Mixed Treatment Comparisons and Network Meta-Analysis: A Comprehensive Guide for Clinical Researchers
This article provides a comprehensive overview of mixed treatment comparison (MTC) models, also known as network meta-analysis, a powerful statistical methodology for comparing multiple interventions simultaneously by combining direct and...
Mixed Treatment Comparisons and Network Meta-Analysis: A Comprehensive Guide for Clinical Researchers
Abstract
This article provides a comprehensive overview of mixed treatment comparison (MTC) models, also known as network meta-analysis, a powerful statistical methodology for comparing multiple interventions simultaneously by combining direct and indirect evidence. Aimed at researchers, scientists, and drug development professionals, it covers foundational concepts, methodological approaches for implementation, strategies for troubleshooting common issues like heterogeneity and inconsistency, and frameworks for validating and comparing MTC results with direct evidence. The synthesis of current guidance and applications demonstrates how MTC strengthens evidence-based decision-making in healthcare policy and clinical development, particularly when head-to-head trial data are unavailable.
What Are Mixed Treatment Comparisons? Building the Foundational Knowledge
Mixed Treatment Comparison (MTC) and Network Meta-Analysis (NMA) are advanced statistical methodologies that enable the simultaneous comparison of multiple interventions, even when direct head-to-head evidence is absent. Within evidence-based medicine, these approaches provide a unified, coherent framework for evaluating the relative efficacy and safety of three or more treatments, addressing a critical need for health technology assessment (HTA) and clinical decision-making [1] [2]. The terminology "Mixed Treatment Comparison" and "Network Meta-Analysis" is often used interchangeably in the scientific literature, though NMA has gained broader usage in recent years [3] [4]. These methods synthesize all available direct and indirect evidence into an internally consistent set of estimates, thereby overcoming the limitations of traditional pairwise meta-analyses, which are restricted to comparing only two interventions at a time [1] [5]. This technical guide delineates the core concepts, assumptions, methodologies, and applications of MTC/NMA, framed within the broader context of comparative effectiveness research.
Core Definitions and Relationship
Foundational Terminology
- Mixed Treatment Comparison (MTC): A statistical analysis that combines direct evidence from head-to-head randomized controlled trials (RCTs) with indirect evidence to compare multiple interventions in a single model [1] [2]. The term emphasizes the "mixing" of different types of comparative evidence.
- Network Meta-Analysis (NMA): A methodology for the simultaneous comparison of multiple treatments that forms a connected network of interventions [6] [5]. The term highlights the "network" structure of the evidence, where treatments are nodes and comparisons are edges.
- Indirect Treatment Comparison (ITC): A broader term encompassing any method that compares treatments indirectly via a common comparator, with MTC/NMA being a specific, sophisticated form of ITC [3].
Conceptual Relationship
Although the terms MTC and NMA originated from different statistical traditions, they are functionally equivalent in their modern application [2] [4]. Both methods synthesize evidence from a network of trials to estimate all pairwise relative effects between interventions. The term NMA is increasingly prevalent in contemporary literature, as evidenced by its coverage in 79.5% of articles describing ITC techniques, compared to other methodologies [3]. These methods answer the pivotal question for healthcare decision-makers: "Which treatment should be used for this condition?" when faced with multiple alternatives [2].
Table 1: Prototypical Situations for MTC and NMA Application
| Analysis Type | Included Studies | Rationale or Outcome |
|---|---|---|
| Standard Meta-analysis | Study 1: Treatment A vs placebo, n=300Study 2: Treatment A vs placebo, n=150Study 3: Treatment A vs placebo, n=500 | Obtain a more precise estimate of effect size of Treatment A vs placebo; increase statistical power [1] |
| Mixed Treatment Comparison/Network Meta-Analysis | Study 1: Treatment A vs placebo, n=150Study 2: Treatment B vs placebo, n=150Study 3: Treatment B vs Treatment C, n=150 | Estimate effect sizes between A vs B, A vs C, and C vs placebo where no direct comparisons exist [1] |
Key Assumptions and Statistical Foundations
The validity of MTC/NMA depends on three fundamental statistical assumptions, which ensure that the combined direct and indirect evidence provides unbiased estimates of relative treatment effects [1] [5] [4].
Similarity
This assumption requires that the trials included for different pairwise comparisons are sufficiently similar in their methodological characteristics, including study population, interventions, comparators, outcomes, and study design [1] [5]. Effect modifiers—variables that influence the treatment effect size—must be balanced across treatment comparisons. For example, in an NMA comparing antidepressants, effect modifiers could include inpatient versus outpatient setting, flexibility of medication dosing, and patient comorbidities [4].
Transitivity
Transitivity extends the similarity assumption across the entire treatment network. It necessitates that the distribution of effect modifiers is similar across the different direct comparisons forming the network [5]. In a network comparing A vs B, A vs C, and B vs C, the patients receiving A in the A vs B trials should be comparable to those receiving A in the A vs C trials in terms of key effect modifiers. Violation of transitivity can lead to biased indirect estimates.
Consistency (Coherence)
Consistency refers to the statistical agreement between direct and indirect evidence for the same treatment comparison [2] [4]. When both direct and indirect evidence exist for a specific pairwise comparison (e.g., A vs B), the estimates derived from each source should be statistically compatible. Significant disagreement, termed "incoherence" or "inconsistency," suggests violation of the similarity or transitivity assumptions or methodological differences between trials [4].
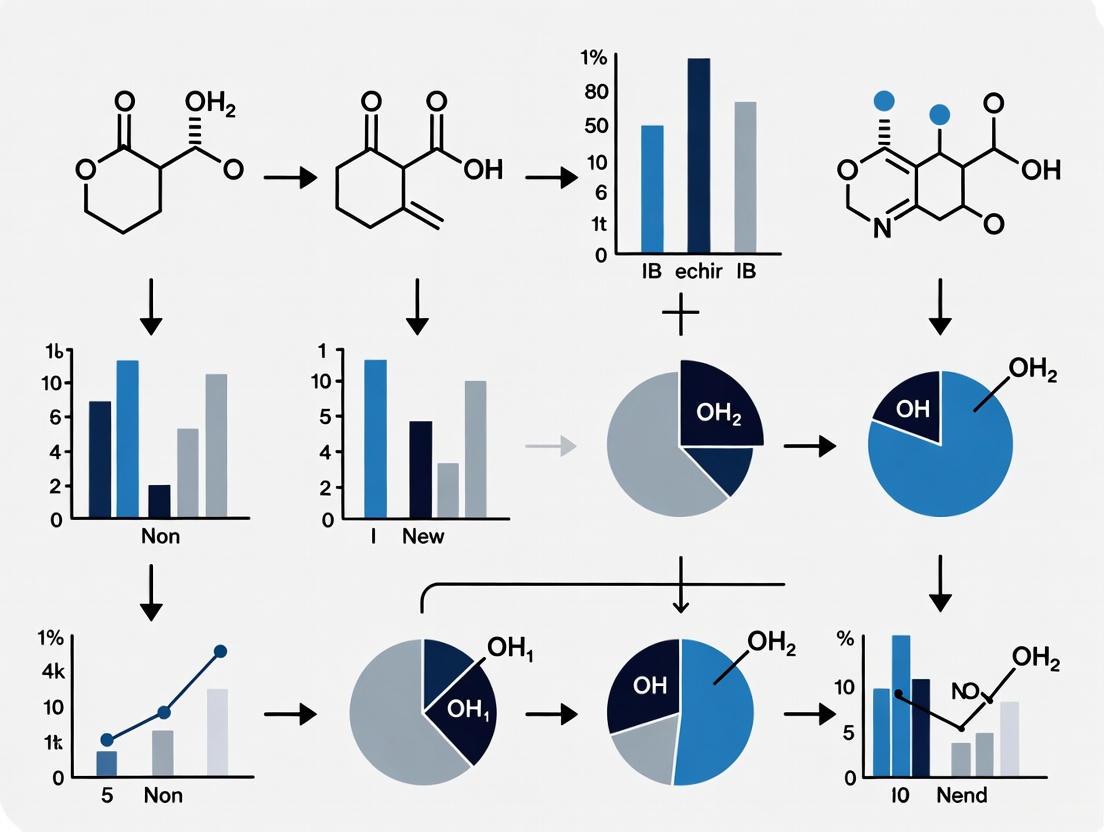
The following diagram illustrates the logical relationships between these core assumptions and the resulting evidence in a network meta-analysis.
Methodological Workflow and Protocol
Executing a robust MTC/NMA requires a rigorous, pre-specified methodology analogous to conducting a high-quality clinical trial [1]. The process follows established guidelines for systematic reviews, such as those from the Cochrane Collaboration and the PRISMA extension for NMA [1] [5].
Systematic Literature Review and Study Selection
The foundation of any MTC/NMA is a comprehensive systematic literature review designed with pre-specified eligibility criteria (PICO framework: Population, Intervention, Comparator, Outcomes) [3]. The search strategy must be documented thoroughly to ensure reproducibility and minimize selection bias. The study selection process is typically visualized using a PRISMA flow diagram [1].
Data Extraction and Quality Assessment
Data extraction from included studies must be performed in a blinded and pre-specified manner [1]. Key extracted information includes study characteristics, patient demographics, intervention details, outcomes, and effect modifiers. The quality of individual RCTs should be assessed using validated tools (e.g., the Jadad scale or Cochrane Risk of Bias tool) [1] [4].
Network Geometry and Evidence Structure
The collection of included studies and their comparisons forms the network geometry [5]. This is visually represented by a network plot where:
- Nodes: Represent the interventions or treatments being compared.
- Edges: Represent the direct head-to-head comparisons between interventions.
- The size of nodes is often proportional to the number of participants receiving that intervention.
- The thickness of edges is often proportional to the number of trials making that direct comparison [5].
Table 2: Quantitative Data Extraction Template for Included Studies
| Study ID | Treatment Arms | Sample Size (n) | Baseline Characteristics (e.g., Mean Age, % Male) | Outcome Data (e.g., Events, Mean, SD) | Effect Modifiers (e.g., Disease Severity, Prior Treatment) | Quality Score (e.g., Jadad) |
|---|---|---|---|---|---|---|
| Smith et al. 2020 | A, B | 150 | Age: 45y, 60% Male | Resp A: 45/75, Resp B: 30/75 | High-risk: 40% | 4/5 |
| Jones et al. 2021 | A, C | 200 | Age: 50y, 55% Male | Resp A: 60/100, Resp C: 40/100 | High-risk: 50% | 3/5 |
| Chen et al. 2022 | B, C | 180 | Age: 48y, 58% Male | Resp B: 50/90, Resp C: 45/90 | High-risk: 45% | 5/5 |
Statistical Analysis and Model Implementation
The statistical synthesis involves several key steps:
- Choice of Model: Analysts must choose between a fixed-effects model (assumes a single true treatment effect across all studies) and a random-effects model (allows for heterogeneity in treatment effects across studies) [1] [4]. Random-effects models are often preferred to account for between-study variation.
- Effect Measure Selection: The choice of effect measure (e.g., Odds Ratio [OR], Risk Ratio [RR] for dichotomous outcomes; Mean Difference [MD], Standardized Mean Difference [SMD] for continuous outcomes) depends on the outcome type and must be pre-specified [5].
- Estimation Framework: Analysis can be conducted within a frequentist or Bayesian framework. Bayesian methods, using Markov Chain Monte Carlo (MCMC) simulation, have been widely adopted for MTC/NMA as they facilitate probabilistic statements about treatment rankings [4].
- Assessment of Heterogeneity and Inconsistency: Statistical tests (e.g., I² for heterogeneity) and specific methods (e.g., side-splitting for inconsistency) are used to evaluate the validity of the model's assumptions [1] [2] [4].
The following flowchart outlines the core experimental protocol for conducting an MTC/NMA.
Analytical Outputs and Interpretation
The results of an MTC/NMA provide a comprehensive summary of the relative effectiveness of all treatments in the network.
League Table
A league table presents all pairwise comparisons in a matrix format, providing the effect estimate and its confidence or credible interval for each treatment comparison [5]. This allows for a direct assessment of which treatments are statistically significantly different from one another.
Table 3: Hypothetical League Table for Sleep Interventions (Outcome: Standardized Mean Difference)*
| Intervention | A (Aromatherapy) | B (Earplugs) | C (Eye Mask) | D (Virtual Reality) |
|---|---|---|---|---|
| B (Earplugs) | -0.61 (-1.18, -0.04) | |||
| C (Eye Mask) | -0.18 (-0.48, 0.13) | 0.44 (-0.05, 0.92) | ||
| D (Virtual Reality) | -0.84 (-1.10, -0.58) | -0.23 (-0.75, 0.29) | -0.66 (-1.01, -0.31) | |
| E (Music) | -0.72 (-1.05, -0.39) | -0.11 (-0.67, 0.45) | -0.54 (-0.85, -0.23) | 0.12 (-0.21, 0.45) |
Note: Data from a hypothetical NMA [5]. Cell entry is the SMD (95% CI) of the row-defining treatment compared to the column-defining treatment. SMD < 0 favors the row treatment.
Treatment Ranking
MTC/NMA models, particularly Bayesian ones, can estimate the probability of each treatment being the best, second best, etc., based on the selected outcome [2] [4]. These rankings are often presented as rankograms or cumulative ranking curves (SUCRA).
Applications and Feasibility Assessment in Drug Development
MTC/NMA has become a cornerstone of comparative effectiveness research, directly informing healthcare policy and clinical practice.
Primary Applications
- Health Economic Evaluations and HTA: MTC/NMA is frequently used to support submissions to HTA bodies, such as the UK's National Institute for Health and Care Excellence (NICE), by providing comparative efficacy evidence for reimbursement decisions [1] [4].
- Informing Clinical Practice Guidelines: By synthesizing all available evidence, NMA can identify the most effective interventions for inclusion in clinical guidelines, helping to answer "which treatment is best?" [5] [2].
- Evidence Gap Identification: The network structure can reveal where direct comparisons are missing, potentially guiding the design of future clinical trials [2].
Feasibility and Challenges
A critical preliminary step is assessing the feasibility of conducting a valid MTC/NMA. Key considerations include:
- Network Connectivity: A valid NMA requires a connected network where there is a path of comparisons between all treatments [7].
- Clinical and Methodological Heterogeneity: Significant differences in trial populations, interventions, definitions of outcomes, or standard of care can violate the key assumptions and render an NMA unfeasible or invalid [7] [4]. For example, an NMA in polycythemia vera was deemed unfeasible due to heterogeneity in patient populations (newly diagnosed vs. hydroxyurea-resistant), variable definitions of "standard of care," and inconsistent endpoint definitions [7].
- Publication Bias: The tendency for positive results to be published more often than negative ones can lead to biased summary effects in any meta-analysis, including NMA [1].
Table 4: Indirect Treatment Comparison Techniques: Strengths and Limitations
| ITC Technique | Description | Key Strengths | Key Limitations |
|---|---|---|---|
| Network Meta-Analysis (NMA) | Simultaneously compares multiple treatments in a connected network [3]. | Synthesizes all available evidence; provides internally consistent estimates for all comparisons; can rank treatments [1] [2]. | Requires strict similarity, transitivity, and consistency assumptions; complex to implement and interpret [4]. |
| Bucher Method | Simple indirect comparison between two treatments via a common comparator [3]. | Simple and intuitive; no specialized software needed [3]. | Limited to three treatments/two trials; does not incorporate heterogeneity; cannot integrate direct and indirect evidence [3]. |
| Matching-Adjusted Indirect Comparison (MAIC) | Population-adjusted method that re-weights individual patient data (IPD) from one trial to match the aggregate baseline characteristics of another [3]. | Useful when IPD is available for only one trial; can adjust for cross-trial imbalances in effect modifiers [3]. | Relies on the availability of IPD for at least one trial; limited to comparing two treatments; depends on chosen effect modifiers [3]. |
The Scientist's Toolkit: Key Reagent Solutions
While MTC/NMA is a statistical methodology, its execution relies on several essential tools and resources. The following table details key components of the analytical toolkit.
Table 5: Essential Research Reagent Solutions for MTC/NMA
| Tool/Resource | Function | Application in MTC/NMA |
|---|---|---|
| PRISMA-NMA Guidelines | A reporting checklist ensuring transparent and complete reporting of systematic reviews incorporating NMA [1] [5]. | Guides the entire process from protocol to reporting, ensuring methodological rigor and reproducibility. |
| Cochrane Handbook | Methodological guidance for conducting systematic reviews and meta-analyses of interventions [5]. | Provides the foundational standards for study identification, quality assessment, and data synthesis. |
| Bayesian Statistical Software (e.g., WinBUGS, OpenBUGS, JAGS) | Specialized software that uses Markov Chain Monte Carlo (MCMC) simulation for fitting complex statistical models [4]. | The primary computational environment for implementing Bayesian NMA models, enabling probabilistic treatment ranking. |
| R packages (e.g., *netmeta, gemtc)* | Statistical packages within the R programming environment for conducting meta-analysis and NMA [3]. | Provide both frequentist and Bayesian frameworks for NMA, facilitating model implementation, inconsistency checks, and visualization. |
| GRADE for NMA | A framework for rating the quality (certainty) of a body of evidence in systematic reviews [5]. | Used to assess the certainty of evidence for each pairwise comparison derived from the NMA, informing clinical recommendations. |
| Sarmentocymarin | Sarmentocymarin|Cardiac Glycoside|For Research Use | Sarmentocymarin is a crystalline steroid cardiac glycoside for research. This product is For Research Use Only and is not intended for diagnostic or personal use. |
| Bruceantinol | Bruceantinol, CAS:53729-52-5, MF:C30H38O13, MW:606.6 g/mol | Chemical Reagent |
The exponential growth of medical evidence has necessitated the development of sophisticated statistical methods to synthesize research findings comprehensively. Evidence synthesis has evolved substantially from traditional pairwise methods to increasingly complex network approaches. This evolution represents a paradigm shift in how researchers compare healthcare interventions, moving from direct head-to-head comparisons toward integrated analyses that can simultaneously evaluate multiple interventions. Network meta-analysis (NMA), also known as mixed treatment comparison, has emerged as a critical methodology that extends standard pairwise meta-analysis by enabling indirect comparisons and ranking of multiple treatments [8] [9]. This advancement is particularly valuable for healthcare decision-makers who must often choose among numerous competing interventions, many of which have never been directly compared in randomized controlled trials.
The fundamental advantage of NMA lies in its ability to leverage both direct and indirect evidence, creating a connected network of treatment comparisons that provides a more comprehensive basis for decision-making [8]. While standard pairwise meta-analysis synthesizes evidence from trials comparing the same interventions, NMA facilitates comparisons of interventions that have not been studied head-to-head by connecting them through common comparators [9]. This methodological expansion, however, introduces additional complexity and requires careful attention to underlying assumptions that ensure validity. The core assumptions of transitivity and consistency form the foundation of NMA, distinguishing it conceptually and methodologically from traditional pairwise approaches [8] [9].
This technical guide examines the evolution from pairwise to network meta-analysis within the broader context of mixed treatment comparison models research. Aimed at researchers, scientists, and drug development professionals, it provides an in-depth examination of methodological foundations, key assumptions, implementation protocols, and current challenges in advanced evidence synthesis methodologies.
Methodological Foundations
Pairwise Meta-Analysis: The Traditional Paradigm
Traditional pairwise meta-analysis represents the foundational approach to evidence synthesis, statistically combining results from multiple randomized controlled trials (RCTs) that investigate the same intervention comparison [8]. This methodology generates a pooled estimate of the treatment effect between two interventions (typically designated as intervention versus control) by synthesizing all available direct evidence. The internal validity of each included RCT stems from the random allocation of participants to intervention groups, which balances both known and unknown prognostic factors across comparison arms [8].
Within pairwise meta-analysis, variation in treatment effects can manifest at two distinct levels. Within-study heterogeneity occurs when patient characteristics that modify treatment response (effect modifiers) vary among participants within an individual trial [8]. For example, RCTs evaluating statins might include patients with and without coronary artery history, and these subgroups may respond differently to treatment. Between-study heterogeneity arises from systematic differences in study characteristics or patient populations across different trials investigating the same comparison [8]. This occurs because while randomization protects against bias within trials, patients are not randomized to different trials in a meta-analysis.
Table 1: Types of Variation in Pairwise Meta-Analysis
| Type of Variation | Description | Source | Statistical Manifestation |
|---|---|---|---|
| Within-study heterogeneity | Variation in true treatment effects among participants within a trial | Differences in effect modifiers among participants within a trial | Not typically observable with aggregate data |
| Between-study heterogeneity | Systematic differences in treatment effects across trials | Imbalance in effect modifiers across different studies | Measurable via I², Q, or τ² statistics |
When combining studies in pairwise meta-analysis, the presence of between-study heterogeneity does not inherently introduce bias but may render pooled estimates less meaningful if the variation is substantial [8]. In such cases, analysts may pursue alternative strategies such as subgroup analysis or random-effects models that account for this heterogeneity in the precision of estimates.
Network Meta-Analysis: An Integrated Framework
Network meta-analysis extends pairwise methodology by simultaneously synthesizing evidence from a network of RCTs comparing multiple interventions [8] [9]. Whereas standard meta-analysis examines one comparison at a time, NMA integrates all direct and indirect evidence into a unified analysis, enabling comparisons among all interventions in the network. This approach effectively broadens the evidence base considered for each treatment effect estimate [8].
The conceptual foundation of NMA rests on indirect comparisons, which can be illustrated through a simple example. Consider trial 1 comparing treatments B versus A (yielding effect estimate d̂_AB), and trial 2 comparing treatments C versus B (yielding effect estimate d̂_CB). An indirect estimate for the comparison C versus A can be derived as d̂_CA = d̂_CB + d̂_AB [9]. This indirect comparison maintains the benefits of randomization within each trial while allowing for differences across trials, provided these differences affect only prognosis and not treatment response [9].
In NMA, three types of treatment effect variation can occur: (1) true within-study variation (only observable with individual patient data), (2) true between-study variation for a particular treatment comparison (heterogeneity), and (3) true between-comparison variation in treatment effects [8]. This additional source of variability distinguishes NMA from standard pairwise meta-analysis and introduces the critical concepts of transitivity and consistency.
Table 2: Evolution from Pairwise to Network Meta-Analysis
| Feature | Pairwise Meta-Analysis | Network Meta-Analysis |
|---|---|---|
| Comparisons | Direct evidence only | Direct, indirect, and mixed evidence |
| Interventions | Typically two (e.g., intervention vs. control) | Multiple interventions simultaneously |
| Evidence Use | Synthesizes studies of identical comparisons | Synthesizes studies of different but connected comparisons |
| Output | Single pooled effect estimate | Multiple effect estimates with ranking possibilities |
| Key Assumptions | Homogeneity (or explainable heterogeneity) | Transitivity and consistency |
| Complexity | Relatively straightforward | Increased complexity in modeling and interpretation |
Critical Assumptions and Evaluation Methods
Transitivity: The Conceptual Foundation
The assumption of transitivity constitutes the conceptual foundation underlying the validity of network meta-analysis. Transitivity requires that the distribution of effect modifiers—study or patient characteristics associated with the magnitude of treatment effect—is similar across the different types of direct comparisons in the network [8]. In practical terms, this means that the participants in studies of different comparisons (e.g., AB studies versus AC studies) are sufficiently similar that their results can be meaningfully combined [8].
The relationship between effect modifiers and transitivity can be illustrated through specific scenarios. When the distribution of effect modifiers is balanced across different direct comparisons (e.g., AB and AC studies), the indirect comparison provides an unbiased estimate [8]. However, when an imbalance exists in the distribution of effect modifiers between different types of direct comparisons, the related indirect comparisons will be biased [8]. For example, if AB studies predominantly include patients with severe disease while AC studies include mostly mild cases, and disease severity modifies treatment response, then the indirect BC comparison would be confounded by this imbalance [8].
The following diagram illustrates the flow of evidence and key assumptions in network meta-analysis:
Network Meta-Analysis Evidence Flow and Key Assumptions
Consistency: The Statistical Manifestation
Consistency represents the statistical manifestation of the transitivity assumption, referring to the agreement between direct and indirect evidence for the same treatment comparison [9]. In a consistent network, the direct estimate of a treatment effect (e.g., from head-to-head studies comparing B and C) agrees with the indirect estimate (e.g., obtained via a common comparator A) within the bounds of random error [9]. The consistency assumption can be expressed mathematically for a simple ABC network as: δ_AC = δ_AB + δ_BC, where δ represents the true underlying treatment effect for each comparison [9].
When consistency is violated, this is referred to as inconsistency or incoherence, which occurs when different sources of evidence (direct and indirect) for the same comparison yield conflicting results [9]. Inconsistency can arise from several sources, including differences in participant characteristics across comparisons, different versions of treatments in different comparisons, or methodological differences between studies of different comparisons [9].
Two specific types of inconsistency have been described in the literature. Loop inconsistency refers to disagreement between different sources of evidence within a closed loop of treatments (typically a three-treatment loop) [9]. Design inconsistency occurs when the effect of a specific contrast differs depending on the design of the study (e.g., whether the estimate comes from a two-arm trial or a multi-arm trial that includes additional treatments) [9]. The presence of multi-arm trials in evidence networks complicates the definition and detection of loop inconsistency [9].
Methods for Evaluating Inconsistency
Several statistical approaches have been developed to evaluate inconsistency in network meta-analyses. The design-by-treatment interaction model provides a general framework for investigating inconsistency that successfully addresses complications arising from multi-arm trials [9]. This approach treats inconsistency as an interaction between the treatment contrast and the design (set of treatments compared in a study) [9].
The node-splitting method is another popular approach that directly compares direct and indirect evidence for specific comparisons [10]. This method "splits" the evidence for a particular comparison into direct and indirect components and assesses whether they differ significantly [10]. Different parameterizations of node-splitting models make different assumptions: symmetrical methods assume both treatments in a contrast contribute to inconsistency, while asymmetric methods assume only one treatment contributes [10].
Novel graphical tools have also been developed to locate inconsistency in network meta-analyses. The net heat plot visualizes which direct comparisons drive each network estimate and displays hot spots of inconsistency, helping researchers identify which suspicious direct comparisons might explain the presence of inconsistency [11]. This approach combines information about the contribution of each direct estimate to network estimates with heat colors corresponding to changes in agreement between direct and indirect evidence when relaxing consistency assumptions for specific comparisons [11].
Implementation and Analytical Protocols
Network Meta-Analysis Workflow
Implementing a valid network meta-analysis requires meticulous attention to each step of the analytical process. The following workflow diagram outlines the key stages in conducting an NMA, from network specification to interpretation of results:
Network Meta-Analysis Implementation Workflow
Statistical Models for Network Meta-Analysis
The statistical foundation of NMA can be implemented through both frequentist and Bayesian frameworks. The general linear model for network meta-analysis with fixed effects can be expressed in matrix notation as: Y = Xθ_net + ε, where Y is a vector of observed treatment effects from all studies, X is the design matrix capturing the network structure at the study level, θ_net represents the parameters of the network meta-analysis, and ε represents the error term [11].
For fixed-effects models, it is assumed that all studies estimating the same comparison share a common treatment effect, with any observed differences attributable solely to random sampling variation. Random-effects models, in contrast, allow for heterogeneity by assuming that the underlying treatment effects for the same comparison follow a distribution, typically normal: θ_i ~ N(δ_JK, τ²) for pairwise comparison JK [9]. The random-effects approach is generally more conservative and appropriate when between-study heterogeneity is present.
The consistency assumption can be incorporated into the model through linear constraints on the basic parameters. For example, in a network with treatments A, B, and C, the consistency assumption implies that δ_AC = δ_AB + δ_BC [9]. Inconsistency can be assessed by comparing models with and without these consistency constraints, using measures such as the deviance information criterion (DIC) in Bayesian analysis or likelihood ratio tests in frequentist analysis.
Research Reagent Solutions for Network Meta-Analysis
Table 3: Essential Methodological Tools for Network Meta-Analysis
| Tool Category | Specific Methods/Software | Function | Key Features |
|---|---|---|---|
| Statistical Software | R (gemtc, netmeta, pcnetmeta packages) | Implement statistical models for NMA | Bayesian and frequentist approaches, inconsistency detection, network graphics |
| Stata (network, mvmeta packages) | Perform NMA in Stata environment | Suite of commands for network meta-analysis | |
| WinBUGS/OpenBUGS/JAGS | Bayesian analysis using MCMC sampling | Flexibility for complex models, random-effects, consistency/inconsistency models | |
| Inconsistency Detection | Node-splitting methods | Evaluate disagreement between direct and indirect evidence | Specific comparison assessment, various parameterizations available |
| Design-by-treatment interaction model | Global test of inconsistency | Handles multi-arm trials appropriately, comprehensive inconsistency assessment | |
| Net heat plot | Graphical inconsistency assessment | Visualizes drivers and hot spots of inconsistency | |
| Visualization | Network diagrams | Illustrate evidence structure | Node size (sample size), edge thickness (number of studies) |
| Contribution matrices | Show contribution of direct estimates to network results | Informs about evidence flow and precision sources | |
| Ranking plots | Display treatment hierarchies | Rankograms, cumulative ranking curves (SUCRA) |
Current Challenges and Methodological Frontiers
Methodological Challenges in Evolving Evidence Networks
Network meta-analysis faces several ongoing methodological challenges, particularly in the context of evolving evidence networks. Living systematic reviews (LSRs) and updated systematic reviews (USRs) represent frameworks for keeping syntheses current with rapidly expanding literature, but they introduce complexities for NMA [12]. Repeatedly updating an NMA can inflate type I error rates due to multiple testing, and heterogeneity estimates may fluctuate with each update, potentially affecting effect estimates and clinical interpretations [12].
In NMA updates, the transitivity assumption must be reassessed each time new studies are added, as introducing new interventions or additional evidence for existing comparisons may alter the distribution of effect modifiers across the network [12]. Similarly, consistency assessment becomes more complex in living reviews, as statistical tests for inconsistency may have insufficient power at early updates when few studies are available [12]. The introduction of new interventions can change the network geometry, potentially creating new loops where inconsistency might occur.
Trial sequential analysis (TSA) has been proposed as one method to address error inflation in updated meta-analyses by adapting sequential clinical trial methodology to evidence synthesis [12]. TSA establishes a required information size and alpha spending function to determine statistical significance, adjusting for the cumulative nature of evidence updates. However, application of TSA to NMA is complex, as it must account for both heterogeneity and potential inconsistency in the network [12].
Advanced Methodological Developments
Recent methodological research has addressed several complex scenarios in network meta-analysis. Generalized linear mixed models with node-splitting parameterizations provide flexible frameworks for evaluating inconsistency, particularly for binary and count outcomes [10]. These approaches allow researchers to specify different parameterizations depending on whether they believe one or both treatments in a comparison contribute to inconsistency.
Advanced graphical tools continue to be developed to enhance the visualization and interpretation of network meta-analyses. The net heat plot, for example, combines information about the contribution of direct estimates to network results with measures of inconsistency to identify potential drivers of disagreement in the network [11]. This matrix-based visualization helps researchers identify which direct comparisons are contributing to inconsistency and which network estimates are affected.
Methodological research has also addressed the challenge of multi-arm trials in network meta-analysis, which complicate the definition and detection of inconsistency because loop inconsistency cannot occur within a multi-arm trial [9]. The design-by-treatment interaction model has emerged as a comprehensive approach to evaluate inconsistency in networks containing multi-arm trials, as it successfully addresses the complications that arise from such studies [9].
The evolution from pairwise to network meta-analysis represents significant methodological progress in evidence synthesis, enabling comprehensive comparison of multiple interventions through integrated analysis of direct and indirect evidence. This advancement has dramatically enhanced the utility of systematic reviews for clinical and policy decision-making by providing comparative effectiveness estimates for all relevant interventions, even in the absence of head-to-head studies.
The validity of network meta-analysis depends critically on the transitivity assumption, which requires balanced distribution of effect modifiers across different treatment comparisons, and its statistical manifestation, consistency, which denotes agreement between direct and indirect evidence. Various statistical methods, including node-splitting and design-by-treatment interaction models, along with graphical tools like net heat plots, have been developed to evaluate these assumptions and identify potential inconsistency in evidence networks.
As evidence synthesis methodologies continue to evolve, network meta-analysis faces new challenges in the context of living systematic reviews and rapidly expanding evidence bases. Ongoing methodological research addresses these challenges through developing sequential methods, advanced inconsistency detection techniques, and enhanced visualization tools. For researchers, scientists, and drug development professionals, understanding both the capabilities and assumptions of network meta-analysis is essential for appropriate application and interpretation of this powerful evidence synthesis methodology.
Mixed Treatment Comparison (MTC) models, also known as Network Meta-Analysis (NMA), represent an advanced statistical methodology that synthesizes evidence from both direct head-to-head comparisons and indirect comparisons across multiple interventions [13] [14]. These models enable clinicians and policymakers to compare the relative effectiveness of multiple treatments, even when direct comparative evidence is absent, by leveraging a network of randomized controlled trials (RCTs) connected through common comparators [15] [16]. The validity and reliability of conclusions drawn from an MTC are contingent upon fulfilling three fundamental assumptions: homogeneity, similarity (transitivity), and consistency [17] [18]. This technical guide provides an in-depth examination of these core assumptions, detailing their conceptual foundations, assessment methodologies, and implications for researchers and drug development professionals engaged in evidence synthesis.
Conceptual Foundations of MTC Core Assumptions
Homogeneity
Homogeneity refers to the degree of variability in the relative treatment effects within the same pairwise comparison across different studies [17] [18]. In a homogeneous set of studies, any observed differences in treatment effect estimates are attributable solely to random chance (sampling error) rather than to systematic differences in study design or patient populations. This concept is specific to each direct head-to-head comparison within the broader network. Violations of homogeneity, termed heterogeneity, indicate that the studies included for a particular treatment pair are not estimating a common effect size, potentially compromising the validity of pooling their results.
Similarity (Transitivity)
The similarity assumption, also referred to as transitivity, concerns the validity of combining direct and indirect evidence across the entire network [17] [18]. It posits that the included trials are sufficiently similar in all key design and patient characteristics that are potential effect modifiers [17]. In practical terms, this means that if we were to imagine all trials as part of one large multi-arm trial, the distribution of effect modifiers would be similar across the different treatment comparison groups. The transitivity assumption underpins the legitimacy of making indirect comparisons; if studies comparing Treatment A vs. Treatment C differ systematically from studies comparing Treatment B vs. Treatment C, then an indirect comparison of A vs. B via C may be biased.
Consistency
Consistency is the statistical manifestation of the similarity assumption, describing the agreement between direct evidence (from studies that directly compare two treatments) and indirect evidence (estimated through a common comparator) for the same treatment comparison [13] [17] [18]. When both direct and indirect evidence exist for a treatment pair within a network, their effect estimates should be coherent, within the bounds of random error. Inconsistency arises when these estimates disagree significantly, suggesting a violation of the underlying similarity assumption or the presence of other biases within the network structure.
Table 1: Overview of Core Assumptions in Mixed Treatment Comparisons
| Assumption | Conceptual Definition | Scope of Application | Primary Concern |
|---|---|---|---|
| Homogeneity | Variability of treatment effects within the same pairwise comparison [18]. | Individual pairwise comparisons (e.g., all A vs. B studies) [17]. | Heterogeneity within a single treatment contrast. |
| Similarity/Transitivity | Similarity of trials across different comparisons with respect to effect modifiers [17] [18]. | The entire network of trials and comparisons. | Systematic differences in study or patient characteristics across different comparisons. |
| Consistency | Agreement between direct and indirect evidence for the same treatment comparison [13] [18]. | Treatment comparisons where both direct and indirect evidence exist. | Discrepancy between different sources of evidence for the same contrast. |
Methodological Assessment and Evaluation
Assessing Homogeneity
The assessment of homogeneity is a two-stage process involving both qualitative and quantitative evaluations.
Qualitative Assessment: Researchers should systematically tabulate and compare the clinical and methodological characteristics of all studies within each pairwise comparison. Key characteristics to examine include patient demographics (e.g., age, disease severity, comorbidities), intervention details (e.g., dosage, formulation), study design (e.g., duration, outcome definitions, risk of bias), and context (e.g., setting, concomitant treatments) [17] [18]. This qualitative review helps identify potential effect modifiers that may explain observed statistical heterogeneity.
Quantitative Assessment: Statistical heterogeneity within each pairwise comparison can be quantified using measures such as the I² statistic, which describes the percentage of total variation across studies that is due to heterogeneity rather than chance [17] [18]. An I² value greater than 50% is often considered to represent substantial heterogeneity [18]. The between-study variance (τ²) is another key metric, estimated within a random-effects model framework.
Table 2: Methods for Assessing the Core Assumptions of MTC
| Assumption | Qualitative/Scientific Assessment Methods | Quantitative/Statistical Assessment Methods |
|---|---|---|
| Homogeneity | Comparison of Clinical/Methodological Characteristics (PICO elements) [18]. | I² statistic, Cochran's Q test, estimation of τ² (between-study variance) [17] [18]. |
| Similarity/Transitivity | Systematic evaluation of the distribution of effect modifiers across the different treatment comparisons in the network [17] [18]. | Network meta-regression to test for interaction between treatment effect and trial-level covariates [19]. |
| Consistency | Evaluation of whether clinical/methodological differences identified could explain disagreement between direct and indirect evidence [17]. | Global Approaches: Design-by-treatment interaction test [13]. Local Approaches: Node-splitting method [17] [18], Comparison of direct and indirect estimates in a specific loop. |
Evaluating Similarity (Transitivity)
Evaluating the similarity assumption is primarily a qualitative and clinical judgment, as it precedes the statistical analysis [17]. There are no definitive statistical tests for transitivity; its assessment relies on a thorough understanding of the clinical context and the disease area.
- Identifying Effect Modifiers: The first step is to identify variables that are known or suspected to modify the relative treatment effect. These are often prognostic factors or baseline characteristics that influence the outcome and whose effect may differ depending on the treatment [17].
- Comparing Distributions: Once potential effect modifiers are identified, researchers must assess whether their distributions are balanced across the different treatment comparisons. For example, if all studies comparing Treatment B versus Treatment C enrolled a population with high disease severity, while studies comparing Treatment A versus Treatment C enrolled a population with low disease severity, and severity is an effect modifier, the assumption of transitivity for an indirect A vs. B comparison may be violated.
Advanced methods like network meta-regression can be used to explore the impact of trial-level covariates on treatment effects, thereby providing a quantitative check on potential intransitivity [19].
Testing for Consistency
Consistency can be evaluated using both global and local methods.
- Global Methods: Approaches like the design-by-treatment interaction model assess inconsistency across the entire network simultaneously [13]. This method evaluates whether the treatment effect estimates depend on the design of the studies (i.e., the set of treatments being compared).
- Local Methods: The node-splitting method is a popular local approach that separates evidence for a particular treatment comparison into direct and indirect components [17] [18]. It then statistically tests for a difference between these two estimates. This method is particularly useful for pinpointing the specific comparisons in the network where inconsistency exists.
Another practical approach involves using residual deviance and leverage statistics to identify studies that contribute most to the model's poor fit, which may indicate inconsistency. Iteratively removing such studies and recalculating the MTC can help explore the robustness of the results [18].
The following diagram illustrates the logical relationship between the core assumptions and the process of evaluating consistency within a network.
Logical Flow for Evaluating MTC Assumptions
A Stepwise Workflow for Practical Application
A structured, stepwise approach is recommended to ensure the robustness of an MTC. The following workflow, derived from practical application in health technology assessments, outlines this process [18].
Step 1: Ensuring Clinical Similarity
The initial phase focuses on constructing a clinically sound and similar study pool, which forms the foundation for all subsequent analyses [18].
- Protocol & Eligibility: Define a precise research question using the PICO (Population, Intervention, Comparator, Outcome) framework and establish strict eligibility criteria before commencing the review [13] [18].
- Systematic Review: Conduct a comprehensive systematic literature review to identify all potentially relevant RCTs, minimizing selection bias [13] [17].
- Assess Effect Modifiers: Critically appraise the included studies for known or suspected effect modifiers. Exclude studies that are fundamentally dissimilar in population, intervention, comparator, or outcome definition from the core network of interest [18]. For instance, studies on a specific sub-population (e.g., treatment-resistant patients) might be analyzed separately from studies on the general population if the treatment effect is expected to differ.
Step 2: Evaluating Statistical Homogeneity
After forming a clinically similar pool, the next step is to assess statistical homogeneity within each direct pairwise comparison [18].
- Pairwise Meta-Analysis: Perform standard pairwise meta-analyses (e.g., using random-effects models) for each treatment comparison where multiple direct studies exist.
- Quantify Heterogeneity: Calculate I² statistics and τ² for each comparison.
- Address Heterogeneity: If substantial heterogeneity (e.g., I² > 50%) is detected, investigate potential causes by examining the clinical and methodological characteristics of the contributing studies. If specific factors (e.g., high risk of bias, a particular patient subgroup) are identified as sources of heterogeneity, consider excluding those studies from the main analysis and conduct sensitivity analyses to assess the impact of their exclusion [18].
Step 3: Checking Network Consistency
The final step involves checking the statistical consistency of the entire network [18].
- Global Check: Use a global method, such as the design-by-treatment interaction test, to get an overview of inconsistency in the network.
- Local Check: Employ local methods, like node-splitting, to identify specific comparisons where direct and indirect evidence disagree.
- Residual Deviance: In Bayesian frameworks, use residual deviance and leverage statistics to identify studies that are outliers or contribute significantly to inconsistency [18].
- Manage Inconsistency: If inconsistency is found, explore its sources. This may involve checking for errors in data extraction, re-examining the clinical similarity of studies in inconsistent loops, or using more complex models that account for inconsistency. As a last resort, excluding the handful of studies contributing most to inconsistency and re-running the analysis can provide a view of robust, consistent results [18].
The Scientist's Toolkit: Essential Reagents for MTC Research
Table 3: Key Software and Methodological Tools for MTC Analysis
| Tool / Reagent | Category | Primary Function / Application | Key Considerations |
|---|---|---|---|
| R (gemtc, netmeta, BUGSnet packages) [13] | Statistical Software | A free software environment for statistical computing and graphics. Specific packages facilitate both frequentist and Bayesian NMA. | Highly flexible and powerful, but requires programming expertise. Active user community. |
| WinBUGS / OpenBUGS [13] [16] | Statistical Software | Specialized software for Bayesian analysis Using Gibbs Sampling. Implements complex hierarchical models like MTC. | Pioneering software for Bayesian MTC. Requires knowledge of the BUGS modeling language. |
| Stata [13] | Statistical Software | A general-purpose statistical software package. Capable of performing frequentist NMA (e.g., with network suite of commands). |
Widely used in medical statistics. Can be more accessible for those familiar with Stata. |
| Node-Splitting Method [17] [18] | Statistical Method | A local approach to evaluate inconsistency by splitting evidence for a specific comparison into direct and indirect components. | Excellent for pin-pointing the location of inconsistency in the network. |
| I² Statistic [17] [18] | Statistical Metric | Quantifies the percentage of total variability in a set of effect estimates due to heterogeneity rather than sampling error. | Standardized and intuitive measure for assessing homogeneity in pairwise meta-analysis. |
| Cochrane Risk of Bias Tool [17] | Methodological Tool | A standardized tool for assessing the internal validity (risk of bias) of randomized trials. | Critical for evaluating the quality of the primary studies feeding into the MTC. |
| Cucurbitaxanthin A | Cucurbitaxanthin A, CAS:103955-77-7, MF:C40H56O3, MW:584.9 g/mol | Chemical Reagent | Bench Chemicals |
| Kushenol L | Kushenol L, CAS:101236-50-4, MF:C25H28O7, MW:440.5 g/mol | Chemical Reagent | Bench Chemicals |
The assumptions of homogeneity, similarity, and consistency are not mere statistical formalities but are the foundational pillars that determine the validity of any mixed treatment comparison. Homogeneity ensures that direct evidence is coherently synthesized, similarity justifies the very possibility of making indirect comparisons, and consistency confirms that both types of evidence tell a congruent story. A rigorous MTC requires a proactive, stepwise approach that begins with a clinically informed systematic review, progresses through quantitative checks for heterogeneity and inconsistency, and involves ongoing critical appraisal of the underlying evidence base. As the use of MTCs continues to grow in health technology assessment and drug development [15], a deep and practical understanding of these core assumptions is indispensable for researchers aiming to generate reliable evidence to inform clinical practice and healthcare policy.
Mixed Treatment Comparisons (MTCs), also known as network meta-analyses, represent a sophisticated statistical methodology that enables the simultaneous comparison of multiple interventions within a unified analytical framework. This in-depth technical guide examines the core principles, rationales, and methodological considerations for implementing MTCs in comparative effectiveness research. Designed for researchers, scientists, and drug development professionals, this whitepaper synthesizes current guidance from leading health technology assessment organizations and regulatory bodies, outlining explicit scenarios where MTCs provide distinct advantages over conventional pairwise meta-analyses. We provide detailed experimental protocols, structured data presentation standards, and visualization tools to support the rigorous application of MTC methodology within the broader context of evidence synthesis and treatment decision-making.
Mixed Treatment Comparisons (MTCs) have emerged as a powerful methodology in evidence-based medicine for comparing multiple treatments simultaneously when head-to-head clinical trial evidence is limited or unavailable. Unlike traditional pairwise meta-analyses that directly compare only two interventions at a time, MTCs incorporate both direct evidence (from studies directly comparing treatments) and indirect evidence (through common comparator interventions) to form a connected network of treatment effects [20]. This approach allows for the estimation of relative treatment effects between all interventions in the network, even for pairs that have never been directly compared in clinical trials.
The fundamental rationale for conducting MTCs stems from the practical realities of clinical research and drug development. Complete sets of direct comparisons between all available treatments for a condition are rarely available, creating significant evidence gaps in traditional systematic reviews. MTC methodology addresses this limitation by enabling researchers to rank treatments according to their effectiveness or safety, inform economic evaluations, and guide clinical decision-making with more complete evidence networks. The value proposition of MTCs is particularly strong in fields with numerous treatment options, such as cardiology, endocrinology, psychiatry, and rheumatology, where they can provide crucial insights for formulary decisions and clinical guideline development [20].
Scopes and Applications of MTCs
Clinical and Policy Decision-Making Contexts
MTCs are particularly valuable in specific clinical and healthcare policy scenarios. According to guidance documents from major health technology assessment organizations, including the National Institute for Health and Care Excellence (NICE), the Cochrane Collaboration, and the Agency for Healthcare Research and Quality (AHRQ), MTCs are most beneficial when [20]:
- Multiple treatment options exist without direct comparative evidence for all relevant pairs
- Clinical guidelines require ranking of therapeutic alternatives by efficacy, safety, or cost-effectiveness
- Resource allocation decisions demand comprehensive understanding of relative treatment benefits
- Drug development priorities need establishment based on existing treatment landscape
- Gaps in the evidence base exist where direct trials are ethically or practically challenging to conduct
The application of MTCs extends beyond pharmacologic interventions to include comparisons of behavioral interventions, surgical procedures, medical devices, and diagnostic strategies, making them versatile tools across healthcare research domains [20].
Quantitative Scope Assessment Framework
Table 1: Criteria for Determining When to Conduct an MTC
| Assessment Factor | Favorable Conditions for MTC | Unfavorable Conditions for MTC |
|---|---|---|
| Number of Interventions | ≥3 competing interventions | Only 2 interventions of interest |
| Evidence Connectivity | Connected network through common comparators | Disconnected network without linking interventions |
| Clinical Relevance | Need to rank multiple treatment options | Only single pairwise comparison needed |
| Evidence Gaps | Missing direct comparisons between important interventions | Complete direct evidence available for all comparisons |
| Policy Urgency | Pressing need for comprehensive treatment guidance | Limited decision-making implications |
Methodological Rationale and Theoretical Foundation
Statistical Assumptions and Requirements
The validity of MTC conclusions depends on several critical statistical assumptions that must be evaluated before undertaking an analysis. These foundational assumptions represent the methodological rationales that justify the use of indirect evidence [20]:
- Transitivity Assumption: The distribution of effect modifiers (patient characteristics that influence treatment outcome) should be similar across treatment comparisons in the network. This implies that were a direct comparison available, it would yield similar results to the indirect comparison.
- Consistency Assumption: Direct and indirect evidence for the same comparison should be in statistical agreement. Consistency validates that the different sources of evidence measure the same underlying treatment effect.
- Homogeneity Assumption: Studies included in each direct comparison should be sufficiently similar in their design and patient populations to be appropriately combined.
Violations of these assumptions threaten the validity of MTC results and must be carefully assessed through clinical and statistical methods before proceeding with analysis.
Experimental Design and Protocol Development
A rigorously developed protocol is essential for conducting a valid MTC. The following detailed methodology outlines the key steps in the MTC process [20]:
Phase 1: Network Specification
- Define precisely the clinical question, including patient populations, interventions, comparators, and outcomes of interest (PICO framework)
- Establish eligibility criteria for study inclusion with particular attention to potential effect modifiers
- Develop a comprehensive search strategy across multiple databases (e.g., MEDLINE, Cochrane Central, EMBASE)
- Document the search strategy explicitly, including dates, databases, and search terms
Phase 2: Data Collection and Management
- Perform dual independent study selection with conflict resolution procedures
- Extract data using standardized forms capturing study characteristics, quality indicators, and outcome data
- Identify and record potential effect modifiers for assessment of transitivity assumption
- Map all available direct comparisons to visualize the evidence network
Phase 3: Statistical Analysis Plan
- Specify Bayesian or Frequentist analytical approach with justification
- Select fixed-effect or random-effects model based on assessment of heterogeneity
- Define prior distributions for Bayesian analyses (if applicable)
- Plan assessment of consistency using appropriate statistical methods (e.g., node-splitting)
- Outline sensitivity analyses to test robustness of findings
Phase 4: Results Interpretation and Reporting
- Apply appropriate methods to rank treatments while acknowledging limitations
- Report findings with measures of uncertainty (e.g., credible intervals or confidence intervals)
- Discuss limitations, including potential violations of assumptions and network weaknesses
- Adhere to reporting guidelines such as PRISMA-NMA
Evidence Network Visualization
MTC Methodology Workflow
Practical Implementation Considerations
Analytical Framework Selection
The choice between Bayesian and Frequentist approaches for MTC implementation represents a critical methodological decision with practical implications for analysis and interpretation. Based on examination of existing MTC applications in systematic reviews, each approach offers distinct advantages [20]:
Table 2: Comparison of Bayesian vs. Frequentist Approaches in MTC
| Characteristic | Bayesian MTC | Frequentist MTC |
|---|---|---|
| Prevalence in Literature | More commonly used (≈80% of published MTCs) | Less frequently implemented (≈20% of published MTCs) |
| Model Parameters | Requires specification of prior distributions | Relies on likelihood-based estimation |
| Results Interpretation | Direct probability statements (e.g., probability Treatment A is best) | Confidence intervals and p-values |
| Computational Requirements | Often more intensive, typically using WinBUGS/OpenBUGS | Generally less intensive, using Stata/SAS/R |
| Handling of Complex Models | More flexible for sophisticated model structures | Can be limited for highly complex networks |
| Treatment Ranking | Natural framework for ranking probabilities | Requires additional methods for ranking |
Research Reagent Solutions and Essential Materials
Successful implementation of MTC requires both methodological expertise and appropriate analytical tools. The following table details key resources in the MTC researcher's toolkit [20]:
Table 3: Essential Research Tools for MTC Implementation
| Tool Category | Specific Examples | Function and Application |
|---|---|---|
| Statistical Software | WinBUGS, OpenBUGS, R, SAS, Stata | Bayesian and Frequentist model estimation and analysis |
| Quality Assessment Tools | Cochrane Risk of Bias, GRADE for NMA | Evaluate study quality and rate confidence in effect estimates |
| Data Extraction Platforms | Covidence, DistillerSR, Excel templates | Systematic data collection and management |
| Network Visualization | R (netmeta, gemtc packages), Stata network maps | Create evidence network diagrams and results presentations |
| Consistency Assessment | Node-splitting, design-by-treatment interaction models | Evaluate statistical consistency between direct and indirect evidence |
| Reporting Guidelines | PRISMA-NMA checklist | Ensure comprehensive and transparent reporting of methods and findings |
Signaling Pathways in MTC Methodology
The methodological foundation of MTCs can be conceptualized as a series of interconnected signaling pathways where evidence flows through the network to inform treatment effects. Understanding these pathways is essential for appropriate implementation and interpretation.
MTC Evidence Flow Network
Mixed Treatment Comparisons represent a methodologically sophisticated approach to evidence synthesis that expands the utility of conventional systematic reviews. The decision to conduct an MTC should be guided by the presence of multiple interventions with incomplete direct comparison evidence, the connectivity of the evidence network, and the need for comprehensive treatment rankings to inform clinical or policy decisions. Successful implementation requires rigorous assessment of key assumptions (transitivity, consistency, homogeneity), appropriate selection of analytical framework (Bayesian or Frequentist), and adherence to established methodological standards. When properly conducted and reported, MTCs provide valuable evidence for comparative effectiveness research, drug development decisions, and clinical guideline development, filling critical gaps where direct evidence is absent or insufficient. The ongoing development of MTC methodology, including more sophisticated approaches to assessing assumption violations and handling complex evidence structures, continues to enhance its value for evidence-based decision-making across healthcare domains.
Network Meta-Analysis (NMA), also known as Mixed Treatment Comparison (MTC), is a sophisticated statistical methodology that extends traditional pairwise meta-analysis by simultaneously synthesizing evidence from a network of interventions [21] [22]. Its core advantage lies in the ability to compare multiple treatments, even those never directly compared in head-to-head trials, by utilizing both direct evidence (from studies comparing treatments directly) and indirect evidence (inferred through a common comparator) [23] [22]. The architecture of this evidence—how the various treatments (nodes) and existing comparisons (edges) interconnect—is termed network geometry. The geometry of a network is not merely a visual aid; it is fundamental to understanding the scope, reliability, and potential biases of an NMA [22]. A well-connected and thoughtfully analyzed network geometry allows for robust ranking of treatments and informs clinical and policy decisions, forming a critical component of modern evidence-based medicine [21].
Core Concepts and Key Assumptions
Before delving into specific geometries, it is essential to grasp the foundational concepts and assumptions that underpin a valid NMA.
- Transitivity: This is the fundamental assumption that makes indirect comparisons plausible. It requires that the effect modifiers—clinical or methodological characteristics that can influence the outcome (e.g., disease severity, patient age, trial duration)—are sufficiently similar across all studies included in the network [21] [23]. For instance, if all trials comparing A vs. B and B vs. C are in a severely ill population, but the trials for A vs. C are in a mildly ill population, the transitivity assumption is violated. Transitivity is a clinical and methodological assumption that cannot be proven statistically but must be critically assessed by experts before conducting an NMA [21].
- Consistency: This is an extension of transitivity into the statistical domain. Consistency refers to the statistical agreement between direct evidence (from head-to-head trials) and indirect evidence (inferred through the network) for the same treatment comparison [23] [22]. When both direct and indirect evidence exist for a comparison, forming a "closed loop," statistical tests can be applied to assess inconsistency. The presence of significant inconsistency suggests a violation of the transitivity assumption or other biases and must be investigated [21].
Table 1: Glossary of Essential Network Meta-Analysis Terms
| Term | Definition |
|---|---|
| Node | Represents an intervention or technology under evaluation in the network [22]. |
| Edge | The line connecting two nodes, representing the availability of direct evidence from one or more studies [22]. |
| Common Comparator | An intervention (e.g., 'B') that serves as an anchor, allowing for indirect comparison between other interventions (e.g., A and C) [22]. |
| Direct Treatment Comparison | A comparison of two interventions based solely on studies that directly compare them (head-to-head trials) [22]. |
| Indirect Treatment Comparison | An estimate of the relative effect of two interventions that leverages their direct comparisons with a common comparator [22]. |
| Network Geometry | The overall pattern or structure formed by the nodes and edges in a network, describing how evidence is interconnected [22]. |
| Closed Loop | A part of the network where interventions are directly connected, forming a closed geometry (e.g., a triangle), allowing for both direct and indirect evidence to inform the comparisons [22]. |
Types of Network Geometry and Their Interpretation
Network geometries can range from simple to highly complex. Each structure presents unique advantages and methodological challenges.
Star Geometry
A star geometry is one of the simplest network forms, characterized by a single, central common comparator connected to all other interventions in the network. There are no direct connections between the peripheral interventions.
Star network with a common comparator
- Interpretation and Implications: In a star network, all comparisons between peripheral interventions (e.g., Drug A vs. Drug B) are purely indirect. The validity of these comparisons rests entirely on the transitivity assumption [21] [22]. If the trials connecting each drug to the common comparator are sufficiently similar in their effect modifiers, the indirect estimates can be valid. However, this geometry offers no means to statistically check for consistency, as there are no closed loops. It is a fragile structure highly dependent on the quality and homogeneity of the included studies.
Loop Geometry
A loop geometry emerges when three or more interventions are directly connected, forming a closed structure. The simplest loop is a triangle.
A closed-loop network enabling consistency checks
- Interpretation and Implications: The presence of a closed loop is methodologically significant. It means that for at least one comparison (e.g., A vs. C), both direct evidence (from A-C trials) and indirect evidence (via A-B-C) are available [22]. This allows for a statistical assessment of consistency between the direct and indirect estimates [21] [23]. Detected inconsistency signals potential problems with transitivity or other biases and requires investigation. Loops therefore strengthen a network by providing a built-in mechanism for verifying the coherence of the evidence.
Complex and Asymmetrical Structures
Most real-world NMAs exhibit complex geometries that combine multiple loops, side-arms, and potentially asymmetrical evidence distribution.
A complex network with varied evidence
- Interpretation and Implications:
- Asymmetry: The thickness of edges and size of nodes often carry meaning, representing the number of trials or participants for a given comparison or intervention [21] [23]. In the diagram above, thicker lines indicate more trials, and larger nodes indicate more participants. This asymmetry highlights which parts of the network are supported by more robust evidence. Comparisons relying on thin edges or long, indirect pathways may yield less precise and potentially less reliable estimates.
- Robustness: Networks with more connections and multiple paths for indirect comparisons are generally more robust. They "borrow strength" across the entire network, improving the precision of effect estimates [21]. The geometry can also inform the design of future trials by identifying the most valuable direct comparisons—those that would fill critical gaps or strengthen weak links in the network [21].
Table 2: Summary of Network Geometries and Methodological Implications
| Geometry Type | Key Characteristics | Strengths | Limitations & Considerations |
|---|---|---|---|
| Star | Single central comparator; no direct links between peripherals. | Simple structure; easy to interpret. | All comparisons are indirect; relies entirely on transitivity; no way to check consistency. |
| Loop | Closed structure (e.g., triangle) with interventions directly connected. | Enables statistical check of consistency between direct and indirect evidence. | Detection of inconsistency requires investigation into its source (bias or diversity). |
| Complex/Asymmetrical | Multiple interconnected loops and side-arms; varied evidence distribution. | Robustness from borrowing strength; identifies evidence gaps for future research. | Interpretation is more complex; requires careful assessment of transitivity across the entire network. |
Methodological Protocols for Network Geometry Analysis
A rigorous NMA requires a structured approach to evaluating its geometry. The following protocol outlines key steps.
Data Collection and Network Diagram Creation
- Systematic Review: Conduct a comprehensive systematic review to identify all relevant randomized controlled trials (RCTs) for the interventions of interest. This forms the evidence base.
- Define Nodes: Clearly define each intervention (node) to ensure they are clinically coherent. Grouping similar interventions (e.g., different doses of the same drug) requires clear justification.
- Plot the Network: Create a network diagram, typically using statistical software like R (with packages like
netmeta) or Bayesian software like WinBUGS/OpenBUGS [21] [23]. The diagram should visually represent all direct comparisons.
Evaluating Transitivity and Consistency
- Transitivity Assessment: Before analysis, compare the distribution of potential effect modifiers (e.g., patient baseline risk, study year, methodological quality) across the different direct comparisons. This is a qualitative/substantive evaluation [21].
- Consistency Assessment: Use statistical models to evaluate consistency in closed loops. Local methods (e.g., the Bucher method for a single loop) and global methods (e.g., design-by-treatment interaction model) can be applied. The presence of significant inconsistency necessitates exploration of its sources, which may include differences in trial populations, interventions, or outcome definitions [21].
The Scientist's Toolkit: Essential Reagents and Software
Table 3: Key Research Reagent Solutions for Network Meta-Analysis
| Item / Resource | Type | Function and Purpose |
|---|---|---|
| R Statistical Software | Software Environment | A free, open-source environment for statistical computing and graphics. It is the primary platform for conducting frequentist and some Bayesian NMAs. |
netmeta package (R) |
Software Library | A widely used R package for conducting frequentist network meta-analyses. It performs meta-analysis, generates network plots, and evaluates inconsistency. |
| WinBUGS / OpenBUGS | Software Application | Specialized software for conducting complex Bayesian statistical analyses using Markov chain Monte Carlo (MCMC) methods. It has been historically dominant for Bayesian NMA [21] [23]. |
| JAGS (Just Another Gibbs Sampler) | Software Application | A cross-platform alternative to BUGS for Bayesian analysis, often used with the R2jags package in R. |
| PRISMA-NMA Checklist | Methodological Guideline | (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for NMA): A reporting guideline to ensure the transparent and complete reporting of NMAs. |
| CINeMA (Confidence in NMA) | Web Application / Framework | A software and methodological framework for evaluating the confidence in the results from network meta-analysis, focusing on risk of bias, indirectness, and inconsistency. |
| 680C91 | 680C91, CAS:163239-22-3, MF:C15H11FN2, MW:238.26 g/mol | Chemical Reagent |
| Garciniaxanthone E | Garciniaxanthone E | Garciniaxanthone E is a natural xanthone for research. Studies suggest potential in oncology and biochemistry. This product is for Research Use Only (RUO). Not for human consumption. |
The interpretation of network geometry—from simple stars to complex, asymmetrical structures—is not a mere descriptive exercise but a core component of a valid and informative Mixed Treatment Comparison. The geometry dictates the strength of the evidence, the validity of the underlying assumptions of transitivity and consistency, and the confidence with which clinicians and policymakers can interpret the resulting treatment rankings and effect estimates. A thorough understanding of these structures, coupled with rigorous methodological protocols for their evaluation, is indispensable for researchers and drug development professionals seeking to navigate and contribute to the evolving landscape of evidence-based medicine.
Implementing MTC Models: Methodological Frameworks and Real-World Applications
Within the evolving landscape of comparative effectiveness research, mixed treatment comparison (MTC) models, also known as network meta-analysis, have become indispensable tools for evaluating the relative efficacy and safety of multiple treatments. These models synthesize evidence from both direct head-to-head comparisons and indirect comparisons, enabling a comprehensive ranking of treatment options even when direct evidence is sparse or absent [24] [25]. The statistical analysis of such complex networks can be approached through two primary philosophical and methodological paradigms: the Frequentist and Bayesian frameworks. The choice between them is not merely philosophical but has practical implications for model specification, computational burden, and the interpretation of results. This whitepaper provides an in-depth technical comparison of these two approaches, grounded in the context of MTC models, to guide researchers, scientists, and drug development professionals in selecting the appropriate framework for their research objectives.
Methodological Foundations
Core Principles of Frequentist and Bayesian Inference
The Frequentist approach to statistics is based on the long-run behavior of estimators. It treats model parameters as fixed, unknown quantities. Inference is drawn by considering the probability of the observed data, or something more extreme, under a assumed null hypothesis (e.g., no treatment effect), which yields the well-known p-value. Confidence intervals are constructed to indicate a range of values that, over repeated sampling, would contain the true parameter value a certain percentage of the time (e.g., 95%) [26].
In contrast, the Bayesian framework treats parameters as random variables with associated probability distributions. It combines prior knowledge or belief about a parameter (encoded in the prior distribution) with the observed data (via the likelihood function) to form an updated posterior distribution. The posterior distribution fully encapsulates the uncertainty about the parameter after seeing the data [27]. This leads to intuitive probabilistic statements, such as "there is a 95% probability that the true treatment effect lies within this credible interval."
Application in Mixed Treatment Comparisons
In MTC models, both frameworks aim to estimate relative treatment effects across a network of evidence.
- The Frequentist Approach often employs multivariable logistic regression models with treatments and patient subgroups included as fixed or random effects. The analysis typically relies on maximum likelihood estimation (MLE) to find the parameter values that make the observed data most probable [28].
- The Bayesian Approach typically employs hierarchical models and uses computational methods, most notably Markov Chain Monte Carlo (MCMC), to sample from the complex posterior distributions of the treatment effect parameters. A key advantage is the direct calculation of the probability that each treatment is the best, second-best, etc., based on the posterior distributions [27] [25].
Experimental Protocols: A Simulation Case Study
To empirically compare the two frameworks, researchers often employ simulation studies. The following details a protocol from a recent investigation into the Personalised Randomised Controlled Trial (PRACTical) design, which is a specific application of MTC principles [28].
Motivational Context and Data Generation
The simulation was motivated by a trial comparing four targeted antibiotic treatments (A, B, C, D) for multidrug-resistant bloodstream infections. The PRACTical design was used because there was no single standard of care, and patients had different eligibility for treatments, forming four distinct subgroups (K=4).
- Primary Outcome: A binary outcome of 60-day mortality was simulated.
- Sample Sizes: Total sample sizes (N) ranging from 500 to 5,000 patients were explored, recruited equally across 10 sites.
- Data Generation: Patient subgroup and site allocation were generated from multinomial distributions. The probability of mortality for a patient in subgroup k assigned to treatment j was denoted by ( P_{jk} ). The primary outcome was then generated from a binomial distribution based on this probability [28].
Personalised Randomisation
Each patient was randomised only among the treatments for which they were eligible. This created four different "patterns" or randomisation lists. For instance, one subgroup might be eligible for treatments {A, B, C}, while another was eligible for {B, C, D}. This structure creates a connected network suitable for indirect comparison [28].
Analytical Models
The same core logistic model was fitted using both frameworks: $$logit(P{jk}) = ln(\alphak / \alpha{k'}) + \psi{jk'}$$ Here, ( \psi{jk'} ) is the log-odds of death for treatment ( j ) in the reference subgroup ( k' ), and ( ln(\alphak / \alpha_{k'}) ) is the log-odds ratio for subgroup k compared to the reference subgroup [28].
- Frequentist Implementation: The model was fitted using standard MLE techniques via the R package 'stats' [28].
- Bayesian Implementation: The model was fitted using the R package 'rstanarm' with MCMC sampling. Three different strongly informative normal priors were tested to evaluate the impact of prior knowledge, including both representative and unrepresentative historical data [28].
Performance Measures
The following performance measures were calculated to compare the two approaches:
- Probability of Predicting the True Best Treatment (( P_{best} )): The proportion of simulations in which the model correctly identified the treatment with the lowest true mortality.
- Probability of Interval Separation (( P_{IS} )): A novel proxy for statistical power, defined as the probability that the 95% confidence or credible interval for the best treatment does not overlap with the intervals of other treatments.
- Probability of Incorrect Interval Separation (( P_{IIS} )): A novel proxy for Type I error, defined as the probability that a treatment's interval is incorrectly separated from the others when no true difference exists [28].
Quantitative Comparison of Framework Performance
Table 1: Summary of Key Performance Metrics from Simulation Studies
| Metric | Frequentist Approach | Bayesian Approach (Informative Prior) | Context / Notes |
|---|---|---|---|
| Probability of Identifying True Best Treatment | ( P_{best} \ge 80\% ) | ( P_{best} \ge 80\% ) | Achieved at N ≤ 500; both methods perform similarly [28] |
| Achieving 80% Power (Probability of Interval Separation) | Sample size of 1500-3000 required | Sample size of 1500-3000 required | ( P_{IS} ) reached a maximum of 96% [28] |
| Type I Error Control (Probability of Incorrect Interval Separation) | ( P_{IIS} < 0.05 ) for all N | ( P_{IIS} < 0.05 ) for all N | Maintained control across sample sizes (N=500-5000) in null scenarios [28] |
| Precision of Estimates | Better precision in some NMA [29] | Can be less precise in some NMA [29] | Highly dependent on network geometry and prior choice |
| Ranking Consistency | Identified same best treatment as Bayesian | Identified same best treatment as Frequentist | Observed in a network meta-analysis of esophageal cancer treatments [29] |
Table 2: Operational and Interpretive Differences Between the Two Frameworks
| Aspect | Frequentist Approach | Bayesian Approach |
|---|---|---|
| Computational Speed | Faster; often orders of magnitude less time [26] | Slower due to MCMC sampling [26] |
| Handling of Complex Networks | Can struggle with sparse networks or lack common comparators [24] | Can produce results for all comparisons in a connected network [24] |
| Incorporation of Prior Evidence | No formal mechanism | Directly incorporated via prior distributions [28] |
| Interpretation of Output | Treatment ranks based on point estimates (e.g., odds ratios) [28] | Probabilistic treatment ranks ("rankograms") showing P(each rank) [27] |
| Model Diagnostics | Relatively straightforward (e.g., check for convergence warnings) [26] | More complex; requires checking MCMC convergence (e.g., trace plots, (\hat{R})) [26] |
| Result Presentation | Confidence Intervals (CI) | Credible Intervals (CrI) |
Visualizing Analytical Workflows
The following diagram illustrates the typical analytical workflow for a Mixed Treatment Comparison using both the Frequentist and Bayesian approaches, highlighting key differences.
The Scientist's Toolkit: Essential Components for MTC Analysis
Table 3: Key Research Reagent Solutions for Implementing MTC Models
| Tool / Component | Function | Relevance to Framework |
|---|---|---|
| Statistical Software (R/Python) | Provides the environment for data manipulation, analysis, and visualization. | Essential for both |
Frequentist Packages (e.g., stats in R) |
Fits generalised linear models using maximum likelihood estimation. | Core for Frequentist analysis [28] |
Bayesian MCMC Packages (e.g., rstanarm, JAGS) |
Fits Bayesian models using Markov Chain Monte Carlo sampling. | Core for Bayesian analysis [28] [27] |
| Prior Distribution | Encodes pre-existing knowledge or beliefs about parameters before seeing the trial data. | Critical for Bayesian analysis [28] |
| MCMC Diagnostics (e.g., (\hat{R}), trace plots) | Tools to assess convergence of MCMC algorithms to the true posterior distribution. | Critical for Bayesian analysis [26] |
| Network Plot | Visualizes the geometry of the treatment network, showing direct comparisons. | Important for both (assessing connectivity) [24] |
| Scoparinol | Scoparinol, MF:C27H38O4, MW:426.6 g/mol | Chemical Reagent |
| ARL 17477 | ARL 17477, CAS:180983-17-9, MF:C20H22Cl3N3S, MW:442.8 g/mol | Chemical Reagent |
The choice between Frequentist and Bayesian approaches for mixed treatment comparisons is not about identifying a universally superior method, but rather about selecting the right tool for a specific research context. The evidence suggests that in many practical scenarios, particularly those with ample data, both frameworks yield concordant results regarding treatment efficacy and ranking [28] [29].
The Frequentist approach offers advantages in computational speed, simplicity of diagnostics, and a familiar inferential framework that avoids the sometimes contentious selection of priors. This makes it highly suitable for initial explorations and analyses where computational resources are limited or where incorporating prior knowledge is not a primary goal [26].
The Bayesian approach provides superior flexibility in model specification, a natural mechanism for incorporating historical evidence through priors, and a more intuitive probabilistic interpretation of results via rankograms and direct probability statements about treatment performance [27]. This is particularly valuable in complex networks with sparse data and in drug development where prior phases of research provide legitimate prior information.
For researchers and drug development professionals, the decision should be guided by the geometry of the evidence network, the availability of reliable prior information, computational constraints, and the specific inferential goals of the analysis. As the field advances, the development of hybrid methods that leverage the strengths of both paradigms may offer the most powerful path forward for comparative effectiveness research.
Mixed Treatment Comparison (MTC) models, also known as network meta-analysis, represent a sophisticated statistical methodology that enables the simultaneous synthesis of evidence for multiple interventions. These models have gained significant prominence in evidence-based medicine as they allow for the comparison of multiple treatments, even when direct head-to-head evidence is absent or limited [30]. The fundamental principle underlying MTC is the integration of both direct evidence (from studies directly comparing treatments) and indirect evidence (from studies connected through common comparators) within a single coherent analytical framework [15] [30].
The rapid development and adoption of MTC methodologies since 2009 highlight their importance in addressing complex clinical questions where multiple competing interventions exist [15]. For researchers and drug development professionals, MTC provides a powerful tool for maximizing the utility of available clinical trial data, facilitating comparative effectiveness research, and informing health policy decisions. By synthesizing all available evidence, MTC models can provide more precise estimates of treatment effects and enable ranking of interventions, thereby supporting clinical decision-making and health technology assessment processes [15] [30].
Foundational Concepts and Terminology
Understanding MTC requires familiarity with several key concepts and terms that form the vocabulary of this methodological approach:
Network Meta-Analysis: A generic term describing the simultaneous synthesis of evidence for all possible pairwise comparisons across more than two interventions [30]. This approach allows for the comprehensive evaluation of multiple treatment options within a single analytical framework.
Mixed Treatment Comparison (MTC): Specifically refers to the statistical approach used to analyze a network of evidence with more than two interventions where at least one pair of interventions has been compared both directly and indirectly, forming a closed loop of evidence [30]. This represents a specific implementation of network meta-analysis that incorporates both direct and indirect evidence.
Direct Evidence: Treatment effect estimates derived from studies that directly compare the interventions of interest (e.g., randomized controlled trials comparing Treatment A vs. Treatment B) [30].
Indirect Evidence: Treatment effect estimates obtained by comparing interventions through a common comparator (e.g., comparing Treatment A vs. Treatment C through their common comparisons with Treatment B) [15] [30].
Closed Loop: A network structure where each comparison has both direct evidence and indirect evidence available [30]. For example, consider AB trials, AC trials, and BC trials - the BC comparison has direct evidence from BC trials and indirect evidence from AB and AC trials.
Bayesian Framework: An analytical approach that combines prior probability distributions with likelihood distributions based on observed data to obtain posterior probability distributions [30]. Bayesian methods have undergone substantial development for MTC applications and offer advantages such as the ability to rank treatments and handle complex random-effects models.
Prerequisites and Preparatory Steps
Systematic Literature Review and Search Strategy
The foundation of any robust MTC is a comprehensive, methodologically sound systematic review. The literature search must be designed to identify all relevant studies comparing any of the interventions of interest within the network.
Key considerations for search strategy development:
- Utilize multiple electronic databases including MEDLINE, Embase, Cochrane Central Register of Controlled Trials, and specialized trial registries
- Develop search strategies using appropriate Boolean operators and database-specific subject headings
- Implement supplementary search methods including reference list checking, citation searching, and consultation with content experts
- Consider both published and unpublished literature to minimize publication bias
Specific challenges in identifying MTCs include the lack of standardized indexing terms in major databases and varying terminology used by authors, making comprehensive identification difficult [15]. A sample search strategy adapted from published methodologies might include:
Study Selection and Data Extraction
Establish explicit, predefined criteria for study inclusion and exclusion based on the PICO framework (Population, Intervention, Comparator, Outcomes). Data extraction should capture both study characteristics and outcome data using standardized forms.
Essential data elements to extract:
- Study identifiers and publication details
- Participant characteristics (including biomarkers when relevant) [19]
- Intervention and comparator details
- Outcome definitions and measurement timepoints
- Effect estimates and measures of variance
- Risk of bias assessment using appropriate tools
Methodological Workflow for Mixed Treatment Comparisons
The following diagram illustrates the comprehensive workflow for conducting an MTC, from initial planning through to interpretation and reporting:
Network Construction and Assessment
The initial analytical step involves mapping the evidence network to visualize the available direct comparisons and identify the structure of the network.
Network types and structures:
- Star structure: Only one intervention has been directly compared with each of the others
- Single-loop structures: Contain direct comparisons between one set of at least three interventions
- Multi-loop structures: Contain direct comparisons between multiple sets of interventions
The network diagram (such as the example in Figure 1 comparing five interventions A-E) illustrates where trial results of direct comparisons exist and demonstrates that while there may be no single common comparator for all interventions, each intervention shares at least one comparator with another in the network [15].
Evaluating Key Assumptions
The validity of MTC results depends on several critical assumptions that must be thoroughly evaluated:
Similarity Assumption: Requires that studies included in the network are sufficiently similar in terms of clinical and methodological characteristics that could effect treatment effects. This includes similarity of populations, interventions, outcomes, and study designs.
Consistency Assumption: Requires that direct and indirect evidence are in agreement. This fundamental assumption means that the indirect estimate of a treatment effect should not systematically differ from its direct estimate.
Homogeneity Assumption: Requires that studies estimating the same pairwise comparison are similar enough to be combined.
Formal and informal methods exist to assess the validity of these assumptions both statistically and clinically [15]. Inconsistency in both assessment and reporting of these assumptions has been noted in the literature, highlighting the need for standardized approaches [15].
Statistical Models and Implementation
MTC analyses can be implemented within both frequentist and Bayesian frameworks, though Bayesian methods have undergone substantially greater development and are more commonly used in practice [15] [30].
Core statistical models for MTC:
Fixed-Effect MTC Model: Assumes a single true treatment effect underlying all studies, with observed variation attributable only to random sampling error. This model can be represented as:
δ̂ᵢ ~ N(δ, σᵢ²)
where δ̂ᵢ is the observed treatment effect in study i, δ is the common true treatment effect, and σᵢ² is the within-study variance of study i [19].
Random-Effects MTC Model: Allows for heterogeneity between studies by assuming that the true treatment effects come from a common distribution:
δ̂ᵢ ~ N(δᵢ, σᵢ²)
δᵢ ~ N(d, τ²)
where δᵢ is the true treatment effect in study i, d is the mean of the distribution of true effects, and τ² is the between-study variance [19].
The selection between fixed-effect and random-effects models should be based on clinical and methodological considerations, assessment of heterogeneity, and model fit statistics.
Advanced Methodological Considerations
Handling Mixed Biomarker Populations
Recent methodological developments have addressed the challenge of synthesizing evidence from trials with mixed biomarker populations, which is particularly relevant in precision medicine. The table below summarizes approaches for evidence synthesis with mixed populations:
Table 1: Methods for Evidence Synthesis with Mixed Biomarker Populations
| Method Category | Data Requirements | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| Pairwise Meta-Analysis with Aggregate Data (AD) [19] | Published summary statistics | Situations with limited biomarker data | Accessibility; utilizes available literature | Potential ecological bias; limited subgroup information |
| Network Meta-Analysis with Aggregate Data (AD) [19] | Network of trials with mixed biomarker data | Comparing multiple targeted therapies | Incorporates both direct and indirect evidence | Requires stronger assumptions about consistency |
| Network Meta-Analysis with AD and Individual Participant Data (IPD) [19] | Combination of aggregate and individual-level data | Scenarios with partial biomarker data | Reduces ecological bias; enables standardized analysis | Requires access to IPD; complex implementation |
These methods are particularly valuable in drug development contexts where targeted therapies may be investigated in different biomarker subgroups across the development lifecycle [19]. For example, treatments like Cetuximab and Panitumumab in metastatic colorectal cancer were initially studied in mixed populations, with subsequent trials focusing on KRAS wild-type patients after predictive biomarkers were identified [19].
Individual Participant Data Meta-Analysis
When available, Individual Participant Data (IPD) enables more sophisticated MTC analyses through one-stage or two-stage approaches:
Two-Stage Approach: Analyzes IPD from each trial separately to obtain trial-specific treatment effect estimates, which are then combined using standard meta-analysis techniques. This approach allows for standardization of inclusion criteria, outcome definitions, and statistical methods across studies [19].
One-Stage Approach: Analyzes IPD from all studies simultaneously using a hierarchical regression model:
yᵢⱼ ~ N(αᵢ + δᵢxᵢⱼ, σᵢ²)
δᵢ ~ N(d, τ²)
where yᵢⱼ is the observed outcome for participant j in study i, xᵢⱼ is the treatment assignment, αᵢ is the study-specific intercept, and δᵢ is the study-specific treatment effect [19].
IPD meta-analysis is generally considered the gold standard as it allows for more detailed exploration of treatment-covariate interactions and reduces ecological bias [19].
Analysis Implementation and Validation
Computational Tools and Software
Implementation of MTC analyses requires specialized statistical software. The following table outlines key research reagents and computational tools:
Table 2: Essential Research Reagents and Computational Tools for MTC
| Tool Category | Specific Software/ Packages | Primary Function | Implementation Considerations |
|---|---|---|---|
| Bayesian MTC Software [15] [30] | OpenBUGS, WinBUGS, JAGS, Stan | Bayesian model fitting using MCMC | Requires specification of prior distributions; monitors convergence |
| Frequentist MTC Software [30] | R packages (netmeta, gemtc), Stata network modules | Frequentist network meta-analysis | Typically faster computation; different uncertainty characterization |
| Network Visualization Tools | R packages (igraph, networkD3), Cytoscape | Evidence network diagram creation | Essential for communicating network structure and identifying gaps |
| Diagnostic and Validation Tools | R packages (dmetar, pcnetmeta) | Assessment of inconsistency and model fit | Critical for validating assumptions and model performance |
Model Validation and Diagnostic Procedures
Robust MTC implementation requires thorough model validation and diagnostic checking:
Convergence Assessment: For Bayesian models using Markov Chain Monte Carlo (MCMC) methods, convergence should be assessed using trace plots, Gelman-Rubin statistics, and effective sample sizes.
Goodness-of-Fit Evaluation: Assess model fit using residual deviance, deviance information criterion (DIC) for Bayesian models, or Akaike information criterion (AIC) for frequentist models.
Inconsistency Checking: Evaluate consistency between direct and indirect evidence using node-splitting approaches, design-by-treatment interaction models, or comparison of direct and indirect estimates in specific loops.
Sensitivity Analyses: Conduct sensitivity analyses to assess the impact of methodological choices, inclusion criteria, prior distributions, and handling of missing data.
Interpretation and Reporting of Results
Presentation of Findings
Effective communication of MTC results requires clear presentation of both the network structure and treatment effect estimates:
Network Diagrams: Visualize the available evidence using standardized network diagrams with nodes proportional to sample size and edges proportional to the number of studies [15].
League Tables: Present all pairwise comparisons in a matrix format with point estimates and confidence/credible intervals.
Ranking Probabilities: Display treatment rankings and the probability that each treatment is the best, second best, etc., particularly when using Bayesian methods [15].
Uncertainty Visualization: Use forest plots, rankograms, or cumulative ranking curves to communicate uncertainty in treatment effects and rankings.
Reporting Guidelines and Standards
Comprehensive reporting of MTC studies should adhere to established guidelines and standards:
PRISMA Extension for Network Meta-Analysis: Provides specific guidance on reporting systematic reviews incorporating network meta-analyses.
ISPOR Task Force Reports: Offer recommendations on good methodological practices for indirect treatment comparisons and network meta-analysis [15] [30].
Clinical Interpretation: Frame results in the context of clinical decision-making, highlighting the strength of evidence, limitations, and implications for practice and policy.
The marked increase in published systematic reviews reporting MTCs since 2009 underscores the importance of this methodology for evidence-based healthcare decision-making [15]. As these methods continue to evolve and be applied to increasingly complex clinical questions, adherence to methodological standards and transparent reporting remains essential for generating trustworthy evidence to inform clinical practice and health policy.
Modern therapeutic development increasingly relies on evidence synthesis methodologies to determine the relative effectiveness of multiple interventions when head-to-head clinical trials are unavailable. Mixed Treatment Comparison (MTC) models, also known as Network Meta-Analysis (NMA), provide a powerful statistical framework for simultaneously comparing multiple treatments by combining both direct and indirect evidence across a network of randomized controlled trials. The validity and reliability of these analyses fundamentally depend on two interconnected pillars: comprehensive data requirements and robust network connectivity.
Building a robust evidence base requires careful consideration of the data types, model selection, and network properties that influence the credibility of treatment effect estimates. The CONSORT 2025 statement emphasizes that "readers should not have to infer what was probably done; they should be told explicitly," highlighting the critical importance of transparent reporting in research synthesis [31]. This technical guide examines the core components necessary for constructing defensible MTC models that can inform clinical and health technology assessment decisions, with particular focus on recent methodological advancements that address complex evidence structures in precision medicine and rare diseases.
Foundational Data Requirements for MTC Models
Data Types and Structures
MTC models can incorporate different levels of data, each with distinct advantages and limitations for evidence synthesis:
Aggregate Data (AD): Traditionally, meta-analyses utilize study-level summary statistics extracted from published trial reports. These data are typically presented as arm-level means and measures of variance for continuous outcomes, or event counts and sample sizes for binary outcomes. The primary limitation of AD is the potential for ecological bias, where relationships observed at the study level may not accurately reflect relationships at the individual level [19].
Individual Participant Data (IPD): IPD represents the gold standard for meta-analysis, consisting of raw data for each participant in the included trials. Access to IPD enables standardization of inclusion criteria, outcome definitions, and statistical methods across studies [19]. IPD facilitates more sophisticated analyses, including adjustment for prognostic factors and examination of treatment-covariate interactions at the individual level.
Hybrid Approaches: Emerging methodologies such as Multilevel Network Meta-Regression (ML-NMR) allow for the simultaneous incorporation of both IPD and AD within a single analytical framework [32]. This approach is particularly valuable when IPD is available for some trials but not others, enabling more comprehensive population adjustment across the evidence network.
Minimum Data Requirements
For each study included in an MTC, the following data elements should be systematically collected to ensure a robust analysis:
- Study identifiers: Citation information, trial registry number, and year of publication
- Patient characteristics: Baseline demographics, disease severity, and relevant comorbidities
- Intervention details: Treatment type, dosage, frequency, and duration
- Comparator information: Standard of care, placebo, or active control
- Outcome data: Primary and secondary endpoints with corresponding measures of variance
- Study design features: Randomization method, blinding approach, and follow-up duration
The CONSORT 2025 guidelines provide a comprehensive checklist of essential items that should be reported in clinical trials, which can serve as a valuable reference for data extraction in evidence synthesis [31].
Network Connectivity and Evidence Structures
Fundamentals of Evidence Networks
Network connectivity refers to the architecture of evidence linking multiple interventions through direct and indirect comparisons. A well-connected network allows for more precise estimation of relative treatment effects and strengthens the validity of MTC conclusions. The simplest network structure is a connected star where multiple interventions have all been compared directly to a common comparator such as placebo. More complex networks include multi-arm trials and partially connected meshes that provide multiple pathways for indirect comparison [32].
The strength of evidence for each treatment comparison depends on several factors:
- Number of studies contributing to each direct comparison
- Sample sizes of the contributing studies
- Methodological quality and risk of bias in the primary studies
- Consistency between direct and indirect evidence sources
Challenges with Mixed Populations and Precision Medicine
Modern therapeutic development, particularly in precision medicine, presents unique challenges for evidence synthesis. The identification of predictive biomarkers has resulted in clinical trials conducted in mixed biomarker populations across the drug development timeline [19]. For example, early trials may be conducted in all-comer populations, while later trials focus exclusively on biomarker-positive subgroups. This heterogeneity creates methodological challenges for traditional MTC models, which assume somewhat comparable populations across studies.
Several advanced methods have been developed to address these challenges:
- Meta-regression approaches that incorporate biomarker status as a covariate
- Hierarchical models that account for population differences across studies
- IPD network meta-analysis that enables subgroup analysis at the individual level
A recent methodological review identified eight distinct methods for evidence synthesis of mixed populations, categorized into those using aggregate data only, IPD only, or a combination of both [19].
Methodological Approaches to MTC
Contrast-Synthesis vs. Arm-Synthesis Models
Two broad statistical approaches are available for conducting MTCs, each with distinct theoretical foundations and implementation considerations:
Table 1: Comparison of Contrast-Synthesis and Arm-Synthesis Models for Network Meta-Analysis
| Feature | Contrast-Synthesis Models (CSM) | Arm-Synthesis Models (ASM) |
|---|---|---|
| Data Input | Relative treatment effects (e.g., log odds ratios, mean differences) | Arm-level summaries (e.g., log odds, means) |
| Theoretical Basis | Combines within-study relative effects, respecting randomization | Combines arm-level outcomes, then constructs relative effects |
| Key Advantage | Intuitive appeal through preservation of within-trial randomization | Ability to compute various estimands (e.g., marginal risk difference) |
| Limitation | Limited ability to adjust for effect modifiers | Potential compromise of randomization, requiring strong assumptions |
| Implementation | Frequentist or Bayesian frameworks | Primarily Bayesian frameworks |
Empirical evaluations comparing these approaches have found that different models can yield meaningfully different estimates of treatment effects and ranking metrics, potentially impacting clinical conclusions [33]. The choice between approaches should be pre-specified and justified based on the specific research question and evidence structure.
Advanced Methodological Extensions
Multilevel Network Meta-Regression (ML-NMR)
ML-NMR represents a significant methodological advancement that extends the NMA framework by allowing simultaneous incorporation of IPD and AD while maintaining population adjustment benefits [32]. This approach is particularly valuable when:
- The target population for decision-making differs materially from the trial populations
- IPD is available for one or more trials but not for all relevant trials
- Conventional matching methods introduce instability due to overfitting or lack of overlap
ML-NMR supports adjustment for effect modifiers across studies, even when IPD is not available for all studies, by modeling IPD treatment effects and integrating over the covariate distribution to create a probabilistic network model [32].
Synthesis Methods for Mixed Biomarker Populations
For targeted therapies where biomarker status modifies treatment effect, specialized methods have been developed:
- Aggregate Data Methods: Approaches that utilize only study-level data, potentially incorporating biomarker subgroup information when available
- IPD Methods: Approaches that utilize individual participant data to enable more nuanced analysis of treatment-effect modification
- Hybrid Methods: Approaches that combine both AD and IPD to leverage all available evidence
The selection of an appropriate method depends on the available data, the clinical context, and the specific decision problem being addressed [19].
Practical Implementation and Reporting Standards
Experimental Design and Analysis Workflow
The following diagram illustrates a comprehensive workflow for designing and analyzing mixed treatment comparisons, integrating multiple data sources and validation steps:
Statistical Software and Analytical Tools
Researchers have access to multiple statistical packages for implementing MTC models, each with different capabilities and requirements:
Table 2: Software Tools for Mixed Treatment Comparison Analysis
| Software Package | Synthesis Model | Framework | Key Features | Data Requirements |
|---|---|---|---|---|
| gemtc | Contrast-synthesis | Bayesian | Arm-based likelihood, random-effects models | Arm-level data |
| netmeta | Contrast-synthesis | Frequentist | Fixed and random-effects models, ranking metrics | Contrast-level data |
| pcnetmeta | Arm-synthesis | Bayesian | Probit link function, heterogeneous variances | Arm-level data |
| SynergyLMM | Specialized for combinations | Frequentist/Bayesian | Longitudinal analysis, time-resolved synergy scores | Individual-level tumor data |
For complex analyses such as ML-NMR, advanced statistical expertise in Bayesian frameworks and Markov Chain Monte Carlo (MCMC) simulation is typically required [32]. These methods are computationally demanding and often require custom programming beyond standard software packages.
Case Study Applications
Drug Combination Synergy Analysis
The SynergyLMM framework provides a comprehensive approach for evaluating drug combination effects in preclinical in vivo studies [34]. This method addresses several limitations of traditional combination analysis by:
- Accommodating complex experimental designs, including multi-drug combinations
- Providing time-resolved evaluation of synergy and antagonism patterns
- Incorporating longitudinal tumor growth measurements through mixed effects models
- Supporting multiple synergy reference models (Bliss independence, Highest Single Agent, Response Additivity)
In a reanalysis of published combination studies, SynergyLMM demonstrated how different synergy models can yield meaningfully different conclusions about the same drug combinations, highlighting the importance of model selection and transparent reporting [34].
Health Technology Assessment Applications
ML-NMR has been successfully applied in several health technology assessment contexts, particularly in oncology and rare diseases where trial data may be limited [32]. Notable applications include:
Acute Myeloid Leukemia (TA1013): An external advisory group for NICE recommended that a company produce an ML-NMR analysis instead of the original matching-adjusted indirect comparison, as it provided estimates more relevant to the NHS target population.
Non-Small Cell Lung Cancer (TA1030): A feasibility assessment determined that ML-NMR was not appropriate due to unsupported assumptions about shared effect modifiers, demonstrating the importance of preliminary methodological evaluation.
These case examples establish that HTA bodies are increasingly considering advanced evidence synthesis methods when conventional approaches are insufficient to address heterogeneity between trial populations.
Building a robust evidence base through mixed treatment comparisons requires meticulous attention to data requirements, network connectivity, and methodological appropriateness. As therapeutic development becomes increasingly complex, with targeted therapies and combination approaches, the evidence synthesis methods must evolve correspondingly.
The emerging generation of MTC methods, particularly those incorporating multilevel modeling and hybrid data structures, offers promising approaches for addressing the challenges of mixed populations and heterogeneous evidence networks. However, these advanced methods require greater technical expertise, computational resources, and transparent reporting to ensure their appropriate application and interpretation.
Researchers should carefully consider the specific decision context, available evidence base, and underlying assumptions when selecting an MTC approach. By adhering to methodological rigor and comprehensive reporting standards, evidence synthesis can provide reliable guidance for clinical and health policy decision-making in an increasingly complex therapeutic landscape.
I was unable to locate specific software tools, quantitative data, or experimental protocols for Mixed Treatment Comparison (MTC) models within the provided search results. The search primarily returned information on data visualization in R, color contrast accessibility, and other unrelated uses of the "MTC" acronym.
To find the information you need, I suggest the following steps:
- Use Precise Keywords: Try more specific search terms in academic databases such as
"network meta-analysis software","mixed treatment comparison modeling tools","Bayesian NMA software", or the names of known tools like"Gemtc","OpenBUGS","JAGS", or"WinBUGS". - Consult Specialized Resources: Focus your search on specialized sources like:
- Methodological Journals: For example, Research Synthesis Methods.
- Software Documentation: Official documentation and user guides for the specific tools mentioned above.
- Academic Repositories: Platforms like GitHub for code and implementation examples.
I hope these suggestions help you locate the necessary technical details for your research. If you find a specific tool or method and need help with its implementation details, please feel free to ask a new question.
Estimates of relative efficacy between alternative treatments are crucial for decision-making in health care. Mixed Treatment Comparison (MTC) models, also known as network meta-analysis, provide a powerful methodology to obtain such estimates when head-to-head evidence is not available or insufficient [35] [30]. This approach allows for the simultaneous synthesis of evidence of all pairwise comparisons across more than two interventions, enabling researchers to compare treatments that have never been directly evaluated in clinical trials [30].
The core strength of MTC lies in its ability to integrate both direct evidence (from head-to-head trials) and indirect evidence (when treatments are connected through a common comparator) within a single analytical framework [30]. When at least one pair of treatments is compared both directly and indirectly—forming a "closed loop"—this statistical approach becomes particularly valuable for generating comprehensive treatment hierarchies and informing healthcare decisions [30].
This technical guide explores the application of MTC methodologies across two distinct clinical domains: nutritional interventions for sarcopenia and therapeutic strategies in oncology. Through these case studies, we demonstrate how MTC models can address complex evidence synthesis challenges while highlighting domain-specific methodological considerations.
Sarcopenia Nutrition: Synthesizing Evidence from Heterogeneous Interventions
Clinical Context and Methodological Challenges
Sarcopenia is a syndrome characterized by progressive and generalized loss of skeletal muscle mass and strength, associated with physical disability, decreased quality of life, and increased mortality [36]. While primary sarcopenia relates to aging, secondary sarcopenia can affect individuals of all ages and may result from various factors including cancer, malnutrition, endocrine disorders, and inflammatory states [36]. In oncology, secondary sarcopenia is particularly prevalent among patients undergoing chemotherapy, with loss of muscle mass significantly predicting lower treatment toxicities and complications during adjuvant chemotherapy [37].
The challenge in evaluating sarcopenia interventions lies in the heterogeneity of approaches, including resistance exercise, nutritional support, and combined interventions, each measured using different outcomes (skeletal muscle mass, lean body mass) across studies with varying designs and populations [37].
Case Study: Network Meta-Analysis of Sarcopenia Interventions
A systematic review and meta-analysis investigating interventions for sarcopenia in cancer patients receiving chemotherapy provides an illustrative example [37]. This analysis included six studies focusing on exercise and/or nutrition interventions, with four cancer types represented (breast cancer being most common at 50%). Participants' mean age was 53.44 years, with intervention times varying from 3 weeks to 6 months.
Table 1: Characteristics of Sarcopenia Interventions Included in Meta-Analysis
| Intervention Type | Number of Studies | Effect on Skeletal Muscle Mass (Mean Difference) | Effect on Lean Body Mass (Mean Difference) |
|---|---|---|---|
| Resistance Exercise Only | 1 | 0.168 (95% CI: -0.015–0.352, P=0.072) | -0.014 (95% CI: -1.291–1.264, P=0.983) |
| Combined Exercise and Nutrition | 4 | 0.168 (95% CI: -0.015–0.352, P=0.072) | -0.014 (95% CI: -1.291–1.264, P=0.983) |
| Nutrition Only | 1 | 0.168 (95% CI: -0.015–0.352, P=0.072) | -0.014 (95% CI: -1.291–1.264, P=0.983) |
The analysis demonstrated a trend toward significantly increasing skeletal muscle mass after intervention across all approaches, with no significant changes in lean body mass [37]. Notably, resistance exercise and combined exercise and nutrition interventions proved more effective at preserving or increasing muscle mass compared to nutrition-only approaches [37].
Methodological Protocol for Sarcopenia Intervention MTC
For researchers conducting MTC in sarcopenia nutrition, the following protocol is recommended:
Systematic Search Strategy: Implement a comprehensive search across MEDLINE via PubMed, Scopus, CINAHL Plus, and Embase using MeSH terms and keywords including "low muscle mass," "sarcopenia," "skeletal muscle mass," "muscular atrophy," combined with "exercise," "physical activity," "diet," "nutrition intervention," "neoplasms," "cancer," "oncology," and "chemotherapy" [37].
Study Selection Criteria: Apply predetermined inclusion criteria: (a) primary original research in peer-reviewed journals; (b) study sample of cancer patients undergoing chemotherapy; (c) inclusion of exercise and/or nutrition intervention; (d) English-language articles [37].
Quality Assessment: Utilize NIH quality assessment tools appropriate to study design (Quality Assessment of Controlled Intervention Studies, Quality Assessment of Case-Control Studies, or Quality Assessment Tool for Before-After Studies with No Control Group) with ratings of good, fair, or poor based on risk of bias [37].
Data Extraction and Analysis: Collect data on sample characteristics, intervention type and duration, and muscle mass measurements. Calculate effect sizes and 95% confidence intervals using appropriate statistical software (e.g., Stata). Assess heterogeneity using I² statistic and Cochran's Q statistics, with I² >50% and P <0.1 indicating substantial heterogeneity. Apply random effects models to estimate overall intervention effects [37].
The following diagram illustrates the sarcopenia intervention workflow from assessment to treatment:
Diagram 1: Sarcopenia Assessment and Intervention Workflow
Cancer Therapeutics: Advanced Applications of MTC in Oncology
Methodological Evolution in Oncology Evidence Synthesis
In oncology, comparative effectiveness research faces unique challenges, including rapidly evolving treatment landscapes, biomarker-defined subgroups, and ethical limitations in conducting head-to-head trials of all available regimens. Matching-Adjusted Indirect Comparisons (MAIC) and other advanced MTC methods have emerged as crucial methodologies when cross-trial heterogeneity exists or only single-arm trials are available [38].
A recent scoping review of MAIC studies in oncology revealed that 72% were unanchored, with an average of 1.9 comparisons per study [38]. The review identified significant reporting gaps, with only 3 of 117 MAICs fulfilling all National Institute for Health and Care Excellence (NICE) recommendations, highlighting the need for more rigorous methodological standards [38].
Case Study: Network Meta-Analysis in Pancreatic Cancer
The application of NMA in pancreatic cancer management demonstrates the methodology's utility in synthesizing evidence across complex treatment networks [39]. One analysis included 9 trials involving 1,294 patients considering 12 different treatments for unresectable locally advanced non-metastatic pancreatic cancer (LAPC), with overall survival as the primary outcome [39].
Table 2: Network Meta-Analysis of Treatments for Locally Advanced Pancreatic Cancer
| Treatment Category | Number of Studies | Patients | Outcome Measures | Reference Treatment |
|---|---|---|---|---|
| Chemotherapy | 9 | 1,294 | Overall Survival (HR) | Gemcitabine |
| Chemoradiotherapy | 9 | 1,294 | Overall Survival (HR) | Gemcitabine |
| Combination Therapy | 9 | 1,294 | Overall Survival (HR) | Gemcitabine |
| Biological Therapies | 9 | 1,294 | Overall Survival (HR) | Gemcitabine |
The analysis utilized Bayesian statistical principles with fixed effects models created in WinBUGS 14, as random effects models could not be run due to no two trials in the NMA comparing the same interventions [39]. For overall survival and progression-free survival, the log hazard ratio for each trial comprised a normal likelihood, while objective response was modeled using a binomial likelihood with a logit link function [39].
Methodological Protocol for Oncology MTC
For researchers conducting MTC in oncology, the following advanced methodologies are recommended:
MAIC Implementation: When conducting Matching-Adjusted Indirect Comparisons, adhere to NICE recommendations including adjustment for all effect modifiers and prognostic variables (for unanchored MAICs), providing evidence of effect modifier status, and reporting distribution of weights [38]. Consider "two-stage MAIC" for improved precision and efficiency while maintaining low levels of bias [40].
Biomarker-Stratified Analysis: For targeted therapies, employ methods for synthesis of data from mixed biomarker populations. These include approaches using aggregate data only, individual participant data only, or a combination of both [41]. When possible, utilize individual participant data to adjust for relevant prognostic factors and standardize analysis at the trial-level [41].
Mathematical Modeling Integration: Incorporate mathematical frameworks to compare treatment strategies, such as intermittent versus continuous adaptive chemotherapy dosing [42]. These models can formally analyze intermittent adaptive therapy in the context of bang-bang control theory and prove that continuous adaptive therapy maximizes time to resistant subpopulation outgrowth relative to intermittent approaches [42].
The following diagram illustrates the MTC workflow for cancer therapeutics:
Diagram 2: MTC Workflow for Cancer Therapeutics
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for MTC Implementation
| Research Tool | Function | Application Context |
|---|---|---|
| WinBUGS 14 | Bayesian analysis software for hierarchical models | Implementation of Bayesian NMA models for time-to-event outcomes [39] |
| Stata Statistical Software | Data analysis and statistical software | Calculation of effect sizes, confidence intervals, and random effects models [37] |
| NIH Quality Assessment Tools | Standardized quality and risk of bias assessment | Evaluation of controlled interventions, case-control, and before-after studies [37] |
| Individual Participant Data (IPD) | Raw patient-level data from clinical trials | Enhanced adjustment for prognostic factors and standardization of analysis [41] |
| Aggregate Data (AD) | Trial-level summary data | Traditional meta-analysis when IPD is unavailable [41] |
| PRISMA Guidelines | Systematic review reporting standards | Ensuring comprehensive reporting of systematic reviews and meta-analyses [37] |
| dCNP | dCNP, CAS:618-80-4, MF:C6H3Cl2NO3, MW:208.00 g/mol | Chemical Reagent |
The application of Mixed Treatment Comparison models across diverse clinical domains—from sarcopenia nutrition to cancer therapeutics—demonstrates their versatility in addressing complex evidence synthesis challenges. As precision medicine continues to evolve, with increasing emphasis on biomarker-defined subgroups and targeted therapies, methodologies for synthesizing evidence from mixed populations will become increasingly important [41].
Future methodological development should focus on enhancing the robustness of approaches like Matching-Adjusted Indirect Comparisons, improving adherence to reporting standards, and integrating mathematical modeling frameworks to address dynamic treatment questions such as adaptive therapy dosing [38] [42]. Through continued refinement and rigorous application, MTC methodologies will remain indispensable tools for generating comparative effectiveness evidence to inform healthcare decision-making across diverse clinical contexts.
Overcoming Challenges in MTC: Addressing Heterogeneity, Inconsistency, and Complex Data
Assessing and Managing Heterogeneity and Inconsistency in Networks
Network meta-analysis (NMA) is an advanced statistical technique that enables the simultaneous comparison of multiple interventions by combining direct evidence from head-to-head randomized controlled trials (RCTs) with indirect evidence obtained through common comparators [43]. This methodology extends beyond conventional pairwise meta-analysis, allowing for the estimation of relative treatment effects between interventions that have never been directly compared in clinical trials and providing more precise estimates for existing comparisons [44] [14]. The validity of NMA depends critically on two fundamental principles: transitivity (the underlying clinical and methodological assumption) and coherence (also called inconsistency, its statistical manifestation) [44] [43]. Understanding, assessing, and managing these elements is paramount for producing reliable NMA results that can confidently inform clinical and policy decisions.
Transitivity requires that the different sets of studies included in an NMA are similar, on average, in all important factors that may affect relative treatment effects [44]. In practical terms, this means that in a hypothetical RCT including all treatments in the network, participants could theoretically be randomized to any of the interventions [43]. Violations of transitivity (intransitivity) occur when studies comparing different interventions differ systematically with respect to effect modifiers—characteristics that influence the size of treatment effects [44]. Coherence/inconsistency refers to the statistical disagreement between different sources of evidence within a network, specifically when direct and indirect estimates for the same comparison yield meaningfully different results [44].
The Transitivity Assumption: Clinical and Methodological Foundations
Theoretical Basis of Transitivity
The transitivity assumption underpins the validity of indirect comparisons and NMA. Mathematically, the relationship can be expressed as follows for a simple ABC network: Δ̂BC​ = Δ̂AC​ - Δ̂AB​, where Δ̂BC​ represents the indirect estimate comparing B and C, while Δ̂AC​ and Δ̂AB​ are the direct estimates comparing A to C and A to B, respectively [44]. This mathematical relationship holds only if the studies forming the direct comparisons are sufficiently similar in all important characteristics other than the interventions being compared.
The transitivity assumption implies three key conditions must be met [44] [43]:
- Clinical Similarity: The studies included for different comparisons should involve similar patient populations in terms of demographic characteristics, disease severity, and comorbidities that may modify treatment effects.
- Methodological Similarity: Studies across different comparisons should have comparable designs, including similar risk of bias, outcome definitions, and follow-up durations.
- Conceptual Consistency: The interventions being compared should be part of a coherent treatment strategy for the same clinical question, rather than representing approaches used in fundamentally different clinical scenarios.
Assessment Protocol for Transitivity
Systematic reviewers should implement the following structured protocol to assess transitivity:
Table 1: Protocol for Assessing Transitivity in Network Meta-Analysis
| Assessment Phase | Key Activities | Documentation Output |
|---|---|---|
| 1. A Priori Planning | - Identify potential effect modifiers based on clinical knowledge and prior literature- Specify these in the study protocol- Define acceptable ranges for each modifier | Pre-specified analysis plan with hypothesized effect modifiers |
| 2. Data Collection | - Systematically extract data on potential effect modifiers from all included studies- Document population characteristics, intervention details, and study methodology | Structured table of study characteristics stratified by comparison |
| 3. Qualitative Evaluation | - Compare the distribution of effect modifiers across different treatment comparisons- Assess whether systematic differences exist that could bias indirect comparisons | Summary assessment of clinical and methodological similarity |
| 4. Quantitative Exploration | - Conduct meta-regression or subgroup analyses to examine treatment-effect interactions- Evaluate whether treatment effects vary according to identified effect modifiers | Statistical analysis of potential effect modification |
The following workflow diagram illustrates the sequential process for transitivity assessment:
Common Scenarios Violating Transitivity
Several clinical scenarios commonly violate the transitivity assumption and warrant careful consideration:
- Treatment Sequences and Lines of Therapy: In chronic conditions like glaucoma, first-line monotherapies and combination therapies used in treatment-resistant cases should not be included in the same NMA, as they apply to fundamentally different patient populations [43].
- Biomarker-Directed Therapies: In oncology, treatments targeting specific biomarkers (e.g., HER2-positive breast cancer) and those for biomarker-negative disease represent distinct populations that cannot be validly compared through NMA [43].
- Disease Severity Stratification: Interventions may demonstrate different effect profiles across disease severity spectra. Including studies with markedly different baseline severity across comparisons may violate transitivity.
- Contextual Factors: Settings with substantially different healthcare delivery systems, companion treatments, or expertise levels may introduce intransitivity when compared indirectly.
Statistical Incoherence: Detection and Analysis Methods
Conceptual Relationship Between Heterogeneity and Incoherence
In NMA, heterogeneity refers to the variability in treatment effects between studies within the same direct comparison, while incoherence (inconsistency) refers to the disagreement between direct and indirect evidence for the same treatment comparison [44]. These concepts are hierarchically related: heterogeneity exists within direct comparisons, while incoherence exists between different types of evidence (direct vs. indirect) for the same comparison. The presence of substantial heterogeneity within direct comparisons may signal potential incoherence in the network.
Methodological Framework for Incoherence Assessment
A comprehensive approach to assessing incoherence involves multiple statistical techniques:
Table 2: Methods for Assessing Incoherence in Network Meta-Analysis
| Method | Description | Application Context | Interpretation |
|---|---|---|---|
| Global Methods | |||
| Design-by-Treatment Interaction | Assesses incoherence across the entire network by comparing consistent and inconsistent models | Networks with multiple independent loops | Significant p-value indicates overall incoherence |
| Q statistic-based approaches | Decomposes total heterogeneity into within-design and between-design components | All network geometries | Large between-design component suggests incoherence |
| Local Methods | |||
| Node Splitting | Separately estimates direct and indirect evidence for each comparison and assesses their difference | Focused assessment of specific comparisons | Significant difference indicates local incoherence |
| Loop-specific Approach | Evaluates incoherence in each closed loop by calculating the difference between direct and indirect evidence | Networks with closed loops | Incoherence factor (IF) > 0 suggests incoherence |
| Side-splitting Method | Compares direct evidence with mixed (network) evidence for each comparison | All connected comparisons | Disagreement suggests local incoherence |
The following diagram illustrates the primary statistical approaches for incoherence evaluation:
Practical Protocol for Incoherence Evaluation
Implement the following stepwise protocol to comprehensively evaluate incoherence:
Visual Network Inspection: Begin by creating a network diagram to identify potential hotspots for incoherence, particularly in densely connected areas with multiple evidence sources [44] [43].
Global Incoherence Assessment:
- Apply the design-by-treatment interaction model using Bayesian or frequentist frameworks.
- Interpret the p-value or Bayesian credibility intervals to determine global statistical significance.
- Calculate the overall I² for inconsistency to quantify its magnitude.
Local Incoherence Investigation:
- Implement node-splitting methods for each comparison with both direct and indirect evidence.
- Calculate incoherence factors (IF) for each closed loop: IF = |ddirect - dindirect| with variance Var(IF) = Var(ddirect) + Var(dindirect) [44].
- Assess statistical significance using z-tests with appropriate multiple testing corrections.
Exploratory Analyses:
- Conduct sensitivity analyses excluding studies at high risk of bias.
- Perform meta-regression to investigate whether specific effect modifiers explain observed incoherence.
- Use subgroup analyses to explore clinical hypotheses regarding sources of incoherence.
Management Strategies for Heterogeneity and Incoherence
Analytical Approaches to Address Heterogeneity
When substantial heterogeneity is detected, consider these analytical strategies:
- Random-Effects Models: Incorporate between-study heterogeneity into the analysis, typically assuming a common heterogeneity variance across comparisons, particularly when few studies exist per comparison [43].
- Meta-Regression: Adjust for continuous or categorical effect modifiers to explain heterogeneity, though this requires adequate study-level data and statistical power.
- Subgroup Analysis: Conduct separate analyses for clinically distinct populations, though this may fragment the network and reduce connectivity.
- Adjusted Analyses: Implement methods like matching-adjusted indirect comparisons (MAIC) when individual patient data are available for some studies [3].
Strategies for Managing Incoherence
When incoherence is detected, implement these management strategies:
Source Investigation: Trace the origin of incoherence by examining clinical and methodological characteristics of studies contributing to problematic comparisons.
Network Fragmentation: Consider separating the network into clinically coherent subgroups when fundamental transitivity violations are identified.
Inconsistency Modeling: Use specialized models that explicitly account for inconsistency, such as inconsistency factors or unrelated mean effects models.
Sensitivity Analysis: Report both consistent and inconsistent models to demonstrate the robustness (or lack thereof) of treatment effect estimates.
Evidence Grading: Downgrade the confidence in estimates derived from incoherent comparisons when using GRADE for NMAs [44] [14].
Reporting and Interpretation Guidelines
Transparent reporting of heterogeneity and incoherence assessments is essential for NMA credibility:
- Clearly document all pre-specified assessments of transitivity and potential effect modifiers.
- Present both global and local assessments of incoherence with appropriate test statistics and p-values.
- Report heterogeneity estimates (τ² or I²) for each direct comparison and the network overall.
- Use league tables and forest plots that explicitly flag comparisons with detected incoherence.
- Acknowledge limitations and interpret results cautiously when substantial heterogeneity or incoherence persists despite adjustment attempts.
Essential Methodological Toolkit
Statistical Software and Packages
Implementing these assessments requires appropriate statistical software:
Table 3: Essential Software Tools for Heterogeneity and Incoherence Assessment
| Software Platform | Key Packages/Functions | Primary Application | Access Method |
|---|---|---|---|
| R | netmeta, gemtc, pcnetmeta |
Comprehensive NMA with incoherence assessment | Open source |
| Stata | network, mvmeta |
NMA with meta-regression capabilities | Commercial |
| WinBUGS/OpenBUGS | Custom Bayesian models | Flexible Bayesian NMA with inconsistency modeling | Open source |
| JAGS | Custom Bayesian models | Bayesian analysis alternative to BUGS | Open source |
| SAS | PROC NLMIXED, PROC MCMC |
Advanced Bayesian and frequentist NMA | Commercial |
Conceptual Framework for Method Selection
The following diagram illustrates the decision process for selecting appropriate methods based on network characteristics:
Proper assessment and management of heterogeneity and inconsistency are fundamental to producing valid and reliable network meta-analyses. By implementing systematic protocols for evaluating transitivity, applying appropriate statistical tests for incoherence, and employing strategic management approaches when issues are detected, researchers can enhance the credibility of their NMA findings. The methodological toolkit presented here provides a comprehensive framework for addressing these challenges throughout the NMA process, from protocol development to result interpretation. As NMA methodology continues to evolve, future developments will likely provide more sophisticated approaches for handling these complex issues, particularly in scenarios with limited data or complex network structures.
Advanced Techniques for Synthesis with Mixed Biomarker Populations
The advancement of precision medicine has fundamentally altered the landscape of clinical trials, leading to the identification of predictive genetic biomarkers and resulting in trials conducted in mixed biomarker populations [19]. Early-phase trials may be conducted in patients with any biomarker status without subgroup analysis, later trials may include subgroup analyses based on biomarker status, and contemporary trials often focus exclusively on biomarker-positive patients [19]. This heterogeneity creates significant challenges for traditional meta-analysis methods, which rely on the assumption of comparable populations across studies. Mixed Treatment Comparison (MTC) models, also known as network meta-analysis, provide a methodological framework for synthesizing such complex evidence structures, enabling researchers to compare multiple treatments simultaneously while respecting the randomization in the evidence [30] [2].
The fundamental challenge arises because predictive biomarkers create treatment effects that depend on the biomarker status of the patient [19]. For example, in metastatic colorectal cancer, retrospective analysis revealed that patients with KRAS mutations did not achieve improved survival when treated with EGFR-targeted therapies compared to chemotherapy, leading to a shift in clinical practice and subsequent trials focusing exclusively on KRAS wild-type patients [19]. This evolution in the evidence base necessitates specialized methodological approaches that can accommodate mixed populations while providing clinically meaningful estimates for specific biomarker subgroups.
Methodological Foundations
Core Concepts and Terminology
Mixed Treatment Comparison (MTC) refers to a statistical approach used to analyze a network of evidence with more than two interventions where at least one pair of interventions is compared both directly and indirectly [30]. This approach allows for the simultaneous synthesis of all pairwise comparisons across more than two interventions, forming what is known as a network meta-analysis [30]. When a comparison has both direct evidence (from head-to-head trials) and indirect evidence (via a common comparator), this forms a closed loop in the evidence network, enabling more robust effect estimation [30].
The key challenge in mixed biomarker populations involves synthesizing evidence from trials with different designs: those conducted in biomarker-positive populations only, those in biomarker-negative populations only, and those in mixed populations with or without subgroup analyses [19]. Traditional meta-analysis assumes that underlying treatment effects are either identical (fixed-effect models) or come from a common normal distribution (random-effects models), but this assumption becomes problematic when biomarker status modifies treatment effects [19].
Foundational Meta-Analysis Methods
Before addressing mixed biomarker populations specifically, it is essential to understand standard meta-analytic methods upon which advanced techniques build. Aggregate data meta-analysis (ADMA) can be conducted using either fixed-effect or random-effects models [19]. Fixed-effect models assume that observed treatment effects across studies differ only due to random error around a common underlying "true" effect, while random-effects models allow the true treatment effects to vary across studies, assuming they come from a common distribution [19].
Meta-regression extends these approaches by explicitly modeling heterogeneity across subgroups or covariate values, using a treatment-covariate interaction term to show the effect of a covariate on the treatment effect [19]. However, meta-regression has limitations, including potential ecological bias, difficulty in interpretation without a wide range of covariate values across studies, and challenges with robust conclusions when few studies are available [19].
The gold standard for evidence synthesis is individual participant data meta-analysis (IPDMA), which can be conducted using one-stage or two-stage approaches [19]. The two-stage approach first analyzes IPD from each trial separately to obtain treatment effect estimates, then combines these in a second stage similar to conventional ADMA. The one-stage model analyzes IPD from all studies simultaneously using a hierarchical regression model, allowing for standardization of analyses across studies and more sophisticated modeling of biomarker-treatment interactions [19].
Table 1: Foundational Meta-Analysis Methods for Mixed Populations
| Method Type | Data Requirements | Key Advantages | Key Limitations |
|---|---|---|---|
| Aggregate Data (AD) Meta-Analysis | Study-level summary data | Accessibility, simplicity | Cannot adjust for individual-level covariates |
| Meta-Regression | Study-level summary data with covariates | Can explore sources of heterogeneity | Ecological bias, requires many studies |
| Two-Stage IPD Meta-Analysis | Individual participant data | Standardization across studies, subgroup analyses | Complex data collection, longer timelines |
| One-Stage IPD Meta-Analysis | Individual participant data | Maximum flexibility, complex modeling | Computational complexity, data accessibility |
Advanced Techniques for Mixed Biomarker Populations
Methodological Framework and Classification
Methodological research has identified eight distinct methods for evidence synthesis of mixed biomarker populations, which can be categorized into three primary groups: methods using aggregate data (AD) only, methods using individual participant data (IPD) only, and hybrid methods using both AD and IPD [19]. Each approach offers distinct advantages and limitations, with IPD-based methods generally achieving superior statistical properties at the expense of data accessibility [19].
The fundamental challenge these methods address is combining evidence from trials with different biomarker population designs to estimate treatment effects in specific biomarker subgroups. This requires making assumptions about the relationship between treatment effects in different populations and appropriately weighting direct and indirect evidence [19]. The selection of the most appropriate methodological framework depends critically on the decision context, available data, and specific research questions [19].
Table 2: Advanced Techniques for Mixed Biomarker Population Synthesis
| Method Category | Applicability | Number of Identified Methods | Key Considerations |
|---|---|---|---|
| Aggregate Data (AD) Methods | Pairwise meta-analysis | 3 | Relies on published subgroup analyses |
| AD Network Meta-Analysis | Network meta-analysis | 3 | Incorporates indirect comparisons |
| IPD-AD Hybrid Methods | Network meta-analysis | 2 | Combines IPD precision with AD breadth |
Aggregate Data Methods for Pairwise Meta-Analysis
For pairwise meta-analysis using aggregate data, three primary methods have been identified [19]. These approaches utilize published subgroup analyses from trials conducted in mixed populations, combining these with results from trials conducted exclusively in biomarker-positive or biomarker-negative populations. The simplest approach involves standard random-effects meta-analysis of subgroup estimates, but this may not adequately account for correlations between subgroup effects within trials or differences in the precision of subgroup estimates [19].
More sophisticated AD methods incorporate trial-level covariates indicating the proportion of biomarker-positive patients or use meta-regression with biomarker status as an effect modifier. These approaches require careful consideration of the potential for ecological bias, where trial-level relationships between biomarker prevalence and treatment effects may not reflect individual-level relationships [19]. Additionally, the availability and quality of subgroup analyses in published trial reports often limit the application of these methods.
Network Meta-Analysis Methods for Mixed Populations
For network meta-analysis of mixed biomarker populations, three aggregate data methods and two hybrid IPD-AD methods have been developed [19]. These approaches extend standard network meta-analysis to accommodate trials with different biomarker population designs, enabling simultaneous comparison of multiple treatments while accounting for biomarker status.
The AD network meta-analysis methods incorporate biomarker status as a trial-level characteristic, either through network meta-regression or by stratifying the evidence network by biomarker status. These methods can provide estimates of treatment effects for different biomarker subgroups while borrowing strength across the entire network of evidence [19]. The hybrid IPD-AD approaches combine individual participant data from some trials with aggregate data from others, maximizing the use of available evidence while maintaining the advantages of IPD for modeling biomarker-treatment interactions [19].
Figure 1: Methodological Framework for Mixed Biomarker Evidence Synthesis
Implementation and Applied Protocols
Data Preparation and Network Structure
The initial step in implementing MTC for mixed biomarker populations involves preparing the data and mapping the evidence network [2]. For the illustrative example in metastatic colorectal cancer, treatments must be consistently categorized, and comparisons formed such that the comparator treatment has a lower numerical value than the experimental treatment [2]. To ensure consistency, it may be necessary to use the inverse of reported relative risks when treatments are entered in the opposite direction [2].
The evidence network should be visualized to identify all available direct comparisons and potential pathways for indirect comparisons. Each treatment in the network is assigned a numerical identifier, and connections between treatments represent direct comparisons available from trials [2]. The network must be connected, meaning there is a route between each treatment and all others through direct or indirect comparisons [2]. In mixed biomarker populations, this network structure may need to be developed separately for different biomarker subgroups or expanded to include biomarker status as a node in the network.
Statistical Analysis and Modeling Approaches
The statistical analysis of mixed biomarker populations can be implemented using either fixed-effect or random-effects models, with the choice depending on the degree of heterogeneity anticipated between studies [2]. When substantial heterogeneity is present, random-effects models are generally preferred as they account for between-study variation in treatment effects [19].
The core MTC model extends standard random-effects meta-analysis to multiple treatment comparisons. For a network with i treatments, the model specifies that the estimated treatment effect δ̂ᵢ for each study is normally distributed around the true treatment effect δᵢ with within-study variance σᵢ² [19]. The true treatment effects δᵢ are then assumed to come from a common normal distribution with mean d and between-study variance τ² [19]. In Bayesian implementations, prior distributions are required for d and τ [19].
For mixed biomarker populations, this basic model is extended to incorporate biomarker status as an effect modifier. This can be achieved through meta-regression, with the model specifying that δᵢ ~ N(α + βzᵢ, τ²), where zᵢ is the trial-level covariate for biomarker status and β gives the interaction between biomarker status and treatment effect [19].
Figure 2: Implementation Workflow for MTC in Mixed Biomarker Populations
Assessment of Consistency and Model Fit
A critical step in MTC is assessing the consistency between direct and indirect evidence [2]. Methods based on the Bucher approach can be used to compare direct estimates of treatment effects with indirect estimates obtained through other comparisons in the network [2]. A composite test of inconsistency can be applied to test the null hypothesis of no difference between all available estimates [2].
When summary relative risks based on fixed-effect meta-analyses show significant inconsistency, those based on random-effects meta-analyses may demonstrate better consistency and form a more reliable basis for decision-making [2]. Model fit can be assessed using measures such as residual deviance and the deviance information criterion (DIC) in Bayesian analyses, with better-fitting models having lower values [2].
Analytical Tools and Research Reagents
Statistical Software and Computational Tools
Implementation of advanced synthesis methods for mixed biomarker populations requires specialized statistical software. Bayesian approaches are commonly implemented using Markov Chain Monte Carlo (MCMC) methods in software such as OpenBUGS, JAGS, or Stan [19] [2]. These environments allow for flexible model specification and can handle the complex hierarchical structures required for MTC models.
Frequentist approaches can be implemented using generalized linear mixed models in standard statistical packages such as R or SAS [30]. The R package netmeta provides specialized functions for network meta-analysis, including tools for network visualization and inconsistency assessment [2]. For IPD meta-analysis, both one-stage and two-stage approaches can be implemented using mixed-effects models in R, SAS, or Stata [19].
Table 3: Essential Research Reagents for Mixed Biomarker Synthesis
| Tool Category | Specific Tools | Primary Function | Application Context |
|---|---|---|---|
| Statistical Software | OpenBUGS, JAGS, Stan | Bayesian MCMC estimation | Complex hierarchical models |
| Statistical Packages | R (netmeta), SAS | Frequentist estimation | Standard network meta-analysis |
| Data Management Tools | MATLAB, Python | Data preprocessing | Handling large IPD datasets |
| Visualization Tools | R (ggplot2), Shiny apps | Results communication | Dynamic visualization of trends |
Data Standardization and Quality Assessment Tools
Successful implementation of MTC for mixed biomarker populations requires careful attention to data standardization and quality assessment. For aggregate data methods, tools for assessing risk of bias in included studies, such as the Cochrane Risk of Bias tool, are essential [19]. For IPD methods, additional tools are needed to standardize variable definitions across studies and handle missing data appropriately.
Visualization tools play a crucial role in understanding complex evidence networks and temporal trends in mixed populations. Dynamic visualization approaches, such as those implemented in Shiny applications in R, can help monitor the evolution of treatment effects over time and identify outliers in the evidence base [45]. These tools can track pairwise distances between study results via line graphs, create dynamic box plots to identify studies with minimum or maximum disparities, and visualize studies that are systematically far from others using proximity plots [45].
Applications and Illustrative Examples
Case Study: Metastatic Colorectal Cancer
The application of advanced synthesis methods to mixed biomarker populations is illustrated by research in metastatic colorectal cancer (mCRC) [19]. The development of EGFR-targeted therapies (cetuximab and panitumumab) created an evidence base consisting of trials with mixed populations: some investigating KRAS wild-type and mutant patients with no subgroup analysis, some with subgroup analysis, and some investigating only KRAS wild-type patients [19].
Applying MTC methods to this evidence base allowed researchers to synthesize all available evidence while accounting for differences in biomarker status across trials. The results provided coherent estimates of treatment effects in specific biomarker subgroups, supporting clinical decision-making for patients with different KRAS status [19]. This case study highlights the practical value of these methods for addressing evolving evidence bases in precision medicine.
Case Study: Childhood Nocturnal Enuresis
An early application of MTC methods to an overview of reviews for childhood nocturnal enuresis demonstrated how these approaches can provide a single coherent analysis of all treatment comparisons and check for evidence consistency [2]. The original overview presented summary estimates from seven separate systematic reviews of ten treatments but lacked a coherent framework for deciding which treatment to use [2].
Application of MTC methods revealed that summary relative risks based on fixed-effect meta-analyses were highly inconsistent, while those based on random-effects meta-analyses were consistent and could form a basis for coherent decision-making [2]. This example illustrates how MTC can overcome limitations of traditional narrative approaches to evidence synthesis when multiple treatments are available.
Figure 3: Clinical Application Workflow for Biomarker-Informed MTC
Future Directions and Methodological Innovations
AI-Driven Biomarker Discovery and Validation
Emerging methodologies are leveraging artificial intelligence and contrastive learning to discover predictive biomarkers in an automated, systematic, and unbiased manner [46]. These AI-driven frameworks can explore tens of thousands of clinicogenomic measurements to identify biomarkers that predict response to specific treatments, particularly in complex fields like immuno-oncology [46].
Application of these approaches to real clinicogenomic datasets has demonstrated the potential to retrospectively contribute to phase 3 clinical trials by uncovering predictive, interpretable biomarkers based solely on early study data [46]. Patients identified using such AI-discovered predictive biomarkers have shown significant improvements in survival outcomes compared to those in the original trials [46]. These methodologies represent a promising direction for enhancing the precision and personalization of evidence synthesis in mixed biomarker populations.
Integrated Modeling Approaches
The future of evidence synthesis in mixed biomarker populations lies in integrated modeling approaches that simultaneously incorporate biomarkers, survival outcomes, and safety data [47]. These model-based approaches, including population pharmacokinetic-pharmacodynamic modeling, have become essential components in clinical phases of oncology drug development [47].
Over the past two decades, models have evolved to describe the temporal dynamics of biomarkers and tumor size, treatment-related adverse events, and their links to survival [47]. Integrated models that incorporate at least two pharmacodynamic/outcome variables are increasingly applied to answer drug development questions through simulations, supporting the exploration of alternative dosing strategies and study designs in subgroups of patients or other tumor indications [47]. These pharmacometric approaches are expected to expand further as regulatory authorities place additional emphasis on early and individualized dosage optimization [47].
Dynamic Visualization and Monitoring
Future methodological developments will likely include enhanced approaches for dynamic mixed data analysis and visualization [45]. These protocols integrate robust distances and visualization techniques for tracking the evolution of evidence over time, particularly important as biomarker definitions and measurement technologies evolve [45].
Novel visualization tools include tracking the evolution of pairwise distances via line graphs, dynamic box plots for identifying studies with minimum or maximum disparities, proximity plots for detecting studies that are systematically far from others, and dynamic multiple multidimensional scaling maps for analyzing the evolution of inter-distances between studies [45]. These approaches facilitate the monitoring of evidence consistency and heterogeneity over time, providing valuable insights for maintaining the validity of synthesis results as new evidence emerges.
Handling Sparse Data, Multi-Arm Trials, and Zero Cells
Mixed Treatment Comparison (MTC) models, also known as network meta-analysis (NMA), have revolutionized evidence synthesis by enabling simultaneous comparison of multiple treatments, even when direct head-to-head evidence is lacking [15]. The application of these methods has grown exponentially since 2009, with their results increasingly informing healthcare policy and clinical decision-making [15]. However, the validity and reliability of MTC findings are heavily dependent on appropriate handling of specific methodological challenges, particularly sparse data, multi-arm trials, and zero-event cells. These issues are especially prevalent in precision medicine contexts where predictive biomarkers create mixed patient populations across trials, and in rare disease research where event rates are naturally low [41] [3].
Sparse data scenarios introduce substantial uncertainty into treatment effect estimates and can lead to computational problems during model fitting. Multi-arm trials contribute valuable direct comparison evidence but require special statistical handling to account for their correlated structure. Zero-event cells, occurring when no events are observed in one or both treatment arms, present fundamental problems for conventional meta-analytic methods that rely on logarithmic transformations or variance calculations that become undefined [48]. This technical guide provides a comprehensive overview of current methodologies for addressing these challenges, framed within the broader context of advancing MTC research and practice.
Handling Zero-Event Studies in Meta-Analysis
The Zero-Events Problem and Classification Framework
Zero-event studies occur frequently in evidence synthesis, particularly for rare outcomes or adverse events. Vandermeer et al. and Kuss found that approximately 30% of meta-analyses in Cochrane reviews included single-zero-event studies (zero events in one group), while 34% contained double-zero-event studies (zero events in both groups) [48]. These studies create computational and methodological challenges because conventional effect size measures (such as odds ratios or relative risks) and their variances become undefined when denominators approach zero.
Xu et al. proposed a classification framework that categorizes meta-analyses with zero-events into six distinct subtypes based on two dimensions: (1) the total events count across all studies, and (2) whether included studies have single or both arms with zero events [49]. This classification provides a structured approach for selecting appropriate statistical methods, with different techniques recommended for each subtype. The framework emphasizes that double-zero-event studies contain valuable information and should not be automatically excluded, as their omission can introduce significant bias into pooled effect estimates [48].
Statistical Methods for Zero-Events
Table 1: Comparison of Methods for Handling Zero-Events in Meta-Analysis
| Method Category | Specific Methods | Key Principles | Advantages | Limitations |
|---|---|---|---|---|
| Continuity Corrections | Constant correction (e.g., +0.5) [48] | Add a small constant to all cells | Simple implementation; Widely supported in software | Can introduce bias; Sensitivity to choice of constant |
| Reciprocal correction [48] | Add values inversely related to group size | More nuanced than constant correction | Still potentially biased | |
| Treatment arm correction [48] | Add constant only to zero cells of treatment arms | Preserves control group integrity | Arbitrary element remains | |
| Model-Based Approaches | Generalized Linear Mixed Models (GLMM) [48] | Uses binomial likelihood with random effects | No arbitrary corrections; Better performance with many studies | Computational complexity; Convergence issues |
| Bayesian methods [41] | Incorporates prior distributions | Naturally handles sparse data; Full uncertainty quantification | Requires specification of priors | |
| Alternative Effect Measures | Risk Difference [48] | Uses absolute rather than relative measure | Avoids ratio statistics | Effect measure less familiar to clinicians |
A new method for continuity correction has been proposed specifically for relative risk estimation, which demonstrates superior performance in terms of mean squared error when the number of studies is small [48]. Simulation studies indicate that this new method outperforms traditional continuity corrections when dealing with few studies, while generalized linear mixed models (GLMM) perform best when the number of studies is large [48]. The application of these methods to COVID-19 data has demonstrated that double-zero-event studies significantly impact the estimate of the mean effect size and should be included in the analysis with appropriate methodological adjustments [48].
Analyzing Complex Interventions and Multi-Arm Trials
Component Network Meta-Analysis for Complex Interventions
Complex interventions consisting of multiple components present unique challenges for evidence synthesis. Standard NMA estimates the effects of entire interventions but cannot quantify the effects of individual components [50]. Component Network Meta-Analysis (CNMA) addresses this limitation by modeling the contributions of individual components, either additively or with interaction terms [50].
The additive CNMA model assumes that the total effect of a complex intervention equals the sum of its individual component effects. For example, if component A lowers a symptom score by 2 points and component B by 1 point, the combination A+B is expected to lower the score by 3 points [50]. When clinical evidence suggests violations of additivity, interaction CNMA models can be specified that include interaction terms to account for synergistic or antagonistic effects between components [50].
Table 2: CNMA Model Types and Applications
| Model Type | Key Assumption | Application Context | Implementation Considerations |
|---|---|---|---|
| Additive CNMA | Component effects sum linearly | Components act independently | Requires strong biological plausibility |
| Interaction CNMA | Components interact synergistically/antagonistically | Known mechanism-based interactions | Selection of interaction terms requires clinical input |
| Standard NMA | Each combination is distinct | Complex, unpredictable interactions | Less parsimonious but more flexible |
CNMA enables researchers to disentangle the effects of intervention components, identify active ingredients, inform component selection for future trials, and explore clinical heterogeneity [50]. The method is particularly valuable for synthesizing evidence on non-pharmacological interventions, which often share common components delivered in different combinations.
Incorporating Multi-Arm Trials in Evidence Networks
Multi-arm trials contribute direct evidence on multiple treatment comparisons simultaneously, making them statistically more efficient than multiple two-arm trials [15]. However, they require special methodological consideration because the treatment effects within a multi-arm trial are correlated. In both frequentist and Bayesian frameworks, this correlation structure must be appropriately modeled to ensure valid inference.
The appropriate handling of multi-arm trials is especially important in networks with sparse connections, where they may provide crucial direct evidence that strengthens the entire network. In Bayesian implementations, multi-arm trials can be modeled using multivariate normal distributions for the relative effects within each trial [41]. In frequentist approaches, generalized least squares or appropriate variance-covariance structures can account for the within-trial correlations.
Diagram 1: Decision Process for Analyzing Complex Interventions
Advanced Methodological Approaches for Sparse Data
Population-Adjusted Methods for Heterogeneous Populations
Precision medicine has introduced new complexities for evidence synthesis, particularly through the identification of predictive biomarkers that create mixed populations across trials [41]. For example, early trials of targeted therapies might include patients with any biomarker status, while later trials focus exclusively on biomarker-positive populations. This heterogeneity violates the traditional similarity assumptions of meta-analysis and requires specialized methods.
Population-adjusted indirect comparisons (PAIC) have been developed to address these challenges, with two primary approaches: Matching-Adjusted Indirect Comparison (MAIC) and Simulated Treatment Comparison (STC) [51] [3]. MAIC uses propensity score weighting to adjust individual patient data (IPD) from one trial to match the aggregate baseline characteristics of another trial. STC uses outcome regression models based on IPD to predict outcomes in the population with aggregate data [51]. These methods rely on the conditional constancy of relative effects, assuming that effect modifiers are consistently measured and adjusted for across studies.
Bayesian Methods for Sparse Networks
Bayesian approaches offer particular advantages for handling sparse data in MTCs through their ability to incorporate prior information and naturally quantify uncertainty [41] [15]. As noted in the ISPOR Task Force report, "Bayesian methods have undergone substantially greater development" for MTCs compared to frequentist approaches [15]. Key benefits include:
- Incorporation of informative priors: External evidence or conservative assumptions can be incorporated through carefully specified prior distributions, which can stabilize estimates in sparse data scenarios.
- Full uncertainty quantification: Bayesian methods naturally propagate all sources of uncertainty, including parameter uncertainty and between-study heterogeneity, providing more accurate credible intervals.
- Ranking probabilities: Bayesian MTCs can calculate the probability that each treatment is best, second best, etc., which is particularly valuable for decision-making under uncertainty.
- Handling of complex models: Bayesian frameworks using Markov chain Monte Carlo (MCMC) methods can estimate complex random-effects models even with limited data.
The Bayesian framework also facilitates sensitivity analyses, allowing researchers to examine how different prior specifications or modeling assumptions affect the conclusions, which is crucial when dealing with sparse data.
Experimental Protocols and Analytical Workflows
Protocol for Handling Zero-Events in Meta-Analysis
Objective: To synthesize evidence from studies with zero events while minimizing bias and maintaining statistical validity.
Pre-specification Steps:
- Define the classification of zero-event studies (single-zero vs. double-zero) according to the framework by Xu et al. [49]
- Specify primary and sensitivity analysis methods based on the anticipated number of studies and events
- For Bayesian analyses, specify prior distributions for basic parameters and heterogeneity
Analytical Sequence:
- Calculate descriptive statistics for event rates across studies
- Classify zero-event studies according to established framework
- Apply primary analysis method (e.g., GLMM for many studies, new continuity correction for few studies)
- Conduct sensitivity analyses using alternative methods
- Compare results across methods, investigating substantial differences
Interpretation Guidelines:
- When methods disagree, prioritize those with best statistical properties for the specific scenario
- Consider clinical plausibility of estimates, especially for extreme values
- Report all methods attempted and their results transparently
Diagram 2: Analytical Workflow for Zero-Events Meta-Analysis
Protocol for Component Network Meta-Analysis
Objective: To estimate the effects of individual components within complex interventions and their potential interactions.
Pre-specification Steps:
- Define all relevant components and their possible combinations based on clinical knowledge
- Specify the additive model as the primary analysis unless strong evidence suggests interactions
- Pre-specify potential interaction terms based on biological plausibility
Analytical Sequence:
- Conduct standard NMA as reference analysis
- Fit additive CNMA model assuming no interactions between components
- Assess model fit using residual deviance and deviance information criterion (DIC)
- If additive model fit is inadequate, consider interaction CNMA models
- Select interaction terms based on clinical knowledge and statistical evidence
- Compare all models using both statistical and clinical criteria
Interpretation Guidelines:
- Prefer more parsimonious models when fit is adequate
- Involve clinical experts in interpreting interaction terms
- Consider predictive validity for untested combinations
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Advanced Evidence Synthesis
| Tool Category | Specific Methods/Software | Primary Function | Application Context |
|---|---|---|---|
| Statistical Software | R packages: metafor, gemtc, netmeta [50] |
Implement various meta-analysis models | General evidence synthesis |
| Bayesian software: WinBUGS, OpenBUGS, JAGS [41] | Fit complex Bayesian models | Sparse data, random-effects models | |
Stata: metan, network packages |
User-friendly meta-analysis | Rapid analyses, educational contexts | |
| Specialized Methods | Component Network Meta-Analysis [50] | Disentangle complex intervention effects | Multi-component interventions |
| Matching-Adjusted Indirect Comparison [51] [3] | Adjust for population differences | Cross-study comparisons with IPD | |
| Generalized Linear Mixed Models [48] | Handle zero events without correction | Binary outcomes with sparse data | |
| Methodological Frameworks | Classification framework for zero-events [49] | Guide method selection | Meta-analyses with zero cells |
| Consistency assessment methods [15] | Evaluate network assumptions | All network meta-analyses |
The methodological landscape for handling sparse data, multi-arm trials, and zero cells in mixed treatment comparisons has evolved substantially in recent years, with sophisticated approaches now available to address these complex challenges. The appropriate application of these methods requires careful consideration of the specific data structure, research question, and underlying assumptions. Methodologists should prioritize approaches that maximize the use of available evidence while appropriately quantifying uncertainty, such as Bayesian methods for sparse networks and component network meta-analysis for complex interventions. As these techniques continue to develop, researchers must maintain focus on the fundamental principles of statistical rigor, clinical relevance, and transparent reporting to ensure that evidence syntheses reliably inform healthcare decision-making. Future methodological development should focus on increasing the accessibility of advanced methods, improving guidance for method selection in specific scenarios, and developing robust approaches for assessing model adequacy in complex evidence syntheses.
Mixed treatment comparison (MTC) models, also known as network meta-analyses, simultaneously synthesize evidence from multiple treatments and studies, comparing interventions that may never have been directly evaluated in head-to-head trials [30]. The validity of any MTC, however, depends critically on whether its underlying statistical assumptions are met and whether the results remain robust under different analytical scenarios [52]. As these models increasingly inform health technology assessments and clinical guideline development, ensuring their methodological rigor through comprehensive model checking and sensitivity analyses becomes paramount.
This technical guide provides researchers and drug development professionals with a structured framework for evaluating model fit and conducting sensitivity analyses within MTCs. We present practical methodologies for verifying key assumptions, detecting potential inconsistencies, and quantifying the stability of treatment effect estimates, framed within the broader context of ensuring that MTC results provide reliable foundations for decision-making in healthcare.
Core Assumptions and Their Implications
The validity of an MTC rests on three fundamental assumptions: similarity, homogeneity, and consistency [52]. Similarity requires that studies included in the network are sufficiently comparable in terms of clinical and methodological characteristics that might modify treatment effects (effect modifiers). Homogeneity refers to the extent that studies estimating the same pairwise comparison yield similar effect sizes, while consistency implies that direct evidence (from head-to-head trials) and indirect evidence (from trials connected via common comparators) agree within a network containing closed loops [30] [52].
Violations of these assumptions can introduce bias and invalidate conclusions. For instance, inconsistency between direct and indirect evidence may indicate systematic differences in effect modifiers across different pairwise comparisons, potentially leading to incorrect rankings of treatments [2]. The following sections provide methodologies to detect and address such issues.
Quantitative Framework for Assessing Model Fit
Statistical Measures for Evaluating Model Fit
Assessing model fit involves evaluating how well the chosen MTC model represents the observed data. The following table summarizes key quantitative measures used for this purpose:
Table 1: Quantitative Measures for Assessing Model Fit in MTCs
| Measure | Calculation/Definition | Interpretation | Threshold/Rule of Thumb |
|---|---|---|---|
| Residual Deviance | Difference between the log-likelihood of the fitted model and the saturated model [52] | Measures model fit; lower values indicate better fit | Ideally, residual deviance should be close to the number of data points for adequate fit [52] |
| Leverage | Influence of individual data points on model parameters | Identifies studies with disproportionate influence on results | Residual deviance + leverage ≤ 3 for all study arms suggests acceptable fit [52] |
| I² Statistic | Percentage of total variability due to heterogeneity rather than sampling error | Quantifies heterogeneity in pairwise comparisons | I² > 50% indicates substantial heterogeneity [52] |
| Between-Study Variance (τ²) | Estimated variance of treatment effects across studies | Measures heterogeneity magnitude in random-effects models | No universal threshold; context-dependent |
Bayesian Measures and Convergence Diagnostics
For Bayesian MTCs, which are commonly implemented using Markov chain Monte Carlo (MCMC) methods, additional diagnostics are essential [53]:
Table 2: Bayesian Diagnostic Measures for MTCs
| Diagnostic | Purpose | Implementation | Interpretation |
|---|---|---|---|
| Monte Carlo Error | Measures simulation accuracy of posterior estimates [53] | Calculated for each parameter | Should be <5% of the posterior standard deviation for reliable estimates [53] |
| Gelman-Rubin Statistic | Assesses MCMC convergence [53] | Compares within-chain and between-chain variability | Values approaching 1.0 indicate convergence |
| Trace Plots | Visual assessment of chain behavior [53] | Plot of parameter values across iterations | Stationary, well-mixed chains indicate convergence |
| Autocorrelation | Measures correlation between successive iterations | Plots autocorrelation at different lags | Rapid decrease to zero suggests efficient sampling |
Methodological Protocols for Sensitivity Analyses
Stepwise Approach to Checking MTC Assumptions
A systematic, stepwise approach ensures comprehensive evaluation of MTC assumptions. The following workflow illustrates this process:
Diagram 1: Stepwise MTC validation
Step 1: Clinical Similarity Assessment
Objective: To ensure studies included in the MTC are sufficiently similar in terms of potential effect modifiers.
Protocol:
- Identify potential effect modifiers a priori based on clinical knowledge (e.g., population characteristics, treatment regimens, outcome definitions)
- Systematically extract data on these effect modifiers from all included studies
- Assess between-study variability in effect modifiers through descriptive statistics or tabular comparison
- Exclude studies that are clinically dissimilar from the majority of the network
Example Implementation: In an MTC of antidepressants, researchers excluded studies conducted in specific populations (e.g., treatment-resistant patients, those with seasonal affective disorder) that differed substantially from the target population of major depression [52]. Additionally, they ensured outcome similarity by applying outcome-specific criteria, excluding studies that did not report the outcome of interest (treatment discontinuation due to adverse events).
Step 2: Statistical Homogeneity Evaluation
Objective: To assess and address heterogeneity within direct pairwise comparisons.
Protocol:
- Conduct pairwise meta-analyses for each direct comparison using random-effects models
- Calculate I² statistic to quantify heterogeneity: I² = (Q - df)/Q × 100%, where Q is the Cochran's heterogeneity statistic and df is degrees of freedom
- Classify heterogeneity as substantial if I² > 50%
- If substantial heterogeneity is detected:
- Identify studies with characteristics that may contribute to heterogeneity (e.g., high risk of bias, specific populations)
- Exclude these studies and recalculate heterogeneity measures
- For studies with no identifiable contributing factors, exclude from primary analysis and include in sensitivity analyses
Example Implementation: In the antidepressants MTC, researchers conducted random-effects meta-analyses for each pairwise contrast and excluded studies contributing to substantial heterogeneity (I² > 50%) before proceeding to the MTC analysis [52].
Step 3: Consistency Assessment
Objective: To verify agreement between direct and indirect evidence within closed loops of the network.
Protocol:
- Identify all closed loops in the evidence network (where both direct and indirect evidence exists)
- Apply the residual deviance approach suggested by Dias et al. [52]:
- Fit consistency model and calculate residual deviance for each study/arm
- Identify studies/arms with high residual deviance and leverage (sum >3 indicates poor fit)
- Sequentially eliminate studies/arms with highest contribution to poor fit
- Recalculate MTC after each exclusion
- Alternative approach: Use the Bucher method for simple indirect comparisons [2]
- Continue exclusion process until network shows acceptable consistency (residual deviance + leverage ≤3 for all study arms)
Example Implementation: In an overview of reviews for childhood nocturnal enuresis treatments, researchers applied a composite test of inconsistency using both fixed-effect and random-effects models, finding that fixed-effect estimates showed significant inconsistency while random-effects models provided consistent estimates [2].
Step 4: Comprehensive Sensitivity Analyses
Objective: To test the robustness of MTC results to different analytical choices and assumptions.
Protocol:
- Compare MTC estimates from the consistent network with estimates from the original network including inconsistencies
- Evaluate notable changes using predefined criteria:
- Change in effect size (e.g., more than two-fold change)
- Change in direction of effect
- Change in statistical significance
- Perform additional sensitivity analyses:
- Different statistical models (fixed-effect vs. random-effects)
- Different prior distributions in Bayesian analyses
- Inclusion/exclusion of studies based on risk of bias
- Different handling of multi-arm trials
- Set acceptability threshold (e.g., <20% of studies excluded for consistency reasons)
Example Implementation: In the antidepressants MTC, researchers considered a change in odds ratio by a factor of 2 as notable, along with changes in direction or statistical significance [52]. They also performed sensitivity analyses comparing networks with and without homogeneity checks.
Advanced Sensitivity Analysis Techniques
For more comprehensive sensitivity assessment, consider these additional approaches:
Node-Splitting: Separately estimates direct and indirect evidence for specific comparisons within the network, formally testing their agreement.
Meta-Regression: Incorporates study-level covariates into the MTC model to explore potential sources of heterogeneity or inconsistency.
Design-by-Treatment Interaction Model: A global approach to assessing inconsistency that accounts for different designs within the network.
Essential Research Reagents and Computational Tools
The following table details key methodological tools and their applications in MTC validation:
Table 3: Research Reagent Solutions for MTC Validation
| Tool/Reagent | Type | Primary Function | Application in MTC Validation |
|---|---|---|---|
| WinBUGS | Software | Bayesian inference Using Gibbs Sampling [53] | Implements Bayesian MTC models; calculates posterior distributions for treatment effects |
| R package 'gemtc' | Software | Network meta-analysis | Conducts MTC analyses with various consistency and heterogeneity models |
| Stata 'network' package | Software | Network meta-analysis | Frequentist approach to MTC; produces network graphs and effect estimates |
| I² Statistic | Statistical measure | Quantifies heterogeneity | Assesses homogeneity assumption in pairwise comparisons [52] |
| Residual Deviance | Diagnostic measure | Model fit assessment | Identifies poorly fitting studies/arms in consistency checking [52] |
| MCMC Sampling | Computational algorithm | Posterior estimation | Generparameter distributions in Bayesian MTCs; requires convergence diagnostics [53] |
| Gelman-Rubin Diagnostic | Convergence statistic | MCMC convergence assessment | Ensures reliability of Bayesian estimates [53] |
Interpretation Framework and Reporting Standards
Interpreting Sensitivity Analysis Results
Establish a priori decision rules for interpreting sensitivity analyses:
Robustness Criterion: MTC results can be considered robust if no notable changes (as predefined in Section 4.1.4) occur across sensitivity analyses.
Exclusion Threshold: The proportion of studies excluded for inconsistency reasons should not exceed 20% of the total network [52].
Impact Assessment: When changes occur, categorize their impact as:
- Minimal: No change in clinical interpretation or decision-making
- Moderate: Change in magnitude but not direction of effect
- Substantial: Change in direction of effect or statistical significance
Reporting Guidelines
Comprehensive reporting should include:
- Flow of Studies: Detailed diagram showing number of studies at each step of the selection process [52]
- Network Diagram: Visual representation of all treatment comparisons and available direct evidence
- Similarity Assessment: Table of study characteristics and effect modifiers across different comparisons
- Heterogeneity Statistics: I² values for each pairwise comparison
- Consistency Assessment: Results of formal consistency tests for each closed loop
- Sensitivity Analyses: Comparison of effect estimates across different analytical scenarios
The following diagram illustrates the logical relationship between different validation components and their impact on result interpretation:
Diagram 2: MTC validation framework
Model fit and sensitivity analyses are not peripheral activities but fundamental components of rigorous MTCs. The methodologies outlined in this guide provide a systematic framework for verifying the underlying assumptions of MTCs and quantifying the robustness of their results. By implementing these stepwise protocols—assessing clinical similarity, evaluating statistical homogeneity, verifying consistency, and conducting comprehensive sensitivity analyses—researchers can enhance the credibility of MTC findings and ensure they provide reliable evidence for healthcare decision-making.
As MTC methodologies continue to evolve, future developments will likely provide more sophisticated tools for assessing model fit, particularly for complex networks with multiple treatments and sparse connections. However, the fundamental principles outlined in this guide will remain essential for distinguishing robust comparisons from those potentially biased by violations of key assumptions.
Power Analysis and Optimal Design for MTC Studies
Mixed Treatment Comparison (MTC), also known as network meta-analysis, is a statistical methodology that enables the simultaneous synthesis of evidence across multiple interventions [30]. As a generalization of standard pairwise meta-analysis, MTC combines both direct evidence (from head-to-head trials) and indirect evidence (from trials connected via a common comparator) to estimate the relative effects among all treatments within a network [15]. This approach provides maximum utilization of available evidence, allowing clinicians and policymakers to compare multiple interventions that may not have been directly studied against each other in randomized controlled trials [30] [15].
The development of MTC methodology traces back to 1990, with substantial methodological advancements occurring since 2009 [15]. Both frequentist and Bayesian approaches can be employed, though Bayesian methods have undergone more extensive development and are more commonly implemented in practice [15]. The rapid increase in published systematic reviews incorporating MTCs reflects their growing importance in informing health policy decisions and health technology assessments [15].
Fundamental Concepts and Assumptions
Key Terminology and Network Structures
- Network Meta-Analysis: The simultaneous synthesis of evidence of all pairwise comparisons across more than two interventions [30].
- Closed Loop: A network structure where each comparison has both direct evidence and indirect evidence [30].
- Mixed Treatment Comparison (MTC): A specific statistical approach for analyzing networks with more than two interventions where at least one pair is compared both directly and indirectly [30].
- Consistency: The fundamental assumption that direct and indirect evidence are in agreement, meaning that the effect estimate from indirect comparisons aligns with that from direct comparisons [15].
Table: Common Network Structures in MTC Studies
| Structure Type | Description | Characteristics |
|---|---|---|
| Star Structure | Only one intervention has been directly compared with each of the others | Central node connects all other interventions |
| Single-Loop Structure | Contains direct comparisons between one set of at least three interventions | Forms one circular connection path |
| Multi-Loop Structure | Contains direct comparisons between multiple sets of interventions | Forms multiple circular connection paths |
Validity Assumptions
The validity of MTC methodology depends on several critical assumptions regarding similarity and consistency across all pairwise sets of trials included in the network [15]. The similarity assumption requires that trials are sufficiently homogeneous in their clinical and methodological characteristics. The consistency assumption implies that direct and indirect evidence are statistically coherent. Both formal statistical tests and clinical reasoning should be employed to assess these assumptions [15].
Challenges in Power Analysis for MTC Studies
Power analysis for MTC studies presents unique challenges compared to standard pairwise meta-analyses or primary clinical trials. Traditional approaches to power analysis typically rely on analytical formulas that lack the necessary flexibility for complex MTC models [54]. The same aspects that provide MTCs with their advantages—multiple sources of variation and complex random-effects structures—also lead to increased difficulties in power analysis and sample size planning [54].
Statistical power is defined as the probability of correctly rejecting the null hypothesis when it is false (typically denoted as 1-β, where β is the type II error probability) [54]. For MTC studies, power depends on multiple factors including network structure, sample sizes of included trials, between-study heterogeneity, and the specific comparisons of interest. The complexity of accounting for all these factors simultaneously makes analytical solutions often infeasible [54].
Methodological Approaches for Power Analysis
Simulation-Based Power Analysis
Simulation-based power analysis represents the most flexible and intuitive approach for MTC studies [54]. This method involves repeatedly simulating datasets under specified alternative hypotheses and analyzing each dataset to determine the proportion of simulations that yield statistically significant results.
The simulation-based power analysis workflow consists of three fundamental steps [54]:
- Simulate new datasets based on a model informed by existing data or hypothesized effect sizes
- Analyze each simulated dataset using the planned MTC model
- Calculate power as the proportion of simulations yielding statistically significant results
Analytical Approximations
While simulation-based methods are generally preferred for complex MTC networks, analytical approximations can provide reasonable power estimates for simpler network structures. Westfall, Kenny, and Judd developed an analytical solution for mixed models with crossed random effects, which can be applied to simple MTC networks with one fixed effect with two levels [54]. However, this approach lacks flexibility for more complex models commonly encountered in practice.
Alignment Between Power and Data Analysis
A critical principle in power analysis for MTC studies is ensuring alignment between the power analysis and the planned data analysis [55]. Without proper alignment, conclusions drawn from power analysis are unreliable. The power analysis must use the same statistical test, model, and assumptions about correlation and variance patterns as the planned analysis of the data [55]. Misaligned power analysis may yield sample size estimates that are either too large (wasting resources) or too small (increasing the risk of missing important associations) [55].
Implementation Frameworks and Software Solutions
Software Tools for Power Analysis
Table: Software Tools for Power Analysis in Complex Models
| Software Tool | Methodology | Access | Key Features |
|---|---|---|---|
| GLIMMPSE | Approximate/exact methods accurate in small and large samples | Free, web-based | Validated against Monte Carlo simulations, supports various covariance structures |
| PASS | Approximate/exact methods | Commercial | Implements preferred methods for correlated longitudinal measures |
| SAS PROC POWER | Approximate/exact methods | Commercial license required | Comprehensive power analysis procedures |
| R-based simulation | Simulation-based | Free, open-source | Maximum flexibility for complex MTC models |
Bayesian vs. Frequentist Approaches
Both Bayesian and Frequentist frameworks can be employed for MTC studies, each with distinct advantages [30] [15]. Bayesian methods have undergone more substantial development and offer additional capabilities such as ranking the effects of interventions by the order of probability that each is best [15]. The choice between frameworks depends on the research question, available resources, and analyst preferences.
Optimal Allocation in Sequential Designs
In complex trial designs such as Sequential Multiple Assignment Randomized Trials (SMART), optimal allocation of subjects to treatment sequences presents additional considerations for power analysis [56]. Equal randomization is not necessarily the best choice, particularly when variances and/or costs vary across treatment arms, or when outcomes are categorical rather than quantitative [56].
Multiple-objective optimal design methodology can be employed to consider all relevant comparisons simultaneously while accounting for their relative importance [56]. This approach combines multiple objectives into a single optimality criterion and seeks a design that is highly efficient for each criterion. The optimal design depends on response rates to first-stage treatments, and maximin optimal design methodology can be used to find robust optimal designs when these parameters are uncertain [56].
Experimental Protocols and Methodological Guidelines
Data Requirements and Input Parameters
Successful power analysis for MTC studies requires careful specification of multiple input parameters [55]:
- Network Structure: The geometry of treatment comparisons and connectivity
- Effect Sizes: Clinically significant differences for key comparisons
- Heterogeneity Parameters: Between-study variance (τ²) estimates
- Sample Sizes: Number of studies and participants per comparison
- Type I Error Rate: Typically set at 0.05 for each comparison
Sensitivity Analysis Framework
Given the uncertainty in input parameters, sensitivity analysis is essential for robust power analysis [55]. This involves calculating power across a range of plausible values for key parameters, particularly between-study heterogeneity and effect sizes. Sensitivity analysis helps determine how power estimates might change if initial assumptions prove incorrect.
Research Reagent Solutions
Table: Essential Methodological Components for MTC Power Analysis
| Component | Function | Implementation Considerations |
|---|---|---|
| Network Geometry Specifier | Defines structure of treatment comparisons | Should reflect clinical reality and evidence availability |
| Heterogeneity Estimator | Quantifies between-study variance | Can be informed from previous meta-analyses or expert opinion |
| Effect Size Generator | Creates hypothesized treatment effects | Should reflect clinically important differences |
| Monte Carlo Engine | Performs simulation iterations | Requires sufficient iterations (typically 1,000+) for stability |
| Model Convergence Checker | Ensures statistical estimation reliability | Particularly important for complex Bayesian MTC models |
Reporting and Interpretation
Comprehensive reporting of power analysis methods and results is essential for transparency and reproducibility. Reports should include detailed descriptions of the network structure, input parameters, software tools, and any assumptions made. When interpreting results, researchers should consider the limitations of their power analysis, particularly the uncertainty in input parameters and the impact of potential violations of model assumptions.
Power analysis should be used exclusively for study planning purposes and not for analyzing or interpreting results once data have been collected [54]. Furthermore, the data and model used for simulation should not stem from the experiment for which power is being estimated, but rather should be independent from it [54].
Power analysis and optimal design for MTC studies require specialized methodological approaches that account for the complexity of combining direct and indirect evidence. Simulation-based methods currently offer the most flexible solution for these complex analyses. Proper implementation requires careful attention to network structure, heterogeneity, and alignment between power analysis and planned data analysis. As MTC methods continue to evolve and gain wider application in evidence-based medicine, robust power analysis will play an increasingly important role in ensuring the reliability and interpretability of network meta-analyses.
Validating MTC Results and Comparative Performance Against Direct Evidence
Guidance from Health Technology Assessment (HTA) Bodies
Health Technology Assessment (HTA) bodies worldwide are tasked with evaluating the clinical and economic value of new health interventions to inform critical healthcare decisions. A significant and common challenge in this process is the frequent lack of head-to-head randomized clinical trial (RCT) data comparing a new technology directly against the standard of care or other relevant alternatives [51]. To make evidence-based recommendations for adopting innovative technologies, allocating finite resources, and developing clinical guidelines, these bodies must find robust ways to generate comparative evidence [51].
Indirect Treatment Comparison (ITC) methods have emerged as a fundamental methodological approach to address this evidence gap [51]. Among these methods, Mixed Treatment Comparisons (MTC), also known as Network Meta-Analysis (NMA), represent a sophisticated statistical technique that allows for the simultaneous comparison of multiple treatments by synthesizing both direct and indirect evidence from a network of clinical trials [30] [16]. This guide provides a comprehensive technical overview of the guidance from major HTA bodies regarding the use of these complex comparison methods, framed within the broader context of MTC model research.
Researchers have developed numerous ITC methods, leading to a landscape of various and sometimes inconsistent terminologies [51]. HTA guidance documents often refer to these methods with specific nuances. The following sections and tables clarify the key methods and their positioning within HTA frameworks.
Fundamental Comparison Methods
- Adjusted Indirect Comparison (Bucher Method): This is a foundational method for pairwise indirect comparisons. It estimates the relative effect of two interventions, A and B, by using their direct comparisons against a common comparator C (e.g., placebo or standard treatment) [16]. Its key assumption is the constancy of relative effects (homogeneity and similarity) across studies [51].
- Mixed Treatment Comparison (MTC) / Network Meta-Analysis (NMA): MTC is a generalization of indirect comparisons. It is a statistical approach used to analyze a network of evidence involving more than two interventions, where at least one pair is compared both directly and indirectly (forming a closed loop) [30]. It synthesizes all available direct and indirect evidence into a single, coherent analysis, allowing for simultaneous inference and ranking of all treatments in the network [30] [16]. It requires consistency between direct and indirect evidence [16].
The diagram below illustrates the logical relationship and workflow for selecting and applying these key methodologies within an HTA framework.
Categorization of ITC Methods and Key Assumptions
HTA bodies require a clear understanding and justification of the methodological assumptions underlying any submitted indirect comparison. The table below summarizes the core methods, their frameworks, and fundamental assumptions [51].
Table 1: Fundamental ITC Methods, Frameworks, and Assumptions
| Method Category | Key Underlying Assumptions | Common Statistical Frameworks | Key Application in HTA |
|---|---|---|---|
| Adjusted Indirect Comparison | Constancy of relative effects (Homogeneity, Similarity) [51]. | Frequentist [51]. | Pairwise comparisons through a common comparator [51]. |
| Network Meta-Analysis (NMA) | Constancy of relative effects (Homogeneity, Similarity, and Consistency) [51] [16]. | Frequentist or Bayesian [51]. | Simultaneous comparison of multiple interventions; ranking treatments [51]. |
| Population-Adjusted ITC (PAIC) | Conditional constancy of relative or absolute effects [51]. | Frequentist or Bayesian [51]. | Adjusting for population imbalance across studies, often with Individual Patient Data (IPD) [51]. |
Methodological Guidance from Major HTA Bodies
HTA bodies have developed specific preferences and recommendations for using ITC and MTC methods. The following section synthesizes experimental protocols and methodological expectations based on current HTA guidelines and research.
Core Analytical Protocol for Mixed Treatment Comparisons
The application of an MTC involves a multi-stage process. Adherence to a rigorous protocol is essential for HTA acceptance. The workflow below details the key phases from systematic review to uncertainty analysis, as guided by HTA good practices [51] [57].
Phase 1: Systematic Review and Network Feasibility The foundation of any MTC is a systematic literature review following established guidelines (e.g., PRISMA-NMA). The objective is to identify all relevant RCTs for the interventions and comparators of interest. The analysis must evaluate if the trials form a connected network and document the available direct and indirect evidence [51] [16].
Phase 2: Assessment of Key Assumptions HTA submissions must explicitly address three critical assumptions:
- Homogeneity: Assesses the variability in treatment effects between trials comparing the same interventions. Statistical tests (e.g., I²) and clinical reasoning are used.
- Similarity: Evaluates the potential for effect modifiers (e.g., baseline risk, patient characteristics) to be balanced across the different treatment comparisons in the network. This is often assessed qualitatively by comparing study and population characteristics (PICO) [51].
- Consistency: Refers to the agreement between direct and indirect evidence for the same treatment comparison. This can be evaluated statistically using methods like node-splitting or by comparing direct and indirect estimates within a closed loop [51] [16].
Phase 3: Model Implementation MTC models can be implemented within either a Bayesian or Frequentist framework. HTA bodies generally accept both, but the choice must be justified.
- Bayesian Framework: Often preferred for its flexibility, especially when source data are sparse. It uses Markov chain Monte Carlo (MCMC) simulation to estimate the posterior distribution of treatment effects. Non-informative priors are typically recommended to let the data dominate the analysis [16].
- Frequentist Framework: Uses methods like multivariate meta-analysis to combine evidence.
Phase 4: Model Fit and Convergence Assessment For Bayesian models, convergence of the MCMC chains must be demonstrated. Techniques include:
- Visual inspection of trace plots.
- Calculating the Gelman-Rubin statistic (R-hat), where a value close to 1.0 indicates convergence.
- Assessing residual deviance to check the model's goodness-of-fit to the data [16].
Phase 5: Analysis and Uncertainty Exploration The final phase involves:
- Generating point estimates (e.g., Odds Ratios, Hazard Ratios) and credible intervals for all pairwise comparisons.
- Presenting treatment rankings (e.g., Surface Under the Cumulative Ranking curve - SUCRA).
- Conducting extensive sensitivity and subgroup analyses to explore heterogeneity and the impact of effect modifiers.
- Assessing transitivity, the underlying principle that allows indirect comparisons to be valid [51].
Essential Research Reagents and Tools for MTC
The successful execution of an MTC for an HTA submission relies on a suite of methodological tools and software solutions.
Table 2: The Scientist's Toolkit for Mixed Treatment Comparisons
| Tool Category / 'Reagent' | Function in MTC Research | Examples & Notes |
|---|---|---|
| Statistical Software | Implements complex Bayesian or Frequentist MTC models. | R (gemtc, netmeta packages), WinBUGS/OpenBUGS (specialized for MCMC), JAGS, Stata(network`` package). |
| Systematic Review Software | Manages the screening, data extraction, and quality assessment of included studies. | Rayyan, Covidence, DistillerSR. |
| Quality/Risk of Bias Assessment | Evaluates the methodological quality of individual studies, a critical factor for HTA. | Cochrane RoB 2.0 (RCTs), ROBIS (systematic reviews). |
| Consistency Evaluation Tools | Statistical methods to check the consistency assumption between direct and indirect evidence. | Node-splitting, Design-by-treatment interaction model. |
| Data & Code Repositories | Ensures transparency, reproducibility, and facilitates HTA body review. | Sharing analysis code (R, WinBUGS) and extracted data. |
Quantitative Comparison of Methodological Performance
Understanding the relative performance and output of different ITC methods is crucial for selecting the most appropriate one for an HTA submission. The following table synthesizes findings from comparative methodological studies.
Table 3: Comparative Validity of MTC versus Adjusted Indirect Comparison
| Comparison Metric | Adjusted Indirect Comparison | Mixed Treatment Comparison (MTC) | Implications for HTA Submission |
|---|---|---|---|
| Statistical Precision | May yield wider confidence intervals as it uses only a subset of the evidence [16]. | Often produces more precise estimates (narrower CrIs) by borrowing strength from the entire network [16]. | MTC can provide more definitive results for decision-making. |
| Handling of Complexity | Limited to pairwise comparisons with a common comparator; cannot use multi-arm trial data efficiently [51] [16]. | Can synthesize complex networks with multi-arm trials and multiple comparators simultaneously [51] [16]. | MTC is preferred for comparing multiple treatments in a single analysis. |
| Methodological Consistency | In less complex networks with a mutual comparator, results are often similar to MTC [16]. | In complex networks, point estimates and intervals may differ importantly from simpler methods [16]. | Justify method choice based on network geometry; use MTC for complex evidence structures. |
| Key HTA Concern | Relies heavily on the similarity assumption for the single common comparator. | Relies on the more complex consistency assumption across the entire network. | HTA bodies require rigorous assessment and statistical testing of consistency in MTCs [51]. |
Emerging Trends and Future Methodological Directions
The field of ITC and HTA guidance is continuously evolving. Two significant areas of development are population-adjusted methods and the role of artificial intelligence.
Population-Adjusted ITC (PAIC): For cases where material heterogeneity in study populations exists, HTA bodies are increasingly considering advanced methods like Matching-Adjusted Indirect Comparison (MAIC) and Simulated Treatment Comparison (STC). These methods, often requiring Individual Patient Data (IPD) for at least one trial, aim to adjust for cross-trial imbalances in effect modifiers [51]. However, their acceptance is conditional on the availability and quality of IPD and the plausibility of having adjusted for all important confounding variables [51].
Artificial Intelligence (AI) in HTA: AI and large language models hold transformative potential for streamlining evidence generation, including automating systematic literature reviews and assisting with complex ITCs [58]. However, HTA bodies are in the early stages of developing guidance. The UK's NICE has issued a position statement emphasizing that AI-driven methods must be clearly declared, transparent, scientifically robust, and reproducible [58]. Other major HTA bodies, such as HAS, IQWiG, and CADTH, are exploring AI tools but lack formal guidance as of 2025 [58]. The core principles of methodological transparency and replicability remain paramount, and "black box" AI models are unlikely to be accepted without thorough validation and human oversight [58].
Comparing MTC with Adjusted Indirect Comparisons and Direct Meta-Analysis
In evidence-based medicine, the comparison of multiple competing interventions is often required for optimal clinical and policy decision-making. While direct, head-to-head randomized controlled trials (RCTs) represent the gold standard for treatment comparisons, they are frequently unavailable for all interventions of interest. This evidence gap has led to the development of advanced statistical methods for synthesizing available data, including direct meta-analysis, adjusted indirect comparisons, and mixed treatment comparisons (MTCs) [59] [60]. These methodologies exist on a spectrum of complexity, with each offering distinct advantages and limitations for treatment effect estimation.
Direct meta-analysis synthesizes evidence from studies comparing the same two interventions, while adjusted indirect comparisons allow for comparisons between interventions that have never been directly evaluated in clinical trials by using a common comparator [30] [60]. MTC methodology, also known as network meta-analysis, represents a more sophisticated approach that combines both direct and indirect evidence within a single analytical framework, creating an "evidence network" where treatments are compared both directly and indirectly [61] [2]. This technical guide examines these three key methodologies, highlighting their comparative strengths, limitations, and appropriate applications within clinical and research contexts.
Methodological Foundations
Direct Meta-Analysis
Direct meta-analysis represents the foundational approach for quantitatively synthesizing evidence from multiple independent studies addressing the same clinical question.
Objective and Approach: The primary objective is to combine results from studies that compare the same two interventions (e.g., Intervention A vs. Intervention B) to increase statistical power, improve precision of effect estimates, and resolve uncertainties or discrepancies found in individual studies [62] [63]. This approach follows a structured process involving formulation of a study question (using the PICO framework—Population, Intervention, Comparison, Outcome), systematic literature search, study selection based on pre-defined criteria, data extraction, and statistical pooling of results [62].
Statistical Models: The two primary statistical models used are fixed-effect and random-effects models. The fixed-effect model assumes that all included studies investigate the same population and share a common true effect size, with observed variations due solely to sampling error [64]. The random-effects model acknowledges that studies may have differing true effect sizes due to variations in study populations, methodologies, or other characteristics, and incorporates this between-study heterogeneity into the analysis [59] [64]. The choice between models depends on the presence and extent of heterogeneity, typically assessed using Cochran's Q test and the I² statistic [62].
Adjusted Indirect Comparisons
Adjusted indirect comparisons provide a methodological solution for comparing interventions that lack direct head-to-head evidence but share a common comparator.
Conceptual Basis: First formally described by Bucher et al., this method preserves the randomization of the originally assigned patient groups by comparing the magnitude of treatment effect of two interventions relative to a common comparator [60]. For example, if Drug A has been compared to Drug C in clinical trials, and Drug B has been compared to Drug C in separate trials, an indirect comparison between A and B can be estimated by comparing the difference between A and C with the difference between B and C [60].
Methodology: The adjusted indirect comparison method statistically combines the effect estimates and their variances from the two direct comparisons (A vs. C and B vs. C). This approach adjusts for the fact that the comparisons come from different trials, unlike naïve direct comparisons which simply contrast results across trials without accounting for systematic differences [60]. This method is accepted by various drug reimbursement agencies including the UK National Institute for Health and Care Excellence (NICE) and the Canadian Agency for Drugs and Technologies in Health (CADTH) [60].
Mixed Treatment Comparisons (MTC)
Mixed treatment comparison, more commonly referred to today as network meta-analysis, represents an advanced methodology that synthesizes both direct and indirect evidence within a unified analytical framework.
Conceptual Framework: MTC is a statistical method that uses both direct evidence (from trials directly comparing the interventions of interest) and indirect evidence (from trials comparing each intervention of interest with a further alternative) to estimate the comparative efficacy and/or safety of interventions for a defined population [61]. The term "mixed" refers to the method's ability to combine these two types of evidence within a single analysis, creating an "evidence network" [61].
Key Requirements and Assumptions: The MTC approach requires a connected network of pairwise comparisons that links each intervention to every other intervention, either directly or through intermediate comparators [59]. Beyond the standard assumptions of pairwise meta-analysis, MTC requires the consistency assumption—that direct and indirect evidence are in agreement—and assumptions regarding the similarity of studies on clinical and methodological grounds, including patient populations, outcome definitions, and intervention characteristics [59] [2].
Analytical Approaches: MTC can be conducted within both Bayesian and Frequentist statistical frameworks. The Bayesian approach has been more commonly implemented, utilizing Markov Chain Monte Carlo (MCMC) methods in software like WinBUGS, and provides a natural framework for estimating probabilities of treatment rankings [59] [30].
Comparative Analysis of Methods
Methodological Comparison
Table 1: Comparison of Key Characteristics Across Methodologies
| Characteristic | Direct Meta-Analysis | Adjusted Indirect Comparison | Mixed Treatment Comparison |
|---|---|---|---|
| Evidence Base | Direct evidence only (e.g., A vs. B) | Indirect evidence only (e.g., A vs. C and B vs. C) | Combined direct + indirect evidence |
| Network Structure | Single pairwise comparison | Simple chain via common comparator | Connected network of multiple interventions |
| Statistical Approach | Fixed-effect or random-effects models | Adjusted comparison via common comparator | Bayesian or Frequentist network meta-analysis |
| Key Assumptions | Homogeneity/exchangeability of studies | Similarity assumption & consistency of effects | Consistency between direct & indirect evidence |
| Treatment Ranking | Limited to the two interventions compared | Limited to the specific indirect comparison | Simultaneous ranking of all interventions in network |
| Handling of Heterogeneity | Standard methods (Q, I², meta-regression) | Limited ability to assess or explain | More complex, requires advanced assessment |
Relative Advantages and Limitations
Table 2: Advantages and Limitations of Each Methodology
| Methodology | Advantages | Limitations |
|---|---|---|
| Direct Meta-Analysis | • Well-established, familiar methodology• Straightforward interpretation• Standard tools for risk of bias & heterogeneity assessment | • Limited to two interventions at a time• Cannot incorporate indirect evidence• May lead to fragmented decision-making when multiple options exist |
| Adjusted Indirect Comparison | • Allows comparisons when direct evidence is lacking• Preserves randomization through common comparator• Methodologically simpler than MTC | • Increased uncertainty compared to direct evidence• Limited to specific pairwise indirect comparisons• Cannot incorporate all available evidence simultaneously |
| Mixed Treatment Comparison | • Synthesizes all available direct and indirect evidence• Improves precision by reducing uncertainty• Enables simultaneous comparison and ranking of all treatments• Maximizes use of available trial data | • Greater methodological complexity• Requires more stringent assumptions (consistency)• Limited tools for assessing network heterogeneity• Requires specialized statistical expertise |
Statistical Precision and Evidence Hierarchy
A key distinction among these methodologies lies in their statistical properties and the strength of evidence they provide:
Precision of Estimates: Direct evidence from head-to-head trials typically provides the most precise estimate of treatment effects. Adjusted indirect comparisons generally produce estimates with greater uncertainty, as the statistical uncertainties of the component comparison studies are summed [60]. For example, if the comparison of A vs. C has a variance of 1 and B vs. C has a variance of 1, the indirect comparison of A vs. B would have a variance of 2 [60]. MTC can improve precision by combining both direct and indirect evidence, potentially reducing uncertainty through the incorporation of a greater share of the available evidence [59].
Evidence Hierarchy: In terms of strength of evidence for a specific comparison, direct evidence from well-conducted RCTs followed by direct meta-analysis is generally considered strongest. Adjusted indirect comparisons provide valid evidence when direct comparisons are unavailable, while MTC aims to strengthen inference by incorporating both direct and indirect evidence, particularly when both are available and consistent [59] [65].
Experimental Protocols and Analytical Workflows
Implementation Workflow for MTC Analysis
The following diagram illustrates the key stages in conducting a mixed treatment comparison:
MTC Analysis Workflow
Protocol for Conducting an MTC Analysis
Define Research Question and Eligibility Criteria: Formulate a focused clinical question using the PICO framework, explicitly defining populations, interventions, comparators, and outcomes of interest. Establish inclusion/exclusion criteria for studies based on study design, patient characteristics, intervention details, and outcome measures [62].
Systematic Literature Search: Conduct a comprehensive, systematic search across multiple electronic databases (e.g., PubMed, Embase, Cochrane Central) using predefined search strategies. Search strategies should include relevant keywords, Boolean operators, and appropriate filters. The search should also incorporate hand-searching of reference lists and attempts to identify gray literature to minimize publication bias [62] [64].
Study Selection and Data Extraction: Implement a standardized process for screening titles, abstracts, and full-text articles, typically involving multiple independent reviewers. Develop a standardized data extraction form to collect information on study characteristics, patient demographics, intervention details, outcome measures, effect estimates, and measures of variance [62].
Network Geometry and Connectivity Assessment: Map the evidence network to visualize and verify connectivity between all interventions of interest. Each intervention must be connected to every other intervention through a path of direct comparisons [59] [2]. Document the number of studies contributing to each direct comparison.
Risk of Bias and Quality Assessment: Evaluate the methodological quality and risk of bias of included studies using standardized tools (e.g., Cochrane Risk of Bias tool for randomized trials). This assessment helps inform the interpretation of results and potential sensitivity analyses [62].
Statistical Analysis:
- Model Selection: Choose between fixed-effect and random-effects models based on assessment of heterogeneity and clinical considerations. Random-effects models are generally preferred when heterogeneity is present or suspected [59] [62].
- Implementation: Conduct analysis using appropriate statistical software (e.g., WinBUGS, R, or other specialized packages). Bayesian approaches typically require specification of prior distributions for model parameters [59].
- Consistency Assessment: Evaluate the statistical consistency between direct and indirect evidence where possible (e.g., in closed loops). Inconsistency can be assessed using node-splitting or other statistical tests [2].
Presentation of Results: Present results using appropriate graphical and tabular displays, including network diagrams, forest plots of comparative effects, and rankings of treatments. Results should include both point estimates and measures of uncertainty (credible or confidence intervals) [62].
The Researcher's Toolkit: Essential Components for MTC Analysis
Table 3: Essential Methodological Components for MTC Analysis
| Component | Function | Examples/Standards |
|---|---|---|
| Systematic Review Methodology | Foundation for identifying, selecting, and critically appraising all relevant research | Cochrane Handbook, PRISMA guidelines |
| Statistical Software | Implementation of complex Bayesian or Frequentist network meta-analysis models | WinBUGS, R, Stata, Python |
| Risk of Bias Assessment Tools | Evaluate methodological quality of included studies | Cochrane RoB tool, ROBINS-I |
| Consistency Assessment Methods | Evaluate agreement between direct and indirect evidence | Node-splitting, side-split methods |
| Heterogeneity Metrics | Quantify between-study variation in treatment effects | I² statistic, τ² (between-study variance) |
| Result Presentation Frameworks | Clear communication of complex network meta-analysis findings | Network diagrams, rankograms, forest plots |
The evolution of meta-analytic methods from direct pairwise comparisons to sophisticated network approaches represents significant progress in evidence-based medicine. Direct meta-analysis remains a robust method for synthesizing evidence for specific pairwise comparisons, while adjusted indirect comparisons provide a valuable tool when direct evidence is lacking. However, mixed treatment comparisons (network meta-analysis) offer a comprehensive framework that integrates all available direct and indirect evidence, providing coherent, simultaneous comparisons of multiple interventions.
The choice among these methodologies depends on the specific clinical question, available evidence, and analytical resources. When facing decisions between multiple interventions and when the evidence base includes both direct and indirect comparisons, MTC provides the most comprehensive approach, maximizing statistical power and enabling meaningful treatment rankings. However, this advanced methodology requires careful attention to its underlying assumptions, particularly regarding consistency and heterogeneity, and should be conducted with appropriate methodological rigor and statistical expertise.
As comparative effectiveness research continues to evolve, MTC methodology is poised to play an increasingly important role in informing healthcare decisions, guiding treatment guidelines, and shaping future research priorities. Its ability to provide a unified, coherent analysis of all relevant evidence makes it particularly valuable for clinicians, policymakers, and researchers navigating complex treatment landscapes.
Evaluating Coherence and Consistency Between Direct and Indirect Evidence
Mixed Treatment Comparison (MTC), also known as network meta-analysis, represents a statistical methodology that synthesizes evidence from a network of clinical trials comparing multiple interventions. This approach is particularly valuable in health technology assessment and comparative effectiveness research, where clinicians and policymakers need to make informed decisions between multiple treatment options. MTC serves two primary roles: strengthening inference concerning the relative efficacy of two treatments by incorporating both direct and indirect evidence, and facilitating simultaneous inference regarding all treatments to enable selection of the optimal intervention [66]. The fundamental principle underlying MTC is the creation of an internally coherent set of estimates that respects the randomization in the underlying evidence, allowing for estimation of the effect of each intervention relative to every other, whether or not they have been directly compared in trials [2].
As the volume of systematic reviews and treatment options has expanded, MTC has become increasingly important for evidence synthesis. With over 3,000 published reviews indexed on the Cochrane Database of Systematic Reviews alone, many addressing competing treatments for single clinical conditions, MTC provides a structured analytical framework to make sense of complex evidence networks [2]. The method has seen a dramatic increase in application since 2009, with published systematic reviews reporting MTCs becoming increasingly common in health policy decisions [15]. This growth reflects the method's ability to maximize the utility of available clinical trial data while providing a coherent basis for decision-making in healthcare.
Fundamental Concepts and Terminology
Types of Evidence in Treatment Networks
Direct Evidence: Obtained from head-to-head trials that directly compare two interventions of interest. This evidence comes from randomized comparisons where treatments are compared within the same trial.
Indirect Evidence: Derived through a common comparator, where the relative effect of two treatments (B vs. C) is inferred through their common comparisons with a third intervention (A). For example, if trial evidence exists for A vs. B and A vs. C, then an indirect estimate for B vs. C can be derived [67].
Mixed Treatment Comparison: The simultaneous synthesis of both direct and indirect evidence within a single analytical framework, producing coherent estimates for all pairwise comparisons in the treatment network [66] [68].
Key Assumptions Underlying Valid Evidence Synthesis
The validity of MTC depends on three critical assumptions:
Similarity: The trials included in the network must be sufficiently similar in their clinical and methodological characteristics (e.g., patient populations, outcome definitions, risk of bias) that combining their results is clinically meaningful.
Homogeneity: For each direct pairwise comparison, the treatment effects should be consistent across trials examining that specific comparison.
Consistency: The agreement between direct and indirect evidence for the same treatment comparison. This fundamental assumption ensures that direct and indirect evidence can be validly combined [2] [67].
Methodological Framework for Mixed Treatment Comparisons
Statistical Models for MTC
MTC analyses typically employ Bayesian hierarchical models using Markov chain Monte Carlo (MCMC) methods implemented in software such as WinBUGS [66]. The core model can be represented as follows for a random-effects MTC:
The basic random-effects model for a pairwise meta-analysis is extended to the network setting. For a trial comparing treatments A and B, the treatment effect is modeled as:
[ \delta{iAB} \sim N(d{AB}, \tau^2) ]
Where (d_{AB}) represents the mean treatment effect of B versus A, and (\tau^2) represents the between-trial variance (heterogeneity). In a network containing multiple treatments, consistency assumptions are incorporated through relationships such as:
[ d{AC} = d{AB} + d_{BC} ]
This fundamental linearity assumption allows the network to maintain internal coherence and permits the estimation of all pairwise comparisons [66] [19].
Both fixed-effect and random-effects models can be implemented, with the latter allowing for variation in true treatment effects across trials. Models may assume homogeneous between-trials variance across treatment comparisons or allow for heterogeneous variance structures. Additionally, models with fixed (unconstrained) baseline study effects can be compared with models where random baselines are drawn from a common distribution [66].
Data Structures and Network Geometry
MTC can accommodate various network structures, each with implications for the strength of indirect evidence:
Star Structure: Only one intervention (typically a common comparator like placebo) has been directly compared with each of the others.
Single-Loop Structures: Contain direct comparisons between one set of at least three interventions.
Multi-Loop Structures: Contain direct comparisons between multiple sets of interventions, providing more opportunities for consistency checking [15].
The connectedness of the network is essential – there must be a path between each treatment and all others through direct comparisons. The geometry of the evidence network influences both the precision of estimates and the ability to evaluate consistency assumptions [2].
Table 1: Types of Evidence Networks in MTC
| Network Type | Structure Description | Consistency Evaluation | Example |
|---|---|---|---|
| Star Network | Single common comparator connected to all other treatments | Limited to indirect comparison loops | Placebo-controlled trials of multiple active treatments |
| Single Loop | Three treatments forming a closed loop | Single consistency check possible | A vs. B, B vs. C, and A vs. C trials |
| Multi-Loop | Multiple interconnected treatments | Multiple consistency checks possible | Complex treatment networks with multiple direct comparisons |
Assessing Coherence and Consistency: Methodological Approaches
Statistical Methods for Detecting Inconsistency
Evaluating the coherence between direct and indirect evidence is a critical step in MTC. Several statistical approaches have been developed for this purpose:
Bucher's Method: A frequentist approach for comparing direct and indirect estimates of a specific treatment comparison. This method calculates the difference between direct and indirect estimates and assesses whether this difference is statistically significant [2] [67].
Node-Splitting Methods: Separate direct and indirect evidence for particular comparisons and evaluate their agreement through Bayesian model comparison. This approach allows for identification of which specific comparisons in the network may be inconsistent [66].
Composite Tests of Inconsistency: Evaluate the global consistency of the entire network through χ² tests that compare all available direct and indirect estimates [2].
The case study on granulocyte colony-stimulating factors illustrates the importance of these methods, where substantial inconsistency was detected between direct and indirect evidence for primary pegfilgrastim versus no primary G-CSF (P value for consistency hypothesis 0.027) [67].
When inconsistency is detected, further investigation is necessary to identify potential sources:
Clinical Diversity: Differences in trial populations, interventions, or outcome measurements.
Methodological Heterogeneity: Variations in trial design, risk of bias, or analysis methods.
Statistical Heterogeneity: Unexplained variation in treatment effects beyond chance.
Specific Inconsistent Trials: Individual trials that deviate substantially from the rest of the evidence base, identifiable through methods like cross-validation [67].
In the granulocyte colony-stimulating factors example, predictive cross-validation revealed that one specific trial comparing primary pegfilgrastim with no primary G-CSF was inconsistent with the evidence as a whole and with other trials making this comparison [67].
Implementing Consistency Assessments: Experimental Protocols
Protocol for Evaluating Consistency in MTC
Objective: To assess the consistency between direct and indirect evidence in a mixed treatment comparison network.
Materials: Aggregate data from systematic review of randomized controlled trials including at least three treatments forming a connected network.
Table 2: Research Reagent Solutions for MTC Consistency Assessment
| Tool/Software | Function | Application Context |
|---|---|---|
| WinBUGS | Bayesian analysis using MCMC | Fitting hierarchical MTC models [66] |
| R packages (gemtc, pcnetmeta) | Frequentist and Bayesian network meta-analysis | Consistency evaluation and network visualization |
| Stata network meta-analysis package | Statistical analysis of treatment networks | Implementation of various inconsistency models |
| Cochrane Collaboration Tool | Risk of bias assessment | Evaluating methodological quality of included trials |
Methodology:
Network Mapping: Create a network diagram visualizing all available direct comparisons between treatments.
Consistency Model Estimation: Fit a consistency model to the complete network using Bayesian or frequentist methods.
Inconsistency Model Estimation: Fit an inconsistency model that allows for disagreement between direct and indirect evidence.
Model Comparison: Compare consistency and inconsistency models using appropriate statistical measures:
- Bayesian Approach: Compare posterior model fits using deviance information criterion (DIC) or Bayes factors
- Frequentist Approach: Use likelihood ratio tests for fixed-effect models
Local Inconsistency Assessment: For networks with multiple loops, apply node-splitting methods to evaluate consistency for each specific comparison.
Sensitivity Analysis: Investigate the impact of excluding trials with high risk of bias or particular clinical characteristics on consistency.
Reporting: Document all consistency assessments, including both global and local evaluations, with measures of uncertainty [66] [2] [67].
Workflow for Consistency Evaluation in MTC
The following diagram illustrates the sequential process for evaluating consistency in mixed treatment comparisons:
Case Study Applications and Findings
Nocturnal Enuresis Treatments
A published overview of treatments for childhood nocturnal enuresis provides an illustrative application of MTC consistency assessment. The evidence network included eight distinct treatments and ten pairwise comparisons, forming a connected network through both direct and indirect evidence pathways [2].
The analysis revealed important findings regarding consistency:
Fixed-effect models showed significant inconsistency, with two of three indirect estimates significantly different from direct estimates based on the composite test (χ² test P < 0.05).
Random-effects models demonstrated consistency between direct and indirect evidence, forming a coherent basis for decision-making.
The case highlighted how overviews of reviews that simply present separate pairwise meta-analyses without MTC synthesis can lead to incoherent conclusions about which treatment is most effective [2].
Febrile Neutropenia Prevention
A case study examining granulocyte colony-stimulating factors for preventing febrile neutropenia after chemotherapy demonstrated substantial inconsistency between direct and indirect evidence:
The median odds ratio of febrile neutropenia for primary pegfilgrastim versus no primary G-CSF was 0.06 based on direct evidence, but 0.27 based on indirect evidence (P value for consistency hypothesis 0.027).
Additional trials conducted after the original analysis were consistent with the earlier indirect evidence rather than the direct evidence.
The inconsistency was traced to one specific trial comparing primary pegfilgrastim with no primary G-CSF, which was inconsistent with the evidence as a whole [67].
This case challenged the common preference for direct evidence over indirect evidence, demonstrating that direct evidence is not always more reliable.
Table 3: Consistency Assessment Findings Across Case Studies
| Clinical Area | Network Characteristics | Consistency Findings | Implications |
|---|---|---|---|
| Nocturnal Enuresis | 8 treatments, 10 direct comparisons | Fixed-effect models inconsistent; Random-effects models consistent | Importance of accounting for heterogeneity in MTC |
| Febrile Neutropenia Prevention | Multiple G-CSF treatments | Significant inconsistency between direct and indirect evidence | Direct evidence not always more reliable than indirect |
| Stroke Prevention in AF | Multiple anticoagulation therapies | Inconsistency identified and addressed through appropriate modeling | Need for careful consistency evaluation in health technology assessment |
Advanced Topics and Future Methodological Developments
Addressing Between-Study Heterogeneity
Between-study heterogeneity presents significant challenges for consistency assessment in MTC. Several advanced methods have been developed to address this issue:
Meta-Regression Approaches: Incorporate study-level covariates to explain heterogeneity and reduce inconsistency.
Multivariate Random-Effects Models: Account for correlated effects across multiple treatment comparisons.
Hierarchical Related Regression: Model the relationship between treatment effects and study characteristics in a hierarchical framework.
These approaches are particularly important when synthesizing evidence from mixed populations, such as in precision medicine where biomarker status may influence treatment effects [19].
Synthesis of Mixed Biomarker Populations
Recent methodological developments address the challenge of synthesizing evidence from trials with mixed biomarker populations:
Methods for Aggregate Data: Approaches that utilize only summary statistics from published trials, including methods that incorporate subgroup analysis results.
Individual Participant Data Methods: Utilize patient-level data to adjust for biomarker status and other prognostic factors.
Hybrid Approaches: Combine both aggregate and individual participant data to maximize the use of available evidence [19].
These methods are particularly relevant in oncology, where targeted therapies may be effective only in specific genetic subgroups, as demonstrated in the case of EGFR-targeted therapies in metastatic colorectal cancer stratified by KRAS mutation status [19].
Evaluating coherence and consistency between direct and indirect evidence represents a critical component of mixed treatment comparison methodology. As the application of MTC continues to grow in health technology assessment and evidence-based medicine, rigorous consistency assessment remains essential for producing valid and reliable treatment effect estimates. The methodological framework outlined in this guide provides researchers with structured approaches to detect, evaluate, and address inconsistency in treatment networks.
The case studies demonstrate that while inconsistency between direct and indirect evidence can occur, statistical methods are available to identify and investigate these discrepancies. Furthermore, these cases challenge the conventional hierarchy that privileges direct evidence over indirect evidence, suggesting that a more robust strategy involves combining all relevant and appropriate information, whether direct or indirect, while carefully evaluating their consistency [67].
As MTC methodology continues to evolve, future developments will likely enhance our ability to synthesize evidence from complex networks, address heterogeneity more effectively, and extend these methods to new applications such as precision medicine and mixed biomarker populations. Through continued methodological refinement and application, MTC will remain an invaluable tool for comparative effectiveness research and healthcare decision-making.
Regulatory Acceptance and Use of MTC in Drug Development and Policy
Mixed Treatment Comparison (MTC), also known as network meta-analysis, has emerged as a critical methodological framework for comparative effectiveness research in drug development and health policy. This technical guide examines the regulatory acceptance, methodological standards, and practical applications of MTC models within the evolving landscape of evidence synthesis. As healthcare decision-makers increasingly require comparisons among multiple treatment options, MTC provides a statistical approach for integrating both direct and indirect evidence across a network of interventions. The adoption of MTC has grown substantially since 2009, with applications spanning health technology assessment, regulatory decision-making, and clinical guideline development [15]. This review synthesizes current methodologies, regulatory frameworks, and implementation considerations to provide researchers and drug development professionals with comprehensive guidance on the appropriate use and acceptance of MTC in evidence generation.
Mixed Treatment Comparison represents an extension of traditional pairwise meta-analysis that enables simultaneous comparison of multiple interventions through a connected network of trials. Unlike standard meta-analysis that compares only two treatments at a time, MTC incorporates all available direct and indirect evidence to provide coherent estimates of relative treatment effects across all interventions in the network [30]. This methodology is particularly valuable in drug development when head-to-head trials are unavailable for all relevant comparisons, allowing researchers to fill evidence gaps while maximizing the use of available clinical trial data.
The fundamental principle underlying MTC is the integration of direct evidence (from trials directly comparing treatments of interest) with indirect evidence (obtained through a common comparator) within a single statistical framework. This approach preserves the randomization of the original trials while providing estimates for treatment comparisons that may not have been studied in direct head-to-head trials [60] [16]. The development of MTC methodology can be traced back to the 1990s, with significant methodological advances occurring since 2003, particularly through Bayesian implementation that enables probabilistic interpretation of treatment effects and ranking [15] [16].
MTC has gained recognition from major health technology assessment agencies worldwide, including the UK's National Institute for Health and Care Excellence (NICE), the Australian Pharmaceutical Benefits Advisory Committee (PBAC), and the Canadian Agency for Drugs and Technologies in Health (CADTH) [60]. Its applications span diverse therapeutic areas, with particularly valuable implementation in oncology, cardiovascular disease, diabetes, and rare diseases where multiple treatment options exist but comprehensive direct comparison evidence is lacking.
Methodological Foundations
Core Statistical Framework
The statistical foundation of MTC relies on connecting treatment effects through a network of comparisons. The basic model extends standard random-effects meta-analysis to multiple treatments. For a multi-arm trial comparing treatments A, B, and C, the effects are modeled with correlations between treatment effects estimated from the same trial [19].
The Bayesian framework has undergone substantial development for MTC implementation. The model can be specified as follows for a random-effects network meta-analysis:
For a trial ( i ) comparing treatments ( A ) and ( B ): [ \text{logit}(p{iA}) = \mui ] [ \text{logit}(p{iB}) = \mui + \delta{iAB} ] where ( \delta{iAB} \sim N(d{AB}, \tau^2) ) represents the treatment effect of B relative to A, with ( d{AB} ) being the mean effect and ( \tau^2 ) the between-trial variance [19].
The consistency assumption is fundamental to MTC, requiring that direct and indirect evidence estimate the same parameters. For example, the indirect comparison of A vs. C through B should be consistent with the direct comparison: ( d{AC} = d{AB} + d_{BC} ) [15] [16].
Key Assumptions and Validity Considerations
The validity of MTC depends on three critical assumptions:
- Similarity: Trials included in the network should be sufficiently similar in terms of clinical and methodological characteristics that would not预期 affect relative treatment effects [1].
- Homogeneity: The treatment effects should be similar across trials within each direct comparison [16].
- Consistency: The direct and indirect evidence should agree within statistical sampling error [16].
Violations of these assumptions can lead to biased estimates. Assessment of these assumptions involves evaluating clinical and methodological heterogeneity across trials, statistical tests for inconsistency, and sensitivity analyses [15].
Figure 1: Foundational Assumptions for Valid Mixed Treatment Comparisons
Regulatory Evolution and Current Status
Historical Development of Regulatory Acceptance
The regulatory acceptance of MTC has evolved significantly over the past two decades. Initial methodological work on indirect comparisons emerged in the 1990s, with Bucher et al.'s 1997 paper on adjusted indirect comparisons representing a key milestone [60] [16]. The foundational concepts for MTC were further developed throughout the early 2000s, with Lu and Ades (2004) establishing the Bayesian framework that enabled more complex network meta-analyses [15].
The period from 2009 onward witnessed a marked increase in published systematic reviews incorporating MTC, reflecting growing acceptance within the research community [15]. Regulatory and health technology assessment bodies began formally recognizing the value of MTC approaches, with organizations including NICE, PBAC, and CADTH incorporating MTC evidence into their assessment processes [60]. Among major regulatory agencies, the US Food and Drug Administration (FDA) has specifically mentioned adjusted indirect comparisons in its guidelines, representing an important step toward formal regulatory acceptance [60].
Current Regulatory Framework
The current regulatory landscape for MTC is characterized by increasing formalization within drug development and assessment frameworks. The International Council for Harmonisation (ICH) M15 guidelines on Model-Informed Drug Development (MIDD), released as a draft for public consultation in November 2024, represent the most significant recent development [69]. These guidelines aim to harmonize expectations regarding documentation standards, model development, data quality, and model assessment for MIDD approaches, including MTC.
The Prescription Drug User Fee Act Reauthorization VI (PDUFA) of 2017 catalyzed FDA efforts to incorporate innovative methodologies, including biomarkers, real-world evidence, and alternative clinical trial designs into the drug approval process [69]. This created a more receptive environment for MTC approaches, particularly in contexts where traditional trial designs are impractical or unethical.
Table 1: Regulatory Timeline for MTC Acceptance
| Year | Regulatory Development | Significance |
|---|---|---|
| 1997 | Bucher et al. introduce adjusted indirect comparisons | Established statistical foundation for indirect treatment comparisons [60] |
| 2004 | Lu and Ades publish Bayesian MTC framework | Enabled complex network meta-analyses with multiple treatments [15] |
| 2009 | Marked increase in MTC publications | Reflected growing research community acceptance [15] |
| 2017 | PDUFA VI provisions for innovative trial designs | Created regulatory pathway for MTC incorporation [69] |
| 2024 | ICH M15 MIDD draft guidelines released | Provided harmonized framework for MTC in drug development [69] |
Implementation in Drug Development
MTC Workflow and Best Practices
Implementing MTC in drug development follows a structured workflow that aligns with the ICH M15 MIDD framework. The process begins with planning that defines the Question of Interest (QOI), Context of Use (COU), and Model Influence, followed by implementation, evaluation, and submission stages [69].
The key stages in the MTC process include:
- Systematic Literature Review: Comprehensive identification of all relevant studies using predefined search strategies and inclusion criteria, following PRISMA guidelines [1].
- Data Extraction and Quality Assessment: Standardized extraction of study characteristics, patient demographics, interventions, comparators, outcomes, and methodological quality indicators.
- Network Geometry Evaluation: Assessment of the connectedness of the treatment network and identification of potential comparators.
- Model Selection and Fitting: Choice between fixed-effect and random-effects models based on heterogeneity assessment, with model fit evaluated using residual deviance and other goodness-of-fit statistics [16].
- Consistency and Sensitivity Analysis: Evaluation of the consistency assumption and assessment of result robustness through sensitivity analyses.
Figure 2: MTC Implementation Workflow in Drug Development
Applications Across Drug Development Stages
MTC methodologies provide value across multiple stages of the drug development continuum:
- Early Development: Informing target product profiles and trial design by identifying comparative efficacy benchmarks and evidence gaps.
- Clinical Development: Supporting dose selection and go/no-go decisions by contextualizing phase II results against established treatments.
- Registration and Labeling: Providing comparative effectiveness evidence for health technology assessment submissions and product labeling.
- Lifecycle Management: Informing additional indications and combination strategies by evaluating relative efficacy across patient subpopulations.
In the context of precision medicine, MTC methods have been adapted to address challenges posed by mixed biomarker populations across trials. For example, in metastatic colorectal cancer, MTC approaches have been used to synthesize evidence from trials with varying biomarker statuses (KRAS wild-type vs. mutant) to inform targeted therapy development [19].
Comparative Analysis of MTC Methodologies
MTC Versus Alternative Approaches
MTC offers distinct advantages and limitations compared to alternative evidence synthesis methods. Understanding these distinctions is crucial for selecting the appropriate analytical approach for a given research question.
Table 2: Comparison of Evidence Synthesis Methods
| Method | Description | Advantages | Limitations |
|---|---|---|---|
| Naïve Direct Comparison | Direct comparison of results from different trials without adjustment | Simple to implement and interpret | Violates randomization; susceptible to confounding and bias [60] |
| Adjusted Indirect Comparison | Indirect comparison through common comparator using Bucher method | Preserves randomization; accepted by HTA bodies | Limited to comparisons with common comparator; increased uncertainty [60] [16] |
| Mixed Treatment Comparison | Integrated analysis of direct and indirect evidence across treatment network | Uses all available evidence; enables multiple treatment comparisons; provides treatment rankings | Complex implementation; requires consistency assumption; computationally intensive [30] [16] |
Evidence Synthesis in Complex Interventions
Component Network Meta-Analysis (CNMA) represents an extension of standard MTC that enables estimation of individual component effects within complex interventions. This approach is particularly valuable for evaluating multicomponent interventions, such as non-pharmacological strategies or combination therapies, by modeling the contributions of individual components and their potential interactions [50].
In CNMA, the additive model assumes that the total effect of a complex intervention equals the sum of its individual component effects, while interaction CNMA accounts for synergistic or antagonistic effects between components [50]. This approach provides enhanced insights for clinical decision-making and intervention optimization by identifying which components drive effectiveness.
Case Studies and Applications
Oncology Applications
MTC has been extensively applied in oncology drug development, where multiple treatment options often exist but comprehensive direct comparisons are lacking. A recent meta-analysis of immune checkpoint inhibitors in metastatic melanoma exemplifies the utility of MTC approaches, demonstrating superior long-term clinical benefit with combination therapy compared to monotherapy, albeit with increased toxicity [70].
This analysis incorporated 14 clinical trials with over 5,000 patients, using generalized linear mixed models (GLMMs) to account for study variability and provide robust estimates of treatment efficacy and risk. The findings supported evidence-based decision-making by quantifying the risk-benefit tradeoffs between different immunotherapeutic strategies [70].
Chronic Disease Management
In type 2 diabetes mellitus, where multiple drug classes with different mechanisms of action are available, MTC has been instrumental in informing treatment guidelines. With few head-to-head trials comparing newer drug classes (e.g., GLP-1 analogues and DPP4 inhibitors), MTC has provided essential evidence on their relative efficacies and safety profiles, supporting clinical decision-making in the absence of direct comparative trials [60].
Methodological Challenges and Limitations
Technical and Interpretative Challenges
Despite its advantages, MTC implementation faces several methodological challenges:
- Publication Bias: The tendency for positive results to be published more often than negative findings can skew MTC results, as published data form the core inputs for analysis [1].
- Network Connectivity: Treatments must be connected through a network of comparisons, which may not always be possible if some interventions lack a common comparator.
- Statistical Heterogeneity: Variability in treatment effects across studies can impact the validity and interpretation of MTC results, requiring careful assessment and potential use of random-effects models [19].
- Computational Complexity: Bayesian MTC implementations often require Markov chain Monte Carlo (MCMC) simulation and specialized software, presenting computational challenges [16].
Regulatory and Evidence Standards
Regulatory acceptance of MTC evidence requires demonstration of methodological rigor and validity. Key considerations include:
- Transparent Reporting: Complete documentation of search strategies, inclusion criteria, analytical methods, and sensitivity analyses following PRISMA extensions for network meta-analysis [1].
- Assumption Validation: Comprehensive assessment of similarity, homogeneity, and consistency assumptions through statistical and clinical evaluation.
- Model Credibility: Adherence to credibility frameworks, such as the ASME V&V 40-2018 standard incorporated in ICH M15 guidelines, which provide a structured approach for evaluating model credibility [69].
Future Directions and Emerging Applications
The future evolution of MTC methodology involves integration with diverse data sources and analytical frameworks. Model-Informed Drug Development (MIDD) approaches are increasingly incorporating real-world evidence (RWE) to complement clinical trial data, enhancing the generalizability and contextualization of MTC findings [71] [69].
Artificial intelligence and machine learning approaches are being explored to enhance MTC through automated literature screening, data extraction, and model selection. These technologies have potential to improve the efficiency and reproducibility of MTC implementations while facilitating more complex modeling of treatment effect modifiers [71].
Methodological Innovations
Emerging methodological developments in MTC include:
- Individual Participant Data MTC: Combining aggregate data with individual participant data to enable more detailed subgroup analyses and exploration of treatment-covariate interactions [19].
- Multidimensional Evidence Synthesis: Integrating evidence across multiple outcomes and study designs while accounting for correlations between outcomes.
- Dynamic Treatment Regimens: Evaluating sequences of treatments rather than single interventions to better reflect clinical practice.
Table 3: Essential Methodological Toolkit for MTC Implementation
| Tool Category | Specific Tools/Software | Application in MTC |
|---|---|---|
| Statistical Software | R, Python, WinBUGS, OpenBUGS | Model fitting, statistical analysis, and visualization [16] |
| Quality Assessment | Cochrane Risk of Bias, Jadad Scale | Study quality and bias risk evaluation [1] |
| Reporting Guidelines | PRISMA-NMA, ISPOR Good Practice Guidelines | Ensuring comprehensive and transparent reporting [15] [1] |
| Consistency Evaluation | Node-splitting, Inconsistency Factors | Assessing agreement between direct and indirect evidence [15] |
Mixed Treatment Comparison has evolved from a specialized methodological approach to an established framework for comparative effectiveness research in drug development and health policy. The regulatory acceptance of MTC continues to grow, supported by methodological advances, standardized implementation frameworks, and demonstrated value in addressing evidence gaps. The incorporation of MTC within the ICH M15 MIDD guidelines represents a significant milestone in its regulatory maturation, providing harmonized standards for model development, evaluation, and application.
For researchers and drug development professionals, successful implementation of MTC requires careful attention to methodological assumptions, transparent reporting, and appropriate interpretation of results. As healthcare decision-making increasingly demands comprehensive comparative evidence across all available treatments, MTC methodologies will continue to play an essential role in generating robust evidence to inform drug development, regulatory assessment, and clinical practice.
The Role of Individual Participant Data (IPD) in Enhancing MTC Validity
Mixed Treatment Comparisons (MTC), also known as network meta-analysis, represent a sophisticated statistical methodology that enables the simultaneous comparison of multiple interventions by synthesizing both direct and indirect evidence. This approach has gained substantial traction in health technology assessment and comparative effectiveness research, with published systematic reviews using MTC methods showing a marked increase since 2009 [15]. The fundamental strength of MTC lies in its ability to provide coherent effect estimates for all treatment comparisons within a connected network, even for pairs that have never been directly compared in head-to-head randomized controlled trials (RCTs) [3] [15].
Traditional MTC models typically rely on aggregate data (AD) extracted from published study reports. However, this approach presents significant methodological limitations, including an inability to investigate effect modification at the participant level and susceptibility to ecological bias [19] [72]. The integration of Individual Participant Data (IPD) – the raw data for each participant in a clinical trial – addresses these limitations and enhances the validity and utility of MTC. IPD-MA is increasingly recognized as the 'gold standard' for evidence synthesis, offering substantial improvements to the quantity, quality, and analytical scope of meta-analyses [73] [74]. When even a fraction of studies in an evidence network contribute IPD, it can markedly improve the accuracy of treatment-covariate interaction estimates and reduce inconsistencies within networks [75].
Methodological Advantages of IPD in MTC
Overcoming Limitations of Aggregate Data
The integration of IPD into MTC frameworks addresses several critical limitations inherent to AD-based approaches. Ecological bias, also known as aggregation bias, occurs when relationships observed at the group level (e.g., study-level summaries) do not reflect the true relationships at the individual level [19] [72]. IPD allows for proper investigation of participant-level characteristics and their interaction with treatment effects, thereby eliminating this source of bias. Furthermore, IPD enables standardization of analytical approaches across studies, including consistent application of inclusion/exclusion criteria, outcome definitions, and statistical methods [73] [72]. This is particularly valuable in MTC, where variability in these elements across studies can threaten the validity of transitivity assumptions.
Access to IPD also enhances data quality and completeness. Researchers can check data integrity, verify randomization processes, handle missing data more appropriately, and obtain more complete follow-up information [72] [74]. Perhaps most importantly, IPD facilitates the investigation of treatment-covariate interactions at the participant level, enabling identification of subgroups that may benefit more or less from specific interventions [75] [72]. This is especially crucial in the context of precision medicine, where treatments may target specific biomarker subgroups [19].
Advanced Analytical Capabilities
The availability of IPD significantly expands the analytical possibilities within MTC frameworks. With IPD, researchers can perform adjusted analyses to account for imbalances in prognostic factors across treatment arms, even when such adjustments were not performed in the original trial publications [72]. IPD also enables more sophisticated exploration of heterogeneity by allowing simultaneous examination of study-level and participant-level sources of variation in treatment effects [72].
In the context of time-to-event outcomes, IPD provides particular advantages by allowing standardization of time points across studies and facilitating more sophisticated survival analyses [72] [74]. When trials have different follow-up times, IPD allows analysis at multiple consistent time points, enhancing the comparability of treatment effects across studies [72]. Additionally, IPD offers greater flexibility in investigating multiple outcomes from the same set of trials and examining long-term outcomes that may not have been reported in original publications [72] [74].
Table 1: Comparative Analysis of Aggregate Data versus Individual Participant Data in MTC
| Analytical Aspect | Aggregate Data (AD) | Individual Participant Data (IPD) |
|---|---|---|
| Covariate Adjustment | Limited to study-level covariates | Enables adjustment for participant-level prognostic factors |
| Effect Modification | Prone to ecological bias | Direct investigation of participant-level treatment-covariate interactions |
| Data Quality | Dependent on published reporting | Allows data verification and enhancement |
| Outcome Definitions | Variable across studies | Standardization possible across studies |
| Missing Data | Difficult to address appropriately | Multiple appropriate handling methods available |
| Time-to-Event Analysis | Limited to published time points | Analysis at consistent time points across studies |
Practical Implementation of IPD-MTC
Statistical Models for IPD Integration
Integrating IPD into MTC involves sophisticated statistical models that can accommodate both individual-level and aggregate-level data. The Bayesian framework has undergone substantial development for this purpose and provides a flexible approach for combining different data types [15] [75] [19]. A series of novel Bayesian statistical MTC models have been developed to allow for the simultaneous synthesis of IPD and AD, potentially incorporating both study-level and individual-level covariates [75].
The fundamental distinction in analytical approaches for IPD-MTC lies between one-stage and two-stage methods [73] [72]. In the two-stage approach, the IPD are first analyzed separately in each study to produce study-specific estimates of relative treatment effect (and possible treatment-covariate interactions). These estimates are then combined in the second stage using standard meta-analysis techniques [19] [72]. This approach is conceptually straightforward and allows verification of each study's results, but may not fully account for the hierarchical structure of the data.
In contrast, the one-stage approach analyzes IPD from all studies simultaneously using a single hierarchical model [73] [72]. This method models the participant-level data directly while accounting for clustering of participants within studies. The one-stage approach offers greater flexibility for complex modeling, including non-normal random effects and more sophisticated covariance structures, but requires more computational resources and may face convergence issues with complex models [73] [72]. Under certain conditions, both approaches yield similar treatment effect estimates, though the one-stage approach is generally preferred for its statistical efficiency when modeling participant-level covariates [72].
Figure 1: IPD-MTC Implementation Workflow
Handling Mixed Biomarker Populations with IPD-MTC
A particularly valuable application of IPD-MTC arises in the context of precision medicine, where treatment effects may depend on biomarker status [19]. The development of targeted therapies often results in an evidence base consisting of trials with mixed populations – some including all-comers regardless of biomarker status, others focusing exclusively on biomarker-positive subgroups, and some including both groups with subgroup analyses [19]. This heterogeneity poses significant challenges for traditional meta-analysis methods.
IPD-MTC provides a framework for synthesizing evidence from these mixed biomarker populations [19]. When IPD are available, researchers can standardize biomarker definitions across studies, consistently classify participants into relevant subgroups, and directly estimate biomarker-treatment interactions. Even when IPD are available for only a subset of studies in the network, incorporating this information can substantially improve the accuracy of subgroup effect estimates and help resolve inconsistencies [75] [19]. For instance, in the context of metastatic colorectal cancer, where treatments like Cetuximab and Panitumumab were found to be effective only in KRAS wild-type patients, IPD-MTC methods can synthesize evidence from trials conducted in different biomarker populations over time [19].
Table 2: Methods for Evidence Synthesis in Mixed Biomarker Populations
| Method Category | Data Requirements | Key Applications | Statistical Considerations |
|---|---|---|---|
| Pairwise Meta-Analysis using AD | Aggregate data only | Limited to direct comparisons; basic subgroup analysis | High risk of ecological bias; limited power |
| Network Meta-Analysis using AD | Aggregate data from connected network | Comparing multiple treatments; limited exploration of biomarker effects | Assumes consistency between direct and indirect evidence |
| Network Meta-Analysis using AD and IPD | Combination of aggregate and individual-level data | Exploring treatment-biomarker interactions; synthesizing mixed populations | Reduces ecological bias; improves precision of interaction estimates |
Technical Requirements and Methodological Considerations
Data Acquisition and Harmonization
The IPD-MTC process begins with systematic identification of relevant trials through comprehensive searches of published and unpublished literature [74]. This is followed by the collaborative effort of obtaining IPD from trial investigators, which requires clear communication, data sharing agreements, and ethical approvals [73] [76]. The process typically involves inviting trial investigators to participate formally and requesting the necessary documents, including ethics approvals and data sharing agreements [73].
Once obtained, IPD must be harmonized across studies – a critical step that involves creating a master codebook to standardize data elements, mapping study-specific variables to common definitions, and conducting rigorous quality checks [73]. This harmonization process enables resolution of differences in inclusion criteria, outcome definitions, and variable coding across trials [73] [72]. For example, in an IPD meta-analysis of childhood acute lymphoblastic leukemia, the age criterion was standardized to ≤21 years to resolve differences in age cut-offs used in trials across different countries [73].
The Researcher's Toolkit: Essential Methodological Components
Table 3: Research Reagent Solutions for IPD-MTC
| Component | Function | Implementation Considerations |
|---|---|---|
| Bayesian Hierarchical Models | Simultaneously synthesizes IPD and AD while accounting for data structure | Requires specification of prior distributions; computationally intensive |
| Consistency Assessment | Verifies agreement between direct and indirect evidence within the network | Essential for validating MTC assumptions; can use node-splitting or other approaches |
| One-Stage IPD Analysis | Direct analysis of raw participant data from multiple studies | Maximum statistical efficiency; computationally challenging with complex models |
| Two-Stage IPD Analysis | Separate analysis of each study followed by synthesis | More computationally manageable; allows verification of individual study results |
| Missing Data Handling | Addresses incomplete participant data across studies | Multiple imputation or maximum likelihood methods preferred over complete-case analysis |
| Sensitivity Analysis | Assesses robustness of findings to different assumptions | Should include scenarios with different priors, inclusion criteria, and model structures |
The integration of Individual Participant Data into Mixed Treatment Comparisons represents a significant methodological advancement in evidence synthesis. By overcoming the limitations of aggregate data and enabling more sophisticated investigation of treatment-effect heterogeneity, IPD-MTC provides more detailed, robust, and clinically relevant results. The ability to examine participant-level characteristics and their interaction with treatments is particularly valuable in the era of precision medicine, where therapies may target specific biomarker-defined subgroups.
While IPD-MTC requires substantial resources and collaborative efforts, its potential to inform health care decision-making, clinical guidelines, and future research is considerable. As methods continue to evolve and access to IPD improves, this approach will likely play an increasingly important role in generating reliable evidence for comparing healthcare interventions. Future work should focus on developing standardized practices for implementing IPD-MTC, addressing challenges related to data sharing, and establishing consensus on methodological standards for conduct and reporting.
Conclusion
Mixed Treatment Comparison has established itself as an indispensable methodology in evidence-based medicine, enabling a more complete and powerful synthesis of the available evidence for comparing multiple healthcare interventions. Its rapid adoption since 2009 underscores its value for health technology assessment and clinical decision-making, particularly in the absence of direct head-to-head trials. Successful implementation hinges on the careful assessment of key assumptions like consistency and homogeneity, the selection of an appropriate statistical framework, and rigorous validation of results. Future advancements will likely focus on standardizing terminology and reporting, developing more robust methods for complex data scenarios like mixed biomarker populations, and further integrating MTC within the model-informed drug development paradigm to optimize the entire therapeutic development lifecycle.
References
- 1. Meta-analysis and Mixed Treatment Comparison Analysis [https://www.ismpp-newsletter.com/2017/03/30/meta-analysis-and-mixed-treatment-comparison-analysis-powerful-tools-with-benefits-and-challenges/]
- 2. Mixed treatment comparison analysis provides internally ... [https://www.sciencedirect.com/science/article/abs/pii/S0895435609003072]
- 3. Methods for Indirect Treatment Comparison: Results from a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11036291/]
- 4. Critical evaluation of mixed treatment comparison meta†... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6878270/]
- 5. Understanding Network Metaâ€Analysis: A Practical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271649/]
- 6. A methodological review of network meta-analyses applied ... [https://www.sciencedirect.com/science/article/pii/S0895435625001891]
- 7. Evaluating the Feasibility of a Network Meta-Analysis ... [https://www.ispor.org/heor-resources/presentations-database/presentation-cti/ispor-2025/poster-session-4/evaluating-the-feasibility-of-a-network-meta-analysis-comparing-treatment-options-in-polycythemia-vera]
- 8. Is network meta-analysis as valid as standard pairwise meta ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-11-159]
- 9. Consistency and inconsistency in network meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4433772/]
- 10. Node-Splitting Generalized Linear Mixed Models for ... [https://www.sciencedirect.com/science/article/pii/S1098301516305812]
- 11. A graphical tool for locating inconsistency in network meta ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-13-35]
- 12. Conducting pairwise and network meta-analyses in updated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11892990/]
- 13. Concepts and emerging issues of network meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8497908/]
- 14. Network meta-analysis: a powerful tool for clinicians ... [https://www.sciencedirect.com/science/article/pii/S0895435624002932]
- 15. Review of mixed treatment comparisons in published ... [https://www.sciencedirect.com/science/article/abs/pii/S0895435613003065]
- 16. Incorporating multiple interventions in meta-analysis ... - Trials [https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-10-86]
- 17. The key assumptions of network meta-analysis [https://www.quantics.co.uk/blog/the-key-assumptions-of-network-meta-analysis/]
- 18. Assumptions of Mixed Treatment Comparisons in Health ... [https://journals.plos.org/plosone/article?id=10.1371%2Fjournal.pone.0160712]
- 19. Combining treatment effects from mixed populations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11963434/]
- 20. Methods - Use of Mixed Treatment Comparisons in Systematic ... [https://www.ncbi.nlm.nih.gov/books/NBK107331/]
- 21. The development of network meta-analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9340098/]
- 22. Network meta-analysis: a technique to gather evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5386629/]
- 23. The development of network meta-analysis. [https://www.jameslindlibrary.org/articles/the-development-of-network-meta-analysis/]
- 24. Discussion - Findings of Bayesian Mixed Treatment ... [https://www.ncbi.nlm.nih.gov/books/NBK126112/]
- 25. Case Study Comparing Bayesian and Frequentist Approaches ... [https://www.ncbi.nlm.nih.gov/books/NBK132725/]
- 26. When (if ever) is a frequentist approach substantively better ... [https://stats.stackexchange.com/questions/194035/when-if-ever-is-a-frequentist-approach-substantively-better-than-a-bayesian]
- 27. Comparing Bayesian and frequentist approaches for multiple ... [https://scholars.duke.edu/display/pub1349837]
- 28. A comparison of frequentist and Bayesian approaches to the ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02537-x]
- 29. Comparison of frequentist and Bayesian network meta ... [https://www.sciencedirect.com/science/article/pii/S2213398418300137]
- 30. Introduction - Use of Mixed Treatment Comparisons in ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK107325/]
- 31. CONSORT 2025 explanation and elaboration - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11995452/]
- 32. Multi-level network meta-regression: A step forward in HTA ... [https://www.cencora.com/resources/pharma/htaq-winter-2025-summary/multi-level-network-meta-regression]
- 33. and arm-synthesis models for network meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527487/]
- 34. Improved analysis of in vivo drug combination experiments ... [https://www.nature.com/articles/s41467-025-65218-9]
- 35. Incorporating data from various trial designs into a mixed treatment comparison model - PubMed [https://pubmed.ncbi.nlm.nih.gov/23440610/]
- 36. An Overview of Sarcopenia: Focusing on Nutritional ... [https://www.mdpi.com/2072-6643/17/7/1237]
- 37. The effectiveness of sarcopenia interventions for cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8627517/]
- 38. Matching-Adjusted Indirect Comparison Studies in Oncology [https://pubmed.ncbi.nlm.nih.gov/39999561/]
- 39. Network Meta-Analysis (Mixed Treatment Comparison ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK536651/]
- 40. Advanced Methods for Matching-Adjusted Indirect ... [https://www.ispor.org/heor-resources/presentations-database/presentation/intl2024-3856/17844]
- 41. Combining treatment effects from mixed populations in meta ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02507-3]
- 42. A mathematical framework for comparison of intermittent ... [https://www.nature.com/articles/s41540-024-00461-2]
- 43. Network Meta-Analysis: An Introduction for Clinicians - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5247317/]
- 44. Chapter 11: Undertaking network meta-analyses [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-11]
- 45. Dynamic Mixed Data Analysis and Visualization [https://www.mdpi.com/1099-4300/24/10/1399]
- 46. AI-driven predictive biomarker discovery with contrastive ... [https://www.sciencedirect.com/science/article/pii/S1535610825001308]
- 47. Integrated modeling of biomarkers, survival and safety in ... [https://www.sciencedirect.com/science/article/pii/S0169409X24002989]
- 48. Meta-analysis with zero-event studies: a comparative study ... [https://mmrjournal.biomedcentral.com/articles/10.1186/s40779-021-00331-6]
- 49. A proposed framework to guide evidence synthesis ... [https://www.sciencedirect.com/science/article/pii/S0895435621000494]
- 50. Analysing complex interventions using component network ... [https://www.medrxiv.org/content/10.1101/2025.06.30.25330567v1.full-text]
- 51. Selection of indirect treatment comparisons for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11938225/]
- 52. Assumptions of Mixed in Health Technology... Treatment Comparisons [https://pmc.ncbi.nlm.nih.gov/articles/PMC4979893/]
- 53. Antifungal treatment for invasive Candida infections: a mixed ... [https://ann-clinmicrob.biomedcentral.com/articles/10.1186/1476-0711-8-23]
- 54. Estimating power in (generalized) linear mixed models [https://link.springer.com/article/10.3758/s13428-021-01546-0]
- 55. Power and sample size analysis for longitudinal mixed models ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-022-01819-y]
- 56. Optimal allocation to treatments in a sequential multiple ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8649474/]
- 57. Good Practices for Health Technology Assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11703621/]
- 58. Acceptance of Artificial Intelligence in Evidence and ... [https://www.putassoc.com/insights/acceptance-of-artificial-intelligence-in-evidence-and-dossier-developments-by-hta-bodies-challenges-and-opportunities/]
- 59. Multiple treatment comparison meta-analyses: a step ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3130904/]
- 60. Overview of methods for comparing the efficacies of drugs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3895352/]
- 61. Mixed Treatment Comparison - York ... [https://www.yhec.co.uk/glossary-term/mixed-treatment-comparison/]
- 62. Meta-Analysis 101: What You Want to Know in the Era of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4115319/]
- 63. Meta-Analysis - an overview [https://www.sciencedirect.com/topics/neuroscience/meta-analysis]
- 64. Meta-analysis [https://en.wikipedia.org/wiki/Meta-analysis]
- 65. Interpreting Indirect Treatment Comparisons and Network ... [https://www.sciencedirect.com/science/article/pii/S1098301511014045]
- 66. Combination of direct and indirect evidence in mixed ... [https://pubmed.ncbi.nlm.nih.gov/15449338/]
- 67. Consistency between Direct and Indirect Trial Evidence [https://www.sciencedirect.com/science/article/pii/S1098301511014823]
- 68. Use of Indirect and Mixed Treatment Comparisons for ... [https://pubmed.ncbi.nlm.nih.gov/18767896/]
- 69. Scoping review of the role of pharmacometrics in model- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528282/]
- 70. Comparative Meta-Analysis of Survival, Risk, and ... [https://pubmed.ncbi.nlm.nih.gov/40725709/]
- 71. An AI Approach to Generating MIDD Assets Across the ... [https://link.springer.com/article/10.1208/s12248-023-00838-x]
- 72. Get real in individual participant data (IPD) metaâ€analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC5042043/]
- 73. Individual participant data (IPD) meta-analysis: An introduction [https://pmc.ncbi.nlm.nih.gov/articles/PMC11878366/]
- 74. Individual Participant Data (IPD) Meta-analyses of ... [https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1001855]
- 75. Mixed treatment comparisons using aggregate and ... [https://pubmed.ncbi.nlm.nih.gov/22764016/]
- 76. How should individual participant data (IPD) from publicly ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-015-0532-z]