Optimizing Cancer Combination Therapy: A Comprehensive Guide to Scheduling with Optimal Control Theory
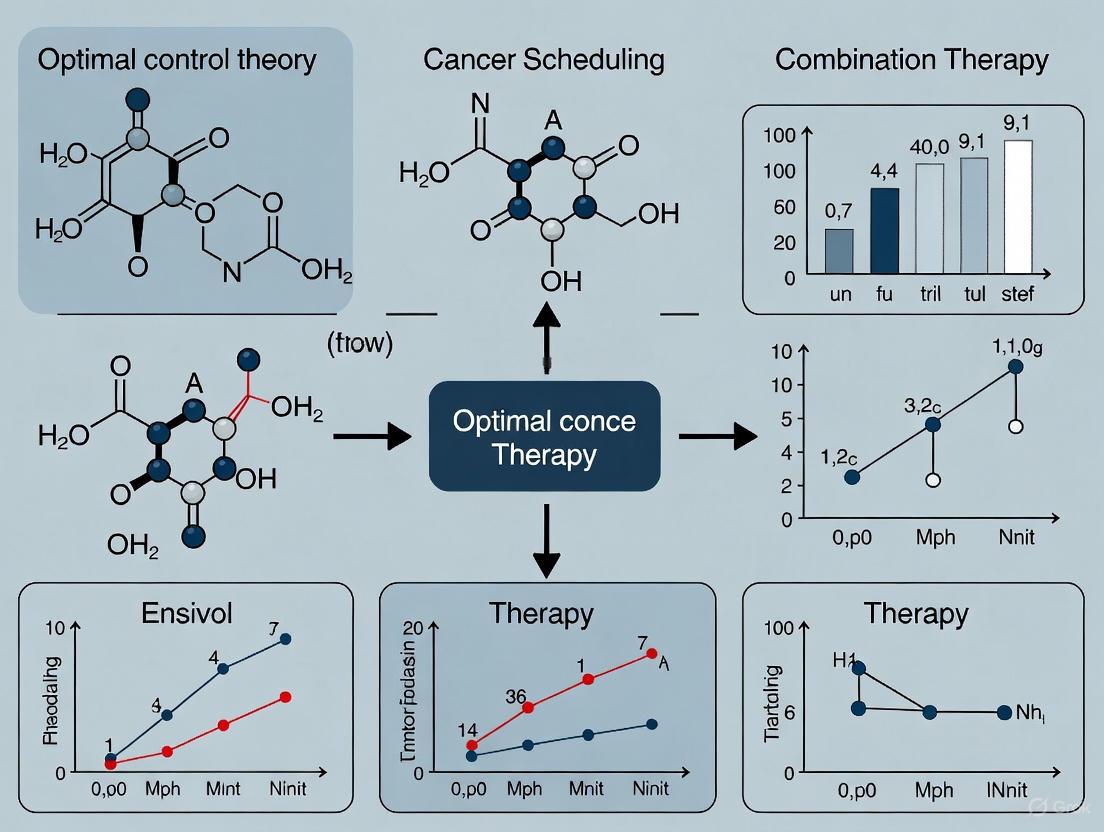
This article provides a comprehensive overview of the application of Optimal Control Theory (OCT) to optimize the scheduling of cancer combination therapies.
Optimizing Cancer Combination Therapy: A Comprehensive Guide to Scheduling with Optimal Control Theory
Abstract
This article provides a comprehensive overview of the application of Optimal Control Theory (OCT) to optimize the scheduling of cancer combination therapies. Tailored for researchers, scientists, and drug development professionals, it explores the foundational mathematical principles of OCT and its use in designing personalized treatment regimens. The content delves into methodological advances, including the use of ordinary differential equation (ODE) models and pan-cancer signaling pathways to simulate tumor dynamics and predict treatment responses. It addresses key challenges such as managing toxicity, overcoming drug resistance, and accounting for patient heterogeneity. Furthermore, the article reviews validation techniques and comparative analyses of different OCT strategies, highlighting their potential to improve therapeutic efficacy, minimize side effects, and pave the way for more precise and effective cancer treatments.
The Foundation of Optimal Control in Oncology: From Basic Principles to Modern Combination Therapy
Core Concepts of Optimal Control Theory
Optimal Control Theory (OCT) is a mathematical framework for determining how to steer a dynamic system over time to optimize a specific performance criterion while adhering to system constraints [1]. It bridges the gap between theory and practice, allowing for the solving of complex problems by finding the best control inputs over time [2].
Fundamental Problem Formulation
Formally, an optimal control problem aims to minimize a cost functional [1] [3]: [ J[x(·),u(·),t0,tf] := E[x(t0),t0,x(tf),tf] + \int{t0}^{t_f} F[x(t),u(t),t] dt ] This is subject to the system's dynamic constraints: [ \dot{x}(t) = f[x(t),u(t),t], ] as well as any path and boundary constraints [1]. In this formulation:
- ( x(t) ) represents the state variables (e.g., tumor cell count, immune cell concentration) [2] [3].
- ( u(t) ) represents the control inputs (e.g., drug dosage, radiation intensity) [2] [3].
- The function ( F ) quantifies the running cost (e.g., transient tumor size, drug toxicity), while ( E ) is the terminal cost [1].
Key Mathematical Principles
Two primary methods for solving these problems are:
- Pontryagin's Maximum Principle: This necessary condition leads to a Pontryagin system, which introduces co-state variables ((λ)) that represent the marginal value of the state variables [1] [4]. The solution involves defining a Hamiltonian function ( H = F + λ^T f ) and finding the control that minimizes ( H ) at each point in time [2] [4].
- Hamilton-Jacobi-Bellman Equation: This provides a sufficient condition for optimality via dynamic programming [1].
The following diagram illustrates the workflow for deriving an optimal control using Pontryagin's Maximum Principle.
OCT in Cancer Therapy: FAQs & Troubleshooting
FAQ: Core Concepts
What makes OCT suitable for cancer therapy optimization? Cancer is a dynamic system where tumor cells evolve and interact with treatments and the immune system. OCT provides a rigorous framework to compute the best therapeutic regimen—optimizing the timing, dosage, and combination of treatments to maximize tumor cell kill while minimizing toxicity to healthy tissues [5] [3]. It allows for the in-silico testing of numerous alternative regimens that are impossible to systematically evaluate in clinical trials [5].
How is a cancer treatment problem formally translated into an OCT problem?
- State Variables (x(t)): Quantities describing the system's state (e.g., populations of cancer cells, immune cells like CD8+ T cells, and healthy tissue cells) [6] [3].
- Control Inputs (u(t)): Adjustable therapy parameters (e.g., doses of chemotherapy, immunotherapy, or radiation) [5] [3].
- Dynamics (f): A system of differential equations modeling the interactions between state variables and controls [3].
- Cost Functional (J): A mathematical expression balancing treatment goals (e.g., minimize tumor size and treatment toxicity over time) [3].
What are the main types of control strategies used?
- Open-Loop Control: The optimal treatment schedule is computed upfront for the entire treatment period. It is sensitive to model inaccuracies.
- Closed-Loop (Feedback) Control: The treatment plan is adjusted in real-time based on frequent measurements of the patient's response (e.g., via biomarkers or imaging), making it more robust to uncertainties [6].
Troubleshooting Guide: Common Computational Challenges
Problem: Model Predictions Diverge from Expected Biological Behavior
- Potential Cause 1: Poorly Calibrated Model Parameters. The mathematical model's parameters (e.g., cell growth/death rates) are not accurately tuned to represent a specific patient's tumor biology.
- Solution: Increase the use of patient-specific data for calibration. Utilize longitudinal data (e.g., from quantitative imaging or circulating tumor DNA (ctDNA) assays) to inform and adjust the model parameters [5] [7].
- Potential Cause 2: Oversimplified System Dynamics. The model may lack crucial biological mechanisms, such as drug resistance, immune suppression, or spatial heterogeneity.
- Solution: Develop multiscale models that incorporate additional layers of biology, such as intracellular signaling networks or the tumor microenvironment [5]. Consider using spatial transcriptomics or single-cell sequencing data to inform these models [7].
Problem: Optimization Fails to Converge or Yields Impractical Solutions
- Potential Cause 1: Violation of Physical Constraints. The computed control may suggest drug doses that are toxic or physically impossible to administer.
- Solution: Re-formulate the problem with hard constraints on the maximum dose per fraction (for radiation) or cumulative dose (for chemotherapy) [5] [2] [3]. Explicitly include constraints on healthy tissue toxicity in the cost functional [3].
- Potential Cause 2: Non-convexity of the Optimization Landscape. The problem may have multiple local minima, causing the solver to get stuck in a sub-optimal solution.
- Solution: Employ global optimization algorithms or stochastic methods. Try different initial guesses for the control trajectory to explore the solution space. For nonlinear systems, consider methods like the State-Dependent Riccati Equation (SDRE) [6].
Problem: The Control Strategy is Sensitive to Small Measurement Errors
- Potential Cause: Lack of Observability. Not all critical state variables (e.g., resistant cancer cell sub-populations) can be accurately estimated from available clinical measurements.
- Solution: Perform an observability analysis of your model. Invest in developing and integrating better biomarkers and sensing technologies (e.g., advanced ctDNA analysis) that provide a more complete picture of the tumor state [7] [3].
Experimental Protocols & Data Analysis
Protocol: Applying OCT to a Combination Therapy Model
This protocol outlines the steps for formulating and solving an optimal control problem for cancer combination therapy scheduling.
1. System Identification and Model Formulation:
- Objective: Develop a mathematical model of the tumor-immune-treatment interplay.
- Methodology:
- Select state variables (e.g., sensitive cancer cells, resistant cancer cells, CD8+ T cells, normal tissue cells) [6] [3].
- Based on literature and preclinical data, write a system of ordinary differential equations (ODEs) describing the rates of change for each state variable. Include terms for natural growth/decay, immune-mediated killing, and drug-induced cell death [6] [3].
- For chemotherapy, model the drug effect as proportional to the drug concentration and the cell population size. For immunotherapy, model the activation and proliferation of immune cells [3].
2. Optimal Control Problem Formulation:
- Objective: Define the goal of therapy as a mathematical cost functional.
- Methodology:
- Define the cost functional ( J ). A common form is: ( J = \int{0}^{T} [x{tumor}(t) + w \cdot u^2(t)] dt ) where ( u(t) ) is the drug dose and the weight ( w ) balances the importance of minimizing tumor size versus minimizing cumulative drug toxicity [3].
- Set constraints: Define upper bounds for ( u(t) ) (maximum tolerated dose) and for the nadir of normal tissue cells [3].
3. Numerical Solution and Simulation:
- Objective: Compute the optimal drug administration schedule ( u^*(t) ).
- Methodology:
- Discretize the continuous-time problem for numerical computation.
- Use appropriate numerical solvers. The table below compares several methods used in recent research [6].
Table 1: Comparison of Numerical Methods for Optimal Control
| Method | Description | Key Features |
|---|---|---|
| IPOPT | Interior Point Optimizer | An open-source tool for large-scale nonlinear optimization; suitable for direct transcription methods [6]. |
| SDRE | State-Dependent Riccati Equation | Adapts linear control methods (LQR) for nonlinear systems; provides a suboptimal feedback law [6]. |
| ASRE | Approximate Sequence Riccati Equation | A globally optimal feedback control approach for nonlinear systems [6]. |
4. Validation and Analysis:
- Objective: Assess the performance and robustness of the optimal protocol.
- Methodology:
- Simulate the system dynamics under the computed optimal control.
- Perform sensitivity analysis by perturbing model parameters and initial conditions to test the robustness of the protocol.
- Compare the outcome (e.g., final tumor size, total drug used) against standard-of-care dosing schedules [6].
Quantitative Results from Recent Studies
The following table summarizes sample outcomes from a computational study applying different OCT methods to a cancer therapy model, demonstrating the performance of various controllers in minimizing a defined cost function [6].
Table 2: Sample Performance Metrics from an OCT Study [6]
| Control Method | Cost Value (J) | Final Tumor Cell Count (C) | Final CD8+ T Cell Count (C) |
|---|---|---|---|
| IPOPT | 52.3573 | 0.0007 | 1.6499 |
| SDRE | 52.4240 | 0.0006 | 1.6499 |
| ASRE | 52.4240 | 0.0006 | 1.6499 |
Note: (C) denotes a continuous dosing strategy. The lower cost value for IPOPT indicates a marginally better performance in this specific optimization [6].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for OCT Cancer Therapy Research
| Item / Reagent | Function in OCT Research |
|---|---|
| Ordinary Differential Equation (ODE) Solvers | Software (e.g., in MATLAB, Python's SciPy) to numerically simulate the system dynamics and solve state/costate equations [3]. |
| Nonlinear Programming Solvers | Algorithms (e.g., IPOPT) used in direct methods to solve the discretized optimization problem [6] [2]. |
| Patient-Derived Xenograft (PDX) Models | In-vivo models that provide realistic, patient-specific data for calibrating and validating the biological models [5]. |
| Circulating Tumor DNA (ctDNA) | A liquid biopsy biomarker used to measure tumor burden and response, providing real-time data for feedback control or model validation [7]. |
| Spatial Transcriptomics | Technology to analyze gene expression in the context of tissue architecture, informing models of the tumor microenvironment and heterogeneity [7]. |
| HIV gp120 (318-327) | HIV gp120 (318-327), MF:C48H80N16O12, MW:1073.2 g/mol |
| sGC activator 1 | sGC activator 1, CAS:2101645-33-2, MF:C27H22ClF5N6O3, MW:608.9 g/mol |
Visualizing Therapy Action and Workflow
Many chemotherapeutic agents are cell-cycle specific. The following diagram illustrates the phases of the cell cycle and where different classes of drugs act, which is a critical consideration for building accurate dynamic models [3].
Historical Context and Clinical Limitations of Standard Combination Therapy Schedules
The establishment of standard combination therapy schedules in oncology has been largely shaped by the clinical trial system, which focuses on determining maximum tolerated doses and average efficacy for a population. This approach makes it systematically impossible to evaluate all possible dosing and scheduling options. Consequently, multi-modality treatment policies remain largely empirical, subject to individual clinicians' experience and intuition rather than being derived from rigorous, personalized optimization [5]. The paradigm has historically followed a "stepped care" approach, often initiating treatment with monotherapy, despite evidence that most patients require combination therapy for effective disease control [8]. This guideline-practice gap arises because clinical trials operate under strict protocols with high patient adherence, whereas real-world clinical practice must contend with variable patient compliance and physician concerns about over-treatment [8].
Core Clinical Limitations of Standard Schedules
Therapeutic Inertia and the Guideline-Practice Gap
A significant limitation of standard scheduling is therapeutic inertia. Real-world data demonstrates that once patients are initiated on monotherapy, clinicians rarely intensify treatment even when control is inadequate. A study of 125,635 hypertensive patients revealed that 80.4% were initially prescribed monotherapy. After three years, only 36% of these had been switched to combination therapy, compared to 78% of those who started with combination drugs [8]. This inertia means the initial therapeutic strategy often dictates the final management plan, frequently leading to suboptimal disease control.
Ignoring Scheduling and Sequencing Effects
Preclinical studies demonstrate that the sequence and timing of drug administration significantly impact the emergence of resistance and overall efficacy. Research in triple-negative breast cancer (TNBC) evaluating crizotinib and navitoclax combinations tested 696 sequential and concomitant treatment regimens. The findings revealed that patterns of resistance depend critically on the schedule and sequence in which drugs are given [9]. For example:
- Drug holiday duration significantly influences outcomes. In a two-cycle single-agent navitoclax regimen, increasing recovery periods from 2 days to 10 days between cycles caused a 9-fold increase in viable cells at the end of the second cycle [9].
- Dose proportions in equivalent combinations affect long-term efficacy. Two IC90-equivalent concomitant combinations (1μM navitoclax/1μM crizotinib vs. 0.5μM navitoclax/2.5μM crizotinib) showed dramatically different outcomes over 26 days, with the latter proving more effective at controlling growth and reducing mammosphere formation [9].
One-Size-Fits-All Dosing Paradigms
Systemic therapy dosing typically relies on body surface area (BSA), a practice established over 60 years ago for inter-species dosage extrapolation. However, BSA fails to account for critical factors affecting drug distribution and efficacy, including hepatic and renal function, body composition, enzyme activity, drug resistance, gender, age, and concomitant medications [5]. Consequently, BSA-based dosing does not effectively reduce variability in drug efficacy between patients [5].
Inadequate Consideration of Resistance Evolution
Standard scheduling often fails to account for the eco-evolutionary dynamics of cancer resistance. Treatment is frequently administered continuously until disease progression, effectively applying maximal selective pressure that enriches resistant clones [10]. Feedback mechanisms can be triggered by specific schedules; for instance, certain drug combinations can upregulate anti-apoptotic proteins like Bcl-xL via negative feedback loops, associated with increased phosphorylated AKT and ERK, rendering cells insensitive to retreatment [9].
Table 1: Key Limitations of Standard Combination Therapy Schedules
| Limitation | Clinical Consequence | Supporting Evidence |
|---|---|---|
| Therapeutic Inertia | Delayed treatment intensification leading to inadequate disease control | Only 36% of patients on initial monotherapy switch to combinations within 3 years [8] |
| Fixed Dosing Intervals | Suboptimal drug exposure and recovery periods | 9-fold increase in viable cells with longer drug holidays (2 vs. 10 days) [9] |
| BSA-Based Dosing | High inter-patient variability in efficacy and toxicity | Fails to account for organ function, body composition, and other key factors [5] |
| Ignoring Drug Sequencing | Accelerated emergence of therapeutic resistance | Resistance patterns depend entirely on administration sequence [9] |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Materials for Investigating Therapy Scheduling
| Research Tool | Function in Scheduling Research | Experimental Application |
|---|---|---|
| DNA-Integrated Barcodes | Tracks clonal dynamics and population evolution under different schedules | Identifying resistant subpopulations that emerge under specific sequencing [9] |
| Single-Cell RNA Sequencing (scRNAseq) | Reveals transcriptional patterns linking treatment schedule to resistance mechanisms | Characterizing fitness of individual cell clones under specific treatment schedules [9] |
| siRNA/shRNA Libraries | Identifies synthetic lethal interactions for rational combination design | Genome-wide screens to find novel therapeutic combinations targeting resistance [10] |
| Pharmacokinetic/Pharmacodynamic (PK/PD) Models | Predicts drug concentration and effect relationships for personalized scheduling | In silico optimization of administration schedules based on patient-specific parameters [11] |
| Bruceine J | Bruceine J, MF:C25H32O11, MW:508.5 g/mol | Chemical Reagent |
| Dap-81 | Dap-81, MF:C25H20N6O4, MW:468.5 g/mol | Chemical Reagent |
Experimental Protocols for Scheduling Research
Protocol: Extended In Vitro Scheduling Screen
Background: Standard 3-day viability assays assess killing potential but fail to model schedule-dependent resistance emergence [9].
Methodology:
- Cell Model: MDA-MB-231 triple-negative breast cancer cells.
- Treatment Regimens: Test single agents, sequential administrations, and concomitant combinations.
- Schedule Variations:
- Treatment cycle durations: 1, 2, or 3 days
- Drug-free recovery periods: 2, 5, or 10 days
- Total study duration: 26 days
- Assessment Endpoints:
- Viable cell counts at schedule completion
- Apoptosis rates via flow cytometry
- Clonal dynamics using DNA barcoding
- Transcriptional profiling via scRNAseq
- Analytical Methods:
- Flow cytometric analysis of surface markers (EpCAM, CD24, CD44)
- Mammosphere formation assays for tumorigenicity
- Western blotting for apoptotic regulators (Bcl-xL, pAKT, pERK)
Application: This protocol generated 696 unique treatment conditions, revealing that specific scheduling parameters dramatically influence resistance development and long-term efficacy [9].
Protocol: Markov Decision Process for Treatment Optimization
Background: MDPs provide a mathematical framework for optimizing sequential decisions under uncertainty, ideal for therapy scheduling [12] [13].
Methodology:
- State Space Definition: Patient health states (e.g., responsive, stable, progressive disease) incorporating tumor burden and normal tissue side effects [13].
- Action Space: Treatment options including no treatment, single modalities, or combinations with defined doses [14].
- Transition Probabilities: Calibrated from cohort data or patient-specific models.
- Reward Function: Quality-Adjusted Life Years (QALYs) balancing tumor control against treatment toxicity [12].
- Optimization Algorithm: Dynamic programming to derive policy maximizing discounted expected QALYs.
Application: This approach has been used to determine optimal intervention timing, duration, and sequencing for breast cancer patients, revealing that optimal strategies often differ from standard protocols [14].
Troubleshooting Guides & FAQs
Q: Our in vitro combination shows strong synergy in short-term assays, but fails in longer-term models. What factors should we investigate?
A: Focus on schedule-dependent resistance mechanisms:
- Clonal Evolution: Use DNA barcoding to track whether different administration sequences select for distinct resistant subpopulations [9].
- Feedback Signaling: Analyze adaptive responses in survival pathways (e.g., AKT, ERK phosphorylation) following drug exposure [9].
- Drug Holiday Impact: Systematically vary recovery periods between treatment cycles; even 2-day differences can cause 9-fold changes in viable cell mass [9].
Q: How can we prioritize which of many possible drug combinations to test for schedule optimization?
A: Implement a tiered screening approach:
- Primary Unbiased Screens: Use high-throughput combination screening to identify unexpected synergistic interactions [10].
- Mechanistic Follow-up: Employ siRNA screens to identify synthetic lethal interactions that inform rational combination design [10].
- Computational Prioritization: Apply PK/PD modeling to simulate different scheduling scenarios before laborious experimental testing [11].
Q: What computational approaches best address the multi-dimensional optimization of therapy schedules?
A: Several mathematical frameworks show promise:
- Optimal Control Theory: Formulate therapy design as a control problem aiming to optimize an objective function (e.g., tumor reduction minus toxicity costs) [5] [11].
- Markov Decision Processes: Model treatment as a sequential decision process with states, actions, and rewards to derive optimal policies [12] [13] [14].
- Game-Theoretic Approaches: Model cancer as a reactive player that evolves resistance, enabling strategies that preempt resistance evolution [12].
Signaling Pathways and Experimental Workflows
Treatment Resistance Pathways
Optimal Control Framework
Table 3: Experimental Data on Scheduling Parameters and Outcomes
| Scheduling Parameter | Range Tested | Impact on Outcome | Quantitative Effect |
|---|---|---|---|
| Drug Holiday Duration | 2, 5, 10 days | Viable cell mass | 9-fold increase with longer holidays (2 vs. 10 days) [9] |
| Concomitant Dose Ratio | 1:1 vs. 0.5:2.5 (Nav:Criz) | Long-term growth control | 6-times greater viable cells with suboptimal ratio [9] |
| Treatment Cycle Duration | 1, 2, 3 days | Apoptotic induction | Varies by specific sequence and timing [9] |
| Administration Sequence | Drug A→B vs. B→A | Resistance mechanism | Distinct clonal selection patterns [9] |
This guide provides technical support for researchers implementing control-theoretic frameworks in cancer combination therapy scheduling.
Troubleshooting Guides
Guide 1: System State Model Fails to Reflect Observed Tumor Dynamics
Problem: Your mathematical model, which describes the system state (e.g., tumor cell populations), does not align with experimental or clinical data. The model's predictions are inaccurate.
Solution: Perform rigorous system identification and model validation.
- Troubleshooting Steps:
- Reassess Model Structure: Verify that your model's equations reflect the correct biological phenomena. A common model for heterogeneous tumors uses a system of coupled ordinary differential equations (ODEs) to represent different cell populations (the state vector, x) and their interactions [15].
- Verify Model Observability: Ensure that the system's internal states (e.g., counts of specific cell subpopulations) can be inferred from your available output measurements (e.g., total tumor volume) over time [16].
- Parameter Estimation: Use experimental data to calibrate model parameters (e.g., cell growth rates, drug efficacy coefficients). Employ nonlinear programming techniques and differential equation solvers, such as the Implicit Euler method, to achieve accurate fits [17].
- Validate with New Data: Test the calibrated model against a new, unused dataset to confirm its predictive power.
Related Experiments: The work on constrained optimal control for cancer chemotherapy utilizes discretization and nonlinear programming (e.g., with IPOPT solver) to determine model parameters and extremal solutions that satisfy system constraints [17].
Guide 2: Optimal Control Solution is Computationally Intractable or Yields Counter-Intuitive Dosing
Problem: The algorithm to find the optimal control (drug schedule) fails to converge, takes too long, or suggests a therapy regimen that is clinically impractical (e.g., excessive toxicity).
Solution: Analyze and refine your objective function and control constraints.
- Troubleshooting Steps:
- Inspect the Objective Function: The objective function (or cost function, ( J )) must precisely encode the treatment goal. A typical formulation aims to minimize the tumor cell count at the end of the treatment horizon while penalizing excessive drug usage and toxicity [15] [18]. For example, a linear quadratic regulator (LQR) cost function is of the form ( J{LQR} = \sum ( \mathbf{x}^T Q \mathbf{x} + \mathbf{u}^T R \mathbf{u} ) ), where ( Q ) and ( R ) are weighting matrices that balance the importance of state regulation against control effort [19].
- Check Control Constraints: Ensure that the bounds on your control variables (u), which represent drug doses, are physiologically realistic (e.g., ( 0 \leq uk \leq 1 ), representing the minimum and maximum effective doses) [15].
- Apply Pontryagin's Maximum Principle (PMP): For complex, non-linear systems, PMP is a powerful tool to derive necessary conditions for optimality. This can reveal whether the optimal solution has a "bang-bang" structure (switching between min and max doses) or is a smoother, singular arc [17].
- Simplify the Model: If the system is too complex, consider if a linear or "pseudo-linear" approximation (e.g., using the State-Dependent Riccati Equation approach) is sufficient for your control objectives [19].
Related Experiments: Studies on drug-induced plasticity use PMP to show that the optimal strategy often involves steering the tumor to a fixed equilibrium composition between sensitive and tolerant cells, balancing cell kill against tolerance induction [18].
Guide 3: Therapy Schedule Performs Poorly Against Heterogeneous or Evolving Tumors
Problem: A treatment schedule that is optimal in simulation fails in a real-world context due to tumor heterogeneity, the emergence of drug-resistant clones, or phenotypic plasticity.
Solution: Incorporate evolutionary dynamics and adaptive (closed-loop) control strategies.
- Troubleshooting Steps:
- Expand System States: Augment your state vector to explicitly include multiple cell populations (e.g., drug-sensitive and drug-tolerant/resistant cells) [15] [18]. Model transitions between these states, which may themselves be dependent on drug concentration (u) [18].
- Implement Adaptive Therapy Principles: Shift from a static, open-loop schedule to a closed-loop feedback control system. Design the controller to monitor tumor response (e.g., via biomarkers) and dynamically adjust the dosing (the control input) to maintain a stable tumor burden, exploiting the competitive interference between cell types [20] [21] [22].
- Validate with Evolutionary Models: Test your control strategy using models that integrate evolutionary game theory, where the "fitness" of different cell types determines the outcome of millions of simulated competitions within the tumor ecosystem [21].
Related Experiments: Clinical trials in prostate cancer based on adaptive therapy principles cycle treatment on and off in response to tumor biomarker levels, successfully delaying progression by maintaining a population of therapy-sensitive cells that suppress resistant ones [20].
Frequently Asked Questions
Q1: What is the fundamental difference between open-loop and closed-loop control in therapy scheduling?
- A: In open-loop control (feedforward), the drug administration schedule is pre-determined and does not change based on the patient's response. An example is a fixed three-week chemotherapy cycle [23]. In closed-loop control (feedback), the drug dose is continuously adjusted based on feedback measurements of the process variable (e.g., tumor size or a biomarker). A "closed-loop controller" uses this feedback to minimize the deviation between the desired and actual state [23]. Adaptive therapy is a prime example of a closed-loop strategy in oncology [20].
Q2: How do I decide on the weighting factors in my objective function?
- A: The weighting matrices ( Q ) and ( R ) in an LQR objective function, for instance, are often determined through a combination of sensitivity analysis and clinical intuition. There is no single formula. You should perform a systematic sweep of different weights and observe the resulting trade-off between tumor cell reduction (governed by ( Q )) and drug usage/toxicity (governed by ( R )) [19]. The chosen weights should produce a control trajectory that aligns with clinical priorities.
Q3: My model is highly nonlinear. What control methods are available beyond LQR?
- A: For nonlinear systems, several advanced techniques are available. The State-Dependent Riccati Equation (SDRE) method is a powerful approach that transforms the nonlinear system into a "pseudo-linear" structure, allowing for the application of extended LQR-like techniques at each time step [19]. Another foundational method is the Pontryagin Maximum Principle (PMP), which provides necessary conditions for optimality and is widely used to derive optimal control policies for complex biological systems [17].
Q4: What is a "bang-bang" control solution and when does it occur?
- A: A "bang-bang" control solution is one where the optimal drug dose is always at either its minimum (e.g., zero) or maximum permissible value, switching abruptly between these extremes. This type of solution frequently arises in cancer chemotherapy models when using the Pontryagin Maximum Principle, particularly when the system dynamics and objective function are linear in the control variable [17].
Experimental Data and Models
The table below summarizes key parameters and components from cited control-theoretic experiments in cancer therapy.
Table 1: Key Components of Control-Theoretic Frameworks in Cancer Therapy Research
| Component | Description | Example from Literature |
|---|---|---|
| System States (x) | Variables describing the dynamic system. | Counts of drug-sensitive and drug-tolerant cancer cells [18]; Tumor volume/weight [19]. |
| Control Inputs (u) | Adjustable variables that influence the system. | Effective drug concentration/dose of chemotherapeutic agents [15] [19]. |
| Objective Function (J) | A mathematical expression defining the goal of control. | Minimize tumor cell count at final time + minimize total drug usage/toxicity [18] [19]. |
| Key Parameters | Constants that define system behavior. | Cell growth/death rates (λ, d); Phenotypic transition rates (μ, ν) [18]; Pharmacodynamic parameters [17]. |
| Optimization Method | Algorithm used to find the optimal control. | Pontryagin Maximum Principle (PMP) [17]; Linear Quadratic Regulator (LQR) [19]; State-Dependent Riccati Equation (SDRE) [19]. |
Research Reagent Solutions
Table 2: Essential Materials and Computational Tools for Control-Theoretic Cancer Research
| Item | Function in Research |
|---|---|
| Ordinary Differential Equation (ODE) Systems | The core mathematical model describing the rates of change of tumor cell populations under treatment [17] [15]. |
| Nonlinear Programming Solver (e.g., IPOPT) | Software used to numerically solve optimization problems with nonlinear constraints, such as finding parameters or optimal controls [17]. |
| Applied Modelling Programming Language (AMPL) | An algebraic modeling language for describing and solving large-scale optimization problems [17]. |
| Pontryagin Maximum Principle (PMP) | A fundamental theorem used to derive necessary conditions for an optimal control, often pointing to bang-bang solution structures [17]. |
| State-Dependent Riccati Equation (SDRE) | A method for designing suboptimal controls for nonlinear systems by solving a sequence of algebraic Riccati equations [19]. |
Framework Visualization
The diagram below illustrates the logical structure and information flow of a closed-loop, control-theoretic framework for adaptive cancer therapy.
Diagram 1: Closed-loop control framework for adaptive therapy.
Mathematical Modeling of Tumor-Immune-Treatment Dynamics using Ordinary Differential Equations (ODEs)
Foundational ODE Models for Tumor-Immune Dynamics
Ordinary Differential Equation (ODE) models are a cornerstone for quantifying the complex interactions between tumors, immune cells, and therapeutic agents. The table below summarizes fundamental model structures used in the field [24] [25].
Table 1: Core ODE Model Structures for Tumor-Immune-Treatment Dynamics
| Model Purpose | Exemplary Equations | Key Variables & Parameters | Biological Interpretation |
|---|---|---|---|
| Natural Tumor Growth | dT/dt = k_g * T (Exponential) [25] |
T: Tumor cell population; k_g: Growth rate constant; T_max: Carrying capacity |
Assumes unrestricted growth; often used for early, avascular tumor phases [25]. |
dT/dt = k_g * T * (1 - T/T_max) (Logistic) [25] |
Incorporates self-limiting growth due to environmental constraints like space and nutrients [25]. | ||
| Tumor-Immune Interaction (Predator-Prey) | dT/dt = f(T) - d_1 * I * T [25] |
I: Immune effector cell concentration (e.g., CTLs, NK cells); d_1: Immune-mediated kill rate |
Describes immune cells "preying" on tumor cells. f(T) represents intrinsic tumor growth [24] [25]. |
| Macrophage Polarization | dx_M1/dt = (a_s * x_Ts + a_m1 * x_Th1) * x_M1 * (1 - (x_M1 + x_M2)/β_M) - δ_m1 * x_M1 - k_12 * x_M1 * x_M2 + k_21 * x_M1 * x_M2 [24] |
x_M1/x_M2: M1/M2 macrophage density; k_12, k_21: Phenotype switching rates; β_M: Carrying capacity |
Models dynamic repolarization of macrophages between anti-tumor (M1) and pro-tumor (M2) phenotypes [24]. |
| Treatment & Resistance | dS/dt = f(S) - k_d * Exposure * S - m_1 * S + m_2 * R dR/dt = f(R) + m_1 * S - m_2 * R [25] |
S: Sensitive cell population; R: Resistant cell population; m_1, m_2: Mutation/ reversion rates |
Captures emergence of resistant subpopulations via spontaneous mutation and adaptation during treatment [25]. |
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: My ODE model of tumor-immune interactions becomes unstable, with immune cell populations dropping to zero or growing infinitely. What could be the cause and how can I fix it?
Potential Cause 1: Poorly calibrated parameters. Unrealistic parameter values, especially for proliferation and death rates, can lead to non-physiological dynamics.
- Troubleshooting Guide:
- Sensitivity Analysis: Perform a local or global sensitivity analysis (e.g., using Latin Hypercube Sampling and Partial Rank Correlation Coefficient) to identify which parameters most significantly impact model stability and outputs. Focus calibration efforts on these sensitive parameters [25].
- Literature Calibration: Rigorously search published experimental studies for realistic parameter ranges. For instance, the proliferation rate of Cytotoxic T Lymphocytes (CTLs) upon antigen encounter is a critical parameter that must be within a biologically plausible range [24].
- Steady-State Check: Ensure your model can maintain a non-trivial equilibrium (i.e., a state of tumor-immune dormancy) in the absence of treatment, reflecting the biological concept of immunosurveillance [24].
- Troubleshooting Guide:
Potential Cause 2: Missing a key biological feedback mechanism.
- Troubleshooting Guide:
- Model Auditing: Review your model against the latest literature. A common omission is the role of T regulatory cells (Tregs) which suppress effector immune responses. Adding a term for Treg-mediated suppression of CTLs or NK cells can stabilize models and prevent uncontrolled immune activation [24].
- Include Saturation: Replace simple linear interaction terms (e.g.,
d_1 * I * T) with saturated functional responses (e.g.,(d_1 * I * T) / (h + T)), wherehis a half-saturation constant. This represents the finite capacity of immune cells to kill targets, preventing infinite consumption of tumor cells [24] [25].
- Troubleshooting Guide:
FAQ 2: How can I extend a basic tumor growth ODE model to investigate optimal control theory for combination therapy scheduling?
- Solution: Develop a multi-compartment model with pharmacodynamic interactions.
- Methodology:
- Define Cell Populations: Model the tumor as a heterogeneous system. A minimal framework includes therapy-sensitive cells (
S), therapy-resistant cells (R), and a key immune effector population (I) [25] [26]. - Formulate the ODE System:
Here,
CandRadrepresent chemotherapy and radiotherapy doses,k_Candk_Iare kill rates,m_Sandm_Rare mutation rates, andr(C, Rad)is a treatment-dependent immune recruitment function [26] [27]. - Incorporate Drug Synergy: For combination chemotherapy, model the drug effect
k_Cnot as a constant, but as a function of multiple drug concentrations (u_1,u_2). A general framework can capture synergistic effects where the combined effect is greater than the sum of individual effects [26]. - Apply Optimal Control: Define an objective function (
J) to be minimized, for example:J = ∫ [ w_1*(S+R) + w_2*(C + Rad) ] dtThis balances tumor burden (S+R) against treatment toxicity (C+Rad) over time. Pontryagin's Maximum Principle can then be used to compute the optimal drug dosing schedulesC*(t)andRad*(t)that minimizeJ[26] [27].
- Define Cell Populations: Model the tumor as a heterogeneous system. A minimal framework includes therapy-sensitive cells (
- Methodology:
FAQ 3: When simulating combination therapy, my model predicts that maximum continuous dosing is always optimal. This contradicts clinical practice which uses intermittent schedules. Why?
- Potential Cause: The model lacks key toxicities and constraints.
- Troubleshooting Guide:
- Incorporate Toxicity Compartments: Add an ODE to track the health of a "dose-limiting" tissue (e.g., bone marrow-derived immune cells):
dL/dt = γ * L * (1 - L/L_max) - η_C * C * L - η_Rad * Rad * LImpose a state constraintL(t) > L_criticalthroughout the treatment window. This alone can force the optimal solution to become intermittent, allowingLto recover during drug holidays [27]. - Enforce Realistic Control Constraints: Define maximum tolerable doses per administration (
0 ≤ C(t) ≤ C_max,0 ≤ Rad(t) ≤ Rad_max). Optimal control solutions under these bounded constraints often naturally yield intermittent, or "bang-bang," scheduling to maximize tumor kill while staying within safety limits [26]. - Model Immune Exhaustion: Continuous high antigen load from rapid tumor killing can exhaust T cells. Adding an exhausted T cell compartment that loses cytotoxic function can make continuous dosing suboptimal, favoring schedules that allow immune recovery [24].
- Incorporate Toxicity Compartments: Add an ODE to track the health of a "dose-limiting" tissue (e.g., bone marrow-derived immune cells):
- Troubleshooting Guide:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for ODE Modeling and Validation
| Item/Tool Name | Function/Biological Correlate | Use Case in Modeling Context |
|---|---|---|
| ODE-toolbox (Python) [28] | Solver benchmarking and selection for dynamical systems. | Automates the choice of the most efficient numerical integrator for your specific ODE system, improving simulation speed and reliability. |
| Arbor [28] | High-performance library for multi-compartment cell simulations. | Enables detailed, tissue-scale spatial simulations that can be used to validate predictions from simpler, non-spatial ODE models. |
| BioExcel Building Blocks [28] | Workflows for molecular dynamics of proteins and ligands. | Useful for parameterizing drug-receptor binding kinetics (k_on, k_off) that can inform pharmacodynamic terms in the ODE model. |
| Positive Switched Systems [27] | A control-theoretic framework for scheduling different treatment modalities. | Used to formally determine the optimal switching sequence between radiotherapy and chemotherapy in combined treatment plans. |
| Multiplicative Control Framework [26] | A general ODE model for multi-drug actions on heterogeneous cell populations. | Provides a template for modeling synergistic drug interactions and calculating optimal pharmacodynamic dosing. |
| Sorivudine | Sorivudine, CAS:77181-69-2; 80434-16-8, MF:C11H13BrN2O6, MW:349.13 g/mol | Chemical Reagent |
| Tocainide | Tocainide, CAS:53984-26-2, MF:C11H16N2O, MW:192.26 g/mol | Chemical Reagent |
Visualizing Workflows and Pathways
The following diagrams, generated with Graphviz, illustrate key experimental and conceptual frameworks.
ODE Modeling and Optimal Control Workflow
Diagram 1: ODE Modeling and Control Workflow.
Key Signaling Pathways in Tumor-Immune Context
Diagram 2: Tumor-Immune Signaling Pathways.
Exploring Synergistic and Antagonistic Drug Interactions in Combined Modalities
Quantitative Foundation: Measuring Drug Interactions
Table 1: Key Models for Quantifying Drug Synergy and Antagonism [29] [30]
| Model Name | Type | Formula | Interpretation |
|---|---|---|---|
| Bliss Independence | Effect-based | ( S = E{A+B} - (EA + EB - EA \cdot E_B) ) | S > 0: Synergy; S < 0: Antagonism |
| Loewe Additivity | Dose-effect-based | ( 1 = \frac{DA}{D{x,A}} + \frac{DB}{D{x,B}} ) | CI < 1: Synergy; CI = 1: Additive; CI > 1: Antagonism |
| Combination Index (CI) | Dose-effect-based | ( CI = \frac{C{A,x}}{IC{x,A}} + \frac{C{B,x}}{IC{x,B}} ) | CI < 1: Synergy; CI = 1: Additive; CI > 1: Antagonism |
| HSA | Effect-based | ( S = E{A+B} - \max(EA, E_B) ) | S > 0: Synergy |
Table 2: Prevalence of Synergistic and Antagonistic Interactions in AML Cell Lines (Sample Data) [31]
| Drug Name | Mechanism/Target | Kasumi-1 | HL-60 | TF-1 | K-562 |
|---|---|---|---|---|---|
| Enasidenib | IDH2 inhibitor | High Synergy | High Synergy | Medium Synergy | Low Synergy |
| Venetoclax | BCL-2 inhibitor | High Synergy | Medium Synergy | High Synergy | Antagonism |
| 6-Thioguanine | Purine analog | Antagonism | Antagonism | Antagonism | Antagonism |
| Cytarabine | Antimetabolite | Medium Synergy | Additive | Additive | Antagonism |
Experimental Protocols for Combination Screening
High-Throughput Cell Viability Assay for Drug Pair Screening
This protocol is designed to systematically test 105 drug pairs across multiple cell lines, as described in recent AML studies [31].
Workflow Overview
Detailed Methodology:
Cell Culture and Plating:
- Maintain AML cell lines (e.g., Kasumi-1, HL-60, TF-1) in appropriate media supplemented with 10% FBS and penicillin/streptomycin [31].
- Plate cells in 384-well microtiter plates at optimized densities (e.g., 1,200-10,000 cells/well depending on the cell line) in a total volume of 60 µL per well [31].
- Incubate overnight at 37°C and 5% CO₂.
Drug Preparation and Dispensing:
- Dissolve test compounds in DMSO or aqueous solvent.
- Use an acoustic liquid handler (e.g., Echo555/655) to transfer compounds to 384-well plates [31].
- For combination assays, dose pairs of compounds in an 8x8 grid format, with concentrations determined by the pre-established ICâ‚…â‚€ for each compound.
Incubation and Viability Measurement:
- Incubate plates for 96 hours at 37°C and 5% CO₂.
- Add CellTiter-Glo reagent (diluted 1:2) to each well, mix, and incubate for 5 minutes at room temperature [31].
- Measure luminescence using a multimodal plate reader.
Data Normalization and Analysis:
- Normalize raw luminescence values using the equation: (v{i,j} = \frac{y{i,j} - ni}{pi - ni}), where (y{i,j}) is the measured absorbance, (ni) is the median of negative controls (DMSO), and (pi) is the median of positive controls (e.g., 10 mM BFA) [31].
- Fit dose-response curves using a sigmoid model: (f(x, b{pos}, b{shape}) = \frac{1}{1 + e^{-b{shape} * (x - b{pos})}}), where (x) is the logâ‚‚(drug concentration), (b{pos}) is ICâ‚…â‚€, and (b{shape}) is curve steepness [31].
- Calculate synergy scores using the Bliss Independence or other reference models.
Computational Prediction of Synergistic Combinations
Machine learning frameworks leverage diverse data types to predict drug interactions in silico, accelerating the discovery process [32] [30].
Computational Prediction Workflow
Detailed Methodology:
Data Collection and Annotation:
- Collect large-scale drug combination screening datasets (e.g., O'Neil dataset) [32].
- Annotate drug combinations with generic names, mechanisms of action (MoA), and known targets.
- Integrate multi-omics data for cell lines, including gene expression profiles, copy number variations, and mutation data [30].
Data Preprocessing:
- Perform normalization and standardization of omics data (e.g., log-transformation, batch-effect removal) [30].
- Partition the dataset into stratified training and test sets.
Model Building and Evaluation:
- Construct classification models (e.g., random forests, deep neural networks) to categorize combinations as synergistic, additive, or antagonistic [32].
- Build regression models to predict continuous synergy scores (e.g., CSS scores) [32].
- Evaluate models using cross-validation and metrics like Pearson correlation coefficient or AUC [30].
Troubleshooting Guides & FAQs
FAQ 1: How do I determine if a drug interaction is truly synergistic and not just additive?
Answer: True synergy is confirmed when the combined effect is statistically greater than the expected effect under a reference model of non-interaction (e.g., Bliss Independence or Loewe Additivity) [29]. The choice of model is critical, as different models have different assumptions and mathematical frameworks [29]. It is essential to:
- Use Multiple Models: Cross-validate your findings with at least two different reference models (e.g., Bliss and CI) to ensure robustness [29].
- Statistical Testing: Perform statistical tests to confirm that the calculated synergy score is significantly different from zero (for Bliss) or that the CI is significantly less than 1 [31].
- Dose-Range Dependence: Be aware that a pair might be synergistic at certain dose ratios and antagonistic at others. Always test a full matrix of concentrations [31].
FAQ 2: Why are drug interactions not conserved across different cancer cell lines?
Answer: The context-specific nature of drug interactions is a major challenge. A pair synergistic in one cell line may be antagonistic in another due to differences in [31]:
- Genetic Mutations: Specific driver mutations (e.g., IDH2, TP53) can drastically alter pathway dependencies and drug responses. A single mutation can turn a synergistic interaction into an antagonistic one [31].
- Pathway Activity: Variations in the activity of signaling pathways (e.g., MAPK, PI3K) between cell lines influence how drugs interact [33].
- Tumor Microenvironment: Factors like hypoxia and stromal interactions, though less captured in 2D cultures, contribute to heterogeneous responses [29].
Troubleshooting Table: Common Experimental Issues
| Problem | Possible Cause | Solution |
|---|---|---|
| High variability in replicate synergy scores. | Inconsistent cell seeding density or drug dispensing. | Standardize cell counting and use automated liquid handlers for drug transfer [31]. |
| A known synergistic pair shows no effect. | Drug concentrations are below effective levels or incubation time is too short. | Re-determine ICâ‚…â‚€ values for your specific cell line and ensure a sufficient incubation period (e.g., 96 hours) [31]. |
| Computational model fails to predict known synergies. | Lack of relevant biological features in the training data for the specific cancer type. | Incorporate more context-specific data, such as cell line-specific mutational status or pathway activity, into the model [32] [30]. |
| Antagonism is consistently observed. | Overlapping toxicities or pharmacokinetic interference (e.g., one drug affects the metabolism of the other). | Review the pharmacodynamic and pharmacokinetic profiles of the drugs. Consider adjusting the dosing schedule (sequential vs. simultaneous) [34]. |
FAQ 3: How can Optimal Control Theory (OCT) be integrated with synergy data?
Answer: OCT provides a mathematical framework to design personalized treatment schedules that leverage synergy while minimizing toxicity [5] [6] [3]. The process involves:
- Model Formulation: The patient's tumor dynamics are described as a dynamical system, often using differential equations. The state variables ((x(t))) represent tumor cell populations, and the control inputs ((u(t))) represent drug doses or their effects [3].
- Incorporating Synergy: The model's equations are structured so that the inhibitory effect on tumor growth from a synergistic drug pair is greater than the sum of individual effects, as quantified by your experimental synergy scores [33].
- Defining the Objective: A performance measure ((J)) is formulated, typically aiming to minimize the tumor cell count at the end of the treatment period ((t_f)) while constraining the cumulative toxicity to healthy tissues [6] [3].
- Solving the Control Problem: Optimization algorithms (e.g., IPOPT, SDRE) are used to compute the optimal drug administration schedule—the sequence and timing of doses that maximize efficacy and minimize side effects [6].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for Drug Combination Studies [32] [34] [33]
| Item | Function/Application | Key Considerations |
|---|---|---|
| AML Cell Line Panel (e.g., Kasumi-1, HL-60, TF-1) | In vitro models representing genetic heterogeneity of AML. | Select cell lines with diverse genetic backgrounds (e.g., different mutations, translocations) to assess context-specificity of interactions [31]. |
| Targeted Inhibitors (e.g., Venetoclax, Enasidenib, kinase inhibitors) | Drugs targeting specific proteins or pathways crucial for cancer cell survival. | Purity and stability are critical. Prepare fresh stock solutions in recommended solvents (DMSO) and store as per manufacturer's guidelines [32] [31]. |
| CellTiter-Glo Luminescent Assay | Quantifies ATP levels as a marker of metabolically active (viable) cells. | Offers high sensitivity and a wide dynamic range for 384-well plate formats. Ensure reagent is equilibrated to room temperature before use [31]. |
| Acoustic Liquid Handler (e.g., Echo 555/655) | Non-contact dispenser for highly precise and miniaturized drug transfers in DMSO. | Essential for creating accurate 8x8 dose-response matrices while minimizing solvent volume, which can affect cell health [31]. |
| Proton Pump Inhibitors (e.g., Omeprazole) | Used to study pharmacokinetic DDIs related to altered gastric pH. | Can reduce the solubility and bioavailability of concomitant oral TKIs (e.g., Pazopanib, Erlotinib). Separate administration times may be required [34]. |
| CYP3A4 Inhibitors/Inducers (e.g., Ketoconazole, Rifampicin) | Tools to investigate metabolic drug-drug interactions. | Many anticancer drugs (e.g., Ibrutinib) are CYP3A4 substrates. Coadministration can lead to significant changes in systemic exposure and toxicity [34]. |
| Pan-Cancer Pathway Model | Large-scale ODE model simulating the effect of 7 targeted agents on 1228 molecular species [33]. | Used for in silico prediction of combination effects and optimization of therapy schedules before experimental validation [33]. |
| Excisanin B | Excisanin B, MF:C22H32O6, MW:392.5 g/mol | Chemical Reagent |
| 3-Hydroxychimaphilin | 3-Hydroxychimaphilin, MF:C12H10O3, MW:202.21 g/mol | Chemical Reagent |
Methodological Advances: Applying OCT to Pan-Cancer Models and Personalized Regimens
Constructing Large-Scale Mechanistic Models of Signaling Pathways for In Silico Prediction
Frequently Asked Questions
What are the primary software tools available for constructing and simulating large-scale mechanistic models? Multiple specialized software tools are available. The Julia programming language is used for generating synthetic signaling networks and has gained traction in the systems biology community [35]. Python-based pipelines are employed for creating models that are high-performance and cloud-computing ready, converting structured text files into the standard SBML format [36]. R/Bioconductor packages, such as the HiPathia package, implement algorithms for interpreting transcriptomic data within mechanistic models [37]. Rule-based modeling software like BioNetGen and PySB can also be used to define reaction patterns [36].
How can I ensure my model is reusable and interoperable? Adhering to community standards is crucial. Using the Systems Biology Markup Language (SBML) is a gold-standard practice for ensuring model portability between different software tools [36]. Providing comprehensive metadata and annotations for all model components (e.g., using ENSEMBL or HGNC identifiers) is essential for findability and reusability [36]. Furthermore, using simple, structured text files to define model specifics makes the model easy to alter and process programmatically [36].
My model simulations are computationally expensive. What are my options? For large-scale models, local machine simulation can be prohibitive. Leveraging High Performance Computing (HPC) or Cloud Computing (CC) platforms is recommended for tasks like parameter estimation or multiple single-cell simulations [36]. Using simulation packages specifically designed for efficiency, such as AMICI for Python, can significantly reduce CPU time [36].
What is a reliable method to validate a novel network inference or parameter fitting algorithm? Using synthetic signaling networks as ground truth models is a powerful validation strategy. You can generate artificial networks with known topology and parameters using tools like the provided Julia script [35]. These networks can then be used to produce synthetic "experimental" data, providing a known target against which to test your algorithm's performance [35].
Troubleshooting Common Experimental Issues
Problem 1: Poor Model Performance or Inaccurate Predictions
This can stem from several issues, including overfitting, non-identifiable parameters, or an incorrect network topology.
- Potential Cause 1: Overfitting and parameter non-identifiability due to a large number of state variables and parameters and limited calibration data [35].
- Potential Cause 2: The model topology lacks key biological features found in real signaling pathways, such as feedback loops [35].
- Solution: Compare the topology of your generated network against established models from databases like the BioModels Database. Use metrics like reaction degree and reaction distance to assess topological similarity [35].
- Potential Cause 3: Missing key cellular contexts, such as sequestration effects in phosphorylation cycles, which can significantly alter network behavior [35].
- Solution: Review model reaction rules to include critical processes like sequestration, especially when substrates and catalytic proteins (e.g., phosphatases) are present at comparable concentrations [35].
Problem 2: Model is Difficult to Simulate, Share, or Extend
This often results from using non-standard or custom-coded formats that are not easily portable.
- Potential Cause: Use of a custom-structured, non-standard model format that is not supported by mainstream simulation software [36].
Problem 3: Difficulty Integrating Transcriptomic Data for Functional Predictions
It can be challenging to connect gene expression levels to downstream functional activities like cell proliferation or death.
- Potential Cause: Treating the pathway as a single multifunctional entity rather than decomposing it into specific functional circuits [37].
- Solution: Deconstruct pathways into signaling circuits—elementary functional entities that connect receptors to effector proteins. Use an algorithm like HiPathia to simulate signal propagation through these circuits based on protein activity levels (e.g., from gene expression data) to generate functional profiles [37].
Experimental Protocols for Key Tasks
Protocol 1: Generating a Synthetic Signaling Network for Algorithm Testing
Purpose: To create a realistic, artificial signaling network with known topology and parameters that can serve as ground truth for validating network inference and parameter fitting algorithms [35].
Methodology:
- Define Reaction Motifs: Start with a list of core signaling unit processes. These typically include [35]:
- Catalyzed transformations
- Binding and unbinding reactions (following mass-action kinetics)
- Phosphorylation/dephosphorylation cycles (both single and double)
- Network Generation: Use a computational script (e.g., the provided Julia script) to randomly assemble these motifs into a larger network [35].
- Topological Validation: Calculate the reaction degree and reaction distance distributions of your synthetic network. Compare these distributions to those of curated signaling models from the BioModels Database to assess topological realism [35].
- Dynamic Validation: Compare the behavioral dynamics (e.g., steady states, oscillations) of your synthetic network with those of BioModels to ensure dynamic similarities [35].
Table: Core Reaction Motifs for Synthetic Network Generation
| Motif Type | Description | Kinetic Law |
|---|---|---|
| Catalyzed Transformation | Enzyme-catalyzed conversion of a substrate | Reversible Michaelis-Menten |
| Binding/Unbinding | Formation and dissociation of protein complexes | Mass-action |
| Phosphorylation Cycle | Addition/removal of a phosphate group by kinase/phosphatase | Reversible Michaelis-Menten |
Workflow for generating and validating a synthetic signaling network.
Protocol 2: Constructing a Large-Scale Model for Single-Cell Simulations
Purpose: To build a large-scale, mechanistic model (e.g., encompassing proliferation and death signaling) that is scalable, standards-compliant, and ready for single-cell level simulations and data integration [36].
Methodology:
- Define Model in Structured Files: Create a set of simple, structured text files that define the model's genes, species, reactions, stoichiometry, compartments, and parameters. This approach minimizes coding and allows for easy alteration [36].
- Convert to Standard Format: Process these input files using a script (e.g., a Jupyter notebook) to create a human-readable Antimony file. Then, convert the Antimony file into a standard SBML model file [36].
- Simulate the Model: Use SBML-compatible Python packages like AMICI for efficient deterministic simulation of large-scale models [36]. For single-cell simulations, incorporate a submodule for stochastic gene expression [36].
- Scale Computations: For large tasks (e.g., parameter estimation across many single cells), deploy the simulation pipeline on High Performance Computing (HPC) or Cloud Computing (CC) platforms like Kubernetes [36].
Table: Key Files for Large-Scale Model Construction
| File Type | Contents | Purpose |
|---|---|---|
| Gene List | Modeled genes with identifiers | Defines genetic components |
| Reaction File | List of all biochemical reactions | Specifies network interactions |
| Stoichiometry File | Stoichiometric coefficients for reactions | Defines mass balance |
| Parameter File | Kinetic parameters and initial conditions | Sets model dynamics |
| Compartment File | Cellular locations (e.g., cytosol, nucleus) | Provides spatial context |
Pipeline for constructing and simulating a large-scale, standards-compliant model.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Computational Tools and Resources
| Item Name | Function / Application | Key Features |
|---|---|---|
| Julia Scripts [35] | Generate synthetic signaling networks for algorithm validation. | Creates networks with topological & dynamic similarity to BioModels. |
| SPARCED Pipeline [36] | Python-based creation & simulation of large-scale single-cell models. | Input text files, outputs SBML via Antimony, HPC/CC ready. |
| HiPathia [37] | R package for mechanistic modeling of signaling pathways from transcriptomic data. | Simulates signal transduction through functional circuits; estimates mutation/drug effects. |
| BioModels Database | Repository of curated, published mathematical models of biological systems. | Source of realistic models for topological and dynamic comparison [35]. |
| AMICI [36] | Python/C++ package for simulation of differential equation models. | High-performance simulation of SBML models; fast gradient computation. |
| Antimony [36] | Human-readable language for describing biochemical models. | Facilitates the creation of complex SBML models through a simplified text format. |
| Spinorhamnoside | Spinorhamnoside, MF:C34H40O15, MW:688.7 g/mol | Chemical Reagent |
| 4,5-Diepipsidial A | 4,5-Diepipsidial A, MF:C30H34O5, MW:474.6 g/mol | Chemical Reagent |
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary goal of applying optimal control to cancer combination therapy? The primary goal is to compute a control function (e.g., a drug dosing schedule) that optimizes a performance metric related to the state of the disease (e.g., tumor cell count) and the control effort (e.g., drug dosage and associated toxicity). This involves minimizing a cost functional that balances treatment benefits against side effects and dosage costs [38] [39].
FAQ 2: What are the key components of a standard optimal control problem in this context? A standard problem formulation includes:
- A dynamical system: A set of ordinary differential equations (ODEs) that model the evolution of the disease (e.g., cell populations) under the influence of therapies [26] [38].
- A cost functional: A mathematical expression that quantifies the treatment goal, typically an integral of a "running cost" over time, sometimes with a terminal cost [39].
- Constraints: These can include initial conditions, upper and lower limits on drug doses, and state constraints [38] [39].
FAQ 3: My model is very complex and non-linear. Can optimal control still be applied? Yes. While analytical solutions (like those provided by Pontryagin's Maximum Principle) may be intractable for highly complex models, numerical optimal control techniques are designed for this purpose. These methods discretize the continuous-time problem into a finite-dimensional optimization problem that can be solved with nonlinear programming solvers [39] [40].
FAQ 4: How do I account for patient-reported toxicity and quality of life in the optimal control framework? Toxicity and quality of life can be incorporated into the cost functional. For instance, the running cost ( L(x,u,t) ) can include terms that penalize high drug concentrations (representing toxicity) and terms that penalize a low quality of life or the occurrence of specific adverse events, often quantified using patient-reported outcome measures (PROMs) [41] [42]. This creates a multi-objective optimization where the goal is to find a Pareto-optimal balance between efficacy and tolerability [41].
FAQ 5: What is the difference between a finite-horizon and an infinite-horizon optimal control problem?
- Finite-horizon problems consider a fixed treatment end time ( T ). The cost functional integrates cost from time 0 to ( T ) and may include a terminal cost ( \Phi(x(T)) ) that penalizes the final state [39].
- Infinite-horizon problems consider an infinite time period, which can be ill-posed. They are often made tractable by adding a discount factor that decays over time, ensuring the cost integral remains finite [39].
Troubleshooting Guides
Issue 1: ODE Solver is Slow or Fails to Converge
Problem: The numerical simulation of your model's ODEs is unstable, slow, or produces nonsensical results, preventing the optimal control algorithm from finding a solution.
Diagnosis and Resolution:
Step 1: Check for Stiffness
- Symptoms: The ODE solver (particularly non-stiff solvers like
ode45) takes an extremely long time or takes very small time steps. - Solution: Stiffness occurs when there is a drastic difference in scaling or time scales within the problem [43]. Switch to a solver designed for stiff systems, such as
ode15s[43].
- Symptoms: The ODE solver (particularly non-stiff solvers like
Step 2: Verify Your Model Equations and Parameters
- Symptoms: The solver fails entirely or states become NaN (not a number).
- Solution:
- Double-check the equations for typos and dimensional consistency.
- Ensure all parameter values are physically plausible and in the correct units.
- Simplify the model if possible. Using linear growth rates, for example, can make the optimal control problem more analytically tractable and numerically stable [26].
Step 3: Choose the Right Solver Refer to the following table for guidance on selecting an ODE solver in MATLAB [43].
| Solver | Problem Type | When to Use |
|---|---|---|
ode45 |
Nonstiff | This should be your first choice for most problems. |
ode23 |
Nonstiff | Can be more efficient than ode45 at problems with crude tolerances or moderate stiffness. |
ode113 |
Nonstiff | Can be more efficient than ode45 at problems with stringent error tolerances. |
ode15s |
Stiff | Use when ode45 fails or is slow and you suspect the problem is stiff. Also for DAEs of index-1. |
ode23s |
Stiff | Can be more efficient than ode15s at problems with crude error tolerances. |
ode23t |
Moderately Stiff | Use for moderately stiff problems where a solution without numerical damping is needed. |
Issue 2: The Optimized Dosing Schedule is Not Clinically Feasible
Problem: The optimal control solution suggests a highly variable, continuous dosing regimen that cannot be implemented in a real-world clinical setting (e.g., continuous IV infusion with rapidly changing rates).
Diagnosis and Resolution:
Step 1: Reformulate the Problem with Clinical Constraints
- The unconstrained optimal solution is often theoretically ideal but impractical. You must explicitly add constraints to your optimization problem [38].
- Discrete Dosing: Formulate the problem in discrete time, where controls are constant over a fixed period (e.g., 24 hours), representing a daily dose [39].
- Dose Levels: Constrain the control
u(t)to a finite set of allowed doses (e.g., 0 mg, 100 mg, 200 mg). - Dose Timing: Fix the times at which doses can be administered.
Step 2: Use a Discrete-Time Formulation Discretize your continuous-time model. The discrete-time optimal control problem seeks a sequence of states ( (x1, \ldots, xN) ) and controls ( (u0, \ldots, u{N-1}) ) that minimize: [ J(\mathbf{x},\mathbf{u}) = \sum{i=0}^{N-1} L(xi,ui,i) + \Phi(xN) ] subject to ( x{i+1} = g(xi, u_i) ), where
gis a simulation function (e.g., from Euler integration) that approximates the continuous dynamics [39].
Issue 3: Difficulty Balancing Multiple, Conflicting Objectives
Problem: You need to minimize tumor size, minimize drug toxicity, and minimize the total drug used, but these goals are in conflict. Manually tuning the weights in the cost functional is time-consuming and unsatisfactory.
Diagnosis and Resolution:
Step 1: Adopt a Multi-Objective Optimization (MOO) Framework
- Instead of combining all objectives into a single cost functional with weights, treat them as separate objectives [41].
- The goal of MOO is not to find a single "best" solution but to find a set of Pareto-optimal solutions. A solution is Pareto-optimal if no objective can be improved without worsening another [41].
Step 2: Compute and Analyze the Pareto Front
- Use MOO algorithms (e.g., evolutionary algorithms) to compute the Pareto front.
- This front, often visualized as a surface in objective space, provides a clear picture of the trade-offs between, for example, cancer cell count and side effects [41].
- A clinician can then examine the Pareto front and select a treatment regimen based on a patient's specific tolerance for side effects versus aggressiveness of treatment.
Issue 4: High-Dimensional State Space Leads to Intractable Computation
Problem: Your model has many cell populations and drug interactions, leading to a high-dimensional state space. The optimal control problem becomes computationally too expensive to solve.
Diagnosis and Resolution:
Step 1: Model Reduction
- Create a "semi-mechanistic" or "fit-for-purpose" model that includes only the key populations and interactions necessary to answer your specific question [38]. This reduces the state dimension
n. - The general framework for heterogeneous cell populations can be a template for building a simpler, tailored model [26].
- Create a "semi-mechanistic" or "fit-for-purpose" model that includes only the key populations and interactions necessary to answer your specific question [38]. This reduces the state dimension
Step 2: Efficient Discretization and solver choice
- Carefully choose the number of discretization time points
N. A finer grid is more accurate but much more costly. - Investigate solvers that are efficient for large-scale nonlinear optimization problems, such as Interior Point OPTimizer (IPOPT), which has been used successfully in cancer treatment optimization [44].
- Carefully choose the number of discretization time points
Experimental Protocols & Reference Tables
Table 1: Key Parameters for a Sample Optimal Control Problem in CML
This table summarizes parameters from a published model for Chronic Myeloid Leukemia (CML), which includes quiescent and proliferating leukemic cells and an immune effector cell population [38].
| Parameter / Variable | Description | Value / Unit |
|---|---|---|
| ( x_1 ) | Quiescent leukemic cell population | Cells |
| ( x_2 ) | Proliferating leukemic cell population | Cells |
| ( x_3 ) | Immune effector cell level | Cells |
| ( u_1 ) | Dose of targeted therapy 1 (e.g., Imatinib) | mg |
| ( u_2 ) | Dose of targeted therapy 2 | mg |
| ( u_3 ) | Dose of immunotherapy | mg |
| ( L(x,u) ) | Running cost (( = w1x1 + w2x2 + w3u1^2 + w4u2^2 + w5u3^2 )) | Cost units |
| ( w1, w2 ) | Weights on tumor cell populations | 1/(cell²) |
| ( w3, w4, w_5 ) | Weights on drug usage (penalizing toxicity/cost) | 1/(mg²) |
Table 2: Comparison of Optimal Control Techniques for a Sample Tumor Model
This table compares different control strategies applied to a malignant tumor model, demonstrating the performance of various numerical techniques [44].
| Technique | Description | Cost Value Achieved |
|---|---|---|
| IPOPT (Interior Point Optimizer) | An open-source tool for large-scale nonlinear optimization. | 52.3573 |
| SDRE (State-Dependent Riccati Equation) | Adapts linear control methods for nonlinear systems. | 52.4240 |
| ASRE (Approximate Sequence Riccati Equation) | A globally optimal feedback control approach for nonlinear systems. | 52.4240 |
The Scientist's Toolkit: Research Reagent Solutions
This table lists essential components of the modeling and optimization "toolkit" for implementing optimal control in cancer therapy.
| Item | Function in the Experiment |
|---|---|
| Ordinary Differential Equation (ODE) System | The core semi-mechanistic model describing the dynamics of cancer cell populations, immune cells, and drug interactions [26] [38]. |
ODE Solver (e.g., ode45, ode15s) |
A numerical routine for simulating the forward dynamics of the model given a control input. Essential for evaluating the cost functional [43]. |
| Nonlinear Programming (NLP) Solver (e.g., IPOPT) | The computational engine that performs the actual optimization, finding the control sequence that minimizes the cost functional subject to constraints [44] [39]. |
| Cost Functional Weights (( w_i )) | Tuning parameters that balance the relative importance of different objectives (e.g., tumor reduction vs. toxicity) in the overall goal [41] [39]. |
| Patient-Reported Outcome Measures (PROMs) | Standardized questionnaires (e.g., PRO-CTCAE) used to quantify the patient's perspective on treatment toxicity and quality of life, providing data for the toxicity terms in the cost functional [42]. |
| Orpinolide | Orpinolide, MF:C30H45NO4, MW:483.7 g/mol |
| Armeniaspirol B | Armeniaspirol B, MF:C18H19Cl2NO4, MW:384.2 g/mol |
Workflow and System Diagrams
Optimal Control Workflow
Multi-Objective Optimization Trade-offs
This section addresses fundamental questions about the CMA-ES algorithm and its relevance to computational research in cancer therapy optimization.
What is CMA-ES and why is it suitable for non-convex optimization in cancer therapy design?
The Covariance Matrix Adaptation Evolution Strategy (CMA-ES) is a stochastic, derivative-free numerical optimization method for difficult non-linear, non-convex black-box problems in continuous domain [45] [46]. It evolves a population of candidate solutions by adapting a multivariate normal distribution, effectively learning a second-order model of the objective function similar to approximating an inverse Hessian matrix [45]. This makes it particularly effective for problems where gradient-based methods fail due to rugged search landscapes containing discontinuities, sharp ridges, noise, or local optima [45].
In cancer therapy optimization, CMA-ES is valuable because it can handle complex, non-convex objective functions that arise when balancing multiple treatment goals such as minimizing tumor proliferation while controlling drug dosage to reduce side effects [33]. The algorithm's invariance properties make it robust across different problem formulations, and it requires minimal parameter tuning from users [45].
How does CMA-ES differ from traditional gradient-based optimization methods?
citation:10
| Feature | CMA-ES | Gradient-Based Methods (e.g., BFGS) |
|---|---|---|
| Derivative Requirement | No gradients required | Requires gradient information |
| Problem Types | Effective on non-convex, noisy, discontinuous problems | Best for smooth, convex problems |
| Convergence Speed | Slower on purely convex-quadratic functions | Typically 10-30x faster on convex-quadratic functions |
| Parameter Tuning | Minimal tuning required (mostly automated) | Often requires careful parameter adjustment |
| Solution Sampling | Population-based sampling | Point-to-point optimization |
What are the key internal state variables maintained by CMA-ES during optimization?
The CMA-ES algorithm maintains several critical state variables throughout the optimization process [46]:
- Mean vector ($m_k$): Represents the current favorite solution point in the search space
- Step-size ($\sigma_k$): Controls the overall scale of the search distribution
- Covariance matrix ($C_k$): Encodes the pairwise relationships between variables and the orientation of the search distribution
- Evolution paths ($p\sigma$, $pc$): Track the correlation between consecutive steps and enable cumulative step-size adaptation
These variables are updated iteratively based on the success of sampled candidate solutions, allowing the algorithm to learn effective search directions and scales without explicit gradient information [46].
Implementation and Configuration
This section provides practical guidance for implementing CMA-ES in scientific computing environments, particularly for cancer therapy optimization problems.
How do I properly configure CMA-ES parameters for drug dosage optimization problems?
For cancer therapy optimization where the search space typically involves drug concentration parameters, we recommend the following configuration approach based on the experimental setup described in [33]:
- Initialization: Set the initial mean vector $m_0$ to the center of your search space or based on prior knowledge of effective drug combinations
- Step-size: Set the initial step-size $\sigma_0$ to approximately 1/3 to 1/6 of the parameter range to ensure effective exploration
- Population size: For problems with 5-20 drug parameters, use population sizes ($\lambda$) between 20-100 individuals
- Stopping criteria: Implement termination based on fitness stagnation, maximum evaluations, or convergence thresholds
The following table summarizes key parameter settings for different problem scales in therapy optimization:
citation:1] [47][citation:3
| Problem Scale | Population Size ($\lambda$) | Initial Step-size ($\sigma_0$) | Restart Strategy |
|---|---|---|---|
| Small (2-5 drugs) | 20-40 | min_range / 6 |
bipop recommended |
| Medium (5-10 drugs) | 40-80 | min_range / 5 |
ipop or bipop |
| Large (10-20 drugs) | 80-150 | min_range / 4 |
ipop recommended |
What are the different restart strategies available and when should I use them?
CMA-ES supports several restart strategies to escape local optima, which is particularly important in complex therapy optimization landscapes [47]:
- No restart: Basic CMA-ES without restarts - suitable for unimodal problems or preliminary experiments
- IPOP-CMA-ES: Restarts with Increasing Population Size - effective for multimodal problems where increasing population size helps explore broader areas
- BIPOP-CMA-ES: Restarts with varying population sizes (both increasing and decreasing) - particularly effective for complex multimodal problems with multiple local optima
For cancer therapy optimization where the response landscape often contains multiple local optima corresponding to different drug combination strategies, BIPOP-CMA-ES is generally recommended [47] [33].
Troubleshooting Common Issues
This section addresses specific problems researchers encounter when applying CMA-ES to therapy optimization.
How can I handle categorical parameters in my optimization problem since CMA-ES doesn't support them directly?
CMA-ES operates exclusively on continuous parameters, which presents challenges for problems that include categorical drug choices or treatment scheduling options [48] [47]. Below are practical workarounds:
- Integer Relaxation: Represent categorical choices as continuous parameters during optimization, then round to the nearest integer for evaluation
- Hybrid Approach: Use CMA-ES for continuous parameters (e.g., drug dosages) combined with a separate sampler (e.g., RandomSampler or TPESampler) for categorical parameters [48]
- One-Hot Encoding with Continuous Relaxation: Encode categorical variables using a continuous simplex constraint approach
For the pan-cancer pathway model optimization described in [33], researchers used CMA-ES exclusively for continuous dosage parameters while pre-selecting the drug combinations based on mechanistic insights.
Why does my CMA-ES optimization show poor performance in parallel computing environments?
CMA-ES inherently operates sequentially because each generation updates the internal state based on the evaluation of all individuals in the population [48] [47]. When evaluations are parallelized, the algorithm cannot incorporate intermediate results until all evaluations complete. Consider these solutions:
- Asynchronous CMA-ES variants: Implement modified versions that can update with incomplete generations
- Increased population size: Compensate for parallelization overhead by using larger populations
- Restart strategies: Use IPOP or BIPOP approaches to maintain diversity in parallel settings [49]
- State persistence: Enable
store_optimizer_state_in_storage=Truewhen using distributed computing [47]
Recent advances in massively parallel CMA-ES show that with proper implementation, substantial speedups (up to several thousand times) can be achieved on high-performance computing architectures [49].
How can I enforce safety constraints on drug dosage parameters during optimization?
Standard CMA-ES doesn't explicitly handle constraints, but several techniques can enforce safety limits in therapy optimization [50]:
- Projection: Sample points normally, then project them to the nearest feasible point before evaluation
- Penalty functions: Add large penalty terms to the objective function for constraint violations
- Repair mechanisms: Modify infeasible solutions to meet constraints while preserving direction information
- Safe CMA-ES: Recent variants explicitly incorporate safety constraints using Lipschitz continuity assumptions [50]
For the pan-cancer model optimization, researchers employed a combination of projection for simple bound constraints and penalty functions for more complex safety considerations [33].
Experimental Protocols and Methodologies
This section provides detailed experimental protocols for applying CMA-ES to cancer therapy optimization problems.
Protocol: Optimizing Combination Therapy Using Pan-Cancer Signaling Pathway Model
This protocol is adapted from the methodology described in [33] for in silico combination treatment optimization.
Research Reagent Solutions
citation:3
| Reagent/Resource | Function in Experiment |
|---|---|
| Pan-cancer signaling pathway model | Mechanistic ODE model predicting molecular response to perturbations |
| 7 targeted anti-cancer agents | Small molecule inhibitors targeting cancer-associated pathways |
| Cancer Cell Line Encyclopedia data | Individualized model parameters for specific cancer cell lines |
| Proliferation scoring function | Maps molecular abundances to proliferation scores ($R(\tau,e)$) |
| CMA-ES implementation | Optimization core algorithm (cmaes or pycma packages) |
Workflow Description:
- Model Individualization: Parameterize the pan-cancer pathway model using genomic data from specific cancer cell lines
- Objective Formulation: Define the optimization goal (e.g., minimize proliferation score while limiting total drug exposure)
- Parameter Bounding: Establish minimum and maximum clinically relevant concentrations for each drug
- CMA-ES Configuration: Set up the optimizer with appropriate population size and restart strategy
- Optimization Execution: Run CMA-ES while tracking progression of candidate solutions
- Result Validation: Validate promising candidates through additional in silico analyses
Protocol: Sequential Treatment Planning Using CMA-ES with Hamiltonian Monte Carlo Sampling
This advanced protocol extends the basic methodology to optimize sequential treatment plans, which apply varying drug combinations over time to counter acquired resistance [33].
Workflow Description:
- Temporal Discretization: Divide the treatment horizon into discrete time intervals (e.g., 2-4 week cycles)
- Extended Parameterization: Represent the optimization problem as a sequence of drug combination decisions
- Enhanced Sampling: Implement Hamiltonian Monte Carlo sampling for efficient exploration of the high-dimensional search space
- Multi-objective Balancing: Optimize trade-offs between immediate tumor reduction and long-term resistance management
- Robustness Testing: Evaluate candidate sequences across different resistance scenarios
Advanced Topics and Extensions
This section covers specialized CMA-ES variants and their applications to challenging aspects of therapy optimization.
What specialized CMA-ES variants are available for specific challenges in therapy optimization?
Recent research has developed several specialized CMA-ES variants that address specific limitations of the standard algorithm:
citation:1][citation:9
| Variant | Purpose | Application in Therapy Optimization |
|---|---|---|
| CMA-ES with Margin | Prevents samples in discrete distributions from being fixed to a single point | Maintaining diversity in discrete dosage levels |
| Safe CMA-ES | Explicitly handles safety constraints without evaluation of unsafe points | Ensuring all tested drug combinations stay within safety limits |
| CMA-ES with LR Adaptation | Automatically adapts learning rates for multimodal/noisy problems | Handling noisy response measurements in biological systems |
| Warm-Started CMA-ES | Transfers knowledge from previous optimization tasks | Leveraging results from similar cancer cell lines |
| Separable CMA-ES | Constrains covariance matrix to diagonal for faster adaptation | Suitable for problems where drug effects are approximately independent |
How can I implement warm-starting to transfer knowledge between related optimization problems?
Warm-starting CMA-ES is particularly valuable in cancer therapy optimization where you may want to transfer knowledge from:
- Previously optimized treatments for similar cancer types
- Related cell line experiments
- Preliminary in vitro to in vivo translation
The source_trials parameter allows initializing the search distribution based on previously successful trials [48]. Implementation steps:
- Collect source data: Gather successful candidate solutions from previous optimizations
- Distribution estimation: Compute the mean and covariance of promising historical solutions
- Optimizer initialization: Initialize the new CMA-ES instance using the estimated distribution
- Adaptation period: Allow brief adaptation to the new problem context
This approach significantly reduces the number of evaluations needed to find effective therapies for new but related cancer types or cell lines.
What metrics should I track to diagnose CMA-ES performance during therapy optimization?
Comprehensive monitoring is essential for diagnosing optimization performance in complex biological problems:
- Fitness progression: Best, median, and worst fitness per generation
- Step-size evolution: Track $\sigma_k$ adaptation over generations
- Covariance matrix condition number: Monitor numerical stability and scaling
- Evolution path lengths: Assess convergence state and search effectiveness
- Restart triggers: Log automatic restart events and their causes
- Constraint violations: Track frequency and severity of safety boundary approaches
These metrics help identify whether poor performance stems from inadequate exploration, premature convergence, or problematic objective function landscapes.
Designing Sequential and Adaptive Treatment Plans to Counter Drug Resistance
Frequently Asked Questions: A Technical Support Guide
FAQ 1: What is the fundamental principle behind using optimal control for treatment scheduling?
Optimal control theory provides a mathematical framework for designing treatment schedules that systematically minimize a cost function, which typically includes tumor cell count and drug usage, while adhering to the biological constraints of the system. This approach transforms the clinical goal of balancing efficacy and toxicity into a solvable mathematical problem. A key finding from numerical simulations is that the optimal solution often manifests as a bang-bang control, where the drug is administered at either its maximum safe dose or at zero, with sharp switches between these states. This strategy has demonstrated superior performance, achieving the highest performance index and the lowest residual cancer cell count in studies [17].
FAQ 2: My model is not converging to a feasible solution. What could be wrong?
This is a common issue in computational modeling. Please check the following troubleshooting steps:
- Verify Constraint Formulation: Ensure that all physiological constraints, such as maximum cumulative toxicity and allowable drug concentration levels, are correctly implemented in your model. Overly restrictive constraints can make a feasible solution impossible.
- Check the Numerical Solver Settings: The choice of solver and discretization method can significantly impact results. Studies have successfully used the Interior-Point optimization solver (IPOPT) with the Applied Modelling Programming Language (AMPL) for similar problems. Using an Implicit Euler method for discretization with a small-time step (e.g., 0.01) has been shown to secure accuracy up to four decimal places [17].
- Inspect the System Dynamics: Review the underlying ordinary differential equations (ODEs) that model tumor growth and drug effect. A general ODE model for multiple cell populations treated with multiple drugs can be formulated, where the effect of drugs and their synergies are captured as linear combinations of terms involving drug actions and cell counts [26].
FAQ 3: How can I model the effect of multiple drugs on a heterogeneous cell population?
A general optimal control framework for this uses a system of coupled, semi-linear ordinary differential equations. The model should capture three key phenomena:
- Cell Proliferation and Death: Modeled with linear growth rates in the absence of drugs for analytical tractability.
- Cell Conversion: Allows cells to spontaneously convert to another type at fixed rates, which can also be mediated by drug treatment.
- Drug-Drug Interactions: Incorporates synergistic effects by making drug-mediated pathways depend on combinations of drugs.
In this framework, the pharmacodynamic effects of the drugs are represented by a control vector, ( u ), where each component ( 0 \leq u_k \leq 1 ) represents the effect of one drug. The governing equation for a cell population then includes terms for drug effects and drug-drug interactions [26].
FAQ 4: What does "steering evolution" mean in the context of antibiotic resistance, and is it applicable to cancer?
"Steering evolution" refers to a strategy where sequences of drugs are used to guide a pathogen population through genotype space to a state that is sensitive to treatment and from which resistance is unlikely to emerge. This approach is based on the non-commutativity of selective pressures, meaning the order of drug application matters. While this concept was developed for bacterial infections, the core principle is directly applicable to cancer. The evolutionary trajectories of cancer cells can be similarly influenced by the selective pressure of chemotherapeutic agents. The goal is to use drug sequences to shepherd the cancer cell population to a phenotypic state that is vulnerable to a final, decisive drug, thereby avoiding the emergence of multi-drug resistance [51].
Quantitative Data from Key Studies
Table 1: Performance Comparison of Optimal Control Strategies in a Cancer Chemotherapy Model [17]
| Model Feature | Heaviside Function Model | Sigmoid Function Model |
|---|---|---|
| Performance Index | 31.1132 | 31.1132 |
| Residual Cancer Cell Count | 0.0307 | 0.0307 |
| Optimal Control Structure | Bang-Bang | Bang-Bang |
| Numerical Method | Discretization & Nonlinear Programming (AMPL/IPOPT) | Discretization & Nonlinear Programming (AMPL/IPOPT) |
Table 2: Analysis of Sequential Antibiotic Treatment Outcomes [51]
| Category | 2-Drug Sequences | 3-Drug Sequences | 4-Drug Sequences |
|---|---|---|---|
| Sequences Promoting Final Drug Resistance | ~70% | ~70% | ~70% |
| Key Concept | Non-commutativity of natural selection | Non-commutativity of natural selection | Non-commutativity of natural selection |
| Proposed Strategy | Evolutionary steering to avoid resistant genotypes | Evolutionary steering to avoid resistant genotypes | Evolutionary steering to avoid resistant genotypes |
Detailed Experimental Protocols
Protocol 1: Implementing an Optimal Control Framework for Chemotherapy Scheduling
This protocol outlines the steps to numerically solve an optimal control problem for cancer drug scheduling, based on the methodology in [17].
Model Formulation:
- Define the system dynamics using a set of ordinary differential equations for tumor cell population, drug concentration, and cumulative toxicity.
- Replace discontinuous functions like the Heaviside function with smoother alternatives (e.g., a sigmoid function) to aid numerical convergence, though studies show this may not change the optimal bang-bang solution.
Discretization:
- Transform the continuous-time optimal control problem into a nonlinear programming problem using a discretization method. The Implicit Euler method is recommended for its stability and accuracy.
Solver Application:
- Code the discretized problem in a modeling language like AMPL (Applied Modelling Programming Language).
- Use an optimization solver such as IPOPT (Interior-Point OPTimizer) to compute the optimal drug doses over time.
Solution Validation:
- Analyze the solution structure; expect a bang-bang control profile.
- Verify that all physiological constraints (e.g., maximum toxicity) are satisfied.
Protocol 2: A Data-Driven Workflow for Navigating Collateral Sensitivity
This protocol describes how to build a computational framework to predict effective sequential antibiotic therapies, which can be adapted for cancer [52].
Data Collection:
- Conduct adaptive laboratory evolution to evolve resistance to individual drugs.
- For each resistant population, measure the Minimum Inhibitory Concentration (MIC) fold-change for all other drugs in the candidate pool. This generates a collateral sensitivity network.
Mathematical Formalization:
- Construct a multivariable switched system of ODEs. The system state represents the size of different bacterial (or cancer cell) variants.
- Define switching rules based on the collateral sensitivity data. For example, a rule ( R: CS \to S ) means a population resistant (R) to drug A, when exposed to a drug B to which it has collateral sensitivity (CS), becomes susceptible (S) to drug B.
Computational Simulation and Ternary Analysis:
- Simulate the evolutionary dynamics of a mixed population under different drug sequences.
- Use ternary diagrams to visualize and identify optimal 3-drug combinations based on the proportions of CS, CR, and IN interactions. The goal is to find combinations that minimize the risk of multi-drug resistance emergence.
Pathway and Workflow Visualizations
Diagram 1: Data-driven sequential therapy design workflow.
Diagram 2: Multi-drug control of a heterogeneous population.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Computational Tools for Treatment Optimization Research
| Item Name | Function / Description | Example Use Case |
|---|---|---|
| Applied Modelling Programming Language (AMPL) | An algebraic modeling language for linear and nonlinear optimization problems. | Formulating the discretized optimal control problem for the solver [17]. |
| IPOPT Solver | An open-source software package for large-scale nonlinear optimization using interior-point methods. | Solving the numerical optimization problem to find the optimal drug dose schedule [17]. |
| Collateral Sensitivity Network Data | A matrix of MIC fold-changes for resistant strains against a panel of drugs. | Informing the switching rules in the mathematical model for sequential therapy [52]. |
| Ordinary Differential Equation (ODE) System | A set of equations describing the rates of change of tumor cells, drug concentration, and toxicity. | Serving as the dynamic constraints in the optimal control problem [17] [26]. |
| Strong Selection Weak Mutation (SSWM) Model | A Markov chain model that abstracts evolutionary dynamics as a random walk on a fitness landscape. | Predicting the probability of resistance emerging under different drug sequences [51]. |
| Arenicolin B | Arenicolin B, MF:C34H48O12, MW:648.7 g/mol | Chemical Reagent |
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary advantage of using optimal control theory for cancer combination therapy scheduling?
Optimal control theory provides a mathematical framework to compute precise, patient-specific drug administration schedules. The primary advantage is its ability to systematically balance multiple, often competing, objectives: maximizing tumor cell kill while minimizing cumulative drug toxicity and severe side effects. Unlike empirical protocols, it uses dynamic models of tumor-immune-drug interactions to predict outcomes and identify dosing strategies that would be difficult to discover through intuition or trial-and-error alone [53] [54] [55]. This data-driven approach is particularly valuable for managing the complex interactions between chemotherapy, immunotherapy, and radiotherapy [53] [56].
FAQ 2: How can combination therapy overcome drug resistance in heterogeneous tumors?
Combination therapies target cancer through multiple distinct mechanisms simultaneously, reducing the probability that a population of heterogeneous cancer cells will be resistant to all treatment components. Using a pan-cancer pathway model, optimization algorithms can identify drug combinations that are effective across a population of different cancer cell lines, thereby controlling for both innate and acquired resistance [33]. Furthermore, optimized sequential treatment plans—where the drug cocktail is changed over time—can be computed to preempt and counteract the evolution of resistance [33].
FAQ 3: What are common synergistic combinations identified by computational models, and how are they validated?
Machine learning frameworks and mechanistic models have identified several promising synergistic pairs. For instance, kinase inhibitors often show synergy when combined with mTOR inhibitors, DNA damage-inducing drugs, or HDAC inhibitors. Drugs like Gemcitabine, MK-8776, and AZD1775 frequently appear in synergistic combinations across various cancer types, including ovarian, melanoma, prostate, lung, and colorectal carcinomas [32]. These predictions are first generated in silico and then must be validated through in vitro and in vivo laboratory studies before clinical consideration [32] [33].
FAQ 4: What role does fractional-order modeling play in optimizing cancer therapies?
Fractional-order calculus provides a more accurate framework for modeling biological processes with "memory," meaning the current state of the system depends on its past history. This is particularly relevant for capturing the long-term dynamics of tumor-immune interactions and the effects of drugs. When integrated with optimal control, fractional-order models can lead to more personalized and effective treatment strategies for complex cancers like heterogeneous lung cancer, often resulting in different dosing schedules compared to traditional integer-order models [57].
Troubleshooting Common Experimental and Computational Issues
Issue 1: High Cumulative Toxicity in Chemotherapy Models
- Problem: The optimized drug schedule results in unacceptably high levels of cumulative toxicity (e.g., cardiotoxicity from anthracyclines), violating patient safety constraints [54].
- Solution:
- Revise the Model: Incorporate a second control variable for a toxicity-reduction drug, such as Dexrazoxane. Expand the system dynamics to include an equation that reduces the cumulative toxicity metric:
μ‾(t) = ∫[v(t) - θω(t)] dt, whereω(t)is the injection rate of the protective drug andθis its efficacy parameter [54]. - Adjust the Optimization Goal: Ensure the objective function heavily penalizes high cumulative toxicity. The Gauss pseudospectral method (GPM) has been shown to effectively solve such models, significantly reducing toxicity while maintaining tumor reduction efficacy [54].
- Revise the Model: Incorporate a second control variable for a toxicity-reduction drug, such as Dexrazoxane. Expand the system dynamics to include an equation that reduces the cumulative toxicity metric:
- Prevention: Proactively include toxicity dynamics from the outset of model design rather than simply constraining it with an upper limit.
Issue 2: Failure to Account for Synergy, Additivity, or Antagonism in Drug Combinations
- Problem: A model treats drug effects as purely additive, leading to inaccurate predictions of tumor response and suboptimal therapy schedules [32].
- Solution:
- Leverage Machine Learning: Use a pre-trained classifier (e.g., on the O’Neil drug interaction dataset) to predict whether a specific drug pair is synergistic, additive, or antagonistic for a given cancer type [32].
- Incorporate Synergy Metrics: Integrate a quantitative synergy score (e.g., Combination Sensitivity Score - CSS) directly into the objective function of the optimal control problem. This encourages the selection of synergistic drug pairs and dosages [32].
- Prevention: Before constructing a dynamic model, screen potential drug combinations using published datasets or machine learning tools to inform which interactions require more sophisticated modeling.
Issue 3: Poor Performance or Non-Convergence of Optimization Algorithms
- Problem: The numerical algorithm used to solve the optimal control problem fails to find a solution or converges to a clinically unrealistic schedule.
- Solution:
- Algorithm Selection: Consider using derivative-free global optimization methods like the Iterative Dynamic Programming Algorithm (IDPA) or the Covariance Matrix Adaptation Evolution Strategy (CMA-ES). These are robust for non-convex problems and do not require calculating derivatives, which can be complex [55] [33].
- Improve Sampling: For constrained optimization, combine CMA-ES with a scalable sampling scheme, such as one based on Hamiltonian Monte-Carlo, to efficiently handle bounds on drug doses and toxicity [33].
- Model Transformation: For complex dynamics, employ a model transformation technique to simplify the equations before applying the optimization algorithm, as demonstrated with the GPM [54].
Issue 4: Inability to Capture Long-Term Tumor Dynamics and Treatment Effects
- Problem: An integer-order differential equation model fails to accurately reflect the observed progression of cancer and the lasting effects of treatment.
- Solution: Transition to a Fractional-Order Model. Fractional derivatives incorporate memory effects, providing a more accurate representation of biological systems. This is especially useful for modeling the interactions between regular cancer cells, mutated cells, and immune responses over time [57].
- Implementation: Combine the fractional-order model with a feedback control mechanism, such as a Proportional-Integral-Derivative (PID) controller. This allows for dynamic, real-time adjustment of immunotherapy and targeted therapy dosages based on the simulated tumor response, enhancing the personalization and adaptability of the treatment schedule [57].
Experimental Protocols & Workflows
Protocol 1: Developing an Optimal Control Schedule for Combination Chemotherapy with Toxicity Management
This protocol details the steps to create an optimized drug schedule using a model that includes a protective agent.
Define the Dynamic System:
- Tumor Growth: Use a Gompertz growth model:
NË™(t) = λN(t)ln[Ï/N(t)] - ζ[v(t)-α]H[v(t)-α]N(t), whereN(t)is tumor size,λis growth rate,Ïis carrying capacity,ζis drug killing factor,v(t)is drug concentration, andαis the minimum effective concentration [54]. - Drug Concentration: Model as
v˙(t) = u(t) - γv(t), whereu(t)is the anticancer drug injection rate andγis the decay rate [54]. - Cumulative Toxicity with Protection: Model as
μ‾(t) = ∫[v(t) - θω(t)] dt, whereω(t)is the injection rate of the protective drug (e.g., Dexrazoxane) andθis its efficacy [54].
- Tumor Growth: Use a Gompertz growth model:
Formulate the Optimization Problem:
- Objective Function: Minimize a weighted sum of final tumor size and total drug usage, e.g.,
J = N(t_f) + ∫[Q*u(t) + R*ω(t)] dt. WeightsQandRbalance efficacy versus toxicity [54]. - Constraints: Impose upper bounds on
v(t),ω(t), andμ‾(t)to reflect physiological and safety limits.
- Objective Function: Minimize a weighted sum of final tumor size and total drug usage, e.g.,
Discretize and Solve:
- Apply the Gauss Pseudospectral Method (GPM) to transcribe the continuous optimal control problem into a nonlinear programming problem [54].
- Solve the resulting problem using a standard NLP solver.
Validate and Interpret:
- Run simulations with the optimized control inputs
u*(t)andω*(t). - Compare the results (tumor size and toxicity) against conventional fixed-dose protocols or models without toxicity protection.
- Run simulations with the optimized control inputs
Diagram 1: Workflow for Chemotherapy Schedule Optimization with Toxicity Management.
Protocol 2: Pan-Cancer Pathway Model for Identifying Synergistic Combination Therapies
This protocol uses a large-scale mechanistic model to find effective multi-drug combinations across diverse cancer cell lines.
Model Individualization:
- Select the pan-cancer signaling pathway model, an ODE system with 1228 molecular species and 2704 reactions [33].
- Input genomic or proteomic data for a specific cancer cell line (or a population of cell lines) to tailor the model's parameters.
Define the Treatment Optimization Problem:
- Decision Variables: The doses of up to 7 targeted anti-cancer agents [33].
- Objective: Minimize a composite score, e.g.,
J = Proliferation_Score + β * (Total_Drug_Concentration). The proliferation score is derived from the model's steady-state output. The regularization parameterβcontrols the trade-off between efficacy and dose-induced side effects [33].
Run Optimization Algorithm:
- Use the Covariance Matrix Adaptation Evolution Strategy (CMA-ES), a robust evolutionary algorithm [33].
- Enhance CMA-ES with an efficient Hamiltonian Monte-Carlo-based sampler to handle the constraints on drug concentrations.
Analyze Results for Heterogeneity and Resistance:
- Solve the problem for a single cell line to find a tailored therapy.
- To address tumor heterogeneity, solve a multi-objective problem targeting a population of cell lines, minimizing the maximum or average proliferation across all lines [33].
- For sequential therapy optimization, run the optimization over multiple time windows, allowing the drug combination to change at each interval to suppress resistant clones [33].
Diagram 2: Workflow for Pan-Cancer Model-Based Combination Therapy Optimization.
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Key Computational and Biological Resources for Combination Therapy Optimization Research.
| Item Name | Type | Function in Research | Key Features / Notes |
|---|---|---|---|
| Pan-Cancer Signaling Pathway Model [33] | Computational Model | Predicts molecular-level response to single and combination targeted therapies. Serves as the "virtual patient" for in-silico screening. | Large-scale ODE model; 1228 molecular species, 7 targeted agents; Can be individualized with genomic data. |
| Gauss Pseudospectral Method (GPM) [54] | Optimization Algorithm | Solves optimal control problems by discretizing state and control variables on a Gaussian grid. Highly accurate for constrained problems. | Used for scheduling chemotherapy with toxicity constraints; Provides high accuracy in converting continuous problems to NLP. |
| Covariance Matrix Adaptation Evolution Strategy (CMA-ES) [33] | Optimization Algorithm | A robust, derivative-free evolutionary algorithm for difficult non-convex optimization problems. | Ideal for searching large spaces of possible drug combinations; Can be paired with HMC sampling for constraints. |
| Iterative Dynamic Programming Algorithm (IDPA) [55] | Optimization Algorithm | A dynamic programming-based method that performs an exhaustive search within a defined region. | Reliable for finding global optima in immunotherapy models; Does not require derivative calculations. |
| Fractional-Order Model with PID Control [57] | Modeling & Control Framework | Captures memory effects in cancer-immune dynamics and enables real-time, adaptive dosing feedback. | Provides more realistic biological modeling than integer-order ODEs; PID controller allows dynamic treatment adjustment. |
| Dexrazoxane [54] | Pharmaceutical Reagent | Used as a second control input in chemotherapy models to reduce cumulative cardiotoxicity. | Clinically recognized cardioprotective agent; Modeled with an efficacy parameter θ to quantify its effect. |
| O’Neil Drug Interaction Dataset [32] | Experimental Dataset | Provides ground-truth data on drug synergy, additivity, and antagonism for training machine learning models. | Used to build classifiers that predict interaction outcomes for novel drug pairs. |
Overcoming Clinical Hurdles: Troubleshooting Toxicity, Heterogeneity, and Scheduling Complexity
Addressing Inter-Patient and Intra-Tumor Heterogeneity in Treatment Planning
Frequently Asked Questions (FAQs)
Q1: What are the primary types of tumor heterogeneity that impact treatment planning? Tumor heterogeneity manifests at multiple levels, each presenting distinct challenges for therapy. Inter-patient heterogeneity refers to the genotypic and phenotypic diversity in tumors across different patients who have histopathologically similar cancers originating from the same sites. This diversity explains why patients with seemingly identical cancer types experience different progression and treatment responses [58]. Intra-tumor heterogeneity describes the genetic and phenotypic diversity within a single tumor, driven by the continuous evolution of multiple clonal populations under selective pressure, leading to subclones with distinct molecular alterations [58]. Spatial heterogeneity involves the uneven distribution of genetically diverse tumor cell subpopulations within a single lesion or between the primary tumor and its metastases. Temporal heterogeneity refers to changes in the molecular composition of cancer cells over time, often accelerated by therapeutic selective pressure [59].
Q2: How does tumor heterogeneity lead to treatment failure? Heterogeneity drives treatment failure primarily through the pre-existence or emergence of resistant cell populations. In a heterogeneous tumor, drug-sensitive cells are eliminated by therapy, while minor, resistant subclones survive, proliferate, and ultimately cause disease recurrence [58] [59]. This is compounded by cross-resistance and collateral sensitivity within the tumor cell population. Furthermore, standard treatments based on a single tumor biopsy often fail to capture the complete genomic landscape of the cancer, leading to therapies that are ineffective against some subclones [59].
Q3: What methodologies can accurately characterize intra-tumor heterogeneity? Characterizing heterogeneity requires technologies capable of resolving cellular differences. The following table summarizes key methodologies:
Table: Methodologies for Characterizing Tumor Heterogeneity
| Technology | Principle | Application in Heterogeneity | Reference |
|---|---|---|---|
| Next-Generation Sequencing (NGS) | Massively parallel sequencing of sample DNA | Comprehensive genomic analysis for detecting clonal architecture and novel genetic signatures across subpopulations. | [58] |
| Single-Cell RNA Sequencing (scRNA-seq) | Transcriptome profiling of individual cells | Identifies distinct cell subpopulations and their unique gene expression patterns within a tumor. | [60] |
| Liquid Biopsy | Analysis of circulating tumor DNA (ctDNA) from blood | Captures a composite genomic profile from multiple tumor sites, overcoming spatial sampling bias. | [58] |
| Immunohistochemistry (IHC) | Chromogenically visualized antibody binding | Visualizes protein expression and localization at the tissue level, including mutant proteins. | [58] |
Q4: How can Optimal Control Theory (OCT) address heterogeneity in combination therapy scheduling? Optimal Control Theory provides a mathematical framework to design personalized therapeutic regimens that account for dynamic, heterogeneous cell populations. OCT uses differential equation models of tumor growth and treatment response to systematically compute the best possible dosing and timing for multiple drugs. The goal is to minimize a cost function that typically includes tumor burden and drug toxicity [5] [15]. For heterogeneous populations, OCT can be used to design regimens that simultaneously target multiple co-existing subclones, exploit drug synergies, and manage the evolutionary dynamics of resistance, moving beyond one-size-fits-all treatment protocols [15] [61].
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent or Unreliable Measurement of Intra-Tumor Heterogeneity
- Problem: Measurements of heterogeneity, such as the Tumor Heterogeneity (TH) index, vary significantly between technical replicates or fail to correlate with clinical outcomes.
- Solution:
- Ensure Adequate Genomic Coverage: The accuracy of the TH index is highly dependent on the number of genes sequenced. A panel of ~300 cancer-related genes provides a reliable estimate, whereas panels with only 50 genes show poor correlation with whole-exome sequencing results [62].
- Control for Tumor Purity: Low tumor cell content in a sample can artificially lower heterogeneity measurements. Always determine and report tumor purity (e.g., via pathological review or computational estimation) and consider it when interpreting TH indices [62].
- Validate with Orthogonal Methods: Correlate findings from bulk sequencing (e.g., TH index from panel sequencing) with higher-resolution techniques like single-cell RNA-seq on a subset of samples to confirm the inferred subclonal architecture [60].
Challenge 2: Failure of Preclinical Models to Recapitulate Human Tumor Heterogeneity
- Problem: Drug efficacy seen in homogeneous cell lines or animal models does not translate to heterogeneous human tumors.
- Solution:
- Utilize Molecularly Characterized Models: Employ patient-derived xenografts (PDXs) or organoids that have been stratified according to known molecular subtypes (e.g., the Consensus Molecular Subtypes (CMS) in colon cancer). These models better preserve the heterogeneity and signaling pathways of original tumors [63].
- Incorporate the Tumor Microenvironment (TME): Use co-culture systems or models that include stromal cells, as the TME is a critical source of non-genetic heterogeneity and can drive therapeutic resistance [59].
Challenge 3: Designing Effective Combination Therapies for Heterogeneous Cancers
- Problem: With countless possible drug-dose-timing combinations, empirically testing regimens to overcome heterogeneity is infeasible.
- Solution:
- Implement Mathematical Modeling: Develop pharmacokinetic-pharmacodynamic (PK-PD) models that incorporate multiple cell populations with different drug sensitivities. These models can simulate tumor response to various regimens in silico [64] [61].
- Apply Optimal Control Theory: Use OCT to identify synergistic drug sequences and schedules. For example, models can predict that administering a targeted radionuclide therapy and CAR-T cell therapy with a specific interval between them maximizes tumor kill while minimizing off-target effects, a finding that has been validated preclinically [64].
Key Experimental Protocols
Protocol 1: Calculating a Tumor Heterogeneity Index from Targeted Sequencing Data
This protocol is adapted from research using targeted deep sequencing to prognosticate in colorectal cancer [62].
Objective: To quantify intra-tumor heterogeneity from targeted panel sequencing data of a solid tumor sample.
Materials:
- DNA extracted from FFPE or fresh frozen tumor tissue with matched normal DNA (e.g., from blood).
- Targeted sequencing panel for cancer-related genes (recommended ≥300 genes).
- Standard bioinformatics pipeline for variant calling (e.g., BWA, GATK).
Method:
- Sequencing and Variant Calling: Perform deep sequencing (high coverage >500x recommended) on the tumor and normal samples. Identify somatic mutations (SNVs, small indels) and their corresponding Variant Allele Frequencies (VAFs).
- Calculate Shannon's Diversity Index: The TH index is calculated using Shannon's index, defined as:
- TH index = -Σ (pi * ln(pi))
- where pi is the frequency of the i-th mutated allele (VAFi / Σ VAF). Only non-synonymous, somatic mutations in the panel genes are used.
- Classification: A higher TH index indicates greater heterogeneity. The cohort's average TH index can be used as a cutoff to classify tumors as "High-Heterogeneity" or "Low-Heterogeneity" for survival analysis.
Protocol 2: In Silico Optimization of Combination Therapy Timing
This protocol outlines the use of a mathematical model and Optimal Control Theory to design a combination therapy schedule, as demonstrated for Targeted Radionuclide Therapy (TRT) and CAR-T cell therapy [64].
Objective: To determine the optimal timing interval between two therapies to maximize progression-free survival.
Materials:
- Preclinical data from monotherapy treatments (dose-response curves).
- A system of ordinary differential equations (ODEs) modeling tumor cell populations and therapy interactions.
Method:
- Model Calibration: Use monotherapy experimental data to calibrate the parameters of the ODE model. For example:
- dNT/dt = ÏNT - kRxT NT - k1 NT NC
- This equation describes the change in unirradiated tumor cells (
N_T), incorporating proliferation (Ï), killing by TRT (k_Rx_T), and killing by CAR-T cells (k_1).
- Define the Cost Function: In the OCT framework, define a function to be minimized. This often includes the final tumor burden and the cumulative drug toxicity over the treatment period.
- Solve the Optimal Control Problem: Apply numerical solvers (e.g., forward-backward sweep method) to the calibrated model to compute the drug administration schedule (
u(t)) that minimizes the cost function. - Model Validation: Test the in-silico-optimized schedule (e.g., a 7-day interval between TRT and CAR-T) in a preclinical animal model and compare the outcome (e.g., tumor growth delay, survival) against other scheduling strategies.
Visualizing the Problem: Heterogeneity and Treatment Resistance
The following diagram illustrates how intra-tumor heterogeneity and clonal evolution form the basis for treatment resistance.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Resources for Studying Tumor Heterogeneity and Treatment Optimization
| Tool / Reagent | Function | Key Consideration |
|---|---|---|
| Targeted Sequencing Panel (e.g., 381 genes) | Measures tumor heterogeneity index from bulk tissue. | Panel size is critical; <300 genes reduces accuracy [62]. |
| Single-Cell RNA-seq Kit | Resolves cellular composition and transcriptomic states of subpopulations. | Essential for identifying non-genetic heterogeneity and rare cell states [60]. |
| Patient-Derived Organoids (PDOs) | Preclinical models that retain patient-specific genetics and heterogeneity. | Recapitulate inter-patient heterogeneity and drug response profiles [63]. |
| Liquid Biopsy Assay | Non-invasive monitoring of clonal dynamics via ctDNA. | Captures spatial heterogeneity and tracks evolution in real-time [58]. |
| Optimal Control Software (e.g., MATLAB, Python) | Solves differential equations to compute optimal drug schedules. | Requires a calibrated mathematical model of tumor-immune-drug interactions [5] [15]. |
Strategies for Managing Toxicity and Minimizing Adverse Side Effects in Optimal Regimens
Troubleshooting Guides
Guide 1: Troubleshooting Model Inaccuracies in Optimal Control Theory (OCT) Applications
Problem: Mathematical model predictions do not align with observed experimental or clinical toxicity data.
- Potential Cause 1: Insufficient Model Calibration
- Potential Cause 2: Oversimplified Toxicity Compartment
- Solution: Integrate a dedicated compartment for the specific toxicity into your model. For instance, when modeling Immune Checkpoint Inhibitors (ICIs), incorporate a heart compartment to simulate the risk of autoimmune myocarditis, tracking damaged heart cells and relevant immune cell populations [65].
- Potential Cause 3: Ignoring Off-Target Immune Effects
- Solution: Account for the unidirectional flow of activated immune cells. In linked heart-tumor models, ensure the model includes a flow of harmful T cells from the tumor compartment to the organ at risk (e.g., the heart) to simulate cross-reactive damage [65].
Guide 2: Troubleshooting Suboptimal Dosing Schedules
Problem: An optimized schedule controls tumor growth but triggers unacceptable toxicity in simulations.
- Potential Cause 1: Overly Aggressive Initial Dosing
- Solution: Apply OCT to adjust the timing and sequence of doses. Optimized schedules often spread doses more evenly over time and may bring initial doses forward to allow the immune system to reset, thereby lowering toxicity risk while maintaining efficacy [65].
- Potential Cause 2: Inadequate Balance in Objective Function
- Solution: Recalibrate the payoff function in your optimal control algorithm. Assign a higher weight to the penalty for toxicity to force the algorithm to find a schedule that more aggressively minimizes adverse effects [65].
- Potential Cause 3: Fixed, Non-Adaptive Dosing
- Solution: Develop adaptive dosing protocols. Use real-time biomarkers like ctDNA to inform dose adjustments during treatment, moving from a static regimen to a dynamic, patient-responsive one [7].
Guide 3: Troubleshooting Combination Therapy Toxicity
Problem: Severe or unexpected toxicities arise when simulating or implementing combination therapies.
- Potential Cause 1: Antagonistic Drug Interactions
- Potential Cause 2: Cumulative Payload Toxicity
- Solution: For combinations involving Antibody-Drug Conjugates (ADCs), investigate the properties of the linker and payload. Novel ADC designs with different payloads can offer a higher therapeutic index and reduce cumulative toxicities like myelosuppression [7].
- Potential Cause 3: Overlapping Toxicity Profiles
- Solution: Conduct a thorough review of each drug's known toxicities before combination. Use mechanistic models to simulate the compounded effect on specific organs and explore dose reduction or alternative scheduling for the offending agents [67].
Frequently Asked Questions (FAQs)
FAQ 1: What is the core value of using Optimal Control Theory (OCT) for toxicity management? OCT provides a rigorous mathematical framework to design therapeutic regimens that explicitly balance the competing objectives of maximizing tumor cell death and minimizing damage to healthy tissues. It allows for the systematic, in silico exploration of countless dosing and scheduling options to find the one that optimally manages this trade-off for an individual patient [5] [65].
FAQ 2: How can preclinical models better predict immune-related Adverse Events (irAEs) like myocarditis? Incorporate a two-compartment mathematical model that links tumor growth dynamics with the dynamics of the specific irAE. For myocarditis, this involves modeling the interactions between damaged heart cells, innate immune cells, pro-inflammatory T cells, and regulatory T cells, and then connecting this compartment to the tumor model via a flow of activated T cells [65].
FAQ 3: What are the key challenges in translating optimized schedules from models to the clinic? Key challenges include the lack of readily accessible, high-frequency patient-specific data to calibrate models; the regulatory and practical hurdles of implementing complex, non-standard dosing schedules; and the need for clinical trials that validate these model-derived regimens against standard-of-care [5] [67].
FAQ 4: Can OCT be applied to newer therapies like Cell Therapies or ADCs? Yes. For CAR-T cell therapy, OCT could help optimize the conditioning regimen or manage toxicities like Cytokine Release Syndrome (CRS). For ADCs, OCT can inform scheduling to maximize tumor killing while minimizing payload-related toxicities, such as by optimizing the interval between doses to allow healthy tissue recovery [7] [68].
FAQ 5: How do we optimize therapy when toxicity is patient-specific? The future lies in personalizing the OCT framework. This involves building models initialized with a patient's own data—such as imaging, genomic profiles, and biomarkers—to predict their unique risk of toxicity and response, thereby computing a truly personalized optimal regimen [5].
Quantitative Data Tables
Table 1: Optimization Outcomes for Immune Checkpoint Inhibitor Scheduling
Data derived from applying Optimal Control Theory to a two-compartment heart-tumor model [65].
| Therapy | Standard Schedule Result | Optimized OCT Schedule Result | Key OCT Scheduling Change |
|---|---|---|---|
| Nivolumab (anti-PD-1) | Moderate tumor control, higher myocarditis risk | Effective tumor control, significantly reduced myocarditis risk | Doses spread out more evenly over time |
| Ipilimumab (anti-CTLA-4) | High tumor burden reduction, triggers autoimmune issues | Effective tumor control, avoided autoimmune toxicity | Doses spaced apart, allowing immune system reset |
| Combined Nivolumab + Ipilimumab | Complex interactions, high toxicity probability | Balanced efficacy with significantly lower toxicity probability | Doses spread further apart, careful sequencing |
Table 2: Common Cancer Therapy Toxicities and Research-Grade Management Strategies
Synthesized from clinical and preclinical optimization studies [5] [65] [69].
| Toxicity | Associated Therapies | OCT-Informed Management Strategy | Experimental/Mechanistic Insight |
|---|---|---|---|
| Autoimmune Myocarditis | Immune Checkpoint Inhibitors | Optimized dosing schedule to lower harmful T-cell peak levels [65] | Model shows a critical threshold of harmful T cells exists; ICIs lower this threshold [65] |
| Diarrhea | Afatinib, other TKIs | Dose interruption and symptom management guided by model [69] | Community pharmacists are a key resource for managing mild-moderate cases [69] |
| Neuropathy | Cytotoxic Chemotherapy | Not a primary OCT focus, managed via dose reduction [69] | Guidelines focus on risk factors, symptoms, and management rather than scheduling [69] |
| Cytokine Release Syndrome (CRS) | CAR-T Cell Therapy, Bispecifics | Protocol-based management of adverse events [68] | Early recognition and intervention are critical for patient safety [68] |
Experimental Protocols
Protocol 1: Developing and Calibrating a Two-Compartment Heart-Tumor Model
Purpose: To create a mechanistic mathematical model for optimizing Immune Checkpoint Inhibitor (ICI) schedules that control tumor growth while minimizing the risk of autoimmune myocarditis [65].
Methodology:
- Define the Heart Compartment: Model the dynamics of autoimmune myocarditis using a system of ordinary differential equations (ODEs) that track:
- Damaged Heart Cells (Hd): Initial damage can be set via a parameter.
- Innate Immune Cells (M): Rapid, non-specific response.
- Harmful T Cells (Th): Pro-inflammatory cells (e.g., CD4+).
- Regulatory T Cells (T_r): Anti-inflammatory cells that suppress the immune response.
- Define the Tumor Compartment: Model tumor growth using a simplified ODE model (e.g., logistic growth) that includes the suppressive effect of T cells activated by ICIs.
- Link the Compartments: Introduce a unidirectional flow of harmful T cells (
F_Th) from the tumor compartment to the heart compartment. This represents T cells activated against the tumor that cross-react with heart tissue. - Incorporate Therapy: Add the effect of ICIs (e.g., anti-PD-1, anti-CTLA-4) as control variables (
u) in the equations governing T cell activation and proliferation in both compartments. - Model Calibration: Parameterize the model using data from preclinical studies or clinical trial results. Sensitivity analysis should be performed to identify the most influential parameters.
- Optimal Control Setup: Define an objective function that minimizes a weighted sum of final tumor size and cumulative toxicity (e.g., peak level of
T_hin the heart compartment) over the treatment horizon, subject to the system's dynamics and constraints on the maximum dose.
Protocol 2: In Silico Testing of Alternative Dosing Regimens
Purpose: To systematically compare the efficacy and toxicity profiles of standard versus optimized dosing schedules using a calibrated mathematical model.
Methodology:
- Establish Baseline: Simulate the standard-of-care dosing regimen (e.g., fixed doses every two weeks) in your model. Record key endpoints: final tumor volume, peak toxicity metric, and area under the curve for both.
- Formulate Optimal Control Problem: Apply Pontryagin's Maximum Principle or a direct optimization method to find the control trajectory (dosing over time) that minimizes your objective function.
- Compute Optimized Schedule: Run the optimal control algorithm to generate a new, potentially non-uniform, dosing schedule.
- Simulate and Compare: Simulate the optimized schedule in the same model used to generate it.
- Validate Robustness: Perform robustness checks by simulating the optimized schedule under different parameter sets (e.g., representing inter-patient variability) to ensure it is not overly sensitive to small changes in model assumptions.
Signaling Pathways and Workflow Diagrams
Diagram 1: Two-Compartment Heart-Tumor Model for ICI Toxicity
Diagram 2: Optimal Control Workflow for Regimen Design
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Components for OCT-Informed Toxicity Research
| Item | Function in Research | Example Application |
|---|---|---|
| Mechanistic Mathematical Models | Provides the computational framework to simulate tumor and toxicity dynamics over time. | The two-compartment heart-tumor model used to optimize ICI schedules [65]. |
| Optimal Control Algorithm | The computational engine that solves for the best possible dosing schedule given the model and constraints. | Used to find dosing schedules that minimize an objective function combining tumor size and T-cell-mediated heart damage [5] [65]. |
| Patient-Derived Data | Used to initialize and calibrate models, moving them from theoretical to patient-specific tools. | Quantitative imaging, ctDNA levels, and biomarker data (e.g., T-cell counts) [5] [7]. |
| Circulating Tumor DNA (ctDNA) | A dynamic biomarker for monitoring tumor burden and early response to therapy. | Can be integrated into models to guide adaptive dosing decisions in clinical trials [7]. |
| Spatial Transcriptomics | Technology to analyze gene expression in the context of tissue architecture. | Helps understand the tumor microenvironment and identify novel predictive biomarkers for toxicity and response [7]. |
Troubleshooting Guides
Guide 1: Resolving Discrepancies Between Theoretical and Real-World Schedules
Problem: My optimal control model produces a theoretically perfect drug schedule, but it fails when applied to a real-world clinical context. The computed "optimal" schedule is not followed by patients or clinicians.
- Potential Cause 1: Patient Adherence Barriers. The model does not account for human factors leading to medication non-adherence.
- Solution: Integrate adherence modeling into your cost function. Model adherence as a function of regimen complexity (e.g., number of daily doses, food restrictions) and known socioeconomic barriers [70]. Use this to simplify the optimal schedule without significantly compromising efficacy, for instance, by reducing dosing frequency.
- Potential Cause 2: Operational Workflow Mismatch. The optimized schedule does not align with clinical workflows (e.g., administration times conflict with nurse rounds, or drug preparation logistics are too complex).
- Solution: Incorporate hard constraints into your nonlinear programming problem that reflect immutable operational timelines. Use discretization techniques with time steps that match the clinic's scheduling blocks (e.g., 30-minute or 1-hour intervals) to ensure generated schedules are executable [17].
Guide 2: Addressing Unpredictable Toxicity in Combination Therapies
Problem: A schedule optimized for a combination of chemotherapy drugs leads to unexpected, high toxicity in a subset of patients, derailing the treatment plan.
- Potential Cause: Inadequate Modeling of Heterogeneous Cell Response. The model treats the tumor as a homogeneous population and fails to account for different cell subtypes that may metabolize drugs differently, leading to variable toxicity and efficacy [26].
- Solution:
- Reframe your ODE model: Transition from a single-population model to a multi-population model that includes different cancer cell types and a state variable for healthy cells or cumulative toxicity [17] [26].
- Implement a modified cost function: Add a penalty term that severely constrains the cumulative toxicity metric. The Pontryagin Maximum Principle will then inherently work to keep toxicity below the defined bound [27].
- Validate with sigmoid functions: Replace sharp, discontinuous functions (like a Heaviside function for drug effect) with smoother sigmoid functions to ensure more realistic and numerically stable solutions [17].
Guide 3: Handling Numerical Instabilities in Optimal Control Solvers
Problem: The interior-point optimization solver (e.g., IPOPT) fails to converge to a solution, or the solution exhibits oscillatory behavior that is not clinically feasible.
- Potential Cause 1: Discontinuities in the System Dynamics. The use of non-smooth functions can cause solver failures.
- Solution: As implemented in successful studies, replace all Heaviside functions with smooth sigmoid approximations. This often resolves convergence issues without changing the fundamental optimal control strategy [17].
- Potential Cause 2: Poorly Scaled Variables. State and control variables (e.g., cell counts vs. drug concentration) are on vastly different numerical scales.
- Solution: Non-dimensionalize your system of differential equations before applying the discretization and nonlinear programming techniques. This normalizes all variables to a similar order of magnitude, significantly improving solver stability and convergence speed [17] [26].
Frequently Asked Questions (FAQs)
Q1: My model is mathematically sound, but clinicians reject the schedule as impractical. How can I bridge this gap? A1: This is a common challenge. True optimization requires integrating real-world constraints, not just solving the math [71]. Engage clinicians early in the model-building process to identify and codify unbreakable clinical rules (e.g., maximum daily infusion time, specific drug sequencing requirements). Embed these as hard constraints in your optimal control framework. Furthermore, present schedules in a format that seamlessly integrates with existing hospital workflows and electronic health records to increase adoption.
Q2: What is the most robust numerical method for solving these optimal control problems? A2: For problems with complex, constrained dynamics, the method of discretization followed by nonlinear programming has proven highly effective. This involves using a differential equation solver like the Implicit Euler method with a small time step (e.g., 0.01) to discretize the continuous system, transforming it into a large-scale, but finite, nonlinear programming problem. This problem can then be solved with robust solvers like IPOPT (Interior Point OPTimizer) linked through modeling languages such as AMPL [17].
Q3: Why does my optimal control solution often result in a "bang-bang" controller, and is this clinically acceptable? A3: For a wide class of linear-quadratic optimal control problems in cancer therapy, the optimal solution is indeed a bang-bang control, where drugs are administered at either their maximum or minimum (zero) dose [17]. This arises from the linearity of the system dynamics and the nature of the constraints. While mathematically optimal, this can be challenging clinically. Studies show that incorporating a sigmoid function for drug effect instead of a sharp switch does not necessarily change this bang-bang nature, suggesting it may be a fundamental property of the problem. Clinical acceptability depends on the specific drugs and patient tolerance; one strategy is to interpret the bang-bang schedule as a guide for when to initiate and pause therapy, rather than forcing instantaneous switching.
Q4: How can I model the synergistic effect of multiple drugs on a heterogeneous tumor? A4: A general ODE framework has been developed for this purpose [26]. The dynamics of multiple cell populations ((x \in R^n)) under multiple drugs ((u \in R^m)) can be modeled to include:
- Linear growth and death rates for each cell type.
- Terms for spontaneous cell differentiation/conversion.
- Drug-mediated effects (on proliferation and differentiation) modeled as linear combinations of (uk xi).
- Drug-drug synergy effects modeled by including terms for products of different drugs (e.g., (uk ul x_i)).
The following table summarizes key quantitative findings from recent studies on optimal control in cancer therapy.
Table 1: Performance of Optimal Control Strategies in Cancer Therapy Models
| Study Focus | Key Metric | Reported Value | Modeling Approach | Solver/Method |
|---|---|---|---|---|
| Constrained Drug Scheduling [17] | Highest Performance Index | 31.1132 | Bang-bang control via discretization & NLP | IPOPT with AMPL |
| Lowest Residual Cancer Cell Count | 0.0307 | Sigmoid/Heaviside function for drug effect | Implicit Euler method | |
| Combination Therapy for Heterogeneous Populations [26] | General ODE Framework | N/A | Multi-population model with drug synergy & spontaneous conversion | Pontryagin Maximum Principle |
| Combined Chemo-Radiation Therapy [27] | Application to Heterogeneous Tumors | N/A | Positive switched systems (Metzler matrices) | Switched system optimal control |
Experimental Protocols
Protocol 1: Implementing and Solving a Bang-Bang Optimal Control Problem for Drug Scheduling
This protocol is adapted from studies on cytotoxic drug scheduling (e.g., Doxorubicin, Cisplatin) using discretization and nonlinear programming [17].
1. Model Formulation:
- Define States and Dynamics: Establish a system of differential equations. A common structure includes:
- ( \frac{dN}{dt} = f(N, C, T) ) (Tumor cell dynamics)
- ( \frac{dC}{dt} = u(t) - \gamma C ) (Drug concentration dynamics; (u(t)) is the control)
- ( \frac{dT}{dt} = g(C, T) ) (Cumulative toxicity dynamics)
- Define the Cost Functional: Typically, the goal is to minimize tumor size and total drug use, subject to toxicity constraints. Example: ( J(u) = \int0^{tf} [N(t) + B \cdot u(t)] \, dt ), with ( T(t) \leq T_{max} ).
2. Numerical Discretization:
- Apply the Implicit Euler method with a small time step (e.g., ( \Delta t = 0.01 )) to convert the continuous-time system of ODEs and the cost functional into a discrete-time nonlinear programming problem.
3. Implementation and Solution:
- Code the discretized problem in a modeling language like AMPL (Applied Modeling Programming Language).
- Link the model to a large-scale nonlinear solver, such as IPOPT (Interior-Point OPTimizer).
- Run the optimization to compute the optimal state and control trajectories.
4. Validation and Analysis:
- Compare the results using different drug effect models (e.g., Heaviside vs. sigmoid function). Studies show the optimal strategy (bang-bang) may remain unchanged [17].
- Quantify the performance using indices like the final cost ( J ) and the residual cancer cell count at the final time.
Protocol 2: Modeling Multi-Drug Synergy in Heterogeneous Cell Populations
This protocol provides a framework for modeling the effect of multiple drugs on multiple cell types, including drug synergies [26].
1. General ODE Framework Setup:
- Let ( x \in R^n ) represent the counts of
ndifferent cell populations. - Let ( u \in R^m ) represent the effective pharmacodynamic action of
mdifferent drugs, where ( 0 \leq u_k \leq 1 ).
2. Model Structure:
- The general form of the ODE for the j-th cell type is: ( \frac{dx_j}{dt} = \text{(Linear growth term)} + \text{(Spontaneous conversion terms)} + \text{(Drug-mediated terms)} )
- Drug-mediated terms should include:
- Single-drug effects: Linear combinations of ( uk xi ) for different drugs
kand cell typesi. - Drug synergy effects: Linear combinations of ( uk ul x_i ) for
k ≠lto capture interactions between different drugs.
- Single-drug effects: Linear combinations of ( uk xi ) for different drugs
3. Optimal Control Application:
- Apply the Pontryagin Maximum Principle to this general ODE framework to derive the optimality conditions for the multi-drug control problem.
- The solution will define the optimal dosing policy ( u_k^*(t) ) over time for each drug to achieve a specified therapeutic goal, such as minimizing total tumor burden.
Research Reagent Solutions
Table 2: Essential Components for Optimal Control of Combination Therapy
| Item | Function in Research | Example/Note |
|---|---|---|
| Nonlinear Programming Solver | Solves the discretized optimal control problem numerically. | IPOPT (Interior-Point OPTimizer) is widely used for its efficiency with large-scale problems [17]. |
| Modeling Language | Provides a high-level language for expressing optimization models, simplifying interaction with solvers. | AMPL (Applied Modeling Programming Language) is commonly linked with IPOPT [17]. |
| ODE Numerical Solver | Discretizes continuous-time dynamics for numerical optimization. | The Implicit Euler Method is used for its stability and accuracy [17]. |
| Multi-Population ODE Framework | Models the response of heterogeneous cell populations to multiple drugs, including synergy. | A general framework includes terms for (uk xi) and (uk ul x_i) [26]. |
| Positive Switched System Models | Models cancer evolution under different treatment modalities (e.g., chemo vs. radiation). | Uses Metzler matrices and a switching law to design optimal therapy planning [27]. |
Visualizations: Signaling Pathways and Workflows
Computational Workflow for Therapy Optimization
Multi-Population Drug Interaction Framework
Frequently Asked Questions (FAQs)
FAQ 1: My optimal control model for drug scheduling is becoming computationally intractable with multiple cell populations and drugs. What strategies can I use to manage this high-dimensional state space? A primary strategy is to employ dimensionality reduction (DR) techniques to project your high-dimensional data into a lower-dimensional space while preserving critical structural relationships [72]. The choice of technique depends on the nature of your data's intrinsic geometry.
- Linear DR: Methods like Principal Component Analysis (PCA) are fast and interpretable, identifying orthogonal directions of maximal variance [72]. They are a good baseline but struggle with complex nonlinear manifolds [73] [74].
- Nonlinear DR (Manifold Learning): For data existing on nonlinear manifolds, techniques like t-SNE, UMAP, Isomap, and Locally-Linear Embedding (LLE) are more appropriate [72]. These are excellent for visualization and preserving local topology but can be computationally expensive and harder to interpret [74].
- Deep Learning-based DR: Autoencoders (AEs) and Variational Autoencoders (VAEs) use neural networks to learn efficient, nonlinear data encodings [72] [75]. These are powerful for complex representation learning and have been successfully coupled with optimization methods like Bayesian Optimization for high-dimensional problems [75].
Table 1: Comparison of Dimensionality Reduction Techniques for High-Dimensional Biological Data
| Method | Type | Key Principle | Advantages | Disadvantages |
|---|---|---|---|---|
| PCA [72] | Linear | Projects data onto directions of maximum variance. | Fast, interpretable, less prone to overfitting. | Fails to capture nonlinear relationships. |
| t-SNE [72] | Nonlinear | Preserves local similarities and neighborhood structures. | Excellent for visualization and clustering. | High computational cost, sensitive to parameters. |
| UMAP [72] | Nonlinear | Preserves both local and global topological structure. | Faster than t-SNE, better global structure preservation. | Can be sensitive to initialization and parameters. |
| Autoencoders [72] | Nonlinear (Deep Learning) | Neural network learns to compress and reconstruct data. | Highly flexible, can capture complex non-linearities. | "Black-box" nature, requires large data and tuning. |
FAQ 2: How can I efficiently model the nonlinear and synergistic interactions between different drugs in a combination therapy? Nonlinear dynamics are inherent in cancer biology, particularly in drug synergies and cell population interactions [26]. Optimal control frameworks address this by using systems of differential equations.
A general ODE model for multiple cell populations ((x \in R^n)) and drugs ((u \in R^m)) can be formulated to include terms for drug-drug interactions [26]. The model can capture phenomena like:
- Linear drug effects: Terms like (uk xi) represent the effect of a single drug on a cell population.
- Nonlinear synergistic effects: Terms like (xi uk u_\ell) (where (k \neq \ell)) model the interaction between two drugs [26].
From an algorithmic perspective, solving the resulting optimal control problem often requires discretization and nonlinear programming techniques. For example, one study used the Applied Modelling Programming Language (AMPL) with the Interior-Point optimization solver (IPOPT), employing an Implicit Euler method for discretization to handle the nonlinear system dynamics [17].
Table 2: Computational Tools for Solving Nonlinear Optimal Control Problems
| Tool/Algorithm | Function | Application Context |
|---|---|---|
| IPOPT [17] | Interior-Point optimizer for large-scale nonlinear programming. | Solving discretized optimal control problems for drug scheduling. |
| AMPL [17] | Algebraic modeling language for mathematical optimization. | Formulating and managing optimization models and data. |
| Implicit Euler Method [17] | Numerical procedure for solving differential equations. | Discretizing continuous-time ODE models for control. |
| Pontryagin Maximum Principle (PMP) [17] | Analytical method for optimal control. | Determining optimality conditions; often leads to "bang-bang" controls. |
FAQ 3: The computational cost of simulating combination therapy over long time horizons is prohibitive. How can I reduce the runtime? High computational cost arises from complex models, long time horizons, and the need for repeated simulations in optimization loops. Mitigation strategies include:
- Dimensionality Reduction: As outlined in FAQ 1, using DR as a preprocessing step can significantly reduce the problem size fed to the optimization algorithm [72] [75].
- Model Simplification: Consider using simplified, yet representative, model forms. Some frameworks use linear growth rates in the absence of drugs to maintain analytical tractability, which is appropriate in certain contexts [26].
- Efficient Numerical Solvers: Leverage state-of-the-art solvers like IPOPT that are designed for large-scale problems [17]. Employing fixed-step, implicit solvers can enhance stability and speed for stiff ODE systems.
- Scalable Algorithms: For Bayesian optimization in high dimensions, methods like Latent-Space Bayesian Optimization (LSBO) using VAEs, coupled with Sequential Domain Reduction (SDR), have shown improved optimization quality and efficiency by narrowing the search space adaptively [75].
Troubleshooting Guides
Problem: Unstable or Oscillatory Solutions in Optimal Control Schedule
- Check: The numerical discretization scheme and step size. A too-large step size can cause instability in solving the model's differential equations.
- Solution: Implement a more stable implicit method (e.g., Implicit Euler) and consider reducing the time step [17]. Validate your solution across different step sizes to ensure consistency.
Problem: Optimized Dosing Schedule is Impractical (Extremely Frequent Dosing Changes)
- Check: The structure of the optimal control solution. Applications of the Pontryagin Maximum Principle (PMP) often result in "bang-bang" controls, where drug dosing switches abruptly between maximum and minimum values [17].
- Solution: This may be a feature of the model rather than a bug. To find more practical schedules, you can reformulate the cost function to penalize frequent switching or enforce a minimum dwell time for each dosing level.
Problem: Dimensionality Reduction Method Performs Poorly, Obscuring Biological Meaning
- Check: If the assumptions of the DR method match your data. Using linear PCA on data with strong nonlinear manifold structure will yield poor results [73].
- Solution: Experiment with nonlinear DR methods like UMAP or Isomap. If interpretability is crucial, use methods that allow for inverse mapping (like PCA or certain autoencoders) to relate results back to the original features [72] [74].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Key Computational and Biological Resources
| Item | Function/Description | Example Application |
|---|---|---|
| Interior-Point Optimizer (IPOPT) [17] | Solves large-scale nonlinear optimization problems. | Finding optimal drug doses in discretized control models. |
| Applied Modelling Programming Language (AMPL) [17] | High-level language for defining optimization models. | Prototyping and solving optimal control scheduling problems. |
| Variational Autoencoder (VAE) [75] | Deep learning model for nonlinear dimensionality reduction. | Reducing high-dimensional cell population or genomic data for efficient optimization. |
| Pontryagin Maximum Principle (PMP) [17] | Analytical framework for deriving optimal control trajectories. | Theoretical analysis of optimal drug scheduling; often confirms bang-bang solutions. |
| Synergistic Drug Interaction Term [26] | A nonlinear term (e.g., (xi uk u_\ell)) in an ODE model. | Modeling the enhanced effect of two drugs used in combination. |
| CAR-T Cells [76] | Genetically engineered T-cells for immunotherapy. | Used in combination therapy models with targeted radionuclide therapy. |
| Targeted Radionuclide Therapy (TRT) [76] | Radiation therapy delivered via tumor-targeting agents. | Combined with immunotherapy in mathematical models to optimize timing. |
Experimental Protocol: Calibrating a Combination Therapy Model
This protocol outlines the steps for calibrating a mathematical model of combination therapy, such as one combining Targeted Radionuclide Therapy (TRT) and CAR-T cell immunotherapy [76].
Objective: To estimate model parameters (e.g., killing rates, proliferation rates, clearance rates) from experimental data to enable in-silico optimization of dosing and scheduling.
Workflow Diagram: Combination Therapy Model Calibration
Materials and Reagents:
- Preclinical Model: (e.g., mouse model engrafted with cancer cells) [76].
- Therapeutic Agents: Stocks of all drugs and biologics used in the combination (e.g., CAR-T cells, TRT agent like ²²âµAc-daratumumab) [76].
- Data Collection Tools: Equipment for in-vivo imaging (e.g., bioluminescence for tumor burden) and flow cytometry for immune cell counts.
Procedure:
- Monotherapy Experiments: Treat separate cohorts with each therapy (TRT or CAR-T) as a monotherapy across a range of doses [76].
- Data Collection: Collect high-frequency time-series data on tumor volume and relevant immune cell populations (e.g., CAR-T cell counts in blood/tumor) until the end of the study or animal euthanasia [76].
- Parameter Fitting: Use the monotherapy data to fit the model parameters. For example, use TRT monotherapy data to estimate radiation killing rates ((kR)) and CAR-T monotherapy data to estimate tumor killing ((k1)) and CAR-T proliferation/exhaustion ((k_2)) rates [76]. This is typically done via optimization algorithms that minimize the error between model output and experimental data.
- Model Validation: Use a separate set of experimental data where therapies are combined, especially with different timings (e.g., CAR-T cells administered at various days post-TRT), to validate the predictive power of the calibrated model [76].
- In-Silico Optimization: Once validated, use the model with the calibrated parameters within an optimal control framework to simulate and identify superior dosing and scheduling regimens for testing.
Experimental Protocol: Implementing Latent-Space Bayesian Optimization
This protocol is for using dimensionality reduction to manage high computational cost in optimizing expensive black-box functions, such as tuning combination therapy parameters.
Objective: To efficiently optimize a high-dimensional objective function (e.g., tumor reduction with toxicity penalty) by reducing its dimensionality using a VAE and performing Bayesian Optimization in the latent space.
Workflow Diagram: Latent-Space Bayesian Optimization
Materials and Software:
- High-Dimensional Dataset: A dataset of therapy parameters (e.g., drug doses, timing) and their outcomes for initial VAE training.
- Software Stack: GPU-accelerated deep learning framework (e.g., PyTorch, TensorFlow) for VAE training, and a Bayesian optimization library (e.g., BoTorch, GPyOpt) [75].
Procedure:
- VAE Training: Train a Variational Autoencoder (VAE) on the available high-dimensional parameter data. The VAE learns a compressed, lower-dimensional latent representation (the encoder) and how to reconstruct data from it (the decoder) [75].
- Latent Space Definition: The optimization problem is now redefined in the VAE's latent space. The goal is to find the latent vector (z) that, when decoded, yields high-performing therapy parameters.
- Bayesian Optimization Loop:
- Build a Gaussian process surrogate model of the objective function in the latent space.
- Use an acquisition function (e.g., Expected Improvement) to select the next most promising latent point (z) to evaluate.
- Decode the selected (z) back to the original high-dimensional parameter space using the VAE decoder.
- Evaluate the decoded parameters on the expensive objective function (e.g., run a simulation).
- Update the surrogate model with the new ((z, \text{result})) pair.
- Iteration: Repeat step 3 until convergence to a set of optimal parameters. Optionally, the VAE can be retrained periodically as new data is collected to improve the latent space representation [75].
Integrating Multi-Omics and Patient-Specific Data for Robust Model Calibration
Frequently Asked Questions & Troubleshooting Guides
This technical support resource addresses common challenges researchers face when integrating multi-omics data for calibrating patient-specific models in optimal control theory for cancer therapy.
Data Integration & Preprocessing
FAQ: What are the primary strategies for multi-omics data integration, and how do I choose between them?
Three primary integration strategies exist, each with distinct advantages and limitations:
Early Integration: Combines raw or preprocessed data from different omics sources into a single dataset before analysis.
Intermediate Integration: Uses statistical or ML models to extract features from each omics dataset separately before integration.
- Best for: Balancing the unique characteristics of each data type while capturing cross-omics interactions.
- Example: Methods like MOFA+ learn a shared low-dimensional representation across omics datasets [78].
Late Integration: Analyzes each omics dataset independently and combines the results at the final stage.
Troubleshooting Guide: My integrated model performance is poor due to high-dimensional data and noise. What should I do?
- Problem: Model accuracy decreases as more omics modalities are added.
- Solution:
- Implement Dimensionality Reduction: Use feature selection techniques like LASSO (Least Absolute Shrinkage and Selection Operator) or elastic net to identify and retain the most informative variables from each omics dataset [77] [79].
- Apply Robust Normalization: Normalize concatenated data to a mean of zero and variance of one. For datasets with differing variable counts and noise levels, consider Matrix Factorization Analysis (MFA) normalization, which weights each platform equally by dividing its data block by the square root of its first eigenvalue [77] [79].
- Prioritize Informative Modalities: Rely on modalities with known predictive value for your specific cancer type. Studies show that incorporating non-informative or overly noisy data degrades model performance [80].
- Leverage Noise-Resistant Algorithms: Consider methods that have demonstrated better noise resistance, such as PriorityLasso or BlockForest, when the informativeness of all modalities is uncertain [80].
Model Calibration & Validation
FAQ: How can I handle missing data in multi-omics datasets for patient-specific model calibration?
- Problem: Missing data points for specific omics measurements in patient samples.
- Solution:
- Advanced Imputation: Employ advanced imputation strategies like matrix factorization or deep learning-based reconstruction to estimate missing values [81].
- Algorithm Selection: Choose modeling approaches that can handle missing data natively. Some methods, like certain Bayesian models, can be robust to missingness without requiring direct imputation.
Troubleshooting Guide: My patient-specific model fails to generalize or calibrate accurately. How can I improve robustness?
- Problem: Model is overfit to training data or fails to converge during calibration.
- Solution:
- Incorporate Biological Constraints: Use "mechanistic learning" by integrating prior biological knowledge (e.g., known signaling pathways) into your deep learning architecture. This combines AI's scalability with the interpretability and robustness of mechanistic models [82].
- Rigorous External Validation: Always validate your calibrated models on independent, external datasets. Performance on the training set is not a reliable indicator of real-world utility [81].
- Utilize Explainable AI (XAI): Apply techniques like SHapley Additive exPlanations (SHAP) to interpret your model's predictions. This helps identify which omics features are driving the calibration and can reveal spurious correlations or biological insights [81].
- Federated Learning for Data Scarcity: If patient data is limited, consider federated learning approaches. This allows for collaborative model training across multiple institutions without sharing raw patient data, preserving privacy while increasing effective sample size [81].
The table below summarizes quantitative performance data from recent multi-omics integration studies in oncology, providing benchmarks for model evaluation.
Table 1: Performance Metrics of Multi-Omics Integration in Cancer Research
| Study Application | Cancer Type(s) | Method(s) Used | Key Performance Metric | Result | Citation |
|---|---|---|---|---|---|
| Survival Analysis | Breast Cancer | Genetic Programming-based Integration | Concordance Index (C-index) | 67.94 (test set) | [78] |
| Survival Analysis | Pan-Cancer (TCGA) | PriorityLasso, BlockForest | Noise Resistance & Discriminative Performance | Superior to most deep learning models | [80] |
| Early Detection | Various | Integrated Classifiers | Area Under Curve (AUC) | 0.81 - 0.87 | [81] |
| Subtype Classification | Breast Cancer | DeepMO (Deep Neural Network) | Binary Classification Accuracy | 78.2% | [78] |
| Survival Prediction | Liver, Breast Cancer | DeepProg | Concordance Index (C-index) | 0.68 - 0.80 | [78] |
Experimental Protocols for Robust Workflows
Protocol 1: Standardized Multi-Omics Data Preprocessing for Model Calibration
This protocol ensures data quality and compatibility before integration.
- Data Acquisition: Source data from public repositories like The Cancer Genome Atlas (TCGA) or internal cohorts. Ensure data includes genomics, transcriptomics, epigenomics, and proteomics where available.
- Platform-Specific QC & Normalization:
- Data Harmonization:
- Feature Reduction:
Protocol 2: Calibrating a Patient-Specific "Digital Twin" for Therapy Optimization
This protocol outlines steps to create and calibrate a model for simulating treatment.
- Model Selection: Choose a mechanistic model (e.g., a system of ordinary differential equations) that describes tumor-immune-drug interactions relevant to your cancer type [82] [84].
- Parameterization:
- Define Patient-Specific Parameters: Identify model parameters that will be calibrated using the integrated multi-omics data (e.g., proliferation rates, drug sensitivity coefficients).
- Set Population Priors: Use literature or population-level data to define plausible initial ranges for these parameters.
- Model Calibration:
- Input: Use the preprocessed, integrated multi-omics profile of a single patient.
- Optimization: Employ optimization algorithms (e.g., interior point optimization - IPOPT) to find the parameter set that minimizes the difference between the model's output and the patient's actual molecular and clinical data [84].
- Validation and Simulation:
- Internal Validation: Ensure the calibrated model can recapitulate the patient's known disease trajectory.
- In-Silico Treatment Screening: Run the calibrated model with different combination therapy schedules (e.g., varying timing and doses of chemo- and immunotherapy) to predict outcomes [85] [84].
- Optimal Control Application: Apply optimal control theory (OCT) to the validated model to compute the therapy schedule that maximizes tumor cell kill while minimizing toxicity [84].
Experimental Workflow Visualization
The diagram below illustrates the logical workflow for integrating multi-omics data to calibrate a patient-specific model for therapy optimization.
Research Reagent Solutions
The table below lists key computational tools and resources essential for multi-omics integration and model calibration.
Table 2: Essential Computational Tools for Multi-Omics Integration & Model Calibration
| Tool / Resource | Function | Use Case in This Context |
|---|---|---|
| mixOmics (R) [83] | Multi-omics data integration and exploration. | Performing early and intermediate integration; dimensionality reduction. |
| INTEGRATE (Python) [83] | Multi-omics data integration and analysis. | An alternative Python-based environment for building integrated analysis pipelines. |
| MOFA+ [78] | Bayesian group factor analysis. | Learning a shared low-dimensional representation from multiple omics datasets in an unsupervised manner. |
| PriorityLasso [80] | Regularized regression with pre-defined data block priority. | Building noise-resistant survival models when the informativeness of omics modalities differs. |
| IPOPT [84] | Interior Point Optimizer for large-scale nonlinear optimization. | Solving the parameter estimation problem during the calibration of complex, patient-specific mechanistic models. |
| TCGA [81] [78] | The Cancer Genome Atlas database. | A primary source for standardized multi-omics cancer data for model training and validation. |
Validation and Comparative Analysis: Benchmarking OCT Strategies for Clinical Translation
In silico validation uses computational simulations to predict how cancer cell lines will respond to treatment, playing a crucial role in modern oncology research and drug development. These models integrate multi-omics datasets (genomics, transcriptomics, proteomics) with mathematical frameworks to simulate tumor dynamics and therapeutic interventions before laboratory testing. The primary goal is to provide a robust, computational foundation for predicting treatment efficacy, optimizing combination therapies, and ultimately accelerating the development of personalized cancer treatments. For researchers focusing on optimal control theory for cancer combination therapy scheduling, in silico models provide the essential experimental platform for testing and validating sophisticated dosing algorithms in a virtual, controlled environment.
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental purpose of in silico validation in the context of optimal therapy scheduling?
In silico validation serves as a critical bridge between theoretical control models and clinical application. It uses computational simulations to test and validate mathematical models that predict tumor response to drug combinations. For optimal control theory, which aims to determine the best possible drug dosing schedules to maximize efficacy and minimize toxicity, in silico models provide a virtual testing ground. They allow researchers to simulate how different control policies (e.g., bang-bang control, continuous control) affect heterogeneous cell populations over time, incorporating realistic constraints like drug synergies and cell conversion rates before moving to costly and time-consuming in vitro or in vivo studies [26] [86].
FAQ 2: What are the key data requirements for building a predictive in silico model?
A robust in silico model is built on a foundation of high-quality, multi-faceted data. The core requirements include:
- Genetic Profiles: Data on genetic variants, mutations, and gene expression patterns from sources like whole exome or whole genome sequencing of cancer cell lines. These help define the inherent characteristics of each cell line [87] [88].
- Drug Response Data: Dose-response curves and viability assays for various drugs, which are used to calibrate and validate the model's predictions against empirical results [89] [86].
- Tumor Dynamics Data: Information on cell proliferation rates, death rates, and heterogeneity. Models often use systems of ordinary differential equations (ODEs) to simulate these dynamics, requiring parameters for growth and death rates [26] [90].
- Treatment Constraints: Parameters related to drug toxicity and pharmacokinetics, which are essential for designing realistic and clinically relevant optimal control schedules [17] [91].
FAQ 3: How do I account for cell line misidentification and contamination in my model?
Cell line misidentification is a pervasive problem that can invalidate research findings. To address this computationally, tools like the Uniquorn R-package can be integrated into your validation workflow. Uniquorn performs robust in-silico identification of cancer cell lines based on their variant profiles derived from sequencing data (WES or WGS). It compares a query sample's profile against a reference library of known cell lines, achieving high sensitivity (97%) and specificity (99%). This ensures the genetic identity of the cell lines used in your simulations matches their presumed origin, safeguarding the integrity of your validation results [87].
FAQ 4: My model's predictions do not match experimental results. What are the primary areas to troubleshoot?
Discrepancies between simulation and experiment often originate from a few key areas:
- Data Quality and Quantity: Incomplete, low-quality, or biased training datasets are a leading cause of model inaccuracy. Ensure your data is curated from diverse, reliable sources and is of sufficient scale [86].
- Model Overfitting: The model may perform well on training data but fail to generalize. This can be mitigated through techniques like cross-validation and by using simpler models if appropriate [88].
- Incorrect Parameterization: The mathematical parameters governing tumor growth, drug effect, or immune cell interaction may be inaccurate. Perform sensitivity analysis, like Latin Hypercube Sampling, to identify which parameters most influence your model's output and refine them [90].
- Inadequate Biological Complexity: The model might be missing a key biological process, such as drug-drug synergies, the tumor microenvironment, or specific immune cell interactions. Review the biology and consider extending your model's framework to incorporate these elements [26] [91].
FAQ 5: Can in silico models incorporate the side effects of cancer therapies?
Yes, and they should for a holistic optimization approach. Advanced models now include multi-compartment designs to simulate side effects. For example, a heart-tumour model was developed to simulate autoimmune myocarditis, a rare but fatal side-effect of Immune Checkpoint Inhibitors (ICIs). This model was then used within an optimal control framework to design ICI dosing schedules that effectively balance tumor inhibition with the risk of triggering myocarditis, demonstrating that side-effects significantly impact the predicted optimal dosing strategy [91].
Essential Protocols for Key Experiments
Protocol: Simulating Combination Therapy on Heterogeneous Cell Populations
This protocol is designed for researchers applying optimal control theory to multi-drug regimens, using a framework based on systems of coupled, semi-linear ordinary differential equations [26].
1. Problem Formulation and Model Selection:
- Define Cell Populations: Identify the distinct cell types (e.g., drug-sensitive, drug-resistant, differentiated states) to be modeled. Represent their counts in a state vector (\mathbf{x} \in \mathbb{R}^n).
- Define Drug Controls: Identify the drugs in the combination therapy. Represent their pharmacodynamic effects (not raw concentrations) in a control vector (\mathbf{u} \in \mathbb{R}^m), where (0 \leq u_k \leq 1).
- Select Growth and Interaction Laws: Use linear growth rates for simplicity and analytical tractability. Incorporate terms for spontaneous cell conversion and drug-mediated conversion.
2. Model Implementation:
- Governing Equations: Implement the core system of ODEs. The general form for the j-th cell type includes:
- Linear proliferation and death terms.
- Terms for spontaneous conversion from other cell types.
- Terms for drug-mediated killing ((uk xi)).
- Terms for synergistic drug-drug interactions ((xi uk u_\ell)).
- Parameterization: Acquire model parameters (growth rates, conversion rates, drug efficacy) from prior literature or calibrate them using experimental data.
3. Optimal Control Solution:
- Apply Pontryagin's Maximum Principle (PMP): Use PMP to derive the necessary conditions for optimality. This involves defining the Hamiltonian and adjoint systems [17] [90].
- Numerical Solution: Solve the resulting boundary value problem using discretization and non-linear programming solvers like IPOPT (Interior-Point Optimizer) [17].
4. In Silico Validation:
- Simulate Treatment Scenarios: Run the model with the obtained optimal control policy (\mathbf{u}^*(t)).
- Output Analysis: Analyze the resulting dynamics of all cell populations over time to verify that the therapy achieves the desired objective (e.g., tumor eradication, containment) while respecting constraints.
Protocol: Validating Predictions with Patient-Derived Models
This protocol outlines how to cross-validate in silico predictions using experimental data from advanced pre-clinical models, a service emphasized by organizations like Crown Bioscience [86].
1. Generate Predictions from In Silico Model:
- Input the genetic and molecular profile of a specific cancer cell line or patient-derived model into your validated in silico tool.
- Output a prediction of the tumor's response (e.g., growth trajectory, viability) to a specific drug or drug combination.
2. Cross-Validate with Experimental Data:
- Acquire Experimental Models: Use relevant patient-derived xenografts (PDXs), organoids, or tumoroids that match the genetic profile used in the simulation.
- Perform Drug Assay: Treat the experimental models with the same therapy predicted in silico.
- Measure Response: Quantify the treatment response using metrics like cell viability, tumor volume, and apoptosis assays.
3. Compare and Refine:
- Quantitative Comparison: Statistically compare the simulated growth curves with the experimentally observed data.
- Iterative Refinement: If a significant discrepancy exists, troubleshoot by re-examining model parameters, data quality, and underlying biological assumptions. Use longitudinal data from the experiments to further refine the AI algorithms powering the model [86].
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Essential Computational Tools and Resources for In Silico Validation
| Tool / Resource Name | Function / Purpose | Key Characteristics |
|---|---|---|
| Uniquorn [87] | Cancer Cell Line Identification | R/Bioconductor package; uses WES/WGS data to verify cell line identity, preventing misidentification. |
| OncoOrigin [88] | Primary Cancer Site Prediction | XGBoost-based classifier; predicts tissue of origin for CUPs; features a GUI for clinical use. |
| IPOPT Solver [17] | Optimal Control Solution | Interior-Point Optimizer; used for large-scale, non-linear optimization problems in discretized control. |
| COMSOL Multiphysics [92] | Spheroid & Microenvironment Modeling | Simulates nutrient diffusion, growth, and necrosis in 3D tumor spheroids. |
| Digital Twin Technology [86] | Hyper-Personalized Therapy Simulation | Creates a virtual replica of a patient's tumor for simulating and optimizing treatment outcomes. |
Troubleshooting Guides
Common Errors in Model Calibration and Parameter Fitting
Problem: Poor Model Fit to Training Data
- Potential Cause 1: The objective function for calibration is poorly formulated.
- Solution: Use maximum likelihood estimators or other robust statistical methods for parameter estimation to better recapitulate observed tumor growth [17].
- Potential Cause 2: The model is structurally incorrect for the biology being modeled.
- Solution: Revisit model assumptions. For example, for nutrient-limited growth in spheroids, ensure the model includes terms for nutrient diffusion and consumption, which are critical for predicting necrotic core formation [92].
Problem: Model Fails to Generalize to New Data
- Potential Cause: Overfitting to the calibration dataset.
- Solution: Implement cross-validation during the calibration process. Split data into training and validation sets, and use regularization techniques to penalize overly complex models [88].
Addressing Numerical Instabilities in Optimal Control Solutions
Problem: Bang-Bang Control is Overly Simplistic or Impractical
- Solution: Instead of optimizing a continuous drug concentration, optimize the timing of fixed-dose administrations. This approach is more clinically realistic for therapies like Immune Checkpoint Inhibitors (ICIs) which are administered intermittently [91].
Problem: Numerical Artifacts in Control Trajectories
- Solution: Be aware that different optimization software (e.g., MATLAB, Pyomo, AMPL, JuMP) can produce suboptimal or varying results for the same problem due to differences in numerical implementations. Verify solutions across multiple platforms if possible [90].
Workflow and Pathway Visualizations
In Silico Validation and Optimal Control Workflow
The following diagram visualizes the complete integrated workflow for developing and validating an optimal control schedule using in silico models.
Core Components of an Optimal Control Framework for Therapy
This diagram breaks down the key mathematical components of an optimal control problem as applied to cancer therapy scheduling.
Quantitative Performance Comparison of OCT Algorithms
The following tables summarize the key quantitative findings from a study that directly compared the performance of Interior Point Optimization (IPOPT), State-Dependent Riccati Equation (SDRE), and Approximate Sequence Riccati Equation (ASRE) in optimizing cancer combination therapy [6] [93].
Table 1: Overall Optimization Performance Metrics
| Algorithm | Full Name | Cost Value | Key Characteristics |
|---|---|---|---|
| IPOPT | Interior Point OPTimizer | 52.3573 [6] [93] | Open-source tool for large-scale nonlinear optimization [6] [93]. |
| SDRE | State-Dependent Riccati Equation | 52.424 [6] [93] | Adapts linear control methods for nonlinear situations; a "pseudo-linear" method [6] [19]. |
| ASRE | Approximate Sequence Riccati Equation | 52.424 [6] [93] | A globally optimal feedback control approach for nonlinear systems [6] [93]. |
Table 2: Biological Outcome Comparison
| Biological Variable | Algorithm | Continuous (C) Value | Dosed (D) Value |
|---|---|---|---|
| CD8+ T cells | IPOPT, SDRE, ASRE | 1.6499 (all techniques) [6] [93] | 1.6499 (all techniques) [6] [93] |
| Tumor Cell Counts | IPOPT | 0.0007 [6] [93] | 0 [6] [93] |
| Tumor Cell Counts | SDRE, ASRE | 0.0006 [6] [93] | 0 [6] [93] |
Essential Research Reagents & Computational Tools
Table 3: Key Components for OCT Experiments in Cancer Therapy
| Item Name | Function/Description | Relevance to OCT Experiments |
|---|---|---|
| Tumor Growth Inhibition (TGI) Model | A mathematical model, often nonlinear, that describes how tumor volume changes over time in response to treatment [19]. | Serves as the core dynamic system in the optimal control problem; its equations form the constraints that the controller must optimize against [19]. |
| State-Space Model | A set of differential equations representing the system dynamics, where the state vector includes variables like tumor cell count and immune cell concentration [19]. | Provides the formal framework ( ( \dot{x} = f(x(t)) + G(x(t))u(t) ) ) required for applying SDRE, ASRE, and other state-space control methods [19]. |
| SDC Parameterization | The process of factoring the nonlinear state-space model into State-Dependent Coefficient (SDC) matrices, i.e., ( \dot{x} = A(x)x + B(x)u ) [19]. | A critical first step for implementing the SDRE and ASRE algorithms, which rely on this pseudo-linear form [19]. |
| Cost Function Weights (Q, R) | User-defined matrices that penalize the state variables (e.g., tumor size) and control inputs (e.g., drug dose) in the quadratic cost function [19]. | Central to all three algorithms (IPOPT, SDRE, ASRE). The balance between these weights dictates the trade-off between treatment efficacy and drug toxicity [6] [19]. |
Experimental Protocol: Implementing and Comparing OCT Algorithms
This protocol outlines the key steps for implementing and comparing SDRE, ASRE, and IPOPT for cancer therapy optimization.
Problem Formulation
- Define the Dynamical System: Start with a validated, patient-specific mathematical model of tumor-immune dynamics and treatment response. The model should be a state-space system where the state vector (x) includes variables such as tumor cell population, immune cell concentrations (e.g., CD8+ T cells), and drug concentration [19].
- Formulate the Cost Function: Establish a quadratic cost function, ( J = \sum (x^T Q x + u^T R u) ), where (Q) and (R) are weighting matrices that reflect the relative importance of minimizing tumor burden versus treatment toxicity [19]. This function is the objective that the optimal control seeks to minimize.
Algorithm Implementation
- SDRE (State-Dependent Riccati Equation) Workflow:
- SDC Parameterization: Factor the nonlinear system dynamics into the form ( \dot{x} = A(x)x + B(x)u ). This representation is not unique and is a critical design choice [19].
- Solve the SDRE: At each time step, given the current state (x), compute the matrix (A(x)) and (B(x)). Then, solve the state-dependent Riccati equation: ( A^T(x)P + P A(x) - P B(x) R^{-1} B^T(x) P + Q = 0 ) for the matrix (P) [19].
- Compute Control Law: Calculate the suboptimal control input as ( u = -R^{-1} B^T(x) P x ) [19].
- ASRE (Approximate Sequence Riccati Equation) Workflow:
- IPOPT (Interior Point OPTimizer) Workflow:
- Discretization: Transform the continuous-time optimal control problem into a large-scale, but finite-dimensional, nonlinear programming (NLP) problem by discretizing both the state and control trajectories over the treatment horizon [6].
- Solve the NLP: Use the IPOPT solver to find the sequence of control inputs (drug doses) that minimize the cost function while satisfying the discretized system dynamics and any other constraints (e.g., maximum dose) [6]. This typically produces an open-loop optimal control trajectory.
Performance Evaluation
- Run Simulations: Apply the control laws generated by each algorithm to the original tumor growth model in simulation.
- Compare Metrics: Record and compare the final cost value (J), the final tumor cell count, the health of critical immune cells (e.g., CD8+ T cells), and the resulting drug dosage profiles [6] [93].
Troubleshooting Guides & FAQs
FAQ 1: My SDRE controller is becoming unstable or failing to converge. What could be wrong?
This is a common issue that often stems from the core properties of the SDC parameterization or the solver.
Potential Cause 1: Poor State-Dependent Coefficient (SDC) Parameterization.
- Explanation: The factorization of the nonlinear dynamics into (A(x)x + B(x)u) is not unique. An poorly chosen (A(x)) can lead to uncontrollable pseudo-linearizations at certain state values, causing the Riccati equation solver to fail [19].
- Solution: Experiment with different SDC factorizations. The primary goal is to find a parameterization where the pair ((A(x), B(x))) is pointwise stabilizable for all relevant states (x) in the operating region.
Potential Cause 2: Numerical Issues in Solving the Riccati Equation.
- Explanation: The Riccati equation must be solved numerically at each integration time step. If the system matrices are ill-conditioned or the solver is not robust, it can produce invalid results.
- Solution:
- Use a reliable and robust numerical solver for the continuous-time algebraic Riccati equation.
- Check the condition numbers of your (A(x)) and (B(x)) matrices.
- Consider implementing a backup strategy, such as holding the previous control value, if the solver fails at a single point.
FAQ 2: When should I choose a direct method like IPOPT over a feedback method like SDRE/ASRE?
The choice involves a fundamental trade-off between computational burden, optimality, and practical implementation.
Choose IPOPT (Direct/Open-Loop) when:
- You need high numerical accuracy for a pre-computed plan and can run optimizations offline.
- Your model and problem are highly nonlinear and complex, making feedback law derivation difficult.
- You need to easily incorporate complex path and endpoint constraints (e.g., cumulative dose limits) [6].
Choose SDRE/ASRE (Feedback/Closed-Loop) when:
- Robustness to uncertainties is a primary concern. These methods automatically adjust the control input based on the current simulated state of the tumor, making them more adaptive to model discrepancies or unexpected patient responses [6] [19].
- You require real-time computability. While still computationally intensive, the state-feedback form can be more efficient for on-the-fly recalculations.
FAQ 3: The cost values for my algorithms are much higher than reported in the literature. How can I adjust my setup?
This typically indicates an issue with the scaling of your problem or the tuning of the cost function weights.
Solution 1: Re-scale your state and control variables.
- Explanation: If the numerical values of your tumor cell count (e.g., 1,000,000) and drug dose (e.g., 0.5) are orders of magnitude apart, it can lead to poorly conditioned optimization problems.
- Action: Normalize your state and control variables to be on a similar scale (e.g., between 0 and 1, or around a nominal value of 1).
Solution 2: Re-tune the weighting matrices Q and R.
- Explanation: The balance between the state penalty (Q) (tumor size) and the control penalty (R) (treatment cost/toxicity) directly determines the final cost value (J) and the aggressiveness of the therapy [19].
- Action: Systematically vary the values in (Q) and (R). Increasing (R) relative to (Q) will lead to less aggressive treatment, higher final tumor burden, but a lower overall cost (J). This is an iterative process that defines the clinical objectives of the therapy.
## Frequently Asked Questions (FAQs)
FAQ 1: What are the key early indicators of treatment efficacy beyond traditional RECIST categories? Early Tumor Shrinkage (ETS) and Depth of Response (DpR) are two key metrics that provide a more dynamic and predictive assessment of treatment efficacy. ETS measures the percentage reduction in the sum of the longest diameters (SLD) of target lesions at the first radiological assessment (typically 6-12 weeks after treatment initiation) and serves as an early signal of treatment sensitivity. DpR quantifies the maximum tumor shrinkage achieved during the entire course of therapy and is more strongly correlated with long-term survival outcomes such as Overall Survival (OS). Both are continuous variables that offer more granular information than the categorical CR, PR, SD, and PD of standard RECIST criteria [94] [95].
FAQ 2: How do I handle non-proportional hazards and heterogeneous treatment effects in survival analysis?
The hazard ratio (HR) can be difficult to interpret when the treatment benefit is not consistent over time or across patient subgroups. The personalized chance of a longer survival is a patient-focused measure that quantifies the probability that a random patient in the treatment group survives longer than a random patient in the control group by at least a pre-specified amount of time (denoted m months), adjusted for the inherent variability in the control arm. This measure, defined as Δ(m) = P{T(1) > T(0) + m} - P{T̃(0) > T(0) + m}, is intuitively interpretable and remains valid even when the proportional hazards assumption is violated [96].
FAQ 3: What modeling frameworks are available for optimizing combination therapy scheduling? Optimal Control Theory (OCT) provides a powerful mathematical framework for designing personalized combination therapy schedules. It uses a system of differential equations to model the dynamics of tumor cell populations, immune responses, and drug interactions. The goal is to compute a drug dosing strategy that minimizes a cost function, which typically includes terms for tumor cell count and drug toxicity. Solution methods include bang-bang control (which suggests alternating between maximum and zero drug doses) and non-linear programming solvers like the Interior-Point Optimizer (IPOPT) [17] [26] [6]. These models can be adapted to account for heterogeneous cell populations and multi-drug synergies [26].
FAQ 4: How can tumor burden be quantified from medical images in preclinical models? In genetically engineered mouse models (GEMMs), where manual measurement is challenging, fully automated volumetric analysis of micro-CT images provides a robust and high-throughput solution. The method involves segmenting a consistent region of interest within the rib cage and calculating the total soft tissue volume, while automatically estimating and subtracting the heart volume. This automated tumor burden metric has been validated against manual methods and shows high correlation, enabling efficient screening and randomization of animals in preclinical drug studies [97].
## Troubleshooting Guides
Problem 1: Inconsistent or Ambuous Early Tumor Shrinkage (ETS) Definitions
Symptoms: Inability to compare ETS values across different clinical trials; uncertainty in selecting a meaningful cutoff point for clinical decision-making. Solution:
- Pre-define Assessment Timing: Standardize the first tumor assessment to a specific time window, most commonly 6 to 12 weeks after treatment initiation [94].
- Justify Cut-off Selection: Base the ETS threshold (e.g., 10%, 20%, or 30% reduction in SLD) on the specific cancer type, treatment modality, and available historical data from similar trials. For instance, a 10% reduction at week 6 has been used as a cutoff in NSCLC studies involving immunotherapy [94].
- Report Continuously: Whenever possible, report ETS as a continuous variable alongside binary classifications to preserve information and facilitate cross-trial comparisons [94].
Problem 2: Suboptimal Dosing Schedules in Combination Therapy
Symptoms: Excessive toxicity leading to treatment interruption; suboptimal tumor cell kill; emergence of drug resistance. Solution:
- Formulate an Optimal Control Problem:
- Define System Dynamics: Create a mathematical model (e.g., a system of ODEs) describing tumor growth, immune cell activity, and drug effects [26] [6].
- Define Cost Function: Formulate an objective function to be minimized. This typically includes the final tumor volume and the cumulative drug toxicity, weighted appropriately [6].
- Apply Constraints: Impose constraints on maximum allowable drug doses and overall toxicity [17].
- Compute the Optimal Control: Use computational solvers like IPOPT to calculate the drug administration schedule (e.g., bang-bang control or continuous dosing) that minimizes the cost function [17] [6].
- Validate Clinically: Correlate the model-predicted optimal schedules with clinically observed outcomes, such as ETS and DpR, to refine the model parameters [26].
## Quantitative Data Tables
Table 1: Key Efficacy Metrics for Solid Tumors
| Metric | Definition | Measurement Method | Typical Assessment Time | Primary Correlation |
|---|---|---|---|---|
| Early Tumor Shrinkage (ETS) | Percentage reduction from baseline in the sum of the longest diameters (SLD) of target lesions [94] | RECIST v1.1 via CT/MRI [94] [95] | 6-12 weeks [94] | Early treatment sensitivity; PFS [94] |
| Depth of Response (DpR) | Maximum percentage reduction from baseline in SLD observed during treatment [94] | RECIST v1.1 via CT/MRI [94] [95] | Throughout treatment period [94] | Long-term outcomes; OS [94] |
| Objective Response Rate (ORR) | Proportion of patients with a best overall response of CR or PR [95] | RECIST v1.1 [95] | At each cycle/evaluation | Treatment activity |
| Personalized Chance of Longer Survival, Δ(m) | Probability of surviving ≥ m months longer on new treatment vs. control, adjusted for control arm variability [96] |
Nonparametric estimation from survival data [96] | End of study | Individualized treatment benefit, valid under non-proportional hazards [96] |
Table 2: Comparison of Tumor Response Criteria
| Feature | WHO Criteria (1979) | RECIST 1.0 (2000) | RECIST 1.1 (2009) |
|---|---|---|---|
| Measurement | Bidimensional (product of diameters) [95] | Unidimensional (longest diameter) [95] | Unidimensional (longest diameter for non-nodal, short axis for nodal) [95] |
| Lesion Number | All lesions [95] | Max 10 total, 5 per organ [95] | Max 5 total, 2 per organ [95] |
| PR Threshold | ≥ 50% decrease in sum of products [95] | ≥ 30% decrease in sum of longest diameters [95] | ≥ 30% decrease in sum of longest diameters [95] |
| PD Threshold | ≥ 25% increase in sum of products [95] | ≥ 20% increase in sum of longest diameters [95] | ≥ 20% increase (and 5mm absolute increase) [95] |
## Experimental Protocols
Protocol 1: Assessing Early Tumor Shrinkage (ETS) and Depth of Response (DpR) in a Clinical Trial
Objective: To evaluate the predictive value of ETS and DpR for Progression-Free Survival (PFS) and Overall Survival (OS) in patients with advanced solid tumors. Materials: Contrast-enhanced CT or MRI scanner, workstation with image analysis software, electronic data capture system. Procedure:
- Baseline Imaging: Perform a diagnostic-quality CT or MRI scan within 28 days prior to treatment initiation. Identify and measure all target lesions according to RECIST 1.1 [94] [95].
- First On-Treatment Imaging: Schedule the first follow-up scan for 6 to 12 weeks after treatment begins. Adhere strictly to this window across all patients to ensure consistency [94].
- Lesion Measurement and Calculation:
- Measure the same target lesions identified at baseline.
- Calculate the Sum of the Longest Diameters (SLD).
- Compute the percentage change from baseline:
% Change = [(SLD_baseline - SLD_follow-up) / SLD_baseline] * 100. - This value at the first assessment is the ETS.
- Serial Assessment: Continue imaging at predefined intervals (e.g., every 6-12 weeks). For each assessment, calculate the percentage change from baseline [94].
- Determine DpR: Identify the maximum observed percentage reduction in SLD from baseline across all post-baseline assessments. This is the patient's DpR [94].
- Statistical Analysis:
- Classify patients as "ETS responders" and "non-responders" using a pre-defined cutoff (e.g., 20% reduction).
- Compare PFS and OS between these groups using Kaplan-Meier curves and the log-rank test.
- Analyze DpR as both a continuous and categorical variable for its association with OS using Cox regression models [94].
Protocol 2: Implementing an Optimal Control Framework for Combination Therapy Scheduling
Objective: To compute an optimal drug administration schedule that minimizes tumor burden while constraining cumulative toxicity. Materials: Mathematical modeling software (e.g., MATLAB, Python with SciPy), nonlinear optimization solver (e.g., IPOPT). Procedure:
- Model Formulation:
- Define State Variables: These typically include the population of tumor cells (
x), healthy cells (h), and drug concentration (u). - Specify System Dynamics: Write a system of Ordinary Differential Equations (ODEs). A simplified structure is:
dx/dt = f(x, h, u)(Tumor growth and kill)dh/dt = g(x, h, u)(Healthy cell damage)du/dt = -λu + d(t)(Drug pharmacokinetics) [17] [6] - Formulate the Cost Function: Define the objective, e.g.,
J = x(t_f) + ∫(Q*u(t))dt, to minimize final tumor size and cumulative drug usage/toxicity [17] [6].
- Define State Variables: These typically include the population of tumor cells (
- Discretization: Discretize the continuous-time problem over the treatment horizon using a method like the Implicit Euler method to convert it into a nonlinear programming problem [17].
- Apply Solver: Use a solver like IPOPT to find the sequence of drug doses
d(t)that minimizes the cost functionJwhile respecting constraints on maximum dose and toxicity [17] [6]. - Solution Analysis: The solver output is the optimal control trajectory. This often results in a bang-bang control policy, switching between maximum and zero doses, or a continuous dosing profile [17].
- Validation: Compare the model-predicted tumor dynamics under the optimal schedule with experimental or clinical data, using metrics like ETS and DpR for correlation [26].
## Visualizations
Efficacy Metrics in Treatment Planning
Optimal Control for Therapy Scheduling
## The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Efficacy and Control Research
| Item | Function/Application |
|---|---|
| RECIST 1.1 Guidelines | Standardized protocol for measuring tumor lesions on CT/MRI to ensure consistent response classification across trials [95]. |
| Micro-CT Scanner | Provides high-resolution 3D in vivo imaging for longitudinal, automated tumor burden quantification in preclinical mouse models [97]. |
| Optimal Control Solver (e.g., IPOPT) | Open-source software for solving large-scale nonlinear optimization problems to compute optimal drug doses in mathematical models [17] [6]. |
| Kaplan-Meier Survival Analysis | Non-parametric statistic used to estimate the survival function from lifetime data, crucial for analyzing PFS and OS [98]. |
| Genetically Engineered Mouse Model (GEMM) | Preclinical models that closely recapitulate human disease stroma and genetics, used for validating therapeutic efficacy [97]. |
Benchmarking Against Standard-of-Care Dosing and Scheduling Protocols
This technical support resource provides guidance for researchers applying optimal control theory to the scheduling of cancer combination therapies. A core challenge in this field is benchmarking novel, optimized dosing regimens against established standard-of-care (SoC) protocols. Effective benchmarking requires a robust understanding of both historical clinical trial performance data and advanced mathematical modeling techniques. This guide addresses common methodological issues through a structured FAQ and troubleshooting format, supported by quantitative benchmarks and conceptual frameworks.
Frequently Asked Questions (FAQs)
1. What is the primary purpose of benchmarking in optimal control research for cancer therapy?
Benchmarking is used to quantitatively evaluate whether a novel, computationally derived dosing schedule shows a potential improvement over the current SoC. It provides a empirical baseline for comparing key outcomes such as tumor reduction efficiency, emergence of drug resistance, and treatment toxicity. Furthermore, benchmarking against historical clinical data helps to ground theoretical models in clinically achievable results and justifies further experimental investigation [99] [100].
2. What are the main categories of clinical trial benchmarks relevant to dosing protocol design?
Benchmarks can be divided into two primary categories [100]:
- Clinical Comparisons: These assess the effectiveness of a single intervention, a set of interventions, or an entire clinical pathway. The goal is to compare outcomes between different healthcare providers or treatment strategies for a well-defined patient group.
- System Comparisons: These evaluate the impact of broader health and social care system features (e.g., financing, reimbursement models, resource allocation) on the effectiveness of interventions.
3. My model suggests a continuous low-dose regimen is superior to maximum tolerated dose (MTD). How can I benchmark this against real-world data?
This is a common finding in models accounting for drug-induced plasticity, where high doses can accelerate the development of drug-tolerant cell populations [18]. To benchmark this:
- Identify Historical Controls: Use clinical trial databases to find SoC regimens for your specific cancer and drug combination. Key performance indicators (KPIs) to compare include median progression-free survival and overall survival rates.
- Model Validation: Calibrate your model's parameters (e.g., cell division and death rates, transition rates between sensitive and tolerant states) using in vitro data. Then, simulate the SoC regimen within your model and compare the simulated outcome (e.g., final tumor cell count) to the historical clinical data [18].
- Performance Metrics: The improvement of your optimal control strategy can be measured as a percentage reduction in predicted tumor size or a delay in time to recurrence compared to the simulated SoC benchmark.
4. What are the critical performance benchmarks for clinical trial protocols that I should consider in my models?
Recent analyses of phase I-III protocols highlight key design and performance variables that influence trial success and can be used for benchmarking [99]:
- Protocol Complexity: Number of endpoints, eligibility criteria, and total procedures.
- Operational Scope: Number of investigative sites, countries involved, and total data points collected.
- Trial Performance: Patient randomization rates (ratio of enrolled to screened patients) and completion rates (ratio of patients completing the trial to those enrolled).
- Cycle Times: Duration of study initiation, patient enrollment, treatment, and study close-out.
Troubleshooting Guides
Issue 1: Poor Patient Recruitment or Retention in Modeled Clinical Trial Scenario
Problem: Your simulated optimal dosing regimen is theoretically effective, but when placed in a simulated clinical trial environment, patient recruitment or retention rates are too low, jeopardizing the trial's feasibility.
Diagnosis and Resolution:
- Check Protocol Complexity: Overly complex protocols are strongly associated with lower physician referral rates and diminished patient willingness to participate [99]. Compare your trial's design benchmarks against industry averages.
- Action: Simplify the protocol by reducing the number of non-core procedures and patient visits if possible, aiming to meet or exceed the benchmarks for your trial's phase and therapeutic area [99].
- Analyze Benchmark Data: Oncology and rare disease protocols typically have much lower enrolled-to-completion rates and face intense recruitment challenges [99].
- Action: Incorporate historically low recruitment and retention rates for your specific disease area into your feasibility model. Explore how decentralized clinical trial (DCT) elements (e.g., telemedicine, wearable devices) could improve these rates in the implementation of your protocol [99].
Issue 2: Inability to Reproduce SoC Outcomes in a Computational Model
Problem: Your mathematical model fails to reproduce the clinical outcomes observed with the standard-of-care regimen, making it unreliable for testing novel strategies.
Diagnosis and Resolution:
- Isolate the Issue (Model vs. Parameters): Follow a structured troubleshooting process [101].
- Understand: Ensure the SoC regimen (drug doses, schedule, cycle length) is correctly implemented in the model.
- Isolate: Simplify the model to a known working state. For example, start by modeling a single drug before introducing combinations and synergies. Verify the model's behavior against a single, well-understood clinical dataset [27].
- Fix: Recalibrate model parameters. Use a clinical dataset (e.g., from a published trial) to validate the model for chemotherapy-alone outcomes before introducing more complex elements like radiation therapy or drug-drug interactions [27].
- Account for Cell Heterogeneity: SoC outcomes result from effects on a heterogeneous cell population. A model that treats the tumor as a uniform mass will be inaccurate.
Issue 3: Optimal Control Strategy is Clinically Impractical
Problem: The dosing schedule generated by the optimal control algorithm is too complex or variable (e.g., continuously changing doses) for practical clinical administration.
Diagnosis and Resolution:
- Compare to Optimal Control Classes: The optimal strategy from a model with drug-induced plasticity often falls into one of several classes, ranging from continuous low-dose therapy to intermittent high-dose therapy [18]. A complex solution might be an artifact of the model's assumptions.
- Action: Analyze the structure of the optimal solution. If the solution is a constant dose, this is highly practical. If it's intermittent, it may be implementable. If it is highly complex, consider constraining the control algorithm to a pre-defined set of clinically feasible patterns (e.g., "one week on, one week off") and re-computing.
- Validate with a Switched System Model: To directly design practical schedules, model the treatment using a positive switched system [27].
- Action: In this framework, the model consists of different state-space matrices representing the tumor's evolution under different treatments (e.g., "drug A on," "all drugs off"). The optimal control problem then becomes finding the optimal switching law between these discrete states, which naturally generates implementable, timed schedules [27].
Quantitative Benchmarking Tables
Table 1: Average Protocol Design Complexity Benchmarks (Phase II & III Trials) [99]
| Design Characteristic | Phase II Mean | Phase III Mean |
|---|---|---|
| Total Endpoints | 20.7 | 18.6 |
| Total Eligibility Criteria | ~30 | ~30 |
| Distinct Procedures | Information Missing | 34.5 |
| Total Procedures | Information Missing | 266.0 |
| Total Protocol Pages | Information Missing | 115.9 |
| Total Data Points Collected | ~2.09 Million | ~3.45 Million |
Table 2: Clinical Trial Performance Benchmarks [99]
| Performance Metric | Definition | Oncology & Rare Disease Trials | Non-Oncology & Non-Rare Disease Trials |
|---|---|---|---|
| Patient Randomization Rate | Number enrolled / Number screened | Lower | Higher |
| Patient Completion Rate | Number completing trial / Number enrolled | Much Lower | Higher |
| Operational Scale | Average number of countries and sites | Much Higher | Lower |
| Cycle Times | Duration from protocol approval to database lock | Longer | Shorter |
Experimental Protocols for Benchmarking
Protocol: Validating an Optimal Control Model Using Historical Clinical Data
Objective: To calibrate and validate a mathematical model of combination therapy so it can reliably reproduce SoC outcomes and test novel dosing regimens.
Methodology:
- Model Selection: Choose a model structure that captures key biological phenomena. A general ODE framework is recommended [26]:
- Cell Populations: Model drug-sensitive (S) and drug-tolerant (T) cells.
- Dynamics: Include terms for linear cell proliferation/death, spontaneous conversion between types, and, crucially, drug-mediated conversion (e.g., drug-induced plasticity) [18].
- Drug Synergy: Include terms for the multiplicative effects of drug combinations on cell death or phenotypic transition rates [26].
- Parameter Estimation: Use historical in vitro or in vivo data to estimate parameters for cell growth rates ((bi, di)) and transition rates ((\mu, \nu)).
- Simulation of SoC: Implement the exact dosing schedule of the SoC regimen in the model. Run the simulation to predict the tumor growth curve and the evolution of sensitive/tolerant subpopulations over time.
- Benchmarking Comparison: Compare the model's output (e.g., final tumor burden, time to progression) to the reported outcomes from the clinical trial serving as your benchmark. Statistical measures (e.g., R²) should be used to quantify the goodness-of-fit.
- Optimal Control Application: Once validated, apply optimal control theory to the model to determine the drug dosing schedule (c(t)) that minimizes a cost function (e.g., final tumor size) over the treatment horizon [26] [18].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Research |
|---|---|
| System of Coupled ODEs | The core mathematical framework for modeling the dynamics of multiple, interacting cell populations under treatment [26]. |
| Optimal Control Solver | Software (e.g., implemented in MATLAB) used to solve the optimization problem, often using methods like forward-backward sweep [18]. |
| Clinical Trial Dataset | Historical data from sources like clinical trial registries or published studies, used for model validation and benchmarking [27]. |
| Positive Switched System Model | A control-theoretic model that is particularly appropriate for determining optimal, clinically practical switching schedules between different treatment modalities [27]. |
Conceptual Diagrams
Diagram: Optimal Control in Drug-Induced Plasticity
Diagram: Benchmarking Controlled Trial Workflow
Frequently Asked Questions (FAQs)
Q1: Why is understanding cellular heterogeneity critical for designing cancer combination therapies?
Traditional population-averaged measurements can mask the presence of distinct cellular subpopulations that respond differently to treatment. For instance, a tumor might appear to have an intermediate response to a drug in bulk analysis, while in reality, it is composed of a mixture of completely responsive and completely non-responsive cells [102]. This heterogeneity can lead to competitive release, where therapy eliminates drug-sensitive cells, inadvertently releasing resistant subpopulations from competition, ultimately leading to treatment failure [21]. Optimal control theory (OCT) leverages mathematical models that account for this competition between cell types to design schedules that proactively manage resistant populations, for example, by using adaptive therapy to maintain a stable population of sensitive cells that suppress resistant ones [20] [21].
Q2: What are the primary sources of heterogeneity observed in cancer cell lines?
Even within clonal cancer cell lines grown in controlled conditions, significant heterogeneity exists. This intra-cell-line heterogeneity can be categorized as follows [103]:
- Transcriptomic Heterogeneity: Single-cell RNA-sequencing reveals that cell lines can be classified as having "discrete" (distinct subclones) or "continuous" (a gradient of states) heterogeneity patterns.
- Epigenetic Heterogeneity: Variations in chromatin accessibility, as measured by single-cell ATAC-seq, contribute to diverse gene regulatory programs within a single cell line.
- Genetic Heterogeneity: Copy number variations (CNVs) and the distribution of extrachromosomal DNA (ecDNA) can drive functional differences between cells.
- Phenotypic Plasticity: Cellular states are not fixed; heterogeneity can be reshaped by environmental stresses like hypoxia, demonstrating a dynamic and adaptable system.
Q3: How can single-cell data be integrated with mathematical models for therapy optimization?
Single-cell technologies provide the high-resolution, multi-parameter data needed to initialize and calibrate patient-specific mathematical models. For example:
- Model Initialization: Mass cytometry can quantify the initial proportions of sensitive and resistant cell populations in a tumor before treatment begins [104].
- Parameter Calibration: Single-cell multi-omics data can inform the growth rates, drug sensitivities, and competitive fitness costs for different subpopulations within the model [103].
- Schedule Testing: OCT uses these calibrated models to run in-silico simulations of millions of potential treatment combinations and schedules, predicting outcomes that cannot be systematically tested in clinical trials [5] [21]. This allows for the pre-selection of the most promising regimens for a specific patient's tumor composition.
Troubleshooting Guides
Table 1: Common Experimental Challenges in Heterogeneity Analysis
| Challenge | Potential Cause | Solution |
|---|---|---|
| Failure to detect rare subpopulations | Insufficient cell sampling or low-resolution techniques. | Utilize high-throughput single-cell technologies like mass cytometry (CyTOF), which can profile millions of cells while measuring 40+ parameters, ensuring rare populations (e.g., dormant stem cells) are captured [104]. |
| Misinterpretation of population-averaged data | Ensemble measurements average out critical bimodal or multimodal distributions. | Employ single-cell assays (scRNA-seq, scATAC-seq) to decompose the population into its constituent states. Use multivariate analysis to identify coupled relationships between markers within individual cells [102] [103]. |
| Inconsistent therapy response in vitro vs. in vivo | Homogeneous cell line models do not recapitulate the complex heterogeneity and microenvironment of human tumors. | Characterize the heterogeneity of your model system using single-cell methods. Consider using patient-derived organoids or co-cultures that better preserve tumor heterogeneity for therapy testing [103]. |
| Difficulty tracking metabolic heterogeneity | Standard single-cell omics lose spatial context and may not directly measure metabolites. | Implement integrated spatial omics. For example, combine imaging mass cytometry (IMC) for immunophenotyping with mass spectrometry imaging (MSI) on the same tissue section to link single-cell metabolite abundance with cell type [105]. |
Guide: Protocol for Characterizing Intra-Cell-Line Heterogeneity
This protocol outlines a multi-omics approach to characterize heterogeneity in cancer cell lines, providing essential data for mathematical modeling.
1. Experimental Design:
- Cell Line Selection: Choose cell lines relevant to your cancer type. Include multiple molecular subtypes if possible (e.g., for breast cancer: luminal, HER2+, triple-negative) [103].
- Replicates and Controls: Plan for biological and technical replicates. Include sample pooling controls if multiplexing.
2. Sample Preparation and Single-Cell Sequencing:
- Create Single-Cell Suspensions: Use standard tissue culture techniques and dissociation protocols to create a high-viability single-cell suspension.
- Library Preparation:
- For transcriptomic heterogeneity, use single-cell RNA-sequencing (scRNA-seq). The 10x Genomics platform is commonly used. Aim for a target of ~5,000 cells per cell line to capture diversity [103].
- For epigenetic heterogeneity, use single-cell ATAC-sequencing (scATAC-seq) on isolated nuclei to assess chromatin accessibility.
- Multiplexing: To increase throughput and reduce batch effects, use cell hashing or genetic barcoding to pool multiple cell lines in one sequencing run, followed by computational demultiplexing [103].
3. Data Integration and Analysis:
- Quality Control: Filter cells based on metrics like unique molecular identifier (UMI) counts, number of genes detected, and mitochondrial read percentage.
- Dimensionality Reduction and Clustering: Use Seurat (for scRNA-seq) or similar tools. Perform principal component analysis (PCA) followed by graph-based clustering and visualization with UMAP [103].
- Quantifying Heterogeneity: Calculate a "diversity score" by projecting all cells to a PCA space and computing the average distance of cells to the centroid of their respective cell line. This provides a quantitative measure of heterogeneity [103].
- Subpopulation Analysis: Identify discrete subclusters. Perform differential expression and pathway analysis on marker genes to assign biological meaning to each subpopulation (e.g., EMT-high, cell-cycle active).
4. Integration with Mathematical Models:
- Parameter Estimation: Use the proportions and growth-related gene signatures of identified subpopulations to estimate initial conditions and growth rates for models based on evolutionary game theory or optimal control [21].
- Model Validation: Test model predictions (e.g., response to a specific drug schedule) against in vitro experiments on the same characterized cell lines.
Workflow for Heterogeneity Analysis and Therapy Optimization
Research Reagent Solutions
Table 2: Essential Tools for Single-Cell Heterogeneity Studies
| Reagent / Technology | Function | Application in Therapy Optimization |
|---|---|---|
| Metal-Labeled Antibodies (for Mass Cytometry) | Antibodies conjugated to heavy metal isotopes allow multiplexed measurement of >40 protein markers on single cells with minimal signal overlap [104]. | Quantifying the pre-treatment proportion of drug-resistant (e.g., Sca-1 high) or immune checkpoint-expressing (e.g., PD-L1+) subpopulations to initialize models [102] [106]. |
| Single-Cell Multi-Omics Kits (e.g., 10x Genomics Multiome) | Simultaneously profiles gene expression (RNA) and chromatin accessibility (ATAC) from the same single nucleus [103] [107]. | Uncovering the coupled transcriptomic and epigenetic drivers of heterogeneity, providing mechanistic insights for targeting specific cell states. |
| Viability and Cell Cycle Stains | Dyes like cisplatin (for mass cytometry) or propidium iodide (for fluorescence) identify dead cells. Nucleotide analogs (IdU) mark DNA synthesis [104]. | Ensuring high-quality data from viable cells and tracking proliferative subpopulations that may be more vulnerable to cycle-specific chemotherapies. |
| Integrated IMC-MSI Workflow | Combines Imaging Mass Cytometry (IMC) for spatial phenotyping with Mass Spectrometry Imaging (MSI) for in-situ metabolite detection on one tissue section [105]. | Links cellular identity directly to metabolic state within the tumor microenvironment, identifying metabolic vulnerabilities for combination therapies. |
Comparative Analysis of Therapeutic Strategies
Optimal control theory models various scheduling strategies. The performance of each strategy depends on tumor growth rates and heterogeneity.
Table 3: Comparison of Chemotherapy Scheduling Strategies
| Strategy | Description | Pros | Cons | Best-Suited Context (from models) |
|---|---|---|---|---|
| Maximum Tolerated Dose (MTD) | High-dose chemotherapy administered with long breaks for patient recovery [20] [21]. | Rapid tumor debulking; simple, standardized schedules. | Selects for resistant clones via competitive release; high toxicity [21]. | Slow-growing tumors (e.g., prostate cancer), where high-dose pulses can effectively control growth [21]. |
| Metronomic Therapy | Frequent, low-dose administration of chemotherapy without extended breaks [20]. | Lower toxicity; may inhibit angiogenesis; milder impact on anti-tumor immunity. | Lower per-dose efficacy; finding the optimal low dose is challenging. | Elderly or frail patients; often requires oral chemotherapeutics for practical administration [20]. |
| Dose-Dense Scheduling | Administration of standard drug doses with reduced time between cycles [20]. | Increases total dose intensity over time; limits tumor regrowth between cycles; proven survival benefit in trials. | Requires careful management of cumulative toxicity (e.g., bone marrow suppression). | Fast-growing tumors; based on the Norton-Simon hypothesis that regrowth rate correlates with growth rate [20]. |
| Adaptive Therapy | Treatment dose and timing are dynamically adjusted based on real-time measurement of tumor burden (e.g., PSA levels) [20] [21]. | Maintains a stable tumor by exploiting competition to suppress resistant cells; delays progression. | Requires frequent monitoring; not yet standard; optimal triggers for dosing are under investigation. | Tumors with high fitness cost of resistance; aims for long-term containment rather than cure [20] [21]. |
Conclusion
Optimal Control Theory provides a powerful, quantitative framework to revolutionize the scheduling of cancer combination therapies. By integrating sophisticated mathematical models with advanced optimization algorithms, OCT enables the in silico design of personalized regimens that systematically balance maximal tumor cell kill with minimal toxicity. The key takeaways underscore OCT's ability to navigate complex drug interactions, manage patient heterogeneity, and design adaptive schedules that proactively counter drug resistance. Future directions must focus on the rigorous clinical validation of these in silico predictions, the refinement of models with real-time patient data, and the development of more scalable algorithms. The ultimate translation of these strategies into clinical practice holds the promise of significantly improving survival and quality of life for cancer patients, marking a critical step toward truly personalized oncology.
References
- 1. Optimal control [https://en.wikipedia.org/wiki/Optimal_control]
- 2. 14.1 Optimal Control Theory - Intro To Dynamic Systems [https://fiveable.me/introduction-dynamic-systems/unit-14/optimal-control-theory/study-guide/CT81dem9gh2doDjq]
- 3. Control Theory and Cancer Chemotherapy: How They ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2020.621269/full]
- 4. What is a Pontryagin System? - Jon Law - Medium [https://jonwlaw.medium.com/what-is-a-pontryagin-system-pontryagin-maximum-principle-control-theory-dynamic-optimization-e22b9d39bd41]
- 5. Optimal Control Theory for Personalized Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7290915/]
- 6. Optimizing cancer treatment using optimal control theory [https://www.aimspress.com/article/doi/10.3934/math.20241526?viewType=HTML]
- 7. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 8. Combination therapy at the start of hypertension treatment [https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-17/combination-therapy-at-the-start-of-hypertension-treatment-pros-and-cons]
- 9. Treatment scheduling effects on the evolution of drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8154902/]
- 10. Combine and conquer: challenges for targeted therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6135233/]
- 11. Frontiers | An Optimal Framework for the Automated Design... Control [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2020.00523/full]
- 12. A Markovian decision model of adaptive cancer treatment ... [https://www.sciencedirect.com/science/article/abs/pii/S0022519322002338]
- 13. A Markov decision process approach to optimizing cancer ... [https://pubmed.ncbi.nlm.nih.gov/30863847/]
- 14. Markov Decision Process Modeling for Multi-stage ... [https://pubmed.ncbi.nlm.nih.gov/33019200/]
- 15. Optimal Control in Combination Therapy for ... [https://link.springer.com/article/10.1007/s11538-025-01508-z]
- 16. Control Theory - Neuroscience [https://www.sciencedirect.com/topics/neuroscience/control-theory]
- 17. Constrained optimal control drug scheduling models with ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809425006871]
- 18. Optimal dosing of anti-cancer treatment under drug- ... [https://www.nature.com/articles/s41540-025-00571-5]
- 19. Linear and Non-Linear Optimal Control Methods to ... [https://www.mdpi.com/2227-9059/13/2/315]
- 20. how mathematical models inform treatment schedules for cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC9117454/]
- 21. Using mathematical models to determine the best ... [https://hscnews.usc.edu/using-mathematical-models-to-determine-the-best-chemotherapy-schedules]
- 22. Optimizing the future: how mathematical models inform ... [https://www.sciencedirect.com/science/article/abs/pii/S2405803322000413]
- 23. Control theory [https://en.wikipedia.org/wiki/Control_theory]
- 24. Mathematical Modeling of Tumor-Immune Cell Interactions [https://pmc.ncbi.nlm.nih.gov/articles/PMC6579737/]
- 25. A Review of Mathematical Models for Tumor Dynamics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6813171/]
- 26. Optimal Control in Combination Therapy for Heterogeneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521341/]
- 27. Optimal control of combined chemo-radiation therapy ... [https://resolver.tudelft.nl/uuid:8e3d0e43-e6bc-4f93-9e57-44c99ac83459]
- 28. ODE-toolbox - Tools [https://www.ebrains.eu/tools/ode-toolbox]
- 29. Evaluation of synergism in drug combinations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9127325/]
- 30. Computational frameworks transform antagonism to ... [https://www.nature.com/articles/s41746-025-01435-2]
- 31. Synergistic and antagonistic drug interactions are prevalent but not conserved across acute myeloid leukemia cell lines | Scientific Reports [https://www.nature.com/articles/s41598-025-03242-x]
- 32. Harnessing machine learning to find synergistic combinations for FDA-approved cancer drugs | Scientific Reports [https://www.nature.com/articles/s41598-024-52814-w]
- 33. Combination treatment optimization using a pan-cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8747684/]
- 34. Clinical relevance and methodological approach for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12182795/]
- 35. Generating synthetic signaling networks for in silico ... [https://www.sciencedirect.com/science/article/abs/pii/S0022519324001851]
- 36. A scalable, open-source implementation of a large-scale ... [https://www.nature.com/articles/s41467-022-31138-1]
- 37. Genome-scale mechanistic modeling of signaling pathways ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8170118/]
- 38. How to mathematically optimize drug regimens using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5847021/]
- 39. Chapter 17. Optimal control [https://motion.cs.illinois.edu/RoboticSystems/OptimalControl.html]
- 40. How do I approach Optimal Control? [https://mathoverflow.net/questions/44015/how-do-i-approach-optimal-control]
- 41. Exploring trade-offs in drug administration for cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S0025556425000306]
- 42. Leveraging Patient-Reported Outcome Measures for Optimal ... [https://cancer.jmir.org/2025/1/e64611]
- 43. Choose an ODE Solver - MATLAB & Simulink [https://www.mathworks.com/help/matlab/math/choose-an-ode-solver.html]
- 44. Optimizing cancer treatment using optimal control theory [https://www.aimspress.com/article/id/672da324ba35de7eae907f29]
- 45. CMA-ES [https://cma-es.github.io/]
- 46. CMA-ES [https://en.wikipedia.org/wiki/CMA-ES]
- 47. CMA-ES Sampler that support IPOP-CMA-ES and BIPOP- ... [https://hub.optuna.org/samplers/restart_cmaes/]
- 48. optuna.samplers.CmaEsSampler - Read the Docs [https://optuna.readthedocs.io/en/latest/reference/samplers/generated/optuna.samplers.CmaEsSampler.html]
- 49. Massively parallel CMA-ES with increasing population [https://arxiv.org/abs/2409.11765]
- 50. [2405.10534] CMA-ES for Safe Optimization [https://arxiv.org/abs/2405.10534]
- 51. Steering Evolution with Sequential Therapy to Prevent the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4567305/]
- 52. Computational framework for streamlining the success of ... [https://www.nature.com/articles/s44259-025-00160-w]
- 53. [2101.12120] An Optimal Strategy for Control ... Mathematically [https://arxiv.org/abs/2101.12120]
- 54. Optimization of drug scheduling for cancer chemotherapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10361382/]
- 55. Using an Iterative Dynamic Programming Algorithm to ... [https://www.sciencedirect.com/science/article/abs/pii/B9780444632340500294]
- 56. Synergistic effects of radiotherapy and targeted ... [https://pubmed.ncbi.nlm.nih.gov/35913663/]
- 57. A fractional-order model for optimizing combination therapy ... [https://www.nature.com/articles/s41598-024-66531-x]
- 58. Heterogeneity in Cancer - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11816170/]
- 59. A narrative review of tumor heterogeneity and challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8422119/]
- 60. Tumour heterogeneity and personalized treatment ... [https://www.sciencedirect.com/science/article/pii/S2001037024004409]
- 61. Pharmacometric and Digital Twin modeling for adaptive ... [https://www.sciencedirect.com/science/article/pii/S0169260725003360]
- 62. Intratumor heterogeneity inferred from targeted deep ... [https://www.nature.com/articles/s41598-019-41098-0]
- 63. Exploring and modelling colon cancer inter-tumour ... [https://www.nature.com/articles/s41389-020-00250-6]
- 64. Designing combination therapies for cancer treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC11063284/]
- 65. Balancing Cancer Treatment and Autoimmune Risks - Simple Science [https://scisimple.com/en/articles/2025-07-26-balancing-cancer-treatment-and-autoimmune-risks--a9rd8jl]
- 66. (PDF) Optimal for control in combination therapy cancer [https://www.academia.edu/143726951/Optimal_control_for_combination_therapy_in_cancer]
- 67. Strategies to reduce the cancer burden and improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12161469/]
- 68. 2025 Oncologic Toxicity Management Symposium: Novel ... [https://mskcc.cloud-cme.com/course/courseoverview?EID=55968]
- 69. Cancer Therapy: Adverse Event Prevention and ... [https://jhoponline.com/issue-archive/2014-issues/september-vol-4-no-3/cancer-therapy-adverse-event-prevention-and-management-education-for-all-pharmacists]
- 70. Enhancing Therapy Adherence: Impact on Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11766829/]
- 71. What Optimization Really Means in 2025: Beyond the Math [https://www.beyondtrucks.com/blog/technology-and-ai/what-optimization-really-means-in-2025]
- 72. Comprehensive review of dimensionality reduction algorithms [https://pmc.ncbi.nlm.nih.gov/articles/PMC12453773/]
- 73. Nonlinear dimensionality reduction [https://en.wikipedia.org/wiki/Nonlinear_dimensionality_reduction]
- 74. A Comprehensive Guide to Dimensionality Reduction [https://medium.com/@adnan.mazraeh1993/a-comprehensive-guide-to-dimensionality-reduction-from-basic-to-super-advanced-techniques-5-d6e0caf7d17f]
- 75. Nonlinear Dimensionality Reduction Techniques for ... [https://www.arxiv.org/abs/2510.15435]
- 76. Designing combination therapies for cancer treatment [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1358478/full]
- 77. Methods for multi-omic data integration in cancer research [https://pmc.ncbi.nlm.nih.gov/articles/PMC11446849/]
- 78. Adaptive multi-omics integration framework for breast ... [https://www.nature.com/articles/s41598-025-22202-z]
- 79. Methods for multi-omic data integration in cancer research [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1425456/full]
- 80. Systematic comparison of multi-omics survival models ... [https://www.sciencedirect.com/science/article/pii/S2667237523000802]
- 81. AI-driven multi-omics integration in precision oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634751/]
- 82. MathOnco25 Conference [https://mathematical-oncology.org/mathonco25]
- 83. Ten quick tips for avoiding pitfalls in multi-omics data ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1011224]
- 84. Optimizing cancer treatment using optimal control theory [https://www.aimspress.com/article/doi/10.3934/math.20241526]
- 85. Next-gen cancer therapy: The convergence of artificial ... [https://www.sciencedirect.com/science/article/pii/S294982952500155X]
- 86. In Silico Models in Oncology: Validating AI-Driven ... [https://blog.crownbio.com/in-silico-models-in-oncology-validating-ai-driven-predictive-frameworks]
- 87. Robust in-silico identification of cancer cell lines based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5470969/]
- 88. In Silico Validation of OncoOrigin: An Integrative AI Tool for ... [https://www.mdpi.com/1422-0067/26/6/2568]
- 89. Development and validation of a computational tool to ... [https://pubmed.ncbi.nlm.nih.gov/41244344/]
- 90. Optimal control of a mathematical model of CAR-T cell ... [https://www.aimsciences.org/article/doi/10.3934/dcdsb.2025080]
- 91. Optimal Control of Immune Checkpoint Inhibitor Therapy in ... [https://link.springer.com/article/10.1007/s11538-025-01468-4]
- 92. Integrating simulation and experimental validation of ... [https://www.sciencedirect.com/science/article/pii/S0928098725003677]
- 93. Optimizing cancer treatment using optimal control theory [https://www.sciopen.com/article/10.3934/math.20241526]
- 94. Early Tumor Shrinkage and Depth of Response as Predictive Markers of Treatment Response and Prognosis in Solid Tumors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12441742/]
- 95. Objective response rate assessment in oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC7046919/]
- 96. Quantifying treatment effects using the personalized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6842038/]
- 97. Quantification of Tumor Burden in a Genetically Engineered Mouse Model of Lung Cancer by Micro-CT and Automated Analysis - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4415142/]
- 98. Survival Analysis Part I: Basic concepts and first analyses [https://pmc.ncbi.nlm.nih.gov/articles/PMC2394262/]
- 99. Protocol Design and Performance Benchmarks by Phase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9373886/]
- 100. Benchmarking Controlled Trial—a novel concept covering all ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4673508/]
- 101. The Art of Troubleshooting for Customer Support ... [https://www.helpscout.com/helpu/art-of-troubleshooting-support/]
- 102. Cellular heterogeneity: when do differences make a difference? [https://pmc.ncbi.nlm.nih.gov/articles/PMC2918286/]
- 103. Single cell multi-omics reveal intra-cell-line heterogeneity ... [https://www.nature.com/articles/s41467-023-43991-9]
- 104. Mass Cytometry: Single Cells, Many Features - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4860251/]
- 105. Integration of mass cytometry and mass spectrometry ... [https://www.nature.com/articles/s41592-024-02392-6]
- 106. In vivo single-cell high-dimensional mass cytometry analysis ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1011900]
- 107. Analysis of population heterogeneity in CHO cells by ... [https://www.sciencedirect.com/science/article/pii/S0168165624002852]