Validating Real-World Evidence for Health Technology Assessment: A Framework for Robust Decision-Making in Drug Development
This article provides a comprehensive guide for researchers and drug development professionals on validating Real-World Evidence (RWE) for Health Technology Assessment (HTA).
Validating Real-World Evidence for Health Technology Assessment: A Framework for Robust Decision-Making in Drug Development
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on validating Real-World Evidence (RWE) for Health Technology Assessment (HTA). It explores the foundational role of RWE from Real-World Data (RWD) in bridging evidence gaps between clinical trials and real-world clinical practice. The content details advanced methodological frameworks, including causal inference and the target trial approach, endorsed by regulatory and HTA bodies like the FDA and NICE. It addresses critical challenges in data quality and governance and offers optimization strategies. Through a comparative analysis of regulatory and HTA use cases, the article establishes validation criteria to ensure RWE is fit-for-purpose, supporting robust and timely healthcare decision-making for pricing, reimbursement, and patient access.
The Rising Imperative of Real-World Evidence in Modern Healthcare Assessment
The paradigm of evidence generation for healthcare decision-making is undergoing a fundamental shift. While randomized controlled trials (RCTs) remain the gold standard for establishing efficacy under controlled conditions, Health Technology Assessment (HTA) bodies are increasingly recognizing their limitations in reflecting real-world clinical practice [1]. This gap has catalyzed the strategic adoption of real-world data (RWD) and real-world evidence (RWE) to strengthen the assessment of medical technologies across their lifecycle.
The 21st Century Cures Act of 2016 in the United States was a pivotal moment, designed to accelerate medical product development and bring innovations to patients more efficiently [2]. In response, the U.S. Food and Drug Administration (FDA) created a framework for evaluating RWE to support regulatory decisions, signaling a formal recognition of its value [2]. This movement is equally strong in Europe, with initiatives like the European Data Analysis and Real-World Interrogation Network (DARWIN EU) expected to conduct hundreds of RWE studies annually to support regulatory decision-making [1].
For researchers, scientists, and drug development professionals, understanding the precise distinction between RWD and RWE—and how they are operationalized within HTA—is no longer academic; it is a practical necessity for navigating modern evidence requirements and demonstrating the value of new therapies in diverse patient populations.
Defining the Terms: The Fundamental Distinction Between RWD and RWE
A clear conceptual and practical separation between Real-World Data and Real-World Evidence is the foundation for their correct application in HTA research.
Real-World Data (RWD) are the raw, unprocessed data relating to patient health status and/or the delivery of health care routinely collected from a variety of sources [2] [3]. Think of RWD as the foundational building blocks or the "raw material" for generating evidence [4]. These data are captured during routine clinical care and daily life, not within the strict protocols of a traditional clinical trial.
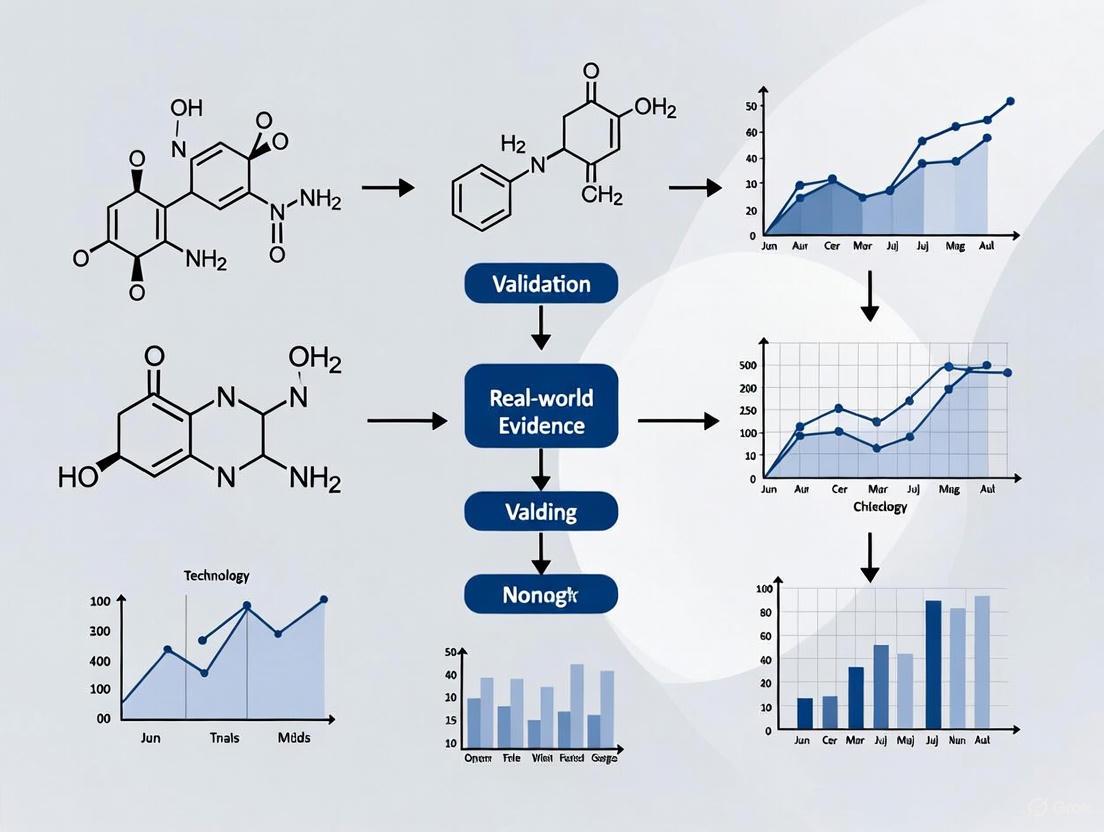
Real-World Evidence (RWE), in contrast, is the clinical evidence derived from the analysis and interpretation of RWD [2] [3]. It is the "knowledge gained from analyzing and interpreting RWD" [5]. RWE provides insights into the usage, potential benefits, and risks of a medical product in real-world clinical settings [2] [6]. The following diagram illustrates this transformative relationship and the process of generating RWE.
RWD is a diverse ecosystem of data types, each offering unique insights into the patient journey. The table below catalogs the primary sources of RWD relevant to HTA research.
Table: Primary Sources and Applications of Real-World Data in HTA
| Data Source | Description | Key Applications in HTA & Research |
|---|---|---|
| Electronic Health Records (EHRs) | Digital records of patient health information, including medical history, diagnoses, treatments, and lab results [4] [7]. | Provides rich clinical detail on disease progression, treatment patterns, and outcomes in routine practice [5] [7]. |
| Claims & Billing Data | Administrative data generated from healthcare claims for reimbursement [4] [6]. | Ideal for understanding healthcare resource utilization, costs, and treatment patterns at a population level [7]. |
| Disease & Product Registries | Organized systems that collect uniform data on a specific disease, condition, or exposure to a product [2] [4]. | Provides longitudinal data on natural history of disease, treatment outcomes, and safety in specific patient populations [6] [5]. |
| Patient-Generated Data | Data collected directly from patients, including patient-reported outcomes (PROs), wearable device data, and mobile app data [5] [7]. | Offers insight into patient-experienced symptoms, quality of life, and daily health metrics outside clinical settings [6]. |
| Pharmacy Data | Information on prescribed and dispensed medications [4] [7]. | Sheds light on medication adherence, persistence, and therapy sequences in real-world populations [4]. |
The Critical Role of RWD and RWE in Health Technology Assessment
HTA agencies are tasked with determining the value of new health technologies, a process that extends beyond regulatory approval for market entry to include pricing, reimbursement, and guidance on use within healthcare systems. RWD and RWE are becoming indispensable in this process by addressing key evidence gaps left by traditional RCTs.
How RWE Complements RCT Evidence
RCTs are designed for high internal validity but can suffer from limited generalizability due to strict eligibility criteria, homogeneous patient populations, and short follow-up periods [1] [5]. RWE addresses these limitations by:
- Providing Long-Term Outcomes Data: RWE can monitor the safety and durability of treatment response over a much longer timeframe than typical RCTs [8].
- Assessing Effectiveness in Heterogeneous Populations: RWE includes outcomes from older patients, those with comorbidities, and other groups often excluded from RCTs, providing a more representative picture of effectiveness in clinical practice [7].
- Informing Decisions in Rare Diseases and Oncology: For rare diseases or novel oncology treatments where large RCTs are unfeasible or unethical, RWE from external control arms (ECAs) can provide crucial contextual evidence for treatment effects [9] [8].
Key Applications of RWE in the HTA Lifecycle
The use of RWE in HTA is not monolithic; it serves distinct purposes throughout the technology lifecycle. A study analyzing European HTA bodies found that RWE is used for various endpoints, with varying levels of acceptance across different agencies [9].
Table: RWE Acceptance for Different Purposes in HTA (Adapted from PMC [9])
| Purpose of RWE in HTA | Description | Example Use Case |
|---|---|---|
| Supporting Efficacy Claims | Using RWE (e.g., from an External Control Arm) to substantiate the effectiveness of a treatment, often for single-arm trials [9]. | Tisagenlecleucel (Kymriah) in lymphoma was assessed using an ECA comparing it to historical standard of care [9]. |
| Informing Disease Background | Using RWE to characterize the natural history of a disease, burden of illness, or epidemiology [9]. | Establishing the incidence and prevalence of a rare disease to demonstrate unmet need and contextualize the value of a new therapy. |
| Post-Marketing Surveillance | Monitoring the safety of a product after it has entered the market [2] [6]. | Using EHR or claims data to identify potential adverse events not detected in pre-market clinical trials. |
| Supporting Reassessments | Using RWE in HTA reassessments to refine coverage, pricing, and reimbursement decisions after initial market entry [8]. | The UK's Cancer Drugs Fund (CDF) uses RWE to collect additional evidence on drugs granted provisional access [8]. |
Methodological Protocols: Generating Regulatory and HTA-Grade RWE
Transforming RWD into RWE that is fit-for-purpose and deemed reliable by HTA bodies and regulators requires rigorous methodology. The following section outlines key experimental and study design protocols.
The RWE Generation Workflow: From Data to Evidence
The process of generating RWE is iterative and requires careful planning and execution at every stage to ensure the evidence produced is valid and reliable. The following diagram details this multi-stage workflow.
1. Define Research Question & Protocol: The foundation of any robust RWE study is a pre-specified research question and analysis plan [1]. This includes defining the patient population, interventions, comparators, and outcomes, and outlining the statistical methods to address potential confounding.
2. Data Sourcing & Collection: This involves identifying and accessing RWD from one or more of the sources listed in Section 2.1. A critical consideration is whether the data are fit-for-purpose—that is, relevant, valid, and reliable for the specific research question [1] [7].
3. Data Curation & Harmonization: Raw RWD is often unstructured, inconsistent, and stored across disparate systems. This stage involves significant data engineering to clean, standardize, and transform the data into a structured format suitable for analysis [5]. This may include processing unstructured physician notes from EHRs or linking datasets (e.g., linking EHR data with claims data) to create a more complete picture of the patient journey [7].
4. Study Design & Analysis: This is the core of transforming RWD into RWE. Key methodological approaches include:
- Non-Interventional Studies: Observational studies that analyze RWD without intervening in patient care. These require advanced statistical methods like propensity score matching to control for confounding and emulate a randomized study as closely as possible [9] [3].
- External Control Arms (ECAs): Using existing RWD to create a control group for a single-arm trial. This is particularly valuable in oncology and rare diseases [9]. For example, the therapy avelumab (Bavencio) for Merkel Cell Carcinoma was assessed using an ECA derived from a retrospective observational study [9].
- Pragmatic Clinical Trials: Trials that are interventional in nature but are designed to closely reflect real-world clinical practice and often leverage RWD collection infrastructure [1].
5. Evidence Interpretation & Submission: The final analyzed evidence must be interpreted in the context of its limitations, such as residual confounding or potential data quality issues, and transparently reported for submission to HTA bodies and regulators [5].
The Scientist's Toolkit: Essential Components for RWE Generation
Table: Essential Reagents and Solutions for RWE Generation
| Component / Solution | Function in RWE Generation |
|---|---|
| Data Governance Framework | A set of international standards and policies to ensure the ethical and acceptable use of RWD, covering data privacy, security, and patient consent [1]. |
| Data Curation & Linkage Tools | Software and algorithms used to clean, standardize, and harmonize disparate RWD sources, and to link patient records across datasets while maintaining privacy [5] [7]. |
| Statistical Analysis Packages | Software (e.g., R, Python with pandas) containing libraries for advanced statistical methods like propensity score matching, inverse probability weighting, and multivariate regression to address confounding [5]. |
| Sentinel Initiative / DARWIN EU | Large-scale, regulatory-grade data networks that provide curated and validated RWD for safety monitoring and study execution [1] [5]. |
| ML395 | ML395, MF:C26H29N5O2, MW:443.5 g/mol |
| m-PEG8-thiol | m-PEG8-thiol, CAS:651042-83-0, MF:C17H36O8S, MW:400.5 g/mol |
Comparative Analysis: RWE Acceptance Across HTA Bodies
The acceptance and use of RWE in HTA decision-making are not uniform. A comparative analysis reveals significant differences in receptivity and focus across major HTA agencies.
Table: Comparative Use and Acceptance of RWE in Select HTA Bodies (Synthesized from [9] [8])
| HTA Body / Country | Receptivity to RWE | Primary Focus & Common Use of RWE |
|---|---|---|
| NICE (UK) | More receptive [9]. | Cost-effectiveness and clinical outcomes; uses RWE within frameworks like the Cancer Drugs Fund for managed access and reassessment [8]. |
| AEMPS (Spain) | More receptive [9]. | Budgetary impact and epidemiological analysis [9]. |
| AIFA (Italy) | Intermediate. | Primarily focused on budgetary impact analysis [9]. |
| HAS (France) | Less accepting [9]. | Prioritizes clinical relevance; uses RWE in specific post-registration studies and temporary use programs [8]. |
| G-BA (Germany) | Less accepting [9]. | Focuses on clinical benefit; reassessment of products (often limited to orphan drugs) can incorporate RWE [8]. |
A study examining ten technologies found that the level of scrutiny from HTA bodies is "considerably higher" when RWE is used to substantiate efficacy claims compared to when it is used for other purposes, such as describing disease background [9]. The key criteria driving acceptance across all markets are the representativeness of the data source, overall transparency in the study, and robust methodologies [9].
The distinction between Real-World Data as the raw material and Real-World Evidence as the derived, actionable insights is more than semantic—it is a fundamental concept that shapes how robust, credible evidence is generated for HTA. The landscape is evolving rapidly: the proportion of HTA reports incorporating RWE rose from 6% in 2011 to 39% in 2021 [1].
For researchers and drug development professionals, success in this new paradigm requires a commitment to methodological rigor, transparency, and early engagement with HTA bodies. By strategically employing RWD and RWE to answer questions that RCTs cannot, the industry can provide the comprehensive evidence needed to demonstrate the true value of new therapies in real-world practice, ultimately leading to more efficient and informed healthcare decision-making for all patients.
The evaluation of new medical treatments has long been dominated by the randomized controlled trial (RCT), widely considered the gold standard for establishing therapeutic efficacy due to its rigorous design that minimizes bias through randomization and strict protocol adherence [10]. However, a significant challenge has emerged in what researchers term the efficacy-effectiveness gap—the disconnect between the significant results seen in highly controlled RCTs and the inconsistent outcomes observed when treatments are applied in routine clinical practice [10]. This gap exists because RCTs often exclude patients with comorbidities, complex medications, or socioeconomic factors that represent a substantial proportion of those treated in real-world settings [10].
Real-world evidence (RWE), derived from the analysis of real-world data (RWD) collected outside the constraints of traditional clinical trials, offers a complementary perspective that addresses these limitations [11]. RWD sources include electronic health records (EHRs), insurance claims data, patient registries, and data from wearable devices and mobile health platforms [10] [12]. Regulatory bodies like the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) are increasingly accepting RWE to support regulatory decisions, with studies showing that between 1998 and 2019, 17 FDA or EMA new drug applications used RWD in oncology and metabolism, all receiving approval [11].
The following diagram illustrates how RCTs and RWE function as complementary, rather than competing, sources of evidence throughout the therapeutic development lifecycle:
Comparative Analysis: RCTs vs. RWE Across Critical Dimensions
The fundamental differences between RCTs and RWE stem from their distinct purposes, methodologies, and applications. The table below provides a systematic comparison of their key characteristics:
Table 1: Comprehensive Comparison of RCTs and RWE Across Critical Dimensions
| Dimension | Randomized Controlled Trials (RCTs) | Real-World Evidence (RWE) |
|---|---|---|
| Primary Purpose | Establish efficacy under ideal, controlled conditions [10] | Evaluate effectiveness in routine clinical practice [10] |
| Study Design | Experimental, with random allocation to intervention and control groups [10] | Observational, analyzing data from actual clinical practice [12] |
| Population Characteristics | Homogeneous populations with strict inclusion/exclusion criteria; often excludes elderly, those with comorbidities, or complex medications [10] [13] | Heterogeneous populations reflecting diversity seen in clinical practice, including typically excluded groups [10] [12] |
| Data Collection Methods | Prospective collection using standardized protocols and predetermined endpoints [10] | Collection from routine care sources: EHRs, claims data, registries, patient-reported outcomes [10] [14] |
| Key Strengths | High internal validity, controls confounding through randomization, establishes causal relationships [10] | High external validity, captures long-term outcomes and safety signals, represents diverse populations [10] [12] |
| Key Limitations | Limited generalizability, high cost and time requirements, may miss rare adverse events [10] | Potential for confounding and bias, variable data quality, methodological challenges [10] |
| Regulatory Acceptance | Foundation for initial approval by FDA and EMA [10] | Increasingly accepted for post-market studies, label expansions, and in rare diseases [9] [11] |
| Ideal Applications | Pivotal trials for regulatory approval, establishing proof of concept [10] | Post-market surveillance, comparative effectiveness research, outcomes in rare diseases [9] [11] |
Methodological Protocols: Generating Valid Real-World Evidence
Data Source Selection and Validation
The foundation of robust RWE generation lies in the selection and validation of appropriate real-world data sources. Common sources include electronic health records (EHRs), which provide clinical data from routine care; claims databases, containing billing information that reveals treatment patterns and healthcare utilization; patient registries, which systematically collect data on specific populations or conditions; and emerging data sources such as wearable devices and mobile health applications that capture patient-generated health data [10] [14] [12].
To ensure data quality, researchers must implement rigorous validation protocols. These include cross-validation against other data sources where possible, completeness checks for critical variables, plausibility testing to identify outliers or inconsistent entries, and temporal validation to ensure proper sequencing of events [14]. For example, in a study using EHR data to examine treatment patterns for chronic pain, researchers would verify that pain scores are recorded at appropriate intervals and that medication prescriptions align with diagnosed conditions [10].
Advanced Methodological Approaches
Overcoming the inherent limitations of observational data requires sophisticated methodological approaches. Propensity score matching (PSM) is frequently employed to minimize selection bias by creating comparable treatment and control groups based on observed characteristics [10]. This statistical technique calculates the probability (propensity) that a patient would receive a specific treatment based on their baseline characteristics, then matches patients across treatment groups with similar propensities, effectively mimicking randomization for observed covariates [10].
Target trial emulation represents a more advanced framework for designing observational studies that closely mirror the structure of RCTs [11]. This approach involves explicitly defining key trial components—including eligibility criteria, treatment strategies, outcomes, and follow-up periods—before analyzing observational data, thereby reducing methodological biases [11]. For instance, when using RWD to create an external control arm (ECA) for a single-arm trial in oncology, researchers would apply the same inclusion and exclusion criteria as the clinical trial to the real-world population, ensure comparable outcome measurements, and align the analysis timeframes [9].
Additional techniques include instrumental variable analysis to address unmeasured confounding, difference-in-differences approaches to account for secular trends, and Bayesian methods that incorporate prior knowledge to strengthen inferences from observational data [11]. The UK's National Institute for Health and Care Excellence (NICE) has demonstrated the acceptability of these approaches, as exemplified by their recommendation of mobocertinib for advanced non-small-cell lung cancer based on a single-arm trial that used RWD as an external comparator [11].
Practical Applications: Case Studies Demonstrating RWE's Value
Addressing Evidence Gaps in Rare Diseases and Oncology
RWE has proven particularly valuable in therapeutic areas where traditional RCTs face practical or ethical challenges. In rare diseases, patient populations are often too small to conduct adequately powered RCTs. Similarly, in oncology, the rapid evolution of treatment standards and the heterogeneity of cancer types complicate the design and interpretation of RCTs [9] [11].
Several compelling case examples illustrate this application:
Tisagenlecleucel (Kymriah): For relapsed or refractory diffuse large B-cell lymphoma, this CAR-T cell therapy utilized an external control arm constructed from multiple data sources (SCHOLAR-1, ZUMA-1, CORAL, Eyre, and PIX301) to demonstrate comparative effectiveness when a randomized design was not feasible [9].
Avelumab (Bavencio): For Merkel cell carcinoma, researchers developed an ECA from a retrospective observational study (100070-Obs001) designed to evaluate outcomes under current clinical practices, including both first-line and second-line patients from the US and Europe [9].
Blinatumomab (Blincyto): For acute lymphoblastic leukemia, an ECA compared blinatumomab with continued chemotherapy using data from a retrospective study (study20120148) [9].
These examples demonstrate how RWE can provide contextualization for single-arm trials, offering insights into how experimental therapies perform compared to existing standards of care when randomized head-to-head comparisons are unavailable.
Post-Marketing Surveillance and Safety Monitoring
Even after rigorous RCTs lead to regulatory approval, important safety questions often remain due to the limited sample sizes and relatively short duration of most clinical trials. RWE plays a critical role in post-marketing surveillance by detecting rare adverse events and evaluating long-term safety profiles in broader patient populations [14] [12].
A prominent example comes from COVID-19 vaccine safety monitoring. While phase III trials for vaccines included tens of thousands of participants, they were still insufficiently powered to detect very rare events. RWE analysis discovered rare cases of cerebral venous sinus thrombosis with thrombocytopenia following ChAdOx1 nCoV-19 vaccination, with incidence rates ranging from 1 per 26,000 to 1 per 127,000—far too rare to detect in clinical trials of 21,635 participants [14]. This RWE directly informed changes to vaccine administration guidelines in the UK as early as April 2021 [14].
Informing Health Technology Assessment (HTA) and Reassessment
Health technology assessment bodies worldwide are increasingly incorporating RWE into their decision-making processes. A targeted review of 40 HTAs across six agencies (including NICE, HAS, and CADTH) found that 55% used RWE, particularly for orphan therapies [15]. These reassessments employed RWE primarily to address uncertainties related to primary and secondary endpoints, long-term outcomes, and treatment utilization patterns [15].
The acceptance of RWE varies across HTA bodies, with UK and Spanish agencies being more receptive, while French and German agencies are more cautious [9]. The key criteria driving RWE acceptance across markets include representativeness of the data source, overall transparency in the study, and robust methodologies [9].
The Research Toolkit: Essential Components for RWE Generation
Generating valid RWE requires both methodological expertise and appropriate technological resources. The table below outlines essential components of the modern RWE research toolkit:
Table 2: Research Reagent Solutions for Real-World Evidence Generation
| Tool Category | Specific Solutions | Function & Application |
|---|---|---|
| Data Infrastructure | Secure Data Environments (SDEs) [14] | Provide secure, governed access to sensitive patient data while maintaining privacy and compliance with regulations |
| Observational Medical Outcomes Partnership (OMOP) Common Data Model [14] | Standardizes data structure and terminology across different sources to enable systematic analysis | |
| Methodological Approaches | Propensity Score Matching (PSM) [10] | Balances observed covariates between treatment groups to reduce selection bias in observational comparisons |
| Target Trial Emulation [11] | Provides a structured framework for designing observational studies that mimic the key features of RCTs | |
| Analytical Technologies | Bayesian Statistical Methods [11] | Incorporates prior knowledge and continuously updates probability estimates as new data becomes available |
| Artificial Intelligence & Machine Learning [12] | Identifies complex patterns in large, heterogeneous datasets and helps address confounding | |
| Data Linkage Tools | Privacy-Preserving Record Linkage (PPRL) [14] | Enables connection of patient records across different data sources while protecting personal information |
| Application Programming Interfaces (APIs) [12] | Facilitates efficient data extraction and integration from diverse healthcare systems and platforms | |
| N-(Azido-PEG3)-N-bis(PEG3-acid) | N-(Azido-PEG3)-N-bis(PEG3-acid), CAS:2055042-57-2, MF:C26H50N4O13, MW:626.7 g/mol | Chemical Reagent |
| PDE8B-IN-1 | PDE8B-IN-1, MF:C14H18N8OS, MW:346.41 g/mol | Chemical Reagent |
The evidence landscape in healthcare is evolving from a rigid hierarchy with RCTs at the apex to a complementary ecosystem where RCTs and RWE each contribute their unique strengths. RCTs remain indispensable for establishing causal efficacy under controlled conditions, while RWE provides crucial insights into clinical effectiveness in diverse real-world populations [10] [12]. This synergistic relationship enables more comprehensive evidence generation throughout the therapeutic lifecycle—from early development through post-market surveillance.
The successful integration of these approaches requires ongoing methodological innovation, cross-stakeholder collaboration, and the development of standardized best practices. Regulatory and HTA bodies are increasingly formalizing their frameworks for RWE evaluation, as exemplified by NICE's RWE Framework and the EMA's DARWIN EU initiative [14] [1]. As these frameworks mature and methodological rigor advances, the strategic combination of RCTs and RWE will ultimately accelerate the development of effective treatments and improve patient outcomes through evidence-based medicine that reflects both scientific rigor and clinical reality.
The integration of real-world evidence (RWE) into regulatory and health technology assessment (HTA) decision-making represents one of the most significant advancements in healthcare policy and drug development. As innovative therapies, particularly in oncology, rare diseases, and advanced therapeutic medicinal products (ATMPs), emerge at an unprecedented rate, regulatory bodies and HTA agencies worldwide are developing structured frameworks to incorporate data beyond traditional randomized controlled trials. The Food and Drug Administration (FDA), European Medicines Agency (EMA), and National Institute for Health and Care Excellence (NICE) have each launched strategic initiatives to formalize the generation and assessment of RWE, aiming to accelerate patient access to safe, effective, and cost-effective treatments.
This comparative guide examines the current operational frameworks, methodological requirements, and strategic priorities of these three major agencies regarding RWE validation and use. For researchers and drug development professionals, understanding the comparative landscape of evidence requirements is crucial for designing efficient development programs that satisfy both regulatory and reimbursement evidentiary standards. The drive toward RWE represents a fundamental shift from a siloed approach to an integrated evidence generation paradigm that spans the entire product lifecycle from pre-market approval to post-market surveillance and value assessment.
Agency Comparison: Strategic Frameworks and Operational Priorities
Table: Comparative Overview of Key RWE Initiatives at FDA, EMA, and NICE
| Agency/Aspect | FDA (United States) | EMA (European Union) | NICE (United Kingdom) |
|---|---|---|---|
| Primary Strategic Focus | Building RWE infrastructure and addressing clinical trial transparency [16] | Implementing EU HTA Regulation with joint clinical assessments [17] [18] | Evolving HTA methods for challenging therapies and leveraging AI [19] |
| Key RWE Initiative | Real-World Evidence Framework; Clinical trial transparency enforcement [16] | Joint Clinical Assessment (JCA) for medicines & medical devices [17] [20] | 2025 RWE Framework update; HTA Innovation Lab [21] [19] |
| Current Implementation Status | Ongoing framework development with recent enforcement pushes [16] | Mandatory for oncology/ATMPs (2025); orphan medicines (2028); all medicines (2030) [18] | Modular updates to HTA manual; severity modifier implementation [19] [22] |
| Patient Engagement Focus | Patient Experience Data (PED) guidance in development [23] | Structured patient input in JCA and Joint Scientific Consultation [18] | Patient input in severity assessment; ILAP patient engagement [22] |
| Technology Scope | Pharmaceuticals, biologics, medical devices, digital health technologies [16] | Pharmaceuticals, ATMPs, and high-risk medical devices (Class IIb/III) [20] | Pharmaceuticals, medical technologies, digital health, diagnostics [19] |
Table: RWE Assessment Methodologies and Acceptance Criteria
| Methodological Aspect | FDA Approach | EMA/EU HTA Network Approach | NICE Approach |
|---|---|---|---|
| Study Design Acceptance | Emphasis on real-world data quality and fit-for-purpose study designs [24] | Joint Clinical Assessments focus on comparative clinical effectiveness [18] | Accepts RWE alongside RCT data; target trial emulations encouraged [21] [19] |
| Data Quality Standards | Assessing reliability and relevance of real-world data sources [24] | Harmonized evidence requirements across member states [17] | 2025 RWE Framework strengthens validation and reporting standards [21] |
| Evidence Gaps Addressed | Framework to address uncertainties in effectiveness [24] | Addresses fragmentation in European HTA processes [18] | Managed Access Agreements for evidence generation [22] |
| External Control Arms | Accepts under specific conditions with rigorous validation [24] | Considered within JCA for rare diseases and oncology [18] | Accepted, particularly for ultra-rare diseases with natural history data [21] |
FDA: RWE Framework and Regulatory Modernization
Strategic Priority Structure
The FDA's Human Foods Program recently underwent a significant reorganization, centralizing risk management activities into three key areas, though its principal RWE initiatives reside within its drug and device centers [25]. The agency's RWE Framework, coupled with its focus on clinical trial transparency, represents a comprehensive approach to evidence generation. In October 2025, the FDA emphasized closing the "clinical trial reporting gap" through enhanced enforcement of reporting requirements on ClinicalTrials.gov, highlighting transparency as an ethical obligation for human subjects research [16].
RWE Program Implementation
The FDA is actively expanding its information-gathering efforts for AI-enabled medical devices, including a scheduled November 2025 meeting of its Digital Health Advisory Committee to discuss benefits, risks, and risk mitigation measures for generative AI-enabled digital mental health devices [16]. The agency has also published a Request for Public Comment on approaches to measuring and evaluating the performance of AI-enabled medical devices in real-world settings, indicating a growing focus on real-world performance assessment of digital health technologies [16].
EMA: EU HTA Regulation Implementation
Joint Clinical Assessment Framework
The implementation of the EU Health Technology Assessment Regulation (HTAR) on January 12, 2025, marks a transformative shift in how medicines are evaluated across the European Union [18]. The regulation establishes a framework for Joint Clinical Assessments (JCAs) that will provide a harmonized clinical evaluation available to all member states. The rollout is phased, beginning in 2025 with new oncology medicines and advanced therapy medicinal products (ATMPs), expanding to orphan medicinal products in 2028, and encompassing all new medicines authorized by the EMA by 2030 [18].
Operational Infrastructure
The technical implementation of the HTAR is being facilitated through a centralized HTA secretariat and close cooperation with the EMA [17]. The EMA provides the HTA secretariat with business pipeline information on planning and forecasting for joint clinical assessments and joint scientific consultations for both medicines and medical devices [17]. For medical devices, which will come into scope in 2026, the implementing act on Joint Scientific Consultation (JSC) outlines procedures for parallel consultations that coordinate with existing expert panel consultations, creating a streamlined pathway for high-risk devices [20].
Diagram: EU HTA Regulation Process Flow and Implementation Timeline
NICE: Methodological Evolution and Access Pathways
HTA Methodological Innovations
NICE's 2025 updates reflect a sophisticated evolution in HTA methodology designed to address challenging therapeutic areas while maintaining rigorous health economic standards. The severity modifier, introduced in 2022 and reviewed in 2024, operates by calculating both absolute and proportional quality-adjusted life year (QALY) shortfalls, allowing for a higher cost-effectiveness threshold for treatments addressing more severe conditions [22]. The implementation has resulted in a higher proportion of positive recommendations (84.4%) compared with the previous end-of-life modifier (82.7%), demonstrating its practical impact on access decisions [22].
Specialized Appraisal Pathways
For ultra-rare diseases, NICE has refined its highly specialized technologies (HST) criteria effective April 2025, providing clearer definitions for ultra-rare prevalence (1:50,000 or less in England), disease burden, and eligibility thresholds (no more than 300 people in England) [22]. The Innovative Licensing and Access Pathway (ILAP) was relaunched in January 2025 with more selective entry criteria and a streamlined service offering a single point of contact from pre-pivotal trial to routine reimbursement [22]. For technologies with evidence uncertainties, Managed Access Agreements (MAAs) enable temporary funding while additional data is collected, typically lasting up to five years [22].
Experimental Protocols for RWE Generation
RWE Study Validation Protocol
Table: Essential Reagents and Solutions for RWE Study Implementation
| Research Component | Function/Application | Implementation Considerations |
|---|---|---|
| Electronic Health Record (EHR) Data | Source for patient demographics, clinical characteristics, and outcomes | Data mapping to common data model; validation of key clinical fields [21] |
| Validated Patient-Reported Outcome (PRO) Instruments | Capture patient-experienced symptoms and functional impacts | Alignment with FDA/EMA PRO guidance; linguistic validation for multinational studies [23] |
| Common Data Model (e.g., OMOP) | Standardize data structure across disparate sources | Implementation of ETL processes; quality checks for vocabulary mapping [24] |
| Propensity Score Methods | Balance measured covariates between treatment groups | Selection of appropriate variables; assessment of balance achieved [24] |
| Sensitivity Analysis Framework | Assess robustness to unmeasured confounding | Implementation of quantitative bias analysis; E-value calculations [24] |
Decentralized Clinical Trial (DCT) Implementation
Recent methodological advances have positioned decentralized clinical trials as a valuable approach for generating RWE, particularly for rare diseases where traditional trials face recruitment challenges. The protocol incorporates electronic patient-reported outcomes (ePROs), telemedicine platforms, and home health nursing to collect clinical trial data in real-world settings [21]. Implementation requires meticulous planning of digital infrastructure, validation of remote measurement systems, and compliance with regional regulatory requirements for decentralized trial elements [21].
The regulatory and HTA landscape is undergoing rapid transformation, with the FDA, EMA, and NICE each developing distinctive yet increasingly aligned approaches to real-world evidence incorporation. The FDA emphasizes evidence generation infrastructure and transparency enforcement, the EMA is focused on harmonizing assessment methodologies across member states through the HTA Regulation, while NICE continues to refine its value assessment framework with specialized pathways for challenging therapeutic areas. For drug development professionals, success in this evolving environment requires early strategic planning, engagement with regulatory and HTA bodies throughout the development process, and robust evidence generation strategies that address both regulatory requirements and health technology assessment needs. The convergence of these initiatives signals a broader industry transition toward integrated evidence generation capable of demonstrating both clinical and economic value across the product lifecycle.
The landscape of evidence generation for Health Technology Assessment (HTA) is undergoing a fundamental transformation. While Randomized Controlled Trials (RCTs) remain the gold standard for establishing efficacy under controlled conditions, they often leave critical evidence gaps regarding performance in routine clinical practice [26]. Real-World Evidence (RWE), derived from data collected outside traditional clinical trials, is increasingly bridging these gaps by providing insights into treatment effectiveness, long-term safety, and patient outcomes in diverse, real-world populations [27]. This shift is driven by the need to understand the true value of health technologies in the context of daily clinical care, where patient heterogeneity, co-morbidities, and variable treatment patterns are the norm [28]. The growing prevalence of RWE in HTA submissions marks a pivotal evolution in how stakeholders—including regulators, payers, and providers—evaluate new medical interventions, moving from a pure efficacy focus to a more comprehensive assessment of effectiveness and value in real-world settings [21].
Quantitative Analysis of RWE Adoption in HTA
Global HTA Body Acceptance and Guidelines
The integration of RWE into HTA processes is progressing at varying speeds across different jurisdictions. A 2022 survey of Roche subsidiaries across seven countries provides a quantitative snapshot of the methodological guidance and acceptance landscape at that time [26].
Table 1: Status of RWE Methodological Guidelines in HTA Bodies (as of June 2022)
| Country | HTA Body | RWE Methodological Guidelines Published? |
|---|---|---|
| France | HAS | Yes |
| Germany | IQWiG/G-BA | Yes |
| United Kingdom | NICE | Yes |
| Brazil | Conitec | No |
| Canada | CADTH/INESSS | No |
| Italy | AIFA | No |
| Spain | MSSSI/AEMPS | No |
The data reveals that by mid-2022, less than half of the major HTA bodies surveyed had published formal methodological guidelines for RWE, indicating a developing but not yet mature regulatory landscape [26]. However, this picture is evolving rapidly. By 2025, additional agencies including NICE have refined their RWE frameworks, with NICE's 2025 update specifically marking "a shift toward treating RWE as a strategic, rather than supplementary, evidence source" [21].
RWE Utilization in European HTA Submissions
The implementation of the European Union's Joint Clinical Assessment (JCA) in January 2025 represents a significant milestone for standardized evidence assessment across member states [29]. While the full impact is still emerging, early data demonstrates concrete integration of RWE into these processes.
Table 2: Early JCA Volumes and RWE Context (2025 Data)
| Therapeutic Category | Projected JCAs (2025) | Actual JCAs (Early 2025) | RWE Context |
|---|---|---|---|
| Oncology Medicines | 17 | 9 | RWE used to support value in reimbursement cases |
| Advanced Therapy Medicinal Products (ATMPs) | 8 | 1 (plus 1 oncology ATMP) | Critical for evidence in rare diseases |
The slightly lower-than-expected volume of early JCA submissions (9 for oncology versus 17 projected) suggests manufacturers may be adopting a cautious approach, potentially learning from initial assessments before submitting their own dossiers [21]. Within these submissions, RWE has played a substantively important role. Analysis of European pricing and reimbursement cases between 2014 and 2025 demonstrated that RWE played a key role in securing full reimbursement in 7 out of 16 European cases for orphan medicines and provided supporting input in conditional agreements for the remaining cases [21].
Methodological Frameworks for RWE Generation
Real-World Evidence (RWE) is the clinical evidence regarding the usage and potential benefits or risks of a medical product derived from the analysis of Real-World Data (RWD) [2]. RWD encompasses data relating to patient health status and/or healthcare delivery routinely collected from diverse sources [27]. These data sources can be categorized into three main groups based on their inherent quality and collection methodology [30]:
- Studies and Registries: Highest quality data collected purposefully for analysis using scientific methods and defined protocols (e.g., disease registries, prospective observational studies).
- Clinical Records: Data originating from routine medical care without study protocols but under healthcare professional supervision (e.g., Electronic Health Records (EHRs), claims and billing data).
- Unsupervised Sources: Data collected without professional supervision or protocol (e.g., patient-generated data from mobile apps, wearables, patient forums).
Each category requires different methodological approaches to address challenges related to data quality, completeness, and potential biases [30].
Experimental Protocols for RWE Generation
Protocol for Retrospective Database Studies
Objective: To generate comparative effectiveness evidence using existing healthcare databases (e.g., EHR, claims data) to inform HTA submissions.
Methodology:
- Data Source Selection: Identify fit-for-purpose databases with sufficient population size, relevant variables, and longitudinal follow-up. Common sources include EHR systems like Flatiron Health (specializing in oncology) and claims databases like Optum [31] [27].
- Cohort Definition: Apply explicit inclusion/exclusion criteria to define patient cohorts. The study population should align with the HTA population of interest (PICO framework) [26].
- Outcome Measurement: Identify and validate outcome measures within the database. For example, overall survival or progression-free survival in oncology studies often requires curation from unstructured EHR data [31].
- Confounder Adjustment: Implement advanced statistical methods to address confounding by indication, including:
- Propensity Score Matching: Create balanced treatment groups based on observed baseline characteristics [26].
- Multivariable Regression: Adjust for multiple confounders simultaneously in outcome models [30].
- Instrumental Variable Analysis: Address unmeasured confounding when suitable instruments are available [30].
Validation: Perform sensitivity analyses to test robustness of findings to different methodological assumptions [30].
Protocol for Prospective RWE Generation
Objective: To collect targeted RWD prospectively to address specific evidence gaps in HTA submissions.
Methodology:
- Registry Design: Establish a disease or product registry with a predefined protocol, data collection forms, and statistical analysis plan. For example, the European Cystic Fibrosis Society Registry collects demographic and clinical data to monitor treatment patterns and outcomes [27].
- Site Selection: Recruit diverse clinical sites to ensure population representativeness, including academic centers, community hospitals, and private practices [21].
- Data Collection: Implement standardized data collection procedures, often using electronic data capture systems. Define core data elements relevant to HTA needs (e.g., patient characteristics, treatment patterns, clinical outcomes, healthcare resource utilization, patient-reported outcomes) [27].
- Quality Assurance: Establish data quality checks, source data verification procedures, and audit trails to ensure data reliability [31].
Analysis: Pre-specified statistical analyses comparing outcomes across treatment groups with appropriate adjustment for confounding factors.
Diagram: RWE Generation Workflow for HTA. This diagram illustrates the sequential process for generating RWE, from defining the research question through to HTA submission, highlighting key methodological stages.
Comparative Analysis: RWE vs. RCT Evidence
The complementary strengths and limitations of RWE and RCT evidence make them suitable for answering different types of research questions in HTA.
Table 3: Comparison of RCT and RWE Characteristics [28] [27]
| Characteristic | Randomized Controlled Trials | Real-World Evidence |
|---|---|---|
| Purpose | Efficacy | Effectiveness |
| Setting | Experimental, controlled | Real-world clinical practice |
| Patient Selection | Strict inclusion/exclusion criteria | Heterogeneous, representative populations |
| Intervention | Fixed, per protocol | Variable, at physician's discretion |
| Comparator | Placebo or selective active control | Multiple alternative interventions as used in practice |
| Follow-up | Fixed duration, per protocol | Variable, as per routine care |
| Sample Size | Limited by design and cost | Potentially very large |
| Key Strength | High internal validity, controls confounding | High external validity, generalizability |
| Primary Limitation | Limited generalizability to broader populations | Potential for unmeasured confounding |
RCTs remain preferred for establishing causal efficacy under ideal conditions, while RWE provides crucial insights into clinical effectiveness in routine practice [28]. For HTA bodies, this distinction is critical—while regulators focus primarily on benefit-risk balance, HTA agencies assess comparative benefit versus existing options, making RWE particularly valuable for understanding a technology's performance in relevant healthcare systems and patient populations [29].
Essential Research Reagent Solutions for RWE Generation
The successful generation of RWE for HTA requires specialized "research reagents"—tools and platforms that enable robust data collection, management, and analysis.
Table 4: Essential Research Reagent Solutions for RWE Generation
| Solution Category | Representative Platforms | Primary Function in RWE Generation |
|---|---|---|
| EHR-Based Analytics | Flatiron Health, IQVIA EMR | Structure and analyze unstructured electronic health record data, particularly valuable for oncology |
| Claims Data Analytics | Optum, IQVIA Claims | Analyze healthcare utilization, treatment patterns, and costs from administrative billing data |
| Data Linkage Platforms | TriNetX, Aetion | Link and harmonize data from multiple sources (EHR, claims, registries) for comprehensive analysis |
| Analytical & Validation Tools | IBM Watson Health, Aetion | Apply advanced analytics and methodological validation to address confounding and bias in RWD |
| Regulatory Science Platforms | FDA Sentinel Initiative | Provide regulatory-grade RWE infrastructure for safety monitoring and effectiveness research |
These platforms address critical methodological challenges in RWE generation, including data interoperability, confounder control, and analytic transparency [31]. For instance, Flatiron Health's platform structures unstructured EHR data from a network of oncology clinics, enabling research on real-world treatment patterns and outcomes in diverse patient populations [31]. Similarly, the FDA's Sentinel Initiative provides a distributed data system that enables active monitoring of medical product safety using routinely collected healthcare data [27].
Country-Specific Variations in RWE Acceptance
The acceptance and use of RWE in HTA processes vary significantly across countries, reflecting different evidentiary standards, healthcare systems, and policy priorities.
- United Kingdom: NICE has emerged as a progressive adopter of RWE, with its 2025 framework update strengthening methodological standards. NICE tends to accept external comparators and natural history data, particularly for rare diseases [21].
- Germany: The G-BA/IQWiG system maintains stricter requirements, limiting RWE use mainly to ultra-rare diseases where RCTs are not feasible. They require rigorous data collection systems and often commission their own observational studies [21].
- France: HAS uses RWE extensively for re-evaluating technologies already reimbursed based on RCT evidence, and has published comprehensive guidelines on RWE use in HTA [26] [21].
- Italy: AIFA frequently employs RWE to inform outcome-based agreements, linking reimbursement to real-world performance metrics [21].
- United States: The FDA has developed a comprehensive framework for evaluating RWE to support regulatory decisions, including drug approvals and post-market studies [2].
These variations present challenges for global evidence generation strategies, requiring tailored approaches for different HTA bodies [26]. However, the implementation of the EU JCA may drive greater harmonization in RWE standards across European markets over time [21].
The quantification of RWE's growing prevalence in HTA submissions reveals a fundamental shift in evidence generation paradigms. From supporting 7 out of 16 European orphan drug reimbursement cases to being integrated into the newly launched EU Joint Clinical Assessment process, RWE has transitioned from a supplementary source to a strategic asset in health technology assessment [21]. The ongoing development of methodological guidelines by HTA bodies, advances in analytical techniques, and the emergence of specialized technology platforms all point toward continued growth in RWE's role and importance.
For researchers, scientists, and drug development professionals, mastering RWE generation is no longer optional but essential for successful HTA submissions and market access. Future success will depend on understanding country-specific requirements, implementing methodologically robust study designs, and leveraging appropriate technology platforms to generate regulatory-grade real-world evidence that addresses the evolving needs of health technology assessment bodies worldwide.
Frameworks and Methods for Generating Regulatory-Grade RWE
In health technology assessment (HTA) and drug development, randomized controlled trials (RCTs) represent the gold standard for establishing causal effects of interventions. However, RCTs are often impractical, unethical, untimely, or unable to address the sheer volume of causal questions in real-world settings [32]. Real-world evidence (RWE) derived from observational data—such as electronic health records, insurance claims databases, and medical registries—has emerged as a critical alternative [33] [34]. The fundamental challenge lies in ensuring that analyses of this observational data yield valid, actionable causal estimates rather than biased associations.
The target trial framework provides a systematic methodology to overcome this challenge. This approach involves two critical steps: first, specifying the protocol of a hypothetical randomized trial (the "target trial") that would ideally answer the causal question of interest; second, explicitly emulating this protocol using observational data [32]. By forcing researchers to articulate a precise causal question and design before analysis, this framework helps avoid common methodological pitfalls that have historically led to dramatic failures of observational inference, such as the erroneous protective effects of hormone therapy on coronary heart disease initially reported in observational studies but later contradicted by RCTs [32].
This guide provides a comprehensive comparison of the target trial emulation approach against conventional observational methods, detailing its implementation protocols, experimental validation, and essential methodological tools for researchers and drug development professionals working within the evolving landscape of RWE validation for HTA.
Core Components of the Target Trial Framework
The target trial framework requires researchers to meticulously define all components of a hypothetical RCT that would answer their causal question. The table below outlines the key components that must be specified in the protocol, their role in the target trial, and how they are emulated with observational data [32] [35].
Table 1: Core Protocol Components of a Target Trial and Their Emulation
| Protocol Component | Role in the Target Trial | Emulation with Observational Data |
|---|---|---|
| Eligibility Criteria | Defines the study population at time zero (start of follow-up) using only baseline information. | Apply identical criteria to select individuals from the observational database at their time zero. |
| Treatment Strategies | Precisely defines the interventions or treatment regimens being compared. | Identify individuals in the database whose treatment records align with the strategies. |
| Treatment Assignment | Randomization ensures comparability between treatment groups. | Use adjustment methods (e.g., weighting) to control for confounding and emulate randomization. |
| Outcome | Defines the primary outcome of interest and how it is measured. | Map the outcome definition to available data items (e.g., diagnosis codes, lab values). |
| Follow-up Period | Specifies the start, end, and duration of follow-up for each participant. | Define the start of follow-up (time zero) and censor at the earliest of: outcome, end of follow-up, or loss to data. |
| Causal Contrast | Defines the causal effect of interest (e.g., intention-to-treat or per-protocol effect). | Specify the same contrast and use appropriate statistical methods to estimate it. |
| Analysis Plan | Describes the statistical analysis for estimating the causal effect. | Implement an analysis (e.g., cloning/censoring/weighting) that accounts for the observational nature of the data. |
The power of this framework lies in its discipline. A conventional observational analysis might start with the data and fit a model, whereas a target trial emulation starts with a scientific question and designs a perfect study to answer it, only then looking to the data to execute that design [36]. This "question-first" approach is fundamental to generating evidence that can reliably inform regulatory and HTA decisions [34].
A Comparative Experiment: Target Trial Emulation vs. Conventional Methods
A landmark cohort study during the COVID-19 pandemic provides a compelling experimental comparison of target trial emulation against conventional model-first approaches [36].
Experimental Protocol and Methodology
- Research Question: What is the association of a corticosteroid treatment regimen with 28-day mortality for hospitalized patients with moderate to severe COVID-19?
- Benchmark: The World Health Organization (WHO) meta-analysis of RCTs on corticosteroids, which found an odds ratio of 0.66 (95% CI, 0.53-0.82) [36].
- Data Source: Retrospective data from 3,298 patients hospitalized within the NewYork-Presbyterian hospital system between March and May 2020 [36].
Table 2: Summary of Experimental Designs Compared
| Methodology | Core Approach | Treatment Definition | Analytical Technique |
|---|---|---|---|
| Target Trial Emulation | Question-first, emulating a hypothetical RCT. | A 6-day corticosteroid regimen initiated if and when a patient met severe hypoxia criteria. | Doubly robust estimation. |
| Model-First (Cox Regression) | Model-first, using common clinical literature designs. | Varied definitions: no time frame, 1-day, and 5-day windows from time of severe hypoxia. | Cox Proportional Hazards model. |
Target Trial Emulation Protocol:
- Eligibility: Adult patients with confirmed SARS-CoV-2 infection, excluding those with chronic corticosteroid use or transfers from outside hospitals.
- Treatment Strategies: A dynamic regimen (6 days of corticosteroids if/when severe hypoxia criteria are met) versus a static regimen (no corticosteroids).
- Outcome: All-cause mortality within 28 days of hospitalization.
- Causal Contrast: The per-protocol risk difference.
- Analysis: A doubly robust estimator was used to account for confounding, combining models for both the treatment and outcome to ensure validity even if one model is misspecified [36].
Results and Comparative Performance
The results demonstrated a stark contrast in the ability of each method to recover the established benchmark from RCTs.
Table 3: Comparison of Results Against the RCT Benchmark
| Analytical Method | Estimate of Corticosteroid Effect | Alignment with RCT Benchmark |
|---|---|---|
| WHO RCT Meta-Analysis (Benchmark) | Odds Ratio = 0.66 (95% CI, 0.53-0.82) | Gold Standard |
| Target Trial Emulation | Risk: 25.7% (Treated) vs. 32.2% (Untreated); qualitatively identical to benchmark. | High Alignment |
| Cox Model (Various Specifications) | Hazard Ratios ranged from 0.50 (95% CI, 0.41-0.62) to 1.08 (95% CI, 0.80-1.47). | Low/Inconsistent Alignment |
The target trial emulation successfully recovered a treatment effect that was qualitatively identical to the RCT benchmark, demonstrating a clear reduction in 28-day mortality. In contrast, the hazard ratios from the conventional Cox models varied widely in both size and direction depending on the treatment definition used, failing to provide a consistent or reliable estimate [36]. This experiment underscores that the correctness of estimates from observational data depends more on the design principles and causal question formulation than on the specific model fitted to the data.
Implementing the Framework: A Practical Workflow
Successfully implementing the target trial framework requires a structured workflow. The diagram below visualizes this process from conceptualization to result interpretation.
Addressing Critical Methodological Challenges
A key challenge in emulation is ensuring the alignment of three critical time points: eligibility assessment, treatment assignment, and the start of follow-up (time zero). A review of 199 studies explicitly aiming to emulate target trials found that 49% had misalignment of these time points. Among these, 67% did not use any method to correct for this misalignment in their analysis, introducing a significant risk of bias [37].
Common Biases from Misalignment:
- Immortal Time Bias: Occurs when the start of follow-up precedes treatment assignment, creating a period where the outcome cannot occur (the patient is "immortal") in the treated group by design [33]. For example, in a study of antidepressants and manic switch, if follow-up starts at depression diagnosis but treatment begins later, the treated group has a guaranteed survival period that the control group does not [33].
- Prevalent User Bias: Occurs when follow-up starts for patients who are already using a treatment ("prevalent users"), who may differ systematically from new users, for instance, by having already tolerated the treatment well [33].
Solutions for Time Alignment: The cloning, censoring, and weighting approach is a sophisticated method to address time-related biases by creating copies ("clones") of participants at the point of eligibility and then using statistical weighting to emulate a randomized assignment over time [37] [38]. Alternatively, researchers can design the emulation so that a participant's time zero is precisely the moment they meet all eligibility criteria and are assigned to a treatment strategy.
The Researcher's Toolkit for Target Trial Emulation
Implementing this framework requires a specific set of methodological "reagents." The following table details essential components of the research toolbox for a successful target trial emulation.
Table 4: Essential Reagents for Target Trial Emulation
| Tool Category | Specific Method/Technique | Primary Function |
|---|---|---|
| Study Design | Sequential Trials / Cloning-Censoring-Weighting | Manages time-varying treatments and confounders; corrects for time alignment issues. |
| Confounding Control | Inverse Probability of Treatment Weighting (IPTW) | Creates a pseudo-population where treatment assignment is independent of measured confounders. |
| Confounding Control | G-Methods (G-Formula, Marginal Structural Models) | Adjusts for both baseline and time-varying confounding, even when affected by prior treatment. |
| Censoring Handling | Inverse Probability of Censoring Weighting (IPCW) | Corrects for selection bias introduced by loss to follow-up or other forms of censoring. |
| Estimation | Doubly Robust Estimation (e.g., Targeted Maximum Likelihood) | Combines outcome and treatment models to provide a valid estimate even if one model is misspecified. |
| Software & Algorithms | The Target Trial Toolbox (e.g., from Yale PEW) | Provides curated, easy-to-use algorithms for implementing the above designs and analyses. |
| (3S,4S)-PF-06459988 | (3S,4S)-PF-06459988, CAS:1428774-45-1, MF:C19H22ClN7O3, MW:431.9 g/mol | Chemical Reagent |
| PhIP-d3 | PhIP-d3, CAS:210049-13-1, MF:C13H12N4, MW:227.28 g/mol | Chemical Reagent |
These tools move beyond conventional regression modeling by directly addressing the structural biases inherent in observational data. Their use is critical for generating effect estimates that can be meaningfully interpreted as causal [36] [38].
Validation and Acceptance in Regulatory and HTA Contexts
The ultimate test for any RWE methodology is its acceptance by regulatory and HTA bodies. Frameworks like FRAME (Framework for Real-World Evidence Assessment to Mitigate Evidence Uncertainties for Efficacy/Effectiveness) are being developed to standardize the evaluation of RWE submissions [24]. Furthermore, leading HTA agencies such as the UK's National Institute for Health and Care Excellence (NICE) explicitly recommend designing non-randomized studies "to emulate the preferred randomised controlled trial (target trial approach)" [34].
This institutional endorsement signals a paradigm shift. The focus is moving from a default skepticism of all observational data to a critical appraisal of how well a study is designed to answer a specific causal question, with the target trial framework providing the necessary structural rigor. This is particularly vital for use cases like supporting single-arm trials with external controls, assessing effectiveness in broader populations, and generating evidence in rare diseases where RCTs are not feasible [24] [34].
The target trial framework is not merely another statistical technique but a fundamental shift in approach—from a model-first to a question-first paradigm. As the experimental comparison shows, this approach, when implemented with careful attention to protocol specification and time-related biases, can yield estimates from observational data that align with those from gold-standard RCTs. For researchers and drug development professionals, mastering the tools and workflows of target trial emulation is no longer optional but essential for generating the valid, impactful real-world evidence required by modern regulators, payers, and HTA bodies.
In the evaluation of health technologies and interventions, the gold standard for establishing efficacy is the randomized controlled trial (RCT). However, RCTs are often too complex, expensive, unethical, or simply infeasible for many large-scale policy interventions and real-world clinical settings [39]. In these circumstances, researchers increasingly turn to quasi-experimental designs and advanced causal inference methods to estimate treatment effects from observational data [14] [39]. These methodologies provide powerful alternatives when random assignment is not possible, allowing researchers to draw causal inferences from real-world data (RWD) that can inform health technology assessment (HTA) and policy decisions [40].
The growing importance of real-world evidence (RWE) in regulatory and HTA decision-making has accelerated the adoption of these methods [14]. As health systems increasingly rely on evidence beyond traditional clinical trials, understanding the strengths, limitations, and proper application of quasi-experimental designs and g-methods becomes essential for researchers, scientists, and drug development professionals [40]. This guide provides a comprehensive comparison of these advanced causal methods, their experimental protocols, and their application within the context of RWE validation for HTA research.
Quasi-Experimental Designs: Theory and Applications
Fundamental Concepts and Definitions
Quasi-experimental designs are research methodologies that lie between the rigor of true experiments and the flexibility of observational studies [41]. Unlike RCTs where investigators randomly assign participants to groups, quasi-experiments evaluate interventions without random assignment, often leveraging naturally occurring circumstances that create experimental and control groups [41] [42]. The defining feature that distinguishes quasi-experiments from other observational designs is that they specifically evaluate the impact of a clearly defined event or process which results in differences in exposure between groups [42].
These designs are particularly valuable when investigating real-world interventions such as policy changes, health system reforms, or large-scale public health initiatives where randomization is impractical or unethical [41] [39]. For example, studying the health impacts of natural disasters, evaluating the effect of a new hospital funding model, or assessing the effectiveness of a public health campaign are all scenarios well-suited to quasi-experimental approaches [41] [39] [42].
Core Quasi-Experimental Designs: Methodologies and Protocols
Interrupted Time Series (ITS)
Experimental Protocol: ITS analysis identifies intervention effects by comparing the level and trend of outcomes before and after an intervention at multiple time points [39]. The design requires collecting data at regular intervals both pre- and post-intervention.
Model Specification: The basic ITS model can be represented as [39]: Yâ‚œ = β₀ + βâ‚T + β₂Xâ‚œ + β₃TXâ‚œ + εₜ Where Yâ‚œ is the outcome at time t, T is time since study start, Xâ‚œ is a dummy variable representing the intervention (0 = pre, 1 = post), and TXâ‚œ is the interaction term.
Key Elements: β₀ represents the baseline outcome level, β₠captures the pre-intervention trend, β₂ estimates the immediate level change following intervention, and β₃ quantifies the change in trend post-intervention [39].
Application Example: Researchers used ITS to evaluate the impact of Activity-Based Funding on patient length of stay following hip replacement surgery in Ireland, analyzing data points before and after the policy implementation in 2016 [39].
Difference-in-Differences (DiD)
Experimental Protocol: DiD estimates causal effects by comparing outcome changes between a treatment group exposed to an intervention and a control group not exposed, both before and after the intervention [39].
Design Requirements: The method requires at least two groups (treatment and control) and two time periods (pre- and post-intervention). The key assumption is that both groups would have followed parallel trends in the absence of the intervention.
Implementation: When studying Ireland's Activity-Based Funding reform, researchers used private patients as a control group since they continued to be reimbursed under the previous per-diem system, while public patients transitioned to the new DRG-based funding model [39].
Analysis: The DiD estimator is calculated as: (YÌ„treatment,post - YÌ„treatment,pre) - (YÌ„control,post - YÌ„control,pre).
Regression Discontinuity Design (RDD)
Experimental Protocol: RDD assigns participants to treatment based on a cutoff score of a pretreatment variable, comparing outcomes between individuals just above and below the threshold [43] [42].
Key Elements: This design capitalizes on the assumption that individuals immediately on either side of the cutoff are fundamentally similar except for their treatment eligibility [43].
Application Example: A study of England's RSV vaccination program used RDD by leveraging the sharp age cutoff at 75 years to create a natural experiment. Researchers compared hospitalization rates between individuals just above and below the eligibility threshold to isolate the vaccine's causal effect [43].
Pretest-Posttest Design with Control Group
Experimental Protocol: In this widely used quasi-experimental design, researchers select a treatment group and a control group with similar characteristics [41]. Both groups complete a pretest, the treatment group receives the intervention, and then both groups complete a posttest.
Methodological Considerations: It is ideal if the groups' mean scores on the pretest are similar (p-value > .05), and researchers should compare demographic characteristics and other variables that might influence posttest scores [41].
Application Example: To assess the impact of an app-based game on memory in older adults, participants from Senior Center A used the game while those from Senior Center B continued usual activities. Both groups underwent memory tests before and after the 30-day intervention period [41].
G-Methods for Complex Longitudinal Data
Theoretical Foundation and Need for Advanced Methods
When using observational data to estimate causal effects of treatments on clinical outcomes, researchers must adjust for confounding variables. In the presence of time-dependent confounders that are affected by previous treatment, adjustments cannot be made via conventional regression approaches or standard propensity score methods [44]. These scenarios require more sophisticated approaches known collectively as g-methods [44].
Time-dependent confounding occurs when a variable influences both future treatment and the outcome, while also being affected by past treatment. This creates a situation where traditional adjustment methods lead to biased estimates. G-methods were developed specifically to address this challenge, enabling estimation of the causal effects of treatment strategies defined by treatment at multiple time points [44].
Key G-Methods: Approaches and Protocols
The G-Formula
Experimental Protocol: The g-formula (or parametric g-formula) involves simulating potential outcomes under different treatment strategies by modeling the outcome conditional on treatment and covariate history, then standardizing results to the observed covariate distribution [44].
Implementation Steps:
- Model the conditional distribution of outcomes given treatment history and time-dependent covariates.
- Model the distribution of time-dependent covariates given prior treatment and covariate history.
- Simulate outcomes for the population under different treatment strategies using these models.
- Compare average outcomes across strategies to estimate causal effects.
Key Assumptions: The method relies on exchangeability (no unmeasured confounding), consistency (well-defined interventions), and positivity (all treatments possible at all levels of covariates) [44].
Inverse Probability-Weighted Marginal Structural Models
Experimental Protocol: This approach uses inverse probability weights to create a pseudo-population in which the distribution of time-dependent confounders is balanced across treatment groups, breaking the association between past treatment and current confounders [44].
Implementation Steps:
- Model treatment assignment at each time point conditional on past covariate history.
- Calculate inverse probability of treatment weights for each participant.
- Fit a marginal structural model (typically a weighted regression) for the outcome as a function of treatment history.
- Use the model to estimate outcomes under different treatment strategies.
Application Context: These methods are particularly valuable in neurosurgical research and other clinical settings where treatment decisions evolve over time based on patient response and changing clinical characteristics [44].
Comparative Analysis of Methodological Approaches
Method Performance and Application Contexts
Table 1: Comparison of Quasi-Experimental Designs and Their Applications
| Method | Key Features | Data Requirements | Primary Applications | Key Assumptions |
|---|---|---|---|---|
| Interrupted Time Series | Analyzes pre- and post-intervention trends | Multiple observations pre- and post-intervention | Policy evaluations, system-level interventions [39] | No other concurrent changes affecting outcome |
| Difference-in-Differences | Compares changes between treatment and control groups | Pre/post data for both groups | Natural policy experiments, regional implementations [39] | Parallel trends between groups |
| Regression Discontinuity | Exploits sharp eligibility thresholds | Data around cutoff point | Program evaluations with clear eligibility rules [43] | Continuity of potential outcomes at cutoff |
| Synthetic Control | Constructs weighted comparator from multiple units | Panel data for treatment and pool of control units | Evaluating interventions affecting single units (states, countries) [39] | No unmeasured time-varying confounding |
Table 2: Comparison of G-Methods for Time-Dependent Confounding
| Method | Approach | Strengths | Limitations | Suitable Contexts |
|---|---|---|---|---|
| G-Formula | Simulates outcomes under treatment strategies | Handles complex interactions; direct standardization | Requires correct specification of multiple models | Long-term treatment effects; dynamic treatment regimes [44] |
| Inverse Probability-Weighted MSMs | Weighting to balance confounders | Simpler model specification; handles time-varying confounding | Unstable weights with strong confounding; positivity violations | Sustained treatment comparisons; complex longitudinal data [44] |
Empirical Performance and Validation
A comprehensive comparison of four quasi-experimental methods evaluating Ireland's introduction of Activity-Based Funding revealed important differences in performance and interpretation [39]. The study focused on length of stay following hip replacement surgery and found that:
- Interrupted Time Series analysis produced statistically significant results suggesting a reduction in length of stay, differing in interpretation from control-treatment methods [39].
- Difference-in-Differences, Propensity Score Matching DiD, and Synthetic Control methods incorporating control groups suggested no statistically significant intervention effect on patient length of stay [39].
- This comparison highlights that different analytical methods for estimating intervention effects can provide substantially different assessments of the same intervention [39].
These findings underscore the importance of employing appropriate designs that incorporate a counterfactual framework, as methods with control groups tend to be more robust and provide a stronger basis for evidence-based policy-making [39].
Implementation in Real-World Evidence Generation
Methodological Integration in Health Technology Assessment
The use of quasi-experimental designs and g-methods in RWE generation for HTA requires careful attention to methodological rigor and validation. Several frameworks have been developed to improve the acceptability of these approaches [40]:
Target Trial Framework: This approach involves emulating a hypothetical randomized trial that would answer the research question, then designing the observational analysis to approximate this target trial [42]. This framework strengthens causal claims from natural experiment studies by clarifying the strength of evidence underpinning effectiveness claims [42].
Transparent Reporting: The Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) guideline provides a 22-item checklist for researchers using quasi-experimental designs [41].
Demonstration Projects: These projects benchmark nonrandomized study results against RCT evidence to highlight the value and applicability of best-practice methods [40].
Addressing Methodological Challenges
Several challenges persist in the application of advanced causal methods in RWE generation:
Residual Confounding: Despite sophisticated methods, residual confounding remains a concern in nonrandomized studies [40]. Recommended approaches include negative-control outcomes and comprehensive sensitivity analyses [43].
Data Quality and Accessibility: Timely access to high-quality RWD remains a barrier, requiring improvements in data quality, integration, and accessibility [40].
Transportability: Applying results based on data from one population to estimate effects for another population requires adjusting for relevant differences in demographic, clinical, and other factors [14].
Table 3: Research Reagent Solutions for Causal Inference Studies
| Research Tool | Function | Application Context | Considerations |
|---|---|---|---|
| TREND Guidelines | 22-item checklist for reporting quasi-experimental studies [41] | Improving transparency and reproducibility of nonrandomized designs | Essential for publication and peer review |
| Target Trial Framework | Protocol for emulating hypothetical randomized trials [42] | Strengthening causal inference from observational data | Clarifies assumptions and estimands |
| Propensity Score Methods | Balancing covariates between treatment and control groups [14] | Reducing confounding in observational studies | Requires careful model specification |
| Synthetic Control Algorithm | Constructs counterfactual from weighted combinations of control units [39] | Evaluating interventions affecting single units | Particularly useful for policy evaluations |
| G-Methods Software | Implementation of g-formula and IPW-MSM | Addressing time-dependent confounding | Requires specialized statistical packages |
Visualizing Methodological Approaches and Applications
Quasi-Experimental Design Selection Framework
G-Methods Application Workflow
Advanced causal methods including quasi-experimental designs and g-methods provide powerful approaches for generating real-world evidence when randomized trials are not feasible or ethical. The proper application of these methods requires careful consideration of design elements, underlying assumptions, and potential sources of bias. As regulatory and HTA bodies increasingly accept well-conducted nonrandomized studies, researchers must employ robust methodologies that incorporate counterfactual thinking, transparent reporting, and comprehensive validation. By selecting appropriate designs based on the research question and available data, and by addressing key methodological challenges, researchers can strengthen the evidence base for health technology assessment and policy decision-making.
Building External Control Arms for Single-Arm Trials in Rare Diseases
The development of therapies for rare diseases faces a unique set of challenges that render traditional randomized clinical trials (RCTs) frequently impractical, unethical, or simply unfeasible [45] [46]. The fundamental obstacle is patient scarcity; with small, geographically dispersed populations, recruiting enough participants to power both a treatment and a concurrent control arm is often impossible [45] [47]. Evidence suggests that up to 30% of clinical trials in rare diseases are prematurely discontinued due to patient accrual issues, while many others fail to achieve target recruitment or suffer severe delays [45].
Furthermore, ethical concerns are pronounced. In life-threatening rare diseases with no approved standard of care, assigning patients to a placebo arm can be unethical [46]. Patient populations are also less willing to participate or remain in placebo-controlled trials given the potential for being assigned to the control arm [45]. To overcome these critical barriers, researchers are increasingly turning to single-arm trials supplemented with External Control Arms (ECAs) [45]. According to regulatory guidelines, an externally controlled trial is defined as "one in which the control group consists of patients who are not part of the same randomized study as the group receiving the investigational agent" [45]. By providing a rigorously matched comparator group constructed from historical data, ECAs enable the assessment of treatment efficacy and safety, thereby supporting regulatory submissions and accelerating the delivery of new therapies to patients with high unmet medical needs [45] [47].
Methodological Approaches for Constructing External Control Arms
Constructing a scientifically rigorous ECA requires a structured methodology to minimize bias and confounding, which are inherent risks when using non-randomized data. The goal is to emulate a hypothetical randomized trial as closely as possible.
Core Principles and the Target Trial Framework
The most robust approach for designing an ECA is Target Trial Emulation (TTE) [48]. This framework involves explicitly specifying the protocol of an ideal randomized trial (the "target trial") that would answer the research question, and then closely emulating its key elements using Real-World Data (RWD) [48]. The main pillars of this approach include [49]:
- Eligibility Mirroring: Applying the same inclusion and exclusion criteria from the single-arm trial to the RWD cohort.
- Temporal Alignment: Ensuring index dates (e.g., start of treatment) and follow-up periods are defined consistently between the trial and external control patients.
- Covariate Harmonization: Using a common data model to guarantee consistent definitions for patient characteristics, exposures, and outcomes across different data sources.
- Estimand Clarity: Pre-specifying the treatment effect of interest (e.g., average treatment effect on the treated) and how intercurrent events (like treatment switching) will be handled [48].
Key Analytical Techniques for Bias Mitigation
Without randomization, statistical methods are critical to adjust for differences in baseline characteristics between the treatment and control groups.
- Propensity Score (PS) Methods: This is a cornerstone technique for creating comparable groups [45] [47]. A propensity score is the probability of a patient being assigned to the treatment group, given their observed covariates. The primary methods using PS are:
- Propensity Score Weighting: Patients from the external control arm are weighted so that the distribution of their baseline characteristics resembles that of the trial population. A common technique is Inverse Probability of Treatment Weighting (IPTW) [50].
- Propensity Score Matching: Each patient in the treatment arm is matched to one or more patients in the external control arm with a similar propensity score, creating a matched cohort for analysis [51].
- Federated Learning for ECAs: Data privacy regulations can make pooling patient data from multiple sources impossible. Federated ECA methods, like FedECA, have been developed to address this [50]. These methods allow for model training (e.g., propensity score models or Cox models) across multiple data centers without moving or pooling the raw data, thus preserving privacy while enabling robust analyses [50].
Comparative Analysis of ECA Methodologies and Applications
The selection of an appropriate ECA methodology depends on the research context, data availability, and specific constraints of the study. The table below provides a structured comparison of the primary methodological approaches.
Table 1: Comparison of Primary Methodologies for Constructing External Control Arms
| Methodology | Core Principle | Key Advantages | Inherent Challenges | Ideal Application Context |
|---|---|---|---|---|
| Propensity Score Matching | Creates 1:1 or 1:N matched cohorts from the ECA to the treatment arm based on similar probability of treatment [51]. | Intuitive; creates a directly comparable cohort; simple to analyze post-matching. | Can exclude unmatched treatment patients, potentially reducing sample size and power [51]. | When the RWD source is large enough to find high-quality matches for most trial participants. |
| Inverse Probability Weighting (IPTW) | Weights patients in the ECA to balance the covariate distribution with the treatment arm [50]. | Uses all data from both arms; avoids discarding patients. | Can be sensitive to extreme weights (if PS is near 0 or 1), leading to unstable estimates. | Standard approach for covariate balancing; suitable for a wide range of scenarios. |
| Federated ECA (e.g., FedECA) | Performs IPTW or other analyses without pooling raw data from different sources, using privacy-enhancing technology [50]. | Enables multi-institutional collaboration where data sharing is prohibited; maintains data privacy. | Increased technical complexity; requires a federated network infrastructure. | When control data is distributed across multiple hospitals or registries that cannot share data. |
| Matching-Adjusted Indirect Comparison (MAIC) | Weights individual patient data from a treatment arm to match aggregate-level statistics (e.g., means) from an external arm [50]. | Can be used when only summary statistics are available for the comparator. | Only balances the moments of the distribution communicated in the summary; does not guarantee full multivariate balance. | When Individual Patient Data (IPD) is available for the treatment arm but only aggregate data for the control. |
Quantitative Trends in ECA Adoption and Regulatory Acceptance
The use of ECAs is gaining significant traction in regulatory and Health Technology Assessment (HTA) submissions, particularly in fields like oncology and rare diseases. The data below highlights this growing acceptance.
Table 2: Quantitative Evidence of ECA Adoption in Regulatory and HTA Decisions
| Metric | Quantitative Data | Source / Context |
|---|---|---|
| HTA Submissions with ECs | 52% of 433 single-arm trial-based HTA submissions (2011-2019) contained external comparator data [48]. | Global HTA submissions [48]. |
| NICE Submissions with RW-ECAs | 18 submissions between 2019-2024, 16 in oncology [49]. | UK's National Institute for Health and Care Excellence [49]. |
| Growth in HTA Submissions | 20% increase in RW-ECAs submitted to global HTA agencies (2018-2019 vs. 2015-2017) [49]. | Analysis of HTA submission trends [49]. |
| FDA Accelerated Approvals | 67% of FDA accelerated approvals (1992–2017) were based on single-arm trials [49]. | Oncology and hematology drug approvals [49]. |
| FDA Approvals with External Controls | 45 U.S. FDA approvals with external control data in their benefit/risk assessment over two decades [47]. | Primarily in rare diseases and oncology [47]. |
Experimental Protocols for Robust External Control Arm Construction
To ensure credibility with regulators and HTA bodies, the construction of an ECA must follow a pre-specified, transparent protocol. The following workflow details the key steps.
Workflow for ECA Generation
The diagram below outlines the standard operational workflow for generating and validating an External Control Arm.
Protocol Steps and Methodological Details
Feasibility Assessment: Before beginning, a comprehensive assessment is essential to confirm that the available RWD source is fit-for-purpose [45]. This involves verifying that the database contains a sufficient number of patients from a largely comparable target population, captures accurate data on key confounders, treatments, and endpoints, and that patient management practices are consistent with the trial setting [45].
Data Source Selection: Choose the most appropriate RWD source. Electronic Health Records (EHRs) and disease-specific registries are often preferred for their detailed clinical information, while claims databases are richer in treatment utilization data but may have less robust clinical outcomes [45] [52].
Study Design & Target Trial Emulation: Specify all elements of the "target trial," including eligibility criteria, treatment strategies, assignment procedures, start and end of follow-up, outcomes, and estimand [48]. This plan should be documented in a pre-registered statistical analysis plan.
Covariate Harmonization and Cohort Construction: A Common Data Model (CDM), such as the OMOP CDM, is used to standardize data from both the clinical trial and the RWD source into a consistent format [49] [53]. The trial's eligibility criteria are then operationalized and applied to the RWD to select the external control cohort [49].
Bias Mitigation Analysis: Implement a pre-specified statistical method to adjust for confounding.
- Protocol: For PS weighting, first fit a logistic regression model (the propensity model) where the dependent variable is treatment assignment (trial vs. ECA) and independent variables are all pre-specified potential confounders. Then, calculate weights, typically using Inverse Probability of Treatment Weighting (IPTW) [50]. Assess covariate balance after weighting using metrics like Standardized Mean Differences (SMD), aiming for an SMD <0.1 for all key variables [50].
- Experimental Consideration: The propensity model must be informed by clinical expertise to ensure all relevant prognostic variables are included. The choice of variables is a critical step to reduce residual confounding [49].
Outcome Comparison and Sensitivity Analysis: After balancing the cohorts, compare the time-to-event or binary outcomes between the weighted or matched groups using appropriate statistical models (e.g., a weighted Cox proportional hazards model) [50]. To assess robustness, conduct extensive sensitivity analyses [49]. This includes varying the covariate set in the propensity model, using different analytical methods, and performing quantitative bias analysis (e.g., E-value analysis) to quantify how much unmeasured confounding would be needed to explain away the observed effect [49].
The Scientist's Toolkit: Essential Reagents for ECA Research
Building a regulatory-grade ECA requires a suite of methodological "reagents" and tools. The following table catalogs the key components and their functions in the experimental workflow.
Table 3: Essential Research Reagents for Constructing External Control Arms
| Tool / Component | Category | Function in ECA Research |
|---|---|---|
| Real-World Data (RWD) Sources | Data Foundation | Provides the raw patient-level data for constructing the control cohort. Sources include EHRs, claims databases, disease registries, and historical clinical trials [45] [46]. |
| Common Data Model (CDM) | Data Standardization | A standardized data structure (e.g., OMOP CDM) that enables harmonization of disparate data sources by transforming them into a common format, ensuring consistent definitions of variables [49] [53]. |
| Propensity Score Model | Statistical Algorithm | A model (typically logistic regression) that estimates the probability of a patient being in the treatment arm vs. the control arm based on their covariates. It is the engine for balancing confounding variables [45] [47]. |
| Balance Diagnostics (SMD) | Validation Metric | A quantitative measure (Standardized Mean Difference) used to assess the effectiveness of propensity score methods in achieving comparability between groups for each covariate. SMD <0.1 indicates good balance [50]. |
| Inverse Probability Weighting (IPTW) | Analytical Technique | A weighting technique that uses the propensity score to create a pseudo-population in which the distribution of measured confounders is independent of treatment assignment [50]. |
| Quantitative Bias Analysis | Sensitivity Tool | A set of methods (e.g., E-value analysis) used to quantify the potential impact of residual unmeasured confounding on the study results, thus assessing the robustness of the findings [49]. |
| Federated Learning Platform | Privacy-Enabling Technology | Software infrastructure that enables the execution of analytical models (e.g., propensity score or survival models) across multiple decentralized data sources without moving or pooling the data [50]. |
| Propargyl-PEG12-OH | Propargyl-PEG13-alcohol|Click Chemistry Reagent | Propargyl-PEG13-alcohol for copper-catalyzed click chemistry with azides. Features a hydrophilic PEG spacer. For Research Use Only. Not for human use. |
| Propargyl-PEG5-NHS ester | Propargyl-PEG5-NHS ester, CAS:1393330-40-9, MF:C18H27NO9, MW:401.4 g/mol | Chemical Reagent |
The construction and validation of External Control Arms represent a paradigm shift in clinical development for rare diseases, offering a scientifically rigorous solution when traditional RCTs are not viable. The successful application of this methodology, as evidenced by a growing number of regulatory and HTA approvals, hinges on a commitment to methodological rigor [45] [49] [52]. This involves the principled emulation of a target trial, the diligent application of robust statistical methods like propensity scores to mitigate bias, and the transparent reporting of extensive sensitivity analyses [49] [48].
While ECAs are not a replacement for randomization when it is feasible, they provide a powerful tool for augmenting single-arm trials, accelerating patient access to novel therapies, and fulfilling the urgent unmet needs in rare diseases [51]. As regulatory frameworks and methodological standards continue to evolve, the role of ECAs is poised to expand, solidifying their place as an indispensable component in the modern clinical development toolkit.
Validating Surrogate Endpoints with RWE for Long-Term Outcome Prediction
In the accelerated development of modern therapies, particularly in oncology and rare diseases, surrogate endpoints have become indispensable. These intermediate outcomes—such as Progression-Free Survival (PFS) in oncology or biomarker levels in chronic diseases—allow for smaller, faster, and less expensive clinical trials compared to those requiring final clinical outcomes like Overall Survival (OS) or quality of life (QoL) measures [54]. However, their predictive value for these ultimate patient-relevant outcomes is not automatic and requires rigorous validation [55]. This is where Real-World Evidence (RWE) plays an increasingly critical role.
RWE, derived from the analysis of Real-World Data (RWD) collected during routine healthcare delivery, provides a mechanism to bridge the evidence gap between the controlled environment of randomized controlled trials (RCTs) and long-term, real-world clinical effectiveness [27]. For health technology assessment (HTA) bodies like the National Institute for Health and Care Excellence (NICE) and the Federal Drug Administration (FDA), establishing a validated link between a surrogate endpoint and a final outcome is paramount for positive reimbursement and access decisions [54] [55]. This guide compares the evolving methodologies and applications of RWE in this validation process, providing researchers and drug development professionals with the experimental frameworks and data standards needed to navigate this complex landscape.
Quantitative Landscape: Use and Validation of Surrogate Endpoints in HTA
The use of surrogate endpoints in HTA submissions is widespread but accompanied by varying levels of validation evidence. A 2025 review of recent NICE oncology appraisals provides a clear quantitative snapshot of this landscape [55].
Table 1: Use of Surrogate Endpoints in NICE Oncology Appraisals (2022-2023)
| Aspect of Use | Metric | Value |
|---|---|---|
| Appraisal Scope | Total NICE Technology Appraisals (TAs) reviewed | 47 |
| Utilization | TAs utilizing surrogate endpoints | 18 (38%) |
| Endpoints Analyzed | Separate surrogate endpoints discussed | 37 |
| Evidence for Validation | Based on Randomized Controlled Trial (RCT) evidence | 11 endpoints |
| Based on observational study evidence | 7 endpoints | |
| Based on clinical opinion only | 12 endpoints | |
| Providing no evidence for use | 7 endpoints |
This data reveals a critical insight: despite the availability of advanced statistical methods for validation, the evidence supporting surrogate relationships in HTA submissions is highly inconsistent [55]. This inconsistency directly contributes to uncertainty in HTA decision-making and can constrain market access and pricing [54]. For example, the case of Olaparib (Lynparza) demonstrates that even with regulatory approval based on PFS, HTA bodies like HAS in France and G-BA in Germany limited broad access due to uncertainties about whether PFS gains would translate into OS or QoL improvements [54].
Methodological Frameworks for Validation
Conceptual Validation Pathway
The process of validating a surrogate endpoint is a multi-stage journey from evidence generation to HTA acceptance. The following diagram outlines the key conceptual stages and the role of RWE at each step.
Ciani et al. Three-Stage Validation Framework
A widely recognized framework for surrogate endpoint validation, proposed by Ciani et al., involves a structured, three-stage process [55]:
Establish the Level of Evidence: This initial stage categorizes the available evidence supporting the surrogate relationship.
- Lowest Level: Biological plausibility of the relationship.
- Intermediate Level: Demonstration of an association between the surrogate endpoint and the final outcome.
- Highest Level: Evidence that the treatment effect on the surrogate endpoint is consistently associated with the treatment effect on the final outcome across multiple studies.
Assess the Strength of Association: This involves quantifying the statistical relationship between the surrogate and the final outcome, for example, through correlation coefficients or meta-regression.
Quantify the Predictive Relationship: The final stage involves developing a model to predict the treatment effect on the final outcome based on the observed effect on the surrogate endpoint.
RWE is uniquely positioned to contribute across all three stages, particularly in strengthening the external validity of evidence generated in RCTs [56].
Experimental Protocols for RWE Generation
To generate robust RWE for surrogate validation, researchers can employ several key methodological approaches. The following workflow details the sequential steps for two primary study designs.
Protocol 1: Target Trial Emulation
This framework designs an observational study to mimic a hypothetical, pragmatic RCT [57].
- Define the Protocol: Specify the eligibility criteria, treatment strategies of interest (including dose, timing, and switching rules), treatment assignment process, primary outcome (the final clinical outcome, e.g., OS), and follow-up period.
- Implement the Study: Identify a cohort from RWD sources (e.g., EHRs, registries) that meets the eligibility criteria. "Clone" patients eligible for either treatment strategy and censor them when they deviate from their assigned strategy.
- Adjust for Confounding: To account for the lack of randomization, use causal inference methods like Propensity Score (PS) matching, weighting, or stratification to balance baseline covariates between the treatment and control groups. Alternatively, use doubly robust methods (e.g., Augmented Inverse Probability Weighting - AIPW) that combine PS and outcome models for more robust estimation [57].
- Analyze and Validate: Estimate the effect of treatment on both the surrogate and the final outcome. The association between these estimated effects across different patient subgroups or RWD sources can provide evidence for surrogacy.
Protocol 2: Construction of an External Control Arm (ECA)
Used when single-arm trial data is available for the new treatment, but a comparator is needed [56].
- Cohort Identification: Identify a relevant control cohort from RWD sources such as disease registries, historical clinical trials, or EHR-derived datasets. The FDA has accepted ECAs from sources like the Center for International Blood and Marrow Transplant Research (CIBMTR) registry [58].
- Apply Eligibility Criteria: Apply the same inclusion and exclusion criteria from the single-arm trial to the potential ECA cohort to ensure population comparability.
- Control Matching: Use PS matching or other matching techniques to select patients from the ECA pool who are similar to the patients in the single-arm trial across key prognostic factors [59].
- Outcome Comparison: Compare the treatment effect on the surrogate endpoint between the single-arm trial and the ECA. Subsequently, use RWD to track the long-term final outcome in both groups to establish the link between the surrogate and the final outcome.
The Scientist's Toolkit: Essential Reagents and Data Solutions
Generating high-quality RWE for surrogate validation requires a suite of "research reagents"—in this context, data sources, analytical tools, and methodological standards.
Table 2: Essential Research Reagent Solutions for RWE Generation
| Category | Item | Function in Validation |
|---|---|---|
| Data Sources | Electronic Health Records (EHRs) | Provides deep clinical granularity, including lab results, diagnoses, and rich unstructured notes for understanding disease progression and patient profiles [59] [27]. |
| Disease & Product Registries | Curated, prospective data on patients with specific conditions or using specific treatments; ideal for long-term outcome tracking and studying rare diseases [27]. | |
| Claims & Billing Data | Offers a longitudinal view of patient journeys, healthcare resource utilization, and treatment patterns at a large scale [59]. | |
| Patient-Reported Outcomes (PROs) | Captures the patient's voice on symptoms, functioning, and quality of life, which is often the ultimate final outcome of interest [59]. | |
| Analytical Methods | Propensity Score Matching | Reduces selection bias in observational studies by creating balanced comparison groups that mimic randomization [59] [56]. |
| Doubly Robust Estimators (AIPW, TMLE) | Combines PS and outcome models to provide valid effect estimates even if one of the two models is misspecified, strengthening causal inference [57]. | |
| Transportability/Generalizability Analysis | Uses weighting methods to extend or transport findings from an RCT to a broader, real-world population represented in RWD [57] [56]. | |
| Methodological Standards | Target Trial Emulation Framework | Provides a structured blueprint for designing observational studies to minimize bias and strengthen causal conclusions [57]. |
| ISPOR/ISPE Good Practice Guidelines | Offers best-practice recommendations for the design, analysis, and reporting of RWE studies to ensure scientific rigor [56]. | |
| PS47 | (E)-5-(4-Chlorophenyl)-3-phenylpent-2-enoic Acid|RUO | High-quality (E)-5-(4-Chlorophenyl)-3-phenylpent-2-enoic acid for research use only (RUO). Explore its value in scientific discovery. Not for human or veterinary use. |
| RG2833 | RG2833, CAS:1215493-56-3, MF:C20H25N3O2, MW:339.4 g/mol | Chemical Reagent |
Regulatory and HTA Perspectives: A Shift Towards Conditional Acceptance
Global regulatory and HTA bodies are increasingly accepting RWE, but this acceptance is conditional upon methodological rigor and data quality.
- FDA: The FDA has utilized RWE to support regulatory decisions, including drug approvals and label expansions. Examples include using medical records as confirmatory evidence for Aurlumyn (iloprost) and a registry-based ECA for Orencia (abatacept) [58]. The FDA's RWE Framework and Sentinel Initiative demonstrate a commitment to integrating real-world data into regulatory science [58] [57].
- NICE: While NICE accepts surrogate endpoints, it often requires a robust evidence package linking them to final outcomes. A 2025 analysis of NICE appraisals found that committees accepted the highest level of evidence for surrogate endpoints when companies submitted it [60]. However, uncertainty often leads to managed access agreements, such as the Cancer Drugs Fund, which mandates the collection of further RWE to reduce uncertainty [54] [55].
- EMA & Other HTAs: European regulators and HTA bodies like HAS (France) and IQWiG (Germany) have revised their guidance on surrogates, reflecting a demand for more rigor and transparent validation, often supported by RWE [54].
The overarching trend is clear: HTA bodies rarely accept surrogate endpoints in isolation. They increasingly expect a holistic evidence package that combines surrogate data from RCTs with complementary RWE, patient-reported outcomes, and plans for confirmatory studies [54].
The validation of surrogate endpoints with RWE is no longer a theoretical exercise but a practical necessity for successful drug development and market access. As demonstrated by recent HTA appraisals, the variability in validation evidence directly impacts decision-making and patient access. By employing rigorous experimental protocols like target trial emulation and external control arm design, and by leveraging the growing toolkit of data sources and causal analytical methods, researchers can build the robust evidence needed. The future of surrogate validation lies in the principled integration of RCT and RWE, creating a continuous evidence generation cycle that begins with accelerated approval and culminates in confirmed long-term value for patients and healthcare systems.
Real-world evidence (RWE) is increasingly recognized as a crucial component in the regulatory decision-making process for medical products. Defined as clinical evidence regarding a medical product's use and potential benefits or risks derived from the analysis of real-world data (RWD), RWE has moved beyond its traditional role in postmarket safety monitoring to support both efficacy and safety determinations in regulatory approvals [2]. The 21st Century Cures Act of 2016 significantly accelerated this trend by encouraging the Food and Drug Administration (FDA) to develop a framework for evaluating RWE to support drug approval [61]. This article examines specific case studies where RWE played a pivotal role in FDA regulatory decisions, providing researchers and drug development professionals with practical insights into successful RWE implementation strategies.
The FDA has established a comprehensive framework for evaluating the potential use of RWE, creating specialized committees such as the RWE Subcommittee within CDER's Medical Policy and Program Review Council to guide policy development and provide advisory recommendations on RWE submissions [61]. This institutional support has facilitated the growing acceptance of RWE across therapeutic areas, particularly in oncology, rare diseases, and areas where randomized controlled trials (RCTs) present ethical or practical challenges.
Quantitative Landscape of RWE in Regulatory Decisions
Recent data reveals a steady increase in RWE incorporation into regulatory submissions. A comprehensive review of supplemental new drug applications (sNDAs) and biologic license applications (sBLAs) from January 2022 to May 2024 found that RWE supported approximately 24% of labeling expansion approvals during this period [62]. The analysis identified 218 supplemental approvals aimed at expanding indications or populations, with RWE present in regulatory documents for numerous approvals.
Table 1: Therapeutic Areas Utilizing RWE in Labeling Expansions (2022-2024)
| Therapeutic Area | Percentage of RWE Submissions | Primary RWE Applications |
|---|---|---|
| Oncology | 43.6% | Comparative effectiveness, safety monitoring, external controls |
| Infectious Diseases | 9.1% | Treatment outcomes, population effectiveness |
| Dermatology | 7.3% | Long-term safety, dosing patterns |
| Other Areas | 40.0% | Varied applications across specialties |
The same study found that the majority of RWE submissions supported drug applications (69.1%) versus biological products, and most were intended for expanding indications (78.2%) rather than broadening populations within existing indications [62]. This distribution reflects the strategic application of RWE to address specific evidence gaps throughout the product lifecycle.
Case Studies: RWE for Regulatory Decision-Making
RWE as Confirmatory Evidence: Aurlumyn (Iloprost)
In February 2024, the FDA approved Aurlumyn (iloprost) for severe frostbite, with RWE serving as confirmatory evidence in the regulatory decision [58]. The approval leveraged a multicenter retrospective cohort study of frostbite patients using historical controls derived from medical records. This approach was particularly valuable for studying a condition where conducting a randomized controlled trial would be ethically challenging due to the urgent nature of frostbite treatment.
- Data Source: Medical records from multiple treatment centers
- Study Design: Retrospective cohort study with historical controls
- Regulatory Role: Confirmatory evidence supporting efficacy
- Outcome: Demonstrated improved outcomes compared to natural history of severe frostbite
The successful incorporation of RWE in this approval demonstrates how historical control groups derived from real-world data can provide adequate comparators when randomized controls are impractical or unethical.
RWE for Safety Assessment: Vimpat (Lacosamide)
In April 2023, the FDA approved a new loading dose regimen for Vimpat (lacosamide) in pediatric patients with epilepsy, using RWE to address specific safety concerns [58]. While efficacy for partial onset seizures was extrapolated from existing adult data, additional safety data were needed for the new proposed loading dose regimen in pediatric populations.
- Data Source: Medical records from the PEDSnet data network
- Study Design: Retrospective cohort study
- Regulatory Role: Safety assessment for new dosing regimen
- Outcome: Provided sufficient safety evidence to support new pediatric loading dose
This case illustrates how RWE can complement extrapolated efficacy data by providing product-specific safety information, particularly for special populations like children where dedicated clinical trials may be limited.
RWE as Pivotal Evidence: Orencia (Abatacept)
The December 2021 approval of Orencia (abatacept) for prophylaxis of acute graft-versus-host disease (aGVHD) demonstrated the use of RWE as pivotal evidence in a regulatory decision [58]. The approval was based on two components: a traditional RCT in patients with matched unrelated donors and a non-interventional study using RWE in patients with one allele-mismatched unrelated donors.
- Data Source: Center for International Blood and Marrow Transplant Research (CIBMTR) registry
- Study Design: Non-interventional study
- Regulatory Role: Pivotal evidence for specific subpopulation
- Outcome: Demonstrated improved overall survival compared to historical controls
This hybrid approach allowed for efficient evidence generation across multiple patient populations, with RWE providing crucial evidence for a subset where randomized trial data was unavailable.
RWE in Postmarket Safety Monitoring: Prolia (Denosumab)
The case of Prolia (denosumab) illustrates the important role of RWE in identifying and quantifying serious safety risks in postmarket settings. An FDA-conducted retrospective cohort study using Medicare claims data identified an increased risk of severe hypocalcemia in patients with advanced chronic kidney disease taking denosumab [58].
- Data Source: Medicare claims data
- Study Design: Retrospective cohort study
- Regulatory Role: Safety signal identification and quantification
- Outcome: Addition of Boxed Warning for increased risk in advanced CKD patients
This case highlights the value of systematic postmarket safety surveillance using routinely collected healthcare data to identify population-specific risks that may not have been fully apparent in premarketing trials.
Methodological Approaches in RWE Generation
Study Designs for RWE Generation
The credibility of RWE depends heavily on appropriate methodological approaches and study designs. The case studies above exemplify several robust methodologies that can generate regulatory-grade evidence.
Table 2: Methodological Approaches in RWE Studies
| Study Design | Key Applications | Regulatory Examples |
|---|---|---|
| Retrospective Cohort Studies | Safety assessment, comparative effectiveness, external controls | Vimpat, Aurlumyn, Prolia |
| Non-interventional Studies | Single-arm trial support, natural history comparisons | Orencia, Vijoice |
| Registry Studies | Long-term outcomes, rare disease endpoints | Orencia (CIBMTR registry) |
| Externally Controlled Trials | Natural history comparisons in rare diseases | Voxzogo, Nulibry |
| Pragmatic Clinical Trials | Real-world effectiveness in routine practice | Emerging approach across therapeutic areas |
Each methodology presents distinct advantages and limitations. Retrospective cohort designs offer efficiency and real-world generalizability but require careful attention to confounding control. Registry-based studies provide rich clinical data across multiple centers but may have variability in data collection practices. Externally controlled trials are particularly valuable in rare diseases but require meticulous attention to comparability between treatment and control groups [63].
The quality and appropriateness of data sources fundamentally impact the validity of RWE. Commonly used sources include:
- Electronic Health Records (EHR): Provide detailed clinical information including laboratory results, clinical assessments, and treatment details [62]
- Medical Claims Data: Offer comprehensive information on healthcare utilization, procedures, and diagnoses across systems [58]
- Disease Registries: Collect standardized data on specific patient populations, often with rich clinical detail [58]
- Medical Records: Facilitate deep clinical characterization through manual abstraction [58]
Recent research indicates that EHR data represents the most common source (75%) in RWE studies supporting labeling expansions, followed by claims data and registries [62]. The increasing sophistication of data linkages and curation methods continues to enhance the utility of these sources for regulatory decision-making.
Data to Evidence Pathway
The Research Toolkit: Essential Components for RWE Generation
Generating regulatory-grade RWE requires careful attention to data quality, methodological rigor, and appropriate analytical techniques. The following components represent essential elements for successful RWE generation.
Table 3: Research Reagent Solutions for RWE Generation
| Component | Function | Application Examples |
|---|---|---|
| Propensity Score Methods | Control for confounding in non-randomized studies | Balancing treatment and control groups in comparative effectiveness research |
| Electronic Health Record Systems | Capture structured and unstructured clinical data | Source for clinical endpoints, comorbidities, concomitant medications |
| Data Quality Assurance Tools | Ensure completeness, accuracy, and consistency | Validation checks, source data verification, anomaly detection |
| Terminology Mappings | Standardize coding across data sources | Mapping local codes to standard terminologies (e.g., SNOMED, ICD-10) |
| Clinical Registry Platforms | Collect prospective, standardized disease-specific data | Long-term outcomes assessment in rare diseases |
| Validated Patient-Reported Outcome Measures | Capture symptom and quality of life data | Effectiveness endpoints from patient perspective |
| RU 752 | Steroid Research Compound|(8S,9S,10R,11S,13S,14S)-11-hydroxy-10,13-dimethylspiro[2,6,7,8,9,11,12,14,15,16-decahydro-1H-cyclopenta[a]phenanthrene-17,5'-oxolane]-2',3-dione | High-purity (8S,9S,10R,11S,13S,14S)-11-hydroxy-10,13-dimethylspiro[2,6,7,8,9,11,12,14,15,16-decahydro-1H-cyclopenta[a]phenanthrene-17,5'-oxolane]-2',3-dione for Research Use Only (RUO). Not for human or veterinary diagnostic or therapeutic use. |
| S-acetyl-PEG6 | S-acetyl-PEG6-alcohol|PEG Linker |
Each component addresses specific methodological challenges in RWE generation. Propensity score methods help mitigate confounding by creating balanced comparison groups. Standardized terminology mappings enable consistent analysis across heterogeneous data sources. Clinical registry platforms facilitate prospective data collection with predefined elements relevant to specific diseases [63].
Analytical Framework for RWE Assessment
Regulatory assessment of RWE relies on systematic evaluation of study quality and relevance. The FDA and other regulatory bodies have developed frameworks to assess RWE submissions, focusing on key dimensions of validity and relevance.
RWE Assessment Framework
The assessment framework emphasizes several critical elements. Data quality assurance requires demonstration that RWD are fit-for-purpose, with sufficient completeness, accuracy, and provenance documentation. Study design appropriateness involves selecting designs that address specific research questions while minimizing inherent biases in non-randomized data. Confounding control remains paramount, requiring sophisticated statistical methods to address systematic differences between comparison groups. Comprehensive sensitivity analyses demonstrate the robustness of findings to various assumptions and methodological choices [1].
The case studies presented demonstrate that RWE can successfully support regulatory decisions across diverse contexts, from rare diseases to pediatric populations and postmarket safety monitoring. The expanding role of RWE reflects both methodological advances and evolving regulatory frameworks that recognize the value of well-generated real-world evidence.
Successful implementation requires strategic planning beginning early in product development. Engaging with regulatory agencies during the planning stages allows for alignment on evidence needs and study feasibility. Selecting appropriate data sources matched to specific research questions ensures that evidence will be fit-for-purpose. Employing rigorous methodological approaches with comprehensive sensitivity analyses enhances the credibility of generated evidence.
As RWE continues to evolve, emerging areas include greater use of digitally-derived endpoints, advanced causal inference methods, and international data collaborations. For researchers and drug development professionals, understanding these trends and methodologies will be essential for leveraging RWE throughout the product lifecycle, from early development through postmarket surveillance. The continued alignment between regulators, industry, and academia on standards for RWE generation will further enhance its role in supporting efficient therapeutic development and rigorous regulatory decision-making.
Navigating Data and Methodological Hurdles in RWE Validation
The validation of real-world evidence (RWE) for health technology assessment (HTA) research hinges on a fundamental prerequisite: establishing that the underlying real-world data (RWD) are fit-for-purpose. This concept signifies that data possess sufficient quality, relevance, and reliability to answer a specific research question and support subsequent regulatory and reimbursement decisions [64]. Within the evolving evidence landscape, HTA bodies are increasingly considering RWE to address uncertainties identified at product launch, particularly where traditional clinical trial data is limited or non-existent [15]. The critical appraisal of RWD quality and relevance therefore forms the cornerstone of generating trustworthy RWE that can confidently inform HTA deliberations and healthcare policy.
International regulatory and HTA bodies have aligned around key terms to describe fit-for-use RWE. As of early 2025, four major regulators – the US Food and Drug Administration (FDA), European Medicines Agency (EMA), Taiwan FDA, and Brazil ANVISA – have directly defined at least two of the three critical concepts: relevance, reliability, and quality [64]. This convergence indicates a growing global consensus on the essential attributes of RWD, even as practical implementation continues to evolve.
Defining the Core Dimensions of Fitness-for-Purpose
Regulatory and HTA Perspectives on Key Criteria
The Duke-Margolis International Harmonization of RWE Standards Dashboard has identified both areas of definitional alignment and misalignment across regulators [64]. The table below synthesizes how major regulatory and HTA bodies conceptualize the core dimensions of fitness-for-purpose.
Table 1: Regulatory and HTA Body Definitions of Fitness-for-Purpose Criteria
| Criterion | Definitional Alignment | Areas of Potential Misalignment |
|---|---|---|
| Relevance | - Data representativeness: Sufficient numbers of representative patients [64]- Research and regulatory concern: Dataset contains data elements useful to answer a given research question [64] | - Scenarios where clinical context drives data needs [64]- Ensuring adequate sample sizes for specific study questions [64] |
| Reliability | - Accuracy in data interpretation: Degree to which data accurately represent observed reality [64]- Quality and integrity during data accrual: Data accuracy, completeness, provenance, and traceability [64] | - Operationalizing data representation as a function of both reliability and relevance [64] |
| Quality | - Data quality assurance across sites and time: Assessment of completeness, accuracy, and consistency [64]- High quality data presents clarity and traceability in every aspect of its origin [64] | - Determining whether data element usefulness relates to 'relevance' versus 'quality' [64] |
Quantitative Landscape of RWD Guidance
The regulatory landscape for RWD is rapidly evolving, with significant growth in guidance documents from authorities worldwide. As of February 2025, the United States Food and Drug Administration (FDA) has released the most RWE guidance documents (13 total; 4 draft, 9 final), followed by the European Medicines Agency (EMA), China's National Medical Products Administration/Center for Drug Evaluation (NMPA/CDE), and Japan's Pharmaceuticals and Medical Devices Agency (PMDA), each with seven guidance documents [64]. This proliferation of guidance reflects the increasing importance of establishing standardized approaches to RWD evaluation across the lifecycle of medical products.
Methodological Frameworks for RWD Appraisal
Experimental Protocols for Assessing RWD Fitness
Researchers and HTA professionals can implement standardized methodological approaches to critically appraise RWD fitness-for-purpose. The following experimental protocols provide structured frameworks for evaluation.
Table 2: Methodological Protocols for RWD Fitness-for-Purpose Assessment
| Assessment Phase | Protocol Objective | Key Methodological Steps | Output Metrics |
|---|---|---|---|
| Data Accrual Quality Control | Evaluate quality and integrity during data collection [64] | 1. Document data provenance and traceability2. Implement accuracy checks at point of entry3. Establish completeness thresholds for required fields4. Monitor consistency across collection sites [64] | - Data accuracy rates- Completeness percentages- Cross-site consistency metrics |
| Representativeness Assessment | Determine how well data represents target population [64] | 1. Compare baseline characteristics to target population2. Analyze patterns of missing data3. Assess sampling framework adequacy4. Evaluate temporal representativeness [64] | - Standardized differences- Missing data patterns- Sample diversity indices |
| Relevance Verification | Confirm data contains elements needed for research question [64] | 1. Map available data elements to evidence needs2. Assess variable granularity for endpoint construction3. Verify clinical context documentation4. Evaluate follow-up duration adequacy [64] | - Data element coverage rate- Endpoint constructibility score- Clinical context documentation quality |
The Researcher's Toolkit: Essential Reagents for RWD Assessment
The successful implementation of RWD appraisal protocols requires specific analytical tools and frameworks. The table below details key "research reagents" – essential methodologies, tools, and approaches – for conducting fitness-for-purpose assessments.
Table 3: Research Reagent Solutions for RWD Fitness-for-Purpose Assessment
| Research Reagent | Function/Purpose | Application Context |
|---|---|---|
| Duke-Margolis RWE Standards Dashboard | Online tool tracking international regulatory guidance and definitions for RWD/E [64] | Comparative analysis of regulatory expectations; Identification of alignment/misalignment areas |
| CTTI Recommendations for RWD Use | Actionable tools for determining if RWD are fit-for-purpose for study planning [65] | Protocol development for clinical trials using RWD; Eligibility criteria assessment |
| Electronic Health Record (EHR) Data Quality Framework | Best practices for evaluating EHR-sourced data quality, relevance, and reliability at accrual phase [66] | Assessment of EHR-derived datasets for regulatory decision-making |
| Claims vs. EHR Comparative Analysis | Framework for understanding advantages/disadvantages of different RWD sources [65] | Selection of appropriate data sources for specific research questions |
| Quality by Design (QbD) Approach | Methodology for engaging stakeholders and focusing resources on errors that matter to decision-making [65] | Overall study design and conduct within broader clinical trial framework |
RWE Application in HTA Decision-Making
Current Landscape of RWE Use in HTA Reassessments
The integration of RWE into HTA processes is increasingly evident across international agencies. A recent review of 40 health technology assessment reassessments (HTARs) across six agencies found that 55% used RWE, with these reassessments tending to focus on orphan therapies [15]. The analysis revealed that RWE was primarily submitted to address clinical uncertainties, with the most common uncertainties relating to primary/secondary endpoints [15].
The majority of RWE studies (57.1%) came from registry data, demonstrating the importance of this data source in the HTA context [15]. Notably, the proportion of HTARs resulting in no change in patient access was similar between HTARs that did and did not use RWE, suggesting that RWE is playing a complementary rather than determinative role in many reassessments [15].
Addressing Selection Bias in RWD Analysis
Selection bias remains a significant methodological challenge in RWE generation for HTA. As noted by experts, dealing with selection bias requires first identifying potential sources, understanding how they could interfere with interpretation, and then applying appropriate methodological approaches to correct them [67]. The field has seen "tremendous progress" in methodologies to address such biases over recent years, providing researchers with improved tools to ensure valid inference from RWD analyses [67].
Diagram 1: RWD fitness-for-purpose appraisal workflow for HTA
Emerging Trends in RWD Appraisal
The parallel progress in artificial intelligence (AI) and RWE is creating new opportunities for clinical evidence generation [68]. Machine learning approaches show potential for enabling predictive treatment effect modeling from RWD, though challenges remain in consistently ensuring high-quality, reliable, and representative data while addressing bias, missing data, and other fundamental questions [68].
Internationally, regulatory harmonization continues to be a focus, with recent efforts including the ICH M14 guidelines on "General Principles on Plan, Design, and Analysis of Pharmacoepidemiological Studies That Utilize Real-World Data for Safety Assessment of Medicines" [68]. This alignment is crucial for establishing consistent standards for RWD acceptability across regulatory and HTA bodies.
The critical appraisal of RWD quality and relevance represents a fundamental requirement for validating real-world evidence in HTA research. As regulatory bodies increasingly align on core definitions of relevance, reliability, and quality, researchers must implement systematic methodological approaches to demonstrate fitness-for-purpose. The frameworks, protocols, and tools outlined in this guide provide a foundation for rigorous RWD assessment. As the field evolves, continued collaboration between regulators, HTA bodies, and researchers will be essential to refine these approaches and ensure that RWE reliably informs healthcare decision-making to improve patient outcomes.
The validation of real-world evidence (RWE) for health technology assessment (HTA) research hinges on the robust handling of bias and confounding. Unlike data from randomized controlled trials (RCTs), which are collected under highly controlled conditions, real-world data (RWD) are observational by nature, generated from routine clinical practice through sources like electronic health records (EHRs), insurance claims, and patient registries [69]. This fundamental characteristic introduces significant challenges, including selection bias, confounding by indication, measurement error, and missing data, which can compromise the internal validity of a study and the reliability of its evidence [69] [70]. Consequently, HTAs are increasingly defining methodological standards for using RWD, where a core requirement is the transparent identification and statistical adjustment for these biases to ensure that RWE is fit for purpose in decision-making [26] [56].
The journey from data collection to evidence-based conclusion requires a systematic approach to mitigate these threats. This process begins with a thorough understanding of the data's origin and inherent limitations, moves through the precise identification of potential biases, and culminates in the application of rigorous statistical methods to adjust for them [71] [70]. For HTA submissions, demonstrating a deliberate and well-executed strategy to manage bias and confounding is not merely a technical exercise but a critical factor in establishing the credibility and acceptability of the RWE presented [26] [67].
Identification of Common Biases in Real-World Data
Before any statistical adjustment can be applied, researchers must first identify the specific biases present in their RWD. The inherently observational and non-standardized nature of RWD sources makes them susceptible to several forms of bias that can distort the relationship between an intervention and an outcome.
- Selection Bias: This occurs when the study population is not representative of the target population, leading to systematic differences in characteristics between compared groups. In RWD, this can arise from how patients are selected into a healthcare system, specific hospitals, or registries [69]. For example, data from tertiary care centers may over-represent patients with more severe or complex diseases.
- Confounding: A confounder is a variable that is associated with both the exposure (e.g., treatment) and the outcome, but is not a consequence of the exposure. Confounding by indication is a particularly pervasive form in pharmacoepidemiology, where the underlying reason for prescribing a specific drug is also a prognostic factor for the outcome [70]. Failure to adjust for key confounders can lead to spurious conclusions about a treatment's effect.
- Information Bias: This encompasses errors in the measurement of exposure, outcome, or other variables. Misclassification bias, a type of information bias, is common in claims data where diagnosis codes may be used for billing rather than clinical accuracy [71].
- Immortal Time Bias: A specific, often overlooked bias in observational studies involving time-to-event analyses. It refers to a period in the follow-up of a cohort during which, by design, the outcome of interest (e.g., death) cannot occur, leading to an overestimation of survival or benefit [71].
The following table summarizes these key biases, their sources, and their potential impact on RWE.
Table 1: Key Biases in Real-World Data and Their Implications
| Bias Type | Description | Common Sources in RWD | Impact on RWE |
|---|---|---|---|
| Selection Bias | Systematic differences between study participants and the target population [69]. | Non-random entry into healthcare systems or registries; loss to follow-up [69]. | Compromises external validity and generalizability [56]. |
| Confounding | Distortion of the exposure-outcome relationship by a third, extraneous variable [70]. | Differences in patient demographics, disease severity, or comorbidities between treatment groups (e.g., confounding by indication) [70]. | Leads to incorrect estimates of treatment effect (either over or under-estimation). |
| Information Bias | Inaccuracies in the measurement or classification of variables [71]. | Inconsistent coding practices in claims data; incomplete EHR entries; patient recall error [71] [69]. | Introduces noise and error, biasing effect estimates towards or away from the null. |
| Immortal Time Bias | Misclassification of follow-up time during which the outcome could not occur [71]. | Incorrect alignment of time origins in cohort studies, such as in studies of drug exposure [71]. | Systematically inflates perceived survival or treatment benefit. |
Statistical Methods for Adjustment: A Comparative Guide
Once biases are identified, particularly confounding, researchers can employ a range of statistical methods to adjust for baseline differences between groups and strengthen causal inference. The following section provides a comparative guide to the most widely used approaches, summarizing their principles, advantages, and limitations in the context of RWE generation for HTA.
Table 2: Comparison of Statistical Methods for Adjusting for Confounding
| Method | Key Principle | Advantages | Disadvantages / Key Considerations |
|---|---|---|---|
| Multivariate Regression Adjustment | Controls for confounders by including them as covariates in a statistical model (e.g., Cox regression for survival outcomes) [71]. | - Simple and widely understood.- Efficiently controls for measured confounders.- Directly provides effect estimates. | - Assumes a specific model form (e.g., linearity).- Does not address baseline imbalances; model-dependent.- Can be unstable with many covariates [71]. |
| Propensity Score (PS) Matching | Creates a matched sample where treated and control units have similar probabilities (scores) of receiving the treatment [71]. | - Intuitively creates balanced groups mimicking RCTs.- Results are easy to communicate. | - Can discard unmatched data, reducing sample size and power.- Only controls for measured confounders used in the PS model.- Matching quality must be carefully assessed [71]. |
| Inverse Probability of Treatment Weighting (IPTW) | Uses the propensity score to create a pseudo-population where the distribution of confounders is independent of treatment assignment [71]. | - Uses all available data, preserving sample size.- Creates a balanced pseudo-population for analysis. | - Can be unstable if propensity scores are very close to 0 or 1, leading to extreme weights.- Use of stabilized weights is recommended to improve efficiency [71]. |
| Doubly Robust Estimation | Combines a model for the treatment (e.g., PS) and a model for the outcome (e.g., regression). Produces an unbiased estimate if either model is correct [71] [57]. | - More robust to model misspecification than methods relying on a single model.- Increases confidence in the results. | - Computationally more complex.- Requires specification of two models. |
| Target Trial Emulation | Applies the design principles of an RCT to the analysis of observational RWD by explicitly defining protocol components like eligibility, treatment strategies, and outcomes [69]. | - Provides a rigorous framework for causal inference.- Makes study assumptions and limitations transparent. | - Requires deep understanding of both trial design and RWD limitations.- Cannot fully replicate randomization. |
The workflow below illustrates the logical relationship between the problem of confounding and the selection of an appropriate statistical adjustment method.
Experimental Protocols for Key Methodologies
To ensure the scientific rigor demanded by HTA bodies, the application of adjustment methods must follow detailed, pre-specified protocols. Below are detailed methodologies for two cornerstone approaches: Propensity Score Matching and Target Trial Emulation.
Protocol for Propensity Score Matching and Analysis
This protocol outlines the step-by-step process for designing and executing a propensity score-matched analysis.
Step 1: Propensity Score Estimation
- Objective: To estimate each patient's probability of receiving the treatment of interest, conditional on their observed baseline covariates.
- Method: Fit a logistic regression model where the dependent variable is treatment assignment (e.g., 1=new drug, 0=comparator). Include all pre-specified baseline confounders believed to be associated with both treatment assignment and the outcome (e.g., age, sex, disease severity, comorbidities, prior medications).
- Output: A propensity score (PS) for each patient, ranging from 0 to 1 [71].
Step 2: Matching
- Objective: To create a new cohort where treated and control patients have similar distributions of PS (and thus measured covariates).
- Method: Use a 1:1 nearest-neighbor matching algorithm without replacement and a caliper width (e.g., 0.2 of the standard deviation of the logit of the PS) to prevent poor matches. Consider greedy or optimal matching algorithms [71].
Step 3: Assessing Balance
- Objective: To validate that the matching procedure successfully balanced baseline covariates between the groups.
- Method: Calculate the standardized mean difference (SMD) for each covariate before and after matching. An SMD <0.1 after matching is generally considered to indicate good balance. Visualize balance using love plots or jitter plots [71].
Step 4: Outcome Analysis
- Objective: To estimate the treatment effect within the matched cohort.
- Method: Analyze the outcome (e.g., overall survival, hospitalization) in the matched sample using a appropriate model. For time-to-event outcomes, use a Cox proportional hazards model. The model may either be unadjusted or include covariates for which minor residual imbalance exists to improve precision [71].
Step 5: Sensitivity Analysis
- Objective: To assess the potential impact of unmeasured confounding on the results.
- Method: Conduct a quantitative bias analysis, such as an E-value, which quantifies the strength of association an unmeasured confounder would need to have with both the treatment and outcome to explain away the observed effect [71].
Protocol for Target Trial Emulation
Target trial emulation applies the structured design of an RCT to RWD, forcing explicit specification of all key study components and minimizing ad hoc analytical decisions [69].
Step 1: Specify the Protocol of the "Target" Randomized Trial
- Define all core components of an ideal RCT that would answer the research question:
- Eligibility Criteria: Explicitly define inclusion and exclusion criteria based on variables available in the RWD.
- Treatment Strategies: Clearly define the initiation, dosage, and duration of the treatment and comparator regimens.
- Treatment Assignment: The protocol acknowledges that in RWD, assignment is not random but observational.
- Outcome: Define the primary and secondary outcomes, including how and when they are measured.
- Follow-up: Define the start of follow-up (time zero), and the end of follow-up (e.g., outcome occurrence, death, end of data availability).
- Causal Contrast: Define the effect of interest, such as the intention-to-treat or per-protocol effect [69] [56].
- Define all core components of an ideal RCT that would answer the research question:
Step 2: Emulate the Target Trial using RWD
- Eligibility: Apply the pre-specified eligibility criteria to the RWD source to create the study cohort.
- Treatment Assignment: Identify individuals who initiated the treatment strategies of interest during the enrollment period.
- Time Zero: Align time zero for all participants at the point of treatment initiation (or eligibility) to avoid immortal time bias.
- Follow-up: Follow patients from time zero until the occurrence of the outcome, a censoring event (e.g., end of data, loss to follow-up), or the end of the study period.
Step 3: Statistical Analysis to Estimate the Treatment Effect
- Objective: To estimate the causal effect as defined in the target trial protocol.
- Method: To account for confounding due to non-random assignment, use one of the adjustment methods described in Section 3, such as IPTW or doubly robust estimation. The analysis should be aligned with the causal contrast; for example, an intention-to-treat analysis would estimate the effect of treatment initiation, regardless of subsequent changes [69].
The Scientist's Toolkit: Essential Reagents for RWE Validation
Generating robust RWE requires a suite of methodological "reagents" and tools. The following table details key solutions essential for mitigating bias and confounding, framed as a toolkit for the RWE scientist.
Table 3: Essential Research Reagents for Mitigating Bias and Confounding
| Tool / Solution | Function / Purpose | Application in RWE Studies |
|---|---|---|
| Structured Treatment Patterns Algorithm | To operationalize the definition of treatment exposure (start, stop, switch) from messy, longitudinal RWD (e.g., claims, EHR). | Creates a clean analytic dataset for emulating treatment strategies in a target trial or defining cohorts for propensity score analysis [69] [56]. |
| Clinical Code Mapping System | To accurately identify patient populations, comorbidities, and outcomes using standardized code systems (e.g., ICD-10, CPT, NDC). | Ensures the valid construction of inclusion/exclusion criteria, confounders, and study endpoints from administrative data [71] [69]. |
| Propensity Score Engine | To estimate and apply propensity scores for matching, weighting, or stratification. Includes algorithms for balance assessment. | The core engine for controlling measured confounding and creating comparable treatment groups in observational analyses [71]. |
| Doubly Robust Estimator Library | A collection of implemented statistical methods (e.g., TMLE, AIPW) that provide robustness against model misspecification. | Used in the final outcome analysis to provide a more reliable estimate of the treatment effect than single-model approaches [71] [57]. |
| Quantitative Bias Analysis Framework | A set of methods (e.g., E-value calculation, probabilistic sensitivity analysis) to quantify the potential impact of unmeasured confounding. | Critical for HTA submissions to transparently acknowledge limitations and assess the robustness of study conclusions [71] [56]. |
| High-Fidelity RWD Source | A curated, linkable, and quality-controlled database (e.g., linked EHR-genomic data, national registry) with complete capture of patient journeys. | Provides the foundational, high-quality data necessary to minimize measurement error, missing data, and selection bias from the outset [67]. |
The strategic application of these methods and tools is paramount for HTA acceptance. As noted in the search results, HTA bodies welcome RWE that transparently addresses data quality and potential biases through robust methodological approaches [26] [67]. The diagram below outlines the strategic process of transitioning from RCT evidence to validated RWE, highlighting the role of advanced methodologies.
For researchers and drug development professionals, the acceptance of Real-World Evidence (RWE) in regulatory and Health Technology Assessment (HTA) submissions hinges on demonstrably robust data governance. While regulatory and HTA agencies globally recognize the potential of RWE to transform evidence generation, they consistently express skepticism about data quality and validity, creating a significant "trust deficit" that rigorous data governance practices must overcome [72] [73]. The landscape of guidance has evolved from minimal to crowded, with numerous frameworks from agencies like the US FDA, EMA, and NICE creating a complex maze for evidence generation [73]. This guide compares international standards and provides a structured checklist to help researchers navigate the critical data governance requirements for RWD acceptability, ensuring that generated evidence meets the stringent expectations of global decision-making bodies.
The core challenge lies in the transition from Real-World Data (RWD)—the raw data collected from routine healthcare—to regulatory-grade RWE. As international agencies increase their collaboration and develop more sophisticated data networks like EMA's DARWIN EU, the emphasis on transparent, well-governed data processes has become paramount for successful submissions [73]. A strong preference among decision-making bodies for local real-world data generation further complicates global evidence strategies, making adherence to internationally recognized governance standards not just best practice, but a necessity [73].
Comparative Analysis of International RWD Guidance Frameworks
Major regulatory and HTA agencies have developed distinct but overlapping frameworks to guide the acceptable use of RWD in decision-making. The table below summarizes the core approaches of key international bodies.
Table 1: International Framework Comparison for RWD Acceptability
| Agency/Organization | Primary Guidance Document | Scope & Focus | Key Data Governance Emphases |
|---|---|---|---|
| U.S. FDA | Multiple RWE Guidances (Framework, Guidance, Considerations) | Regulatory decisions, including effectiveness and safety [73] | Data reliability and relevance, fit-for-purpose data, transparency in reporting [73] |
| European Medicines Agency (EMA) | Reflection Paper on RWD in Non-Interventional Studies (NIS) [74] | Methodological standards for NIS to generate RWE for regulatory purposes [74] | Data quality, suitability of RWD sources, mitigating bias in non-interventional designs [74] |
| UK's NICE | Real-World Evidence Framework (2022) [75] | Health technology assessment, value-based pricing, and reimbursement [76] [75] | Data provenance, quality, and relevance for cost-effectiveness and addressing decision modifiers [76] |
| China's CDE | Based Disease Registry Guidance (2024) [77] | Application of disease registry data to support drug development and regulatory decisions [77] | Prospective design, data standardization, quality control, and longitudinal data completeness [77] |
| International Societies (ISPOR, ISPE) | Task forces, best practices, toolkits, and checklists [73] | Standardizing RWE methods and data quality issues across the research community [73] | Study design transparency, methodological rigor, and promoting replicability [73] |
A 2024 environmental scan identified 46 RWE guidance documents across various agencies, revealing that while all address fundamental methodological issues, inconsistencies in terminology and specific preferences create challenges for global submissions [73]. The US FDA has been the most prolific in issuing RWE-related guidance, whereas some HTA bodies like the UK's National Institute for Health and Care Excellence (NICE) and Canada's Drug Agency have opted to centralize their guidance under a single, unified framework to improve clarity [73]. This disparity underscores the need for sponsors to carefully navigate the specific requirements of each target agency.
Commonalities and Divergences in Agency Expectations
Despite the variability in guidance documents, a consensus is emerging on several core pillars of RWD acceptability. All agencies emphasize:
- Fit-for-Purpose Data: The selected data source must be appropriate for the research question [73].
- Study Planning and Design Rigor: A well-defined protocol with a priori hypotheses is increasingly mandated to combat "data dredging" [72] [73].
- Transparency and Complete Reporting: Detailed documentation of data provenance, handling, and analytical choices is essential for auditability and assessment of potential biases [78] [73].
However, key divergences remain, particularly in the acceptance of specific data sources and methodological approaches. For instance, agencies like EMA, NICE, and Haute Autorité de Santé (HAS) include specific recommendations on analytical approaches to address RWE complexities, reflecting their unique perspectives on evidence validity [73]. Furthermore, a strong preference for local data generation can hinder the use of international federated data networks, requiring sponsors to plan for region-specific data strategies [73].
The Data Governance Checklist: A Pathway to Regulatory Acceptance
The following checklist synthesizes international standards into a actionable pathway for researchers. Adherence to this governance protocol significantly increases the likelihood of RWE acceptance by major agencies.
Table 2: The Data Governance Checklist for RWD Acceptability
| Phase | Checklist Item | Key Actions & International Standards | Considerations for HTA/Regulatory Submissions |
|---|---|---|---|
| Study Planning & Protocol | 1. Define a priori hypothesis and analysis plan | - Publicly register study (e.g., on platforms like clinicaltrials.gov) to enhance transparency [72].- Pre-specify statistical analysis plan to avoid "data dredging" or selective reporting [72]. | NICE's framework emphasizes the need for a clear research question aligned with the decision problem [75]. |
| 2. Justify data source selection | - Demonstrate the "fit-for-purpose" of the chosen RWD source for the research question [73].- For disease registries, ensure prospective design with standardized data collection [77]. | FDA and EMA require detailed rationale for why the chosen data source is adequate to address the study objectives [73]. | |
| Data Quality & Management | 3. Ensure data relevance and reliability | - Map data elements to a common data model (e.g., OMOP CDM) to standardize structure and content [78].- Document data provenance and lineage thoroughly. | Transcelerate's initiative highlights the need to prepare for audits by establishing relevance and reliability in a way that is meaningful to regulators [78]. |
| 4. Implement rigorous quality control (QC) | - Apply QC measures at point of data entry (e.g., in disease registries) and throughout the data processing pipeline [77].- Measure and report data completeness, accuracy, and consistency. | CDE's guidance on disease registries stresses the importance of persistent quality control to avoid bias and ensure data is fit-for-use [77]. | |
| Study Conduct & Analysis | 5. Address bias and confounding | - Use pre-specified methods (e.g., propensity score matching, stratification) to adjust for known confounders [72].- Acknowledge and discuss potential for unmeasured confounding and other biases. | EMA's reflection paper discusses methodological aspects for mitigating bias in non-interventional studies [74]. |
| 6. Ensure analytical robustness and reproducibility | - Perform sensitivity analyses to test the robustness of findings under different assumptions or methods.- Prepare to share analysis code to facilitate replication of results. | International societies like ISPOR and ISPE promote checklists to standardize analysis and reporting for reproducibility [73]. | |
| Reporting & Transparency | 7. Document and report with full transparency | - Adhere to recognized reporting guidelines (e.g., RECORD, STROBE).- Disclose all study limitations, data quality issues, and potential sources of bias openly. | A key expectation across all agencies is transparent reporting to establish trust in the RWE [72] [73]. |
| 8. Prepare for audit | - Maintain a comprehensive audit trail documenting all data transformations and analytical decisions [78].- Ensure all processes are documented for regulatory inspection. | The "Transcelerate RWD Audit Readiness" initiative is designed to help sponsors prepare for regulatory audits of their RWD sources and processes [78]. |
Visualizing the RWD Governance Pathway for Regulatory Acceptance
The following diagram maps the logical sequence and iterative nature of transforming raw data into trusted evidence, integrating the key checks and balances required by international standards.
Essential Research Reagents: Tools for RWE Governance
Beyond conceptual frameworks, researchers require practical tools and methodologies to implement robust data governance. The following table details key "research reagents" – including protocols, standards, and software solutions – that are essential for generating compliant RWE.
Table 3: Essential Research Reagents for RWE Governance
| Tool Category | Specific Tool/Standard | Function in RWE Generation | Application in Regulatory/HTA Context |
|---|---|---|---|
| Data Standardization Tools | OMOP Common Data Model (CDM) | Standardizes the structure and content of heterogeneous RWD sources (e.g., EMR, claims) to a consistent format, enabling large-scale analytics and cross-institutional collaboration. | Facilitates the use of federated data networks, though agencies may still prefer local data instantiation [73]. |
| Study Registration Platforms | ClinicalTrials.gov, EU PAS Register | Provides a public, pre-study record of the research hypothesis, design, and analysis plan, enhancing transparency and reducing risks of publication bias [72]. | Increasingly expected by agencies to confirm that analyses were pre-specified and not the result of "data dredging" [72]. |
| Methodological Toolkits | ISPOR/ISPE Task Force Recommendations, Duke-Margolis Checklists | Provides best-practice guidance on complex methodological issues such as design selection, bias adjustment, and confounding control [73]. | Helps align study conduct with evolving agency expectations on methodology, as seen in EMA and NICE guidance [73] [74]. |
| Quality Assessment Frameworks | Transcelerate RWD Audit Readiness Framework [78] | A structured approach to prepare RWD sources and processes for regulatory audit, focusing on establishing relevance and reliability [78]. | Directly addresses the need to demonstrate data trustworthiness to regulatory auditors in a formal inspection setting [78]. |
| Reporting Guidelines | RECORD (Reporting of studies Conducted using Observational Routinely-collected Data) | An extension of the STROBE guidelines, providing a checklist of items that should be reported in studies using RWD to ensure complete and transparent communication. | Adherence to such guidelines is a minimal requirement for manuscript publication and is viewed favorably by HTA bodies assessing evidence quality. |
Experimental Protocol: Validating a Disease Registry for Use as an External Control
A prominent application of RWD is serving as an external control in single-arm trials, particularly in oncology and rare diseases. The following detailed protocol, based on China's CDE guidance, outlines the methodology for validating a disease registry for this purpose [77].
Objective: To establish the fitness-for-purpose of a specific disease registry database to serve as an external control arm for a single-arm trial of a novel therapy for a rare disease.
Methodology:
Registry Design Assessment:
- Confirm the registry was designed and implemented with a prospective data collection plan, following a predefined protocol [77].
- Evaluate the scientific rationale for the collected data points, ensuring they align with key outcomes and potential confounders relevant to the disease and therapy under investigation.
Population Representativeness Analysis:
- Compare the baseline characteristics (e.g., demographics, disease severity, prior treatment history, comorbidities) of the registry population to the target population of the single-arm trial.
- Apply the same inclusion and exclusion criteria of the trial to the registry data to create a synthetic control cohort. Assess the proportion of the registry population that qualifies and report reasons for exclusion.
Data Quality and Completeness Audit:
- Perform a quantitative data quality check on the synthetic control cohort. Key metrics include:
- Completeness: Calculate the percentage of missing data for critical variables (e.g., primary outcome, key prognostic factors). A predefined threshold (e.g., >95% completeness for core variables) should be met.
- Plausibility: Check data for logical inconsistencies (e.g., dates of death before diagnosis, implausible values for lab tests).
- Longitudinality: Verify that follow-up data is available for a sufficient duration for the required endpoints, with documented follow-up schedules and intervals [77].
- Perform a quantitative data quality check on the synthetic control cohort. Key metrics include:
Outcome Validation and Comparator Benchmarking:
- If feasible, validate the registry's outcome measures. For instance, compare the overall survival recorded in the registry against a trusted national cancer registry for a subset of patients.
- Benchmark the outcomes (e.g., progression-free survival, response rates) of the synthetic control cohort against outcomes from historical clinical trials in the same patient population, if available, to assess face validity.
Expected Outputs and Success Criteria: The validation is deemed successful if the registry demonstrates: 1) a prospective design with low risk of bias; 2) a synthetic control cohort with baseline characteristics closely aligned to the expected trial population; 3) data completeness and quality metrics meeting pre-specified targets; and 4) outcome data that is consistent with established historical benchmarks. This protocol provides a replicable experimental framework for establishing the reliability of a key RWD source.
Navigating the complex landscape of international standards for RWD acceptability requires a meticulous, proactive approach to data governance. The convergence of agency expectations around transparency, methodological rigor, and data quality provides a clear roadmap for researchers [73]. By adopting the integrated checklist, utilizing essential research reagents, and implementing rigorous validation protocols, drug development professionals can systematically build trust in their RWE. This structured approach is critical for bridging the current "trust deficit" and successfully integrating real-world evidence into the core of regulatory and HTA decision-making, ultimately supporting the development and access of valuable new therapies for patients. The future points towards closer inter-agency collaboration, and researchers who embed these governance standards now will be best positioned for the evolving evidentiary requirements.
Real-world evidence (RWE) is increasingly critical for regulatory decisions and health technology assessments (HTA), yet its value depends entirely on how well study populations represent intended target groups [14]. Unlike randomized controlled trials (RCTs) with strict inclusion criteria, RWE studies derive from heterogeneous data collected during routine clinical practice, creating significant challenges for generalizability [79] [80]. Representativeness—the extent to which a study population reflects the broader target population—is threatened by selection biases, heterogeneous data quality, and methodological inconsistencies that limit evidence transportability across healthcare systems [14] [81].
The growing prominence of RWE in regulatory and HTA decision-making intensifies the consequences of unrepresentative data. Analyses of European HTA submissions reveal troubling inconsistencies in RWE acceptability, largely driven by concerns about population comparability and methodological biases [81]. Similarly, regulatory bodies emphasize that data must be "fit-for-purpose"—relevant and suitable for the specific research question and target population [82]. This guide examines methodological frameworks and practical approaches to ensure RWE populations adequately represent target groups, enabling more reliable evidence for healthcare decision-making.
Foundational Concepts: Defining Representativeness in Real-World Data
Key Terminology and Principles
Real-world data (RWD) encompasses health information collected from routine clinical practice, including electronic health records (EHRs), claims data, patient registries, and data from wearable devices [80] [83]. Real-world evidence (RWE) is the clinical evidence derived from analyzing RWD [80]. A fundamental distinction exists between routinely collected RWD (gathered during healthcare delivery) and prospectively collected RWD (specifically assembled for research purposes in non-experimental settings) [14].
Representativeness in RWE refers to the degree to which a study sample reflects the target population across key characteristics—demographics, clinical profiles, treatment patterns, and socioeconomic factors [14]. This differs from transportability, which involves applying results from one population to another by adjusting for relevant differences [14]. The target trial framework—conceptualizing a hypothetical randomized trial that the RWE study emulates—provides crucial methodological rigor for ensuring representativeness and valid causal inference [79] [83].
Table 1: Common Real-World Data Sources and Representativeness Considerations
| Data Source | Key Characteristics | Representativeness Strengths | Representativeness Limitations |
|---|---|---|---|
| Electronic Health Records (EHRs) | Clinical data from routine patient care | Rich clinical detail, diverse patient populations | Fragmented records, limited data standardization across systems |
| Insurance Claims Databases | Billing and reimbursement records | Large populations, complete capture of billed services | Limited clinical detail, coding inaccuracies, excludes uninsured |
| Patient Registries | Disease-specific longitudinal data | Detailed information on specific conditions | Potential selection bias toward severe cases or specialized centers |
| Digital Health Technologies | Wearables, patient-reported outcomes | Continuous monitoring, patient perspectives | Digital divide excludes non-users, variability in device accuracy |
Methodological Frameworks for Enhancing Representativeness
The Target Trial Emulation Framework
The target trial framework provides structured methodology for designing RWE studies that minimize bias and enhance representativeness [79] [83]. By explicitly specifying the protocol of a hypothetical randomized trial that would answer the research question, researchers can design their RWE study to emulate this ideal, clarifying eligibility criteria, treatment strategies, outcomes, and causal contrasts of interest [79]. This approach exposes tensions between generalizability goals and the restrictions needed for valid causal inference, forcing deliberate consideration of how to balance these competing demands [83].
Implementing this framework begins with defining time zero (analogous to randomization in an RCT)—the point at which patients become eligible for inclusion [79]. Using new-user designs (selecting patients at treatment initiation) rather than prevalent-user designs (including patients already on treatment) reduces selection biases that threaten representativeness [79] [83]. The framework also clarifies appropriate follow-up periods, outcome measurement, and analytic approaches that align with the causal question, whether intention-to-treat or on-treatment effects [79].
PICOT Alignment Assessment
The PICOT framework (Population, Intervention, Comparator, Outcome, Timing) provides systematic methodology for evaluating how well an RWE study's research question aligns with the decision problem at hand [79]. Breaking down the research question into these components enables direct comparison between the study parameters and the target population of interest.
Table 2: PICOT Framework for Assessing RWE Representativeness
| PICOT Element | Assessment Questions | Common Misalignments |
|---|---|---|
| Population | How similar are inclusion/exclusion criteria to target population? | Narrow age ranges, excluding comorbidities, different disease severity |
| Intervention | Does drug formulation, dosage, administration match real-world use? | Different formulations, stricter adherence requirements |
| Comparator | Is the comparison group relevant to clinical decision? | Inappropriate active comparator, non-standard care |
| Outcome | Are endpoints clinically meaningful and measurable in practice? | Surrogate endpoints, different measurement frequency |
| Timing | Does follow-up duration reflect actual treatment experience? | Fixed follow-up regardless of treatment discontinuation |
As illustrated in Table 2, a study potentially relevant for a policy decision might misalign across multiple PICOT components—focusing on patients aged 40-65 when the policy affects those 65+, comparing drug X to Z rather than the relevant comparator Y, and using fixed follow-up regardless of treatment discontinuation [79]. Such misalignments substantially limit a study's relevance for specific decisions, regardless of its internal validity.
Experimental Protocols for Validating Representativeness
Protocol 1: Transportability Analysis for Cross-Population Generalization
Purpose: To quantitatively assess whether results from a source population can be generalized to a target population, adjusting for relevant differences [14].
Methodology:
- Define source and target populations: Clearly specify the RWE study population (source) and the clinical or policy population of interest (target)
- Identify effect modifiers: Determine variables that may modify treatment effects between populations (e.g., age, disease severity, comorbidities)
- Measure population differences: Quantify differences in effect modifiers between source and target populations
- Apply transportability methods: Use statistical techniques (e.g., weighting, g-computation) to adjust for differences in effect modifiers
- Validate transportability: Compare adjusted estimates to observed outcomes when possible
Key Applications:
- Generalizing US RWE findings to European or Asian populations [67]
- Applying clinical trial eligibility criteria to broader real-world populations [14]
- Adjusting for differences in demographic or clinical characteristics
Protocol 2: Quantitative Bias Analysis for Unmeasured Confounding
Purpose: To quantify how unmeasured confounding might affect effect estimates and assess robustness of conclusions [79].
Methodology:
- Identify potential unmeasured confounders: Determine variables not available in dataset that may affect both treatment and outcome
- Specify bias parameters: Estimate strength of relationship between unmeasured confounder and treatment/outcome based on external data or plausible ranges
- Calculate bias-adjusted estimates: Apply quantitative methods (e.g., sensitivity analysis, bias analysis algorithms) to adjust effect estimates
- Interpret results: Determine whether conclusions change under plausible bias scenarios
Implementation Considerations:
- Use historical data on known confounders to inform bias parameters
- Consider multiple scenarios representing different magnitudes of confounding
- Report range of possible effect estimates rather than single point estimates when substantial residual confounding is plausible
Analytical Tools and Research Reagent Solutions
Table 3: Essential Methodological Tools for Assessing RWE Representativeness
| Tool Category | Specific Methods | Function in Representativeness Assessment |
|---|---|---|
| Study Design Visualization | Temporal design diagrams [83] | Illustrate timing of study elements relative to cohort entry date |
| Bias Mitigation | Propensity score matching [14], New-user designs [83] | Balance measured confounders, avoid prevalent user biases |
| Transportability Methods | Weighting, G-computation [14] | Adjust for differences between study and target populations |
| Sensitivity Analysis | Quantitative bias analysis, E-value calculation | Quantify impact of unmeasured confounding on results |
| Data Quality Assessment | Fit-for-purpose evaluation frameworks [82] | Evaluate data relevance, completeness, and accuracy for research question |
Regulatory and HTA Perspectives on Representativeness
Evolving Regulatory Standards
Regulatory bodies increasingly provide guidance on RWE standards, emphasizing data quality and relevance for decision-making. The FDA's framework highlights reliability of RWD—requiring accuracy, completeness, and traceability—and robustness of study designs with detailed protocols that include causal diagrams and bias mitigation strategies [82]. The fit-for-purpose principle underscores that data must be appropriate for the specific research question and target population [82].
Early engagement with regulatory agencies is strongly recommended to align on study designs, data sources, and analytical approaches before study initiation [84] [82]. Regulatory case studies demonstrate successful RWE integration when representativeness concerns are adequately addressed. For example, Amgen's application for Lumakras (sotorasib) used multiple real-world data sources to characterize patient populations, addressing evidence gaps through comprehensive data integration [84].
HTA Acceptance Across Jurisdictions
HTA bodies demonstrate varying acceptance of RWE, with representativeness concerns significantly influencing decisions. A review of European HTA submissions found RWE was "mostly rejected due to methodological biases" related to population comparability [81]. Similarly, a global review of HTA guidelines revealed only four of eight countries had published RWE guidance, though most expressed desire for more structured RWE use in assessments [85].
HTA bodies particularly value RWE for addressing evidence gaps when RCTs are infeasible or unethical—such as rare diseases, progressive conditions with predictable outcomes, or situations with high unmet need [84] [67]. Successful submissions typically demonstrate:
- Transparency in data sources and methodological limitations [67]
- Relevance of study population to HTA jurisdiction [67]
- Robustness through sensitivity analyses addressing potential biases [81]
- Substantial evidence complementing other data sources rather than standing alone [84]
Ensuring RWE represents target populations requires methodological rigor throughout study design, implementation, and interpretation. The target trial framework provides essential structure for minimizing biases, while PICOT alignment assessment systematically evaluates relevance to specific decisions. Successful applications demonstrate that transparent reporting, appropriate bias mitigation methods, and validation against known relationships substantially enhance RWE credibility.
As RWE continues evolving, methodological advances in transportability methods and quantitative bias analysis will further improve ability to generate representative evidence. However, these technical approaches must complement—not replace—transparent engagement with regulatory and HTA bodies regarding study limitations. The increasing standardization of data formats and growth of linked data resources promise enhanced opportunities for generating RWE that reliably informs decisions for diverse target populations. Through continued methodological innovation and stakeholder collaboration, RWE can fulfill its potential to provide valid, generalizable evidence across the healthcare spectrum.
For researchers, scientists, and drug development professionals, assessing the robustness of real-world evidence (RWE) findings is paramount for informing regulatory and health technology assessment (HTA) decisions. Unlike randomized controlled trials (RCTs), observational RWE studies are particularly susceptible to biases, especially from uncontrolled confounding due to unmeasured variables [86]. A systematic review of active-comparator cohort studies published in high-impact medical and epidemiologic journals revealed that while 93% of studies acknowledged residual confounding as a potential concern, only about 53% implemented any sensitivity analysis to assess this bias [86]. This gap in rigorous validation underscores the critical need for comprehensive sensitivity and bias analysis frameworks to strengthen the credibility of RWE used in HTA research.
Sensitivity analyses provide a structured methodology to quantify how much the estimated treatment effect would need to change to alter the study's conclusions. These techniques enable researchers to test the robustness of their findings against potential unmeasured confounders, selection biases, and other systematic errors [87]. With regulatory agencies and HTA bodies increasingly considering RWE for decision-making – including the FDA's guidance on RWE use and the European Union's upcoming Joint Clinical Assessment – establishing methodological rigor through systematic bias assessment has never been more critical [26] [81].
Key Methodological Approaches for Sensitivity Analysis
Quantitative Techniques for Unmeasured Confounding
E-Value Analysis The E-value is a quantitative metric that measures the minimum strength of association an unmeasured confounder would need to have with both the treatment and outcome to explain away an observed treatment effect [86]. This approach has gained significant traction, particularly in medical literature, for its intuitive interpretation and computational simplicity. The E-value is calculated based on the observed risk ratio and its confidence interval limit, providing a concrete measure of how robust the findings are to potential unmeasured confounding.
Propensity Score-Based Methods While propensity score matching and weighting are primarily used to address measured confounding, advanced applications can incorporate sensitivity parameters to assess potential unmeasured bias. These methods evaluate how the distribution of unmeasured confounders might differ between treatment groups and how this could impact effect estimates [88].
Quantitative Bias Analysis This comprehensive framework systematically quantifies the potential impact of multiple bias sources, including unmeasured confounding, selection bias, and misclassification [86]. It involves specifying bias parameters based on external knowledge or plausible ranges, then recalculating effect estimates after adjusting for these biases.
Table 1: Comparative Analysis of Quantitative Sensitivity Methods
| Method | Primary Application | Key Advantages | Implementation Complexity |
|---|---|---|---|
| E-Value | Unmeasured confounding | Intuitive interpretation; easy computation | Low |
| Propensity Score with Sensitivity | Measured and unmeasured confounding | Integrates with standard approaches | Medium |
| Quantitative Bias Analysis | Multiple bias sources | Comprehensive assessment of various biases | High |
| Instrumental Variable | Unmeasured confounding | Can provide unbiased estimates if valid instrument available | High |
Handling Treatment Crossovers and Time-Varying Confounding
In real-world settings, patients frequently switch, discontinue, or combine treatments – a phenomenon known as treatment crossover. These deviations from initial treatment paths introduce significant analytical challenges, including biased treatment effect estimates and confounding [89]. Several advanced statistical methods have been developed to address these issues:
Marginal Structural Models (MSMs) MSMs incorporate inverse probability weighting to adjust for time-varying confounders – factors that change over time and affect both subsequent treatment and outcomes. These models are particularly valuable in chronic disease studies where treatment modifications are common based on disease progression or response [89].
Inverse Probability Weighting (IPW) IPW assigns weights to patients based on their probability of following a particular treatment trajectory. This approach creates a pseudo-population in which the treatment assignment is independent of measured confounders, allowing for less biased effect estimation [89].
Instrumental Variable Analysis (IVA) IVA utilizes external variables that influence treatment choice but do not directly affect outcomes (except through treatment) to estimate causal effects. Valid instruments might include regional variations in prescribing patterns, hospital policy differences, or physician preferences [89].
Experimental Protocols for Bias Assessment
Protocol for E-Value Sensitivity Analysis
Objective: To quantify the robustness of study findings to potential unmeasured confounding.
Materials and Data Requirements:
- Final adjusted effect estimate (hazard ratio, risk ratio, or odds ratio) from primary analysis
- Confidence interval for the effect estimate
- Statistical software with E-value calculation capabilities (e.g., R
EValuepackage, SAS macros)
Procedure:
- Calculate E-value for effect estimate: Compute the minimum strength of association that an unmeasured confounder would need to have with both the treatment and outcome to explain away the observed effect estimate.
- Calculate E-value for confidence interval: Determine the E-value for the confidence limit closest to the null value.
- Interpret results: If the E-value is large relative to known confounders in the field, the result is considered more robust to potential unmeasured confounding.
- Contextualize findings: Compare the E-value to the strength of associations observed for known measured confounders in the current study or literature.
Reporting Standards:
- Report both E-values (for point estimate and confidence interval)
- Discuss plausible unmeasured confounders in the clinical context
- Compare E-values to measured confounder associations in the study
Protocol for Treatment Crossover Adjustment Using MSMs
Objective: To obtain unbiased treatment effect estimates when patients switch treatments during follow-up.
Materials and Data Requirements:
- Longitudinal patient-level data with treatment history
- Measurements of time-varying confounders at regular intervals
- Outcome data aligned with treatment changes
- Statistical software capable of handling MSMs (e.g., R
ipwpackage, SAS PROC GENMOD)
Procedure:
- Model treatment probabilities: Estimate the probability of treatment at each time point given covariate history using appropriate models (e.g., logistic regression).
- Calculate stabilized weights: Compute inverse probability of treatment weights for each patient-time observation, with stabilization to minimize variability.
- Assess weight distribution: Examine the distribution of weights to identify extreme values that might unduly influence results.
- Fit outcome model: Apply the weights to a marginal structural model (typically a weighted regression) to estimate the treatment effect on the outcome.
- Validate model assumptions: Check for positivity, correct model specification, and no unmeasured confounding.
Analytical Considerations:
- Account for censoring using inverse probability of censoring weights if informative censoring is present
- Use robust variance estimators to account for weighting
- Conduct sensitivity analyses with different model specifications
Diagram 1: MSM Analysis Workflow for Treatment Crossover
Protocol for Comprehensive Sensitivity Analysis Framework
Objective: To systematically evaluate the impact of multiple potential biases on RWE findings.
Materials and Data Requirements:
- Primary analysis dataset
- List of potential bias sources with plausible parameter ranges
- Sensitivity analysis software (e.g., R
sensemakr, SAS macros) - Literature on bias parameter estimates for similar study designs
Procedure:
- Identify bias sources: Catalog potential sources of bias (unmeasured confounding, selection bias, misclassification, etc.) specific to the study context.
- Define bias parameters: Specify parameters that quantify the strength and direction of each bias (e.g., prevalence differences of unmeasured confounders, selection probabilities).
- Specify parameter ranges: Define plausible ranges for each bias parameter based on literature, clinical knowledge, or external data.
- Implement bias adjustments: Recalculate effect estimates after adjusting for biases using specified parameters.
- Conduct probabilistic analysis: Vary multiple parameters simultaneously using Monte Carlo simulation to assess combined bias impact.
- Interpret results: Determine under what conditions the study conclusions would change and assess the plausibility of those conditions.
Reporting Standards:
- Clearly document all assumptions and parameter values
- Present bias-adjusted effect estimates across plausible parameter ranges
- Discuss the plausibility of scenarios that would substantially change conclusions
The Researcher's Toolkit: Essential Reagents for RWE Robustness Assessment
Table 2: Essential Methodological Tools for Sensitivity and Bias Analysis
| Tool/Technique | Primary Function | Application Context | Implementation Considerations |
|---|---|---|---|
| E-Value Calculator | Quantifies unmeasured confounding strength needed to nullify effect | All RWE studies with point estimates | Easy to implement; requires R packages or online calculators |
| Propensity Score Models | Balances measured confounders between treatment groups | Comparative effectiveness research | Sensitivity to model specification; requires checking balance |
| Marginal Structural Models | Adjusts for time-varying confounding and treatment changes | Longitudinal studies with treatment changes | Complex implementation; requires correct weight specification |
| Instrumental Variable Methods | Addresses unmeasured confounding using natural experiments | When valid instruments are available | Challenging to find valid instruments; weak instrument problems |
| Quantitative Bias Analysis | Comprehensively assesses multiple bias sources | High-stakes decision contexts | Requires bias parameters from external sources |
| Machine Learning Algorithms | Predicts treatment switching or missing data patterns | Large datasets with complex relationships | Black-box nature; requires careful validation |
Case Studies in Regulatory and HTA Contexts
The implementation of sensitivity analyses has demonstrated critical importance in regulatory and HTA decision-making. A comparative case study analysis of European regulatory and HTA decisions for oncology medicines revealed that RWE was primarily used as external controls or for contextualizing clinical trial results [81]. However, these applications were frequently rejected due to methodological concerns, highlighting the importance of robust sensitivity analyses.
In one notable example, a study comparing two sarcoma multidisciplinary teams utilized an interoperable digital platform (Sarconnector) for real-world time data assessment, establishing a framework for standardized quality and outcome benchmarking [90]. This approach enabled identification of variations in clinical processes and outcomes, demonstrating how structured data collection and analysis can enhance RWE reliability.
The diverging acceptance of RWE across the European Medicines Agency and various HTA bodies (NICE, G-BA, HAS) further underscores the need for standardized sensitivity analysis approaches [81]. Studies that incorporated comprehensive sensitivity analyses were more likely to be accepted across multiple agencies, particularly when these analyses transparently addressed potential biases and confounding.
Sensitivity and bias analysis represents an indispensable component of RWE generation for HTA research. As regulatory and reimbursement bodies increasingly consider RWE in their decision-making frameworks, the implementation of rigorous sensitivity analyses will be crucial for establishing evidence credibility.
The current state of RWE validation reveals significant opportunities for methodological advancement. While techniques like E-value analysis and propensity score methods have gained traction, more sophisticated approaches addressing complex biases – such as marginal structural models for treatment crossovers and quantitative bias analysis for multiple simultaneous biases – remain underutilized [86] [89].
For researchers and drug development professionals, integrating comprehensive sensitivity analyses throughout the RWE generation process – from study design through analysis and interpretation – is essential for producing evidence fit for regulatory and HTA purposes. This approach not only strengthens study validity but also enhances transparency, allowing decision-makers to appropriately weigh the evidence in context.
As the RWE landscape evolves with advancing analytical techniques and growing data resources, sensitivity analysis methodologies must similarly advance. Future directions should include standardized reporting guidelines for sensitivity analyses, development of validated bias parameters for common clinical scenarios, and integration of machine learning approaches to identify and adjust for complex bias patterns. Through these advancements, RWE can fulfill its potential as a robust source of evidence for healthcare decision-making.
Benchmarking Success: A Comparative Review of RWE in Regulatory and HTA Decisions
Real-world evidence (RWE) has emerged as a transformative component in therapeutic product development and regulatory decision-making. Derived from real-world data (RWD) sourced from electronic health records, claims data, disease registries, and other routine healthcare settings, RWE offers insights into medical product performance under actual use conditions [2]. As regulatory agencies and health technology assessment (HTA) bodies face increasing pressure to accelerate patient access to innovative treatments, particularly in oncology and rare diseases, RWE presents a promising tool to complement traditional randomized controlled trials (RCTs) [81] [1].
This guide objectively compares the acceptance and application of RWE across major regulatory and HTA bodies, with a specific focus on the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and European HTA organizations. Despite general momentum toward integrating RWE, significant divergences persist in methodological standards, evidentiary requirements, and decision-making frameworks [81] [91]. Understanding these disparities is crucial for researchers, scientists, and drug development professionals navigating the increasingly complex landscape of evidence generation for regulatory approval and reimbursement.
Comparative Analysis of RWE Acceptance
Regulatory and HTA Approaches to RWE
The table below summarizes the key characteristics, strategic initiatives, and primary use cases of RWE within the FDA, EMA, and European HTA bodies.
Table 1: Comparative Analysis of RWE Acceptance Across Regulatory and HTA Bodies
| Agency/Body | Strategic Initiatives & Frameworks | Primary RWE Use Cases | Data Infrastructure |
|---|---|---|---|
| U.S. FDA | - Advancing RWE Program (PDUFA VII) [92]- RWE Framework (2018) [2]- Target Trial Emulation (TTE) endorsement [91] | - Supporting new indications for approved drugs [2] [61]- Post-market safety monitoring and study requirements [2] [92]- External controls for single-arm trials [91] | - Multiple funded demonstration projects [61]- Focus on fit-for-purpose data sources [92] |
| European Medicines Agency (EMA) | - DARWIN EU (Data Analysis and Real World Interrogation Network) [93]- Big Data Steering Group [94]- HMA-EMA catalogues of RWD sources and studies [93] | - Disease epidemiology and medicine utilization [93]- Post-authorization safety studies (PASS) [93]- Medicine effectiveness and impact of regulatory actions [93] | - DARWIN EU network: ~30 partners, ~180 million patient data from 16 countries [93]- Metadata list describing RWD [94] |
| European HTA Bodies | - FRAME methodology for RWE assessment [91] [24]- CanREValue Collaboration (Canada) [91]- EUnetHTA collaboration | - Indirect treatment comparisons and contextualization [81]- Addressing uncertainties in cost-effectiveness [1] [91]- Reassessment of drugs post-launch [91] | - Varied data access and capabilities across national systems [91]- Exploration of administrative data for RWE [91] |
Quantitative Comparison of RWE Utilization and Impact
The following table provides a data-driven perspective on how RWE is utilized and the impact it has on decision-making processes within these organizations.
Table 2: Quantitative Comparison of RWE Utilization and Impact
| Metric | FDA | EMA | European HTA Bodies |
|---|---|---|---|
| Volume of RWE Activities | Multiple grants and demonstration projects ongoing [61] | 59 studies completed or ongoing (Feb 2024-Feb 2025) [93] | 39% of HTA reports included RWE in 2021 (up from 6% in 2011) [1] |
| Role of RWE in Decisions (as primary evidence) | 20% of regulatory assessments (across 68 submissions) [91] | Used in regulatory-led studies for safety, effectiveness, epidemiology [93] | 9% of HTA body evaluations (across 68 submissions) [91] |
| Role of RWE in Decisions (as supportive evidence) | 46% of regulatory assessments [91] | Used for contextualization and supporting clinical trial results [81] | 57% of HTA body evaluations [91] |
| Key Determinant for Acceptance | Large treatment effect sizes and rigorous methods like TTE [91] | Data reliability and relevance, addressed via DARWIN EU and metadata guides [93] [94] | Large effect sizes; also considers health equity, administration [91] |
| Reported Challenges | Need for improved quality and acceptability of RWE approaches [92] | Inconsistent acceptability across the agency and HTA bodies [81] | Methodological biases in external controls; divergence in assessments [81] [91] |
Key Methodologies and Experimental Protocols
The FRAME Methodology for RWE Assessment
The Framework for Real-World Evidence Assessment to Mitigate Evidence Uncertainties for Efficacy/Effectiveness (FRAME) provides a systematic approach for evaluating the use and impact of RWE in regulatory and HTA submissions [91] [24].
Objective: To systematically analyze and characterize how regulatory and HTA agencies evaluate RWE in their decision-making processes. Data Collection: The methodology involves extracting information on 74 variables from publicly available assessment reports. These are grouped into:
- 43 variables describing submission characteristics and RWE type.
- 30 variables influencing RWE's role in decisions, covering clinical context, strength of evidence, and process factors [91]. Application: Researchers applied FRAME to analyze 15 medicinal products across 68 submissions to authorities in North America, Europe, and Australia between January 2017 and June 2024 [91]. Key Findings:
- Low Granularity: Public assessment reports often lack detailed commentary on the variables influencing decisions.
- Agency Variability: Different authorities assess the same RWE studies differently, with some alignment between EMA/FDA and between HTA bodies like HAS and G-BA.
- Effect Size Critical: RWE was most accepted as primary evidence when treatment effect sizes were large [91].
Target Trial Emulation (TTE)
The FDA has placed Target Trial Emulation at the center of its regulatory modernization strategy, signaling a transformative shift in how RWE shapes drug approval processes [91].
Objective: To provide a structured approach for designing observational studies that mirror the design principles of randomized trials, thereby minimizing biases inherent in traditional observational research [91]. Protocol:
- Define a Protocol: Specify all core components of a randomized trial, including eligibility criteria, treatment strategies, treatment assignment procedures, outcome measures, follow-up period, and causal contrasts of interest.
- Analyze Data: Implement the protocol using RWD, emulating the treatment assignment and follow-up processes that would have occurred in a randomized trial.
- Compare Analyses: Compare the emulated trial results with those of actual randomized trials when available to validate the approach. Regulatory Impact: The FDA has suggested that well-designed TTE studies may support a regulatory shift from requiring two pivotal clinical trials to accepting a single well-designed study, particularly for rare diseases where traditional trials are impractical [91].
The CanREValue Collaboration Framework
The Canadian Real-world Evidence for Value of Cancer Drugs (CanREValue) collaboration offers a structured, multi-phase framework for incorporating RWE into cancer drug reassessment decisions [91].
Objective: To develop a framework that facilitates the use of RWE by decision-makers for reassessment of cancer drugs and refinement of funding decisions and drug price negotiations. Four-Phase Approach:
- Phase I - Identification and Prioritization: Uses a multicriteria decision analysis rating tool with seven criteria to assess both the importance of the RWE question and the feasibility of conducting an RWE study.
- Phase II - Planning and Initiation: Develops a standardized implementation plan and study protocol collaboratively with all relevant stakeholders before undertaking the RWE study.
- Phase III - Execution: Focuses on robust data collection and analysis methods, coordinating data access across multiple sites, and sharing analysis plans and code between provinces.
- Phase IV - Reassessment: Formats RWE study results into reassessment submission templates for evaluation by HTA agencies for potential changes to funding recommendations [91].
Essential Research Reagent Solutions
The following table details key methodological frameworks, tools, and infrastructures that function as essential "reagents" for conducting rigorous RWE studies intended for regulatory and HTA submission.
Table 3: Key Research Reagent Solutions for Regulatory-Grade RWE
| Tool/Framework | Function | Application Context |
|---|---|---|
| Target Trial Emulation (TTE) | Provides a structured design framework for observational studies to minimize bias by emulating randomized trials [91]. | Ideal for generating comparative effectiveness evidence from RWD when randomized trials are not feasible. |
| FRAME Methodology | Systematic framework with 74 variables to assess how RWE is evaluated by agencies, identifying gaps and inconsistencies [91] [24]. | Used to analyze past submissions and plan future RWE strategies that align with agency expectations. |
| DARWIN EU | Centralized EU network that provides timely and reliable RWE from healthcare databases across member states [93]. | Provides regulatory-grade data for disease epidemiology, drug utilization, safety, and effectiveness studies. |
| HARPER Template | A reporting template for RWE studies that promotes transparency and completeness of reporting [91]. | Critical for protocol development and study reporting to meet evolving standards of regulators and HTA bodies. |
| HMA-EMA Catalogues | Online catalogues of real-world data sources and studies to help identify suitable data and promote transparency [93]. | Essential for researchers to identify fit-for-purpose data sources and assess the landscape of existing RWE. |
| CanREValue Framework | A structured four-phase approach for generating and using RWE in cancer drug reassessment [91]. | Provides a collaborative model for engaging with HTA bodies and payers on post-market evidence generation. |
Discussion
Analysis of Divergence and Alignment
The comparative analysis reveals a complex landscape of both divergence and alignment in RWE acceptance. A significant alignment exists in the recognition of RWE's potential value across all agencies. The FDA, EMA, and HTA bodies all acknowledge that high-quality RWE can play a crucial role in decision-making, particularly in contexts where RCTs are impractical or unethical [81] [2] [1]. There is also growing methodological alignment around rigorous approaches like Target Trial Emulation, which is increasingly endorsed by both regulators and HTA agencies [91].
However, substantial divergence remains. The most evident is the discrepancy in the acceptance of the same RWE studies across different agencies. The FRAME analysis found that while there was some alignment between the EMA and FDA, HTA bodies frequently diverged in their assessments from regulators and from each other [91]. A specific scoping review of oncology medicines found that RWE used as external controls was "mostly rejected due to methodological biases" by HTA bodies, creating a significant hurdle for drug developers [81]. Furthermore, HTA agencies have broader evidence considerations than regulators, incorporating factors such as health equity and mode of administration into their assessments, which influences their requirements for RWE [91].
Logical Workflow for Navigating RWE Requirements
The following diagram outlines a strategic workflow for researchers to navigate the complex requirements of generating RWE for multiple agencies, integrating tools like FRAME and TTE.
The journey toward fully aligned acceptance of RWE by the FDA, EMA, and HTA bodies remains a work in progress. While the visionary goals of the EMA for 2025 and the structured frameworks of the FDA's Advancing RWE Program demonstrate significant commitment, the practical reality is characterized by persistent divergence in evaluation standards and acceptability [81] [91] [94]. The upcoming implementation of the European Union Joint Clinical Assessment in 2025 presents a critical opportunity for HTA bodies and the EMA to develop more synergetic standards for RWE use [81].
For researchers and drug development professionals, success in this evolving landscape requires a proactive and strategic approach. This involves: early adoption of rigorous methodological frameworks like Target Trial Emulation; leveraging assessment tools like FRAME to anticipate agency concerns; engaging in early and structured dialogue with regulators and HTA bodies through available pathways; and maintaining a commitment to transparency and high-quality reporting. As these efforts converge, the potential for RWE to ensure more equitable and timely patient access to effective medicines will be substantially realized.
The integration of real-world evidence (RWE) into regulatory and health technology assessment (HTA) processes represents a significant shift in how oncology medicines are evaluated in Europe. RWE, defined as clinical evidence derived from analysis of real-world data (RWD) relating to patient health status and healthcare delivery, holds potential to complement traditional clinical trial data by providing insights into treatment effectiveness in routine clinical practice [2]. However, its acceptance across different decision-making bodies varies considerably, creating a complex landscape for drug developers and researchers.
The European Medicines Agency (EMA) and national HTA bodies have different mandates and evidence requirements, leading to challenges in evidence generation and submission strategies. With the implementation of the EU HTA Regulation in January 2025, which introduces Joint Clinical Assessments (JCAs) for oncology drugs and advanced therapy medicinal products, understanding these divergences becomes increasingly critical for ensuring timely patient access to innovative therapies [95] [96]. This case study analysis examines the current state of RWE acceptance across European regulatory and HTA bodies through recent oncology drug approvals, identifying both disparities and opportunities for alignment.
Methodology: Data Collection and Analytical Approach
This analysis employed a systematic approach to identify and examine recent oncology drug approvals and corresponding HTA appraisals across European institutions. Data collection focused on several key sources:
- Regulatory Approval Data: Publicly available approval documents from the European Medicines Agency (EMA) and individual national regulatory bodies for oncology medicines approved between 2024 and 2025.
- HTA Appraisal Documents: Final reports and assessments from major European HTA bodies, including the UK's National Institute for Health and Care Excellence (NICE), Germany's Gemeinsamer Bundesausschuss (G-BA), and France's Haute Autorité de Santé (HAS).
- RWE References: Identification of documents containing references to real-world evidence, RWD sources, or specific RWE study designs through targeted search terms including "real-world evidence," "observational data," "external controls," "indirect treatment comparisons," and "registry data" [81] [97].
Selection Criteria and Case Study Identification
Case studies were selected based on predefined criteria to enable comparative analysis:
- Oncology Focus: Included medicines with oncology indications approved by EMA between 2024-2025.
- Multi-Agency Assessment: Priority given to medicines assessed by at least two different HTA bodies to enable cross-comparison.
- RWE Utilization: Selection of cases where RWE was explicitly referenced in either regulatory or HTA assessment documents.
- Data Availability: Inclusion required publicly accessible assessment reports containing sufficient methodological detail on RWE use and critique.
Analytical Framework
A qualitative framework was developed to systemize data extraction across multiple dimensions:
- RWE Study Design: Classification of RWE approaches (external controls, contextualization, indirect comparisons).
- Data Sources: Documentation of RWD origins (registries, electronic health records, claims databases).
- Methodological Quality: Assessment of biases addressed (selection, confounding, channeling).
- Decision Impact: Evaluation of how RWE influenced final regulatory and HTA outcomes.
- Acceptance Rationale: Analysis of stated reasons for RWE acceptance or rejection across bodies.
Comparative Analysis of RWE Acceptance Across European Agencies
Regulatory and HTA Body Perspectives on RWE
European regulatory and HTA bodies have developed varying stances on RWE acceptance, reflecting their different institutional mandates and evidence standards.
Table 1: RWE Acceptance Profiles of Major European Regulatory and HTA Bodies
| Agency | Primary RWE Uses | Acceptance Level | Common Methodological Concerns | Notable Preferences |
|---|---|---|---|---|
| EMA | External controls, contextualization, post-authorization safety studies | Moderate to High | Residual confounding, selection bias | Specific analytical approaches to address RWE complexities [73] |
| NICE | Indirect treatment comparisons, economic model inputs | Moderate | Comparability of populations, unmeasured confounding | Unified framework for RWE assessment [73] |
| G-BA/IQWiG | Comparative effectiveness in routine care | Low to Moderate | Methodological rigor, relevance to German healthcare context | High methodological standards for non-randomized evidence [96] |
| HAS | Contextualization of trial results, natural history studies | Moderate | Data quality, representativeness of French population | Specific recommendations for analytical methods [73] |
Case Studies in Oncology Drug Appraisals
Analysis of recent oncology drug approvals reveals patterns in how RWE is utilized and assessed across the EMA and national HTA bodies.
Table 2: Comparative Case Studies of Oncology Drug Approvals and HTA Appraisals
| Drug (Brand) | Indication | EMA Approval Date | RWE Use in EMA Assessment | HTA Body | RWE Acceptance in HTA |
|---|---|---|---|---|---|
| Nirogacestat (Ogsiveo) | Progressing desmoid tumors | August 2025 [98] | Supported by phase 3 trial; RWE for context in rare disease | NICE | Under assessment; RWE likely for contextualization in rare population |
| Zanubrutinib (Brukinsa) | B-cell malignancies | August 2025 (tablet) [98] | Safety data from compiled EU prescribing information (n=1550) | G-BA | Previous assessments show skepticism toward indirect comparisons |
| Tislelizumab (Tevimbra) | Resectable NSCLC | August 2025 [98] | Phase 3 trial primary basis; RWE not prominently featured | HAS | Awaiting assessment; likely to require comparative RWE |
| UM171 cell therapy (Zemcelpro) | Hematologic malignancies | August 2025 [98] | Supported by prospective trials; RWE potential in post-authorization | Multiple | Conditional approval suggests post-authorization RWE collection |
Divergence in RWE Acceptability
The comparative assessment reveals significant discrepancies in RWE acceptability for the same oncology medicines across agencies [81] [97]. These divergences manifest in several key areas:
- Methodological Standards: Variable thresholds for accepting RWE study designs, particularly regarding control group comparability and confounding adjustment.
- Evidence Hierarchy: Differing positions on where RWE sits in the evidence hierarchy, with some agencies placing greater weight on randomized trial data.
- Data Source Preferences: Inconsistent acceptance of RWD sources across jurisdictions, with some bodies expressing strong preferences for local data generation [73].
- Contextualization vs. Substantial Evidence: Disagreement on whether RWE should primarily contextualize trial findings or serve as substantial evidence of effectiveness.
The Impact of EU HTA Regulation on RWE Standards
Joint Clinical Assessment Implementation
The implementation of the EU HTA Regulation in January 2025 establishes a new framework for evidence assessment across member states. JCAs will particularly affect oncology drugs and advanced therapy medicinal products, requiring manufacturers to navigate both regulatory and HTA evidence requirements simultaneously [95]. The JCA process involves:
- PICO Development: Definition of population, intervention, comparator, and outcomes through a collaborative scoping process involving multiple HTA bodies.
- Evidence Synthesis: Systematic compilation and comparative analysis of available clinical evidence against defined PICOs.
- Uncertainty Assessment: Evaluation of the certainty of evidence, including from RWE sources, using standardized methodologies.
Implications for RWE Generation
The JCA process creates both opportunities and challenges for RWE utilization:
- Harmonization Potential: Opportunity to establish more consistent standards for RWE acceptance across European markets.
- Evidence Planning Necessity: Requirement for early integrated evidence planning that anticipates both regulatory and HTA evidence needs.
- Increased Scrutiny: Heightened methodological expectations for RWE study design and analysis to meet multiple agency requirements simultaneously.
The compressed JCA timeline, with manufacturers having approximately 90 days to complete dossiers after PICO finalization, necessitates proactive RWE generation strategy and early engagement with HTA bodies through Joint Scientific Consultations [95].
Experimental Protocols for RWE Generation
Protocol for External Control Arm Studies
Objective: To generate comparative effectiveness evidence using external controls when randomized controls are infeasible or unethical.
Methodology:
- Data Source Selection: Identify fit-for-purpose RWD sources with complete capture of patient journeys, including electronic health records, disease registries, and claims databases.
- Cohort Definition: Apply eligibility criteria mirroring the clinical trial population to the RWD source, including diagnosis, prior therapies, and key clinical characteristics.
- Variable Mapping: Define and extract comparable baseline characteristics, outcome measures, and follow-up schedules.
- Confounding Control: Implement advanced statistical methods including propensity score matching, weighting, or stratification to balance measured covariates.
- Outcome Analysis: Compare outcomes between trial intervention group and external control using appropriate statistical models with sensitivity analyses to assess robustness.
Validation Requirements: Assessment of RWD source completeness, accuracy, and representativeness; evaluation of residual confounding through quantitative bias analysis.
Protocol for Indirect Treatment Comparisons
Objective: To compare interventions that have not been directly compared in head-to-head trials using RWE.
Methodology:
- Systematic Literature Review: Identify all relevant studies (RCTs and RWE studies) for each intervention of interest.
- Feasibility Assessment: Evaluate transitivity assumption (whether studies are sufficiently similar in key effect modifiers).
- Data Extraction: Collect aggregated or individual patient data on baseline characteristics and outcomes.
- Statistical Analysis: Conduct network meta-analysis or matching-adjusted indirect comparison using frequentist or Bayesian approaches.
- Uncertainty Quantification: Assess heterogeneity and inconsistency in the network; evaluate impact of methodological differences between studies.
Validation Requirements: Assessment of similarity and consistency assumptions; evaluation of cross-study differences in patient populations, definitions, and follow-up.
Visualization of European HTA and Regulatory Relationships
RWE Assessment Workflow Across European Agencies
The following diagram illustrates the complex pathway and decision points for RWE in European regulatory and HTA assessments:
RWE Acceptance Factors Across European Agencies
This diagram visualizes the key factors influencing RWE acceptance decisions across different European regulatory and HTA bodies:
Research Reagent Solutions for RWE Generation
The generation of high-quality RWE requires specialized methodological approaches and analytical tools. The following table outlines key solutions for addressing common challenges in RWE studies.
Table 3: Essential Research Reagent Solutions for RWE Generation
| Research Reagent | Function | Application Context | Key Considerations |
|---|---|---|---|
| Propensity Score Methods | Balance measured covariates between treatment groups | Comparative effectiveness studies with non-randomized treatment assignment | Requires complete capture of confounders; sensitivity analysis essential |
| Quantitative Bias Analysis | Quantify impact of unmeasured confounding | All observational studies with potential residual confounding | Multiple bias parameters may be needed; transparent reporting required |
| Federated Data Networks | Enable multi-database studies while maintaining data privacy | Studies requiring larger sample sizes or broader generalizability | Implementation of common data models and analytic packages |
| Natural Language Processing | Extract structured information from unstructured clinical notes | Augmenting structured data with clinical detail | Validation against manual chart review essential for accuracy |
| Target Trial Emulation | Apply randomized trial principles to observational study design | Causal inference from non-randomized data | Requires precise specification of trial protocol elements before analysis |
The case study analysis reveals ongoing discrepancies in RWE acceptance between EMA and European HTA bodies, with no clear consensus on optimal leveraging of RWE in oncology drug approvals [81] [97]. This misalignment creates challenges for drug developers seeking to generate evidence that satisfies both regulatory and reimbursement requirements efficiently.
The implementation of the EU HTA Regulation and Joint Clinical Assessments beginning in 2025 presents a critical opportunity to develop more synergetic standards for RWE use [95] [96]. Success will require:
- Methodological Alignment: Development of harmonized approaches to RWE study design, data quality assessment, and analytical methodology across agencies.
- Early Engagement: Strategic use of joint scientific consultations to align evidence requirements before study conduct.
- Transparent Reporting: Comprehensive documentation of RWE generation processes, including limitations and bias assessment.
- Iterative Learning: Continuous refinement of RWE standards based on accumulated experience with different study designs and data sources.
As novel methodologies for RWE generation continue to emerge, closer collaboration between regulatory and HTA bodies will be essential to establish clear, consistent expectations while maintaining rigorous evidence standards. This alignment is crucial for realizing the potential of RWE to improve patient access to innovative oncology therapies while ensuring appropriate assessment of their clinical and economic value.
Real-world evidence (RWE) is increasingly pivotal in health technology assessment (HTA), providing critical insights for decisions on comparative clinical effectiveness and cost-effectiveness. Derived from real-world data (RWD) gathered outside traditional randomized controlled trials (RCTs)—such as electronic health records, claims data, and patient registries—RWE offers a complementary perspective on how medical technologies perform in routine clinical practice [9] [99]. For HTA bodies, RWE helps address evidence gaps concerning long-term outcomes, treatment durability, and patient-centric benefits often not captured in RCTs [100]. However, the integration of RWE into HTA submissions presents distinct challenges, including potential confounding bias, missing data, and concerns about the reliability and relevance of data sources [101] [9]. This guide objectively examines the use of RWE from the HTA perspective, comparing its application across different contexts and outlining established methodologies to validate its suitability for informing reimbursement and policy decisions.
HTA Acceptance of RWE: A Comparative Landscape
The acceptance and appraisal of RWE by HTA bodies vary significantly across different jurisdictions, influenced by the intended use of the evidence and the robustness of the underlying data and methodologies.
Acceptance Criteria and Regional Variations
A key determinant of RWE acceptance is its intended use. HTA bodies apply a higher level of scrutiny when RWE is submitted to substantiate efficacy claims, such as through external control arms (ECAs) for single-arm trials, compared to its use in characterizing the natural history of a disease or the burden of illness [9]. Across European HTA bodies, the representativeness of the data source, overall transparency in the study, and use of robust methodologies are consistently cited as key criteria driving acceptance [9]. However, receptiveness to RWE is not uniform. Recent analyses indicate that among major European HTA bodies, the United Kingdom (NICE) and Spain (AEMPS) are more receptive to accepting RWE, whereas France (HAS) and Germany (G-BA) are less accepting [9].
Documented Uses of RWE in HTA Submissions
The application of RWE in successful HTA submissions is well-documented, particularly in contexts where RCTs are unfeasible, such as in rare diseases and oncology. The table below summarizes illustrative examples of technologies that successfully incorporated RWE into their regulatory and HTA evidence packages.
Table 1: Examples of RWE Use in HTA Submissions for Approved Technologies
| Therapy (INN) | Indication | Type of RWD Used | Purpose of RWE in Submission | Relevant HTA Body Appraisals |
|---|---|---|---|---|
| Avelumab | 1st/2nd-line Merkel Cell Carcinoma | Retrospective observational study data [9] | Construct an External Control Arm to compare outcomes against current clinical practice [9] | Supported efficacy claims in HTA assessment [9] |
| Blinatumomab | Acute Lymphoblastic Leukemia | Historical data from a retrospective study [9] | ECA to compare therapy with continued chemotherapy [9] | Supported efficacy claims in HTA assessment [9] |
| Tisagenlecleucel | Relapsed/Refractory Diffuse Large B-cell Lymphoma | Multiple data sources (e.g., SCHOLAR-1, ZUMA-1) [9] | ECA to compare therapy with historical standard of care [9] | Supported efficacy claims in HTA assessment [9] |
| Eculizumab | Paroxysmal Nocturnal Hemoglobinuria (subpopulation) | Registry data [9] | Demonstrate efficacy in a subpopulation not included in pivotal trials [9] | Supported label expansion in HTA assessment [9] |
A Framework for Assessing the Suitability of RWE
To ensure RWE is fit for purpose in HTA, a structured framework for assessing data quality and relevance is essential. The ISPOR SUITABILITY Checklist provides a standardized good practice framework for this assessment, focusing on two core components: Data Delineation and Data Fitness for Purpose [102].
The SUITABILITY Framework and Validation Workflow
The framework's components can be visualized as a sequential workflow for validating RWE, from data characterization to its final application in HTA.
Diagram 1: RWE Suitability Assessment Workflow
- Data Delineation: This initial phase establishes a complete understanding of the data and assesses its trustworthiness. It involves describing:
- Data Fitness for Purpose: This phase evaluates how well the data can answer the specific HTA question, comprising:
Experimental Protocols for RWE Generation
Generating robust RWE for HTA requires carefully designed observational studies. The protocols below detail established methodologies for creating external control arms and conducting comparative effectiveness research.
Protocol for Constructing an External Control Arm from EHR Data
This protocol is commonly employed in single-arm trials for rare diseases or oncology products [9].
- Step 1: Define the ECA Cohort. Identify patients from the EHR database who meet the same eligibility criteria as the single-arm trial's intervention group. This includes matching on key factors such as diagnosis, prior lines of therapy, disease stage, and demographic characteristics [9] [99].
- Step 2: Index Date Alignment. Assign an index date for each patient in the ECA cohort that corresponds to the start of a defined therapy (the comparator). This aligns the start of follow-up between the trial and ECA cohorts [9].
- Step 3: Outcome Ascertainment. Extract and validate the outcomes of interest (e.g., overall survival, progression-free survival) from the EHR for the ECA cohort using the same definitions as the clinical trial [9] [102]. This may involve abstracting data from unstructured clinical notes.
- Step 4: Statistical Analysis. Account for potential confounding and selection bias using statistical techniques such as propensity score matching or weighting to balance baseline characteristics between the trial and ECA cohorts. Subsequently, comparative analyses (e.g., Cox proportional hazards models) are performed [9].
Protocol for a Multi-Source RWE Study on Comparative Effectiveness
This protocol leverages multiple data sources to capture a comprehensive, longitudinal view of the patient journey [99].
- Step 1: Data Source Linkage. Link electronic medical records (EMR) and healthcare claims data at the patient level to obtain a foundational view of diagnosis, treatment patterns, and healthcare resource utilization. This combination provides a "big picture" of the clinical and economic pathway [99].
- Step 2: Integrate Patient-Generated Health Data (PGHD). Incorporate patient-reported outcomes (PROs) from consented surveys and questionnaires. PGHD adds granularity on treatment compliance, quality of life, symptom burden, and factors influencing adherence that are often absent from claims or EMRs [99].
- Step 3: Biospecimen Analysis (Optional). For deeper clinical insights, link the clinical and PRO data to biorepository data (e.g., whole blood, serum, tissue). This allows for retrospective genotyping or biomarker analysis to understand treatment response in specific patient subpopulations [99].
- Step 4: Advanced Analytics and Visualization. Apply sophisticated analytics and interactive data visualization tools to the integrated dataset. This enables dynamic stratification analyses, exploration of disease progression, and comparison of outcomes between treatment cohorts in a real-world setting [103] [99].
The Application of RWE in Cost-Effectiveness Analyses
RWE can provide critical, practice-based parameter estimates for decision-analytic models used in cost-effectiveness analyses (CEAs), though this application presents specific challenges.
Data Inputs and Methodological Challenges
In economic modeling, RWE is particularly valuable for informing absolute event probabilities, long-term natural history of diseases, real-world resource use, and cost data drawn from actual clinical practice [101]. However, a literature review highlights significant methodological limitations, including confounding bias, missing data, lack of accurate drug exposure records, and general errors during the record-keeping process [101]. Furthermore, guidance from HTA bodies on appropriate methods to deal with these biases and integrate RWE into models remains scarce [101]. The table below contrasts the applications and challenges of using RWE versus RCT data in economic evaluations.
Table 2: Comparison of RWE and RCT Data in Cost-Effectiveness Analysis
| Parameter | RWE for CEA | RCT Data for CEA | Key Challenges with RWE [101] |
|---|---|---|---|
| Treatment Effectiveness | Estimates effectiveness in heterogeneous routine care populations [101] [100] | Measures efficacy in a selected, controlled population | Confounding by indication, missing data, unmeasured confounding |
| Resource Use & Costs | Provides actual observed patterns of care and associated costs [101] | Often relies on protocols or assumptions, may not reflect real-world use | Incomplete records, coding errors, data not collected for research purposes |
| Long-Term Outcomes | Can inform long-term extrapolations and natural history [101] [100] | Limited by trial duration, requires modeling beyond follow-up | Requires large, longitudinal datasets; loss to follow-up |
| Patient Subgroups | Can explore cost-effectiveness in specific subpopulations [99] | Often underpowered for subgroup analysis | Requires sufficient sample size; multiple testing issues |
| HTA Scrutiny | Varies by agency; higher scrutiny for pivotal efficacy claims [9] | Generally accepted as gold standard for efficacy | Lack of clear HTA guidance on methods for handling RWE biases [101] |
The Scientist's Toolkit: Essential Reagents for RWE Generation
Generating high-quality RWE requires a suite of data, methodological, and analytical "reagents." The following toolkit details essential components for constructing robust real-world studies intended for HTA.
Table 3: Essential Reagents for RWE Generation in HTA Research
| Tool Category | Specific Item | Function & Application in RWE Studies |
|---|---|---|
| Core Data Sources | Electronic Health Records (EHR) & Claims Data | Provides foundational information on diagnoses, treatments, and healthcare utilization in broad populations; crucial for characterizing care pathways and resource use [99] [102]. |
| Patient-Generated Health Data (PGHD) | Supplies granular, patient-centric data on outcomes, quality of life, and adherence from the patient's perspective, adding context to structured clinical data [99]. | |
| Disease & Drug Registries | Offers structured, longitudinal data on specific patient populations, often used for natural history studies and constructing external control arms [9] [100]. | |
| Methodological & Quality Frameworks | ISPOR SUITABILITY Checklist | Provides a standardized framework for assessing and reporting the quality and suitability of EHR data for HTA, ensuring transparency and rigor [102]. |
| Propensity Score Methods | A key statistical technique to balance measured confounders between treatment groups in non-randomized studies, improving the validity of comparative effectiveness estimates [9]. | |
| Analytical & Visualization Platforms | Interactive RWE Dashboards (e.g., R/Shiny) | Enables dynamic data exploration, cohort creation, and visualization of patient journeys, medical patterns, and outcomes; facilitates deeper insight generation [103]. |
| Advanced Analytics Capabilities | Allows for complex analyses, including longitudinal modeling and machine learning, to infer and predict patient outcomes from deep and broad datasets [99]. |
In the evolving landscape of health technology assessment (HTA) and regulatory decision-making, Real-World Evidence (RWE) has emerged as a crucial complement to traditional randomized controlled trials (RCTs). The 21st Century Cures Act of 2016 accelerated this shift by encouraging the development of a framework for using RWE to support drug approval and post-approval studies [2]. Validated RWE represents clinical evidence derived from the analysis of Real-World Data (RWD) that meets stringent criteria for relevance, reliability, and scientific validity sufficient to inform regulatory and HTA decisions [2] [104]. This guide synthesizes the multifaceted criteria for RWE validation from major stakeholders—regulatory agencies, HTA bodies, and research consortia—providing researchers and drug development professionals with a structured framework for generating compliant and impactful evidence.
The distinction between RWD and RWE is fundamental. RWD encompasses "data relating to patient health status and/or the delivery of health care routinely collected from a variety of sources," while RWE is "the clinical evidence about the usage and potential benefits or risks of a medical product derived from analysis of RWD" [2] [27]. For RWD to generate validated RWE, it must undergo rigorous methodological processes to ensure it constitutes valid scientific evidence that can reliably support specific regulatory and HTA decisions [104].
Stakeholder Criteria for RWE Validation
Major stakeholders have established overlapping but distinct criteria for validating RWE. The following table synthesizes the core requirements across key organizations.
Table 1: Comparative Criteria for Validated RWE Across Major Stakeholders
| Stakeholder | Primary Validation Focus | Data Quality Requirements | Methodological Standards | Key Application Contexts |
|---|---|---|---|---|
| US FDA | Relevance and Reliability of RWD [2] [104] | - Comprehensive data provenance- Source data verification where appropriate- Complete and accurate records [104] | - Controlled protocols with standard data definitions- Pre-specified analysis plans- Bias minimization strategies [104] | - Support new indications for approved drugs- Post-market safety surveillance- Satisfy post-approval study requirements [2] |
| European HTA Bodies (e.g., NICE, G-BA, HAS) | Comparative effectiveness and contextualization of RCT findings [81] | - Fitness for purpose in specific healthcare contexts- Appropriate population representativeness [81] | - Robust indirect treatment comparisons- Appropriate handling of confounding- Transparent uncertainty assessment [81] | - Indirect treatment comparisons- Economic modeling inputs- Contextualization of clinical trial results [81] |
| Research Consortia (e.g., EHDEN) | Data standardization and interoperability [27] | - Standardization to common data models- Extensive data quality characterization [27] | - Network analysis capabilities- Federated analysis protocols [27] | - Natural history studies- Disease progression modeling- Healthcare utilization research [27] |
US Food and Drug Administration (FDA) Framework
The FDA's framework for validated RWE emphasizes regulatory-grade evidence suitable for decision-making. The agency requires that RWD be "relevant and reliable" for informing or supporting a specific regulatory decision [104]. For pre-market applications, the FDA expects controlled protocols with standard data definitions, established data integrity controls, and comprehensive description of patient selection criteria to minimize bias and ensure representativeness of the target population [104].
The FDA has clarified that an Investigational Device Exemption (IDE) is typically not required for gathering RWD when the collection process is purely observational—capturing device use during normal medical practice for its intended use. However, if RWD describes off-label use intended for regulatory submission, an IDE is required [104]. This distinction is crucial for researchers planning RWE generation strategies.
European Regulatory and HTA Bodies
European Medicines Agency (EMA) and HTA bodies such as the UK's National Institute for Health and Care Excellence (NICE), Germany's Gemeinsamer Bundesausschuss (G-BA), and France's Haute Autorité de Santé (HAS) demonstrate divergent acceptance criteria for RWE, particularly in oncology [81]. While these bodies increasingly leverage RWE as external controls for indirect treatment comparisons or to contextualize clinical trial results, methodological concerns frequently limit acceptance.
A scoping review of European oncology medicine approvals found inconsistent acceptability of RWE across agencies, with rejections primarily due to methodological biases related to confounding, selection bias, and non-comparability of datasets [81]. This highlights the critical need for researchers to engage early with both regulatory and HTA bodies to align evidence generation strategies with divergent stakeholder requirements.
Methodological Protocols for RWE Validation
Experimental Design and Data Quality Assessment
Validated RWE generation requires meticulous attention to study design and data quality assessment protocols. The foundational principle is fitness for purpose—the methodology must align with the specific research question and intended use of the evidence [2] [104].
Table 2: Methodological Approaches for RWE Validation
| Study Design | Protocol Requirements | Bias Control Mechanisms | Appropriate Use Cases |
|---|---|---|---|
| Prospective Cohort Studies | - Pre-specified data collection points- Standardized outcome definitions- Prospective data management plan [27] | - Multivariate adjustment- Propensity score methods- Sensitivity analyses [27] | - Natural history studies- Post-market safety surveillance- Comparative effectiveness research [27] |
| Retrospective Database Analysis | - Comprehensive data mapping- Validation of key variables- Cross-validation across data sources [104] | - New-user designs- Active comparator frameworks- Quantitative bias analysis [105] | - Treatment pattern analyses- Healthcare resource utilization- Outcomes in understudied populations [105] |
| Registry-Based Studies | - Pre-defined eligibility criteria- Standardized data collection forms- Periodic data quality audits [27] | - Statistical matching methods- High completeness of follow-up- Analysis of missing data patterns [27] | - External control arms- Long-term outcomes assessment- Rare disease research [27] |
| Pragmatic Clinical Trials | - Simplified participant procedures- Heterogeneous practice settings- Outcome assessment through routine care [27] | - Randomization within clinical care- Blinded outcome assessment- Intent-to-treat analysis [27] | - Effectiveness in routine practice- Implementation research- Heterogeneous treatment effects [27] |
Workflow for RWE Generation and Validation
The following diagram illustrates the end-to-end workflow for generating validated RWE, from data source identification through regulatory submission, integrating requirements from multiple stakeholders.
Stakeholder Engagement and Evidence Requirements
The evolving landscape of RWE validation requires proactive engagement with multiple stakeholders throughout the evidence generation process. Researchers should anticipate differing evidence requirements between regulatory and HTA bodies, particularly regarding comparative effectiveness and economic value [81].
Table 3: Stakeholder-Specific Evidence Requirements for Validated RWE
| Stakeholder Category | Primary Evidence Needs | Acceptable RWE Study Designs | Common Methodological Concerns |
|---|---|---|---|
| Regulatory Agencies (FDA, EMA) | - Causal treatment effects- Safety in broader populations- New indication support [2] [104] | - Prospective registry studies- Well-controlled retrospective studies- Pragmatic clinical trials [104] | - Confounding control- Missing data handling- Outcome validation [104] |
| HTA Bodies (NICE, G-BA, HAS) | - Comparative effectiveness- Generalizability to local populations- Long-term outcomes [81] | - Indirect treatment comparisons- High-quality registry data- Prospective observational studies [81] | - Population comparability- Unmeasured confounding- Outcome relevance to decision context [81] |
| Payers | - Outcomes in relevant subpopulations- Resource utilization impacts- Comparative cost-effectiveness [105] | - Claims data analyses- EHR-based outcomes studies- Registry analyses [105] | - Generalizability across settings- Adequate follow-up duration- Complete cost capture [105] |
The Scientist's Toolkit: Essential Reagents for RWE Generation
Generating validated RWE requires both methodological rigor and specialized analytical tools. The following table details essential components of the RWE researcher's toolkit.
Table 4: Essential Research Reagent Solutions for RWE Generation
| Tool Category | Specific Solutions | Function in RWE Generation | Validation Considerations |
|---|---|---|---|
| Data Source Platforms | - Electronic Health Records (EHR)- Medical claims databases- Disease registries- Digital health technologies [27] [104] | Provide structured access to longitudinal patient data from routine care settings | - Data completeness verification- Variable accuracy assessment- Representativeness evaluation [104] |
| Analytical Platforms | - IQVIA RWE Platform- Optum RWE Platform- Flatiron Health RWE Platform- TriNetX [31] | Enable large-scale data analysis with standardized methodologies across diverse datasets | - Algorithm validation- Processing transparency- Reproducibility documentation [31] |
| Data Standardization Tools | - OMOP Common Data Model- Sentinel Common Data Model- CDISC standards [27] | Harmonize heterogeneous data sources to enable federated analysis and cross-validation | - Mapping accuracy assessment- Semantic consistency verification- Structural validity checks [27] |
| Bias Assessment Frameworks | - Quantitative bias analysis- Propensity score methods- Negative control outcomes [27] [105] | Identify, quantify, and adjust for systematic errors in observational study designs | - Sensitivity of conclusions to assumptions- Residual confounding quantification- Transportability assessment [105] |
Case Studies in RWE Application
Regulatory Case Studies
Recent FDA approvals demonstrate the application of RWE validation criteria in practice. The Inspire Upper Airway Stimulation device expanded its indication using real-world evidence from the ADHERE Registry, an ongoing observational study [104]. Similarly, the PALMAZ MULLINS XD Pulmonary Stent utilized a retrospective, multicenter analysis of data from the Congenital Cardiovascular Interventional Study Consortium (CCISC) Registry to assess safety and effectiveness outcomes associated with real-world use [104].
These examples illustrate successful applications of the FDA's RWE framework, where data from rigorously maintained registries with predefined data collection protocols met the threshold for "valid scientific evidence" [104].
HTA Case Studies
A scoping review of European oncology medicines revealed that while RWE was frequently submitted to HTA bodies like NICE, G-BA, and HAS, acceptance varied substantially [81]. The comparative assessment of RWE acceptability for the same oncology medicines across agencies revealed significant discrepancies, with no clear consensus on the most effective way to leverage RWE in approvals [81]. This highlights the ongoing challenges in generating RWE that meets the distinct validation criteria of multiple HTA stakeholders simultaneously.
The validation of RWE represents a complex interplay between methodological rigor, stakeholder requirements, and evolving regulatory science. As the European Union implements its Joint Clinical Assessment in 2025, the development of synergetic standards for RWE use across EMA and European HTA bodies becomes increasingly crucial for ensuring equitable and timely patient access to innovative therapies [81].
Successful generation of validated RWE requires researchers to navigate the sometimes divergent criteria of regulatory and HTA stakeholders through early engagement, meticulous study design, and comprehensive validation of both data sources and analytical approaches. By adhering to the synthesized framework presented in this guide, researchers and drug development professionals can generate RWE that meets the stringent criteria of major stakeholders and ultimately enhances the evidence base for medical product evaluation across the development lifecycle.
The implementation of the EU Joint Clinical Assessment (JTA) marks a transformative shift in how clinical evidence is evaluated across Europe. This new regulation establishes a unified procedure for assessing the clinical value of new health technologies, moving away from fragmented national assessments toward a harmonized European approach [106]. For real-world evidence (RWE), this represents both an unprecedented opportunity and a significant challenge. The JCA framework creates a pivotal platform that will likely accelerate the standardization and maturation of RWE methodologies, potentially establishing new benchmarks for evidence validity that will influence health technology assessment (HTA) practices globally [107] [108]. As drug development professionals and researchers navigate this changing landscape, understanding the evolving standards for RWE within the JCA context becomes critical for successful market access and demonstrating therapeutic value in the European market.
JCA Implementation Timeline and Evolving Evidence Requirements
Phased Implementation of Joint Clinical Assessments
The EU HTA Regulation (EU 2021/2282) follows a carefully staged implementation schedule designed to allow gradual adaptation by all stakeholders [106]. This phased approach prioritizes therapeutic areas with high unmet medical needs and particularly complex evidence requirements, beginning with oncology and advanced therapies.
Table: EU JCA Implementation Timeline
| Effective Date | Therapeutic Scope | Key Implications for RWE |
|---|---|---|
| January 2025 | New active substances in oncology and all Advanced Therapy Medicinal Products (ATMPs) | RWE may be utilized to address evidence gaps, particularly for novel mechanisms and single-arm trial contexts [106] [109] |
| January 2028 | All orphan medicines | Critical for rare diseases where traditional RCTs are challenging; RWE can complement limited clinical trial data [110] [108] |
| January 2030 | All other medicines covered by the regulation | Expected maturation of RWE standards and methodologies across broader therapeutic areas [110] |
Comparative Analysis of Current vs. Future RWE Applications
The JCA framework introduces structured evidence requirements that differ significantly from previous fragmented national approaches. Understanding these distinctions is essential for strategic evidence planning.
Table: Evolution of RWE Applications in European HTA
| Evidence Application | Current National HTA Practices | Future JCA Framework |
|---|---|---|
| Comparative Effectiveness | Variable acceptance across member states; often rejected due to methodological concerns [97] | Explicitly recognized for indirect treatment comparisons and external control arms, though with acknowledged limitations [111] |
| Trial Contextualization | Limited systematic application | Formalized role in understanding clinical management, epidemiology, and treatment patterns [111] |
| Unmet Need Demonstration | Country-specific requirements and data preferences | Harmonized approach across member states with potential for standardized RWE frameworks [108] |
| Post-Authorization Evidence | Diverse national requirements for follow-up evidence | Structured lifecycle evidence generation with potential for coordinated RWE collection [111] |
Methodological Framework: Experimental Protocols for RWE Validation
Protocol for RWE in External Control Arm Construction
The use of real-world data to construct external control arms represents one of the most promising applications within the JCA framework, particularly for single-arm trials in oncology and ATMPs [106]. The following protocol outlines a standardized methodology for this application:
Objective: To generate robust comparative evidence when randomized controls are ethically or practically infeasible, by creating a balanced external control cohort from real-world data sources [97].
Data Source Selection: Identify and curate high-quality RWD sources with complete capture of patient journeys. Preferred sources include national cancer registries, prospectively maintained disease registries, and electronic health record systems with structured treatment and outcome data [108]. Document data provenance, completeness, and transformation processes.
Covariate Selection and Balance: Pre-specify prognostic covariates based on clinical knowledge and literature. Implement propensity score methods (matching, weighting, or stratification) to achieve balance between treatment and external control groups. Target effective sample size and covariate balance metrics should be specified a priori [97].
Sensitivity Analyses: Plan comprehensive sensitivity analyses to assess robustness of findings to unmeasured confounding. These may include quantitative bias analysis, inclusion of prognostic covariates not used in primary analysis, and application of different propensity score methodologies [97].
The JCA guidance acknowledges this application while highlighting limitations, specifically noting a "high risk of confounding bias" that must be addressed through rigorous methodological approaches [111].
Protocol for RWE in Indirect Treatment Comparisons
Within the JCA's Population, Intervention, Comparator, Outcomes (PICO) structure, indirect treatment comparisons (ITCs) will play a crucial role in establishing comparative effectiveness [111]. The following protocol details a validated approach:
Objective: To estimate relative treatment effects between interventions when head-to-head evidence is lacking, by synthesizing evidence across different study sources through a common comparator.
Systematic Literature Review: Conduct comprehensive literature search following PRISMA guidelines to identify all relevant RCTs and high-quality observational studies for each intervention. Document search strategy, inclusion/exclusion criteria, and data extraction methods.
Feasibility Assessment: Evaluate clinical and methodological heterogeneity between studies assessing different interventions. Assess similarity of patient populations, outcome definitions, and study designs across the evidence network.
Statistical Analysis: Implement appropriate ITC methodologies, including network meta-analysis for connected evidence networks or matching-adjusted indirect comparison (MAIC) and simulated treatment comparison (STC) for individual-level data adjustments. All analyses should adjust for key effect modifiers and prognostic factors [111].
Quality Evaluation: Assess strength of evidence using modified GRADE criteria for network meta-analysis or the ISPOR questionnaire for good research practices in ITC.
The Scientist's Toolkit: Essential Reagent Solutions for RWE Generation
Generating robust RWE that meets JCA standards requires specialized methodological tools and approaches. The following table details essential components of the research toolkit for professionals working in this evolving landscape.
Table: Essential Research Reagent Solutions for JCA-Compliant RWE
| Tool Category | Specific Methodologies | Application in JCA Context |
|---|---|---|
| Data Quality Assurance | Data provenance frameworks, completeness metrics, consistency checks | Ensures RWD sources meet minimum quality thresholds for inclusion in JCA submissions [108] |
| Confounding Control | Propensity score methods, instrumental variable analysis, high-dimensional propensity scoring | Addresses key methodological concern of confounding bias highlighted in JCA guidance [111] [97] |
| Sensitivity Analysis | Quantitative bias analysis, E-value calculation, probabilistic sensitivity analysis | Demonstrates robustness of RWE findings to potential biases and unmeasured confounding [97] |
| Evidence Synthesis | Network meta-analysis, matching-adjusted indirect comparison, simulated treatment comparison | Supports indirect treatment comparisons within the PICO framework [111] |
| Transparency Tools | Pre-analysis plans, analysis code repositories, structured result reporting | Meets JCA requirements for methodological transparency and reproducibility [95] |
Strategic Implications for Drug Development Professionals
The introduction of JCAs necessitates fundamental changes in evidence generation strategies throughout the drug development lifecycle. Success in this new environment requires cross-functional collaboration and early strategic planning, particularly regarding the role of RWE [95].
Early Integration of RWE and HTA Considerations
The compressed JCA timeline, with dossier submission required around day 170 of the EMA review process—before the final marketing authorization—demands unprecedented early planning [110]. Market access and HEOR teams must be engaged during Phase II trials to ensure that evidence generation strategies address both regulatory and HTA requirements [110]. This includes strategic use of Joint Scientific Consultations (JSCs), which provide parallel advice from both regulatory and HTA bodies, though securing these slots is competitive due to strict eligibility criteria [110].
Operationalizing RWE for JCA Success
PICO Forecasting and Strategic Alignment: Companies should internally forecast potential PICOs early in development to anticipate evidence needs [95]. This involves understanding varying standards of care across member states and strategically planning for potential subgroup analyses and comparator choices that may be required in the JCA process [110].
Evidence Gap Mitigation: Proactively identify where RWE can address inevitable evidence gaps, particularly for long-term outcomes, underrepresented populations, and comparative effectiveness against relevant standards of care [108]. Developing a comprehensive RWE generation plan as part of the overall clinical development program is essential.
Governance and Process Adaptation: Successful navigation of the JCA process requires breaking down traditional silos between regulatory, clinical, and market access functions [95]. Companies should establish clear cross-functional governance models with defined responsibilities for JCA preparation and submission.
The implementation of the EU Joint Clinical Assessment represents a pivotal moment for the evolution of real-world evidence standards. While the JCA framework currently maintains a preference for randomized clinical trial evidence, it creates structured pathways for RWE to address critical evidence gaps, particularly for comparative effectiveness and external controls [111]. The success of this integration will depend on continued methodological rigor, transparency in study conduct and reporting, and proactive engagement between industry, regulators, and HTA bodies.
For researchers and drug development professionals, the changing landscape necessitates a fundamental shift in evidence generation strategies. Early planning, cross-functional collaboration, and strategic RWE integration throughout the development lifecycle will be essential for navigating the JCA process successfully [95]. As the framework matures and expands to include more therapeutic areas by 2030, the standards established through these early JCAs will likely become benchmarks for RWE validity that influence global HTA practices [107]. The organizations that invest in building robust RWE capabilities and methodologies today will be best positioned to demonstrate the value of their innovations in the European market of tomorrow.
Conclusion
The validation of Real-World Evidence for Health Technology Assessment is no longer an aspirational goal but a necessary standard for efficient and evidence-based drug development. This synthesis demonstrates that robust RWE validation rests on a triad of pillars: the application of rigorous methodological frameworks like the target trial approach, unwavering attention to data quality and governance, and a clear understanding of the distinct but converging needs of regulators and HTA bodies. While challenges of data suitability and methodological bias persist, the growing body of successful regulatory precedents and evolving HTA guidance provides a clear path forward. For researchers and drug development professionals, mastering this landscape is paramount. Future progress hinges on continued multi-stakeholder collaboration to harmonize standards, the development of more sophisticated causal inference techniques, and the strategic use of RWE to support dynamic treatment evaluations and early access for patients, ultimately making medicine more personalized, precise, and accessible.
References
- 1. Real-world evidence to support health technology assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12018852/]
- 2. Real-World Evidence [https://www.fda.gov/science-research/science-and-research-special-topics/real-world-evidence]
- 3. Comparison of two assessments of realâ€world data and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10766019/]
- 4. What is the Difference Between RWE and RWD? [https://pro.carenity.com/library/difference-rwe-rwd/]
- 5. Guide to real-world data vs real-world evidence [https://within3.com/blog/what-is-real-world-data]
- 6. What is the difference between RWD and RWE? [https://www.mmitnetwork.com/what-is-difference-between-rwd-and-rwe/]
- 7. Real-World Data: What Is It and Why Does It Matter? [https://www.datavant.com/real-world-data]
- 8. Real-World Evidence in Health Technology Reassessments [https://evidence-hub.aetion.com/real-world-evidence-in-health-technology-reassessments-a-new-era-in-evidence-based-decision-making]
- 9. The role and value of real-world evidence in health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12019763/]
- 10. FDA-Regulated Clinical Trials vs. Real-World Data [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562589/]
- 11. Beyond RCTs: the real-world evidence revolution [https://pharmaceutical-journal.com/article/feature/beyond-rcts-the-real-world-evidence-revolution]
- 12. The Intersection of Real-World Evidence and Clinical Trials [https://medipharmsolutions.com/blog/the-intersection-of-real-world-evidence-and-clinical-trials/]
- 13. How to transform your clinical insights with real-world ... [https://www.clinicaltrialsarena.com/sponsored/transformation-with-real-world-evidence-rwe/]
- 14. Real-world evidence: state-of-the-art and future perspectives [https://pmc.ncbi.nlm.nih.gov/articles/PMC11963347/]
- 15. Use of Real-World Evidence in Health Technology ... [https://www.sciencedirect.com/science/article/pii/S1098301525000907]
- 16. FDA in Flux – October 2025 Newsletter [https://www.mintz.com/insights-center/viewpoints/2791/2025-10-16-fda-flux-october-2025-newsletter]
- 17. Health technology assessment bodies [https://www.ema.europa.eu/en/partners-networks/health-technology-assessment-bodies]
- 18. Health Technology Assessments in 2025: What changes ... [https://www.eurordis.org/what-happens-hta-2025/]
- 19. Key Takeaways from the NICE Conference 2025 [https://lumanity.com/perspectives/the-nice-conference-2025-a-celebration-of-25-years-of-nice/]
- 20. The era of EU HTA has officially begun—but how will ... [https://www.cencora.com/resources/pharma/htaq-spring-2025-summary/the-era-of-eu-hta-has-officially-begun]
- 21. 2025 Market Access Trends: Key Shifts Shaping Global ... [https://remapconsulting.com/market-access-trends/2025-market-access-trends/]
- 22. NICE 2025 Appraisal Reforms: Impact on HST & STA ... [https://remapconsulting.com/hta/nice-2025-appraisal-reforms-hst-sta-submissions/]
- 23. Identification and Description of Regulatory and Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579653/]
- 24. Regulatory and Payer Evaluation of Real-World Evidence [https://www.drugepi.org/dope/rwe-roundtable-2025]
- 25. FDA Human Foods Program: FY 2025 Priority Deliverables [https://www.fda.gov/food/hfp-constituent-updates/fda-human-foods-program-fy-2025-priority-deliverables]
- 26. Real-World Evidence to Reinforce Clinical Trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11130860/]
- 27. Real-World Evidence: A Primer - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9815890/]
- 28. Real-world Evidence versus Randomized Controlled Trial [https://pmc.ncbi.nlm.nih.gov/articles/PMC6097073/]
- 29. JCA & HTA 2025: Evidence, RWE, and AI Trends in Market ... [https://trinitylifesciences.com/blog/learnings-to-kick-start-2025-jca-and-hta/]
- 30. Integration of real-world evidence from different data sources ... [https://www.frontierspartnerships.org/journals/journal-of-pharmacy-pharmaceutical-sciences/articles/10.3389/jpps.2023.11460/full]
- 31. 36 Top RWE Platforms in 2025 [https://www.mahalo.health/insights/top-real-world-evidence-rwe-platforms]
- 32. The target trial framework for causal inference from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11936718/]
- 33. Target Trial Emulation: A Concept Simply Explained [https://www.psychiatrist.com/jcp/target-trial-emulation-a-concept-simply-explained/]
- 34. Methods for real-world studies of comparative effects [https://www.nice.org.uk/corporate/ecd9/chapter/methods-for-real-world-studies-of-comparative-effects]
- 35. Target trial framework for determining the effect of changes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11227826/]
- 36. Comparison of a Target Trial Emulation Framework vs Cox ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9530966/]
- 37. Review of methods to deal with the misalignment of times ... [https://www.sciencedirect.com/science/article/pii/S0895435625002318]
- 38. The Target Trial Toolbox | Yale PEW [https://medicine.yale.edu/lab/pew/project-highlights/trial-toolbox/]
- 39. A comparison of four quasi-experimental methods: an analysis ... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-022-08657-0]
- 40. Acceptability of Using Real-World Data to Estimate ... [https://www.sciencedirect.com/science/article/pii/S1098301524000706]
- 41. An Introduction to the Quasi-Experimental Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11741180/]
- 42. Conceptualising natural and quasi experiments in public health [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-021-01224-x]
- 43. R WE ready for reimbursement? A round up of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12403379/]
- 44. Application of Causal Inference Methods in the Analysis ... [https://www.sciencedirect.com/science/article/pii/S1878875021014947]
- 45. External control arms for rare diseases: building a body of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10673956/]
- 46. Realâ€world evidence to support regulatory decision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7687199/]
- 47. Understanding external controls in clinical trials [https://www.sarepta.com/newsroom/understanding-external-controls-and-their-importance-clinical-trials-rare-diseases]
- 48. Editorial: External control arms for single-arm studies [https://www.frontiersin.org/journals/drug-safety-and-regulation/articles/10.3389/fdsfr.2025.1579171/full]
- 49. Why Real-World External Control Arms Are Gaining ... [https://www.putassoc.com/insights/why-real-world-external-control-arms-are-gaining-ground-in-health-technology-assessment/]
- 50. FedECA: federated external control arms for causal ... [https://www.nature.com/articles/s41467-025-62525-z]
- 51. Pink Sheet - External Control Arms: Better Than Single ... [https://friendsofcancerresearch.org/news/pink-sheet-external-control-arms-better-than-single-arm-studies-but-no-replacement-for-randomization/]
- 52. The feasibility of using real world data as external control ... [https://www.sciencedirect.com/science/article/pii/S1359644625000376]
- 53. Real-World Evidence for External Control Arms in Clinical ... [https://tfscro.com/resources/harnessing-real-world-evidence-rwe-for-effective-external-control-arms-in-clinical-trials/]
- 54. Surrogate Endpoints in HTA: Linking Evidence to Pricing & ... [https://remapconsulting.com/hta/surrogate-endpoints-hta-pricing-access/]
- 55. Use of surrogate endpoints in health technology assessment [https://pmc.ncbi.nlm.nih.gov/articles/PMC11894387/]
- 56. highlighting existing strategies for effective drug evaluation [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02683-2]
- 57. Integrating RCTs, RWD, AI/ML and Statistics [https://arxiv.org/html/2511.19735v1]
- 58. FDA use of Real-World Evidence in Regulatory Decision ... [https://www.fda.gov/science-research/real-world-evidence/fda-use-real-world-evidence-regulatory-decision-making]
- 59. Real world data clinical trials: Essential 2025 [https://lifebit.ai/blog/real-world-data-clinical-trials/]
- 60. Reviewing implementation in practice of the NICE Health ... [https://www.abpi.org.uk/publications/reviewing-implementation-in-practice-of-the-nice-health-technology-evaluation-manual-connie-october-2025/]
- 61. CBER and CDER Real-World Evidence (RWE) [https://www.fda.gov/science-research/real-world-evidence/center-biologics-evaluation-and-research-center-drug-evaluation-and-research-real-world-evidence]
- 62. Real-World Evidence in FDA Approvals for Labeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446098/]
- 63. Exploring Methodologies in Real-World Evidence (RWE) ... [https://pro.carenity.com/library/methodologies-rwe-research/]
- 64. A Brief Report on Proposed Areas of International ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11907323/]
- 65. CTTI Recommendations: Use of Real-World Data to Plan ... [https://ctti-clinicaltrials.org/about/ctti-projects/real-world-data/ctti-recommendations-use-of-real-world-data-to-plan-eligibility-criteria-and-enhance-recruitment/]
- 66. Real-World Evidence Collaborative White Papers [https://healthpolicy.duke.edu/real-world-evidence-collaborative-white-papers]
- 67. Using EHR-derived real-world data for HTA decision ... [https://resources.flatiron.com/real-world-evidence/real-world-data-hta-market-access]
- 68. Parallel Progress in Artificial Intelligence and Real-World ... [https://globalforum.diaglobal.org/issue/august-2025/parallel-progress-in-artificial-intelligence-and-real-world-evidence-creates-a-new-vision-for-clinical-evidence/]
- 69. Real-world data: a brief review of the methods, applications ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-022-01768-6]
- 70. Measuring Real-World Intervention Effectiveness using ... [https://www.sciencedirect.com/science/article/pii/S0002916523488995]
- 71. Statistical Methods for Baseline Adjustment and Cohort ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11876781/]
- 72. 用好真实世界数æ®è¿˜æœ‰å¤šè¿œ - 新医改评论 [http://xygpl.com/contents/3/19814.html]
- 73. The maze of real-world evidence frameworks - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11367564/]
- 74. Real World Evidence: Final Reflection Paper on RWD in NIS [https://www.gmp-compliance.org/gmp-news/real-world-evidence-final-reflection-paper-on-rwd-in-nis]
- 75. 医ä¿çš„é’±æ€Žä¹ˆèŠ±ï¼ŸçœŸå®žä¸–ç•Œç ”ç©¶æˆ–å°†ç»™å‡ºæ–°ç”案 [https://www.phirda.com/artilce_40635.html?module=trackingCodeGenerator]
- 76. 真实世界è¯æ®é©±åŠ¨åŒ»ä¿å†³ç–å‡çº§â€”—解æžè‹±å›½å®žè·µ [https://view.inews.qq.com/a/20251118A05RML00]
- 77. CDEå‘布《基于疾病登记的真实世界数æ®åº”用指导原则(试行)》 [https://bydrug.pharmcube.com/news/detail/ce222f240c924b67abfab4972d001550]
- 78. Transcelerate RWD Audit Readiness: Data Service ... [https://www.transceleratebiopharmainc.com/mc-resource/transcelerate-rwd-audit-readiness-data-service-provider-survey-detailed-report/]
- 79. Assessing and Interpreting Real-World Evidence Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC8771197/]
- 80. A Guide to Real-World Evidence in Clinical Trials [https://www.quanticate.com/blog/real-world-evidence-in-clinical-drug-development]
- 81. A Review and Comparative Case Study Analysis of Real- ... [https://www.sciencedirect.com/science/article/pii/S1098301524028596]
- 82. The FDA's RWE Guidance - Castor EDC [https://www.castoredc.com/blog/5-key-takeaways-from-the-fdas-real-world-evidence-guidance/]
- 83. Transparency in real-world evidence (RWE) studies to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7472869/]
- 84. Real-World Evidence: Best Practices for Successful ... [https://acrpnet.org/2025/02/14/real-world-evidence-best-practices-for-successful-regulatory-engagements]
- 85. Real-World Evidence (RWE) in Health Technology ... [https://www.ispor.org/heor-resources/presentations-database/presentation-cti/ispor-2025/poster-session-1/real-world-evidence-rwe-in-health-technology-assessment-hta--global-guidelines-on-the-use-of-rwe-in-evidence-generation-for-hta-evaluation]
- 86. Use of sensitivity analyses to assess uncontrolled ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272854/]
- 87. RWE 101 - How Robust is RWE? [https://rwr-regs.com/rwe-101-how-robust-is-rwe/]
- 88. Generating real-world evidence at scale using advanced ... [https://www.mckinsey.com/industries/life-sciences/our-insights/generating-real-world-evidence-at-scale-using-advanced-analytics]
- 89. Treatment Crossover Adjustments in RWE Outcome Analysis [https://healthark.ai/handling-real-world-treatment-crossovers-to-improve-rwe-outcomes/]
- 90. Unlocking the Power of Benchmarking: Real-World-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10486409/]
- 91. R WE ready for reimbursement? A round-up of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580926/]
- 92. Advancing Real-World Evidence Program [https://www.fda.gov/drugs/development-resources/advancing-real-world-evidence-program]
- 93. Real-world evidence | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/about-us/how-we-work/data-regulation-big-data-other-sources/real-world-evidence]
- 94. EU | EMA 2025 Vision for the Regulatory Use of RWE [https://rwr-regs.com/eu-ema-2025-vision-for-the-regulatory-use-of-rwe-connecting-the-pieces/]
- 95. EU HTA Regulation Joint Clinical Assessments [https://globalforum.diaglobal.org/issue/august-2024/eu-hta-regulation-are-you-ready-for-2025-joint-clinical-assessment/]
- 96. European health technology assessment | IQWiG.de [https://www.iqwig.de/en/presse/in-the-focus/european-health-technology-assessment/]
- 97. A Review and Comparative Case Study Analysis of Real ... [https://pubmed.ncbi.nlm.nih.gov/39393564/]
- 98. OncLive's August EMA Regulatory Recap: Key EU ... [https://www.onclive.com/view/onclive-s-august-ema-regulatory-recap-key-eu-approvals-in-oncology]
- 99. Leveraging real-world evidence with analytics: 3 essential ... [https://www.targetrwe.com/research/news/leveraging-real-world-evidence-with-analytics-3-essential-components-to-capture-a-360-degree-view-of-your-patient-population/]
- 100. Considering Clinical, Real-World, and Unpublished Evidence [https://icer.org/our-approach/methods-process/considering-clinical-real-world-and-unpublished-evidence/]
- 101. Cost-effectiveness analyses using real-world data [https://pubmed.ncbi.nlm.nih.gov/30816067/]
- 102. ISPOR Report Assessing Real-World Data From Electronic ... [https://www.sciencedirect.com/science/article/pii/S109830152400069X]
- 103. Data Visualization & Dashboard Development [https://kmkconsultinginc.com/solutions/heor-rwe/real-world-evidence-data-visualization/data-visualization-dashboard-development/]
- 104. FDA Real-World Evidence: What Does It Really Mean and ... [https://namsa.com/resources/blog/fda-real-world-evidence/]
- 105. A Review of the Importance and Relevance of Real-World ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12400973/]
- 106. Regulation HTA 2025 : JCA and industrial impacts [https://www.sneci.com/en/regulation-hta-2025-jca-and-industrial-impacts/]
- 107. Evolving RWE Under IRA & JCA: Implications for Asia's HTA Standards [https://www.ispor.org/conferences-education/event/2025/09/03/default-calendar/evolving-rwe-standards-under-ira---jca--implications-for-asias-hta]
- 108. Real-World Evidence & AI in EU's Joint Clinical ... [https://wlcus.com/value_rwe_and_eu_jca/]
- 109. Harnessing RWE for EU Joint Clinical Assessments [https://lumanity.com/perspectives/harnessing-real-world-evidence-for-european-joint-clinical-assessments/]
- 110. Joint Clinical Assessment and RWE: Navigating the Process [https://clarivate.com/life-sciences-healthcare/blog/navigating-joint-clinical-assessment-and-the-role-of-rwe-in-the-new-process/]
- 111. Increasing the use of RWE : Key European initiatives for 2025 [https://www.linkedin.com/pulse/increasing-use-rwe-key-european-initiatives-2025-h4cve]