study. |
| Real-World Data (RWD) Sources | Data Infrastructure | Established, ready-to-analyze data sources such as electronic health records (EHRs), insurance claims databases, and patient registries (e.g., PCORnet). These provide the large, representative populations needed for observational CER [39]. |
Discussion and Forward Look
The body of evidence demonstrates that observational studies and RCTs frequently agree on the direction and magnitude of relative treatment effects for pharmaceuticals. However, the observed rate of significant disagreement—approximately one in five comparisons—demands a sophisticated approach to evidence generation and synthesis.
Implications for Research and Policy
- Moving Beyond Design Hierarchy: The focus should shift from a simplistic hierarchy of evidence (RCTs over observational studies) to a focus on the fitness for purpose of each study design and the rigor of its execution. Observational studies are invaluable for assessing long-term outcomes, rare adverse events, and effectiveness in general practice, particularly when RCTs are infeasible or unethical [91] [92].
- Emphasis on Methodological Rigor: The observed discrepancies are often attributable to avoidable errors in study design and analysis. Adherence to good research practices is paramount. This includes drafting a detailed protocol a priori, using designs like inception cohorts and new-user designs, proactively addressing confounding through advanced statistical methods, and transparently reporting all choices [95] [94].
- The Promise of Prospective IVs and Emulation: Innovative approaches are being developed to strengthen observational CER. The prospective creation of instrumental variables (IVs)—such as systematically varying treatment preferences across different hospitals in a coordinated, stepwise manner—can mimic randomization and substantially reduce unmeasured confounding, making observational estimates more reliable [94]. Similarly, the practice of trial emulation, where observational studies are designed to closely mirror the eligibility criteria and endpoint definitions of a specific RCT, provides a powerful framework for assessing consistency.
For the pharmaceutical research community, the path forward lies in leveraging the complementary strengths of RCTs and observational studies. By applying rigorous methodologies detailed in this whitepaper, researchers can enhance the reliability of real-world evidence, thereby building a more robust, complete, and actionable evidence base for drug development and clinical decision-making.
In pharmaceutical research, comparative effectiveness research (CER) aims to inform clinical and regulatory decisions by identifying which treatments work best for specific patient populations. A fundamental challenge in CER lies in reconciling variation in relative treatment effects observed across different study types, particularly between randomized controlled trials (RCTs) and observational studies. This technical guide examines the sources of this variation, providing methodological frameworks for its investigation and proposing advanced analytical approaches to enhance the validity and applicability of evidence synthesis. Through systematic analysis of heterogeneity sources and implementation of robust methodologies, drug development professionals can better interpret conflicting evidence and generate more reliable real-world insights for healthcare decision-making.
Comparative effectiveness research (CER) in pharmaceuticals represents "a rigorous evaluation of the impact of different treatment options that are available for treating a given medical condition for a particular set of patients" [96]. Unlike efficacy trials that establish whether a treatment works under ideal conditions, CER seeks to determine how treatments perform in real-world settings across diverse patient populations [13]. This distinction is crucial for clinicians, patients, and policymakers who need to understand not just average treatment effects, but how those effects vary across specific patient subgroups and care settings.
The Agency for Healthcare Research and Quality (AHRQ) emphasizes that CER often focuses on broad populations, potentially lacking information relevant to particular patient subgroups of concern to stakeholders [13]. This limitation becomes particularly apparent when comparing evidence from different study designs, each with distinct methodological approaches and inherent limitations. The healthcare community continues to seek better methods to develop information that can foster improved medical care at a "personal" or "individual" level, moving beyond population averages to understand variation in treatment response [13].
Quantitative Landscape of Variation Between RCTs and Observational Studies
A systematic assessment of treatment effect comparability between RCTs and observational studies reveals substantial variation in a significant proportion of comparisons. A 2021 analysis of 30 systematic reviews across 7 therapeutic areas provided quantitative insights into this phenomenon [91].
Table 1: Comparison of Relative Treatment Effects Between RCTs and Observational Studies
| Comparison Metric | Findings | Number/Percentage of Pairs |
|---|---|---|
| Total analysis pairs | Pairs of pooled relative effect estimates from RCTs and observational studies | 74 pairs from 29 reviews |
| Statistical significance difference | No statistically significant difference (based on 95% CI) in relative effect estimates | 79.7% of pairs |
| Extreme differences | Ratio of relative effects < 0.70 or > 1.43 | 43.2% of pairs |
| Clinically significant disagreements | Statistically significant difference with estimates pointing in opposite directions | 17.6% of pairs |
These findings demonstrate that while the majority of RCTs and observational studies show no statistically significant differences in relative treatment effects, a substantial proportion (approximately 20%) exhibit significant variation, with nearly one-fifth demonstrating effects in opposite directions [91]. This variation underscores the importance of understanding its sources to properly interpret evidence from different study designs.
Conceptual Framework: Types of Heterogeneity in Evidence Synthesis
Variation in treatment effects across studies arises from different forms of heterogeneity, each with distinct implications for evidence interpretation. The literature primarily describes three interconnected types of heterogeneity that collectively influence observed treatment effects.
Clinical Heterogeneity
Clinical heterogeneity refers to "variation in study population characteristics, coexisting conditions, cointerventions, and outcomes evaluated across studies" that may influence the magnitude of intervention effects [13]. This type of heterogeneity arises from differences in participant characteristics (e.g., age, sex, baseline disease severity, ethnicity, comorbidities), intervention characteristics (e.g., dose, frequency, duration), types or timing of outcome measurements, and research settings [97]. In pharmaceutical research, clinical heterogeneity manifests when studies include patients with different demographic profiles, disease stages, comorbidity burdens, or concomitant medications that modify treatment response.
Methodological Heterogeneity
Methodological heterogeneity stems from "variability in trial design and analysis" [97]. This encompasses differences in study design (e.g., parallel-group vs. crossover trials), allocation concealment, blinding procedures, randomization methods, follow-up duration, and analytical approaches (e.g., intention-to-treat vs. per-protocol analysis) [97]. Methodological heterogeneity is particularly relevant when comparing RCTs and observational studies, as their fundamental design approaches differ substantially in controlling for bias and confounding.
Statistical Heterogeneity
Statistical heterogeneity represents "variability in observed treatment effects that is beyond what would be expected by random error (chance)" [13]. It is quantitatively assessed using tests such as the I² statistic, which quantifies the percentage of total variation across studies due to heterogeneity rather than chance [98]. The relationship between clinical, methodological, and statistical heterogeneity can be conceptualized as a cause-and-effect sequence: clinical and methodological heterogeneity present across studies can lead to observed statistical heterogeneity in meta-analyses [13].
Figure 1: Relationship Between Heterogeneity Types in Treatment Effects. Clinical and methodological heterogeneity act as causative factors that manifest as statistical heterogeneity, ultimately leading to observed variation in treatment effects between studies.
Methodological Protocols for Investigating Heterogeneity
Assessment of Clinical Heterogeneity
Systematic investigation of clinical heterogeneity requires explicit methodologies implemented during evidence synthesis [97]. The following protocol provides a structured approach:
A Priori Planning: Pre-specify planned investigations of clinical heterogeneity in the systematic review protocol, including identified potential effect modifiers and analytical approaches [97].
Expert Engagement: Include clinical experts on the review team to identify clinically relevant variables that may modify treatment effects [97].
Covariate Selection: Select clinical covariates considering variables at multiple levels:
- Participant level (age, sex, disease severity, comorbidities)
- Intervention level (dose, frequency, duration)
- Outcome level (event type, length of follow-up)
- Research setting (academic medical center vs. community practice) [97]
Scientific Rationale: Ensure selected covariates have a clear scientific rationale as potential effect modifiers rather than testing all available variables [97].
Adequate Data: Verify sufficient numbers of studies or patients per covariate category to support meaningful analysis.
Cautious Interpretation: Interpret findings with caution, recognizing the potential for spurious associations, especially with multiple testing [97].
Subgroup Analysis for Heterogeneity of Treatment Effects
Subgroup analysis represents the most common analytical approach for examining heterogeneity of treatment effects (HTE) [96]. This method evaluates treatment effects within predefined patient subgroups, typically using a test for interaction to determine if subgroup variables significantly modify treatment effects.
Table 2: Subgroup Analysis Framework for Heterogeneity of Treatment Effects
| Component | Description | Considerations |
|---|---|---|
| Definition | Evaluation of treatment effect for multiple subgroups one variable at a time | Uses baseline or pretreatment variables to define mutually exclusive subgroups |
| Statistical test | Test for interaction evaluates if subgroup variable significantly modifies treatment effect | Generally has low power to detect true differences in subgroup effects |
| Sample size implications | Sample size ~4× larger needed to detect subgroup difference of same magnitude as ATE | Sample size ~16× larger needed to detect difference half the magnitude of ATE |
| Multiple testing | Risk of false positive findings when testing multiple subgroup variables | Bonferroni correction maintains Type I error but increases Type II error |
| Interpretation | If interaction significant, estimate treatment effects separately for each subgroup | Focus on magnitude of difference rather than statistical significance alone |
When implementing subgroup analysis, researchers should select subgroups based on mechanism and plausibility, incorporating clinical judgment and prior knowledge of treatment effect modifiers [96]. Pre-specification of subgroup analyses in study protocols reduces the risk of data-driven false positive findings.
Network Meta-Analysis Methodology
Network meta-analysis (NMA) extends traditional pairwise meta-analysis by simultaneously comparing multiple interventions using both direct and indirect evidence [99]. This methodology is particularly valuable in pharmaceutical research when multiple treatment options exist but have not all been directly compared in head-to-head trials.
The validity of NMA depends on satisfying key assumptions:
- Similarity: Different sets of studies included in the analysis should be similar, on average, in all important factors that may affect relative effects [100].
- Transitivity: The distribution of effect modifiers should be similar across treatment comparisons [100].
- Consistency: Direct and indirect evidence for a particular treatment comparison should agree within statistical bounds [100].
Figure 2: Network Meta-Analysis Geometry. Network meta-analysis combines direct comparisons (solid lines) and indirect comparisons (dashed lines) to estimate relative treatment effects between all interventions in the network, even those not directly compared in head-to-head trials.
The NMA process involves:
- Systematic Identification: Attempt to include all relevant RCTs comparing any of the interventions of interest [99].
- Network Geometry Exploration: Graphically depict the network of interventions to visualize direct and indirect comparison pathways [99].
- Assumption Assessment: Evaluate transitivity and consistency assumptions through clinical and methodological review and statistical testing [100].
- Statistical Synthesis: Perform frequentist or Bayesian NMA to estimate relative treatment effects and ranking probabilities [99].
- Incoherence Evaluation: Assess disagreement between direct and indirect evidence using specific statistical tests [100].
Analytical Tools and Research Reagents
Advanced statistical software and methodologies are essential for implementing the complex analyses required to investigate variation in treatment effects.
Table 3: Research Reagent Solutions for Heterogeneity Analysis
| Tool/Method | Function | Application Context |
|---|---|---|
| I² statistic | Quantifies proportion of total variation due to heterogeneity rather than chance | Meta-analysis of multiple studies |
| Chi-squared (χ²) test | Determines if observed differences in results stem from heterogeneity or random variation | Meta-analysis heterogeneity assessment |
| Meta-regression | Examines relationship between study characteristics and effect sizes | Investigation of heterogeneity sources |
| Subgroup analysis | Divides studies into groups based on characteristics to explore effect modification | HTE assessment for patient subgroups |
| Network meta-analysis | Simultaneously compares multiple interventions using direct and indirect evidence | Mixed treatment comparisons |
| Bayesian regression (beanz) | Evaluates HTE using formal incorporation of prior information | Patient-centered outcomes research |
| E-value | Measures minimum strength of unmeasured confounding needed to explain away effect | Observational study robustness assessment |
Software implementations for these analyses include both frequentist and Bayesian approaches. Frequentist NMA can be performed using R (netmeta package) and Stata, while Bayesian NMA can be implemented using WinBUGS, OpenBUGS, R (gemtc, pcnetmeta, and BUGSnet packages), and other specialized software [99]. For Bayesian analysis of HTE, the beanz package provides a user-friendly interface for comprehensive Bayesian HTE analysis [101].
Implications for Pharmaceutical Research and Development
Understanding sources of variation in treatment effects between study types has profound implications for drug development and evaluation. The observed discrepancies between RCTs and observational studies highlight the limitations of relying exclusively on either design alone and emphasize the value of triangulating evidence from multiple sources [102].
For drug development professionals, several strategic considerations emerge:
- Clinical Trial Design: Adaptive trials, sequential trials, and platform trials represent innovative designs that may enhance the efficiency and applicability of pharmaceutical RCTs [102].
- Real-World Evidence Integration: Observational studies using causal inference methods can complement RCTs by providing evidence on effectiveness in broader patient populations under real-world conditions [102].
- Subgroup Identification: Proactive investigation of HTE can identify patient subgroups that benefit most (or least) from specific treatments, supporting personalized treatment approaches [96].
- Evidence Synthesis: Advanced meta-analytic techniques, including NMA, provide frameworks for comparing all available treatments simultaneously, even when direct comparisons are lacking [99] [100].
Methodological innovations in both RCTs and observational studies continue to blur the traditional boundaries between these designs. EHR-based clinical trials leverage real-world data to enhance trial efficiency and generalizability, while causal inference methods applied to observational data increasingly approximate the rigor of randomized designs [102]. These converging methodologies promise to enhance the quality and applicability of pharmaceutical evidence in the future.
Variation in relative treatment effects between RCTs and observational studies represents a multifactorial phenomenon rooted in clinical, methodological, and statistical heterogeneity. Through systematic application of rigorous investigative methodologies—including subgroup analysis, meta-regression, and network meta-analysis—researchers can better characterize these sources of variation and generate more reliable evidence for healthcare decision-making. The pharmaceutical research community continues to develop increasingly sophisticated approaches to investigate and account for these sources of variation, ultimately enhancing the quality and applicability of evidence for patients, clinicians, and policymakers. As methodological innovations continue to emerge, the integration of diverse evidence sources through transparent and rigorous analytical frameworks will remain essential for advancing comparative effectiveness research in pharmaceuticals.
The Evolving Regulatory and Payer Landscape for CER and Real-World Evidence
Comparative Effectiveness Research (CER) is defined by the Institute of Medicine as "the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care" [1]. The core question of CER is which treatment works best, for whom, and under what circumstances [26]. Unlike traditional efficacy studies that compare a treatment against placebo under ideal conditions, CER typically compares two or more active treatments to inform real-world clinical decisions [103].
Real-World Evidence (RWE) refers to clinical evidence derived from the analysis of Real-World Data (RWD)—data collected outside of conventional randomized controlled trials (RCTs) [104]. These data sources include electronic health records (EHRs), claims and billing data, product and disease registries, patient-generated data (including from mobile devices), and other sources that reflect patient health status and the delivery of healthcare [104].
The integration of RWE into CER represents a paradigm shift in pharmaceutical research, moving beyond traditional clinical trials to incorporate evidence from routine clinical practice. This evolution is driven by the need to understand how medical products perform in diverse patient populations, across varied healthcare settings, and over longer timeframes than typically studied in pre-market trials [105] [106].
The Expanding Regulatory Use of RWE
Regulatory agencies worldwide are increasingly recognizing the value of RWE in drug evaluation and monitoring. The U.S. Food and Drug Administration (FDA) has developed a framework for using RWE to support regulatory decision-making across the product lifecycle [105].
FDA Use of RWE in Regulatory Decisions
The FDA's Center for Drug Evaluation and Research (CDER) and Center for Biologics Evaluation and Research (CBER) have utilized RWE in various regulatory capacities, including supporting new drug approvals, informing labeling changes, and post-market safety monitoring [105]. The table below summarizes notable examples of FDA's use of RWE in regulatory decisions.
Table 1: FDA Use of Real-World Evidence in Regulatory Decision-Making
| Drug/Product | Regulatory Action Year | Data Source | Study Design | Role of RWE |
|---|---|---|---|---|
| Aurlumyn (Iloprost) | 2024 | Medical records | Retrospective cohort | Confirmatory evidence for frostbite treatment |
| Vimpat (Lacosamide) | 2023 | PEDSnet data network | Retrospective cohort | Safety data for pediatric dosing |
| Actemra (Tocilizumab) | 2022 | National death records | Randomized controlled trial | Primary endpoint assessment (mortality) |
| Vijoice (Alpelisib) | 2022 | Medical records | Single-arm study | Substantial evidence of effectiveness |
| Orencia (Abatacept) | 2021 | CIBMTR registry | Non-interventional | Pivotal evidence for graft-versus-host disease prevention |
| Prolia (Denosumab) | 2024 | Medicare claims | Retrospective cohort | Safety warning for hypocalcemia risk |
International Regulatory Landscape
Globally, health technology assessment (HTA) bodies and regulatory agencies are developing frameworks for evaluating RWE. The National Institute for Health and Care Excellence (NICE) in the UK, the Federal Institute for Drugs and Medical Devices (BfArM) in Germany, and the Pharmaceuticals and Medical Devices Agency (PMDA) in Japan are all establishing approaches for incorporating RWE into their assessment processes [107]. A key challenge identified across these agencies is the transportability of RWE—determining whether evidence generated in one healthcare system or population can be reliably applied to another [108]. Differences in population demographics, healthcare systems, and clinical practice patterns can limit the applicability of nonlocal RWE, necessitating methodological approaches to address these challenges [108].
Methodological Frameworks and Experimental Protocols
CER Study Designs and Their Applications
CER employs a spectrum of research methodologies, each with distinct strengths and appropriate use cases [26] [1]:
Table 2: Comparative Effectiveness Research Study Designs
| Study Design | Key Features | Strengths | Limitations | Best Use Cases |
|---|---|---|---|---|
| Pragmatic Randomized Controlled Trials | Random assignment in routine practice settings | High internal validity, reflects real-world practice | Costly, time-consuming, may not be feasible for rare outcomes | Comparing treatments when equipoise exists |
| Systematic Reviews and Meta-Analyses | Structured synthesis of existing evidence | Comprehensive, minimizes bias, identifies evidence gaps | Dependent on primary study quality, potential publication bias | Establishing overall evidence base, informing guidelines |
| Prospective Observational Studies | Data collection following study protocol | Can study diverse populations, captures long-term outcomes | Potential for confounding, requires significant resources | Studying long-term effects, rare adverse events |
| Retrospective Observational Studies | Analysis of existing data (claims, EHRs) | Rapid, cost-effective, large sample sizes | Data quality issues, confounding by indication | Hypothesis generation, post-market safety monitoring |
Framework for CER Study Design Selection
A structured framework can guide researchers in selecting appropriate CER study designs based on clinical context and evidence needs [103]. The following diagram illustrates a decision pathway for determining when comparative effectiveness designs are justified:
Addressing Bias in RWE Studies
Observational RWE studies are susceptible to various biases, particularly confounding by indication, where treatment assignments are influenced by patient characteristics [1]. Methodological approaches to address these challenges include:
Propensity Score Methods: Creating a single score that represents the probability of receiving a treatment given observed covariates, allowing researchers to balance treatment groups across measured potential confounders [1].
Risk Adjustment: Using statistical models to account for differences in patient case mix across treatment groups, enabling more valid comparisons of outcomes [1].
Active Comparator Designs: Selecting active comparators with similar indications and contraindications to reduce channeling bias, where patients with different prognoses are directed toward different treatments [1].
The APPRAISE tool, presented at a 2025 regulatory roundtable, provides a structured approach for appraising potential for bias in RWE studies, helping regulators and researchers assess study quality and validity [107].
The Scientist's Toolkit: Essential Research Reagents and Data Solutions
Table 3: Research Reagent Solutions for CER and RWE Studies
| Tool Category | Specific Solutions | Function/Application | Key Considerations |
|---|---|---|---|
| Data Networks | Sentinel System [105], PEDSnet [105], PCORnet [26] | Distributed data networks for safety monitoring and outcomes research | Data standardization, privacy protection, network representation |
| Common Data Models | OMOP (OHDSI) [106] | Standardized structure and vocabulary for heterogeneous data sources | Enables scalable analysis, facilitates multi-database studies |
| Analytic Methods | Propensity scoring [1], Risk adjustment [1], Transportability methods [108] | Address confounding and improve validity of causal inferences | Requires specialized expertise, sensitivity analyses recommended |
| Patient-Generated Data | Wearables, Mobile health apps, Patient registries [104] [106] | Capture patient-centered outcomes and experiences outside clinical settings | Data quality variability, privacy considerations, engagement challenges |
| RWD Repositories | EHR systems, Claims databases, Disease registries [104] | Provide large-scale longitudinal data on treatment patterns and outcomes | Data completeness, accuracy, and representativeness must be assessed |
Payer Perspectives and Health Technology Assessment
Payers and HTA bodies are increasingly considering RWE when making coverage and reimbursement decisions. The Institute for Clinical and Economic Review (ICER) in the United States provides independent evaluations of the clinical effectiveness and comparative value of healthcare interventions [26]. However, HTAs often face challenges with nonlocal RWE, particularly when data from other jurisdictions may not be directly applicable to their local population or healthcare system [108].
The FRAME (Framework for Real-World Evidence Assessment to Mitigate Evidence Uncertainties for Efficacy/Effectiveness) tool has been developed to help HTAs and regulators evaluate RWE submissions consistently [107]. This framework addresses key dimensions of RWE assessment, including data relevance and reliability, study design appropriateness, and potential for bias.
A 2025 roundtable discussion involving multiple HTA agencies highlighted ongoing efforts to harmonize approaches to RWE assessment, though inconsistencies in review processes and acceptability thresholds remain across organizations [107]. This evolving landscape underscores the importance of early engagement with relevant HTA bodies and regulators when planning RWE generation strategies.
Future Directions and Strategic Implications
The field of CER and RWE is rapidly evolving, with several key trends shaping its future:
Advanced Analytics: Artificial intelligence and machine learning are being applied to RWE to identify patterns, predict outcomes, and personalize treatment plans [106].
Global Collaboration: International initiatives are working to develop global RWE standards and facilitate cross-border data exchange while addressing transportability challenges [108] [106].
Patient-Centricity: Patients are increasingly contributing to RWE generation through wearable devices, mobile health apps, and patient registries, enhancing the relevance of research outcomes [106].
Regulatory Harmonization: Efforts such as the International Council for Harmonisation (ICH) are working to develop harmonized approaches to RWE across regulatory agencies [109].
For drug development professionals, these trends highlight the growing importance of integrating RWE generation into overall development strategies. This includes considering how RWE can complement traditional clinical trial data, support post-market evidence needs, and demonstrate the value of new therapies in diverse patient populations and real-world settings.
Comparative Effectiveness Research (CER) is defined by the Institute of Medicine as "the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care" [1]. In the pharmaceutical sector, CER moves beyond traditional efficacy trials conducted in ideal settings to answer critical questions about how drugs perform in real-world clinical practice against relevant alternatives. This research paradigm focuses on determining which treatment works best, for whom, and under what circumstances, providing essential evidence for healthcare decision-makers [110] [1].
The fundamental goal of pharmaceutical CER is to assist consumers, clinicians, purchasers, and policymakers in making informed decisions that improve healthcare outcomes at both individual and population levels. CER achieves this by generating evidence on the comparative benefits, harms, and effectiveness of pharmaceuticals through various methodological approaches, including systematic reviews, randomized controlled trials, and observational studies [1]. In recent years, investment in CER has grown substantially, driven by the need to understand how interventions perform in real-world settings and populations that may differ significantly from those in traditional clinical trials [110].
Methodological Approaches in CER
CER Study Designs and Their Applications
CER employs a range of methodological approaches, each with distinct strengths and applications for pharmaceutical research. The choice of method depends on the research question, available resources, ethical considerations, and the need for generalizability versus control.
Table 1: Comparative Effectiveness Research Methodologies
| Method Type | Key Characteristics | Best Use Cases | Limitations |
|---|---|---|---|
| Randomized Controlled Trials (RCTs) | Participants randomly assigned to treatment groups; considers gold standard for clinical research [1] | Research requiring high certainty; established efficacy comparisons [1] | Expensive, time-consuming, may lack generalizability to real-world populations [1] |
| Pragmatic Clinical Trials | RCTs designed to reflect real-world practice conditions; more flexible protocols [110] | Effectiveness comparisons in routine care settings [110] | Balance between internal validity and generalizability |
| Observational Studies | Participants not randomized; treatments chosen by patients/physicians [1] | Rare diseases, when RCTs cannot be performed, large representative populations [1] | Potential for selection bias and confounding [1] |
| Systematic Reviews | Critical assessment of all research on clinical issue using specific criteria [1] | Synthesizing body of evidence; informing guidelines and policy [1] | Dependent on quality of primary studies |
| Network Meta-Analyses | Indirect comparison of multiple treatments using connected evidence networks [110] | Multiple treatment comparisons when head-to-head trials lacking [110] | Requires methodological expertise and connectivity assumptions |
Addressing Methodological Challenges in CER
Observational CER studies using real-world data present specific methodological challenges, particularly concerning confounding and selection bias. Several statistical approaches have been developed to address these issues. Risk adjustment identifies risk scores for patients based on conditions identified via claims or medical records, calibrating for relative health status [1]. Propensity score methods calculate the conditional probability of receiving treatment given predictive variables, then match treatment and control patients based on these scores to estimate outcome differences between balanced patient groups [1]. These techniques help mitigate biases that naturally occur when treatments are not randomly assigned.
The growing importance of real-world evidence (RWE) in regulatory and reimbursement decisions has highlighted the need for rigorous methodological standards. As noted in a case study of pembrolizumab, "substantial variability in outcomes based on methodological choices" underscores the importance of transparent reporting and sensitivity analyses [74]. The U.S. FDA has increasingly incorporated RWE into regulatory decision-making, using it for purposes ranging from supporting new indications to informing safety labeling changes [105].
Figure 1: Decision Pathway for CER Methodology Selection
Case Studies in Pharmaceutical Decision-Making
Case Study 1: Pembrolizumab in Advanced Non-Small Cell Lung Cancer
Study Background and Objectives
A recent comprehensive analysis examined the comparative effectiveness of first-line pembrolizumab versus therapeutic alternatives in advanced non-small cell lung cancer (aNSCLC) among Medicare-eligible patients [74]. This case study is particularly relevant given the imminent eligibility of pembrolizumab for price negotiations under the Inflation Reduction Act and the need for robust real-world evidence to inform these discussions. The study aimed to evaluate how methodological decisions impact real-world comparative effectiveness outcomes, using electronic health record data from the Flatiron Health database comprising approximately 280 U.S. cancer clinics [74].
Experimental Protocol and Methodology
The study employed a retrospective observational design analyzing data from 2011 to 2023. Patient cohorts were divided into three groups based on FDA indications for pembrolizumab: (1) metastatic non-squamous NSCLC without EGFR or ALK mutations; (2) metastatic squamous NSCLC; and (3) metastatic NSCLC with PD-L1 expression ≥1% without EGFR or ALK mutations [74]. The methodology included several key components:
- Data Source: Electronic health record-derived deidentified database from Flatiron Health, including structured and unstructured data curated via technology-enabled abstraction [74].
- Patient Selection: Included patients aged ≥65 years or those <65 years with Medicare insurance, diagnosed with stage IIIB-IVB NSCLC, and initiating first-line systemic therapy [74].
- Treatment Assignment: Pembrolizumab combinations (with chemotherapy) for indications 1-2; pembrolizumab monotherapy for indication 3. Control groups received common non-platinum-based chemotherapy regimens [74].
- Biomarker Assessment: EGFR, ALK, and PD-L1 status verified using test results within 30 days before first-line therapy initiation [74].
- Statistical Analysis: Propensity score-based inverse probability weighting applied to balance covariates. Primary outcomes were real-world progression-free survival and overall survival [74].
- Scenario Analyses: Multiple analyses examined influence of time period selection, PD-L1 inclusion, therapeutic alternative definitions, and treatment switching [74].
Table 2: Key Research Reagents and Data Solutions for Real-World CER
| Research Component | Function in CER | Application in Pembrolizumab Study |
|---|---|---|
| Electronic Health Record Data | Provides real-world clinical data from routine practice | Flatiron Health database with data from ~280 cancer clinics [74] |
| Biomarker Assays | Identifies molecular characteristics for patient stratification | EGFR, ALK, and PD-L1 testing within 30 days pre-treatment [74] |
| Propensity Score Methods | Balances covariates between treatment groups in observational studies | Inverse probability weighting to adjust for confounding [74] |
| Overall Survival Analysis | Measures time from treatment initiation to death from any cause | Primary effectiveness endpoint across all indications [74] |
| Progression-Free Survival | Measures time from treatment initiation to disease progression or death | Secondary effectiveness endpoint in the analysis [74] |
Key Findings and Implications
The analysis revealed substantial variability in outcomes based on methodological choices. For the non-squamous cohort, overall survival benefits of pembrolizumab therapies compared to alternatives varied from a non-significant difference to an improvement of 2.7 months (95% CI 1.2, 4.8), depending on analytical decisions [74]. In the squamous cohort, pembrolizumab combinations consistently demonstrated overall survival benefits ranging from 1.4 months (95% CI 0.1, 3.0) to 3.6 months (95% CI 0.1, 5.9) [74]. However, for pembrolizumab monotherapy, overall survival differences were statistically non-significant across analyses [74].
This case study underscores critical methodological considerations for CER intended to inform policy decisions. The researchers emphasized that "transparent reporting and scenario analyses in real-world evidence [are essential] to support Centers for Medicare & Medicaid Services decision making during drug price negotiations" [74]. The variability in outcomes based on analytical choices highlights the need for rigorous methodological standards to ensure both internal validity and real-world generalizability of CER findings.
Case Study 2: FDA Regulatory Applications of Real-World Evidence
Regulatory Framework and Background
The U.S. Food and Drug Administration has increasingly incorporated real-world evidence into regulatory decision-making, with documented cases of RWE supporting product approvals, labeling changes, and postmarket safety assessments [105]. This represents a significant expansion of CER applications beyond traditional health technology assessment domains into core regulatory functions. The FDA has utilized RWE from various sources, including medical records, disease registries, claims data, and specialized data networks like Sentinel [105].
Experimental Protocols Across Case Examples
Multiple regulatory case examples demonstrate varied applications of CER methodologies:
- Iloprost (Aurlumyn) for Frostbite: Approval supported by a multicenter retrospective cohort study using medical records with historical controls. The RWE served as confirmatory evidence for effectiveness [105].
- Tocilizumab (Actemra): Approval based in part on a randomized controlled trial that leveraged RWD collected from national death records to evaluate 28-day mortality, the trial's primary endpoint [105].
- Vedolizumab (Entyvio): Safety assessment using a descriptive Sentinel study to evaluate risk of interstitial lung disease, resulting in labeling changes [105].
- Abatacept (Orencia): Approval for graft-versus-host disease prophylaxis based partly on a non-interventional study using the Center for International Blood and Marrow Transplant Research registry. The RWE provided pivotal evidence comparing overall survival post-transplantation between patients treated with abatacept versus those without [105].
Figure 2: Real-World Data Sources and Regulatory Applications in CER
Impact and Implications
These regulatory case examples demonstrate the expanding role of CER and RWE in pharmaceutical decision-making throughout the product lifecycle. The FDA's systematic approach to incorporating RWE includes assessing data quality, study design robustness, and the appropriateness of analytical methods. The cases illustrate that RWE can serve varied roles in regulatory contexts, from providing confirmatory evidence to serving as pivotal evidence for approval decisions [105]. This evolution in regulatory science creates new opportunities for pharmaceutical manufacturers to leverage real-world data for label expansions and optimization of use conditions, particularly when randomized trials are impractical or unethical.
Value Assessment and Stakeholder Perspectives in CER
Stakeholder Incentives and Value Proposition
The value of comparative effectiveness research varies significantly across stakeholder groups, creating complex incentives for investment and utilization. From a conceptual framework, CER can provide value in three primary scenarios: (1) identifying when one intervention is consistently superior to alternatives; (2) identifying patient subsets where interventions with heterogeneous treatment effects are superior; or (3) identifying when interventions are sufficiently similar in effectiveness that decisions can be based on cost [111].
Table 3: Stakeholder Perspectives on CER Value
| Stakeholder | Primary Value Drivers | Investment Incentives |
|---|---|---|
| Patients | Improved health outcomes; personalized treatment selection; informed decision-making [111] | Limited direct investment capacity; reliant on public funding and provider initiatives |
| Pharmaceutical Manufacturers | Product differentiation; price premiums for demonstrated superiority; label expansions [111] | Strong when expected positive results; risk of unfavorable results creates disincentives [111] |
| Payers | Cost containment; optimal resource allocation; improved value of services [111] | Moderate but limited by ability to capture long-term benefits in competitive markets [111] |
| Regulatory Agencies | Improved benefit-risk assessment; postmarket safety monitoring; public health protection [105] | High for safety monitoring; growing for effectiveness assessment in real-world settings [105] |
| Healthcare Providers | Clinical decision support; improved patient outcomes; professional satisfaction | Moderate but constrained by time limitations and implementation challenges |
Patients typically derive the greatest benefit from CER through improved health outcomes from better treatment selection, yet have limited capacity to directly invest in research [111]. Pharmaceutical manufacturers have strong incentives to invest in CER when expecting favorable results but face significant risks from potentially unfavorable findings, creating selective investment patterns [111]. Payers benefit from CER through improved resource allocation but may not capture long-term value in competitive insurance markets, limiting private investment incentives [111]. This misalignment between social value and private incentives creates a compelling case for public investment in CER.
Methodological Framework for Valuing CER
Value of Information (VOI) analysis provides a conceptual framework for quantifying the potential value of comparative effectiveness studies before they are conducted [111]. This approach calculates the expected value of research based on the likelihood and potential impact of different study outcomes, helping prioritize public investments in CER. VOI analysis is particularly valuable for identifying research areas where societal benefits substantially exceed private returns, ensuring efficient allocation of public research funds [111].
The application of VOI techniques is demonstrated in case studies where CER identified superior treatments for specific patient subgroups, leading to optimized resource allocation and improved patient outcomes [111]. In one pharmaceutical example, the publication of comparative effectiveness results was followed by price adjustments reflecting the demonstrated value, illustrating how CER can influence market dynamics beyond clinical decision-making [111].
Future Directions and Implementation Considerations
Emerging Methodological Innovations
The field of comparative effectiveness research continues to evolve with several promising methodological developments. Target trial emulation applies principles of randomized trial design to observational data, creating a structured framework for causal inference [112]. The U.S. FDA has shown "vocal adoption of the target trial emulation framework," signaling growing regulatory acceptance of sophisticated observational methods [112]. Synthetic data approaches are also gaining traction for addressing data access challenges in health technology assessment, with applications as external control arms in clinical trials and in health economic evaluation [113].
International frameworks like Canada's CanREValue provide systematic approaches for incorporating real-world evidence into cancer drug reassessment decisions, offering models for more integrated and continuous evidence generation throughout product lifecycles [112]. The FRAME methodology offers another systematic approach for evaluating the use and impact of RWE in health technology assessment and regulatory submissions [112].
Implementation Challenges and Solutions
Successful implementation of CER in pharmaceutical decision-making requires addressing several persistent challenges. Data quality and completeness remain significant concerns, particularly for electronic health records not originally collected for research purposes. The ISPOR Task Force has established best-practice guidelines for evaluating the suitability of electronic health records for health technology assessments, including assessments of dataset structure, source consistency, and clinical variable completeness [74].
Methodological transparency is another critical requirement, as demonstrated by the substantial variability in outcomes based on analytical choices in the pembrolizumab case study [74]. Pre-specification of analytical methods, comprehensive scenario analyses, and clear reporting of assumptions are essential for generating reliable evidence. The CER Collaborative has developed standardized tools and questionnaires to assess the relevance and credibility of different study designs, promoting greater consistency in CER evaluation [110].
Finally, stakeholder engagement throughout the research process ensures that CER addresses decision-relevant questions and that findings are effectively implemented. PCORI's Foundational Expectations for Partnerships in Research provides a systematic framework for patient and stakeholder engagement that is firmly built on prior evidence, requiring meaningful collaboration in research development and execution [39].
Comparative Effectiveness Research represents a fundamental shift in pharmaceutical evidence generation, moving from isolated efficacy assessment to comprehensive evaluation in real-world settings against relevant alternatives. The case studies presented demonstrate successful applications across diverse contexts, from regulatory decision-making to price negotiations and clinical guideline development. As methodological innovations continue to enhance the validity and reliability of CER, and as regulatory and reimbursement bodies increasingly incorporate these evidences into decision frameworks, the strategic importance of CER throughout the pharmaceutical product lifecycle will continue to grow. The ongoing challenge for researchers, manufacturers, and policymakers will be to maintain rigorous methodological standards while ensuring that evidence generation remains timely, relevant, and responsive to the needs of patients and healthcare systems.
The Role of Organizations like PCORI in Setting CER Standards and Priorities
Comparative Effectiveness Research (CER) is fundamentally designed to inform healthcare decisions by providing evidence on the effectiveness, benefits, and harms of different treatment options [11]. The Institute of Medicine defines CER as "the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care" [1]. Unlike efficacy studies which determine whether an intervention works under ideal conditions, CER focuses on effectiveness—how interventions perform in real-world settings with diverse patients and varying clinical circumstances [18]. This distinction is particularly crucial in pharmaceuticals research, where real-world performance often differs significantly from controlled trial results due to factors such as heterogeneous patient populations, comorbidities, and adherence patterns.
The Patient-Centered Outcomes Research Institute (PCORI) was established to address gaps in evidence needed by healthcare decision-makers [114]. PCORI's specific mission is to fund patient-centered comparative clinical effectiveness research that assists "patients, clinicians, payers, and policy makers in making informed health decisions" [114]. PCORI fulfills this mission not only by funding research but also through an active program to "develop and improve the science and methods of comparative clinical effectiveness research" [114]. This dual focus on both generating evidence and advancing methodological rigor positions PCORI as a pivotal organization in shaping CER standards, particularly for pharmaceutical research where robust methodologies are essential for valid comparisons between drug therapies and other treatment options.
PCORI's Methodology Standards: A Framework for Scientific Rigor
Development and Structure of the Standards
PCORI's Methodology Standards were developed through a systematic, iterative process led by PCORI's legislatively mandated Methodology Committee [115]. The committee assessed potential standards, authored a draft methodology report, solicited public comments, and undertook substantial revisions before formal adoption by PCORI's Board of Governors [115]. This process continues through regular updates, with standards adopted in May 2017, April 2018, February 2019, and March 2024, ensuring the guidance remains current with methodological advances [115]. The standards provide baseline requirements for the development and conduct of patient-centered CER, specifying "the minimal requirements for sound science" [115].
The 67 standards are organized into two broad groups: cross-cutting standards applicable to all patient-centered CER, and standards for specific study designs and methods [115]. All applicants for PCORI research funding are required to demonstrate adherence to these standards in the design, conduct, and reporting of their research [115]. This requirement ensures that PCORI-funded studies meet consistent thresholds for methodological rigor while maintaining focus on patient-centeredness throughout the research process.
Key Cross-Cutting Standards for Pharmaceutical CER
Table 1: Key Cross-Cutting PCORI Methodology Standards Relevant to Pharmaceutical Research
| Standard Category | Standard Code | Key Requirement | Significance for Pharmaceutical Research |
|---|---|---|---|
| Formulating Research Questions | RQ-1 | Identify evidence gaps using systematic reviews | Ensures research addresses genuine evidence gaps in pharmaceutical interventions |
| RQ-5 | Select appropriate interventions and comparators | Requires comparators to represent actual clinical options, not just placebo controls | |
| RQ-6 | Measure outcomes patients notice and care about | Shifts focus from surrogate endpoints to patient-relevant outcomes | |
| Patient-Centeredness | PC-1 | Engage patients and stakeholders throughout research | Incorporates patient perspectives in pharmaceutical study design and implementation |
| PC-3 | Use patient-reported outcomes (PROs) when appropriate | Captures treatment benefits and harms directly from patients' experiences | |
| Data Integrity & Analyses | IR-1 | Specify analysis plans a priori | Reduces data-dependent analysis biases in pharmaceutical trial results |
| IR-2 | Assess data source adequacy | Ensures robust capture of drug exposures, outcomes, and relevant covariates | |
| Heterogeneity of Treatment Effects | HT-1 | Assess HTE on baseline patient characteristics | Identifies which patients benefit most from specific pharmaceutical therapies |
The cross-cutting standards establish fundamental requirements for high-quality CER. The standards for formulating research questions (RQ-1 to RQ-6) require that studies be designed to generate evidence needed to support informed health decisions [116] [115]. For pharmaceutical research, this means ensuring that comparisons reflect real-world clinical decisions—typically comparing new drugs against existing active treatments rather than placebo, unless placebo represents a legitimate clinical option [116]. The standards also mandate measuring "outcomes that people representing the population of interest notice and care about" such as "survival, functioning, symptoms, health-related quality of life" [116]. This requirement shifts the focus in pharmaceutical research from laboratory values or surrogate endpoints to outcomes that directly impact patients' lives.
The standards for patient-centeredness (PC-1 to PC-4) fundamentally transform how pharmaceutical research is conducted by requiring meaningful engagement of patients and other stakeholders throughout the research process [116]. Researchers must describe how they will identify, recruit, and retain stakeholders and justify approaches if engagement is not appropriate [116]. The standards also emphasize using patient-reported outcomes (PROs) when patients are the best source of information, requiring careful consideration of PRO measurement properties including "content validity, construct validity, reliability, responsiveness to change over time, and score interpretability" [116]. For pharmaceutical studies, this means capturing treatment benefits and harms directly from patients' perspectives rather than relying solely on clinician assessments.
The standards for data integrity and rigorous analyses (IR-1 to IR-7) address essential methodological requirements including a priori specification of analysis plans, assessment of data source adequacy, documentation of validated scales, and implementation of data management plans [116]. For pharmaceutical CER, these standards ensure that studies using real-world data (such as electronic health records or claims data) carefully consider the measurement properties of exposures (drug treatments), outcomes, and relevant covariates [116]. The standards also address potential biases by recommending masking (blinding) "when feasible" and discussing the impact when masking is not possible [116].
Figure 1: PCORI Methodology Standards Framework - This diagram illustrates the organization of PCORI's 67 methodology standards into cross-cutting and study design-specific categories, providing a structured framework for rigorous patient-centered CER.
Standards for Specific Study Designs and Methods
Table 2: PCORI Standards for Specific Study Designs Relevant to Pharmaceutical Research
| Standard Category | Key Requirements | Application to Pharmaceutical Research |
|---|---|---|
| Causal Inference Methods | Identify/addressing sources of bias; appropriate methods for observational data | Supports valid treatment effect estimates from non-randomized pharmaceutical studies |
| Adaptive & Bayesian Trial Designs | Pre-specified adaptation rules; operational independence; appropriate analysis | Enables more efficient pharmaceutical trials that can adapt to accumulating evidence |
| Data Networks & Registries | Ensure data quality, relevance, and appropriate use | Facilitates use of real-world evidence from multiple sources for pharmaceutical CER |
| Systematic Reviews | Application of accepted systematic review standards | Ensures comprehensive evidence synthesis for pharmaceutical interventions |
| Studies of Complex Interventions | Address multi-component interventions and their interactions | Relevant for pharmaceutical regimens combined with behavioral or delivery interventions |
The standards for causal inference methods (CI-1 to CI-6) are particularly relevant for pharmaceutical CER using observational data, as they specify requirements for "identifying and addressing possible sources of bias to produce valid conclusions about the benefits and risks of an intervention" [115]. These standards are essential when randomized trials are not feasible or ethical, helping researchers address confounding and other biases common in non-experimental studies of drug effects [114].
The standards for adaptive and Bayesian trial designs provide guidance on the design, conduct, and analysis of these innovative approaches to patient-centered CER [115]. For pharmaceutical research, adaptive designs can make studies more efficient and more responsive to patient needs by allowing modifications to the trial based on accumulating data while preserving trial integrity and validity.
The standards for data registries and data networks help ensure that these infrastructures contain "relevant, high-quality data that are used appropriately" when employed in research [115]. For pharmaceutical CER, these standards support the valid use of real-world data from multiple sources, enabling studies of drug effectiveness in broader patient populations than typically included in clinical trials.
Methodological Priorities and Evolving Research Agenda
Current Methodological Funding Priorities
PCORI maintains an active research agenda to address methodological gaps in patient-centered CER. For the 2025 funding cycles, PCORI has identified four priority areas for methodological research [117] [118]:
- Methods to Improve the Use of Artificial Intelligence (AI) and Machine Learning (ML) in Clinical Research - Developing approaches to leverage these technologies while ensuring valid, reliable, and equitable applications in CER.
- Methods to Improve Study Design - Enhancing the robustness, efficiency, and patient-centeredness of CER study designs.
- Methods to Support Data Research Networks - Improving the infrastructure and methodologies for using distributed data networks in CER.
- Methods Related to Ethical and Human Subjects Protections Issues - Addressing ethical considerations specific to patient-centered CER.
These priorities reflect PCORI's commitment to not only establishing baseline standards but also advancing the methodological frontier for CER. The funding announcements specifically seek projects that will "address high-priority methodological gaps" and "lead to improvements in the strength and quality of evidence generated by CER studies" [117]. For pharmaceutical research, these priorities are particularly relevant given the increasing use of real-world data, artificial intelligence, and complex study designs to evaluate drug effectiveness.
Addressing Key Methodological Challenges in Pharmaceutical CER
PCORI's methods portfolio has specifically targeted several challenging methodological areas relevant to pharmaceutical research. These include:
Improving techniques for handling unmeasured confounding using advanced methods such as high-density propensity scoring, targeted maximum likelihood estimation, and machine learning techniques in large observational datasets [114]. One funded project is developing a specialized toolkit to provide researchers access to advanced analytic techniques, such as inverse probability weighting of marginal structural models and the parametric g-formula approach, to account for time-dependent confounding [114].
Comparing results and patient populations from randomized controlled trials and observational studies for the same health condition to assess and refine statistical methods for causal inference [114]. This research is crucial for understanding when and how real-world evidence can reliably inform decisions about pharmaceutical treatments.
Evaluating propensity score methods with the goal of determining which are optimal for detecting and estimating treatment-effect modification [114]. This work helps identify which patients are most likely to benefit from specific pharmaceutical treatments.
Developing methods to address missing data, including using global sensitivity analysis to account for missing data in clinical trials and investigating imputation methods in observational datasets [114]. Missing data is a common challenge in pharmaceutical research that can compromise study validity if not handled appropriately.
The Scientist's Toolkit: Essential Methods for Pharmaceutical CER
Core Methodological Approaches
Table 3: Essential Methodological Approaches for Pharmaceutical Comparative Effectiveness Research
| Method Category | Specific Methods | Application in Pharmaceutical CER | Key Considerations |
|---|---|---|---|
| Study Designs | Large simple randomized trials | Ideal for definitive comparisons of pharmaceutical interventions with hard endpoints | High cost, long duration, potential for practice patterns to change during trial [18] |
| Observational studies using claims data | Efficient examination of drug effects in real-world populations | Potential for confounding by indication; requires methods to address bias [1] [18] | |
| Evidence synthesis & meta-analysis | Combining evidence from multiple studies of pharmaceutical interventions | Challenges with heterogeneity across studies; may lack head-to-head comparisons [18] | |
| Bias Adjustment Methods | Propensity score matching | Balancing measured covariates between treatment groups in observational drug studies | Addresses measured confounding but not unmeasured confounding [1] [18] |
| Instrumental variable analysis | Addressing unmeasured confounding in pharmaceutical outcomes research | Requires valid instrument strongly related to treatment but not outcome [18] | |
| Risk adjustment | Accounting for differences in patient case mix when comparing drug effects | Can use prospective (predictive) or concurrent (explanatory) models [1] | |
| Outcome Measurement | Patient-reported outcomes (PROs) | Capturing treatment benefits and harms directly from patients | Must demonstrate validity, reliability, responsiveness to change [116] |
| Standardized clinical endpoints | Using consistent definitions for clinical events across studies | Facilitates comparison across pharmaceutical treatment studies |
Practical Implementation Framework
Implementing rigorous pharmaceutical CER requires careful attention to methodological standards throughout the research process. The following framework outlines key considerations:
Research Question Formulation: Begin with a systematic review to identify genuine evidence gaps [116]. Engage patients and clinicians to ensure the question reflects real clinical decisions and outcomes that matter to patients [116]. For pharmaceutical studies, this often means comparing active treatments rather than focusing solely on placebo comparisons.
Study Design Selection: Choose designs that balance methodological rigor with feasibility and relevance. Consider whether randomized designs are feasible or whether observational approaches with appropriate bias-adjustment methods are necessary [18]. For rare diseases or long-term outcomes, observational designs may be the only feasible approach.
Data Source Assessment: Ensure data sources adequately capture drug exposures, outcomes, and relevant covariates [116]. For pharmaceutical studies using claims data, be aware of limitations such as lack of clinical detail, potential misclassification, and incomplete capture of over-the-counter medications [1].
Analytic Plan Specification: Pre-specify analytic approaches including handling of missing data, subgroup analyses, and methods for addressing potential confounding [116]. Document all changes to the analysis plan and justify methodological decisions.
Patient-Centeredness Implementation: Engage patients and other stakeholders throughout the research process—from topic selection through dissemination [116] [119]. Select outcomes that patients notice and care about, and use patient-reported outcomes when appropriate [116].
Dissemination Planning: Plan from the outset how to disseminate results in formats usable by different audiences, including lay language summaries for patients [116]. Engage stakeholders in developing dissemination strategies that will make the findings actionable [116].
PCORI plays an indispensable role in advancing the methodological foundation of comparative effectiveness research for pharmaceuticals through its comprehensive standards and focused research agenda. The 67 methodology standards provide a rigorous framework for generating evidence that is not only scientifically valid but also directly relevant to the decisions faced by patients, clinicians, and other healthcare stakeholders. By emphasizing patient-centeredness throughout the research process—from question formulation through dissemination—PCORI ensures that pharmaceutical CER addresses outcomes that matter to patients and produces evidence usable in real-world clinical decisions.
The ongoing methods research funded by PCORI addresses critical gaps in CER methodology, particularly in areas such as artificial intelligence, adaptive designs, and causal inference methods using real-world data. For pharmaceutical researchers, understanding and applying PCORI's methodology standards is essential for producing evidence that will reliably inform healthcare decisions and ultimately improve patient outcomes. As the field continues to evolve, PCORI's role in setting standards and priorities will remain crucial for advancing the science of comparative effectiveness research in pharmaceuticals.
Conclusion
Comparative Effectiveness Research represents a fundamental shift towards a more evidence-based, patient-centered pharmaceutical ecosystem. By synthesizing key takeaways, it is clear that CER's strength lies in its methodological diversity—harnessing the rigor of RCTs, the generalizability of observational studies, and the power of evidence synthesis to answer critical questions about real-world treatment value. For researchers and drug development professionals, mastering these methods is no longer optional but essential for demonstrating product value in an era of heightened scrutiny on cost and outcomes. The future of CER will be shaped by the integration of artificial intelligence, the expansive growth of real-world data, and its critical role in advancing personalized medicine. Ultimately, CER provides the foundational evidence needed to ensure that the right patients receive the right drugs, improving health outcomes at both the individual and population levels.
References
- 1. Comparative Effectiveness Research [https://actuary.org/comparative-effectiveness-research/]
- 2. Comparative and Cost-Effectiveness Research - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5650552/]
- 3. HHS Should Evaluate Its Performance of Related Activities [https://www.gao.gov/products/gao-25-107462]
- 4. Methodologies for data collection and analysis for monitoring and evaluation | M&E Guidelines [https://mandeguidelines.iom.int/en/clone-methodologies-data-collection-and-analysis-monitoring-and-evaluation]
- 5. Challenges in Modelling the Cost Effectiveness of ... [https://pubmed.ncbi.nlm.nih.gov/40717166/]
- 6. Alzheimer's disease drug development pipeline: 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131090/]
- 7. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 8. Can We Make Health Economic Decision Models as ... [https://link.springer.com/article/10.1007/s40273-025-01515-x]
- 9. Pharmacoeconomic Analyses and Modeling [https://www.sciencedirect.com/science/article/abs/pii/B9780128142769000180]
- 10. Newly Added Guidance Documents [https://www.fda.gov/drugs/guidances-drugs/newly-added-guidance-documents]
- 11. AHRQ Comparative Effectiveness Reviews - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK42934/]
- 12. Comparative Effectiveness Research and Patient ... [https://www.amcp.org/legislative-regulatory-position/comparative-effectiveness-research-and-patient-centered-outcomes-research]
- 13. Introduction - Comparative Effectiveness Review Methods [https://www.ncbi.nlm.nih.gov/books/NBK53313/]
- 14. A Review of Heterogeneity in Comparative Economic ... [https://link.springer.com/article/10.1007/s40273-025-01478-z]
- 15. Comparison of the efficacy of updated drugs for ... [https://www.sciencedirect.com/science/article/abs/pii/S0306452224006110]
- 16. Cancer treatment and survivorship statistics, 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223361/]
- 17. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 18. A Primer on Comparative Effectiveness Research Methods [https://www.pharmacytimes.com/view/a-primer-on-comparative-effectiveness-research-methods]
- 19. A framework for understanding cancer comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3461183/]
- 20. Methods in Comparative Effectiveness Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3504326/]
- 21. An Overview of Methods for Comparative Effectiveness ... [https://www.sciencedirect.com/science/article/abs/pii/S1053429613000817]
- 22. Integrating Analytical Methods to Improve Comparative ... [https://www.pcori.org/research-results/2013/integrating-analytical-methods-improve-comparative-effectiveness-research]
- 23. Integrating Analytical Methods to Improve Comparative ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK603795/]
- 24. Data Management for Comparative Effectiveness ... [https://medipharmsolutions.com/blog/data-management-for-comparative-effectiveness-research-cer/]
- 25. Predictive models for clinical decision making: Deep dives in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9544754/]
- 26. Comparative effectiveness research - Wikipedia [https://en.wikipedia.org/wiki/Comparative_effectiveness_research]
- 27. Defining comparative effectiveness research: the importance of getting it right - PubMed [https://pubmed.ncbi.nlm.nih.gov/20473202/]
- 28. Looking at CER from the Pharmaceutical Industry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10437711/]
- 29. Comparative effectiveness research and its utility in In- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4763521/]
- 30. Comparative Effectiveness Research (CER) Inventory | ASPE [https://aspe.hhs.gov/comparative-effectiveness-research-cer-inventory]
- 31. Value Assessment Framework [https://icer.org/our-approach/methods-process/value-assessment-framework/]
- 32. Randomized clinical trial (RCT): An overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11757218/]
- 33. Randomized controlled trials – The what, when, how and why [https://www.sciencedirect.com/science/article/pii/S147751312400617X]
- 34. Pragmatic randomized controlled trials: strengthening the ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-024-07935-y]
- 35. Shifting from Traditional to Pragmatic Randomized Controlled ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11963812/]
- 36. Randomised Controlled Trial - Quantitative study designs [https://deakin.libguides.com/quantitative-study-designs/rct]
- 37. Integrating quantitative and qualitative data and findings ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6886933/]
- 38. Comparative Effectiveness Training (CERTaIN) [https://www.mdanderson.org/education-training/outreach-programs/comparative-effectiveness-research-training.html]
- 39. Retrospective Observational Studies Leveraging Existing ... [https://www.pcori.org/funding-opportunities/announcement/improving-health-decision-making-observational-comparative-clinical-effectiveness-research]
- 40. A Statistical Analysis Plan Template for Observational ... [https://link.springer.com/article/10.1007/s42519-025-00504-9]
- 41. Presenting data in tables and charts - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4008059/]
- 42. SUMMARY OF EVIDENCE AND DATA SYNTHESIS - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK361833/]
- 43. PRISMA statement [https://www.prisma-statement.org/]
- 44. An updated guideline for reporting systematic reviews [https://www.equator-network.org/reporting-guidelines/prisma/]
- 45. Step Five: Data Extraction & Synthesis - Systematic Reviews [https://libguides.unthsc.edu/systematic-reviews/step-five]
- 46. Data Extraction - Evidence Synthesis - LibGuides at Ohio ... [https://hslguides.osu.edu/c.php?g=997383&p=7219141]
- 47. Comparative effectiveness and safety of pharmaceuticals ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-021-02176-1]
- 48. Propensity Score Analysis [https://www.publichealth.columbia.edu/research/population-health-methods/propensity-score-analysis]
- 49. Strong instrumental variables biased propensity scores in ... [https://www.sciencedirect.com/science/article/abs/pii/S0895435623000021]
- 50. Strong instrumental variables biased propensity scores in ... [https://pubmed.ncbi.nlm.nih.gov/36657590/]
- 51. Instrumental variable approaches for estimating time-varying ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02625-y]
- 52. Augmenting Treatment Arms With External Data Through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12380038/]
- 53. Comparative Effectiveness Research: Foundational to ... [https://healthcarevaluehub.org/resource/2020/comparative-effectiveness-research-foundational-to-healthcare-value-efforts/]
- 54. What Is CER and Why Does It Matter? [https://www.pcori.org/blog/2025/what-cer-and-why-does-it-matter]
- 55. How Much Postmarket Surveillance (PMS) Data Should We ... [https://www.orielstat.com/blog/purpose-of-pms-data-in-cer-vs-psur/]
- 56. Comparative Effectiveness Research [https://www.tuftsctsi.org/research-services/stakeholder-community-engagement/comparative-effectiveness-research/]
- 57. Distinguishing selection bias and confounding bias in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4043938/]
- 58. Reducing bias through directed acyclic graphs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2601045/]
- 59. Causal Modeling to Mitigate Selection Bias and Unmeasured ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9307267/]
- 60. Generalized Simple Graphical Rules for Assessing ... [https://arxiv.org/html/2502.00924v3]
- 61. Challenges of Comparative Effectiveness Research with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6467208/]
- 62. What is Claims Data and Its Advantages and Disadvantages? [https://www.datavant.com/real-world-data-rwd/claims-data]
- 63. Challenges in and Opportunities for Electronic Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10938158/]
- 64. Claims Data vs EHRs: Distinct but United in Real-World ... [https://nashbio.com/blog/ehr/claims-data-vs-ehrs/]
- 65. Caveats for the Use of Operational Electronic Health Record ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3748381/]
- 66. Strengths and Limitations of CMS Administrative Data in ... [https://resdac.org/articles/strengths-and-limitations-cms-administrative-data-research]
- 67. How much can we trust electronic health record data? [https://www.sciencedirect.com/science/article/abs/pii/S2213076420300439]
- 68. Christofides | Comparison of electronic health records and ... [https://www.jscdm.org/article/id/224/]
- 69. Advancing the role of real-world evidence in comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11609978/]
- 70. An Introduction to Propensity Score Methods for Reducing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3144483/]
- 71. Use of Machine Learning to Compare Disease Risk Scores ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12130674/]
- 72. Methods to Adjust for Confounding in Test-Negative Design ... [https://formative.jmir.org/2025/1/e58981]
- 73. When and why to use overlap weighting: clarifying its role ... [https://www.sciencedirect.com/science/article/pii/S0895435625002756]
- 74. Key Considerations for Assessing Real-World Comparative ... [https://link.springer.com/article/10.1007/s40273-025-01514-y]
- 75. Real-World Evidence [https://www.fda.gov/science-research/science-and-research-special-topics/real-world-evidence]
- 76. 9 Ways Real-World Evidence is Changing Healthcare [https://www.arbormetrix.com/blog/9-ways-real-world-evidence-is-changing-healthcare/]
- 77. Good practices for real‐world data studies of treatment and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5639372/]
- 78. Real World Evidence [https://www.iqvia.com/solutions/real-world-evidence]
- 79. Generating real-world evidence at scale using advanced ... [https://www.mckinsey.com/industries/life-sciences/our-insights/generating-real-world-evidence-at-scale-using-advanced-analytics]
- 80. Enhancing drug discovery and patient care through ... [https://www.sciencedirect.com/science/article/pii/S2472630324001201]
- 81. Advancing data science in drug development through an ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-021-01409-4]
- 82. The Impact of Big Data Analytics on Pharma Industry [https://binariks.com/blog/big-data-analytics-in-pharma-use-cases/]
- 83. Understanding Data Analytics in the Pharmaceutical Industry [https://careset.com/understanding-data-analytics-in-the-pharmaceutical-industry/]
- 84. Comparative Effectiveness Outcomes Research [https://www.publichealth.columbia.edu/academics/degrees/master-public-health/certificates/comparative-effectiveness-outcomes-research]
- 85. The Potential of Artificial Intelligence in Pharmaceutical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195710/]
- 86. How Machine Learning is Recoding the Future of Drug ... [https://www.drugpatentwatch.com/blog/the-application-of-machine-learning-in-drug-discovery-revolutionizing-pharmaceutical-research/?srsltid=AfmBOoo_vTxsZsDdhvoIpockOcobuN9ymciaA_4PnvFSO_It-Q1abni6]
- 87. Application of Artificial Intelligence In Drug-target ... [https://www.nature.com/articles/s44385-024-00003-9]
- 88. Quality in qualitative evidence: new best practice principles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12224144/]
- 89. Future-Proof Your Career With AI Skills [https://www.pce.uw.edu/news-features/articles/future-proof-your-career-ai]
- 90. Your future career could depend on how quickly you ... [https://www.purdue.edu/online/your-future-career-could-depend-on-how-quickly-you-master-ai-skills-heres-how-to-get-started/]
- 91. Comparative effectiveness and safety of pharmaceuticals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8647453/]
- 92. The role of randomized controlled trials, registries ... [https://www.sciencedirect.com/science/article/pii/S1521692623000841]
- 93. Evaluating agreement between bodies of evidence from ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-022-02369-2]
- 94. Improving Registry-Based Observational Comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11198280/]
- 95. The ISPOR Good Research Practices Task Force Report [https://www.sciencedirect.com/science/article/pii/S1098301512000071]
- 96. Estimation and Reporting of Heterogeneity of Treatment Effects [https://www.ncbi.nlm.nih.gov/books/NBK126188/]
- 97. Investigating clinical heterogeneity in systematic reviews [https://pmc.ncbi.nlm.nih.gov/articles/PMC3564789/]
- 98. Understanding Heterogeneity In Research | CASP [https://casp-uk.net/news/heterogeneity-in-research/]
- 99. Concepts and emerging issues of network meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8497908/]
- 100. Chapter 11: Undertaking network meta-analyses [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-11]
- 101. Filling Two Major Gaps in the Analysis of Heterogeneity of ... [https://www.icpsr.umich.edu/web/pcodr/studies/39522]
- 102. Rethinking the pros and cons of randomized controlled trials ... [https://bmcproc.biomedcentral.com/articles/10.1186/s12919-023-00285-8]
- 103. Comparative effectiveness research for the clinician ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4988047/]
- 104. Integrating RWE into CER for Post-market Devices [https://www.makrocare.com/blog/medical-devices-integrating-rwe-into-cer-for-post-market-devices/]
- 105. FDA use of Real-World Evidence in Regulatory Decision ... [https://www.fda.gov/science-research/real-world-evidence/fda-use-real-world-evidence-regulatory-decision-making]
- 106. RWE as the Top Trend in 2025 [https://www.iqvia.com/blogs/2025/01/rwe-as-the-top-trend-in-2025]
- 107. Regulatory and Payer Evaluation of Real-World Evidence [https://www.drugepi.org/dope/rwe-roundtable-2025]
- 108. Transportability of nonlocal real-world evidence and its ... [https://pubmed.ncbi.nlm.nih.gov/40836909/]
- 109. ICH announces new topics, adopts harmonized template ... [https://www.raps.org/news-and-articles/news-articles/2025/11/ich-announces-new-topics,-adopts-harmonized-templa]
- 110. Got CER? Educating Pharmacists for Practice in the Future [https://pmc.ncbi.nlm.nih.gov/articles/PMC10397932/]
- 111. The Economics of Comparative Effectiveness Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC4023690/]
- 112. R WE ready for reimbursement? A round-up of ... [https://pubmed.ncbi.nlm.nih.gov/41036833/]
- 113. R WE ready for reimbursement? A round-up of ... [https://pubmed.ncbi.nlm.nih.gov/41100059/]
- 114. The Patient-centered Outcomes Research Institute's Role ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4336314/]
- 115. PCORI Methodology Standards and Report FAQ [https://www.pcori.org/research-related-projects/about-our-research/research-methodology/pcori-methodology-standards-and-report-faq]
- 116. PCORI Methodology Standards [https://www.pcori.org/research-related-projects/about-our-research/research-methodology/pcori-methodology-standards]
- 117. Research - Cycle 3 2025 [https://www.pcori.org/funding-opportunities/announcement/improving-methods-conducting-patient-centered-comparative-clinical-effectiveness-research-pcori-funding-announcement-cycle-3-2025]
- 118. Research - Cycle 2 2025 [https://www.pcori.org/funding-opportunities/announcement/improving-methods-conducting-patient-centered-comparative-clinical-effectiveness-research-pcori-funding-announcement-cycle-2-2025]
- 119. PCORI: Homepage [https://www.pcori.org/]