Bridging the Gap: A Comprehensive Guide to In Vitro-In Vivo Correlation (IVIVC) Methods in Modern Drug Development
This article provides a comprehensive overview of In Vitro-In Vivo Correlation (IVIVC) methodologies, essential for predicting the in vivo performance of drug products based on in vitro data.
Bridging the Gap: A Comprehensive Guide to In Vitro-In Vivo Correlation (IVIVC) Methods in Modern Drug Development
Abstract
This article provides a comprehensive overview of In Vitro-In Vivo Correlation (IVIVC) methodologies, essential for predicting the in vivo performance of drug products based on in vitro data. Tailored for researchers, scientists, and drug development professionals, it explores the fundamental principles and regulatory definitions of IVIVC, delves into advanced methodological applications across diverse dosage forms, addresses common challenges and optimization strategies for complex formulations, and outlines rigorous validation and comparative analysis frameworks. By synthesizing the latest advancements and practical insights, this guide aims to equip professionals with the knowledge to develop robust IVIVC models, thereby accelerating formulation development, reducing regulatory burden, and minimizing the need for extensive clinical studies.
Understanding IVIVC: Core Principles, Regulatory Standards, and Correlation Levels
In Vitro-In Vivo Correlation (IVIVC) is a foundational scientific approach in modern pharmaceutical development, defined by the U.S. Food and Drug Administration (FDA) as "a predictive mathematical model describing the relationship between an in vitro property of a dosage form and a relevant in vivo response" [1]. Typically, the in vitro property represents the rate or extent of drug dissolution or release, while the in vivo response reflects plasma drug concentration or the amount of drug absorbed [1]. This correlation serves as a critical bridge between laboratory measurements and clinical performance, enabling researchers to predict a drug's bioavailability and therapeutic effect based on dissolution data.
The regulatory significance of IVIVC is substantial, as recognized by health authorities worldwide. According to FDA guidance issued in September 1997, which remains the primary regulatory document on this topic, IVIVC provides comprehensive recommendations for developing documentation to support IVIVC for oral extended release (ER) drug products submitted in New Drug Applications (NDAs), Abbreviated New Drug Applications (ANDAs), or Antibiotic Drug Applications (AADAs) [2]. The establishment of a validated IVIVC offers multiple strategic advantages throughout the drug development lifecycle and regulatory review process, including serving as a surrogate for in vivo bioequivalence studies under specific conditions and supporting dissolution specification setting [2].
Levels of IVIVC: A Comparative Analysis
The FDA guidance formally recognizes multiple levels of IVIVC, each differing in complexity, predictive power, and regulatory utility. Understanding these categories is essential for selecting the appropriate correlation strategy for a specific drug development program.
Table: Comparative Analysis of IVIVC Levels
| Aspect | Level A | Level B | Level C |
|---|---|---|---|
| Definition | Point-to-point correlation between in vitro dissolution and in vivo absorption | Statistical correlation using mean in vitro and mean in vivo parameters | Correlation between a single in vitro time point and one PK parameter |
| Predictive Value | High – predicts the full plasma concentration–time profile | Moderate – does not reflect individual PK curves | Low – does not predict the full PK profile |
| Regulatory Acceptance | Most preferred by FDA; supports biowaivers and major formulation changes | Less robust; usually requires additional in vivo data | Least rigorous; not sufficient for biowaivers or major formulation changes |
| Use Case | Requires ≥2 formulations with distinct release rates; supports biowaivers | Compares mean dissolution time with mean residence or absorption time | May support early development insights but requires supplementation for regulatory acceptance |
Table: Regulatory Application and Acceptance of IVIVC Levels
| IVIVC Level | Biowaiver Support | Formulation Change Evaluation | Dissolution Specification Setting |
|---|---|---|---|
| Level A | Full support for major changes | Comprehensive evaluation capability | Primary basis for establishing clinically relevant specifications |
| Level B | Limited support, requires justification | Restricted application | Not typically used for specification setting |
| Level C | Generally not accepted for biowaivers | Limited utility for change evaluation | Insufficient for standalone specification setting |
| Multiple Level C | May support certain changes with validation | Moderate evaluation capability | Can support specification setting with comprehensive data |
Among these levels, Level A IVIVC represents the most precise and valuable category, establishing a point-to-point relationship between the entire in vitro dissolution profile and the entire in vivo absorption profile [3]. This level provides the highest predictive capability for the complete plasma concentration-time profile and is consequently the most preferred by regulatory agencies for supporting biowaivers and justifying formulation changes. Level A correlation typically requires data from at least two formulations with different release rates (e.g., slow, medium, and fast), though a single formulation may be acceptable under specific circumstances [3].
In contrast, Level B IVIVC utilizes statistical moment analysis, comparing the mean in vitro dissolution time to the mean in vivo residence time or mean in vivo absorption time [3] [4]. While this approach provides a useful statistical relationship, it does not reflect the actual shape of individual pharmacokinetic curves, limiting its predictive power and regulatory utility. Consequently, Level B correlations are significantly less common in regulatory submissions and are generally not suitable for establishing quality control specifications.
The Level C IVIVC establishes a single-point relationship, correlating one dissolution time point (e.g., t50%, t90%) with one pharmacokinetic parameter (e.g., Cmax, AUC) [3] [4]. This represents the simplest form of correlation but offers the lowest predictive capability as it does not characterize the complete dissolution profile. While Level C correlations can provide valuable insights during early formulation development, they are insufficient as standalone evidence for regulatory decisions such as biowaivers. A variation known as Multiple Level C correlates multiple dissolution time points with one or more pharmacokinetic parameters, offering improved predictive capability and potentially supporting certain regulatory applications when Level A correlation cannot be achieved.
IVIVC Level Relationships and Data Flow
Experimental Protocols for IVIVC Development
Formulation Design and Development
The development of a robust IVIVC begins with careful formulation design. For a Level A IVIVC, which is most valuable for regulatory applications, a minimum of two formulations with different release rates (typically slow, medium, and fast) should be developed [3]. These formulations should differ meaningfully in their release characteristics to establish a meaningful correlation, typically varying by 10-20% in release rates. It is critical that these formulations maintain the same release mechanism while altering only the release rate through modifications in excipient composition, manufacturing process parameters, or structural characteristics. During this phase, researchers must carefully characterize critical quality attributes (CQAs) of each formulation, including drug content uniformity, particle size distribution, and morphological characteristics, as these factors may significantly influence both in vitro dissolution and in vivo performance.
For generic drug products, the formulation development process must also demonstrate pharmaceutical equivalence to the Reference Listed Drug (RLD) while creating meaningful variations in release rates for IVIVC development [1]. This often requires strategic formulation approaches that alter release characteristics without changing fundamental drug release mechanisms. Common techniques include modifying polymer concentrations in matrix systems, adjusting coating thickness in coated systems, or varying the ratio of immediate-release to extended-release components in multiparticulate systems.
In Vitro Dissolution Testing Methodologies
The selection and validation of appropriate in vitro dissolution methods are fundamental to establishing a meaningful IVIVC. The dissolution testing should employ conditions that discriminate between formulations with different release rates while maintaining biorelevance. According to regulatory standards, dissolution testing for IVIVC development should include a sufficient number of time points to adequately characterize the dissolution profile shape—typically a minimum of 5-6 time points for extended-release formulations [1].
Table: Standard Dissolution Apparatus and Media for Different Formulation Types
| Formulation Type | Apparatus | Dissolution Media | Testing Duration | Key Parameters |
|---|---|---|---|---|
| ER Tablets | USP Apparatus I (Basket) or II (Paddle) | 0.1 N HCl, phosphate buffers (pH 6.8-7.4) | Until ≥80% release | Rotation speed (50-100 rpm), sink conditions |
| ER Capsules (Beads/Pellets) | USP Apparatus I (Basket) or II (Paddle) | Phosphate buffers (pH 6.5-7.5) | Until ≥80% release | Use of glass beads to prevent pellet floating |
| Enteric Coated Tablets | USP Apparatus II (Paddle) | 0.01 N HCl followed by phosphate buffer, pH 6.8 | 2 hours in acid, then buffer until ≥80% release | pH change methodology, enzyme addition |
| Lipid-Based Formulations | USP Apparatus II with lipolysis models | Biorelevant media with surfactants, lipolysis models | Variable based on formulation | Digestion kinetics, bile salt concentration |
For complex formulations such as lipid-based systems, traditional dissolution methods may be insufficient, and more sophisticated approaches are required. For lipid-based formulations (LBFs), additional characterization tools such as lipolysis assays and combined digestion-permeation models may be necessary to capture the complex interplay of digestion, solubilization, and permeation processes that influence in vivo performance [4]. Similarly, for long-acting injectable formulations based on poly(lactide-co-glycolide) (PLGA), flow-through cell apparatus and in vivo-mimicking environments have shown promise in improving prediction accuracy [5] [6].
The dissolution method must be properly validated for specificity, accuracy, precision, and robustness according to regulatory standards. Additionally, the method should demonstrate discriminatory power by detecting meaningful differences in release rates between formulations while maintaining adequate reproducibility.
In Vivo Study Design and Data Collection
The clinical component of IVIVC development requires careful study design and execution. For oral dosage forms, a single-dose, crossover study design in healthy human volunteers is typically employed, with a sufficient washout period between treatments. The study should include frequent blood sampling to adequately characterize the absorption phase, peak concentration, and elimination phase of the plasma concentration-time profile—typically 12-18 time points for extended-release formulations.
Key pharmacokinetic parameters including AUC (area under the curve), Cmax (maximum concentration), and Tmax (time to reach Cmax) should be calculated for each formulation. The in vivo absorption or dissolution profile is then determined through mathematical deconvolution methods, which can be model-dependent (e.g., using Wagner-Nelson or Loo-Riegelman methods) or model-independent (numerical deconvolution) [6]. For IVIVC development, the fraction of drug absorbed is typically used as the in vivo response variable.
When designing in vivo studies for IVIVC, it is essential to consider factors such as food effects, circadian rhythms, and demographic characteristics of the study population that might influence drug absorption. The study should be conducted under well-controlled conditions with appropriate ethical approvals and informed consent procedures.
Model Development and Validation
The core of IVIVC establishment involves developing a mathematical relationship between in vitro dissolution and in vivo absorption data. For Level A correlation, this typically involves comparing the mean fraction dissolved in vitro to the mean fraction absorbed in vivo at corresponding time points. The most common approaches include:
- Time-Scaling Approach: Direct point-to-point correlation after appropriate time scaling
- Convolution-Based Approach: Using numerical deconvolution to estimate in vivo absorption
- Nonlinear Modeling: Applying nonlinear regression models when linear relationships are insufficient
Once a preliminary model is developed, its predictive performance must be rigorously validated. According to regulatory standards, an IVIVC model is considered predictive if the absolute prediction error for Cmax and AUC is ≤10% for each formulation, and the overall average prediction error is ≤15% [3] [1]. Internal validation (using the same data set) or external validation (using an independent data set) approaches may be employed, with external validation being more rigorous and persuasive for regulatory purposes.
For models intended to support biowaivers, validation should demonstrate accurate prediction of in vivo performance for formulations with different release rates within the design space. The model should also be evaluated for robustness through sensitivity analysis, assessing how variations in input parameters affect prediction accuracy.
Applications in Drug Development and Regulatory Submissions
Biowaiver Support and Regulatory Submissions
The application of IVIVC in regulatory submissions provides significant advantages for pharmaceutical sponsors. A validated IVIVC, particularly Level A correlation, can support biowaivers—regulatory exemptions from conducting additional in vivo bioequivalence studies—in several scenarios:
- For post-approval changes: When certain scale-up and post-approval changes (SUPAC) are made to formulation, manufacturing process, equipment, or manufacturing site [1]
- For multiple strengths: When requesting waivers for in vivo BE studies for lower or higher strengths that are not proportionally similar in composition to the bio-batch, provided all strengths are qualitatively the same, have the same release mechanism, and demonstrate similar in vitro dissolution profiles [1]
- For dissolution method and specification justification: When setting clinically relevant dissolution specifications [2]
The utility of IVIVC in regulatory submissions is evidenced by real-world application data. Between January 1996 and December 2014, FDA databases recorded 14 ANDA submissions for generic oral ER drug products containing IVIVC data [1]. These submissions utilized IVIVC for various purposes, including supporting changes in dissolution methods and specifications, level 3 site manufacturing changes, waivers for different strengths, and addressing batch-to-batch variations. However, it is noteworthy that only one ANDA submission included adequate IVIVC information enabling completion of bioequivalence review within the first review cycle, highlighting the challenges in developing regulatory-acceptable IVIVC models [1].
Formulation Optimization and Quality Control
Beyond regulatory applications, IVIVC serves as a powerful tool throughout the drug development lifecycle. During formulation development, IVIVC can guide optimization of critical formulation parameters such as excipient selection, particle size distribution, and coating techniques to ensure consistent bioavailability and desired performance characteristics [3]. By establishing a quantitative relationship between formulation variables and in vivo performance, IVIVC enables more efficient and targeted formulation development.
In the context of quality control, IVIVC provides a scientific basis for establishing clinically relevant dissolution specifications. Rather than setting specifications based solely on batch-to-batch consistency, IVIVC allows manufacturers to define dissolution limits that ensure bioequivalence across batches [1]. This approach enhances product quality and consistency while potentially reducing regulatory burdens through justification of wider specification ranges when supported by IVIVC data.
The integration of IVIVC with Quality by Design (QbD) principles further strengthens pharmaceutical development by linking critical quality attributes to clinical performance [3]. This systematic approach to development emphasizes understanding and control based on sound science and quality risk management, with IVIVC serving as a key tool for establishing clinically relevant specifications and design spaces.
Advanced Applications and Special Cases
IVIVC for Complex Dosage Forms
The application of IVIVC principles extends beyond conventional oral extended-release formulations to more complex drug delivery systems. For lipid-based formulations (LBFs), which are crucial for enhancing oral bioavailability of poorly water-soluble drugs, IVIVC development presents unique challenges due to complex processes involving digestion, solubilization, and permeation [4]. Traditional dissolution tests often fail to adequately predict in vivo performance for LBFs, necessitating more sophisticated in vitro models such as lipolysis assays and biorelevant media that better simulate gastrointestinal conditions.
For long-acting injectable (LAI) formulations, particularly those based on biodegradable polymers like poly(lactide-co-glycolide) or PLGA, IVIVC development is complicated by extended release durations (weeks to months) and complex release mechanisms involving polymer erosion and degradation [6]. The small number of FDA-approved LAI formulations (only 25 compared with thousands of oral extended-release formulations) reflects the difficulties in LAI development and characterization [6]. Recent advances in in vitro release testing methods, including flow-through apparatus and in vivo-mimicking environments, show promise for improving IVIVC for these challenging delivery systems [5].
Emerging Technologies and Future Perspectives
The field of IVIVC continues to evolve with advancements in analytical technologies and computational methods. The integration of physiologically based pharmacokinetic (PBPK) modeling with IVIVC represents a promising approach for enhancing predictive capability, particularly for complex formulations [4] [7]. PBPK models incorporate physiological parameters such as organ perfusion rates, tissue distribution kinetics, and metabolic pathways to create more comprehensive and physiologically realistic simulations of drug behavior in humans.
Similarly, the application of artificial intelligence (AI) and machine learning approaches to IVIVC enables analysis of complex datasets to identify patterns and improve prediction accuracy [3]. These technologies can help overcome traditional limitations in IVIVC development by handling multidimensional data and nonlinear relationships that challenge conventional mathematical approaches.
Looking ahead, the convergence of advanced technologies such as microfluidics, organ-on-a-chip systems, and high-throughput screening assays holds immense potential for augmenting the predictive power and scope of IVIVC studies [3]. These technologies enable more sophisticated and biorelevant in vitro testing environments that better capture the complexity of in vivo conditions. Furthermore, the pharmaceutical industry is moving toward more personalized approaches to drug therapy, and IVIVC methodologies are expected to evolve to support the development of tailored formulations with optimized performance for specific patient populations.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Research Reagent Solutions for IVIVC Development
| Reagent/Material | Function in IVIVC Development | Application Examples | Critical Considerations |
|---|---|---|---|
| Biorelevant Dissolution Media | Simulates gastrointestinal fluids to enhance predictive capability | Fasted State Simulated Intestinal Fluid (FaSSIF), Fed State Simulated Intestinal Fluid (FeSSIF) | Buffer capacity, surfactant composition, osmolarity matching physiological conditions |
| USP Dissolution Apparatus | Standardized equipment for in vitro release testing | USP Apparatus I (Basket), II (Paddle), IV (Flow-Through Cell) | Calibration, validation, mechanical specification compliance |
| Lipolysis Assay Components | Models lipid digestion processes for LBFs | Calcium chloride, taurocholate salts, pancreatic extracts | pH-stat control, titration calibration, enzyme activity standardization |
| PLGA Polymers | Biodegradable polymer for long-acting injectables | Various lactide:glycolide ratios, end-group modifications, molecular weights | Characterization of molecular weight, polydispersity, crystallinity |
| Permeability Enhancement Excipients | Improves drug absorption for BCS Class II/IV compounds | Surfactants, permeability enhancers, absorption modifiers | Cytotoxicity assessment, compatibility with absorption pathways |
| Deconvolution Software | Mathematical calculation of in vivo absorption profiles | Wagner-Nelson, Loo-Riegelman, numerical deconvolution methods | Algorithm validation, statistical weighting, model selection criteria |
| PBPK Modeling Platforms | Integrates physiological parameters with formulation performance | GastroPlus, Simcyp, PK-Sim | Population library adequacy, system parameter verification |
In vitro-in vivo correlation represents a powerful methodology that bridges pharmaceutical development and clinical performance, enabling more efficient and scientifically rigorous drug development. The regulatory framework established by FDA guidance, though primarily focused on oral extended-release dosage forms, provides a solid foundation for IVIVC development across various dosage forms and application scenarios. The different levels of IVIVC—A, B, and C—offer varying degrees of predictive capability and regulatory utility, with Level A providing the most comprehensive correlation for supporting critical development and regulatory decisions.
The successful development and application of IVIVC requires careful attention to formulation design, analytical method development, clinical study execution, and mathematical modeling. While challenges remain, particularly for complex dosage forms such as lipid-based systems and long-acting injectables, advances in biorelevant dissolution testing, computational modeling, and emerging technologies continue to expand the applications and predictive power of IVIVC approaches. As pharmaceutical sciences evolve toward more targeted and personalized therapies, IVIVC methodologies will continue to play an essential role in ensuring that in vitro performance reliably predicts in vivo behavior, ultimately supporting the development of safe, effective, and consistent drug products for patients.
In vitro-in vivo correlation (IVIVC) is defined by the U.S. Food and Drug Administration (FDA) as "a predictive mathematical model describing the relationship between an in vitro property of a dosage form and a relevant in vivo response" [8] [9]. In practice, the in vitro property is typically the rate or extent of drug dissolution or release, while the in vivo response is generally the plasma drug concentration or amount of drug absorbed [8] [4]. Since the FDA published its regulatory guidance on IVIVC for extended release (ER) oral dosage forms in 1997, the establishment and application of IVIVC has gained significant importance in the field of pharmaceutics [8].
A well-validated IVIVC model serves as a powerful tool in pharmaceutical development and regulation. Its primary advantage lies in its ability to predict in vivo performance based on in vitro dissolution data, which can reduce the need for costly and time-consuming bioequivalence studies involving human subjects [3] [10]. Furthermore, IVIVC enhances the understanding of a drug product's characteristics, facilitates the establishment of clinically relevant dissolution specifications, and supports regulatory decisions for both New Drug Applications (NDAs) and Abbreviated New Drug Applications (ANDAs) [3] [10].
The IVIVC Hierarchy: Levels and Classifications
The IVIVC hierarchy is categorized into different levels based on the degree of correlation and predictive power. The U.S. FDA guidance recognizes several levels of correlation, with Level A representing the most informative category and Level D being the least informative [8]. The following sections provide a detailed examination of each correlation level.
Level A IVIVC: The Gold Standard
Level A IVIVC represents a point-to-point relationship between the in vitro dissolution rate and the in vivo input rate (e.g., the rate of drug absorption) [8] [3] [10]. It is considered the most informative and robust level of correlation and is the only type that can support a biowaiver (a regulatory waiver for in vivo bioequivalence studies) for certain post-approval changes [8] [3].
- Predictive Power: High; capable of predicting the entire plasma concentration-time profile [3].
- Regulatory Acceptance: Most preferred by regulatory agencies for supporting biowaivers for major formulation and manufacturing changes [3] [10].
- Development Requirements: Typically requires data from at least two or three formulations with different release rates (e.g., slow, medium, and fast) [8] [3].
The mathematical foundation of a Level A correlation often involves a two-step process employing deconvolution techniques to estimate the in vivo absorption time course, which is then directly compared to the in vitro dissolution profile [8] [10]. The relationship is generally linear, though non-linear correlations are also acceptable [8].
Level B IVIVC: Statistical Moments Analysis
Level B IVIVC utilizes the principles of statistical moment analysis. It compares the mean in vitro dissolution time (MDTin vitro) to either the mean in vivo residence time (MRTin vivo) or the mean in vivo dissolution time (MDTin vivo) [8] [10].
- Predictive Power: Moderate; does not reflect the actual shape of the plasma concentration-time curve [8] [3].
- Regulatory Acceptance: Less robust; generally not suitable for setting quality control specifications or for obtaining biowaivers [3].
- Key Limitation: While it uses all available in vitro and in vivo data, it is not a point-to-point correlation. Different in vivo profiles can result in the same mean time values, thus limiting its predictive capability [8].
Level C and Multiple Level C IVIVC: Single-Point and Multi-Point Relationships
Level C IVIVC establishes a single-point relationship, correlating one dissolution parameter (e.g., t50%, the time for 50% of the drug to dissolve) with one pharmacokinetic parameter (e.g., Cmax, AUC) [8] [3].
- Predictive Power: Low; does not represent the complete shape of the plasma profile, which is critical for characterizing the in vivo performance of extended-release products [8].
- Utility: Primarily useful in the early stages of formulation development for screening pilot formulations [8] [3].
Multiple Level C IVIVC extends this concept by relating the amount of drug dissolved at several time points to one or more pharmacokinetic parameters [8]. It requires dissolution data from at least three time points covering the early, middle, and late stages of the dissolution profile [8].
- Predictive Power: Can be as useful as a Level A correlation if it effectively captures the entire dissolution profile [8].
- Regulatory Context: If a Multiple Level C correlation is achievable, then developing a Level A correlation is usually feasible and preferred [8].
Level D IVIVC: Qualitative Ranking
Level D IVIVC is a qualitative or rank-order correlation and is not considered a true correlation for regulatory purposes. It is not mentioned in the FDA IVIVC Guidance and serves only as a tool for early formulation development with no regulatory value [8] [4].
Comparative Analysis of IVIVC Levels
The table below provides a consolidated comparison of the key characteristics of Levels A, B, C, and Multiple Level C IVIVC.
Table 1: Comprehensive Comparison of IVIVC Levels
| Aspect | Level A | Level B | Level C | Multiple Level C |
|---|---|---|---|---|
| Definition | Point-to-point correlation between in vitro dissolution and in vivo absorption [8] [3]. | Correlation of mean in vitro dissolution time to mean in vivo residence or dissolution time [8]. | Single-point relationship between a dissolution parameter (e.g., t50%) and a PK parameter (e.g., Cmax, AUC) [8]. | Relationship between dissolution at several time points and one or more PK parameters [8]. |
| Predictive Value | High: Predicts the full plasma concentration-time profile [3]. | Moderate: Does not reflect the actual in vivo curve shape [8]. | Low: Cannot predict the full PK profile [8] [3]. | Moderate to High: If it captures the entire profile, can be as useful as Level A [8]. |
| Data Used | All data points from dissolution and absorption profiles [8]. | All data, but condensed into mean parameters [8]. | Single dissolution time point and a single PK parameter [8]. | Multiple dissolution time points and PK parameters [8]. |
| Regulatory Acceptance | Gold standard; can support biowaivers [8] [3]. | Limited; usually requires additional in vivo data [3]. | Low; not sufficient for biowaivers [3]. | May support biowaivers if it correlates all critical time points [8] [10]. |
| Primary Use Case | Surrogate for bioequivalence studies; setting dissolution specifications [3] [10]. | Formulation development tool [3]. | Early development screening [8] [3]. | Justifying dissolution specifications; early development [8] [10]. |
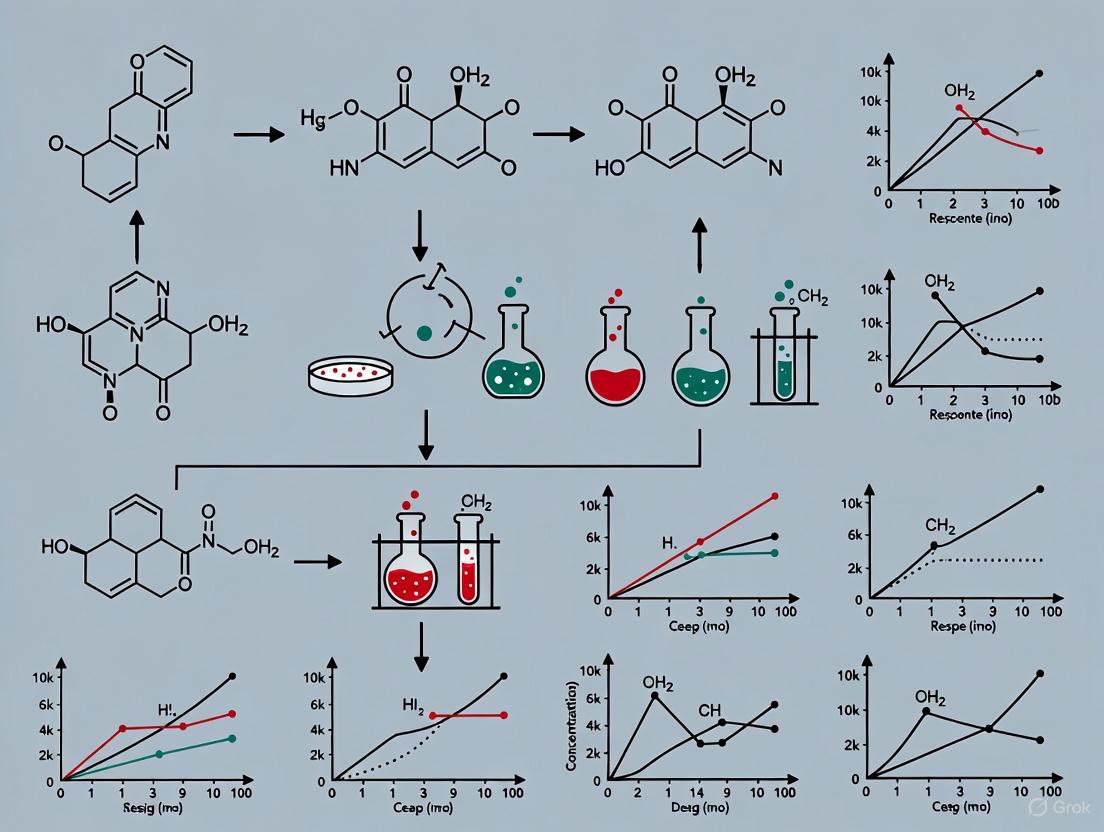
Figure 1: The IVIVC Hierarchy - This diagram illustrates the hierarchy of IVIVC levels, with Level A representing the highest predictive power and regulatory acceptance, descending to Level D, which is qualitative and has no regulatory value.
Methodological Workflow for IVIVC Development
Developing a robust IVIVC, particularly a Level A correlation, requires a systematic and multi-stage approach. The process involves mathematical manipulation to construct a functional relationship between in vitro dissolution (input) and in vivo dissolution or absorption (output) [9].
Key Experimental Protocols
The following workflow outlines the primary steps for establishing a Level A IVIVC, which is the most common type used in regulatory submissions [8] [10]:
- Formulation Selection: Develop and select at least two or three formulations with different release rates (e.g., slow, medium, and fast). The in vitro dissolution profiles should differ meaningfully, ideally by at least 10% at various time points [8] [10].
- In Vivo Data Generation: Obtain in vivo plasma concentration-time profiles for the selected formulations through clinical studies. An immediate-release (IR) formulation or an intravenous (IV) dose is often used as a reference [8] [10].
- Deconvolution Analysis: Estimate the in vivo absorption or dissolution time course from the plasma concentration data. This can be achieved using:
- Correlation Model Establishment: Plot the fraction of drug absorbed in vivo (obtained from deconvolution) against the fraction of drug dissolved in vitro for each formulation. Establish a mathematical relationship, which can be linear or non-linear (e.g., Sigmoid, Weibull, Higuchi) [8].
- Model Validation: Evaluate the predictability of the developed IVIVC model. This involves:
- Internal Validation: Using the data from which the model was built. The prediction error (%PE) for pharmacokinetic parameters (Cmax and AUC) should be ≤10% on average to be considered acceptable [8] [10].
- External Validation: Predicting the in vivo performance of a new formulation not used in building the model [8].
Figure 2: Level A IVIVC Development Workflow - This diagram outlines the key experimental and mathematical steps involved in establishing a predictive Level A IVIVC model.
Critical Considerations and Potential Pitfalls
Successful IVIVC development requires careful consideration of several factors to avoid common traps:
- Use of Mean vs. Individual Data: Averaging in vivo plasma profiles can obscure individual variability, especially if there are significant differences in lag time (Tlag) or time to maximum concentration (Tmax) between subjects. IVIVC is discouraged for highly variable drugs as the inherent variability can mask formulation-dependent differences [11].
- Time Scaling and Lag Time Correction: Disparities between the timescales of in vitro and in vivo release may require the use of time-scaling factors to align the profiles for correlation development [8] [11].
- Flip-Flop Kinetics: In cases where the absorption rate is slower than the elimination rate (flip-flop kinetics), the apparent in vivo release profile estimated by deconvolution may be misleading if not properly accounted for [11].
- Biopharmaceutical and Physiological Factors: Drug properties such as solubility, permeability, and pKa, as well as physiological conditions like gastrointestinal pH and transit time, must be considered as they fundamentally influence both dissolution and absorption [9].
The Scientist's Toolkit: Essential Reagents and Methods
Table 2: Key Research Reagents and Solutions for IVIVC Studies
| Item / Method | Function in IVIVC Development |
|---|---|
| USP Apparatus I/II/III/IV | Standardized dissolution equipment to simulate various drug release conditions under controlled agitation and temperature [12]. |
| Biorelevant Media | Dissolution media (e.g., FaSSIF, FeSSIF) designed to mimic the composition, pH, and surface tension of human gastrointestinal fluids, improving the biopredictiveness of in vitro tests [4] [12]. |
| pH-Stat Titration | A technique used particularly for lipid-based formulations to monitor and control pH during in vitro lipolysis assays, simulating the digestion process in the gut [4]. |
| Deconvolution Software | Computational tools (e.g., Phoenix WinNonlin) for performing model-dependent or numerical deconvolution to estimate the in vivo input rate from plasma concentration data [8] [11]. |
| PBPK Modeling Software | Physiologically Based Pharmacokinetic modeling platforms used to integrate in vitro dissolution data with physiological parameters for more accurate prediction of in vivo performance [3] [12]. |
The hierarchy of IVIVC provides a structured framework for correlating in vitro drug product performance with in vivo outcomes. Level A IVIVC stands as the most robust and regulatory-friendly correlation, offering a point-to-point predictive model that can reduce the need for additional clinical studies. While Level B and Level C correlations offer utility in early formulation development, their predictive power and regulatory acceptance are limited. The development of a successful IVIVC demands a meticulous methodological approach, accounting for formulation characteristics, physiological variables, and potential analytical pitfalls. As pharmaceutical scientists continue to face challenges with complex drug products, such as non-oral dosage forms and lipid-based systems, the principles of IVIVC remain a cornerstone of efficient, predictive, and patient-centric drug development [8] [4] [3].
In Vitro-In Vivo Correlation (IVIVC) is a predictive mathematical model describing the relationship between an in vitro property of a dosage form (typically the rate or extent of drug dissolution or release) and a relevant in vivo response (such as plasma drug concentration or amount of drug absorbed). [3] The establishment of a robust IVIVC plays a pivotal role in modern drug development by enhancing the understanding of dosage form performance, supporting regulatory submissions, and potentially reducing the need for certain clinical bioequivalence studies. [3] For researchers and drug development professionals, a successful IVIVC can expedite product development, optimize formulations, and establish clinically relevant dissolution specifications. However, the path to a successful IVIVC is governed by a complex interplay of physicochemical, biopharmaceutical, and physiological factors. Understanding and controlling these factors is critical, especially for complex drug products like nanomedicines and lipid-based formulations, where traditional correlation models often fall short. [13] [4] This guide provides a comparative analysis of these critical factors and the experimental protocols used to navigate them.
Comparative Analysis of Critical IVIVC Factors
The success of developing a predictive IVIVC model is highly dependent on a triad of factors related to the drug, the formulation, and the biological system. The table below summarizes these critical factors and their impact on IVIVC for different formulation types.
Table 1: Critical Factors Governing IVIVC Success Across Formulation Types
| Factor Category | Specific Factor | Impact on IVIVC | Considerations for Conventional Oral Dosage Forms | Considerations for Complex Formulations (e.g., Nanomedicines, Lipid-Based Formulations) |
|---|---|---|---|---|
| Physicochemical Properties | Drug Solubility & Permeability | Determines absorption mechanism and dissolution limitation. BCS Class II & IV drugs are more challenging. [4] | BCS Class I & III drugs often have more straightforward correlations. | For LBFs, dynamic solubilization supersedes equilibrium solubility. For nanomedicines, surface properties can alter permeability. [13] [4] |
| Particle Size & Crystalline Form | Directly influences dissolution rate. | Critical for immediate-release formulations of poorly soluble drugs. | For ASDs, maintaining the amorphous form is crucial to prevent precipitation and altered performance. [14] | |
| Biopharmaceutical & Formulation Factors | Formulation Design & Release Mechanism | Dictates the drug release profile, which must be mirrored by the in vitro method. [3] | Well-established for standard extended-release (ER) systems. | Highly complex for LBFs (digestion, micellization) and nanomedicines (nanoparticle-specific absorption pathways). Standard dissolution tests are often inadequate. [13] [4] |
| In Vitro Dissolution Method | Must be biorelevant and discriminate formulation changes. [14] | USP apparatus with standard buffers is often sufficient. | Requires sophisticated models (e.g., biphasic, lipolysis) to simulate GI environment. Method must be tailored to formulation. [14] [4] | |
| Physiological & Patient Factors | Gastrointestinal pH & Motility | Affects drug dissolution, solubility, and residence time. [4] | Can be simulated with pH-shift dissolution methods. | A major source of variability. Lipid digestion is pH-dependent and affects LBF performance. [4] |
| Variability in Anatomy & Physiology | Causes inter-subject variability in vivo that is hard to capture in vitro. [13] [4] | Population-based averages are typically used. | A significant hurdle for nanomedicines, leading to "highly deviating in-vitro and in-vivo data." [13] | |
| Food Effects (Fed/Fasted State) | Alters GI physiology, profoundly impacting solubility and absorption. | Commonly assessed in bioavailability studies. | Particularly critical for LBFs, as food intake stimulates bile secretion and lipid digestion, drastically altering formulation performance. [4] |
Experimental Protocols for Robust IVIVC Development
Level A IVIVC Development for Amorphous Solid Dispersions
A 2025 study on itraconazole immediate-release (IR) tablets provides a robust protocol for establishing a Level A IVIVC for a spray-dried solid dispersion (SDD) of a BCS Class II drug. [14]
- Objective: To develop an FDA level A IVIVC that predicts in vivo pharmacokinetic (PK) performance from in vitro dissolution for itraconazole SDD tablets, assessing the impact of polymer grade, disintegrant level, and dry granulation processing. [14]
- Formulation Design: Three tablet formulations with distinct release rates were developed: Fast-, Medium-, and Slow-release. This is a regulatory requirement for Level A IVIVC, as per FDA guidance. [14] [3]
- In Vitro Methodology:
- Apparatus: USP dissolution apparatus.
- Media: Simulated intestinal fluid (phosphate buffer, pH 6.4).
- Key Modification: To better mimic in vivo conditions, tablets were triturated into particles prior to immersion to attenuate disintegration differences observed between the Medium and Slow formulations in vivo. [14]
- In Vivo Study: A human pharmacokinetic study was conducted, comparing the test tablets against an oral solution used to define post-dissolution disposition. [14]
- IVIVC Modeling: A direct, differential-equation-based IVIVC model approach was employed. The model established a point-to-point correlation between the in vitro dissolution profile and the in vivo absorption profile. [14]
- Validation: The model met the FDA's internal predictability requirements for a Level A IVIVC, demonstrating its ability to accurately predict in vivo performance based on in vitro data. [14]
IVIVC Challenges and Protocols for Lipid-Based Formulations
Developing IVIVC for Lipid-based Formulations (LBFs) is particularly challenging due to their complex digestion and solubilization processes. The following protocol outlines a modern approach.
- Objective: To construct a predictive IVIVC for LBFs, which must account for dynamic processes like lipid digestion, micelle formation, and potential lymphatic transport, not captured by traditional tests. [4]
- In Vitro Toolbox:
- USP Dissolution: Often insufficient alone but used as a initial test.
- Lipolysis Assays: The primary tool for LBFs. This pH-stat model simulates the enzymatic digestion of lipids in the GI tract, measuring the rate of drug precipitation or incorporation into colloidal structures. [4]
- Combined Dissolution/Permeation Models: Biphasic systems (aqueous and organic solvent) or those incorporating membranes (e.g., PAMPA) can simultaneously assess drug release and partitioning, which is more biorelevant for absorption prediction. [4]
- In Silico Integration: Given the limitations of in vitro models, Physiologically Based Pharmacokinetic (PBPK) modeling is increasingly integrated. PBPK models can incorporate data from lipolysis assays to simulate and predict human PK, helping to bridge the in vitro-in vivo gap. [4]
- Validation: Correlating in vitro lipolysis parameters (e.g., extent of precipitation) with in vivo pharmacokinetic parameters (AUC, C~max~) from animal or human studies. Success is mixed, with case studies on drugs like fenofibrate and cinnarizine showing only qualitative (Level D) or failed correlations, highlighting the need for model refinement. [4]
The workflow below illustrates the integrated experimental and modeling approach required for developing IVIVC for complex formulations.
Diagram 1: Integrated IVIVC Development Workflow for Complex Formulations
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key reagents, materials, and instruments critical for executing the experimental protocols described in this guide.
Table 2: Essential Research Reagent Solutions for IVIVC Studies
| Item Name | Function/Application in IVIVC | Example from Literature |
|---|---|---|
| Spray-Dried Dispersion (SDD) | Enhances solubility and dissolution rate of poorly soluble drugs by creating an amorphous form. | Itraconazole SDD using polymers like HPMCAS was central to developing a Level A IVIVC. [14] |
| Lipid Excipients (Oils, Surfactants) | Core components of Lipid-Based Formulations (LBFs); solubilize drugs and promote absorption via digestion. | Classified into Types I-IV (e.g., triglycerides, mixed glycerides, surfactants). Critical for formulating SEDDS/SMEDDS. [4] |
| Biorelevant Dissolution Media | Simulate the composition, pH, and surface tension of human gastrointestinal fluids for predictive in vitro release. | Use of USP simulated intestinal fluid (phosphate buffer, pH 6.4) for itraconazole tablets. [14] Lipolysis assays use media containing bile salts and phospholipids. [4] |
| pH-Stat Titrator | Essential apparatus for in vitro lipolysis assays; monitors and maintains pH by titrating NaOH, quantifying fatty acids released from lipid digestion. | Used to evaluate the dynamic digestion of LBFs and its impact on drug precipitation. [4] |
| PBPK Modeling Software | In-silico platform that integrates physiological, drug, and formulation data to simulate and predict human pharmacokinetics. | Used to model subcutaneous injectables and inform IVIVC for complex delivery systems. [7] |
Establishing a successful IVIVC is a cornerstone of efficient and scientifically rigorous drug development. The journey is governed by a critical triad of factors: the physicochemical properties of the API, the biopharmaceutical design of the formulation, and the inherent physiological variability of the patient population. As demonstrated, the strategies and experimental protocols must be tailored to the formulation's complexity. While Level A IVIVC is achievable for solid dispersions with careful biorelevant method design, lipid-based formulations and nanomedicines present greater challenges, necessitating advanced in vitro tools like lipolysis assays and their integration with PBPK modeling. The absence of specific regulatory guidelines for novel nanomedicines further underscores the need for continued research and collaboration between industry and regulators. [13] For scientists, mastering these factors and leveraging the available toolkit is essential for bridging the gap between in vitro performance and in vivo efficacy, ultimately accelerating the delivery of robust and effective drug products to patients.
The Role of the Biopharmaceutics Classification System (BCS) in IVIVC Development
The Biopharmaceutics Classification System (BCS) serves as a fundamental scientific framework for streamlining drug development by categorizing active pharmaceutical ingredients based on their aqueous solubility and intestinal permeability [15]. This classification provides a rational basis for predicting drug absorption and establishing in vitro-in vivo correlations (IVIVC), which are mathematical models relating the rate and extent of drug dissolution to its absorption profile in humans [16]. For regulatory bodies, the BCS guides decisions on biowaivers—approvals that exempt certain drug products from costly and time-consuming bioequivalence studies, particularly for BCS Class I and III compounds [17]. As the pharmaceutical industry faces increasing challenges with poorly soluble compounds, the strategic integration of BCS with IVIVC modeling has become indispensable for developing predictive dissolution methods, optimizing formulations, and ensuring product quality throughout the product lifecycle [12] [18].
The following sections explore how BCS classification directs IVIVC development strategies across different drug classes, with specific experimental case studies and methodological considerations for establishing robust correlations.
BCS Classification and Its Direct Impact on IVIVC Strategy
The BCS categorizes drug substances into four classes based on two key parameters: solubility, determined by the highest dose strength soluble in ≤250 mL of aqueous media across pH 1-7.5, and permeability, based on the extent of absorption ≥90% in humans [15] [18]. These properties directly influence the feasibility and approach for developing IVIVCs.
Table 1: BCS Classification and Corresponding IVIVC Considerations
| BCS Class | Solubility | Permeability | Rate-Limiting Step for Absorption | IVIVC Feasibility & Approach |
|---|---|---|---|---|
| Class I | High | High | Gastric emptying | Generally not necessary for biowaivers; IVIVC may be useful for modified-release formulations |
| Class II | Low | High | Dissolution rate | Excellent candidates for IVIVC; focus on developing biorelevant dissolution methods |
| Class III | High | Low | Permeability rate | Challenging; permeation-limited absorption reduces correlation with dissolution |
| Class IV | Low | Low | Complex (both dissolution and permeability) | Most difficult; requires advanced formulation technologies |
For BCS Class II drugs, which exhibit dissolution rate-limited absorption, IVIVC is particularly advantageous [15]. The low solubility of these compounds means that in vivo dissolution becomes the slowest step in the absorption process, creating a direct mechanistic link between in vitro dissolution profiles and in vivo performance that can be quantitatively modeled [12]. This relationship enables formulators to use dissolution testing as a surrogate for bioequivalence studies, significantly accelerating development timelines for both new drug products and generics [19].
Experimental Approaches for Establishing IVIVC Across BCS Classes
Case Study: BCS Class II Drug – Lamotrigine Extended-Release Tablets
A recent study with lamotrigine, a BCS Class IIb weak base with pH-dependent solubility, demonstrated a systematic approach to IVIVC development for an extended-release formulation [12]. Researchers employed a Quality by Design (QbD) framework to establish patient-centric quality standards through these key experimental steps:
- Dissolution Method Development: Multiple dissolution apparatus (USP II and USP III) with both biorelevant media (fasted-state simulated intestinal fluid) and standard compendial media were evaluated to identify the most biopredictive conditions [12].
- In Vivo Data Collection: Clinical pharmacokinetic data were obtained from reference formulations to establish the in vivo absorption profile [12].
- IVIVC Model Building: A Level A correlation was developed by comparing in vitro dissolution data with in vivo absorption profiles derived through deconvolution [12].
- Predictability Validation: The IVIVC model was validated using internal and external validation sets, demonstrating its predictive capability for new formulations [12].
- PBPK Modeling Integration: A physiologically based pharmacokinetic (PBPK) model combined with the validated IVIVC established clinically relevant dissolution specifications that accounted for inter-individual variability in patient physiology [12].
This integrated approach successfully established a predictive IVIVC that could support biowaiver considerations for post-approval changes and ensure consistent product quality without additional clinical studies [12].
Case Study: BCS Class II Drug – Bicalutamide Immediate-Release Tablets
For the poorly soluble BCS Class II drug bicalutamide, researchers employed a biphasic dissolution system to establish a predictive Level A IVIVC [19]. This innovative methodology addressed the limitations of traditional compendial methods:
- Apparatus: USP Apparatus II (paddle) modified with an organic phase [19]
- Aqueous Phase: 300 mL of pH 6.8 phosphate buffer [19]
- Organic Phase: 200 mL of 1-octanol (pre-saturated with buffer) [19]
- Sampling: Simultaneous collection from both phases at predetermined time points [19]
- Analytical: UV spectrophotometry at 272 nm (octanol) and 273 nm (buffer) [19]
The biphasic system provided an excellent correlation (r² = 0.98) between in vitro partitioning and in vivo absorption data [19]. By simultaneously measuring dissolution and partitioning, this method better simulated the in vivo absorption process, where drug molecules must first dissolve in gastrointestinal fluids before partitioning through the intestinal membrane. The resulting IVIVC successfully predicted the pharmacokinetic parameters of a generic product compared to the reference product, with AUC and Cmax ratios of 1.04 ± 0.01 and 0.951 ± 0.026, respectively, demonstrating its utility in generic product development [19].
Figure 1: Systematic Workflow for IVIVC Development of BCS Class II Drugs. This diagram illustrates the integrated in vitro and in vivo approach required to establish predictive IVIVC models, from initial method development through validation and regulatory applications.
Special Considerations: Advanced Formulations and Correlation Levels
For complex drug delivery systems such as lipid-based formulations (LBFs), establishing IVIVC presents additional challenges. LBFs, which are particularly valuable for enhancing the bioavailability of BCS Class II and IV drugs, involve dynamic processes including digestion, solubilization, and potential lymphatic transport that are not captured by traditional dissolution methods [4] [20]. The predictability of conventional in vitro tests for LBFs has been questionable, with studies showing that only approximately 50% of drugs tested using pH-stat lipolysis models correlated well with in vivo data [20].
Different levels of IVIVC provide varying degrees of predictive power and regulatory utility [4] [20]:
- Level A: Point-to-point correlation between in vitro dissolution and in vivo input rate (most informative, regulatory preferred)
- Level B: Comparison of mean in vitro dissolution time and mean in vivo residence time
- Level C: Single point relationship (e.g., dissolution at one time point vs. AUC or Cmax)
- Multiple Level C: Relationships at several dissolution time points
- Level D: Qualitative ranking (lowest predictive value)
Table 2: Experimental Conditions for IVIVC Development from Case Studies
| Drug Product | BCS Class | Dissolution Apparatus | Dissolution Media | Analytical Method | Correlation Level |
|---|---|---|---|---|---|
| Lamotrigine ER Tablets [12] | IIb | USP II (paddle) and USP III | Biorelevant (FaSSIF) and compendial buffers | HPLC | Level A |
| Bicalutamide IR Tablets [19] | II | Modified USP II with biphasic system | pH 6.8 phosphate buffer + 1-octanol | UV Spectrophotometry | Level A |
| Mesalazine Enteric-Coated Tablets [21] | Not specified | Reciprocating cylinder (USP Apparatus III) | pH progression (1.2, 4.5, 5.5, 6.0, 6.8) | UV Spectrophotometry | Not specified |
Essential Research Reagents and Materials for IVIVC Studies
The experimental protocols for establishing IVIVC require specific reagents, apparatus, and analytical tools. The following table summarizes key research solutions and their applications in IVIVC development based on the case studies examined:
Table 3: Essential Research Reagents and Materials for IVIVC Development
| Reagent/Material | Function in IVIVC Studies | Specific Examples from Literature |
|---|---|---|
| Biorelevant Dissolution Media | Simulates gastrointestinal environment for predictive dissolution testing | Fasted State Simulated Intestinal Fluid (FaSSIF) [12] |
| Biphasic Dissolution Systems | Simultaneously measures dissolution and partitioning kinetics | 1-octanol organic phase with aqueous buffer [19] |
| USP Dissolution Apparatus | Standardized equipment for dissolution testing | USP Apparatus II (paddle), USP III (reciprocating cylinder) [12] [21] |
| Chromatographic Reference Standards | Quantitative analysis of drug concentration | Lamotrigine USP reference standard [12] |
| Surfactants for Sink Conditions | Maintains sink conditions for poorly soluble drugs | Sodium lauryl sulfate (SLS) in dissolution media [19] |
| pH Adjustment Reagents | Modifies dissolution media to simulate GI pH progression | Hydrochloric acid, sodium hydroxide, buffer salts [21] |
The Biopharmaceutics Classification System provides an essential framework for guiding IVIVC development, with BCS Class II drugs representing the most suitable candidates due to their dissolution rate-limited absorption. The integration of biopredictive dissolution methods with physiologically-based modeling enables the establishment of robust IVIVCs that can support regulatory decisions, including biowaivers for scale-up and post-approval changes. As pharmaceutical development increasingly focuses on poorly soluble compounds, the strategic application of BCS-based IVIVC approaches will continue to play a vital role in optimizing drug product quality while reducing the need for extensive clinical studies. Future directions include the development of more sophisticated in vitro models that better capture complex in vivo processes, particularly for advanced drug delivery systems such as lipid-based formulations and nanomedicines.
Advanced IVIVC Modeling Techniques and Applications Across Dosage Forms
In the realm of pharmaceutical development, In Vitro-In Vivo Correlation (IVIVC) represents a critical predictive mathematical model that establishes a relationship between a biological property derived from a dosage form and a physicochemical property of the same formulation [16]. Specifically, a Level A IVIVC is the most stringent and informative category, providing a point-to-point correlation between the in vitro dissolution rate and the in vivo input rate of the drug product [4] [22]. This level of correlation is considered the gold standard for regulatory purposes as it allows for the prediction of in vivo bioavailability based on in vitro dissolution data, thereby reducing the need for extensive and costly human studies [14] [22].
The establishment of a Level A IVIVC is particularly valuable for supporting biowaivers, setting clinically relevant dissolution specifications, and optimizing formulations during development [4]. For poorly soluble drugs, including those formulated as lipid-based formulations (LBFs) and amorphous solid dispersions (ASDs), developing a robust Level A IVIVC presents unique challenges but offers significant rewards in predicting in vivo performance [4] [14]. This guide provides a comprehensive, step-by-step methodology for establishing a Level A IVIVC, from initial deconvolution techniques to final model building and validation.
Fundamental Concepts and Regulatory Framework
Understanding IVIVC Levels
The United States Pharmacopeia (USP) defines IVIVC as "the establishment of a rational relationship between a biological property, or a parameter derived from a biological property, produced by a dosage form and a physicochemical property or characteristic of the same dosage form" [4]. The U.S. Food and Drug Administration (FDA) further clarifies IVIVC as "a predictive mathematical model describing the relationship between an in vitro property of a dosage form and a relevant in vivo response" [4]. Different levels of IVIVC provide varying degrees of predictive power and regulatory acceptance:
- Level A: Represents a point-to-point correlation between in vitro dissolution and in vivo absorption rate, representing the most predictive model that can serve as a surrogate for bioequivalence studies [4] [22].
- Level B: Utilizes the principles of statistical moment analysis, comparing mean in vitro dissolution time to mean in vivo residence time or mean in vitro dissolution time to mean in vivo dissolution time [4].
- Level C: Establishes a single-point relationship between a dissolution parameter (e.g., t50%) and a pharmacokinetic parameter (e.g., AUC or Cmax) [4].
- Multiple Level C: Expands Level C correlation to multiple time points and pharmacokinetic parameters, offering improved predictability over single-point correlations [4].
Regulatory Significance and Applications
Regulatory agencies including the FDA and European Medicines Agency (EMA) recognize validated Level A IVIVC models as sufficient for biowaiver applications, enabling formulation changes without additional clinical studies [22]. Furthermore, a properly validated Level A IVIVC allows for the establishment of clinically relevant dissolution specifications that ensure consistent product quality and performance throughout its lifecycle [4]. The credibility of an IVIVC model is determined through rigorous validation processes, including internal and external predictability assessments, which evaluate how well the model can predict in vivo performance from in vitro data [14].
Table 1: Comparison of IVIVC Levels and Their Characteristics
| IVIVC Level | Type of Correlation | Predictive Capability | Regulatory Utility |
|---|---|---|---|
| Level A | Point-to-point relationship between in vitro dissolution and in vivo absorption rate | High - can predict entire plasma concentration profile | Biowaivers for formulation and process changes; setting dissolution specifications |
| Level B | Compares mean in vitro dissolution time to mean in vivo dissolution time | Moderate - uses statistical moments analysis | Limited regulatory utility; primarily for formulation development guidance |
| Level C | Single-point relationship between dissolution parameter and pharmacokinetic parameter | Low - relates only specific points | Supportive role in development; insufficient for biowaivers |
| Multiple Level C | Multiple point relationships between dissolution parameters and pharmacokinetic parameters | Moderate - improved predictability over Level C | May support biowaivers in certain cases with justification |
Step-by-Step Methodology for Level A IVIVC Development
Formulation Selection and Study Design
The initial phase in developing a Level A IVIVC involves careful formulation selection and study design. Researchers should develop at least three formulations with different release rates – typically fast, medium, and slow-releasing versions – to adequately characterize the relationship between in vitro dissolution and in vivo performance [14]. These formulations should exhibit significant differences in their dissolution profiles to establish a meaningful correlation. For immediate-release formulations of poorly soluble drugs, such as the itraconazole amorphous solid dispersion tablets studied successfully, this may involve varying the polymer grades, disintegrant levels, or employing different processing techniques like dry granulation [14].
For lipid-based formulations, which present unique challenges due to their complex digestion and solubilization processes, formulation selection should consider the Lipid Formulation Classification System (LFCS) [4]. Type I formulations consist purely of oils; Type II include oils and lipophilic surfactants; Type III incorporate oils, surfactants, and co-solvents; while Type IV contain only surfactants and co-solvents without traditional lipids [4]. Each type exhibits different behaviors in both in vitro tests and in vivo environments, necessitating tailored approaches to IVIVC development.
In Vitro Dissolution Method Development
Developing a biorelevant dissolution method is crucial for establishing a meaningful Level A IVIVC. The dissolution conditions should ideally reflect the gastrointestinal environment that the formulation will encounter in vivo. For conventional formulations, standard USP apparatus with appropriate media may suffice, but for more complex systems like LBFs and ASDs, more sophisticated approaches are necessary:
- For lipid-based formulations, incorporating lipolysis models that simulate intestinal digestion processes may be essential for predicting in vivo performance [4].
- For amorphous solid dispersions, methods such as triturating tablets into particles prior to dissolution testing may better mimic the attenuated disintegration that occurs in vivo [14].
- The use of biorelevant media simulating fasted or fed state intestinal fluids can significantly improve the predictability of dissolution tests [4].
Recent research on itraconazole ASDs employed USP simulated intestinal fluid (phosphate buffer) adjusted to pH 6.4, with tablets triturated into particles prior to immersion to better mimic in vivo disintegration patterns [14]. This attention to biopredictive methodology was crucial to their successful Level A IVIVC development.
In Vivo Data Collection and Study Protocols
Conducting well-designed pharmacokinetic studies in appropriate animal models or human subjects is essential for obtaining reliable in vivo data for IVIVC development. Key considerations include:
- Study Population: For human studies, typically 12-36 healthy adult volunteers are employed in crossover designs to minimize variability [14].
- Reference Formulation: Including an oral solution or rapidly dissolving formulation as a reference can help establish the "input function" for deconvolution [14].
- Sampling Strategy: Adequate blood sampling should be conducted to properly characterize the absorption phase – typically 12-18 samples over 24-72 hours depending on the drug's pharmacokinetics.
- Fed vs. Fasted State: For some formulations, particularly LBFs, evaluating both fasted and fed states may be necessary as food effects can significantly impact performance [4].
Table 2: Key Pharmacokinetic Parameters for IVIVC Development
| Parameter | Description | Role in IVIVC |
|---|---|---|
| Cmax | Maximum observed plasma concentration | Reflects rate and extent of absorption |
| Tmax | Time to reach Cmax | Indicates absorption rate |
| AUC0-t | Area under the plasma concentration-time curve from zero to last measurable time point | Measures total drug exposure |
| AUC0-∞ | Area under the plasma concentration-time curve from zero to infinity | Represents complete drug exposure |
| Absorption Profile | Time course of drug absorption derived via deconvolution | Directly correlated with dissolution profile in Level A IVIVC |
Data Analysis Techniques: Deconvolution and Model Building
Deconvolution Methods
Deconvolution is the mathematical process used to determine the time course of drug absorption in vivo, which is then correlated with the in vitro dissolution profile. Two primary approaches are employed:
- Model-Dependent Methods: These techniques assume a specific pharmacokinetic model (e.g., one- or two-compartment models) and fit the observed plasma concentration data to derive the input function.
- Model-Independent Methods: Utilizing numerical deconvolution approaches, these methods do not assume a specific pharmacokinetic model and instead use a reference formulation (typically an oral solution or intravenous administration) to determine the input function.
For the itraconazole ASD Level A IVIVC, researchers employed a "direct, differential-equation-based IVIVC model approach, using an oral solution for post-dissolution disposition" with fast-, medium-, and slow-release tablets [14]. This model-dependent approach successfully met FDA internal predictability requirements for Level A IVIVC.
Correlation Model Development
Once the in vivo absorption time course has been derived via deconvolution, correlation models are developed to relate the fraction dissolved in vitro to the fraction absorbed in vivo. Common mathematical approaches include:
- Linear models: Simple proportional relationships between dissolved and absorbed fractions
- Non-linear models: Including polynomial, logarithmic, or Weibull functions that capture more complex relationships
- Direct differential equation models: As employed in the itraconazole ASD case study [14]
The mathematical relationship is typically expressed as: Fabs(t) = f(Fdiss(t)) where Fabs(t) is the fraction absorbed at time t and Fdiss(t) is the fraction dissolved at time t.
Figure 1: Level A IVIVC Development Workflow
Experimental Protocols and Methodologies
Dissolution Testing Protocols for Different Formulation Types
Lipid-Based Formulations
For lipid-based formulations, traditional dissolution tests often fail to predict in vivo performance due to their inability to simulate lipid digestion processes. The pH-stat lipolysis model has emerged as a more biorelevant approach:
- Preparation of Digestion Medium: Create an intestinal digestion medium containing Tris buffer, bile salts, phospholipids, and calcium ions at physiologically relevant concentrations.
- Lipolysis Reaction: Add the lipid formulation to the medium and initiate digestion with pancreatic extract while maintaining pH stat titration.
- Sampling and Analysis: Collect samples at predetermined time points, immediately inhibit further lipolysis, and analyze for drug content in different phases (aqueous, pellet, oil).
- Data Interpretation: Calculate the percentage of drug in the aqueous phase (representing potentially absorbable drug) over time to generate the dissolution profile.
Studies have shown variable success with this approach – while Feeney et al. found that only half of the drugs studied using the pH-stat lipolysis device correlated well with in vivo data, it remains one of the most promising methods for LBFs [4].
Amorphous Solid Dispersions
For immediate-release ASDs, such as the itraconazole tablets successfully correlated:
- Media Selection: Use USP simulated intestinal fluid (phosphate buffer) adjusted to pH 6.4 to simulate intestinal conditions [14].
- Apparatus Selection: Standard USP Apparatus I or II with appropriate agitation speed (typically 50-75 rpm).
- Sample Preparation: For some formulations, triturating tablets into particles prior to dissolution may better mimic in vivo disintegration [14].
- Sampling and Analysis: Collect samples at appropriate time intervals (e.g., 5, 10, 15, 20, 30, 45, 60 minutes) and analyze for drug content.
- Sink Conditions: Maintain sink conditions where possible, though for poorly soluble drugs this may not be feasible.
Pharmacokinetic Study Protocols
Well-designed clinical or preclinical studies are essential for generating quality in vivo data:
- Study Design: Randomized crossover designs are preferred to minimize inter-subject variability.
- Dosing: Administer test formulations (fast, medium, slow release) and reference standard (solution or immediate-release formulation) with appropriate washout periods.
- Blood Sampling: Collect serial blood samples at strategic time points to adequately characterize the absorption phase – typically more frequent sampling during early time points.
- Bioanalytical Methods: Use validated analytical methods (LC-MS/MS typically) for quantitation of drug concentrations in plasma.
- Data Analysis: Calculate key pharmacokinetic parameters (Cmax, Tmax, AUC) using non-compartmental analysis.
Figure 2: Level A IVIVC Correlation Model Concept
Case Study: Successful Level A IVIVC Implementation
A recent landmark study successfully established an FDA Level A IVIVC for amorphous solid dispersion-enabled itraconazole tablets, representing one of the few reported cases for immediate-release formulations [14]. This case provides a validated template for Level A IVIVC development:
Formulation Strategy and Experimental Design
Researchers developed three tablet formulations with distinct release rates – Fast, Medium, and Slow – containing itraconazole as a spray-dried dispersion [14]. The release rates were modulated through different grades of the same polymer, varying disintegrant levels, and employing dry granulation processing. This careful formulation design created the necessary dissolution rate variability essential for robust correlation development.
Biorelevant Dissolution Method Development
The dissolution method employed USP simulated intestinal fluid (phosphate buffer) at pH 6.4 [14]. Critically, to better mimic the attenuated disintegration that occurs in vivo, tablets were triturated into particles prior to their immersion into dissolution media, addressing a key challenge in establishing IVIVC for immediate-release formulations.
Pharmacokinetic Study and Data Analysis
The human pharmacokinetic study employed an oral solution as a reference for post-dissolution disposition, allowing for accurate determination of the absorption time course [14]. The direct, differential-equation-based IVIVC model approach successfully met all FDA internal predictability requirements for Level A IVIVC, demonstrating the robustness of their methodology.
Model Validation and Regulatory Compliance
The researchers conducted comprehensive credibility assessment of their FDA Level A IVIVC model, including model verification and validation considerations aligned with the question of interest, context of use, and model risk [14]. This rigorous approach highlights the importance of not just developing the correlation but thoroughly validating it against regulatory standards.
Table 3: Key Reagents and Materials for IVIVC Studies
| Reagent/Material | Specifications | Function in IVIVC |
|---|---|---|
| Biorelevant Dissolution Media | Phosphate buffers, FaSSIF/FeSSIF, simulated gastric/intestinal fluids | Mimics gastrointestinal environment for predictive dissolution testing |
| Pancreatic Enzymes | Pancreatin with specified lipase/amylase/protease activity | Essential for lipolysis models evaluating lipid-based formulations |
| Synthetic Surfactants | SLS, Polysorbates, Cremophor types | Enhances solubility and maintains sink conditions in dissolution media |
| Pharmacokinetic Reference Standards | Certified reference materials with documented purity | Quantitation of drug concentrations in biological matrices |
| Chromatographic Columns | C18, phenyl, or other specialized stationary phases | Separation and analysis of drug in dissolution and biological samples |
Advanced Considerations and Troubleshooting
Challenges with Complex Formulations
Lipid-based formulations present particular challenges for IVIVC development due to their complex digestion, solubilization, and potential lymphatic transport [4]. Case studies highlight these difficulties – Do et al. found in vitro dispersion data failed to distinguish between LBFs administered in fasted or fed states in rats, while Larsen et al. observed precipitation during in vitro lipolysis that didn't correlate with in vivo performance [4]. These discrepancies emphasize the need for more sophisticated in vitro models that better simulate the dynamic in vivo environment.
Nanomedicines represent another challenge, as their absorption profile "varies widely with that of its conventional dosage forms mainly due to the physicochemical modifications and results in highly deviating in-vitro and in-vivo data" [13]. The unique properties of nanoparticles necessitate specialized approaches to IVIVC development that account for their distinct absorption mechanisms.
Model Validation and Acceptance Criteria
For regulatory acceptance of a Level A IVIVC, the FDA recommends specific validation criteria focusing on prediction errors:
- Internal Validation: The average absolute percent prediction error (%PE) for Cmax and AUC should be ≤10%, and the prediction error for individual formulations should not exceed 15% [14].
- External Validation: If applicable, the model should successfully predict the in vivo performance of additional formulations not used in model development.
- Context of Use Consideration: Model verification and validation should consider the specific question of interest and model risk [14].
The successful itraconazole Level A IVIVC met these FDA internal predictability requirements, providing a template for appropriate validation approaches [14].
Establishing a Level A IVIVC represents a significant achievement in pharmaceutical development, offering substantial benefits in reducing development costs, streamlining regulatory approvals, and ensuring product quality throughout its lifecycle. The step-by-step methodology outlined – from careful formulation design through biorelevant dissolution testing, robust pharmacokinetic studies, appropriate deconvolution techniques, and rigorous model validation – provides a roadmap for successful implementation.
Future advancements in IVIVC will likely come from improved in vitro tools that better simulate gastrointestinal physiology, particularly for challenging formulations like LBFs and nanomedicines [4]. Additionally, the integration of in silico modeling and machine learning approaches holds promise for enhancing IVIVC predictability, especially for drugs with complex absorption mechanisms [22]. As these methodologies evolve, the pharmaceutical industry can expect more efficient development pathways for even the most challenging drug molecules, ultimately accelerating patient access to important medicines.
In vitro–in vivo correlation (IVIVC) is a critical scientific approach in pharmaceutical development, establishing a predictive relationship between a drug product's in vitro dissolution and its in vivo pharmacokinetic behavior [3]. The primary goal is to create a mathematical model that can serve as a surrogate for in vivo studies, thereby streamlining development, optimizing formulations, and supporting regulatory decisions [4] [3]. For conventional immediate-release or extended-release dosage forms, established IVIVC methodologies are well-documented. However, complex formulations such as lipid-based drug delivery systems (LBDDS) present unique challenges due to their dynamic solubilization processes, interaction with digestive enzymes, and complex absorption pathways [4].
The establishment of a robust IVIVC is particularly valuable for Biopharmaceutics Classification System (BCS) Class II and IV drugs (characterized by poor solubility), for which dissolution is often the rate-limiting step for absorption [4] [12]. A successful correlation can reduce development costs and time by minimizing the number of required clinical bioequivalence studies and supporting biowaivers for post-approval changes [23] [3]. This guide objectively compares the performance of three primary in vitro tools—USP dissolution apparatus, lipolysis assays, and combined models—in predicting the in vivo performance of complex formulations, providing researchers with a clear framework for method selection.
Tool Comparison: Principles, Applications, and Performance Data
The following sections provide a detailed comparison of the fundamental in vitro tools, summarizing their key characteristics, strengths, and limitations for different formulation types.
Table 1: Overview and Comparison of Key In Vitro Tools
| Tool Category | Governing Principle | Primary Formulation Applications | Key Measured Outputs | Regulatory Status |
|---|---|---|---|---|
| USP Dissolution Apparatus [24] | Drug release under standardized hydrodynamic conditions in compendial media. | Immediate-Release (IR) Tablets, Extended-Release (ER) Tablets [12]. | Percent drug dissolved over time (dissolution profile). | Official standardized methods; legal requirement when specified in monographs [24]. |
| Lipolysis Assays [4] | Simulation of enzymatic lipid digestion in the gastrointestinal tract. | Lipid-Based Formulations (LBFs) like SEDDS, SMEDDS, SNEDDS [4] [25]. | Drug concentration in solubilized phase, free fatty acid release (via titration). | Non-compendial, research-focused; used to support ANDAs for complex products [26]. |
| Combined Models [25] | Integration of multiple physiological processes (e.g., digestion + permeation, gastric-to-duodenal transfer). | Complex formulations where digestion and absorption are interlinked [4]. | Drug release and permeation profiles under dynamic conditions. | Emerging field; no formal standardization. |
Table 2: Performance Data and Experimental Evidence from Case Studies
| Formulation Type | In Vitro Tool Used | Key Experimental Findings | IVIVC Outcome & Level | Reference Compound |
|---|---|---|---|---|
| Itraconazole SDD Tablets (ASD) [14] | USP Apparatus (with biorelevant media & trituration). | A Level A IVIVC was established by using a biorelevant method (pH 6.4 phosphate buffer) and triturating tablets to mimic attenuated disintegration. | Successful, Level A; met FDA internal predictability criteria. | Itraconazole |
| Lamotrigine ER Tablets (BCS II) [12] | USP Apparatus II & III with compendial/biorelevant media. | Dissolution in standard compendial media with USP II apparatus was found to be biopredictive. A PBPK model was integrated for virtual bioequivalence. | Successful, Level A; PCQS (Patient-Centric Quality Standards) established. | Lamotrigine |
| Carvedilol SMEDDS (LBF) [25] | Traditional pH-stat Lipolysis. | Solubilized carvedilol concentration increased with decreased pancreatin activity and increased buffer capacity. | Method refinement; profiles were comparable but differences more pronounced in a novel flow-through system. | Carvedilol |
| Various LBFs [4] | pH-stat Lipolysis Assay. | A review found that across eight drugs studied, only half correlated well with in vivo data, highlighting predictability challenges. | Variable Success; cases of failed prediction for fenofibrate and cinnarizine reported. | Fenofibrate, Cinnarizine |
Experimental Protocols for Key Assays
USP Dissolution Testing for Extended-Release Tablets
For establishing a Level A IVIVC with ER formulations, the protocol must be designed for maximum biopredictivity [12].
- Apparatus and Settings: Typically use USP Apparatus II (paddle). Agitation rate (e.g., 50-75 rpm) and medium volume (e.g., 500-900 mL) are set as per product-specific requirements. Apparatus III (reciprocating cylinder) may also be employed for its changing hydrodynamics, which can better simulate the gastrointestinal tract [12].
- Dissolution Media Selection:
- Sample Preparation: In some cases, to better mimic in vivo disintegration, tablets may be triturated into particles prior to immersion in the dissolution vessel [14].
- Sampling and Analysis: Automated sampling at predetermined time points (e.g., 1, 2, 4, 8, 12, 16, 20, 24 hours) is recommended. Samples are filtered and analyzed via HPLC-UV to generate a complete dissolution profile [12].
Traditional pH-Stat In Vitro Lipolysis Assay
This is the most common method for evaluating the drug release from LBFs like SMEDDS under simulated intestinal conditions [4] [25].
- Digestion Medium Preparation: Prepare a digestion medium containing Tris-maleate buffer (e.g., 50-200 mM), 150 mM NaCl, 5 mM CaCl₂·2H₂O, bile salts (e.g., 4.89 mM sodium deoxycholate), and phospholipids (e.g., 1.22 mM L-α-phosphatidylcholine). Adjust pH to 7.5 with NaOH [25].
- Enzyme Preparation: Freshly prepare pancreatin extract from porcine pancreas (activity ≥3× USP) in digestion buffer. The enzyme solution is often stabilized with an inhibitor like 4-bromophenylboronic acid (BBBA) before being added to the reaction [25].
- Assay Execution: Disperse the LBF (e.g., carvedilol-loaded SMEDDS) in the digestion medium at 37°C. Initiate lipolysis by adding the pancreatin solution. The pH is maintained constant (e.g., at 7.5) by automatic titration with NaOH, which neutralizes the free fatty acids released during digestion. The volume of titrant added is a measure of the extent of digestion [25].
- Sampling and Analysis: At timed intervals, withdraw samples from the reaction vessel. Samples are immediately treated to inhibit further enzyme activity (e.g., with BBBA or by ultracentrifugation). The drug concentration in the solubilized phase (typically in the aqueous and colloidal phases) is quantified to determine the proportion of drug released and potentially precipitated [4] [25].
Advanced Two-Step Flow-Through In Vitro Lipolysis
This novel method enhances physiological relevance by simulating gastric retention and transfer to the duodenum, which is critical for weakly basic drugs [25].
- Gastric Step: The LBF (SMEDDS) is first dispersed in a simulated gastric fluid (e.g., FaSSGF, without enzymes) in a reaction vessel and incubated for a period to simulate stomach residence [25].
- Intestinal Step Initiation: The pH is then increased, and a lipolytic reaction is immediately initiated. Instead of titration, the pH is regulated by the flow of a digestion medium with high buffer capacity (e.g., concentrated Tris-maleate buffer, pH 7.8) into the vessel [25].
- Flow-Through System: The use of a flow-through dissolution system, where fresh medium is continuously introduced, allows for a more dynamic simulation of the gastrointestinal environment and better clearance of digested products [25].
- Analysis: Similar to the traditional method, samples are taken and analyzed for drug concentration, yielding a release profile that accounts for both gastric and intestinal processing.
Tool Selection Logic
The Scientist's Toolkit: Essential Research Reagents
Successful execution of these in vitro assays requires specific, high-quality reagents. The table below details essential materials and their critical functions in experimental protocols.
Table 3: Essential Research Reagents for In Vitro Characterization of Complex Formulations
| Reagent / Material | Function in Experiment | Example from Protocols |
|---|---|---|
| Pancreatin (Porcine) | Source of digestive lipases; catalyzes the breakdown of lipid excipients into free fatty acids and monoacylglycerols in lipolysis assays [25]. | Added to Tris-maleate buffer to initiate the intestinal lipolysis phase [25]. |
| Sodium Taurocholate / Sodium Deoxycholate | Bile salts; act as natural surfactants in the intestine, facilitating the formation of mixed micelles that solubilize lipolytic products and drugs [25]. | Used in digestion media at concentrations of ~5 mM to simulate intestinal bile [25]. |
| L-α-Phosphatidylcholine | Phospholipid; a primary component of intestinal bile, working synergistically with bile salts to form mixed micelles and vesicles, enhancing drug solubilization [25]. | Added to digestion media at ~1.2 mM to increase biorelevance [25]. |
| Tris-Maleate Buffer | Provides a stable pH environment for the lipolysis reaction; its concentration (buffer capacity) can significantly impact the measured drug release profile [25]. | Used at various concentrations (2-200 mM) to investigate and control pH during digestion [25]. |
| FaSSIF/FeSSIF Powders | Biorelevant media powders; reconstituted to create dissolution media that mimic the composition (bile salts, phospholipids, pH) of human intestinal fluid in fasted (FaSSIF) or fed (FeSSIF) states [12] [25]. | Used in dissolution testing to generate more physiologically relevant release profiles [12]. |
| 4-Bromophenylboronic Acid (BBBA) | Enzyme inhibitor; used to instantly halt the lipolytic reaction at specific time points during sampling, ensuring an accurate snapshot of drug distribution [25]. | Added to samples immediately after withdrawal from the lipolysis vessel [25]. |
The journey toward a predictive IVIVC for complex formulations requires a strategic and often iterative selection of in vitro tools. As demonstrated, USP dissolution remains the gold standard for conventional solid oral dosages, while lipolysis assays are indispensable for understanding the fate of lipid-based formulations. When these individual tools fail to capture in vivo performance, combined and advanced models that integrate digestion, dynamic media flow, and even permeation represent the frontier of biopredictive in vitro modeling.
The future of IVIVC is closely linked to technological advancement. The integration of these in vitro tools with Physiologically Based Biopharmaceutics Modeling (PBBM) and artificial intelligence is creating powerful, synergistic platforms [12] [3]. These platforms allow for virtual bioequivalence simulations and the establishment of patient-centric quality standards, ultimately promising to accelerate the development of robust and effective complex drug products [12].
In vitro-in vivo correlation (IVIVC) is a pivotal tool in pharmaceutical development, defined by the U.S. Food and Drug Administration (FDA) as "a predictive mathematical model describing the relationship between an in vitro property of a dosage form and a relevant in vivo response" [9] [3]. For conventional dosage forms, establishing IVIVC is relatively straightforward, with Level A correlations (point-to-point prediction of the in vivo input rate from in vitro dissolution) being achievable [3]. However, for advanced drug delivery systems like Lipid-Based Formulations (LBFs) and In Situ Forming Implants (ISFIs), the dynamic processes governing drug release and absorption introduce significant complexity, making robust IVIVC development a substantial scientific challenge [27] [4] [20].
This guide objectively compares the current state of IVIVC for these two systems by presenting successful case studies, their experimental protocols, and the critical reagents that enable these correlations. A foundational understanding of IVIVC levels is essential for interpreting these case studies, as summarized in the table below.
Table 1: Levels of In Vitro-In Vivo Correlation (IVIVC)
| Level | Definition | Predictive Value | Regulatory Acceptance |
|---|---|---|---|
| Level A | Point-to-point correlation between in vitro dissolution and in vivo absorption. | High – predicts the full plasma concentration-time profile. | Most preferred by regulators; can support biowaivers [4] [3]. |
| Level B | Uses statistical moments (e.g., compares mean in vitro dissolution time to mean in vivo residence time). | Moderate – does not reflect actual shape of the plasma profile. | Less common and less robust for regulatory submissions [4] [3]. |
| Level C | Correlates a single dissolution time point (e.g., t~50%~) to a single pharmacokinetic parameter (e.g., AUC, C~max~). | Low – does not predict the full profile. | Least rigorous; often used for early development [4] [3]. |
| Multiple Level C | Correlates multiple dissolution time points to one or more PK parameters. | Improved over Level C. | May justify certain formulation changes [4]. |
| Level D | A qualitative, rank-order analysis without a formal mathematical model. | Very Low – used for formulation ranking. | No regulatory value; serves as a development guide [4]. |
IVIVC for Lipid-Based Formulations (LBFs)
Case Study: Successful Correlation Using In Vitro Digestion Models
While many attempts to establish IVIVC for LBFs have failed, some studies have successfully demonstrated correlations using sophisticated in vitro tools that simulate gastrointestinal physiology.
Experimental Protocol: The key to success lies in moving beyond traditional USP dissolution tests to in vitro lipolysis models that mimic the enzymatic digestion of lipids in the human gut [27] [4]. The standard workflow is as follows:
- Formulation Dispersion: The LBF is introduced into a simulated intestinal fluid (e.g., FaSSIF) containing bile salts and phospholipids to simulate the initial dispersion of the formulation in the gut [4].
- pH-Stat Lipolysis: Pancreatin extract (a source of digestive lipases) is added to the medium. The pH is maintained constant (typically at 6.5) using a pH-stat apparatus, which automatically titrates sodium hydroxide (NaOH) to neutralize the fatty acids released during digestion [27] [4].
- Drug Precipitation Monitoring: The rate of NaOH addition is directly proportional to the extent of lipolysis. Simultaneously, samples are taken from the digestion medium at predefined time points. These samples are ultracentrifuged or filtered to separate the aqueous phase (containing solubilized drug) from the pellet (containing precipitated drug) and the undigested lipid phase [27].
- Analytical Quantification: The drug concentration in the aqueous phase is quantified using HPLC-UV, providing a profile of drug solubilization and potential precipitation over the course of digestion [4].
- Data Correlation: The in vitro solubilization profile is then correlated with the in vivo absorption profile (obtained by deconvolution of plasma concentration data) or key pharmacokinetic parameters like AUC (Area Under the Curve) and C~max~ (peak plasma concentration) from animal or human studies [4].
The following diagram illustrates this integrated experimental and modeling workflow.
Quantitative Data from Case Studies
The table below summarizes key experimental data and correlation levels from documented LBF studies, highlighting both the challenges and successes.
Table 2: IVIVC Case Studies for Lipid-Based Formulations
| Drug Model | In Vitro Model | In Vivo Model | Key Experimental Findings | Correlation Level Achieved |
|---|---|---|---|---|
| Fenofibrate | pH-stat lipolysis | Rat | In vitro dispersion data failed to distinguish LBF performance in fasted vs. fed state; no correlation identified [20]. | No correlation |
| Cinnarizine | pH-stat lipolysis | Dog | Precipitation observed during in vitro lipolysis, but in vivo performance was similar across formulations [4]. | Level D (Qualitative ranking only) [4] |
| General Review | pH-stat lipolysis | Human/Animal | A meta-analysis of 8 drugs found only 4 showed good correlation between in vitro lipolysis and in vivo data [20]. | Variable (50% success rate) |
| Successful Cases | Advanced lipolysis + permeation | Human/Animal | Incorporation of permeation barriers (e.g., Caco-2 cells) and PBPK modeling has improved predictability for some drugs [27] [4]. | Level A / Multiple Level C |
IVIVC for In Situ Forming Implants (ISFIs)
Case Study: Levodopa/Carbidopa ISFI with Ex Vivo Correlation
A 2025 study developed a solvent-induced phase inversion implant for the sustained delivery of levodopa and carbidopa for Parkinson's disease, successfully establishing a strong correlation [28].
Experimental Protocol: The methodology focused on mimicking the subcutaneous environment and using an ex vivo model to bridge the in vitro-in vivo gap.
- Implant Formation In Vitro: The optimized formulation containing PLGA (26%) and Eudragit L-100 (6%) in N-Methyl-2-pyrrolidone (NMP) was injected into a release medium (e.g., phosphate buffer saline, PBS). The water-miscible organic solvent (NMP) diffused out, causing the polymer to precipitate and form a solid implant depot [28].
- Drug Release Testing: The implant was incubated in PBS (pH 7.4) at 37°C under gentle agitation. The release medium was sampled at regular intervals over 7 days and analyzed via HPLC to determine the cumulative drug release profile [28].
- Ex Vivo Model: To better simulate the in vivo environment, a separate set of implants was injected into fresh, excised porcine skin tissue, which was then immersed in the release medium. This setup accounts for the tortuosity and proteinaceous environment of the tissue, which can impact drug release [28].
- Data Correlation: The drug release profiles from the standard in vitro method and the ex vivo tissue model were directly compared. The study reported a high correlation coefficient (0.91 for levodopa and 0.90 for carbidopa) between the two methods, validating the in vitro model as predictive [28].
- In Vivo Prediction: The in vitro release data was used as an input for convolution modeling in R software to predict the in vivo plasma concentration-time profile (AUC, C~max~, T~max~), assuming 100% bioavailability [28].
The workflow for developing and testing the ISFI is summarized below.
Quantitative Data from Case Studies
The table below presents experimental data from key ISFI studies, demonstrating the quantitative basis for IVIVC.
Table 3: IVIVC Case Studies for In Situ Forming Implants
| Drug Model / Study Focus | Polymer System / Key Variable | Key Experimental Findings | Correlation Outcome |
|---|---|---|---|
| Levodopa/Carbidopa [28] | PLGA 50:50 + Eudragit L-100 | Initial 24h burst: ~35%; 7-day release: >80%; release profile was similar in ex vivo porcine tissue. | High ex vivo-in vitro correlation (R = 0.91/0.90). |
| Impact of Hydrophilic Polymers [29] | PLGA + Hydrophilic Polymers (HPMC, Carbopol, HPC, CMC) | HPMC & Carbopol effectively reduced 24h burst release; HPC & CMC increased burst release and porosity. | Level D correlation: Formulation ranking based on burst release and phase inversion rate. |
| Characterization Technique [29] | PLGA + NMP with various polymers | Optical Coherence Tomography (OCT) non-invasively characterized implant formation kinetics and morphology. | Enabled qualitative correlation between polymer type, phase inversion rate, and implant structure. |
The Scientist's Toolkit: Essential Reagents and Materials
Successful IVIVC development for these complex systems relies on specific, high-quality materials. The following table lists critical research reagents and their functions.
Table 4: Essential Research Reagents for IVIVC Studies of LBFs and ISFIs
| Category | Reagent / Material | Function in Experiment | Example Application |
|---|---|---|---|
| Lipid Formulations | Medium/Long-Chain Triglycerides (MCT/LCT) | Lipid core of the formulation; enhances drug solubility and lymphatic transport [27] [30]. | Type I-III LBFs [30]. |
| Surfactants (e.g., Polysorbate 80, Polyoxyl 40 Hydrogenated Castor Oil) | Stabilize emulsion droplets and improve dispersion [27] [30]. | Type II-IV LBFs, SNEDDS/SMEDDS [27]. | |
| Lipophilic & Hydrophilic Cosolvents (e.g., Ethanol, PEG) | Aid drug solubilization in the formulation and influence self-dispersibility [27] [30]. | Type III/IV LBFs [27]. | |
| In Vitro Digestion | Pancreatin Extract | Source of digestive lipases to simulate intestinal lipid digestion [27] [4]. | pH-stat lipolysis model. |
| Sodium Taurodeoxycholate (Bile Salt) | Main component of simulated intestinal fluid; facilitates micelle formation [4]. | Dispersion and digestion media. | |
| In Situ Implants | Biodegradable Polymer (e.g., PLGA 50:50) | Primary matrix-forming polymer; controls drug release via degradation [29] [28]. | Solvent-induced phase inversion implants. |
| Water-Miscible Solvent (e.g., NMP, DMAc) | Dissolves polymer and drug; dissipates upon injection to trigger implant formation [29] [28]. | Solvent for ISFI. | |
| Pore Formers / Release Modifiers (e.g., Eudragit L-100, HPMC) | Modify polymer matrix hydrophilicity, porosity, and degradation to fine-tune release kinetics [29] [28]. | Optimizing 7-day release profile. |
This guide has presented a direct comparison of IVIVC approaches for two advanced drug delivery systems. The path to a successful correlation is system-dependent.
For Lipid-Based Formulations, the primary challenge is replicating the complex dynamic processing of lipids in the GI tract, including digestion, solubilization, and permeation [27] [4]. Success is more likely when using in vitro lipolysis models over simple dissolution, and is further enhanced by integrating permeation barriers and Physiologically Based Pharmacokinetic (PBPK) modeling [27] [4] [20]. However, correlations can be fragile and are not universally successful, as evidenced by the 50% success rate in one meta-analysis [20].
For In Situ Forming Implants, the challenge lies in simulating the tissue environment and the solvent exchange process that governs implant formation and subsequent drug release [29] [28]. The use of ex vivo tissue models and advanced characterization tools like Optical Coherence Tomography (OCT) provides a robust bridge to in vivo performance, allowing for strong correlations as demonstrated in the levodopa/carbidopa case study [28].
The future of IVIVC for both systems lies in the adoption of more sophisticated, integrated tools. Artificial Intelligence (AI) and machine learning are poised to analyze complex datasets to identify hidden patterns and improve prediction accuracy [3]. Furthermore, the continued development of PBPK modeling integrated with biorelevant in vitro data represents the most promising path toward generating predictive IVIVCs that can accelerate the development of these complex and powerful drug delivery technologies [4] [3].
Leveraging In Silico Predictions and PBPK Modeling to Enhance IVIVC
In vitro-in vivo correlation (IVIVC) is a critical scientific approach in pharmaceutical development, establishing a predictive relationship between a drug's dissolution profile and its human pharmacokinetic behavior [3]. A well-defined IVIVC allows researchers to use in vitro dissolution data as a surrogate for in vivo bioavailability studies, optimizing formulations and supporting regulatory submissions for biowaivers [31] [3]. Traditionally, IVIVC models have been categorized into Levels A, B, and C, with Level A representing the most informative point-to-point correlation [3].
The emergence of Physiologically Based Pharmacokinetic (PBPK) modeling and advanced in silico prediction tools has fundamentally transformed IVIVC development. PBPK models incorporate physiological parameters, drug properties, and population variability to simulate drug absorption, distribution, metabolism, and excretion [32] [33]. This mechanistic approach addresses key limitations of conventional IVIVC, particularly its inability to reliably extrapolate across different physiological conditions, such as fed versus fasted states, or between patient populations [34]. The integration of PBPK and IVIVC creates a powerful paradigm for predicting clinical performance from laboratory data with greater confidence and reduced reliance on animal and human studies [3].
Comparative Analysis: Traditional IVIVC vs. PBPK-Enhanced IVIVC
The table below compares the core characteristics of traditional IVIVC approaches against the modern, PBPK-enhanced methodology.
Table 1: Comparison of Traditional and PBPK-Enhanced IVIVC Approaches
| Aspect | Traditional IVIVC | PBPK-Enhanced IVIVC |
|---|---|---|
| Fundamental Basis | Empirical, statistical correlation between in vitro dissolution and in vivo absorption [31]. | Mechanistic, physiology-based model simulating drug disposition via differential equations [32] [33]. |
| Regulatory Utility | Supports biowaivers for formulation changes of extended-release products; defined in specific FDA guidances [3]. | Extends utility to complex scenarios: food effects, drug-drug interactions (DDIs), specific populations (pediatrics, organ impairment) [32] [34]. |
| Extrapolation Capability | Limited; primarily valid for the specific conditions under which it was developed [34]. | High; can simulate and predict PK across diverse physiological and clinical conditions using virtual populations [33] [34]. |
| Key Advantage | Well-established regulatory pathway for Level A correlation [3]. | Provides a "totality of evidence" approach, enabling Virtual Bioequivalence (VBE) for complex products like GI-local and transdermal drugs [34] [35]. |
| Common Application Example | Correlation for extended-release oral dosage forms like propranolol [36]. | Dose selection for pediatric populations (e.g., ALTUVIIIO) [32] and DDI prediction for asciminib [37]. |
Experimental Data and Case Studies
PBPK for Pediatric Dose Selection of a Novel Therapeutic Protein
For ALTUVIIIO, a novel recombinant Factor VIII therapy, a minimal PBPK model was developed to support pediatric dose selection. The model was first validated using clinical data from ELOCTATE, a similar Fc-fusion protein, by accurately predicting its pharmacokinetics in adults and children. The model's prediction errors for key exposure parameters (Cmax and AUC) were within ±25%, demonstrating its credibility. This validated model was then applied to simulate the pharmacokinetic profile of ALTUVIIIO in children under 12 years of age, ensuring FVIII activity levels were maintained above the therapeutic threshold for most of the dosing interval and justifying the once-weekly dosing regimen [32].
Table 2: PBPK Model Performance in Predicting Pharmacokinetics of Fc-Fusion Proteins
| Population | Age (years) | Drug | Dose (IU/kg) | Cmax (ng/mL) | AUC (ng·h/mL) |
|---|---|---|---|---|---|
| Observed / Predicted (%Error) | Observed / Predicted (%Error) | ||||
| Adult | 23-61 | ELOCTATE | 25 | 140 / 105 (-25%) | 3,009 / 2,671 (-11%) |
| Adult | 23-61 | ELOCTATE | 65 | 345 / 272 (-21%) | 7,794 / 6,944 (-11%) |
| Adult | 19-63 | ALTUVIIIO | 25 | 282 / 288 (2%) | 14,950 / 13,726 (-8%) |
| Adult | 19-63 | ALTUVIIIO | 65 | 735 / 749 (2%) | 43,300 / 35,687 (N/A) |
Establishing IVIVC for a Transdermal System
A Level A IVIVC was successfully developed for estradiol transdermal drug delivery systems (TDDS), marking a significant advance for non-oral dosage forms. The methodology involved:
- In Vitro Permeation: Measuring drug permeation across surgically discarded human skin using Franz diffusion cells [31].
- In Vivo Absorption: Determining the fraction of drug absorbed in postmenopausal women using deconvolution methods based on plasma concentration-time profiles from marketed patches with different delivery rates [31].
- Correlation and Validation: A point-to-point (Level A) correlation was established between the percentage of drug permeated in vitro and the percentage absorbed in vivo. The model was validated by demonstrating that the predicted plasma concentrations from the in vitro permeation data met FDA acceptance criteria for prediction error [31].
Virtual Bioequivalence for Vaginal Ring Formulations
A PBPK-based IVIVR (in vitro-in vivo relationship) was developed for progesterone vaginal rings. The MechVAM model in Simcyp Simulator was used to simulate plasma concentrations. An IVIVR was established to translate measured in vitro release rates into simulated in vivo release profiles. This combined PBPK/IVIVR approach was then used to perform Virtual Bioequivalence (VBE) testing, the results of which were consistent with those of actual clinical BE trials. Furthermore, the model was leveraged to establish an "in vitro dissolution safe space," defining the acceptable limits of in vitro release rate variation (±7.36% to +9.40% mg/day) that would ensure maintained bioequivalence, thereby supporting post-approval changes with minimal clinical testing [35].
Essential Methodologies and Workflows
General Workflow for Developing a PBPK Model
The development and application of a PBPK model for IVIVC follow a structured workflow. The process begins with System Configuration, where a virtual population is defined using software-specific databases that incorporate physiological parameters [38]. Next, Compound Data Integration involves gathering the drug's physicochemical properties, permeability, and metabolism data from in vitro assays and literature to create a compound profile [38]. The core Model Development & Validation stage uses clinical data (e.g., from an oral solution or intravenous dose) to calibrate and validate the model, ensuring it can accurately predict observed pharmacokinetics [32] [38]. Finally, the Simulation & Application stage utilizes the validated model to run virtual trials, predict DDIs, or support VBE assessments for new formulations or populations [34] [37].
Diagram 1: PBPK Model Development Workflow
Integrated IVIVC and PBPK Workflow for Virtual Bioequivalence
For complex generic products, an integrated workflow combining IVIVC and PBPK is key to demonstrating virtual bioequivalence. The process starts with developing a biorelevant or biopredictive dissolution method that closely mimics the in vivo environment [34]. A PBPK absorption model is then developed and validated against clinical data for the reference product. A critical step is establishing an IVIVC or IVIVR to convert the in vitro dissolution profile of a test product into a corresponding in vivo input profile. This input is fed into the validated PBPK model to simulate the plasma concentration-time profile of the test product. Virtual bioequivalence is assessed by comparing the simulated exposure of the test product (e.g., Cmax, AUC) against the reference within a virtual population [34] [35].
Diagram 2: IVIVC-PBPK Workflow for VBE
The Scientist's Toolkit: Key Research Reagents and Solutions
The experimental and computational work in this field relies on a suite of specialized tools and reagents.
Table 3: Essential Research Reagents and Tools for IVIVC and PBPK Modeling
| Tool/Reagent | Function/Description | Example Use Case |
|---|---|---|
| Simcyp Simulator | A leading PBPK software platform with built-in virtual populations and the ADAM model for predicting oral absorption [38]. | Used for simulating drug-drug interactions and vaginal absorption (MechVAM model) [35] [38]. |
| USP Dissolution Apparatus | Standardized equipment (e.g., Apparatus I) to measure drug release from solid dosage forms under controlled conditions [36]. | Generating in vitro release profiles for propranolol ER tablets for IVIVC development [36]. |
| Franz Diffusion Cell | A vertical diffusion cell system used to study the permeation of drugs through biological membranes like human skin. | Measuring in vitro permeation of estradiol for transdermal IVIVC [31]. |
| Human Skin/Skin Models | Excised human skin or synthetic membranes to simulate the transdermal absorption barrier. | Serves as the membrane in Franz cell studies for transdermal system development [31]. |
| WIN-NONLIN | A software tool for pharmacokinetic/pharmacodynamic data analysis, including non-compartmental analysis and deconvolution. | Used for numerical deconvolution to estimate in vivo absorption input rates [36]. |
| Hydroxypropyl Methylcellulose (HPMC) | A common polymer used to create hydrophilic matrix systems for controlling drug release in extended-release formulations. | Used as a release-modifying agent in propranolol ER tablets [36]. |
The integration of in silico predictions and PBPK modeling represents a paradigm shift in IVIVC science. This synergistic approach moves beyond empirical correlation to a more mechanistic and predictive framework, enhancing confidence in extrapolating drug performance across different populations and conditions. As evidenced by successful applications in pediatric dosing, complex generic products, and novel drug modalities, the PBPK-enhanced IVIVC is poised to play an increasingly central role in modern, efficient, and patient-centric drug development [32] [34] [3].
Overcoming IVIVC Challenges: Troubleshooting Discrepancies in Complex Drug Products
Addressing the IVIVC Gap in Lipid Nanoparticles (LNPs) and Nucleic Acid Delivery Systems
The development of Lipid Nanoparticles (LNPs) for nucleic acid delivery represents a breakthrough in therapeutic and vaccine applications, as evidenced by their successful deployment in mRNA-based COVID-19 vaccines. However, a significant translational bottleneck persists: the unreliable correlation between in vitro performance and in vivo efficacy (IVIVC). This gap delays clinical translation by impeding accurate prediction of LNP behavior in complex biological systems based on laboratory assays [39] [40]. Establishing robust IVIVC is essential for streamlining formulation optimization, reducing reliance on extensive animal testing, and accelerating the development of future LNP-based therapeutics [41]. This guide objectively compares LNP performance across evaluation models, presents experimental data highlighting IVIVC disparities, and details methodologies to bridge this critical gap for research professionals.
Experimental Evidence of the IVIVC Gap in LNP Performance
Comparative Performance of LNPs with Different Ionizable Lipids
Recent systematic studies directly demonstrate the disconnect between LNP performance in controlled cellular environments and living organisms. Research evaluating four LNP formulations identical except for their ionizable lipids (SM-102, ALC-0315, MC3, and C12-200) revealed significant IVIVC challenges [39] [40].
Table 1: Discrepancy between in vitro and in vivo performance of LNPs with different ionizable lipids
| Ionizable Lipid | In Vitro Protein Expression | In Vivo Protein Expression | Vaccine Immunogenicity |
|---|---|---|---|
| SM-102 | Significantly higher (p < 0.05) | High (no significant difference from ALC-0315) | Strong immune response (no significant differences among formulations) |
| ALC-0315 | Moderate | High (no significant difference from SM-102) | Strong immune response |
| MC3 | Low | Low | Strong immune response |
| C12-200 | Low | Low | Strong immune response |
The data reveals critical IVIVC disruptions: while SM-102 LNPs demonstrated superior in vitro transfection across multiple cell lines (HEK293, HeLa, and THP-1), this advantage disappeared in vivo, where both SM-102 and ALC-0315 performed equivalently [39] [40]. Furthermore, despite differential protein expression in vivo, all formulations elicited equally strong immune responses as vaccines, indicating that in vivo expression levels do not directly predict immunogenicity [40]. These findings highlight the complex relationship between LNP formulation, protein expression, and immune activation that cannot be captured by in vitro systems alone.
Experimental Protocols for IVIVC Assessment
LNP Formulation and Characterization
Methodology: LNPs are typically formulated using microfluidic technology (e.g., NanoAssemblr Ignite) with lipid components dissolved in ethanol rapidly mixed with an aqueous phase containing mRNA at controlled flow rates [39] [40]. Standard formulations maintain an N/P ratio (nitrogen groups from ionizable lipids to phosphate groups in RNA) of approximately 8, with a final mRNA concentration of 70 µg/mL [40].
Critical Quality Attributes:
- Size and Polydispersity: Measured via dynamic light scattering (DLS), optimal range 70-100 nm with PDI <0.5 [39] [42]
- Zeta Potential: Near-neutral charge for reduced non-specific interactions [39]
- Encapsulation Efficiency: Typically >90% for effective delivery [39]
- mRNA Integrity: Assessed via capillary gel electrophoresis [41]
In Vitro and In Vivo Evaluation
Cell-Based Potency Assays: Multiple mammalian cell lines (e.g., HepG2, HEK293, HeLa, THP-1, DC2.4, B16-F10) are transfected with LNPs encoding reporter genes (e.g., firefly luciferase, Green Lantern) [43] [41]. Protein expression is quantified via luciferase activity assays or fluorescent imaging 24-48 hours post-transfection [43].
In Vivo Evaluation: Formulations demonstrating promising in vitro performance advance to animal models (typically mice). mRNA expression is quantified via bioluminescent imaging or immunoassays, while vaccine immunogenicity is assessed through antigen-specific antibody titers and T-cell responses following single or multiple administrations [39] [40].
Figure 1: Experimental workflow for evaluating LNP formulations and assessing IVIVC, integrating high-throughput screening with computational approaches.
Biological Mechanisms Underlying the IVIVC Gap
Molecular and Cellular Factors
The divergence between in vitro and in vivo LNP performance stems from fundamental biological differences between cell culture systems and whole organisms:
Protein Corona Formation: Upon administration, LNPs immediately interact with biological fluids, adsorbing proteins (immunoglobulins, lipoproteins) that form a "corona" altering surface properties, cellular interactions, and biodistribution [44] [39]. This critical modifying layer is absent in standard in vitro systems.
Cellular Uptake Mechanisms: LNP internalization occurs via multiple pathways (micropinocytosis, clathrin-mediated endocytosis) that vary by cell type and LNP properties [39]. The relative contribution of these pathways differs significantly between immortalized cell lines and primary cells in tissues.
Endosomal Escape Efficiency: The protonation of ionizable lipids in acidic endosomes facilitates interaction with anionic phospholipids, enabling mRNA release into the cytosol [39] [45]. This process is influenced by intracellular trafficking pathways that differ in vitro versus in vivo.
Biodistribution Patterns: In vivo, LNPs encounter physiological barriers (cellular, endothelial) absent in vitro, with formulation components (e.g., cholesterol) promoting hepatic accumulation through lipoprotein interactions [39] [46]. This significantly impacts delivery efficiency to target tissues.
Impact of LNP Formulation Components
Table 2: Key LNP components and their influence on IVIVC
| Component | Function | Impact on IVIVC |
|---|---|---|
| Ionizable Lipid | Nucleic acid complexation, endosomal escape | Structure determines pKa, fusogenicity, and organ tropism; performance varies between in vitro and in vivo models [44] [46] |
| PEG-Lipid | Stability, circulation time, reduces immune recognition | Acyl chain length (e.g., DMG vs. DSG-PEG2000) significantly affects in vivo performance regardless of ionizable lipid [47] |
| Cholesterol | Membrane fusion, structural integrity | Enhances hepatic accumulation via lipoprotein interactions; removal enables extrahepatic targeting [46] |
| Phospholipid | Structural stability, endosomal escape | Contributes to liver tropism; can be dispensable in some targeted formulations [46] |
Emerging Approaches to Bridge the IVIVC Gap
Advanced Screening and Computational Technologies
High-Throughput Screening Platforms: Automated systems now enable formulation and testing of hundreds to thousands of LNP compositions in parallel [44] [42]. Microfluidic technologies allow reproducible LNP synthesis in multi-well plates (up to 384 formulations per plate) with minimal reagent consumption, facilitating rapid identification of lead candidates [42].
DNA Barcoding Strategies: Multiplexed in vivo screening employs DNA-barcoded LNPs to simultaneously evaluate hundreds of formulations in a single animal, directly comparing delivery efficiency across tissues and cell types while reducing animal use [44] [42].
Machine Learning and Predictive Modeling: The COMET (Composite Material Transformer) model uses transformer-based neural networks to predict LNP efficacy by integrating multi-component formulation data [43]. Trained on extensive datasets (e.g., LANCE with >3,000 LNP formulations), COMET accurately ranks LNP performance and identifies optimal candidates from virtual libraries of millions of compositions [43].
Biomimetic Systems and Formulation Redesign
Advanced In Vitro Models: Development of more physiologically relevant systems (3D cultures, organ-on-a-chip, biomimetic hydrogels) that better recapitulate in vivo microenvironments and biological barriers [42].
LNP Reformulation Strategies: Systematic component adjustment demonstrates that conventional LNP paradigms can be reimagined. Research shows cholesterol and phospholipid are dispensable for some applications, with simplified formulations (ionizable lipid + PEG-lipid + permanently cationic lipid) enabling true lung-targeted delivery while reducing hepatic accumulation [46].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key research reagents and technologies for LNP IVIVC studies
| Reagent/Technology | Function | Example Applications |
|---|---|---|
| Ionizable Lipids (SM-102, ALC-0315, MC3, C12-200) | Nucleic acid complexation, endosomal escape | Comparative formulation studies, structure-activity relationship analysis [39] [40] |
| Microfluidic Mixers (NanoAssemblr) | Reproducible LNP formulation | High-throughput LNP library generation, precise size control [39] [42] |
| Reporter mRNAs (Firefly Luciferase, Green Lantern) | Transfection efficiency quantification | In vitro and in vivo potency assessment, biodistribution studies [39] [43] |
| DNA Barcoding Systems | Multiplexed formulation screening | Parallel in vivo evaluation of hundreds of LNPs, tissue-specific delivery assessment [44] [42] |
| PEG-Lipids (DMG-PEG2000, DSG-PEG2000) | LNP stability, circulation time | Investigation of PEG shedding kinetics, stability-performance relationships [47] |
Figure 2: Key intracellular pathways in LNP-mediated mRNA delivery, highlighting the critical endosomal escape step where many formulations fail.
Substantial challenges remain in establishing reliable IVIVC for LNP-based nucleic acid delivery systems. The disconnect stems from fundamental biological differences between simplified in vitro systems and complex in vivo environments, particularly in protein corona formation, cellular uptake mechanisms, and intracellular trafficking. However, emerging technologies—including high-throughput screening, DNA barcoding, machine learning, and rational formulation redesign—show significant promise in bridging this gap. By adopting integrated approaches that combine advanced in vitro models with computational prediction and targeted in vivo validation, researchers can accelerate the development of next-generation LNP therapeutics with more predictable clinical performance.
The pursuit of reliable in vitro to in vivo correlation (IVIVC) remains a central challenge in the development of implantable medical devices and drug delivery systems. Among the critical methodological attributes influencing predictive accuracy, surface-to-volume ratio and water uptake behavior stand out as pivotal physicochemical parameters that dictate implant performance and biological integration. These factors directly impact drug release kinetics, degradation profiles, cellular responses, and ultimately, therapeutic efficacy.
Surface characteristics govern the initial biological interactions at the implant-tissue interface, where protein adsorption and cellular adhesion processes commence [48]. Simultaneously, water uptake capacity influences mechanical stability, degradation rates, and drug release mechanisms, particularly in polymeric systems [49]. The complex interplay between these parameters dictates the host immune response, foreign body reactions, and the success of implant integration [48]. This guide systematically compares experimental approaches for characterizing these critical attributes across diverse implant classes, providing researchers with standardized methodologies to enhance IVIVC predictive power.
Quantitative Comparison of Material Performance
Water Uptake and Mechanical Properties of Dental Composites
Table 1: Water Uptake and Bi-axial Flexure Strength (BFS) of Resin-Based Composites
| Material Type | Filler Characteristics | Water Uptake (μg/mm³) | BFS Reduction After Water Storage | Key Findings |
|---|---|---|---|---|
| Nanofilled (Filtek Supreme) | 5-75 nm particles + 1.3 μm clusters | ~40-45 | ~20% over 6 months | Higher surface area fillers increase water uptake and interface degradation [49] |
| Microhybrid (Filtek Z250) | Conventional microhybrid filler system | ~30-35 | ~15% over 6 months | Lower water uptake correlates with better retention of mechanical properties [49] |
Experimental data reveals that filler morphology significantly influences water sorption behavior in resin-based composites. Nanofilled materials containing nanosized particles (5-75 nm) and porous clusters (~1.3 μm) demonstrated approximately 30% higher water uptake compared to conventional microhybrid composites [49]. This increased susceptibility to hydration directly correlated with greater degradation of the filler-matrix interface and more significant reduction in mechanical strength following prolonged aqueous immersion [49].
Cytotoxicity and Biocompatibility Profile of Orthopedic Biomaterials
Table 2: Cytotoxicity and Biocompatibility Assessment of Magnesium-Based Composites
| Material Composition | Test Method | Cell Viability (%) | Key Cytotoxicity Findings | Application Potential |
|---|---|---|---|---|
| Mg-1%Sn-2%HA composite | Extract assay (MTT) on L-929 fibroblasts | 71.51% (undiluted) | Non-cytotoxic (ISO 10993-5) | Promising biodegradable orthopedic implant [50] |
| Mg-1%Sn-2%HA composite (50% dilution) | Extract assay (MTT) on L-929 fibroblasts | 84.93% | Concentration-dependent viability improvement | Enhanced safety with moderate release profile [50] |
| Mg-1%Sn-2%HA composite (12.5% dilution) | Extract assay (MTT) on L-929 fibroblasts | 96.52% | Near-complete viability at low concentrations | Excellent biocompatibility at physiological concentrations [50] |
The Mg-1%Sn-2%HA composite demonstrates exceptional biocompatibility profiles according to ISO 10993-5 standards. The powder metallurgy-fabricated material showed concentration-dependent cell viability, with undiluted extracts maintaining 71.51% viability in L-929 mouse fibroblast cultures—well above the cytotoxicity threshold [50]. This performance stems from the synergistic combination of tin, which enhances corrosion resistance, and hydroxyapatite, which improves osteoconductivity and surface compatibility [50].
Experimental Protocols for Critical Attribute Characterization
Water Uptake and Mechanical Integrity Assessment
Protocol 1: Gravimetric Water Uptake Determination
- Sample Preparation: Prepare composite disks (approximately 2mm thickness × 15mm diameter) using standardized molding techniques. Condition samples in desiccators until constant mass is achieved (≤0.1mg variation over 24h) [49].
- Hydration Phase: Immerse samples in distilled water maintained at 37°C using an environmental chamber. Remove specimens at predetermined intervals (1, 7, 30, 90, 180 days), blot gently with lint-free cloth to remove surface water, and weigh immediately using analytical balance [49].
- Calculation: Water uptake is calculated as weight percentage increase:
[(Ww - Wd)/Wd] × 100, where Ww represents wet weight and Wd represents initial dry weight. - Data Interpretation: Plot water uptake versus square root of time to assess diffusion kinetics. Fickian diffusion typically demonstrates linear initial relationship [49].
Protocol 2: Bi-axial Flexure Strength (BFS) Testing
- Test Configuration: Utilize ball-on-ring configuration with universal testing machine. Position specimens on 10mm diameter support ring and apply load through 4mm spherical indenter at crosshead speed of 1mm/min [49].
- Hydration Conditioning: Test matched sample sets under both dry (24h desiccation) and wet (30-day aqueous immersion) conditions to quantify water plasticization effects [49].
- Statistical Analysis: Employ two-way ANOVA to evaluate significance of material composition and hydration state on mechanical properties, with post-hoc testing for individual mean comparisons (significance threshold p<0.05) [49].
Surface Wettability and Contact Angle Measurement
Protocol 3: Contact Angle Determination via Sessile Drop
- Sample Preparation: Use implant disks with standardized surface roughness. Clean surfaces with argon plasma treatment to remove hydrocarbon contamination before analysis [51].
- Measurement Conditions: Apply 10μL droplets of testing solutions (saline, artificial blood, albumin solution) using automated micropipette. Measure contact angles immediately upon droplet deposition using goniometer with high-resolution camera [51].
- Environmental Control: Maintain constant temperature (37°C) and humidity (40-50%) throughout measurements. Perform minimum of 15 replicates per condition to ensure statistical reliability [51].
- Data Interpretation: Contact angles <90° indicate hydrophilic surfaces favorable for protein adsorption and cell adhesion, while angles >90° suggest hydrophobic character [51].
Protocol 4: In Vitro Release Testing for Implantable Drug Delivery Systems
- Apparatus Selection: For in situ forming depots (ISFD), employ flow-through cells (USP Apparatus 4) with temperature-controlled reaction chambers filled with agarose hydrogel to constrain depot formation [52].
- Dissolution Media: Use phosphate-buffered saline (PBS, pH 7.4) at physiological temperature (37°C). Maintain continuous buffer flow rates between 1-10 mL/h to simulate in vivo conditions [52].
- Sampling and Analysis: Collect aliquots at predetermined timepoints. Analyze drug content using validated HPLC or UV-Vis spectroscopic methods. Compare release profiles with in vivo pharmacokinetic data to establish correlation [52].
Figure 1: Comprehensive workflow for implant performance characterization integrating surface, hydration, mechanical, and biological assessment toward IVIVC establishment.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Equipment for Implant Testing
| Category | Specific Items | Function/Application | Experimental Relevance |
|---|---|---|---|
| Surface Characterization | Contact angle goniometer | Quantifies surface wettability/hydrophilicity | Critical for predicting protein adsorption and cell adhesion [51] |
| 3D laser confocal microscope | Measures surface roughness parameters (Sa, Sz, Sdr) | Correlates topography with biological response [51] | |
| Mechanical Testing | Universal testing machine | Determines bi-axial flexure strength and compression properties | Quantifies hydration-induced mechanical degradation [49] |
| Biological Assessment | L-929 mouse fibroblast cell line | ISO-standardized cytotoxicity testing (MTT assay) | Essential for biocompatibility screening [50] |
| Artificial blood, albumin solutions | Simulates biological fluid interactions in wettability studies | Provides clinically relevant interface conditions [51] | |
| Hydration Analysis | Precision analytical balance | Gravimetric water uptake measurements | Fundamental for hydration kinetics quantification [49] |
| MRI with UTE sequences | Maps T1/T2* relaxation parameters for bound water | Non-invasive hydration assessment in ECM [53] | |
| Drug Release | Flow-through dissolution apparatus (USP 4) | In vitro release testing for implantable systems | Enhances in vivo predictability for ISFD [52] |
| Agarose hydrogel | Constrains depot formation during dissolution testing | Standardizes surface area for release studies [52] |
Figure 2: Surface-induced foreign body response pathway triggered by protein adsorption and conformational changes.
The systematic characterization of surface-to-volume ratio and water uptake behavior provides critical insights for predicting implant performance and establishing robust IVIVC. Experimental evidence demonstrates that nanoscale surface characteristics significantly influence hydration kinetics, with higher surface area materials exhibiting increased water uptake and corresponding mechanical degradation [49]. Furthermore, surface wettability emerges as a crucial determinant of biological response, with hydrophilic surfaces generally promoting favorable interactions [51].
Standardized methodologies for contact angle measurement, gravimetric water uptake analysis, and flow-through dissolution testing provide reproducible frameworks for comparative material evaluation. The integration of these approaches with biologically relevant assessment techniques—including cytotoxicity screening according to ISO 10993-5 standards and advanced magnetic resonance imaging of hydration states—enables comprehensive implant characterization [50] [53]. Through rigorous application of these optimized critical method attributes, researchers can significantly enhance the predictive accuracy of in vitro models, ultimately accelerating the development of advanced implantable therapies with improved clinical outcomes.
In vitro-in vivo correlation (IVIVC) represents a critical biopharmaceutical tool in drug development, establishing a predictive mathematical relationship between a drug product's in vitro dissolution characteristics and its in vivo performance, typically measured by plasma drug concentration or absorption rate [11] [20]. When successfully validated, IVIVC models can significantly accelerate formulation development, support the setting of clinically relevant dissolution specifications, and potentially serve as surrogates for certain in vivo studies, thereby reducing the number of required human trials [11] [54].
However, the transition from controlled laboratory environments to complex biological systems presents substantial scientific challenges. The fundamental assumption that in vitro release data will closely approximate in vivo performance often fails for complex drug delivery systems, leading to costly late-stage development failures and compromised therapeutic outcomes [20] [55]. This analysis systematically examines the common failure points where in vitro data fails to predict in vivo outcomes, providing researchers with experimental protocols for identifying these pitfalls and data presentation standards for objective comparison across formulation strategies.
Common Failure Points in IVIVC
Physiological and Metabolic Complexity
Table 1: Physiological Factors Contributing to IVIVC Failure
| Failure Factor | Impact on IVIVC | Common Formulations Affected |
|---|---|---|
| Gastrointestinal Variability | Altered dissolution, precipitation, or degradation profiles | Lipid-based formulations, enteric-coated systems |
| Hepatic Metabolism | Unpredicted first-pass metabolism reducing bioavailability | All orally administered drugs, especially high-clearance compounds |
| Transporter Effects | Uptake or efflux not captured in vitro | BCS Class III/IV drugs, targeted delivery systems |
| Disease State Influence | Altered physiology affecting drug disposition | Formulations for chronic conditions (NASH, renal impairment) |
| Food Effects | Altered solubility and dissolution patterns | Lipophilic compounds, lipid-based drug delivery systems |
The dynamic physiological environment into which a drug product is introduced represents perhaps the most significant source of IVIVC failure. Unlike the controlled conditions of in vitro testing, in vivo systems introduce numerous variables including gastrointestinal pH gradients, motility patterns, enzymatic activity, bile salt concentrations, and microbial flora [20] [56]. These factors collectively influence drug release, absorption, and metabolism in ways that are difficult to replicate in laboratory settings.
For lipid-based formulations (LBFs), which are particularly susceptible to physiological variability, the complex interplay of lipid digestion, micelle formation, and lymphatic transport introduces multiple potential failure points [20]. As noted in recent research, "LBFs involve dynamic processes that are not easily captured by traditional in vitro dissolution tests or in silico pharmacokinetic models" [20]. Case studies with fenofibrate demonstrate how in vitro dispersion data failed to distinguish between LBF performance in fasted versus fed states, with no meaningful correlation to in vivo outcomes [20].
Limitations in Current In Vitro Models
Table 2: Limitations of Standard In Vitro Systems
| In Vitro System | Primary Applications | Key Limitations | Impact on IVIVC |
|---|---|---|---|
| USP Dissolution Apparatus | Conventional release testing | Does not simulate GI hydrodynamics, absorption, or metabolism | Overestimation of bioavailability for poorly soluble drugs |
| pH-Stat Lipolysis Models | Lipid-based formulations | Variable reproducibility, limited predictive capacity for complex formulations | 50% failure rate in correlating with in vivo data [20] |
| Caco-2 Monolayers | Permeability assessment | Limited metabolic competence, absence of mucus layer | Misprediction of absorption and transporter effects |
| Liver Microsomes/S9 Fractions | Metabolic clearance prediction | Short lifespan, lack of transporter interplay | Underprediction of clearance, especially for low-turnover drugs |
| Suspended Hepatocytes | Hepatic clearance estimation | Rapid decline in enzyme and transporter activity | Inaccurate IVIVE for slowly metabolized compounds |
Traditional in vitro models suffer from significant limitations that compromise their predictive power for in vivo performance. Standard dissolution apparatuses (USP I-IV) provide valuable quality control data but fail to replicate the complex biorelevant conditions of the gastrointestinal tract, including the absorption process that drives sink conditions in vivo [20]. For metabolism assessments, standard in vitro systems like liver microsomes and suspended hepatocytes have short functional lifespans that preclude accurate measurement of clearance for slowly metabolized compounds [56].
The translation of in vitro dissolution data to in vivo absorption becomes particularly problematic for specialized drug delivery systems. Research on multilayered polymer devices for sequential drug delivery demonstrated that while the sequential release pattern was maintained in vivo, the total erosion time was significantly prolonged and release rates differed substantially from in vitro predictions [55]. Specifically, "drugs [were] initially released more quickly and then more slowly in vivo" compared to in vitro projections [55].
Methodological and Statistical Pitfalls
Table 3: Methodological Pitfalls in IVIVC Development
| Methodological Issue | Consequence | Recommended Solution |
|---|---|---|
| Use of Mean Data | Loss of individual variability information | Individual deconvolution approaches where appropriate |
| Inadequate Time Scaling | Misalignment of in vitro and in vivo release profiles | Implementation of validated time-scaling functions |
| Improper Bioavailability Correction | Artificial inflation of correlation quality | Avoidance of correction factors without physiological basis |
| Flip-Flop Kinetics Misinterpretation | Confusion of absorption and elimination rates | Comprehensive pharmacokinetic modeling |
| Overreliance on Correlation Coefficients | False confidence in predictive power | Focus on prediction errors and internal validation |
Statistical and methodological approaches to IVIVC development introduce their own failure modes. The common practice of using mean dissolution and plasma concentration data, while convenient, results in significant information loss, particularly regarding inter-individual variability [11]. This approach becomes particularly problematic for formulations with highly variable gastrointestinal residence times, such as enteric-coated products where gastric emptying rates largely determine absorption kinetics [11].
The selection of inappropriate correlation levels represents another common failure point. While Level A correlation (point-to-point relationship between in vitro dissolution and in vivo input rate) represents the gold standard for regulatory purposes, it is often unattainable for complex formulations [20] [54]. In such cases, researchers may resort to Level B (comparing mean dissolution time to mean residence time) or Level C (single-point correlation) relationships, which provide substantially less predictive power and regulatory utility [20].
Statistical significance presents another potential trap, as a statistically significant correlation does not necessarily imply predictive relevance. As noted in analyses of correlation coefficients, "A statistically significant correlation does not necessarily mean that the strength of the correlation is strong. The p-value shows the probability that this strength may occur by chance" [57]. A correlation coefficient of 0.31 may have the same statistical significance (p < 0.0001) as a coefficient of 0.64, yet the former represents only a weak relationship while the latter indicates a moderate to strong correlation [57].
Experimental Protocols for Assessing IVIVC Failure Points
Protocol for Evaluating Physiological Variability Impact
Objective: To quantify the impact of physiological variables on formulation performance and identify potential IVIVC failures.
Materials:
- Test formulations (multiple lots with controlled variations)
- USP dissolution apparatus with biorelevant media
- pH-stat lipolysis setup (for LBFs)
- Animal model (typically rodent) or human subjects
- Validated bioanalytical method (LC-MS/MS preferred)
Methodology:
- Conduct in vitro dissolution testing using progressively biorelevant media (fasted-state simulated intestinal fluid [FaSSIF], fed-state simulated intestinal fluid [FeSSIF], and their counterparts with added digestive enzymes)
- For LBFs, perform pH-stat lipolysis experiments to simulate intestinal lipid digestion
- Administer formulations to appropriate animal models or human subjects under standardized conditions
- Collect serial blood samples for pharmacokinetic analysis
- Compare in vitro release profiles with in vivo absorption profiles using deconvolution or convolution-based approaches
Data Analysis:
- Calculate prediction errors for C~max~ and AUC using established formulas [54]
- Apply time-scaling functions if necessary to align in vitro and in vivo profiles [11] [54]
- Perform internal validation with acceptance criteria of average %PE ≤ 10% with no individual values > 15% [54]
Protocol for Assessing In Vitro Model Limitations
Objective: To evaluate the predictive limitations of specific in vitro systems for particular formulation types.
Materials:
- Test compounds with known in vivo behavior (positive controls)
- Multiple in vitro systems (traditional dissolution, advanced biorelevant models)
- Plated hepatocyte systems with extended functionality
- Appropriate analytical instrumentation
Methodology:
- Test compounds across multiple in vitro systems with varying complexity
- For clearance predictions, compare traditional suspended hepatocytes with more advanced systems (plated hepatocytes, 3D cultures, relay methods)
- For complex formulations, incorporate absorption sinks and hydrodynamics that better simulate in vivo conditions
- For low-solubility compounds, include methods to maintain sink conditions without artificial surfactants
Data Analysis:
- Calculate intrinsic clearance values from each system
- Perform IVIVE using appropriate scaling factors
- Compare predicted versus observed in vivo clearance values
- Identify systematic biases (underprediction/overprediction) for specific compound classes
Diagram 1: Primary Pathways to IVIVC Failure. This diagram illustrates how in vitro data fails to predict in vivo outcomes through three primary failure pathways, ultimately manifesting as PK/PD disconnects.
Advanced Modeling Approaches to Overcome IVIVC Limitations
Convolution-Based Modeling Techniques
Convolution-based modeling represents a sophisticated approach to IVIVC that avoids many pitfalls of traditional deconvolution methods. This methodology translates convolution integrals into systems of differential equations, creating a single-stage approach that utilizes observed data directly without transformation [54]. The fundamental equation for this approach is:
C~p~(t) = f(t) * I(t)
Where C~p~(t) is the plasma concentration at time t, f(t) is the in vivo input function, I(t) is the unitary impulse response, and * is the convolution operator [54].
This method enables direct prediction of plasma concentration-time courses resulting from specific in vivo input functions, allowing researchers to explore various formulation strategies in silico before committing to costly manufacturing and clinical trials [54]. Implementation typically includes time-scaling functions to account for differences between in vitro and in vivo processes:
r~vivo~(t) = a~1~ + a~2~ · r~vitro~(t~t~) t~t~ = b~1~ + b~2~ · t^b3^
Where r~vivo~(t) and r~vitro~(t) represent the fraction of drug absorbed in vivo and dissolved in vitro, respectively, and the parameters a~1~, a~2~, b~1~, b~2~, and b~3~ define the relationship between them [54].
Finite Element Analysis for Predictive Modeling
In specialized applications such as orthopedic implants, finite element analysis (FEA) and micro-finite element (μFE) models have shown promise in predicting in vivo performance when validated with appropriate in vivo loading data [58] [59]. These approaches combine medical imaging with computational modeling to simulate mechanical behavior under physiological loads.
Recent advances incorporate implantable sensors, such as the AO Fracture Monitor, which provides continuous tracking of implant deformation as a proxy for loading conditions [58]. This methodology achieved 100% sensitivity in predicting plate bending outcomes in a preclinical ovine model, demonstrating how combining real-time in vivo data with computational models can significantly improve predictive accuracy [58].
Diagram 2: Convolution-Based IVIVC Workflow. This diagram illustrates the mathematical workflow for implementing convolution-based IVIVC models, highlighting the critical time-scaling function and validation steps.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for IVIVC Studies
| Reagent/Material | Primary Function | Application Context | Key Considerations |
|---|---|---|---|
| Biorelevant Media (FaSSIF/FeSSIF) | Simulate gastrointestinal fluids | Dissolution testing for oral formulations | Must be prepared fresh; composition varies by fed state |
| pH-Stat Apparatus | Monitor and maintain pH during lipolysis | Lipid-based formulation development | Requires standardized enzyme concentrations |
| Plated Hepatocyte Systems | Predict hepatic clearance | IVIVE for metabolically labile compounds | Superior to suspended hepatocytes for prolonged incubations |
| Caco-2 Cell Lines | Assess intestinal permeability | BCS classification, absorption potential | Requires 21-day differentiation; highly variable between labs |
| USP Dissolution Apparatus | Standardized drug release testing | Quality control, formulation comparison | Limited biorelevance but essential for regulatory compliance |
| LC-MS/MS Systems | Bioanalytical quantification | PK studies, metabolite identification | Requires rigorous validation; sensitivity to matrix effects |
| 3D Hepatocyte Cultures | Improved metabolic competence | Low-clearance compound assessment | Better preservation of transporter function |
| AO Fracture Monitor | Track implant deformation in vivo | Orthopedic device performance | Provides real-time loading data for FEA validation [58] |
The failure of in vitro data to accurately predict in vivo outcomes remains a significant challenge in drug development, particularly for complex formulations like lipid-based systems, extended-release products, and specialized delivery devices. The common failure points identified in this analysis—physiological complexity, model limitations, and methodological pitfalls—collectively highlight the need for more sophisticated, biorelevant approaches to IVIVC development.
Moving forward, successful IVIVC implementation requires careful consideration of formulation-specific challenges, application of advanced modeling techniques like convolution-based approaches, and rigorous validation using appropriate statistical metrics beyond simple correlation coefficients. By systematically addressing these failure points through the protocols and frameworks presented herein, researchers can improve the predictive power of in vitro testing, ultimately accelerating the development of safe and effective drug products while reducing the ethical and financial costs associated with poorly predictive models.
In vitro-in vivo correlation (IVIVC) is a critical scientific tool in drug development, establishing a predictive relationship between a drug product's in vitro dissolution profile and its in vivo pharmacokinetic behavior [3]. For conventional formulations, this relationship is often straightforward, with dissolution serving as the rate-limiting step for absorption. However, lipid-based formulations (LBFs) present unique challenges for IVIVC due to the complex interplay of digestion, permeation, and dynamic solubilization processes that occur following oral administration [4]. These formulations, which include self-emulsifying drug delivery systems (SEDDS) and various lipid nanoparticles, are particularly valuable for enhancing the oral bioavailability of poorly water-soluble drugs classified under the Biopharmaceutics Classification System (BCS) Class II and IV [4] [60].
The fundamental challenge lies in the fact that traditional dissolution methods fail to capture the dynamic transformations LBFs undergo in the gastrointestinal tract. After administration, lipid excipients are subject to digestion by gastric and pancreatic lipases, altering the physicochemical environment and potentially affecting drug solubilization [4] [61]. This dynamic process can lead to unexpected drug precipitation or supersaturation, creating discrepancies between in vitro predictions and in vivo performance [4]. Consequently, developing tailored IVIVC strategies that account for these complex processes is essential for optimizing LBF design, reducing development costs, and securing regulatory approval. This guide systematically compares the performance of different LBF strategies under these complex biophysical conditions, providing researchers with experimental data and methodologies to advance predictive modeling.
LBF Classification and Performance Under Digestive Conditions
Lipid-based formulations are categorized according to the Lipid Formulation Classification System (LFCS), which groups them based on composition and their expected behavior upon dispersion and digestion [4].
- Type I: Simplest formulations comprising oils (e.g., triglycerides). They require digestion for efficient drug release.
- Type II: Include oils and lipophilic surfactants (low HLB). Formulate water-insoluble drugs.
- Type III: More complex systems containing oils, hydrophilic surfactants (high HLB), and potentially co-solvents. They are further divided into IIIA (more oils) and IIIB (more surfactants/co-solvents). These systems self-emulsify but are still influenced by digestion.
- Type IV: Formulations containing only surfactants and co-solvents without traditional lipids [4].
The performance of these different classes is highly dependent on their interaction with the gastrointestinal environment. The following table summarizes key findings from recent studies on how different LBFs respond to digestive processes.
Table 1: Comparison of Lipid-Based Formulation Performance Under Digestive Conditions
| Formulation Type / Model Drug | Key Experimental Variable | Impact on Drug Exposure (AUC) & Peak Concentration (Cmax) | Observed Role of Digestion & Key Findings |
|---|---|---|---|
| Type IIIA LBFs / Cinnarizine [61] | Lipid chain length (Long vs. Medium) | Similar drug exposure between Long-Chain (LC) and Medium-Chain (MC) systems. | Digestion was critical; lipase inhibition reduced AUC by 28-35% for LC systems. |
| Type IIIA LBFs / Cinnarizine [61] | Supersaturation | AUC: 72-178% increase Cmax: 45-130% increase | Supersaturation was beneficial but required management of precipitation. |
| Type IIIA LBFs / Cinnarizine [61] | Addition of Polymer (Soluplus) | Beneficial only for non-supersaturated LBFs ( AUC 26-34%) and specific MC systems. | Precipitation inhibitor had a variable effect, dependent on the base formulation. |
| Various LBFs / Fenofibrate [4] | In vitro lipolysis model vs. in vivo (rat) | In vitro data failed to correlate with or predict in vivo performance in fasted/fed states. | Highlighted the limited predictability of static in vitro models for complex LBFs. |
| Various LBFs / 8 Different Drugs [4] | pH-stat lipolysis assay | Only 50% of the studied drugs showed a good correlation with in vivo data. | Underscored the need for more sophisticated and tailored in vitro models. |
Essential Experimental Protocols for Predictive IVIVC
To build a robust IVIVC for LBFs, in vitro experiments must move beyond standard dissolution and incorporate biorelevant dynamics. The following protocols are central to this approach.
In Vitro Lipolysis Assay
The lipolysis assay is a pivotal experiment for simulating the enzymatic digestion of lipids in the small intestine, a process that fundamentally alters drug solubilization [4].
- Objective: To monitor the dynamic changes in drug concentration and distribution in different phases (aqueous, precipitate, oil) during the digestion of a lipid formulation.
- Materials:
- Lipase Enzyme: Typically porcine pancreatic extract (e.g., from Sigma-Aldrich) to provide digestive enzymes.
- Digestion Buffer: Tris-maleate buffer (pH 6.5) to simulate intestinal pH.
- Bile Salts: Sodium taurodeoxycholate (e.g., from Calbiochem) to mimic fed-state intestinal fluids.
- Calcium Chloride Solution: CaCl₂ (e.g., 0.5 M, from Merck) is added continuously or step-wise to drive the precipitation of fatty acids and simulate in vivo kinetics.
- Apparatus: A thermostatted vessel (37°C) with continuous pH titration (pH-stat) and stirring. In-line UV probes (e.g., MicroDISS Profiler) can be used for real-time concentration monitoring [62].
- Methodology:
- The digestion medium is prepared with buffer, bile salts, and lipase, and the temperature is maintained at 37°C.
- The LBF is introduced into the medium.
- Digestion is initiated by adding a calcium chloride solution.
- The pH is maintained constant by the automatic titration of sodium hydroxide, which neutralizes the fatty acids produced. The consumption of NaOH is a direct measure of the extent of digestion.
- At predetermined time points, samples are withdrawn and ultracentrifuged to separate the aqueous phase, the pellet (precipitated drug), and the oily phase. Drug concentration in each phase is quantified via HPLC [4] [61].
Supersaturation and Precipitation Inhibition Testing
This protocol evaluates a formulation's tendency to generate and maintain a supersaturated state, which is a key mechanism for enhancing absorption, and tests the efficacy of precipitation inhibitors.
- Objective: To assess the kinetic solubility profile of a drug from a LBF and the ability of polymers (e.g., Soluplus) to inhibit drug precipitation.
- Materials:
- Precipitation Inhibitor: Polymers such as Soluplus (BASF), HPMC, or PVP.
- Aqueous Buffer: Biorelevant media (e.g., FaSSIF/FeSSIF) or standard phosphate buffer.
- Analytical Instrumentation: USP Apparatus II (paddles) with in-line UV probes or HPLC for concentration measurement.
- Methodology:
- The LBF, with and without the precipitation inhibitor, is introduced to the dissolution medium under gentle agitation (e.g., 75 rpm) at 37°C.
- The formulation disperses, leading to a rapid increase in dissolved drug concentration, often creating a supersaturated state.
- The drug concentration is monitored in real-time over several hours. The area under the concentration-time curve (AUC) is calculated to quantify the extent and duration of supersaturation [61].
- The performance is compared between formulations with and without inhibitors, and against a non-supersaturated control.
Table 2: Research Reagent Solutions for Lipid Formulation Digestion and Solubilization Studies
| Reagent / Material | Function in Experiment | Application Example |
|---|---|---|
| Porcine Pancreatic Lipase Extract | Mimics the enzymatic digestion of triglycerides in the small intestine. | Core enzyme in the in vitro lipolysis assay to digest lipid-based formulations [4]. |
| Sodium Taurodeoxycholate | A bile salt used to simulate the fed-state intestinal environment and support micelle formation. | Component of biorelevant digestion media to solubilize lipolytic products [4]. |
| Soluplus | A polymeric precipitation inhibitor that stabilizes supersaturated drug solutions. | Added to LBFs to prolong the duration of supersaturation and improve absorption [61]. |
| Tris-Maleate Buffer | Maintains a constant pH (typically 6.5) during lipolysis to simulate intestinal conditions. | Standard buffer system used in pH-stat lipolysis experiments [4]. |
| Polyglycerol Fatty Acid Esters (PGFAs) | Versatile lipid excipients with tunable HLB values that can improve drug loading and wettability. | Used as a component in solid lipid matrices to enhance dispersion and API release [63]. |
Computational and Modeling Approaches
Computational pharmaceutics is increasingly used to predict LBF behavior and support IVIVC, reducing the need for extensive experimental screening.
- Physiologically Based Biopharmaceutics Modeling (PBBM): PBBM integrates the drug's physicochemical properties, formulation characteristics, and human physiology to simulate and predict in vivo absorption. For LBFs, these models can incorporate digestion and supersaturation parameters. When combined with a Level A IVIVC, PBBM can be used to establish patient-centric quality standards and a "safe space" for dissolution specifications [12].
- Multivariate Data Analysis: Techniques like Partial Least Squares (PLS) regression can identify molecular descriptors (e.g., melting point, LogD, number of aromatic rings) that predict how a drug's solubility will change during LBF dispersion and digestion. Multiple linear regression models based on these descriptors have shown good predictivity for solubility ratios pre- and post-digestion [62].
The following diagram illustrates the integrated workflow for developing a predictive IVIVC for lipid-based formulations, combining experimental and computational strategies.
Figure 1: Integrated IVIVC Workflow for Lipid-Based Formulations. This diagram outlines a systematic approach for correlating in vitro performance with in vivo outcomes for LBFs, highlighting the critical role of dynamic digestion and solubilization tests.
Establishing a robust IVIVC for lipid-based formulations requires a paradigm shift from traditional dissolution testing to a more holistic, physiology-oriented approach. As the experimental data and protocols in this guide demonstrate, accounting for lipid digestion, dynamic solubilization, and the potential for supersaturation is non-negotiable for accurate in vivo performance prediction.
The future of IVIVC for LBFs lies in the deeper integration of advanced in vitro tools—such as more sophisticated lipolysis models and permeability assays—with computational modeling, including PBBM and AI-driven analytics [3]. This powerful combination will enable researchers to create a "digital twin" of formulation performance, accelerating the development of robust and effective lipid-based drug products for poorly soluble compounds. By adopting these tailored strategies, scientists can bridge the predictive gap between the laboratory and the human body, ultimately ensuring the delivery of safe, effective, and high-quality medicines.
Ensuring Predictive Power: IVIVC Model Validation and Comparative Analysis
In vitro-in vivo correlation (IVIVC) is a fundamental tool in pharmaceutical development, serving as a predictive model that relates the dissolution of a drug product (in vitro) to its pharmacokinetic behavior in the body (in vivo) [12]. A successfully developed and validated IVIVC model can reduce the need for costly and time-consuming bioequivalence studies, support formulation development, and help establish clinically relevant dissolution specifications [64]. The validation of these models, particularly through the assessment of prediction errors for key pharmacokinetic parameters like maximum plasma concentration (Cmax) and area under the plasma concentration-time curve (AUC), is critical for establishing regulatory confidence and ensuring therapeutic performance.
The assessment of predictive performance occurs through two distinct validation processes: internal and external validation. Internal validation evaluates the model's predictability using the same data from which the model was developed, while external validation tests the model's performance on an entirely independent dataset not used in model development [64]. For both validation types, regulatory agencies have established specific criteria for prediction errors of Cmax and AUC, which form the cornerstone of IVIVC model acceptance.
Fundamental Principles of IVIVC Validation
Validation Criteria and Prediction Error Thresholds
Regulatory guidance for IVIVC validation establishes clear thresholds for prediction accuracy. For internal validation, the average absolute percent prediction error (%PE) for both AUC and Cmax should be ≤15% for each formulation, and the overall average %PE across all formulations should be ≤10% [64]. External validation requires even stricter precision, with prediction errors ≤10% for each parameter to demonstrate the model's robustness when applied to new data [64].
The prediction error is calculated using the following formula: %PE = |(Observed Value - Predicted Value)| / Observed Value × 100%
This quantitative assessment ensures that IVIVC models can reliably predict in vivo performance from in vitro data, providing a surrogate for bioequivalence testing in certain regulatory contexts.
Comparison of IVIVC Modeling Approaches
Two primary mathematical approaches exist for developing IVIVC models: the deconvolution-based method and the convolution-based method. The deconvolution-based approach establishes a point-to-point relationship between the fraction dissolved in vitro and the fraction absorbed in vivo, requiring the use of a reference formulation to determine the unit impulse response [64]. In contrast, the convolution-based approach incorporates the convolution integral and directly uses the in vitro dissolution profile as an input function to predict plasma concentration-time profiles [64].
Table 1: Comparison of IVIVC Modeling Techniques and Their Predictive Performance
| Modeling Approach | Mathematical Foundation | Data Requirements | Prediction Accuracy | Key Limitations |
|---|---|---|---|---|
| Deconvolution-Based | Relates in vitro dissolution to in vivo dissolution (deconvolution of plasma data) | In vitro dissolution data, plasma concentration data for test and reference formulations | Can yield inaccurate predictions; more susceptible to error propagation [64] | Dependent on reference formulation; deconvolution amplifies experimental errors |
| Convolution-Based | Uses convolution integral with in vitro dissolution as input function | In vitro dissolution data, plasma concentration data for test formulations only | Provides more precise predictions of in vivo profiles [64] | Requires assumption of linear, time-invariant system |
Experimental Protocols for Validation
Standard Methodology for IVIVC Development and Validation
The establishment of a predictive IVIVC follows a systematic experimental workflow that integrates in vitro dissolution testing with in vivo pharmacokinetic studies. The following diagram illustrates this comprehensive process:
Formulation Development and Dissolution Testing
The IVIVC development process typically begins with the preparation of at least three formulations with different release rates (fast, medium, and slow) to establish a meaningful correlation across a range of dissolution profiles [64]. Dissolution testing should be conducted using appropriate apparatus (USP I, II, III, or IV) under various physiologically relevant conditions, including different pH media and agitation speeds, to capture the formulation's release characteristics across gastrointestinal conditions [12]. Multiple time points should be collected to adequately characterize the dissolution profile, with a minimum of 12 individual units tested per formulation to ensure statistical reliability.
Clinical Study Design and Bioanalysis
A crossover study design is typically employed where each subject receives all test formulations and an oral solution or immediate-release reference product, with adequate washout periods between administrations [64]. Frequent blood sampling is essential to properly characterize the plasma concentration-time profile, with sampling times designed to capture the absorption, distribution, and elimination phases. Bioanalytical methods (typically LC-MS/MS) must be validated according to regulatory standards to ensure accurate quantification of drug concentrations in biological matrices. From the concentration-time data, primary pharmacokinetic parameters (Cmax, AUC0-t, AUC0-∞) are calculated using non-compartmental analysis.
Model Development and Validation Procedures
For deconvolution-based IVIVC, the in vivo dissolution or absorption time course is determined from plasma concentration data using mathematical deconvolution techniques, with the reference formulation providing the unit impulse response [64]. The relationship between in vitro dissolution and in vivo dissolution is then established using linear or nonlinear regression models. For convolution-based approaches, the in vitro dissolution profile is used directly as the input function in a convolution integral to predict plasma concentrations, with pharmacokinetic parameters estimated from the unit impulse response data [64].
Internal validation involves using the developed IVIVC model to predict the in vivo performance of the formulations used in model development, with calculation of prediction errors for Cmax and AUC [64]. External validation tests the model on a completely independent formulation not used in model development, providing a more rigorous assessment of predictive performance [64].
Comparative Analysis of Prediction Error Assessment
Case Study: Linezolid Cmax vs. Trough Concentration Models
A comparative study evaluating different prediction approaches for linezolid pharmacokinetics demonstrated significant differences in prediction accuracy between models based on Cmax versus trough plasma concentration (Ctrough). The research established linear regression models for both Cmax versus AUC and Ctrough versus AUC relationships, with both models initially showing excellent correlation (r > 0.9760) [65]. However, when assessing prediction accuracy, the Ctrough model demonstrated superior performance, with 78.3% of AUC predictions falling within the acceptable 0.76 to 1.5-fold range compared to only 48.2% for the Cmax model [65].
Table 2: Prediction Accuracy Comparison for Linezolid PK Models
| Prediction Model | Correlation Coefficient (r) | Root Mean Square Error (%) | % Predictions within 0.76-1.5 fold | Suitable for Prospective AUC Prediction |
|---|---|---|---|---|
| Cmax vs. AUC | 0.9760 | 61.34 | 48.2 | No |
| Ctrough vs. AUC | 0.9031 | 28.54 | 78.3 | Yes |
The superior predictive performance of the trough concentration model for linezolid highlights the importance of selecting appropriate sampling points for IVIVC development, with the conclusion that a single time point strategy using Ctrough level provides an effective prospective tool for predicting linezolid AUC in patient populations [65].
Convolution vs. Deconvolution Method Performance
A comprehensive simulation study directly compared the prediction accuracy of convolution-based and deconvolution-based IVIVC modeling techniques across four formulations with different release rates (fast, medium, slow, and external validation) [64]. The results demonstrated markedly different performance between the two approaches.
Table 3: Prediction Error Comparison Between IVIVC Methodologies
| Formulation | Parameter | Deconvolution Method %PE | Convolution Method %PE |
|---|---|---|---|
| Fast Release | Cmax | 21.7 | 0.2 |
| AUC | 16.5 | 0.5 | |
| Medium Release | Cmax | 17.8 | 0.7 |
| AUC | 13.9 | 0.4 | |
| Slow Release | Cmax | 14.6 | 0.4 |
| AUC | 11.2 | 0.3 | |
| External Validation | Cmax | 23.1 | 0.8 |
| AUC | 18.7 | 0.6 |
The convolution-based approach consistently demonstrated superior predictive accuracy, with all prediction errors below 1% compared to the deconvolution-based method which exceeded the 15% threshold for both Cmax and AUC in multiple cases [64]. This significant performance difference highlights the potential advantages of convolution-based methodologies in IVIVC development, particularly their reduced error propagation compared to deconvolution techniques.
Advanced Applications and Integrated Approaches
Integration with Physiologically Based Biopharmaceutics Modeling (PBBM)
Recent advances in IVIVC have incorporated physiologically based biopharmaceutics modeling (PBBM) to establish patient-centric quality standards for dissolution. This integrated approach was successfully demonstrated for lamotrigine extended-release tablets, where a Level A IVIVC was developed using in vitro dissolution data from both biorelevant and compendial media coupled with in vivo pharmacokinetic data [12]. The validated IVIVC was then integrated with a PBBM to establish clinically relevant dissolution specifications that ensure product quality and performance throughout the product lifecycle, reducing the need for additional bioequivalence studies during scale-up and post-approval changes [12].
Amorphous Solid Dispersion Formulations
IVIVC development has been successfully extended to complex formulation strategies such as amorphous solid dispersions, as demonstrated by recent research on itraconazole tablets [14]. The study developed an FDA Level A IVIVC that met internal predictability requirements, using a direct differential-equation-based approach with an oral solution as reference for post-dissolution disposition [14]. This work represented a significant advancement as the first reported successful development of an FDA Level A IVIVC for an amorphous solid dispersion, assessing the impact of polymer grades, disintegrant levels, and dry granulation processing on human pharmacokinetic performance [14].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Materials for IVIVC Studies
| Reagent/Material | Specification | Function in IVIVC Research |
|---|---|---|
| Test Formulations | Fast, medium, and slow release profiles | Provides dissolution rate range for correlation development |
| Reference Formulation | Oral solution or immediate-release product | Provides unit impulse response for deconvolution |
| Dissolution Media | Biorelevant (FaSSGF, FaSSIF, FeSSIF) and compendial buffers (pH 1.2-7.4) | Simulates gastrointestinal environment for in vitro testing |
| LC-MS/MS System | Validated bioanalytical method with appropriate sensitivity | Quantifies drug concentrations in biological samples |
| Pharmacokinetic Software | WinNonlin, NONMEM, or similar | Performs non-compartmental analysis and modeling |
| IVIVC Modeling Software | R, MATLAB, or specialized IVIVC packages | Implements deconvolution/convolution algorithms and statistical analysis |
The assessment of prediction errors for Cmax and AUC through rigorous internal and external validation processes remains fundamental to establishing credible IVIVC models. The evidence demonstrates that modeling approach selection significantly impacts predictive accuracy, with convolution-based methods and trough concentration sampling strategies showing particular promise for enhanced predictability. As IVIVC methodologies continue to evolve through integration with PBBM and application to increasingly complex drug products, the core validation principles of assessing prediction errors against established regulatory thresholds will continue to ensure the scientific rigor and regulatory utility of these important predictive tools.
Comparative Analysis of IVIVE Methods for Predicting Hepatic Metabolic Clearance
In vitro to in vivo extrapolation (IVIVE) represents a critical paradigm in modern drug development, enabling researchers to predict human hepatic metabolic clearance using data generated from in vitro systems. The accuracy of these predictions directly impacts lead optimization, dosing regimen design, and the assessment of potential drug-drug interactions. This guide provides a comparative analysis of the fundamental IVIVE methodologies, evaluating their underlying principles, performance characteristics, and appropriate contexts for application. As regulatory agencies increasingly support approaches that reduce reliance on animal testing, mastering these predictive models has become indispensable for pharmaceutical scientists [66] [3].
Fundamental IVIVE Concepts and Models
Core Principles of Hepatic Clearance Prediction
IVIVE for hepatic clearance aims to bridge data from relatively simple in vitro systems—such as liver microsomes or hepatocytes—to quantitative predictions of in vivo drug disposition. The process typically involves two key steps: first, measuring the intrinsic clearance (CLint) in vitro; second, applying physiologically based scaling factors and a mathematical model of hepatic disposition to estimate in vivo hepatic clearance (CLH) [67]. The well-stirred model (WSM) is the most widely implemented framework for this extrapolation, though several alternative models have been developed to address its limitations [68] [69].
A significant challenge in IVIVE is the consistent underestimation bias observed in predictions. Studies systematically evaluating this bias have found a 3- to 10-fold systematic error, where in vivo clearance is under-predicted from in vitro data [68] [67]. This bias remains partially unresolved and may stem from various factors including unaccounted transporter effects, inappropriate model selection, or discrepancies between in vitro and in vivo conditions [68].
Classification of Hepatic Clearance Models
Several mathematical models have been established for predicting hepatic clearance, each based on different assumptions about liver physiology and drug disposition:
- Well-Stirred Model (WSM): Treats the liver as a single, well-stirred compartment where drug concentration in the liver is uniform and in instantaneous equilibrium with effluent blood. It is the most widely used model due to its mathematical simplicity [68] [69].
- Parallel-Tube Model (PTM): Conceptualizes the liver as a series of parallel tubes lined with hepatocytes, creating a concentration gradient along the sinusoids.
- Dispersion Model (DM): Introduces a dispersion number to characterize the degree of mixing in the liver, bridging the extremes of the well-stirred and parallel-tube models.
- Modified Well-Stirred Model (MWSM): A recently refined version that may provide more precise predictions for specific drugs, particularly those sensitive to protein binding [69].
The following diagram illustrates the logical decision process for selecting an appropriate IVIVE model based on drug characteristics:
Comparative Analysis of IVIVE Methodologies
Model Performance Across Drug Classes
The predictive performance of IVIVE models varies significantly depending on the physicochemical and pharmacokinetic properties of the drug being evaluated. Research has demonstrated that the Biopharmaceutics Drug Disposition Classification System (BDDCS) can serve as a determinant for predicting IVIVE accuracy [68]. The following table summarizes the key characteristics and performance metrics of the primary hepatic clearance models:
Table 1: Comparative Performance of Hepatic Clearance Models
| Model | Key Equation | Best For Drug Class | Accuracy Limitations | Experimental Evidence |
|---|---|---|---|---|
| Well-Stirred Model (WSM) | CLH = (QH × fu × CLint) / (QH + fu × CLint) |
Flow-limited drugs (e.g., fluoxetine) [69] | Under-predicts clearance of drugs with hepatic uptake transporters; 3-10 fold systematic error [68] [67] | Standard model used in 7 major studies; accurate for BDDCS Class 1 compounds [68] |
| Modified Well-Stirred Model (MWSM) | CLH = fu × CLint |
Capacity-limited, binding-sensitive drugs (e.g., rosuvastatin) [69] | Limited validation across diverse drug classes | 48.59% better prediction for rosuvastatin vs. 19.95% for WSM in logistic regression analysis [69] |
| Parallel-Tube Model (PTM) | CLH = QH × (1 - e^(-fu × CLint/QH)) |
Drugs with low extraction ratios | Similar limitations to WSM for transporter-affected drugs | Less commonly applied in recent studies [68] |
| Dispersion Model (DM) | Complex equation involving dispersion number | Theoretical interest | Computationally complex with limited practical advantage | Limited contemporary application in drug development [68] |
Advanced IVIVE Systems and Approaches
Recent innovations in IVIVE methodology have focused on developing more physiologically relevant systems that better capture the complexity of in vivo drug disposition:
Biomimetic Single-Well System: This patented system employs a porous mesh-based design with various pore sizes to simultaneously assess drug diffusion and cellular metabolism. The system incorporates HepaRG cells and uses a Weibull distribution equation to model diffusion kinetics, enabling simultaneous analysis of absorption and metabolism phases [66].
Integrated IVIVE-PBPK Workflow: Combining IVIVE with physiologically-based pharmacokinetic (PBPK) modeling creates a powerful framework for predicting human pharmacokinetics. This approach incorporates in vitro parameters such as permeability and metabolic rates into whole-body models, improving prediction accuracy while reducing reliance on animal testing [66] [3].
Case-Specific Model Selection: Recent research emphasizes that model selection should be driven by drug-specific characteristics. For instance, a multinomial logistic regression analysis based on 16 physicochemical and pharmacokinetic parameters from 223 compounds can guide optimal model selection, particularly for challenging capacity-limited, binding-sensitive drugs like diazepam, diclofenac, and rosuvastatin [69].
Experimental Protocols and Methodologies
Standard IVIVE Protocol for Hepatic Clearance Prediction
The following detailed methodology outlines the core experimental workflow for predicting hepatic clearance using in vitro systems:
In Vitro System Selection and Preparation:
- Choose appropriate metabolic system (human liver microsomes or cryopreserved human hepatocytes) based on research objectives
- For hepatocytes: Culture HepaRG cells in Williams E medium supplemented with 10% FBS, 1% antibiotic-antimycotic solution, ITS-G supplement, 1% GlutaMAX-I, and 8.65 μM hydrocortisone hemisuccinate [66]
- Determine protein concentration and cell viability before experiments
Intrinsic Clearance (CLint) Measurement:
- Incubate test compounds at physiological concentration (typically 1-10 μM) with the metabolic system
- Maintain conditions at 37°C with appropriate oxygenation
- Collect samples at predetermined time points (e.g., 0, 5, 15, 30, 60, 90 minutes)
- Terminate reactions with acetonitrile or other appropriate solvent
- Analyze parent compound disappearance using LC-MS/MS
- Calculate CLint from the disappearance rate constant [67]
IVIVE to Predict Human Hepatic Clearance:
- Scale in vitro CLint to in vivo values using physiological scaling factors:
- Microsomes: Apply microsomal recovery factor
- Hepatocytes: Use hepatocellularity factor (e.g., 99-120 million cells/g liver)
- Apply appropriate liver model (WSM, MWSM, etc.) using human hepatic blood flow (QH = 20.7 mL/min/kg) and plasma protein binding (fu) data [68] [69]
- Verify predictions with commercial compounds with established human PK data
- Scale in vitro CLint to in vivo values using physiological scaling factors:
Model Selection Validation Protocol
For challenging compounds where the appropriate model is uncertain, the following validation protocol is recommended:
In Silico Analysis:
- Compile comprehensive physicochemical and PK parameters (logP, molecular weight, fu, etc.)
- Apply multinomial logistic regression analysis to calculate "percent better prediction" (%BP) values
- Select model with highest %BP value (W=Well-Stirred, M=Modified Well-Stirred, S=Similar) [69]
Ex Situ Experimental Validation:
- Use isolated perfused rat liver (IPRL) system with varying protein concentrations
- Determine fraction unbound (fu) at different albumin concentrations (0-2%) using rapid equilibrium dialysis
- Measure hepatic availability (FH) and clearance at each protein concentration
- Fit experimental data to different model equations to verify prediction accuracy [69]
The following workflow diagram illustrates the key steps in the biomimetic IVIVE system that simultaneously assesses drug diffusion and metabolism:
Essential Research Tools and Reagents
Successful implementation of IVIVE requires specific research tools and reagents designed to mimic physiological conditions while providing reproducible results. The following table details key solutions and their applications in hepatic clearance studies:
Table 2: Essential Research Reagent Solutions for IVIVE Studies
| Research Tool | Function in IVIVE | Application Example | Key Considerations |
|---|---|---|---|
| Cryopreserved Human Hepatocytes | Gold standard for predicting human metabolic clearance; contain full complement of drug-metabolizing enzymes and transporters | Measurement of intrinsic clearance for IVIVE; identification of metabolic pathways [68] | Lot-to-lot variability; require specific supplementation (ITS-G, hydrocortisone) [66] |
| Human Liver Microsomes | Contains cytochrome P450 and other phase I enzymes; higher throughput than hepatocytes | Early screening of metabolic stability; reaction phenotyping [67] | Lack transporters and some phase II enzymes; requires scaling factors |
| HepaRG Cells | Liver-derived cell line with stable metabolic competence; form functional bile canaliculi | Biomimetic IVIVE systems; long-term metabolism studies [66] | Require specific differentiation protocol; maintain metabolic functions for weeks |
| Biomimetic Single-Well System | Patented system with mesh inserts to control drug diffusion; enables simultaneous diffusion and metabolism studies | Modeling absorption and metabolism phases with Weibull distribution [66] | Korean Patent No. 10-2022-0153547; adjustable pore sizes (125-686 mesh) |
| Isolated Perfused Rat Liver (IPRL) | Ex situ system maintaining intact liver architecture and physiological flow | Validation of model predictions under controlled protein binding conditions [69] | Bridges in vitro and in vivo; allows manipulation of perfusion medium composition |
| Rapid Equilibrium Dialysis (RED) | Determination of fraction unbound (fu) in plasma or albumin solutions | Protein binding studies at various albumin concentrations (0-2%) [69] | Essential parameter for WSM and MWSM; affects clearance predictions |
The comparative analysis of IVIVE methods for predicting hepatic metabolic clearance reveals a sophisticated landscape of complementary approaches, each with distinct strengths and limitations. The Well-Stirred Model remains the most widely implemented framework, demonstrating reasonable accuracy for flow-limited drugs and BDDCS Class 1 compounds. However, emerging evidence supports the Modified Well-Stirred Model for capacity-limited, binding-sensitive drugs such as rosuvastatin, where it shows significantly better predictive performance (48.59% BP% vs. 19.95% for WSM).
The integration of advanced biomimetic systems with mechanistic modeling represents the most promising direction for enhancing IVIVE accuracy. These systems, which simultaneously assess drug diffusion and metabolism using physiological relevant cells like HepaRG, address critical limitations of traditional static in vitro models. Furthermore, the development of systematic model selection approaches based on multinomial logistic regression analysis provides a data-driven framework for choosing the optimal clearance model based on drug-specific characteristics.
Despite these advances, fundamental challenges remain, particularly the systematic underprediction bias (3-10 fold) observed across most IVIVE approaches and the accurate prediction of clearance for drugs affected by hepatic transporters. Future progress will likely depend on continued refinement of in vitro systems to better capture in vivo physiology, coupled with the integration of IVIVE into PBPK modeling frameworks that incorporate comprehensive physiological knowledge.
In vitro-in vivo correlation (IVIVC) is a critical scientific tool in pharmaceutical development, defined as a predictive mathematical model that describes the relationship between an in vitro property of a dosage form (typically the rate or extent of drug dissolution or release) and a relevant in vivo response (such as plasma drug concentration or amount of drug absorbed) [9]. For researchers and drug development professionals, establishing a robust IVIVC model provides a mechanistic framework to forecast in vivo pharmacokinetic performance based on in vitro dissolution profiles, thereby streamlining formulation development, supporting quality control, and facilitating regulatory approvals [3] [22].
The ability to accurately predict in vivo response from in vitro observations has far-reaching consequences in pharmaceutical development. IVIVC models can reduce the need for certain clinical bioequivalence studies, help set clinically relevant dissolution specifications, optimize formulation parameters, and evaluate the impact of post-approval manufacturing changes [3]. However, the development of a predictive and reliable IVIVC requires careful consideration of multiple statistical and methodological factors, from the initial choice of modeling approach to the final validation of predictability. This guide systematically compares the core methodologies, benchmarks their performance against regulatory standards, and provides experimental frameworks for establishing IVIVC that meets both scientific and regulatory expectations.
Core IVIVC Methodologies: A Comparative Analysis
The establishment of a meaningful IVIVC involves several mathematical approaches that can be broadly categorized into two main modeling philosophies: deconvolution-based and convolution-based methods. Understanding the nuances, advantages, and limitations of each approach is fundamental to selecting the appropriate strategy for a given drug product.
Deconvolution-Based versus Convolution-Based Modeling
Deconvolution-Based Approach: This traditional method involves relating the fraction of a dosage unit dissolved in vitro to the fraction dissolved in vivo at corresponding times. The critical challenge is that the fraction dissolved in vivo is not directly observable and must be derived from plasma concentration data using mathematical deconvolution techniques [64]. These techniques rely on the availability of a reference immediate-release (IR) formulation or intravenous (IV) dose to characterize the unit impulse response of the body. The deconvoluted in vivo absorption or dissolution time course is then directly correlated with the in vitro dissolution profile.
Convolution-Based Approach: This alternative methodology directly incorporates the convolution integral and is considered a more robust single-stage approach. It utilizes observed data directly without transformation and models the entire system simultaneously [54] [64]. In this approach, a compartmental model is first fitted to unit impulse response data to estimate individual pharmacokinetic parameters. The in vivo plasma concentration-time profile following administration of an extended-release (ER) product is then expressed as the convolution of the in vitro dissolution time course and the unit impulse response function. The parameters linking the in vitro dissolution to the in vivo input are estimated simultaneously, making this method less susceptible to the propagation of errors [64].
Table 1: Comparison of IVIVC Modeling Techniques
| Feature | Deconvolution-Based Approach | Convolution-Based Approach |
|---|---|---|
| Fundamental Principle | Relates in vitro dissolution to deconvoluted in vivo dissolution | Uses convolution integral to model plasma concentration from in vitro data |
| Data Transformation | Requires deconvolution of in vivo data | Directly uses raw plasma concentration data |
| Linearity & Time Invariance | Assumed for the system | Assumed for the system |
| Error Propagation | Potential for instability and error propagation through two-stage modeling | Reduced error propagation via single-stage modeling |
| Regulatory Prediction Accuracy | Can yield inaccurate predictions; may not meet FDA criteria [64] | High precision; typically meets FDA predictability criteria [54] [64] |
| Implementation Complexity | Less complex, but relies on accurate deconvolution | More complex, integrated modeling |
Hierarchical Levels of IVIVC
IVIVC models are also classified into different levels (A, B, and C) based on their complexity and predictive power, with Level A being the most rigorous and preferred for regulatory submissions [3] [22].
Level A IVIVC represents a point-to-point correlation between the fraction of drug dissolved in vitro and the fraction of drug absorbed in vivo. It is the most informative and reliable category, as it predicts the entire in vivo time course from the in vitro dissolution data. Level A correlation is most commonly used for regulatory submissions and can support biowaivers for certain post-approval changes [3]. Its development typically requires data from at least two formulations with different release rates (e.g., slow, medium, fast).
Level B IVIVC uses statistical moment analysis, comparing the mean in vitro dissolution time to the mean in vivo residence time or mean in vivo dissolution time. While it utilizes all the in vitro and in vivo data, it does not reflect the actual shape of the plasma concentration profile and is considered less useful for predicting in vivo performance. Consequently, it is rarely accepted by regulatory agencies for setting dissolution specifications [3].
Level C IVIVC establishes a single-point relationship, correlating a dissolution parameter (e.g., the amount dissolved at a specific time point, like T~50%~) with a pharmacokinetic parameter (e.g., C~max~ or AUC). It is the simplest type of correlation but offers the least predictive power, as it does not characterize the complete shape of the plasma profile. While a Level C correlation can provide useful insights during early formulation development, it is insufficient for biowaiver requests. A multiple Level C correlation, which relates one or several dissolution time points to one or several pharmacokinetic parameters, is more informative but still considered inferior to a Level A correlation [3].
Table 2: Levels of IVIVC and Their Regulatory Utility
| Level | Definition | Predictive Value | Regulatory Acceptance |
|---|---|---|---|
| Level A | Point-to-point correlation between in vitro dissolution and in vivo absorption. | High – predicts the full plasma concentration-time profile. | Most preferred by FDA/EMA; supports biowaivers and major formulation changes [3]. |
| Level B | Statistical comparison of mean in vitro dissolution time and mean in vivo residence/absorption time. | Moderate – does not reflect individual PK curves. | Less robust; usually requires additional in vivo data; not suitable for specifications [3]. |
| Level C | Single-point correlation between a dissolution parameter and a PK parameter (e.g., C~max~, AUC). | Low – does not predict the full PK profile. | Least rigorous; not sufficient for biowaivers; may support early development [3]. |
Statistical and Methodological Considerations for Robustness
Critical Factors in Model Development
Developing a robust IVIVC requires careful consideration of a complex array of factors that influence drug dissolution and absorption [9]:
- Physicochemical Properties: Key drug properties such as solubility, pKa, salt form, and particle size fundamentally govern the dissolution process, as described by classical models like the Noyes-Whitney equation. The drug's ionization constant (pKa) is particularly crucial as it determines stability, solubility, and absorption across the pH gradients of the gastrointestinal (GI) tract [9].
- Biopharmaceutical Properties: Drug permeability, often estimated using parameters like the octanol-water partition coefficient (log P), absorption potential (AP), or polar surface area (PSA), plays a major role in absorption. For orally administered drugs, the Biopharmaceutics Classification System (BCS) provides a useful framework, with BCS Class II drugs (low solubility/high permeability) being particularly strong candidates for IVIVC, as their absorption is often dissolution-rate limited [19] [9].
- Physiological Properties: The physiological environment of the GI tract, including its pH gradient (ranging from 1-2 in the stomach to 7-8 in the colon), fluid volumes, bile salt concentrations, and transit times, significantly affects both drug dissolution and the rate/extent of absorption. These factors must be considered when designing biorelevant dissolution methods [9].
Key Statistical and Practical Considerations
Several statistical and practical "traps" can undermine the development and predictive performance of an IVIVC model [11]:
- Use of Mean vs. Individual Data: Averaging in vitro data is common practice and generally acceptable due to the controlled nature of dissolution testing. However, averaging in vivo plasma concentration data requires caution. If subjects exhibit significant differences in lag time (T~lag~) or time to maximum concentration (T~max~), the mean curve may not reflect individual behaviors, and IVIVC is not recommended. For data with low intra-subject variability and consistent T~lag~ and T~max~, using mean curves may be acceptable, though it results in a loss of information about variability [11].
- Time Scaling and Lag Time Correction: A time-scaling function is often included in the IVIVC model to account for potential time differences between in vitro and in vivo processes. A general time-scaling model can be expressed as
r_vivo(t) = a1 + a2 * r_vitro(t_t), wheret_t = b1 + b2 * t^(b3)[54]. This model includes linear components (intercept a1 and slope a2) and a nonlinear component describing time-shifting (b1), time-scaling (b2), and time-shaping (b3). In the absence of time scaling, the parameters simplify to a1=0, a2=1, b1=0, b2=1, and b3=1 [54]. - Assessment of Predictability: The ultimate validation of an IVIVC model lies in its predictive performance. This is typically assessed by calculating the prediction error (%PE) for key pharmacokinetic parameters like C~max~ and AUC [54]. The standard criteria for internal predictability, as per regulatory guidance, require that the average absolute %PE for each parameter be ≤ 10%, with no individual formulation %PE exceeding 15% [54] [3]. For external validation, the prediction error for each parameter should be ≤ 10% [64] [3].
Experimental Protocols for IVIVC Development
General Workflow for Establishing a Level A IVIVC
The following workflow, derived from successful case studies, outlines the key steps for developing a Level A IVIVC [54] [12]:
- Formulation Selection: Develop and manufacture at least two, preferably three, formulations of the same drug with distinct in vitro release rates (e.g., slow, medium, fast). These formulations should differ only in the release-controlling excipients or manufacturing process parameters.
- In Vitro Dissolution Testing: Conduct dissolution studies on all formulations using a biorelevant method. This may involve compendial apparatus (USP I, II, III, IV) with media that simulate gastrointestinal conditions (e.g., FaSSIF, FeSSIF). The use of alternative systems, such as biphasic dissolution, which models both dissolution and partitioning, has shown promise for drugs like bicalutamide [19].
- In Vivo Clinical Study: Administer the test formulations and a reference (immediate-release or IV solution) to human subjects in a crossover study design. Collect frequent blood samples to characterize the plasma concentration-time profile for each formulation.
- Data Analysis and Model Building:
- For Deconvolution-Based Approach: Deconvolute the plasma data for each ER formulation using the reference product's data to determine the in vivo absorption/time course. Correlate the fraction dissolved in vivo with the fraction dissolved in vitro at the same time points.
- For Convolution-Based Approach: Fit a pharmacokinetic model to the reference product data to define the unit impulse response. Then, use convolution to model the ER formulation's plasma concentration as a function of the in vitro dissolution profile and the impulse response, estimating the correlation parameters simultaneously [54] [64].
- Model Validation: Demonstrate the model's predictive power through internal and/or external validation. Internal validation uses the formulations that built the model, while external validation uses a new, different formulation [54].
Figure 1: Experimental Workflow for Level A IVIVC Development
Case Study Protocol: Convolution-Based IVIVC for Methylphenidate
A study optimizing the benefit-risk ratio of methylphenidate hydrochloride (MPH) provides a concrete example of a convolution-based IVIVC implementation [54]:
- Objective: To identify the dose and in vivo release properties that maximize the benefit-risk ratio for attention deficit hyperactivity disorder (ADHD) treatment.
- Materials: Ritalin LA extended-release capsules (40 mg) with slow, medium, and fast in vitro dissolution rates, and Ritalin immediate-release tablets as a reference.
- In Vivo Data: A single-dose, four-period, randomized crossover study in 16 subjects provided plasma concentration-time data for all formulations.
- Mathematical Model: The plasma concentration from an arbitrary dose was described by convolution:
C_p(t) = f(t) * I(t), wheref(t)is the in vivo input function andI(t)is the unitary impulse response. The IVIVC was established by relating the fraction of drug absorbed in vivo,r_vivo(t), to the fraction of drug dissolved in vitro,r_vitro(t), using a time-scaling model:r_vivo(t) = a1 + a2 * r_vitro(t_t)witht_t = b1 + b2 * t^(b3)[54]. - Outcome: The validated model allowed for in silico optimization of the dose and release properties to achieve a sustained clinical response with minimal risk of adverse events.
Essential Research Reagent Solutions
The following table details key materials and reagents commonly used in the experimental phases of IVIVC development, as referenced in the cited studies.
Table 3: Key Research Reagent Solutions for IVIVC Experiments
| Reagent / Material | Function / Application | Exemplary Use Case |
|---|---|---|
| USP Apparatus I-IV | Standardized equipment for conducting in vitro dissolution testing under controlled conditions. | Used with paddle (USP II) or reciprocating cylinder (USP III) for lamotrigine ER tablets [12]. |
| Biorelevant Dissolution Media | Media simulating gastrointestinal fluids (e.g., FaSSIF, FeSSIF) to better predict in vivo dissolution. | Employed to establish a biopredictive dissolution method for lamotrigine ER [12]. |
| Biphasic Dissolution System | A system containing aqueous buffer and organic solvent (e.g., octanol) to model simultaneous dissolution and absorption. | Used to develop a Level A IVIVC for bicalutamide immediate-release tablets [19]. |
| Reference Standard | Highly characterized drug substance used for analytical method calibration and quantification. | Lamotrigine USP reference standard used for HPLC analysis in dissolution and plasma samples [12]. |
| Model-Dependent Deconvolution Software | Computational tools for estimating in vivo absorption time course using techniques like Wagner-Nelson or numerical deconvolution. | Used to determine the in vivo release profile for correlation with in vitro data [12] [11]. |
The successful establishment of a predictive IVIVC is a multifaceted endeavor that hinges on the careful selection and execution of statistical and methodological principles. The convolution-based modeling approach has demonstrated superior prediction accuracy compared to traditional deconvolution methods and is highly suited for optimizing formulation properties to maximize clinical outcomes [54] [64]. The rigorous Level A correlation remains the gold standard for regulatory applications, including the justification of biowaivers and the establishment of patient-centric quality standards [12] [3].
A robust IVIVC model must be built upon a foundation of well-designed experiments that account for critical physicochemical, biopharmaceutical, and physiological factors. Furthermore, researchers must navigate common pitfalls related to data averaging, time-scaling, and the application of strict predictability criteria during model validation. As the field advances, the integration of IVIVC with emerging modeling approaches like PBPK and machine learning promises to further enhance its predictive power, ultimately accelerating the development of safe and effective drug products across a wider range of therapeutic classes.
In Vitro-In Vivo Correlation (IVIVC) is a pivotal scientific approach in pharmaceutical development, establishing a predictive mathematical model between a drug's dissolution rate in the laboratory (in vitro) and its absorption behavior in the human body (in vivo) [3]. For researchers and drug development professionals, a validated IVIVC model serves as a powerful regulatory tool to obtain bioequivalence waivers (biowaivers), which can exempt certain drug formulations from costly and time-consuming clinical bioequivalence studies [3]. The primary value of IVIVC lies in its ability to predict the in vivo drug absorption impact based on in vitro dissolution data, facilitating formulation optimization, supporting quality control, and enabling the establishment of clinically meaningful dissolution specifications [3] [70]. This is particularly crucial for modified-release dosage forms, where drug release is carefully controlled, and for which regulatory authorities like the U.S. Food and Drug Administration (FDA) specifically recommend IVIVC development [3].
Levels of IVIVC and Their Regulatory Utility
The United States Pharmacopeia (USP) and FDA recognize different levels of IVIVC, which vary in their complexity and predictive power [3] [4]. Understanding these categories is essential for selecting the appropriate correlation strategy for a development program. The following table summarizes the key characteristics of the primary IVIVC levels:
| IVIVC Level | Definition & Methodology | Predictive Value & Regulatory Acceptance | Common Use Cases |
|---|---|---|---|
| Level A | A point-to-point correlation between the in vitro dissolution profile and the in vivo absorption profile (derived via deconvolution) [3] [70]. | High. Predicts the entire plasma concentration-time profile. It is the most preferred and accepted level by regulatory agencies for supporting biowaivers for major formulation changes [3] [70]. | Regulatory submissions for New Drug Applications (NDAs) and Abbreviated New Drug Applications (ANDAs); setting dissolution specifications [3]. |
| Level B | A statistical moment analysis that compares the mean in vitro dissolution time to the mean in vivo residence or absorption time [3] [70]. | Moderate. Does not reflect the actual shape of the plasma concentration curve. It is less robust and generally not sufficient for biowaivers alone [3] [4]. | Early formulation screening; provides insights but is not typically used for quality control specifications [3]. |
| Level C | Correlates a single dissolution time point (e.g., % dissolved at 4 hours) with a single pharmacokinetic parameter (e.g., AUC or Cmax) [3] [70]. | Low. Does not predict the full pharmacokinetic profile. It has limited regulatory utility for biowaivers [3]. | Early development decisions and formulation ranking [3] [4]. |
| Multiple Level C | Expands Level C by correlating several dissolution time points with multiple pharmacokinetic parameters [70]. | More useful than a single-point Level C, but still not as powerful or regulatory-preferred as a Level A correlation [70]. | Justifying certain formulation modifications when a Level A correlation is not feasible [70]. |
The establishment of a Level A IVIVC is considered the gold standard for regulatory purposes. According to FDA guidance, a successful Level A model can support biowaivers for post-approval changes (e.g., in formulation, manufacturing process, or site) and, in some cases, for certain strengths during the initial approval of a drug product, as echoed in the recent ICH M13B draft guidance for immediate-release (IR) dosage forms [3] [71].
Experimental Protocol for Developing and Validating a Level A IVIVC
Developing a robust Level A IVIVC suitable for a biowaiver request is a multi-step process that requires careful experimental design and execution. The workflow below illustrates the key stages from formulation development through to model validation.
Detailed Experimental Methodologies
Formulation Development
The process begins with the creation of multiple formulations with intentionally varying drug release rates. Typically, at least two or three formulations with distinct release profiles (e.g., slow, medium, and fast) are developed [3] [70]. This variance in performance is crucial for establishing a meaningful correlation across a range of possible release behaviors.
In Vitro Dissolution Testing
Dissolution testing is performed on all formulations using apparatuses such as the USP Apparatus I (basket), II (paddle), or IV (flow-through cell) [70]. The test conditions must be biorelevant and discriminatory, meaning they should simulate physiological conditions (e.g., using media at different pH levels like 1.2, 4.5, and 6.8, or biomimetic media such as FaSSIF/FeSSIF) and be capable of distinguishing between the different formulations developed [70]. The goal is to generate complete dissolution profiles showing the percentage of drug released over time.
In Vivo Pharmacokinetic Studies
A clinical pharmacokinetic study is conducted, typically in human volunteers, using the same formulations tested in vitro. The study design must be crossover to allow for intra-subject comparison. Blood samples are collected at frequent intervals to measure plasma drug concentrations over time, from which primary PK parameters like AUC (area under the curve) and Cmax (maximum concentration) are calculated [3] [70].
Data Processing and Deconvolution
This is a critical analytical step to determine the in vivo absorption profile. Mathematical deconvolution techniques, such as the Wagner-Nelson method (for one-compartment models) or the Loo-Riegelman method (for two-compartment models), are applied to the in vivo plasma concentration data [70]. These methods calculate the fraction of drug absorbed over time, which is then directly comparable to the fraction of drug dissolved over time from the in vitro tests.
Model Fitting and Correlation
A point-to-point mathematical model is established by plotting the fraction of drug dissolved in vitro against the fraction of drug absorbed in vivo for each time point. Common models used for this fitting include linear, Weibull, or first-order functions [70]. The resulting model defines the Level A correlation.
Model Validation
Before an IVIVC can be submitted for a biowaiver, its predictive performance must be rigorously validated.
- Internal Validation: This is the first check using the data from which the model was built. The established correlation model is used to predict the in vivo absorption profiles of the formulations used in its development. The predicted profiles are then used to estimate key PK parameters (Cmax and AUC), which are compared to the observed values. The percentage prediction error (%PE) is calculated for each [70].
- External Validation: This is a more robust assessment performed using a new formulation that was not part of the initial model development. The dissolution data from this new formulation is input into the IVIVC model to predict its in vivo profile and PK parameters. These predictions are then compared against the actual results from a clinical study of that formulation [3].
Regulatory Validation Criteria
For a model to be considered acceptable by the FDA for biowaiver purposes, the prediction error must meet the following criteria [70]:
- Mean %PE for both Cmax and AUC should be ≤ 10%.
- The individual %PE for each formulation should be ≤ 15%.
If these criteria are met, the IVIVC model is considered validated and can be used to justify biowaivers for subsequent post-approval changes (e.g., in formulation or manufacturing) or, in the context of ANDAs and recent ICH M13B guidance, for certain additional strengths of a drug product [3] [71].
Essential Research Reagents and Materials
The following table details key reagents, instruments, and software solutions critical for executing the IVIVC development protocol.
| Tool Category | Specific Examples | Function in IVIVC Development |
|---|---|---|
| Dissolution Apparatus | USP Apparatus I (Basket), II (Paddle), IV (Flow-Through Cell) [70]. | Simulates the gastrointestinal environment to measure the rate and extent of drug release from the dosage form under controlled, biorelevant conditions. |
| Dissolution Media | Aqueous buffers (pH 1.2, 4.5, 6.8); Biorelevant Media (FaSSIF, FeSSIF); Surfactant solutions [4] [70]. | Mimics the varying pH and composition of the human GI tract to provide physiologically meaningful dissolution profiles. |
| Bioanalytical Instruments | LC-MS/MS, HPLC-UV | Quantifies the concentration of the drug in plasma samples from PK studies and in dissolution media with high specificity and sensitivity. |
| Pharmacokinetic Software | WinNonlin, PK-Sim, NONMEM | Performs non-compartmental analysis, compartmental modeling, and deconvolution (e.g., Wagner-Nelson) to derive in vivo absorption profiles from plasma concentration data. |
| In Vitro Digestion Models | pH-Stat Lipolysis Assay [4]. | A critical specialized tool for lipid-based formulations (LBFs) that models the dynamic process of lipid digestion in the GI tract, which is key to drug release for these systems. |
| Statistical & Modeling Software | R, Python (with scikit-learn, SciPy), SAS | Used for statistical analysis, fitting correlation models (e.g., Weibull), and performing prediction error calculations for validation. |
Regulatory Framework and Global Considerations
The regulatory landscape for IVIVC is well-established but continues to evolve. The FDA's 1997 guidance "Extended Release Oral Dosage Forms: Development, Evaluation, and Application of In Vitro/In Vivo Correlations" remains a foundational document, outlining how to develop, evaluate, and apply IVIVC for extended-release drug products in NDAs and ANDAs [3]. A significant recent development is the move towards global harmonization through the International Council for Harmonisation (ICH).
The ICH M13A guideline on bioequivalence for immediate-release solid oral dosage forms has been finalized, and the draft ICH M13B guideline, published in June 2025, provides harmonized criteria for granting biowaivers for additional strengths of a drug when in vivo bioequivalence has been established for at least one strength [71]. This harmonization is crucial for streamlining global drug development.
It is important to note that IVIVC is most readily applicable to drugs where dissolution is the rate-limiting step for absorption. This makes it particularly suitable for BCS Class II (low solubility, high permeability) drugs and modified-release formulations of BCS Class I (high solubility, high permeability) drugs [70]. For complex formulations like lipid-based systems, achieving a robust IVIVC is more challenging due to additional dynamic processes like digestion and permeation, often requiring more sophisticated in vitro models [4].
A validated Level A IVIVC represents a scientifically rigorous and regulatorily recognized path to secure bioequivalence waivers. By following a structured development and validation protocol—involving multiple formulations, biorelevant dissolution testing, clinical PK studies, and robust statistical analysis—sponsors can build a powerful predictive model. This model not only supports regulatory strategies for biowaivers, reducing the need for redundant clinical studies, but also enhances product understanding, facilitates quality-by-design, and ultimately accelerates the development of safe and effective medicines for patients.
Conclusion
The establishment of a robust In Vitro-In Vivo Correlation is a powerful asset in the drug development toolkit, offering a reliable pathway to predict clinical performance, optimize formulations, and satisfy regulatory requirements with greater efficiency. As the pharmaceutical landscape evolves with increasingly complex modalities like lipid nanoparticles, nucleic acid therapies, and long-acting injectables, the methodologies for developing IVIVC must also advance. Future success will depend on the creation of more biorelevant in vitro assays, the sophisticated integration of in silico and PBPK modeling, and collaborative efforts to standardize approaches for non-oral dosage forms. By embracing these future directions, researchers can continue to bridge the in vitro-in vivo gap, accelerating the delivery of safe and effective medicines to patients.
References
- 1. Applications of In Vitro–In Vivo Correlations in Generic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4476988/]
- 2. Extended Release Oral Dosage Forms: Development ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/extended-release-oral-dosage-forms-development-evaluation-and-application-vitroin-in-vivo-correlations]
- 3. CMC Perspectives of In Vitro / In Vivo Correlation (IVIVC) ... [https://premier-research.com/perspectives/cmc-perspectives-of-in-vitro-in-vivo-correlation-ivivc-in-drug-development/]
- 4. Improving In Vitro–In Vivo Correlation (IVIVC) for Lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567226/]
- 5. Improving in vivo release prediction from in situ forming ... [https://www.sciencedirect.com/science/article/pii/S0378517325007215]
- 6. In vitro-in vivo correlation (IVIVC) development for long- ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365924007661]
- 7. A Perspective on Model-Informed IVIVC for Development of ... [https://link.springer.com/article/10.1007/s11095-023-03572-3]
- 8. In Vitro-In Vivo Correlation for Complex Non-Oral Drug Products [https://pmc.ncbi.nlm.nih.gov/articles/PMC4739855/]
- 9. In vitro-In vivo Correlation: Perspectives on Model Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC3099258/]
- 10. IVIVC modelling can speed up the drug development process [https://www.biopharmaservices.com/blog/ivivc-modelling-can-speed-up-the-drug-development-process/]
- 11. In vitro–In Vivo Correlations: Tricks and Traps - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3385821/]
- 12. Development of in vitro-in vivo correlation for establishing ... [https://www.sciencedirect.com/science/article/abs/pii/S0939641125002516]
- 13. An overview of the alarming impediments encountered ... [https://www.sciencedirect.com/science/article/pii/S2352952025000398]
- 14. In Vitro-In Vivo Correlation Of Amorphous Solid Dispersion ... [https://pubmed.ncbi.nlm.nih.gov/40069449/]
- 15. Emerging Role of Biopharmaceutical Classification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9780568/]
- 16. Ivivc Conversion Final 2025 | PDF | Bioavailability | In Vitro [https://www.scribd.com/document/896652915/Ivivc-Conversion-Final-2025]
- 17. Biowaiver based on biopharmaceutics classification system [https://www.sciencedirect.com/science/article/pii/S2773216923000181]
- 18. Biopharmaceutical Classification System [https://agnopharma.com/technical-briefs/biopharmaceutical-classification-system/]
- 19. Developing In Vitro–In Vivo Correlation for Bicalutamide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473495/]
- 20. Improving In Vitro–In Vivo Correlation (IVIVC) for Lipid- ... [https://www.mdpi.com/1999-4923/17/10/1310]
- 21. In vitro evaluation of mesalazine enteric-coated tablet ... [https://www.nature.com/articles/s41598-025-05936-8]
- 22. In vivo–In Vitro correlation (IVIVC) in drug development [https://wjarr.com/content/vivo%E2%80%93-vitro-correlation-ivivc-drug-development-bridging-preclinical-and-clinical-outcomes]
- 23. Best Practices for the Development, Scale-up, and Post ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4037495/]
- 24. Dissolution and Drug Release Tests [https://www.usp.org/small-molecules/dissolution]
- 25. The Advancement of In Vitro Lipolysis: Two-Step Flow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114758/]
- 26. In Vitro Release Test Studies for Topical Drug Products [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/in-vitro-release-test-studies-topical-drug-products-submitted-andas]
- 27. In vitro and in vivo correlation for lipid-based formulations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8424225/]
- 28. Development of an in-situ forming implant system for ... [https://link.springer.com/article/10.1007/s13346-025-01892-y]
- 29. In-situ forming solvent-induced phase inversion implants ... [https://www.sciencedirect.com/science/article/pii/S0022354925001753]
- 30. Lipid-Based Drug Delivery Systems - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4590796/]
- 31. Development and validation of in vitro–in vivo correlation ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365915005611]
- 32. Physiologically Based Pharmacokinetic Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541349/]
- 33. Leveraging In Silico and Artificial Intelligence Models to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180087/]
- 34. Advances in Physiologically Based Pharmacokinetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12158835/]
- 35. Demonstration of in vitroin vivo relationship (IVIVR) and ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354925005003]
- 36. Development and validation of an in vitro–in vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9359323/]
- 37. In Silico Pharmacokinetic and Pharmacodynamic (PK-PD) ... [https://www.mdpi.com/journal/pharmaceutics/special_issues/26SP16RBQI]
- 38. Physiologically Based Pharmacokinetic (PBPK) Modeling [https://bio-protocol.org/exchange/minidetail?id=6541157&type=30]
- 39. Exploring the Challenges of Lipid Nanoparticle Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12031360/]
- 40. Exploring the Challenges of Lipid Nanoparticle Development [https://www.mdpi.com/2076-393X/13/4/339]
- 41. Establishing correlation between in vitro potency and in ... [https://www.nature.com/articles/s41541-025-01181-2]
- 42. High‐Throughput Strategies for Streamlining Lipid ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12622538/]
- 43. Designing lipid nanoparticles using a transformer-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534189/]
- 44. Emerging Approaches for the Discovery of Lipid-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473667/]
- 45. Computational approaches to lipid-based nucleic acid ... [https://link.springer.com/article/10.1140/epje/s10189-023-00385-5]
- 46. Reformulating lipid nanoparticles for organ-targeted mRNA ... [https://www.nature.com/articles/s41467-024-50093-7]
- 47. The Dominant role of PEG-Lipids in LNP performance [https://pubmed.ncbi.nlm.nih.gov/40286880/]
- 48. SURFACE CHEMISTRY INFLUENCE IMPLANT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3230929/]
- 49. Water uptake and strength characteristics of a nanofilled ... [https://www.sciencedirect.com/science/article/abs/pii/S0300571207002424]
- 50. A review of cytotoxicity testing methods and in vitro study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534221/]
- 51. Changes in Implant Surface Characteristics and Wettability ... [https://www.mdpi.com/1996-1944/18/12/2844]
- 52. Improving in vivo release prediction from in situ forming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12344484/]
- 53. Water and ions binding to extracellular matrix drives stress ... [https://www.nature.com/articles/s41551-025-01369-w]
- 54. A General Framework for Assessing In vitro/In vivo Correlation as a Tool for Maximizing the Benefit‐Risk Ratio of a Treatment Using a Convolution‐Based Modeling Approach - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6389349/]
- 55. Comparison of Sequential Drug Release in Vitro and in Vivo [https://pmc.ncbi.nlm.nih.gov/articles/PMC4691229/]
- 56. Recent developments in in vitro and in vivo models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8381685/]
- 57. User's guide to correlation coefficients - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6107969/]
- 58. Preclinical validation of finite element models for predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409801/]
- 59. Prediction of failure load using micro-finite element ... [https://www.sciencedirect.com/science/article/abs/pii/S1740674906000242]
- 60. Lipid-based oral formulation in capsules to improve the ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2023.1232012/full]
- 61. Effects of lipid chain length, supersaturation, digestion, and ... [https://pubmed.ncbi.nlm.nih.gov/40360094/]
- 62. Predictions of biorelevant solubility change during ... [https://www.sciencedirect.com/science/article/pii/S0928098724001453]
- 63. Novel development of lipid-based formulations [https://www.sciencedirect.com/science/article/abs/pii/S0939641125002413]
- 64. A Comparison of the Prediction Accuracy of Two IVIVC ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354916326715]
- 65. Applicability of a Single Time Point Strategy for the Prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4767722/]
- 66. Mechanistic in vitro–in vivo extrapolation (IVIVE) approach ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12173689/]
- 67. What Is IVIVE? 7 FAQs About In Vitro-In Vivo Extrapolation [https://labtesting.wuxiapptec.com/2025/09/11/in-vitro-in-vivo-extrapolation-what-developers-should-know/]
- 68. Hepatic Clearance Predictions from In Vitro–In Vivo ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624099367]
- 69. Selection of an Optimal Metabolic Model for Accurately ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299470/]
- 70. In Vitro–In Vivo Correlation (IVIVC) for SR Dosage Forms [https://pharmalesson.com/in-vitro-in-vivo-correlation-ivivc-for-sr-dosage-forms/]
- 71. M13B Bioequivalence for Immediate-Release Solid Oral ... [https://www.federalregister.gov/documents/2025/06/02/2025-09900/m13b-bioequivalence-for-immediate-release-solid-oral-dosage-forms-additional-strengths-biowaiver]