Validating Mixed Treatment Comparisons: A Framework for Confirming MTC Results with Direct Evidence
This article provides a comprehensive guide for researchers and drug development professionals on the critical process of validating Mixed Treatment Comparison (MTC) and Network Meta-Analysis (NMA) results against direct evidence.
Validating Mixed Treatment Comparisons: A Framework for Confirming MTC Results with Direct Evidence
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the critical process of validating Mixed Treatment Comparison (MTC) and Network Meta-Analysis (NMA) results against direct evidence. It covers foundational concepts of MTC, explores key methodological approaches for both fixed-effect and random-effects models, and details techniques for detecting and resolving statistical inconsistency within evidence networks. The content further examines comparative frameworks for assessing MTC validity and discusses the practical acceptance of these analyses by Health Technology Assessment (HTA) bodies. By synthesizing current methodologies and good research practices, this resource aims to enhance the reliability and credibility of indirect treatment comparisons in biomedical research.
The What and Why of Mixed Treatment Comparisons: Foundations for Validation
Network Meta-Analysis (NMA), also known as Mixed Treatment Comparison (MTC), represents an advanced statistical methodology that synthesizes evidence from multiple clinical trials to compare three or more interventions simultaneously within a single, coherent analytical framework [1] [2]. This approach represents a significant evolution beyond traditional pairwise meta-analysis by integrating both direct evidence (from head-to-head trials) and indirect evidence (estimated through a common comparator) to derive comprehensive treatment effect estimates across all competing interventions [3] [4]. The fundamental objective of MTC/NMA is to generate an internally consistent set of relative effect estimates for all treatment comparisons while respecting the randomization within the original trials [5]. This methodology has become increasingly valuable to clinicians, researchers, and healthcare decision-makers who need to determine the most effective interventions among multiple options, especially when direct comparison evidence is limited or nonexistent [1] [2].
The development of MTC/NMA methodology has progressed through several key stages. The initial foundation was laid with the introduction of adjusted indirect treatment comparisons by Bucher et al. in 1997, which provided a method for comparing interventions A and C through a common comparator B [1]. This was subsequently expanded by Lumley, who developed techniques for indirect comparisons utilizing multiple common comparators, introducing the concept of "incoherence" (later termed inconsistency) to measure disagreement between different evidence sources [1]. The most sophisticated methodological framework was established by Lu and Ades, who formalized mixed treatment comparison meta-analysis within a Bayesian framework, enabling simultaneous inference regarding all treatments and providing probability estimates for treatment rankings [3] [1]. This evolution has transformed evidence synthesis by allowing for more comprehensive and precise comparisons of multiple competing healthcare interventions.
Fundamental Concepts and Methodological Framework
Key Terminology and Definitions
Table 1: Essential Terminology in Network Meta-Analysis
| Term | Definition |
|---|---|
| Direct Treatment Comparison | Comparison of two interventions using studies that directly compare them in head-to-head trials [1]. |
| Indirect Treatment Comparison | Estimate derived using separate comparisons of two interventions against a common comparator [1]. |
| Network Meta-Analysis (NMA) | Simultaneous comparison of three or more interventions incorporating both direct and indirect evidence [1] [4]. |
| Mixed Treatment Comparison (MTC) | Synonym for NMA; specifically refers to networks where both direct and indirect evidence inform effect estimates [1]. |
| Transitivity | The core assumption that different sets of randomized trials are similar, on average, in all important factors other than the intervention comparison being made [4]. |
| Consistency | Statistical agreement between direct and indirect evidence for the same treatment comparison [6] [4]. |
| Inconsistency | Statistical disagreement between direct and indirect evidence for the same treatment comparison [6] [7]. |
Statistical Foundation and Evidence Structures
The statistical foundation of MTC/NMA relies on the principle that indirect comparisons can be mathematically derived from direct evidence. In a simple three-treatment scenario with interventions A, B, and C, where direct evidence exists for A vs. B and A vs. C, the indirect estimate for B vs. C can be calculated as the difference between the direct estimates: δBC = δAC - δAB, where δ represents the treatment effect [4]. This relationship preserves the within-trial randomization and forms the basis for more complex network structures. When four or more interventions are involved, indirect estimates can be derived through multiple pathways, with the only requirement that interventions are "connected" within the evidence network [4].
MTC/NMA can be implemented using both frequentist and Bayesian statistical frameworks, with the latter being particularly common in applied research [1]. Bayesian approaches typically employ Markov chain Monte Carlo (MCMC) methods implemented in software like WinBUGS, and allow for the estimation of posterior probability distributions for all treatment effects and rankings [3]. These models can incorporate both fixed-effect and random-effects assumptions, with random-effects models accounting for heterogeneity in treatment effects across studies by assuming that the true effects come from a common distribution [3] [6]. The Bayesian framework also facilitates the calculation of ranking probabilities for each treatment, indicating the probability that an intervention is the best, second best, etc., for a given outcome [1] [2].
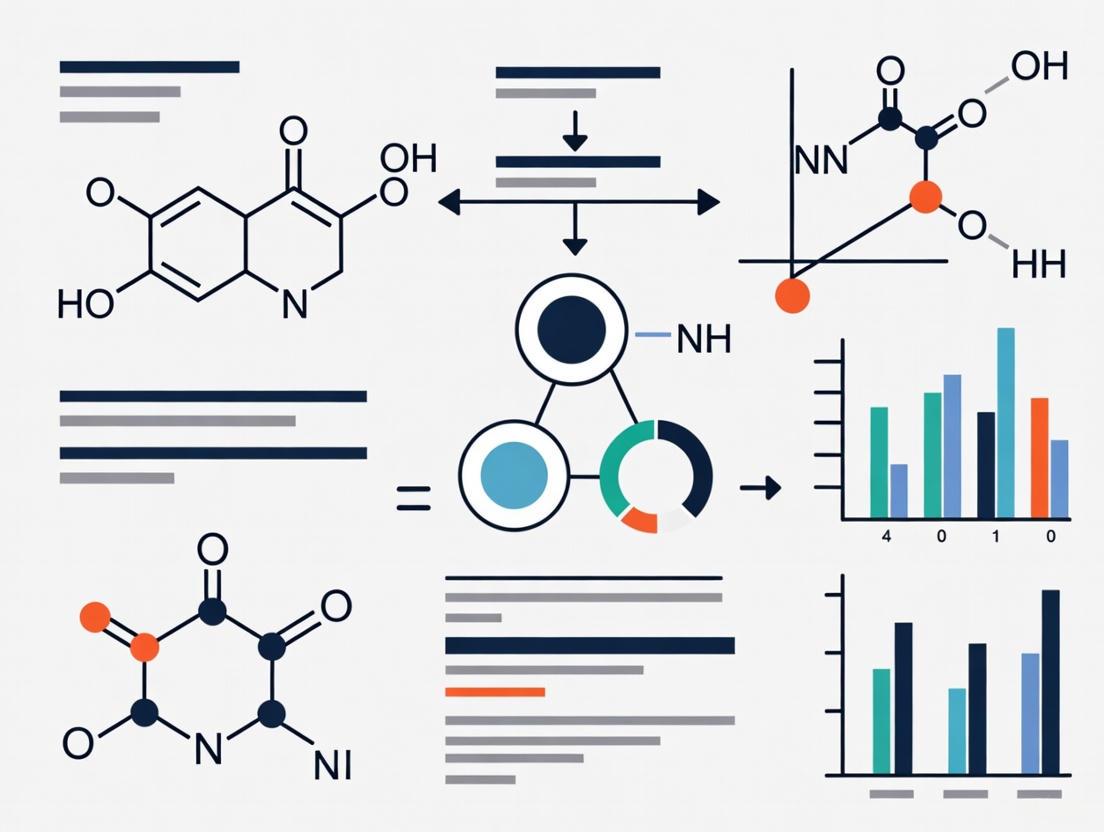
Figure 1: Network Diagram Showing Direct and Indirect Evidence Pathways. Solid lines represent direct evidence from head-to-head trials, while dashed lines represent indirect evidence pathways derived through common comparators.
Core Assumptions: Transitivity and Consistency
The Transitivity Assumption
Transitivity forms the fundamental conceptual assumption underlying the validity of indirect comparisons and MTC/NMA [4]. This assumption requires that the different sets of randomized trials included in the network are similar, on average, in all important factors that may modify treatment effects [4]. In practical terms, transitivity implies that we could potentially imagine a three-arm trial comparing A, B, and C that would yield similar results to what we obtain by combining separate A vs. B and A vs. C trials [6]. Violations of transitivity occur when study characteristics that modify treatment effects differ systematically across the various direct comparisons in the network.
Several factors can threaten the transitivity assumption, including differences in patient characteristics (e.g., disease severity, age, comorbidities), intervention modalities (e.g., dosage, administration route, treatment duration), study methodologies (e.g., blinding, outcome assessment, follow-up duration), or contextual factors (e.g., standard care, publication year, setting) across trials comparing different interventions [6]. For example, if trials comparing A vs. B were conducted in severe disease populations while trials comparing A vs. C were conducted in mild disease populations, and disease severity modifies treatment effects, the transitivity assumption would be violated. Assessing transitivity requires careful examination of the distribution of potential effect modifiers across the different direct comparisons in the network [4].
Consistency and Inconsistency
Consistency refers to the statistical agreement between direct and indirect evidence for the same treatment comparison, representing the statistical manifestation of the transitivity assumption [6] [4]. When both direct and indirect evidence exist for a particular comparison, consistency implies that these different sources of evidence provide similar estimates of the treatment effect. Inconsistency (sometimes termed incoherence) occurs when direct and indirect evidence for the same comparison disagree beyond what would be expected by chance alone [6] [7]. The presence of significant inconsistency threatens the validity of the network meta-analysis and suggests potential violation of the transitivity assumption or other methodological issues.
Methodologists have identified different types of inconsistency in network meta-analyses. Loop inconsistency refers to disagreement between different sources of evidence within closed loops of the network, typically involving three treatments where both direct and indirect evidence exist for all comparisons [6]. Design inconsistency arises when the effect estimates differ depending on the design of the studies (e.g., two-arm trials vs. multi-arm trials) contributing to the comparison [6]. Higgins et al. have proposed that the concept of design-by-treatment interaction provides a useful general framework for investigating inconsistency, particularly when multi-arm trials are present in the evidence network [6]. This approach successfully addresses complications that arise from the presence of multi-arm trials, which complicate traditional definitions of loop inconsistency [6].
Methodological Approaches for Evaluating Consistency
Statistical Methods for Detecting Inconsistency
Table 2: Methods for Assessing Consistency in Network Meta-Analysis
| Method | Description | Application Context |
|---|---|---|
| Node-Splitting | Separates direct and indirect evidence for specific comparisons and tests for significant differences [8] [7]. | Focused assessment of inconsistency at specific comparisons; useful for pinpointing sources of disagreement. |
| Design-by-Treatment Interaction | Evaluates whether treatment effects differ across study designs (e.g., two-arm vs. multi-arm trials) [6]. | Comprehensive approach particularly valuable when network contains multi-arm trials; provides global inconsistency assessment. |
| Loop-Specific Approach | Assesses inconsistency within each closed loop of three treatments in the network [7]. | Traditional method suitable for simple networks; limited utility with multi-arm trials. |
| Net Heat Plot | Graphical tool identifying hot spots of inconsistency and influential comparisons [7]. | Visual diagnostic method for locating inconsistency sources and understanding their impact on network estimates. |
| Bayesian Inconsistency Factors | Incorporates random inconsistency factors into the model within a Bayesian framework [7]. | Sophisticated approach that quantifies and incorporates uncertainty about inconsistency in the analysis. |
Implementation of Consistency Checks
Implementing consistency checks begins with a global test of inconsistency, which assesses whether there is any detectable inconsistency anywhere in the network [7]. The design-by-treatment interaction model provides a comprehensive framework for this global assessment, testing whether treatment effects differ systematically across various study designs in the network [6]. If global inconsistency is detected, local inconsistency methods are applied to identify specific comparisons or loops where inconsistency occurs. Node-splitting methods are particularly valuable for this purpose, as they allow meta-analysts to separate direct and indirect evidence for each comparison and test whether they differ significantly [8].
The implementation of these methods requires careful consideration of statistical modeling choices. For example, in node-splitting models, different parameterizations can yield slightly different results when multi-arm trials are involved [8]. The symmetrical method assumes that both treatments in a comparison contribute to inconsistency, while asymmetrical parameterizations assume that only one of the two treatments contributes to the inconsistency [8]. Similarly, when using design-by-treatment interaction models, the definition of inconsistency degrees of freedom may vary depending on whether direct evidence from two-armed and multi-armed studies is distinguished [7]. These technical considerations highlight the importance of involving experienced statisticians in the implementation of consistency assessments.
Figure 2: Methodological Workflow for Consistency Evaluation in Network Meta-Analysis. This flowchart illustrates the systematic approach to assessing and addressing inconsistency in MTC/NMA, from initial global tests to specific resolution strategies.
Experimental Validation and Application Framework
Case Study: Nutrition Labelling Interventions
A comprehensive network meta-analysis by Song et al. (2021) demonstrates the practical application of MTC methodology to evaluate the impact of different nutrition labelling schemes on consumers' purchasing behavior [9]. This analysis incorporated 156 studies (including 101 randomized controlled trials and 55 non-randomized studies) comparing multiple front-of-package labelling interventions, including traffic light labelling (TLS), Nutri-Score (NS), nutrient warnings (NW), and health warnings (HW) [9]. The researchers performed both direct pairwise meta-analyses and network meta-analyses to synthesize the evidence, allowing for comparison of results from different methodological approaches.
The analysis revealed important differences in intervention effectiveness that informed policy recommendations. The study found that all labelling schemes were associated with improved consumer choices, but with different strengths: colour-coded labels (TLS and NS) performed better in promoting the purchase of more healthful products, while warning labels (NW and HW) were more effective in discouraging unhealthful purchasing behavior [9]. The network meta-analysis allowed for simultaneous comparison of all labelling types, even those that had not been directly compared in primary studies, providing a comprehensive evidence base for policy decisions. The researchers assessed consistency between direct and indirect evidence and explored potential effect modifiers, such as study setting (real-world vs. laboratory) and outcome measurement, to validate the transitivity assumption [9].
The Scientist's Toolkit: Essential Reagents and Methodological Solutions
Table 3: Essential Methodological Tools for MTC/NMA Implementation
| Tool Category | Specific Solutions | Function and Application |
|---|---|---|
| Statistical Software | WinBUGS/OpenBUGS | Bayesian analysis using MCMC methods; implements models described by Lu & Ades [3]. |
| R packages (gemtc, netmeta) | Frequentist and Bayesian approaches; comprehensive NMA implementation [7]. | |
| Stata NMA modules | Statistical implementation for network meta-analysis and inconsistency assessment. | |
| Consistency Assessment | Node-splitting models | Direct evaluation of inconsistency between direct and indirect evidence [8]. |
| Design-by-treatment interaction | Framework for inconsistency assessment addressing multi-arm trials [6]. | |
| Net heat plot | Graphical inconsistency localization and driver identification [7]. | |
| Quality Assessment | GRADE for NMA | Structured approach for rating confidence in network estimates [10] [2]. |
| Risk of Bias tools | Study-level methodological quality assessment (e.g., Cochrane RoB tool). | |
| Visualization | Network diagrams | Evidence structure representation with nodes and edges [4]. |
| Rankograms/SUCRA | Graphical presentation of treatment ranking probabilities [1] [2]. | |
| 3,6-Dihydroxyflavone | 3,6-Dihydroxyflavone|High-Purity Research Compound | |
| 6-Methoxywogonin | 6-Methoxywogonin, CAS:3162-45-6, MF:C17H14O6, MW:314.29 g/mol | Chemical Reagent |
Protocol for Validating MTC Results with Direct Evidence
Define the Network Geometry: Create a network diagram specifying all treatments and direct comparisons, identifying all closed loops where both direct and indirect evidence exist [4] [7]. Document the number of studies contributing to each direct comparison and note potential systematic differences in study characteristics across comparisons.
Assess Transitivity Assumption: Systematically evaluate the distribution of potential effect modifiers across the different direct comparisons in the network [4]. Consider patient characteristics, intervention modalities, outcome definitions, study methodologies, and contextual factors that might modify treatment effects.
Implement Consistency Models: Apply both global and local inconsistency tests using appropriate statistical methods [6] [7]. For networks with multi-arm trials, prioritize design-by-treatment interaction models over simple loop-based approaches [6]. Use node-splitting for focused assessment of specific comparisons of interest.
Conduct Sensitivity Analyses: Perform analyses excluding studies with high risk of bias, different study designs, or specific populations to assess the robustness of findings to these factors [4] [5]. Explore the impact of alternative statistical models (fixed vs. random effects) on consistency assessments.
Interpret and Resolve Inconsistency: If significant inconsistency is detected, investigate potential causes through subgroup analyses or meta-regression [4] [7]. Consider excluding studies contributing to inconsistency if justified by methodological concerns, and report any remaining inconsistency with appropriate caveats for interpretation.
This systematic approach to validation ensures that MTC/NMA results are rigorously evaluated against direct evidence, strengthening the credibility of conclusions derived from mixed treatment comparisons. When properly implemented with careful attention to consistency assessment, MTC/NMA provides a powerful tool for comparative effectiveness research that respects the randomization in the underlying evidence while maximizing the use of all available information [2] [5].
The Critical Role of Direct Evidence in the Validation Framework
Mixed treatment comparison (MTC), more commonly known as network meta-analysis (NMA), is an advanced statistical methodology that synthesizes both direct and indirect evidence to estimate the comparative efficacy and safety of multiple interventions [11]. In an MTC, the term "mixed" refers to the analytical combination of direct evidence (from head-to-head randomized controlled trials) and indirect evidence (from trials that compare interventions of interest via a common comparator) within a single evidence network [12] [11]. This approach allows for the comparison of multiple treatments simultaneously, even when some pairs of treatments have never been directly compared in clinical trials.
While MTCs provide a powerful tool for comparative effectiveness research, they rely on a critical assumption: consistency between direct and indirect evidence [12] [13]. When this assumption is violated—a situation termed "incoherence" or "inconsistency"—the validity of MTC results becomes questionable [12]. Incoherence occurs when estimates based on direct comparisons meaningfully differ from those derived through indirect comparisons [12]. This fundamental vulnerability necessitates a robust validation framework centered on direct evidence, which serves as the benchmark for assessing the reliability of mixed treatment comparisons.
The Critical Role of Direct Evidence in Validation
Direct Evidence as the Validation Gold Standard
Direct evidence, obtained from well-designed randomized controlled trials (RCTs) that compare treatments head-to-head, represents the gold standard for establishing comparative efficacy in clinical research [14]. In the context of MTC validation, direct evidence provides the reference point against which mixed treatment estimates are evaluated. This validation process is essential because MTCs incorporate additional methodological assumptions that extend beyond those required for standard pairwise meta-analyses [12].
The integration of direct evidence into a validation framework serves several critical functions. First, it enables the detection of statistical inconsistency within an evidence network. Second, it provides a mechanism for identifying potential effect modifiers that may vary across studies and influence treatment comparisons. Third, it enhances the robustness and credibility of MTC findings for healthcare decision-makers, including regulatory agencies and health technology assessment bodies [14].
Methods for Validating MTCs with Direct Evidence
Inconsistency Detection and Analysis
A fundamental approach to validating MTC results involves formally testing for inconsistency between direct and indirect evidence. Statistical methods for inconsistency detection include:
- Node-splitting techniques: Separately estimating treatment effects from direct and indirect evidence for specific comparisons and testing for significant differences [13]
- Design-by-treatment interaction models: Assessing whether treatment effects vary by trial design or other study-level characteristics
- Back-calculation methods: Comparing direct estimates from trials with those derived from the network meta-analysis model
When direct and indirect evidence demonstrate consistency, confidence in MTC findings increases substantially. However, when incoherence is detected—where direct comparison estimates fall outside the confidence intervals of corresponding indirect comparison estimates—investigators must explore potential explanations before relying on the mixed treatment estimates [12].
Hierarchical Validation Approach
A comprehensive validation framework for MTCs employs a hierarchical approach across three levels:
- Study-level validation: Critical appraisal of individual RCTs included in the evidence network for risk of bias, methodological quality, and relevance to the research question [12]
- Comparison-level validation: Assessment of transitivity and similarity assumptions across studies contributing to each treatment comparison [12]
- Network-level validation: Evaluation of the overall consistency of the evidence network and exploration of potential sources of heterogeneity
This multi-layered approach ensures that validation occurs at every stage of the MTC process, with direct evidence serving as the anchor point at each level.
Consequences of Inadequate Validation
Failure to properly validate MTC findings against direct evidence can lead to misleading conclusions and potentially harmful healthcare decisions. Empirical studies have demonstrated that discrepancies between direct and indirect evidence are not merely theoretical concerns. For instance, in a comparison of 12 antidepressants, conclusions based solely on indirect evidence were substantially different from those based on direct comparisons [12]. Similarly, in a network meta-analysis of opioid detoxification treatments, MTC techniques produced narrower confidence intervals than direct comparisons alone, creating an illusion of precision that could mask important uncertainties [12].
Experimental Protocols for MTC Validation
Protocol for Consistency Assessment
Objective: To statistically evaluate the consistency between direct and indirect evidence for each treatment comparison within a network meta-analysis.
Methodology:
- Identify all treatment comparisons with both direct and indirect evidence
- Extract or calculate effect estimates and measures of precision for each direct comparison
- Derive indirect estimates using the Bucher method or similar approaches [14]
- Statistically compare direct and indirect estimates using node-split models or similar techniques
- Quantify the degree of inconsistency using appropriate statistical measures (e.g., inconsistency factors, p-values)
- Investigate potential clinical or methodological explanations for any detected inconsistencies
This protocol enables researchers to identify specific comparisons where direct and indirect evidence diverge, guiding further investigation into potential causes.
Protocol for Sensitivity Analysis with Direct Evidence
Objective: To assess the robustness of MTC findings by comparing results from different evidence configurations.
Methodology:
- Conduct the primary analysis including all available evidence (both direct and indirect)
- Perform sensitivity analyses restricted to:
- Only direct evidence where available
- Evidence from studies with low risk of bias
- Studies with similar patient populations and methodologies
- Compare effect estimates, ranking probabilities, and between-study heterogeneity across different analyses
- Evaluate whether conclusions regarding comparative efficacy remain consistent across sensitivity analyses
This protocol helps determine whether MTC findings are unduly influenced by specific studies or types of evidence, with direct evidence serving as a key benchmark.
Signaling Pathways and Methodological Workflows
The following diagram illustrates the core methodological workflow for validating mixed treatment comparisons through integration with direct evidence:
MTC Validation Workflow
This workflow demonstrates how direct evidence serves as the critical validation checkpoint within the MTC analytical process. The consistency assessment phase represents the core validation mechanism where direct and indirect evidence are formally compared.
Comparative Analysis of MTC Validation Methods
The table below summarizes the key methodological approaches for validating mixed treatment comparisons using direct evidence:
Table 1: Methods for Validating Mixed Treatment Comparisons with Direct Evidence
| Validation Method | Application Context | Key Strengths | Key Limitations | Data Requirements |
|---|---|---|---|---|
| Node-Splitting [13] | Local inconsistency detection for specific comparisons | Pinpoints exact location of inconsistency in network | Limited power in sparse networks | Both direct and indirect evidence for specific comparisons |
| Design-by-Treatment Interaction [13] | Global inconsistency assessment across entire network | Comprehensive network evaluation | Does not identify specific inconsistent comparisons | Network with varied study designs |
| Bucher Method [14] | Simple indirect comparisons and validation | Simple implementation and interpretation | Limited to simple indirect comparisons | Two treatments vs. common comparator |
| Sensitivity Analysis [12] | Robustness assessment of MTC findings | Assesses impact of evidence sources on conclusions | Does not provide formal statistical tests | Multiple evidence configurations |
The Scientist's Toolkit: Essential Reagents for MTC Validation
Table 2: Key Methodological Tools for MTC Validation
| Tool/Technique | Primary Function | Application in Validation |
|---|---|---|
| Network Meta-Analysis Software (e.g., R, WinBUGS) [13] | Statistical implementation of MTC models | Provides specialized routines for inconsistency detection and analysis |
| The Bucher Method [14] | Simple indirect treatment comparisons | Creates benchmark indirect estimates for comparison with direct evidence |
| Risk of Bias Tools (e.g., Cochrane RoB) [12] | Quality assessment of individual studies | Identifies methodological limitations that may explain inconsistency |
| Node-Split Models [13] | Statistical detection of local inconsistency | Formally tests differences between direct and indirect evidence |
| Network Graphs | Visualization of evidence structure | Identifies gaps in direct evidence and potential violations of similarity |
| T-1330 | T-1330, CAS:106461-41-0, MF:C22H27N5O2, MW:393.5 g/mol | Chemical Reagent |
| 2-Hydroxy Atorvastatin Lactone-d5 | 2-Hydroxy Atorvastatin Lactone-d5, CAS:265989-50-2, MF:C33H33FN2O5, MW:561.7 g/mol | Chemical Reagent |
Direct evidence serves as the cornerstone of validation for mixed treatment comparisons, providing an essential benchmark against which the reliability of complex evidence networks is assessed. The integration of direct evidence within a comprehensive validation framework enables researchers to detect inconsistencies, investigate their sources, and enhance the credibility of MTC findings. As health technology assessment agencies and regulatory bodies increasingly consider MTCs in their decision-making processes [14], robust validation methodologies centered on direct evidence become increasingly critical. Future methodological developments should focus on enhancing inconsistency detection methods, standardizing validation reporting, and establishing clearer guidelines for when MTC findings can be considered sufficiently validated for healthcare decision-making.
In evidence-based medicine, Mixed Treatment Comparison (MTC), also known as Network Meta-Analysis, has emerged as a powerful statistical tool for comparing the efficacy of multiple treatments simultaneously, even when direct head-to-head trials are unavailable [5] [15]. This methodology allows for the integration of both direct and indirect evidence into a single, coherent analysis, facilitating complex treatment decisions and supporting health technology assessments [14] [15]. The validity of any MTC, however, rests upon three fundamental and interrelated core assumptions: similarity, homogeneity, and consistency. Understanding and verifying these assumptions is paramount for researchers, scientists, and drug development professionals to ensure the reliability of MTC results, particularly when confirming findings with direct evidence research.
The Triad of Core Assumptions
The foundational pillars of MTC define the conditions under which different clinical trials can be legitimately combined and compared within a network. The following table summarizes these core concepts.
Table 1: Core Assumptions of Mixed Treatment Comparisons
| Assumption | Definition | Primary Concern | Key Question for Researchers |
|---|---|---|---|
| Similarity | The assumption that different trials are sufficiently similar in their study-level characteristics (moderators) to permit comparison [16]. | Transitivity across the network | Are the trials comparing different treatments similar enough in terms of patient populations, trial design, and outcomes measurement? [16] |
| Homogeneity | The assumption that trials estimating the same treatment comparison are measuring the same underlying treatment effect [15] [16]. | Variability within pairwise comparisons | Is the treatment effect for a specific head-to-head comparison similar across all trials that study it? |
| Consistency | The assumption that direct evidence (from head-to-head trials) and indirect evidence (derived via a common comparator) are in agreement [15] [16]. | Coherence between direct and indirect evidence | For the same treatment comparison, do the direct and indirect estimates provide the same result? |
Similarity: The Foundation of Transitivity
The similarity assumption forms the logical basis for building a connected network of trials. It requires that the trials included for different treatment comparisons are sufficiently similar in their moderating factors to allow for a fair comparison. In practice, this means that the relative treatment effects being studied should not be influenced by systematic differences in trial design or patient characteristics across the network [16]. For instance, an MTC would be violated if all trials comparing Treatment A to Treatment B were conducted in a population with severe disease, while all trials comparing Treatment A to Treatment C were conducted in a population with mild disease.
Methodological Protocol for Assessing Similarity:
- Identify Potential Effect Modifiers: Systematically identify and record clinical and methodological variables that could modify the treatment effect. These commonly include patient demographics (e.g., age, disease severity, comorbidities), trial characteristics (e.g., duration, blinding, setting), and definitions of outcomes.
- Evaluate Distribution of Modifiers: Examine the distribution of these effect modifiers across the different treatment comparisons in the network. This can be done through summary tables or visual inspection of the study-level characteristics grouped by comparison.
- Statistical Evaluation: While there is no single statistical test for similarity, its violation can contribute to inconsistency. Exploring the distribution of modifiers is a key step in diagnosing the root cause of any inconsistency detected in the network.
Homogeneity: Consistency Within Comparisons
Homogeneity is directly analogous to the assumption underlying a standard pairwise meta-analysis. It posits that the true treatment effect is the same across all trials that directly compare the same two interventions. Significant heterogeneity suggests that the studies are not estimating a single common effect, which may be due to clinical or methodological diversity among the trials [15].
Methodological Protocol for Assessing Homogeneity:
- Visual Inspection: Use forest plots for each direct pairwise comparison to visually assess the overlap of confidence intervals and the point estimates of individual studies.
- Statistical Tests: Calculate the I² statistic and Cochran's Q for each direct comparison. The I² statistic describes the percentage of total variation across studies that is due to heterogeneity rather than chance. An I² value greater than 50% may be considered substantial heterogeneity.
- Subgroup Analysis and Meta-Regression: If significant heterogeneity is detected, researchers can use subgroup analysis or meta-regression to explore the influence of specific study-level covariates on the observed treatment effects.
Consistency: The Harmony of Direct and Indirect Evidence
The consistency assumption is unique to the MTC framework and is critical for its validity. It requires that the direct estimate of a treatment effect (from head-to-head trials) is consistent with the indirect estimate of the same effect (obtained through a common comparator) [15] [16]. When this assumption holds, the combined evidence from the network is coherent.
Methodological Protocol for Assessing Consistency:
- Design-by-Treatment Interaction Test: A global test that assesses inconsistency across the entire network model. A significant result suggests a violation of the consistency assumption somewhere in the network.
- Node-Splitting Method: This is a local test for inconsistency. It separately calculates the direct, indirect, and MTC estimates for a specific treatment comparison and then tests for a significant difference between the direct and indirect estimates [5].
- Bucher's Method: For a simple closed loop of three treatments (A, B, C), this method provides a statistical test to compare the direct estimate of A vs. B with the indirect estimate obtained via C [5] [14]. The analysis of an overview of treatments for childhood nocturnal enuresis found that summary estimates based on fixed-effect meta-analyses were "highly inconsistent," whereas those based on random-effects models were consistent [5].
The logical relationships between evidence types and the core assumptions that govern them can be visualized in the following workflow.
The Scientist's Toolkit: Essential Reagents for MTC Analysis
Conducting a robust MTC requires a suite of statistical and computational tools. The following table details key "research reagents" and their functions in the analytical process.
Table 2: Essential Reagents for MTC Analysis
| Tool/Reagent | Type | Primary Function | Application in MTC |
|---|---|---|---|
| WinBUGS/OpenBUGS | Software | Bayesian statistical analysis using MCMC simulation. | The historical software of choice for fitting Bayesian MTC models, as used in foundational methodology papers [3] [16]. |
| R (with packages) | Software/Programming Language | Statistical computing and graphics. | Modern, flexible environment for conducting MTCs. Packages like gemtc and pcnetmeta facilitate network meta-analysis and inconsistency testing. |
| PRISMA-NMA Guideline | Reporting Guideline | A checklist and framework for reporting. | Ensures transparent and complete reporting of systematic reviews and meta-analyses incorporating network meta-analyses [15]. |
| Node-Split Model | Statistical Model | A local test for inconsistency. | Separately estimates the direct and indirect evidence for a specific comparison within the network to test their consistency [5]. |
| Markov Chain Monte Carlo (MCMC) | Computational Algorithm | A method for sampling from a probability distribution. | Used in Bayesian MTC to estimate the posterior distributions of model parameters, such as relative treatment effects [16]. |
| 5-Nitrouracil | 5-Nitrouracil CAS 611-08-5|Research Chemical | Bench Chemicals | |
| Rsu 1164 | Rsu 1164, CAS:105027-77-8, MF:C10H16N4O3, MW:240.26 g/mol | Chemical Reagent | Bench Chemicals |
The assumptions of similarity, homogeneity, and consistency are not mere statistical formalities; they are the critical safeguards that ensure the validity and interpretability of Mixed Treatment Comparisons. For drug development professionals and researchers, a thorough investigation of these assumptions is a non-negotiable component of the MTC process. This involves meticulous study design, comprehensive data collection, and the application of robust statistical methods to evaluate these assumptions. By rigorously confirming that these core principles are upheld, scientists can have greater confidence in the results of an MTC, especially when using them to triangulate findings from direct evidence research, ultimately leading to more reliable and informed healthcare decisions.
In an era of rapidly expanding therapeutic options, clinicians and healthcare decision-makers are consistently faced with a fundamental challenge: determining the optimal treatment among multiple alternatives without adequate direct comparative evidence. Mixed Treatment Comparison (MTC), also known as network meta-analysis, has emerged as a crucial methodological framework that addresses this evidence gap by enabling the simultaneous comparison of multiple interventions, even when direct head-to-head trials are absent or limited [17]. This advanced analytical approach represents a significant evolution beyond traditional pairwise meta-analysis, allowing researchers to synthesize both direct evidence (from trials comparing treatments directly) and indirect evidence (from trials connected through common comparators) within a unified statistical model [18] [19].
The proliferation of treatment options, particularly in complex disease areas like oncology and rare diseases, has intensified the need for sophisticated comparative effectiveness methodologies. As noted by the ISPOR Task Force on Indirect Treatment Comparisons, "Evidence-based health-care decision making requires comparisons of all relevant competing interventions" [19]. MTC fulfills this need by creating a connected network of evidence where interventions can be compared through both direct and indirect pathways, thereby synthesizing a greater share of the available evidence than traditional meta-analytic approaches [17] [19]. This comprehensive synthesis is particularly valuable for health technology assessment (HTA) agencies and formulary committees tasked with making coverage decisions amidst constrained healthcare resources.
Fundamental Methodological Framework of MTC
Core Concepts and Terminology
MTC methodology operates on several fundamental concepts that form the backbone of its analytical approach:
Network Meta-Analysis: A generic term defining the simultaneous synthesis of evidence for all pairwise comparisons across more than two interventions [17]. This approach creates a connected network where every intervention can be compared to every other intervention through direct or indirect pathways.
Closed Loop: A network structure where at least one pair of treatments has both direct evidence (from trials directly comparing them) and indirect evidence (through connected pathways via common comparators) [17]. For example, if treatment A has been compared to B in some trials, B to C in others, and A to C in yet others, the AC comparison forms a closed loop with both direct and indirect evidence.
Indirect Treatment Comparison (ITC): The estimation of relative treatment effects between two interventions that have not been directly compared in randomized trials but have been connected through a common comparator [18] [14]. The simplest form of ITC is the anchored indirect comparison described by Bucher et al., which allows comparison of interventions that have been evaluated against a common control in separate trials [17].
Bayesian Framework: A statistical approach commonly used for MTC that combines prior probability distributions (reflecting prior belief about possible values of model parameters) with likelihood distributions based on observed data to obtain posterior probability distributions [17]. This framework naturally accommodates complex network structures and provides intuitive probabilistic interpretations of results.
Key Statistical Assumptions
The validity of MTC analyses depends on several critical statistical assumptions that must be carefully evaluated:
Similarity Assumption: Trials included in the network must be sufficiently similar in terms of interventions, patient populations, outcome definitions, and study design characteristics to allow meaningful comparison [18]. Violations of this assumption can introduce bias and compromise the validity of results.
Homogeneity Assumption: For each pairwise comparison, the treatment effect should be reasonably consistent across trials (statistical homogeneity) [18]. When heterogeneity is present, random-effects models can incorporate between-study variance, though this does not explain the sources of heterogeneity.
Consistency Assumption: The direct and indirect evidence for a particular treatment comparison should be in agreement [19]. Inconsistency between direct and indirect evidence suggests potential effect modifiers or methodological issues within the network.
Table 1: Key Methodological Assumptions in Mixed Treatment Comparisons
| Assumption | Definition | Implications for Validity |
|---|---|---|
| Similarity | Trials are sufficiently comparable in design, patients, interventions, and outcomes | Ensures comparisons between trials are clinically meaningful |
| Homogeneity | Treatment effects are consistent across studies for each pairwise comparison | Affects choice between fixed-effect and random-effects models |
| Consistency | Agreement between direct and indirect evidence for the same comparison | Violations suggest potential bias or effect modification |
Experimental and Analytical Protocols
Network Meta-Analysis Workflow
The implementation of MTC follows a structured workflow that ensures methodological rigor and transparency. The following diagram illustrates the key stages in conducting a network meta-analysis:
Detailed Methodological Approaches
Bayesian Implementation
The Bayesian framework for MTC involves specifying prior distributions for model parameters and updating these priors with observed data to obtain posterior distributions [17]. This approach typically utilizes Markov Chain Monte Carlo (MCMC) methods implemented in specialized software such as WinBUGS, OpenBUGS, or JAGS. The Bayesian approach offers several advantages, including natural handling of complex random-effects structures, straightforward probability statements for treatment rankings, and flexible accommodation of various data types. Model convergence must be carefully assessed using diagnostic statistics such as Gelman-Rubin statistics, and posterior distributions should be based on sufficient MCMC iterations after convergence is achieved.
Frequentist Implementation
Frequentist approaches to MTC, such as Lumley's network meta-analysis method, utilize mixed models to combine direct and indirect evidence when at least one closed loop exists in the evidence network [17]. These methods often employ generalized linear mixed models and can be implemented in standard statistical software such as R or SAS. Frequentist approaches provide maximum likelihood estimates of treatment effects and confidence intervals based on asymptotic normality assumptions. While potentially more familiar to many researchers, they may be less flexible than Bayesian methods for handling complex random-effects structures or making probabilistic statements about treatment rankings.
Validation Through Comparison with Direct Evidence
A critical component of MTC methodology involves confirming results through comparison with direct evidence when available. This validation process includes:
Consistency Testing: Statistical evaluation of agreement between direct and indirect evidence for treatment comparisons where both types of evidence exist [19]. Methods for assessing consistency include node-splitting approaches, which separate direct and indirect evidence for specific comparisons, and design-by-treatment interaction models.
Empirical Evaluation: Comparison of MTC results with findings from subsequent direct comparative trials when they become available. This real-world validation provides important evidence regarding the predictive performance of MTC in various clinical contexts.
Sensitivity Analyses: Conducting analyses under different statistical assumptions, inclusion criteria, or model specifications to assess the robustness of MTC findings. These analyses help determine whether conclusions are sensitive to methodological choices or specific studies in the network.
Table 2: MTC Validation Techniques and Their Applications
| Validation Technique | Methodological Approach | Interpretation |
|---|---|---|
| Node-Splitting | Separates direct and indirect evidence for specific comparisons | Inconsistency suggests potential bias or effect modification |
| Design-by-Treatment Interaction Model | Global test for consistency across the entire network | Significant p-value indicates overall inconsistency |
| Comparison with Direct Evidence | Empirical comparison with head-to-head trials when available | Assesses predictive validity of MTC methods |
| Meta-Regression | Adjusts for trial-level covariates | Reduces heterogeneity and inconsistency when effect modifiers are identified |
Comparative Analysis of Indirect Treatment Comparison Methods
The methodological landscape for indirect treatment comparisons has expanded significantly, with multiple techniques now available for different evidence scenarios. A 2024 systematic literature review identified seven distinct ITC techniques reported in the literature, with varying frequencies of application [14]:
Table 3: Indirect Treatment Comparison Techniques and Applications
| ITC Technique | Frequency of Description | Key Applications | Data Requirements |
|---|---|---|---|
| Network Meta-Analysis (NMA) | 79.5% | Connected networks of RCTs with multiple interventions | Aggregate data from multiple trials |
| Matching-Adjusted Indirect Comparison (MAIC) | 30.1% | Single-arm studies with heterogeneous populations | Individual patient data (IPD) for index treatment |
| Network Meta-Regression (NMR) | 24.7% | Networks with suspected effect modifiers | Aggregate data plus trial-level covariates |
| Bucher Method | 23.3% | Simple connected networks with common comparator | Aggregate data from two trials with common comparator |
| Simulated Treatment Comparison (STC) | 21.9% | Single-arm studies with limited comparator data | IPD for index treatment, aggregate for comparator |
| Propensity Score Matching (PSM) | 4.1% | Non-randomized comparisons with limited RCT data | IPD for all treatment groups |
| Inverse Probability of Treatment Weighting (IPTW) | 4.1% | Non-randomized comparisons with confounding | IPD for all treatment groups |
Selection Criteria for ITC Methods
The appropriate choice of ITC technique depends on several factors related to the available evidence base and research question:
Network Connectivity: The presence of a connected network where all treatments are linked through direct or indirect pathways favors NMA approaches. Disconnected networks may require population-adjusted methods like MAIC or STC [14].
Availability of Individual Patient Data (IPD): When IPD is available for at least one treatment, MAIC and STC become feasible options. These methods can adjust for cross-trial differences in patient characteristics through reweighting or matching techniques [14].
Between-Study Heterogeneity: Substantial clinical or methodological heterogeneity across studies may necessitate random-effects models or meta-regression approaches to account for between-study variability [18].
Number of Relevant Studies: Networks with limited numbers of studies may be unsuitable for complex random-effects models, requiring simpler approaches like the Bucher method for basic indirect comparisons.
Implementing MTC analyses requires familiarity with specialized statistical software and methodological resources. The following tools represent essential components of the methodological toolkit for researchers conducting mixed treatment comparisons:
Table 4: Essential Resources for MTC Implementation
| Resource Category | Specific Tools/References | Application in MTC |
|---|---|---|
| Statistical Software | WinBUGS/OpenBUGS, JAGS, R (gemtc, netmeta, pcnetmeta packages) | Bayesian and frequentist model implementation |
| Methodological Guidance | ISPOR Task Force Reports, NICE DSU Technical Support Documents | Best practices for design, analysis, and interpretation |
| Quality Assessment Tools | Cochrane Risk of Bias Tool, GRADE for NMA | Assessing validity and quality of evidence |
| Data Extraction Support | Systematic review management software (DistillerSR, Covidence) | Efficient data collection and management |
| Visualization Tools | Network graphs, rank probability plots, contribution plots | Visual representation of networks and results |
Applications in Evidence-Based Medicine: Case Examples
Oncology Applications
MTC methodologies have been particularly valuable in oncology, where rapid therapeutic advances and multiple treatment options create decision-making challenges with limited direct comparative evidence. A review of MTC applications in oncology identified six published analyses between 2006-2010 spanning various cancer types including ovarian, colorectal, breast, and non-small cell lung cancer [18]. These analyses demonstrated the ability of MTC to synthesize evidence across complex therapeutic landscapes and provide comparative effectiveness estimates for clinical decision-making.
For example, an MTC analysis in advanced breast cancer published in 2008 synthesized evidence from 172 randomized controlled trials involving 22 different interventions [18]. This comprehensive analysis allowed for simultaneous comparison of multiple treatment regimens and provided valuable insights into their relative effects on overall survival. Similarly, an MTC in ovarian cancer analyzed 60 RCTs of 120 different interventions, demonstrating the ability of these methods to handle networks of substantial complexity [18].
Confirming MTC Results with Direct Evidence
The critical test of any indirect comparison method lies in its agreement with direct evidence when it becomes available. Empirical evaluations have generally shown reasonable agreement between properly conducted MTC analyses and subsequent direct comparisons, though discrepancies can occur when key assumptions are violated.
Several studies have compared the results of indirect comparisons with direct evidence, with varying degrees of concordance. The circumstances under which MTC results align with direct evidence include:
Similar Patient Populations: When trials in the network enroll clinically similar populations with comparable baseline risk profiles [18].
Consistent Outcome Definitions: When outcome assessments, follow-up durations, and measurement approaches are consistent across trials.
Absence of Effect Modifiers: When no important treatment effect modifiers are distributed differently across the direct and indirect comparisons.
Conversely, MTC results may diverge from direct evidence when there are important differences in trial design, patient characteristics, or outcome assessments that introduce heterogeneity or inconsistency into the network.
Future Directions and Methodological Challenges
As MTC methodologies continue to evolve, several areas represent important frontiers for methodological development and application:
Individual Patient Data Network Meta-Analysis: The integration of IPD into MTC models offers potential advantages for exploring treatment-effect heterogeneity, assessing individual-level predictors of treatment response, and improving the adjustment for cross-trial differences [14].
Complex Evidence Structures: Methods for handling increasingly complex evidence networks, including multi-arm trials, combination therapies, and treatment sequences, represent an active area of methodological research.
Real-World Evidence Integration: Approaches for incorporating real-world evidence alongside randomized trial data in MTC models may enhance the generalizability and completeness of comparative effectiveness assessments.
Decision-Theoretic Framework: Enhanced methods for integrating MTC results with formal decision-analytic modeling to support healthcare resource allocation decisions.
Despite these advances, important challenges remain in the implementation and interpretation of MTC analyses. These include the need for clearer international consensus on methodological standards, improved transparency in reporting, and continued education for stakeholders involved in healthcare decision-making [14]. As the field progresses, the utility and transparency of MTC methodologies will likely predict their continued uptake by the research and clinical communities [18].
Executing and Analyzing MTCs: Statistical Methods and Good Research Practices
In the context of mixed treatment comparisons (MTCs) and network meta-analysis, the choice between fixed-effect and random-effects models is foundational, influencing the robustness and interpretation of your results when confirming findings with direct evidence. This choice determines whether you are estimating a single universal treatment effect or an average of effects that genuinely vary across studies, populations, and settings.
The distinction is philosophical as much as it is statistical. A fixed-effect model assumes that all studies in your analysis are estimating the same single, true effect size. Variations in individual study results are attributed solely to within-study sampling error. Conversely, a random-effects model assumes that the true effect size itself varies from study to study, and your analysis aims to estimate the mean of this distribution of true effects [20] [21].
This framework is critical for MTCs, which rely on indirect evidence to compare treatments. The model you select dictates how you handle heterogeneity—the variability between studies—which can arise from differences in patient populations, treatment dosages, or study methodologies. Proper model selection ensures that the uncertainty in your indirect comparisons is accurately quantified, which is essential for validating them against any available direct evidence.
Conceptual Foundation and When to Choose
Defining the Models and Their Assumptions
Your choice of model hinges on your assumptions about the data and the goals of your analysis.
Fixed-Effect Model: This model is built on the assumption that every study in your meta-analysis is functionally identical in design, methods, and patient samples, and that all are measuring the same underlying true effect [20]. Any observed differences between study results are presumed to be due entirely to chance (sampling error within studies). It answers the question: "What is the best estimate of this common effect size?"
Random-Effects Model: This model acknowledges that studies are often meaningfully dissimilar. It assumes that each study has its own true effect size, drawn from a distribution of effects [20] [21]. The model explicitly accounts for two sources of variation: the within-study sampling error (as in the fixed-effect model) and the between-study variance in true effects (often denoted as τ², or tau-squared). It answers the question: "What is the average of the varying true effects?"
Decision Framework: Which Model to Use and When
The decision should be made a priori, based on conceptual reasoning about the included studies, and not based on the observed heterogeneity after running the analysis [20] [21].
The following workflow outlines the key questions to guide your model selection:
In practice, for mixed treatment comparisons where studies often differ in design, comparator treatments, and patient characteristics, a random-effects model is frequently the more appropriate and conservative choice [15] [14]. It better accounts for the clinical and methodological diversity expected across a network of studies.
Impact on Analysis and Interpretation
Consequences for Study Weights, Estimates, and Precision
The choice of model directly impacts how studies are weighted in the meta-analysis and the resulting pooled estimate.
- Study Weights: In a fixed-effect model, weights are based almost exclusively on study precision (typically, inverse variance). Larger studies with narrower confidence intervals receive disproportionately greater weight. In a random-effects model, weights are more balanced between large and small studies because the model incorporates the between-study variance, reducing the relative dominance of very large studies [20].
- Pooled Estimate and Confidence Intervals: The random-effects model generally produces a pooled estimate with a wider confidence interval than the fixed-effect model. This is because it accounts for an additional source of uncertainty—the between-study variance [20] [21]. Consequently, a result that is statistically significant under a fixed-effect model may become non-significant under a random-effects model.
Table: Comparative Impact of Model Choice on Meta-Analysis Output
| Aspect | Fixed-Effect Model | Random-Effects Model |
|---|---|---|
| Assumed True Effects | One single true effect | A distribution of true effects |
| Source of Variance | Within-study sampling error only | Within-study + between-study variance |
| Weighting of Studies | Heavily favors larger, more precise studies | More balanced between large and small studies |
| Confidence Intervals | Narrower | Wider |
| Interpretation of Result | Estimate of the common effect | Estimate of the mean of the distribution of effects |
| Generalizability | Limited to the specific set of studied populations | More generalizable to a wider range of settings |
The Critical Role of Heterogeneity
Heterogeneity (I²) statistics quantify the proportion of total variation across studies that is due to heterogeneity rather than chance. While a high I² value might suggest a random-effects model is needed, it should not be the sole driver of your model choice. The decision must be primarily conceptual [21]. A random-effects model is the correct choice when you have reason to believe true effects differ, regardless of the calculated I² value.
A more informative approach in a random-effects framework is to report a prediction interval. While a confidence interval indicates the uncertainty around the estimated mean effect, a prediction interval estimates the range within which the true effect of a new, similar study would be expected to fall. This provides a more realistic picture of the treatment effect's variability in practice [21].
Methodological Protocols and Statistical Considerations
Experimental and Analytical Protocols
Implementing a robust meta-analysis requires a pre-specified, systematic protocol.
- Protocol Registration: The choice between fixed-effect and random-effects models should be specified in advance, ideally in a registered protocol (e.g., with PROSPERO) [20].
- Systematic Review: Conduct a comprehensive literature search following PRISMA guidelines to identify all relevant studies [15] [14]. Data extraction should be blinded and pre-specified.
- Data Extraction and Quality Assessment: Extract data in a standardized format. Assess study quality using tools like the Jadad scale to inform sensitivity analyses [15].
- Statistical Analysis:
- For Random-Effects: Choose an appropriate estimator for the between-study variance (τ²). The Restricted Maximum Likelihood (REML) and Paule-Mandel (PM) estimators are generally preferred over the older DerSimonian-Laird (DL) method, which can underestimate uncertainty with few studies [21].
- For Confidence Intervals: When using a random-effects model, the Hartung-Knapp-Sidik-Jonkman (HKSJ) method for confidence intervals is recommended as it provides better coverage when the number of studies is small [21].
- Sensitivity Analysis: It is good practice to run both fixed-effect and random-effects models and report the results of both, especially if the conclusions differ [20]. This demonstrates the robustness (or lack thereof) of your findings.
Essential Reagents for the Research Toolkit
Table: Key Methodological Tools for Meta-Analysis
| Tool or Method | Function | Considerations for Model Choice |
|---|---|---|
| PRISMA Guidelines | Ensures transparent and complete reporting of the systematic review and meta-analysis. | Mandatory for publishing; framework is independent of model. |
| Cochroke Handbook | Provides comprehensive guidance on conduct of meta-analysis. | Advocates for random-effects as a default in many clinical contexts. |
| I² Statistic | Quantifies the percentage of total variation across studies due to heterogeneity. | Descriptive tool; should not dictate model choice. |
| REML / PM Estimators | Advanced methods to estimate between-study variance (τ²) in random-effects models. | Preferred over DL for better accuracy, especially with few studies. |
| HKSJ Method | A modified method to calculate confidence intervals in random-effects meta-analysis. | Provides more robust intervals with a small number of studies. |
| Prediction Intervals | Estimates the range of true effects in future settings. | Highly recommended for random-effects to show practical implications. |
| Atrazine-d5 | Atrazine-d5, CAS:163165-75-1, MF:C8H14ClN5, MW:220.71 g/mol | Chemical Reagent |
| Pyrene-d10 | Pyrene-d10, CAS:1718-52-1, MF:C16H10, MW:212.31 g/mol | Chemical Reagent |
In the context of confirming mixed treatment comparison results with direct evidence, the model you select fundamentally shapes your conclusions. The fixed-effect model offers a false sense of precision when its core assumption of a single true effect is violated, which is common in real-world clinical research. The random-effects model, by acknowledging and accounting for between-study differences, provides a more realistic and generalizable summary of the evidence.
For researchers and drug development professionals, the following is recommended:
- Default to a Random-Effects Model: Given the inherent clinical and methodological diversity in most networks of studies, a random-effects model is often the more appropriate and conservative starting point [20] [21].
- Justify Your Choice A Priori: Base your decision on the expected similarity of studies and the goal of your analysis, not on post-hoc heterogeneity statistics.
- Use Contemporary Methods: When applying a random-effects model, use robust variance estimators (e.g., REML, PM) and the HKSJ method for confidence intervals.
- Report Prediction Intervals: Move beyond the mean effect and report prediction intervals to communicate the expected range of effects in clinical practice.
- Conduct Sensitivity Analyses: Run both models to assess the robustness of your findings, particularly for key outcomes in your MTC.
By adhering to these principles, you will produce a more rigorous, reliable, and clinically applicable evidence synthesis, strengthening the validity of your indirect comparisons and their confirmation with direct evidence.
Network meta-analysis (NMA) represents a sophisticated evidence synthesis methodology that enables simultaneous comparison of multiple interventions within a single analytical framework. By integrating both direct evidence (from head-to-head trials) and indirect evidence (from trials connected through common comparators), NMA provides a powerful tool for comparative effectiveness research, particularly crucial for drug development professionals and researchers facing limited direct comparison data. This methodology has gained substantial traction across medical fields, with published guidance showing a significant increase since 2011, particularly on evidence certainty and NMA assumptions [22] [23]. The core strength of NMA lies in its ability to confirm mixed treatment comparison results through coherence between direct and indirect evidence, thereby generating a more comprehensive understanding of therapeutic relative effectiveness.
Table 1: Fundamental Concepts in Network Meta-Analysis
| Concept | Definition | Importance in MTC Validation |
|---|---|---|
| Direct Evidence | Evidence from studies directly comparing interventions (e.g., A vs. B) | Serves as reference for validating indirect comparisons |
| Indirect Evidence | Evidence derived through a common comparator (e.g., A vs. B via C) | Extends inference to comparisons lacking head-to-head trials |
| Network Connectivity | The pattern of connections between interventions via direct comparisons | Ensures the feasibility of indirect and mixed treatment comparisons |
| Transitivity Assumption | The assumption that studies comparing different interventions are sufficiently similar in important effect modifiers | Foundational for valid indirect comparisons |
| Consistency/Coherence | Agreement between direct and indirect evidence for the same comparison | Critical for confirming mixed treatment comparison results |
Foundational Principles of Network Meta-Analysis
Core Assumptions and Statistical Framework
The validity of any NMA depends on three fundamental assumptions that researchers must rigorously assess. The transitivity assumption requires that studies comparing different interventions are sufficiently similar in clinical and methodological characteristics that could modify treatment effects. This implies that participants in any pairwise comparison could hypothetically have been randomized to any intervention in the network. The homogeneity assumption dictates that effect sizes for the same pairwise comparison do not differ significantly across studies, while the consistency assumption requires statistical agreement between direct and indirect evidence for the same comparison [22].
The statistical framework for NMA typically employs hierarchical Bayesian or frequentist models that simultaneously analyze all direct and indirect comparisons. These models generate relative treatment effects with measures of precision for all possible pairwise comparisons within the network, even those never directly studied in trials. Recent methodological reviews indicate that guidance documents on assumptions and certainty of evidence have become particularly abundant, with over 13 documents per topic, providing robust resources for researchers implementing these techniques [22].
Step-by-Step Methodology
Protocol Development and Research Question Formulation
The initial phase of any NMA requires meticulous planning and protocol development, an area where methodological reviews have identified comparatively sparse guidance [22]. A well-structured protocol should explicitly define the research question using PICO elements (Population, Intervention, Comparator, Outcome), specify the network geometry (all interventions of interest), and predefine the statistical methods for evaluation of assumptions.
Node-making – the process of defining and grouping interventions for analysis – represents a critical methodological choice, particularly for complex public health interventions. A recent methodological review proposed a typology of node-making elements organized around seven considerations: Approach, Ask, Aim, Appraise, Apply, Adapt, and Assess [24]. In practice, network nodes can be formed by:
- Grouping similar interventions or intervention types (65/102 networks in public health NMAs)
- Comparing named interventions directly (6/102)
- Defining nodes as combinations of intervention components (26/102)
- Using an underlying component classification system (5/102) [24]
Diagram 1: NMA Workflow Overview
Comprehensive Search and Study Selection
A rigorous systematic review constitutes the essential foundation for any valid NMA. This process requires comprehensive searches across multiple databases, grey literature sources, and clinical trial registries to minimize publication bias. Recent methodological guidance emphasizes the importance of specialized search strategies to identify all relevant randomized controlled trials for the interventions of interest, with emerging artificial intelligence-assisted tools showing promise in enhancing search sensitivity without sacrificing specificity [25] [26].
Study selection should follow the standard systematic review process of title/abstract screening followed by full-text assessment, ideally conducted independently by at least two reviewers using tools such as Covidence [22] [23]. The PRISMA-NMA reporting guidelines provide a structured framework for documenting the search and selection process, ensuring transparency and reproducibility.
Data Extraction and Transitivity Assessment
Data extraction for NMA extends beyond standard systematic reviews by requiring additional elements critical for assessing transitivity and potential effect modifiers. These include:
- Patient characteristics that may modify treatment effects (age, disease severity, comorbidities)
- Intervention details (dose, duration, delivery mode, concomitant treatments)
- Study methodology (design, setting, follow-up duration, outcome definitions)
- Result data for all relevant outcomes across all intervention groups
A proposed typology for node-making suggests that reviewers should "Appraise" potential effect modifiers and "Adapt" their analytical approach based on assessment of clinical and methodological diversity [24]. This assessment directly informs the evaluation of the transitivity assumption.
Table 2: Key Methodological Considerations at Each NMA Stage
| Stage | Key Considerations | Validation Approaches |
|---|---|---|
| Protocol Development | Scope of network, node definition, outcomes, analysis plan | Peer review, registration (PROSPERO) |
| Search & Selection | Comprehensiveness, reproducibility, minimization of bias | PRISMA flow diagram, search strategy peer review |
| Transitivity Assessment | Clinical/methodological similarity, potential effect modifiers | Comparison of study characteristics across comparisons |
| Statistical Analysis | Model choice, heterogeneity, consistency evaluation | Sensitivity analyses, model fit statistics, node-splitting |
| Evidence Certainty | Risk of bias, imprecision, inconsistency, indirectness, publication bias | GRADE for NMA approaches |
Network Geometry and Connectivity Evaluation
Before conducting statistical analyses, researchers must evaluate the network structure and connectivity. This involves creating a network diagram (as shown in Diagram 2) that visually represents all treatments and direct comparisons, with node size typically proportional to the number of patients and line thickness proportional to the number of studies for each direct comparison.
Diagram 2: Example Network Geometry
The arrangement of interventions in the network directly enables the confirmation of mixed treatment comparisons with direct evidence. For instance, in Diagram 2, the comparison between Drug A and Drug C has both direct evidence (2 trials) and indirect evidence through Placebo and Drug B, allowing statistical assessment of consistency between these evidence sources [24].
Statistical Analysis and Model Implementation
The analytical phase of NMA involves several sequential steps:
1. Model Selection: Choose between fixed-effect and random-effects models based on heterogeneity assessment. Random-effects models are generally preferred as they account for between-study heterogeneity.
2. Implementation: Most contemporary NMAs use Bayesian methods with Markov Chain Monte Carlo (MCMC) simulation, though frequentist approaches are also available. Guidance resources for software implementation are most abundant for R and Stata packages [22] [23].
3. Ranking: Generate treatment hierarchies using metrics such as Surface Under the Cumulative Ranking Curve (SUCRA) or mean ranks, which estimate the probability of each treatment being the most effective.
4. Consistency Assessment: Evaluate agreement between direct and indirect evidence using statistical methods such as node-splitting, which separately estimates direct and indirect evidence for particular comparisons [22].
For complex interventions, reviewers may face methodological choices between 'splitting' versus 'lumping' interventions and between intervention-level versus component-level analysis. Additive component network meta-analysis models offer an alternative approach, though a review found these were applied in just 6 of 102 networks in public health [24].
Critical Appraisal and Certainty Assessment
The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) framework for NMA provides a systematic approach for rating confidence in estimated effects. This approach categorizes interventions for each outcome based on their positioning from best to worst while considering both effect estimates and certainty of evidence [10]. The certainty rating begins with the assumption that direct evidence provides higher certainty than indirect evidence, then evaluates five factors:
- Risk of bias across studies contributing to the network
- Indirectness of the evidence for the specific research question
- Inconsistency in results (heterogeneity or inconsistency)
- Imprecision of effect estimates
- Publication bias across the network
A recent design validation study developed novel presentation formats for conveying this complex information, using color-coded shading to identify the magnitude and certainty of treatment effects in relation to reference treatments [10].
Results Presentation and Visualization
Effective communication of NMA findings requires specialized presentation approaches that can simultaneously display multiple outcomes and treatments. Through iterative design validation with clinicians, researchers have developed color-coded presentation formats that organize treatments by benefit and harm categories across outcomes [10]. These formats place treatment options in rows and outcomes in columns, with intuitive color coding to facilitate interpretation by audiences with limited NMA familiarity.
Emerging technologies are further enhancing presentation capabilities. Recent artificial intelligence-assisted systems can synthesize and present NMA results through interactive web platforms, though these require further validation against traditional methods [25] [26].
Case Study Application: Pharmacological Obesity Treatments
A recent high-quality NMA evaluated the efficacy and safety of pharmacological treatments for obesity, analyzing 56 randomized controlled trials with 60,307 patients [27]. This analysis exemplifies the complete NMA methodology:
Network Structure: The analysis compared six obesity medications (orlistat, semaglutide, liraglutide, tirzepatide, naltrexone/bupropion, and phentermine/topiramate) against placebo, with limited direct head-to-head comparisons (only liraglutide vs. orlistat and semaglutide vs. liraglutide).
Outcomes: The primary outcome was percentage of total body weight loss (TBWL%) with multiple secondary outcomes including lipid profile, blood pressure, hemoglobin A1c, and adverse events.
Validation of Results: The analysis demonstrated consistency between direct and indirect evidence where available, strengthening confidence in the mixed treatment comparisons. For instance, the direct comparison showing semaglutide superiority to liraglutide was consistent with indirect comparisons through placebo.
Findings: All medications showed significantly greater weight loss versus placebo, with only semaglutide and tirzepatide achieving more than 10% TBWL. The analysis provided crucial evidence for clinical decision-making by simultaneously ranking interventions across multiple efficacy and safety outcomes [27].
Table 3: Essential Research Reagents and Methodological Resources for NMA
| Resource Category | Specific Tools/Solutions | Primary Function | Application Context |
|---|---|---|---|
| Systematic Review Software | Covidence, Rayyan, DistillerSR | Study screening, selection, and data extraction management | Streamlining systematic review process with dual independent review |
| Statistical Analysis Packages | R (gemtc, netmeta), Stata (network), WinBUGS/OpenBUGS | Statistical modeling of network meta-analysis | Implementing Bayesian and frequentist NMA models, consistency checks |
| Quality Assessment Tools | Cochrane Risk of Bias, GRADE for NMA | Methodological quality assessment and evidence certainty rating | Evaluating study limitations and confidence in effect estimates |
| Protocol Registration | PROSPERO, Open Science Framework | Protocol registration and publication | Enhancing transparency and reducing duplication |
| Emerging AI-Assisted Tools | The Umbrella Collaboration (TU) | Automated tertiary evidence synthesis | Rapid evidence mapping and synthesis (requires validation) [25] |
The methodology for conducting network meta-analysis has evolved substantially, with significant increases in available guidance particularly on evidence certainty and NMA assumptions. The step-by-step process from systematic review to validated mixed treatment comparison requires meticulous attention to transitivity assessment, statistical model selection, and rigorous evaluation of consistency between direct and indirect evidence. By following this structured methodology and utilizing the available toolkit of resources, researchers and drug development professionals can generate robust comparative effectiveness evidence to inform clinical decision-making and health policy, even when direct comparison data are limited. Future methodological developments will likely focus on advanced NMA guidance and decision tools to aid reviewers in further navigating the complexities of these analyses [22].
Mixed Treatment Comparison (MTC), also commonly referred to as Network Meta-Analysis (NMA), is a sophisticated statistical technique that enables the simultaneous comparison of multiple interventions for a single medical condition by combining both direct and indirect evidence across a network of studies [17] [4]. This methodology addresses a critical challenge in evidence-based medicine: clinicians and decision-makers often must select the optimal treatment from numerous available interventions, yet head-to-head randomized controlled trials (RCTs) comparing all relevant options are frequently unavailable [17].
MTC serves as a generalization of standard pairwise meta-analysis. While traditional meta-analysis can only compare two interventions that have been directly evaluated against each other in clinical trials, MTC synthesizes evidence from a connected network of studies where at least one pair of interventions is compared both directly and indirectly, forming what is known as a closed loop [17] [28]. This approach allows researchers to derive relative treatment effects between interventions that have never been compared directly in primary studies, thereby filling critical gaps in the evidence base [4].
The importance of MTC has grown substantially in health technology assessment, with organizations such as England's National Institute for Health and Care Excellence (NICE) now accepting well-conducted network meta-analyses to inform clinical guidelines and reimbursement decisions [29] [28]. By leveraging all available direct and indirect evidence, MTC provides more precise estimates of intervention effects compared to single direct or indirect estimates alone, and can establish a hierarchy of treatments based on their relative efficacy and safety [4].
Methodological Framework
Fundamental Concepts and Terminology
Understanding MTC requires familiarity with several key concepts:
- Direct Evidence: Treatment effect estimates derived from studies that directly compare two interventions head-to-head [4].
- Indirect Evidence: Treatment effect estimates obtained by comparing two interventions through a common comparator [17] [4]. For example, if intervention A has been compared to B, and B to C, we can indirectly estimate the effect of A versus C.
- Network Meta-Analysis: The simultaneous synthesis of evidence for all pairwise comparisons across more than two interventions [17].
- Closed Loop: A network structure where each comparison has both direct evidence and indirect evidence [17].
- Transitivity: The core assumption that the different sets of studies included in the analysis are similar, on average, in all important factors that may affect the relative effects [4].
Table 1: Key Terminology in Mixed Treatment Comparisons
| Term | Definition | Importance |
|---|---|---|
| Network Meta-Analysis | Simultaneous synthesis of all pairwise comparisons across >2 interventions [17] | Encompasses various indirect comparison methods |
| Indirect Treatment Comparison | Comparison of two interventions via a common comparator [28] | Foundation of evidence synthesis when direct evidence is lacking |
| Mixed Treatment Comparison | Analysis of networks with both direct and indirect evidence (closed loops) [28] | Allows combination of different evidence types |
| Transitivity | Similarity of studies across different comparisons in effect modifiers [4] | Validity requirement for indirect comparisons |
| Incoherence/Inconsistency | Disagreement between direct and indirect evidence for the same comparison [4] | Signals potential violation of transitivity assumption |
Statistical Approaches
MTC can be implemented through two primary statistical frameworks:
Bayesian Framework: This approach involves a formal combination of a prior probability distribution (reflecting prior belief about possible values of model parameters) with a likelihood distribution (based on observed data) to obtain a corresponding posterior probability distribution [17]. Bayesian methods are particularly well-suited for MTC as they naturally handle complex hierarchical models and provide intuitive probabilistic interpretations, including treatment rankings and credible intervals [29].
Frequentist Framework: This includes approaches such as Lumley's network meta-analysis, which uses a mixed model to combine both direct and indirect evidence when there is at least one closed loop of evidence connecting interventions of interest [17]. Frequentist methods typically employ generalized linear models with appropriate weighting of different evidence sources.
The choice between Bayesian and Frequentist approaches often depends on the complexity of the network, available software expertise, and specific research questions. Bayesian methods have been more widely adopted in recent MTC applications, particularly for complex networks with multiple interventions and sparse direct evidence [29].
Table 2: Comparison of Bayesian and Frequentist Approaches to MTC
| Feature | Bayesian Framework | Frequentist Framework |
|---|---|---|
| Philosophical Basis | Formal combination of prior distributions with likelihood to obtain posterior distributions [17] | Relies on sampling distributions and fixed parameters |
| Output | Posterior probability distributions, credible intervals | Point estimates, confidence intervals, p-values |
| Treatment Ranking | Natural probability statements about rankings [4] | Typically requires additional resampling methods |
| Complexity Handling | Well-suited for complex hierarchical structures [29] | May have limitations with highly complex networks |
| Software Examples | WinBUGS, OpenBUGS, JAGS [29] | R, Stata, SAS |
Key Assumptions and Validity Considerations
Transitivity and Similarity
The validity of any MTC depends critically on the transitivity assumption, which requires that the different sets of studies making different direct comparisons are sufficiently similar in all important factors that might modify treatment effects [4]. Transitivity can be conceptualized through three component assumptions:
Homogeneity: For each pairwise comparison, the studies should be sufficiently similar in their design and patient characteristics. This is equivalent to the assumption in standard pairwise meta-analysis that the true treatment effects are the same across studies [28] [4].
Similarity: Across different comparisons, the studies should be sufficiently similar in potential effect modifiers. For example, the set of studies comparing A versus B should be similar to the set comparing A versus C in terms of patient characteristics, study design, and outcome definitions [28] [4].
Consistency: The direct and indirect evidence for a particular comparison should agree within statistical error. This is the statistical manifestation of transitivity and can be evaluated quantitatively in networks with closed loops [4].
Violations of transitivity can occur when studies of different comparisons differ systematically in effect modifiers such as patient characteristics (e.g., disease severity, age, comorbidities), intervention characteristics (e.g., dose, duration, delivery method), or study design features (e.g., randomization method, blinding, follow-up duration) [28] [4].
Assessment of Incoherence
Incoherence (also called inconsistency) occurs when different sources of information (e.g., direct and indirect) about a particular intervention comparison disagree [4]. Several approaches exist to assess incoherence:
Local Tests: Evaluate disagreement between direct and indirect evidence for specific comparisons in closed loops. The Bucher method is a commonly used approach for simple loops involving three interventions [4].
Global Tests: Assess incoherence across the entire network simultaneously. Methods include the design-by-treatment interaction model and various node-splitting approaches [4].
Comparison of Models: Fitting both consistent and inconsistent models and comparing their fit using deviance information criterion (DIC) or other goodness-of-fit measures [29].
When significant incoherence is detected, researchers should investigate potential causes by examining differences in study characteristics across comparisons and consider subgroup or meta-regression analyses to explain the disagreement [4].
Diagram 1: Components of the Transitivity Assumption in MTC
Implementation and Analysis Workflow
Data Collection and Network Specification
The foundation of a valid MTC is a comprehensive systematic review conducted according to established guidelines (e.g., Cochrane Handbook) [28]. Key steps include:
- Systematic Search: Identify all relevant studies comparing any of the interventions of interest, using predefined inclusion and exclusion criteria [29] [28].
- Data Extraction: Collect study characteristics, patient demographics, intervention details, and outcome data using standardized forms [29].
- Risk of Bias Assessment: Evaluate study quality using appropriate tools (e.g., Cochrane Risk of Bias tool) to identify potential limitations in the evidence base [28].
- Network Diagram: Create a visual representation of the evidence network, with nodes representing interventions and edges representing direct comparisons [4]. The diagram should clearly show which comparisons have direct evidence and how interventions are connected.
Statistical Analysis Process
The statistical analysis typically follows these steps:
Model Specification: Choose an appropriate model (fixed-effect or random-effects) based on the network structure and assumed heterogeneity [29]. Fixed-effect models assume a single true treatment effect across all studies, while random-effects models allow for heterogeneity between studies.
Parameter Estimation: Implement the chosen model using Bayesian or Frequentist methods. For Bayesian analyses, this involves specifying prior distributions for model parameters and using Markov Chain Monte Carlo (MCMC) methods to obtain posterior distributions [29].
Model Assessment: Evaluate model fit using measures such as residual deviance and compare alternative models using appropriate criteria (e.g., DIC for Bayesian models) [29].
Incoherence Evaluation: Test for disagreement between direct and indirect evidence using local or global methods [4].
Results Presentation: Generate estimates of relative treatment effects for all pairwise comparisons, rankings of interventions, and measures of uncertainty [4].
Diagram 2: MTC Implementation Workflow from Systematic Review to Results
Confirming MTC Results with Direct Evidence
The Role of Direct Evidence in Validation
Direct evidence from head-to-head randomized trials serves as the cornerstone for validating results derived from mixed treatment comparisons. When both direct and indirect evidence are available for a specific comparison, their agreement provides confidence in the network estimates, while disagreement (incoherence) may indicate problems with the transitivity assumption or other methodological issues [4].
The integration of direct evidence in MTC follows a hierarchical approach:
- Direct-Only Analysis: Considering only head-to-head comparisons, similar to traditional pairwise meta-analysis.
- Indirect-Only Analysis: Estimating effects solely through indirect pathways in the network.
- Mixed Evidence Synthesis: Combining both direct and indirect evidence in a single MTC model [17] [28].
The comparison between direct-only and mixed evidence estimates provides a natural validation check. When direct and indirect evidence are consistent, the combined estimate typically has greater precision than either source alone [4].
Case Study: Pancreatic Cancer Treatments
A practical example comes from a network meta-analysis of treatments for unresectable locally advanced pancreatic cancer (LAPC) [29]. This analysis included 9 trials involving 1,294 patients comparing 12 different treatments, with overall survival as the primary outcome.
Table 3: Comparison of Direct and Mixed Evidence in Pancreatic Cancer NMA [29]
| Comparison | Direct Evidence HR (95% CrI) | Mixed Evidence HR (95% CrI) | Agreement |
|---|---|---|---|
| Gemcitabine vs Chemoradiotherapy + Gemcitabine | 0.70 (0.51-0.99) | 0.70 (0.51-0.99) | Complete |
| Gemcitabine vs Chemoradiotherapy | No direct evidence | 0.87 (0.69-1.09) | N/A |
| Gemcitabine vs Chemotherapy + Biological | No direct evidence | 0.94 (0.76-1.16) | N/A |
| Gemcitabine vs Chemoradiotherapy + Chemotherapy | No direct evidence | 0.96 (0.75-1.23) | N/A |
In this case, the only comparison with both direct and indirect evidence (Gemcitabine vs Chemoradiotherapy + Gemcitabine) showed perfect agreement, increasing confidence in the mixed treatment estimates for comparisons lacking direct evidence [29]. The model showed good fit, with residual deviance (12.01) nearly identical to the number of data points.
Methodological Considerations for Validation
To robustly confirm MTC results with direct evidence, researchers should:
- Prioritize High-Quality Direct Evidence: Studies with low risk of bias and large sample sizes provide more reliable validation benchmarks [28].
- Evaluate Incoherence Statistically: Use appropriate statistical tests to determine whether differences between direct and indirect estimates exceed what would be expected by chance alone [4].
- Investigate Sources of Disagreement: When incoherence is detected, explore potential effect modifiers through subgroup analysis or meta-regression [4].
- Assess Confidence in Evidence: Use structured frameworks like GRADE for network meta-analysis to rate confidence in effect estimates based on study limitations, inconsistency, indirectness, imprecision, and publication bias [4].
Essential Research Reagents and Tools
Implementing MTC requires specific methodological expertise and statistical tools. The following table outlines key "research reagents" - essential materials and resources needed to conduct a valid mixed treatment comparison.
Table 4: Research Reagent Solutions for Mixed Treatment Comparisons
| Reagent/Tool | Function | Application Notes |
|---|---|---|
| Systematic Review Protocol | Guides comprehensive literature search and study selection [28] | PRISMA extension for NMA provides reporting guidelines |
| Risk of Bias Assessment Tool | Evaluates methodological quality of included studies [28] | Cochrane RoB tool commonly used |
| Statistical Software | Implements Bayesian or Frequentist MTC models [29] | WinBUGS/OpenBUGS for Bayesian; R, Stata for Frequentist |
| Network Diagram Tool | Visualizes connections between interventions [4] | Should show multi-arm trials clearly |
| Incoherence Assessment Methods | Tests agreement between direct and indirect evidence [4] | Local and global approaches available |
| GRADE for NMA Framework | Rates confidence in network estimates [4] | Adapts standard GRADE approach for network context |
Mixed Treatment Comparison represents a powerful methodology for synthesizing both direct and indirect evidence to compare multiple interventions simultaneously. When properly conducted and validated against direct evidence where available, MTC provides comprehensive estimates of relative treatment effects that can inform clinical decision-making and health policy. The validity of MTC depends critically on the transitivity assumption, which requires similarity across studies in important effect modifiers. Statistical evaluation of incoherence between direct and indirect evidence serves as an important validation check, with agreement increasing confidence in estimates for comparisons lacking direct evidence. As the methodology continues to evolve, MTC is playing an increasingly important role in evidence-based medicine, particularly for comparative effectiveness research where multiple treatment options exist but complete direct comparison evidence is unavailable.
ISPOR Good Research Practices for Conducting Indirect Treatment Comparisons
Indirect Treatment Comparisons (ITCs) are statistical methodologies used to assess the comparative effectiveness of interventions in the absence of direct head-to-head evidence. As healthcare decision-makers increasingly require comparative effectiveness evidence for all relevant treatments, ITCs have become essential tools in health technology assessment (HTA) and drug development. The International Society for Pharmacoeconomics and Outcomes Research (ISPOR) has established Good Research Practices to ensure the methodological rigor and appropriate application of these techniques.
Within this context, Mixed Treatment Comparison (MTC) represents a specific statistical approach that combines both direct evidence (from trials directly comparing interventions of interest) and indirect evidence (from trials comparing each intervention with a common comparator) to estimate comparative efficacy and safety. The term "mixed" refers to the method's ability to integrate these evidence types within a single analysis, creating an "evidence network" where treatments are compared both directly and indirectly [11]. This methodology has largely been subsumed under the more general term Network Meta-Analysis (NMA), which now represents the predominant terminology in academic literature [11].
Confirming MTC results with direct evidence research forms a critical validation step, as the combination of direct and indirect evidence can strengthen the robustness of comparative effectiveness estimates and provide a more comprehensive synthesis of the available clinical evidence base.
Foundational Principles of ITC
Key Assumptions and Methodological Framework
ITC methodologies rely on several fundamental assumptions that must be critically evaluated to ensure valid results. The similarity assumption requires that studies being compared are sufficiently similar in their clinical and methodological characteristics, particularly regarding patient populations, interventions, and outcome measurements. When combining direct and indirect evidence in MTC, the consistency assumption (also called homogeneity assumption) becomes paramount, requiring that direct and indirect evidence provide statistically consistent treatment effects for the same comparisons [30].
ISPOR Good Research Practices emphasize that methodological choices in ITC must be guided by the specific clinical question and available evidence base. The task force identifies two primary statistical approaches for conducting these analyses: frequentist methods, which rely on hypothesis testing and p-values, and Bayesian methods, which incorporate prior distributions and update beliefs based on observed data [30]. Each approach offers distinct advantages, with Bayesian methods particularly valuable for incorporating prior knowledge and handling complex evidence networks.
Evidence Network Development and Validation
The foundation of any valid ITC or MTC is a well-structured evidence network that graphically represents all available direct comparisons between interventions. This network should include all relevant treatments for a specific condition and patient population, with lines connecting interventions that have been directly compared in randomized controlled trials [30].
Model validation represents a critical component of ISPOR recommendations, emphasizing the need for comprehensive sensitivity analyses to assess the robustness of findings to different methodological choices. This includes evaluating the impact of using fixed-effects versus random-effects models, assessing heterogeneity across studies, and testing the consistency between direct and indirect evidence [30]. When direct evidence is available, comparing MTC results that incorporate both direct and indirect evidence with those derived solely from indirect comparisons provides an important validation of the consistency assumption.
Current Methodological Trends and Applications
ITC Methodologies in Health Technology Assessment
Recent analyses of HTA submissions reveal distinctive patterns in the application of ITC methodologies across different jurisdictions. The table below summarizes the prevalence of various ITC methods in recent submissions to major HTA bodies:
Table 1: Application of ITC Methods in Recent HTA Submissions
| HTA Body/Region | Time Period | NMA Prevalence | MAIC Prevalence | Other Methods | Primary Data Source |
|---|---|---|---|---|---|
| NICE (UK) | 2022-2025 | 61.4% | 48.2% | STCs: 7.9%ML-NMR: 1.8% | [31] |
| CDA-AMC (Canada) | 2020-2024 | ~35% | - | Unanchored MAIC: ~21% | [32] |
| ICER (US) | 2020-2024 | Minimal | - | - | [32] |
These data reveal that Network Meta-Analysis remains the most frequently employed ITC method in HTA submissions, while more complex techniques like Multilevel Network Meta-Regression (ML-NMR) are emerging but not yet widely adopted [31]. The consistent use of population-adjusted methods like Matching-Adjusted Indirect Comparisons (MAIC) and unanchored ITCs highlights the growing sophistication in addressing heterogeneity across study populations.
Common Methodological Challenges and Critiques
Evidence review groups consistently identify specific methodological concerns in submitted ITCs. A comprehensive review of NICE submissions found that 79% of NMAs raised concerns about heterogeneity in patient characteristics, while 76% of MAICs were critiqued for missing treatment effect modifiers and prognostic variables [31]. Population alignment between the evidence base and target population represents another significant challenge, affecting 24% of NMAs and 44% of MAICs [31].
The choice between fixed-effects and random-effects models also generates considerable discussion in HTA submissions. In 23% of NMAs, companies favored fixed-effects models while the ERG preferred random-effects approaches, though this disagreement has declined substantially over time (from 39% in 2022 to 8% in 2024) [31]. Concurrently, the use of informative priors in Bayesian random-effects models has increased dramatically (from 6% in 2022 to 46% in 2024), suggesting evolving methodological practices [31].
Methodological Considerations for Complex Interventions
Node-Making in Network Meta-Analysis
The process of "node-making" - defining interventions as distinct nodes in an evidence network - presents particular challenges for complex public health interventions. A systematic review of 89 reviews applying NMA to complex interventions identified substantial variation in how nodes are formed [24]. Researchers most commonly grouped similar interventions or intervention types (65/102 networks), while fewer defined nodes as combinations of intervention components (26/102) or used underlying component classification systems (5/102) [24].
This review developed a typology of node-making elements organized around seven considerations: Approach, Ask, Aim, Appraise, Apply, Adapt, and Assess [24]. This framework provides guidance for researchers making critical decisions about how to define interventions in complex NMAs, particularly when validating MTC results with direct evidence. The limited application of additive component NMA models (reported in just six reviews) suggests opportunity for methodological advancement in analyzing complex, multi-component interventions [24].
Enhancing ITC Validity Through Early Planning
A proactive approach to ITC planning represents a promising trend for enhancing methodological validity. One proposed roadmap recommends that manufacturers initiate preliminary ITC assessments before Phase 3 trial design to enable more robust comparative analyses for HTA submissions [33]. This approach includes five key steps:
- Targeted searches and PICO simulations to characterize treatment pathways and identify ongoing comparator trials
- Identification of potential treatment effect modifiers and prognostic factors through literature reviews and clinical expert input
- Formal comparisons of trial designs, populations, and outcomes based on available data
- Recommendations for pivotal trial design elements to facilitate consistent comparisons
- Recommendations for supplementary evidence generation as needed [33]
This structured approach helps address common validity threats in ITCs by ensuring that trial designs generate evidence suitable for subsequent comparative analyses, thereby strengthening the confirmation of MTC results with direct evidence.
Experimental Protocols and Analytical Frameworks
Protocol for Validating Mixed Treatment Comparisons
Confirming MTC results with direct evidence research requires a systematic approach to evidence synthesis and validation. The following protocol outlines key methodological steps:
Table 2: Analytical Framework for MTC Validation
| Step | Methodological Process | Key Considerations |
|---|---|---|
| 1. Evidence Network Specification | Identify all relevant interventions and available direct comparisons | Document search strategy, inclusion/exclusion criteria, and network connectivity |
| 2. Assessment of Validity Assumptions | Evaluate similarity (clinical/methodological homogeneity) and transitivity | Identify potential treatment effect modifiers and prognostic factors |
| 3. Statistical Analysis | Conduct both direct comparisons and combined MTC using appropriate models (fixed/random effects) | Select between Bayesian and frequentist approaches based on evidence network characteristics |
| 4. Consistency Assessment | Evaluate agreement between direct and indirect evidence using statistical tests | Apply node-splitting or other discrepancy detection methods |
| 5. Sensitivity and Scenario Analyses | Test robustness to methodological choices, inclusion criteria, and model assumptions | Assess impact of priors in Bayesian analyses, heterogeneity priors in random-effects models |
This framework aligns with ISPOR Good Research Practices recommendations while addressing the specific challenges of validating mixed treatment comparisons [30]. The protocol emphasizes comprehensive assessment of underlying assumptions, appropriate model selection, and rigorous validation of consistency between direct and indirect evidence sources.
Technical Implementation of Network Meta-Analysis
The statistical implementation of NMA follows distinct methodological approaches depending on the analytical framework. In Bayesian analyses, researchers must specify prior distributions for model parameters, with non-informative priors typically used for treatment effects and carefully selected priors for heterogeneity parameters [30]. Frequentist approaches utilize generalized linear models with appropriate weighting of studies based on their precision.
For random-effects models, the choice of heterogeneity prior requires particular attention, with ISPOR recommendations suggesting sensitivity analyses using different distributional assumptions (e.g., half-normal, uniform, or log-logistic) [30]. Model fit should be assessed using appropriate diagnostics, such as residual deviance, deviance information criterion (DIC) in Bayesian analyses, or Akaike information criterion (AIC) in frequentist approaches.
Diagram 1: Methodological Framework for MTC Validation. This workflow illustrates the sequential process for confirming mixed treatment comparison results through direct evidence validation, incorporating evidence synthesis, statistical analysis, and robustness assessment phases.
Essential Research Reagents and Tools
Table 3: Essential Methodological Tools for ITC Research
| Tool Category | Specific Software/Solutions | Primary Function | Application Context |
|---|---|---|---|
| Statistical Analysis Platforms | R (gemtc, pcnetmeta), SAS, WinBUGS/OpenBUGS | Implementation of statistical models for NMA/ITC | Frequentist and Bayesian estimation of treatment effects and uncertainty |
| Evidence Synthesis Tools | SQL, DistillerSR, Covidence | Systematic literature review management | Study identification, selection, and data extraction |
| Network Visualization Software | Cytoscape, R (network, igraph packages) | Visualization of evidence networks | Graphical representation of treatment comparisons and connectivity |
| Bias Assessment Instruments | Cochrane Risk of Bias tool, ROB-MEN | Methodological quality assessment | Evaluation of individual study quality and network-level bias |
| Data Validation Utilities | R (netmeta, BUGSnet), Consistency diagnostic tests | Model validation and discrepancy detection | Assessment of consistency assumptions and model fit |
Specialized statistical software forms the foundation of rigorous ITC research, with Bayesian analyses typically implemented through BUGS-based platforms (WinBUGS, OpenBUGS) or Stan, while frequentist approaches often utilize R packages such as netmeta or gemtc [31] [30]. The emerging multinma package represents recent methodological advancements, providing tools for both standard and multilevel network meta-regression [31].
Evidence synthesis management systems facilitate the reproducible identification and selection of relevant studies, while specialized network visualization tools help researchers and stakeholders understand the connectivity and potential limitations of evidence networks. Bias assessment instruments adapted for network meta-analysis, such as the recently developed ROB-MEN tool, enable comprehensive evaluation of methodological quality across the evidence base.
ISPOR Good Research Practices provide an essential methodological foundation for conducting valid and reliable Indirect Treatment Comparisons, with particular relevance for confirming mixed treatment comparison results through integration with direct evidence. The established frameworks emphasize careful attention to underlying assumptions, appropriate model selection, and comprehensive validation procedures.
Current applications in health technology assessment demonstrate the evolving sophistication of ITC methods, with increasing use of population-adjusted techniques and more complex analytical approaches. Nevertheless, persistent challenges related to heterogeneity, treatment effect modification, and population alignment necessitate ongoing methodological refinement and validation.
The confirmation of MTC results with direct evidence represents a critical validation step, strengthening the evidentiary foundation for healthcare decision-making. By adhering to established good research practices while incorporating emerging methodologies, researchers can generate robust comparative effectiveness evidence that reliably informs treatment decisions and health policy.
Detecting and Resolving Inconsistency in MTC Networks
Network Meta-Analysis (NMA), also known as Mixed Treatment Comparison (MTC), is a powerful statistical technique that extends conventional pairwise meta-analysis to simultaneously compare multiple interventions. A fundamental assumption underpinning the validity of NMA is consistency—the principle that direct evidence (from head-to-head trials) and indirect evidence (derived through common comparators) should agree within a network of evidence [34] [35]. When this assumption is violated, inconsistency arises, potentially leading to biased treatment effect estimates and unreliable clinical conclusions [36]. Inconsistency can stem from various sources, including clinical or methodological diversity among trials, bias in direct comparisons, or the uneven distribution of effect modifiers across different treatment comparisons [35] [37]. Consequently, detecting and evaluating inconsistency is a critical step in NMA, ensuring that the results are robust and credible for evidence-based decision making. This guide provides a comprehensive overview of the primary statistical and graphical methods used to identify inconsistency, comparing their applications, strengths, and limitations to inform researchers and drug development professionals.
Foundational Concepts and Prevalence
Two key concepts form the bedrock of inconsistency assessment: transitivity and consistency. Transitivity is a clinical and methodological assumption that is a prerequisite for a valid NMA. It requires that the included trials are sufficiently similar in their potential effect modifiers (e.g., patient population, intervention dosage, outcome definitions) such that the different treatment comparisons can be meaningfully combined [35] [37]. The statistical manifestation of transitivity is consistency, which can be defined mathematically. In a simple three-treatment network (A, B, C), the consistency assumption for the comparison between B and C is expressed as:
μBC = μAC - μAB
where μ represents the mean effect size for a given pairwise comparison [35]. Inconsistency (IF) is then quantified as the difference between the direct estimate and the indirect estimate: IF = μBC - (μAC - μAB) [35].
Empirical evidence on the prevalence of inconsistency offers context for its importance. An evaluation of 40 published networks involving 303 evidence loops found that statistical inconsistency was detected in 2% to 9% of loops, depending on the effect measure and heterogeneity estimation method used [35]. Loops containing comparisons informed by only a single study were more likely to be inconsistent, and approximately one-eighth of the networks examined showed global inconsistency [35].
Statistical Tests for Detecting Inconsistency
Statistical methods for detecting inconsistency can be broadly categorized into local approaches, which focus on specific parts of the network, and global approaches, which assess the entire network.
Table 1: Comparison of Statistical Tests for Inconsistency
| Method | Type | Underlying Principle | Key Advantage | Key Limitation |
|---|---|---|---|---|
| Loop-Specific Approach [35] | Local | Quantifies disagreement between direct and indirect evidence in a closed loop. | Intuitive and simple to implement for specific loops. | Becomes cumbersome in large networks; multiple testing requires correction. |
| Node-Splitting [38] | Local | Separates evidence for a specific comparison into direct and indirect; tests for disagreement. | Pinpoints the specific comparison where inconsistency occurs. | Computationally intensive, especially in large networks [39]. |
| Design-by-Treatment Interaction [40] [36] | Global | Evaluates whether treatment effects differ across trial designs (sets of comparisons). | Provides an overall test of inconsistency in the entire network; robust performance. | Does not identify the specific location of inconsistency without follow-up tests. |
| Path-Based Approach [39] | Local/Global | Evaluates agreement among all possible paths of evidence between two treatments, not just direct vs. indirect. | Can assess inconsistency even when direct evidence is absent; reveals nuances between indirect paths. | A novel method requiring further validation and software implementation. |
Detailed Experimental Protocols
Protocol 1: Implementing the Loop-Specific Approach The loop-specific method, as detailed by Bucher et al., is a foundational local method [35].
- Identify Loops: Within the treatment network, identify all closed loops (e.g., triangular loops of three treatments or quadrilateral loops of four treatments).
- Estimate Direct Effects: For each pairwise comparison within a loop (e.g., AB, AC, BC in an ABC loop), perform a standard random-effects meta-analysis to obtain the summary effect size (e.g., log-odds ratio) and its variance.
- The model for a comparison AB is: yi,AB = μAB + δi,AB + εi,AB, where δi,AB ~ N(0, τ²AB) and εi,AB ~ N(0, νi,AB) [35].
- Calculate Indirect Effect and Inconsistency: For each loop, calculate the indirect estimate and its variance. The inconsistency factor (IF) and its standard error are then used to test the null hypothesis of consistency (H₀: IF=0) using a Z-test at significance level α=0.05 [35].
Protocol 2: Performing Node-Splitting The node-splitting method, introduced by Dias et al., is a powerful local technique [38].
- Select a Node: Choose a specific direct treatment comparison (the "node") to test for inconsistency.
- Split the Evidence: Separate all evidence in the network into two parts:
- Direct evidence: Data solely from studies that directly compare the two treatments in the chosen node.
- Indirect evidence: All remaining evidence in the network that informs on this comparison indirectly through other paths.
- Analyze and Compare: Estimate the treatment effect for the chosen node using both the direct and the indirect evidence separately. The difference between these two estimates is the inconsistency factor.
- Statistical Test: Use a Bayesian or frequentist framework to test whether the direct and indirect estimates are significantly different. This process is repeated for each node of interest [38].
Graphical Methods for Visualizing Inconsistency
Graphical tools complement statistical tests by providing an intuitive visual representation of the evidence network and potential inconsistency.
Net Heat Plot: Proposed by Krahn et al., this graphical tool aims to identify and locate inconsistency in a network of trials [36]. It is a matrix-based plot that displays Cochran's Q statistics. The plot is constructed by temporarily removing each study design (set of treatments compared in a trial) one at a time and assessing the contribution of each remaining design to the overall network inconsistency. The coloring of the matrix indicates which designs contribute most to inconsistency (shown in warm colors like red) and which reduce it (shown in cool colors like blue) [36]. However, recent research has highlighted limitations, showing that the net heat plot's calculations constitute an arbitrary weighting of evidence that may not reliably signal or locate inconsistency [36].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Software and Methodological Tools for Inconsistency Assessment
| Tool / Reagent | Type | Primary Function in Inconsistency Analysis | Key Features |
|---|---|---|---|
R package netmeta |
Software | A comprehensive frequentist framework for NMA. | Implements loop-specific, design-by-treatment, and node-splitting methods; includes the new path-based approach [39]. |
| WinBUGS / OpenBUGS | Software | A Bayesian analysis software. | Used for fitting complex hierarchical models for NMA, including node-splitting and the inconsistency parameter approach [38] [18]. |
| MetaInsight | Web Application | An interactive, web-based tool for NMA. | Provides a user-friendly interface for performing NMA and basic inconsistency checks without requiring coding skills [34]. |
| Design-by-Treatment Interaction Model | Methodological Framework | A global hypothesis test for network inconsistency. | Tests if treatment effects differ across trial designs; recommended when the location of inconsistency is unknown [40] [36]. |
| Node-Splitting Model | Methodological Framework | A local method to isolate inconsistency at specific comparisons. | Directly quantifies the conflict between direct and indirect evidence for each pairwise comparison [38]. |
| Deisopropylatrazine | Deisopropylatrazine, CAS:1007-28-9, MF:C5H8ClN5, MW:173.60 g/mol | Chemical Reagent | Bench Chemicals |
Identifying inconsistency is a vital step in validating the results of a mixed treatment comparison. A combination of statistical tests and graphical methods should be employed for a thorough assessment. Based on empirical evaluations and methodological research, the following best practices are recommended:
- Use a Hierarchical Approach: Begin with a global test, such as the design-by-treatment interaction model, to assess the overall consistency of the network. If global inconsistency is detected, use local methods like node-splitting or the loop-specific approach to identify the specific comparisons responsible [40] [36].
- Acknowledge Method Limitations: Be aware that methods like the net heat plot may have limitations in reliably signaling inconsistency. The choice of effect measure (e.g., odds ratio vs. risk difference) and heterogeneity estimator can influence the detection of inconsistency, and sensitivity analyses may be needed [35] [36].
- Consider New Methodologies: Emerging methods, such as the path-based approach, offer promise by evaluating all evidence paths between treatments, providing a more nuanced assessment that can detect inconsistencies masked by traditional direct-versus-indirect comparisons [39].
- Investigate the Source: When inconsistency is found, investigate potential clinical or methodological sources, such as differences in patient populations, intervention intensity, or risk of bias across studies forming the direct and indirect evidence [37].
Network meta-analysis (NMA), also referred to as mixed treatment comparison (MTC), is an advanced statistical methodology that combines direct evidence from head-to-head comparisons and indirect evidence from trials sharing common comparators to evaluate the relative effectiveness of multiple treatments simultaneously [17] [1]. This approach allows for the comparison of treatments that have never been directly evaluated in the same clinical trial and provides a hierarchical ranking of interventions, making it particularly valuable for clinical decision-making [2] [1]. The fundamental principle enabling the valid combination of direct and indirect evidence is the consistency assumption, which requires that the direct and indirect evidence estimating the same treatment effect are in statistical agreement [41] [5]. When this assumption is violated, inconsistency occurs, threatening the validity of the network's conclusions [41] [42].
Inconsistency arises from a conflict between "direct" evidence on a comparison between treatments B and C and "indirect" evidence gained from AC and AB trials [41]. Like heterogeneity, inconsistency is ultimately caused by effect modifiers—variables that influence the magnitude of treatment effect—and specifically by an imbalance in the distribution of these effect modifiers across the studies contributing direct and indirect evidence [41]. Understanding, detecting, and addressing inconsistency is therefore crucial for ensuring that NMA results provide reliable evidence for researchers, clinicians, and drug development professionals tasked with making informed decisions about therapeutic options [42] [2].
Empirical Evidence on the Prevalence of Inconsistency
Empirical studies across a broad range of published networks have quantified how commonly inconsistency occurs in practice. An analysis of 40 published networks involving 303 evidence loops found that statistical inconsistency was detected in 2% to 9% of tested loops, depending on the effect measure and heterogeneity estimation method used [35]. Loops that included comparisons informed by only a single study were more likely to demonstrate inconsistency, and approximately one-eighth (12.5%) of the analyzed networks showed global evidence of inconsistency [35].
A more comprehensive evaluation of 201 published networks revealed that 14% showed evidence of inconsistency at the standard significance threshold (p < 0.05), while 20% showed evidence at a more liberal threshold (p < 0.10) [42]. This higher prevalence in the larger sample underscores that inconsistency is a frequent challenge in evidence synthesis. The analysis also identified specific network characteristics associated with increased likelihood of detecting inconsistency: networks including many studies but comparing few interventions were more likely to show statistical inconsistency, likely because they yielded more precise estimates with greater power to detect genuine disagreements between different evidence sources [42].
Table 1: Prevalence of Inconsistency in Empirical Studies
| Study Scope | Number of Networks Analyzed | Inconsistency Prevalence in Loops | Inconsistency Prevalence in Entire Networks |
|---|---|---|---|
| Loops of evidence | 303 loops from 40 networks | 2-9% (depending on methods) | 12.5% (global test) |
| Entire networks | 201 networks | Not applicable | 14% (p < 0.05), 20% (p < 0.10) |
The relationship between heterogeneity and inconsistency presents a particular challenge for evidence synthesis. Large heterogeneity in treatment effects across studies decreases the precision of both direct and indirect estimates, thereby reducing the statistical power to detect genuine inconsistency [35] [42]. Consequently, networks with substantial heterogeneity may fail to flag inconsistency even when it is present, potentially leading to overconfident conclusions based on inconsistent evidence [35].
Methodological Approaches for Detecting Inconsistency
Loop-Specific Approach
The loop-specific approach, building on the method originally proposed by Bucher et al., evaluates inconsistency within each closed loop of evidence by quantitatively comparing direct and indirect estimates [41] [35]. In a triangular loop comparing treatments A, B, and C, the direct estimate of the B versus C effect is compared against an indirect estimate derived from the AB and AC trials [41]. The inconsistency factor (IF) is calculated as:
[ IF{ABC} = \hat{d}{BC}^{Dir} - (\hat{d}{AC}^{Dir} - \hat{d}{AB}^{Dir}) ]
with variance:
[ Var(IF{ABC}) = Var(\hat{d}{BC}^{Dir}) + Var(\hat{d}{AC}^{Dir}) + Var(\hat{d}{AB}^{Dir}) ]
where (\hat{d}_{XY}^{Dir}) represents the direct estimate of the treatment effect between X and Y [41] [35]. The statistical significance of the inconsistency factor is then tested using a standard normal distribution [35]. This approach can be extended to larger loops involving four or more treatments, though interpretation becomes more complex as loops may not be independent [41].
Diagram 1: Loop-based inconsistency detection workflow
Design-by-Treatment Interaction Model
The design-by-treatment interaction (DBT) model provides a global assessment of inconsistency across an entire network by evaluating whether studies with different designs (sets of treatments compared) yield conflicting results for the same treatment comparisons [35] [42]. This approach is particularly valuable because it accounts for all sources of inconsistency simultaneously and properly handles multi-arm trials, which present challenges for loop-based methods [42]. The DBT model incorporates an additional variance component that reflects variability due to inconsistency beyond what would be expected from heterogeneity or random error alone [42]. In empirical applications, when inconsistency is detected using the DBT model (p < 0.05), the consistency model typically displays higher estimated heterogeneity than the inconsistency model, suggesting that the consistency model may be inappropriately attributing inconsistency to heterogeneity [42].
Node-Splitting and Back-Calculation Methods
Node-splitting represents a more recent methodological development that separates evidence on a particular comparison into direct and indirect components [38]. This approach allows researchers to identify which specific comparisons in the network are contributing to inconsistency, providing more targeted information for investigating potential causes [38]. The back-calculation method offers an alternative approach that infers the contribution of indirect evidence from the direct evidence and the output of an MTC analysis, making it particularly useful when only pooled summaries of pairwise contrasts are available [38]. Both methods facilitate understanding of how direct and indirect evidence combine to produce the final MTC estimates, helping users identify what is "driving" the results [38].
Table 2: Comparison of Inconsistency Detection Methods
| Method | Scope of Assessment | Key Advantages | Key Limitations |
|---|---|---|---|
| Loop-Specific Approach | Individual loops | Intuitive, easy to implement and interpret | Difficulties with multi-arm trials; may miss network-wide inconsistency |
| Design-by-Treatment Interaction | Entire network | Comprehensive; proper handling of multi-arm trials | Does not identify specific problematic comparisons |
| Node-Splitting | Specific comparisons | Pinpoints sources of inconsistency | Computationally intensive; requires trial-level data |
| Back-Calculation | Specific comparisons | Works with summary-level data | Limited to specific network structures |
Case Study: Nocturnal Enuresis Treatments
A published overview of reviews for treatments of childhood nocturnal enuresis provides an illustrative case study of extreme inconsistency and its implications for evidence synthesis [5]. The network included eight distinct treatments (e.g., enuresis alarms, desmopressin, imipramine, dry-bed training) and ten direct comparisons for the outcome "failure to achieve 14 days consecutive dry nights" [5]. When the authors initially applied fixed-effect models to the pairwise meta-analyses, they found extreme inconsistency between different sources of evidence [5].
For the comparison between enuresis alarms and no treatment, three separate indirect estimates could be derived through different pathways in the network [5]. Using fixed-effect models, two of the three indirect estimates differed significantly from the direct estimate, and a composite test of inconsistency across all four estimates (one direct and three indirect) strongly rejected the consistency assumption (χ² = 182.6, df = 3, p < 0.001) [5]. This dramatic inconsistency threatened the validity of any conclusions regarding the relative efficacy of the treatments.
However, when the authors re-analyzed the data using random-effects models, the evidence became consistent (χ² = 5.0, df = 3, p = 0.17), allowing for coherent estimation of all treatment effects and valid ranking of interventions [5]. This case demonstrates how the choice of statistical model can dramatically affect assessments of consistency, with random-effects models often providing more conservative and robust estimates when heterogeneity is present across studies [5].
Diagram 2: Nocturnal enuresis case study outcomes
The Scientist's Toolkit: Key Methodological Approaches
Table 3: Essential Methodological Approaches for Inconsistency Investigation
| Method/Approach | Primary Function | Application Context |
|---|---|---|
| Bucher Loop-Specific Method | Quantifies inconsistency in triangular loops | Initial screening for inconsistency in simple networks |
| Design-by-Treatment Interaction Model | Global test of network consistency | Comprehensive assessment of complex networks with multi-arm trials |
| Node-Splitting Method | Separates direct and indirect evidence for specific comparisons | Identifying specific inconsistent comparisons in networks with trial-level data |
| Random-Effects Meta-Analysis | Accounts for between-study heterogeneity | Reducing false consistency when heterogeneity is present |
| Network Graph Visualization | Illustrates network structure and evidence flow | Identifying potential sources of intransitivity in network geometry |
| Multivariable Meta-Regression | Investigates effect modification | Exploring causes of inconsistency when effect modifier data are available |
Recommendations for Practice and Research
Based on the empirical evidence and methodological considerations, several key recommendations emerge for researchers conducting network meta-analyses. First, routinely assess inconsistency using both global tests (like the design-by-treatment interaction model) and local tests (like loop-based approaches or node-splitting) to obtain a comprehensive evaluation of evidence consistency [42] [38]. Second, conduct sensitivity analyses using different statistical models (fixed-effect vs. random-effects) and heterogeneity estimators, as these choices can substantially impact conclusions about consistency, particularly in networks with few studies [35] [5].
Third, investigate potential effect modifiers when inconsistency is detected, focusing on clinical characteristics (disease severity, patient demographics), methodological features (trial quality, design characteristics), and contextual factors (setting, year of publication) that might differ across the direct and indirect evidence streams [41] [42]. Fourth, report assessments transparently, including detailed descriptions of the methods used, all statistical results, and thoughtful interpretation of the implications of any detected inconsistency for the network's conclusions [42] [2].
Finally, when material inconsistency is identified that cannot be resolved through statistical adjustment or subgroup analysis, consider rating down the certainty of evidence for affected comparisons using structured approaches like GRADE for NMA, and be cautious in interpreting treatment rankings and effect estimates [2]. These practices will enhance the reliability and credibility of network meta-analyses, supporting better decision-making in drug development and clinical practice.
Addressing Heterogeneity and Publication Bias in Evidence Synthesis
Evidence synthesis, particularly through systematic reviews and meta-analyses, occupies a critical role in modern evidence-based medicine, directly informing clinical practice and health policy decisions. [43] Among the various advanced methodologies, Mixed Treatment Comparisons (MTCs), also known as network meta-analyses, have emerged as a powerful statistical approach for comparing multiple interventions simultaneously, even when direct head-to-head comparisons are limited or unavailable. [17] This methodology enables researchers to create a connected network of evidence where treatments are compared both directly and indirectly through common comparators. [16]
However, two significant methodological challenges threaten the validity and reliability of these syntheses: heterogeneity and publication bias. Heterogeneity refers to the variability in study effects beyond what would be expected from chance alone, arising from differences in patient populations, interventions, outcomes measurement, or study design. [44] Publication bias occurs when the publication of research findings depends on their direction or statistical significance, leading to a systematically biased representation of the available evidence. [43] Within the specific context of confirming MTC results with direct evidence, these issues become particularly critical, as both can lead to inconsistent or spurious findings that misinform decision-making.
Understanding Heterogeneity in Mixed Treatment Comparisons
Defining Heterogeneity and Its Implications
In evidence synthesis, heterogeneity represents the presence of effect-modifying mechanisms—interactions between the treatment effect and trial or patient characteristics. [44] A crucial distinction exists between true clinical variability (due to differences in patient populations, settings, or protocols) and bias-related variability (due to imperfections in trial conduct). [44] The former threatens external validity, limiting generalizability, while the latter threatens internal validity, potentially producing biased estimates of treatment effects.
In MTCs, heterogeneity becomes more complex due to the interconnected network of evidence. Variability in relative treatment effects can induce inconsistency—discrepancies between direct and indirect evidence for the same treatment comparison. [44] When heterogeneity remains unexplained, it substantially increases uncertainty about comparative effectiveness. The predictive distribution of a treatment effect in a new trial often becomes more relevant for decision-making than the distribution of the mean effect, as it better represents the range of possible outcomes in real-world applications. [44]
Statistical Approaches to Assessing Heterogeneity
Several statistical methods are available to quantify and explore heterogeneity in evidence synthesis:
- Random Effects Models: These models explicitly account for between-study variation by assuming treatment effects follow a distribution, with the between-trial standard deviation (σ) indicating the extent of heterogeneity. [44]
- Meta-Regression: This technique relates the size of treatment effects to potential effect modifiers (covariates) that may be characteristics of trial participants, settings, or conduct. [44] In MTCs, various meta-regression models can be specified, with the most interpretable for decision-making being a model with a single interaction term applicable to all treatment comparisons. [44]
- I² Statistic and Q Statistics: While not explicitly detailed in the search results, these common measures complement the above approaches by quantifying the proportion of total variation due to heterogeneity rather than chance.
The following table summarizes key aspects of heterogeneity assessment:
Table 1: Methods for Assessing Heterogeneity in Evidence Synthesis
| Method | Primary Function | Interpretation | Considerations |
|---|---|---|---|
| Random Effects Model | Estimates between-study variance | Larger σ values indicate greater heterogeneity | Predictive distributions may be more relevant for decisions than mean effects |
| Meta-Regression | Explores relationship between effects and covariates | Identifies potential effect modifiers | Inherently observational; cannot establish causality |
| Subgroup Analysis | Examines effects within patient subgroups | Interaction tests differences between subgroups | Requires careful pre-specification to avoid false positives |
| Inconsistency Assessment | Checks agreement between direct and indirect evidence | Significant inconsistency suggests heterogeneity | Essential for validating MTC results |
Publication Bias: The File Drawer Problem in Evidence Synthesis
Definition and Impact on Evidence Synthesis
Publication bias is defined as "the failure to publish the results of a study on the basis of the direction or strength of the study findings." [43] This phenomenon means that studies with statistically significant positive results are more likely to be published, while those with negative or non-significant results often remain in the "file drawer." [43] The implications for evidence synthesis are profound, particularly for systematic reviews and meta-analyses that aim to summarize all available evidence on a topic.
When publication bias exists, the published literature represents a biased sample of all conducted studies, leading to overestimation of treatment effects in meta-analyses. [43] For MTCs, which rely on a comprehensive network of evidence, publication bias can distort both the magnitude and ranking of treatment effects, potentially leading to incorrect conclusions about comparative effectiveness. This is especially problematic when the bias differentially affects certain treatment comparisons within the network.
Detection Methods for Publication Bias
Several statistical and graphical methods have been developed to detect publication bias:
- Funnel Plots: Visual scatterplots of effect size against precision (typically standard error or sample size). In the absence of publication bias, the plot should resemble an inverted funnel, symmetric around the true effect size. [43] Asymmetry suggests potential publication bias, with missing studies from areas of lower precision. [43]
- Egger's Regression Test: A statistical test for funnel plot asymmetry that quantifies the relationship between effect size and precision. [45]
- Rosenthal's Fail-Safe N: This method identifies the number of additional negative studies required to increase the P-value in a meta-analysis to above 0.05, providing an indication of how robust the results are to potential unpublished studies. [43]
Table 2: Methods for Detecting and Addressing Publication Bias
| Method | Type | Principle | Limitations |
|---|---|---|---|
| Funnel Plot | Graphical | Visual assessment of symmetry | Subjective interpretation; asymmetry may have other causes |
| Egger's Test | Statistical | Regression test for funnel plot asymmetry | Low power with small number of studies |
| Fail-Safe N | Statistical | Estimates number of missing studies needed to nullify effect | Dependent on P-value; does not estimate true effect |
| Selection Models | Statistical | Models the selection process leading to publication | Complex implementation; requires strong assumptions |
Methodological Framework: Confirming MTC Results with Direct Evidence
Analytical Protocols for Validation
Confirming the results of mixed treatment comparisons with direct evidence requires a structured methodological approach. The following experimental workflow outlines the key steps in this validation process:
Statistical Methods for Comparing Direct and Indirect Evidence
The statistical foundation for validating MTC results with direct evidence rests on assessing the consistency assumption—that direct and indirect evidence provide estimates of the same underlying treatment effect. [16] Several analytical approaches facilitate this validation:
- Adjusted Indirect Comparisons: This method, pioneered by Bucher et al., constructs an indirect estimate of the relative effect of two interventions (A vs. B) using information from randomized trials comparing each against a common comparator (C). [16] [46] The direct estimates of A vs. C and B vs. C are combined to produce an indirect estimate of A vs. B, which can then be compared with any available direct A vs. B evidence.
- Node-Splitting Models: These models separate direct and indirect evidence for particular comparisons within the network, allowing formal statistical tests of disagreement.
- Design-by-Treatment Interaction Model: A comprehensive approach that assesses consistency across the entire network by examining whether treatment effects vary by the specific design of studies.
Empirical research comparing these methods has yielded important insights. One study evaluating 51 comparisons found that in most analyses, adjusted indirect comparisons yielded estimates of relative effectiveness equal to the mixed treatment comparison. [16] However, in 6 of 51 comparisons, the direction of effect differed according to the indirect comparison method chosen, highlighting the importance of validation. [16]
Table 3: Key Methodological Tools for Addressing Heterogeneity and Publication Bias
| Tool/Technique | Primary Function | Application Context | Implementation Considerations |
|---|---|---|---|
| WinBUGS/OpenBUGS | Bayesian MCMC analysis for complex models | Fitting random effects MTCs, meta-regression | Steep learning curve but flexible for advanced models |
| R packages (metafor, netmeta) | Frequentist and Bayesian evidence synthesis | Pairwise and network meta-analysis, meta-regression | Accessible with strong statistical programming skills |
| PRISMA Statement | Reporting guidelines for systematic reviews | Ensuring complete and transparent reporting | Item 16 addresses meta-biases including publication bias |
| Funnel Plots | Visual assessment of publication bias | Screening for potential small-study effects | Asymmetry may reflect heterogeneity rather than bias |
| Meta-Regression | Exploring heterogeneity sources | Identifying effect modifiers across studies | Aggregate level analysis susceptible to ecological fallacy |
Integrated Analysis: Addressing Both Challenges Simultaneously
In practice, heterogeneity and publication bias often coexist and interact in ways that complicate evidence synthesis. Unexplained heterogeneity can magnify the impact of publication bias, while biased evidence can create the appearance of heterogeneity. Therefore, an integrated analytical approach is necessary:
- Comprehensive Sensitivity Analysis: Systematically assess how results change under different assumptions about heterogeneity and missing studies.
- Multivariate Meta-Regression: Simultaneously model the effects of multiple potential effect modifiers while accounting for publication bias.
- Bias-Adjusted Models: Incorporate empirical evidence about the direction and magnitude of biases from meta-epidemiological studies. [44]
When conducting these analyses, researchers should prioritize transparency about methodological choices and their potential impact on results. As noted in the guidance on heterogeneity, "investigators should consider the relative contribution of true variability and random variation due to biases when considering their response to heterogeneity." [44]
Addressing heterogeneity and publication bias is not merely a statistical exercise but a fundamental requirement for producing reliable evidence to guide clinical and policy decisions. The validation of mixed treatment comparison results through comparison with direct evidence represents a critical step in this process. While methodological advances have provided powerful tools for these tasks, they require thoughtful application and interpretation.
Researchers should recognize that all evidence synthesis methods operate under assumptions that may not perfectly hold in practice. Transparency about these assumptions, comprehensive sensitivity analyses, and acknowledgment of limitations remain essential. By rigorously applying the methods outlined in this guide—assessing heterogeneity, detecting publication bias, and validating indirect comparisons—researchers can produce more trustworthy syntheses that better inform healthcare decision-making.
As the field evolves, future methodological developments will likely focus on more sophisticated approaches for handling these challenges, particularly through individual patient data meta-analysis and the integration of real-world evidence. Nevertheless, the fundamental principles of critical appraisal, transparency, and methodological rigor will continue to underpin valid evidence synthesis.
Mixed Treatment Comparisons (MTC), also known as network meta-analysis, represent a powerful statistical methodology that combines both direct evidence (from head-to-head trials) and indirect evidence (via a common comparator) to estimate the relative effects of multiple treatments simultaneously [17] [47]. This approach is particularly valuable in healthcare decision-making where clinicians must select optimal treatments from multiple available interventions, often in the absence of comprehensive direct comparative data [17].
The validity of MTC findings fundamentally depends on the statistical assumption of consistency - that direct and indirect evidence provide similar estimates of treatment effects [48] [38]. When this assumption is violated, conclusions drawn from MTC may be unreliable and misleading. Sensitivity analyses therefore play a critical role in testing the robustness of MTC findings under different assumptions and scenarios, providing essential confidence in the results for researchers, clinicians, and policymakers [49] [50].
Core Methodologies for Sensitivity Analysis in MTC
Node-Splitting Methods
Node-splitting serves as a primary technique for detecting inconsistency within a network meta-analysis. This method separates evidence on a particular treatment comparison into 'direct' and 'indirect' components, allowing researchers to statistically test for disagreement between these evidence sources [38].
Experimental Protocol: The node-splitting process involves several systematic steps:
- Identify all closed loops within the evidence network where both direct and indirect evidence exist for a treatment comparison
- Partition the data for a specific comparison (node) into direct evidence (studies directly comparing treatments A vs. B) and indirect evidence (evidence from studies of A vs. C and B vs. C)
- Estimate treatment effects separately from the direct and indirect evidence
- Compare the estimates statistically to determine if significant differences exist
- Repeat this process for each node in the network where both direct and indirect evidence are available [38]
The node-splitting method can be implemented using Bayesian modeling approaches with software such as WinBUGS in combination with R statistical software [38].
Data Imputation for Star-Shaped Networks
Star-shaped networks present a particular challenge for sensitivity analysis. These networks occur when all treatments have been compared only with a common reference treatment (typically placebo or standard care), but not with each other, forming a star-like pattern without any closed loops [48]. In such networks, standard inconsistency checks are impossible because there is no direct evidence to compare against indirect evidence.
Experimental Protocol for Data Imputation:
- Identify missing comparisons in the star-shaped network (all pairs of non-reference treatments)
- Impute hypothetical RCT data for all missing pairwise comparisons to create a complete network
- Generate imputed data (study-level treatment effect sizes and their variances) to simulate a situation that would allow mixed treatment comparison with a statistically acceptable extent of inconsistency
- Compare agreement between results from the original star-shaped network and the complete network after incorporating imputed data
- Quantify robustness by assessing how frequently treatment rankings change after imputation [48]
Application of this method to real datasets has demonstrated that approximately 33% of results from analyses incorporating imputed data indicated that treatment rankings would differ from those obtained from the original star-shaped network, highlighting the potential fragility of findings from such networks [48].
Prior Distribution Sensitivity Analysis
In Bayesian MTC models, which are commonly used for these analyses, the choice of prior distributions can influence the results. Sensitivity analysis tests how robust the findings are to different reasonable prior specifications [47] [50].
Experimental Protocol:
- Fit the primary model using the chosen default priors (typically non-informative or weakly informative)
- Systematically vary prior specifications for key parameters, including:
- Between-study heterogeneity (τ²)
- Basic treatment effect parameters
- Variance-covariance matrices in multivariate models
- Compare posterior distributions of treatment effects and rankings across different prior scenarios
- Assess impact on conclusions regarding relative treatment efficacy and safety [47] [50]
Guidance from organizations like the Agency for Healthcare Research and Quality (AHRQ) specifically recommends testing alternative specifications of the prior distribution to assess robustness of model results [50].
Multivariate and Correlation Sensitivity Analyses
Many clinical trials report multiple correlated outcomes, and ignoring these correlations can lead to biased results. Multivariate sensitivity analyses assess how modeling correlations among multiple outcomes affects MTC findings [47].
Experimental Protocol:
- Develop a multivariate MTC model that accounts for correlations among multiple outcomes within studies (using copulas) and between studies (through multivariate random effects)
- Compare results with those from univariate MTC models that treat each outcome independently
- Assess the impact on bias reduction and efficiency gain, particularly in the presence of outcome reporting bias [47]
Simulation studies have demonstrated that multivariate approaches can reduce the impact of outcome reporting bias when outcomes are missing at random or missing not at random, providing more robust estimates of treatment effects [47].
Comparative Analysis of Sensitivity Methods
Table 1: Comparison of Key Sensitivity Analysis Methods for MTC
| Method | Primary Application | Key Advantages | Implementation Requirements | Interpretation Guidance |
|---|---|---|---|---|
| Node-Splitting | Networks with closed loops | Directly tests consistency assumption; Pinpoints sources of inconsistency | Trial-level data; Bayesian computational tools (WinBUGS, R) | Significant differences indicate local inconsistency; p-values or posterior probabilities quantify evidence |
| Data Imputation | Star-shaped networks | Enables sensitivity analysis where traditional methods fail; Quantifies robustness of rankings | Complete network data for imputation; Criteria for acceptable inconsistency | Percentage of changed rankings indicates fragility; >30% change suggests low reliability |
| Prior Sensitivity | Bayesian MTC models | Tests dependence on subjective prior choices; Assesses stability of conclusions | Multiple model fits with different priors; Computational resources | Minimal change in effects/rankings indicates robustness; Substantive changes warrant caution |
| Multivariate Modeling | MTC with multiple outcomes | Addresses outcome reporting bias; Improves efficiency through borrowing of information | Multivariate outcome data; Advanced statistical modeling | Reduced bias in effect estimates; More precise confidence intervals |
Visualizing Sensitivity Analysis Workflows
Node-Splitting Methodology
Comprehensive Sensitivity Analysis Framework
Table 2: Essential Research Reagents and Computational Tools for MTC Sensitivity Analysis
| Tool/Resource | Primary Function | Application in Sensitivity Analysis | Implementation Considerations |
|---|---|---|---|
| Bayesian MCMC Software (WinBUGS, JAGS, Stan) | Fitting complex Bayesian MTC models | Enables node-splitting, prior sensitivity, and multivariate analyses | Requires programming expertise; Computationally intensive; Needs convergence assessment |
| R Statistical Environment with netmeta, gemtc packages | Frequentist and Bayesian network meta-analysis | Provides framework for data imputation and various sensitivity analyses | Steep learning curve but highly flexible; Extensive documentation available |
| Consistency Models | Synthesizing evidence under consistency assumption | Serves as baseline comparison for inconsistency models | Assumes direct and indirect evidence are in agreement |
| Inconsistency Models | Estimating treatment effects without consistency assumption | Reference point for assessing impact of consistency assumption | Equivalent to separate pairwise meta-analyses with shared heterogeneity |
| Variance-Covariance Structures | Modeling correlations between multiple outcomes | Key component for multivariate sensitivity analysis | Complexity increases with number of outcomes; Copulas offer flexible approach |
| Residual Deviance Measures | Assessing model fit | Comparing consistency vs. inconsistency models | Lower values indicate better fit; Useful for detecting overall inconsistency |
Interpretation and Reporting Guidelines
Effective interpretation of sensitivity analyses requires careful attention to both statistical and clinical significance. When node-splitting analyses identify significant inconsistencies, researchers should investigate potential effect modifiers or methodological differences that might explain the disagreement between direct and indirect evidence [38]. For star-shaped networks, the data imputation approach provides a quantitative measure of robustness - when more than 30% of treatment rankings change after incorporating imputed data under acceptable inconsistency, the original results should be interpreted with considerable caution [48].
Reporting of sensitivity analyses should follow established guidelines, such as the ISPOR checklist for conducting and synthesizing network meta-analysis [50]. Transparent reporting should include detailed descriptions of all sensitivity methods employed, software and tools used, criteria for interpreting results, and a clear statement about how the sensitivity analyses influenced the final conclusions regarding treatment efficacy and safety.
Sensitivity analyses are not merely supplementary components but fundamental requirements for establishing the credibility of MTC findings. The methodologies discussed - including node-splitting for detecting inconsistency, data imputation for assessing robustness in star-shaped networks, prior sensitivity for Bayesian models, and multivariate approaches for correlated outcomes - collectively provide a comprehensive framework for testing the stability of network meta-analysis results.
By systematically applying these sensitivity analysis techniques, researchers can provide drug development professionals and clinical decision-makers with appropriately qualified evidence regarding comparative treatment effectiveness, ultimately supporting more informed and reliable healthcare decisions.
Evidence Synthesis and HTA Acceptance: Proving MTC Validity
In the field of evidence-based medicine, determining the comparative efficacy of multiple treatments relies on two fundamental approaches: direct evidence from head-to-head comparisons and indirect evidence constructed through statistical methods. As therapeutic landscapes become more complex with the advent of precision medicine and targeted therapies, researchers increasingly face mixed evidence bases where some treatments have been compared directly while others have not [51]. This creates a significant methodological challenge for synthesizing evidence across studies conducted in populations with different biomarker statuses and study designs [51]. The core thesis of this guide is that while indirect comparison methods provide valuable tools for comparative effectiveness research, their results require confirmation through direct evidence whenever possible to ensure validity and reliability for drug development decisions.
The fundamental distinction between these approaches lies in their basic structure:
- Direct comparisons involve evidence from randomized controlled trials (RCTs) that randomly assign patients to different treatments and compare outcomes directly within the same study [52].
- Indirect comparisons utilize statistical methods to compare treatments that have not been studied head-to-head in primary research but share common comparators [53].
Methodological Frameworks
Direct Comparison Methodology
Experimental Protocol for Direct Head-to-Head Trials: Direct evidence primarily comes from randomized controlled trials (RCTs) that follow a specific experimental protocol designed to minimize bias and confounding [52] [54]. In a true or classic experimental design, there are at least two groups: the experimental group and the control group. Participants are randomly assigned to both groups, which are identical except that one is exposed to the experimental intervention while the other serves as a control [52]. The core principle is that if a significant difference emerges between groups, it can be inferred that there is a cause-and-effect link between the treatment and outcome [52].
The key methodological steps include:
- Randomization: Assigning participants randomly to treatment groups to ensure comparable baseline characteristics [54].
- Blinding: Implementing single, double, or triple-blind procedures to prevent assessment bias [54].
- Sample Size Calculation: Determining appropriate participant numbers through power analysis to detect clinically significant effects [54].
- Outcome Measurement: Using standardized, predefined endpoints to ensure consistent assessment across sites in multicenter trials [54].
Table 1: Key Characteristics of Direct Comparison Methods
| Feature | Description | Advantages | Limitations |
|---|---|---|---|
| Study Design | Randomized controlled trials with head-to-head comparison [52] | Minimizes confounding through randomization [54] | Requires large sample sizes for adequate power [54] |
| Bias Control | Random allocation, blinding, intention-to-treat analysis [54] | Reduces selection and assessment bias [54] | Complete blinding not always possible |
| Internal Validity | High when properly implemented [53] | Strong causal inference [52] | Results may be specific to trial population |
| Statistical Methods | Traditional frequentist or Bayesian analysis of comparative data [51] | Straightforward interpretation | Limited to treatments studied in same trial |
Indirect Comparison Methodology
Experimental Protocol for Adjusted Indirect Comparisons: Indirect treatment comparisons utilize statistical modeling to compare interventions that have not been directly studied in the same trial. The most common approach is the adjusted indirect comparison, which requires a common comparator (typically a standard treatment or placebo) that links the interventions of interest [53]. For example, if Treatment A has been compared to Treatment C in one trial, and Treatment B has been compared to Treatment C in another trial, an indirect comparison between A and B can be made through their common comparator C.
The methodological framework involves:
- Systematic Literature Review: Identifying all relevant studies comparing treatments of interest to the common comparator [51].
- Quality Assessment: Evaluating methodological quality and potential biases in included studies [53].
- Statistical Synthesis: Using meta-analytic techniques to combine evidence across studies [51].
- Validation Analyses: Assessing consistency and conducting sensitivity analyses to test robustness of findings [53].
The three primary statistical methods for indirect comparisons identified in methodological reviews are [51]:
- Meta-regression: Explains heterogeneity through treatment-covariate interactions.
- Logistic regression models: Handles binary outcomes with adjustment for study-level characteristics.
- Adjusted indirect comparisons: Utilizes common comparators with statistical adjustment for study differences.
Table 2: Framework for Indirect Comparison Methods
| Method Type | Statistical Approach | Data Requirements | Appropriate Use Cases |
|---|---|---|---|
| Adjusted Indirect Comparison | Bucher method with common comparator [53] | Aggregate data from trials with common control | Pairwise comparisons with shared comparator |
| Network Meta-Analysis | Mixed treatment comparisons combining direct/indirect evidence [51] | Multiple trials forming connected network | Comparing multiple interventions simultaneously |
| Meta-Regression | Regression models with treatment-covariate interaction [51] | Study-level covariates and effects | Exploring sources of heterogeneity |
| Individual Participant Data NMA | Hierarchical models with IPD [51] | Individual-level data from all studies | Examining treatment-covariate interactions |
Comparative Analysis of Frameworks
Quantitative Performance Metrics
Methodological studies have provided quantitative comparisons between direct and indirect evidence. A seminal study by Bucher et al. (1997) found that adjusted indirect comparisons generally yield results similar to those from direct comparisons, with most discrepancies falling within expected random variation [53]. However, the precision of indirect comparisons is typically lower due to the inherent limitations of combining evidence across separate studies.
Table 3: Quantitative Comparison of Direct vs. Indirect Evidence
| Performance Metric | Direct Comparisons | Indirect Comparisons | Evidence Source |
|---|---|---|---|
| Type I Error Rate | Controlled at nominal level (e.g., 5%) | Similar to direct when properly adjusted [53] | Methodological simulations [53] |
| Statistical Power | Higher for given sample size | Reduced due to between-study heterogeneity [53] | Empirical evaluations [51] |
| Effect Size Estimates | Unbiased with proper randomization | Similar to direct in 70-80% of cases [53] | Comparison studies [53] |
| Confidence Interval Width | Narrower for same number of patients | 20-30% wider on average [53] | Statistical simulations [51] |
| Transitivity Violations | Not applicable | Major threat to validity [53] | Methodological reviews [51] |
Validation Against Direct Evidence
The critical test for indirect comparison methods is their agreement with direct evidence when both are available. Gartlehner and Moore (2008) conducted a comprehensive summary of the evidence and concluded that well-conducted methodological studies provide good evidence that adjusted indirect comparisons can lead to results similar to those from direct comparisons [53]. This validation framework includes:
- Node-splitting Analysis: Comparing direct and indirect evidence within network meta-analysis to assess consistency [51].
- Design-by-treatment Interaction Model: Testing whether treatment effects vary by study design [51].
- Comparison with Gold Standard: Evaluating how closely indirect estimates match high-quality direct evidence when it emerges [53].
However, serious limitations persist, including unverifiable assumptions about the similarity of compared studies and low statistical power to detect meaningful differences [53]. These limitations necessitate cautious interpretation of indirect comparison results, particularly when direct evidence is scarce or methodologically weak.
Advanced Methodological Integration
Mixed Treatment Comparisons
Network meta-analysis (NMA), also known as mixed treatment comparisons, represents the most sophisticated integration of direct and indirect evidence. This methodology allows for simultaneous comparison of multiple treatments while combining direct head-to-head evidence with indirect evidence from a network of trials [51]. The fundamental requirement is that the network must be connected, meaning all treatments can be linked through direct or indirect pathways.
The experimental protocol for NMA includes:
- Comprehensive Search: Identifying all relevant studies for all treatments of interest.
- Network Geometry Mapping: Visualizing and describing the connections between treatments.
- Consistency Assessment: Evaluating statistical agreement between direct and indirect evidence.
- Ranking Probabilities: Estimating probability of each treatment being most effective.
Handling Mixed Populations in Evidence Synthesis
Modern drug development, particularly in precision medicine, frequently creates mixed evidence bases where trials are conducted in populations with different biomarker statuses [51]. For example, early trials of targeted therapies might include all-comers, while later trials focus exclusively on biomarker-positive populations. This creates significant methodological challenges for traditional meta-analysis, which assumes comparable populations across studies [51].
Advanced methods for handling mixed populations include:
- Meta-regression: Adjusting for differences in population characteristics across studies [51].
- Individual Participant Data (IPD) Meta-analysis: Allowing standardized reanalysis of patient-level data across trials [51].
- Hierarchical models: Accounting for different levels of evidence within the same analysis [51].
The Researcher's Toolkit
Essential Research Reagents and Solutions
Table 4: Key Methodological Tools for Comparison Research
| Tool Category | Specific Solutions | Function | Application Context |
|---|---|---|---|
| Statistical Software | R (gemtc, netmeta), WinBUGS, SAS | Implement complex statistical models for indirect comparisons | All phases of evidence synthesis |
| Quality Assessment Tools | Cochrane Risk of Bias, GRADE framework | Evaluate methodological quality of primary studies | Systematic review and evidence grading |
| Data Extraction Platforms | Covidence, Systematic Review Data Repository (SRDR) | Standardized data collection from primary studies | Systematic review conducting |
| Consistency Evaluation Methods | Node-splitting, Design-by-treatment interaction test | Validate agreement between direct and indirect evidence | Network meta-analysis validation |
| Biomarker Assay Standardization | Standardized laboratory protocols, QC materials | Ensure consistent biomarker measurement across studies | Precision medicine applications |
The methodological framework for comparing direct and indirect evidence continues to evolve, particularly with the development of sophisticated statistical models for network meta-analysis and methods for handling mixed biomarker populations [51]. While adjusted indirect comparisons can provide valuable information when direct evidence is absent, they remain subject to unverifiable assumptions and should be interpreted with appropriate caution [53].
For researchers and drug development professionals, the key implications are:
- Hierarchy of Evidence: Direct comparisons should be prioritized when available and methodologically sound.
- Transparency in Methods: All indirect comparisons should explicitly state assumptions and conduct sensitivity analyses.
- Validation Imperative: Indirect comparison results should be confirmed with direct evidence when it emerges.
- Contextual Decision-Making: The choice between methodological approaches depends on the decision context, available resources, and specific research question [51].
In the rapidly advancing field of evidence synthesis, the integration of direct and indirect evidence through network meta-analysis represents the most promising approach for comprehensive treatment comparison, provided that statistical consistency is rigorously assessed and clinical heterogeneity is appropriately addressed.
The Bucher Method and Other Techniques for Formal Validation
In health technology assessment (HTA) and drug development, randomized controlled trials (RCTs) represent the gold standard for comparing the efficacy and safety of treatments. However, direct head-to-head comparisons are not always ethically permissible, financially feasible, or practical, particularly in oncology and rare diseases [14]. When such direct evidence is absent, researchers and HTA bodies must rely on indirect treatment comparisons (ITCs) to evaluate the relative effects of competing interventions [55]. These methodologies enable comparative effectiveness research by linking treatments through a common comparator, such as placebo or a standard therapy, using evidence from separate studies.
The validation of mixed treatment comparison (MTC) results, which combine direct and indirect evidence, remains a critical challenge. Confidence in network meta-analysis findings depends on formally verifying that the results from indirect pathways are consistent with any available direct evidence [56]. This guide objectively compares the Bucher method, a foundational ITC technique, against other advanced population-adjusted and network meta-analysis methods. It provides researchers and drug development professionals with a structured framework for selecting and applying these methods to robustly confirm treatment effects within a connected evidence network.
Classification and Terminology
Indirect treatment comparison is a broad term encompassing various statistical techniques used to compare interventions that have not been studied directly in a single trial [55]. The field is characterized by evolving methodologies and sometimes inconsistent terminologies across the literature. These methods can be classified based on underlying assumptions—primarily the constancy of relative treatment effects—and the number of treatments being compared [55].
Fundamentally, ITC methods aim to provide unbiased estimates of relative treatment effects by preserving the randomization of the originally assigned patient groups from different trials, in contrast to naïve comparisons that simply compare study arms as if they were from the same RCT [14] [46]. The most common techniques include the Bucher method (also known as adjusted or standard ITC), network meta-analysis (NMA), and various population-adjusted indirect comparisons (PAIC) such as matching-adjusted indirect comparison (MAIC) and simulated treatment comparison (STC) [14] [55].
Critical Assumptions for Valid Indirect Comparisons
All ITC methods rely on key statistical assumptions that must be critically assessed for valid results:
- Similarity: The studies being compared must be sufficiently similar in their clinical and methodological characteristics (e.g., patient populations, outcome definitions, study design) to permit meaningful comparison [56].
- Homogeneity: For a given treatment comparison, the treatment effects should be similar across different studies. Significant heterogeneity can invalidate indirect comparisons [56].
- Consistency: The direct and indirect evidence for a treatment comparison should be in agreement. This assumption is crucial for the validity of network meta-analyses that combine both types of evidence [56].
Violations of these assumptions can lead to biased treatment effect estimates and incorrect conclusions about comparative effectiveness.
The Bucher Method: Foundation for Adjusted Indirect Comparisons
Methodology and Experimental Protocol
The Bucher method, also known as adjusted indirect treatment comparison or simple ITC, provides a foundational approach for comparing two treatments indirectly through a common comparator [14] [56]. This frequentist method preserves the randomization of the originally assigned patient groups by using the results of direct meta-analyses of each treatment against a common control.
The experimental protocol involves first conducting systematic literature reviews to identify all relevant RCTs comparing treatment A vs. C and treatment B vs. C. For each comparison pair, meta-analyses are performed to pool the results, typically expressed as log odds ratios or log hazard ratios. The indirect estimate for the A vs. B comparison is then calculated as:
[ d{AB}^{Ind} = d{AC} - d_{BC} ]
with variance:
[ \text{Var}(d{AB}^{Ind}) = \text{Var}(d{AC}) + \text{Var}(d_{BC}) ]
where ( d{AC} ) and ( d{BC} ) represent the pooled estimates of the log relative treatment effects from the meta-analyses of A vs. C and B vs. C, respectively [56].
This method can be implemented using standard statistical software such as R, SAS, or Stata, by extracting results from the direct meta-analyses and applying the formulas above. The analysis may use either fixed-effect or random-effects models for the initial meta-analyses, depending on the presence of heterogeneity.
Applications and Validation in Research
The Bucher method is particularly valuable in pairwise comparisons where only a common comparator links the treatments of interest. It has been applied across therapeutic areas, from HIV to rheumatoid arthritis, and serves as a validation tool for more complex network meta-analyses [46] [56].
To confirm the validity of results obtained via the Bucher method, researchers should:
- Test the similarity assumption by comparing trial and patient characteristics across the studies
- Assess heterogeneity within each direct comparison using I² statistics or similar measures
- Evaluate consistency by comparing indirect estimates with any available direct evidence, if present
- Conduct sensitivity analyses to examine the impact of excluding studies at high risk of bias
Simulation studies have shown that when the underlying assumptions are met, the Bucher method provides unbiased treatment effect estimates, though with less precision than direct comparisons [56].
Comparative Analysis of ITC Techniques
Methodological Comparison Framework
Table 1: Comparison of Key Indirect Treatment Comparison Methods
| Method | Key Assumptions | Framework | Key Applications | Data Requirements |
|---|---|---|---|---|
| Bucher Method | Constancy of relative effects (homogeneity, similarity) | Frequentist | Pairwise indirect comparisons through a common comparator | Aggregate data from two sets of RCTs with a common comparator |
| Network Meta-Analysis (NMA) | Constancy of relative effects (homogeneity, similarity, consistency) | Frequentist or Bayesian | Multiple interventions comparison simultaneously; treatment ranking | Aggregate data from multiple RCTs forming a connected network |
| Matching-Adjusted Indirect Comparison (MAIC) | Constancy of relative or absolute effects | Frequentist (often) | Adjusting for population imbalance across studies; single-arm studies | Individual patient data (IPD) for one treatment and aggregate data for comparator |
| Simulated Treatment Comparison (STC) | Constancy of relative or absolute effects | Bayesian (often) | Adjusting for population imbalance using outcome models | IPD for one treatment and aggregate data for comparator |
| Network Meta-Regression | Conditional constancy of relative effects with shared effect modifier | Frequentist or Bayesian | Exploring impact of study-level covariates on treatment effects | Aggregate data with study-level covariates |
Quantitative Performance Evaluation
Table 2: Statistical Properties of ITC Methods Based on Simulation Studies
| Method | Statistical Power | Bias | Mean Squared Error | Type I Error Rate |
|---|---|---|---|---|
| Bucher Method | Lower than direct comparisons | Unbiased when assumptions met | Largest among ITC methods [56] | Appropriately controlled |
| Direct Treatment Comparison | Highest | Unbiased | Lowest | Appropriately controlled |
| Bayesian MTC | Generally better than direct comparisons under no bias/inconsistency [56] | Unbiased when assumptions met | Lower than Bucher method | Appropriately controlled |
| Frequentist MTC | Generally better than direct comparisons under no bias/inconsistency [56] | Unbiased when assumptions met | Lower than Bucher method | Appropriately controlled |
Simulation studies have comprehensively evaluated the statistical properties of ITC methods. When primary studies contain no biases, all major ITC methods produce, on average, unbiased treatment effect estimates [56]. However, the Bucher method demonstrates the largest mean squared error among the methods investigated, reflecting its lower precision compared to more sophisticated approaches [56].
Direct treatment comparisons remain superior to indirect methods in terms of both statistical power and precision (as measured by mean squared error). However, under conditions of no systematic biases and inconsistencies, mixed treatment comparison methods (which combine direct and indirect evidence) generally outperform direct comparisons alone [56].
Experimental Protocols for Key ITC Methods
Network Meta-Analysis Protocol
Network meta-analysis extends the Bucher approach to multiple treatments simultaneously, enabling comprehensive treatment ranking and comparative effectiveness research across an entire evidence network.
Step-by-Step Experimental Protocol:
- Develop Systematic Review Protocol: Define PICOS criteria (Population, Intervention, Comparator, Outcomes, Study designs) and search strategy
- Conduct Comprehensive Literature Search: Search multiple databases and grey literature sources; document using PRISMA guidelines
- Extract Data and Assess Risk of Bias: Use standardized forms; employ Cochrane risk of bias tool or similar
- Create Network Geometry Diagram: Map all treatment comparisons visually to ensure connected network
- Select Statistical Model: Choose between frequentist or Bayesian framework, fixed or random effects
- Check Consistency Assumption: Use node-splitting or other methods to evaluate agreement between direct and indirect evidence
- Estimate Relative Treatment Effects: Calculate effect sizes with confidence/credible intervals for all treatment comparisons
- Rank Treatments: Generate rank probabilities and surface under cumulative ranking curve (SUCRA) values
- Assess Heterogeneity and Inconsistency: Calculate I² statistics, evaluate inconsistency factors
- Perform Sensitivity Analyses: Test robustness of findings to model choices, risk of bias, and inclusion criteria
The analysis can be implemented using specialized software such as R (with netmeta or gemtc packages), WinBUGS/OpenBUGS, or Stata's network meta-analysis commands.
Population-Adjusted Indirect Comparison Protocol
When patient characteristics differ across trials, population-adjusted methods like MAIC and STC can reduce bias by reweighting or modeling outcomes to improve comparability.
Matching-Adjusted Indirect Comparison (MAIC) Protocol:
- Obtain Individual Patient Data (IPD): Secure IPD for at least one treatment (typically the newer intervention)
- Identify Effect Modifiers: Select baseline characteristics expected to modify treatment effect based on clinical knowledge
- Create Balanced Populations: Use propensity score weighting to adjust IPD population to match aggregate data population characteristics
- Assess Balance: Check standardized mean differences after weighting to confirm improved comparability
- Estimate Comparative Effects: Compare reweighted outcomes from IPD study with aggregate outcomes from comparator study
- Evaluate Uncertainty: Use bootstrapping or robust variance estimators to account for weighting in confidence intervals
Simulated Treatment Comparison (STC) Protocol:
- Develop Outcome Model: Using IPD, create regression model predicting outcomes based on baseline characteristics and treatment
- Validate Model Performance: Assess model calibration and discrimination using appropriate metrics
- Simulate Counterfactual Outcomes: Apply the model to the aggregate population characteristics to estimate outcomes if they had received the IPD treatment
- Compare Treatment Effects: Contrast simulated outcomes with observed outcomes from aggregate data
- Propagate Uncertainty: Use Bayesian methods or multiple imputation to account for uncertainty in model parameters
Visualization of Method Relationships and Applications
ITC Method Selection and Relationship Diagram
ITC Method Selection Pathway
Validation Framework for Mixed Treatment Comparisons
MTC Validation Framework
Essential Research Reagent Solutions
Table 3: Research Reagent Solutions for Indirect Treatment Comparisons
| Tool Category | Specific Tools | Function | Implementation Considerations |
|---|---|---|---|
| Statistical Software | R (netmeta, gemtc, metafor packages) | Conduct meta-analyses and network meta-analyses | Open-source; requires programming expertise |
| Bayesian Analysis Platforms | WinBUGS/OpenBUGS, JAGS, Stan | Fit complex Bayesian models for network meta-analysis | Flexible but computationally intensive |
| Quality Assessment Tools | Cochrane Risk of Bias tool, ROBINS-I | Assess methodological quality of included studies | Essential for sensitivity analyses and grading evidence |
| Data Extraction Utilities | SRDR, Covidence | Manage systematic review data extraction | Streamline collaborative review process |
| Network Visualization | CINeMA, netmeta package | Visualize treatment networks and confidence assessment | Critical for interpreting complex evidence networks |
The formal validation of mixed treatment comparison results remains a methodological cornerstone for robust comparative effectiveness research. The Bucher method provides a foundation for indirect comparisons, offering unbiased estimates when its assumptions are met, though with less precision than more advanced techniques [56]. As therapeutic landscapes grow more complex, researchers must strategically select ITC methods based on available data structures, network connectivity, and between-study heterogeneity [14] [55].
Network meta-analysis extends the Bucher approach to multiple treatments, while population-adjusted methods like MAIC and STC address cross-trial heterogeneity when individual patient data are available [14]. The validation framework presented enables researchers to confirm MTC results through statistical consistency checks, similarity assessments, and sensitivity analyses. As HTA bodies worldwide increasingly accept well-conducted indirect comparisons, mastery of these methods becomes essential for informing healthcare decision-making and drug development strategies [14] [55].
Assessing MTC Credibility for Health Technology Assessment Submissions
Mixed Treatment Comparison (MTC), also commonly referred to as Network Meta-Analysis (NMA), is an advanced statistical methodology that enables the simultaneous comparison of multiple interventions by combining direct evidence (from head-to-head randomized controlled trials) and indirect evidence (estimated through a common comparator) within a single analytical framework [2] [1]. This approach is particularly valuable in health technology assessment (HTA) for determining the comparative effectiveness of treatments that may not have been directly compared in clinical trials, thereby providing crucial evidence for healthcare decision-making [14] [17].
MTC represents a significant evolution beyond traditional pairwise meta-analysis. While conventional meta-analysis compares only two interventions at a time, MTC facilitates a comprehensive analysis of all relevant interventions for a clinical condition, enabling the estimation of relative effects for every possible pairwise comparison in the network, even between treatments lacking direct head-to-head studies [1]. This methodology has matured considerably, with models now available for all types of raw data, producing different pooled effect measures using both Frequentist and Bayesian frameworks [1].
Fundamental Principles of MTC
Key Terminology and Concepts
Table 1: Essential MTC Terminology
| Term | Definition | Importance in MTC |
|---|---|---|
| Direct Evidence | Evidence obtained from studies that directly compare interventions (head-to-head trials) [1]. | Provides the foundation for treatment effect estimates; considered more reliable when available and unbiased. |
| Indirect Evidence | Evidence derived through a common comparator when two treatments have not been directly compared [17] [1]. | Allows estimation of relative effects between interventions not studied together directly. |
| Common Comparator | The intervention (e.g., placebo or standard care) to which multiple treatments are compared, serving as the "anchor" for indirect comparisons [1]. | Essential for forming connected networks and enabling indirect comparisons. |
| Network Geometry | The structure and connectivity of the treatment network, visually represented by nodes (treatments) and edges (direct comparisons) [1]. | Influences the reliability and precision of estimates; well-connected networks are generally more robust. |
| Inconsistency | Disagreement between direct and indirect evidence for the same treatment comparison (also called incoherence) [1]. | A critical validity check; significant inconsistency may indicate biased estimates or violations of underlying assumptions. |
Statistical Frameworks for MTC
MTC analyses can be conducted within two primary statistical frameworks:
- Bayesian Framework: Utilizes prior probability distributions combined with observed data likelihood to obtain posterior distributions for treatment effects. This approach allows for probabilistic statements about treatment rankings and is frequently used in complex network meta-analyses [17] [1].
- Frequentist Framework: Employs methods like network meta-regression and multivariate meta-analysis to estimate treatment effects and account for correlation structure in the network [14] [17].
The choice between these frameworks often depends on the complexity of the evidence network, the availability of software, and analyst preference. Both aim to synthesize all available evidence—direct and indirect—to produce more precise and comprehensive estimates of relative treatment effects [1].
Methodological Protocols for MTC Evaluation
Core Analytical Assumptions
The validity of any MTC depends on three fundamental assumptions that must be critically evaluated [1]:
- Homogeneity: The treatment effects are similar across studies comparing the same interventions. This assumption is shared with pairwise meta-analysis.
- Similarity: The studies included in the network are sufficiently similar in their clinical and methodological characteristics (e.g., patient populations, outcome definitions, study design) to allow meaningful comparison. This is crucial for the transitivity of treatment effects across the network.
- Consistency: The direct and indirect evidence for a given treatment comparison are in agreement. Significant inconsistency suggests potential bias or violation of the similarity assumption.
Experimental Protocol for Assessing MTC Credibility
A robust assessment of MTC credibility involves a systematic, multi-step process. The following workflow outlines the key stages, from network formation to the final interpretation of results.
Figure 1: Workflow for Assessing MTC Credibility. This diagram outlines the sequential process for evaluating the reliability of a Mixed Treatment Comparison, from defining the research question to final interpretation.
The credibility assessment protocol involves several critical phases:
Network Formation and Connectivity Assessment: The first step involves systematically identifying all relevant studies and mapping the geometry of the evidence network. Networks should be evaluated for connectivity, with special attention to closed loops (where interventions form direct connections allowing both direct and indirect evidence) and loose ends (treatments with limited connections) [1]. Well-connected networks with multiple direct comparisons generally yield more reliable estimates.
Evaluation of Methodological and Clinical Similarity: This involves a qualitative assessment of potential effect modifiers across studies, including patient characteristics (e.g., disease severity, age), intervention details (e.g., dosage, administration route), and study methodologies (e.g., blinding, outcome assessment) [1]. Substantial differences in these characteristics may violate the similarity assumption and threaten the validity of indirect comparisons.
Statistical Analysis and Inconsistency Testing: After fitting the MTC model, formal statistical tests for inconsistency should be performed. Methods include:
- Node-splitting: Separately estimating direct and indirect evidence for specific comparisons and testing for significant differences.
- Design-by-treatment interaction model: A global test for inconsistency across the entire network [1]. The case study by which substantial inconsistency was found between direct and indirect evidence for primary pegfilgrastim versus no primary G-CSF (P value for consistency hypothesis 0.027) highlights the importance of this step [57].
Sensitivity and Subgroup Analyses: These analyses test the robustness of the findings to different assumptions, inclusion criteria, or methodological choices. Sensitivity analyses might explore the impact of using different statistical models, prior distributions (in Bayesian analysis), or handling of missing data [58].
Quantitative Assessment of MTC Credibility
Comparative Analysis of Indirect Treatment Comparison Techniques
Table 2: Comparison of Key Indirect Treatment Comparison Techniques
| Technique | Description | Key Strengths | Key Limitations | Frequency of Description in Literature [14] |
|---|---|---|---|---|
| Network Meta-Analysis (NMA) | Simultaneous synthesis of evidence for all pairwise comparisons across >2 interventions [17]. | Most comprehensive approach; combines direct & indirect evidence; provides ranking probabilities. | Requires complex statistical expertise; assumptions can be difficult to verify. | 79.5% |
| Bucher Method | Adjusted indirect comparison for 3 treatments using a common comparator [14] [1]. | Simple and intuitive; good introduction to indirect comparison concepts. | Limited to 3 treatments; cannot incorporate direct evidence simultaneously. | 23.3% |
| Matching-Adjusted Indirect Comparison (MAIC) | Population-adjusted method using individual patient data to re-weight trials [14]. | Adjusts for cross-trial differences in patient characteristics; useful for single-arm studies. | Requires IPD for at least one trial; can only adjust for observed differences. | 30.1% |
| Simulated Treatment Comparison (STC) | Models treatment effect as a function of patient baseline characteristics [14]. | Adjusts for cross-trial differences using published data; applicable when IPD is unavailable. | Relies on strong modeling assumptions; can only adjust for observed differences. | 21.9% |
Impact of Data Type on MTC Performance
The choice of outcome measure significantly influences the statistical power and reliability of MTC findings. Continuous data generally provide more powerful and sensitive analyses compared to dichotomized measures:
Table 3: Continuous vs. Binary Outcome Measures in MTC
| Characteristic | Continuous Data | Binary/Dichotomized Data |
|---|---|---|
| Statistical Power | Higher power to detect differences between treatments [58]. | Lower power due to information loss during categorization [58]. |
| Information Retained | Uses all available information from the original scale [58]. | Loses information by reducing continuous measures to categories [58]. |
| Sample Size Requirements | Requires smaller sample sizes for equivalent power [58]. | Requires larger sample sizes to demonstrate equivalent effects. |
| Interpretability | May require clinical expertise to interpret magnitude of effect. | Often easier to communicate (e.g., response rates). |
| Case Study Example | HAQ improvement in rheumatoid arthritis detected more differences between anti-TNF agents [58]. | ACR 20 response in rheumatoid arthritis detected fewer differences between anti-TNF agents [58]. |
The Researcher's Toolkit for MTC
Table 4: Essential Methodological Tools for MTC Credibility Assessment
| Tool/Technique | Primary Function | Application Context |
|---|---|---|
| Network Graphs | Visual representation of the evidence structure [1]. | Initial screening for network connectivity and identification of potential evidence gaps. |
| Inconsistency Models | Statistical tests for disagreement between direct and indirect evidence [1]. | Validation of key assumption; should be applied whenever closed loops exist in the network. |
| Subgroup Analysis/Meta-Regression | Explore impact of clinical or methodological effect modifiers [1]. | Investigation of heterogeneity and assessment of similarity assumption. |
| Ranking Metrics (SUCRA) | Provide treatment hierarchy based on probability of being best/worst [2]. | Aid interpretation for decision-makers; should be presented with caution and uncertainty measures. |
| Risk of Bias Tools | Assess methodological quality of included studies. | Inform interpretation of findings and explore potential sources of bias in sensitivity analyses. |
Interpreting MTC Findings in HTA Submissions
When evaluating MTC results for HTA submissions, several critical interpretation factors must be considered:
Context of Evidence Gaps: MTC is particularly valuable when head-to-head trials are unavailable, unethical, or impractical. In such scenarios, MTC provides the best available evidence for comparative effectiveness [14] [17]. However, a 2011 case study demonstrated that direct evidence is not always more reliable than indirect evidence, highlighting the importance of a critical appraisal of all available evidence rather than an automatic preference for direct comparisons [57].
Dealing with Inconsistency: When significant inconsistency is detected between direct and indirect evidence, investigators should explore potential sources through subgroup analyses and meta-regression. In some cases, excluding studies causing inconsistency may be warranted, but this decision must be transparently reported and justified [57] [1].
Regulatory and HTA Perspective: Health technology assessment agencies increasingly accept MTC evidence but evaluate submissions on a case-by-case basis [14]. The acceptability of MTC submissions to HTA bodies remains variable, highlighting the need for clearer international consensus and guidance on methods [14]. Recent good practice guidelines for HTA emphasize transparency, stakeholder engagement, and appropriate institutional arrangements for implementation, all of which apply to the use of MTC within HTA [59].
The relationship between MTC, direct evidence, and the broader HTA decision-making context can be visualized as an interconnected system where different forms of evidence inform each other, as shown in the following diagram.
Figure 2: MTC Evidence Integration in HTA. This diagram shows how Mixed Treatment Comparisons synthesize both direct and indirect evidence to support HTA decision-making, with inconsistency checks creating a feedback loop for evidence re-evaluation.
Assessing the credibility of MTC for HTA submissions requires a multifaceted approach that systematically evaluates the evidence network structure, verifies key statistical assumptions, and interprets findings within the context of clinical and methodological considerations. The case study in febrile neutropenia demonstrated that direct evidence is not invariably more reliable than indirect evidence, reinforcing the value of combining all relevant evidence through MTC methodology [57].
As MTC methodologies continue to evolve, future directions include developing more sophisticated approaches for evaluating similarity assumptions, handling complex evidence structures with multi-arm trials, and establishing standardized reporting guidelines specific to MTC. For HTA submissions, transparency in all methodological choices, comprehensive sensitivity analyses, and cautious interpretation of treatment rankings remain paramount for demonstrating MTC credibility and supporting healthcare decision-making.
Comparative Analysis of MTC Performance Across Therapeutic Areas
Mixed Treatment Comparison (MTC), also commonly known as Network Meta-Analysis (NMA), represents a sophisticated methodological extension of traditional pairwise meta-analysis that allows for the simultaneous comparison of multiple interventions. This approach is particularly valuable in evidence-based healthcare evaluation when head-to-head randomized controlled trials (RCTs) are unavailable for all treatment comparisons of interest [18] [60]. By synthesizing both direct evidence (from trials comparing treatments directly) and indirect evidence (through a common comparator), MTC strengthens inferences concerning relative efficacy and facilitates simultaneous inference regarding all treatments within a connected network [18] [16].
The fundamental principle underlying MTC involves creating a connected network of treatment comparisons where each intervention is linked to every other through a pathway of direct or indirect comparisons [18]. This methodology has two primary roles: strengthening inference concerning the relative efficacy of two treatments by incorporating both direct and indirect evidence, and enabling simultaneous comparison and potential ranking of all treatments within the network [18]. As regulatory agencies and healthcare decision-makers increasingly require comparative effectiveness assessments, MTC has emerged as a powerful tool for informing clinical and policy decisions, particularly in therapeutic areas where multiple competing interventions exist but comprehensive direct comparison evidence is lacking [60].
Methodological Framework of MTC
Core Assumptions and Statistical Foundations
The methodological validity of MTC depends on several key assumptions that extend beyond those required for standard pairwise meta-analysis. The homogeneity assumption requires that trials included in the analysis are sufficiently similar in design and patient characteristics to be quantitatively combined. The similarity assumption necessitates that trials are comparable for potential effect modifiers across treatment comparisons. Most critically, the consistency assumption requires that direct and indirect evidence are in agreement, forming the foundation for valid quantitative combination of these evidence types [16].
MTC can be implemented using both frequentist and Bayesian statistical frameworks, with the Bayesian approach being particularly common due to its flexibility in handling complex evidence structures and producing probabilistic treatment rankings [18]. The Bayesian framework employs Markov chain Monte Carlo (MCMC) simulation methods, typically implemented using specialized software like WinBUGS or its open-source alternatives [16]. Model convergence is assessed through visualization of chain histories and statistical diagnostics, with inferences based on posterior distributions of relevant parameters such as odds ratios or mean differences with 95% credible intervals (the Bayesian equivalent of confidence intervals) [16].
Advancements in MTC Methodology
Recent methodological advancements have expanded the application of MTC to increasingly complex clinical scenarios. Component Network Meta-Analysis (CNMA) represents a significant innovation, particularly for evaluating complex interventions comprising multiple components [61]. Unlike standard MTC that estimates effects of entire interventions, CNMA disentangles the effects of individual components, enabling clinicians and policymakers to identify which components drive effectiveness, either alone or through synergistic interactions [61].
Another important development involves multivariate MTC models that simultaneously analyze multiple correlated outcomes. For instance, a bivariate Bayesian NMA can combine efficacy and safety outcomes to form a single probability ranking that accounts for both beneficial and harmful effects [62]. This approach offers advantages over traditional univariate methods, including improved precision in effect estimation, reduced outcome reporting bias, and the ability to model dependency between correlated outcomes [62].
The extension of MTC methodology to prognostic score comparison (Multiple Score Comparison meta-analysis) further demonstrates the versatility of these approaches, enabling concurrent external validation and comparison of multiple prognostic scores using individual patient data [63].
MTC Application Across Therapeutic Areas
Oncology
MTC has been extensively applied in oncology, where numerous treatment options often exist without comprehensive direct comparisons. The table below summarizes key characteristics of MTC applications in selected oncology fields:
Table 1: MTC Applications in Oncology
| Cancer Type | Number of Trials | Number of Interventions | Key Outcomes | Methodological Notes |
|---|---|---|---|---|
| Ovarian Cancer [18] | 198 | 120 | Overall survival | Combined first- and second-line treatments; interventions collapsed into class effects |
| Colorectal Cancer [18] | 242 | 137 | Overall survival, disease progression | Combined first-, second-, and third-line treatments; adjusted for improving patient status over time |
| Breast Cancer (Advanced) [18] | 370 | 22 | Overall survival | Classified interventions into "older combinations"; covered trials from 1971-2007 |
| Cancers of Unknown Primary [18] | 10 | 10 | Overall survival | Majority trials in untreated patients; small sample sizes |
| Non-small Cell Lung Cancer [18] | 6 | 4 | Overall survival | Focused exclusively on second-line treatments |
Oncologic MTC applications face unique challenges, including rapidly evolving treatment landscapes and changing patient populations over time. For example, a breast cancer MTC incorporating trials from 1971 to 2007 demonstrated shifting baseline risks, possibly reflecting the introduction of new co-interventions that improved outcomes over this period [18]. Similarly, an MTC in cancers of unknown primary sites noted a 6% performance status improvement per decade in enrolled patients, highlighting the importance of considering temporal trends in oncologic MTCs [18].
Chronic Disease Management
Rheumatoid Arthritis
MTC has played a crucial role in comparing the efficacy of anti-tumor necrosis factor (TNF) agents for rheumatoid arthritis (RA), where head-to-head trials are limited. A notable methodological study in RA compared continuous versus binary outcome measures in MTC models, demonstrating that continuous measures (such as mean change in Health Assessment Questionnaire score) provided greater power to detect between-treatment differences compared to dichotomized measures (such as ACR20 response rates) [64].
The analysis included 16 RCTs comparing five anti-TNF agents (adalimumab, certolizumab, etanercept, golimumab, and infliximab) against placebo or conventional disease-modifying antirheumatic drugs [64]. The continuous outcome analysis detected significant differences between treatments that were not identified using binary outcomes, highlighting how information loss during dichotomization translates to reduced sensitivity in MTC models [64].
Chronic Low Back Pain
A proposed bivariate Bayesian NMA for chronic low back pain exemplifies the application of multivariate MTC methods to balance efficacy and safety considerations [62]. This analysis aims to compare pharmacological interventions including NSAIDs, antidepressants, anticonvulsants, muscle relaxants, and weak opioids while excluding strong opioids due to dependency concerns [62]. The methodology incorporates both pain intensity scores and dropout rates due to adverse events, generating a single probability ranking that integrates both effectiveness and tolerability [62].
Public Health and Complex Interventions
MTC methods have been increasingly applied to evaluate complex public health interventions, which present unique methodological challenges due to their multicomponent nature [24]. A systematic review of 89 reviews applying NMA to complex public health interventions identified substantial diversity in how intervention nodes were formed, with nodes created by grouping similar interventions (65/102 networks), comparing named interventions (6/102), defining nodes as component combinations (26/102), or using component classification systems (5/102) [24].
This review proposed a typology of "node-making" elements organized around seven considerations: Approach, Ask, Aim, Appraise, Apply, Adapt, and Assess [24]. This framework addresses the critical methodological challenge of deciding between "splitting" versus "lumping" interventions and whether to conduct intervention-level versus component-level analysis when evaluating complex public health interventions [24].
Metabolic Disorders and Obesity
Recent applications of MTC methodology have extended to the evaluation of glucagon-like peptide-1 receptor agonists (GLP-1RAs) for weight management, though real-world evidence comparisons present unique challenges [65]. While RCT evidence demonstrates clear efficacy for GLP-1RAs including liraglutide, semaglutide, and tirzepatide, real-world effectiveness tends to be lower due to issues with adherence and discontinuation [65]. Real-world studies show discontinuation rates of 20-50% within the first year, with patients frequently using lower doses than those evaluated in clinical trials [65].
Comparative Performance of MTC Methods
Methodological Comparisons
A systematic evaluation compared the performance of MTC with adjusted indirect comparison methods across multiple therapeutic areas [16]. The analysis included 7 reviews encompassing 51 comparisons, with findings summarized below:
Table 2: Comparison of MTC and Adjusted Indirect Methods
| Comparison Metric | MTC Results | Adjusted Indirect Results | Clinical Implications |
|---|---|---|---|
| Statistically significant findings | 2 additional significant comparisons | Fewer significant comparisons | MTC may provide greater statistical power in complex networks |
| Direction of effect differences | Consistent in most comparisons | 6 examples of differing direction | Important potential for conflicting clinical recommendations |
| Confidence/credible interval precision | Generally more precise | Wider intervals in complex comparisons | MTC may provide more precise estimates in connected networks |
| Applicability to network structures | Suitable for all connected networks | Requires shared comparator | MTC offers greater flexibility for complex treatment networks |
The analysis found that in most comparisons, adjusted indirect methods yielded estimates of relative effectiveness similar to MTC approaches [16]. However, as comparisons became more complex, MTC demonstrated advantages in statistical power and estimation precision [16].
Component Network Meta-Analysis vs. Standard NMA
The emergence of Component Network Meta-Analysis (CNMA) has provided a methodological framework specifically designed for complex interventions [61]. The table below compares key characteristics of these approaches:
Table 3: CNMA vs. Standard NMA for Complex Interventions
| Characteristic | Standard NMA | CNMA |
|---|---|---|
| Unit of analysis | Entire interventions | Individual components |
| Assumption | Consistency between direct and indirect evidence | Additivity of component effects (unless interaction terms included) |
| Clinical utility | Identifies most effective intervention package | Identifies active components and synergistic/antagonistic interactions |
| Implementation complexity | Moderate | High (requires multidisciplinary team) |
| Data requirements | Network of intervention comparisons | Network including components and combinations |
CNMA enables estimation of individual component effects even when delivered in combination, addressing key clinical questions about which intervention components drive effectiveness [61]. For example, in a prehabilitation analysis evaluating exercise, nutrition, cognitive, and psychosocial components, CNMA could disentangle their individual contributions to preventing postoperative complications [61].
Experimental Protocols and Analytical Workflows
Standard MTC Analytical Workflow
The following diagram illustrates the standard analytical workflow for conducting an MTC:
MTC Analytical Workflow
The analytical process begins with a comprehensive systematic literature review to identify all relevant RCTs for the treatments and conditions of interest [62]. Following data extraction covering population characteristics, interventions, comparators, and outcomes, researchers map the network geometry to visualize connections between treatments [16]. Critical assessment of homogeneity and similarity assumptions precedes statistical model specification, which includes selection between fixed and random effects models based on heterogeneity considerations [18] [16]. The MTC analysis proper is conducted using either Bayesian or frequentist methods, followed by consistency evaluation between direct and indirect evidence [16]. The process concludes with treatment ranking and comprehensive sensitivity analyses to validate findings [62].
Component NMA Workflow
For complex interventions, CNMA follows a modified analytical workflow:
CNMA Analytical Workflow
The CNMA process begins with component identification and classification, engaging clinical experts to define meaningful intervention components [61]. Each intervention in the network is then coded according to its constituent components, followed by assessment of the additivity assumption [61]. Based on this assessment, researchers select either an additive CNMA model (assuming component effects sum linearly) or an interaction CNMA model (accommodating synergistic or antagonistic effects between components) [61]. The analysis proceeds with component effect estimation, with the interaction model additionally quantifying interaction effects [61]. The process concludes with model comparison and validation to select the most appropriate representation of the complex interventions [61].
The Scientist's Toolkit: Essential Research Reagents and Methodological Solutions
Table 4: Essential Methodological Tools for MTC Research
| Tool Category | Specific Solutions | Function & Application | Therapeutic Area Examples |
|---|---|---|---|
| Statistical Software | WinBUGS, R2BUGS, R with gemtc package | Bayesian MCMC implementation for complex MTC models | Oncology [18], Rheumatoid Arthritis [64] |
| Model Assessment Tools | Residual deviance, DIC, node-splitting | Goodness-of-fit evaluation and inconsistency detection | Multiple therapeutic areas [16] |
| Data Extraction Tools | WebPlotDigitizer | Data extraction from published figures when numerical data unavailable | Chronic low back pain [62] |
| Risk of Bias Assessment | Cochrane ROB tool, ROB2 | Methodological quality assessment of included trials | All therapeutic areas [62] |
| Evidence Grading Systems | GRADE framework | Quality assessment of MTC evidence | Public health interventions [24] |
| Visualization Tools | Network graphs, rankograms, forest plots | Results communication and network geometry representation | All therapeutic areas [63] |
Validation of MTC Results with Direct Evidence
The critical validation step in any MTC involves confirming consistency between direct and indirect evidence, which serves as a foundational assumption of the methodology [16]. Several statistical approaches exist for this validation, including the Bucher method for simple indirect comparisons, node-splitting techniques for detecting local inconsistency in specific comparisons, and design-by-treatment interaction models for assessing overall network consistency [16].
Empirical comparisons have demonstrated that in most analyses, adjusted indirect comparisons yield estimates of relative effectiveness equivalent to MTC approaches, particularly in less complex networks where all studies share a common comparator [16]. However, as networks become more complex, MTC may provide advantages through incorporation of both direct and indirect evidence within a single coherent analysis [60] [16].
A comprehensive evaluation of 51 comparisons across multiple therapeutic areas found only limited instances of significant differences between MTC and adjusted indirect comparison methods [16]. Specifically, researchers identified 2 examples where MTC results were statistically significant while adjusted indirect comparisons were not, 1 example of the reverse pattern, 6 examples where direction of effect differed between methods, and 9 examples where confidence intervals were importantly different [16]. These findings suggest that while methodological choices can influence results, both approaches generally provide similar inferences particularly in networks with shared comparators.
Recent methodological advancements have strengthened validation approaches, with multivariate MTC models offering the potential to reduce outcome reporting bias and improve precision through incorporation of correlated outcomes [62]. Additionally, the development of CNMA models enables more biologically plausible representations of complex interventions, potentially enhancing the validity of treatment effect estimates when component interactions are properly specified [61].
Mixed Treatment Comparison methodology has evolved substantially from its initial development, expanding from simple networks with common comparators to complex applications including component-based analyses and multivariate outcome models. Across therapeutic areas including oncology, chronic disease management, public health, and metabolic disorders, MTC has demonstrated value for comparative effectiveness research when direct evidence is limited.
The performance of MTC methods varies according to network characteristics, with advantages over simpler indirect comparison approaches becoming more pronounced in complex networks with multiple interconnected treatments. Critical evaluation of consistency assumptions remains essential, with recent methodological developments providing enhanced tools for validation of MTC results against direct evidence. As healthcare decision-makers increasingly require comparative effectiveness evidence for multiple competing interventions, proper application and validation of MTC methods will continue to play a crucial role in informing clinical and policy decisions across therapeutic areas.
Conclusion
Confirming Mixed Treatment Comparison results with direct evidence is not merely a statistical exercise but a fundamental requirement for credible evidence-based decision making. The synthesis of insights across all four intents reveals that successful validation hinges on a rigorous, multi-faceted approach: a solid understanding of foundational assumptions, meticulous application of methodological standards, proactive troubleshooting for inconsistency, and systematic comparative validation. As biomedical research continues to generate a proliferation of treatment options, the role of MTC and NMA will only grow in importance. Future directions should focus on developing more sophisticated methods for inconsistency detection, establishing standardized validation protocols accepted by global HTA agencies, and exploring the integration of real-world evidence to further strengthen MTC networks. By adhering to these principles, researchers can generate reliable, internally coherent treatment effect estimates that truly inform clinical and policy decisions.
References
- 1. Network meta-analysis: a technique to gather evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5386629/]
- 2. Network meta-analysis: a powerful tool for clinicians ... [https://www.sciencedirect.com/science/article/pii/S0895435624002932]
- 3. Combination of direct and indirect evidence in mixed ... [https://pubmed.ncbi.nlm.nih.gov/15449338/]
- 4. Chapter 11: Undertaking network meta-analyses [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-11]
- 5. Mixed treatment comparison analysis provides internally ... [https://www.sciencedirect.com/science/article/abs/pii/S0895435609003072]
- 6. Consistency and inconsistency in network meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4433772/]
- 7. A graphical tool for locating inconsistency in network meta ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-13-35]
- 8. Node-Splitting Generalized Linear Mixed Models for ... [https://www.sciencedirect.com/science/article/pii/S1098301516305812]
- 9. Impact of color-coded and warning nutrition labelling schemes [https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003765]
- 10. Development and design validation of a novel network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9189833/]
- 11. Mixed Treatment Comparison - York ... [https://www.yhec.co.uk/glossary-term/mixed-treatment-comparison/]
- 12. Critical evaluation of mixed treatment comparison meta†... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6878270/]
- 13. Report of the ISPOR Task Force on Indirect Treatment ... [https://www.sciencedirect.com/science/article/pii/S1098301511013283]
- 14. Methods for Indirect Treatment Comparison: Results from a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11036291/]
- 15. Meta-analysis and Mixed Treatment Comparison Analysis [https://www.ismpp-newsletter.com/2017/03/30/meta-analysis-and-mixed-treatment-comparison-analysis-powerful-tools-with-benefits-and-challenges/]
- 16. Incorporating multiple interventions in meta-analysis ... - Trials [https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-10-86]
- 17. Introduction - Use of Mixed Treatment Comparisons in ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK107325/]
- 18. Multiple treatment comparison meta-analyses: a step ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3130904/]
- 19. Interpreting Indirect Treatment Comparisons and Network ... [https://www.sciencedirect.com/science/article/pii/S1098301511014045]
- 20. Fixed Effect Versus Random Effects Models in Meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12571769/]
- 21. Fixed-Effect or Random-Effects Models? How to Choose, ... [https://www.preprints.org/manuscript/202509.0126/v1]
- 22. Methods resources for authors new to conducting ... [https://www.sciencedirect.com/science/article/pii/S0895435625000927]
- 23. Methods resources for authors new to conducting ... [https://pubmed.ncbi.nlm.nih.gov/40107390/]
- 24. A methodological review of network meta-analyses applied ... [https://www.sciencedirect.com/science/article/pii/S0895435625001891]
- 25. Validation of The Umbrella Collaboration for Tertiary Evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12262930/]
- 26. Validation of The Umbrella Collaboration for Tertiary Evidence ... [https://formative.jmir.org/2025/1/e75215]
- 27. A systematic review and meta-analysis of the efficacy and ... [https://www.nature.com/articles/s41591-025-03978-z]
- 28. An introduction to network meta-analysis (mixed treatment ... [https://www.quantics.co.uk/blog/an-introduction-to-network-meta-analysis/]
- 29. Network Meta-Analysis (Mixed Treatment Comparison ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK536651/]
- 30. Conducting Indirect Treatment Comparison and Network ... [https://www.ispor.org/heor-resources/good-practices/article/conducting-indirect-treatment-comparison-and-network-meta-analysis-studies]
- 31. Indirect Treatment Comparisons in Health Technology ... [https://www.ispor.org/heor-resources/presentations-database/presentation-cti/ispor-europe-2025/poster-session-3-2/indirect-treatment-comparisons-in-health-technology-assessment-submissions-a-review-and-critique-of-best-practice]
- 32. Trends in Indirect Treatment Comparison (ITC) Methods ... [https://www.ispor.org/heor-resources/presentations-database/presentation-cti/ispor-2025/poster-session-1/trends-in-indirect-treatment-comparison-itc-methods-used-in-reimbursement-submissions-in-canada-and-the-us]
- 33. An Early Start: Preliminary Indirect Treatment Comparison ... [https://www.ispor.org/heor-resources/presentations-database/presentation-cti/ispor-europe-2025/methodological-developments-in-indirect-treatment-comparisons-and-network-meta-analyses/an-early-start-preliminary-indirect-treatment-comparison-assessments-informing-evidence-generation-planning-for-joint-clinical-assessment]
- 34. Network meta-analysis: The way forward for evidence- ... [https://www.sciencedirect.com/science/article/pii/S2213398424000277]
- 35. Evaluation of inconsistency in networks of interventions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5411010/]
- 36. Identifying inconsistency in network metaâ€analysis: Is the net ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6899484/]
- 37. 5 Tips For Understanding Network Meta-Analysis [https://absolutelymaybe.plos.org/2024/02/01/5-tips-for-understanding-network-meta-analysis/]
- 38. Checking consistency in mixed treatment comparison meta ... [https://pubmed.ncbi.nlm.nih.gov/20213715/]
- 39. Path-Based Approach for Detecting and Assessing ... [https://arxiv.org/html/2506.20364v1]
- 40. A Comparison of Two Models for Detecting Inconsistency ... [https://eric.ed.gov/?q=source%3A%22Research+Synthesis+Methods%22&ff1=subComparative+Analysis&id=EJ1447267]
- 41. Evidence Synthesis for Decision Making 4: Inconsistency in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3704208/]
- 42. Prevalence of evidence of inconsistency and its association ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-021-01401-y]
- 43. Publication bias - Importance of studies with negative results! [https://pmc.ncbi.nlm.nih.gov/articles/PMC6573059/]
- 44. Evidence Synthesis for Decision Making 3 [https://pmc.ncbi.nlm.nih.gov/articles/PMC3704206/]
- 45. Re-evaluating heterogeneity in evidence synthesis [https://ecoevorxiv.org/repository/view/8866/]
- 46. The results of direct and indirect treatment comparisons in ... [https://www.sciencedirect.com/science/article/abs/pii/S0895435697000498]
- 47. Bayesian mixed treatment comparisons meta-analysis for correlated outcomes subject to reporting bias [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5846497/]
- 48. A method for assessing robustness of the results of a star- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8171049/]
- 49. Top 6 Statistical Methods in Network Meta-Analysis Uncovered [https://www.numberanalytics.com/blog/top-6-statistical-methods-network-meta-analysis-uncovered]
- 50. Results - Use of Mixed Treatment Comparisons in Systematic ... [https://www.ncbi.nlm.nih.gov/books/NBK107335/]
- 51. Combining treatment effects from mixed populations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11963434/]
- 52. Experiments and Quantitative Research [https://researchmethodscommunity.sagepub.com/blog/experiments-quantitative-methodologies]
- 53. cambridge.org/core/journals/international-journal-of-technology... [https://www.cambridge.org/core/journals/international-journal-of-technology-assessment-in-health-care/article/abs/direct-versus-indirect-comparisons-a-summary-of-the-evidence/CA5C46615EB22CC0174DC451E9F9189B]
- 54. Experimental data and design, and the role of statistics [https://www.sciencedirect.com/science/article/abs/pii/S0263931909001720]
- 55. Selection of indirect treatment comparisons for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11938225/]
- 56. Simulation evaluation of statistical properties of methods for ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-12-138]
- 57. Consistency between Direct and Indirect Trial Evidence [https://www.sciencedirect.com/science/article/pii/S1098301511014823]
- 58. The use of continuous data versus binary data in MTC models [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-12-167]
- 59. Good Practices for Health Technology Assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11703621/]
- 60. How Valuable are Multiple Treatment Comparison ... [https://www.sciencedirect.com/science/article/pii/S1098301510000306]
- 61. Analysing complex interventions using component network ... [https://www.medrxiv.org/content/10.1101/2025.06.30.25330567v1.full-text]
- 62. A Systematic Review and Bivariate Bayesian Network Meta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12481260/]
- 63. Multiple Score Comparison: a network meta-analysis ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-017-0433-2]
- 64. The use of continuous data versus binary data in MTC models [https://pmc.ncbi.nlm.nih.gov/articles/PMC3576322/]
- 65. Realâ€world evidence on the utilization, clinical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12000858/]