Propensity Score Methods in Pharmacoepidemiology: A Modern Guide to Confounding Control and Causal Inference
This article provides a comprehensive overview of the application of propensity score (PS) methods in pharmacoepidemiology, targeting researchers and drug development professionals.
Propensity Score Methods in Pharmacoepidemiology: A Modern Guide to Confounding Control and Causal Inference
Abstract
This article provides a comprehensive overview of the application of propensity score (PS) methods in pharmacoepidemiology, targeting researchers and drug development professionals. It covers foundational principles, from defining causal estimands within the potential outcomes framework to implementing key designs like the new-user active comparator design to mitigate biases. The scope extends to practical guidance on methodological execution, including matching, weighting, and the use of high-dimensional propensity scores (hdPS) with machine learning for covariate selection. It also addresses troubleshooting for common challenges such as the 'PSM paradox,' model dependence, and unmeasured confounding, while validating methods through balance assessment and alignment with emerging frameworks like ICH E9(R1) and target trial emulation. The synthesis aims to equip researchers with the knowledge to produce more valid and reliable real-world evidence on drug safety and effectiveness.
Laying the Groundwork: Core Principles and Causal Frameworks for Propensity Scores
The Role of Propensity Scores in Addressing Confounding by Indication
Confounding by indication represents a fundamental methodological challenge in pharmacoepidemiology and comparative effectiveness research. This form of confounding arises when the clinical indications for prescribing a particular medication are themselves associated with the study outcome, creating a spurious association between treatment and outcome that does not reflect a causal relationship [1]. In clinical practice, healthcare professionals appropriately prescribe treatments based on patients' prognostic factors, channeling specific medications toward patients with particular characteristics or disease severities [1]. This channeling phenomenon, while clinically appropriate, creates substantial imbalances in baseline prognosis between treated and untreated groups in observational studies, potentially leading to severely biased treatment effect estimates if not adequately addressed.
Propensity score (PS) methods were specifically developed to address such confounding in observational studies by modeling how prognostic factors influence treatment decisions [1]. The propensity score, defined as the conditional probability of receiving treatment given observed covariates, provides a powerful tool for creating balanced comparison groups that mimic the balance achieved in randomized controlled trials [2]. By balancing measured baseline characteristics across treatment groups, propensity score methods help isolate the true effect of the treatment from the confounding influence of the treatment indications [3]. The application of propensity scores has become increasingly sophisticated, with recent advances including machine learning integration, high-dimensional propensity scores, and extensions for complex treatment regimens [4] [5].
Theoretical Foundations of Propensity Score Methods
The Propensity Score Framework
The theoretical foundation of propensity score analysis rests on the potential outcomes framework for causal inference [1]. For each patient, we consider potential outcomes under treatment (Y(1)) and control (Y(0)) conditions. The propensity score, defined as e(X) = P(Z=1|X), where Z indicates treatment assignment and X represents observed covariates, possesses the key property of being a balancing score [1]. This means that conditional on the propensity score, the distribution of observed baseline covariates is independent of treatment assignment: X ⊥ Z | e(X).
For valid causal inference using propensity scores, two critical assumptions must be satisfied. The first is strong ignorability, which requires that all common causes of treatment and outcome are measured and included in the propensity score model [2]. The second is the positivity assumption, which stipulates that every patient has a non-zero probability of receiving either treatment: 0 < P(Z=1|X) < 1 for all X [2]. When these assumptions hold, the propensity score can be used to remove confounding by indicated factors, enabling unbiased estimation of average treatment effects.
Evolution of Propensity Score Applications
Propensity score methods have evolved significantly since their introduction by Rosenbaum and Rubin in 1983 [4]. Initially applied primarily in settings with limited numbers of predefined confounders, these methods have expanded to address the challenges of high-dimensional healthcare databases, which may contain hundreds of potential covariates [1]. This evolution has included the development of automated variable selection algorithms, extensions for time-varying treatments, and incorporation of machine learning techniques for model specification [5].
Table 1: Key Developments in Propensity Score Methodology
| Development | Description | Application Context |
|---|---|---|
| High-Dimensional Propensity Score (hdPS) | Automated algorithm to select and prioritize covariates from large healthcare databases | Claims data analysis with numerous potential confounders [1] |
| Generalized Propensity Scores | Extension to categorical and continuous treatments | Comparative effectiveness of multiple treatments [1] |
| Machine Learning Integration | Use of ensemble methods, autoencoders, and other ML approaches for PS estimation | High-dimensional data with complex nonlinear relationships [4] |
| Target Trial Emulation | Framework for designing observational studies that mimic randomized trials | Addressing time-related biases and confounding [6] |
Practical Implementation of Propensity Score Methods
Propensity Score Estimation Protocols
The first step in implementing propensity score methods involves building an appropriate model for treatment assignment. Traditional approaches typically use logistic regression with investigator-specified covariates based on clinical knowledge and literature review [1]. However, in high-dimensional settings such as healthcare claims databases, several advanced approaches have been developed:
High-Dimensional Propensity Score (hdPS) Algorithm: This automated approach identifies and prioritizes covariates from large healthcare databases based on their potential for confounding adjustment [1]. The hdPS algorithm empirically identifies data dimensions (e.g., medication codes, diagnosis codes, procedure codes) and selects covariates based on their prevalence and potential for bias reduction.
Dimensionality Reduction Techniques: Recent methodological advances include the application of principal component analysis (PCA), logistic PCA, and autoencoders for propensity score estimation [4]. In a 2025 cohort study comparing dialysis exposure in heart failure patients, autoencoder-based propensity scores achieved superior covariate balance compared to traditional methods, with only 8 covariates showing standardized mean differences >0.1 versus 20-83 covariates with other methods [4].
Machine Learning Approaches: Ensemble methods, random forests, and regularized regression can accommodate complex nonlinear relationships and interactions without overfitting [7]. These approaches are particularly valuable when the true treatment assignment mechanism is complex or unknown.
Table 2: Comparison of Propensity Score Estimation Methods in a 2025 Cohort Study [4]
| Propensity Score Method | Number of Covariates with SMD>0.1 | Relative Performance |
|---|---|---|
| Autoencoder-based PS | 8 | Best balance |
| Principal Component Analysis (PCA) | 20 | Good balance |
| Logistic PCA | 25 | Moderate balance |
| High-Dimensional Propensity Score (hdPS) | 37 | Limited balance |
| Investigator-specified Covariates | 83 | Poorest balance |
Propensity Score Application Protocols
After estimating propensity scores, researchers must select an appropriate method for incorporating these scores into the analysis. The four primary approaches are:
Propensity Score Matching: This method creates matched sets of treated and untreated subjects with similar propensity scores [7]. The most common implementation is 1:1 nearest-neighbor matching without replacement, often with a caliper width (typically 0.2 of the standard deviation of the logit of the propensity score) to prevent poor matches [7]. After matching, balance should be assessed using standardized mean differences (target <0.1) and variance ratios.
Propensity Score Weighting: Inverse probability of treatment weighting (IPTW) creates a pseudo-population in which treatment assignment is independent of measured covariates [2]. Weights are defined as w = Z/e(X) + (1-Z)/(1-e(X)). Alternative weighting schemes include matching weights and overlap weights, which may improve precision and balance in regions of poor propensity score overlap [1].
Propensity Score Stratification: Subjects are stratified into quantiles (typically 5-10 strata) based on their propensity scores, and treatment effects are estimated within each stratum before pooling [2]. This approach works well when the relationship between propensity score and outcome is approximately constant within strata.
Covariate Adjustment: The propensity score is included directly as a covariate in the outcome regression model [7]. While straightforward to implement, this approach requires correct specification of both the propensity score model and the outcome model.
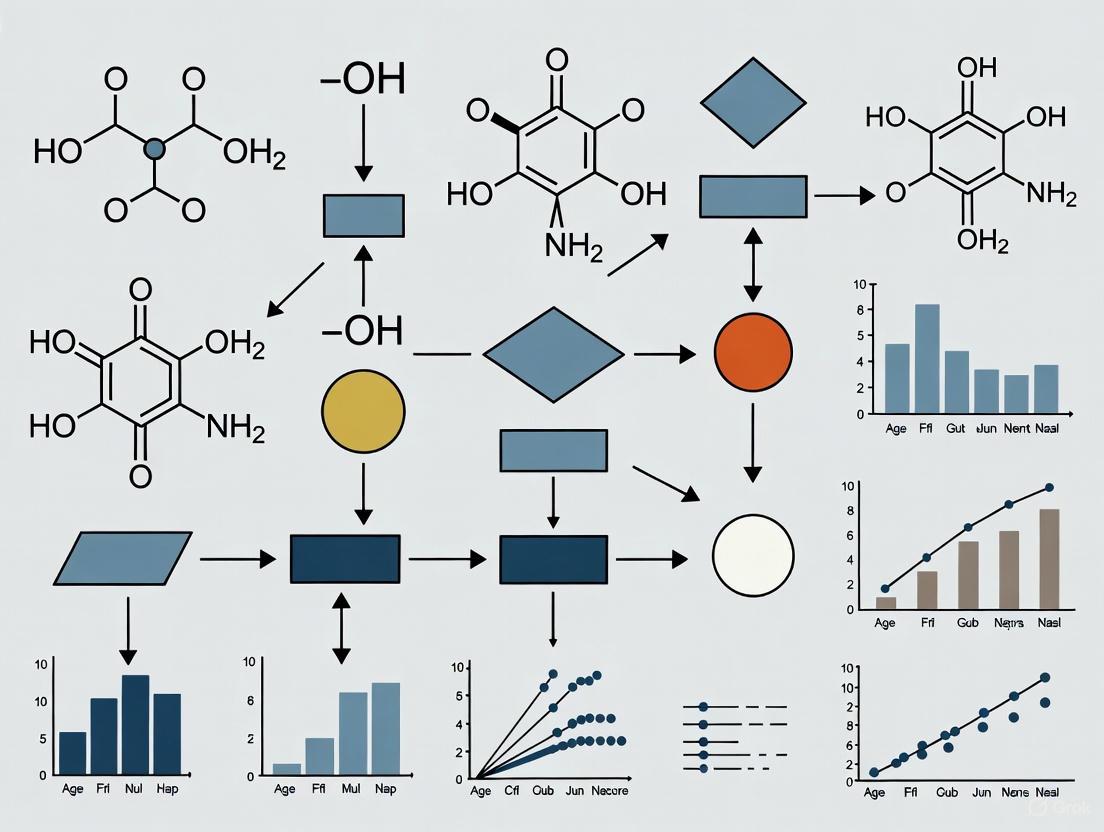
Figure 1: Propensity Score Analysis Workflow. This diagram illustrates the sequential process for implementing propensity score methods, highlighting the iterative balance assessment stage.
Advanced Applications and Case Studies
Addressing Complex Biases in Pharmacoepidemiology
Recent applications of propensity score methods have demonstrated their utility in addressing multiple methodological challenges simultaneously. A 2025 study in multiple sclerosis research implemented a high-dimensional propensity score analysis within a nested case-control framework to simultaneously address immortal time bias and residual confounding [6]. This innovative approach combined the design-based control of immortal time bias through the nested case-control design with the confounding control of hdPS, demonstrating a 28% reduction in mortality risk associated with disease-modifying drugs (HR: 0.72, 95% CI: 0.62-0.84) [6].
The hdPS algorithm was particularly valuable in this context as it could empirically identify hundreds of potential confounders from healthcare claims data, including diagnostic codes, procedure codes, and medication records [6]. The algorithm prioritizes covariates based on their potential for confounding control, allowing researchers to address residual confounding that might remain after adjustment for predefined covariates.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Methodological Tools for Propensity Score Analysis
| Tool Category | Specific Examples | Function in PS Analysis |
|---|---|---|
| Statistical Software | R (MatchIt, twang, WeightIt), SAS (PROC PSMATCH), Python (causalinference, psmatching) | Implementation of propensity score estimation and application methods |
| Balance Metrics | Standardized mean differences, variance ratios, Kolmogorov-Smirnov statistics | Quantifying covariate balance between treatment groups after PS adjustment |
| High-Dimensional Covariate Algorithms | hdPS, LASSO, Bayesian confounding adjustment | Automated covariate selection in settings with numerous potential confounders |
| Machine Learning Approaches | Random forests, gradient boosting, autoencoders, principal component analysis | Flexible propensity score estimation with minimal model misspecification |
| Sensitivity Analysis Methods | Rosenbaum bounds, E-values, propensity score calibration | Assessing robustness to unmeasured confounding |
| MurA-IN-4 | MurA-IN-4, CAS:318280-69-2, MF:C8H12ClNO3, MW:205.64 g/mol | Chemical Reagent |
| Tetramethyl-d12-ammonium bromide | Tetramethyl-d12-ammonium bromide, CAS:284474-82-4, MF:C4H12BrN, MW:166.12 g/mol | Chemical Reagent |
Validation and Sensitivity Analysis Protocols
Assessing Covariate Balance
The critical step in validating any propensity score analysis is assessing whether the method has successfully balanced covariates between treatment groups. The following protocol should be implemented:
Calculate standardized mean differences (SMD) for all covariates before and after propensity score adjustment. The SMD should be ≤0.1 for all important confounders to indicate adequate balance [4].
Examine variance ratios (ratio of variances between treatment groups) for continuous covariates, with ideal values between 0.5 and 2.0.
Visualize balance using Love plots, which display SMDs before and after adjustment, and empirical cumulative distribution function plots for continuous variables.
Assess propensity score distribution overlap using histograms or kernel density plots by treatment group.
In the 2025 dialysis study, the superiority of autoencoder-based propensity scores was demonstrated through superior balance metrics, with only 8 covariates showing SMD>0.1 compared to 20-83 with other methods [4].
Sensitivity Analysis for Unmeasured Confounding
Since propensity scores can only adjust for measured confounders, sensitivity analysis is essential to assess potential residual confounding:
Propensity Score Calibration: This method uses additional information on a subset of patients to correct for unmeasured confounding [1] [8].
External Adjustment: Incorporate estimates of the strength of association between unmeasured confounders and both treatment and outcome from external literature [3].
E-Value Calculations: Quantify the minimum strength of association that an unmeasured confounder would need to have with both treatment and outcome to explain away the observed effect [3].
Figure 2: Propensity Score Role in Addressing Confounding by Indication. This causal diagram illustrates how propensity scores (derived from measured covariates) help block backdoor paths created by treatment indications.
Propensity score methods represent a powerful approach for addressing confounding by indication in pharmacoepidemiological studies. When properly implemented, these methods can create balanced comparison groups that approximate the balance achieved in randomized trials, substantially reducing bias in treatment effect estimates [3]. The recent methodological advances in propensity score applications—including high-dimensional propensity scores, machine learning integration, and sophisticated weighting approaches—have enhanced their utility in modern healthcare database studies [4] [5].
Future developments in propensity score methodology will likely focus on improving robustness to model misspecification, enhancing approaches for time-varying treatments, and developing more sophisticated integration with machine learning techniques [1]. Additionally, there is growing interest in transparent reporting standards and sensitivity analysis frameworks that appropriately communicate the strength of evidence from propensity score analyses [3]. As these methods continue to evolve, they will play an increasingly important role in generating valid real-world evidence about treatment benefits and harms in clinical practice.
The Potential Outcomes Framework and Assumptions for Causal Inference
The Potential Outcomes Framework (POF), also known as the Rubin Causal Model (RCM), provides a formal mathematical foundation for defining and estimating causal effects. In the context of pharmacoepidemiological studies, which often rely on observational data from sources like health claims databases, this framework is indispensable for estimating the causal effects of drug exposures on patient outcomes while accounting for confounding [9] [10]. The framework augments the observed data by considering the outcomes that would occur under all possible treatment states, thus enabling a rigorous articulation of the assumptions required for causal inference.
Core Concepts of the Potential Outcomes Framework
Potential Outcomes and Causal Estimands
Consider a binary treatment (Z) (e.g., (Z=1) for drug exposure and (Z=0) for control). The potential outcome framework augments the joint distribution of ((Z,Y)) by introducing two random variables, ((Y(1), Y(0))), where:
- (Y(1)) is the outcome if the unit receives treatment.
- (Y(0)) is the outcome if the unit does not receive treatment [9].
The observed outcome (Y) is then defined as: [ Y = \begin{cases} Y(1) & \text{if } Z = 1 \ Y(0) & \text{if } Z = 0 \end{cases} ] or, more compactly, (Y^{\text{obs}} = Z \cdot Y(1) + (1-Z) \cdot Y(0)) [9]. The key problem of causal inference is that for any individual unit, only one of these potential outcomes is observed; the other is counterfactual [9] [10].
Within this framework, several causal estimands can be defined. The table below summarizes the most common ones.
Table 1: Key Causal Estimands in the Potential Outcomes Framework
| Estimand | Definition | Interpretation |
|---|---|---|
| Individual Treatment Effect (ITE) | (\taui = Yi(1) - Y_i(0)) | The causal effect for a single unit (i) [9]. |
| Average Treatment Effect (ATE) | (\mathrm{E}[Y(1) - Y(0)]) | The expected effect of moving an entire population from control to treatment [9] [10]. |
| Average Treatment Effect on the Treated (ATT) | (\mathrm{E}[Y(1)-Y(0)|Z=1]) | The average effect for those who actually received the treatment [10]. |
In pharmacoepidemiology, the choice between ATE and ATT depends on the research question. The ATE is often relevant for policy decisions (e.g., what is the effect of introducing a new drug to the entire population?), whereas the ATT is useful for understanding the effect on patients who typically receive a particular treatment [10].
The Fundamental Problem of Causal Inference
The core challenge is that the ITE (\taui) is fundamentally unobservable because it requires simultaneously observing both (Yi(1)) and (Y_i(0)) for the same unit [9] [10]. Therefore, statistical methods for causal inference must rely on comparisons between groups under assumptions that allow the unobserved potential outcomes to be inferred from the observed data.
Critical Assumptions for Causal Identification
For causal effects to be identified from observed data, certain assumptions must hold. The following diagram illustrates the core structure of the problem and the role of these assumptions.
Diagram 1: Potential Outcomes and Confounding. Y(1) and Y(0) are potential outcomes. Solid lines represent observed relationships, while dashed lines represent unobserved influences. Confounders (X, U) affect both treatment and outcomes.
Unconfoundedness (Ignorability)
This is the most critical assumption for causal inference in observational studies. It states that, conditional on observed covariates (X), the treatment assignment (Z) is independent of the potential outcomes [9] [10] [11]: [ (Y(1), Y(0)) \perp ! ! ! \perp Z \mid X ] This means that, within strata defined by the covariates (X), the assignment to treatment or control is as good as random [10]. This assumption is also known as the "no unmeasured confounding" assumption. In Diagram 1, this assumption would hold if all common causes of (Z) and (Y) (the confounders) are captured in (X), with no role for (U) [12] [13].
Positivity (Overlap)
This assumption requires that every unit has a positive probability of receiving either treatment, given the covariates [10]: [ 0 < P(Z=1 \mid X) < 1 ] In practice, this means that for all values of the observed covariates (X), there are both treated and untreated units. This ensures that there is a comparable control unit for every treated unit, and vice-versa, allowing for meaningful comparisons.
Consistency
The consistency assumption links the potential outcomes to the observed data. It states that the observed outcome for a unit that received treatment (Z=z) is exactly that unit's potential outcome under (z) [10]: [ \text{If } Z=z, \text{ then } Y^{\text{obs}} = Y(z) ] This implies that the treatment is well-defined and that there is no interference between units (the potential outcome of one unit is not affected by the treatment assignment of other units).
Application in Pharmacoepidemiology: The Role of Propensity Scores
In high-dimensional pharmacoepidemiological studies, directly conditioning on all covariates (X) is often impractical due to the curse of dimensionality. The propensity score, defined as the probability of treatment assignment conditional on observed covariates, (e(X) = P(Z=1|X)), addresses this issue [10] [11]. Rosenbaum and Rubin showed that if treatment assignment is unconfounded given (X), it is also unconfounded given the propensity score (e(X)) [10]: [ (Y(1), Y(0)) \perp ! ! ! \perp Z \mid e(X) ] This allows researchers to adjust for confounding by using the scalar propensity score instead of the high-dimensional vector (X).
Table 2: Common Propensity Score Methods in Pharmacoepidemiology
| Method | Protocol Description | Key Considerations |
|---|---|---|
| Propensity Score Matching (PSM) | Treated subjects are matched to untreated subjects with similar propensity scores. The ATE or ATT is estimated by comparing outcomes between matched groups [10]. | Requires decisions on matching algorithm (e.g., 1:1 nearest-neighbor), caliper width, and with/without replacement. Assess balance of covariates post-matching. |
| Inverse Probability of Treatment Weighting (IPTW) | Subjects are weighted by the inverse of their probability of receiving the treatment they actually received. Weights: (1/e(X)) for treated, (1/(1-e(X))) for untreated [10] [11]. | Creates a "pseudo-population" where confounding is eliminated. Can be unstable with extreme weights; truncated or stabilized weights are often used. |
| Stratification (Subclassification) | The sample is divided into strata (e.g., quintiles) based on the propensity score. Treatment effects are estimated within each stratum and then pooled [10]. | Typically, 5 strata remove ~90% of bias from a continuous confounder. Assess balance within strata. |
| Covariate Adjustment | The propensity score is included as a covariate in a regression model for the outcome [10]. | Simple to implement but relies on correct specification of the outcome model. |
The following workflow diagram illustrates a standard protocol for applying propensity score methods in a pharmacoepidemiological study.
Diagram 2: Propensity Score Analysis Workflow. This iterative process ensures confounding is adequately addressed before effect estimation.
Advanced Applications: High-Dimensional Propensity Scores (hdPS)
Pharmacoepidemiological studies using claims data often contain hundreds of potential covariates. The high-dimensional propensity score (hdPS) algorithm is a semi-automated data-driven method to efficiently select and adjust for a large number of covariates from such databases [4]. The protocol involves:
- Identifying Covariate Proxies: Identifying all recorded diagnoses, procedures, and drug prescriptions as potential covariates.
- Prioritizing Covariates: Ranking these covariates by their potential for confounding based on their prevalence and association with the treatment and outcome.
- Score Estimation: Including the top (n) covariates (e.g., 500) in the propensity score model [4] [6].
Recent research has shown that combining hdPS with dimensionality reduction techniques like autoencoders can further improve covariate balance in such high-dimensional settings [4].
The Scientist's Toolkit: Essential Reagents for Causal Inference
Table 3: Key Research Reagent Solutions for Causal Inference Studies
| Reagent / Tool | Function | Application Notes |
|---|---|---|
| Structured Healthcare Databases | Provide longitudinal data on drug exposure, patient outcomes, and confounders. | Examples: Claims data (e.g., Optum's Clinformatics Data Mart), electronic health records (EHR). Data quality and completeness are critical [4] [6]. |
| Propensity Score Estimation Algorithms | Model the probability of treatment assignment given covariates. | Logistic regression is standard. Advanced methods: hdPS, machine learning (boosted regression, random forests, autoencoders) for high-dimensional data [4] [10] [11]. |
| Balance Diagnostics | Quantify the similarity of covariate distributions between treated and control groups after PS adjustment. | Primary metric: Standardized Mean Differences (SMD). Target: SMD < 0.1 for all covariates. Visualization: Love plots, overlap plots [4] [10]. |
| Causal Graphical Models | Visually represent assumptions about causal relationships between variables. | Used to identify a sufficient set of confounders and to spot sources of bias like colliders [12] [13]. |
| Sensitivity Analysis Frameworks | Quantify how strong an unmeasured confounder would need to be to explain away an observed effect. | Assesses the robustness of causal conclusions to potential violations of the unconfoundedness assumption [14]. |
| Amethopterin-d3 | Amethopterin-d3, MF:C20H22N8O5, MW:457.5 g/mol | Chemical Reagent |
| Dodecanedioic acid-d20 | Dodecanedioic acid-d20, CAS:89613-32-1, MF:C12H22O4, MW:250.42 g/mol | Chemical Reagent |
Experimental Protocol: A Case Study on Dialysis and Mortality
To illustrate, here is a detailed protocol based on a real pharmacoepidemiological study investigating the association between dialysis and mortality in older heart failure patients [4].
Aim: To estimate the average treatment effect of dialysis on in-hospital mortality. Data Source: Optum's de-identified Clinformatics Data Mart Database. Design: Retrospective cohort study with propensity score matching.
Step-by-Step Protocol:
- Cohort Definition:
- Inclusion: Patients with heart failure and advanced chronic kidney disease.
- Exposure: Initiation of dialysis (Z=1) vs. no dialysis (Z=0).
- Outcome: All-cause in-hospital mortality (dichotomous).
- Final Cohort: 485 exposed and 1,455 unexposed after matching.
Propensity Score Estimation:
- Covariates (X): A high-dimensional set of covariates derived from claims data, including demographics, comorbidities, medications, and healthcare utilization.
- Method Comparison: The study compared PS estimated via:
- Investigator-specified covariates: Expert-selected variables.
- hdPS: A data-driven algorithm.
- Dimensionality Reduction Techniques: Principal Component Analysis (PCA), logistic PCA, and autoencoders [4].
Propensity Score Application:
- Matching: 1:1 matching was performed without replacement within a specified caliper.
- Balance Assessment: Covariate balance was assessed using SMDs across all PS methods.
Outcome Analysis:
- Effect Estimation: Hazard ratios for mortality were estimated using Cox proportional hazards models on the matched cohorts.
- Result: Autoencoder-based PS achieved the best covariate balance (only 8 covariates with SMD > 0.1), and hazard ratios for mortality were similar across all PS methods [4].
This case study demonstrates the application of the potential outcomes framework and highlights how advanced PS methods can improve confounding control in real-world research.
In pharmacoepidemiological studies research, which often relies on large, observational healthcare databases, defining the precise causal question is the critical first step before any analysis begins [1]. The causal estimand is a precise description of the causal quantity one seeks to learn from the data, specifying the target population, the treatment contrast of interest, and the outcome [15]. Within the potential outcomes framework, three fundamental estimands are the Sample Average Treatment Effect (SATE), the Sample Average Treatment Effect on the Treated (SATT), and the Population Average Treatment Effect (PATE) [1] [16]. The choice between them hinges on the underlying clinical question and dictates the analytical approach, the interpretation of results, and the scope of inference. Propensity score methods are a primary tool for estimating these estimands from observational data by attempting to mimic the balance achieved in randomized trials [1] [17]. This document outlines the definitions, applications, and estimation protocols for SATE, SATT, and PATE, framed specifically for pharmacoepidemiology research.
Defining the Estimands
Core Definitions and Formulations
The following table summarizes the core definitions and formulations of the three primary estimands.
Table 1: Core Definitions of SATE, SATT, and PATE
| Estimand | Full Name | Definition | Causal Question | Primary Application Context |
|---|---|---|---|---|
| SATE | Sample Average Treatment Effect | SATE = (1/n) * Σ [Y_i(1) - Y_i(0)] for all units i in the study sample [1]. |
What is the average treatment effect for all individuals in our study sample? | Efficacy evaluation within a randomized controlled trial (RCT) or a well-defined observational cohort [16]. |
| SATT | Sample Average Treatment Effect on the Treated | SATT = (1/n_t) * Σ [Y_i(1) - Y_i(0)] for all units i who actually received the treatment in the sample [1]. |
What is the average treatment effect for those individuals who actually received the treatment in our study? | Effectiveness and safety research in pharmacoepidemiology, where inference is for the patients who are prescribed the drug in real-world practice [18] [1]. |
| PATE | Population Average Treatment Effect | PATE = E[Y(1) - Y(0)] for all units in the broader target population [16]. |
What is the average treatment effect for the entire target population of interest? | Guiding broad policy or formulary decisions for a entire patient population (e.g., all patients with a specific condition in a country) [16]. |
These estimands are defined within the potential outcomes framework (or Rubin Causal Model) [1] [15]. For each individual i, there exists a potential outcome under treatment, Y_i(1), and a potential outcome under control, Y_i(0). The individual treatment effect is Ï„_i = Y_i(1) - Y_i(0). The fundamental problem of causal inference is that we can never observe both Y_i(1) and Y_i(0) for the same individual [15]. Therefore, we define average effects, like SATE, SATT, and PATE, over groups of individuals.
Conceptual Relationships and Workflow
The following diagram illustrates the conceptual relationship between the different estimands and the general workflow for defining a causal question.
Estimation in Pharmacoepidemiology
The Role of Propensity Scores
In observational pharmacoepidemiology, treatment is not randomly assigned. This leads to confounding, as treated and untreated groups differ in their prognostic characteristics [17]. Propensity score methods are a primary tool to control for this confounding by modeling the probability of treatment assignment given observed covariates [1].
The propensity score for a binary treatment A given covariates X is defined as e(X) = P(A=1 | X) [1]. Rosenbaum and Rubin proved that, under the assumption of conditional exchangeability (ignorability), conditioning on the propensity score balances the distribution of observed covariates X between treatment and control groups. This allows for the estimation of causal effects as if treatment had been randomized [1].
Linking Estimands to Propensity Score Methods
The choice of estimand directly influences how propensity scores are applied.
- SATT: When the goal is to estimate the SATT, the analysis is focused on achieving balance and making inferences for the treated individuals. Propensity score matching (PSM) is a natural choice, where each treated individual is matched to one or more untreated individuals with similar propensity scores. The effect is then estimated by contrasting outcomes within these matched pairs, effectively creating a pseudo-population that resembles the treated group but with similar covariate distributions [1] [17].
- SATE/PATE: To estimate the SATE or PATE, which pertain to the entire sample or population, inverse probability of treatment weighting (IPTW) is often used. IPTW creates a weighted pseudo-population where the weights,
w = A/e(X) + (1-A)/(1-e(X)), are inversely proportional to the probability of receiving the treatment actually received. This effectively simulates a scenario where every unit had the same chance of being treated, thus allowing for the estimation of an effect for the entire group [1]. A key challenge for PATE is that the study sample may not be perfectly representative of the target population, requiring additional transportability methods [19].
Table 2: Application of Propensity Score Methods by Estimand
| Estimand | Recommended Propensity Score Method | Intuitive Explanation | Key Considerations |
|---|---|---|---|
| SATT | Matching (e.g., 1:1 nearest neighbor) | Finds a control "twin" for each treated individual based on their probability of being treated. The effect is the average outcome difference between each treated individual and their twin. | Preserves the original treated group. The quality of the estimate depends on the ability to find good matches for all treated individuals. |
| SATE | Inverse Probability of Treatment Weighting (IPTW) | Uses weights to make the treated group look like the full sample and the control group look like the full sample. The weighted groups represent a pseudo-population where everyone had the same chance to be treated or not. | Can be inefficient if some propensity scores are very close to 0 or 1. Requires careful checking of weight distributions. |
| PATE | IPTW + Transportability Methods | First uses IPTW to balance the study sample, then uses a second set of weights (inverse odds of sampling weights) to make the balanced study sample resemble the target population. | Requires data on covariates from the target population. Relies on the strong assumption that all effect modifiers are measured and accounted for [19]. |
Detailed Experimental Protocol: Estimating SATT via Propensity Score Matching
The following workflow details the steps for estimating the SATT using propensity score matching, a common application in pharmacoepidemiology.
Protocol Steps:
Variable Definition [17]:
- Treatment Variable: Clearly define the treatment (e.g., initiation of a new drug vs. an active comparator).
- Outcome Variable: Define the clinical outcome of interest (e.g., hospitalization, mortality).
- Confounding Variables: Select a set of pre-treatment covariates
Xthat are potential common causes of both the treatment and the outcome. This should include demographic information, clinical comorbidities, medication history, and healthcare utilization measures. Leverage clinical expertise and guidelines to build a plausible model.
Estimate Propensity Scores [17]:
- Fit a model, typically a logistic regression, where the treatment indicator is the dependent variable and all confounding covariates are independent variables.
logit(P(A=1 | X)) = β₀ + βâ‚Xâ‚ + ... + βₖXâ‚–- The predicted values from this model are the estimated propensity scores,
ê(X), for each individual. - Advanced methods like Generalized Boosted Models (GBM) or Bayesian Additive Regression Trees (BART) can also be used for more flexible estimation.
Perform Matching [17]:
- Use a matching algorithm to pair treated individuals with untreated individuals who have a similar propensity score.
- Nearest-neighbor matching is the most common. Each treated individual is matched to the untreated individual with the closest propensity score, often within a pre-specified "caliper" (e.g., 0.2 standard deviations of the logit of the propensity score) to prevent poor matches.
- Unmatched individuals are excluded from the subsequent analysis.
Check Covariate Balance [17]:
- After matching, it is imperative to check if the distribution of covariates is now similar between the treated and control groups.
- Use quantitative measures like standardized mean differences (SMD) for each covariate. An SMD below 0.1 (10%) is generally considered indicative of good balance.
- If imbalance persists, the propensity score model or matching parameters may need to be revised (e.g., adding interaction terms, using a different caliper).
Estimate Treatment Effect (SATT):
- In the matched sample, compare the outcomes between the treated and control groups.
- Since matching creates paired data, a paired t-test (for continuous outcomes) or conditional logistic regression (for binary outcomes) can be used. Alternatively, a generalized linear model (e.g., logistic regression) that includes the matched pairs as strata can be fitted [17].
- The resulting coefficient for the treatment variable is an estimate of the SATT.
Sensitivity Analysis:
- Conduct analyses to assess how sensitive the results are to unmeasured confounding. Methods like the Rosenbaum bounds can be used to determine how strong an unmeasured confounder would need to be to qualitatively change the study conclusions [1].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Software for Causal Inference Analysis
| Tool / Reagent | Category | Function in Causal Workflow | Examples & Notes |
|---|---|---|---|
| 'MatchIt' R Package [17] | Software | A comprehensive tool for performing propensity score matching and other matching methods. | Implements nearest-neighbor, optimal, full, and genetic matching. Integrates with the R ecosystem for balance assessment and outcome analysis. |
| 'cobalt' R Package [17] | Software | Covariate Balance Assessment Tables and Plots. | Provides a wealth of functions and graphics (e.g., love plots) to evaluate covariate balance before and after applying propensity score methods. |
| High-Dimensional Propensity Score (hdPS) [1] | Algorithm | Automates the selection of a large number of potential confounders from healthcare claims data. | Identifies and prioritizes covariates based on their prevalence and potential for confounding. Useful for dealing with the high dimensionality of administrative databases. |
| DAGitty [20] | Software | A browser-based tool for creating, editing, and analyzing causal Directed Acyclic Graphs (DAGs). | Helps researchers visually articulate and test their causal assumptions, identify minimal sufficient adjustment sets, and detect potential biases like M-bias. |
| Stable Unit Treatment Value Assumption (SUTVA) [16] | Conceptual Assumption | The foundational assumption that one unit's outcome is unaffected by another unit's treatment assignment. | Violations (e.g., interference or contagion) complicate causal inference. Must be considered in the study design phase. |
| Generalized Linear Model (GLM) [17] | Statistical Model | The standard workhorse for estimating the propensity score (via logistic regression) and for outcome analysis after matching or weighting. | Flexible framework for different types of outcomes (binary, continuous, count). |
| N-Myristoyl-Lys-Arg-Thr-Leu-Arg | N-Myristoyl-Lys-Arg-Thr-Leu-Arg, CAS:125678-68-4, MF:C42H82N12O8, MW:883.2 g/mol | Chemical Reagent | Bench Chemicals |
| Uracil-15N2 | Uracil-15N2, CAS:5522-55-4, MF:C4H4N2O2, MW:114.07 g/mol | Chemical Reagent | Bench Chemicals |
The explicit definition of the causal estimand—SATE, SATT, or PATE—is a fundamental prerequisite for rigorous pharmacoepidemiological research. SATT is often the most relevant estimand for questions of drug effectiveness and safety in real-world practice, as it directly concerns the patients who are actually prescribed the treatment. Propensity score methods, particularly matching for SATT, provide a powerful design-based approach to minimize confounding by indication in observational studies. However, no analytical method can compensate for a poorly defined causal question. By starting with a clear estimand, researchers can select an appropriate methodology, justify their analytical choices, and ultimately produce evidence that is interpretable and meaningful for clinical and regulatory decision-making.
Pharmacoepidemiology bridges clinical pharmacology and epidemiology, studying the use and effects of medications in large human populations [21]. While randomized controlled trials (RCTs) remain the gold standard for establishing efficacy, they have inherent limitations including strict inclusion criteria, short follow-up durations, and limited power for rare adverse events [22] [21]. Consequently, observational studies using real-world data (RWD) provide essential complementary evidence on drug effectiveness and safety in routine clinical practice [23].
However, analyses of observational data face formidable methodological challenges, primarily confounding by indication and various selection biases [1] [24]. In clinical practice, treatments are prescribed selectively based on clinical parameters—healthcare professionals prescribe when anticipating benefit and withhold treatment when concerned about adverse events [1]. This fundamental aspect of clinical decision-making creates systematic differences between treatment groups that, if unaddressed, render crude outcome comparisons uninterpretable [24].
The new-user design and active comparator design constitute a paradigm shift in pharmacoepidemiology that addresses these fundamental methodological challenges [24] [25]. When combined into the active comparator, new user (ACNU) design, these approaches enable observational studies to emulate the design of head-to-head randomized trials, significantly improving the validity of real-world evidence [24] [22]. This article explores the foundational concepts, implementation protocols, and analytical framework of these designs within the context of modern pharmacoepidemiologic research employing propensity score methods.
Conceptual Foundations and Rationale
The Active Comparator Design
The active comparator design (also known as active comparator design) compares the drug of interest ('Drug A') to another active drug ('Drug B') used for the same indication, rather than comparing to non-users [22] [25]. This approach provides three distinct methodological advantages:
First, it increases overlap of measured characteristics between treatment groups. By selecting comparator drugs with similar therapeutic indications, the design creates treatment groups that are more similar in terms of measured baseline characteristics, facilitating more effective statistical adjustment [22].
Second, it reduces potential for unmeasured confounding. Non-user groups often include patients with contraindications to treatment or those with very mild disease, introducing systematic differences in unmeasured characteristics like frailty or disease severity [22]. As demonstrated in studies of influenza vaccine, comparisons with non-users can yield implausibly strong protective effects against all-cause mortality due to such confounding [24]. Active comparator groups minimize these differences by restricting comparisons to patients with clear treatment indications [22].
Third, it addresses more clinically relevant questions. For many chronic conditions where some treatment is necessary, the relevant clinical question is not whether to treat but which treatment to choose [22]. The active comparator design directly answers this question by providing evidence on comparative effectiveness and safety between therapeutic alternatives [22].
The New-User Design
The new-user design (also known as incident user design or initiator design) identifies patients at the time of treatment initiation and begins follow-up at this point [22] [25]. This approach offers several critical advantages over prevalent user designs, which include both new and existing users:
This design enables assessment of time-varying hazards and drug effects. The risk of many adverse events changes over time, often highest shortly after treatment initiation [22]. For instance, studies of TNF-α inhibitors in rheumatoid arthritis have demonstrated the highest infection risk occurs within the first 90 days of treatment [22]. Prevalent user designs miss these time-varying hazards because they include persons who have already tolerated the treatment [22].
The new-user approach also ensures appropriate confounding adjustment by clearly establishing a baseline measurement point. This allows investigators to accurately distinguish pretreatment covariates from posttreatment variables, preventing adjustment for mediators that lie on the causal pathway between treatment and outcome [22].
Additionally, this design eliminates immortal time bias when combined with an active comparator. Immortal time refers to follow-up period during which the outcome cannot occur because of the study design [22]. By aligning start of follow-up for both treatment groups at treatment initiation, the new-user design avoids this methodological pitfall [22].
Table 1: Key Advantages of Foundational Design Components
| Design Component | Key Advantages | Methodological Threats Addressed |
|---|---|---|
| Active Comparator | - Increases overlap of measured characteristics- Reduces unmeasured confounding- Answers clinically relevant questions | - Confounding by indication- Healthy user/sick stopper effects- Channeling bias |
| New-User Design | - Captures time-varying hazards- Ensures appropriate covariate measurement- Defines accurate treatment duration | - Immortal time bias- Prevalent user bias- Depletion of susceptibles |
Implementation Protocols
Cohort Definition and Eligibility Criteria
Implementing the ACNU design begins with defining a source population and establishing eligibility criteria that emulate the inclusion criteria of a target randomized trial [26]. The process involves:
- Identifying the disease cohort: Define a population of patients with the medical condition for which the study and comparator drugs are indicated [24].
- Establishing drug exposure definitions: Clearly define the pharmaceutical agents of interest, including specific formulations, dosages, and administration routes [27].
- Applying inclusion/exclusion criteria: Apply criteria related to demographics, clinical characteristics, and healthcare utilization to create a study population that would be eligible for either treatment in clinical practice [22].
- Defining the cohort entry date: For both treatment groups, the cohort entry date ("time zero") is the date of treatment initiation after meeting all eligibility criteria [27] [22].
Follow-Up Period and Outcome Assessment
The follow-up protocol must be specified a priori to ensure temporal precedence of exposure before outcome:
- Start of follow-up: Follow-up begins immediately after the cohort entry date for both treatment groups [27] [22].
- End of follow-up: Follow-up continues until the earliest of: outcome occurrence, treatment discontinuation, switching to comparator drug, end of study period, loss to follow-up, or death [27].
- Risk window specification: Define biologically plausible risk windows based on the pharmacodynamics and pharmacokinetics of the drugs under study [27].
- Outcome ascertainment: Implement validated algorithms to identify outcomes of interest, using specific combinations of diagnosis codes, procedures, and medications to maximize specificity and sensitivity [26].
Figure 1: Implementation Workflow for Active Comparator, New-User Design. This diagram illustrates the sequential process of defining study cohorts and follow-up periods according to ACNU principles.
Covariate Selection and Measurement
A critical step in implementing the ACNU design is the appropriate selection and measurement of potential confounders:
- Define baseline period: Establish a fixed period before treatment initiation (e.g., 6-12 months) for assessing all covariates [22].
- Identify confounder domains: Consider demographics, clinical characteristics, comorbidities, healthcare utilization patterns, concomitant medications, and laboratory values [1].
- Apply causal knowledge: Prioritize variables that are risk factors for the outcome and associated with treatment assignment, while avoiding instruments (predictors of treatment only) and mediators (variables on causal pathway) [1] [28].
- Address high-dimensional data: In databases with numerous potential covariates, consider algorithms like the high-dimensional propensity score (hdPS) that systematically select covariates based on their association with both treatment and outcome [1].
Analytical Framework: Integration with Propensity Score Methods
Propensity Score Estimation in ACNU Studies
The ACNU design creates an ideal foundation for propensity score methods by ensuring appropriate covariate measurement and temporal alignment [1] [22]. The propensity score is defined as the probability of treatment assignment conditional on observed baseline covariates [1] [28]. In ACNU studies:
- Model specification: The propensity score model includes all measured baseline covariates identified in the design phase, typically using logistic regression for binary treatments [1] [28].
- Modeling goal: The objective is not prediction perfection but achieving balance in covariates between treatment groups; thus, predictive performance metrics like c-statistics should not guide model specification [1].
- Extended applications: For multiple active comparators, the generalized propensity score can be estimated using multinomial regression models [1].
Propensity Score Application and Balance Assessment
After estimation, propensity scores can be applied through various methods:
- Matching: Creates comparable groups by matching each treated individual with one or more comparator individuals with similar propensity scores [28].
- Weighting: Creates a pseudo-population using inverse probability of treatment weights where covariates are balanced between groups [1].
- Stratification: Divides the study population into strata based on propensity score quantiles and estimates treatment effects within each stratum [28].
- Covariate adjustment: Includes the propensity score as a covariate in the outcome regression model [28].
Table 2: Propensity Score Applications in ACNU Studies
| Application Method | Implementation | Considerations for ACNU Studies |
|---|---|---|
| Propensity Score Matching | 1:1 or variable ratio matching with caliper | - May reduce sample size- Optimizes comparability at individual level- Targets effect in the treated |
| Inverse Probability Weighting | Weights = 1/PS for treated, 1/(1-PS) for untreated | - Maintains original sample size- Creates pseudo-population- Can be unstable with extreme weights |
| Stratification | Subclassification into 5-10 quantiles | - Simple implementation- Allows effect modification assessment- May have residual within-stratum imbalance |
| Covariate Adjustment | Include PS as covariate in outcome model | - Simple approach- Assumes correct functional form- Less robust than other methods |
Crucially, the success of propensity score methods depends on achieving covariate balance between treatment groups after application. Balance should be assessed using standardized differences rather than statistical significance tests, with differences <0.1 generally indicating adequate balance [1] [28].
Outcome Analysis and Effect Estimation
Following propensity score application and balance verification, outcome analysis proceeds:
- Model specification: Choose an appropriate regression model (e.g., Cox proportional hazards, logistic, or Poisson regression) based on the outcome type and distribution [27].
- Effect measure selection: Report both relative (hazard ratios, risk ratios) and absolute (risk differences) effect measures to facilitate clinical interpretation [27].
- Precision estimation: Use robust variance estimators for weighting approaches and account for matched design in matched analyses [1].
- Sensitivity analyses: Conduct analyses to assess potential impact of unmeasured confounding, including quantitative bias analysis and E-values [1].
Figure 2: Analytical Framework Integrating ACNU Design with Propensity Scores. This workflow demonstrates the iterative process of propensity score application with balance assessment as the critical decision point.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Methodological Reagents for ACNU Studies with Propensity Scores
| Research Reagent | Function/Purpose | Implementation Considerations |
|---|---|---|
| Active Comparator Drugs | Therapeutic alternative with similar indications | - Should represent viable clinical alternative- Similar mechanism of action preferred but not required- Must have sufficient sample size |
| New-User Cohort | Population of treatment initiators | - Requires washout period to establish new use- Clear operational definition of initiation- Captures all eligible initiators in source population |
| Propensity Score Model | Predicts treatment probability given covariates | - Includes all measured confounders- Avoids overfitting- Focus on balance rather than prediction |
| Balance Metrics | Assesses comparability after PS application | - Standardized differences preferred over p-values- Threshold <0.1 indicates balance- Assess both individual covariates and overall balance |
| High-Dimensional Propensity Score (hdPS) | Algorithmic covariate selection in large databases | - Identifies covariates from data dimensions- Particularly useful in claims data- Requires sufficient sample size |
| 1-Hydroxyoctadecane-d2 | 1-Hydroxyoctadecane-d2, MF:C18H38O, MW:272.5 g/mol | Chemical Reagent |
| 1-(~2~H)Ethynyl(~2~H_5_)benzene | 1-(~2~H)Ethynyl(~2~H_5_)benzene, CAS:25837-47-2, MF:C8H6, MW:108.17 g/mol | Chemical Reagent |
The new-user design and active comparator design represent foundational methodological advances in pharmacoepidemiology that substantially strengthen the validity of real-world evidence. When implemented through the structured protocols outlined in this article and integrated with propensity score methods, these approaches enable observational studies to more closely approximate randomized trials, addressing pervasive biases like confounding by indication and healthy user effects.
The ACNU framework provides the methodological foundation for generating high-quality evidence on the comparative effectiveness and safety of medical products across their lifecycle. As pharmacoepidemiology continues to evolve with increasing access to large healthcare databases and advanced analytical techniques, these core design principles remain essential for producing reliable evidence to inform clinical practice and regulatory decision-making.
Pharmacoepidemiology, which assesses the use and effects of drugs in large populations, relies heavily on observational studies using secondary healthcare databases. Unlike randomized controlled trials (RCTs), where randomization balances both known and unknown prognostic factors, observational studies are susceptible to multiple systematic biases that can distort the true relationship between drug exposure and patient outcomes [29] [30]. Failure to adequately identify and mitigate these biases can lead to erroneous conclusions about a drug's safety or effectiveness, with significant implications for clinical practice and public health [29] [31]. Within the broader context of a thesis on propensity score methods in pharmacoepidemiological research, this document provides detailed application notes and protocols for three common and impactful biases: immortal time bias, selection bias (with a focus on channeling bias), and confounding by indication. The aim is to equip researchers with structured, practical methodologies to enhance the validity of their observational studies.
Table 1: Definitions and Impact of Key Biases
| Bias Type | Definition | Common Impact on Effect Estimates |
|---|---|---|
| Immortal Time Bias | A period of follow-up during which the outcome under study cannot occur, by design, due to how exposure is defined [32] [33]. | Often exaggerates treatment benefit; can artificially reverse the direction of effect [33] [34]. |
| Channeling Bias | A selection bias where drugs with similar indications are preferentially prescribed to groups of patients with varying baseline prognoses or risk levels [29] [30]. | Can create a spurious association by making one drug appear more harmful or beneficial due to the underlying risk profile of its users. |
| Confounding by Indication | Occurs when the underlying diagnosis or clinical reason for prescribing a drug is itself a risk factor for the outcome under study [29]. | Severely confounds the exposure-outcome relationship, as the treatment indicator is a marker for the severity of the underlying illness. |
Application Notes & Experimental Protocols
Immortal Time Bias
Application Notes
Immortal time bias is a pervasive time-related bias that arises from a misalignment between the start of follow-up (time-zero) and the assignment of exposure [32] [33]. It frequently occurs in pharmacoepidemiology when exposure is defined by a first prescription fill that happens some time after a patient qualifies for cohort entry (e.g., after a diagnosis or hospital discharge). The period between cohort entry and this first prescription is "immortal" because the patient must necessarily have survived and not experienced the outcome to have received the exposure [33]. When this immortal person-time is misclassified as exposed time—or excluded entirely—it artificially inflates the survival time of the exposed group, leading to a spurious protective effect [32]. This bias has been shown to substantially distort findings, sometimes even reversing the conclusions of a study [33].
Experimental Protocol for Identification and Mitigation
Objective: To design and analyze an observational cohort study that accurately accounts for immortal time between cohort entry and first drug exposure.
Materials and Data Requirements:
- A longitudinal healthcare database with information on patient demographics, drug prescriptions, hospital admissions, and vital status.
- Clearly defined:
- Cohort entry date (e.g., date of diagnosis, hospital discharge).
- Exposure of interest (e.g., a specific drug class).
- Study outcome (e.g., mortality, hospital readmission).
Procedure:
- Cohort Definition: Define a population of incident users, where patients enter the cohort at the start of a new treatment episode [35]. Apply a washout period to ensure no prior use of the study drug.
- Time-Zero Alignment: Align the start of follow-up (time-zero) and exposure assignment. A patient should be classified as exposed from the date of their first prescription fill onwards. All person-time before this date is considered unexposed.
- Time-Dependent Analysis: Employ a statistical model that treats drug exposure as a time-varying covariate.
- In a Cox proportional hazards model, this means creating a dataset where each patient's follow-up is split into multiple rows based on changes in exposure status.
- Person-time from cohort entry until the first prescription is coded as "unexposed."
- Person-time from the first prescription onward is coded as "exposed."
- Analysis: Run the Cox regression model using the time-varying exposure variable to estimate the hazard ratio for the outcome.
Validation: Where possible, specify a target trial that the observational study aims to emulate, ensuring alignment of time-zero, eligibility criteria, and exposure definition to prevent self-inflicted injuries like immortal time bias [5].
The following diagram illustrates the core methodological flaw and the recommended corrective analysis for immortal time bias.
Figure 1: Analytical Approaches for Immortal Time Bias
Channeling Bias
Application Notes
Channeling bias is a specific form of selection bias prevalent in comparative drug studies. It occurs when a newly marketed drug is "channeled" toward specific patient subgroups, such as those for whom established treatments have failed, those with more severe disease, or those with specific comorbidities [30]. Conversely, the older drug may be used predominantly in a more stable, "healthier" population. This creates a systematic imbalance in prognostic factors between the treatment groups at baseline. If these factors are also associated with the outcome, the resulting comparison is confounded. For example, the new drug may appear to have a higher rate of adverse events simply because it is prescribed to sicker patients [30].
Experimental Protocol for Mitigation Using Propensity Scores
Objective: To balance measured baseline covariates between patients initiating a new drug versus a comparator drug, thereby reducing channeling bias.
Materials and Data Requirements:
- A healthcare database with rich information on patient characteristics, comorbidities, concomitant medications, and healthcare utilization.
- Statistical software capable of performing logistic regression and propensity score matching/weighting.
Procedure:
- Cohort Definition: Define two cohorts of incident users: one for the new drug and one for the active comparator. The cohorts should be contemporary and have similar indications [35].
- Covariate Assessment: Identify and measure all potential pre-treatment confounders (e.g., age, sex, disease severity markers, prior medications, comorbidities) in a baseline period prior to the first prescription.
- Propensity Score (PS) Estimation:
- Fit a logistic regression model where the dependent variable is treatment assignment (1=new drug, 0=comparator).
- The independent variables are all measured baseline covariates.
- The predicted probability from this model is the propensity score—the conditional probability of receiving the new drug given the covariates [30] [36].
- PS Implementation: Choose one of the following methods:
- Matching: Match each patient on the new drug to one or more patients on the comparator drug with a similar PS (using a caliper, e.g., 0.2 of the standard deviation of the PS logit) [36].
- Weighting: Use inverse probability of treatment weighting (IPTW), where weights are created as 1/PS for the new drug group and 1/(1-PS) for the comparator group. This creates a "pseudo-population" where the distribution of covariates is balanced between groups [37] [36].
- Balance Assessment: After applying the PS method, check the balance of all covariates between the treatment groups. The standardized mean difference for each covariate should be <0.1 to indicate adequate balance [36].
- Outcome Analysis: Analyze the association between treatment and outcome in the matched or weighted sample, using a regression model that may further adjust for any residual imbalance.
Limitations: Propensity scores can only adjust for measured confounders. Residual confounding from unmeasured variables (e.g., disease severity not fully captured in the database) may persist [30].
Confounding by Indication
Application Notes
Confounding by indication is perhaps the most fundamental challenge in pharmacoepidemiology. It arises because drugs are prescribed for specific medical conditions, and those conditions are often strong predictors of the study outcome [29]. For instance, studying the effect of antidepressants on mortality is complicated by the fact that depression itself is associated with an increased risk of death. The "indication" for the drug confounds the relationship between the drug (exposure) and the outcome. This bias is inherent in the non-randomized nature of treatment decisions and must be addressed through careful study design and analysis.
Experimental Protocol for Mitigation with an Active Comparator New-User Design
Objective: To mitigate confounding by indication by comparing two active drugs used for the same condition, and to balance baseline risks using propensity scores.
Materials and Data Requirements:
- The same data requirements as in Section 2.2.2.
Procedure:
- Active Comparator Selection: Identify a clinically relevant alternative drug used for the same primary indication as the drug of interest. This helps ensure that the two groups are more comparable in their underlying disease state than if one were compared to non-users [35].
- New-User Design: Restrict the cohort to incident users of either drug, ensuring patients are observed from the start of their treatment episode. This avoids biases associated with prevalent users, who are "survivors" of the early treatment period and may be healthier [35].
- Propensity Score Application: Follow the same steps for PS estimation and implementation as outlined in the protocol for channeling bias (Section 2.2.2). The goal is to create a balanced comparison group that has a similar probability of receiving one drug over the other, based on all measured baseline characteristics.
- Sensitivity Analysis: Conduct sensitivity analyses to quantify how strong an unmeasured confounder would need to be to explain away the observed effect [36].
The following workflow integrates the protocols for addressing channeling bias and confounding by indication through the use of propensity score methods within an active comparator, new-user design.
Figure 2: Propensity Score Workflow for Channeling Bias and Confounding
The Scientist's Toolkit: Research Reagent Solutions
In the context of methodological research for mitigating bias, "research reagents" refer to the essential conceptual frameworks, study designs, and analytical techniques required to conduct a valid pharmacoepidemiologic study.
Table 2: Essential Methodological Toolkit for Bias Mitigation
| Tool | Function & Application | Key Considerations |
|---|---|---|
| Active Comparator New-User Design | Foundational design that reduces confounding by indication and selection bias by comparing two active drugs and starting follow-up at treatment initiation [35]. | Ensures comparability of treatment groups from the beginning of therapy. |
| Time-Dependent Cox Model | Statistical model used to correctly classify person-time and eliminate immortal time bias by treating drug exposure as a variable that changes over time [32] [33]. | Requires careful data management to split patient follow-up into unexposed and exposed periods. |
| Propensity Score (PS) | A single score (probability of treatment) summarizing all measured baseline covariates; used to balance confounders across treatment groups [37] [30] [36]. | Balances only measured covariates. Model specification and balance assessment are critical. |
| High-Dimensional Propensity Score (hd-PS) | An algorithm that automatically screens a large number of predefined covariates (e.g., diagnosis codes, procedure codes) in administrative data to supplement researcher-specified confounders [5]. | Useful when rich clinical data are lacking; helps control for unmeasured confounding by proxy. |
| Standardized Difference | A balance metric used to assess the effectiveness of PS methods. It is not influenced by sample size, unlike p-values [36]. | A value <0.1 after PS adjustment indicates adequate balance for a covariate. |
| Target Trial Emulation | A framework for designing observational studies by explicitly specifying the protocol of a hypothetical RCT that the study aims to emulate [5]. | Helps avoid common biases (like immortal time) by forcing alignment of time-zero, eligibility, and treatment strategies. |
| Sulfadoxine D3 | Sulfadoxine D3, CAS:1262770-70-6, MF:C12H14N4O4S, MW:313.35 g/mol | Chemical Reagent |
| Aphidicolin 17-acetate | Aphidicolin 17-acetate, MF:C8H6BrF2NO3, MW:282.04 g/mol | Chemical Reagent |
From Theory to Practice: Implementing Propensity Score Analysis in Real-World Data
A Step-by-Step Guide to Propensity Score Estimation and Covariate Selection
In pharmacoepidemiological studies, researchers routinely use real-world data to assess the safety and effectiveness of pharmaceutical products. Unlike randomized controlled trials, observational studies are prone to confounding bias due to imbalanced baseline characteristics between treatment groups. Propensity score (PS) methods have emerged as a powerful statistical approach to address this challenge by creating pseudo-randomized conditions when analyzing observational data. A propensity score, defined as the probability of treatment assignment conditional on observed covariates, enables researchers to simulate the balancing properties of randomization.
The growing availability of large-scale healthcare databases has expanded opportunities for pharmacoepidemiological research, but it has also intensified methodological challenges related to confounding control and model specification. This guide provides a comprehensive framework for propensity score estimation and covariate selection, with particular emphasis on applications in drug development and safety research. We detail both established and emerging methodologies, including machine learning approaches and hybrid techniques that combine propensity scores with prognostic scores to enhance causal inference from non-randomized study designs.
Theoretical Foundations and Key Concepts
Defining the Propensity Score
The propensity score for subject i (i = 1, ..., N) is defined as the conditional probability of receiving the treatment given the observed covariates: e(Xi) = P(Ai = 1 | Xi) where Ai is the treatment indicator (1 for treatment, 0 for control) and X_i is the vector of observed pre-treatment covariates. Rosenbaum and Rubin demonstrated in 1983 that, under the strong ignorability assumption, treatment assignment and potential outcomes are independent conditional on the propensity score. This foundational property allows researchers to adjust for confounding by balancing the distribution of observed covariates across treatment groups based on the propensity score.
The strong ignorability assumption requires two conditions: first, that the treatment assignment is independent of potential outcomes given the covariates (unconfoundedness), and second, that every subject has a positive probability of receiving either treatment (positivity). In pharmacoepidemiological applications, these assumptions must be carefully considered in the context of the clinical question and available data. Violations of these assumptions, particularly unmeasured confounding, remain a fundamental limitation that propensity scores cannot fully address.
Covariate Selection Principles and Approaches
Causal diagrams (directed acyclic graphs) provide a theoretical framework for identifying an appropriate set of confounders for inclusion in the propensity score model. The goal is to include covariates that are associated with both treatment and outcome while avoiding instruments (variables affecting only treatment) and mediators (variables on the causal pathway between treatment and outcome). Including instrumental variables can increase variance without reducing bias, while including mediators can introduce overadjustment bias by blocking causal pathways.
For pharmacoepidemiological studies, researchers should prioritize covariates with known clinical relevance to the disease process and treatment decision-making. A structured approach to covariate selection might include:
- Clinical knowledge-based selection: Using subject matter expertise to identify potential confounders
- High-dimensional propensity score (hdPS): Data-adaptive algorithm for selecting covariates from large healthcare databases
- Hybrid approaches: Combining clinical knowledge with automated variable selection techniques
Recent methodological research emphasizes that prioritizing covariates strongly associated with the outcome, rather than treatment, generally leads to better bias reduction in treatment effect estimates. This principle has motivated the development of prognostic score-based approaches to propensity score estimation and evaluation.
Methodological Approaches to Propensity Score Estimation
Traditional Statistical Methods
Logistic regression represents the most widely used approach for propensity score estimation. The model specification follows standard logistic regression framework, with treatment status as the dependent variable and selected covariates as independent variables: logit(P(Ai = 1 | Xi)) = β0 + β1X1i + ... + βpX_pi
The reference method in pharmacoepidemiology typically involves logistic regression with covariates selected based on clinical knowledge and prior literature. This approach performs well when the relationship between covariates and treatment assignment is linear and additive, and when all relevant confounders have been correctly identified and measured. However, model misspecification remains a concern, particularly when complex interactions or nonlinear relationships exist in the data.
Regularized regression methods, such as LASSO (Least Absolute Shrinkage and Selection Operator), introduce penalty terms to the likelihood function to handle high-dimensional covariate spaces: β̂ = argminβ { -l(β | A, X) + λΣ|β_j| } where l(β | A, X) is the log-likelihood function and λ is the tuning parameter that controls the strength of the penalty. LASSO performs both variable selection and shrinkage, making it particularly useful when dealing with numerous potential confounders. Simulation studies have shown that LASSO performs well in linear settings with small sample sizes and common treatment prevalence [38].
Machine Learning Approaches
Machine learning methods offer flexible alternatives to traditional logistic regression, particularly for capturing complex relationships in high-dimensional data. The following table summarizes key machine learning approaches for propensity score estimation:
Table 1: Machine Learning Methods for Propensity Score Estimation
| Method | Key Mechanism | Advantages | Limitations | Performance Characteristics |
|---|---|---|---|---|
| LASSO | L1 regularization with variable selection | Automatic variable selection, handles correlated predictors | Shrinks coefficients toward zero, may exclude weak predictors | Best in linear settings with small samples and common treatment prevalence [38] |
| XgBoost | Gradient boosted decision trees | Captures complex nonlinearities and interactions, robust to outliers | Computationally intensive, requires careful tuning | Outperforms in nonlinear settings with large samples and low treatment prevalence [38] [39] |
| Multilayer Perceptron (MLP) | Neural network with multiple hidden layers | Models complex nonlinear relationships, handles high-dimensional data | Requires extensive tuning, prone to overfitting without proper validation | Performs similarly to other ML methods in complex data scenarios [38] |
Model Averaging and Hybrid Approaches
Model averaging approaches integrate multiple propensity score estimates to improve robustness against model misspecification. The model-averaged propensity score is calculated as: ē(Xi) = Σλm êm(Xi) where λm are mixing parameters that sum to 1, and êm(X_i) represents the propensity score estimate from candidate model m.
Recent methodological developments have introduced prognostic score-based model averaging, which selects the optimal mixing parameters by minimizing between-group differences in prognostic scores (predicted outcomes under control) rather than focusing solely on covariate balance. This approach recognizes that imbalance in prognostic scores is more strongly associated with bias in treatment effect estimates than imbalance in individual covariates. Simulation studies demonstrate that this method consistently yields lower bias and less variability in treatment effect estimates across various scenarios [40].
Practical Implementation Protocol
Step-by-Step Estimation Procedure
The following workflow diagram illustrates the comprehensive process for propensity score estimation and application:
Diagram 1: Propensity Score Analysis Workflow
Step 1: Define the Causal Question and Target Estimand Clearly specify the treatment comparison, outcome, target population, and causal contrast of interest. Determine whether the target estimand is the average treatment effect in the overall population (ATE), treated population (ATT), or overlap population (ATO). This decision guides the selection of appropriate propensity score methods [41].
Step 2: Assemble the Study Cohort and Define Variables Identify the source population, eligibility criteria, and index dates. Precisely define treatment exposure, outcome, and potential confounders using structured healthcare data. Implement a covariate assessment period preceding treatment initiation to ensure proper temporal ordering.
Step 3: Select Covariates for Inclusion Incorporate covariates that are potential common causes of treatment and outcome. Use clinical knowledge, literature review, and data-driven approaches. Consider using high-dimensional propensity score (hdPS) algorithms when dealing with large-scale healthcare data with numerous potential covariates [42].
Step 4: Estimate Propensity Scores Select an appropriate estimation method based on sample size, treatment prevalence, and data complexity. For conventional analyses, use logistic regression with pre-specified covariates. For high-dimensional data or complex relationships, consider machine learning approaches like LASSO or XgBoost with proper hyperparameter tuning.
Step 5: Evaluate Covariate Balance Assess the success of propensity score estimation by comparing balance between treatment groups before and after adjustment. Use standardized mean differences (aim for <0.1) and variance ratios. Consider incorporating prognostic score balance as an additional metric [40].
Step 6: Estimate Treatment Effects Use the propensity scores to create balanced groups through matching, weighting, or stratification. Estimate the treatment effect in the balanced sample using an appropriate outcome model. For time-to-event outcomes, consider using propensity score adjustment within a nested case-control design to address both immortal time bias and confounding [42].
Step 7: Conduct Sensitivity Analyses Evaluate the robustness of findings to potential unmeasured confounding, model specifications, and methodological choices. Vary propensity score estimation approaches, covariate sets, and balance thresholds to assess consistency of results.
Advanced Considerations for Pharmacoepidemiology
Handling Rare Treatments and Outcomes When treatment prevalence is low (<10%), disease risk scores (DRS) may outperform propensity scores in reducing bias, particularly in nonlinear data settings [38]. DRS represents the probability of the outcome conditional on confounders in the untreated population. In scenarios with very rare treatments, consider using overlap weighting, which naturally focuses on the population with clinical equipoise and avoids extreme weights [41].
Addressing Time-Dependent Confounding and Immortal Time Bias For studies with time-varying exposures, consider implementing propensity score adjustment within a nested case-control framework to simultaneously address immortal time bias and confounding. This approach involves matching cases to controls based on time and then applying propensity score methods to address residual confounding [42].
High-Dimensional Propensity Score Implementation The hdPS algorithm systematically selects and prioritizes covariates from large healthcare databases through seven defined steps: (1) identify data dimensions, (2) identify candidate covariates, (3) assess recurrence, (4) assign priorities, (5) select covariates, (6) estimate propensity scores, and (7) evaluate balance. For time-to-event outcomes, LASSO prioritization may outperform the traditional Bross formula for covariate selection [42].
Performance Evaluation and Validation
Comparative Performance Across Scenarios
Simulation studies provide valuable insights into the relative performance of different propensity score estimation methods under various data conditions. The following table summarizes evidence-based recommendations based on comprehensive simulation studies:
Table 2: Method Selection Guide Based on Data Scenarios
| Data Scenario | Recommended PS Method | Recommended Estimation Approach | Evidence |
|---|---|---|---|
| Low treatment prevalence (<0.1) | Disease Risk Score (DRS) | XgBoost for nonlinear data | DRS shows lower bias than PS when treatment prevalence is below 0.1, especially in nonlinear data [38] |
| Moderate-high treatment prevalence (0.1-0.5) | Propensity Score | Logistic regression or LASSO | PS has comparable or lower bias than DRS in this range [38] |
| Linear data with small samples | Propensity Score | LASSO or logistic regression | DRS does not outperform PS in linear or small sample data [38] |
| High-dimensional covariates | Propensity Score | LASSO or hdPS | ML methods can outperform logistic regression for PS estimation [38] [42] |
| Focus on clinical equipoise population | Overlap Weighting | Logistic regression with overlap weights | Overlap weighting targets ATO with bounded weights and exact balance [41] |
Balance Metrics and Diagnostics
Comprehensive balance assessment should include both traditional covariate balance metrics and prognostic score balance. The absolute standardized mean difference (ASMD) for each covariate j is calculated as: ASMDj = |X̄j,treatment - X̄j,control| / σj,treatment where X̄j,treatment and X̄j,control are the sample means of covariate j in the treatment and control groups, and σ_j,treatment is the standard deviation in the treatment group. The mean ASMD across all covariates provides a summary measure of overall balance.
Prognostic score balance assessment involves calculating the ASMD for the predicted outcomes under control: ASMDPS = |Ȳ̂treatment - Ȳ̂control| / σŶ,treatment where Ȳ̂treatment and Ȳ̂control are the mean prognostic scores in the treatment and control groups. Research has demonstrated that imbalance in prognostic scores is more strongly associated with bias in treatment effect estimates than imbalance in individual covariates [40].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Methodological Tools for Propensity Score Analysis
| Tool Category | Specific Methods/Software | Application Context | Implementation Considerations |
|---|---|---|---|
| Statistical Software | R (cobalt, MatchIt, glmnet), Python (sklearn, causalinference), SAS (PROC PSMATCH) | General implementation | R provides the most comprehensive set of specialized packages for propensity score analysis and balance diagnostics |
| Machine Learning Libraries | XgBoost, scikit-learn, mlr3 | High-dimensional data, complex relationships | Require careful hyperparameter tuning; default settings often suboptimal [39] |
| High-Dimensional PS Algorithms | hdPS package in R | Healthcare claims data with numerous potential covariates | Implements 7-step algorithm for automated covariate selection and prioritization [42] |
| Balance Metrics | Absolute Standardized Mean Difference (ASMD), Kolmogorov-Smirnov statistic, Prognostic score difference | Evaluating covariate balance | Prognostic score balance more directly related to bias in effect estimates [40] |
| Sensitivity Analysis Methods | E-value, Rosenbaum bounds, Unmeasured confounder models | Assessing robustness to unmeasured confounding | E-value increasingly recommended for reporting in pharmacoepidemiological studies |
| WWL154 | 4-Nitrophenyl 4-(4-Methoxyphenyl)piperazine-1-carboxylate | Research chemical 4-Nitrophenyl 4-(4-Methoxyphenyl)piperazine-1-carboxylate (CAS 1338574-93-8). For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
| Venlafaxine-d6 | Venlafaxine-d6 Stable Isotope - 940297-06-3 | Venlafaxine-d6 internal standard for bioanalysis. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
Propensity score methods represent a powerful approach for addressing confounding in pharmacoepidemiological studies, but their successful implementation requires careful attention to model specification, covariate selection, and balance assessment. This guide has outlined a structured framework for propensity score estimation that incorporates both established practices and recent methodological innovations. As the field evolves, researchers should consider scenario-specific recommendations, particularly regarding the choice between propensity scores and disease risk scores based on treatment prevalence, and the integration of machine learning methods for complex data environments. Most importantly, methodological decisions should be guided by the causal question of interest, with transparent reporting of all analytical choices and their potential limitations.
In pharmacoepidemiological studies, researchers are often faced with the challenge of using observational data to estimate the effects of treatments, interventions, and exposures on patient outcomes. Unlike randomized controlled trials (RCTs)—considered the gold standard for estimating treatment effects—observational studies involve treatment assignments that are nonrandom processes, often influenced by patient characteristics [10]. This leads to systematic differences in baseline characteristics between treated and untreated subjects, a phenomenon known as confounding [10] [43]. Propensity score (PS) methods have emerged as a powerful set of statistical tools to achieve comparability between treatment groups in terms of their observed covariates, thereby controlling for confounding in the estimation of treatment effects [43].
The propensity score, defined as the probability of treatment assignment conditional on a subject's observed baseline covariates, serves as a balancing score [10]. Conditional on the propensity score, the distribution of observed baseline covariates is expected to be similar between treated and untreated subjects, allowing the estimation of treatment effects in a way that mimics some of the key characteristics of an RCT [10]. This article provides a detailed comparison of the four primary propensity score methods—matching, stratification, inverse probability of treatment weighting (IPTW), and covariate adjustment—within the context of pharmacoepidemiological research, offering application notes and experimental protocols for implementation.
Theoretical Framework and Key Concepts
The Potential Outcomes Model and Causal Inference
The theoretical foundation for propensity score methods rests on the potential outcomes framework (also known as the Rubin Causal Model) [10]. In this framework, each subject has a pair of potential outcomes: the outcome under the active treatment, Y(1), and the outcome under the control treatment, Y(0). However, only one of these outcomes is observed for each subject, depending on the actual treatment received. The individual treatment effect is defined as Y(1) - Y(0), but this cannot be directly calculated [10].
Instead, researchers focus on aggregate measures, primarily the Average Treatment Effect (ATE), defined as E[Y(1) - Y(0)] across the entire population, and the Average Treatment Effect on the Treated (ATT), defined as E[Y(1) - Y(0)|Z=1], which is the average effect for those who actually received the treatment [10]. In randomized controlled trials, these measures coincide due to random assignment, but in observational studies, they generally differ, and the researcher must decide which is more relevant to their research question [10].
The Propensity Score and Strong Ignorability
The propensity score, formally defined as e = P(Z=1|X), where Z is the treatment indicator and X is a vector of observed covariates, allows for unbiased estimation of treatment effects under the strong ignorability assumption [10]. This assumption requires that: (1) treatment assignment is independent of potential outcomes conditional on observed covariates (Y(0), Y(1)) â•© Z|X (the "no unmeasured confounders" assumption), and (2) every subject has a nonzero probability of receiving either treatment (0 < P(Z=1|X) < 1) [10]. When these conditions are met, conditioning on the propensity score enables the estimation of unbiased average treatment effects.
Estimation of the Propensity Score
In practice, the true propensity score is unknown and must be estimated from the data, most commonly using logistic regression where treatment status is regressed on observed baseline characteristics [10]. The predicted probabilities from this model serve as the estimated propensity scores. While logistic regression remains the most frequently used method, alternative approaches include machine learning techniques such as bagging, boosting, recursive partitioning, random forests, and neural networks, which may offer advantages, particularly in high-dimensional settings [10] [4].
Table 1: Propensity Score Estimation Methods
| Method | Description | Best Use Cases |
|---|---|---|
| Logistic Regression | Traditional generalized linear model with logit link function | Standard settings with limited covariates; requires manual specification of interactions and nonlinear terms |
| High-Dimensional Propensity Score (hdPS) | Automated algorithm for covariate selection and model specification in databases with many potential covariates | Pharmacoepidemiological studies using claims data with large number of diagnosis, procedure, and prescription codes |
| Machine Learning Methods (e.g., boosting, random forests) | Data-adaptive algorithms that can capture complex relationships without manual specification | High-dimensional data; complex confounding patterns; large sample sizes |
| Dimensionality Reduction Techniques (e.g., PCA, autoencoders) | Projects high-dimensional covariate space into lower-dimensional representation | Situations with extreme high-dimensionality where traditional methods may overfit |
Recent research has explored dimensionality reduction techniques such as principal component analysis (PCA), logistic PCA, and autoencoders for propensity score estimation in high-dimensional data, such as healthcare claims databases [4]. These approaches have demonstrated superior performance in achieving covariate balance compared to traditional methods in some applications, with autoencoder-based propensity scores showing particular promise [4].
Comparative Analysis of Propensity Score Methods
Four primary propensity score methods are commonly used to remove the effects of confounding in observational studies: propensity score matching, stratification on the propensity score, inverse probability of treatment weighting (IPTW), and covariate adjustment using the propensity score [10]. Each method employs the propensity score differently to create conditions under which treatment effects can be validly estimated.
Performance Comparison Across Study Designs
Evaluations of these methods in real-world scenarios provide critical insights for method selection. A comparison using datasets from four large-scale cardiovascular observational studies found that the performance of these methods varies considerably depending on study characteristics [44].
Table 2: Comparative Performance of Propensity Score Methods Based on Cardiovascular Studies
| Method | Performance Characteristics | Key Limitations | Recommended Context |
|---|---|---|---|
| Matching | Produced good balance; comparable estimates to covariate adjustment | Tended to give less precise estimates in some cases; reduces sample size | When ATT is of interest; sufficient overlap between treatment groups |
| Stratification | Performed poorly with few outcome events | Increased bias with limited events; suboptimal balance within strata | Large studies with ample outcome events across all strata |
| Inverse Probability Weighting (IPTW) | Gave imprecise estimates; undue influence to small number of observations | Unstable with substantial confounding; extreme weights problematic | When ATE is of interest; well-specified propensity score model |
| Covariate Adjustment | Performed well across all examples; precise estimates | Relies on correct model specification for both PS and outcome | General purpose application; requires careful model checking |
This comparative analysis suggests that propensity score methods are not necessarily superior to conventional covariate adjustment, and care should be taken to select the most suitable method for a given research context [44]. The performance depends on factors such as sample size, prevalence of the outcome, degree of confounding, and overlap between treatment groups.
Application Protocols for Pharmacoepidemiology
Standardized Workflow for Propensity Score Analysis
Implementing propensity score methods requires a systematic approach to ensure valid and reproducible results. The following workflow outlines the key steps in a comprehensive propensity score analysis:
Figure 1. Standardized workflow for conducting a propensity score analysis in pharmacoepidemiological studies.
Protocol 1: Propensity Score Matching
Purpose: To create a matched sample where treated and untreated subjects have similar distributions of observed covariates by matching each treated subject to one or more untreated subjects with similar propensity scores.
Procedures:
- Estimate propensity scores using an appropriate method (e.g., logistic regression including all pre-specified covariates)
- Choose matching algorithm: Nearest-neighbor matching (with or without caliper), optimal matching, or genetic matching
- Set matching parameters: Typically a caliper width of 0.2 standard deviations of the logit of the propensity score is recommended
- Execute matching without replacement to maximize statistical precision or with replacement to improve balance
- Assess matching performance by comparing covariate balance before and after matching using standardized mean differences (target <0.1) and variance ratios
- Analyze matched sample using appropriate statistical methods (e.g., paired t-tests for continuous outcomes, conditional logistic regression for binary outcomes)
Considerations:
- Most appropriate when the ATT is the causal contrast of interest
- Matching on the logit of the propensity score often improves performance
- Always report the number of treated subjects matched and the resulting effective sample size
Protocol 2: Stratification on the Propensity Score
Purpose: To divide the study population into strata (typically quintiles) based on the propensity score and then estimate treatment effects within each stratum before pooling.
Procedures:
- Estimate propensity scores for all subjects
- Create strata based on propensity score quantiles (typically 5 strata)
- Assess balance within each stratum to ensure covariates are balanced between treatment groups
- Check outcome events within each stratum to ensure adequate numbers for stable estimation
- Estimate stratum-specific treatment effects using outcome models appropriate for the data type
- Pool stratum-specific estimates to obtain an overall treatment effect estimate
Considerations:
- Performance deteriorates with few outcome events per stratum [44]
- May not completely eliminate confounding within strata if propensity score distributions differ substantially
- Generally requires regression adjustment within strata to address residual confounding
Protocol 3: Inverse Probability of Treatment Weighting (IPTW)
Purpose: To create a pseudo-population in which treatment assignment is independent of observed covariates by weighting subjects by the inverse probability of receiving their actual treatment.
Procedures:
- Estimate propensity scores for all subjects
- Calculate weights: For treated subjects, weight = 1/PS; for untreated subjects, weight = 1/(1-PS)
- Assess weight distribution: Identify extreme weights that may indicate poor overlap or model misspecification
- Consider stabilized weights to improve efficiency: For treated subjects, stabilized weight = P(Z=1)/PS; for untreated subjects, stabilized weight = P(Z=0)/(1-PS)
- Evaluate balance in the weighted sample using standardized mean differences
- Analyze weighted data using appropriate weighted regression models
Considerations:
- Can produce imprecise estimates and give undue influence to observations with extreme weights when substantial confounding is present [44]
- Primarily estimates the ATE rather than ATT
- Weight truncation may be necessary to handle extreme weights
Protocol 4: Covariate Adjustment Using the Propensity Score
Purpose: To control for confounding by including the propensity score as a covariate in the outcome regression model.
Procedures:
- Estimate propensity scores for all subjects
- Specify outcome model that includes both treatment assignment and the propensity score as covariates
- Consider functional form of the propensity score in the model (linear, quadratic, restricted cubic splines)
- Check model assumptions for the outcome regression (linearity, homoscedasticity, etc.)
- Estimate treatment effect from the outcome model
Considerations:
- Performed well across various scenarios in comparative studies [44]
- Requires correct specification of both the propensity score model and the outcome model
- Simpler implementation than other methods but provides less transparent balancing of covariates
Advanced Applications in Pharmacoepidemiology
High-Dimensional Propensity Scores in Claims Data
Pharmacoepidemiological studies frequently utilize administrative claims data, which contain hundreds of potential covariates in the form of diagnosis codes, procedure codes, and prescription records. The high-dimensional propensity score (hdPS) algorithm was developed specifically to address the challenges of such data environments [4] [6]. This algorithm automates the process of covariate selection and prioritization by identifying and selecting the most prevalent and imbalanced codes across a large number of candidate covariates.
A recent application in a study of disease-modifying drugs in multiple sclerosis implemented hdPS within a nested case-control framework to simultaneously address both immortal time bias and residual confounding [6]. This approach demonstrated a 28% reduction in mortality risk associated with exposure to DMDs (HR: 0.72, 95% CI: 0.62-0.84), with consistent results across sensitivity analyses [6].
Dimensionality Reduction Techniques
Emerging methodologies for handling high-dimensional covariates include dimensionality reduction techniques such as principal component analysis (PCA), logistic PCA, and autoencoders [4]. In a comparative study evaluating the association between dialysis and mortality in older heart failure patients, autoencoder-based propensity scores achieved superior covariate balance compared to traditional methods:
Table 3: Performance of Dimensionality Reduction Techniques for PS Estimation
| Method | Covariates with SMD > 0.1 | Balance Performance |
|---|---|---|
| Autoencoder-based PS | 8 | Best |
| PCA-based PS | 20 | Good |
| Logistic PCA-based PS | 25 | Moderate |
| High-Dimensional PS (hdPS) | 37 | Fair |
| Investigator-Specified PS | 83 | Poor |
These advanced methods may offer improved covariate balance in pharmacoepidemiological studies using propensity score-matched designs in large healthcare databases [4].
The Researcher's Toolkit: Essential Components for PS Analysis
Software and Computational Tools
Implementing propensity score analyses requires appropriate statistical software and packages. While many software environments support basic propensity score methods, specialized packages offer enhanced functionality:
- R: The
MatchIt,optmatch,WeightIt, andCBPSpackages provide comprehensive implementations of various propensity score methods - SAS: PROC PSMATCH and related procedures offer robust propensity score analysis capabilities
- Stata:
teffects psmatch,psmatch2, andpscorecommands facilitate propensity score estimation and application - Python: The
causalinference,psmpy, anddowhylibraries offer growing support for propensity score methods
Balance Assessment and Diagnostics
A critical step in any propensity score analysis is assessing whether the propensity score model has been adequately specified to achieve balance in observed covariates between treatment groups [10]. Key diagnostics include:
- Standardized mean differences (SMD): Absolute values <0.1 indicate adequate balance for a covariate
- Variance ratios: Values between 0.5 and 2 generally indicate acceptable balance
- Visual assessments: Love plots, jitter plots, and distributional comparisons
- Statistical tests: Kolmogorov-Smirnov tests for distributional differences
Recent methodological developments emphasize the superiority of balance diagnostics over traditional goodness-of-fit measures for propensity model selection [10]. The goal is not to maximize prediction of treatment assignment but to achieve balance in covariate distributions between treatment groups.
Propensity score methods offer powerful approaches for controlling confounding in pharmacoepidemiological studies, each with distinct strengths, limitations, and appropriate applications. Based on current evidence, no single method dominates across all scenarios, and method selection should be guided by study objectives, data characteristics, and the specific causal contrast of interest [44]. Covariate adjustment using the propensity score and matching generally perform well across diverse scenarios, while stratification and IPTW require more specific conditions for optimal performance [44].
Emerging methodologies, particularly those addressing high-dimensional confounding in claims data, continue to enhance the applicability of propensity score methods in pharmacoepidemiology [4] [6]. Regardless of the specific method chosen, rigorous implementation following established protocols—including thoughtful covariate selection, careful balance assessment, and comprehensive sensitivity analyses—remains essential for producing valid and reliable evidence from observational studies in clinical nutrition and pharmacoepidemiological research [43].
In pharmacoepidemiology, accurate estimation of treatment effects using real-world data is fundamentally challenged by confounding bias. The high-dimensional propensity score (hdPS) addresses this by automating the selection and adjustment for hundreds of candidate covariates from healthcare databases such as administrative claims and electronic health records (EHRs) [45]. This method empirically identifies and prioritizes proxy variables for unmeasured or poorly measured confounders, moving beyond the limitations of investigator-specified covariate sets alone [45] [46]. The growing complexity and volume of real-world data have spurred the integration of machine learning (ML) techniques with the hdPS framework, enhancing its ability to manage high-dimensional data and uncover complex relationships [46]. This document details advanced protocols for implementing hdPS and machine learning for covariate selection, providing researchers and drug development professionals with practical tools for robust comparative effectiveness and safety research.
Background and Theoretical Foundations
The traditional propensity score, defined as the probability of treatment assignment conditional on observed covariates, relies on investigator-specified variables chosen from domain knowledge [46]. This approach may omit crucial confounders, particularly those that are unmeasured or imperfectly captured. The hdPS algorithm, introduced in 2009, builds upon this by conceptualizing information in healthcare databases as proxies for underlying clinical constructs [45] [47]. It is a semi-automated, data-driven procedure that systematically generates and ranks a large number of covariates from predefined data dimensions (e.g., diagnoses, drug prescriptions, procedures) [45] [48].
A key conceptual advantage of hdPS is its use of proxy measure adjustment. For confounders like frailty that are difficult to measure directly, hdPS can leverage proxies such as the use of a wheelchair or oxygen canisters, which are correlated with the underlying confounder [45]. By automatically identifying and incorporating such proxies, hdPS aims to improve confounding control beyond what is possible with traditional methods [45] [47]. The method is data source-independent and has been successfully applied across diverse healthcare systems, including those in North America, Europe, and Japan [45].
Comparative Performance of hdPS and Machine Learning Methods
Recent research has systematically evaluated the performance of traditional hdPS against various multivariate statistical and machine learning methods within the hdPS framework. Performance varies based on epidemiological scenarios, such as the prevalence of exposure and outcome, and the choice of metric (e.g., bias, Mean Squared Error (MSE), or coverage) [46].
The table below summarizes the comparative performance of different methods based on a plasmode simulation study using real-world data structure [46].
Table 1: Performance Comparison of Variable Selection Methods within the hdPS Framework
| Method | Key Strengths | Key Limitations | Ideal Use Case |
|---|---|---|---|
| Bross-based hdPS | Low bias, balanced approach, well-established [46]. | May miss complex variable interactions [46]. | Standard applications prioritizing bias minimization. |
| Hybrid hdPS | Balanced bias and MSE, combines strengths of different approaches [46]. | Coverage can vary by scenario [46]. | Scenarios seeking a robust balance between bias and precision. |
| XGBoost | Strong precision, good coverage, handles complex patterns [46]. | Higher bias, especially with rare exposures; "black-box" [46]. | Applications where precision is the primary goal. |
| LASSO / Elastic Net | Effective in high-dimensional settings, automatic variable selection [46]. | Performance can be outperformed by other ML methods [46]. | High-dimensional data with many correlated covariates. |
| Genetic Algorithm (GA) | Automates model selection [46]. | Consistently high bias and MSE; least reliable [46]. | Not generally recommended based on current evidence. |
| Forward/Backward Selection | Low bias, comparable coverage to sophisticated ML, computationally efficient [46]. | May not capture all complex relationships [46]. | Computationally efficient alternative with good bias control. |
| Nonan-1-ol-d4 | Nonan-1-ol-d4, MF:C9H20O, MW:148.28 g/mol | Chemical Reagent | Bench Chemicals |
| Nadolol D9 | Nadolol D9, MF:C17H27NO4, MW:318.46 g/mol | Chemical Reagent | Bench Chemicals |
The findings indicate no single method dominates all others. The choice depends on study priorities: XGBoost is effective for precision, while Bross-based hdPS and traditional forward/backward selection are better for minimizing bias [46]. Simpler methods often provide a viable, computationally efficient alternative to complex ML models [46].
Detailed Experimental Protocols
Protocol 1: Implementing the Standard hdPS Algorithm
This protocol outlines the five core steps of the standard hdPS implementation, which requires careful pre-specification of parameters in the study protocol and statistical analysis plan [45] [47].
Table 2: Key Decisions for Standard hdPS Implementation
| Step | Decision Point | Options & Recommendations |
|---|---|---|
| 1. Specify Data Dimensions | Identify types of patient data for variable generation. | Typical dimensions: diagnoses, procedures, drug prescriptions. Report each dimension and its clinical aspect [45] [47]. |
| 2. Generate Pre-exposure Features | Define code granularity and apply prevalence filter. | Truncate codes (e.g., 3-digit ICD-10). Select top 200 most prevalent codes per dimension. Justify granularity and filter use [47]. |
| 3. Assess Feature Recurrence | Create binary indicators for frequency. | Standard: indicators for ≥once, ≥median, ≥75th percentile. Can consider proximity to exposure start. Report chosen cut-offs [47]. |
| 4. Prioritize Covariates | Select ranking method for variable selection. | Default: Bross formula (exposure- and outcome-associated). For rare outcomes: exposure-based ranking. Report method used [46] [47]. |
| 5. Select Covariates & Estimate PS | Determine number of hdPS variables and PS model. | Typical: top 200-500 hdPS variables. Combine with investigator-specified confounders in logistic regression. Report final variable count and software [45] [48] [47]. |
Protocol 2: Integrating Machine Learning for Covariate Prioritization
This protocol modifies Step 4 of the standard hdPS, replacing the Bross formula with an ML-based prioritization to capture complex, multivariate relationships [46].
Procedure:
- Input Data Preparation: Follow Steps 1-3 of Protocol 1 to generate the pool of candidate binary covariates. Combine this pool with the investigator-specified covariates.
- Model Training for Prioritization: Instead of univariate Bross scores, use a machine learning algorithm to predict the exposure (treatment). Algorithms such as LASSO, Elastic Net, or XGBoost are suitable as they perform built-in variable selection or importance ranking [46].
- Variable Ranking: Rank all covariates based on the variable importance metric from the trained ML model (e.g., coefficient magnitude in LASSO/Elastic Net, or gain in XGBoost).
- Covariate Selection: Select the top k covariates from the ML-based ranking. The value of k can be determined via cross-validation aimed at optimizing the model's predictive performance or set to a predefined number (e.g., 500) for consistency [46].
- Propensity Score Estimation: Use the selected covariates in a logistic regression model to estimate the propensity score. Alternatively, the predicted probabilities from the ML model itself can be used as the propensity score, though this may complicate variance estimation [46].
Protocol 3: A Hybrid hdPS-ML Workflow
A robust approach combines the data-driven covariate generation of hdPS with the multivariate selection capabilities of ML, followed by a final PS estimation using traditional regression.
Procedure:
- Initial Covariate Screening: Execute Steps 1-4 of the standard hdPS protocol (Protocol 1) to generate a prioritized list of, for example, 1000 candidate covariates using the Bross formula.
- Refined ML Selection: Input the pre-selected 1000 covariates into a machine learning algorithm with variable selection properties, such as LASSO or Elastic Net. Use the outcome variable (not the exposure) as the response in this ML model to identify a subset of covariates most predictive of the outcome from the hdPS-prescreened set [46].
- Final Model Specification: Create the final set for PS estimation by combining:
- All investigator-specified covariates (deemed essential based on subject-matter knowledge).
- The subset of hdPS-derived covariates selected by the ML model in the previous step.
- Estimate Propensity Score: Estimate the propensity score using a logistic regression model with the final covariate set from Step 3. This "doubly refined" approach leverages the strengths of both hdPS and ML while maintaining the interpretability of a parametric PS model [46].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Software and Analytical Tools for hdPS and ML Implementation
| Tool Name | Category | Function & Application |
|---|---|---|
| R hdPS Package [47] | Software Package | Implements the core hdPS algorithm in R for automated covariate identification and prioritization from data dimensions. |
| SAS hdPS Macro [47] | Software Package | Provides a SAS macro for implementing the hdPS procedure within the SAS analytics environment. |
| Aetion Platform | Software Platform | A commercial platform that incorporates hdPS capabilities for rapid-cycle analytics on real-world evidence. |
| XGBoost [46] | ML Library | A gradient boosting framework that provides high precision in variable selection and can be integrated for hdPS covariate prioritization. |
| glmnet [46] | ML Library | A software library for fitting LASSO and Elastic Net models, useful for multivariate variable selection within the hdPS covariate pool. |
| Glyceryl tri(hexadecanoate-2,2-D2) | Glyceryl tri(hexadecanoate-2,2-D2), CAS:241157-06-2, MF:C51H98O6, MW:813.4 g/mol | Chemical Reagent |
| N-Octadecyl-D37 alcohol | N-Octadecyl-D37 alcohol, MF:C18H38O, MW:307.7 g/mol | Chemical Reagent |
Workflow Visualization and Diagnostics
hdPS and Machine Learning Integration Workflow
The following diagram illustrates the core steps and decision points in a generalized hdPS workflow, highlighting where machine learning can be integrated.
Essential Diagnostic and Reporting Checklist
Transparent reporting and rigorous diagnostics are critical for validating hdPS analyses and combating "black-box" criticisms [47]. The following checklist synthesizes key reporting items and diagnostic tools.
Table 4: hdPS Reporting Checklist and Diagnostic Tools
| Reporting Item | Description | Diagnostic Tool / Action |
|---|---|---|
| Data Dimensions | Clearly list all data dimensions used. | Report the aspect of care each dimension captures and coding systems used [47]. |
| Covariate Prioritization | Specify the method used for ranking. | State whether Bross, ML, or other method was used and justify the choice [47]. |
| Covariate Count | Report the number of hdPS variables selected. | Justify the chosen number (e.g., 500) and conduct sensitivity by varying this number (e.g., k=200, 500) [48] [47]. |
| Balance Diagnostics | Assess the reduction in confounding. | Create a "Table 1" to compare baseline characteristics before and after PS adjustment. Report standardized mean differences [45] [47]. |
| Software | Document the software used. | Name the specific software package (R, SAS, Aetion) and version [47]. |
| Sensitivity Analyses | Evaluate robustness of findings. | Vary key parameters (e.g., number of hdPS covariates) and assess impact on treatment effect estimate [47]. |
Pharmacoepidemiologic studies investigating the effects of time-dependent drug exposures on rare outcomes face significant methodological challenges. Two predominant issues are immortal time bias and residual confounding, which can severely distort effect estimates if not properly addressed [6]. The nested case-control (NCC) design offers an efficient framework for studying rare events within established cohorts, while propensity score (PS) methods provide powerful approaches to control for confounding. However, traditional PS methods treat exposure as a binary, time-fixed variable, which is often misaligned with real-world clinical practice where treatments are initiated and modified at different times during patient follow-up [49].
This integration of time-dependent PS methods within NCC designs represents a significant methodological advancement for addressing complex exposure scenarios in pharmacoepidemiology. The hybrid "NCC-hdPS" approach (incorporating high-dimensional propensity scores) has recently demonstrated utility in simultaneously dealing with both immortal time bias and residual confounding, substantially improving the validity of causal effect estimates from observational data [6]. These developments are particularly relevant within modern pharmacoepidemiologic frameworks such as the ICH E9(R1) estimand framework, which emphasizes precise definition of treatment effects despite intercurrent events [50].
Methodological Foundations
The Nested Case-Control Design
The nested case-control study incorporates the strengths of both cohort and case-control designs by embedding case-control methodology within an established prospective cohort [51] [52]. In this design, all cases of the outcome event are identified from the cohort, and for each case, a small number of controls are randomly selected from those cohort members who remain at risk at the time of the case's event (the risk set) [52]. This approach has several key advantages over standard case-control designs:
- Same population source: Cases and controls are sampled from the same underlying population, minimizing selection bias [52]
- Temporal clarity: Exposure status is ascertained prior to the outcome event, preserving causal interpretation [52]
- Efficiency: Particularly valuable when exposure assessment is costly or labor-intensive [51]
- Time-matching: Cases can be matched to controls at the time of the outcome event, addressing time-dependent exposures and confounding [52]
A recent simulation study comparing cohort and NCC designs for time-varying exposures found that once tied event times were correctly accounted for using exact methods, NCC estimates were very similar to those from full cohort analysis, supporting the validity of this approach [53].
Time-Dependent Propensity Scores
Conventional PS methods generate a single probability of treatment assignment for each individual at study entry, ignoring the time-varying nature of many treatments [49]. Time-dependent propensity score methods address this limitation by modeling the probability of treatment initiation at each point in time during follow-up, considering the evolving clinical characteristics of patients [49] [54].
Two primary approaches have been developed for time-dependent PS estimation:
Cox-based PS: Treatment initiation is modeled as a time-to-event process using Cox proportional hazards regression, where the probability of receiving treatment at time t is estimated conditional on not having been treated before time t [49] [54]
Logistic regression with time strata: Treatment status is modeled using logistic regression within specific time windows, creating a piecewise approach to time-dependent confounding [49]
Simulation studies have demonstrated that conventional PS methods ignoring time-to-exposure property introduce significant bias, while time-dependent PS matching can achieve results approaching the true treatment effect [49]. After time-dependent PS matching, the matched cohort can be analyzed with conventional Cox regression or conditional logistic regression models with time strata, performing comparably to correctly specified Cox regression models with time-varying covariates [49].
Integrated Workflow: NCC with Time-Dependent hdPS
The integration of time-dependent high-dimensional propensity score (hdPS) within a nested case-control framework provides a robust approach to address both immortal time bias and residual confounding simultaneously. The workflow can be visualized as follows:
Figure 1: Integrated workflow for nested case-control design with time-dependent propensity score
Protocol for Implementing the Combined Design
Cohort Definition and Risk Set Specification
- Base cohort: Define a retrospective cohort from appropriate data sources (e.g., administrative claims, electronic health records, disease registries) with clearly specified inclusion/exclusion criteria [6] [50]
- Time axis: Establish the time scale for analysis (e.g., time since diagnosis, calendar time, age), with time zero appropriately defined based on the research question [52]
- Risk sets: At each distinct event time, define the risk set as all cohort members who are still under follow-up and have not experienced the event prior to that time [52]
Case and Control Selection
- Case definition: Identify all individuals who experience the outcome event during follow-up [52]
- Control selection: For each case, randomly select controls from the corresponding risk set (typically 3-5 controls per case) using sampling without replacement [6] [52]
- Matching factors: Consider matching on potential confounders (e.g., age, sex, disease severity) and time factors (calendar time, disease duration) to improve efficiency [52]
Time-Dependent hdPS Estimation
- Variable selection: Identify candidate covariates for PS estimation, including baseline characteristics, time-fixed confounders, and time-varying covariates [6]
- Exposure modeling: Model the time to exposure initiation using Cox proportional hazards regression, including all identified covariates as predictors [49] [54]
- PS estimation: For each individual in the risk set, estimate the probability of being exposed at the event time of the case, conditional on not being exposed before that time [49]
Analysis of Matched Sets
- Conditional logistic regression: Analyze the matched case-control sets using conditional logistic regression, conditioning on the matching strata [6] [53]
- Effect estimation: Report hazard ratios with 95% confidence intervals to quantify the association between exposure and outcome [6]
- Sensitivity analyses: Assess robustness of findings using different PS estimation techniques, control-to-case ratios, and methods for handling tied event times [6] [53]
Application in Multiple Sclerosis Research
Case Study: DMDs and Mortality in MS
A recent study applied the integrated NCC-hdPS approach to examine the relationship between disease-modifying drugs (DMDs) and all-cause mortality in multiple sclerosis patients, demonstrating the utility of this methodology [6].
Table 1: Study characteristics and results from MS mortality study using NCC-hdPS design
| Study Component | Details |
|---|---|
| Data Source | Retrospective cohort of 19,360 individuals with MS in British Columbia, Canada |
| Exposure | Disease-modifying drugs (DMDs) for MS |
| Outcome | All-cause mortality |
| NCC Components | 3,209 cases matched to 12,293 controls (1:4 ratio) |
| hdPS Application | High-dimensional propensity score to address residual confounding |
| Primary Result | 28% reduction in mortality risk (HR: 0.72, 95% CI: 0.62-0.84) |
| Sensitivity Analyses | Consistent results across different PS techniques (HR range: 0.70-0.77) |
The implementation successfully addressed both immortal time bias (through the NCC framework) and residual confounding (through hdPS), providing a more valid estimate of the treatment effect than conventional approaches [6].
Simulation Evidence
Simulation studies have quantitatively compared the performance of cohort and NCC designs for estimating time-varying exposure effects:
Table 2: Performance characteristics of cohort versus nested case-control designs for time-varying exposures
| Performance Metric | Cohort Design | Nested Case-Control Design |
|---|---|---|
| Relative Bias | Small | Bias toward null (decreases with more controls) |
| Precision | Greater | Moderate loss of precision |
| Impact of Event Proportion | Minimal | Marked increase in bias with higher event rates |
| Handling of Tied Events | Robust with exact methods | Bias with Breslow's/Efron's methods; reduced with exact method |
| Confounder Control | Multivariable adjustment | Matching on confounders reduces bias |
These simulations confirm that NCC estimates are very similar to full cohort analysis once ties are correctly accounted for, supporting the validity of the NCC design for time-varying exposures [53].
The Scientist's Toolkit
Table 3: Essential methodological tools for implementing NCC with time-dependent PS
| Tool/Resource | Function | Implementation Notes |
|---|---|---|
| TDPSM() Function | Performs time-dependent PS matching [49] | Available R function; iteratively matches treated subjects to at-risk controls across time strata |
| hdPS Algorithm | Automates covariate selection and PS estimation [6] | Identifies candidate covariates from large datasets; requires specification of dimensions and parameters |
| Conditional Logistic Regression | Analyzes matched case-control data | Conditions on matching strata; available in standard statistical packages |
| tmerge() Function | Creates counting process dataset for survival analysis [49] | Expands data into multiple intervals for time-varying exposures and covariates |
| Risk Set Sampling | Selects controls from appropriate population | Must specify sampling with/without replacement and exclusion of cases from own risk set |
| Mahalanobis Distance Matching | Selects controls with similar characteristics [52] | Accounts for correlation between matching factors; useful for collinear variables |
Discussion
Methodological Considerations
The integration of time-dependent PS methods within NCC designs requires careful attention to several methodological aspects. Time scale selection is crucial, as the choice between time-on-study, age, or calendar time can substantially impact results [52]. Control selection strategies must balance statistical efficiency with computational feasibility, with evidence suggesting that increasing the control-to-case ratio to 5:1 or more can reduce bias toward the null [53]. Proper handling of tied event times is essential, as standard approximations (Breslow's, Efron's) can introduce bias, while exact methods perform better [53].
The hdPS component enhances confounding control by incorporating a large number of empirically identified covariates, which is particularly valuable in complex clinical settings with numerous potential confounders [6]. However, this approach requires careful parameter specification and sensitivity analyses to ensure robust findings.
Alignment with Modern Pharmacoepidemiologic Frameworks
The NCC-hdPS approach aligns well with emerging frameworks for observational research. The ICH E9(R1) estimand framework emphasizes precise definition of treatment strategies, intercurrent events, and target populations [50]. The time-dependent PS explicitly addresses the "treatment" attribute by appropriately handling time-varying exposures, while the NCC design's risk set sampling naturally accommodates various strategies for handling intercurrent events.
Similarly, the target trial emulation framework benefits from this integrated approach, as the NCC design embedded within a cohort mirrors the structure of a randomized trial, with cases and controls sampled from a clearly defined study population [50] [52]. The time-dependent PS further strengthens the emulation by ensuring appropriate comparison groups that account for treatment timing.
The integration of time-dependent propensity score methods within nested case-control designs represents a significant methodological advancement for pharmacoepidemiologic studies of time-varying exposures. This hybrid approach simultaneously addresses two major challenges—immortal time bias and residual confounding—that frequently complicate observational drug safety and effectiveness research.
The availability of reproducible code [6] and specialized functions [49] facilitates implementation of these methods, making them increasingly accessible to researchers. As pharmacoepidemiology continues to evolve toward more rigorous causal inference frameworks, this integrated methodology offers a powerful tool for generating valid evidence from real-world data, particularly for studying dynamic treatment regimens and their effects on rare outcomes.
Future methodological development should focus on extending these approaches to more complex exposure patterns (e.g., repeated, intermittent, or cumulative exposures), refining software implementation for computational efficiency, and further integrating with modern causal inference frameworks to enhance the robustness of observational drug safety research.
Propensity score (PS) methods have become a cornerstone in pharmacoepidemiology for addressing confounding bias in non-randomized studies of treatment effectiveness and safety. These methods facilitate the estimation of causal treatment effects from observational data by creating balanced comparison groups, mimicking some properties of randomized controlled trials (RCTs). This application note provides a detailed protocol for the practical implementation of propensity score methods, from initial model building to final treatment effect estimation, specifically tailored for pharmacoepidemiological research.
Theoretical Foundations and Assumptions
Core Concepts
The propensity score is defined as the probability of a study participant being assigned to a treatment group, conditional on their measured baseline covariates [28]. In pharmacoepidemiology, this translates to the probability of receiving a specific drug given patient characteristics, comorbidities, concomitant medications, and other potential confounders. Propensity scores serve as a dimension-reducing balancing score, creating treatment and reference groups with comparable distributions of measured pretreatment covariates [28].
Causal Inference Assumptions
The valid application of propensity score methods rests on several critical assumptions [28] [55]:
- Conditional Ignorability: All common causes of treatment assignment and outcome must be measured and included in the propensity score model.
- Positivity: Every patient must have a non-zero probability of receiving either treatment, formalized as 0 < P(A=1|X=x) < 1 for all x.
- Stable Unit Treatment Value Assumption (SUTVA): The potential outcomes of any unit must not be affected by the treatments assigned to other units.
Table 1: Core Assumptions for Valid Causal Inference with Propensity Scores
| Assumption | Definition | Practical Implication in Pharmacoepidemiology |
|---|---|---|
| Conditional Ignorability | No unmeasured confounding given covariates | All clinically relevant confounders must be measured |
| Positivity | All patients have chance of receiving either treatment | Avoid including patients with absolute contraindications |
| SUTVA | No interference between patients | Treatment of one patient doesn't affect another's outcome |
Propensity Score Workflow: A Step-by-Step Protocol
Study Design and Covariate Selection
The initial phase involves emulating a target trial through careful study design [5]. Implement a new-user design to avoid prevalent user bias by identifying patients at the initiation of treatment. Define a clean period without treatment exposure before cohort entry and ensure all covariates are measured during this baseline period.
Covariate selection should be guided by subject matter knowledge rather than purely algorithmic approaches [28] [56]. Include variables that are risk factors for the outcome and associated with treatment assignment. A recent benchmarking study demonstrated that traditional logistic regression with a priori confounder selection based on clinical knowledge produced estimates that more closely aligned with RCT results compared to machine learning approaches with data-driven variable selection [56].
Table 2: Essential Components of Propensity Score Study Design
| Design Element | Protocol Specification | Rationale |
|---|---|---|
| Population | Define inclusion/exclusion criteria | Ensure clinical homogeneity |
| Treatment Groups | New users of treatments being compared | Avoid prevalent user bias |
| Covariate Assessment | Fixed baseline period before treatment initiation | Ensure proper temporal ordering |
| Outcome Definition | Clearly specified with validated algorithms | Maximize validity of endpoint ascertainment |
Propensity Score Estimation
Estimate the propensity score using an appropriate statistical model. For binary treatments, logistic regression is most common, though machine learning methods are increasingly used:
While machine learning approaches like generalized boosting models have been explored, recent evidence suggests they may not outperform traditional logistic regression and can potentially introduce overadjustment bias when combined with data-driven confounder selection [56].
Propensity Score Application Methods
Choose an appropriate method for implementing the propensity scores:
- Matching: Pair treated and untreated subjects with similar propensity scores using algorithms (e.g., 1:1 nearest-neighbor matching with caliper)
- Stratification: Divide subjects into strata based on propensity score quantiles
- Weighting: Create a pseudo-population using inverse probability of treatment weights
- Covariate adjustment: Include the propensity score as a covariate in outcome models
Recent methodological research supports matching as it most closely approximates the conditions of a randomized experiment [55]. A caliper width of 0.2 times the standard deviation of the logit of the propensity score has been shown to effectively eliminate over 90% of confounding bias [55].
Balance Assessment and Model Refinement
After applying propensity scores, assess covariate balance between treatment groups using standardized mean differences (aim for <0.1) and variance ratios. Visual assessment using love plots is recommended. If imbalance persists, consider refining the propensity score model by adding interaction terms or higher-order terms for continuous variables.
Outcome Analysis
Once adequate balance is achieved, proceed with outcome analysis. In matched designs, use methods that account for the matched nature of the data, such as conditional logistic regression or robust variance estimators. The specific model should be chosen based on the outcome type (e.g., logistic regression for binary outcomes, Cox regression for time-to-event outcomes).
Workflow Visualization
The following diagram illustrates the complete propensity score analysis workflow:
Advanced Applications and Extensions
Multiple Treatment Comparisons
Conventional propensity score methods address binary treatments, but many clinical decisions involve choosing among multiple therapeutic options. The generalized propensity score (GPS) extends the framework to multiple treatments, whether ordinal (e.g., different drug doses) or categorical (e.g., different drug classes) [57]. Research has shown that simple extensions of binary propensity score methods can produce misleading results when applied to multiple treatments, and specialized matching procedures are required [57].
High-Dimensional Covariate Settings
In pharmacoepidemiology utilizing healthcare claims data, researchers often face high-dimensional covariate spaces. The high-dimensional propensity score (hdPS) algorithm provides a systematic approach to empirically identify and adjust for potential confounders from large healthcare databases [5]. However, recent evidence suggests that domain knowledge should guide confounder selection even in high-dimensional settings [56].
Case Study: Cardiovascular Safety of Diabetes Medications
A recent study applied advanced propensity score methods to examine the cardiovascular safety of second-line noninsulin antihyperglycemic treatments added to metformin in type 2 diabetes [57]. Using data from the Clinical Practice Research Datalink (CPRD), researchers compared multiple treatment regimens including metformin plus sulfonylureas, thiazolidinediones, or dipeptidyl peptidase-4 inhibitors.
Implementation Protocol
The analysis employed generalized propensity scores with Mahalanobis distance matching to address the multiple treatment comparisons. The protocol included:
- Population: Adults with type 2 diabetes initiating second-line therapy after metformin
- Covariates: Demographics, comorbidities, concomitant medications, healthcare utilization
- Matching: Fuzzy matching on the generalized propensity score with caliper
- Outcome: Major adverse cardiovascular events (MACE) and mortality over 3 years
Key Findings
The propensity score analysis revealed that metformin plus gliclazide (sulfonylurea) increased the 3-year risk of MACE compared to metformin plus pioglitazone (thiazolidinedione), and increased mortality risk compared to both metformin plus pioglitazone and metformin plus sitagliptin (DPP-4 inhibitor) [57]. These findings demonstrate how propensity score methods can provide clinically relevant comparative effectiveness evidence from observational data.
Table 3: Research Reagent Solutions for Propensity Score Analysis
| Tool Category | Specific Solutions | Application Context |
|---|---|---|
| Statistical Software | R (package: MatchIt), SAS, Stata | Primary analysis platforms |
| Propensity Score Estimation | Logistic regression, Generalized boosting models, Random forests | Model building for treatment probability |
| Balance Assessment | Standardized mean differences, Variance ratios, Love plots | Evaluating covariate balance post-matching |
| Outcome Analysis | Conditional logistic regression, Cox regression with robust variances, G-computation | Treatment effect estimation |
Validation and Sensitivity Analysis
Benchmarking Against RCTs
Whenever possible, validate propensity score analyses against existing RCT evidence. A recent study benchmarking observational analyses using propensity scores against the PARADIGM-HF randomized trial found that traditional logistic regression with clinical knowledge-based confounder selection most closely aligned with trial results [56].
Sensitivity Analysis for Unmeasured Confounding
Conduct sensitivity analyses to quantify how strong an unmeasured confounder would need to be to explain away the observed treatment effect. Methods such as the E-value approach or probabilistic sensitivity analysis should be routinely implemented.
This application note provides a comprehensive protocol for implementing propensity score methods in pharmacoepidemiological research. The workflow emphasizes proper study design, clinically informed covariate selection, rigorous balance assessment, and appropriate outcome analysis. When correctly applied, propensity score methods offer a powerful tool for generating real-world evidence on treatment effects, though they require careful attention to methodological assumptions and limitations. Recent advances in multiple treatment comparisons and high-dimensional confounding adjustment continue to enhance the utility of these methods for drug development and comparative effectiveness research.
Navigating Pitfalls and Enhancing Robustness in PS Analysis
The "Propensity Score Matching (PSM) Paradox," a phenomenon where increased pruning of matched pairs based on propensity score distance reportedly leads to greater covariate imbalance and bias, has sparked considerable debate in pharmacoepidemiologic methodology. This application note examines this paradox through the lens of practical pharmacoepidemiologic research, where large healthcare databases and complex confounding structures present unique challenges. We synthesize recent empirical evidence suggesting that with proper implementation—including appropriate caliper sizes and balance diagnostics—PSM remains a valuable tool for controlling confounding in observational drug safety and effectiveness studies. Detailed protocols for assessing covariate balance and minimizing model dependence are provided to guide researchers in applying robust PSM methodologies.
Propensity score matching has become a cornerstone method in pharmacoepidemiology due to its ability to control for numerous confounders present in healthcare databases such as insurance claims and electronic health records [37] [5]. The method creates balanced comparison groups by matching treated patients with untreated patients with similar probabilities (propensity scores) of receiving the treatment based on observed covariates [58]. However, King and Nielsen (2019) identified what they termed the "PSM Paradox"—the counterintuitive finding that after achieving initial balance, further pruning of matched pairs with the largest propensity score distances can increase rather than decrease covariate imbalance, model dependence, and bias [59] [60].
This paradox has particularly significant implications for pharmacoepidemiologic studies, which often rely on large, complex datasets to evaluate drug safety and effectiveness in real-world populations [61] [62]. Understanding whether this paradox represents a fundamental methodological flaw or a misuse of PSM is crucial for maintaining the validity of evidence generated from observational pharmacoepidemiologic research.
Examining the Contours of the Paradox
Theoretical Mechanism of the Paradox
The PSM paradox arises from a fundamental property of propensity scores: while PSM guarantees balance on the propensity score itself, it only guarantees balance on the underlying covariates asymptotically [59] [61]. In finite samples, particularly those with already good balance, pruning matched pairs based solely on propensity score distance may inadvertently remove pairs that, despite having slightly different propensity scores, are well-matched on actual covariates [59] [60]. This occurs because PSM attempts to approximate a completely randomized experiment rather than a more efficient fully blocked randomized experiment, making it "uniquely blind" to imbalance that could be eliminated by methods that directly balance covariates [60].
Table 1: Key Studies Investigating the PSM Paradox
| Study | Data Source | Key Findings on PSM Paradox |
|---|---|---|
| King & Nielsen (2019) [59] [60] | Political science data; simulations | PSM increases imbalance, model dependence, and bias by approximating completely randomized experiments |
| Wan (2025) [55] [63] | Simulations and analytical formulas | Paradox stems from misuse of imbalance metrics; not a legitimate concern with proper PSM implementation |
| Franklin et al. (2018) [61] | PACE and MAX insurance claims databases | Imbalance sometimes increased after pruning, but standard calipers prevented deterioration of balance |
Empirical Evidence in Pharmacoepidemiologic Settings
Research specifically examining the PSM paradox in pharmacoepidemiologic contexts has yielded nuanced findings. A 2018 study investigated the paradox using two healthcare claims databases: the Pharmaceutical Assistance Contract for the Elderly (PACE) with 49,919 beneficiaries and the Medicaid Analytic eXtract (MAX) with 886,996 completed pregnancies [61]. The authors created multiple 1:1 propensity-score-matched datasets while manipulating key parameters including covariate set richness, exposure prevalence, and matching algorithms.
The findings demonstrated that while covariate imbalance sometimes increased after progressive pruning of matched sets, the application of standard propensity score calipers (typically 0.2 standard deviations of the logit propensity score) consistently stopped pruning near the lowest region of the imbalance trend [61]. This resulted in improved balance compared to the pre-matched data set, leading the authors to conclude that "PSM does not appear to induce increased covariate imbalance when standard propensity score calipers are applied in these types of pharmacoepidemiologic studies" [61].
Essential Methodological Protocols for PSM Implementation
Propensity Score Estimation and Matching Workflow
The following diagram illustrates the comprehensive workflow for proper PSM implementation, emphasizing balance assessment and model refinement:
Balance Assessment Protocol
Comprehensive balance assessment is critical for detecting and addressing the potential PSM paradox. The following protocol should be implemented after initial matching:
Calculate Standardized Mean Differences (SMD): For each covariate, compute SMD before and after matching using the formula:
Continuous variables: SMD = (x̄ₜᵣₑâ‚ₜₑ𒹠- x̄ᶜᵒâ¿áµ—ʳᵒˡ) / √[(s²ₜᵣₑâ‚ₜₑ𒹠+ s²ᶜᵒâ¿áµ—ʳᵒˡ)/2]
Dichotomous variables: SMD = (pₜᵣₑâ‚ₜₑ𒹠- pᶜᵒâ¿áµ—ʳᵒˡ) / √[(pₜᵣₑâ‚ₜₑð’¹(1-pₜᵣₑâ‚ₜₑð’¹) + pᶜᵒâ¿áµ—ʳᵒˡ(1-pᶜᵒâ¿áµ—ʳᵒˡ))/2]
An SMD <0.1 is generally considered indicative of good balance [64].
Evaluate Variance Ratios: For continuous variables, calculate the ratio of variances between treatment groups after matching. A ratio close to 1.0 indicates good balance, with values below 2.0 generally acceptable [64].
Assess Prognostic Scores: Regress the outcome on covariates in the control group only, then use this model to predict outcomes for all subjects (prognostic scores). Compare SMD of prognostic scores between groups, as this measure highly correlates with bias [64].
Visual Inspection: Create Love plots displaying SMD for all covariates before and after matching, and examine distributional balance through density plots for continuous variables and histograms for categorical variables [64].
Table 2: Balance Assessment Metrics and Interpretation
| Metric | Calculation | Interpretation | R Package/Function |
|---|---|---|---|
| Standardized Mean Difference (SMD) | Difference in means divided by pooled standard deviation | <0.1 indicates balance; >0.1 indicates meaningful imbalance | cobalt::bal.tab() |
| Variance Ratio | Ratio of variances in treatment vs control groups | 1.0 indicates perfect balance; <2.0 generally acceptable | cobalt::bal.tab() |
| Prognostic Score SMD | SMD of predicted outcomes under control condition | Correlates highly with bias; lower values preferred | Custom calculation using outcome model |
| Empirical CDF | Difference in cumulative distribution functions | Smaller values indicate better distributional balance | MatchIt::summary() |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Software Tools for PSM Implementation in Pharmacoepidemiology
| Tool/Software | Primary Function | Application in PSM | Key Features |
|---|---|---|---|
| R MatchIt Package [59] [58] | Data preprocessing via matching | Performs various PSM algorithms (nearest neighbor, optimal, full) | Supports multiple distance measures, caliper imposition, and matching with or without replacement |
| R cobalt Package [64] | Covariate balance assessment | Generates balance statistics and Love plots after matching | Computes SMD, variance ratios, and other balance metrics with publication-quality graphics |
| R tableone Package [64] | Descriptive statistics | Creates baseline characteristic tables before and after matching | Automatically calculates SMD for group comparisons appropriate for observational studies |
| High-Dimensional Propensity Score (hdPS) [61] [5] | Automated covariate selection | Identifies potential confounders in large healthcare databases | Uses algorithm to select covariates based on their potential for bias reduction |
Strategic Approaches to Mitigate Paradox Effects
Appropriate Caliper Selection
The PSM paradox primarily manifests when researchers continue pruning matched pairs beyond what is necessary to achieve balance [55]. To prevent this:
- Implement a caliper width of 0.2 standard deviations of the logit propensity score as this has been shown to eliminate over 90% of confounding bias [55] [63]
- Avoid excessively narrow calipers that unnecessarily discard valuable data, particularly when balance has already been achieved
- Use variable ratio calipers when exposure prevalence differs substantially between groups
Model Specification and Refinement
When balance diagnostics indicate residual imbalance, consider these propensity score model refinements:
- Test for and add clinically relevant interaction terms between covariates
- Incorporate non-linear terms for continuous covariates using polynomial or spline functions
- Utilize machine learning algorithms like random forests or generalized boosted models to flexibly estimate propensity scores without strong parametric assumptions [5]
- Employ high-dimensional propensity score algorithms to systematically select covariates from large healthcare databases [61] [5]
Alternative Matching Strategies
When PSM repeatedly produces unsatisfactory balance despite model refinements:
- Consider Mahalanobis distance matching either alone or in combination with propensity scores
- Evaluate coarsened exact matching for key categorical confounders
- Implement full matching or optimal matching to maximize sample size while improving balance
- Use propensity score weighting as a complement or alternative to matching
The PSM paradox represents an important methodological consideration rather than a fatal flaw in propensity score approaches. In pharmacoepidemiologic studies using typical large healthcare databases, proper PSM implementation with appropriate calipers and comprehensive balance assessment effectively controls confounding without succumbing to the paradoxical deterioration of balance [61] [55]. Researchers should view the paradox as a reminder of the importance of rigorous balance diagnostics and thoughtful matching strategy selection rather than as a reason to abandon PSM entirely. When properly implemented with attention to caliper selection, model specification, and balance assessment, PSM remains a valuable method for generating valid evidence on drug safety and effectiveness in real-world populations.
Propensity score matching (PSM) is a cornerstone methodological approach in pharmacoepidemiological studies for mitigating confounding bias in observational treatment comparisons. A fundamental challenge in designing a robust PSM study involves optimizing the matched sample size through strategic decisions regarding caliper width, matching ratios, and pruning techniques. These interconnected choices directly impact the bias-variance trade-off, influencing the precision and validity of resultant treatment effect estimates [65] [66]. This application note provides detailed protocols for optimizing sample size in pharmacoepidemiological research, synthesizing current methodological evidence to guide researchers and drug development professionals.
Key Concepts and Definitions
The propensity score is defined as the probability of treatment assignment conditional on a subject's observed baseline covariates [10]. In practice, the propensity score is frequently estimated using logistic regression, though machine learning methods are increasingly employed [10] [67]. PSM uses these scores to construct a matched sample where treated and untreated subjects have similar covariate distributions, thereby approximating the balance achieved in randomized controlled trials [10].
The optimization challenge centers on the intrinsic relationship between sample size and match quality. Excessively narrow matching criteria may prune too many subjects, reducing statistical power and potentially increasing bias if the pruned sample is non-representative [55] [65]. Conversely, overly broad criteria retain more subjects but can produce poor covariate balance, introducing residual confounding [65]. Strategic implementation of caliper widths, matching ratios, and principled pruning is therefore essential for deriving valid causal inferences from observational data.
Optimization Strategies and Evidence-Based Protocols
Caliper Width Selection
The caliper width defines the maximum permitted distance in propensity scores (or their logit transformation) for a valid match. This parameter represents a critical balance between bias reduction and sample retention.
Evidence-Based Recommendation
Extensive Monte Carlo simulations demonstrate that a caliper width of 0.2 standard deviations of the logit of the propensity score generally optimizes the bias-variance trade-off [65]. This specification eliminates at least 98% of the bias in the crude estimator while maintaining confidence intervals with appropriate coverage rates [65]. This finding holds consistently when estimating differences in means for continuous outcomes and risk differences for binary outcomes [65] [68].
Practical Implementation Protocol
- Estimate Propensity Scores: Fit a logistic regression model with treatment status as the dependent variable and all pre-specified baseline confounders as independent variables.
- Calculate Logit Scores: Transform the predicted probabilities using the logit function:
logit(ps) = ln(ps / (1 - ps)). - Compute Pooled Standard Deviation: Calculate the standard deviation of the logit propensity scores separately for treated and untreated groups, then compute the pooled estimate.
- Apply Caliper: Implement nearest-neighbor matching using the specified caliper width (e.g., 0.2 × pooled SD of logit PS).
For studies comparing three treatment groups, similar principles apply, with matching performed based on multiple propensity scores derived from multinomial logistic regression [68].
Matching Order and Ratio
The matching order in greedy nearest-neighbor algorithms can significantly impact result stability, particularly in small-to-medium samples.
Evidence-Based Recommendation
Avoid random order matching due to its potential for cherry-picking and result instability across multiple analyses [69]. Instead, pre-specify deterministic matching orders. Simulation studies indicate that "lowest to highest" score matching provides superior stability, or researchers can report the median estimate from multiple random matches [69].
Practical Implementation Protocol
- Pre-specify Matching Order: In your statistical analysis plan, specify a non-random matching order ("smallest" for lowest-to-highest).
- Implement 1:1 Matching: Begin with a 1:1 matching ratio without replacement, which is most common in pharmacoepidemiology.
- Consider Variable Ratio: If control subjects are abundant, variable-ratio matching can increase precision while maintaining balance [67].
Pruning and Common Support
Pruning involves excluding subjects lacking suitable matches in the alternative treatment group, thereby defining the region of common support.
Evidence-Based Recommendation
Pruning should be performed judiciously to eliminate only non-overlapping regions of the propensity score distribution [66]. Excessive pruning after initial balance is achieved is unnecessary and can be counterproductive, potentially increasing imbalance and bias—a phenomenon termed the "PSM paradox" [55]. Once balance on baseline covariates is achieved with a reasonable caliper, further narrowing provides no benefit and sacrifices valuable data [55].
Practical Implementation Protocol
- Visualize Propensity Score Distributions: Plot density curves or histograms of propensity scores for treated and untreated groups to identify regions of poor overlap.
- Apply Common Support Restriction: Prune only subjects in the non-overlapping regions of the propensity score distribution.
- Document Pruning Impact: Report the number of subjects excluded due to common support restrictions and compare baseline characteristics between retained and excluded subjects.
Comprehensive Optimization Workflow
The following diagram illustrates the integrated workflow for optimizing sample size in propensity score matching studies:
Comparative Strategies Table
The table below summarizes the key optimization strategies, their impact on sample size, and empirical evidence supporting their implementation:
Table 1: Evidence-Based Strategies for Optimizing Sample Size in Propensity Score Matching
| Strategy | Recommended Specification | Impact on Sample Size | Key Evidence |
|---|---|---|---|
| Caliper Width | 0.2 × SD of logit PS | Eliminates ~98% bias while retaining adequate sample | Austin (2010) [65] |
| Matching Order | Deterministic (lowest to highest) | Reduces cherry-picking & improves stability | Maruo et al. (2025) [69] |
| Pruning Approach | Restrict to common support only | Prevents excessive pruning & PSM paradox | Li et al. (2025) [55] |
| Balance Assessment | Standardized differences < 0.1 | Ensures adequacy of final matched sample | Austin (2011) [10] |
The Scientist's Toolkit
Table 2: Essential Methodological Components for Propensity Score Matching Studies
| Research Component | Function in PSM | Implementation Considerations |
|---|---|---|
| Logistic Regression | Estimates propensity scores | Baseline covariates must be pre-specified; consider machine learning alternatives with high-dimensional data [10] [67] |
| Standardized Differences | Assesses covariate balance | More appropriate than hypothesis tests; target <0.1 for adequate balance [68] |
| Caliper Implementation | Controls match quality | Apply to logit of propensity score; 0.2 SD generally optimal [65] |
| Common Support Restriction | Defines analyzable population | Prune only non-overlapping regions; document excluded subjects [55] [66] |
| Sensitivity Analyses | Assesses unmeasured confounding | Quantifies how strong unmeasured confounder would need to be to alter conclusions [66] |
Optimizing sample size through strategic implementation of caliper width, matching ratios, and pruning techniques is fundamental to deriving valid causal inferences from pharmacoepidemiological studies. The evidence-based protocols presented herein support the use of a 0.2 standard deviation caliper on the logit of the propensity score, deterministic matching orders, and judicious pruning limited to regions of non-overlap. By adhering to these structured approaches, researchers can enhance the robustness, reproducibility, and regulatory acceptance of real-world evidence generated through propensity score matching methods.
Observational studies using real-world data, such as electronic health records (EHR) and insurance claims data, are essential for assessing treatment effectiveness and safety in real-world populations. However, these studies face significant methodological challenges that can compromise the validity of their findings if not properly addressed. Unmeasured confounding, missing data, and complex time-varying treatment patterns represent three fundamental obstacles to obtaining reliable causal inferences in pharmacoepidemiological research. This article explores advanced propensity score methodologies to address these challenges within the broader context of a thesis on advancing propensity score methods in pharmacoepidemiology. We provide structured protocols, quantitative comparisons, and practical implementation guidance to enhance the rigor of observational research in drug development and outcomes research.
Core Methodological Challenges in Pharmacoepidemiology
The Triad of Analytical Challenges
The validity of pharmacoepidemiological studies is frequently threatened by interconnected methodological challenges that can introduce substantial bias in treatment effect estimates. The following table summarizes these key challenges and their implications:
Table 1: Core Methodological Challenges in Pharmacoepidemiological Studies
| Challenge Category | Specific Manifestations | Impact on Validity | Common Data Sources Affected |
|---|---|---|---|
| Unmeasured Confounding | Omitted variables, imperfect measurement, unrecorded patient characteristics | Residual selection bias, distorted treatment effect estimates | All observational data sources |
| Data Missingness | Partially observed confounders, incomplete clinical variables, systematic missing data | Incomplete confounding control, selection bias | EHR (especially lifestyle factors, lab values) |
| Complex Treatment Patterns | Treatment switching, dose escalation, combination therapy, non-adherence | Immortal time bias, time-dependent confounding, informative censoring | Claims data, pharmacy records, EHR |
These challenges are particularly pronounced in studies investigating mental health disorders, where treatment pathways are often complex and multidimensional. For example, studies of major depressive disorder (MDD) have documented numerous treatment patterns including persistence, discontinuation, switching, dose escalation, augmentation, and combination therapy [70]. Similarly, research on post-traumatic stress disorder (PTSD) treatment reveals complex patterns of pharmacotherapy management with frequent modifications [71].
Interrelationships Between Challenges
These methodological challenges often coexist and interact in ways that compound their threat to validity. For instance, missing data on key confounders such as ethnicity or chronic kidney disease stage (which can be missing in over 50% of records in EHR studies) exacerbates problems of unmeasured confounding [72]. Simultaneously, complex treatment patterns over time can introduce immortal time bias if not properly accounted for in the study design [6]. The convergence of these issues requires integrated methodological approaches rather than piecemeal solutions.
Advanced Methodological Approaches
High-Dimensional Propensity Score (hdPS) with Nested Case-Control Design
The integration of hdPS with nested case-control (NCC) designs represents a sophisticated approach to simultaneously address unmeasured confounding and immortal time bias. This method was effectively implemented in a study of disease-modifying drugs (DMDs) for multiple sclerosis and all-cause mortality [6].
Experimental Protocol: hdPS-NCC Implementation
Step 1: Cohort Definition and Follow-up
- Define a retrospective cohort with clear inclusion/exclusion criteria
- Establish baseline period for covariate assessment
- Define follow-up period from index date until outcome occurrence, censoring, or end of study
- Identify all outcome cases (e.g., mortality events) during follow-up
Step 2: Nested Case-Control Sampling
- For each case, randomly select 4-5 controls matched on time-in-study using incidence density sampling
- This sampling approach inherently addresses immortal time bias by ensuring comparable follow-up time between cases and controls
- In the multiple sclerosis application, this resulted in 3,209 cases matched to 12,293 controls [6]
Step 3: High-Dimensional Propensity Score Estimation
- Identify all candidate covariates across five data dimensions: diagnoses, procedures, medications, etc.
- Apply the hdPS algorithm to empirically identify and prioritize covariates based on their potential for confounding
- Select top covariates for inclusion in the propensity score model (typically 100-500 variables)
- Estimate propensity scores using logistic regression including both investigator-specified and empirically-identified covariates
Step 4: Treatment Effect Estimation
- Conduct conditional logistic regression conditioned on the matched sets
- Incorporate the estimated propensity score as either a matching variable or regression covariate
- Calculate hazard ratios with appropriate confidence intervals
Step 5: Sensitivity Analyses
- Vary parameters of the hdPS algorithm (number of covariates, preprocessing preferences)
- Test different matching ratios (1:1, 1:3, 1:4)
- Evaluate robustness of findings across analytical scenarios
In the multiple sclerosis application, this approach demonstrated a 28% reduction in mortality risk associated with DMD exposure (HR: 0.72, 95% CI: 0.62-0.84), with consistent results across sensitivity analyses (HRs: 0.70-0.77) [6].
Workflow Visualization
Missingness Pattern Approach for Partial Confounder Data
The Missingness Pattern Approach (MPA) provides a framework for handling partially observed confounders in propensity score analysis, which is particularly relevant for EHR studies where missing data is common.
Theoretical Foundation
MPA operates by estimating propensity scores separately within each missingness pattern present in the data. Unlike simple missing indicator methods, MPA acknowledges that the mechanism of missingness may be informative and incorporates this information into the analysis. The approach requires that the missingness mechanism is conditionally independent of the outcomes given the observed data and treatment assignment [72].
In a study of angiotensin-converting enzyme inhibitors (ACEI/ARBs) and acute kidney injury, two key confounders had substantial missingness: ethnicity (59.0%) and chronic kidney disease stage (52.9%) [72]. Only 21% of patients had complete data for both variables, making complete-case analysis problematic.
Experimental Protocol: MPA Implementation
Step 1: Missingness Pattern Identification
- Identify all variables with missing values, particularly potential confounders
- Document the proportion missing for each variable
- Create missingness indicator variables for each confounder with missing data
- Identify all unique missingness patterns in the dataset
Step 2: Propensity Score Estimation Within Patterns
- Stratify the analysis by missingness pattern
- Within each pattern, include only the confounders that are observed
- Estimate propensity scores separately within each stratum using the available confounders
- Alternatively, include interaction terms between treatment and missingness indicators in a unified model
Step 3: Treatment Effect Estimation
- Conduct outcome analysis within each missingness pattern
- Pool stratum-specific estimates using appropriate weights (e.g., inverse variance weighting)
- Alternatively, include the propensity score and missingness indicators in the outcome model
Step 4: Assumption Validation
- Evaluate the plausibility of missing-at-random assumptions using causal diagrams
- Assess whether missingness is associated with treatment assignment or outcomes after accounting for observed variables
- Conduct sensitivity analyses to evaluate the impact of potential violations of missingness assumptions
Table 2: Performance Comparison of Missing Data Handling Methods in Propensity Score Analysis
| Method | Key Assumptions | Advantages | Limitations | Suitable Scenarios |
|---|---|---|---|---|
| Complete Case Analysis | Missing completely at random | Simple implementation | Inefficient, potentially biased | <5% missing, MCAR plausible |
| Missing Indicator Method | Missingness independent of outcome | Uses all observations | Can introduce severe bias | Generally not recommended |
| Multiple Imputation | Missing at random | Uses all information, valid uncertainty | Computationally intensive | MAR plausible, multivariate missingness |
| Missingness Pattern Approach (MPA) | Missingness independent of outcome given observed data | Incorporates missingness information | Complex implementation, pattern sparsity | Large samples, informative missingness |
Dimensionality Reduction for Propensity Score Specification in High-Dimensional Data
High-dimensional healthcare data presents both opportunities and challenges for confounding control. While abundant variables enable more complete confounding control, they also increase the risk of model misspecification and finite-sample bias. Dimensionality reduction techniques offer promising approaches to improve propensity score specification in such settings.
Comparative Performance of Dimensionality Reduction Methods
A recent study compared dimensionality reduction techniques for propensity score estimation in claims data analyzing the association between dialysis and mortality in heart failure patients with advanced chronic kidney disease [73]. The study included 485 dialysis-exposed and 1,455 unexposed individuals after matching.
Table 3: Performance Comparison of Dimensionality Reduction Techniques for Propensity Scores
| Method | Covariates with SMD >0.1 | Key Implementation Features | Relative Advantages | Computational Requirements |
|---|---|---|---|---|
| Investigator-Specified | 83 | Domain knowledge-driven selection | Clinical interpretability | Low |
| High-Dimensional Propensity Score (hdPS) | 37 | Algorithmic covariate prioritization | Automated, reproducible | Moderate |
| Principal Component Analysis (PCA) | 20 | Linear dimensionality reduction | Computational efficiency | Moderate |
| Logistic PCA | 25 | Nonlinear dimensionality reduction for binary data | Handles binary features well | High |
| Autoencoders | 8 | Neural network-based representation learning | Optimal balance achievement | Very high |
The study found that autoencoder-based propensity scores achieved superior covariate balance, with only 8 covariates showing standardized mean differences (SMD) > 0.1 compared to 83 for investigator-specified covariates [73]. Despite these differences in balance, hazard ratios for mortality were similar across methods, suggesting that the primary benefit of advanced dimensionality reduction techniques lies in improved covariate balance rather than substantially different effect estimates.
Implementation Protocol: Autoencoder-Based Propensity Scores
Step 1: Data Preprocessing
- Organize high-dimensional covariates into a structured matrix
- Handle missing values using appropriate imputation methods
- Standardize continuous variables to mean 0 and variance 1
- Convert categorical variables to appropriate representations
Step 2: Autoencoder Architecture Specification
- Define encoder structure with progressively decreasing layers (e.g., 500 → 250 → 100 units)
- Create bottleneck layer with significantly reduced dimensions (e.g., 10-50 units)
- Define symmetric decoder structure for reconstruction
- Select appropriate activation functions (e.g., tanh, relu)
Step 3: Model Training
- Implement reconstruction loss minimization (mean squared error)
- Apply regularization techniques to prevent overfitting (e.g., dropout, L2 penalty)
- Use adaptive learning rate methods (e.g., Adam optimizer)
- Employ early stopping based on validation set performance
Step 4: Propensity Score Estimation
- Extract latent representations from the bottleneck layer
- Use these reduced-dimensional representations as covariates in propensity score model
- Estimate propensity scores using logistic regression with latent factors as predictors
- Apply conventional propensity score methods (weighting, matching) using the estimated scores
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of advanced propensity score methods requires both methodological expertise and appropriate analytical tools. The following table details essential components of the methodological toolkit for addressing confounding and data challenges in pharmacoepidemiology.
Table 4: Essential Research Reagents for Advanced Propensity Score Analysis
| Tool Category | Specific Tools/Techniques | Primary Function | Implementation Considerations |
|---|---|---|---|
| Bias Addressing Methods | Nested case-control design, Marginal structural models, Sequential conditioning | Address time-related biases (immortal time, time-dependent confounding) | Requires specialized design and analysis techniques |
| Missing Data Handling | Missingness Pattern Approach (MPA), Multiple imputation, Pattern mixture models | Handle partially observed confounders | Dependent on missingness mechanism assumptions |
| High-Dimensional Control | hdPS algorithm, Autoencoders, PCA, Regularized regression | Control for extensive covariate sets | Computational intensity, requires validation |
| Software & Computing | R (hdPS, ggplot2), Python (TensorFlow), SAS macros, High-performance computing | Implement complex analytical workflows | Reproducibility, computational resources |
| Balance Diagnostics | Standardized mean differences, Empirical covariate balance metrics, Love plots | Assess propensity score performance | Pre-specified balance thresholds required |
Integrated Analytical Framework for Complex Treatment Patterns
Analysis of complex treatment patterns requires specialized frameworks that can capture the temporal sequencing of treatment events and their relationship to outcomes. The following workflow illustrates an integrated approach for analyzing pharmacotherapy treatment patterns and their association with outcomes, as applied in a study of 252,179 veterans with major depressive disorder [74].
In the MDD application, this framework revealed that ten prescription patterns accounted for nearly 70% of treatment pathways among individuals starting antidepressants at 20-39 mg fluoxetine equivalents [74]. The analysis further identified specific associations between dosage changes and clinical outcomes, providing insights for personalized treatment monitoring.
Addressing unmeasured confounding, missing data, and complex treatment patterns requires sophisticated methodological approaches that extend beyond conventional propensity score methods. The integrated application of high-dimensional propensity scores with nested case-control designs, missingness pattern approaches, and dimensionality reduction techniques provides a robust framework for generating more valid evidence from pharmacoepidemiological studies. These advanced methods enable researchers to better approximate the conditions of randomized trials using observational data, enhancing the evidence base for drug development and clinical decision-making. Future methodological research should focus on developing more accessible implementations of these techniques and establishing comprehensive guidelines for their application across diverse therapeutic areas and data sources.
In pharmacoepidemiology, intercurrent events (ICEs) are events that occur after treatment initiation and affect either the interpretation or the existence of the measurements associated with the clinical question of interest [50]. In observational studies, common ICEs include treatment discontinuation, switching to alternative medications, and terminal events such as death [50]. These events present significant methodological challenges for estimating causal treatment effects from real-world data, necessitating robust analytical frameworks and precise definitional approaches.
The ICH E9(R1) estimand framework provides a structured approach for precisely defining treatment effects by accounting for ICEs through its five core attributes: (1) the target population, (2) the variable (endpoint), (3) the treatment conditions, (4) the strategy for handling intercurrent events, and (5) the population-level summary measure [75] [50]. This framework brings clarity and transparency to the scientific question of interest, ensuring alignment between study objectives, design, conduct, and analysis. Although originally developed for randomized controlled trials, the estimand framework's principles are increasingly recognized as relevant for observational pharmacoepidemiologic studies, where ICEs are ubiquitous [50].
Propensity score methods serve as a powerful companion to this framework by enabling researchers to adjust for confounding in observational studies, thus creating analysis sets where treated and reference groups have comparable distributions of measured baseline covariates [28] [76]. When combined with a clearly defined estimand, propensity score methods help emulate a target trial, reducing bias in treatment effect estimation even in the presence of complex ICE patterns [5].
Classifying Intercurrent Events and Defining Strategies
Classification of Common Intercurrent Events
In pharmacoepidemiologic studies, ICEs can be systematically categorized to inform appropriate analytical strategies. Table 1 outlines common ICE types, their characteristics, and examples.
Table 1: Classification of Intercurrent Events in Pharmacoepidemiology
| ICE Category | Definition | Common Examples | Key Characteristics |
|---|---|---|---|
| Treatment Discontinuation | Cessation of the study treatment before the planned endpoint | Early discontinuation due to adverse events, cost, or patient preference [50] | May be informative or non-informative; often requires strategy specification |
| Treatment Switching | Initiation of an alternative or additional therapy | Addition of rescue medication, switch to competitor drug [75] | Complicates isolation of initial treatment effect; common in chronic diseases |
| Terminal Events | Events that preclude subsequent measurement of the outcome | Death from any cause [50] | Precludes existence of outcome measurement for some strategies |
| Administrative Events | Events unrelated to treatment efficacy or safety | Relocation, loss to follow-up due to external factors, pandemic-related disruptions [77] | Often considered treatment-unrelated; may be addressed with hypothetical strategies |
A critical advancement in ICE management involves classifying events as either treatment-related or treatment-unrelated [77]. Treatment-related ICEs (e.g., discontinuation due to adverse events or lack of efficacy) are considered informative about treatment response and often warrant strategies that classify them as treatment failures. Conversely, treatment-unrelated ICEs (e.g., discontinuation due to relocation or insurance changes) may be addressed through hypothetical strategies that envision scenarios where these events did not occur [77].
Estimand Strategies for Handling ICEs
The ICH E9(R1) addendum describes several primary strategies for handling ICEs, each yielding a different interpretation of the treatment effect [75] [50]:
- Treatment Policy Strategy: The ICE is considered irrelevant to the treatment effect assessment. Outcomes are analyzed regardless of whether ICEs occurred, reflecting the real-world effectiveness of initiating treatment.
- Hypothetical Strategy: Estimates the treatment effect under a scenario where the ICE would not have occurred, requiring explicit assumptions about the ICE mechanism.
- Composite Strategy: Incorporates the occurrence of the ICE directly into the outcome definition, typically by assigning a poor outcome value to patients who experience the ICE.
- While-on-Treatment Strategy: Focuses on the treatment effect before the occurrence of an ICE, capturing only the initial treatment response.
- Principal Stratum Strategy: Restricts the analysis to the subgroup of patients who would not experience the ICE under either treatment assignment.
Table 2: Mapping ICE Types to Appropriate Handling Strategies
| ICE Type | Recommended Strategy | Interpretation of Treatment Effect | Key Considerations |
|---|---|---|---|
| Treatment Discontinuation (unrelated) | Hypothetical [77] | Effect if patients had remained on treatment | Requires assumption that ICE is conditionally independent of outcome |
| Treatment Discontinuation (related) | Composite [77] | Effect including discontinuation as failure | Clinically relevant for tolerability assessment |
| Treatment Switching | Treatment Policy or Hypothetical [75] | Effect of initial treatment strategy | Choice depends on whether switching is part of routine care |
| Death | Composite [77] | Effect including mortality | Necessary when death precludes outcome measurement |
| Administrative Censoring | Hypothetical | Effect in absence of administrative constraints | Useful for addressing non-informative censoring |
The following diagram illustrates the decision pathway for selecting appropriate strategies based on ICE characteristics:
Quantitative Evidence from Recent Studies
Recent large-scale studies have quantified the associations between intercurrent events and clinical outcomes, providing empirical support for their role as potential surrogate endpoints or prognostic factors.
Table 3: Quantified Associations Between Intercurrent Events and Clinical Outcomes in Non-Diabetic CKD (n=504,924) [78]
| Intercurrent Event | Clinical Outcome | Hazard Ratio | 95% Confidence Interval | Clinical Interpretation |
|---|---|---|---|---|
| Outpatient heart failure diagnosis | Hospitalization for heart failure | 12.92 | 12.67–13.17 | Strong predictor of future HF hospitalization |
| CKD stage 4 diagnosis | Kidney failure/need for dialysis | 3.75 | 3.69–3.81 | Moderate predictor of renal failure progression |
| Potassium-removing resin dispensation | Worsening of CKD stage | 4.83 | 4.51–5.17 | Electrolyte management as marker of disease severity |
| eGFR decline (laboratory subset, n=295,174) | Hospitalization for heart failure | Progressive increase with eGFR decline | N/A | Continuous relationship between renal function and CV risk |
| eGFR decline (laboratory subset, n=295,174) | Kidney failure/need for dialysis | Progressive increase with eGFR decline | N/A | Strong association between renal function decline and failure |
This study demonstrates how intercurrent events can serve as early indicators of more severe clinical outcomes, supporting their use in pharmacoepidemiologic research to understand disease progression and treatment effects [78].
Propensity Score Methods for Addressing Confounding in ICE Analysis
Propensity score methods are essential tools for addressing confounding in observational studies of treatment effects, particularly when ICEs are present [28]. The propensity score is defined as the probability of treatment assignment conditional on observed baseline covariates [28] [5]. These methods create analysis sets where treated and reference groups have comparable distributions of measured covariates, mimicking the balance achieved through randomization in clinical trials.
The four primary propensity score approaches are:
- Propensity Score Matching: Creates matched sets of treated and untreated subjects with similar propensity scores, enabling direct comparison of outcomes [76].
- Propensity Score Weighting: Uses inverse probability of treatment weights to create a pseudo-population where treatment assignment is independent of measured covariates [76].
- Propensity Score Stratification: Groups subjects into strata based on propensity score quantiles and estimates treatment effects within each stratum.
- Covariate Adjustment Using Propensity Score: Includes the propensity score as a covariate in outcome regression models to adjust for confounding.
When applied to time-to-event outcomes in the presence of ICEs, propensity score methods can estimate both marginal hazard ratios and absolute risk differences, providing comprehensive information about treatment effects [76].
Implementation Protocol for Propensity Score Analysis with ICEs
Protocol 1: Comprehensive Propensity Score Analysis with ICE Handling
Objective: To estimate the effect of a target treatment on a time-to-event outcome while appropriately addressing intercurrent events through the estimand framework and propensity score methods.
Step 1: Define the Target Estimand
- Specify all five attributes of the estimand framework:
- Target Population: Clearly define inclusion/exclusion criteria
- Treatment Conditions: Define index dates, exposure definitions, and comparator groups
- Endpoint: Precisely define the outcome measurement and timing
- Intercurrent Events: Pre-specify all relevant ICEs and handling strategies
- Population Summary: Define the target measure of association (e.g., hazard ratio) [75] [50]
Step 2: Assemble the Cohort and Define Variables
- Identify all eligible subjects meeting the target population definition
- Operationalize all baseline covariates, exposure definitions, and outcome measurements
- Document the occurrence and timing of all pre-specified ICEs during follow-up
Step 3: Estimate Propensity Scores
- Select covariates for inclusion based on subject matter knowledge
- Estimate propensity scores using logistic regression or machine learning methods
- Assess propensity score distribution overlap between treatment groups
- Evaluate covariate balance before and after propensity score application [28]
Step 4: Apply Propensity Score Method
- Implement the chosen propensity score method (matching, weighting, or stratification)
- Verify that adequate covariate balance has been achieved (standardized differences <0.1)
- Document the final analysis population characteristics
Step 5: Implement ICE Handling Strategy
- Apply the pre-specified ICE handling strategy consistent with the estimand:
- Treatment Policy: Analyze outcomes regardless of ICE occurrence
- Composite: Incorporate ICEs into the outcome definition
- Hypothetical: Use appropriate methods (e.g., inverse probability censoring weighting)
- For competing ICEs, implement appropriate statistical methods to address the competing risks [77]
Step 6: Estimate Treatment Effects
- Fit appropriate outcome models to estimate the treatment effect
- For time-to-event outcomes, use Cox regression or other survival models
- Report both relative and absolute measures of effect [76]
- Conduct sensitivity analyses to assess robustness to unmeasured confounding
Advanced Considerations and Recent Methodological Developments
Handling Competing Intercurrent Events
A significant methodological challenge arises when multiple ICEs compete to occur first, where the initial ICE censors subsequent events [77]. For example, if a patient discontinues treatment due to relocation (treatment-unrelated ICE), it remains unknown whether an adverse event (treatment-related ICE) would have occurred later in the follow-up period. This competing ICE structure has been largely overlooked in previous methodologies but is ubiquitous in practice [77].
Novel approaches now address this challenge by:
- Classifying ICEs as treatment-related or treatment-unrelated
- Applying a composite strategy to treatment-related ICEs
- Applying a hypothetical strategy to treatment-unrelated ICEs
- Developing weighting, outcome regression, and doubly robust estimators that account for the competing nature of these events [77]
Table 4: Essential Analytical Tools for ICE Analysis in Pharmacoepidemiology
| Tool Category | Specific Methods | Primary Application | Key References |
|---|---|---|---|
| Causal Frameworks | Estimand Framework (ICH E9[R1]), Target Trial Emulation | Study design and objective specification | [75] [50] |
| Confounding Control | Propensity score matching, Inverse probability of treatment weighting, High-dimensional propensity scoring | Addressing measured confounding in observational studies | [28] [76] [5] |
| ICE Handling Methods | Composite strategy, Hypothetical strategy (using IPCW), Treatment policy strategy | Addressing specific ICE types according to classification | [77] [50] |
| Sensitivity Analysis | E-value analysis, Monte Carlo sensitivity analysis, Proxy approach | Assessing robustness to unmeasured confounding and model assumptions | [5] |
Integrated Analytical Workflow for ICE Handling
The following diagram illustrates a comprehensive workflow for handling ICEs in pharmacoepidemiologic studies, integrating both the estimand framework and propensity score methods:
Handling intercurrent events appropriately is essential for generating valid evidence from pharmacoepidemiologic studies. The integration of the ICH E9(R1) estimand framework with robust propensity score methods provides a comprehensive approach for addressing these challenges. By pre-specifying ICE handling strategies through the estimand framework and implementing them using appropriate propensity score methods, researchers can produce more transparent, interpretable, and clinically relevant evidence from real-world data. Future methodological developments should focus on standardized approaches for classifying ICEs, handling competing events, and enhancing sensitivity analyses for unmeasured confounding in complex real-world settings.
In pharmacoepidemiological studies, estimating the causal effect of drug exposures on health outcomes is often challenged by confounding bias. Propensity score (PS) methods have emerged as powerful tools to address this issue by balancing observed baseline covariates between treated and untreated patients, thereby mimicking the conditions of a randomized experiment [10]. The validity of any PS analysis, however, hinges critically on the appropriate selection of covariates for the propensity score model. Mis-specification, including the inclusion of inappropriate variables or model overfitting, can introduce substantial bias or imprecision into treatment effect estimates [79] [80]. This application note provides detailed protocols for covariate selection, focusing specifically on the critical tasks of identifying and excluding instrumental variables and preventing model overfitting, within the context of pharmacoepidemiological research.
Scientific Foundation: Principles of Covariate Selection
Variable Types and Their Impact
The propensity score is defined as a patient's probability of receiving the treatment of interest conditional on their observed baseline covariates [10]. The goal of covariate selection is to include a sufficient set of variables to achieve conditional exchangeability between treatment groups without introducing new biases or statistical inefficiencies. Covariates can be categorized based on their relationships with the treatment and outcome, which determines their appropriateness for inclusion.
Table 1: Types of Covariates and Recommendations for Propensity Score Models
| Covariate Type | Relationship to Treatment & Outcome | Inclusion Recommendation | Rationale |
|---|---|---|---|
| True Confounder | Associated with both treatment and outcome | Always include | Necessary to eliminate confounding bias [79] |
| Predictor of Outcome Only | Associated with outcome but not treatment | Always include | Increases precision without increasing bias [79] [81] |
| Predictor of Treatment Only (Potential Instrument) | Associated with treatment but not outcome | Generally exclude | Decreases precision without reducing bias; can increase variance [79] [81] |
| Risk Factor for Outcome | Causes or proxies for outcome risk factors | Include | Helps control for prognostic differences |
| Pre-Treatment Measures | Measured before treatment assignment | Include | Not affected by the treatment [81] |
| Post-Treatment Measures | Measured after treatment assignment | Exclude | Could be affected by the treatment itself [81] |
Theoretical Rationale for Excluding Instruments
Instrumental variables (IVs)—variables that predict treatment assignment but are independent of the outcome—should generally be excluded from PS models. While IV methods are a distinct causal inference approach that leverages such variables, they play a harmful role in PS analysis [82]. Including IVs in a PS model is detrimental for both theoretical and practical reasons. Theoretically, since IVs are unrelated to the outcome, they cannot confound the treatment-outcome relationship and thus their adjustment is unnecessary for bias reduction [79]. Practically, their inclusion can substantially increase the variability of the treatment effect estimate. This occurs because IVs create divisions in the data that do not correspond to prognostic differences, leading to inefficient comparisons and less precise effect estimates [79] [81]. In scenarios with limited sample size, this variance inflation can be severe enough to overwhelm any minimal bias reduction, resulting in higher mean squared error [80].
Protocol 1: Identifying and Handling Instrumental Variables
Experimental Workflow
The following diagram illustrates the systematic decision process for identifying and handling potential instrumental variables during covariate selection.
Diagram 1: Instrumental Variable Identification Workflow
Detailed Methodology
Step 1: Pre-Specify Covariates Using Subject-Matter Knowledge
- Action: Before analyzing the data, compile a list of potential covariates based on clinical knowledge, literature review of the disease domain, and understanding of treatment prescribing patterns [83] [81].
- Rationale: Data-driven variable selection increases the risk of including spurious relationships and instruments.
- Documentation: Maintain a structured log documenting the theoretical justification for each candidate covariate, specifically noting the hypothesized relationship to both treatment assignment and outcome.
Step 2: Assess Temporal Priority
- Action: Verify that all considered covariates were measured and recorded prior to the treatment assignment or exposure [81].
- Rationale: Variables measured after treatment initiation may be mediators or consequences of the treatment, and adjusting for them can introduce bias by blocking causal pathways [81].
- Protocol: Create a data timeline for each patient, marking the sequence of covariate measurement, treatment initiation, and outcome occurrence.
Step 3: Evaluate Covariate-Outcome Relationships
- Action: For covariates strongly associated with treatment, formally assess their relationship with the outcome.
- Statistical Testing: While preliminary analyses (e.g., univariate regression of each covariate on the outcome) can be informative, prioritize theoretical knowledge over statistical significance due to the multiple testing problem [81].
- Decision Rule: If a covariate has a strong known association with treatment but no plausible direct effect on the outcome (e.g., physician prescribing preference, healthcare system characteristics), classify it as an instrumental variable and exclude it [81].
Step 4: Apply the Inclusion Principle When Uncertain
- Action: When uncertainty exists about whether a treatment-associated covariate affects the outcome, default to inclusion rather than exclusion [81].
- Rationale: Excluding a true confounder can perpetuate bias, while including a weak instrument has less severe consequences in large samples [79].
Protocol 2: Preventing Model Overfitting
Experimental Workflow
The following diagram outlines the protocol for preventing overfitting during propensity score model estimation.
Diagram 2: Overfitting Prevention Protocol
Quantitative Guidance and Diagnostics
Overfitting occurs when a model captures random noise in the data rather than true underlying relationships, leading to poor performance in subsequent effect estimation. In PS analysis, overfitting can produce propensity scores that fail to balance covariates and inflate the variance of treatment effect estimates [80].
Table 2: Overfitting Prevention Strategies and Diagnostic Metrics
| Strategy | Operationalization | Threshold/Guideline | Interpretation |
|---|---|---|---|
| Events-per-Variable (EPV) | Number of patients in the rarest treatment category divided by number of parameters in PS model | EPV ≥ 10-20 [80] | EPV < 10 indicates high overfitting risk; EPV < 5 indicates severe overfitting risk |
| Covariate Prioritization | Rank covariates by theoretical importance as confounders | Include strongest confounders first when limiting parameters | Ensures most important confounders are adjusted even when sample size is limited |
| Regularization Methods | Use penalized regression (e.g., lasso, ridge) or machine learning (e.g., boosting, random forests) | Cross-validate hyperparameters | Reduces overfitting by penalizing model complexity; particularly useful with many covariates [10] |
| Balance Diagnostics | Calculate standardized mean differences after PS adjustment | Absolute value < 0.1 [83] | Good balance indicates well-specified model regardless of statistical fit |
| Variance Inflation Assessment | Compare standard errors of treatment effect from overfit vs. parsimonious models | Qualitative comparison | Substantially larger SEs in complex model suggest overfitting [80] |
Detailed Methodology
Step 1: Calculate Effective Sample Size
- Action: Determine the number of patients in the smaller treatment group (either treated or untreated), as this represents the limiting sample for PS model estimation.
- Example: In a study with 2,000 treated and 500 untreated patients, the effective sample size for EPV calculation is 500.
Step 2: Apply Events-per-Variable (EPV) Rule
- Action: Divide the effective sample size by the number of parameters (including main effects and interaction terms) in the proposed PS model.
- Protocol Adjustment: If EPV < 10-20, reduce the number of parameters by:
- Removing lower-priority covariates (e.g., those with weaker confounding evidence)
- Combining correlated covariates into composite scores
- Using dimension reduction techniques before PS estimation
Step 3: Implement Regularization for High-Dimensional Data
- Action: When many important confounders must be considered relative to sample size, use regularization techniques.
- Options:
- Penalized Logistic Regression: LASSO or ridge regression to shrink coefficient estimates
- Machine Learning Algorithms: Boosted regression, random forests, or neural networks for propensity score estimation [10]
- Validation: Use cross-validation to tune hyperparameters and avoid over-optimism.
Step 4: Diagnose Overfitting Empirically
- Action: After PS application (matching, weighting, or stratification), assess whether overfitting has occurred.
- Primary Diagnostic: Check covariate balance using standardized mean differences for all covariates [83].
- Secondary Diagnostic: Compare the standard error of the treatment effect estimate from the PS-adjusted model to simpler models; substantial inflation suggests overfitting [80].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Propensity Score Analysis
| Research Tool | Function | Application Notes |
|---|---|---|
| Directed Acyclic Graphs (DAGs) | Visual representation of causal assumptions | Identifies minimal sufficient adjustment set; reveals instrumental variables and mediators [83] |
| Standardized Mean Differences | Quantifies covariate balance between groups | Primary diagnostic for PS model adequacy; target <0.1 for all covariates [83] |
| Events-per-Variable (EPV) Calculator | Determines maximum sustainable model complexity | Critical for preventing overfitting; implemented in R, SAS, or Stata |
| Regularized Regression Methods | Estimates PS while preventing overfitting | Essential for high-dimensional covariate situations; available via glmnet in R [10] |
| Machine Learning Packages | Flexible PS estimation with cross-validation | Boosted regression (twang package), random forests; can handle non-linearities [10] |
| Balance Assessment Software | Comprehensive diagnostic tools | cobalt package in R provides unified balance assessment across PS methods [83] |
Performance Characteristics
The following table summarizes the expected performance outcomes when correctly implementing these covariate selection protocols compared to common pitfalls.
Table 4: Performance Characteristics of Covariate Selection Approaches
| Selection Approach | Bias | Variance | Mean Squared Error | Balance Achievement |
|---|---|---|---|---|
| Including all confounders and outcome predictors | Low | Moderate | Low | High |
| Including instruments | Unchanged or slightly reduced | High | High | Variable |
| Excluding weak confounders | Moderate to high | Low | Moderate to high | Low to moderate |
| Overfit model (low EPV) | Low to moderate | Very high | High | Poor despite good apparent fit |
| Protocol-compliant selection | Low | Moderate | Low | High |
Appropriate covariate selection is fundamental to valid causal inference using propensity score methods in pharmacoepidemiology. By systematically excluding instrumental variables and preventing model overfitting through the protocols outlined herein, researchers can produce more reliable estimates of drug effects from observational data. These application notes provide actionable guidance for implementing these critical methodological safeguards, contributing to more robust evidence generation in drug development and safety research.
Ensuring Validity: Balance Assessment, Framework Alignment, and Method Comparison
Gold Standards for Assessing Covariate Balance After PS Application
Propensity score (PS) methods are fundamental in pharmacoepidemiology to control for confounding in observational studies. The validity of these methods hinges on achieving adequate covariate balance between treatment groups after PS application. This protocol outlines gold-standard methodologies for assessing covariate balance, providing a structured framework for researchers to evaluate the success of propensity score adjustment. We detail diagnostic tools, quantitative metrics, visualization techniques, and interpretation guidelines essential for confirming that balanced distributions of baseline characteristics have been achieved, thereby strengthening causal inference in drug safety and effectiveness research.
In pharmacoepidemiology, propensity score (PS) methods have become a cornerstone for estimating treatment effects using observational data, confronting formidable obstacles that arise from the use of large, complex healthcare databases [1]. The propensity score, defined as the probability of treatment assignment conditional on observed baseline covariates, functions as a balancing score [10]. Its core property is that conditional on the true propensity score, the distribution of observed baseline covariates is similar between treated and untreated subjects [10].
The "propensity score tautology" asserts that we know we have a consistent estimate of the propensity score when matching on the propensity score balances the raw covariates [84]. Thus, the appropriateness of the specification of the propensity score is assessed by examining whether its application has resulted in a sample where the distribution of measured baseline covariates is similar between treatment groups [84]. Careful testing of propensity scores is required before using them to estimate treatment effects [85]. This document establishes standardized protocols for conducting these critical balance assessments.
Quantitative Balance Metrics
Standardized Mean Differences
The standardized mean difference (SMD) is the most widely recommended metric for assessing balance in baseline covariates after propensity score application. It quantifies the difference between group means in standardized units, making it comparable across covariates with different measurement scales [84].
Table 1: Standardized Mean Difference Interpretation Guidelines
| SMD Value | Balance Interpretation | Recommended Action |
|---|---|---|
| < 0.1 | Adequate balance | Proceed to outcome analysis |
| 0.1 - 0.25 | Moderate imbalance | Consider model respecification |
| > 0.25 | Substantial imbalance | Revise propensity score model |
For a continuous covariate, the SMD is calculated as:
[ \text{SMD} = \frac{\bar{x}{\text{treat}} - \bar{x}{\text{control}}}{\sqrt{\frac{s^2{\text{treat}} + s^2{\text{control}}}{2}}} ]
where (\bar{x}) represents the group mean and (s^2) the group variance [84]. For binary covariates, the SMD is calculated as the difference in proportions divided by the pooled standard deviation.
In small sample sizes, chance imbalance can cause large SMD deviations. Austin suggests measuring the empirical distribution of SMD to account for chance imbalance [86]. For studies with many covariates or small sample sizes, consider testing whether SMD statistically significantly exceeds the 0.1 threshold rather than using a simple nominal threshold [86].
Advanced Distributional Diagnostics
Balance assessment should extend beyond means to include the entire covariate distribution. Variance ratios (ratio of variances in treated versus control groups) should be close to 1, with values outside 0.5-2.0 indicating potential imbalance [84]. Higher-order moments and interactions should also be assessed [84].
Table 2: Comprehensive Balance Assessment Metrics
| Metric Category | Specific Tests | Target Value |
|---|---|---|
| Central Tendency | Standardized mean differences, t-tests | SMD < 0.1 |
| Distributional Shape | Variance ratios, quantile-quantile plots | Ratio 0.5-2.0 |
| Extreme Values | Five-number summaries, boxplots | Similar distributions |
| Multivariate Balance | Interaction terms, higher-order moments | Non-significant differences |
Visual Balance Diagnostics
Visual assessments provide intuitive understanding of balance that complements quantitative metrics.
Love Plots
Love plots (also called balance plots) display SMD values for all covariates before and after propensity score application, providing an immediate overview of balance improvement [87]. These visualizations powerfully communicate whether results pass statistical tests that determine balance [87].
Distributional Plots
Covariate distribution plots including histograms, density plots, boxplots, and quantile-quantile (Q-Q) plots allow direct comparison of the entire distribution of key covariates between treatment groups before and after propensity score application [84]. If matching was successful, covariate distributions should be more similar in the matched sample than in the unmatched sample [87].
Covariate Balance Assessment Workflow
Implementation Protocols
Comprehensive Balance Assessment Protocol
- Calculate standardized mean differences for all baseline covariates included in the propensity score model and other potential confounders [84]
- Compute variance ratios for continuous covariates to assess distributional similarity beyond means [84]
- Generate visual diagnostics including Love plots, Q-Q plots, and side-by-side boxplots [87] [84]
- Assess higher-order terms and interactions if clinically relevant [84]
- Formally test balance using appropriate statistical tests when sample size permits [86]
- Document all findings including both pre- and post-adjustment balance metrics
Special Considerations for Pharmacoepidemiology
- New-user designs: Anchor balance assessment at initial prescription dispensing after period of non-use [1]
- High-dimensional covariates: With large numbers of covariates, use Bonferroni correction or statistical testing of SMD thresholds to avoid false rejections due to chance imbalance [86]
- Database heterogeneity: In distributed network studies, assess balance within each database and through meta-analysis [86]
- Target population: Consider whether balance is needed for average treatment effect (ATE) or average treatment effect on treated (ATT) populations [1]
The Scientist's Toolkit
Table 3: Essential Tools for Balance Assessment
| Tool Category | Specific Solutions | Primary Function |
|---|---|---|
| Statistical Software | R MatchIt, Cobalt packages | Implement propensity score matching and generate balance diagnostics [87] |
| Balance Metrics | Standardized mean differences, variance ratios | Quantify balance for continuous and categorical covariates [84] |
| Visualization Packages | ggplot2, Cobalt balance plots | Create Love plots, distribution comparisons [87] |
| High-Dimensional PS | High-dimensional propensity score, machine learning algorithms | Address confounding when hundreds of covariates are available [1] |
Balance Visualization Framework
Rigorous assessment of covariate balance is not merely an optional diagnostic step but a fundamental requirement for valid causal inference using propensity score methods in pharmacoepidemiology. The gold standards outlined in this document—combining quantitative metrics with visual diagnostics—provide a comprehensive framework for evaluating the success of propensity score applications. Implementation of these protocols will enhance the credibility of observational drug studies and support more reliable decision-making in drug development and safety assessment. Future methodological developments will likely focus on improving balance assessment for high-dimensional covariates and complex longitudinal treatment regimens.
The increasing complexity of causal inference in pharmacoepidemiology demands rigorous frameworks to align observational research with clinical trial standards. This protocol details the integration of ICH E9(R1) estimands with target trial emulation (TTE) and advanced propensity score (PS) methods to enhance the validity of real-world evidence. The ICH E9(R1) framework provides a structured approach to precisely define treatment effects of interest, accounting for intercurrent events that complicate interpretation. Simultaneously, TTE creates a quasi-experimental structure within observational data by emulating a hypothetical randomized trial that would ideally answer the research question. When combined with sophisticated PS approaches like high-dimensional propensity score (hdPS) and machine learning techniques, these frameworks address critical biases including immortal time bias and residual confounding that frequently plague observational studies [6] [88].
This guidance document provides practical application notes and experimental protocols for implementing these integrated frameworks within pharmacoepidemiological studies, with specific examples drawn from recent research advancements. The structured approach ensures clarity in defining causal effects of interest while implementing robust methodological safeguards against common biases.
Conceptual Framework and Integration
Core Principles and Relationships
The integration of ICH E9(R1) estimands, target trial emulation, and propensity score methods creates a synergistic framework for robust causal inference. Estimands provide the precise mathematical definition of the treatment effect, including how intercurrent events are handled, while TTE provides the structural design that mimics an randomized controlled trial (RCT), and PS methods enable statistical adjustment to approximate randomization in observational data [88] [89].
ICH E9(R1) Estimand Components in Observational Studies
The estimand framework comprises five attributes that collectively provide a precise definition of the treatment effect for a specific clinical question: treatment, population, variable, population-level summary, and handling of intercurrent events. In pharmacoepidemiology, intercurrent events such as treatment switching, discontinuation, or initiation of concomitant medications are particularly common and must be addressed through appropriate strategies [89].
Table: Estimand Attributes and Their Application in Pharmacoepidemiology
| Estimand Attribute | Definition | Observational Study Considerations | Example |
|---|---|---|---|
| Treatment | Intervention and conditions being compared | Clearly define exposure timing, dose, and duration | Disease-modifying drugs vs. no treatment |
| Population | Target population of interest | Specify inclusion/exclusion criteria that can be implemented in real-world data | Patients with multiple sclerosis, aged 18-65 |
| Variable | Outcome or endpoint | Ensure accurate and consistent measurement in real-world data | All-cause mortality |
| Population-level Summary | How treatment effect is summarized | Choose appropriate statistical measure | Hazard ratio |
| Handling of Intercurrent Events | Strategy for events affecting interpretation | Implement causal methods to address informative censoring | Treatment discontinuation handled via principal stratification |
Experimental Protocols
Protocol 1: Integrated Estimand Specification and TTE Design
This protocol establishes the foundation for aligning observational studies with the ICH E9(R1) framework through target trial emulation.
Objectives and Hypotheses
- Primary Objective: To emulate the target trial of disease-modifying drugs (DMDs) on all-cause mortality in multiple sclerosis patients, defining the estimand according to ICH E9(R1) principles.
- Hypothesis: Compared to no treatment, DMDs reduce all-cause mortality with a hazard ratio of 0.70 after addressing immortal time bias and residual confounding.
Target Trial Protocol
- Eligibility Criteria: Define inclusion/exclusion criteria mirroring an ideal RCT, including: confirmed MS diagnosis, age 18-65, no prior DMD treatment, and minimum 1-year baseline data.
- Treatment Strategies: Specify treatment arms as "initiation of DMDs" versus "no DMD treatment" with clear operational definitions for exposure.
- Treatment Assignment: In the emulation, implement a pseudo-randomization process using hdPS to balance baseline covariates.
- Outcome Definition: All-cause mortality ascertained from death registries with precise timing.
- Follow-up Period: Define start (eligibility date) and end (death, end of study period, or 5 years) with intent-to-treat principle maintained.
- Causal Contrast: Specify the comparison of survival outcomes between treatment strategies regardless of subsequent treatment changes (treatment policy strategy for intercurrent events) [6] [88].
Protocol 2: hdPS with Nested Case-Control for Bias Mitigation
This protocol combines high-dimensional propensity scores with a nested case-control design to simultaneously address immortal time bias and residual confounding, as demonstrated in multiple sclerosis research [6].
Cohort Definition and Follow-up
- Data Source: Utilize administrative claims or electronic health records with sufficient sample size (e.g., 19,360 patients in the reference study).
- Baseline Period: Establish a 1-year baseline period for assessing covariates prior to eligibility date.
- Time-zero: Define cohort entry at the first date meeting all eligibility criteria (addressing immortal time bias by ensuring this occurs after exposure assessment).
- Follow-up: Track patients from time-zero until outcome occurrence, censoring, or study end.
hdPS Implementation Steps
- Covariate Selection: Identify candidate covariates across five data dimensions: diagnoses, procedures, medications, and other available domains.
- Dimension Reduction: Apply autoencoder or other dimensionality reduction techniques for improved covariate balance compared to conventional hdPS [73].
- PS Estimation: Calculate propensity scores using logistic regression or machine learning algorithms, including both investigator-specified and empirically identified covariates.
- Covariate Balance: Assess balance using standardized mean differences (target <0.1 for all covariates).
Nested Case-Control Implementation
- Case Definition: Identify all patients experiencing the outcome event during follow-up.
- Control Selection: Randomly select up to 4 controls per case from patients at risk at the time of the case event, matched on time-in-study and other potential confounders.
- Analysis: Apply conditional logistic regression adjusted for the propensity score to estimate hazard ratios.
Table: Comparison of Propensity Score Estimation Techniques
| Method | Covariates with SMD >0.1 | Implementation Complexity | Recommended Use Case |
|---|---|---|---|
| Investigator-specified | 83 | Low | Studies with strong prior knowledge of confounders |
| High-dimensional PS (hdPS) | 37 | Medium | Routine pharmacoepidemiology with claims data |
| Principal Component Analysis (PCA) | 20 | Medium-High | High-dimensional covariate spaces |
| Autoencoders | 8 | High | Optimal covariate balance prioritized |
Analytical Workflow
The complete analytical workflow integrates estimand specification, study design, and analytical methods to produce valid causal estimates.
The Scientist's Toolkit
Research Reagent Solutions
Table: Essential Methodological Components for Implementation
| Component | Function | Implementation Example |
|---|---|---|
| High-dimensional Propensity Score (hdPS) | Empirically identifies and adjusts for confounders in large healthcare databases | Automatically selects covariates from diagnosis, procedure, and prescription data using predefined algorithms [6] [73] |
| Nested Case-Control Design | Addresses immortal time bias and increases computational efficiency | For each case, select 4 controls matched on time-in-study and other potential confounders [6] |
| Dimensionality Reduction Techniques | Improves propensity score specification and covariate balance | Autoencoders outperform conventional methods, reducing covariates with imbalance (SMD >0.1) from 83 to 8 [73] |
| Sensitivity Analysis Framework | Tests robustness of findings to key assumptions | Vary hdPS parameters, control matching strategies, and model specifications [6] |
| Reproducible Code | Facilitates methodology adoption and verification | Share R or Python scripts implementing the complete analytical pipeline [6] |
Application Notes
Case Study: Disease-Modifying Drugs in Multiple Sclerosis
A recent study exemplifies the integrated framework, examining DMDs and all-cause mortality in 19,360 MS patients [6]. The implementation demonstrated:
- Estimand Specification: Treatment effect defined as the difference in survival between DMD initiators and non-initiators, addressing intercurrent events through a treatment policy strategy.
- Immortal Time Bias Resolution: Using the nested case-control design with appropriate time-zero definition.
- Residual Confounding Control: hdPS achieved substantial confounding adjustment, with only 37 covariates remaining imbalanced (SMD >0.1) compared to 83 with investigator-specified PS.
- Mortality Effect: The integrated approach demonstrated a 28% reduction in mortality risk (HR: 0.72, 95% CI: 0.62-0.84) associated with DMD exposure.
Performance Metrics and Validation
The robustness of this approach was validated through comprehensive sensitivity analyses:
- Effect Consistency: Hazard ratios remained stable across different PS estimation techniques (HR range: 0.70-0.77).
- Covariate Balance: Dimensionality reduction techniques, particularly autoencoders, achieved superior balance compared to conventional methods.
- Bias Reduction: The combination of NCC and hdPS simultaneously addressed both time-related and confounding biases.
This structured approach provides pharmacoepidemiologists with a robust framework for generating evidence that aligns with regulatory standards while addressing the inherent limitations of observational data.
Within pharmacoepidemiology, researchers are tasked with estimating the effects of drugs and medical products using observational data, where treatment assignment is not random [28]. This reality introduces confounding by indication, a phenomenon where treatment decisions are influenced by a patient's prognosis, systematically distorting the relationship between treatment and outcome [1]. For decades, traditional multivariable regression has been the cornerstone for controlling confounding in observational studies. More recently, propensity score (PS) methods have emerged as a powerful alternative, offering a different approach to achieving causal inference [90].
This article provides application notes and protocols for comparing these two analytical frameworks. We frame this within a broader thesis on PS methods, positing that while traditional regression adjusts for confounders in the outcome model, PS methods excel by focusing first on modeling the treatment assignment process. This creates a design stage that separates covariate balancing from outcome analysis, potentially offering advantages in transparency, diagnostics, and handling of high-dimensional data [91] [81].
Theoretical Foundations and Key Differences
Conceptual Frameworks
The fundamental goal of both PS methods and traditional regression is to achieve conditional exchangeability—that is, to make the treatment and control groups comparable on all measured baseline covariates, as if randomization had occurred [1].
- Traditional Regression Adjustment: This method models the outcome directly. It estimates the association between treatment and outcome while simultaneously adjusting for confounding covariates by including them in the outcome model. For a binary outcome, a logistic regression model might take the form:
Outcome ~ Treatment + Covariate1 + Covariate2 + ... + CovariateK[90]. The model relies on correctly specifying the functional form between the outcome and each confounder. - Propensity Score Methods: The PS is defined as a patient's probability of receiving the treatment of interest, conditional on their measured baseline covariates [28]. It is estimated using a model (e.g., logistic regression) where treatment status is the outcome:
Treatment ~ Covariate1 + Covariate2 + ... + CovariateK. The resulting PS, a single composite score, is then used to balance covariates across treatment groups via matching, weighting, or stratification [90]. This approach separates the design of the study (creating balanced groups) from the analysis of the outcome [91].
Comparative Advantages and Disadvantages
The core differences between the methods lead to distinct practical advantages and limitations, which are summarized in Table 1 below.
Table 1: Comparative advantages and disadvantages of traditional regression and propensity score methods.
| Feature | Traditional Regression Adjustment | Propensity Score Methods |
|---|---|---|
| Primary Approach | Adjusts for confounders in the outcome model [90] | Models the treatment assignment process; separates design from analysis [91] |
| Dimensionality | Adjusts for all confounders simultaneously in the outcome model; can be high-dimensional [28] | Reduces multiple covariates to a single score for balancing (dimension reduction) [91] |
| Handling of Rare Outcomes | Efficient with a sufficient number of outcome events per covariate (e.g., rule of 10) [28] | Advantageous when outcome events are rare, as the treatment model is not limited by outcome rarity [28] [81] |
| Covariate Balance Assessment | Balance of covariates between groups is typically not formally assessed after regression [91] | Allows for direct checking of covariate balance between groups after matching/weighting (e.g., using standardized mean differences) [90] [28] |
| Extrapolation | Can extrapolate using the linearity assumption, even in regions with no overlap [92] | Limits analysis to regions of common support; avoids extrapolation by trimming non-overlapping PS tails [92] [81] |
| Key Assumptions | Correct model specification (functional form, no interactions) for the outcome [90] | Correct model specification for the treatment assignment; requires positivity and overlap [28] |
A key conceptual difference lies in their approach to extrapolation. Regression inherently extrapolates based on its modeled assumptions, which can be problematic if the treatment and control groups are very different. In contrast, PS methods allow for a visual inspection of the score distributions, enabling researchers to identify and trim patients with no comparable counterparts in the other group, thus focusing the inference on the region of common support [92] [81].
Quantitative Performance Comparison
Empirical studies and simulations have been conducted to evaluate the relative performance of these methods. A clinical case study on gram-negative bloodstream infections directly compared four methods, as summarized in Table 2.
Table 2: Results from a clinical case study comparing methods for estimating the effect of IV-to-oral antibiotic transition on 30-day mortality (Adapted from [90]).
| Analytical Method | Odds Ratio for 30-Day Mortality | Key Interpretation Notes |
|---|---|---|
| Multivariable Logistic Regression | 0.84 | Adjusted for confounders in the outcome model. |
| Propensity Score Matching (PSM) | 0.84 | Created matched cohorts with similar baseline characteristics. |
| Propensity Score Inverse Probability of Treatment Weighting (IPTW) | 0.95 | Created a pseudo-population; can be influenced by extreme weights. |
| Propensity Score Stratification | 0.87 | Stratified analysis by propensity score quintiles. |
While the point estimates were broadly similar in this example, the authors noted relevant differences in interpretation, particularly for IPTW, which can be sensitive to patients with very high or low propensity scores [90]. A systematic review of artificial intelligence in pharmacoepidemiology found that in 50% of comparisons, machine learning techniques (including some for PS estimation) outperformed traditional pharmacoepidemiological methods [93].
Detailed Experimental Protocols
Protocol 1: Implementing Propensity Score Matching
Propensity Score Matching (PSM) is a widely used method to create a balanced cohort for analysis. The following workflow outlines the key steps, and Figure 1 provides a visual representation of the process.
Figure 1: Propensity Score Matching Workflow
Step-by-Step Methodology:
Data Preprocessing and Covariate Selection:
- Aim: Prepare a clean dataset with all necessary variables.
- Actions: Identify and address outliers and missing values through imputation or other methods [91]. Select covariates for the PS model based on subject matter knowledge. Include variables that are risk factors for the outcome and/or associated with treatment assignment. Avoid variables that are consequences of the treatment [28] [81].
- Tools: R packages:
Hmisc,DMwRfor imputation [91].
Propensity Score Estimation:
- Aim: Model the probability of treatment assignment for each patient.
- Actions: Typically, a logistic regression model is used where the dependent variable is treatment assignment (e.g., 1 for treated, 0 for control). The independent variables are the selected pretreatment covariates. The goal is to achieve balance, not prediction per se, so overfitting is less of a concern and interactions/higher-order terms can be included to improve balance [90] [28].
- Tools: Logistic regression in R (
glm),MatchItpackage [91].
Matching:
- Aim: Create a matched sample where treated and control units have similar PS distributions.
- Actions: Use a matching algorithm such as 1:1 nearest-neighbor matching without replacement. A caliper (e.g., 0.2 standard deviations of the logit of the PS) is often applied to prevent poor matches [90]. This step may drop unmatched units, refining the sample to the region of common support.
- Tools:
MatchItpackage in R [91].
Assessing Covariate Balance:
- Aim: Diagnose whether the matching procedure successfully balanced the covariates.
- Actions: Do not rely on p-values from significance tests. Instead, use standardized mean differences (SMDs) for each covariate. An SMD of less than 10% (or 0.1) generally indicates good balance [90] [28]. Generate love plots or other balance diagnostic charts.
- Tools:
tableone,cobaltpackages in R [91]. If balance is inadequate, return to Step 2 and respecify the PS model.
Estimating the Treatment Effect:
- Aim: Quantify the association between treatment and outcome in the balanced sample.
- Actions: In the matched cohort, analyze the outcome using methods appropriate for the matched data structure. For a binary outcome, a simple logistic regression model (
Outcome ~ Treatment) can be used. For a more robust estimate, use a model that adjusts for any residual imbalance in key covariates (doubly robust estimation) [90]. - Tools: Standard regression models in R or Stata.
Sensitivity Analysis:
- Aim: Assess how sensitive the findings are to potential unmeasured confounding.
- Actions: Perform analyses such as testing how strong an unmeasured confounder would need to be to nullify the observed effect [91]. Trimming the tails of the PS distribution (e.g., excluding patients outside the 2.5th-97.5th percentiles of the opposite group's PS) is another sensitivity check for residual confounding [81].
- Tools: Specialist R packages or functions.
Protocol 2: Traditional Multivariable Regression Adjustment
This protocol serves as a benchmark comparison for the PSM approach.
Step-by-Step Methodology:
Model Specification:
- Aim: Define the regression model that relates the outcome to the treatment and confounding variables.
- Actions: Specify a model where the outcome is a function of the treatment indicator and all pre-specified confounders. For a binary outcome, this is typically a logistic model:
Outcome ~ Treatment + Covariate1 + Covariate2 + ... + CovariateK. The functional form (e.g., linear, squared terms) for continuous covariates must be considered [90].
Model Fitting and Assumption Checking:
- Aim: Fit the model and check for violations of regression assumptions.
- Actions: Fit the model to the entire dataset (no matching). Check for multicollinearity among covariates and assess model fit using appropriate diagnostics (e.g., residual plots for linear models). Ensure the number of outcome events per variable is adequate to prevent overfitting (a common rule of thumb is 10-15 events per variable) [90] [28].
Treatment Effect Estimation:
- Aim: Obtain the adjusted estimate of the treatment effect.
- Actions: Extract the coefficient for the treatment variable and its confidence interval from the fitted model. This represents the log-odds ratio (for logistic regression) of the outcome associated with the treatment, adjusted for all other covariates in the model.
Successful implementation of these methods requires both statistical software and methodological rigor. Table 3 lists key "research reagents" for a pharmacoepidemiologist.
Table 3: Essential tools and resources for comparative analyses of PS methods and traditional regression.
| Tool / Resource | Type | Function / Purpose | Key Considerations |
|---|---|---|---|
| R Statistical Software | Software Environment | Free, open-source platform for statistical computing and graphics. Supports all PS methods and traditional regression. | Extensive package ecosystem (e.g., MatchIt, cobalt) [91]. Steep learning curve but highly flexible. |
| Stata | Software Environment | Commercial software popular in epidemiology and economics. | Has dedicated modules for PS analysis (e.g., psmatch2). Often favored for its reproducibility and command-based interface [91] [94]. |
MatchIt Package (R) |
Software Tool | Implements a variety of matching methods for causal inference, including PSM. | Simplifies the process of matching and subsequent balance checking [91]. A core package for PSM in R. |
cobalt Package (R) |
Software Tool | Designed for covariate balance assessment and presentation. | Provides superior plots and tables for balance diagnostics (e.g., love plots) after matching or weighting [91]. |
| Standardized Mean Difference (SMD) | Metric | Quantifies the balance of a covariate between treatment groups, standardized by the pooled standard deviation. | The primary metric for assessing balance in PS analyses. SMD <0.1 indicates good balance [90] [28]. |
| "Table One" | Reporting Standard | A table presenting the baseline characteristics of the study population, overall and by treatment group. | Essential for both before and after matching/weighting to demonstrate the success of the balancing method [91]. |
Both traditional regression adjustment and propensity score methods are valid approaches for controlling confounding in pharmacoepidemiological studies. The choice between them is not a matter of one being universally superior, but rather depends on the specific research context, data structure, and analytical goals.
PS methods offer distinct advantages in their ability to visually inspect and ensure covariate balance, to separate study design from analysis, and to handle scenarios with rare outcomes or a large number of confounders. Traditional regression remains a powerful, efficient, and straightforward tool, particularly when the model is correctly specified and sample sizes are large.
The modern pharmacoepidemiologist should be proficient in both methodologies. The protocols and tools outlined herein provide a foundation for conducting rigorous comparative analyses, ultimately leading to more reliable evidence on the real-world effects of medicinal products.
In pharmacoepidemiological research, the validity of findings from non-randomized, post-market safety studies is paramount. The propensity score (PS), defined as the probability of a patient receiving a specific treatment conditional on their measured baseline covariates, has become a cornerstone method for controlling for confounding in such analyses [28]. By balancing the distribution of covariates between treated and reference groups, PS methods emulate the random allocation of a clinical trial, thus providing more reliable estimates of treatment effects on safety outcomes in observational data [1] [28]. This document outlines application notes and detailed protocols for implementing propensity score methods, framed within the context of recent case studies from the pharmacoepidemiological literature.
Contemporary Practice in Safety Studies: A Case Review
A recent review of 25 post-marketing safety studies published in 2020 provides a snapshot of current methodological practices [95] [96]. The findings demonstrate the integral role of confounding control methods in the field.
Table 1: Characteristics of Recent Pharmacoepidemiologic Safety Studies (2020)
| Study Characteristic | Category | Number of Studies (N=25) | Percentage |
|---|---|---|---|
| Study Design | Cohort Studies | 19 | 76% |
| Nested Case-Control Studies | 6 | 24% | |
| Primary Confounder Control Method | Propensity Score (PS) Methods | 7 (of 19 cohort) | ~37% |
| Covariate Adjustment via Modeling | 9 (of 19 cohort) | ~47% | |
| Both PS & Covariate Adjustment | 2 (of 19 cohort) | ~11% | |
| Matching & Covariate Adjustment | 6 (of 6 case-control) | 100% |
This review confirms that all recent studies employed robust methods to control for confounding, with propensity score techniques being a prevalent choice [95]. Furthermore, the analysis through the lens of the ICH E9(R1) estimand framework revealed that while studies consistently defined key attributes like treatment, outcome, and population, the handling of intercurrent events (ICEs)—such as drug discontinuation or treatment switching—was often discussed without using the formal ICE terminology. This highlights an area where methodological reporting can be further standardized [95].
Experimental Protocols for Propensity Score Application
The following protocol provides a step-by-step guide for implementing propensity score methods in a pharmacoepidemiologic safety study.
Protocol 1: Propensity Score-Based Analysis for a Post-Market Safety Study
Objective: To estimate the comparative risk of a specific safety outcome (e.g., gastrointestinal bleeding) between initiators of a new drug (e.g., COX-2 inhibitors) and initiators of an active comparator (e.g., non-selective NSAIDs) using real-world data.
Key Assumptions:
- Exchangeability: All common causes of treatment assignment and the outcome are measured in the data (no unmeasured confounding).
- Positivity: Every patient has a non-zero probability of receiving either treatment, conditional on their covariates.
- SUTVA: The treatment and outcome of one patient are not affected by the treatment assignment of another [28].
Procedure:
Study Population Definition & Design
- Implement a new-user (incident user) design to minimize selection bias. Define the cohort entry date as the first prescription dispensing of either the study drug or comparator after a defined period of non-use [1].
- Clearly define the target population based on the clinical question of interest. Common targets are the Average Treatment Effect in the Overall Sample (SATE) or the Average Treatment Effect on the Treated (SATT) [1].
Covariate Selection and PS Model Building
- Identify Covariates: Select pre-treatment covariates (e.g., demographics, comorbidities, prior medications, healthcare utilization) that are risk factors for the outcome and/or associated with treatment selection. This should be guided by subject matter knowledge and clinical expertise [1] [28].
- Model Specification: Estimate the propensity score using a logistic regression model where the dependent variable is treatment assignment (e.g., 1=COX-2 inhibitor, 0=NSAID) and the independent variables are the selected pre-treatment covariates.
- Goal: The goal is not prediction but covariate balance. Avoid using model fit statistics (e.g., c-statistic) to guide covariate selection [1].
Implementing the Propensity Score
- Choose one of the following primary methods:
- Matching: Create matched sets (e.g., 1:1 nearest-neighbor matching within a caliper) of treated and reference patients with similar PS. Discard unmatched patients.
- Weighting: Create a pseudo-population using inverse probability of treatment weights (IPTW). The weight for a patient is defined as 1/PS for the treated and 1/(1-PS) for the reference group.
- Stratification: Stratify the entire study population into quintiles or deciles based on the PS. Analyze outcomes within each stratum.
- Choose one of the following primary methods:
Assessing Covariate Balance
- After applying the PS (via matching, weighting, or stratification), assess the balance of all pre-treatment covariates between the treatment groups.
- Use standardized mean differences (SMD), where a value < 0.1 after adjustment generally indicates good balance. Visually inspect the distribution of covariates and PS before and after adjustment.
Outcome Analysis
- In the balanced sample (matched, weighted, or stratified), estimate the association between treatment and the safety outcome.
- For time-to-event outcomes (e.g., time to GI bleed), use a Cox proportional hazards model. For binary outcomes, use a logistic model. Incorporate the PS method used (e.g., use a robust variance estimator for IPTW models; include stratification variables in the outcome model).
Sensitivity Analysis
- Conduct analyses to assess the robustness of findings, such as using different PS models, calipers for matching, or accounting for unmeasured confounding.
The workflow for this protocol is summarized in the diagram below.
The Scientist's Toolkit: Essential Reagents & Materials
Successful implementation of propensity score analyses requires both conceptual and technical tools. The following table details key "research reagents" for this field.
Table 2: Essential Research Reagents for Propensity Score Analysis
| Item / Concept | Category | Function / Explanation |
|---|---|---|
| High-Dimensional Propensity Score (hdPS) | Algorithm | An automated algorithm to select and adjust for a large number of candidate covariates from administrative databases, acting as a proxy to reduce unmeasured confounding [1]. |
| Standardized Mean Difference (SMD) | Diagnostic Metric | A statistical measure used to quantify the balance of a covariate between treatment groups after PS application, independent of sample size. An SMD <0.1 indicates good balance. |
| Inverse Probability of Treatment Weighting (IPTW) | PS Application Method | A weighting technique that creates a pseudo-population where the distribution of measured covariates is independent of treatment assignment, allowing for direct estimation of marginal risk differences [28]. |
| Stable Unit Treatment Value Assumption (SUTVA) | Core Assumption | The fundamental assumption that one patient's outcome is unaffected by the treatment assignment of another patient, and that there is only one version of each treatment [1] [28]. |
| Estimand Framework (ICH E9(R1)) | Regulatory & Conceptual Framework | A structured approach to ensure alignment between a study's objective and its design, analysis, and interpretation. It precisely defines how to handle intercurrent events (e.g., treatment discontinuation) when estimating the treatment effect [95]. |
Advanced Application: Integrating the Estimand Framework
Modern pharmacoepidemiology is moving towards integrating the ICH E9(R1) estimand framework with established causal inference methods like propensity scores. This integration brings clarity to the definition of the causal question, particularly regarding intercurrent events (ICEs) [95].
An ICE-handling strategy must be pre-specified. The following diagram illustrates the logical relationship between a common ICE, strategies to handle it, and the corresponding scientific question, all within a study employing PS for confounding control.
For example, to answer a question aligned with the treatment policy strategy (addressing the effect of treatment assignment regardless of discontinuation), the outcome analysis would include events that occur after the ICE, with no special adjustment. In contrast, a hypothetical strategy might require the use of complex g-methods like inverse probability of censoring weighting to adjust for post-baseline factors associated with the ICE [95].
The growing use of real-world evidence (RWE) in pharmacoepidemiology has created an urgent need for standardized approaches that ensure methodological rigor and reproducibility. Simultaneously, advances in propensity score (PS) methods have provided powerful tools to address confounding in observational studies, but their application remains inconsistent. This application note explores the integration of two harmonized protocol templates—STaRT-RWE and HARPER—with advanced propensity score methods to create a robust framework for generating reliable real-world evidence on treatment effects. These frameworks address critical gaps in transparency and reproducibility while providing structured guidance for implementing complex confounding adjustment techniques [97] [98] [99].
The synergy between standardized protocols and sophisticated analytic methods represents a path forward for pharmacoepidemiological research. By embedding advanced propensity score techniques within structured research protocols, investigators can enhance study validity, improve communication of methodological choices, and strengthen the evidence base for healthcare decision-making [4] [41].
Understanding the Protocol Frameworks
The STaRT-RWE Framework
The Structured Template for Planning and Reporting on the Implementation of Real World Evidence Studies (STaRT-RWE) was developed by a public-private consortium to guide the design and conduct of reproducible RWE studies. This template serves as a comprehensive tool for communicating study methods with sufficient specificity to reduce misinterpretation [98]. The framework is compatible with multiple study designs, data sources, reporting guidelines, and bias assessment tools, making it particularly valuable for complex pharmacoepidemiologic studies investigating treatment safety and effectiveness.
STaRT-RWE addresses a critical need in the field, as evidenced by a recent systematic review which uncovered significant deficiencies in RWE study reporting. This review found that studies inadequately reported empirically defined covariates, power and sample size calculation, attrition, sensitivity analyses, and other key methodological parameters [100]. By providing a structured approach to documenting these elements, STaRT-RWE has the potential to substantially improve the robustness and credibility of RWE studies.
The HARPER Template
The HARmonized Protocol Template to Enhance Reproducibility (HARPER) emerged from a joint task force convened by the International Society for Pharmacoepidemiology (ISPE) and ISPOR–The Professional Society for Health Economics and Outcomes Research. This template builds upon existing efforts, including STaRT-RWE, to create a harmonized protocol structure specifically for RWE studies that evaluate treatment effects [97] [101] [99].
HARPER is designed to create a shared understanding of intended scientific decisions through a common text, tabular, and visual structure. The template's over-arching principle is to achieve sufficient clarity regarding data, design, analysis, and implementation to help investigators thoroughly consider and document their choices and rationale for key study parameters that define the causal question [99]. The template includes nine main sections with structured free text, tables, and figures, encouraging researchers to provide context and rationale for investigative decisions [101].
Table: Comparison of STaRT-RWE and HARPER Protocol Templates
| Feature | STaRT-RWE | HARPER |
|---|---|---|
| Developer | Public-private consortium | Joint ISPE/ISPOR Task Force |
| Primary Focus | Planning and reporting RWE studies | Enhancing reproducibility of RWE studies |
| Structure | Guided template with tables, design diagram | Common text, tabular, and visual structure |
| Key Innovation | Library of published studies | Integration of rationale and context for decisions |
| Compatibility | Multiple study designs, data sources | Builds on existing templates including STaRT-RWE |
| Implementation Status | Used for critical appraisal of published studies | Pilot testing with international stakeholders |
The Role of Standardized Protocols in Propensity Score Applications
Addressing Methodological Heterogeneity
Standardized protocols like STaRT-RWE and HARPER play a crucial role in addressing the methodological heterogeneity that currently plagues propensity score applications in pharmacoepidemiology. These templates provide structured guidance for documenting key decisions in the propensity score process, including variable selection, model specification, and implementation approach (matching, weighting, or stratification) [102].
Recent research demonstrates the significant impact of propensity score methodological choices on study results. For example, a 2025 study compared various dimensionality reduction techniques for propensity score estimation in high-dimensional claims data and found that autoencoder-based PS achieved the best covariate balance (8 covariates with SMD > 0.1), followed by principal component analysis (PCA) (20 covariates), logistic PCA (25 covariates), high-dimensional propensity score (hdPS) (37 covariates), and investigator-specified approaches (83 covariates) [4]. Without standardized documentation of these methodological choices, as facilitated by STaRT-RWE and HARPER, comparing results across studies and assessing their validity becomes challenging.
Enhancing Causal Inference Transparency
The HARPER template specifically enhances transparency in causal inference by requiring researchers to explicitly define their target estimand and align their analytic methods with this causal question [102] [41]. This is particularly important for propensity score weighting methods, where different approaches target different populations and estimands.
For example, overlap weighting has gained popularity for its ability to produce bounded, stable weights and achieve exact mean covariate balance. However, this method specifically targets the average treatment effect in the overlap population (ATO)—a statistically defined subgroup of patients with overlapping treatment probabilities near 0.5, those considered to be in clinical equipoise [41]. The HARPER protocol requires researchers to explicitly justify why this estimand is appropriate for their research question, preventing misinterpretation of results that may not be generalizable to the entire study population.
Advanced Propensity Score Methods: Case Studies and Protocols
Dimensionality Reduction Techniques for Propensity Scores
High-dimensional healthcare data presents both opportunities and challenges for propensity score estimation. A 2025 cohort study compared various dimensionality reduction techniques for improving propensity score specification when studying the association between dialysis and mortality in older patients with heart failure and advanced chronic kidney disease [4].
Table: Performance Comparison of Propensity Score Methods in Achieving Covariate Balance
| Propensity Score Method | Covariates with SMD > 0.1 | Key Features | Applications |
|---|---|---|---|
| Autoencoder-based PS | 8 | Best performance in covariate balance | High-dimensional claims data |
| Principal Component Analysis (PCA) | 20 | Linear dimensionality reduction | Large-scale pharmacoepidemiology |
| Logistic PCA | 25 | Nonlinear dimension reduction | Complex confounding patterns |
| High-dimensional Propensity Score (hdPS) | 37 | Automated variable selection | Routine healthcare data |
| Investigator-specified | 83 | Subject-matter knowledge | Targeted confounding adjustment |
The study utilized Optum's de-identified Clinformatics Data Mart Database and included 485 dialysis-exposed and 1455 unexposed individuals after matching. While hazard ratios for in-hospital mortality were similar across PS methods, the substantial differences in achieved covariate balance highlight the importance of method selection and documentation [4].
Experimental Protocol: Autoencoder-Based Propensity Score Estimation
Research Reagent Solutions:
- Data Source: Optum's de-identified Clinformatics Data Mart Database or equivalent claims data
- Software: R or Python with keras/tensorflow for autoencoder implementation
- Balance Assessment: Standardized Mean Differences (SMD) calculation package
- Matching Algorithm: Optimal matching with caliper restriction
Methodology:
- Data Preparation: Structure data according to the OMOP Common Data Model or similar standardized structure
- Feature Selection: Identify high-dimensional covariates including diagnoses, procedures, medications
- Autoencoder Architecture: Implement a symmetric neural network with bottleneck layer for dimensionality reduction
- Propensity Score Estimation: Train logistic regression model using encoded features as inputs
- Matching: Perform 1:3 matching without replacement using nearest neighbor algorithm
- Balance Assessment: Calculate SMD for all covariates before and after matching
- Outcome Analysis: Apply Cox proportional hazards model to estimate hazard ratios
This protocol can be documented within the HARPER template's "Data Analysis" section, with detailed rationale provided for each architectural decision and parameter specification [4] [102].
Addressing Complex Biases with Integrated Designs
Advanced propensity score applications often require integrated designs to address multiple biases simultaneously. A 2025 study in multiple sclerosis research implemented a high-dimensional propensity score approach within a nested case-control framework to address both immortal time bias and residual confounding when examining the relationship between disease-modifying drugs and all-cause mortality [6].
The study used a retrospective cohort of 19,360 individuals with multiple sclerosis in British Columbia, Canada. The nested case-control analysis addressed immortal time bias, while hdPS was applied to handle residual confounding. This integrated approach demonstrated a 28% reduction in mortality risk associated with exposure to DMDs (HR: 0.72, 95% CI: 0.62-0.84) [6].
Diagram: Integrated NCC-hdPS Framework for Addressing Multiple Biases
Experimental Protocol: Integrated NCC-hdPS Design
Research Reagent Solutions:
- Cohort Data: Retrospective cohort with comprehensive follow-up (e.g., administrative claims, electronic health records)
- hdPS Algorithm: Automated variable selection for confounder identification
- Matching Framework: Incidence density sampling for case-control selection
- Sensitivity Analysis Package: Multiple parameter specifications for robustness testing
Methodology:
- Cohort Definition: Apply inclusion/exclusion criteria to define study population
- Case Identification: Identify all cases with outcome of interest during follow-up
- Control Sampling: Select up to 4 controls per case using incidence density sampling
- hdPS Implementation:
- Identify candidate covariates from data dimensions (diagnoses, procedures, medications)
- Apply predetermined algorithm for variable prioritization
- Estimate propensity scores using selected covariates
- Matching: Implement propensity score matching within NCC framework
- Outcome Analysis: Conditional logistic regression to estimate odds ratios
- Sensitivity Analyses: Test robustness across different hdPS parameters and matching strategies
This integrated design can be comprehensively documented using the STaRT-RWE template's structured approach to study design specification, particularly through the use of design diagrams and detailed variable definitions [6] [98].
Implementation Framework: Integrating Advanced Methods with Standardized Protocols
Structured Documentation of Propensity Score Workflows
The integration of advanced propensity score methods with standardized protocols requires systematic documentation of key methodological decisions. The HARPER template provides specific sections for this purpose, enabling researchers to clearly communicate their analytic choices and the rationale behind them [102].
Table: HARPER Template Sections for Propensity Score Documentation
| HARPER Section | Propensity Score Application | Documentation Requirements |
|---|---|---|
| Research Question | Target estimand definition | Specify whether estimating ATE, ATT, or ATO |
| Variables | Confounding variables | Rationale for covariate selection approach |
| Data Analysis | PS estimation and implementation | Detailed specification of model and matching/weighting |
| Sensitivity Analyses | Methodological robustness | Alternative PS specifications or implementations |
| Limitations | Positivity violations and model misspecification | Assessment of PS method limitations |
For overlap weighting specifically, researchers should document:
- The explicit justification for targeting the ATO
- Characteristics of both the unweighted and overlap-weighted populations
- Assessment of the clinical interpretability of the overlap population
- Comparison with other weighting methods when appropriate [41]
Visualizing the Integrated Framework
The STaRT-RWE template emphasizes the use of visualizations to communicate study design, an approach that can be extended to propensity score workflows.
Diagram: Integrated PS-Protocol Framework for RWE Studies
The integration of STaRT-RWE and HARPER protocol templates with advanced propensity score methods represents a significant advancement for pharmacoepidemiological research. These harmonized frameworks provide the structure necessary to ensure methodological transparency, enhance reproducibility, and facilitate critical appraisal of study validity. As propensity score methods continue to evolve in complexity—from dimensionality reduction techniques to integrated bias-reduction designs—standardized protocols offer the foundation for their responsible implementation and clear communication.
The path forward requires widespread adoption of these templates throughout the research community, along with continued refinement based on implementation experience. By embedding advanced propensity score applications within these structured frameworks, researchers can generate more reliable real-world evidence capable of informing healthcare decisions with greater confidence.
Conclusion
Propensity score methods are indispensable tools for mitigating confounding and strengthening causal inference in pharmacoepidemiology. When grounded in robust design principles like the new-user design and carefully executed through matching, weighting, or advanced techniques like hdPS, they can yield estimates that more closely approximate those from randomized trials. Success hinges on rigorous balance assessment, thoughtful handling of intercurrent events, and transparency in reporting. Future progress lies in the continued integration of machine learning for variable selection, broader adoption of formalized frameworks like ICH E9(R1) and target trial emulation, and the development of robust methods to address unmeasured confounding. Embracing these practices and directions will enhance the credibility and utility of real-world evidence for informing drug safety and regulatory decision-making.
References
- 1. Propensity Scores in Pharmacoepidemiology - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5810585/]
- 2. Frontiers | Propensity Methods in Health Technology... Score [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2019.00973/full]
- 3. Propensity scores for confounder adjustment when assessing ... [https://pubmed.ncbi.nlm.nih.gov/24520806/]
- 4. An Application to a Cohort Study Using Claims Data [https://pubmed.ncbi.nlm.nih.gov/41285559/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1PIb741EQUeidKmML9QHq2Wbd0FMv0mQJnDdTPnuZ5mW3ju5O&fc=None&ff=20251125031343&v=2.18.0.post22+67771e2]
- 5. in Pharmacoepidemiology: Beyond the Horizon Propensity Scores [https://link.springer.com/article/10.1007/s40471-017-0131-y]
- 6. A Case Study of a High-Dimensional Propensity Score ... [https://pubmed.ncbi.nlm.nih.gov/40552744/]
- 7. Propensity Score Matching: Identifying Opportunities for ... [https://www.mdpi.com/2039-4403/15/5/142]
- 8. for Indications and review of their use in... propensity scores [https://pubmed.ncbi.nlm.nih.gov/16611199/]
- 9. Chapter 4 Potential Outcomes Framework | Causal Inference ... [https://alexdeng.github.io/causal/rcm.html]
- 10. An Introduction to Propensity Score Methods for Reducing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3144483/]
- 11. The application of propensity score methods in ... [https://www.frontiersin.org/journals/applied-mathematics-and-statistics/articles/10.3389/fams.2024.1384217/full]
- 12. Eight basic rules for causal inference [https://pedermisager.org/blog/seven_basic_rules_for_causal_inference/]
- 13. 04 - Graphical Causal Models - Matheus Facure [https://matheusfacure.github.io/python-causality-handbook/04-Graphical-Causal-Models.html]
- 14. Editorial Propensity score methods in observational research [https://www.sciencedirect.com/science/article/pii/S0007091223003604]
- 15. Methods in causal inference. Part 1: causal and... diagrams [https://pmc.ncbi.nlm.nih.gov/articles/PMC11588567/]
- 16. Average treatment effect [https://en.wikipedia.org/wiki/Average_treatment_effect]
- 17. for comparative studies: a tutorial with... Propensity score matching [https://pmc.ncbi.nlm.nih.gov/articles/PMC11187614/]
- 18. Sample average treatment effect on the treated ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/38057320/]
- 19. Transporting treatment effects from difference-in- ... [https://arxiv.org/html/2310.17806v2]
- 20. DAGitty - drawing and analyzing causal diagrams (DAGs) [https://www.dagitty.net/]
- 21. Pharmacoepidemiology Research-Real-World Evidence ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2021.723427/full]
- 22. Active-comparator design and new-user ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4486631/]
- 23. Concepts of Designing and Implementing ... [https://www.sciencedirect.com/science/article/pii/S2667026723000528]
- 24. The active comparator, new user study design in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4778958/]
- 25. The Active Comparator, New User Study Design in ... [https://link.springer.com/article/10.1007/s40471-015-0053-5]
- 26. Chapter 4: Study design - ENCePP - European Union [https://encepp.europa.eu/encepp-toolkit/methodological-guide/chapter-4-study-design_en]
- 27. Fundamentals of the cohort and case–control study designs [https://pmc.ncbi.nlm.nih.gov/articles/PMC9545534/]
- 28. Research and scholarly methods: Propensity scores - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9980423/]
- 29. Core concepts in pharmacoepidemiology: Key biases arising ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10204604/]
- 30. Addressing the issue of channeling bias in observational ... [https://www.sciencedirect.com/science/article/abs/pii/S1551741105001300]
- 31. Bias in pharmacoepidemiologic studies using secondary ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-019-0695-y]
- 32. Immortal time bias in pharmaco-epidemiology [https://pubmed.ncbi.nlm.nih.gov/18056625/]
- 33. Immortal time bias [https://catalogofbias.org/biases/immortal-time-bias/]
- 34. Immortal time bias in pharmacoepidemiological studies [https://pubmed.ncbi.nlm.nih.gov/25487848/]
- 35. Chapter 6: Methods to address bias and confounding - ENCePP [https://encepp.europa.eu/encepp-toolkit/methodological-guide/chapter-6-methods-address-bias-and-confounding_en]
- 36. Improving Propensity in Pharmacoepidemiology Score Methods [https://dspace.library.uu.nl/handle/1874/298481]
- 37. in Pharmacoepidemiology: Beyond the Horizon Propensity Scores [https://pubmed.ncbi.nlm.nih.gov/29456922/]
- 38. Use of Machine Learning to Compare Disease Risk Scores ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12130674/]
- 39. a plasmode simulation and real-world data cohort analysis [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1395707/full]
- 40. Prognostic score-based model averaging approach for ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02350-y]
- 41. When and why to use overlap weighting: clarifying its role ... [https://www.sciencedirect.com/science/article/pii/S0895435625002756]
- 42. A Case Study of a Highâ€Dimensional Propensity Score ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12186589/]
- 43. Best (but oft-forgotten) practices: propensity score methods ... [https://www.sciencedirect.com/science/article/pii/S0002916522045361]
- 44. Comparison of Propensity Score Methods and Covariate ... [https://www.sciencedirect.com/science/article/pii/S073510971637036X]
- 45. Highâ€dimensional propensity scores for empirical covariate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10099872/]
- 46. Is there a competitive advantage to using multivariate ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0324639]
- 47. Transparency of highâ€dimensional propensity score analyses [https://pmc.ncbi.nlm.nih.gov/articles/PMC9305520/]
- 48. A methodological review of the high-dimensional ... [https://www.sciencedirect.com/science/article/pii/S089543562400060X]
- 49. Propensity score analysis for time-dependent exposure [https://pmc.ncbi.nlm.nih.gov/articles/PMC7154493/]
- 50. Review of Recent Pharmacoepidemiologic Post-Market ... [https://link.springer.com/article/10.1007/s43441-025-00780-4]
- 51. II: the Pharmacoepidemiology - nested study--a novel... case control [https://scispace.com/papers/pharmacoepidemiology-ii-the-nested-case-control-study-a-s2y1zxdaa0]
- 52. Application of the matched nested case-control design to the ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-020-01007-w]
- 53. Comparison of cohort and nested case-control designs for ... [https://pubmed.ncbi.nlm.nih.gov/36846937/]
- 54. Time-Dependent Propensity Score for Assessing the Effect ... [https://www.semanticscholar.org/paper/Time-Dependent-Propensity-Score-for-Assessing-the-Xu-Luo/f6317becfd7cc3236ba5526dc542bf71c8ab9626]
- 55. Propensity Score Matching: should we use it in designing ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02481-w]
- 56. Evaluation of Machine Learning-Based Propensity Score ... [https://www.medrxiv.org/content/10.1101/2025.06.16.25329708v1]
- 57. Creating and Testing Methods to Estimate Treatment Effect in ... [https://www.ncbi.nlm.nih.gov/books/NBK593642/]
- 58. Propensity score matching [https://en.wikipedia.org/wiki/Propensity_score_matching]
- 59. Examining the Propensity Score Matching Paradox [https://iqss.github.io/MatchingFrontier/articles/psm-paradox.html]
- 60. Why Propensity Scores Should Not Be Used for Matching [https://gking.harvard.edu/publications/why-propensity-scores-should-not-be-used-formatching]
- 61. Implications of the Propensity Score Matching Paradox in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6118075/]
- 62. Methodological considerations in pharmacoepidemiology and... [https://research.monash.edu/en/publications/methodological-considerations-in-pharmacoepidemiology-and-pharmac]
- 63. Propensity Score Matching: should we use it in designing ... [https://pubmed.ncbi.nlm.nih.gov/39875810/]
- 64. Balance diagnostics after propensity score matching - Zhang [https://atm.amegroups.org/article/view/22865/html]
- 65. Optimal caliper widths for propensity-score matching when ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3120982/]
- 66. Matching Methods for Confounder Adjustment - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9005055/]
- 67. Streamlining Propensity Score Adjustment with Substantiate [https://evidence-hub.aetion.com/feature-spotlight-streamlining-propensity-score-adjustment-with-substantiate]
- 68. Optimal Caliper Width for Propensity Score Matching of Three ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0081045]
- 69. Instability of estimation results based on caliper matching with ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0325317]
- 70. Treatment patterns, healthcare resource utilization, and costs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5477263/]
- 71. Treatment patterns and characteristics of patients with Post ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0309704]
- 72. Propensity scores using missingness pattern information [https://pmc.ncbi.nlm.nih.gov/articles/PMC7612316/]
- 73. An Application to a Cohort Study Using Claims Data [https://pubmed.ncbi.nlm.nih.gov/41285559/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0MUDgoX_3AKQ_8FjIHbDSim-inHbHvZmzgZIOj5My8q&fc=None&ff=20251125130633&v=2.18.0.post22+67771e2]
- 74. A framework for inferring and analyzing pharmacotherapy ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-024-02469-4]
- 75. Estimands in Oncology Trials | PPD [https://www.ppd.com/blog/estimands-oncology-trials/]
- 76. The use of propensity score methods with survival or time-to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4285179/]
- 77. Estimating treatment effects with competing intercurrent ... [https://arxiv.org/html/2503.03049v2]
- 78. Associations between intercurrent and cardiorenal clinical... events [https://pmc.ncbi.nlm.nih.gov/articles/PMC11984034/]
- 79. Variable selection for propensity score models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1513192/]
- 80. Propensity score model overfitting led to inflated variance of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5756087/]
- 81. Tools & Techniques - Statistics: Propensity score techniques [https://eurointervention.pcronline.com/article/tools-amp-techniques-statistics-propensity-score-techniques]
- 82. When should one use Propensity Matching instead of... Score [https://stats.stackexchange.com/questions/551704/when-should-one-use-propensity-score-matching-instead-of-instrumental-variables]
- 83. Is it possible of overfit using Propensity score matching with ... [https://stats.stackexchange.com/questions/429033/is-it-possible-of-overfit-using-propensity-score-matching-with-the-matchit-r-pac]
- 84. Balance diagnostics for comparing the distribution of baseline ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3472075/]
- 85. Methods for Constructing and Assessing Propensity Scores [https://pmc.ncbi.nlm.nih.gov/articles/PMC4213057/]
- 86. Assessing Covariate Balance with Small Sample Sizes [https://www.medrxiv.org/content/10.1101/2024.04.23.24306230v1.full-text]
- 87. Creating Data Visualizations to Assess Covariate Balance ... [https://dlab.berkeley.edu/news/propensity-score-matching-causal-inference-creating-data-visualizations-assess-covariate]
- 88. Target Trial Emulation: A Concept Simply Explained [https://pubmed.ncbi.nlm.nih.gov/39937060/]
- 89. E9(R1) Statistical Principles for Clinical Trials: Addendum [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/e9r1-statistical-principles-clinical-trials-addendum-estimands-and-sensitivity-analysis-clinical]
- 90. Comparing Propensity Score Methods Versus Traditional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7713675/]
- 91. Propensity score matching with R: conventional methods and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8246231/]
- 92. How are propensity scores different from adding covariates ... [https://stats.stackexchange.com/questions/8604/how-are-propensity-scores-different-from-adding-covariates-in-a-regression-and]
- 93. Artificial Intelligence in Pharmacoepidemiology [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.568659/full]
- 94. Propensity score matching with R: conventional methods and ... [https://atm.amegroups.org/article/view/61857/html]
- 95. Review of Recent Pharmacoepidemiologic Post-Market ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446131/]
- 96. Review of Recent Pharmacoepidemiologic Post-Market ... [https://pubmed.ncbi.nlm.nih.gov/40425936/]
- 97. HARmonized Protocol Template to Enhance ... [https://www.ispor.org/heor-resources/good-practices/article/harmonized-protocol-template-to-enhance-reproducibility-of-hypothesis-evaluating-real-world-evidence-studies-on-treatment-effects]
- 98. STaRT-RWE: structured template for planning and ... [https://pubmed.ncbi.nlm.nih.gov/33436424/]
- 99. ISPOR Report HARmonized Protocol Template to Enhance ... [https://www.sciencedirect.com/science/article/pii/S1098301522021532]
- 100. Use of Structured Template and Reporting Tool for Real ... [https://www.sciencedirect.com/science/article/pii/S1098301522021799]
- 101. The HARmonized Protocol Template to Enhance ... [https://marksmanhealthcare.com/2023/05/15/the-harmonized-protocol-template-to-enhance-reproducibility-harper-in-rwe/]
- 102. HARPER - Study protocol [https://drugepi.gitlab-pages.partners.org/harper/protocol/Quarto_template/protocol.html]