Strategic Framework for Formulating Key Questions in Drug Comparative Effectiveness Research (CER)
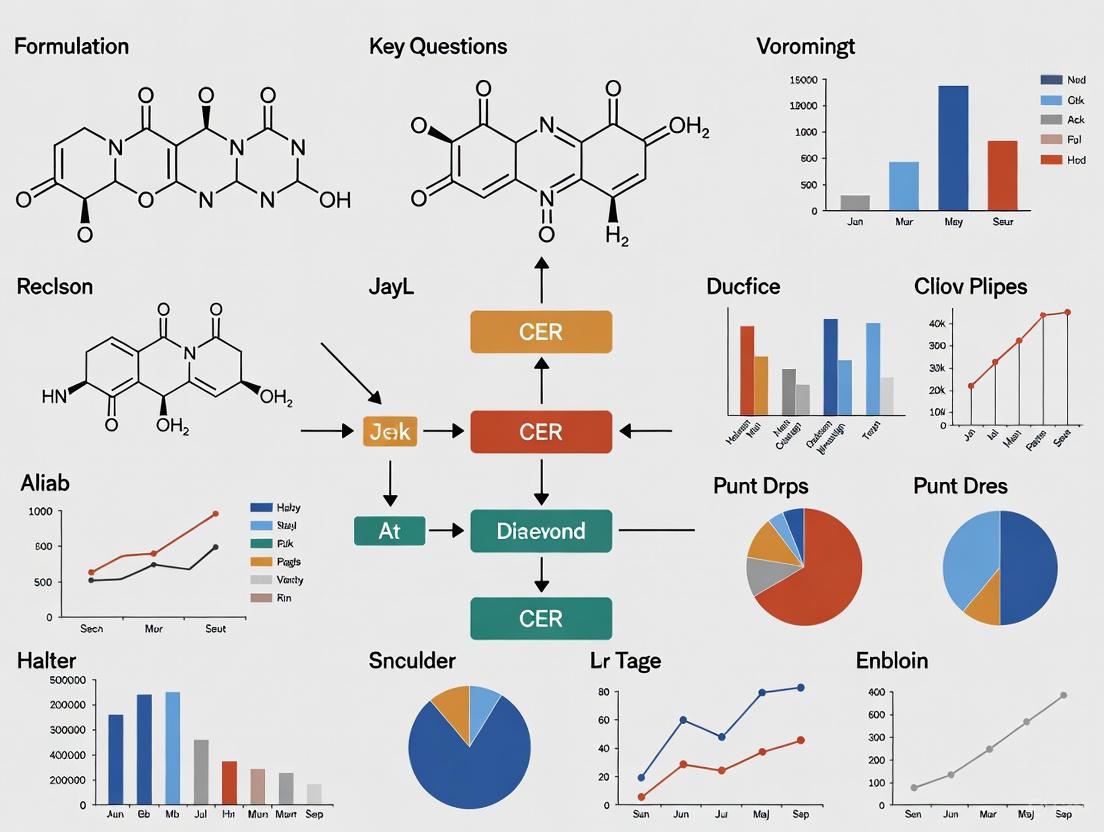
This article provides a comprehensive guide for researchers and drug development professionals on formulating pivotal questions for Drug Comparative Effectiveness Research (CER).
Strategic Framework for Formulating Key Questions in Drug Comparative Effectiveness Research (CER)
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on formulating pivotal questions for Drug Comparative Effectiveness Research (CER). It outlines a strategic framework covering foundational principles, methodological applications, troubleshooting for common challenges, and validation techniques. By addressing these four core intents, the guide aims to enhance the design, execution, and regulatory acceptance of CER studies, ultimately supporting the development of safe and effective medicines with robust, real-world evidence.
Laying the Groundwork: Core Principles and Regulatory Expectations for Drug CER
Understanding the Purpose of CER in the Drug Development Lifecycle
Comparative Effectiveness Research (CER) plays a pivotal role in the modern drug development lifecycle by generating evidence on the benefits and harms of available treatment options for specific patient populations. Framed within the context of formulating key research questions, CER moves beyond establishing whether a treatment works under ideal conditions (efficacy) to determine how it performs in real-world settings against alternative therapies (effectiveness). This in-depth guide explores the methodologies and standards for integrating CER throughout drug development to inform critical healthcare decisions.
The Fundamental Role of CER in Drug Development
CER transforms drug development from a linear process focused solely on regulatory approval to a more dynamic, evidence-driven lifecycle that emphasizes value to patients and healthcare systems. Its core purpose is to fill critical evidence gaps that exist after a drug's initial efficacy and safety are established, providing answers that are directly relevant to patients, clinicians, and payers [1]. This is achieved by comparing drugs, medical devices, tests, surgeries, or ways to deliver healthcare to determine which work best for which patients and under what circumstances [2].
The integration of CER is particularly crucial as the industry faces rising challenges, including the complexity of new therapies like cell and gene treatments, increased regulatory scrutiny, and pressure to contain costs [3]. By providing robust evidence on a treatment's real-world performance, CER helps maximize the return on investment in drug development by ensuring that new products can demonstrably improve patient outcomes relative to existing alternatives. Furthermore, a well-executed CER strategy supports the adoption of new therapies by providing the evidence needed for reimbursement decisions and clinical guideline development.
Formulating Key Questions for CER Studies
The foundation of valid and useful CER lies in the meticulous formulation of its research questions. This process ensures that the study addresses decisions of genuine importance and produces actionable results.
The PICOTS Framework
A structured approach to defining the research scope is the PICOTS framework, which delineates the Population, Interventions, Comparators, Outcomes, Timeframe, and Setting of the study [2]. This framework forces researchers to precisely define each component, reducing ambiguity and ensuring the research is fit-for-purpose to inform a specific health decision.
- Population: CER should strive to include participants representative of the spectrum of the population of interest, including those historically underrepresented in research [1]. This is critical for understanding how treatment effects may vary across subgroups.
- Interventions and Comparators: The interventions and comparators must correspond to actual healthcare options faced by patients and providers. "Usual care" or "non-use" comparator groups should generally be avoided unless they represent legitimate and coherent clinical options [1].
- Outcomes: CER must measure outcomes that the population of interest notices and cares about, such as survival, functioning, symptoms, and health-related quality of life [1]. These are known as patient-centered outcomes.
- Timeframe and Setting: The study duration and the real-world or routine practice setting in which it is conducted are essential for assessing the practical effectiveness of a treatment.
Engaging Stakeholders in Question Development
A hallmark of patient-centered CER is the early and meaningful engagement of stakeholders in formulating research questions. Stakeholders include individuals affected by the condition, their caregivers, clinicians, payers, and policy makers [1]. Their involvement increases the applicability of the study to end-users and facilitates the translation of results into practice [2]. Engaging patients helps ensure that the selected outcomes are truly meaningful to those living with the disease, moving beyond purely clinical or surrogate endpoints to those that impact daily life.
Synthesizing Evidence and Conceptualizing the Problem
Before designing a new CER study, researchers must conduct a comprehensive review and synthesis of the existing knowledge base. This involves identifying systematic reviews, critically appraising published studies, and pinpointing where evidence is absent, insufficient, or conflicting [2]. This synthesis justifies the need for the new research. Furthermore, developing a conceptual model or framework is recommended to diagram the theorized relationships between the treatment, outcome, and other key variables, which guides the entire study design [2].
Methodologies and Experimental Protocols in CER
CER employs a variety of study designs, each with specific protocols tailored to generate robust real-world evidence.
Core CER Study Designs
| Study Design | Description | Key Protocol Considerations | Best Use Cases |
|---|---|---|---|
| Randomized Controlled Trials (Pragmatic) | Participants are randomly assigned to treatment groups in a real-world setting. | Design should align closely with routine clinical practice; broad eligibility criteria; use of patient-centered outcomes [4]. | Considered the gold standard for causal inference when feasible to conduct; ideal for head-to-head comparisons of active treatments. |
| Observational Studies | Analyzes data from real-world settings (e.g., EHRs, claims) without intervention. | Must use causal models (e.g., DAGs) to identify and control for confounding; clearly define "time zero" and follow-up to avoid immortal time bias [2] [5]. | When RCTs are not ethical or practical; to study long-term safety and effectiveness; to assess treatment effects in diverse populations. |
| Master Protocols (Umbrella, Basket, Platform) | Complex trials that evaluate multiple therapies or diseases within a single, overarching structure [6]. | Protocol must define biomarker stratification (umbrella), common molecular alteration (basket), or adaptive entry/exit of treatments (platform) [6]. | Accelerating development in precision medicine, especially in oncology and rare diseases with genetic markers. |
Visualization for Causal Inference and Study Design
Visual tools are critical for ensuring transparency and validity in CER, particularly in observational studies.
Causal Diagram (DAG)
Observational Study Timeline
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key resources required for conducting rigorous CER.
| Item/Resource | Function in CER | Technical Specifications |
|---|---|---|
| Real-World Data (RWD) | Provides information on patient health status and/or delivery of healthcare from diverse sources. | Includes Electronic Health Records (EHRs), claims data, patient registries. Must be assessed for reliability (accuracy, completeness) and relevance (availability of key data elements) [5]. |
| Validated Patient-Reported Outcome (PRO) Measures | Instruments to directly capture the patient's perspective on their health status. | Must demonstrate content validity, construct validity, reliability, and responsiveness to change in the population of interest [1]. |
| Directed Acyclic Graph (DAG) Tools | Software to create and analyze causal diagrams for identifying confounding variables. | Tools like DAGitty (free, web- or R-based) help identify the minimally sufficient set of covariates to control for to reduce bias [5]. |
| Standardized Protocol Templates | Provides a structured format for developing a detailed study protocol. | ICH M11 template (FDA recommended), NIH templates for clinical trials, and NCI templates for oncology studies ensure all key components are addressed [6]. |
| Glycinexylidide | Glycinexylidide, CAS:18865-38-8, MF:C10H14N2O, MW:178.23 g/mol | Chemical Reagent |
| Creatine Monohydrate | Creatine Monohydrate|High-Purity Reagent|RUO | High-purity Creatine Monohydrate for research. Study energy metabolism, neuroprotection, and myopathies. For Research Use Only. Not for human consumption. |
Data Integrity, Visualization, and Regulatory Compliance
Maintaining the highest standards of data integrity is paramount for CER to be trusted by decision-makers.
Data Management and Analysis Plans
A formal Data Management Plan (DMP) is critical, specifying how data will be collected, organized, handled, preserved, and shared to ensure it is accessible and reproducible [1]. Furthermore, an a priori Statistical Analysis Plan (SAP) must be specified in the study protocol before analysis begins. This includes defining key exposures, outcomes, covariates, plans for handling missing data, and approaches for subgroup and sensitivity analyses [1].
Regulatory and Reporting Standards
CER must adhere to evolving regulatory expectations for data presentation and transparency. The FDA has issued guidelines on standard formats for tables and figures in submissions to enhance clarity and consistency [7]. Furthermore, study results must be registered in public platforms like ClinicalTrials.gov and reported according to established guidelines such as CONSORT for randomized trials or STROBE for observational studies [1]. Engaging with regulatory agencies early through mechanisms like pre-ANDA meetings is encouraged, especially for complex products [8].
Integrating Comparative Effectiveness Research throughout the drug development lifecycle is no longer optional but essential for demonstrating the real-world value of new therapeutics. By rigorously formulating research questions using the PICOTS framework, engaging stakeholders, employing appropriate and transparent methodologies, and adhering to the highest standards of data integrity, researchers can generate the evidence needed to inform critical health decisions. This patient-centered approach ensures that the drug development process ultimately delivers not just new medicines, but treatments that truly improve outcomes that matter to patients.
Navigating Key FDA Regulatory Pathways and Guidance Documents
The U.S. Food and Drug Administration (FDA) provides several regulatory pathways to facilitate efficient drug development and approval, particularly for serious conditions and rare diseases. Understanding these pathways is crucial for designing robust Comparative Effectiveness Research (CER) that meets regulatory standards. These pathways balance the need for rigorous evidence with practical considerations for diseases where traditional randomized controlled trials may be infeasible. Recent innovations, including the Plausible Mechanism Pathway announced in November 2025, reflect FDA's evolving approach to evidence generation for targeted therapies [9] [10]. This guide examines key pathways, recent guidance documents, and methodological considerations essential for drug development professionals.
Core FDA Regulatory Pathways
Accelerated Approval Program
The Accelerated Approval Program allows earlier approval of drugs that treat serious conditions and fill an unmet medical need based on a surrogate endpoint [11]. A surrogate endpoint is a marker—such as a laboratory measurement, radiographic image, or physical sign—that is reasonably likely to predict clinical benefit but is not itself a measure of clinical benefit. This approach can considerably shorten the time required prior to receiving FDA approval.
- Post-Approval Requirements: Sponsors must conduct studies to confirm the anticipated clinical benefit. If confirmatory trials verify clinical benefit, the drug receives traditional approval. If not, FDA has regulatory procedures that could lead to removing the drug from the market [11].
- Applicability: This pathway is particularly valuable for diseases where long-term outcomes take considerable time to measure, but shorter-term surrogate endpoints have been validated.
Plausible Mechanism Pathway
Announced in November 2025, the Plausible Mechanism Pathway represents a significant shift in FDA's approach to bespoke therapies, especially for ultra-rare conditions where randomized trials are not feasible [9] [10]. This pathway operates under FDA's existing statutory authorities and requires clinical data meeting statutory standards of safety and efficacy.
The pathway is built around five core elements that must be demonstrated through successive patients with different bespoke therapies:
- Specific Molecular Abnormality: Identification of a specific molecular or cellular abnormality with a direct causal link to the disease, not a broad set of consensus diagnostic criteria [9] [10].
- Targeted Biological Alteration: The medical product must target the underlying or proximate biological alterations [9] [10].
- Characterized Natural History: Well-characterized natural history of the disease in the untreated population [9] [10].
- Confirmed Target Engagement: Evidence exists confirming that the target was successfully drugged or edited, which may come from biopsies or non-animal models [9].
- Clinical Improvement: Demonstration of improvement in clinical outcomes or disease course that excludes regression to the mean [9] [10].
- Postmarket Evidence Requirements: Sponsors must collect real-world evidence (RWE) to demonstrate preservation of efficacy, absence of off-target edits, effect of early treatment on childhood development milestones, and detection of unexpected safety signals [9].
- Therapeutic Scope: While initially focused on cell and gene therapies for rare childhood diseases, the pathway is also available for common diseases with no proven alternatives or considerable unmet need after available therapies [9] [10].
Rare Disease Evidence Principles (RDEP)
The Rare Disease Evidence Principles (RDEP) process, announced in September 2025, facilitates approval of drugs for rare diseases with known genetic defects that drive pathophysiology [9]. To be eligible, products must target conditions with:
- A known, in-born genetic defect as the major disease driver
- Progressive deterioration leading to significant disability or death
- Very small patient populations (e.g., fewer than 1,000 persons in the U.S.)
- Lack of adequate alternative therapies that alter disease course
Under RDEP, substantial evidence of effectiveness can be established through one adequate and well-controlled trial (which may be single-arm) accompanied by robust confirmatory evidence, which may include appropriately selected external controls or natural history studies [9].
Comparison of Key Pathways
Table: Comparative Analysis of FDA Drug Development Pathways
| Pathway Feature | Accelerated Approval | Plausible Mechanism Pathway | Rare Disease Evidence Principles |
|---|---|---|---|
| Evidence Standard | Surrogate endpoint reasonably likely to predict clinical benefit | Five core elements demonstrating biological targeting and clinical improvement | One adequate well-controlled trial plus confirmatory evidence |
| Postmarket Requirements | Confirmatory trial required | RWE collection for efficacy preservation, safety signals, and off-target effects | Not specified in available documents |
| Population Focus | Serious conditions with unmet need | Ultra-rare diseases, initially fatal or severely disabling childhood conditions | Rare diseases with known genetic defects (<1,000 U.S. patients) |
| Trial Design Flexibility | Traditional trial designs | Successive single-patient demonstrations | Single-arm trials with external controls accepted |
| Statistical Evidence Level | Standard statistical thresholds | Clinical data strong enough to exclude regression to the mean | "Robust data" providing strong confirmatory evidence |
Recent FDA Guidance Documents for Drug Development
Clinical Trial Design and Conduct
- Innovative Designs for Clinical Trials of Cellular and Gene Therapy Products in Small Populations (September 2025): This draft guidance provides recommendations for planning, designing, conducting, and analyzing trials for cell and gene therapy products in rare diseases [12]. It describes considerations for using various trial designs and endpoints to generate clinical evidence supporting product licensure when patient populations are limited [12].
- Conducting Clinical Trials With Decentralized Elements (Final, September 2024): This guidance offers recommendations for implementing decentralized elements in clinical trials, which can facilitate patient recruitment and retention in rare disease studies [13].
- E20 Adaptive Designs for Clinical Trials (Draft, September 2025): This ICH guidance addresses the use of adaptive designs that may modify trial specifications based on accumulating data while maintaining trial integrity and validity [13].
Gene Therapy and Rare Disease Development
- Expedited Programs for Regenerative Medicine Therapies for Serious Conditions (Draft, September 2025): This guidance outlines expedited programs available for regenerative medicine therapies, including those for rare diseases [14].
- Accelerated Approval of Human Gene Therapy Products for Rare Diseases (Planned 2025 Guidance): This carried-over guidance from 2024 is expected to provide specific recommendations for obtaining accelerated approval for gene therapies targeting rare conditions [15].
- Postapproval Methods to Capture Safety and Efficacy Data for Cell and Gene Therapy Products (Draft, September 2025): This guidance discusses methods for collecting postapproval data, particularly relevant for products approved under novel pathways like the Plausible Mechanism Pathway [14].
Analytical and Computational Approaches
- Considerations for the Use of Artificial Intelligence To Support Regulatory Decision-Making (Draft, January 2025): This guidance addresses the use of AI in regulatory decision-making for drug and biological products [13].
- M15 General Principles for Model-Informed Drug Development (Draft, December 2024): This ICH guidance provides principles for using quantitative models in drug development to support regulatory decision-making [13].
- Real-World Data: Assessing Electronic Health Records and Medical Claims Data (Final, July 2024): This guidance supports the use of real-world data in regulatory decision-making, particularly relevant for postmarket evidence generation [13].
Table: Recent FDA Guidance Documents Relevant to Drug CER Research
| Guidance Document Title | Issue Date | Status | CER Research Relevance |
|---|---|---|---|
| Innovative Designs for Clinical Trials of Cellular and Gene Therapy Products in Small Populations | 09/2025 | Draft | Alternative trial designs for limited populations |
| Considerations for the Use of Artificial Intelligence To Support Regulatory Decision-Making | 01/2025 | Draft | AI applications in regulatory science |
| Patient-Focused Drug Development: Selecting, Developing, or Modifying Fit-for-Purpose Clinical Outcome Assessments | 10/2025 | Final | Patient-centered endpoint development |
| Real-World Data: Assessing Electronic Health Records and Medical Claims Data | 07/2024 | Final | RWD assessment for regulatory decisions |
| Integrating Randomized Controlled Trials for Drug and Biological Products Into Routine Clinical Practice | 09/2024 | Draft | Hybrid trial designs incorporating real-world evidence |
| Clinical Pharmacology Considerations for Human Radiolabeled Mass Balance Studies | 07/2024 | Final | Drug disposition and metabolism studies |
| M14 General Principles on Plan, Design, and Analysis of Pharmacoepidemiological Studies That Utilize Real-World Data | 07/2024 | Draft | RWE study design methodologies |
Experimental Design and Methodological Considerations
Framework for Plausible Mechanism Pathway Applications
The Plausible Mechanism Pathway requires specific methodological approaches to establish product effectiveness [9] [10]. The following workflow outlines key experimental components:
Key Research Reagents and Materials
Table: Essential Research Reagents for Targeted Therapy Development
| Reagent/Material | Function in CER Research | Regulatory Application |
|---|---|---|
| Gene Editing Components (CRISPR-Cas systems, base editors) | Precise modification of disease-associated genetic targets | Demonstration of target engagement for Plausible Mechanism Pathway |
| Animal Disease Models | Preliminary efficacy and safety assessment | Limited use; FDA encourages non-animal models where possible |
| Non-Animal Model Systems (organoids, microphysiological systems) | Target validation and therapeutic screening | Alternative to animal studies per FDA's updated stance |
| Molecular Diagnostic Assays | Patient selection and molecular abnormality confirmation | Eligibility determination for targeted therapies |
| Biomarker Assay Kits | Target engagement measurement and pharmacodynamic assessment | Confirmatory evidence for biological activity |
| Next-Generation Sequencing Platforms | Comprehensive molecular characterization and off-target effect assessment | Safety evaluation and molecular abnormality identification |
| Flow Cytometry Panels | Cellular phenotype and immune cell profiling | Cellular abnormality characterization and product potency assessment |
Natural History Study Methodology
Natural history studies form a critical evidence component for rare disease therapeutic development, particularly under the Plausible Mechanism Pathway and RDEP [9]. A robust natural history study should include:
- Prospective Data Collection: Standardized collection of clinical, patient-reported, and biomarker data at regular intervals in untreated patients
- Comprehensive Phenotyping: Detailed characterization of disease manifestations, progression patterns, and variability
- Biomarker Correlations: Association between molecular measures and clinical outcomes
- Endpoint Validation: Development of clinically meaningful endpoints for interventional trials
- Statistical Considerations: Appropriate handling of missing data, patient heterogeneity, and disease trajectory modeling
Regulatory Strategy and CER Research Questions
Pathway Selection Framework
Choosing the appropriate regulatory pathway requires systematic assessment of product and disease characteristics. Key considerations include:
- Population Size and Distribution: The Plausible Mechanism Pathway and RDEP are specifically designed for very small populations (under 1,000 U.S. patients) where traditional trials are infeasible [9]
- Understanding of Disease Biology: The Plausible Mechanism Pathway requires a known and specific molecular abnormality with direct causal relationship to disease [9] [10]
- Endpoint Selection and Validation: Accelerated Approval requires surrogate endpoints reasonably likely to predict clinical benefit, while traditional approval requires direct clinical benefit demonstration [11]
- Manufacturing Considerations: Bespoke therapies under the Plausible Mechanism Pathway must demonstrate consistent manufacturing despite product individualization [10]
Formulating CER Research Questions for Regulatory Submissions
Well-designed CER research questions should align with pathway-specific evidence requirements:
- For Plausible Mechanism Pathway: "Does successive application of bespoke therapies targeting distinct molecular abnormalities in the same disease class demonstrate consistent target engagement and clinical improvement across multiple patients?" [9] [10]
- For Accelerated Approval: "To what extent does the proposed surrogate endpoint correlate with long-term clinical outcomes in the target population, and what level of surrogate validation exists?" [11]
- For RDEP Applications: "Can a single-arm trial with carefully matched historical controls and comprehensive natural history data provide substantial evidence of effectiveness for a genetic disorder affecting <1,000 U.S. patients?" [9]
Emerging Trends and Future Directions
FDA's regulatory science continues evolving, with several notable developments impacting CER research:
- Real-World Evidence Integration: Recent guidances support using RWE for regulatory decisions, particularly in postmarket settings [13]
- Artificial Intelligence Applications: FDA is developing frameworks for AI/ML in drug development and regulatory decision-making [13]
- Complex Innovative Trial Designs: Adaptive, basket, and platform trials are increasingly accepted for targeted therapies and rare diseases [13] [12]
- Patient-Focused Endpoint Development: Recent guidances emphasize incorporating patient experience into endpoint selection and modification [13]
These developments highlight the growing flexibility in FDA's approach to evidence generation while maintaining rigorous standards for safety and effectiveness demonstration.
Defining the research scope throughout the drug development lifecycle represents a critical strategic exercise that directly impacts a product's ultimate success or failure. The contemporary drug development landscape faces a fundamental paradox: despite massive increases in research and development expenditure, the number of yearly approvals for new molecular entities has remained stagnant, with 40–50% of development programs being discontinued even in clinical Phase III [16]. This inefficiency underscores the vital importance of precisely scoping research questions and methodology at each development stage to build a compelling evidence portfolio.
Within this context, comparative effectiveness research (CER) has emerged as a crucial paradigm for evaluating and comparing the benefits and harms of alternative healthcare interventions to inform real-world clinical and policy decisions [17]. This technical guide provides a structured framework for formulating key questions for drug CER research across preclinical, clinical, and post-marketing phases, enabling researchers to establish a scientifically valid scope that generates meaningful evidence for healthcare decision-makers.
Quantitative Foundations for Research Scoping
Core Quantitative Disciplines in Drug Development
The strategic scoping of drug development research relies heavily upon several interconnected quantitative disciplines. Understanding these foundational approaches is essential for formulating precise research questions.
Table 1: Key Quantitative Disciplines in Drug Development Scoping
| Discipline | Definition | Primary Application in Research Scoping |
|---|---|---|
| PK-PD Modeling | Mathematical approach linking drug concentration over time to the intensity of observed response [16] | Describes complete time course of effect intensity in response to dosing regimens |
| Exposure-Response Modeling | Similar to PK-PD modeling but uses exposure metrics (AUC, Cmax, Css) and any type of response (efficacy, safety) [16] | Bridges preclinical and clinical findings; supports dose selection and trial design |
| Pharmacometrics | Scientific discipline using mathematical models based on biology, pharmacology, physiology for quantifying drug-patient interactions [16] | Integrates data from various sources; quantitative decision-making across development phases |
| Quantitative Pharmacology | Multidisciplinary approach integrating relationships between diseases, drug characteristics, and individual variability across studies [16] | Moves away from study-centric approach to continuous quantitative integration |
| Model-Based Drug Development (MBDD) | Paradigm promoting modeling as both instrument and aim of drug development [16] | Formal summary of all available information; full utilization throughout development |
The Model-Based Drug Development Framework
Model-based drug development represents a fundamental mindset shift in which models constitute both the instruments and aims of drug development efforts [16]. Unlike traditional approaches, MBDD covers the whole spectrum of the drug development process instead of being limited to specific modeling techniques or application areas. This approach uses available data, information, and knowledge to their maximum potential to improve development efficiency, forming an iterative cycle where a well-designed MBDD strategy enhances model quality, which in turn refines the development strategy [16].
In practice, MBDD applies modeling to diverse aspects of drug development, including drug design, target screening, formulation choices, exposure-biomarker response, disease progression, healthcare outcome, patient behavior, and socio-economic impact [16]. Knowledge in these areas is formally summarized and reflected in these models and carried over to subsequent development steps, creating a continuous knowledge base rather than siloed stage-specific data.
Phase-Specific Research Scoping Frameworks
Preclinical Research Scoping
Key Scoping Questions for Preclinical Research
The preclinical phase requires scoping research questions that effectively bridge from discovery to first-in-human studies. Critical questions include:
- What are the fundamental mechanisms of action and how do they modulate disease pathways?
- What pharmacokinetic properties (absorption, distribution, metabolism, excretion) demonstrate adequate exposure at the target site?
- What efficacy biomarkers correlate with target engagement and disease modification?
- What safety margins exist between efficacious and toxic exposures across relevant species?
- How does the candidate compound compare to existing standard of care treatments in predictive models?
Antitarget Assessment and Safety Profiling
A crucial aspect of preclinical scoping involves assessing interactions with "antitargets" – human proteins associated with adverse drug reactions that should not interact with drugs [18]. Quantitative and qualitative structure-activity relationship models ((Q)SAR) represent valuable tools for predicting these interactions, with studies showing that qualitative SAR models demonstrate higher balanced accuracy (0.80-0.81) than quantitative QSAR models (0.73-0.76) for predicting Ki and IC50 values of antitarget inhibitors [18].
Table 2: Experimental Protocols for Preclinical Antitarget Assessment
| Protocol Component | Methodology Description | Key Outputs |
|---|---|---|
| Data Set Curation | Extract structures and experimental Ki/IC50 values from databases (e.g., ChEMBL); transform to pIC50 = -log10(IC50(M)) and pKi = -log10(Ki(M)); use median values for compounds with multiple measurements [18] | Standardized data sets with >100 compounds per antitarget |
| Model Creation | Use GUSAR software with QNA and MNA descriptors; apply self-consistent regression; validate via fivefold cross-validation [18] | Validated (Q)SAR models with defined accuracy metrics |
| Applicability Domain Assessment | Determine compounds falling within model applicability domain; higher for SAR models versus test sets [18] | Reliability assessment for specific compound predictions |
Clinical Development Scoping
Quantitative and Systems Pharmacology Framework
The clinical development phase benefits tremendously from a quantitative and systems pharmacology approach, which integrates physiology and pharmacology to accelerate medical research [19]. QSP provides a holistic understanding of interactions between the human body, diseases, and drugs by simultaneously considering receptor-ligand interactions of various cell types, metabolic pathways, signaling networks, and disease biomarkers [19].
A key advantage of QSP is its ability to integrate data and knowledge through both "horizontal" and "vertical" integration. Horizontal integration entails going beyond narrow focus on specific pathways or targets to understand them within broader contexts by simultaneously considering multiple receptors, cell types, metabolic pathways, or signaling networks. Vertical integration involves integrating knowledge across multiple time and space scales, allowing models to capture both short-term dynamics (e.g., hourly variations in plasma glucose) and longer-term outcomes (e.g., HbA1c levels over months to years) [19].
Clinical Trial Scoping with CER Principles
When scoping clinical trials for comparative effectiveness, researchers should design studies that "address critical decisions faced by patients, families, caregivers, clinicians, and the health and healthcare community and for which there is insufficient evidence" [20]. Proposed trials should compare interventions that already have robust evidence of efficacy and are in current use, focusing on practical clinical dilemmas rather than establishing preliminary efficacy [21].
The Patient-Centered Outcomes Research Institute recommends that CER trials employ a two-phase funding approach where an initial feasibility phase (up to 18 months, $2 million direct costs) supports study refinement, infrastructure establishment, patient and stakeholder engagement, and feasibility testing of study operations [20]. This is followed by a full-scale study phase (up to five years, $20 million direct costs) contingent on achieving specific milestones from the feasibility phase [21].
Post-Marketing Research Scoping
Proactive Safety Surveillance Scoping
Post-marketing research scoping must address the reality that serious safety issues often emerge only after products are marketed to larger, more diverse populations. Analysis of FDA data reveals that among 219 new molecular entities approved from 1997-2009, 11 experienced safety withdrawal and 30 received boxed warnings by 2016 [22]. Contrary to prevailing hypotheses, neither clinical trial sample sizes nor review time windows were associated with post-marketing boxed warnings or safety withdrawals [22].
However, drugs approved with either a boxed warning or priority review were significantly more likely to experience post-marketing boxed warnings (3.88 and 3.51 times more likely, respectively) [22]. This suggests that post-marketing research scoping should prioritize these higher-risk products for intensified surveillance.
Post-Marketing Clinical Follow-up Framework
Under the European Medical Device Regulation framework – which offers relevant parallels for pharmaceutical post-marketing requirements – manufacturers must establish a Post-Market Clinical Follow-up plan as a continuous process to proactively collect and evaluate clinical data [23]. The clinical evaluation must be updated regularly throughout the product lifecycle, particularly when new post-market surveillance data emerges that could affect the current evaluation or its conclusions [24].
Table 3: Post-Marketing Safety Signal Detection Framework
| Pre-marketing Factor | Association with Post-marketing Safety Events | Implications for Research Scoping |
|---|---|---|
| Clinical Trial Sample Size | No significant association [22] | Larger pre-approval trials alone unlikely to predict safety issues |
| Review Time Windows | No significant association [22] | Regulatory review deadlines not primary factor in missed safety signals |
| Initial Boxed Warning | 3.88x more likely to receive post-marketing boxed warning [22] | Prioritize intensified monitoring for drugs with initial boxed warnings |
| Priority Review Status | 3.51x more likely to receive post-marketing boxed warning [22] | Enhanced surveillance pathways for rapidly approved drugs |
| Therapeutic Category | Varied by specific category [22] | Category-specific risk profiles should inform monitoring intensity |
The Scientist's Toolkit: Essential Research Reagents and Solutions
GUSAR Software: Utilizes quantitative neighborhoods of atoms and multilevel neighborhoods of atoms descriptors for (Q)SAR model creation; employs self-consistent regression for predicting antitarget interactions and compound activity [18].
Physiology-Based Pharmacokinetic Modeling Tools: Provide mechanistic insights into complex and novel modalities; estimate drug distribution in remote compartments; accommodate different populations (pediatrics, elderly, impaired renal function) [19].
Ordinary Differential Equation Solvers: Implement sophisticated mathematical models representing mechanistic details of pathophysiology; capture data from multiple scales from molecular to clinical outcomes [19].
ChEMBL Database: Publicly available database providing structures and experimental Ki and IC50 values for compounds tested on inhibition of various targets; essential for creating training sets for (Q)SAR models [18].
Post-Market Surveillance Data Systems: Systems for collecting clinically relevant post-market surveillance data with emphasis on post-market clinical follow-up; crucial for updating clinical evaluations [24].
Healthcare Administrative Databases: Sources for real-world data on comparative effectiveness and safety of pharmaceutical drugs; particularly valuable for assessing outcomes in population subgroups underrepresented in clinical trials [17].
Integrated Scoping Framework for Drug CER
Cross-Phase Research Question Alignment
Effective research scoping requires alignment of questions across all development phases to build a coherent evidence portfolio for comparative effectiveness. The following diagram illustrates the integration of CER principles throughout the drug development lifecycle:
Stakeholder Engagement in Research Scoping
Meaningful patient and stakeholder engagement represents an essential component of effective research scoping throughout development. The Patient-Centered Outcomes Research Institute's "Foundational Expectations for Partnerships in Research" provides a systematic framework for this engagement, emphasizing multiple approaches along a continuum from input to shared leadership [20] [25]. This engagement is particularly crucial during the feasibility phase of CER trials to ensure that research questions address genuine decisional dilemmas faced by patients and clinicians [21].
Defining research scope from preclinical to post-marketing phases requires a systematic, integrated approach that embraces model-based development frameworks, proactively addresses comparative effectiveness questions, and engages relevant stakeholders throughout the process. By implementing the structured scoping frameworks outlined in this technical guide, drug development professionals can formulate precise research questions that generate meaningful evidence for healthcare decision-makers, ultimately improving the efficiency and success rate of drug development programs. The beneficiaries of this disciplined approach to research scoping will ultimately be the patients in need of safe, effective, and properly targeted therapies.
Identifying Critical Stakeholders and Information Needs
Identifying critical stakeholders and their information needs is not an administrative formality but a foundational scientific activity in drug comparative effectiveness research (CER). It ensures that the research addresses questions that are not only clinically relevant but also meaningful to the end-users of the evidence: patients, clinicians, and healthcare systems. CER is fundamentally defined by its purpose to "assist consumers, clinicians, purchasers, and policy-makers to make informed decisions" [26]. A well-formulated CER question thus rests on a precise understanding of which stakeholders are critical and what evidence they require to make those decisions. This guide provides a technical roadmap for researchers to systematically integrate this stakeholder analysis into the earliest phases of drug CER study design.
Defining and Identifying Critical Stakeholders in Drug CER
A Standardized Definition and Categorization
In the context of drug CER, a stakeholder is defined as "Individuals, organizations or communities that have a direct interest in the process and outcomes of a project, research or policy endeavor" [26]. This definition emphasizes the vested interest these groups have in the research findings and their application.
Stakeholder engagement is the iterative process of actively soliciting their knowledge and values to create a shared understanding and enable relevant, transparent decisions [26]. For drug development professionals, moving beyond a simple list to a categorized and prioritized inventory is crucial. The following table synthesizes key stakeholder groups and their primary CER interests.
Table 1: Key Stakeholder Groups and Their Core Interests in Drug CER
| Stakeholder Group | Typical CER Interests & Information Needs |
|---|---|
| Patients & Caregivers | Outcomes that matter to daily life (quality of life, symptoms, function); treatment side effects; out-of-pocket costs; understanding of uncertain or negative results [27] [28] [29]. |
| Clinicians | Comparative safety and efficacy in real-world patients; evidence for specific subpopulations; practical implementation of treatments; impact on clinical workflows [27] [26]. |
| Payers & Policymakers | Value relative to existing standards of care; cost-effectiveness; budget impact; generalizability of findings to broader populations [26] [30]. |
| Pharmaceutical Industry | Evidence for product differentiation; value proposition; regulatory and reimbursement requirements; impact on innovation incentives [26] [31]. |
| Research Funders | Relevance of research to address evidence gaps; methodological rigor; potential for findings to be implemented and improve care [27]. |
| 5-Deoxystrigol | 5-Deoxystrigol, CAS:151716-18-6, MF:C19H22O5, MW:330.4 g/mol |
| Quinovic acid | Quinovic acid, CAS:465-74-7, MF:C30H46O5, MW:486.7 g/mol |
Methodological Protocol: The Stakeholder Identification and Analysis Process
A rigorous, multi-step approach ensures no critical perspective is overlooked. The following protocol, adapted from project management and CER-specific literature, provides a detailed methodology [26] [32].
Protocol: Five-Step Stakeholder Analysis
- Stakeholder Identification: Brainstorm a comprehensive list of all potential individuals, groups, and organizations affected by the drug or the CER question. Use techniques like snowball sampling, where identified stakeholders suggest others.
- Stakeholder Mapping and Categorization: Plot stakeholders on an influence/interest matrix. This visual tool helps categorize them as:
- High Power, High Interest: Key players who require close engagement (e.g., primary funders, regulatory bodies).
- High Power, Low Interest: Groups that need to be kept satisfied (e.g., senior organizational leadership).
- Low Power, High Interest: Groups to keep informed (e.g., patient advocacy groups, specific clinician societies).
- Low Power, Low Interest: Groups to monitor with minimal effort.
- Requirements Analysis: For each key stakeholder group, document their specific derived requirements—both communicated and uncommunicated. This goes beyond technical specs to include needs for communication frequency, format, and involvement in the research process [32].
- Interrelationship Analysis: Map the interfaces and relationships between different stakeholder groups. Understanding potential coalitions, conflicts, or overlaps of interest is critical for managing the engagement process effectively.
- Strategy Development and Monitoring: Create a tailored communication and engagement plan for each stakeholder group. This plan should be revisited at major project milestones, as stakeholder interests and influence can change throughout the research lifecycle [32].
The diagram below visualizes the iterative workflow for identifying and analyzing stakeholders.
Eliciting and Structuring Information Needs
The Spectrum of Information Needs
Information needs represent the specific evidence gaps that stakeholders seek to fill to make an informed decision. For drug CER, these needs can be thematically organized. Patient needs often center on "awareness-oriented needs," which include understanding the nature of the disease, how to control it, and the details of treatment options and complications [28]. A systematic review of cancer screening information needs further refines this, showing that needs evolve along an event timeline, focusing on risk factors, benefits/harms of interventions, detailed procedures, and result interpretation [33].
Different stakeholders prioritize different information. For instance, while patients highly value information from genetics professionals and healthcare workers, the internet is also a highly utilized source [29]. This underscores the need for CER to produce evidence that is not only robust but also accessible and communicable through various channels.
Methodological Protocol: Qualitative Assessment of Information Needs
To move from assumptions to validated information needs, researchers should employ structured qualitative methodologies.
Protocol: Conducting a Qualitative Needs Assessment
- Study Design: Conventional qualitative content analysis using a descriptive-explorative design.
- Data Collection: In-depth, semi-structured interviews and/or focus groups. Interviews should be conducted in a setting and language preferred by the participant to ensure comfort and candor [28] [29].
- Interview Guide Development: Develop a guide with open-ended questions, such as:
- "Please explain your informational needs when you first began considering this treatment."
- "What information is most important for you when deciding between different medications?"
- "Can you provide an example of a time you felt you lacked the information to make a good health decision?"
- Sampling: Purposive sampling is used to ensure a diversity of perspectives (e.g., patients of different ages, disease stages, clinicians from different specialties). Data collection continues until thematic saturation is achieved, typically after 10-15 interviews [28].
- Data Analysis: Interviews are audio-recorded, transcribed verbatim, and analyzed systematically.
- The text is divided into meaning units (words, sentences, or paragraphs related by content).
- Meaning units are condensed while preserving the core concept.
- Condensed units are coded.
- Codes are grouped into sub-categories and then abstracted into categories representing the main informational themes [28].
- Trustworthiness: Techniques like peer checking among researchers and member checking (where findings are validated with participants) enhance the credibility and confirmability of the results [28].
The quantitative data from a systematic review of cancer screening information needs demonstrates the prevalence of specific topics, providing a model for how drug CER needs can be categorized.
Table 2: Categorized Information Needs from a Systematic Review of Cancer Screening (Model for Drug CER) [33]
| Theme (by Event Timeline) | Specific Information Needs | Associated Factors for Information-Seeking |
|---|---|---|
| Background & Importance | Disease risk factors; signs and symptoms; importance of early detection. | Passive Attention: Driven by demographic factors (age, education) and fear of the disease. |
| Benefits, Harms & Decision-Making | Comparative benefits and harms of available options; what to expect during and after. | Active Searching: Primarily triggered by a lack of information or a specific decision point. |
| Procedural Details | The detailed screening/treatment process; preparation required; duration. | Information Channel Preference: Interpersonal (clinicians), traditional media, or internet-based. |
| Results & Follow-up | How and when results are provided; interpretation of results; next steps. | Editorial Tone Preference: Desire for clear, understandable, non-judgmental language. |
The Researcher's Toolkit: Essential Reagents for Stakeholder Engagement
Executing a rigorous stakeholder and information needs analysis requires specific methodological "reagents." The following table details these essential tools and their functions for the research team.
Table 3: Research Reagent Solutions for Stakeholder and Needs Analysis
| Research Reagent / Tool | Function in the CER Formulation Process |
|---|---|
| Stakeholder Interview Guide | A semi-structured protocol to ensure consistent, open-ended elicitation of needs and expectations across diverse stakeholders. |
| Influence/Interest Matrix | A 2x2 grid used as a visual mapping tool to categorize and prioritize stakeholders based on their relative power and interest in the CER project. |
| Qualitative Data Analysis Software (e.g., NVivo) | Software designed to manage, code, and analyze non-numerical data from interviews and focus groups, aiding in the identification of themes and categories. |
| Stakeholder Engagement Plan | A living document that outlines tailored communication strategies, frequency of engagement, and responsible parties for each key stakeholder group. |
| Informed Consent Forms | Ethical and regulatory documents ensuring participants understand the study's purpose, the use of their data, and their rights, particularly crucial when engaging patients. |
| CER Priority-Setting Framework (e.g., from CANCERGEN) | A structured process, potentially involving an External Stakeholder Advisory Group (ESAG), to formally prioritize CER topics and study designs based on stakeholder input [26]. |
| Epitulipinolide diepoxide | Epitulipinolide diepoxide, CAS:39815-40-2, MF:C17H22O6, MW:322.4 g/mol |
| Acetylcephalotaxine | Acetylcephalotaxine, CAS:24274-60-0, MF:C20H23NO5, MW:357.4 g/mol |
Integrating Stakeholder Input into CER Question Formulation
The ultimate output of this analytical process is a sharply defined, patient-centered CER question. The gathered data on stakeholder-specific information needs directly informs the PICOT (Population, Intervention, Comparator, Outcome, Time) framework:
- Population: Defined by stakeholder-identified subpopulations of interest (e.g., by age, comorbidities, genetic markers).
- Intervention & Comparator: Chosen based on the clinical dilemmas most frequently cited by clinicians and patients.
- Outcomes: Centered on the outcomes that matter most to patients and caregivers, such as quality of life, functional status, and symptom burden, rather than solely on biomedical biomarkers [27].
- Time: Informed by the time horizons relevant to decision-making, such as short-term side effects versus long-term survival or functional decline.
This integration ensures the resulting CER study is relevant, practical, and has a clear pathway to implementation, ultimately fulfilling the core mission of CER: to provide useful, trustworthy evidence to those who need it most [27].
Establishing the Foundation for Patient-Centered Outcomes
Comparative clinical effectiveness research (CER) is fundamental to understanding which healthcare options work best for specific patient populations. When applied to drug development, patient-centered outcomes research (PCOR) ensures that the evidence generated addresses the questions and outcomes that matter most to patients and those who care for them. The core objective is to provide patients, clinicians, and other stakeholders with the evidence needed to make better-informed health decisions [34]. This guide details the foundational elements—from conceptual frameworks and methodological rigor to practical implementation—required to formulate key questions and conduct robust, patient-centered drug CER.
Foundational Principles of Patient-Centered CER
Patient-centered CER, as championed by the Patient-Centered Outcomes Research Institute (PCORI), is defined by several core principles. It directly compares two or more healthcare options, generating evidence about any differences in potential benefits or harms [34]. Crucially, it emphasizes the engagement of patients, caregivers, and the broader healthcare community as equitable partners throughout the entire research process [35]. These individuals leverage their lived experience to make the research more relevant, useful, and patient-centered. The ultimate goal is to bridge the gap between research and practice, ensuring findings are disseminated and implemented to improve care delivery and patient outcomes [35].
Methodological Frameworks for Drug CER
Formulating the Core Research Question
A well-defined research question is the cornerstone of any CER study. For drug-related CER, the question must be comparative, patient-centered, and actionable. The PIO (Population, Intervention, Outcome) framework is a standard starting point, expanded to include the key comparator.
- Population: Precisely define the patient population, including disease characteristics, severity, comorbidities, and prior treatments. Consider subgroups that may experience differential benefits or harms.
- Intervention: Specify the drug therapy, including dosage, administration route, and treatment duration.
- Comparator: Define the alternative against which the intervention is being compared. This could be another active drug, a different dosage of the same drug, a placebo, or non-drug therapy.
- Outcomes: Identify the outcomes that matter to patients. These typically go beyond traditional clinical endpoints (e.g., biomarker levels) to include patient-reported outcomes (PROs) like quality of life, symptom burden, functional status, and treatment burden.
The SPIRIT 2025 Framework for Protocol Development
A complete, transparent protocol is critical for the planning, conduct, and reporting of randomised trials, which are often the source of CER evidence. The updated SPIRIT 2025 statement provides an evidence-based checklist of 34 minimum items to address in a trial protocol, reflecting methodological advances and a greater emphasis on open science and patient involvement [36]. Key updates relevant to drug CER include:
- Item 5 (Protocol and Statistical Analysis Plan): Guidance on where the trial protocol and statistical analysis plan can be accessed, promoting transparency [36].
- Item 6 (Data Sharing): Details on where and how individual de-identified participant data, statistical code, and other materials will be accessible [36].
- Item 11 (Patient and Public Involvement): A new, critical item requiring details on how patients and the public will be involved in the trial's design, conduct, and reporting [36]. This formalizes the principle of patient-centeredness within the research protocol.
Adherence to SPIRIT 2025 enhances the transparency and completeness of trial protocols, benefiting investigators, trial participants, funders, and journals [36].
Visualizing the Patient-Centered CER Workflow
The following diagram illustrates the integrated, iterative workflow for establishing patient-centered outcomes in drug research, highlighting key stages from stakeholder engagement to evidence dissemination.
Current Priorities and Experimental Protocols in Drug CER
Landscape of Active CER Research
PCORI's recent funding announcements highlight active priority areas in drug CER, which serve as practical examples of the framework in action. These studies often compare drug therapies to other interventions or evaluate different strategies for using medications [34].
Table 1: Examples of Recent Patient-Centered Drug CER Studies
| Health Focus | Comparative Interventions | Patient-Centered Outcome |
|---|---|---|
| Pediatric Infections [34] | Commonly prescribed antibiotics vs. placebo | Resolution of acute ear and sinus infections |
| Pediatric & Adult Weight Management [34] | Different intensities of behavioral/lifestyle treatments paired with obesity medication | Effective and sustainable weight loss |
| Chronic Low Back Pain [34] | Drug therapies vs. non-drug therapies (e.g., physical therapy) | Pain reduction and improved function |
| Severe Aortic Stenosis [34] | Surgical vs. transcatheter aortic valve replacement | Procedure success, recovery time, and quality of life |
Detailed Protocol for a CER Trial on Pediatric Antibiotics
The following workflow details the methodology for a CER study comparing antibiotics to placebo for acute otitis media, incorporating SPIRIT 2025 and patient-centered principles.
Protocol Title: A Randomized, Double-Blind, Placebo-Controlled Trial Comparing Amoxicillin-Clavulanate to Placebo for the Management of Acute Otitis Media in Children.
1. Background & Rationale: Despite the high prevalence of antibiotic prescriptions for pediatric acute otitis media (AOM), evidence on the balance of benefits and harms for uncomplicated cases is contested. This study aims to provide clear, comparative evidence on whether antibiotics significantly improve patient-centered outcomes compared to supportive care alone.
2. Objectives:
- Primary Objective: To compare the effect of amoxicillin-clavulanate versus placebo on the duration of significant ear pain, as reported by parents/caregivers.
- Secondary Objectives: To compare the rates of treatment failure, use of rescue analgesics, overall symptom burden, and occurrence of adverse events (e.g., diarrhea, rash).
3. Methods:
- Trial Design: Multicenter, randomized, double-blind, placebo-controlled trial.
- Participants (P): Children aged 6-12 years with a clinical diagnosis of uncomplicated AOM.
- Intervention (I): Oral amoxicillin-clavulanate (dose based on weight) for 7 days.
- Comparator (C): Matching oral placebo for 7 days.
- Outcomes (O):
- Primary Outcome: Time from randomization to resolution of significant ear pain, measured twice daily via a validated patient-reported outcome (PRO) diary completed by parents.
- Secondary Outcomes:
- Proportion of participants requiring rescue medication within 72 hours.
- Overall symptom severity score (AOM-SOS) over days 1-7.
- Incidence of treatment-related adverse events.
- Rate of disease recurrence within 30 days.
4. Patient and Public Involvement (SPIRIT Item 11): A parent advisory panel was involved in the final selection of the primary outcome measure and the design of the patient-facing materials and diary to ensure they are clear and feasible for use in a stressful home environment.
5. Data Analysis: A time-to-event analysis (Kaplan-Meier curves and Cox proportional hazards model) will be used for the primary outcome. The statistical analysis plan (SAP) was finalized before database lock and is publicly available.
The Scientist's Toolkit: Essential Reagents for CER
Successful execution of patient-centered CER relies on a suite of methodological "reagents" and tools. The following table details key resources for ensuring methodological rigor, patient engagement, and data integrity.
Table 2: Essential Research Reagent Solutions for Patient-Centered CER
| Tool / Resource | Function in CER | Relevance to Patient-Centeredness |
|---|---|---|
| SPIRIT 2025 Checklist [36] | Provides a structured framework for drafting a complete and transparent trial protocol. | Includes a specific item (Item 11) mandating the description of patient and public involvement in design, conduct, and reporting. |
| PCORI Methodology Standards | A comprehensive set of methodological standards for conducting rigorous, patient-centered CER. | Guides researchers on how to incorporate patient perspectives in design and ensure studies address outcomes important to patients. |
| Patient-Reported Outcome (PRO) Measures | Validated instruments (e.g., diaries, questionnaires) to directly capture the patient's experience of their health. | Moves beyond clinical biomarkers to measure what matters most to patients, such as symptom burden and quality of life. |
| Structured Data Sharing Platforms | Repositories and systems for making de-identified participant data and analytical code accessible. | Promotes transparency, reproducibility, and allows for further research by other scientists, maximizing the value of patient participation. |
| WebAIM Contrast Checker [37] [38] | Tool to verify color contrast ratios in patient-facing digital materials (e.g., ePRO apps, consent forms). | Ensures accessibility for users with low vision or color blindness, aligning with inclusivity principles. Meets WCAG AA standards (4.5:1 for normal text) [37]. |
| Hypocrellin A | Hypocrellin A|CAS 77029-83-5|For Research Use | Hypocrellin A is a natural perylenequinone photosensitizer for cancer PDT, antiviral, and antimicrobial research. For Research Use Only. Not for human use. |
| COMC-6 | 2-Crotonyloxymethyl-2-cyclohexenone|Antitumor Research | 2-Crotonyloxymethyl-2-cyclohexenone is a cytotoxic compound for cancer research. This product is For Research Use Only. Not for human or personal use. |
Implementation and Future Directions
Establishing a foundation for patient-centered outcomes is an active process that extends beyond the research study's conclusion. The ultimate value of CER is realized when evidence is implemented into clinical practice. PCORI's Health Systems Implementation Initiative (HSII) is an example of this, funding projects that accelerate the uptake of practice-changing findings into care delivery settings [34]. Future directions in the field are being shaped by several key trends, including a focus on improving enrollment of underrepresented study populations to ensure equity, leveraging artificial intelligence for more efficient data management and analysis, and prioritizing complete data transparency between sponsors and contract research organizations (CROs) to improve trial quality and trust [39]. By adhering to rigorous methodologies, engaging patients as authentic partners, and embracing evolving standards and technologies, researchers can consistently generate drug CER evidence that is not only scientifically sound but also meaningful and useful for real-world decision-making.
From Theory to Practice: Designing and Implementing Robust CER Studies
The Clinical Evaluation Plan (CEP) serves as the foundational roadmap for generating the clinical evidence required to demonstrate a drug's safety and efficacy within the European Union's regulatory framework. More than just regulatory paperwork, a well-constructed CEP is a strategic document that directs a systematic and planned process to continuously generate, collect, analyze, and assess the clinical data pertaining to a device in order to verify its safety and performance, including clinical benefits, when used as intended [23]. For drug developers, the CEP establishes the rationale and methodology for the entire clinical evaluation process, ensuring that the subsequent Clinical Evaluation Report (CER) provides sufficient, robust evidence for market approval under the Medical Device Regulation (MDR) [24] [40].
The development of a CEP must be framed within the broader context of formulating precise research questions that will guide evidence generation. A "fail fast" approach in drug discovery emphasizes identifying molecules that lack desired efficacy, safety, or performance characteristics early, saving significant time and resources [41]. Similarly, a rigorously developed CEP helps prevent "fail later" situations by addressing potential formulation, manufacturing, and clinical evidence challenges during the planning phase rather than during regulatory review [41]. This proactive approach is particularly crucial for complex biologic drugs, where issues such as aggregation, degradation, and three-dimensional structure stability can significantly impact biological activity and must be carefully considered during evaluation planning [41].
Formulating Key Research Questions for Drug CER
The foundation of a successful CER protocol lies in formulating rigorous research questions that will direct the evidence generation strategy. The PICO framework (Patient/population; Intervention; Comparison; Outcome) provides a structured approach to ensure research questions encompass all relevant components [42] [43]. For drug development, this framework can be adapted to ensure the CEP addresses all critical aspects of clinical evaluation.
PICO Component Specification for Drugs
Table: PICO Framework Adaptation for Drug CER Protocols
| PICO Component | Definition | Drug Development Considerations |
|---|---|---|
| Patient/Population | The subjects of interest [42] | Define specific patient groups by age, medical condition, disease severity, contraindications, and previous treatment history [42] [23]. |
| Intervention | The drug formulation and administration being studied [42] | Specify drug type, dosage form, strength, route of administration, dosing frequency, and delivery system. For biologics, include details on structure and stability [41]. |
| Comparison | The alternative against which the intervention is measured [42] | Define appropriate comparators (active drugs, placebo, usual care, sham procedures) and specify their details as closely as the intervention [42]. |
| Outcome | The effects being evaluated [42] | Define primary and secondary outcomes (economic, clinical, humanistic), considering beneficial outcomes and potential harms. Specify outcome measures and assessment timepoints [42] [23]. |
Beyond proper construction, research questions must be capable of producing valuable and achievable results. The FINER criteria (Feasible; Interesting; Novel; Ethical; Relevant) provide a tool for evaluating research questions for practical considerations [42]:
- Feasible: Consider availability of resources including funding, time, institutional support, data accessibility, and required personnel expertise [42].
- Interesting: The question should appeal to both the researcher and the wider scientific community, making the eventual findings more competitive for funding and publication [42].
- Novel: The question should address a clear knowledge gap through a rigorous literature review, either by improving upon previous studies, investigating unknown areas, or purposefully replicating existing work [42].
- Ethical: Researchers must consider ethical implications and engage with appropriate oversight bodies during the early conceptualization phase [42].
- Relevant: The question should have significance to scientific knowledge, clinical practice, and policy decisions [42].
Research Question Formulation Workflow
The following diagram illustrates the systematic process for developing research questions within a CER protocol:
Core Components of a Comprehensive CER Protocol
A robust CER protocol must systematically address all regulatory requirements while establishing a clear methodology for evidence generation and assessment. The following components are essential for MDR compliance and demonstrating sufficient clinical evidence.
Strategic Planning and Scope Definition
The initial section of the CEP establishes the foundation for the entire clinical evaluation:
- Device/Drug Intended Purpose: Precisely define the therapeutic indication, target population with clear indications and contraindications, and the intended clinical benefits to patients [23].
- Clinical Claims and Acceptance Criteria: Specify clinical claims relevant to performance, safety, and benefits, along with specific thresholds that will serve as acceptance criteria for determining clinical acceptability [23].
- State of the Art Definition: Establish the current, generally accepted best practices and standards in medical technology and treatment for the condition, which serves as a benchmark for comparing the drug's performance and risk-benefit profile [23].
- Evaluation Strategy: Define the approach for demonstrating compliance with the MDR, which may rely on clinical data pertaining to the drug under evaluation and/or other approaches such as equivalence [23].
Clinical Development Plan
The CEP should outline a clinical development plan that describes the progression from early exploratory investigations to confirmatory studies and post-market clinical follow-up (PMCF), including milestones and acceptance criteria [23]. This plan should explicitly address:
- Data Sources Identification: Specify sources for obtaining relevant clinical data (literature reviews, manufacturer-sponsored clinical studies, post-market surveillance reports, registries, etc.) [24] [23].
- Literature Search Protocol: Detail the methodology for systematic literature reviews, including search strategies, databases, inclusion/exclusion criteria, and quality assessment methods to ensure objective, non-biased review methods [23].
- Equivalence Demonstration (if applicable): For drugs claiming equivalence to an existing product, establish detailed justification and evidence supporting equivalence in clinical, technical, and biological characteristics [23].
- Post-Market Clinical Follow-up (PMCF) Planning: Define the strategy for proactively collecting and evaluating clinical data from the use of the drug after market entry to update the clinical evaluation throughout the device lifecycle [24] [23].
Methodology for Data Identification, Appraisal, and Analysis
The CEP must establish rigorous methodologies for handling clinical data:
- Data Identification Process: Describe systematic approaches for identifying all pertinent data, both favorable and unfavorable, from published literature and manufacturer-held sources [23].
- Data Appraisal Framework: Define criteria for objectively evaluating the scientific validity and relevance of included data, including study design quality, potential biases, and statistical robustness [23].
- Data Analysis Plan: Specify analytical methods for synthesizing evidence across studies, assessing consistency of results, and evaluating the overall body of evidence regarding safety and performance [23].
- Benefit-Risk Assessment Methodology: Establish parameters for determining the acceptability of the benefit-risk ratio, including methods for qualitative and quantitative assessment of clinical safety, residual risks, and side effects [23].
Regulatory Framework and Compliance Requirements
Understanding the regulatory context is essential for developing a compliant CER protocol. The European Medical Device Regulation (MDR 2017/745) imposes specific requirements for clinical evaluations that manufacturers must follow throughout the device lifecycle.
Regulatory Evolution and Current Standards
The MDR introduced significantly stricter requirements compared to the previous Medical Device Directive (MDD), including [23]:
- Mandatory PMCF: Requirement for continuous clinical data collection post-market approval [23].
- Explicit CEP Requirement: Formal requirement for a documented Clinical Evaluation Plan [23].
- Stricter Equivalence Criteria: More rigorous requirements for demonstrating equivalence to existing products [23].
- Sufficient Clinical Evidence: Introduction of the concept of "sufficient clinical evidence," interpreted as "the present result of the qualified assessment which has reached the conclusion that the device is safe and achieves the intended benefits" [23].
Clinical Evaluation Process Workflow
The clinical evaluation follows a defined process from planning through reporting and updating, as shown in the following workflow:
This continuous process requires regular updates to the CER throughout the device lifecycle, particularly when new post-market surveillance (PMS) or PMCF data emerges that could affect the current evaluation or its conclusions [24].
Experimental Protocols and Data Quality Assessment
Robust experimental protocols and rigorous data quality assessment are fundamental to generating valid clinical evidence for the CER.
Essential Research Reagents and Materials
Table: Key Research Reagent Solutions for Drug CER
| Reagent/Material | Function in CER Development | Application Context |
|---|---|---|
| Systematic Review Software | Facilitates structured literature search, data extraction, and quality assessment of clinical studies | Literature review and data identification phase [23] |
| Data Quality Assessment Framework | Provides systematic approach to evaluate completeness, accuracy, and reliability of clinical data | Appraisal of all relevant clinical data from various sources [44] |
| Statistical Analysis Tools | Enable quantitative synthesis of clinical evidence, meta-analysis, and benefit-risk modeling | Data analysis phase for synthesizing evidence across studies [23] |
| Predictive Modeling Programs | Assist in determining dose frequency, formulation stability, and route of administration | Early development phase for informing clinical trial design [41] |
| Biomarker Assay Kits | Provide objective measures of drug activity, safety parameters, and treatment response | Clinical studies for generating supplemental evidence of mechanism [41] |
Data Quality Assessment Framework
For CERs leveraging real-world data or secondary data sources, a comprehensive data quality assessment (DQA) framework is essential. The harmonized DQA model developed through the Electronic Data Methods Forum addresses key dimensions [44]:
- Completeness: Assessment of missing data elements that could impact study validity, with explicit definitions tailored to specific research needs [44].
- Accuracy: Evaluation of data correctness through validation against source documents or through consistency checks across related data elements [44].
- Consistency: Determination of whether data values are consistent across time and between related data elements within the dataset [44].
- Plausibility: Assessment of whether data values are clinically meaningful and within expected ranges for the patient population [44].
- Timeliness: Evaluation of whether data is current and available within the required timeframes for analysis [44].
The DQA process should generate standardized reports such as the Observational Source Characteristics Analysis Report (OSCAR) for summarizing data source characteristics and Generalized Review of OSCAR Unified Checking (GROUCH) for identifying implausible or suspicious data patterns [44].
Common Pitfalls and Best Practices
Strategies to Overcome Common Challenges
Drug developers frequently encounter several challenges when preparing CER protocols:
- Insufficient Clinical Evidence: Provide robust evidence for all populations, indications, and device variants. Gaps in clinical evidence are frequently challenged by notified bodies and may result in non-conformities [23].
- CEP-CER Inconsistency: Adhere to the CEP throughout the evaluation process. Document any necessary deviations thoroughly, as inconsistencies between the CEP and CER often result in non-conformities [23].
- Inadequate Benefit-Risk Analysis: Develop a structured, quantitative approach to benefit-risk assessment that considers both beneficial outcomes and potential harms, using the state of the art as a benchmark [23].
- Poorly Defined Strategy: Ensure the evaluation strategy is thoroughly described in the CEP. An unclear or poorly defined CEP typically leads to frequent updates and revisions throughout the evaluation process [23].
- Data Transparency: Include all relevant data, even unfavorable findings, to maintain scientific credibility and regulatory trust [23].
Best Practices for MDR-Compliant CER Protocols
- Early Engagement: Engage with qualified experts and notified bodies during the protocol development phase to identify potential issues before implementation [41].
- Systematic Literature Review: Employ objective, non-biased systematic review methods with predefined search protocols and inclusion criteria [23].
- Alignment with Device Documentation: Ensure consistency between the CEP/CER and the device's technical documentation, including the risk management file and instructions for use [23].
- Qualified Personnel: Ensure that individuals conducting the clinical evaluation possess the necessary expertise in relevant clinical specialties, research methodology, and regulatory requirements [23].
- Proactive Planning for Updates: Establish a plan for regular CER updates based on predetermined schedules and triggers, incorporating PMS and PMCF findings [24] [23].
Developing a comprehensive CER protocol requires meticulous planning, strategic thinking, and adherence to regulatory requirements. By formulating precise research questions using structured frameworks like PICO and FINER, establishing robust methodologies for evidence generation and assessment, and implementing rigorous data quality processes, drug developers can create CER protocols that not only meet regulatory expectations but also genuinely demonstrate the safety and efficacy of their products. A well-constructed CER protocol serves as both a regulatory requirement and a strategic asset, facilitating efficient market access while ensuring patient safety through scientifically valid clinical evaluation.
Selecting Appropriate Study Endpoints and Comparators
Within drug comparative effectiveness research (CER), the formulation of key research questions fundamentally hinges on two core elements: the endpoints that definitively measure a treatment's effect and the comparators against which this effect is evaluated. The strategic selection of these components is not merely a procedural step but a critical determinant of a study's validity, relevance, and ultimate utility for healthcare decision-making [45]. In the evolving landscape of drug development, regulatory and health technology assessment (HTA) bodies are increasingly emphasizing evidence that demonstrates value in real-world terms, making the choice of endpoints and comparators more consequential than ever [46] [47]. This guide provides a structured framework for researchers to navigate these complex decisions, ensuring that CER studies are robust, patient-centric, and aligned with the requirements of regulators, payers, and clinicians.
The Critical Role of Endpoints and Comparators in CER
Endpoints and comparators form the foundational architecture of any clinical research study. The endpoint is a predefined, measurable variable that serves as evidence of a drug's efficacy and safety [48] [49]. These must be reproducible, well-defined, validated, and statistically measurable to provide credible, actionable evidence [49]. The comparator is the intervention against which the investigational drug is evaluated, which can be a placebo, standard of care, or an active drug from another class.
Their selection directly influences a trial's design, execution, regulatory approval, and subsequent adoption into clinical practice [45]. Poor selection can lead to ambiguous outcomes, prolonged approval processes, or outright rejection of study findings, even if the trial is otherwise well-executed [45] [49]. For CER, which aims to inform real-world clinical and policy decisions, the stakes are particularly high. The evidence generated must resolve uncertainties that matter to patients, clinicians, and healthcare systems [47].
A Framework for Endpoint Selection
Types and Classifications of Endpoints
Endpoints can be categorized along several dimensions, each with distinct strengths, weaknesses, and appropriate use cases. A comprehensive understanding of these categories is a prerequisite for effective selection.
Table: Classification of Clinical Trial Endpoints
| Endpoint Category | Definition | Examples | Strengths | Weaknesses |
|---|---|---|---|---|
| Clinical Endpoints | Directly measure how a patient feels, functions, or survives [48]. | Overall survival, symptom control, prevention of hospitalization [50] [48]. | High clinical relevance and patient-centricity. | Can require large sample sizes and long follow-up times; may become less feasible as disease severity declines [50]. |
| Surrogate Endpoints | Substitute for clinical endpoints; measure biomarkers or other laboratory measures [48]. | Blood pressure, cholesterol levels, tumor shrinkage [48]. | Faster to measure, can reduce trial size and duration, and lower costs. | May not reliably predict the true clinical benefit; risk of misleading conclusions if not validated [48]. |
| Patient-Reported Outcomes (PROs) | A type of clinical endpoint reported directly by the patient without interpretation by a clinician [51]. | Quality of life assessments, pain scales, symptom diaries [51] [45]. | Capture the patient's perspective on their health and treatment. | Subjective; can be influenced by numerous factors; requires validated instruments [45]. |
| Performance Outcomes (PerfOs) | Based on standardized tasks performed by patients [51]. | Cognitive function tests, motor skills assessments. | Objective and standardized. | May not correlate perfectly with real-world functional ability. |
Beyond this primary classification, endpoints are also defined by their role in the trial's statistical analysis:
- Primary Endpoint: The main outcome the study is powered to assess; it must align directly with the primary study objective [48].
- Secondary Endpoints: Provide supplementary information on the treatment's effects and contribute to a broader understanding of its impact [45].
- Exploratory Endpoints: Used to generate hypotheses for future research and are not the main focus of the current analysis [45].
Core Criteria for Selecting Endpoints
Selecting an appropriate endpoint requires balancing scientific rigor with practical feasibility. The following criteria provide a systematic checklist for evaluation [45]:
- Relevance: The endpoint must capture an outcome that is meaningful to patients, clinicians, and other stakeholders. It should answer the question, "Does this outcome matter?" For example, while a change in a viral load is objective, its importance is limited if it does not correlate with severe outcomes or the patient experience [50].
- Measurability: The endpoint must be quantifiable and can be consistently measured across all study participants and sites. Inconsistent measurement, such as at-home versus in-clinic SpO2 readings, prevents timely comparative evaluation [50] [49].
- Sensitivity: The endpoint should be sensitive enough to detect a meaningful change attributable to the intervention. As the overall risk of severe outcomes like hospitalization declines due to vaccines or less virulent variants, this endpoint may lose its sensitivity and feasibility [50].
- Feasibility: Researchers must assess whether the endpoint can be realistically measured within the study's constraints of time, budget, and participant burden. The logistical difficulty of outpatient trials, for instance, necessitates different endpoints than inpatient studies [50].
- Regulatory Alignment: Endpoints should align with the expectations of regulatory and HTA bodies. Understanding FDA guidance and other regulatory frameworks is essential for a streamlined approval process [45] [47].
The Evolving Landscape: Patient-Centricity and Novel Endpoints
There is a growing regulatory and HTA mandate for endpoints that reflect aspects of health meaningful to patients, such as the ability to perform daily activities [51] [47]. This shift, coupled with technological advances, is reshaping endpoint selection.
The emergence of Digital Health Technologies (DHTs) allows for the collection of both actively-collected and passively-monitored Clinical Outcome Assessments (COAs) [51]. An aligned ontological framework helps researchers compare these new digital measures with traditional COAs, enabling trade-off decisions that can reduce patient burden and eliminate data redundancy [51]. For instance, in a neurological condition, a traditional patient questionnaire about mobility can be complemented or replaced by a passively-collected digital measure of gait speed.
Simultaneously, regulatory trends show a renewed emphasis on Overall Survival (OS) as the gold standard for efficacy, particularly in oncology. There is a declining reliance on surrogate endpoints like progression-free survival when they fail to correlate with longer survival [46]. The FDA now requires OS not only as an efficacy measure but also as an essential safety endpoint to identify potential long-term harms [46].
Diagram: A Framework for Endpoint Selection
A Strategic Approach to Comparator Selection
Defining the Comparator Arm
The choice of comparator is a pivotal strategic decision that determines the context in which a new drug's value is judged. A well-justified comparator arm is essential for the results of a CER study to be credible and informative for healthcare decisions. The European Access Academy identifies comparator choice as one of the four key challenge areas for a joint European HTA, highlighting its complexity and importance [47].
The conceptual basis for the comparator should be the standard of care (SOC) that is most relevant to the study's intended patient population and clinical setting. However, the "standard of care" is not a universal constant. It can vary significantly based on geographical location, treatment line, and local reimbursement policies [46].
Navigating Global Variability in Standard of Care
A major challenge in designing global trials, which are the norm for drug development, is that the SOC is not consistent worldwide [46]. A treatment commonly used in the United States may not be available or reimbursed in Europe or emerging markets. This variation makes it "logistically and ethically impossible to choose a single, consistent comparator" for a global randomized controlled trial [46].
A recommended and increasingly accepted strategy to address this is the use of an investigator’s choice design [46]. In this pragmatic design, the site investigator selects a control treatment from a pre-defined, clinically relevant group of locally appropriate and available SOC regimens. This approach ensures that patients in the control arm receive ethical, locally relevant care, making the trial operationally feasible across a global footprint.
Regulatory agencies generally accept this approach, provided two key requirements are met [46]:
- The statistical analysis plan is robust enough to handle the potential heterogeneity.
- The sponsor provides a clear justification for why the specific choices are appropriate regional comparators.
Key Considerations for Comparator Selection
When formulating the comparator strategy, researchers should address the following questions derived from the core domains identified for European HTA [47]:
- What are the criteria for the choice of comparator in an increasingly fragmented treatment landscape? The selection must be defensible based on current clinical guidelines and real-world treatment patterns.
- What is a reasonable number of comparators? While a single comparator simplifies analysis, it may not reflect clinical reality. A basket of comparators may be necessary.
- How can Early Advice be shaped so that the comparator fulfills both regulatory and HTA needs? Engaging with regulators and HTA bodies like the EMA and EUnetHTA in joint scientific consultations can align expectations early, preventing costly missteps later [47].
- What is the acceptability of Indirect Treatment Comparisons (ITC)? When a direct head-to-head trial is not feasible, the plan to use ITC to generate comparative evidence must be agreed upon with stakeholders in advance.
Diagram: Strategy for Comparator Selection
Integrating Endpoints and Comparators into CER Protocols
Methodological and Statistical Considerations
The integration of endpoints and comparators must be meticulously planned in the study protocol and statistical analysis plan (SAP). For trials with multiple endpoints, employing a Global Statistical Test (GST) can offer enhanced power, flexibility, and error control by leveraging relationships among outcomes [45]. Furthermore, when using a time-to-event endpoint like overall survival, the SAP must pre-specify plans for interim analyses to detect harm or futility early [46]. If OS data are immature at the time of submission, sponsors should be prepared to provide projections or scenario analyses that demonstrate the likelihood of ruling out a detrimental effect with further follow-up [46].
For studies using an investigator’s choice comparator, the statistical analysis must account for the potential heterogeneity introduced by multiple control therapies. This often involves sophisticated statistical techniques to ensure the interpretability and validity of the results.
Essential Research Reagents for CER
The following table details key methodological components and their functions in designing and executing robust CER on endpoints and comparators.
Table: Key Methodological Components for CER Design
| Component | Category | Function in CER |
|---|---|---|
| Global Statistical Test (GST) | Statistical Method | Provides enhanced power and error control in studies with multiple, correlated endpoints by combining them into a single test [45]. |
| Statistical Analysis Plan (SAP) | Study Document | Pre-specifies all planned analyses, including the handling of primary/secondary endpoints, interim analyses, and subgroup analyses; critical for regulatory credibility [46]. |
| Patient/ Intervention/ Comparator/ Outcomes (PICO) | Framework | The structured framework used by HTA bodies to define the scope of an assessment; early agreement on PICO elements is critical [47]. |
| Indirect Treatment Comparison (ITC) | Methodological Approach | Used to estimate comparative efficacy when head-to-head trial data is not available; acceptability must be discussed with regulators [47]. |
| Digital Health Technology (DHT) | Data Collection Tool | Enables collection of actively- and passively-collected data, potentially reducing patient burden and providing more granular endpoint measurement [51]. |
| Clinical Outcome Assessment (COA) | Endpoint Instrument | A standardized tool (e.g., questionnaire, performance task) to measure how a patient feels or functions [51]. |
| Joint Scientific Consultation (JSC) | Regulatory Process | A meeting with both regulatory and HTA bodies to gain aligned advice on development plans, including endpoints and comparators [47]. |
The selection of study endpoints and comparators is a foundational process that translates a CER hypothesis into actionable evidence. This process requires a strategic, multi-stakeholder approach that balances scientific rigor with patient relevance and practical feasibility. The current trends are clear: regulatory and HTA expectations are escalating, demanding more comprehensive dose optimization, a renewed focus on overall survival for safety and efficacy, and endpoints that reflect what is truly meaningful to patients [46] [51] [47]. Success in this environment depends on early and inclusive collaboration with all stakeholders—including patients, clinicians, regulators, and HTA bodies—to ensure that the key questions formulated for drug CER research are answerable, relevant, and capable of demonstrating genuine value in the treatment of disease.
Integrating Real-World Evidence (RWE) and Qualitative Data
The landscape of drug development and comparative effectiveness research (CER) is undergoing a significant transformation, driven by an increasing emphasis on patient-centeredness and real-world impact [52]. Health technology assessment (HTA) and regulatory frameworks are evolving to prioritize evidence that captures the full spectrum of patient experiences, outcomes, and values [52]. In this context, the integration of Real-World Evidence (RWE) and qualitative data represents a paradigm shift, moving beyond the traditional reliance on quantitative data alone to inform critical healthcare decisions.
RWE, derived from the analysis of Real-World Data (RWD) collected during routine clinical care, provides insights into the effectiveness and safety of medical products in everyday settings [53] [54]. Simultaneously, qualitative research methods capture rich, contextual information on people’s beliefs, experiences, attitudes, behaviors, and interactions [52]. This integration is particularly crucial for understanding how patients and clinicians adapt to, perceive, and interact with innovations, nuances that traditional quantitative approaches alone cannot capture [52]. For CER, this combined approach ensures that research questions and resulting evidence are not only statistically robust but also deeply relevant to the patients and clinicians who face specific health decisions daily [1].
Framing Research Questions for Integrated CER Studies
The foundation of any robust CER study is a rigorously formulated research question. For research that integrates RWE and qualitative data, this requires careful consideration of frameworks and standards that ensure both scientific validity and patient-centeredness.
Foundational Frameworks for Question Formulation
The PICO framework (Patient/Population, Intervention, Comparison, Outcome) is a cornerstone for structuring clinical research questions [42] [43]. Its components prompt researchers to define the specific subject of the research, the intervention or exposure being studied, the appropriate comparator, and the outcomes of interest [42]. For integrated studies, the definition of the outcome (O) is critical; it should encompass both quantitative measures of effect and qualitative descriptions of patient-experienced phenomena, such as attitudes, experiences, or implementation challenges [42].
Table 1: Adapting the PICO Framework for Integrated RWE and Qualitative Studies
| PICO Component | Definition | Considerations for Integrated RWE & Qualitative Studies |
|---|---|---|
| Patient/Population | The subject(s) of interest [42]. | Define relevant baseline and clinical characteristics. Plan to include a spectrum of the population, including those historically underrepresented in research [1]. |
| Intervention | The action/exposure being studied [42]. | For qualitative aspects, define the specific phenomenon (e.g., behavior, experience, perspective) and contextual factors (e.g., workflow integration) [42]. |
| Comparison | The alternative action/exposure measured against [42]. | The comparator should represent a legitimate clinical option. "Usual care" should be avoided unless it is a coherent clinical option [1]. |
| Outcome | The effect being evaluated [42]. | Include outcomes people notice and care about (e.g., functioning, symptoms) [1]. Combine quantitative effect measures with qualitative descriptions of experience [42]. |
For studies where a comparator is not relevant, such as those focused purely on understanding patient experiences, alternative frameworks like SPIDER (Sample; Phenomenon of Interest; Design; Evaluation; Research type) may be more appropriate [52] [42].
Ensuring Patient-Centeredness and Relevance
Beyond structural frameworks, the PCORI Methodology Standards provide critical guidance for ensuring that CER questions are meaningful and useful to decision-makers [1]. Key standards for formulating research questions include:
- RQ-3: Identify the specific health decision the research is intended to inform and the population for whom this decision is pertinent [1].
- RQ-5: Select interventions and comparators that correspond to actual healthcare options for patients and providers [1].
- RQ-6: Measure outcomes that the population of interest notices and cares about, such as survival, functioning, symptoms, and health-related quality of life [1].
Furthermore, engaging people representing the population of interest and other relevant stakeholders (e.g., clinicians, payers) from the outset is essential for defining research questions that address genuine evidence gaps and reflect real-world priorities [1].
Methodologies for Data Collection and Generation
A robust integrated study employs systematic methodologies for collecting both RWD and qualitative data, ensuring the evidence generated is fit-for-purpose and reliable.
RWD is routinely collected from a diverse array of sources, each offering unique strengths for CER [55] [54].
Table 2: Common Sources and Applications of Real-World Data
| Data Source | Description | Key Applications in CER |
|---|---|---|
| Electronic Health Records (EHRs) | Digital records of patient health information generated from clinical encounters [53] [56]. | Capturing clinical notes, laboratory values, treatment patterns, and outcomes in heterogeneous patient populations [53] [56]. |
| Insurance Claims & Billing Data | Data generated from healthcare billing and reimbursement processes [53]. | Understanding treatment patterns, healthcare resource utilization, costs, and comorbidities across healthcare systems [53]. |
| Patient Registries | Organized systems that collect uniform data to evaluate specific outcomes for a population defined by a particular disease or exposure [55]. | Studying natural history of disease, treatment patterns, and outcomes, especially for rare diseases [55]. |
| Patient-Reported Outcomes (PROs) | Data reported directly by patients about their health status, without interpretation by a clinician [55] [1]. | Measuring outcomes that matter to patients, such as symptoms, functioning, and quality of life [1]. |
| Genomic & Biomarker Data | Molecular and biological data linked to other RWD sources [56] [55]. | Enabling precision medicine approaches and understanding disease heterogeneity [56]. |
Qualitative Research Methodologies
Systematic qualitative methodologies are vital for generating robust, analyzable data on patient and stakeholder perspectives.
- Concept Elicitation (CE): These are open-ended, narrative-style one-to-one interviews designed to understand patient needs, experiences, and the outcomes they find most important without imposing preconceived categories [57].
- Cognitive Interviews: This methodology is used to understand how respondents interpret and answer specific questions, which is crucial for developing valid quantitative surveys and PRO instruments for use in RWE studies [57].
The conduct of these interviews should be documented with verbatim transcripts, which form the basis for rigorous qualitative analysis [57]. A review of submissions to the National Institute for Health and Care Excellence (NICE) highlighted that a common concern is the "lack of systematic evidence generation or inconsistent adherence to quality standards," underscoring the need for formal methods in qualitative data collection and analysis [52].
Analytical Approaches for Evidence Integration
Transforming collected data into credible evidence requires analytical rigor and, for qualitative data, a structured process to identify key themes and insights.
Qualitative Data Analysis
Thematic analysis is a widely used method that allows for a bottom-up approach where patient concerns and experiences emerge directly from the data [57]. The process typically involves:
- Transcription: Creating verbatim transcripts from interview audio [57].
- Coding: Systematically tagging relevant excerpts of text from the transcripts with codes that summarize their meaning. Software like NVivo can significantly speed up this process with autocoding features and helps manage large volumes of unstructured data [57].
- Theme Development: Collating codes into potential themes, gathering all data relevant to each potential theme, and refining them to ensure they form a coherent pattern [57].
This process allows researchers to tease out repeated patterns and construct themes, providing a systematic account of the qualitative data [57]. The analysis should also distinguish between spontaneous (unaided) patient comments and those that are prompted by an interviewer, as this can speak to the relative importance of different concepts [57].
Assessing Data Quality and Robustness
For both RWE and qualitative components, adherence to quality standards is critical. The PCORI Methodology Standards emphasize:
- IR-1: Specifying plans for quantitative data analysis a priori, including definitions of key exposures, outcomes, covariates, and plans for handling missing data [1].
- IR-2: Assessing the adequacy of data sources, ensuring they can robustly capture exposures, outcomes, and relevant covariates [1].
- IR-7: Developing a formal data management plan that addresses data collection, organization, handling, preservation, and sharing for both quantitative and qualitative data [1].
For RWE, a growing number of tools and frameworks are available to help assess study quality and reporting, such as the ESMO Guidance for Reporting Oncology Real-World Evidence (ESMO-GROW) [54]. Selecting the appropriate tool depends on the study's intended purpose, design, and the availability of study documentation [54].
The following diagram illustrates the integrated workflow for generating and analyzing RWE and qualitative data, from study conception through to the generation of insights for decision-making.
Successfully integrating RWE and qualitative data in CER requires a suite of methodological tools, analytical software, and awareness of key industry players setting standards in the field.
Table 3: Essential Tools and Resources for Integrated RWE and Qualitative CER
| Category | Tool/Resource | Function & Application |
|---|---|---|
| Methodological Frameworks | PICO/SPIDER Frameworks [42] [43] | Provides structure for formulating focused, answerable research questions. |
| PCORI Methodology Standards [1] | Ensures research questions and study designs are patient-centered and methodologically rigorous. | |
| FINER Criteria (Feasible, Interesting, Novel, Ethical, Relevant) [42] | Evaluates the practical aspects and broader value of a research question. | |
| Qualitative Data Analysis Software | NVivo [57] | Software for organizing, coding, and analyzing unstructured qualitative data (e.g., interview transcripts); supports thematic analysis and collaboration. |
| RWE Analytics Platforms | Aetion Evidence Platform [55] | Enables transparent and validated analysis of RWD for regulatory-grade RWE generation. |
| Sentinel & OHDSI Networks [53] | Distributed data networks that leverage EHR and claims data for large-scale pharmacoepidemiology and safety studies. | |
| Key RWE Insight Companies | IQVIA, Optum Life Sciences, Flatiron Health [55] | Organizations providing large-scale, curated RWD datasets and advanced analytics, often with therapeutic area specializations (e.g., Flatiron in oncology). |
| Quality Assessment Tools | ESMO-GROW, EQUATOR Network Guidelines [1] [54] | Tools and reporting guidelines (e.g., COREQ for qualitative research) to ensure and communicate study quality and transparency. |
The integration of RWE and qualitative data marks a pivotal advancement in drug comparative effectiveness research, moving the field toward a more holistic and patient-centered paradigm. This approach combines the generalizable, quantitative insights from real-world practice with the deep, contextual understanding of patient experiences and values. By formulating research questions using established frameworks like PICO and the PCORI standards, employing rigorous and systematic methodologies for data collection and analysis, and leveraging modern tools and platforms, researchers can generate evidence that truly reflects the needs and priorities of patients and clinicians. This integrated evidence is increasingly critical for informing regulatory decisions, health technology assessments, and ultimately, ensuring that patients receive care that is not only effective but also aligned with their lived experiences.
Leveraging Best Practices for FDA Communication and Meetings
Within the comprehensive framework of drug development, Comparative Effectiveness Research (CER) provides critical evidence on the real-world benefits and risks of medical products. Formulating pivotal CER questions, however, requires proactive and strategic regulatory planning. Engaging with the U.S. Food and Drug Administration (FDA) through formal meetings and compliant communication is not merely a regulatory hurdle; it is a fundamental practice for aligning research objectives with regulatory expectations and public health standards. This guide provides drug development professionals with advanced methodologies for navigating FDA interactions, with a specific focus on how these dialogues shape and validate the key questions at the heart of robust CER. Mastering these interactions ensures that the resulting evidence is not only scientifically sound but also regulatorily relevant, thereby supporting informed healthcare decisions and efficient product development.
The Framework of Formal FDA Meetings
Formal meetings with the FDA are critical touchpoints throughout a drug's lifecycle. They offer sponsors the opportunity to seek guidance, align on development plans, and mitigate risks, thereby directly influencing the design of clinical studies, including those aimed at generating comparative effectiveness data.
Types of Formal Meetings
The Prescription Drug User Fee Act (PDUFA) establishes several distinct meeting types, each serving a specific purpose within the drug development timeline [58]. Understanding the nuances of each meeting type is essential for requesting the appropriate forum for your questions. The following table summarizes these key meeting types and their primary applications in the context of drug development and CER.
Table 1: Types of Formal FDA Meetings Under PDUFA
| Meeting Type | Purpose & Context | Common Use Cases in Drug Development |
|---|---|---|
| Type A [59] | For stalled development programs or to address critical safety issues. | Dispute resolution, clinical hold discussions, post-action meetings (within 3 months of a regulatory action). |
| Type B [58] [59] | To discuss specific, scheduled stages of drug development. | Pre-IND, End of Phase 1 (for certain products), Pre-NDA/BLA, and certain Risk Evaluation and Mitigation Strategies (REMS) discussions. |
| Type B (EOP) [58] [59] | Held at critical junctures to review progress and plan future studies. | End of Phase 2 / Pre-Phase 3 meetings to discuss adequate study design for the pivotal trials. |
| Type C [58] [59] | For any other topic not covered by Type A, B, or D meetings. | Early consultations on novel biomarkers or surrogate endpoints. |
| Type D [58] [59] | Focused on a narrow set of issues (no more than two topics). | Follow-up questions on a new issue after a prior meeting, or narrow developmental questions. |
| INTERACT [58] [59] | For novel questions early in development, prior to an IND submission. | Advice on novel drug platforms, pre-clinical models, CMC issues, and design of first-in-human trials. |
The Meeting Process: From Request to Follow-Up
Navigating a formal FDA meeting is a multi-stage process that requires meticulous preparation. The workflow below outlines the key steps from initial request through post-meeting follow-up, which are critical for securing valuable Agency feedback.
Diagram 1: FDA Formal Meeting Workflow. The process involves multiple preparation and feedback stages over several weeks.
- Meeting Request: A sponsor's journey begins with a written request that must clearly articulate the drug development program's strategies, anticipated challenges, and the specific questions for the Agency [58]. This document should be both concise and comprehensive, as the FDA uses it to assess the meeting's necessity and determine the appropriate participants.
- FDA Response and Scheduling: After review, the FDA typically issues a written response within 14 to 21 days, granting or denying the meeting [58]. If granted, the response will confirm the date, time, and format (e.g., in-person, videoconference, or Written Response Only). The FDA aims to schedule meetings within 30 to 75 days of receiving the request, depending on the meeting type [58].
- The Meeting Package: This is a critical document that the sponsor prepares to enable a productive discussion. It contains all essential information, rationale, and scientific data related to the questions asked. For most meeting types, the package is due 30 to 50 days before the scheduled meeting date, though some meeting types (like Type A) require it with the initial request [58].
- Conducting the Meeting and Follow-Up: During the meeting, sponsors should focus on clarifying their pre-submitted questions. The FDA will subsequently issue official meeting minutes, which serve as a critical record of the Agency's recommendations [60]. These minutes should directly inform the refinement of CER hypotheses and study protocols.
Communicating Scientific Information on Unapproved Uses
Effectively communicating robust scientific information, particularly concerning unapproved uses of approved drugs, is a complex but vital aspect of generating real-world evidence. FDA's 2025 guidance, "Communications From Firms to Health Care Providers Regarding Scientific Information on Unapproved Uses," provides an enforcement policy for such communications [61] [62].
Key Principles for SIUU Communications
The guidance outlines a framework for disseminating Scientific Information on Unapproved Uses (SIUU) that is both compliant and valuable to healthcare providers (HCPs). The following diagram illustrates the decision-making and requirements for preparing these communications.
Diagram 2: Framework for preparing communications on scientific information for unapproved uses (SIUU). Ensuring scientific soundness and complete disclosures is critical.
- Substantiation and Scientific Soundness: The foundational requirement is that the SIUU communication must be based on source publications that are scientifically sound [62]. This means the studies must "meet generally accepted design and other methodological standards for the particular type of study or analysis performed." Notably, the final guidance removed the previously proposed "clinically relevant" standard, acknowledging that certain early-phase data could be scientifically sound and fall within this policy [62].
- Recommended Disclosures and Presentation: To be non-misleading, the communication must provide HCPs with a balanced view. Required disclosures include a clear statement that the use is not approved, a description of the study's limitations, and—importantly—"any conclusions from other scientifically sound studies... that are in conflict with the conclusions" in the SIUU communication [62]. The tone must be factual, avoiding persuasive marketing techniques such as emotional appeals, celebrity endorsements, or pre-judgmental calls to value [62].
- Separation from Promotional Activities: SIUU communications should be separate from promotional communications about the product's approved uses [62]. For example, if a firm representative shares an SIUU communication during an in-person visit, it should not be intermingled with promotional materials. Personnel discussing SIUU should have specialized training to handle scientific information accurately [62].
The Scientist's Toolkit for Regulatory Submissions
Preparing for FDA interactions requires not only strategic planning but also the use of specific regulatory tools and documents. The following table details essential materials and their functions in the context of regulatory meetings and CER planning.
Table 2: Essential Research Reagent Solutions for Regulatory Submissions
| Tool/Document | Primary Function | Application in CER & Drug Development |
|---|---|---|
| Meeting Request (Formal) | To officially request a specific type of meeting with the FDA and outline proposed questions. | Secures a dedicated forum to gain FDA alignment on CER study designs, endpoints, and data requirements. |
| Meeting Package | Provides the FDA with comprehensive background data and specific questions to allow for prepared discussion. | Presents the rationale for the CER approach, including proposed comparators, patient populations, and statistical methods. |
| Form FDA 1571 (IND) | Used to initiate an Investigational New Drug application, required to begin clinical trials in the U.S. [63]. | The vehicle for obtaining exemption to ship an investigational drug across state lines for clinical investigations [63]. |
| Form FDA 1572 | Completed by clinical investigators to commit to key obligations in conducting a clinical trial [63]. | Ensures all investigators in a CER trial adhere to FDA regulations, protecting data integrity and subject welfare. |
| Institutional Review Board (IRB) | A committee that reviews and monitors biomedical research to protect the rights and welfare of human subjects [63]. | Mandatory for FDA-regulated clinical investigations; provides ethical oversight for all CER studies involving human participants [63]. |
| SIUU Communication Dossier | A curated collection of scientific reprints, clinical guidelines, and disclosures for sharing off-label data. | Enables the scientifically valid and compliant dissemination of real-world evidence and comparative data to HCPs. |
| Furaquinocin A | Furaquinocin A|C22H26O7|Meroterpenoid Research Compound | High-purity Furaquinocin A for Research Use Only (RUO). Explore this potent natural meroterpenoid's antitumor activity and unique biosynthesis. |
| IST5-002 | Benzyl-adenosine monophosphate|High-Purity Reference Standard | Benzyl-adenosine monophosphate is a nucleotide analog for biochemical research. This product is For Research Use Only and is not intended for diagnostic or personal use. |
Experimental Protocols for Regulatory Strategy
Implementing a successful regulatory strategy involves defined protocols for both internal preparation and external engagement.
Protocol for Drafting a Pre-Phase 3 Meeting Package
Objective: To secure FDA agreement on the design of Phase 3 trials, which often serve as the pivotal evidence for effectiveness and safety, and to discuss plans for CER.
- Background Section: Provide a concise summary of the drug, its mechanism of action, and results from Phase 1 and 2 studies. Integrate a summary of any prior CER-relevant findings or health economics outcomes research (HEOR) data.
- Proposed Phase 3 Protocol: Include the full, detailed study protocol. Key elements are:
- Primary and Secondary Endpoints: Justify the choice of endpoints, particularly if using surrogate endpoints or patient-reported outcomes relevant to comparative effectiveness.
- Comparator Selection: Explicitly justify the choice of comparator (placebo, active control, standard of care) with a strong rationale rooted in the current treatment landscape.
- Statistical Analysis Plan (SAP): Detail the planned statistical analyses, including methods for handling missing data and any planned subgroup analyses that may inform CER.
- Questions for FDA: Pose specific, focused questions to the Agency. For a Pre-Phase 3 meeting, these should address the adequacy of the proposed trial design to support a marketing application and the acceptability of the proposed endpoints and analyses.
Protocol for Developing a Compliant SIUU Communication
Objective: To create a firm-generated presentation based on a scientific publication about an unapproved use, ensuring it is truthful, non-misleading, and consistent with FDA enforcement policy.
- Source Validation: Select a source publication (e.g., a reprint, clinical practice guideline) and conduct a methodological assessment to confirm it is "scientifically sound" [62]. Document this assessment.
- Content Development: Create slides that accurately represent the data from the source publication. The presentation must:
- Objectively summarize the study design, results, and conclusions.
- Highlight study limitations explicitly identified in the publication or known from the broader scientific context.
- Disclosure and Formatting: Incorporate all required disclosures prominently. Ensure the presentation is visually neutral, avoiding persuasive marketing techniques, emotional imagery, or promotional taglines [62]. Finally, implement a process for continuing review to ensure the communication is not disseminated if subsequent research shows the original study to be unreliable [62].
Formulating pivotal CER questions is a scientific endeavor that exists within a defined regulatory ecosystem. Proactive engagement with the FDA through formal meetings and adherence to compliant communication practices are not ancillary activities; they are integral to ensuring that the resulting evidence is robust, regulatory-grade, and capable of informing clinical and payer decisions. By mastering the frameworks and protocols outlined in this guide—from selecting the appropriate meeting type to disseminating scientific information with integrity—drug development professionals can de-risk their development programs and enhance the impact of their comparative effectiveness research. Ultimately, a deep understanding of these best practices empowers scientists to navigate the regulatory landscape with confidence, accelerating the delivery of meaningful treatments to patients.
The development of drugs, biologics, and medical devices faces increasing complexity in 2025, driven by scientific advancement, regulatory evolution, and heightened emphasis on patient-centricity. Clinical trials now target smaller, more specific patient populations while navigating stricter global regulations and demands for robust real-world evidence [64]. Furthermore, regulatory disparities across international markets complicate global study execution, creating a challenging environment for researchers and sponsors [64]. This whitepaper examines the distinct challenges across therapeutic product categories and provides technical guidance for formulating pivotal clinical evaluation research (CER) questions that meet contemporary scientific and regulatory standards. The focus on adaptive trial designs and decentralized elements represents a paradigm shift from traditional models, requiring sophisticated methodological approaches [65].
For drug and biologic developers, challenges include reduced investment environments, the need for more efficient trial designs, and legislative impacts such as the Inflation Reduction Act in the U.S., which may influence the number of clinical trials initiated [64]. Medical device manufacturers face stringent implementation of the European Medical Device Regulation (MDR), requiring more rigorous clinical evidence throughout the device lifecycle [66] [23]. Understanding these product-specific challenges is fundamental to designing research that generates sufficient evidence for regulatory approval and clinical adoption.
Current Regulatory Framework and Impact on Research
Key Regulatory Developments in 2025
The global regulatory landscape is undergoing significant transformation, with updates directly impacting clinical evidence requirements across all product types.
Table 1: Key Regulatory Updates and Implications for Clinical Research
| Regulatory Body | Update Type | Key Focus Areas | Impact on Research Questions |
|---|---|---|---|
| FDA (U.S.) [67] | Multiple Draft & Final Guidances (2025) | ICH E6(R3) GCP; Expedited Programs for Regenerative Medicine; Post-approval Data for Cell/Gene Therapies; Innovative Trial Designs for Small Populations | Promotes flexible, risk-based approaches; emphasizes long-term follow-up for novel therapies; encourages novel endpoints and statistical designs for rare diseases. |
| EMA (E.U.) [67] | Draft Reflection Paper | Patient Experience Data | Encourages systematic inclusion of patient perspectives throughout medicine lifecycle, affecting endpoint selection and data collection methods. |
| NMPA (China) [67] | Final Policy Revision | Accelerated Trial Approvals; Adaptive Designs | Reduces approval timelines by ~30%; allows real-time protocol modifications, enabling more responsive and efficient trial designs. |
| MDCG (E.U.) [66] [68] [23] | Updated MDR Guidance & MDCG Documents | Clinical Evaluation Reports (CERs); Post-market Surveillance; Sufficient Clinical Evidence | Mandates stronger post-market clinical follow-up (PMCF); stricter equivalence claims; requires clear benefit-risk analysis with defined parameters. |
Cross-Cutting Regulatory Themes
Several overarching themes define the 2025 regulatory environment. There is a pronounced shift toward decentralized clinical trials (DCTs), with both the FDA and EMA issuing specific guidance to facilitate their implementation [65]. These models aim to enhance patient access and diversity but introduce operational complexities in data privacy and cross-border compliance. Simultaneously, regulatory agencies increasingly accept Real-World Evidence (RWE) to support decision-making. The FDA's Advancing RWE Program and similar EMA initiatives highlight this trend, encouraging researchers to consider how RWE can complement traditional clinical trial data [65]. Furthermore, a global emphasis on diversity and inclusion in clinical trials has moved from recommendation to expectation. Regulatory reviewers now scrutinize enrollment strategies to ensure representative participant populations, particularly for diseases disproportionately affecting minority groups [64] [65].
Product-Specific Challenges and Research Question Frameworks
Pharmaceutical Drugs
Core Challenges
The small molecule drug sector faces intense pressure to maximize profitability and demonstrate value under evolving legislation. The U.S. Inflation Reduction Act (IRA) is anticipated to impact trial initiation, potentially leading to a reduction in the overall number of clinical trials and a strategic shift toward multi-indication trials to maximize a product's value [64]. Additionally, achieving patient diversity remains a significant hurdle, with social, economic, and trust barriers limiting participation from underrepresented groups [64].
Formulating Key Research Questions
Research questions for pharmaceutical drugs must be framed within the PICOTS (Populations, Interventions, Comparisons, Outcomes, Timeframe, Settings) framework to ensure they address both clinical and economic value [69].
- Comparative Effectiveness: "In a diverse patient population with [Condition] (P), how does [New Drug] (I) compare to [Standard of Care] (C) in reducing [Primary Outcome] (O) over [Timeframe] (T), while accounting for intercurrent events like treatment switching?"
- Efficiency & Value: "Can a multi-indication, platform trial design simultaneously evaluate the efficacy of [New Drug] for three related indications, reducing development time and costs while providing sufficient evidence for regulatory review and pricing negotiations?"
Biologics and Advanced Therapy Medicinal Products (ATMPs)
Core Challenges
Cell and gene therapies present unique development challenges that render traditional randomized controlled trial models inadequate. These include small patient populations for rare diseases, ethical considerations around placebo controls, and the need for long-term follow-up to understand durability of effect and delayed risks [64] [67]. The high cost and complexity of manufacturing also necessitate efficient trial designs that maximize the information gained from every patient.
Formulating Key Research Questions
Research for ATMPs requires questions that accommodate small sample sizes, use innovative endpoints, and plan for long-term observation, often leveraging expedited regulatory pathways like the FDA's RMAT designation [67].
- Trial Design for Small Populations: "In patients with [Rare Disease] (P), can a Bayesian adaptive trial design for [Gene Therapy] (I) using a synthetic control arm (C) provide valid evidence of efficacy on a surrogate endpoint (O) that is reasonably likely to predict long-term clinical benefit, supporting accelerated approval?"
- Durability & Safety: "What is the long-term persistence of clinical benefit and incidence of late-onset adverse events over 15 years (T) in patients treated with [Cell Therapy],
necessitating a robust post-approval study design integrated into the initial clinical development plan?"
Medical Devices
Core Challenges
The enforcement of the EU MDR represents the most significant challenge for medical device manufacturers. It demands a higher standard of clinical evidence, even for legacy devices, and requires a continuous process of evaluation throughout the device lifecycle [66] [23]. Demonstrating equivalence to an existing device has become substantially more difficult, requiring rigorous comparison of technical, biological, and clinical characteristics [66] [23]. Furthermore, defining and validating clinical benefits and conducting a comprehensive benefit-risk analysis that reviewers find acceptable are common areas of pushback [68].
Formulating Key Research Questions
Device research questions must be precisely linked to the device's intended purpose and the General Safety and Performance Requirements of the MDR. The Clinical Evaluation Plan must define these questions upfront [66] [23].
- Clinical Sufficiency: "Does the existing clinical data, supplemented by a targeted post-market clinical follow-up study, constitute sufficient clinical evidence to demonstrate compliance with all relevant GSPRs for the device's intended purpose in [Specific Indication]?"
- Real-World Performance: "How does the real-world performance and safety profile of [Medical Device], collected via a structured PMCF study (S), compare to the clinical data generated in the pre-market pivotal investigation?"
Table 2: Essential Research Reagents and Solutions for 2025 Clinical Development
| Research Tool | Function/Application | Product-Type Specificity |
|---|---|---|
| AI-Powered Trial Design Platforms [64] | Uses predictive algorithms to optimize protocol design, simulate trial outcomes, and identify potential operational hurdles. | All types, particularly valuable for complex adaptive designs in ATMPs and drugs. |
| Real-World Data (RWD) Linkage Platforms | Aggregates and standardizes data from electronic health records, claims databases, and patient registries for generating RWE. | Critical for post-market device surveillance and long-term follow-up for ATMPs. |
| Decentralized Clinical Trial (DCT) Technologies [65] | Enables remote patient monitoring, eConsent, and direct-to-patient drug shipment, facilitating more inclusive recruitment. | Drugs and Biologics where remote administration and monitoring are feasible. |
| Systematic Literature Review Software | Supports a structured, reproducible review of existing clinical data, a cornerstone for a MDR-compliant Clinical Evaluation Report. | Primarily for Medical Devices leveraging existing literature to support equivalence or substantial equivalence. |
| Standardized Patient-Reported Outcome (PRO) Instruments | Captures the patient experience and clinical benefit in a validated, quantifiable manner for regulatory review. | All types, increasingly required for labeling claims. |
Methodologies and Experimental Protocols for Robust CER
Adaptive and Innovative Trial Designs
To address the challenges of specificity and efficiency, adaptive trial designs are becoming essential. These include umbrella trials, which test multiple targeted therapies for a single disease type, and platform trials, which allow for the continuous addition of new treatments against a shared control arm in a perpetual protocol [64]. The protocol for such a trial must be meticulously predefined in the statistical analysis plan. Key methodological steps include:
- Pre-specification of Adaptation Points: Clearly define interim analysis points in the protocol, including the timing and the data (e.g., primary endpoint, safety data) that will be reviewed.
- Bayesian Statistical Methods: Implement Bayesian models to accumulate evidence and calculate probabilities of success, which inform decisions like early stopping for efficacy/futility or sample size re-estimation [65].
- Independent Data Monitoring Committee: Establish a charter for an independent committee to review unblinded interim results and make recommendations on protocol adaptations, protecting trial integrity.
- Alpha Spending Functions: Pre-specify statistical methods (e.g., O'Brien-Fleming, Pocock) to control the overall Type I error rate despite multiple looks at the data.
Systematic Approaches to Clinical Evaluation for Devices
The MDR mandates a "systematic and planned process" for clinical evaluation of devices [23]. The methodology, detailed in MEDDEV 2.7/1 rev 4 and MDCG guidance, involves a rigorous, multi-stage workflow.
Diagram 1: MDR Clinical Evaluation Workflow. This shows the structured, iterative process mandated for medical devices.
The protocol for a systematic literature review, a core component of Stage 1, must be defined in the CEP and should include:
- Search Strategy: Detailed search strings for multiple databases (e.g., PubMed, Embase), including PICO elements, limits (date, language), and a record of the search execution date.
- Inclusion/Exclusion Criteria: Objective criteria for selecting relevant articles, based on study design, patient population, intervention/comparator, and outcomes.
- Data Extraction and Appraisal: A standardized form for extracting key data from each study. Each study must then be appraised for its scientific validity (e.g., using risk of bias tools like ROBINS-I) and clinical relevance to the device under evaluation.
- State-of-the-Art Analysis: A synthesis of current best practices and alternative treatments, used as a benchmark for the benefit-risk analysis of the new device.
Integrating Real-World Evidence Generation
Protocols for generating RWE must be as rigorous as those for interventional studies. A protocol for a prospective, real-world study embedded within a PMCF plan for a device would include:
- Objective: Clearly state the research questions, e.g., to characterize the device's performance and safety in routine clinical practice.
- Data Source and Collection: Define the data sources (e.g., patient registry, electronic health records), the variables to be collected, and the methods for ensuring data quality and completeness.
- Statistical Analysis Plan: Detail the statistical methods for analyzing outcomes, including how confounding factors will be addressed (e.g., via propensity score matching or multivariate regression).
- Ethics and Governance: Outline patient consent procedures, data privacy measures, and the study governance structure.
Navigating the clinical development pathway for drugs, biologics, and devices in 2025 demands a sophisticated, product-specific approach. Success hinges on formulating precise research questions that are deeply informed by the evolving regulatory landscape—from the FDA's and EMA's embrace of decentralized trials and RWE to the stringent, continuous evidence requirements of the EU MDR. By leveraging innovative methodologies such as adaptive trial designs, systematic evaluation workflows, and robust real-world data collection protocols, researchers can generate the high-quality, sufficient evidence required for regulatory approval and market access. Ultimately, a proactive strategy that integrates regulatory science, patient-centricity, and advanced statistical methods is paramount for transforming scientific innovation into safe and effective patient therapies across all product types.
Navigating Complexities: Solving Common CER Challenges and Protocol Deviations
Identifying and Classifying Important Protocol Deviations
In clinical research, a protocol deviation is defined as any change, divergence, or departure from the study design or procedures defined in the protocol [70]. The U.S. Food and Drug Administration's (FDA) 2024 draft guidance provides a critical framework for identifying, classifying, and reporting these deviations, emphasizing their impact on data integrity and subject safety [70]. For professionals conducting drug comparative effectiveness research (CER), proper management of protocol deviations is not merely an administrative task but a scientific imperative. The reliability and interpretability of study results—foundational for CER—are directly dependent on the systematic control of study conduct. Identifying which deviations are "important" is a key step in formulating research questions that yield valid, regulatory-compliant conclusions about drug performance in real-world settings.
The International Conference on Harmonisation (ICH) E3(R1) document, adopted by the FDA, further defines important protocol deviations as a subset that might significantly affect the completeness, accuracy, and/or reliability of the study data or that might significantly affect a subject's rights, safety, or well-being [70]. This dual focus on data integrity and ethical conduct forms the cornerstone of effective deviation management.
Classification of Protocol Deviations
Protocol deviations can be categorized along two primary dimensions: intent and significance. A clear understanding of these classifications is essential for determining the appropriate reporting pathway and corrective actions.
- Unintentional Deviations: These are the most common type and represent inadvertent departures from the IRB-approved protocol. They are typically identified after they have occurred. Examples include a subject missing a scheduled visit outside of a pre-defined window or an accidental administration of a prohibited concomitant medication [70].
- Intentional or Planned Deviations: These occur when a sponsor or site consciously decides to deviate from the protocol for a specific participant. A common example is the conscious decision to enroll a participant who meets an exclusion criterion because the investigator and sponsor agree it is in the best interest of the individual [70]. Such deviations often require prior approval unless in an emergency situation.
Furthermore, deviations are stratified based on their potential impact:
- Important Protocol Deviations: This subset has the potential to significantly impact any of the following:
- Subject's rights, safety, or well-being.
- Completeness, accuracy, and/or reliability of the study data [70].
- Other (Not Important) Deviations: These are minor, non-critical, and non-significant departures that do not affect rights, safety, well-being, or data reliability [70].
The following workflow diagram illustrates the logical process for classifying a discovered protocol deviation, incorporating the key decision points of intent and impact.
Reporting Requirements and Responsibilities
The classification of a deviation directly dictates its reporting timeline and the responsible parties. The FDA's draft guidance outlines specific obligations for both sponsors and investigators, which are summarized in the tables below. These requirements are critical for designing monitoring plans and data collection tools for CER.
Sponsor Reporting Requirements
Table 1: Summary of FDA reporting requirements for sponsors of clinical investigations, based on deviation type and study product [70].
| Protocol Deviation Type | Drug Studies | Device Studies |
|---|---|---|
| Intentional & Important | Obtain IRB approval prior to implementation. Notify FDA per sponsor's reporting timelines. For urgent situations: implement immediately, report to IRB ASAP, and notify FDA. [70] | Obtain FDA and IRB approval prior to implementation. For urgent situations: implement immediately, inspect records, report to IRB within 5 business days. [70] |
| Unintentional & Important | Report to FDA and share information with investigators and the IRB within specified reporting timelines. [70] | Report to FDA and share information with investigators and the IRB within specified reporting timelines. [70] |
| Not Important | Not required to report to IRB immediately; may be reported via cumulative events report (semi-annual/annual). [70] | Investigators may implement deviations; sponsors review records that meet five days' notice requirements. [70] |
Investigator Reporting Responsibilities
Table 2: Summary of reporting responsibilities for clinical investigators, based on deviation type and study product [70].
| Protocol Deviation Type | Drug Studies | Device Studies |
|---|---|---|
| Intentional & Important | Obtain sponsor and IRB approval prior to implementation. For urgent situations: implement immediately, promptly report to sponsor and IRB. [70] | Obtain sponsor, FDA, and IRB approval prior to implementation. For urgent situations: implement immediately, maintain records, report to sponsor and IRB within 5 business days. [70] |
| Unintentional & Important | Report to sponsor and IRB within specified reporting timelines. [70] | Report to sponsor and IRB within specified reporting timelines. [70] |
| Not Important | Obtain sponsor approval prior to implementation. [70] | Implement and report to sponsor within 5 days' notice. [70] |
Methodologies for Identification and Monitoring
A proactive, systematic approach to identifying and monitoring deviations is essential for quality CER. The following experimental protocols and methodologies are foundational to this process.
Protocol Deviation Identification Protocol
Objective: To establish a standardized procedure for the consistent and timely identification of protocol deviations at the clinical site level. Materials:
- Study Protocol and Manual of Procedures
- Source Documents and Case Report Forms (CRFs)
- Site delegation logs and training records
- Protocol Deviation Log (electronic or paper-based)
Procedure:
- Source Data Verification: During or after each subject visit, the Clinical Research Coordinator will compare data recorded in source documents against the specific procedures and schedules outlined in the study protocol.
- Check Eligibility: Confirm that the subject continues to meet all inclusion/exclusion criteria. Any subject found to have been enrolled in violation of these criteria must be documented as a deviation.
- Verify Visit Windows: For each scheduled visit, calculate the actual visit date against the permissible window defined in the protocol. Visits outside this window constitute a deviation.
- Review Concomitant Medications: Cross-reference the subject's medication log with the protocol's list of prohibited medications.
- Log the Finding: Immediately upon identification, record all potential deviations in the site's Protocol Deviation Log, including a full description, dates, and subject identifier.
- Internal Review: The Principal Investigator will review each logged entry within a pre-specified timeframe to confirm its validity and classify its importance.
Important Deviation Classification Protocol
Objective: To provide a consistent methodology for assessing the significance of an identified deviation, focusing on its impact on subject safety and data integrity. Materials:
- Identified protocol deviation record
- FDA guidance definitions for "Important Protocol Deviations" [70]
- Study-specific data collection tools and endpoints
Procedure:
- Assess Impact on Subject: Determine if the deviation increased a risk or caused actual harm to the subject's rights, safety, or well-being. For example, failure to report a Serious Adverse Event (SAE) according to protocol timelines would directly impact subject safety.
- Assess Impact on Data: Evaluate if the deviation affects the reliability of data used for the primary or key secondary efficacy endpoints. For instance, a subject missing a primary endpoint assessment would constitute an important deviation.
- Apply the "Significance" Test: Using the FDA/ICH definition, ask: "Could this deviation significantly affect the completeness, accuracy, or reliability of the study data or the subject's rights, safety, or well-being?" [70]
- Document Rationale: The reviewer must document the rationale for the final classification (important vs. not important). This is a critical step for audit trails and regulatory inspection.
Effective management of protocol deviations in clinical research relies on a suite of essential tools and documents. The following table details key resources that form the backbone of a robust quality management system.
Table 3: Key resources and tools for managing protocol deviations in clinical research.
| Item/Tool | Function/Explanation |
|---|---|
| FDA Draft Guidance (2024) | Provides the current regulatory framework and recommendations for defining, identifying, and reporting protocol deviations for drugs and devices [70]. |
| Protocol & Manual of Procedures | The definitive source for defined study procedures; serves as the benchmark against which all conduct is measured for compliance. |
| Protocol Deviation Log | A centralized document (often part of the Trial Master File) for tracking all identified deviations, their classification, and reporting status [70]. |
| ICH E3(R1) Guideline | Provides the internationally harmonized definition of a protocol deviation and an "important" protocol deviation [70]. |
| Electronic Data Capture System | Used to capture study data and often includes edit checks and reports designed to automatically flag potential deviations (e.g., out-of-window visits). |
| Quality Management System | A systematic process designed to ensure trials are conducted and data are generated in compliance with the protocol and GCP; focuses on "critical to quality" factors [70]. |
Implications for Drug Comparative Effectiveness Research
The rigorous identification and classification of protocol deviations are not isolated regulatory activities; they are deeply intertwined with the scientific validity of CER. The following diagram maps the relationship between deviation management and the formulation of key CER research questions, highlighting how data integrity issues can propagate into research conclusions.
For CER, which often relies on data from less-controlled settings than traditional RCTs, understanding the pattern and nature of deviations is critical. A high frequency of important deviations related to patient eligibility, for example, may indicate that the protocol is not feasible for the intended real-world population, thereby challenging the external validity of the research. Consequently, a key question in any drug CER research must be: "To what extent did protocol deviations impact the internal and external validity of the observed comparative effects?" The systematic approach to identifying and classifying deviations outlined in this guide provides the necessary framework to answer this question transparently and defend the resulting conclusions.
Managing Changes in Manufacturing and Quality Control
In the specific context of drug Comparative Effectiveness Research (CER), managing changes in manufacturing and quality control is not merely an operational concern but a foundational scientific prerequisite. CER aims to provide evidence on the effectiveness, benefits, and harms of different treatment options for real-world patients [71]. A change in a drug's manufacturing process, however subtle, can introduce variability that confounds these comparisons, potentially rendering research findings invalid or misleading. Therefore, a robust, systematic approach to managing change is critical to ensuring that the key questions driving drug CER—such as "How does Drug A compare to Drug B for a specific patient population?"—are answered with reliable, reproducible, and unbiased evidence. This guide outlines the technical frameworks and methodologies required to maintain this scientific integrity.
A Framework for Change Control in Regulated Drug Development
A formal change control system is the cornerstone of quality management during manufacturing changes. It provides a structured procedure for proposing, evaluating, approving, implementing, and verifying changes [72]. The primary goal is to ensure that modifications do not adversely affect the quality, safety, or efficacy of the drug product, thereby protecting patient safety and the validity of subsequent research data.
Change Classification System
Changes must be classified based on their potential impact, which dictates the level of scrutiny and documentation required [72]:
- Minor Changes: Have little likelihood of affecting product quality. They require routine documentation and review.
- Major Changes: Require careful analysis and validation before implementation.
- Critical Changes: Have a significant potential to affect product quality, safety, or efficacy. They demand a thorough review, extensive validation, and often, prior approval from regulatory bodies.
The Cross-Functional Change Control Board (CCB)
A cross-functional team is essential for a comprehensive evaluation of any proposed change. The CCB typically includes leadership from [72]:
- Quality Assurance
- Manufacturing Operations
- Regulatory Affairs
- Process Engineering
- Supply Chain Management
Experimental and Validation Protocols for Change Management
Implementing a manufacturing change requires a structured, phase-gated approach to validate that the change produces the intended result without introducing unforeseen risks. The following methodologies are considered best practice.
The Incremental Change Management Methodology
This approach involves completing and validating individual phases of a transformation before moving to the next phase. It prevents cumulative risk caused by the simultaneous rollout of multiple changes and adheres to the fundamental rule: do not change more than one variable at a time [72].
Detailed Protocol:
- Baseline Establishment: Prior to any change, collect definitive performance data (e.g., yield, purity, dissolution profile) from the existing, validated process. This serves as the comparator.
- Single Variable Isolation: Implement the change to one discrete process parameter (e.g., mixing speed, temperature, raw material supplier) while holding all others constant.
- Phase Validation and Data Review: Execute the modified process at a designated scale (e.g., pilot scale) and collect a pre-determined set of quality data. The CCB reviews this data against the baseline and pre-defined acceptance criteria.
- Approval for Progression: Only upon successful validation of the first phase does the project proceed to the next isolated change or scale-up level.
- Full-Scale Validation: Once all individual changes are validated, a full-scale validation batch (or batches) is produced to confirm the integrated process's robustness and consistency.
The "Lift and Shift" Approach
This methodology involves relocating an existing, validated process to a new facility or piece of equipment before making any technology or operational enhancements [72]. This isolates the variable of the new environment and simplifies troubleshooting during the transition.
Quantitative Monitoring and Key Performance Indicators (KPIs)
To gauge the effectiveness of change control initiatives, organizations must track specific, quantitative metrics. These KPIs provide objective data for the "S" (Study) in the PICOTS (Populations, Interventions, Comparators, Outcomes, Timeframes, and Settings) framework used to formulate CER questions [69].
Table 1: Key Performance Indicators for Change Control Effectiveness
| KPI Category | Specific Metric | Definition & Measurement | Target Outcome |
|---|---|---|---|
| Implementation Accuracy | Deviation Rate | The number of process deviations incurred during change implementation. | Zero deviations [72]. |
| Process Efficiency | Approval Cycle Time | Elapsed time from a requested change to its approved implementation [72]. | Reduction in cycle time. |
| Process Efficiency | Total Cycle Time | Elapsed time from change initiation to final results validation [72]. | Reduction in total cycle time. |
| Quality Cost | Cost of Quality | The total cost of quality-related activities (appraisal, prevention) versus the cost of nonquality (failure, rework) [72]. | Favorable ratio; reduction in cost of nonquality. |
| Quality of Output | Rate of Quality Events | The number of quality events (e.g., deviations, out-of-specification results) attributed to the change. | Zero quality events. |
Visualization of Change Management Workflows
Visualizing the process flow is critical for understanding the logical sequence of events, responsibilities, and decision points in change management. The following diagram illustrates the high-level workflow from change initiation to closure.
Implementation Strategy Selection
For the "Develop Implementation & Validation Plan" stage, a strategic decision is required. The following diagram outlines the two primary methodologies.
The Scientist's Toolkit: Essential Research Reagent Solutions
In the context of managing manufacturing changes, certain "reagents" or tools are essential for conducting the necessary experiments and validation studies. These tools enable scientists to generate the high-quality data required for informed decision-making.
Table 2: Key Research Reagent Solutions for Change Management
| Tool Category | Specific Tool/Technique | Function in Change Management |
|---|---|---|
| Statistical Analysis Software | R, SAS, SPSS | Performs quantitative comparison techniques (e.g., t-tests, ANOVA, regression analysis) to statistically validate that process changes do not result in significant differences in critical quality attributes [73]. |
| Data Visualization Platforms | Tableau, Power BI, Qlik | Creates interactive dashboards and control charts for real-time monitoring of process performance and KPI tracking before, during, and after a change is implemented [73]. |
| Quality Management Software (QMS) | AI-Powered QMS (e.g., MasterControl) | Digitizes and automates the change control workflow; uses AI to streamline investigations and predict potential outcomes of proposed changes [72] [74]. |
| Stable Reference Standards | Pharmacopeial Reference Standards (USP, EP) | Provides an unchanging benchmark against which the quality, identity, and strength of materials produced by the changed process can be accurately measured and compared. |
| Advanced Analytical Instruments | HPLC/UPLC, LC-MS/MS | Delivers high-resolution, precise, and accurate data on drug substance and product quality attributes (e.g., impurity profiles, content uniformity) essential for detecting subtle impacts of a process change. |
| Odoroside H | Odoroside H, CAS:18810-25-8, MF:C30H46O8, MW:534.7 g/mol | Chemical Reagent |
Within the rigorous framework of drug CER, where the objective is to generate reliable evidence for healthcare decisions, managing manufacturing changes is a scientific discipline in its own right. The methodologies, metrics, and tools outlined in this guide provide a pathway to maintaining product consistency and, by extension, the integrity of research data. By adhering to a systematic change control process, employing rigorous validation protocols, and leveraging quantitative data for decision-making, pharmaceutical manufacturers and researchers can ensure that the key questions of CER are answered with the highest degree of confidence, ultimately leading to better-informed treatment decisions and improved patient outcomes.
Addressing Uncertainties in Clinical and Economic Evidence
In drug development and comparative effectiveness research (CER), evidence is inherently uncertain. Addressing these uncertainties is not merely a procedural step but a foundational aspect of generating evidence that is valid, trustworthy, and useful for informing healthcare decisions [71]. For researchers and drug development professionals, a systematic approach to uncertainty involves three critical phases: identification of potential uncertainties, rigorous assessment of their potential impact, and proactive mitigation through study design and analysis [75] [76]. This guide provides a technical framework for navigating this process, ensuring that the key questions formulated for drug CER research are both answerable and clinically relevant, thereby supporting better healthcare decisions and outcomes [69].
A Framework for Identifying Uncertainties
The first step in managing uncertainty is its systematic identification. This process should be integrated from the earliest stages of research protocol development [69]. A comprehensive review of methodological literature has identified numerous tools specifically designed for this purpose [75].
Integrating Stakeholder Perspectives
Engaging patients and other stakeholders during the formulation of research questions is a critical success factor in CER [69]. This collaboration helps ensure that the study addresses uncertainties that matter to the end-users of the evidence. Stakeholders are defined as individuals or organizations that use scientific evidence for decisionmaking and therefore have an interest in research results [69]. Their early involvement increases the applicability of the study and facilitates the appropriate translation of results into healthcare practice [69].
Conceptualizing the Research Problem
Formal conceptual models are invaluable for identifying potential uncertainties in the relationship between interventions and outcomes. Directed Acyclic Graphs (DAGs) provide a particularly powerful framework for this purpose, as they help researchers diagram assumed relationships between variables, making underlying assumptions explicit and testable [69]. The process of developing these models with stakeholders creates opportunities to identify and enumerate major assumptions that might otherwise remain hidden [69].
Table: Major Sources of Uncertainty in Clinical and Economic Evidence
| Source Category | Specific Sources of Uncertainty | Potential Impact on Evidence |
|---|---|---|
| Methodological | Inappropriate methods, model structure choices, analytical approaches [75] | Bias in effect estimates, compromised validity [75] |
| Parameter | Imprecision in measurement, sampling error [75] | Reduced precision in confidence intervals and p-values [75] |
| Structural | Model simplifications, incorrect assumptions about causal pathways [75] [76] | Limited generalizability, biased conclusions [76] |
| Evidence Base | Bias, indirectness, unavailability of data [75] | Gaps in evidence, reduced relevance to decision context [75] |
| Heterogeneity | Variability in treatment effects across patient subgroups [69] | Reduced applicability to individual patients or subgroups [69] |
Methodologies for Uncertainty Assessment
Analytic Techniques for Quantitative Assessment
Once uncertainties are identified, they must be rigorously analyzed. A comprehensive review has catalogued 28 distinct methods for uncertainty analysis, which can be categorized by their primary purpose [75].
Probabilistic Sensitivity Analysis (PSA) is considered a cornerstone technique for handling parameter uncertainty. In PSA, model inputs are represented by probability distributions rather than fixed values. When the model is run repeatedly (e.g., 10,000 iterations), these distributions are sampled, generating a distribution of outcome results that reflects the combined uncertainty from all parameters [77].
Value of Information (VOI) Analysis extends uncertainty assessment by quantifying the economic value of collecting additional information to reduce decision uncertainty [75]. This methodology is particularly valuable for informing decisions about whether further research is justified and what type of evidence would be most valuable [75].
Sensitivity Analysis encompasses a range of approaches beyond PSA, including one-way, two-way, and scenario analyses. These techniques systematically vary key parameters or assumptions to test the robustness of study conclusions [77]. Despite guidelines recommending their use, reviews have found that only 30% of economic evaluations conduct sensitivity analysis, and of those, just over half are limited in scope [77].
Handling Specific Data Challenges
Continuous Outcomes in Meta-Analysis: When synthesizing continuous outcomes from multiple studies, investigators face specific methodological challenges. The choice of effect measure (mean difference vs. standardized mean difference) depends on whether studies use the same or different scales [78]. For trials with baseline imbalance, Analysis of Covariance (ANCOVA) approaches provide less biased estimates compared to simple change scores or follow-up scores alone [78].
Dealing with Baseline Imbalance: In randomized trials, baseline characteristics should be similar across groups, but imbalance can occur by chance, particularly in small trials, or due to selection bias from inadequate randomization concealment [78]. Assessment should focus on the clinical importance of differences rather than statistical significance testing [78].
Table: Analysis Methods for Different Uncertainty Types
| Uncertainty Type | Primary Assessment Methods | Key Outputs |
|---|---|---|
| Parameter Uncertainty | Probabilistic Sensitivity Analysis, One-way/Tornado Analysis [77] | Confidence Intervals, Cost-Effectiveness Acceptability Curves [77] |
| Structural Uncertainty | Scenario Analysis, Model Averaging [76] | Comparison of results across different model structures [76] |
| Heterogeneity | Subgroup Analysis, Meta-Regression [69] | Estimates of differential treatment effects across patient subgroups [69] |
| Methodological Uncertainty | Alternative Statistical Models, Bias Analysis [75] | Range of possible estimates under different methodological choices [75] |
The following diagram illustrates the comprehensive workflow for addressing uncertainty in clinical and economic evidence:
Advanced Applications and Implementation
Evidence Synthesis Methods for Complex Interventions
Public health and drug interventions often involve multiple components, creating challenges for evidence synthesis. While methodological advancements have created tools to address these issues, uptake remains limited. A review of National Institute for Health and Care Excellence (NICE) public health guidelines found that only 31% used meta-analysis, though this represented an increase from 23% in 2012 [79]. More sophisticated approaches like network meta-analysis (NMA) and component NMA enable the evaluation of multiple interventions and their combinations, providing decision-makers with fuller information for policy development [79].
Practical Implementation Considerations
Case studies on comprehensive uncertainty assessment reveal both facilitators and barriers to implementation. Key facilitators include multidisciplinary team expertise and the availability of established tools like the Transparent Uncertainty Assessment Tool (TRUST) and EXPLICIT for expert elicitation [76]. Significant barriers include time and resource constraints for research teams and clinical experts, plus a lack of detailed guidance for specific methodological challenges such as expert elicitation question framing, evidence aggregation, and handling structural uncertainty [76].
Table: Research Reagent Solutions for Uncertainty Assessment
| Tool/Toolkit | Primary Function | Application Context |
|---|---|---|
| TRUST Tool [75] [76] | Systematic uncertainty identification across multiple sources | Health economic evaluations, model-based studies |
| Expert Elicitation Frameworks(e.g., EXPLICIT) [76] | Parameter estimation when empirical data is unavailable | Quantifying uncertainties where evidence is lacking |
| Directed Acyclic Graphs (DAGs) [69] | Visualizing causal assumptions and identifying bias | Research conceptualization, confounding control |
| CHEERS Reporting Checklist [75] | Ensuring comprehensive reporting of economic evaluations | Improving transparency and reproducibility |
| GRADE System [75] | Assessing quality of evidence and confidence in estimates | Evidence grading for clinical guidelines |
Addressing uncertainties in clinical and economic evidence requires a systematic, integrated approach throughout the research process. By formally identifying uncertainties through stakeholder engagement and conceptual modeling, applying appropriate analytic techniques tailored to different uncertainty types, and implementing advanced evidence synthesis methods, researchers can produce more robust and decision-relevant evidence for drug development. While practical challenges remain in implementing comprehensive uncertainty assessment, the methodologies and frameworks outlined in this guide provide researchers with a solid foundation for formulating key questions in drug CER that acknowledge, characterize, and address the inherent uncertainties in clinical and economic evidence.
Optimizing Strategies for Data Collection and Integrity
In drug comparative effectiveness research (CER), data integrity is not merely a regulatory hurdle but the foundational element that determines the validity, reliability, and ultimate utility of study findings. The primary goal of CER is to inform specific health decisions by comparing the benefits and harms of alternative interventions in real-world populations [1]. Within this context, data integrity—ensuring data are accurate, complete, consistent, and reliable throughout their lifecycle—is paramount for generating evidence trusted by patients, clinicians, and regulators [80] [81]. Compromised data can lead to incorrect conclusions about a drug's effectiveness, directly impacting patient safety and healthcare decisions [81].
The process of formulating key research questions in drug CER is inextricably linked to data collection strategies. A well-defined research question dictates the necessary data elements, appropriate sources, and rigorous methodologies required to maintain integrity from study inception through dissemination [2] [1]. This guide outlines a comprehensive framework for optimizing data collection and ensuring data integrity, specifically tailored to the demands of modern drug CER.
Foundational Principles: ALCOA+ and CER Standards
The ALCOA+ Framework
For researchers and drug development professionals, the ALCOA+ principles provide a practical framework for operationalizing data integrity. These principles have been widely adopted by regulators and are considered the cornerstone of reliable data in clinical research [82] [83].
- Attributable: Data must clearly indicate who collected it and when. This establishes accountability and traceability for every data point [82].
- Legible: Data must be readable and permanent, preventing misinterpretation over time. This requires transparent documentation methods and adherence to Standard Operating Procedures (SOPs) [82].
- Contemporaneous: Data must be recorded at the time the activity is performed. Retrospective entry increases the risk of errors and memory bias [82].
- Original: The first recorded data (the "source data") must be preserved. Certified copies are acceptable, but the provenance of the data must be clear [82].
- Accurate: Data must be correct, truthful, and free from errors. Robust validation processes and independent review methods are essential for ensuring accuracy [82].
- Complete: All data, including any repeats or corrections, must be included. No data should be omitted [82].
- Consistent: The data should follow a logical sequence, with timestamps that are in the correct order and format [82].
- Enduring: Data must be recorded in a permanent medium (e.g., a dedicated notebook or electronic system) and preserved for the required retention period [82].
- Available: Data must be accessible for review, audit, or inspection throughout its required retention period [82].
Cross-Cutting CER Methodology Standards
The Patient-Centered Outcomes Research Institute (PCORI) outlines critical methodology standards that directly influence data integrity in CER [1]. Key among these are:
- Standard RQ-3: The research must identify the specific population and health decision affected by the research. This ensures the data collected is relevant and directly applicable to a real-world clinical dilemma [1].
- Standard RQ-6: Outcomes measured must be those that "people representing the population of interest notice and care about." This patient-centered focus dictates that data collection extends beyond traditional clinical biomarkers to include patient-reported outcomes (PROs) that matter to individuals living with the condition [1].
- Standard IR-1: Researchers must specify plans for quantitative data analysis a priori. This pre-definition of analytical methods in the study protocol prevents post-hoc data manipulation and ensures the analytical strategy is aligned with the research question [1].
- Standard IR-2: Researchers must assess data source adequacy, ensuring that selected sources can robustly capture exposures, outcomes, and relevant covariates. This is a critical step in the design phase to prevent inherent data quality issues [1].
A Framework for Optimized Data Collection in CER
A rigorous, multi-stage process is essential for collecting high-integrity data capable of supporting robust CER. The following workflow details the key stages, from defining the research question to data analysis, and highlights critical integrity checks at each step.
Phase 1: Planning and Research Design
The initial planning phase is critical for ensuring that the subsequent data collection will be fit-for-purpose and uphold integrity standards.
- Define the CER Question using PICOTS: A structured framework is essential. The PICOTS framework (Population, Intervention, Comparator, Outcomes, Timeframe, Setting) ensures the research question is specific and actionable [2]. For example, a CER study might focus on "Patients with type 2 diabetes (Population) treated with I drug SGLT2 inhibitors versus C DPP-4 inhibitors (Intervention/Comparator) on O heart failure hospitalization and quality of life (Outcomes) over a T 2-year period (Time) in S real-world practice settings (Setting)."
- Conduct a Systematic Review: As per PCORI Standard RQ-1, a systematic review should be performed to identify evidence gaps and justify the need for the new study, ensuring it does not unnecessarily duplicate existing efforts [1].
- Engage Stakeholders: Involve patients, clinicians, and payers throughout the research process. This engagement, highlighted in PCORI Standard PC-1, helps ensure that the research addresses questions and outcomes that are truly important to decision-makers, thereby enhancing the relevance and applicability of the data collected [1].
- Develop a Formal Study Protocol and Analysis Plan: The protocol should be registered on a public platform (e.g., ClinicalTrials.gov) and detail all aspects of the study, including the pre-specified statistical analysis plan (PCORI Standard IR-1). This prevents bias from post-hoc changes to study endpoints or analytical methods [1].
- Select and Assess Data Sources: Whether using existing electronic health records, claims data, or planning primary data collection, the adequacy of the data source must be rigorously assessed (PCORI Standard IR-2). This involves evaluating its ability to accurately capture the key PICOTS elements [1].
Phase 2: Tooling and Pilot Testing
With the protocol defined, the focus shifts to preparing the instruments for data capture.
- Design the Data Collection Tool: Tools can range from Electronic Data Capture (EDC) systems for clinical research to forms designed for abstracting data from medical records. The design must enforce ALCOA+ principles through features like automated audit trails, required fields (to promote completeness), and dropdown menus with predefined values (to ensure consistency and accuracy) [81] [83].
- Pilot Test the Data Collection Tool: A small-scale pilot test is indispensable. It helps identify logistical challenges, confusing questions, technical glitches, and unanticipated data quality issues before full-scale study initiation [84]. Feedback from the pilot should be used to refine the tool and procedures.
- Train Study Personnel: All personnel involved in data collection must receive comprehensive training on the protocol, SOPs, the data collection tool, and the critical importance of data integrity. This minimizes variability and errors introduced by human factors [85] [81].
Phase 3: Execution and Ongoing Quality Control
The execution phase requires vigilant monitoring to maintain data integrity.
- Collect Data: Data should be collected as outlined in the protocol. For primary data collection, real-time entry is preferred over retrospective documentation to adhere to the "Contemporaneous" principle of ALCOA+ [83].
- Implement Real-Time Validation and Monitoring: Automated validation checks within EDC systems can immediately flag out-of-range values, inconsistent entries, or missing data, allowing for prompt correction [81] [86]. A Risk-Based Monitoring approach focuses audit and monitoring resources on the most critical data points and highest-risk study sites, enhancing oversight efficiency [83].
- Clean and Organize Data: This involves a structured process of checking for and resolving discrepancies, validating data against source documents, and handling missing data according to the pre-specified statistical plan [84]. This step ensures the dataset is accurate and consistent before analysis.
Phase 4: Analysis, Preservation, and Dissemination
The final phase ensures the integrity of the data through analysis and beyond.
- Analyze Data per Pre-Specified Plan: The analysis should follow the registered statistical analysis plan to avoid data dredging and p-hacking, which can lead to spurious findings [1].
- Preserve and Archive Data: A formal Data Management Plan (DMP), as required by PCORI Standard IR-7, describes how data will be preserved, documented, and shared to support reproducibility and future scientific inquiry [1].
Quantitative Impacts and Validation Techniques
Understanding the consequences of data integrity failures and the effectiveness of mitigation strategies is crucial for resource allocation and planning.
Table 1: Quantitative Impact of Data Integrity Failures and Validation Techniques
| Metric | Impact/Description | Source |
|---|---|---|
| Annual Cost of Bad Data (US) | $3.1 Trillion | [80] |
| Average Annual Cost per Company | $12.9 Million | [80] |
| Cost of Clinical Trial Termination | Millions of dollars, years of lost research effort | [81] |
| Enterprises Citing Data Quality as a Major Challenge | 71% | [86] |
| Anomaly Detection | A real-time validation method that identifies unusual patterns in data streams that may indicate errors or fraud. | [86] |
| Rule-Based Filters | A real-time validation method that automatically flags data that does not meet predefined criteria or thresholds. | [86] |
| Double Data Entry | A quality control measure where data is entered by two independent individuals to identify discrepancies. | [83] |
The Scientist's Toolkit: Essential Reagents for Data Integrity
Successful implementation of a data integrity strategy relies on a combination of technological solutions, methodological frameworks, and quality control processes. The following table details these essential "research reagents."
Table 2: Essential Research Reagents for Ensuring Data Integrity
| Tool / Solution | Function in Data Integrity |
|---|---|
| Electronic Data Capture (EDC) Systems | Secure digital platforms for collecting and managing study data. They reduce human error, provide real-time data validation, and maintain secure, organized records. [81] [83] |
| Audit Trails | Automated, secure logs that record details of all data changes (who, what, when, and why). They are essential for ensuring data is attributable and traceable. [81] |
| Standard Operating Procedures (SOPs) | Documents that provide transparent, step-by-step processes for every aspect of a clinical trial, minimizing the risk of errors and inconsistencies. [82] [83] |
| Systematic Review Protocols | A pre-defined method for comprehensively synthesizing existing literature to identify evidence gaps and justify new research, as per PCORI Standard RQ-1. [1] |
| Data Management Plan (DMP) | A formal document outlining how data will be collected, organized, preserved, and shared, ensuring data is enduring and available for future use. [1] |
| Patient-Reported Outcome (PRO) Measures | Standardized questionnaires used to collect data directly from patients on outcomes they notice and care about, such as symptoms and quality of life (PCORI Standard PC-3). [1] |
Integrated Data Quality Control Cycle
Maintaining data integrity is not a linear process but a continuous cycle of planning, prevention, monitoring, and improvement. The following diagram illustrates this integrated quality control system, showing how various components interact to create a self-correcting and reinforcing framework.
For drug comparative effectiveness research to reliably inform healthcare decisions, the integrity of the underlying data is non-negotiable. By anchoring research in a clearly formulated question using the PICOTS framework, adhering to ALCOA+ principles and CER methodology standards, and implementing a rigorous, multi-stage data collection process with continuous quality control, researchers can produce evidence that is not only scientifically valid but also truly meaningful for patients and clinicians. As the complexity and scale of CER grow, a proactive and systematic commitment to data integrity remains the most critical factor in ensuring research findings translate into better, safer patient care.
Mitigating Risks in Studies for Rare Diseases and Innovative Therapies
Drug development for rare diseases presents a distinct set of challenges that demand innovative approaches to mitigate risk. These challenges stem from small patient populations, limited natural history data, and often poorly characterized disease mechanisms, making traditional clinical trial designs and drug development pathways ill-suited or infeasible [9] [87]. The imperative to generate robust evidence of efficacy and safety despite these limitations has driven the creation of new regulatory pathways, advanced trial designs, and the strategic use of all available data sources. For developers, a proactive risk mitigation strategy is not merely beneficial but essential for navigating the scientific and regulatory complexities of this field. This guide provides a technical framework for formulating key questions and implementing strategies that protect the integrity of comparative clinical effectiveness research (CER) in rare diseases, ensuring that new therapies deliver meaningful benefits to patients.
Foundational Challenges and Regulatory Evolution
Quantifying the Development Hurdles
The inherent difficulties in rare disease drug development are quantifiable. An analysis of 40 new molecular entities (NMEs) for rare genetic diseases approved between 2015 and 2020 revealed that only 53% of development programs conducted at least one dedicated dose-finding study [87]. This critical gap underscores the challenge of optimizing a drug's benefit-risk profile in small populations. Furthermore, the same analysis found that the majority of primary endpoints (69%) used in these limited dose-finding studies were biomarkers, highlighting the frequent reliance on surrogate endpoints in the face of constrained patient numbers for measuring clinical outcomes [87].
Table 1: Key Quantitative Challenges in Rare Disease Drug Development (2015-2020)
| Challenge Area | Metric | Finding | Implication |
|---|---|---|---|
| Dose-Finding | Programs with ≥1 dedicated dose-finding study | 21 of 40 (53%) | High risk of suboptimal dosing in pivotal trials |
| Endpoint Selection | Biomarkers as primary endpoints in confirmatory trials | 32 of 61 trials (52%) | Need for robust biomarker validation and regulatory alignment |
| Endpoint Alignment | Dose-finding & confirmatory trial primary endpoint match | 9 of 13 programs (69%) | Critical for ensuring dose-response data is relevant to approval endpoint |
Evolving Regulatory Frameworks for Ultra-Rare Diseases
Recognizing that the standard development paradigm is failing for many ultra-rare conditions, the U.S. Food and Drug Administration (FDA) has introduced new frameworks. A significant development in late 2025 is the Plausible Mechanism Pathway [9]. This pathway is designed for situations where randomized controlled trials are not feasible and is structured around five core elements that a sponsor must demonstrate:
- Identification of a specific molecular or cellular abnormality, not a broad set of consensus diagnostic criteria.
- The medical product targets the underlying or proximate biological alterations.
- The natural history of the disease in the untreated population is well-characterized.
- Confirmation exists that the target was successfully drugged or edited.
- There is an improvement in clinical outcomes or course of disease [9].
This pathway leverages the expanded access, single-patient Investigational New Drug (IND) paradigm as an evidentiary foundation. Successive successful outcomes in patients with different bespoke therapies can support a marketing application. Crucially, the pathway requires a significant post-market evidence-gathering commitment, including the collection of real-world evidence (RWE) to demonstrate preserved efficacy and monitor for unexpected safety signals [9].
Complementing this, the FDA's Rare Disease Evidence Principles (RDEP) process clarifies that for certain rare diseases with known genetic defects and very small populations (e.g., fewer than 1,000 U.S. patients), substantial evidence of effectiveness can be established through one adequate and well-controlled trial, which may be a single-arm design, accompanied by robust confirmatory evidence from external controls or natural history studies [9].
Strategic Risk Mitigation in Study Design and Data Generation
Innovative Clinical Trial Designs
Traditional trial designs are often unsuitable for the rare disease space. Adopting innovative designs is a primary method for de-risking development by maximizing the information gained from every single patient [88].
- Bayesian and Adaptive Designs: These designs allow for the incorporation of external information or for modifying the trial based on accumulating data, making them highly efficient. Bayesian trials can require between 30% and 2,400% fewer participants than frequentist trials because they allow information to be "borrowed" from past or similar studies [88]. This is achieved through statistical techniques that use prior probability distributions, which are updated with data from the current trial to form a posterior distribution. This approach is particularly valuable for dose-finding and proof-of-concept studies.
- Master Protocols: These overarching frameworks, such as basket, umbrella, or platform trials, enable the efficient evaluation of multiple therapies or patient subpopulations within a single infrastructure. This is especially useful for genetically heterogeneous rare diseases [89].
- Single-Arm Trials with External Control Arms (ECAs): When randomization is impractical or unethical, a well-constructed ECA can provide the necessary comparative context. ECAs are built by emulating a control group from real-world data (RWD), historical clinical trial data, or via predictive models and synthetic patient generation using artificial intelligence [88]. A key example is the accelerated approval of a drug for refractory precursor B-cell acute lymphoblastic leukemia, which was based on a single-arm phase II trial supplemented by a historical control arm [88].
Leveraging Real-World Data and Data Augmentation
The past five years have seen unprecedented advances in the access to and interoperability of RWD, transforming drug development paradigms [88].
- Informing Trial Design: RWD can be used to characterize disease progression profiles, identify relevant and sensitive endpoints, and anticipate baseline risks and standard-of-care treatment effects. This de-risks trial design by ensuring it is grounded in realistic clinical scenarios [88].
- Data Augmentation via Bayesian Borrowing: This analytical technique formally incorporates information from clinically relevant external evidence, such as historical trial data or RWD, into the analysis of a new trial. This increases the statistical power without compromising validity, which is crucial for underpowered studies in small populations. For instance, this approach has been used to support drug registration in new geographic regions by borrowing strength from a global study, considerably accelerating medicine availability [88].
In Silico Technologies and Computational Modeling
Computational tools, or in silico technologies, offer scalable, hypothesis-driven methods to overcome the scarcity of patient data. Their applications span the entire development lifecycle [90].
Table 2: In Silico Technologies for De-risking Rare Disease Research
| Context of Use (CoU) | Technology Examples | Application in Risk Mitigation |
|---|---|---|
| CoU1: Diagnosis & Characterization | AI-enhanced genomic pipelines, NLP for EHR analysis, structural modeling (SWISS-MODEL) | Identifies specific patient populations and elucidates disease mechanisms for trial enrichment [90]. |
| CoU2: Drug Discovery | Virtual screening, QSAR modeling, network pharmacology (e.g., PandaOmics) | Accelerates target identification and drug repurposing, reducing early-stage resource commitment [90]. |
| CoU3: Preclinical Development | Quantitative Systems Pharmacology (QSP), mechanistic multiscale models, organ-on-chip simulations | Predicts drug responses and identifies biomarkers, informing first-in-human trial design and reducing animal use [90]. |
| CoU4: Clinical Trial Design | Pharmacokinetic/pharmacodynamic (PK/PD) models, virtual trials, synthetic control arms | Supports dose selection, extrapolation across age groups, and generates external comparators, optimizing trial feasibility [90]. ``` |
The Scientist's Toolkit: Key Research Reagent Solutions
The successful execution of the methodologies above often depends on critical reagents and tools.
Table 3: Essential Research Reagent Solutions for Rare Disease Studies
| Reagent/Tool | Function | Application in Risk Mitigation |
|---|---|---|
| Validated Biomarker Assays | Quantitatively measure a biological process or pharmacological response to a therapeutic intervention. | Serves as a surrogate endpoint in dose-finding studies where clinical outcome data is limited; requires rigorous analytical validation [87]. |
| Patient-Derived Cell Lines & Organoids | In vitro models derived from patient tissues that recapitulate key aspects of the disease biology. | Provides a human-relevant system for target validation, efficacy testing, and dose-response modeling, de-risking early development [90]. |
| Genomic Reference Standards | Well-characterized controls for genomic sequencing assays (e.g., for variant calling). | Ensures accuracy and reproducibility in patient stratification and molecular diagnosis, a cornerstone of targeted therapies [90]. |
| High-Quality Natural History Data | Longitudinal data on the course of a disease in the absence of treatment. | Serves as a historical control for single-arm trials; critical for validating endpoints and interpreting trial results [9] [88]. |
Experimental Protocols for Key Methodologies
Protocol: Establishing an External Control Arm (ECA) from Real-World Data
Objective: To create a robust historical control for a single-arm interventional trial by emulating the trial's eligibility criteria and endpoint assessment in a RWD source.
Methodology:
- RWD Source Selection: Identify high-quality, fit-for-purpose RWD sources (e.g., disease registries, electronic health records from specialized centers) that capture the relevant patient population, treatments, and outcomes.
- Trial Emulation: Apply the key eligibility criteria of the interventional trial to the RWD cohort to select a comparable patient group. This process must be meticulously documented.
- Endpoint Harmonization: Define and validate the method for ascertaining the trial's primary endpoint within the RWD. This may require adjudication committees or algorithmic mapping of clinical data to the endpoint definition.
- Statistical Analysis Plan:
- Propensity Score Matching/Weighting: To account for confounding factors, each patient in the interventional arm is matched with one or more patients from the ECA based on propensity scores, which model the probability of being in the interventional group given baseline characteristics.
- Outcome Comparison: Compare the outcome between the matched groups using appropriate statistical models (e.g., Cox regression for time-to-event endpoints, logistic regression for binary endpoints). The analysis should include sensitivity analyses to assess the robustness of findings to unmeasured confounding [88].
Protocol: Bayesian Dynamic Borrowing for a Regional Trial
Objective: To augment the evidence from a new, small regional trial by borrowing strength from a previously conducted global study, thereby increasing the statistical power for regulatory decision-making.
Methodology:
- Prior Elicitation: Define a prior distribution for the treatment effect in the new regional trial based on the results of the historical global study. The prior can be, for example, a normal distribution centered on the global study's estimated treatment effect.
- Borrowing Strength Mechanism: Implement a model, such as a power prior or commensurate prior, that dynamically controls the amount of information borrowed from the historical data. The degree of borrowing is based on the similarity (commensurability) between the historical and new data. If the new data strongly conflicts with the historical data, the model automatically borrows less to avoid bias.
- Analysis: Fit a Bayesian model (e.g., using Markov Chain Monte Carlo methods) that combines the prior distribution with the likelihood of the observed data from the new regional trial.
- Inference: The output is a posterior distribution for the treatment effect, which provides a probabilistically combined estimate. Regulatory conclusions are drawn based on this posterior, for instance, by determining the probability that the treatment effect is greater than a pre-specified threshold [88].
Workflow Visualization: Integrating Strategies for a Cohesive Development Plan
The following diagram illustrates how these risk mitigation strategies can be integrated throughout the drug development lifecycle for a rare disease therapy, creating a cohesive and evidence-driven plan.
Diagram Title: Integrated Risk Mitigation Across Drug Development
For researchers and drug development professionals, mitigating risks in rare disease studies requires a paradigm shift from reactive problem-solving to proactive, strategic planning. The key is to formulate and continuously revisit critical questions that force a rigorous evaluation of the development strategy within the modern regulatory and methodological context. These questions should include:
- Regulatory Strategy: Is our pathway (e.g., Plausible Mechanism, RDEP, Accelerated Approval) still the most relevant given the latest FDA guidance and the nature of our evidence? [9] [91]
- Trial Design & Analysis: Have we fully exploited innovative designs (Bayesian, adaptive) and data augmentation techniques (ECA, RWE) to maximize power and minimize patient burden? [88]
- Dose Selection: Is our dose justification, potentially based on biomarker data and PK/PD modeling, robust enough to meet regulatory standards for approval? [87]
- Data & Analytics: How robust is our data analytics approach, and are we leveraging in silico technologies to de-risk decisions from discovery through post-market monitoring? [90] [91]
- Post-Market Commitment: Do we have a feasible and rigorous plan for post-market evidence generation that will confirm the therapy's value and ensure its continued availability? [9]
By systematically addressing these questions and integrating the advanced strategies outlined in this guide, developers can navigate the high-stakes landscape of rare disease therapy development with greater confidence, ultimately accelerating the delivery of effective treatments to patients who face significant unmet medical needs.
Ensuring Credibility: Validating CER Outcomes and Demonstrating Value
Techniques for Validating CER Methods and Analytical Approaches
In the context of drug development, Comparative Effectiveness Research (CER) provides essential evidence on the benefits and harms of available prevention, diagnosis, and treatment options. The analytical methods that generate bioanalytical and clinical chemistry data are foundational to this evidence. Validating these methods ensures that the results are consistent, reproducible, and reliable, making them suitable for supporting critical research conclusions and regulatory decisions [92]. This guide details the technical requirements and protocols for establishing this suitability, framed within the broader objective of formulating precise CER research questions.
Formulating Key Research Questions for Drug CER
A well-constructed research question is the cornerstone of any rigorous CER study, as it directs the scientific methodology and analytical validation strategy. The PICO framework is a established tool for formulating a focused clinical research question [42] [43].
- P (Patient/Population): The specific patient group or population of interest. This should be defined by relevant baseline and clinical characteristics such as age, medical condition, and disease severity [42].
- I (Intervention): The intervention, exposure, or action being studied (e.g., a new drug therapy, a diagnostic method) [42].
- C (Comparison): The alternative to which the intervention is compared (e.g., an active control, a placebo, or usual care) [42].
- O (Outcome): The effect or outcome being evaluated, which the analytical methods must reliably measure (e.g., change in biomarker concentration, pharmacokinetic parameters) [42].
Beyond a sound structure, a good CER research question should also meet the FINER criteria, ensuring it is Feasible, Interesting, Novel, Ethical, and Relevant to the field [42]. This disciplined approach to question formulation ensures that the subsequent analytical method validation is targeted and fit-for-purpose.
Core Validation Parameters and Experimental Protocols
For an analytical method to be deemed 'suitable for its intended use,' a set of key performance characteristics must be experimentally demonstrated. The following sections detail the core parameters, their definitions, and standard validation protocols [92].
Specificity and Selectivity
- Definition: The ability of the method to measure the analyte unequivocally in the presence of other components, such as impurities, degradants, or matrix components [92].
- Experimental Protocol:
- Analyze a blank sample (the biological matrix without the analyte).
- Analyze samples containing the analyte of interest.
- Analyze samples with potential interfering substances (e.g., metabolites, concomitant medications, matrix components).
- The method should demonstrate no significant interference from other components at the retention time of the analyte, confirming its ability to discriminate the analyte from everything else [92].
Linearity and Range
- Definition: Linearity is the ability of the method to obtain results directly proportional to the concentration of the analyte. The range is the interval between the upper and lower concentration levels for which linearity, accuracy, and precision have been demonstrated [92].
- Experimental Protocol:
- Prepare and analyze a minimum of 5 to 8 concentration levels across the expected range, typically from the Lower Limit of Quantification (LLOQ) to the Upper Limit of Quantification (ULOQ).
- Analyze each concentration level in replicate (e.g., 3-5 times).
- Plot the measured response against the nominal concentration.
- Perform a linear regression analysis. The correlation coefficient (r), y-intercept, slope, and residual sum of squares should be reported. A coefficient of determination (r²) of ≥ 0.99 is typically expected for chromatographic assays [92].
Precision
- Definition: The closeness of agreement between a series of measurements from multiple sampling of the same homogenous sample. It is usually expressed as relative standard deviation (%RSD) [92].
- Experimental Protocol:
- Repeatability: Intra-assay precision assessed by analyzing a minimum of 6 replicates at 100% of the test concentration within a single run [92].
- Intermediate Precision: Precision assessed by analyzing the same samples over different days, with different analysts, or on different equipment. A minimum of 6 determinations at 100% concentration is standard [92].
- Acceptance Criteria: For bioanalytical assays, %RSD should generally be ≤ 15%, and ≤ 20% at the LLOQ.
Accuracy
- Definition: The closeness of agreement between the measured value and a reference value, considered the true or accepted value. It is reported as percentage recovery [92].
- Experimental Protocol:
- Prepare quality control (QC) samples at a minimum of 3 concentration levels (e.g., low, mid, and high) covering the analytical range.
- Analyze a minimum of 5 to 6 replicates at each QC level.
- Calculate the mean measured concentration for each level.
- Accuracy (%) = (Mean Measured Concentration / Nominal Concentration) × 100.
- Acceptance Criteria: Accuracy is generally within ±15% of the nominal value, and ±20% at the LLOQ [92].
Quantification Limit (LOQ) and Detection Limit (LOD)
- LOQ: The lowest amount of analyte that can be quantified with acceptable accuracy and precision [92].
- LOD: The lowest amount of analyte that can be detected, but not necessarily quantified [92].
- Experimental Protocol (Signal-to-Noise Ratio):
- Analyze samples with known low concentrations of analyte.
- Compare the magnitude of the analyte signal with the background noise.
- A signal-to-noise ratio of 10:1 is generally acceptable for LOQ, and 3:1 for LOD.
- Alternative methods include visual evaluation or calculation based on the standard deviation of the response and the slope of the calibration curve [92].
Robustness
- Definition: A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters, indicating its reliability during normal usage [92].
- Experimental Protocol:
- Deliberately introduce small changes to method parameters (e.g., mobile phase pH (±0.2 units), column temperature (±2°C), flow rate (±10%)).
- Analyze system suitability or QC samples under these modified conditions.
- Evaluate the impact on key performance metrics like resolution, tailing factor, and precision.
The following table summarizes the typical acceptance criteria for these key validation parameters in a quantitative impurity or assay method.
Table 1: Summary of Key Analytical Method Validation Parameters and Acceptance Criteria
| Performance Characteristic | Validation Protocol Summary | Typical Acceptance Criteria |
|---|---|---|
| Specificity | Analyze blank, analyte, and potential interferents. | No interference observed at the analyte retention time [92]. |
| Linearity | Analyze 5-8 concentration levels in replicate. | Correlation coefficient (r²) ≥ 0.99 [92]. |
| Precision (Repeatability) | Analyze ≥6 replicates at 100% test concentration. | Relative Standard Deviation (%RSD) ≤ 15% [92]. |
| Accuracy | Analyze ≥5 replicates at 3 concentration levels (low, mid, high). | Mean recovery within 100% ± 15% [92]. |
| Range | Established from linearity, accuracy, and precision data. | The interval from LLOQ to ULOQ where all parameters are met [92]. |
| LOQ (Quantification Limit) | Determine lowest level with acceptable accuracy/precision. | Signal-to-Noise ≥10:1; Accuracy ±20%; Precision ≤20% RSD [92]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful execution of a validated analytical method relies on a set of high-quality materials and reagents. The following table details essential items for a typical bioanalytical workflow, such as a Liquid Chromatography-Mass Spectrometry (LC-MS) assay.
Table 2: Key Research Reagent Solutions for Bioanalytical Method Validation
| Item | Function / Explanation |
|---|---|
| Analyte Reference Standard | A highly characterized substance used to prepare calibration standards; its purity and stability are critical for data accuracy [92]. |
| Stable Isotope-Labeled Internal Standard (IS) | Added to all samples to correct for variability in sample preparation and ionization efficiency in MS detection, improving precision and accuracy. |
| Appropriate Biological Matrix | The blank material (e.g., plasma, serum, urine) from the species of interest, used to prepare calibration standards and QCs, matching the study samples. |
| LC-MS Grade Solvents & Reagents | High-purity solvents and additives for mobile phase and sample preparation to minimize background noise and ion suppression in MS. |
| Quality Control (QC) Samples | Samples with known analyte concentrations, prepared independently from calibration standards, used to monitor assay performance during validation and study runs. |
Workflow and Decision Pathway for Method Validation
The following diagram illustrates the logical workflow for developing and validating an analytical procedure, from initial question formulation to final application in drug CER.
Advanced Validation Paradigms: Lifecycle and Modern Approaches
The traditional approach to validation is increasingly being supplemented by more dynamic, holistic frameworks. The Quality-by-Design (QbD) principles, as outlined in ICH Q8 and Q9, advocate for building quality into the method from the beginning [93]. This involves:
- A Priori Risk Assessment: Identifying potential variables that may impact method performance early in development [93].
- Design of Experiments (DoE): Using statistical models to systematically optimize method conditions and establish a Method Operational Design Range (MODR), which defines the space within which method parameters can be adjusted without impacting validity [93].
- Analytical Procedure Lifecycle Management: As per ICH Q12, this views validation as an ongoing process involving three stages: (1) procedure design, (2) procedure performance qualification, and (3) ongoing procedure performance verification [93]. This aligns with modern regulatory expectations, including those in the forthcoming ICH Q2(R2) and Q14 guidelines [93].
Furthermore, technologies like Multi-Attribute Methods (MAM) using LC-MS are streamlining the analysis of complex biologics by consolidating the measurement of multiple quality attributes into a single assay [93]. The integration of Real-Time Release Testing (RTRT) and Process Analytical Technology (PAT) allows for quality control to be performed in-line during manufacturing, moving away from traditional end-product testing [93].
In pharmaceutical research and development, generating robust comparative evidence is paramount for informing regulatory decisions, health technology assessment (HTA), and clinical practice. While head-to-head randomized controlled trials (RCTs) represent the gold standard for direct treatment comparison, ethical considerations, practical constraints, and economic factors often make such direct comparisons unfeasible or impractical. In these situations, indirect treatment comparisons (ITCs) provide valuable analytical frameworks for estimating relative treatment effects when direct evidence is absent. These methodologies enable researchers and drug developers to formulate critical questions about a drug's relative performance within the therapeutic landscape, thereby supporting comprehensive comparative effectiveness research (CER).
The selection of an appropriate comparative framework is not merely a statistical exercise but a fundamental strategic decision that influences a drug's evidentiary foundation throughout its lifecycle. Within health technology assessment bodies, there is a clear preference for head-to-head RCTs when assessing the comparative efficacy of two or more treatments [94]. However, HTA agencies recognize that ITCs can provide alternative evidence where direct comparative evidence may be missing, though their acceptability remains variable and is typically evaluated on a case-by-case basis [94]. Understanding the strengths, limitations, and appropriate application contexts for both head-to-head and indirect comparison approaches is essential for constructing valid, reliable, and persuasive comparative effectiveness data.
Head-to-Head Comparisons: The Gold Standard
Fundamental Principles and Design
Head-to-head comparisons in randomized controlled trials (RCTs) represent the most methodologically rigorous approach for evaluating the relative efficacy and safety of two or more interventions. These studies are characterized by their controlled experimental design, which involves the direct, concurrent comparison of treatments under standardized conditions. The core principle underpinning RCTs is randomization, a process that randomly allocates participants to different treatment groups, thereby minimizing selection bias and ensuring that both known and unknown confounding factors are distributed equally across groups. This design creates a balanced baseline, allowing researchers to attribute outcome differences directly to the treatments being compared rather than extraneous variables.
The superiority of head-to-head RCTs stems from their ability to establish causal relationships between interventions and outcomes with high internal validity. By controlling experimental conditions, implementing blinding procedures (where feasible), and applying strict protocolized treatments, RCTs significantly reduce the risk of bias that often plagues observational study designs. This controlled environment enables a clear, unconfounded assessment of relative treatment effects, providing the most reliable evidence for regulatory and reimbursement decisions. Health technology assessment (HTA) agencies consistently express a clear preference for head-to-head RCTs when they are available and ethically feasible [94].
Comparative Framework: Head-to-Head vs. Real-World Evidence
The table below contrasts the fundamental characteristics of data generated from traditional head-to-head clinical trials versus real-world data sources, highlighting their complementary roles in evidence generation [95].
Table 1: Comparison of Head-to-Head Clinical Trial Data and Real-World Data
| Characteristic | Head-to-Head Clinical Trials | Real-World Data |
|---|---|---|
| Primary Aim | Efficacy assessment under ideal conditions | Effectiveness/response in clinical practice |
| Study Setting | Controlled research environment | Real-world clinical practice |
| Patient Inclusion | Strict criteria for patient inclusion | No strict criteria for patient inclusion |
| Data Driver | Investigator-centered | Patient-centered |
| Comorbidities & Concomitant Medications | Included only according to study protocol | Reflect real-world clinical practice |
| Treatment Protocol | Fixed, according to study protocol | Variable, determined by market and physician |
| Comparator | Placebo or standard care | Patient need, variable real-world treatments |
| Role of Physician | Designated investigator | Multiple physicians, as decided by patient |
| Response Monitoring | Continuous throughout study duration | Variable, determined by clinical practice |
Experimental Design Considerations
Designing a robust head-to-head trial requires meticulous planning of several key elements. The target population must be carefully defined to balance internal validity with generalizability, while endpoint selection should include clinically meaningful outcomes relevant to patients, clinicians, and regulators. Sample size calculation is crucial to ensure adequate statistical power to detect clinically important differences between treatments, with adjustments for multiple comparisons if necessary. Additionally, blinding procedures (single, double, or open-label) must be implemented where feasible to minimize performance and detection bias, though each approach has practical and ethical considerations in specific clinical contexts.
Indirect Treatment Comparisons: Methodological Frameworks
Foundations and Rationale for ITCs
Indirect treatment comparisons (ITCs) encompass a suite of statistical methodologies that enable comparative effectiveness assessments when direct head-to-head evidence is unavailable. These techniques are particularly valuable in scenarios where ethical constraints prevent direct comparison (e.g., in life-threatening diseases where placebo controls may be unethical), practical limitations restrict feasibility (e.g., in rare diseases with small patient populations), or multiple comparators make comprehensive direct testing impractical [94]. Furthermore, the rapidly evolving treatment landscapes in many therapeutic areas often outpace the completion of long-term RCTs, creating evidence gaps that ITCs can help address.
The fundamental premise of ITCs is the use of a common comparator to facilitate indirect comparison between treatments of interest. Typically, this common comparator is placebo or a standard care treatment that has been evaluated in separate studies. By establishing how Treatment A performs versus Common Comparator C, and how Treatment B performs versus the same Common Comparator C, statistical methods can infer the relative performance of Treatment A versus Treatment B. This approach moves beyond naïve comparisons (which simply compare outcomes across different trials without adjustment) and employs sophisticated statistical adjustments to account for between-trial differences, thereby providing more valid estimates of relative treatment effects [94].
Key ITC Techniques and Applications
Systematic literature reviews have identified several established ITC techniques, each with distinct methodological approaches, data requirements, and application contexts [94]. The most frequently applied techniques include:
Table 2: Key Indirect Treatment Comparison Techniques and Characteristics
| ITC Technique | Description | Primary Application Context | Data Requirements |
|---|---|---|---|
| Network Meta-Analysis (NMA) | Simultaneously compares multiple treatments in a connected evidence network using Bayesian or frequentist methods | Comparing multiple interventions when a connected network exists | Aggregate data from multiple studies |
| Bucher Method | Simple adjusted indirect comparison for two treatments via common comparator | Basic indirect comparison of two treatments with common comparator | Aggregate data from two studies |
| Matching-Adjusted Indirect Comparison (MAIC) | Reweights individual patient data from one trial to match aggregate baseline characteristics of another | Single-arm trials or when IPD available for only one study | IPD for at least one study |
| Simulated Treatment Comparison (STC) | Models treatment effect using individual patient data to adjust for effect modifiers | When effect modifiers are known and measured | IPD for at least one study |
| Network Meta-Regression | Extends NMA by incorporating trial-level covariates to explain heterogeneity | When heterogeneity is present in the evidence network | Aggregate data from multiple studies |
Among these techniques, Network Meta-Analysis (NMA) is the most frequently described and applied method, featured in 79.5% of included articles in a recent systematic review [94]. The appropriate selection of an ITC technique depends on several factors, including the feasibility of a connected evidence network, the presence and extent of heterogeneity between studies, the number of relevant studies available, and access to individual patient-level data (IPD) [94].
Methodological Workflow for Indirect Comparisons
The following diagram illustrates the systematic workflow for conducting robust indirect treatment comparisons, from evidence identification through to interpretation and validation.
Methodological Considerations and Best Practices
Assessing Similarity and Heterogeneity
A fundamental assumption underlying valid indirect comparisons is the similarity assumption, which requires that the studies being compared are sufficiently similar in their clinical and methodological characteristics. This encompasses similarities in trial populations, study designs, treatment protocols, outcome definitions, and measurement timepoints. Methodological approaches to assess and address heterogeneity include:
- Clinical and Methodological Similarity Assessment: Systematic evaluation of potential effect modifiers across studies, including patient demographics, disease severity, concomitant treatments, and study design features.
- Statistical Heterogeneity Evaluation: Quantitative assessment of variability in treatment effects beyond chance, typically using I² statistics or similar measures.
- Network Meta-Regression: Incorporation of trial-level covariates into statistical models to explore and potentially adjust for sources of heterogeneity [94].
Formal methods to determine similarity in the context of ITC are emerging but have not yet been widely applied in practice. A review of National Institute for Health and Care Excellence (NICE) technology appraisals found that companies frequently used narrative summaries to assert similarity, often based on a lack of significant differences, rather than applying formal statistical methods for assessing equivalence [96].
Analytical Framework for Comparative Effectiveness Research
The following diagram outlines a comprehensive decision framework for selecting appropriate comparative methodologies based on evidence availability and research objectives.
Validation and Sensitivity Analysis
Robust ITC requires comprehensive validation and sensitivity analyses to assess the reliability of findings and explore the impact of methodological assumptions. Key approaches include:
- Consistency Assessment: Evaluation of agreement between direct and indirect evidence where both are available (node-splitting analysis).
- Sensitivity Analyses: Exploration of how results vary under different statistical models (fixed vs. random effects), inclusion criteria, or outlier scenarios.
- Goodness-of-Fit Evaluation: Assessment of model fit using deviance information criteria (DIC) in Bayesian analyses or similar measures in frequentist approaches.
Implementing Comparative Frameworks in Drug Development
Successful implementation of comparative analysis frameworks requires access to specialized methodological expertise and analytical resources. The following table outlines essential components of the methodological toolkit for comparative effectiveness research.
Table 3: Research Reagent Solutions for Comparative Effectiveness Research
| Tool/Resource | Function/Application | Examples/Specifications |
|---|---|---|
| Statistical Software Packages | Implement advanced statistical models for ITC and NMA | R (gemtc, pcnetmeta), Python, SAS, WinBUGS/OpenBUGS |
| Systematic Review Tools | Facilitate literature identification, screening, and data extraction | DistillerSR, Covidence, Rayyan |
| Risk of Bias Assessment Tools | Evaluate methodological quality of included studies | Cochrane RoB tool, ROBINS-I |
| Data Standardization Frameworks | Harmonize outcome definitions and data collection across studies | CDISC standards, COMET initiative for core outcome sets |
| Visualization Tools | Present complex comparative evidence clearly and accurately | ChartExpo, Ajelix BI, R ggplot2, Python matplotlib |
Integrating Comparative Evidence Throughout the Product Lifecycle
Strategic planning for comparative evidence generation should begin early in drug development and continue throughout the product lifecycle. In early development phases, formulation studies and pre-formulation characterization provide critical foundation data that will influence later comparative assessments [97]. Key pharmaceutical development questions that ultimately affect comparative profiles include salt selection, particle size optimization, and solid-state form characterization, all of which influence bioavailability and therapeutic performance [97].
As development progresses, comparative frameworks should be integrated with real-world evidence (RWE) generation strategies to complement and extend findings from controlled trials [95]. Real-world data from sources such as electronic health records, claims databases, and patient registries can provide insights into effectiveness in broader patient populations, long-term outcomes, and economic implications that may not be fully captured in traditional clinical trials [95].
Comparative analysis frameworks, encompassing both head-to-head comparisons and indirect treatment comparisons, provide essential methodologies for generating robust comparative effectiveness evidence throughout the drug development lifecycle. While head-to-head RCTs remain the gold standard for direct treatment comparison, ITC methods offer valuable approaches when direct evidence is unavailable or impractical to obtain. The expanding methodological sophistication of ITC techniques, including network meta-analysis, matching-adjusted indirect comparisons, and related approaches, continues to enhance their utility and applicability across diverse therapeutic areas.
The strategic application of these frameworks requires careful consideration of methodological assumptions, potential sources of bias, and validation through comprehensive sensitivity analyses. Furthermore, the emerging role of real-world evidence offers complementary insights that can strengthen comparative assessments. As these methodologies continue to evolve, clearer international consensus and guidance on methodological standards will be essential to improve the quality and acceptability of comparative evidence submitted to regulatory and health technology assessment agencies [94] [96]. By systematically applying these comparative frameworks, drug developers and researchers can generate more comprehensive and reliable evidence to inform clinical practice, regulatory decisions, and healthcare policy.
Assessing Robustness through Sensitivity and Scenario Analyses
In the field of drug comparative effectiveness research (CER), the validity of study findings is paramount for informing clinical and regulatory decisions. Sensitivity analysis serves as a crucial methodology for assessing the robustness of research findings against potential biases and unmeasured confounding factors. A recent systematic review of observational studies using routinely collected healthcare data revealed that over 40% conducted no sensitivity analyses whatsoever, and among those that did, 54.2% showed significant differences between primary and sensitivity analysis results, with an average effect size difference of 24% [98]. This underscores the critical importance of rigorously assessing robustness in CER. These analyses provide researchers with a systematic approach to evaluate how strongly their conclusions depend on specific methodological choices, data handling techniques, or statistical assumptions.
Within the Model-Informed Drug Development (MIDD) framework, a "fit-for-purpose" approach ensures that analytical tools are closely aligned with key questions of interest and context of use [99]. This philosophy extends directly to sensitivity and scenario analyses, where the selection of appropriate methods must be driven by the specific research questions, data limitations, and potential sources of bias in a given CER study. Properly conducted sensitivity analyses not only test the stability of results but also provide quantitative estimates of how potential biases might affect the observed treatment effects, thereby strengthening the evidentiary value of CER findings for decision-makers [99] [98].
Fundamental Concepts and Definitions
Key Terminology
- Sensitivity Analysis: A comprehensive assessment procedure that investigates the robustness of research findings by evaluating how results vary with different methodological choices, statistical models, or assumptions [98]. These analyses help determine whether the primary study conclusions change substantially when alternative approaches are employed.
- Scenario Analysis: A specific form of sensitivity analysis that examines how results perform under different plausible scenarios, such as varying definitions of exposure, outcomes, or population characteristics. This approach is particularly valuable for assessing the impact of clinical uncertainties on CER findings.
- Primary Analysis: The principal statistical analysis specified in the study protocol or the first reported multivariable analysis that forms the basis for the main study conclusions [98].
- Effect Estimate: A quantitative measure of the relationship between treatment and outcome, such as hazard ratios, risk ratios, odds ratios, or mean differences [98].
- Robustness: The degree to which a study's conclusions remain consistent and unchanged when subjected to variations in analytical approaches, definitions, or assumptions [98].
Classification of Sensitivity Analyses
Sensitivity analyses in drug CER can be systematically categorized into three primary dimensions, each addressing different potential sources of bias:
Table 1: Categories of Sensitivity Analyses in Comparative Effectiveness Research
| Category | Description | Common Applications in CER |
|---|---|---|
| Alternative Study Definitions | Using different coding algorithms or classifications to identify exposures, outcomes, or confounders [98] | - Varying outcome definitions- Alternative exposure windows- Different confounder specifications |
| Alternative Study Designs | Modifying the fundamental study design parameters or population selection criteria [98] | - Changing inclusion/exclusion criteria- Using different data sources- Modifying study period |
| Alternative Modeling Approaches | Applying different statistical methods or handling techniques for data limitations [98] | - Different statistical models- Alternative approaches to missing data- Methods for unmeasured confounding |
Methodological Framework for Sensitivity Analyses
Systematic Approach to Implementation
Implementing a comprehensive sensitivity analysis framework requires careful planning and execution across multiple stages of the research process. The following workflow outlines the key components of a robust sensitivity assessment strategy:
Experimental Protocols for Key Sensitivity Analyses
Protocol for Alternative Outcome Definitions
Purpose: To assess whether findings are sensitive to variations in how the outcome is defined or identified, which is particularly relevant when using routinely collected data where outcome misclassification is common [98].
Methodology:
- Primary Definition: Implement the pre-specified outcome algorithm as defined in the study protocol
- Alternative Definitions: Create at least two alternative outcome definitions:
- A more specific definition (higher positive predictive value)
- A more sensitive definition (higher completeness)
- Comparison: Calculate effect estimates for each definition and compare direction, magnitude, and statistical significance
- Quantitative Assessment: Compute the ratio of effect estimates between sensitivity and primary analyses using the formula: Ratio = Point Estimate~Sensitivity~ / Point Estimate~Primary~ [98]
Interpretation: Findings are considered robust if effect estimates remain consistent in direction and magnitude across alternative definitions, with overlapping confidence intervals.
Protocol for Unmeasured Confounding
Purpose: To quantify how strong an unmeasured confounder would need to be to explain away the observed treatment effect [98].
Methodology:
- E-value Calculation: Compute the E-value, which represents the minimum strength of association that an unmeasured confounder would need to have with both the treatment and outcome to explain away the observed effect [98]
- Scenario-based Assessment: Specify plausible values for unmeasured confounder prevalence and strength based on clinical knowledge or literature
- Quantitative Bias Analysis: Apply bias adjustment formulas to estimate what the effect would be after accounting for specified unmeasured confounding
- Threshold Analysis: Determine the confounder strength that would change the clinical interpretation of results
Interpretation: Larger E-values indicate greater robustness to potential unmeasured confounding. Results should be interpreted in context of plausible confounders known in the clinical domain.
Data Presentation and Quantitative Assessment
Comparative Analysis of Effect Estimates
Systematic documentation and comparison of effect estimates from primary and sensitivity analyses are essential for interpreting robustness. The following table structure provides a standardized approach for presenting these comparisons:
Table 2: Template for Comparing Primary and Sensitivity Analysis Results
| Analysis Type | Effect Estimate (95% CI) | Ratio vs. Primary | P-value | Clinical Interpretation | Robustness Assessment |
|---|---|---|---|---|---|
| Primary Analysis | 0.72 (0.58-0.89) | 1.00 | 0.002 | Significant benefit | Reference |
| Sensitivity 1: Alternative Outcome | 0.75 (0.60-0.94) | 1.04 | 0.01 | Significant benefit | High |
| Sensitivity 2: Alternative Model | 0.69 (0.54-0.88) | 0.96 | 0.003 | Significant benefit | High |
| Sensitivity 3: UCC Adjustment | 0.81 (0.64-1.02) | 1.13 | 0.07 | Non-significant benefit | Moderate |
Empirical Evidence on Sensitivity Analysis Performance
Recent methodological research provides important insights into the performance and interpretation of sensitivity analyses in observational CER:
Table 3: Empirical Findings from Sensitivity Analysis Assessment [98]
| Characteristic | Finding | Implications for CER Practice |
|---|---|---|
| Prevalence of Use | 59.4% of studies conducted sensitivity analyses | Over 40% of studies lack basic robustness assessment |
| Number of Analyses | Median of 3 per study (IQR: 2-6) | Multiple approaches are needed for comprehensive assessment |
| Result Consistency | 54.2% showed significant differences from primary analysis | Discordance is common and must be addressed |
| Effect Size Divergence | Average 24% difference (95% CI: 12%-35%) | Magnitude of variation can be substantial |
| Reporting Quality | 51.2% clearly reported sensitivity analysis results | Transparency in reporting needs improvement |
| Interpretation of Discordance | Only 9 of 71 studies discussed impact of inconsistencies | Critical gap in current interpretation practices |
Integration with Drug Development and Regulatory Context
Alignment with Model-Informed Drug Development
Sensitivity and scenario analyses play a crucial role within the Model-Informed Drug Development (MIDD) framework, particularly for strengthening the evidence base for regulatory and reimbursement decisions [99]. The "fit-for-purpose" approach emphasized in MIDD guidance ensures that sensitivity analyses are appropriately tailored to the specific questions of interest and context of use throughout the drug development lifecycle [99]. For CER specifically, this means:
- Early Development: Assessing robustness of preclinical predictions and pharmacokinetic/pharmacodynamic models
- Clinical Development: Evaluating sensitivity of trial results to various analytical approaches and patient populations
- Post-Market: Examining robustness of comparative effectiveness findings across different data sources and methodological approaches
Regulatory Considerations and Recent Developments
Global regulatory agencies are increasingly emphasizing the importance of comprehensive sensitivity analyses in drug development and evaluation:
- The European Medicines Agency has incorporated sensitivity analysis requirements in various therapeutic area guidelines and reflects the growing recognition of their importance in regulatory decision-making [67]
- Health Canada has recently adopted the ICH E9(R1) addendum on estimands and sensitivity analysis, highlighting the importance of predefined approaches to handling intercurrent events in clinical trials [67]
- The U.S. FDA has advocated for model-informed drug development approaches that inherently include sensitivity and scenario analyses to support more robust decision-making [99]
Essential Methodological Toolkit
Research Reagent Solutions for Sensitivity Analysis
Table 4: Essential Methodological Tools for Sensitivity Analysis in CER
| Tool Category | Specific Methods | Primary Application | Implementation Considerations |
|---|---|---|---|
| Unmeasured Confounding | E-value analysis [98], Quantitative bias analysis, Propensity score calibration | Assessing impact of potential unmeasured confounders | Requires specification of plausible confounder parameters |
| Model Specification | Alternative covariate selection, Different functional forms, Machine learning approaches | Evaluating modeling assumptions | Balance between flexibility and interpretability |
| Missing Data | Multiple imputation, Complete case analysis, Inverse probability weighting | Handling missing covariate or outcome data | Assumptions about missingness mechanism |
| Classification Uncertainty | Alternative outcome definitions, Varying exposure windows, Different algorithm specifications | Addressing misclassification bias | Validation studies inform plausible parameters |
| Population Heterogeneity | Subgroup analyses, Interaction testing, Stratified models | Assessing effect modification | Pre-specification reduces selective reporting |
Implementation Workflow for Comprehensive Assessment
The following diagram illustrates the integrated workflow for implementing and interpreting a comprehensive sensitivity analysis plan within a drug CER study:
Interpretation and Reporting Standards
Guidelines for Interpreting Discordant Results
When sensitivity analyses produce results that differ meaningfully from primary findings, researchers should follow a structured interpretation framework:
- Quantify the Magnitude of Divergence: Calculate the ratio of effect estimates and differences in confidence intervals, similar to the approach used in recent methodological research that found an average 24% difference between primary and sensitivity analyses [98]
- Assess Clinical Significance: Determine whether observed differences would change clinical decision-making or recommendations
- Evaluate Plausibility: Consider the biological and clinical plausibility of assumptions underlying each analysis
- Contextualize with External Evidence: Integrate findings from other studies, prior knowledge, and mechanistic understanding
- Acknowledge Limitations Transparently: Clearly document how methodological choices and potential biases might affect conclusions
Reporting Recommendations for Transparency
Comprehensive reporting of sensitivity analyses is essential for research reproducibility and credibility. Based on empirical assessment of current practices [98], the following elements should be included:
- Clear specification of all sensitivity analyses in study protocols
- Complete reporting of effect estimates and confidence intervals for all analyses
- Quantitative comparison of results between primary and sensitivity analyses
- Explicit discussion of any clinically meaningful differences in findings
- Assessment of how potential biases might affect the study conclusions
- Transparent acknowledgment of limitations and uncertainties
Recent evidence indicates that only about half of studies currently report sensitivity analysis results clearly, and fewer than 15% adequately discuss inconsistencies between primary and sensitivity analyses [98]. Adhering to comprehensive reporting standards will significantly enhance the interpretability and credibility of drug CER findings.
Aligning CER Outcomes with Regulatory and HTA Requirements
In contemporary drug development, the success of a product hinges not only on achieving regulatory approval but also on demonstrating value to secure market access. Comparative Effectiveness Research (CER) serves as the critical bridge between these two milestones, providing evidence on how a new drug compares to existing alternatives in real-world settings. Formulating a CER strategy that is prospectively aligned with the requirements of both regulatory bodies, such as the European Medicines Agency (EMA), and Health Technology Assessment (HTA) organizations is no longer an ancillary activity but a core component of clinical development. A CER study that fails to meet the distinct, and sometimes divergent, needs of these decision-makers can jeopardize a product's commercial success, even after securing regulatory marketing authorization. This guide provides a structured approach for researchers and drug development professionals to design CER studies that generate evidence capable of satisfying this dual mandate, thereby informing both regulatory and reimbursement decisions.
The Evolving Regulatory and HTA Landscape
The New EU HTA Framework for Medicinal Products
A significant shift in the European evidence-generation landscape commenced on 12 January 2025, with the implementation of Joint Clinical Assessments (JCAs) for specific categories of medicinal products under Regulation (EU) 2021/2282 [100]. The JCA process is designed to support national HTA processes by providing a standardized, scientific analysis of the relative effects of a health technology on patient health outcomes [100]. This framework establishes a unified procedure for clinical assessment across member states, fundamentally altering the market access pathway for new drugs.
- Scope and Timelines: From January 2025, new medicines for oncology and advanced therapy medicinal products (ATMPs) fall within the mandatory scope of JCAs [100]. The formal JCA process is initiated upon the appointment of an assessor and co-assessor, which occurs after a developer simultaneously submits a summary of product characteristics and a clinical overview to the HTA secretariat alongside its marketing authorisation application to the EMA [100]. The entire JCA process is extensive, spanning approximately 345 days from certification to the final report [101].
- Procedural Requirements: The process is governed by strict timelines and procedural rules. Health technology developers must communicate with the HTA secretariat via a secure IT platform, requesting product-specific access well in advance of submissions [100]. A key implementing act, Commission Implementing Regulation (EU) 2025/2086, lays down detailed procedural rules for the interaction, exchange of information, and participation in the preparation of JCAs [101].
Foundational Principles of Regulatory CER
Underpinning any advanced strategy are the core principles of CER, which emphasize relevance to stakeholder decision-making. As defined by the Agency for Healthcare Research and Quality (AHRQ), the foundation of a CER protocol is a meticulously formulated set of study objectives and research questions [69]. The development of these questions should be a collaborative process involving researchers and stakeholders to ensure the resulting evidence is applicable and can be translated into healthcare practice. The PICOTS framework (Population, Intervention, Comparator, Outcomes, Timeframe, Setting) is a critical tool for conceptualizing the research problem and ensuring all key parameters relevant to decision-makers are considered [69]. Furthermore, the Patient-Centered Outcomes Research Institute (PCORI) has developed a comprehensive set of Methodology Standards to guide the conduct of valid, trustworthy patient-centered CER, which are regularly updated to reflect methodological advances [71].
Table 1: Key Regulatory and HTA Terminology
| Term | Definition | Relevance to CER |
|---|---|---|
| Joint Clinical Assessment (JCA) | A mandatory EU-level clinical effectiveness assessment for in-scope products to inform national HTA/reimbursement decisions [100]. | Defines the specific evidence requirements, including PICO structure and comparative data, for EU market access. |
| Joint Scientific Consultation (JSC) | A voluntary process where developers can obtain advice from HTA bodies on clinical development plans and evidence needs [102]. | Critical opportunity to align CER study design (endpoints, comparators) with HTA expectations pre-trial. |
| Real-World Evidence (RWE) | Clinical evidence derived from analysis of real-world data (e.g., EHRs, registries) [103]. | Used to complement trial data, fill evidence gaps, and support generalizability in CER and JCAs. |
| PICOTS Framework | A structured tool for formulating research questions (Population, Intervention, Comparator, Outcomes, Time, Setting) [69]. | Ensures CER study design comprehensively addresses the needs of regulatory and HTA decision-makers. |
| Transportability | The methodological process of assessing whether RWE from one country/population can predict outcomes in another [103]. | Key for using non-local data in HTA submissions when local data is unavailable. |
Methodological Frameworks for Aligned CER
A Stepwise Protocol Development Process
Designing a CER study that meets the dual demands of regulators and HTA bodies requires a disciplined, sequential approach. The following workflow outlines the critical stages from conceptualization to final protocol development.
The process begins by identifying the specific decisions that regulators and HTA bodies face, the context in which they are made, and the key areas of uncertainty [69]. This foundational step ensures the research is purpose-built from the outset. Subsequently, a comprehensive synthesis of the current knowledge base is essential. This involves a systematic literature review to identify established guidelines, summarize what is known about efficacy, effectiveness, and safety, and, crucially, to pinpoint where evidence is absent, insufficient, or conflicting [69].
With a firm understanding of the decision context and evidence gaps, researchers can then conceptualize the research problem. This stage involves engaging with multiple stakeholders to describe the potential relationships between the intervention and health outcomes, developing preliminary hypotheses, and enumerating major assumptions [69]. The output of this conceptual work is the formulation of precise research questions that are then translated into formal study objectives and the PICOTS framework, which operationalizes the key study parameters [69]. Finally, a methodological approach is selected—whether observational, pragmatic trial, or other—that is robust enough to meet the evidence standards of both regulators and HTA bodies [71].
Incorporating Real-World Evidence and Transportability
The use of Real-World Evidence (RWE) in CER is increasingly vital for demonstrating a treatment's effectiveness in routine clinical practice. For HTA submissions, the transportability of RWE—the ability to generalize findings from one country or population to another—is a key methodological challenge [103]. Initial empirical studies in oncology, such as those in advanced non-small cell lung cancer, have demonstrated that with proper adjustment for population and treatment differences, US RWE could predict outcomes in Canada and the UK with reasonable accuracy [103]. This underscores the potential of non-local RWE to reduce decision uncertainty when local data are unavailable. Research consortia like the Flatiron FORUM are actively expanding this work to other cancer types to develop a framework for the use of global RWE in oncology HTA decision-making [103].
The Scientist's Toolkit: Essential Reagents for CER
Executing a high-quality CER study requires a suite of methodological "reagents"—standardized components and approaches that ensure rigor, reproducibility, and relevance.
Table 2: Key Research Reagent Solutions for CER
| Item | Function in CER | Application Example |
|---|---|---|
| Systematic Literature Review | A methodologically rigorous review to identify, appraise, and synthesize all relevant studies on a specific research question [104]. | Foundation for defining the state-of-the-art, identifying gaps, and justifying the choice of comparator. |
| PICOTS Framework | A structured template for defining the core elements of a research question (Population, Intervention, Comparator, Outcomes, Time, Setting) [69]. | Ensures the CER protocol explicitly addresses all elements critical to regulatory and HTA decision-makers. |
| Directed Acyclic Graphs (DAGs) | Causal diagrams used to map assumptions about the relationships between variables, informing variable selection for confounding control [69]. | Critical for planning the statistical analysis of observational CER to minimize bias and support causal inference. |
| HTA JCA Dossier Template | The prescribed template (Annex I of Implementing Regulation) for submitting evidence for Joint Clinical Assessment in the EU [101]. | Provides the exact structure and required content for presenting CER evidence to EU HTA bodies. |
| Real-World Data (RWD) Sources | Curated databases of electronic health records, claims data, or disease registries that reflect routine clinical care [103]. | Source for generating RWE on long-term outcomes, comparative effectiveness, and treatment patterns. |
Operationalizing Alignment: From Strategy to Submission
Prospectively Designing Studies for JCA
Achieving alignment is not a retrospective activity but must be embedded in the clinical development plan from its inception. The European HTA regulation provides a powerful mechanism for this: the Joint Scientific Consultation (JSC). Through a JSC, developers of medicinal products can receive parallel advice from HTA bodies and regulators on their clinical development strategy, including trial design, endpoints, and comparators [102]. The first formal request periods for JSCs for medicines began in 2025 [102]. Engaging in this process allows a company to fine-tune its CER strategy and evidentiary requirements before costly trials are finalized, thereby de-risking the subsequent JCA submission.
The evidence package for a JCA must extend beyond what was sufficient for regulatory approval. It requires a comprehensive clinical evaluation that includes all studies—published and unpublished—and must be structured according to the PICO framework [101]. The assessment focuses squarely on comparative effectiveness versus the relevant standard of care, not just standalone safety and performance [101]. Furthermore, the HTA secretariat mandates that all product-specific communication and document uploads for a JCA occur through a secure HTA IT platform, for which developers must request personalized, product-specific access [100].
Quantitative Data Requirements and Timelines
The following table summarizes the critical quantitative data and deadlines that must be managed for a successful CER and HTA submission under the new EU framework.
Table 3: Critical Quantitative Data and Timelines for EU HTA Submissions
| Data Point / Milestone | Requirement / Timeline | Context & Importance |
|---|---|---|
| JCA Dossier Submission | 100 days (with a possible 30-day extension) [101]. | The period after device certification to complete the submission of the comprehensive evidence dossier to the HTA secretariat. |
| Total JCA Process Duration | ~345 days [101]. | The total estimated timeframe from device certification to the publication of the final JCA report. |
| Certification Document Submission | 7 days after device approval [101]. | The short window to submit key certification documents to the HTA bodies, triggering the JCA process. |
| Response to Information Requests | 7-30 days during assessment [101]. | The limited time available to respond to queries or requests for additional information from the assessing HTA bodies. |
| JSC Request Period (2025 Example) | 2 June - 30 June 2025 [102]. | The defined annual window during which manufacturers can submit requests for a Joint Scientific Consultation. |
In an era of increasingly constrained healthcare budgets and heightened scrutiny of a treatment's real-world value, aligning CER outcomes with both regulatory and HTA requirements is a non-negotiable element of successful drug development. This alignment is not serendipitous but must be strategically engineered by prospectively identifying the evidentiary needs of all decision-makers, leveraging new mechanisms like Joint Scientific Consultations, and rigorously applying methodological standards to study design—particularly for the incorporation of Real-World Evidence. By adopting the integrated frameworks and tools outlined in this guide, researchers and drug development professionals can formulate key CER questions that not only demonstrate a product's safety and efficacy but also convincingly establish its comparative value, thereby paving the way for regulatory approval, favorable HTA outcomes, and ultimately, patient access.
Communicating CER Value to Regulators, Payers, and Clinicians
Comparative Effectiveness Research (CER) is an increasingly critical component of the health care landscape, with the potential to improve decisions about appropriate treatments for patients by comparing drugs against other active treatments rather than just placebo [31]. For pharmaceutical researchers and drug development professionals, effectively communicating the value derived from CER to key stakeholders—regulators, payers, and clinicians—has become essential for successful product development and market access. This technical guide provides a comprehensive framework for formulating key CER questions and communicating resulting evidence within a rapidly evolving ecosystem where real-world evidence (RWE) and economic value are intensively scrutinized.
The growing expectations for CER coincide with significant regulatory and policy shifts. The U.S. Food and Drug Administration (FDA) has demonstrated an increased commitment to using real-world data (RWD) and RWE in regulatory decision-making, with numerous recent examples spanning product approvals, labeling changes, and postmarket safety assessments [105]. Simultaneously, payers are sharpening their focus on long-term outcomes, real-world impact, and economic value, with over 80% now considering RWE essential in their decision-making processes [106]. This evolving landscape presents both challenges and opportunities for pharmaceutical companies to differentiate their products through robust CER strategies and effective evidence communication.
CER in Regulatory Decision-Making
FDA's Evolving Framework for Real-World Evidence
The FDA has developed a structured approach for incorporating RWE into regulatory decisions, with the Center for Drug Evaluation and Research (CDER) and the Center for Biologics Evaluation and Research (CBER) applying RWE in various regulatory contexts since 2011 [105]. The agency utilizes RWE across multiple aspects of regulatory decision-making, including supporting new drug approvals, informing labeling changes, and contributing to postmarket safety evaluations. This regulatory acceptance has created significant opportunities for sponsors to leverage CER in their development programs.
Recent FDA decisions illustrate the agency's acceptance of RWE in various roles, from serving as confirmatory evidence to functioning as pivotal evidence in approval decisions. The regulatory body has employed diverse data sources, including medical records, disease registries, claims data, and national death records, to inform these decisions. The study designs accepted range from retrospective cohort studies to randomized controlled trials that incorporate RWD elements, demonstrating flexibility in methodological approaches while maintaining rigorous standards for evidence generation.
Key Regulatory Case Studies
Table 1: Recent FDA Regulatory Decisions Incorporating RWE
| Drug/Product | Approval Date | Data Source | Study Design | Role of RWE |
|---|---|---|---|---|
| Aurlumyn (Iloprost) | Feb 2024 | Medical records | Retrospective cohort study | Confirmatory evidence |
| Vimpat (Lacosamide) | Apr 2023 | PEDSnet medical records | Retrospective cohort study | Safety evidence |
| Actemra (Tocilizumab) | Dec 2022 | National death records | Randomized controlled trial | Primary efficacy endpoint |
| Vijoice (Alpelisib) | Apr 2022 | Medical records | Non-interventional single-arm study | Substantial evidence of effectiveness |
| Orencia (Abatacept) | Dec 2021 | CIBMTR registry | Non-interventional study | Pivotal evidence |
| Voxzogo (Vosoritide) | Nov 2021 | Natural history registry | Externally controlled trial | Confirmatory evidence |
Table 2: RWE in Postmarket Safety and Labeling Decisions
| Drug/Product | Action Date | Data Source | Regulatory Action |
|---|---|---|---|
| Prolia (Denosumab) | Jan 2024 | Medicare claims data | Boxed Warning for severe hypocalcemia |
| Beta Blockers | Jul 2025 | Sentinel System | Safety labeling changes for hypoglycemia risk |
| Oral Anticoagulants | Jan 2021 | Sentinel System | Class-wide label change for uterine bleeding risk |
| Oral Methotrexate | Dec 2021 | Sentinel System | Labeling change to address dosing errors |
Experimental Protocols for Regulatory-Grade CER
For regulatory submissions, CER studies must meet specific methodological standards. The following protocols outline approaches for generating regulatory-grade evidence:
Protocol 1: Retrospective Cohort Study Using Electronic Health Records
- Data Source Selection: Identify fit-for-purpose data sources with sufficient granularity for confounding control (e.g., PEDSnet, Sentinel System) [105]
- Cohort Definition: Apply explicit inclusion/exclusion criteria to create matched treatment cohorts
- Outcome Validation: Implement chart verification for critical endpoints where feasible
- Confounding Control: Utilize propensity score matching, inverse probability weighting, or high-dimensional propensity scores
- Sensitivity Analyses: Plan multiple analyses to test robustness of findings to methodological assumptions
Protocol 2: Externally Controlled Trials
- Control Source: Identify appropriate external controls from natural history studies or historical clinical trials [105]
- Covariate Adjustment: Pre-specified statistical plan to adjust for prognostic differences between treatment and control groups
- Endpoint Ascertainment: Ensure consistent endpoint definition and ascertainment methods between groups
- Bias Assessment: Evaluate potential sources of bias through quantitative bias analysis
Communicating CER Value to Payers
Evolving Payer Expectations and Value Frameworks
Payers have transitioned from acting primarily as cost gatekeepers to functioning as sophisticated value evaluators who consider a holistic range of evidence in coverage and reimbursement decisions [106]. This evolution has significant implications for how pharmaceutical companies should communicate CER value. Contemporary payers prioritize real-world evidence to validate whether benefits observed in controlled trials translate to routine clinical practice, scrutinize budget impact and economic justification—particularly for high-cost therapies—and increasingly align with established value frameworks such as those developed by the Institute for Clinical and Economic Review (ICER) and the National Comprehensive Cancer Network (NCCN) [106].
To meet these elevated expectations, market access teams must initiate evidence generation and strategic planning earlier in the development process. Forward-looking organizations are integrating health economics and outcomes research (HEOR), RWE, and pricing insights during Phase 2 trials to shape studies that address future payer questions [106]. This proactive approach requires cross-functional collaboration, with commercial, medical, regulatory, and development teams aligning to build an integrated value story that extends beyond clinical efficacy to encompass real-world performance, patient quality of life, and financial sustainability.
Methodologies for Payer-Focused CER
Protocol 3: Real-World Treatment Pattern and Outcome Studies
- Data Source: Leverage longitudinal claims data supplemented with electronic health records where available
- Comparator Identification: Identify appropriate active comparators reflecting current standard of care
- Outcome Measures: Include clinical outcomes, healthcare resource utilization, and patient-reported outcomes
- Subgroup Analyses: Pre-specify subgroups of payer interest (e.g., line of therapy, comorbidities)
- Economic Endpoints: Capture cost offsets and productivity impacts where feasible
Protocol 4: Budget Impact and Cost-Effectiveness Analysis
- Model Framework: Develop transparent models aligned with ISPOR, NICE, or other relevant guidelines
- Input Sourcing: Derivate clinical inputs from CER studies and network meta-analyses
- Population Definition: Define target populations consistent with anticipated label and clinical practice
- Scenario Analyses: Test model under varying assumptions regarding market share, pricing, and adherence
- Validation: Conduct internal and external validation of models
Engaging Clinicians with CER Evidence
Effective Communication Frameworks for Clinical Adoption
Clinicians require CER evidence that is directly applicable to individual patient decision-making, presented in formats that integrate seamlessly into clinical workflow. Effective communication to this audience must address the limitations of applying average results from population-level studies to individual patients with unique characteristics and circumstances [31]. Successful clinical communication strategies often incorporate point-of-care tools that provide accessible CER summaries, shared decision-making aids that facilitate patient-clinician conversations about treatment alternatives, and clinical pathways that embed CER findings into routine practice guidelines.
The October 2025 implementation of new rules requiring real-time prescription benefit information in electronic health records presents both challenges and opportunities for communicating CER to clinicians [107]. These systems will enable providers to access coverage information and cost alternatives at the point of prescribing, creating natural opportunities to discuss comparative effectiveness in the context of individual patient needs and constraints. Pharmaceutical companies should prepare for this shift by developing concise, actionable CER summaries compatible with these emerging digital platforms.
Implementation Protocols for Clinical CER
Protocol 5: CER Integration into Clinical Decision Support
- Evidence Distillation: Create guideline-compliant summaries of CER findings
- Stakeholder Engagement: Collaborate with key opinion leaders and medical societies
- Tool Development: Design decision aids that present benefits and risks of alternatives
- Implementation Strategy: Plan for integration into clinical workflow with minimal disruption
- Outcome Tracking: Monitor adoption and impact on treatment patterns
Protocol 6: Cluster-Randomized Implementation Trial
- Site Selection: Identify diverse practice settings to test generalizability
- Randomization: Randomize at clinic or provider level to minimize contamination
- Intervention Design: Develop multi-faceted implementation strategy (education, decision support, audit/feedback)
- Outcome Assessment: Measure both implementation outcomes (adoption, fidelity) and patient outcomes
- Qualitative Component: Include mixed methods to understand barriers and facilitators
Integrated Strategic Framework
Aligning CER Questions with Stakeholder Priorities
Formulating optimal CER questions requires understanding the distinct evidentiary needs of each stakeholder group and identifying areas of overlap where single studies can efficiently address multiple needs. The most successful CER strategies develop research questions that simultaneously advance regulatory, payer, and clinical understanding of a product's value proposition while complying with relevant regulatory restrictions on industry communication [31]. This alignment necessitates early and continuous stakeholder engagement throughout the evidence generation process.
Strategic CER question development should consider the entire product lifecycle, from early development through postmarket surveillance. Early-phase CER can inform go/no-go development decisions and trial design choices, while late-phase CER can support regulatory submissions and initial market access. Post-approval CER addresses evidence gaps identified during regulatory review, supports label expansions, and responds to evolving competitor landscapes. Throughout this continuum, maintaining a consistent value narrative while adapting evidence generation to changing market conditions is essential for maximizing impact.
Visualizing the Integrated CER Strategy
The following diagram illustrates the integrated framework for developing and communicating CER value across stakeholder groups:
Integrated CER Development and Communication Framework
Essential Research Reagent Solutions for CER
Table 3: Key Research Reagent Solutions for CER
| Research Tool Category | Specific Examples | Function in CER |
|---|---|---|
| Real-World Data Platforms | Sentinel System, PEDSnet, EHR systems | Provide longitudinal patient data for observational CER studies |
| Data Standardization Tools | FHIR standards, OMOP Common Data Model | Enable interoperability and pooling of data from multiple sources |
| Statistical Analysis Packages | High-dimensional propensity score algorithms, marginal structural models | Address confounding in non-randomized studies |
| Economic Modeling Platforms | Cost-effectiveness analysis software, budget impact models | Quantify economic value of interventions compared to alternatives |
| Evidence Synthesis Tools | Network meta-analysis software, systematic review platforms | Enable indirect comparisons when head-to-head data are limited |
| Patient-Reported Outcome Measures | PROMIS, EQ-5D, disease-specific instruments | Capture patient-centered outcomes in comparative studies |
Effectively communicating CER value to regulators, payers, and clinicians requires a strategic, integrated approach that begins with well-formulated research questions and continues through tailored evidence dissemination. Success in this evolving landscape depends on understanding each stakeholder's unique evidentiary requirements, leveraging appropriate real-world data sources and methodological approaches, and communicating findings through targeted channels and formats. As regulatory acceptance of RWE grows and payer expectations for real-world and economic evidence intensify, pharmaceutical companies that excel at generating and communicating robust CER will gain significant competitive advantages in product development and market access.
The future of CER communication will likely involve greater integration of artificial intelligence tools for evidence generation, increased standardization of real-world data methodologies, and more sophisticated digital platforms for evidence dissemination. By establishing strong CER foundations now—including cross-functional collaboration, early stakeholder engagement, and strategic evidence planning—drug development professionals can position their organizations to thrive in this evolving evidence landscape and ultimately deliver greater value to patients and health systems.
Conclusion
Formulating precise and strategic questions is the cornerstone of impactful Drug Comparative Effectiveness Research. A methodical approach—from establishing a solid regulatory foundation and applying rigorous methodologies to proactively troubleshooting issues and rigorously validating outcomes—ensures that CER generates reliable, decision-grade evidence. As the landscape evolves with advanced therapies and digital health technologies, the integration of robust qualitative data and real-world evidence will become increasingly critical. By adopting this comprehensive framework, researchers can enhance the relevance and utility of their studies, ultimately accelerating the delivery of effective treatments to patients and informing sound healthcare decisions.
References
- 1. PCORI Methodology Standards [https://www.pcori.org/research-related-projects/about-our-research/research-methodology/pcori-methodology-standards]
- 2. Study Objectives and Questions - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK126193/]
- 3. The biggest challenges clinical trials will face in 2025 [https://pharma.nridigital.com/pharma_feb25/clinical-trials-challenges-expect-2025]
- 4. Challenges and Lessons Learned in Conducting Comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3935288/]
- 5. Visualizations throughout pharmacoepidemiology study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9826437/]
- 6. Comprehensive Guide to Clinical Trial Protocol Design & ... [https://www.clinicalleader.com/topic/clinical-trial-protocol-design-development]
- 7. Clinical Trial Data Visualization: The New FDA Guideline ... [https://beaconcure.com/resources/clinical-trial-data-visualization/]
- 8. Exploring the challenges faced by generic version of complex ... [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-025-02931-y]
- 9. FDA's New “Plausible Mechanism Pathway†and Other ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/11/fda-plausible-mechanism-pathway-and-other-initiatives-drugs-for-ultra-rare-conditions]
- 10. FDA Outlines “Plausible Mechanism†Approval Pathway for ... [https://www.ropesgray.com/en/insights/alerts/2025/11/fda-outlines-plausible-mechanism-approval-pathway-for-personalized-therapies-but-significant]
- 11. Accelerated Approval Program [https://www.fda.gov/drugs/nda-and-bla-approvals/accelerated-approval-program]
- 12. Innovative Designs for Clinical Trials of Cellular and Gene ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/innovative-designs-clinical-trials-cellular-and-gene-therapy-products-small-populations]
- 13. Newly Added Guidance Documents [https://www.fda.gov/drugs/guidances-drugs/newly-added-guidance-documents]
- 14. Recently Issued Guidance Documents [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/recently-issued-guidance-documents]
- 15. REGULATORY UPDATE: FDA Releases 2025 Guidance ... [https://www.aabb.org/news-resources/news/article/2025/01/03/regulatory-update--fda-releases-2025-guidance-agenda]
- 16. Concepts and Challenges in Quantitative Pharmacology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2628212/]
- 17. Comparative Effectiveness Training (CERTaIN) [https://www.mdanderson.org/education-training/outreach-programs/comparative-effectiveness-research-training.html]
- 18. Comparison of Quantitative and Qualitative (Q)SAR Models ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2018.01136/full]
- 19. Applying quantitative and systems pharmacology to drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11483046/]
- 20. Phased Large Awards for Comparative Effectiveness ... [https://www.pcori.org/funding-opportunities/announcement/phased-large-awards-comparative-effectiveness-research-pcori-funding-announcement-cycle-2-2025]
- 21. Phased Large Awards for Comparative Effectiveness ... [https://www.pcori.org/funding-opportunities/announcement/phased-large-awards-comparative-effectiveness-research-pcori-funding-announcement-cycle-3-2025]
- 22. Evaluation of Pre-marketing Factors to Predict Post ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8422863/]
- 23. Guide to Clinical Evaluation Reports (CER) for Medical ... [https://namsa.com/resources/blog/guide-clinical-evaluation-reports-medical-devices/]
- 24. Guide to Clinical Evaluation Reports for Medical Devices [https://www.emergobyul.com/resources/what-clinical-evaluation-report]
- 25. Research - Cycle 3 2025 [https://www.pcori.org/funding-opportunities/announcement/improving-methods-conducting-patient-centered-comparative-clinical-effectiveness-research-pcori-funding-announcement-cycle-3-2025]
- 26. Stakeholder participation in comparative effectiveness research [https://pmc.ncbi.nlm.nih.gov/articles/PMC3371639/]
- 27. What Is CER and Why Does It Matter? [https://www.pcori.org/blog/2025/what-cer-and-why-does-it-matter]
- 28. Informational Needs of Patients with Cancer: A Qualitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6897024/]
- 29. Information-seeking preferences in diverse patients ... [https://www.sciencedirect.com/science/article/pii/S1098360023009127]
- 30. Comparative Effectiveness Research (CER): Informing ... [https://medipharmsolutions.com/blog/comparative-effectiveness-research-cer-informing-treatment-choices/]
- 31. Looking at CER from the Pharmaceutical Industry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10437711/]
- 32. Stakeholder analysis [https://www.pmi.org/learning/library/stakeholder-analysis-pivotal-practice-projects-8905]
- 33. Information needs for cancer screening and associated factors ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-21096-2]
- 34. PCORI awards new patient-centered CER to support ... [https://www.pcori.org/news-release/2025/pcori-awards-new-patient-centered-cer-support-informed-health-care-decisions]
- 35. PCORI: Homepage [https://www.pcori.org/]
- 36. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 37. Color Contrast Accessibility: Complete WCAG 2025 Guide ... [https://www.allaccessible.org/blog/color-contrast-accessibility-wcag-guide-2025]
- 38. Contrast Checker [https://webaim.org/resources/contrastchecker/]
- 39. Five Predictions That Will Drive R&D Effectiveness in 2025 [https://www.appliedclinicaltrialsonline.com/view/five-predictions-rd-effectiveness-2025]
- 40. Clinical Evaluation Report (CER): Key to EU Market Approval [https://bioexcelife.com/clinical-evaluation-report-cer-a-critical-component-for-eu-market-access/]
- 41. Seeking Early Answers to Formulation Questions [https://www.biopharminternational.com/view/seeking-early-answers-formulation-questions]
- 42. Back to the basics: guidance for formulating good research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11129835/]
- 43. Formulating research questions for evidence-based studies [https://www.sciencedirect.com/science/article/pii/S2949916X23000464]
- 44. A comprehensive framework for data quality assessment in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3845781/]
- 45. Choosing Endpoints for Medical Device Trials: A Step-by-Step Guide [https://www.bioaccessla.com/blog/choosing-endpoints-for-medical-device-trials-a-step-by-step-guide]
- 46. Tightening rules, global trials: Sponsors’ concerns at ESMO [https://www.parexel.com/insights/blog/tightening-rules-global-trials-sponsors-concerns-at-esmo-2025]
- 47. Shaping a research agenda to ensure a successful European health... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9636785/]
- 48. A Guide to Clinical Trial Endpoints [https://www.tldrpharmacy.com/content/a-guide-to-clinical-trial-endpoints]
- 49. What Is a Clinical Trial Endpoint , and Why Is Endpoint ... Selection [https://meritcro.com/what-is-a-clinical-trial-endpoint-and-why-is-endpoint-selection-crucial/]
- 50. The importance of appropriate selection of clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10107578/]
- 51. Enabling Evidence-Based Study Endpoint Selection [https://www.appliedclinicaltrialsonline.com/view/enabling-evidence-based-study-endpoint-selection]
- 52. Quality in qualitative evidence: new best practice principles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12224144/]
- 53. A New Era in Pharmacovigilance: Toward Realâ€World ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8058244/]
- 54. Finding the right tool for the specific task: navigating RWE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490408/]
- 55. Best RWE Companies for Patient Insights in 2025 [https://www.mamahealth.com/resources/best-rwe-companies-patient-insights]
- 56. Top 5 Trends in Real-World Data and ... [https://veranahealth.com/top-5-trends-in-real-world-data-and-real-world-evidence-for-2025/]
- 57. Coding the Real World [https://lumivero.com/resources/coding-the-real-world-understanding-real-world-evidence-in-healthcare-with-nvivo-qualitative-data-analysis-software/]
- 58. Navigating FDA Meetings: Drug Development & Approval ... [https://www.allucent.com/resources/blog/inroads-approval-navigating-formal-fda-meetings-optimize-your-drug-development-program]
- 59. Formal FDA meeting types [https://bgtcplaybook.document360.io/docs/formal-fda-meeting-types]
- 60. Formal Meetings Between the FDA and Sponsors or ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/formal-meetings-between-fda-and-sponsors-or-applicants-pdufa-products]
- 61. Communications From Firms to Health Care Providers ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/communications-firms-health-care-providers-regarding-scientific-information-unapproved-uses]
- 62. FDA Finalizes Guidance on Communication of Scientific ... [https://www.ropesgray.com/en/insights/alerts/2025/01/fda-finalizes-guidance-on-communication-of-scientific-information]
- 63. Frequently Asked Questions on Drug Development and ... [https://www.fda.gov/drugs/cder-small-business-industry-assistance-sbia/small-business-assistance-frequently-asked-questions-drug-development-and-investigational-new-drug]
- 64. The biggest challenges clinical trials will face in 2025 [https://www.clinicaltrialsarena.com/features/clinical-trials-challenges-expect-2025/]
- 65. Clinical trial regulations in 2025: navigating the constraints [https://clinicaltrialrisk.org/clinical-trial-design/clinical-trial-regulations-navigating-the-constraints/]
- 66. MDR 2025: Clinical Evaluation Requirements Explained [https://www.scimedconsult.com/blog/is-your-clinical-evaluation-mdr-ready]
- 67. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 68. Navigating the 2025 Landscape of Clinical Evaluation ... [https://www.prp-compliance.com/post/navigating-the-2025-landscape-of-clinical-evaluation-reports-under-new-mdcg-guidance]
- 69. Study Objectives and Questions - NCBI - NIH [https://www.ncbi.nlm.nih.gov/sites/books/NBK126193/]
- 70. Protocol Deviations Explained: Understanding the FDA's ... [https://www.wcgclinical.com/insights/protocol-deviations-explained-understanding-the-fdas-draft-guidance/]
- 71. Research Methodology [https://www.pcori.org/research-related-projects/about-our-research/research-methodology]
- 72. Quality Management During Manufacturing Changes [https://www.qualitydigest.com/inside/lean-article/quality-management-during-manufacturing-changes-111225.html]
- 73. Comparative Analysis: Mastering Techniques for Effective ... [https://www.storytellingwithcharts.com/blog/a-comparative-analysis-mastering-techniques-for-effective-data-comparison/]
- 74. 2025 Quality Management Trends in Life Sciences ... [https://www.mastercontrol.com/gxp-lifeline/quality-management-trends-reshaping-life-sciences-manufacturing/]
- 75. Comprehensive Review of Methods to Assess Uncertainty ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10163110/]
- 76. Exploring the Feasibility of Comprehensive Uncertainty ... [https://www.sciencedirect.com/science/article/pii/S1098301521001017]
- 77. Handling Uncertainty in the Results of Economic Evaluation [https://www.ohe.org/publications/handling-uncertainty-results-economic-evaluation/]
- 78. Handling Continuous Outcomes in Quantitative Synthesis - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK154408/]
- 79. A review of the quantitative effectiveness evidence synthesis ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-10162-8]
- 80. How to Ensure Data Integrity: Best Practices and Tools [https://www.acceldata.io/blog/how-to-ensure-data-integrity-strategies-tools-and-best-practices]
- 81. Data Integrity in Clinical Research [https://ccrps.org/clinical-research-blog/data-integrity-in-clinical-research]
- 82. Best Practices for Data Integrity in Pharmaceutical Industry ... [https://www.avslifesciences.com/blog-post/best-practices-for-data-integrity-in-pharmaceutical-industry-compliance]
- 83. Ensuring Data Integrity in Clinical Trials [https://www.freyrsolutions.com/blog/ensuring-data-integrity-in-clinical-trials-a-sponsors-guide-to-oversight]
- 84. Mastering the data collection process: essential steps, tools ... [https://www.dataguard.com/blog/data-collection-process-tools-and-software/]
- 85. Principles and Strategies for Monitoring Data Collection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3272671/]
- 86. Top Data Collection Strategies to Optimize Real-Time ... [https://www.sapien.io/blog/data-collection-strategies]
- 87. Dose-finding studies in drug development for rare genetic ... [https://ojrd.biomedcentral.com/articles/10.1186/s13023-022-02298-6]
- 88. How innovative trial designs de-risk drug development ... [https://rarerevolutionmagazine.com/rare-insider/how-innovative-trial-designs-de-risk-drug-development-in-rare-diseases/]
- 89. Preparing for 2025: Key Trends in FDA Guidance Agendas [https://www.mwe.com/insights/preparing-for-2025-key-trends-in-fda-guidance-agendas/]
- 90. Advancing the frontier of rare disease modeling: a critical ... [https://www.nature.com/articles/s41746-025-02068-1]
- 91. Ten Questions for 2025! [https://www.linkedin.com/pulse/ten-questions-every-small-emerging-biotech-drug-development-program-50orc]
- 92. : are your Analytical ... | QbD Group Method Validation analytical [https://www.qbdgroup.com/en/blog/analytical-method-validation-are-your-methods-suitable-for-intended-use/]
- 93. Trends In Pharmaceutical 2025 Development... Analytical Methods [https://agnopharma.com/blog/trends-in-pharmaceutical-analytical-methods-development-validation/]
- 94. Methods for Indirect Treatment Comparison: Results from a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11036291/]
- 95. A Review of the Importance and Relevance of Real-World ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12400973/]
- 96. How Similar is Similar Enough? Assessment of Indirect ... [https://www.sciencedirect.com/science/article/pii/S1098301525023629]
- 97. Select your drug formulation before starting clinical studies [https://www.certara.com/blog/select-drug-formulation-before-starting-clinical-studies/]
- 98. Evaluating the agreement between sensitivity and primary ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04199-4]
- 99. Advancing drug development with “Fit-for-Purpose†modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 100. Joint Clinical Assessments - Public Health [https://health.ec.europa.eu/health-technology-assessment/implementation-regulation-health-technology-assessment/joint-clinical-assessments_en]
- 101. New EU HTA Regulation for Medical Devices - Are You ... - Gsap [https://gsapglobal.com/new-eu-hta-regulation-for-medical-devices-are-you-prepared/]
- 102. EU HTA Regulation for Medical Devices Starts in 2025 [https://remapconsulting.com/hta/eu-hta-regulation-2025-medical-devices/]
- 103. Crossing borders: the need for empirical evidence of real- ... [https://pubmed.ncbi.nlm.nih.gov/40637151/]
- 104. Blog: EU MDR CER Requirements in 2025 [https://www.globalrwc.com/blogs/eu-mdr-cer-requirements-in-2025]
- 105. FDA use of Real-World Evidence in Regulatory Decision ... [https://www.fda.gov/science-research/real-world-evidence/fda-use-real-world-evidence-regulatory-decision-making]
- 106. Redefining value: how payer expectations are evolving in ... [https://www.inizioevoke.com/latest/article/redefining-value-how-payer-expectations-are-evolving-in-2025-and-what-pharma-must]
- 107. What the October 2025 Rule Means for Healthcare - MyCabinet [https://mycabinet.com/a-new-era-in-prescription-transparency-what-the-october-2025-rule-means-for-healthcare/]