Managing Inconsistency in Network Meta-Analysis: A Comprehensive Guide to Detecting and Resolving Direct-Indirect Evidence Conflicts
This article provides a comprehensive guide for researchers and drug development professionals on handling inconsistency between direct and indirect evidence in Network Meta-Analysis (NMA).
Managing Inconsistency in Network Meta-Analysis: A Comprehensive Guide to Detecting and Resolving Direct-Indirect Evidence Conflicts
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on handling inconsistency between direct and indirect evidence in Network Meta-Analysis (NMA). As NMA becomes increasingly vital for comparing multiple treatments simultaneously, ensuring the validity of its findings through proper inconsistency management is crucial. The content explores the fundamental concepts of inconsistency, including the assumptions of transitivity and coherence that underpin NMA validity. It details established and emerging methodological approaches for detection and quantification, such as node-splitting, design-by-treatment interaction models, and novel evidence-splitting techniques. The guide further addresses practical troubleshooting strategies for when inconsistency is identified, including the use of meta-regression and sensitivity analyses. Finally, it offers a comparative analysis of validation techniques and software implementation, empowering researchers to produce more reliable and clinically relevant evidence syntheses for informed decision-making in biomedical research.
Understanding Inconsistency: The Bedrock of Valid Network Meta-Analysis
Frequently Asked Questions (FAQs)
1. What is the fundamental difference between heterogeneity and inconsistency in Network Meta-Analysis?
Heterogeneity refers to variability in the treatment effects between different studies that are investigating the same pairwise comparison (e.g., Treatment A vs. Treatment B). It is a concept inherited from conventional pairwise meta-analysis. Inconsistency, on the other hand, occurs when the direct evidence (e.g., from studies directly comparing A and C) conflicts with the indirect evidence (e.g., evidence for A vs. C obtained through a common comparator B, via A vs. B and B vs. C studies) [1]. In essence, heterogeneity exists within a treatment comparison, while inconsistency exists between different sources of evidence (direct and indirect) for the same treatment comparison [2] [1].
2. What are the primary causes of inconsistency in a network?
Inconsistency can arise from several factors, often related to differences in the studies that contribute to different comparisons in the network. Key causes include:
- Effect Modifiers: When the distribution of effect modifiers (e.g., disease severity, patient age, dose of a drug) differs across the sets of studies making different treatment comparisons [2].
- Bias: Different types of bias (e.g., optimism bias, publication bias, sponsorship bias) may act differently in studies of different comparisons [2].
- Protocol Differences: Fundamental differences in the versions of a treatment used in different comparisons (e.g., different doses or formulations of Treatment B in studies of A vs. B and studies of B vs. C) or differences in the settings or time periods in which studies were conducted [1].
3. What statistical methods are available to detect and quantify inconsistency?
Several statistical approaches have been developed, ranging from simple to complex. The table below summarizes the key methods, their approaches, and considerations for use.
Table 1: Key Statistical Methods for Assessing Inconsistency in NMA
| Method | Statistical Approach | What it Assesses | Key Considerations |
|---|---|---|---|
| Loop-based Approach [3] | Calculates the difference between direct and indirect evidence in a treatment loop. Tests the statistical significance of this difference. | Inconsistency within closed loops of three treatments. | Simple but can be cumbersome in large networks due to multiple testing. Not designed for networks with multi-arm trials [2] [1]. |
| Node-Splitting [2] | Separates the evidence for a specific comparison into direct and indirect components and tests for a discrepancy between them. | Local, comparison-specific inconsistency. | Provides a direct assessment of which specific comparisons are inconsistent. Can be computationally intensive as it tests one comparison at a time [2]. |
| Design-by-Treatment Interaction Model [1] | A global model that accounts for inconsistency by introducing interaction terms between designs and treatments. | Global inconsistency across the entire network. | Considered a general framework that successfully addresses complications from multi-arm trials. It encompasses both loop and design inconsistency [1]. |
| Inconsistency Parameter Approach (Lu & Ades) [1] | A Bayesian hierarchical model that relaxes the consistency assumption by including specific inconsistency parameters. | Global inconsistency. | Model choice (which parameters to include) can be arbitrary and, in the presence of multi-arm trials, can depend on the order of treatments [2] [1]. |
| Net Heat Plot [4] | A graphical tool that temporarily removes each design (set of treatments compared) one-by-one to visualize its contribution to network inconsistency. | A visual assessment to locate potential sources of inconsistency. | The underlying calculations constitute an arbitrary weighting of evidence and may not reliably signal or locate inconsistency [2]. |
4. How does the presence of multi-arm trials affect inconsistency assessment?
Multi-arm trials (trials with more than two treatment groups) complicate the assessment of inconsistency. A key principle is that inconsistency cannot occur within a single multi-arm trial because the treatment effects within the trial are internally consistent by design [1]. Therefore, standard loop-inconsistency methods, which assume all trials are two-armed, are not adequate. Methods like the Design-by-Treatment Interaction model are specifically designed to handle networks that include multi-arm trials correctly [1].
Troubleshooting Guides
Scenario 1: Your Network Contains a Closed Loop, and You Suspect Inconsistency
Problem: You have a network of interventions forming at least one closed loop (e.g., a triangle of A, B, and C, with studies for A-B, B-C, and A-C). You want to check if the direct and indirect evidence for one of the comparisons (e.g., A-C) are in agreement.
Step-by-Step Protocol:
- Visualize the Network: Begin by creating a network graph to understand the structure of your evidence. This helps identify all closed loops.
- Apply a Loop Inconsistency Test: For the loop in question (A-B-C), use the method described by Bucher et al. to calculate the inconsistency factor (IF) [3].
- Let
d_AB,d_BC, andd_ACbe the pooled direct estimates from meta-analyses of the A-B, B-C, and A-C studies, respectively. - The indirect estimate for A-C is:
ind_AC = d_AB + d_BC. - The inconsistency factor is:
IF = d_AC - ind_AC. - The variance of IF is:
var(IF) = var(d_AC) + var(d_AB) + var(d_BC). - A Z-test can be performed:
Z = IF / sqrt(var(IF)). A large absolute Z-value (e.g., |Z| > 1.96) suggests significant inconsistency in that loop.
- Let
- Confirm with Node-Splitting: To verify and localize the inconsistency, perform a node-split analysis for the A-C comparison. This will formally test the difference between the direct evidence for A-C and the indirect evidence for A-C obtained from the rest of the network [2].
- Investigate Clinically: If statistical inconsistency is found, investigate potential clinical or methodological reasons (e.g., differences in patient populations, interventions, or study quality across the A-B, B-C, and A-C studies) that could explain the conflict.
Scenario 2: You Need a Global Assessment of Inconsistency in a Complex Network
Problem: Your network has multiple treatments and complex loops, possibly including multi-arm trials. You need a single, overall test for inconsistency and to understand its distribution.
Step-by-Step Protocol:
- Fit a Consistency Model: First, fit a standard NMA model that assumes the consistency assumption holds throughout the network.
- Fit an Inconsistency Model: Next, fit a model that allows for inconsistency. The Design-by-Treatment Interaction model is a robust choice, especially if your network contains multi-arm trials [1].
- Compare Models: Statistically compare the fit of the consistency and inconsistency models. This is often done using the deviance information criterion (DIC) in a Bayesian framework. A lower DIC for the inconsistency model suggests a better fit, indicating that the consistency assumption may be violated. A large difference in DIC (e.g., > 5 points) is typically considered meaningful.
- Interpret and Explore: If global inconsistency is detected, use local methods like node-splitting or inspection of the inconsistency model parameters to identify which parts of the network are contributing most to the inconsistency.
Essential Research Reagent Solutions
Table 2: Key Software and Methodological Tools for NMA Inconsistency Analysis
| Item Name | Function / Application | Key Features |
|---|---|---|
R package netmeta [5] |
A comprehensive package for conducting frequentist NMA. | Implements various statistical methods for NMA, including the net heat plot [4] and component NMA models. Provides functions for generating network graphs. |
| Bayesian Frameworks (WinBUGS/OpenBUGS/JAGS/Stan) [6] | Provides a flexible environment for fitting complex hierarchical models. | Essential for implementing models like the Lu & Ades inconsistency model [1] and the Design-by-Treatment model. Allows for full quantification of uncertainty. |
| Design-by-Treatment Interaction Model [1] | A statistical model to account for global inconsistency. | Provides a general framework for inconsistency that is not reliant on arbitrary loop choices and correctly handles multi-arm trials. |
| Node-Splitting Method [2] | A technique to assess local inconsistency for individual comparisons. | Directly separates and tests direct and indirect evidence for each comparison, helping to pinpoint the source of conflict in a network. |
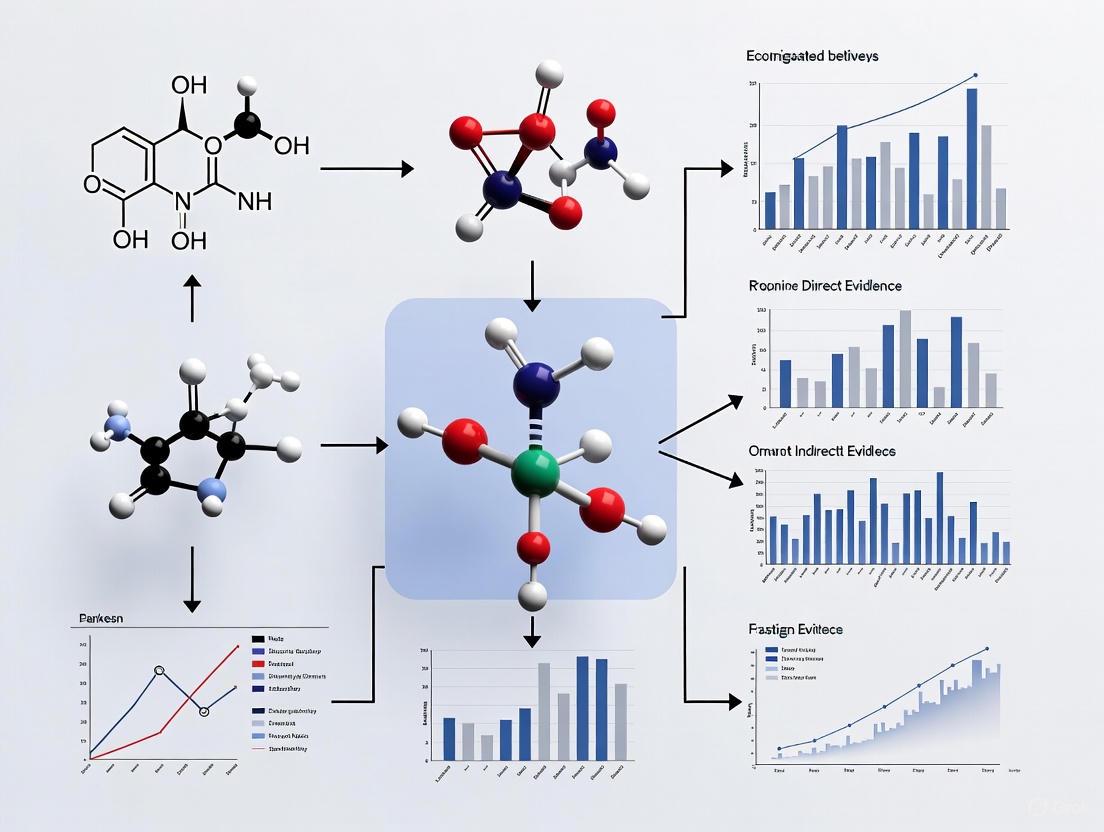
Supporting Visualizations
Diagram 1: Inconsistency Assessment Methods
Diagram 2: Loop Inconsistency Concept
Frequently Asked Questions
What are the core assumptions that ensure a Network Meta-Analysis is valid? The validity of an NMA rests on three critical, interconnected assumptions: transitivity, coherence (also known as consistency), and similarity. Transitivity and similarity are methodological assumptions about the included studies, while coherence is the statistical manifestation of these assumptions. If the studies in the network are similar enough (transitivity), then the direct and indirect evidence should agree (coherence) [7] [8] [9].
What should I do if my network shows significant inconsistency? Significant inconsistency indicates a violation of the transitivity assumption. You should [7] [9]:
- Re-examine Effect Modifiers: Investigate if study characteristics (PICO factors) are imbalanced across the treatment comparisons.
- Use Statistical Models: Employ models specifically designed to detect and handle inconsistency, such as the node-splitting method.
- Report the Findings: Clearly document the presence and extent of inconsistency in your results, as it affects the confidence in the network estimates.
How can the network's geometry itself be a source of bias? The structure of the evidence network (its geometry) can reveal biases in the underlying research. For example, if most trials only compare new drugs to an old standard rather than to each other, the network will be star-shaped. This can reflect commercial sponsorship biases where manufacturers choose favorable comparators. Such imbalances are a threat to transitivity and should be discussed in your review [9].
Troubleshooting Guides
Diagnosing and Resolving Incoherence
Incoherence occurs when different sources of evidence (e.g., direct and indirect) for the same treatment comparison disagree statistically [7]. Follow this diagnostic protocol:
Table: Protocol for Investigating Incoherence
| Step | Action | Key Tool/Method |
|---|---|---|
| 1. Confirm | Check if direct and indirect estimates disagree. | Node-splitting method; Incoherence models (e.g., side-split method) [7]. |
| 2. Investigate | Search for clinical/methodological dissimilarities (effect modifiers). | Subgroup analysis or meta-regression on potential effect modifiers [7] [9]. |
| 3. Act | Based on findings, present results and qualify conclusions. | Report separate direct/indirect estimates; use inconsistency models; discuss limitations [7]. |
Evaluating the Transitivity Assumption
Transitivity cannot be tested statistically but must be assessed qualitatively during the review process. Use this checklist to evaluate its plausibility [8] [9]:
Table: Checklist for Assessing Transitivity
| Aspect to Evaluate | Guiding Question | Mitigation Strategy |
|---|---|---|
| Population (P) | Would the participants in studies for different comparisons be eligible for the other comparisons in the network? | Define strict, uniform inclusion criteria. |
| Interventions (I) | Are the interventions and their delivery similar across comparisons? | Standardize the definition of each treatment node. |
| Comparators (C) | Are the control groups comparable in their standard of care? | Ensure common comparators are equivalent. |
| Outcomes (O) | Are the outcome measurements and timing similar? | Pre-define a core outcome set for the network. |
| Study Methods | Are the study designs and risk of bias similar? | Exclude studies with a high risk of bias that may introduce confounding. |
Quantitative Data and Experimental Protocols
Table: Summary of Key Statistical Measures for Coherence
| Statistical Measure | Formula | Interpretation | Use Case |
|---|---|---|---|
| Indirect Effect Estimate | (\hat{\theta}{\text{A,C}}^{\text{indirect}} = \hat{\theta}{\text{B,A}}^{\text{direct}} - \hat{\theta}_{\text{B,C}}^{\text{direct}}) [8] | The mathematically derived effect of A vs. C via common comparator B. | Foundational for all indirect evidence. |
| Variance of Indirect Estimate | (\text{Var} (\hat{\theta}{\text{A,C}}^{\text{indirect}}) = \text{Var} (\hat{\theta}{\text{B,A}}^{\text{direct}}) + \text{Var} (\hat{\theta}_{\text{B,C}}^{\text{direct}})) [8] | Quantifies the increased uncertainty of an indirect estimate. | Explains why indirect evidence is less precise. |
| Incoherence (ω) | ( \omega = \hat{\theta}{\text{A,C}}^{\text{direct}} - \hat{\theta}{\text{A,C}}^{\text{indirect}} ) | The difference between direct and indirect evidence. A value significantly different from zero indicates incoherence [7]. | Used in statistical models to measure inconsistency (e.g., design-by-treatment interaction model). |
Experimental Protocol: Node-Splitting Analysis This protocol is used to statistically test for local incoherence at specific comparisons [7].
- Objective: To detect disagreement between direct and indirect evidence for a specific treatment comparison.
- Method: For a given comparison (e.g., A vs. C), the model "splits" the evidence into two distinct parameters: one for the direct evidence and one for the indirect evidence.
- Analysis: The model estimates the difference between these two parameters. A statistically significant difference (p-value < 0.05) suggests incoherence for that comparison.
- Software: Can be implemented in Bayesian or frequentist software packages like
gemtcin R orBUGS/JAGS.
The Scientist's Toolkit
Table: Essential Reagents and Materials for NMA
| Item | Function |
|---|---|
| PRISMA-NMA Checklist | Ensures comprehensive and transparent reporting of the systematic review and NMA [9]. |
| Risk of Bias Tool (e.g., RoB 2.0) | Assesses the methodological quality of individual randomized trials, a key factor for assessing similarity/transitivity [7]. |
Statistical Software (R with netmeta, gemtc) |
Performs all statistical analyses, including meta-analysis, network estimation, and inconsistency checks [8]. |
| Network Geometry Map | A visual representation of the evidence base, highlighting well-connected treatments and evidence gaps [7] [9]. |
| SKA-111 | SKA-111, MF:C12H10N2S, MW:214.29 g/mol |
| SR9238 | SR9238, MF:C31H33NO7S2, MW:595.7 g/mol |
Logical and Conceptual Workflows
Transitivity and Coherence Relationship
Incoherence Investigation Workflow
In Network Meta-Analysis (NMA), inconsistency refers to statistical disagreement between direct and indirect evidence. This technical guide explores the sources and common causes of inconsistency, providing researchers with troubleshooting methodologies to identify and address these issues in clinical networks.
Frequently Asked Questions
What is inconsistency in Network Meta-Analysis? Inconsistency occurs when direct evidence (from head-to-head trials) and indirect evidence (from a connected network of trials) provide conflicting estimates of treatment effects [2]. This represents a violation of the consistency assumption, which is fundamental to the validity of NMA results [10].
How common is inconsistency in published NMAs? Empirical evidence from 201 published networks shows that evidence of inconsistency is present in a significant proportion of analyses [11] [12]:
Table: Prevalence of Inconsistency in Published Networks (n=201)
| Evidence Threshold | Prevalence | Interpretation |
|---|---|---|
| p-value < 0.05 | 14% of networks | Strong evidence of inconsistency |
| p-value < 0.10 | 20% of networks | Evidence of inconsistency |
Networks with many studies comparing few interventions were more likely to show evidence of inconsistency, likely due to higher statistical power to detect differences [12].
What are the primary sources of inconsistency?
- Violation of Transitivity: This occurs when the distribution of effect modifiers (patient characteristics, trial methodology, etc.) differs across treatment comparisons [10]. For example, if trials comparing Treatment A vs. B enrolled predominantly severe cases, while trials for A vs. C enrolled mild cases, the indirect comparison of B vs. C would be biased.
- Bias in Direct Comparisons: Inconsistency can arise when specific biases, such as publication bias, sponsorship bias, or optimism bias, affect certain direct comparisons differently within the network [2].
What is the relationship between heterogeneity and inconsistency? There is an inverse association between heterogeneity and the statistical power to detect inconsistency [11] [12]. High heterogeneity makes direct and indirect estimates less precise, which can mask underlying inconsistency. When inconsistency is present, the standard consistency model often displays higher estimated heterogeneity than an inconsistency model [12].
Experimental Protocols for Detecting Inconsistency
Protocol 1: Design-by-Treatment (DBT) Interaction Test
Purpose: To provide a global assessment of inconsistency across the entire network [11] [12].
Methodology:
- Model Fitting: Fit a random-effects DBT model that incorporates an extra parameter to account for variability due to inconsistency beyond what is expected from heterogeneity.
- Hypothesis Testing: Test all inconsistency parameters globally using a Wald-type chi-squared test.
- Interpretation: A significant p-value (commonly <0.05 or <0.10) indicates evidence of inconsistency in the network. This method is particularly valuable as it is insensitive to the parameterization of multi-arm trials [11].
Protocol 2: Node-Splitting Method
Purpose: To perform a local, comparison-specific assessment of inconsistency [2].
Methodology:
- Evidence Separation: For a specific treatment comparison (e.g., B vs. C), separate the evidence into direct (from trials directly comparing B and C) and indirect (formed via other treatments in the network, such as A) components.
- Estimate Calculation: Calculate the direct estimate, ( \hat{d}{BC}^{Dir} ), and the indirect estimate, ( \hat{d}{BC}^{Ind} = \hat{d}{AC}^{Dir} - \hat{d}{AB}^{Dir} ).
- Discrepancy Assessment: Assess the discrepancy between the direct and indirect estimates. The inconsistency, ( \hat{\omega}{BC} ), is calculated as: ( \hat{\omega}{BC} = \hat{d}{BC}^{Dir} - \hat{d}{BC}^{Ind} ) with variance: ( Var(\hat{\omega}{BC}) = Var(\hat{d}{BC}^{Dir}) + Var(\hat{d}{AB}^{Dir}) + Var(\hat{d}{AC}^{Dir}) ) [10].
- Statistical Testing: An approximate test for inconsistency is performed by referring ( z{BC} = \frac{\hat{\omega}{BC}}{\sqrt{Var(\hat{\omega}_{BC})}} ) to the standard normal distribution.
Table: Comparison of Key Methods for Detecting Inconsistency
| Method | Scope of Assessment | Key Strength | Key Limitation |
|---|---|---|---|
| Design-by-Treatment (DBT) | Global (entire network) | Insensitive to parameterization of multi-arm trials [11] | Does not locate the source of inconsistency |
| Node-Splitting | Local (specific comparison) | Pinpoints which comparisons are inconsistent [2] | Computationally intensive in large networks |
| Bucher Method | Local (single loop) | Simple calculation for a 3-treatment loop [10] | Not suitable for complex networks with multi-arm trials |
| Cochran's Q | Global (entire network) | Familiar statistic from pairwise meta-analysis [2] | Does not distinguish between heterogeneity and inconsistency |
Troubleshooting Guide: Addressing Detected Inconsistency
If inconsistency is detected in your network:
- Investigate Effect Modifiers: Systematically check for imbalances in patient-level (e.g., disease severity, age) or trial-level (e.g., year, duration, risk of bias) characteristics across the different direct comparisons [10].
- Subgroup and Meta-Regression Analyses: If potential effect modifiers are identified, perform subgroup analyses or network meta-regression to adjust for them and explore if inconsistency is reduced.
- Use Inconsistency Models: Consider using models that explicitly account for inconsistency, such as the Bayesian hierarchical model with inconsistency parameters proposed by Lu and Ades [2].
- Report and Interpret with Caution: Clearly report the findings and degree of inconsistency. If the source cannot be explained or resolved, interpret the NMA results with caution, as they may be unreliable.
The Scientist's Toolkit
Table: Essential Reagents and Methods for Inconsistency Investigation
| Tool / Method | Primary Function | Application in Inconsistency Analysis |
|---|---|---|
| Design-by-Treatment Model | Statistical Model | Provides a global test for the presence of inconsistency in the entire network [11]. |
| Node-Splitting | Statistical Method | Separates direct and indirect evidence for a specific comparison to test their agreement [2]. |
| Network Diagram | Visual Tool | Helps visualize the network structure, identify independent loops, and hypothesize where inconsistency may arise [10]. |
| Meta-Regression | Analytical Technique | Adjusts for continuous effect modifiers to see if they explain the observed inconsistency [10]. |
Stata (network suite) |
Software Command | Fits NMA models, including the DBT model, for inconsistency assessment [11]. |
R (netmeta package) |
Software Package | Performs NMA and includes functions for local and global inconsistency tests [11]. |
| T-3364366 | T-3364366, MF:C18H16F3N3O3S2, MW:443.5 g/mol | Chemical Reagent |
| TAK-828F | TAK-828F | TAK-828F is a potent, selective, orally available RORγt inverse agonist for autoimmune disease research. This product is for research use only (RUO). |
Visualizing the Pathway to Inconsistency
Sources of Inconsistency Flowchart: This diagram illustrates the logical pathway from underlying causes, like imbalanced effect modifiers or specific biases, to the emergence of statistical inconsistency, ultimately compromising NMA validity [10] [2].
Inconsistency Investigation Workflow: A decision flowchart outlining the recommended steps for investigating inconsistency, starting with a global test and proceeding to local methods if needed [11] [2].
Troubleshooting Guides and FAQs
What is inconsistency in Network Meta-Analysis and why is it a problem?
Inconsistency occurs when the direct evidence (from head-to-head trials) and indirect evidence (estimated through a common comparator) for a treatment comparison are in statistical disagreement [2]. This poses a significant problem because it can result in biased treatment effect estimates, compromising the reliability of the NMA and any clinical conclusions or decisions derived from it [2]. Inconsistency may arise from biases in direct comparisons (like publication bias) or when trial populations differ in important characteristics that modify treatment effects (effect modifiers) [2].
How common is inconsistency in published Network Meta-Analyses?
Empirical evidence from a large sample of published NMAs indicates that inconsistency is a relatively frequent issue [11]. The table below summarizes the prevalence of evidence of inconsistency based on the Design-by-Treatment (DBT) interaction model:
| Evidence Threshold (DBT p-value) | Prevalence in Published NMAs | Interpretation |
|---|---|---|
| Less than 0.05 | 14% of networks [11] | Strong evidence against consistency |
| Less than 0.10 | 20% of networks [11] | Evidence against consistency |
Networks that include many studies but compare few interventions are more likely to show evidence of inconsistency, partly because they produce more precise estimates and have higher power to detect differences between designs [11].
What are the main statistical methods to detect inconsistency?
Several statistical approaches exist to assess inconsistency, ranging from simple to complex methods. The table below compares the key techniques:
| Method | Primary Function | Key Characteristics |
|---|---|---|
| Cochran's Q Statistic [2] | Global assessment of heterogeneity/inconsistency | A common method for assessing heterogeneity; its generalized form can quantify inconsistency across the whole network. |
| Loop Inconsistency Approach [2] | Local assessment in loops of three treatments | Involves calculating the difference between direct and indirect evidence in a treatment loop; can be cumbersome in large networks due to multiple testing. |
| Design-by-Treatment (DBT) Interaction Model [11] | Global assessment for the entire network | Provides a global test insensitive to the parameterization of multi-arm trials; p-value indicates evidence against consistency. |
| Inconsistency Parameter Approach (Lu & Ades) [2] | Model-based assessment | A Bayesian hierarchical model that includes inconsistency parameters in each loop; model choice (fixed/random effects) can be arbitrary. |
| Node-Splitting [2] | Local, comparison-specific assessment | Separates direct and indirect evidence for a specific treatment comparison to assess their discrepancy. |
| Net Heat Plot [2] | Graphical identification of inconsistency sources | A graphical tool that displays the contribution of each design to network inconsistency by temporarily removing designs one at a time. |
The net heat plot did not signal inconsistency, but other methods did. Why?
This discrepancy can occur because the net heat plot does not reliably signal inconsistency [2]. The calculations underlying the net heat plot constitute an arbitrary weighting of the direct and indirect evidence, which may be misleading. Therefore, the absence of a signal in a net heat plot should not be interpreted as the absence of inconsistency. It is recommended to use multiple statistical methods to assess inconsistency rather than relying on a single approach [2].
What should I do if I detect significant inconsistency in my network?
If inconsistency is detected, you should not ignore it. The following steps are recommended:
- Investigate Clinical and Methodological Causes: Explore potential effect modifiers (e.g., differences in patient populations, intervention doses, or outcome definitions) across studies forming the direct and indirect evidence [2].
- Check for Transitivity Violations: Assess whether the distribution of these effect modifiers is similar across the different treatment comparisons [11].
- Consider Inconsistency Models: If inconsistency cannot be resolved, consider using statistical models that account for it, such as the inconsistency parameter approach or node-splitting models [2]. Note that in the presence of inconsistency, the standard consistency model may display higher heterogeneity than the inconsistency model [11].
- Interpret Results with Caution: Acknowledge the presence of inconsistency in the limitations section and interpret the NMA results with caution, as they may be less reliable.
Experimental Protocols for Key Inconsistency Assessments
Protocol 1: Global Inconsistency Test via Design-by-Treatment (DBT) Interaction Model
Purpose: To assess inconsistency across the entire network of interventions. Methodology Summary:
- Model Framework: Synthesize evidence using a model that incorporates extra variability attributable to inconsistency, beyond what is expected from heterogeneity or random error. This model evaluates the potential conflict between studies with different sets of interventions (designs) [11].
- Hypothesis Testing: Test the null hypothesis that the network is consistent.
- Test Statistic: Use a Wald-type chi-squared test statistic. A p-value below a pre-specified threshold (e.g., 0.05 or 0.10) provides evidence against the consistency assumption [11].
- Heterogeneity Estimation: Estimate the between-study variance (heterogeneity) using estimators like DerSimonian and Laird (DL) or Restricted Maximum Likelihood (REML) [11].
Protocol 2: Local Inconsistency Test via Node-Splitting
Purpose: To assess inconsistency for a specific treatment comparison within the network. Methodology Summary:
- Evidence Separation: For the treatment comparison of interest (e.g., A vs. B), separate the available evidence into two parts:
- The direct evidence from studies that directly compare A and B.
- The indirect evidence for A vs. B, estimated from the remaining network (e.g., via a common comparator C).
- Effect Estimation: Estimate the treatment effect for A vs. B from both the direct and the indirect evidence.
- Discrepancy Assessment: Statistically assess the discrepancy (difference) between the direct and indirect estimates. A significant difference indicates local inconsistency for that comparison [2].
Logical Relationship of Inconsistency Assessment Methods
The following diagram illustrates the logical workflow for assessing inconsistency in a Network Meta-Analysis, showing how global and local methods interrelate.
The Scientist's Toolkit: Essential Reagents for Inconsistency Investigation
| Tool or Method | Primary Function | Key Features and Considerations |
|---|---|---|
| Design-by-Treatment (DBT) Interaction Model [11] | Global inconsistency test | Provides a single p-value for the entire network; insensitive to parameterization of multi-arm trials. |
| Node-Splitting Model [2] | Local inconsistency test | Allows pinpointing which specific treatment comparisons are inconsistent. |
| Loop Inconsistency Approach [2] | Local inconsistency test | Assesses inconsistency in loops of three treatments; may require adjustment for multiple testing. |
| Cochran's Q Statistic [2] | Global heterogeneity/inconsistency measure | A generalized statistic that can quantify both within-design heterogeneity and between-design inconsistency. |
| Net Heat Plot [2] | Graphical exploration | A visual aid for exploring potential sources of inconsistency; should not be relied upon alone due to reliability concerns. |
| Statistical Software (R/Stata) | Analysis platform | Implementations available in packages like netmeta in R and the network suite in Stata [11]. |
| TAMRA-PEG4-Alkyne | TAMRA-PEG4-Alkyne|Click Chemistry Reagent | TAMRA-PEG4-Alkyne is a CuAAC reagent for fluorescent bioimaging and nucleotide labeling. For Research Use Only. Not for human use. |
| TAN-452 | TAN-452 Chemical Reagent For Research | TAN-452 is a high-purity research reagent for biochemical studies. For Research Use Only. Not for diagnostic or therapeutic use. |
Frequently Asked Questions
1. What is the primary purpose of a node-splitting analysis in Network Meta-Analysis?
A node-splitting analysis is used to evaluate potential inconsistency in a network meta-analysis [13]. It works by splitting the evidence for a specific treatment comparison into two parts: the direct evidence (from studies that directly compare the two treatments) and the indirect evidence (from the rest of the network) [13] [14]. A separate estimate is obtained for each part, and the agreement between these direct and indirect estimates is then statistically assessed. Significant disagreement indicates local inconsistency for that particular comparison [13].
2. How do I decide which treatment comparisons to split in my network?
Choosing which comparisons to split can be complex, especially in networks that include multi-arm trials. An unambiguous decision rule has been developed to automate this process [13]. This rule ensures that:
- You only split comparisons that are part of potentially inconsistent loops in the network.
- All potentially inconsistent loops in the network are investigated.
- Problems with the parameterization of multi-arm trials are circumvented, making model generation straightforward [13].
3. What are the different ways to parameterize a node-splitting model, and why does it matter?
When multi-arm trials are involved, there are different ways to assign the inconsistency parameter, and this choice can yield different results [14]. The main parameterizations are:
- Symmetrical: Assumes that both treatments in the comparison contribute equally to the inconsistency.
- Asymmetrical (one-treatment): Assumes that only one of the two treatments contributes to the inconsistency [14]. Your choice should be guided by your understanding of the treatments and the network structure, as each method makes slightly different assumptions about the source of inconsistency.
4. What should I do if my node-splitting analysis detects significant inconsistency?
The detection of significant inconsistency warrants a careful investigation. The statistical analysis alone does not resolve the problem; you must try to understand its source [13]. This involves:
- A thoughtful re-evaluation of the included trials, focusing on differences in design, population characteristics, or risk of bias that might explain the discrepant results.
- If a confounding factor is identified, you may address it via sensitivity analysis (e.g., excluding a problematic subset of trials) or meta-regression.
- Unexplained and significant inconsistency may mean that the results of the network meta-analysis are unreliable and must be interpreted with extreme caution [13].
Experimental Protocols & Methodologies
Protocol 1: Implementing a Bayesian Node-Splitting Model
This protocol outlines the steps for evaluating inconsistency using a Bayesian node-splitting model [13].
Objective: To assess the inconsistency for a specific treatment comparison (e.g., treatment X vs. Y) by separating direct and indirect evidence.
Methodology:
- Model Specification: For the comparison of interest ( d{x,y} ), define two parameters: a parameter for the direct evidence ( d{x,y}^{dir} ) and a parameter for the indirect evidence ( d_{x,y}^{ind} ) [13].
- Data Separation: The likelihood for the direct evidence is based only on studies that directly compare X and Y. The indirect evidence is informed by the remaining studies in the network.
- Prior Distributions: Specify non-informative or weakly informative prior distributions for the model parameters, including the heterogeneity variance.
- Estimation: Use Markov Chain Monte Carlo (MCMC) sampling in software like WinBUGS, JAGS, or Stan to estimate the posterior distributions of ( d{x,y}^{dir} ) and ( d{x,y}^{ind} ) [13].
- Assessment: Compare the posterior distributions of the direct and indirect estimates. The hypothesis of consistency is that ( d{x,y}^{dir} = d{x,y}^{ind} ). This can be evaluated by checking if the credible interval of their difference includes zero or by calculating a Bayesian p-value [13].
Table 1: Key Outputs from a Bayesian Node-Splitting Analysis
| Output Parameter | Description | How to Interpret Results |
|---|---|---|
| ( d_{x,y}^{dir} ) | The relative treatment effect estimate from direct evidence. | Compare the posterior mean/median and 95% credible interval (CrI) with the indirect estimate. |
| ( d_{x,y}^{ind} ) | The relative treatment effect estimate from indirect evidence. | Compare the posterior mean/median and 95% CrI with the direct estimate. |
| ( d{x,y}^{dir} - d{x,y}^{ind} ) | The difference between direct and indirect estimates. | Inconsistency is present if the 95% CrI for this difference does not contain zero. |
| Heterogeneity (τ²) | The estimate of between-study variance. | A high value may complicate the detection of inconsistency [13]. |
Protocol 2: Applying a Frequentist Side-Splitting Model using GLMM
This protocol describes an alternative, frequentist approach to node-splitting using generalized linear mixed models (GLMMs) [14].
Objective: To evaluate direct-indirect inconsistency using an arm-based, frequentist model framework.
Methodology:
- Model Framework: Use an arm-based generalized linear mixed model. This models study-specific absolute effects and assumes random intercepts [14] [15].
- Parameterization Choice: Decide on the inconsistency parameterization:
- Symmetrical: Inconsistency is split between both treatments.
- Asymmetrical: Inconsistency is assigned to one of the two treatments [14].
- Model Fitting: Fit the model using frequentist software capable of handling GLMMs, such as the
netmetapackage in R [14]. - Hypothesis Testing: Assess the statistical significance of the inconsistency factor using a Wald test or likelihood ratio test. A significant p-value indicates evidence of inconsistency.
Table 2: Comparison of Node-Splitting Model Approaches
| Feature | Bayesian Node-Splitting [13] | Frequentist Side-Splitting (GLMM) [14] |
|---|---|---|
| Framework | Bayesian statistics | Frequentist statistics |
| Output | Posterior distributions and credible intervals | Point estimates, confidence intervals, and p-values |
| Handling of Multi-arm Trials | Addressed via decision rules for model generation [13] | Different parameterizations (symmetrical/asymmetrical) can yield different results [14] |
| Interpretation | Probability of inconsistency given the data | Statistical significance of the inconsistency factor |
| Common Software | WinBUGS, JAGS, Stan | R (e.g., netmeta package) |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for NMA Inconsistency Analysis
| Item | Function / Description | Example Use in NMA |
|---|---|---|
| Automated Model Generation Algorithm | A decision rule that automatically selects which comparisons to split and generates the corresponding models [13]. | Eliminates manual work in node-splitting; ensures all potentially inconsistent loops are investigated. |
| Contrast-Based (CB-NMA) Model | A model that focuses on synthesizing study-specific relative effects (contrasts) and assumes fixed study-specific intercepts [15]. | The traditional framework for implementing consistency and node-splitting models [13]. |
| Arm-Based (AB-NMA) Model | A model that uses study-specific absolute effects and assumes random intercepts, offering greater flexibility in estimands [15]. | Can be used to implement a frequentist side-splitting model for inconsistency [14]. |
| Composite Likelihood Method | An advanced statistical approach that provides accurate inference without requiring knowledge of typically unreported within-study correlations [15]. | Helps overcome a key challenge in NMA that can lead to biased estimates if ignored. |
| PRISMA-NMA Guidelines | The Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Network Meta-Analyses [16]. | Ensures complete and transparent reporting of your NMA, including methods for assessing inconsistency. |
| TASP0390325 | TASP0390325, CAS:1642187-96-9, MF:C25H30Cl2FN5O, MW:554.4444 | Chemical Reagent |
| Boc-Aminooxy-PEG2 | Boc-Aminooxy-PEG2, CAS:1807503-86-1, MF:C9H19NO5, MW:221.25 g/mol | Chemical Reagent |
Visualizing Evidence Flow and Inconsistency
The following diagram illustrates the fundamental concept of separating evidence in a node-splitting analysis.
This workflow outlines the decision-making process when inconsistency is detected.
Detection and Quantification: A Toolkit for Identifying Inconsistency
Frequently Asked Questions
Q1: What is the core difference between node-splitting and the Bucher method for evaluating inconsistency in NMA?
Both methods assess inconsistency between direct and indirect evidence but differ fundamentally in approach. The Bucher method is a frequentist approach that performs adjusted indirect comparisons for a single treatment contrast in a loop of evidence, providing a single inconsistency estimate [17]. Node-splitting is a more general method, available in both Bayesian and frequentist frameworks, that separates direct and indirect evidence for a particular comparison and tests for their disagreement [13] [14]. It can evaluate multiple comparisons within a network and is particularly useful for identifying the specific location of inconsistencies [13].
Q2: When implementing node-splitting for a treatment comparison involved in multi-arm trials, I get different results depending on the parameterization. Why does this happen, and how should I proceed?
This occurs because multi-arm trials introduce ambiguity in how the inconsistency parameter is assigned [14]. Different parameterizations make different assumptions:
- Asymmetric parameterization assumes only one of the two treatments in the contrast contributes to the inconsistency.
- Symmetric parameterization assumes both treatments contribute to the inconsistency [14].
There is no universal "correct" choice. You should select the parameterization that best aligns with your clinical knowledge of the evidence network. The symmetric method is often preferred when there is no a priori reason to suspect one treatment over the other is the source of inconsistency.
Q3: My node-splitting analysis fails to run, citing disconnected nodes. What does this mean, and how can I fix it?
This error occurs when splitting the specified comparison would result in part of the network becoming disconnected from the reference treatment, making the indirect estimate incalculable [18]. To resolve this:
- Check your network connectivity using network graphs.
- Ensure that all treatments are connected through a path of comparisons.
- If using software, set the
drop.disconargument toTRUE(if available) to automatically drop disconnected treatments, though this should be done with caution as it alters the evidence base for the analysis [18]. - Consider selecting an alternative comparison to split that maintains network connectivity.
Q4: The Bucher method identified significant inconsistency in a loop. What are the potential next steps?
A significant inconsistency factor (IF) indicates that direct and indirect estimates for a contrast are statistically different. You should:
- Scrutinize the trials forming the direct and indirect evidence for clinical, methodological, or demographic dissimilarities that might explain the discrepancy.
- Check for the presence of effect modifiers across studies.
- Consider using meta-regression or subgroup analysis to account for identified differences, if sufficient data are available.
- Report the inconsistency and interpret the NMA results for the affected comparisons with extreme caution. Unexplained significant inconsistency may invalidate the consistency assumption for that part of the network [13].
Troubleshooting Guides
Issue 1: Automated Selection of Comparisons for Node-Splitting
Problem: In a complex network, it is labor-intensive to decide which comparisons to split, and manual selection is prone to error and may miss important loops [13].
Solution: Implement a pre-specified decision rule to automatically select comparisons.
- Step 1: Use an algorithm to identify all closed loops in the evidence network where independent sources of evidence exist [13] [18].
- Step 2: Apply a decision rule that selects only one comparison per loop to split, typically the one with the most direct evidence or the one of primary clinical interest. A valid rule ensures all potentially inconsistent loops are investigated without redundancy [13].
- Step 3: Automated model generation can then be used to fit the node-splitting models for the selected comparisons, significantly reducing manual effort [13].
Issue 2: Handling Multi-Arm Trials in Node-Splitting
Problem: Results from a node-split are sensitive to how multi-arm trials are handled, leading to different conclusions based on parameterization [14].
Solution: Understand and correctly specify the model for multi-arm trials.
- Step 1: Identify all treatment comparisons in the network that are informed by at least one multi-arm trial.
- Step 2: Choose a parameterization method based on your assumptions about the source of inconsistency:
- Asymmetric Method: Use if you hypothesize that inconsistency originates from a single specific treatment in the comparison.
- Symmetric Method: Use if you believe both treatments contribute equally to the inconsistency. This is often the default when no prior hypothesis exists [14].
- Step 3: In your statistical code, ensure the covariance structure of multi-arm trials is correctly specified (the covariance is typically σ²/2 in a homogeneous variance model) [13]. Use software that explicitly allows for this specification.
Table: Comparison of Node-Splitting Parameterizations for Multi-Arm Trials
| Parameterization Type | Underlying Assumption | Best Use Case | Key Consideration |
|---|---|---|---|
| Asymmetric | Inconsistency is attributable to a single treatment in the contrast being split. | When clinical knowledge suggests one treatment's effect is estimated differently across trial designs. | Results differ depending on which treatment is assigned the inconsistency parameter. |
| Symmetric | Both treatments in the contrast contribute to the inconsistency. | The default choice when there is no strong prior hypothesis about the source of inconsistency [14]. | Provides a single, averaged estimate of the direct-indirect difference. |
| Boc-Aminoxy-PEG4-OH | Boc-Aminoxy-PEG4-OH|PROTAC Linker|918132-14-6 | Bench Chemicals | |
| Propargyl-PEG2-NHBoc | Propargyl-PEG2-NHBoc, CAS:869310-84-9, MF:C12H21NO4, MW:243.30 g/mol | Chemical Reagent | Bench Chemicals |
Issue 3: Interpreting Conflicting Results Between Global and Local Inconsistency Tests
Problem: A global test (e.g., design-by-treatment interaction model) finds significant inconsistency, but node-splitting finds no significant local inconsistencies.
Solution: This pattern suggests that inconsistency may be diffusely distributed across the entire network rather than localized in specific loops [13].
- Step 1: Do not ignore the global test. It has power to detect diffuse inconsistency that local tests might miss.
- Step 2: Re-examine the network for clinical or methodological heterogeneity, such as differences in patient populations, dosages, or study designs that are widespread across the network.
- Step 3: Consider using a meta-regression or subgroup analysis to explore potential effect modifiers if the global test is significant.
- Step 4: If no explanation is found, the results of the NMA should be interpreted with caution, and the uncertainty from the global inconsistency should be reflected in the conclusions.
Experimental Protocols
Protocol 1: Implementing a Node-Splitting Analysis
This protocol provides a step-by-step methodology for performing a node-splitting analysis to evaluate inconsistency at the treatment comparison level [13] [18].
Objective: To split the evidence for a given treatment comparison into direct and indirect components and statistically test their discrepancy.
Materials & Software: Statistical software with NMA capabilities (e.g., R using the gemtc or MBNMAdose packages, OpenBUGS, JAGS).
Procedure:
Model Specification:
- For the comparison of interest (e.g., A vs. B), define two parameters:
d_AB_directandd_AB_indirect. - Specify a model where the
d_AB_directis informed only by studies that directly compare A and B. - The
d_AB_indirectis informed by the rest of the network, estimated via the consistency relations from the other basic parameters [13].
- For the comparison of interest (e.g., A vs. B), define two parameters:
Model Fitting:
- Fit the model using Bayesian Markov chain Monte Carlo (MCMC) methods.
- Use vague priors for the basic parameters and the heterogeneity variance.
- Run multiple chains (e.g., 3) to assess convergence.
Output and Calculation:
- The key output is the posterior distribution of the difference between the direct and indirect estimates:
d_AB_direct - d_AB_indirect. - Calculate the posterior mean and 95% Credible Interval (CrI) for this difference.
- The key output is the posterior distribution of the difference between the direct and indirect estimates:
Interpretation:
- If the 95% CrI for the difference includes 0, there is no statistically significant inconsistency between the direct and indirect evidence for the comparison A vs. B.
- A 95% CrI that excludes 0 indicates significant local inconsistency.
Protocol 2: Executing the Bucher Loop-Based Method
This protocol outlines the steps for implementing the Bucher method, an adjusted indirect comparison for a single loop of evidence [17].
Objective: To obtain an indirect estimate of a treatment effect and compare it with the direct estimate to calculate an inconsistency factor.
Materials & Software: Standard statistical software (e.g., R, Stata, SAS) or even spreadsheet software capable of performing basic meta-analytic calculations.
Procedure:
Define the Loop: Identify a closed loop of three treatments (A, B, C) and the three pairwise comparisons (A vs. B, A vs. C, B vs. C). The loop must be informed by independent sources of evidence (e.g., from different sets of trials).
Extract Effect Estimates:
- For each of the three pairwise comparisons, obtain the pooled effect estimate (e.g., log odds ratio, mean difference) and its standard error from pair-wise meta-analyses or from the NMA consistency model.
Calculate the Indirect Estimate:
- The indirect estimate for A vs. B (for example) is calculated as:
Effect_AB_indirect = Effect_AC - Effect_BC. - The variance of the indirect estimate is:
Var(Effect_AB_indirect) = Var(Effect_AC) + Var(Effect_BC).
- The indirect estimate for A vs. B (for example) is calculated as:
Calculate the Inconsistency Factor (IF):
IF_AB = Effect_AB_direct - Effect_AB_indirect.- The variance of the IF is:
Var(IF_AB) = Var(Effect_AB_direct) + Var(Effect_AB_indirect).
Statistical Test:
- A 95% Confidence Interval (CI) for the IF is calculated as:
IF_AB ± 1.96 * sqrt(Var(IF_AB)). - If the 95% CI excludes 0, the inconsistency is statistically significant at the 5% level.
- A 95% Confidence Interval (CI) for the IF is calculated as:
Table: Data Collection Table for Bucher Method (Example: Log Odds Ratios)
| Comparison | Direct Estimate (logOR) | Variance of Direct Estimate | Source Studies | Indirect Estimate (logOR) | Variance of Indirect Estimate |
|---|---|---|---|---|---|
| A vs. B | -0.45 | 0.05 | Studies 1, 2, 3 | Effect_AC - Effect_BC = -0.20 |
Var(AC) + Var(BC) = 0.03 |
| A vs. C | -0.60 | 0.02 | Studies 4, 5 | Not Applicable | Not Applicable |
| B vs. C | -0.40 | 0.01 | Studies 6, 7 | Not Applicable | Not Applicable |
| Inconsistency Factor (A vs. B) | -0.45 - (-0.20) = -0.25 |
0.05 + 0.03 = 0.08 |
95% CI: -0.25 ± 1.96√0.08 = [-0.80, 0.30] |
The Scientist's Toolkit
Table: Essential Reagents and Software for Inconsistency Analysis in NMA
| Item Name | Type | Specification / Function | Example / Note |
|---|---|---|---|
R gemtc package |
Software Library | Provides a complete suite for Bayesian NMA, including node-splitting [13]. | Used for model specification, MCMC sampling, and results extraction. |
R MBNMAdose package |
Software Library | Contains the nma.nodesplit() function for performing node-splitting on a given network [18]. |
Allows specification of likelihood, link function, and random/common effects. |
| JAGS / OpenBUGS | Software | Bayesian analysis software used for Gibbs sampling. Can be called from R. | Provides the computational engine for fitting complex Bayesian hierarchical models. |
| Effect Size Data | Data Input | Pooled effect estimates and their variances (e.g., Log Odds Ratio, Hazard Ratio, Mean Difference). | The fundamental data for performing the Bucher method or feeding into NMA models. |
| Homogeneous Variance Prior | Statistical Parameter | The common between-study heterogeneity variance (τ²) assumed across the network. | A key assumption in the homogeneous variance model; its prior must be specified carefully [13]. |
| TC-G 1005 | TC-G 1005, MF:C25H25N3O2, MW:399.5 g/mol | Chemical Reagent | Bench Chemicals |
| TC-I 2014 | TC-I 2014, MF:C23H19F6N3O, MW:467.4 g/mol | Chemical Reagent | Bench Chemicals |
Frequently Asked Questions
1. What is the Design-by-Treatment Interaction Model in network meta-analysis?
The Design-by-Treatment Interaction Model is a statistical framework developed to assess inconsistency (also called incoherence) in network meta-analysis (NMA). Inconsistency occurs when direct evidence (from head-to-head trials) and indirect evidence (estimated through a common comparator) about treatment effects are in disagreement. This model provides a global test for inconsistency across the entire network of evidence by introducing interaction terms between the study design (the set of treatments being compared) and the treatment effects. When these interaction terms are statistically significant, it indicates the presence of inconsistency that threatens the validity of the NMA results [19] [20].
2. When should I use this model instead of other inconsistency assessment methods?
You should use the Design-by-Treatment Interaction Model when you need a comprehensive, global assessment of inconsistency in a network that may include multi-arm trials (trials with three or more treatment arms). Unlike simpler methods like the Bucher method, which only assesses inconsistency in simple three-treatment loops, this model can handle complex networks with various designs. It is considered one of the best methods for this purpose, particularly because it successfully addresses complications that arise from the presence of multi-arm trials [19] [20] [2].
3. What are the key limitations of this model I should be aware of?
Recent simulation studies have highlighted important limitations. The model can suffer from a high Type I error (approximately 0.4 to 0.45 in some scenarios), meaning it may incorrectly detect inconsistency when none exists. It may also lack sufficient statistical power (ranging from approximately 0.5 to 0.75 depending on the scenario) to reliably detect true inconsistency in a network. The power and error rates are heavily influenced by the assumed inconsistency factor in the data. These limitations suggest that while the model is valuable, its results should be interpreted cautiously, and further methodological work is needed to improve inconsistency assessment [20].
4. What software tools can I use to implement this model?
Several software options are available. The nmaINLA R package implements the model using Integrated Nested Laplace Approximations for Bayesian inference, providing a fast alternative to Markov chain Monte Carlo methods. The newly developed NMA R package offers a frequentist implementation with a user-friendly interface, incorporating functions for this model alongside other inconsistency assessment tools. Additionally, Stata's network package provides implementation within the multivariate meta-regression framework [21] [22].
Troubleshooting Guides
Problem: Model Fails to Converge or Produces Errors
Potential Causes and Solutions:
- Insufficient Data: The model requires adequate direct evidence for each treatment comparison. Networks with sparse direct evidence or many treatments but few studies are problematic.
- Complexity: For highly connected networks with many treatments, the model becomes computationally demanding. Consider using alternative estimation methods like INLA [21].
- Implementation: Ensure you are using appropriate software. The
NMApackage in R is designed to handle the multivariate meta-regression framework required for this model and provides helpful error messages [22].
Problem: Model Detects Inconsistency but I Can't Identify the Source
Investigation Steps:
- Supplement with Local Methods: Use node-splitting methods to examine inconsistency for each treatment comparison individually. This helps pinpoint which direct comparisons conflict with the indirect evidence [2].
- Check for Effect Modifiers: Conduct network meta-regression by incorporating trial-level covariates (e.g., patient characteristics, risk of bias) into the model. These covariates might explain the observed inconsistency [19] [21].
- Evaluate Network Geometry: Use network graphs to visually identify poorly connected treatments or unusual patterns in the evidence structure that might contribute to inconsistency [23].
Problem: Interpreting the Random-Effects vs. Fixed-Effects Formulation
Decision Guidance:
- Random-Inconsistency Effects: This approach, as proposed by Jackson et al., models inconsistency parameters as following a common distribution. It is particularly useful for ranking treatments under inconsistency and for sensitivity analyses, as it involves fewer parameters. It facilitates the estimation of average treatment effects across all designs [19] [24].
- Fixed-Inconsistency Effects: This approach treats each inconsistency parameter as a separate, unrelated fixed effect. Higgins et al. argue this is more plausible when each inconsistency parameter has its own unique interpretation. A key practical advantage is that the resulting model can be fitted as a multivariate meta-regression [19].
- Recommendation: The random-effects formulation is often preferred for treatment ranking and when modeling inconsistency as an additional source of variation, similar to how between-study heterogeneity is handled in conventional meta-analysis [19].
Quantitative Data and Experimental Protocols
Table 1: Statistical Performance of the Design-by-Treatment Interaction Model
| Performance Metric | Reported Value/Range | Influencing Factors |
|---|---|---|
| Type I Error | 0.4 to 0.45 [20] | Inconsistency factor, number of studies |
| Statistical Power | 0.5 to 0.75 [20] | True odds ratio, inconsistency factor, number of studies per comparison |
| Model Framework | Random-effects inconsistency model [19] [24] | Assumes inconsistency parameters follow a common distribution |
Table 2: Essential Research Reagent Solutions
| Tool / Resource | Function in Analysis | Implementation Example |
|---|---|---|
| Multivariate Meta-regression Framework | Provides the statistical foundation for implementing the model and estimating parameters. | White et al. framework [22] |
R NMA Package |
A comprehensive R package for frequentist NMA, includes functions for the Design-by-Treatment model, inconsistency assessment, and graphical tools. | setup() function for data preparation [22] |
| INLA Estimation Method | A Bayesian computational method for latent Gaussian models; offers a faster alternative to MCMC for model fitting. | nmaINLA R package [21] |
| Global Inconsistency Test (Higgins) | A specific statistical test within the multivariate framework to check for the presence of global inconsistency in the network. | Available in the NMA package [22] |
Methodological Workflow and Visualization
The following diagram illustrates the key steps and decision points involved in implementing and interpreting the Design-by-Treatment Interaction Model for assessing inconsistency in a network meta-analysis.
Troubleshooting Guides
Guide 1: Resolving Parameterization Ambiguities in Node-Splitting
Problem: Different parameterizations of node-splitting models yield conflicting results when multi-arm trials are present in the network.
Explanation: Inconsistent outcomes occur because multi-arm trials contribute to multiple treatment comparisons simultaneously. When splitting a node (treatment comparison), the model must decide how to handle the dependencies within multi-arm trials. Three parameterization approaches exist, each making different assumptions about which treatment contributes to the inconsistency [14].
Solution:
- Identify the nature of your multi-arm trials: Determine how many multi-arm trials contribute to the comparison you are splitting.
- Select the appropriate parameterization method:
- Symmetrical method: Use when both treatments in the contrast may contribute to inconsistency.
- Single-treatment method: Use when only one specific treatment is suspected as the inconsistency source.
- Alternative single-treatment method: Use when the other treatment is suspected.
- Run analyses using all three parameterizations if the source of inconsistency is unknown, and compare results to understand the sensitivity of your findings.
Guide 2: Handling Inconsistency Detection in Complex Networks
Problem: Standard inconsistency detection methods fail or provide ambiguous results in networks with multi-arm trials.
Explanation: Traditional loop inconsistency approaches assume all trials are two-arm, but real-world networks often include multi-arm trials. Loop inconsistency cannot be defined unambiguously when multi-arm trials are present because inconsistency cannot occur within a multi-arm trial [1]. This complicates the detection and interpretation of inconsistency.
Solution:
- Use the design-by-treatment interaction model as a comprehensive approach that handles multi-arm trials naturally [1].
- Implement automated node-splitting with a decision rule that selects only comparisons in potentially inconsistent loops and ensures all potentially inconsistent loops are investigated [13].
- Validate findings with multiple inconsistency detection methods, noting that some methods like the net heat plot may not reliably signal inconsistency in all scenarios [2].
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental concept behind node-splitting models in network meta-analysis?
Node-splitting is a method to evaluate inconsistency between direct and indirect evidence in network meta-analysis. It works by separating the evidence for a specific treatment comparison into two parts: (1) direct evidence from studies that directly compare the two treatments, and (2) indirect evidence from the remainder of the network. The method then assesses whether these two sources provide statistically different estimates of the treatment effect, which would indicate inconsistency in the network [13].
FAQ 2: Why do multi-arm trials present special challenges for evidence-splitting models?
Multi-arm trials present challenges because they contribute to multiple treatment comparisons simultaneously, creating complex dependencies in the evidence network. This leads to three specific issues:
- Parameterization ambiguity: There may be several valid node-splitting models for the same comparison when multi-arm trials are involved [13].
- Unclear inconsistency definition: Loop inconsistency cannot be defined unambiguously when multi-arm trials are present in the network [1].
- Different results from different parameterizations: Assigning the inconsistency parameter to one treatment versus another, or splitting it symmetrically, can yield different results [14].
FAQ 3: What are the different parameterization options for node-splitting models with multi-arm trials, and how do I choose?
Three parameterizations are available, each with different assumptions [14]:
| Parameterization | Assumption | Best Use Case |
|---|---|---|
| Symmetrical | Both treatments contribute equally to inconsistency | When no prior information about inconsistency source |
| Single-Treatment A | Only treatment A contributes to inconsistency | When theory suggests one specific treatment is problematic |
| Single-Treatment B | Only treatment B contributes to inconsistency | When theory suggests the other treatment is problematic |
FAQ 4: How can I implement automated node-splitting in my network meta-analysis?
Automated node-splitting requires:
- A decision rule to select which comparisons to split that investigates all potentially inconsistent loops [13].
- Accounting for multi-arm trials in the parameterization to ensure valid models [13].
- Software implementation that can handle the complex model generation, such as the methods described by van Valkenhoef et al. that build on automated model generation for network meta-analysis [13].
Experimental Protocols
Protocol: Implementing Node-Splitting Analysis for Multi-Arm Trial Networks
Purpose: To detect and evaluate inconsistency between direct and indirect evidence in a network meta-analysis containing multi-arm trials.
Methodology:
- Network Setup: Map all treatment comparisons, identifying multi-arm trials and potential loops where inconsistency may occur.
- Comparison Selection: Apply decision rules to select comparisons for splitting that cover all potentially inconsistent loops [13].
- Model Specification: For each selected comparison, specify three separate node-splitting models using the different parameterizations (symmetrical and two single-treatment approaches) [14].
- Model Estimation: Fit all models using Bayesian methods with appropriate priors and convergence diagnostics.
- Inconsistency Assessment: Compare direct and indirect estimates for each split node, evaluating statistical significance of differences.
- Sensitivity Analysis: Compare results across different parameterizations to assess robustness of findings.
Interpretation: Significant differences between direct and indirect evidence for any split node indicates local inconsistency in the network. Consistent results across parameterizations strengthen evidence for presence or absence of inconsistency.
Data Presentation
Table 1: Comparison of Inconsistency Detection Methods for Network Meta-Analysis
| Method | Handling of Multi-Arm Trials | Key Advantage | Key Limitation |
|---|---|---|---|
| Node-Splitting [13] | Requires special parameterization | Straightforward interpretation of local inconsistencies | Labour-intensive without automation |
| Design-by-Treatment Interaction [1] | Handles naturally through design concept | Unambiguous model specification | Harder conceptual interpretation |
| Loop Inconsistency Approach [2] | Problematic with multi-arm trials | Simple implementation for two-arm trials | Cannot be defined unambiguously with multi-arm trials |
| Net Heat Plot [2] | Not clearly specified | Graphical presentation | Does not reliably signal inconsistency |
Methodological Visualization
Node-Splitting Conceptual Workflow
Multi-Arm Trial Complexity in Network Meta-Analysis
The Scientist's Toolkit
Research Reagent Solutions for Evidence-Splitting Models
| Item | Function | Specification |
|---|---|---|
| Bayesian Modeling Software | Estimate node-splitting models | Supports random-effects models and complex variance-covariance structures [13] |
| Automated Model Generation | Implement decision rules for comparison selection | Applies unambiguous decision rules for splitting comparisons [13] |
| Heterogeneity Assessment | Evaluate between-study variability | Calculates homogeneous-variance random-effects models [13] |
| Consistency Evaluation | Check agreement between direct and indirect evidence | Implements statistical tests for difference between evidence sources [13] [14] |
Frequently Asked Questions
1. What is a Net Heat plot and what does it visualize? A Net Heat plot is a graphical matrix tool used to locate and identify inconsistency within a network meta-analysis. It displays the contribution of direct evidence from specific designs (treatment comparisons) to network estimates and highlights "hot spots" of inconsistency between direct and indirect evidence [2] [25].
2. What do the colors in a Net Heat plot represent? In the matrix, the colors indicate the change in inconsistency when the consistency assumption is relaxed for a single design. Warm colors (e.g., red, orange) signify a decrease in inconsistency, while cool colors (e.g., blue) signify an increase. The intensity of the color corresponds to the magnitude of this change. The gray squares show the contribution of a direct estimate to a network estimate [25].
3. My Net Heat plot is empty or missing designs. Why does this happen? This is expected behavior for certain designs. The plot automatically excludes designs where only one treatment is involved in other parts of the network, or where removing the corresponding studies would cause the network to split into unconnected parts. These designs do not contribute to the inconsistency assessment and are therefore not shown [25].
4. How do I interpret a "hot spot" of inconsistency? A cluster of warm-colored cells (e.g., red) on the plot, particularly on the diagonal, indicates a design that is a potential source of inconsistency. If the colors in a column match the colors on the diagonal, detaching that specific design's effect may dissolve the total inconsistency in the network [25].
5. What are the main limitations of the Net Heat plot? The method has been criticized for potentially using an arbitrary weighting of direct and indirect evidence that can be misleading. Studies have shown that it may fail to reliably signal inconsistency or identify inconsistent designs, even when other statistical methods (like node-splitting or the Bucher method) suggest its presence [2].
6. What is the difference between a fixed-effect and random-effects Net Heat plot? The underlying statistical model can be changed. The plot can be based on a common (fixed) effects model or a random-effects model that incorporates between-study variance (τ²). The choice of model can affect the appearance and interpretation of the plot [25].
Troubleshooting Guides
Issue: Difficulty Interpreting Net Heat Plot Colors and Values
Problem: The meaning of the colors (Q_diff) and gray squares in the plot is unclear, making interpretation challenging.
Solution: Interpret the plot elements systematically as outlined in the table below.
| Plot Element | Meaning | Interpretation |
|---|---|---|
| Gray Square Area | Contribution of a direct estimate (column) to a network estimate (row). | A larger area signifies a greater contribution of that direct evidence to the overall network estimate [25]. |
| Diagonal Color | Inconsistency contribution of the corresponding design. | Warm colors here indicate that the design itself is a source of inconsistency [25]. |
| Off-Diagonal Color | Change in inconsistency for a row's estimate after detaching a column's design. | Cool (Blue): Increase in inconsistency. Warm (Red): Decrease in inconsistency [25]. |
Resolution Steps:
- Identify Clusters: Look for rows and columns with similar warm coloring, which are clustered by the algorithm to highlight inconsistency [25].
- Focus on the Diagonal: Check the diagonal for warm-colored cells to quickly identify designs that are primary drivers of inconsistency.
- Check Column Patterns: If a column's off-diagonal colors are identical to the diagonal, detaching that design may resolve the network's overall inconsistency [25].
Issue: Technical Implementation and Customization in R
Problem: Uncertainty about how to generate and customize the plot using the netmeta package in R.
Solution:
Use the netheat() function from the netmeta package. The R code snippet below shows a basic implementation and key parameters.
Parameters for Troubleshooting:
random: Set toTRUEto use a random-effects model instead of the default common effects model [25].tau.preset: Allows you to preset a value for the between-study variance τ² for the plot [25].showall: By default (FALSE), designs with minimal contribution to the inconsistency statistic are not shown. Set toTRUEto force them to appear [25].nchar.trts: Defines the minimum number of characters for creating unique treatment names, which can help with readability [25].
Issue: Low Contrast in Network Graph Visualization
Problem: A network graph has poor contrast, making it difficult to distinguish nodes and edges.
Solution: Manually define a high-contrast color for each node. This can be done by creating a color map. The following pseudocode and diagram illustrate the logic of assigning colors to maximize contrast between connected nodes.
Diagram 1: Logic for assigning high-contrast colors to network nodes.
Resolution Steps:
- Create a Color Map: Define a list to store the color for each node [26].
- Iterate and Assign: For each node in the graph, check the colors already assigned to its neighbors.
- Maximize Contrast: From your predefined palette, select a color that is most distinct from the neighbors' colors [27].
- Apply the Map: Pass the finalized color map to your graphing function's
node_colorparameter [26].
Research Reagent Solutions
Essential computational tools and statistical packages for creating Net Heat and Net Path plots.
| Item Name | Function/Brief Explanation |
|---|---|
| R Statistical Software | The primary software environment for performing statistical computing and generating NMA visualizations. |
netmeta R Package |
A comprehensive frequentist package for network meta-analysis. It contains the netheat() function to create Net Heat plots [25]. |
| NetworkX (Python) | A Python library for creating and manipulating complex networks. While not for NMA-specific statistics, it is excellent for customizing network graph visuals, such as setting node colors for contrast [26] [28]. |
| Graphviz (DOT language) | A tool for representing graph structures. It is used here to create clear, high-contrast diagrams of workflows and network relationships. |
Comparative Analysis of Inconsistency Detection Methods
The table below summarizes key methods for detecting inconsistency in NMA, providing context for where Net Heat plots fit in the researcher's toolkit [2].
| Method | Type of Assessment | Key Characteristics | Primary Output |
|---|---|---|---|
| Net Heat Plot | Local & Global | Graphical matrix; Identifies locations and potential drivers of inconsistency. | Heat matrix with colors indicating inconsistency change [2] [25]. |
| Cochran's Q Statistic | Global | Single test statistic; Quantifies heterogeneity/inconsistency across the whole network. | Q statistic and p-value [2]. |
| Loop Inconsistency Approach | Local | Assesses inconsistency in loops of three treatments; Suitable only for two-arm trials. | Difference between direct and indirect evidence for each loop [2]. |
| Node-Splitting | Local | Separates direct and indirect evidence for a specific comparison to test their disagreement. | p-value for the difference between direct and indirect evidence for each split node [2]. |
| Inconsistency Parameter approach | Global | A hierarchical model that includes inconsistency parameters in each loop where inconsistency could occur. | Model fit statistics and parameter estimates for inconsistency [2]. |
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary software options for performing a Network Meta-Analysis, and how do I choose? There are three primary frameworks for NMA: frequentist implementations in R and Stata, and Bayesian platforms [29]. The choice depends on your statistical background and analysis needs. Bayesian frameworks are used in an estimated 60-70% of NMA studies and are often considered logically well-suited for handling indirect and multiple comparisons [29]. However, if setting prior probabilities is complex for your research question, a frequentist approach using Stata or R might be more accessible [29].
FAQ 2: I've found inconsistency in my network. What is the immediate step-by-step procedure to handle this? When inconsistency is detected, you should [29]:
- Investigate Effect Modifiers: Use sensitivity analysis or meta-regression to identify and adjust for variables that may modify the treatment effect [29].
- Check Transitivity Assumption: Inconsistency often suggests a violation of the transitivity assumption. Re-examine the clinical and methodological similarity of the studies in your network [29].
- Explore Locally: Use local approaches like node-splitting to identify which specific treatment comparisons are contributing to the inconsistency [29].
FAQ 3: How can I incorporate evidence from single-arm trials or a mixture of data types into my NMA? Advanced Bayesian methods allow for the synthesis of different data types. You can use models that combine Individual Participant Data (IPD) and Aggregate Data (AD), and incorporate Single-Arm Trials (SATs) by assuming exchangeability between the baseline response parameters of SATs and the control arms of RCTs [30]. This is particularly useful when a treatment is disconnected from the network due to a lack of direct comparative evidence [30].
FAQ 4: My network has many treatments. Is there a way to simplify the analysis and interpretation? Yes, if treatments can be logically grouped (e.g., different drugs within the same class), you can use NMA with class effects. This hierarchical model informs recommendations at the class level and can help address challenges with sparse data [31]. A model selection strategy is recommended to choose the most appropriate class effect model [31].
Troubleshooting Common NMA Software Implementation Issues
Issue 1: Preparing Data for netmeta in R
- Problem: Incorrect data format leads to errors when running the
netmetafunction. - Solution: For
netmeta, data is typically expected in a long format where each row represents a treatment arm within a study [29]. Essential columns include:- Study identifier
- Treatment identifier
- Number of events (for binary outcomes) or mean (for continuous outcomes)
- Sample size (for binary outcomes) or standard deviation (for continuous outcomes)
- Protocol: A correctly formatted dataset is the first critical step. Ensure your data is structured with these columns before any analysis.
Issue 2: Testing and Resolving Inconsistency in Stata
- Problem: The global test indicates significant inconsistency in the network.
- Solution: Stata's
networksuite offers tools for this [29].- Global Test: First, perform a global inconsistency test via the Wald test [29].
- Local Test: If global inconsistency is found, use the
nodesplitcommand to perform local tests. This separates direct and indirect evidence for each specific comparison and tests their agreement statistically [29]. - Protocol: The workflow is to 1) run the global test, 2) if significant, run node-splitting, and 3) investigate effect modifiers for comparisons showing significant local inconsistency.
Issue 3: Incorporating Single-Arm Trials in a Bayesian Framework
- Problem: A key treatment is only evaluated in single-arm trials, disconnecting it from the network of RCTs.
- Solution: Use an Arm-Based (AB) model or a Contrast-Based (CB) model with exchangeable baselines [30].
- Protocol: In the CB approach, the baseline response parameters (e.g., log-odds of an event in the control arm) for SATs and RCTs are modeled as exchangeable, drawing from a common distribution. This allows the SATs to borrow strength from the control arms of the RCTs, enabling indirect comparison [30].
Issue 4: Conducting NMA with Class Effects in R
- Problem: Estimating a model where treatments are nested within classes.
- Solution: Use the
multinmaR package, which supports hierarchical NMA models with class effects [31].- Protocol: The guide suggests a structured model selection strategy to choose between fixed and random treatment-level effects, and between exchangeable and common class-level effects. This involves testing assumptions of heterogeneity, consistency, and class effects, and assessing model fit [31].
Essential Experimental Protocols
Protocol 1: The Standard 5-Step NMA Process (Frequentist in Stata)
This protocol outlines the core analytical steps for a valid NMA [29].
- Draw Network Geometry: Visualize the network of treatments and comparisons to understand the evidence structure.
- Check Consistency Assumption: Statistically evaluate the agreement between direct and indirect evidence using global and local tests.
- Generate Forest/Interval Plots: Illustrate the summary comparative effectiveness sizes among the various interventions.
- Calculate Cumulative Rankings: Estimate and present ranking probabilities to identify the most superior interventions.
- Evaluate Publication Bias: Assess the risk of bias, such as through comparison-adjusted funnel plots, for valid inference.
Protocol 2: Handling Inconsistency via Node-Splitting Analysis
This is a detailed methodology for a key step in Protocol 1 [29].
- Objective: To identify which specific treatment comparison(s) are causing global inconsistency.
- Method: For each treatment comparison where both direct and indirect evidence exists:
- Split the node (treatment) to separate the direct evidence from the indirect evidence.
- Estimate the treatment effect using only the direct evidence.
- Estimate the treatment effect using only the indirect evidence.
- Perform a statistical test to check for a significant difference between the direct and indirect estimates.
- Software: This method is implemented in both Stata (
nodesplit) and R (e.g.,netmetapackage).
Key NMA Software and Methodological Tools
Table 1: Research Reagent Solutions: Software & Packages
| Software/Package | Primary Framework | Key Function/Use Case | Key Reference |
|---|---|---|---|
Stata (network) |
Frequentist | Comprehensive suite for NMA, including network graphs, inconsistency tests, and meta-regression. | [29] |
R (netmeta) |
Frequentist | A widely used package for frequentist NMA in R. | [8] |
R (multinma) |
Bayesian | Designed for NMA with class effects and advanced hierarchical models. | [31] |
| Bayesian (Various) | Bayesian | Flexible framework for complex data synthesis (IPD+AD, single-arm trials). | [30] |
Table 2: Key Methodological Tests and Checks
| Concept | Description | How to Test/Check | |
|---|---|---|---|
| Similarity | Methodological and clinical comparability of studies. | Qualitative assessment using PICO (Population, Intervention, Comparator, Outcome). | [29] |
| Transitivity | The logical basis for indirect comparisons. | Assessed indirectly via statistical consistency; underpinned by similarity. | [29] [8] |
| Consistency | Statistical agreement between direct and indirect evidence. | Global test (Wald test) and Local test (Node-splitting). | [29] |
Conceptual Diagrams for NMA Workflows and Relationships
NMA Evidence Network and Transitivity
Process for Investigating Inconsistency
Resolving Real-World Problems: Strategies When Inconsistency is Detected
Frequently Asked Questions (FAQs) on Inconsistency and Effect Modifiers
FAQ 1: What is the fundamental difference between heterogeneity and inconsistency in Network Meta-Analysis? Heterogeneity refers to the variability in treatment effects within the same direct comparison (e.g., across different studies comparing treatment A vs. B). Inconsistency (or incoherence), however, occurs when the direct evidence and the indirect evidence for a specific treatment comparison are in disagreement. This is a specific problem for NMA, as it violates the core assumption of consistency between different sources of evidence [2] [7].
FAQ 2: How can effect modifiers lead to inconsistency in an NMA? Inconsistency can arise when study-level or patient-level characteristics that modify the relative treatment effect (effect modifiers) are imbalanced across the different direct comparisons in the network. For example, if the studies comparing treatment A to B were conducted in a population with high disease severity, and studies comparing A to C were in a population with low severity, the distribution of this effect modifier (severity) is unbalanced. This intransitivity can cause the direct estimate of B vs. C to be inconsistent with the indirect estimate derived via A [7] [32].
FAQ 3: When should I consider using meta-regression in an NMA? Meta-regression should be considered to explore sources of heterogeneity or to investigate potential causes of inconsistency identified by statistical tests. It is a valuable tool for assessing whether a specific covariate (a potential effect modifier) can explain the variation or discrepancy in observed treatment effects across studies [32].
FAQ 4: What is the relationship between transitivity and consistency? Transitivity is an underlying assumption about the study design and the included populations. It requires that the different sets of trials included in the analysis are similar, on average, in all important factors that may affect the relative effects. Consistency (or the absence of incoherence) is the statistical manifestation of this assumption. If transitivity holds, the direct and indirect evidence are expected to be consistent. Violations of transitivity often lead to statistical inconsistency [7].
Troubleshooting Guides for NMA Inconsistency
Problem 1: Significant Global Inconsistency is Detected in the Network
Symptoms:
- Statistical tests (e.g., the design-by-treatment interaction model) indicate the presence of global inconsistency.
- The
I²statistic for inconsistency is high.
Diagnosis and Solution Protocol:
- Confirm the Result: Ensure that the model has been correctly specified and that data extraction is accurate.
- Localize the Inconsistency: Use local methods to identify which specific comparison or loop in the network is driving the inconsistency. Recommended methods include:
- Investigate Effect Modifiers: For the comparison or loop identified in step 2, hypothesize and test for clinical or methodological effect modifiers that may be distributed differently across the studies contributing to the direct and indirect evidence. This is where meta-regression becomes critical.
Problem 2: A Specific Node-Split Shows a Significant Difference Between Direct and Indirect Evidence
Symptoms:
- The node-splitting model for the comparison between treatments
XandYyields a p-value < 0.05, and the confidence intervals for the direct and indirect estimates do not overlap.
Diagnosis and Solution Protocol:
- Characterize the Studies: Create a table summarizing the characteristics of the studies that provide direct evidence for
X vs. Yand the studies that provide the indirect evidence (typically via a common comparatorZ). - Formulate Hypotheses: Based on clinical knowledge, identify covariates that may act as effect modifiers (e.g., year of study, baseline risk, proportion of a specific patient subtype, treatment dose, study duration).
- Apply Meta-Regression: Extend your NMA model to include the suspected covariate. The model can be specified to have:
- Interpret the Findings: A meta-regression model that successfully explains the inconsistency will show a non-significant interaction term and a reduced between-study heterogeneity. If the inconsistency remains, other unmeasured effect modifiers may be at play.
Methodologies for Investigating Inconsistency
| Method | Scope of Assessment | Primary Output | Key Advantage | Key Limitation |
|---|---|---|---|---|
| Cochran's Q (Global) | Global Network | Single Q statistic & p-value | Simple, familiar statistic [2] | Does not locate the source of inconsistency |
| Design-by-Treatment Model | Global Network | Global test for inconsistency | Comprehensive global assessment | Does not identify which comparison is inconsistent |
| Node-Splitting | Local (per comparison) | Direct vs. indirect estimate for each split node | Pinpoints specific inconsistent comparisons [2] | Computationally intensive in networks with many treatments |
| Loop-specific Approach | Local (per loop) | Inconsistency factor for each loop | Intuitive for simple networks [2] | Cumbersome in large networks; limited to loops of three treatments |
Detailed Protocol: Implementing Meta-Regression with Treatment-by-Covariate Interaction
Aim: To adjust for a suspected effect modifier X_j (e.g., baseline risk) and explain heterogeneity/inconsistency in a network meta-analysis of survival outcomes.
Model Specification (based on [32]): This protocol uses a two-dimensional treatment effect model for survival data, extended with a covariate.
Model the Hazard Function: The underlying hazard rate in trial
jfor interventionkat follow-up timetis modeled as:ln(h_jkt) = β_0jk + β_1jk * t^pwheret^0 = ln(t).Define Treatment Effects and Covariate Interaction: The scale (
β_0jk) and shape (β_1jk) parameters are modeled as:The random effects for the scale parameter are drawn from a distribution that includes the covariate:
Here,
β_xbkreflects the impact of study-level covariateX_jon the log hazard ratio of treatmentkversus comparatorb. This can be re-parameterized as(β_xAk - β_xAb), whereβ_xAkis the effect of the covariate for treatmentkversus the overall referenceA.Implementation:
- Software: This model can be implemented in Bayesian software like
OpenBUGSorJAGS, or using frequentist approaches inRorStata. - Likelihood: The model must be coupled with an appropriate likelihood for the time-to-event data (e.g., exponential, Weibull, or Poisson likelihood for aggregate data).
- Assumptions: The choice of
pfor the fractional polynomial and the structure of the covariate interaction (treatment-specific vs. constant) are key model assumptions that should be pre-specified or tested for model fit.
- Software: This model can be implemented in Bayesian software like
The following diagram illustrates the logical workflow for investigating inconsistency, from initial detection to resolution using meta-regression.
Research Reagent Solutions: Methodological Toolkit
Table 2: Essential Methodological Tools for NMA Inconsistency Investigation
| Tool / Method | Function in Investigation | Key Consideration |
|---|---|---|
| Node-Splitting Model | Isolates and quantifies the conflict between direct and indirect evidence for a specific comparison [2]. | Computationally demanding. Best used after a global test signals a problem. |
| Meta-Regression | Tests and adjusts for the influence of study-level covariates (effect modifiers) on treatment effects, potentially explaining inconsistency [32]. | Requires a plausible hypothesis. Power is often low if the number of studies is small. |
| Network Diagrams | Visualizes the available evidence, including the number of studies for each comparison and how treatments are connected. | The thickness of lines can be weighted by the number of studies or patients, helping to identify influential comparisons [33] [34]. |
| GRADE for NMA | Provides a structured framework to rate the certainty (quality) of evidence for each network estimate, allowing for downgrading due to inconsistency [34]. | Inconsistent direct and indirect evidence should lead to downgrading the certainty of the evidence. |
How do I investigate inconsistency between direct and indirect evidence in my NMA?
Answer: Inconsistency (or incoherence) occurs when the relative treatment effects from direct evidence (e.g., from head-to-head trials) disagree with the effects from indirect evidence for the same comparison. To investigate this, you should use both statistical and graphical methods.
Detailed Methodology:
- Local Approaches: Use the node-splitting method to separately calculate the direct and indirect evidence for a specific comparison. A significant difference (p-value < 0.05) between these two estimates indicates local inconsistency. This method is suitable when you have a limited number of closed loops in your network.
- Global Approaches: Implement a design-by-treatment interaction model. This model provides a global test for inconsistency across the entire network. A significant result suggests that the assumption of transitivity may be violated somewhere in the network. This is more suitable for complex networks with many interventions and loops.
You should report the results of both methods, noting the specific comparisons where inconsistency was detected and its potential impact on your network estimates.
What is the difference between a sensitivity analysis and a subgroup analysis in an NMA?
Answer: While both are used to test the robustness of findings, they address different types of uncertainty.
- Subgroup Analysis investigates whether the relative treatment effects vary across different levels of a specific clinical or methodological characteristic (e.g., patient population, disease severity, risk of bias). It directly tests the transitivity assumption by checking if an observed factor modifies the treatment effect.
- Sensitivity Analysis assesses whether the overall conclusions of the NMA are robust to methodological decisions made during the review process. This includes testing the impact of including studies with a high risk of bias, using different statistical models, or varying the set of included studies based on specific criteria.
The table below summarizes the key differences:
| Feature | Subgroup Analysis | Sensitivity Analysis |
|---|---|---|
| Primary Goal | Assess effect modification; test transitivity | Assess robustness to methodological choices |
| What is Varied | Patient or study characteristic (e.g., age, risk of bias) | Inclusion criteria or statistical model |
| Key Question | "Does the treatment effect differ for this subgroup?" | "Do our conclusions change if we alter a key assumption?" |
My sensitivity analysis gives different results. How should I proceed?
Answer: Different results in a sensitivity analysis indicate that your findings are not robust to a particular methodological choice. Your course of action should be as follows:
- Interpret with Caution: Clearly state in your report and conclusions that the findings are sensitive to a specific factor. The overall confidence (or certainty) in the evidence should be downgraded.
- Investigate the Cause: Determine why the results changed. For example, if excluding high risk-of-bias studies alters the result, it suggests that the original estimate was biased by lower-quality studies.
- Present All Results: Report the results from both the primary and sensitivity analyses. This ensures transparency and allows readers to understand the influence of your methodological decisions.
- Base Conclusions on Robust Evidence: Where possible, base your primary conclusions on the analysis deemed most reliable (e.g., the analysis excluding high risk-of-bias studies).
When should I use a random-effects model versus a common-effect model in my NMA?
Answer: The choice between a common-effect (also called fixed-effect) and a random-effects model depends on the presence of heterogeneity.
- Use a common-effect model only if you have strong evidence that heterogeneity is absent (i.e., all studies are estimating the same underlying treatment effect).
- Use a random-effects model when you anticipate or observe heterogeneity, meaning the studies are estimating different, yet related, treatment effects. This is the more conservative and commonly recommended approach in meta-analysis, as it accounts for between-study variation.
The following workflow diagram outlines the decision process:
How do I assess the transitivity assumption in my network?
Answer: Transitivity is the core assumption that the different sets of studies included for the various direct comparisons are sufficiently similar, on average, in all important factors that could modify the treatment effect (effect modifiers). Assessing it involves:
- Identify Potential Effect Modifiers: Based on clinical and methodological knowledge, list factors that could influence the relative treatment effect (e.g., patient baseline risk, disease duration, trial design, year of publication).
- Compare the Distribution of Modifiers: Create a table comparing the distribution of these potential effect modifiers across the different direct comparisons in your network (e.g., A vs. B, A vs. C, B vs. C).
- Evaluate Similarity: Judge whether the distributions are similar enough to satisfy the transitivity assumption. Statistical tests or summary statistics can aid this evaluation.
The table below provides a template for this assessment:
| Direct Comparison | Number of Trials | Mean Patient Age | Disease Severity | Proportion of High RoB Trials |
|---|---|---|---|---|
| Intervention A vs. B | 5 | 65.2 | Moderate | 20% |
| Intervention A vs. C | 8 | 63.8 | Moderate | 25% |
| Intervention B vs. C | 3 | 67.1 | Severe | 33% |
In this hypothetical example, the B vs. comparison shows a different profile for disease severity, which could be a violation of transitivity and should be investigated further with subgroup or meta-regression analysis.
How should I handle multi-component interventions in an NMA?
Answer: Network meta-analysis of multicomponent interventions requires special care to avoid confounding. The goal is to disentangle the effect of individual components.
- Define Components Clearly: Pre-define all relevant components of the interventions (e.g., mode of delivery, provider, intensity).
- Use Appropriate Models: Consider using additive component network meta-analysis models, which assume the effect of a multi-component intervention is the sum of the effects of its individual components.
- Account for Interactions: If interactions between components are suspected (i.e., the effect of one component depends on the presence of another), more complex models that include interaction terms are needed.
- Visualize Component Networks: Use specific graphical tools to visualize the network of components, which can help in understanding the available evidence and the model's assumptions [35].
What are the key reagents and materials for implementing NMA?
Answer: The "research reagents" for conducting a robust NMA are primarily software tools and methodological frameworks.
Research Reagent Solutions Table:
| Item | Function | Example Tools / Frameworks |
|---|---|---|
| Systematic Review Software | To manage the screening and data extraction process. | Covidence, Rayyan |
| Statistical Software & Packages | To perform the statistical NMA, test for inconsistency, and create rankings. | R (packages: netmeta, gemtc, BUGSnet), Stata (network package) |
| Risk of Bias Tool | To assess the methodological quality of individual studies. | Cochrane RoB 2.0 tool, ROBINS-I |
| Certainty of Evidence Framework | To rate confidence in each NMA estimate. | GRADE for NMA [34] [7] |
| Data & Code | To ensure transparency and reproducibility. | Published analysis code (e.g., in R or WinBUGS) and datasets |
How do I use subgroup analysis to explore a potential transitivity violation?
Answer: Subgroup analysis is a direct method to test a hypothesized cause of a transitivity violation. If you suspect a factor (e.g., disease severity) is an effect modifier and is imbalanced across comparisons, you can conduct separate NMAs for each level of that factor (e.g., separate NMAs for 'mild' and 'severe' disease populations).
Methodology:
- Stratify the Network: Split all studies into subgroups based on the potential effect modifier.
- Perform Separate NMAs: Conduct an independent NMA within each subgroup.
- Compare Results: Compare the relative treatment effects and treatment rankings between the subgroup NMAs. If they differ substantially, it provides evidence that the factor is an effect modifier and that transitivity was likely violated in the overall analysis.
This approach helps in understanding how the comparative effectiveness of interventions changes in different clinical contexts.
Frequently Asked Questions
FAQ 1: What are the primary challenges when conducting a Network Meta-Analysis (NMA) with a sparse network? The main challenges involve increased uncertainty and potential instability in effect size estimates. Sparse networks often have limited direct comparison data, making the results highly dependent on the assumptions of consistency between direct and indirect evidence. This can lead to wide confidence intervals and reduced statistical power to detect true effects.
FAQ 2: How can I handle rare events in an NMA? For rare events, standard models can be unstable. Methodological adjustments include:
- Using alternative statistical models like binomial regression models instead of the standard generalized linear model with a logit link.
- Implementing continuity corrections, though the choice of correction method can influence results.
- Considering Bayesian methods with carefully chosen priors to help stabilize estimates.
- Presenting results as risk differences alongside relative effect measures, as they can be more stable in these scenarios.
FAQ 3: What steps can I take to assess the robustness of my NMA findings from a sparse network? Robustness can be assessed through several methods:
- Sensitivity Analyses: Conduct analyses that vary the statistical model (e.g., fixed-effect vs. random-effects) and explore the impact of different prior distributions in Bayesian analyses.
- Inconsistency Checks: Use local and global approaches to check for inconsistency between direct and indirect evidence. If inconsistency is detected, an inconsistency model (e.g., unrelated mean effects model) may be considered.
- Comparison-Adjusted Funnel Plots: Use these to investigate the potential for small-study effects or publication bias within the network.
Troubleshooting Guides
Problem: My network graph is difficult to interpret due to overlapping labels and poor color contrast.
- Issue: Labels on network nodes or edges are not clearly readable.
- Solution: Ensure sufficient color contrast between text and its background. For text within a node, explicitly set the text color (
fontcolor) to have high contrast against the node's fill color (fillcolor) [36]. For standard text, the contrast ratio should be at least 4.5:1 (or 7:1 for enhanced contrast, Level AAA) [37] [38]. For large text, the ratio should be at least 3:1 (or 4.5:1 for enhanced contrast) [37]. - Solution: Use a limited, high-contrast color palette. The following table provides a compliant palette using the specified colors:
| Color Name | HEX Code | Recommended Use |
|---|---|---|
| Google Blue | #4285F4 |
Node fill, Primary edges |
| Google Red | #EA4335 |
Highlighted nodes, Inconsistency |
| Google Yellow | #FBBC05 |
Warning elements, Caution |
| Google Green | #34A853 |
Positive outcomes, Consistency |
| White | #FFFFFF |
Background, Label text on dark nodes |
| Light Grey | #F1F3F4 |
Graph background, Secondary elements |
| Dark Grey | #202124 |
Primary text, Node text on light fills |
| Mid Grey | #5F6368 |
Secondary text, Edge strokes |
Problem: I have concerns about the consistency assumption in my sparse network.
- Issue: Inconsistency between direct and indirect evidence threatens the validity of the NMA.
- Solution:
- Evaluate: Use statistical methods to evaluate inconsistency. A common approach is to use the
ifstatement design-by-treatment interaction model [39]. - Investigate: If inconsistency is found, investigate its source by examining specific closed loops in the network for local inconsistency using the node-splitting method [39].
- Address: If the inconsistency cannot be resolved, consider presenting results from both consistent and inconsistent models, or focus on reporting only the direct evidence.
- Evaluate: Use statistical methods to evaluate inconsistency. A common approach is to use the
Problem: My model fails to converge, or I get highly uncertain estimates.
- Issue: Sparse data can lead to computational and statistical problems.
- Solution:
- Simplify the Model: Start with a fixed-effect model, as random-effects models require estimating more parameters and may not converge with sparse data.
- Use Informative Priors: In a Bayesian framework, consider using more informative priors for the heterogeneity parameter, based on external evidence or expert opinion, to stabilize the model.
- Reduce the Network: If certain interventions have very limited data, consider grouping them or conducting an analysis on a subset of the network.
Methodological Adjustments for Sparse Data and Rare Events
The following table summarizes key methodological adjustments for handling data challenges in NMA.
| Methodological Challenge | Standard Approach | Adjusted Approach for Sparse Networks/Rare Events | Key Considerations |
|---|---|---|---|
| Model Specification | Random-Effects Model | Fixed-Effect Model | Use a fixed-effect model initially to avoid over-parameterization and aid convergence in sparse networks [39]. |
| Handling Rare Events (Zero Cells) | Exclude study or use continuity correction (e.g., add 0.5) | Use advanced statistical models (e.g., Bayesian logistic regression with penalized priors) | Standard corrections can introduce bias; Bayesian methods with carefully chosen priors can provide more stable estimates. |
| Assessing Heterogeneity & Inconsistency | I² statistic, Global inconsistency test (e.g., if statement) |
Node-splitting for local inconsistency, Sensitivity analysis with different priors | Global tests may be underpowered; focus on local tests to pinpoint inconsistency loops [39]. |
| Data Presentation | League tables, Forest plots | Rankograms, Surface Under the Cumulative Ranking curve (SUCRA) with caution, Risk difference plots | Present ranking measures with great caution due to high uncertainty; consider presenting absolute effects. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in NMA Methodology |
|---|---|
R (with netmeta/gemtc packages) |
A free software environment for statistical computing. These packages are essential for performing frequentist and Bayesian NMA, respectively, including network graphics and statistical tests. |
| PRISMA-NMA Checklist | (Preferred Reporting Items for Systematic Reviews and Meta-Analyses): A guideline to ensure the transparent and complete reporting of the NMA, which is critical for assessing validity. |
| CINeMA | (Confidence in Network Meta-Analysis): A software and methodological framework for evaluating the confidence of findings from an NMA across multiple domains, including heterogeneity and inconsistency. |
Stata (network package suite) |
A commercial software for data analysis. The network package suite provides a comprehensive set of commands for performing, visualizing, and evaluating NMA. |
Experimental Protocol: Workflow for a Robust Sparse NMA
The following diagram outlines a recommended workflow for conducting and validating an NMA where sparsity of data or rare events are a concern.
Workflow for Sparse Network Meta-Analysis
Framework for Evaluating Inconsistency
A key part of the methodological adjustment is a rigorous evaluation of the consistency assumption. The diagram below details a framework for investigating inconsistency between direct and indirect evidence.
Inconsistency Evaluation Framework
Frequently Asked Questions
Q1: What is network geometry in a Network Meta-Analysis? Network geometry refers to the arrangement of interventions (nodes) and the available comparisons between them (edges) in an evidence network. It visually represents how direct and indirect evidence connect to form the entire network used for analysis [33].
Q2: How does network connectivity influence my NMA results? Greater connectivity generally strengthens your NMA. When nodes have multiple connections, this provides more pathways for evidence to flow through the network, typically yielding more precise and robust effect estimates. Sparse networks with limited connectivity may produce unstable results [33].
Q3: What are loops in NMA and why are they important? Loops occur when both direct and indirect evidence exists for the same comparison. First-order loops involve one additional intervention, while higher-order loops include more interventions. These loops are crucial because they allow statisticians to check for inconsistency between direct and indirect evidence [33].
Q4: How can I identify potential inconsistency in my network? Inconsistency often appears in closed loops where you have both direct and indirect evidence for the same comparison. Statistical methods like node-splitting can help detect significant differences between direct and indirect estimates within these loops. The presence of inconsistency may violate the transitivity assumption [33].
Q5: What should I do if my network has poorly connected interventions? If certain interventions have few connections, consider whether additional studies might fill these evidence gaps. In analysis, recognize that estimates for poorly connected interventions will rely heavily on indirect evidence and may have wider confidence intervals. Graphical representation can quickly highlight these weak spots in your network [33].
Network Geometry Evaluation Framework
Table: Key Network Geometry Characteristics and Their Impact on NMA Results
| Characteristic | Description | Impact on NMA | Evaluation Method |
|---|---|---|---|
| Network Density | Ratio of existing edges to possible edges | Denser networks typically provide more precise estimates | Visual inspection of network plot; count edges and nodes |
| Node Connectivity | Number of connections each intervention has | Well-connected nodes yield more reliable estimates | Calculate degree centrality for each node |
| Loop Presence | Existence of both direct and indirect evidence paths | Enables inconsistency checking; strengthens evidence base | Identify closed loops in network diagram |
| Evidence Flow | Pathways through which evidence propagates | Multiple pathways reduce reliance on single studies | Trace evidence paths between intervention pairs |
| Network Components | Separate sub-networks without connections | Disconnected components cannot be compared | Check if all nodes connect to the main network |
Table: Troubleshooting Common Network Geometry Issues
| Problem | Detection | Potential Solutions |
|---|---|---|
| Sparse Network | Few edges relative to nodes; isolated interventions | Acknowledge limited evidence; use Bayesian methods with conservative priors; seek additional studies |
| Inconsistency | Significant disagreement between direct and indirect evidence | Test inconsistency statistically; investigate effect modifiers; use inconsistency models |
| Poorly Connected Interventions | Interventions with only one or two connections | Interpret estimates cautiously; highlight uncertainty; consider network meta-regression |
| Asymmetric Evidence | Some comparisons have abundant evidence while others have little | Weight results appropriately; acknowledge evidence imbalance in conclusions |
Experimental Protocols for Network Geometry Assessment
Protocol 1: Visual Network Mapping Methodology
Purpose: To create a standardized visual representation of evidence networks for geometry evaluation.
Materials:
- Network plot software (R, Stata, Python)
- Study inclusion/exclusion criteria
- Intervention classification scheme
Procedure:
- Node Definition: Define each node to represent a specific intervention. Ensure consistent intervention definitions across studies.
- Edge Creation: Draw edges between nodes where direct head-to-head comparisons exist.
- Proportional Scaling: Scale node size according to the number of participants receiving that intervention.
- Edge Weighting: Set edge thickness proportional to the number of trials available for that comparison.
- Layout Optimization: Arrange nodes to minimize edge crossing and improve readability.
- Connectivity Assessment: Visually identify poorly connected nodes and evidence gaps.
Interpretation: A well-connected, dense network suggests robust evidence. Isolated nodes or tenuous connections indicate evidence limitations.
Protocol 2: Quantitative Geometry Analysis Method
Purpose: To numerically characterize network geometry and identify potential problems.
Materials:
- Network data matrix
- Statistical software with network meta-analysis packages
- Inconsistency testing tools
Procedure:
- Calculate Network Density: Divide the number of existing edges by the number of possible edges.
- Assess Node Degree: For each intervention, count its connections to other interventions.
- Identify Evidence Flow: Map all possible evidence pathways between intervention pairs.
- Detect Closed Loops: Systematically identify all first-order and higher-order loops.
- Measure Centrality: Calculate betweenness centrality to identify pivotal interventions.
- Test Consistency: Apply statistical tests (node-splitting, design-by-treatment interaction) to check inconsistency in identified loops.
Interpretation: Networks with density >0.5 and balanced node degrees generally support more reliable NMA.
Research Reagent Solutions
Table: Essential Tools for Network Meta-Analysis Geometry Evaluation
| Tool/Resource | Function | Application Context |
|---|---|---|
| R 'netmeta' package | Comprehensive NMA implementation | Statistical analysis and network visualization |
| Network Plot Diagram | Visual representation of evidence network | Initial geometry assessment and communication |
| Node-Splitting Method | Statistical inconsistency detection | Identifying disagreement between direct and indirect evidence |
| SUCRA Values | Surface under cumulative ranking curve | Treatment hierarchy presentation despite network uncertainty |
| Network Graph Theory Metrics | Quantitative characterization of network structure | Objective assessment of connectivity and complexity |
Network Geometry Visualization
Network Geometry Evidence Flow
Direct and Indirect Evidence Pathways
Technical Guidance for Complex Network Scenarios
Addressing Sparse Networks
When facing limited connectivity, Bayesian approaches with conservative priors can help stabilize estimates. Consider conducting sensitivity analyses to assess how much your conclusions depend on specific connections. Network meta-regression may help account for heterogeneity when direct comparisons are scarce.
Managing Inconsistency
When detecting inconsistency between direct and indirect evidence:
- Investigate potential effect modifiers across studies
- Check for differences in study populations, outcomes, or methodologies
- Consider using random-effects inconsistency models
- Present both consistent and inconsistent models in your results
Complex Intervention Networks
For networks involving complex, multi-component interventions, consider Component Network Meta-Analysis (CNMA). This advanced method estimates individual component effects, whether additive or interactive, providing insights into which components drive effectiveness [40].
Best Practices for Reporting and Interpreting Inconsistency Findings
Frequently Asked Questions
1. What is inconsistency in Network Meta-Analysis? Inconsistency occurs when the direct evidence (e.g., from studies comparing Treatment A vs. B) and the indirect evidence (e.g., inferring A vs. B via a common comparator C) for the same treatment pair disagree. This violates the key NMA assumption of evidence consistency and can threaten the validity of the results [41].
2. What are the primary causes of inconsistency? Inconsistency often stems from clinical or methodological diversity (heterogeneity) across the studies forming the direct and indirect evidence loops. Examples include differences in patient populations, intervention dosages, outcome definitions, or study risk of bias [41].
3. What tools can I use to detect inconsistency? Common approaches include:
- Design-by-treatment interaction model: A global test for the presence of inconsistency anywhere in the network [41].
- Node-splitting: A local test that separately calculates the direct, indirect, and combined evidence for specific treatment pairs to check for disagreement [41].
- Tipping point analysis for correlation: A novel sensitivity analysis in arm-based NMA that assesses how robust the conclusions are to different assumptions about the correlation between treatment effects, which can identify fragile findings in sparse networks [41].
4. My NMA has inconsistency. What should I do next? First, investigate potential effect modifiers by conducting subgroup or meta-regression analyses. If the source is identified, model it explicitly. Second, ensure your model adequately accounts for heterogeneity. Finally, interpret results with caution, clearly report the inconsistency, and consider using methods that account for it, like the arm-based NMA model with a tipping point analysis [41].
5. How can I visualize complex evidence structures to understand inconsistency? Standard network diagrams can become cluttered. For component NMA, consider novel visualizations like CNMA-UpSet plots, CNMA heat maps, or CNMA-circle plots to better represent the data structure and the combinations of components tested across trials [5].
Troubleshooting Guides
Problem: Inconsistent findings between direct and indirect evidence (Node-split shows significant disagreement).
Investigation Protocol:
- Verify Data: Re-check data extraction and coding for accuracy, particularly for the studies involved in the inconsistent loop.
- Assume a Common Heterogeneity Variance: Check if the model assumes a common heterogeneity parameter across the network. If not, consider this alternative model.
- Check for Effect Modifiers:
- Action: Use subgroup analysis or meta-regression to test if a specific clinical or methodological factor (e.g., disease severity, year of publication, intervention dose) explains the disagreement.
- Interpretation: If an effect modifier is found, it may justify presenting stratified results or using a model that incorporates this covariate.
- Evaluate Network Connectivity:
- Action: Examine the network diagram for sparse data and a "star-shaped" structure, where many treatments are only compared to a common control.
- Interpretation: Sparse networks are prone to instability and inaccurate inconsistency estimates [41]. A tipping point analysis is highly recommended in this scenario [41].
Problem: Sparse network with wide credible intervals and unstable estimates.
Investigation Protocol:
- Confirm Sparsity: Create a network diagram and a table of available direct comparisons. A high number of treatments with very few direct head-to-head studies indicates sparsity.
- Perform a Tipping Point Analysis:
- Method: In an Arm-Based NMA model, vary the correlation parameter between the random effects of different treatments. Search for the "tipping point" where the conclusion about a treatment effect's significance (interval conclusion) or its magnitude changes substantively [41].
- Interpretation: If a tipping point is found near the estimated correlation value, the conclusion is fragile and should be reported with caution. This analysis provides a novel measure of robustness [41].
Problem: Difficulty visualizing the evidence structure in a Component NMA.
Investigation Protocol:
- Identify the Limitation: Standard network diagrams may fail when there are many components and complex combinations [5].
- Select an Appropriate Visualization:
- CNMA-UpSet Plot: Use for networks with a large number of components to show which combinations are tested in which trials [5].
- CNMA-Heat Map: Use to inform decisions about which pairwise component interactions to include in the model [5].
- CNMA-Circle Plot: Use to visualize the combinations of components that differ between trial arms [5].
Data Presentation
Table 1: Comparison of Common Inconsistency Detection Methods
| Method | Type of Test | Principle | Key Interpretation |
|---|---|---|---|
| Design-by-treatment interaction | Global | Tests for inconsistency across the entire network of evidence. | A significant p-value (e.g., <0.05) indicates the presence of inconsistency somewhere in the network. |
| Node-splitting | Local | Separately estimates the direct and indirect evidence for a specific treatment comparison. | A significant p-value indicates a disagreement between the direct and indirect evidence for that particular pair. |
| Tipping Point Analysis (for correlation) | Sensitivity (Local) | Varies the correlation strength in an Arm-Based NMA to see how it impacts conclusions [41]. | Identifies the value of the correlation parameter at which a conclusion about a treatment effect changes, indicating fragility. |
Table 2: Key Steps for a Tipping Point Analysis in Arm-Based NMA
| Step | Action | Description / Output |
|---|---|---|
| 1 | Fit AB-NMA Model | Estimate the posterior distribution for the correlation parameter and the treatment effects (e.g., Risk Ratio) [41]. |
| 2 | Select Percentiles | Choose a series of percentiles (e.g., 1%, 2.5%, 5%, 10%, 25%, 50%, ...) from the posterior distribution of the correlation to test [41]. |
| 3 | Refit Model | Fix the correlation parameter at each selected percentile value and refit the AB-NMA model [41]. |
| 4 | Identify Tipping Points | For each treatment pair, determine if and where the 95% CrI includes the null value (interval conclusion) or if the effect magnitude change exceeds a pre-set threshold (e.g., 15%) [41]. |
Experimental Protocols
Protocol 1: Executing a Node-Splitting Analysis
- Model Specification: Use a Bayesian or frequentist NMA framework. The node-splitting model separately estimates the direct evidence (for a specific comparison) and the indirect evidence (from the rest of the network).
- Implementation: This can be implemented in R (using packages like
gemtcorBUGSnet) or in Bayesian software like OpenBUGS, JAGS, or Stan. - Output Monitoring: For the comparison of interest, monitor the posterior distribution (or point estimates) for the direct (
d.dir), indirect (d.ind), and the inconsistency factor (IF = d.dir - d.ind). - Convergence Check: Ensure Markov Chain Monte Carlo (MCMC) chains have converged (using statistics like Gelman-Rubin ˆR < 1.05).
- Interpretation: If the 95% credible interval for the inconsistency factor (
IF) does not include zero, it suggests significant inconsistency for that node.
Protocol 2: Implementing a Tipping Point Analysis for Correlation
- Base Model Fitting: Fit an Arm-Based NMA model with a random effects structure. Use a separation strategy for the variance-covariance matrix, assigning a uniform prior to the correlation parameter [41].
- Posterior Sampling: Extract a chain of posterior samples for the correlation parameter after confirming model convergence.
- Define Analysis Parameters: Select a set of percentiles from the posterior of the correlation (e.g., 1%, 5%, 10%, 25%, 50%, 75%, 90%, 95%, 99%) and a meaningful threshold for effect magnitude change (e.g., 15%) [41].
- Conditional Model Fitting: Refit the AB-NMA model multiple times, each time fixing the correlation parameter (
Ï) at one of the selected percentile values. - Result Synthesis: For each fixed-
Ïmodel and each treatment pair, record the relative effect estimate (e.g., Risk Ratio) and its 95% credible interval. Systematically compare these across the differentÏvalues to identify tipping points [41].
Mandatory Visualization
NMA Inconsistency Investigation Workflow
The Scientist's Toolkit
Table 3: Research Reagent Solutions for NMA
| Item | Function in NMA Research |
|---|---|
| R Statistical Software | The primary programming environment for conducting statistical analyses, including data manipulation, statistical testing, and generating visualizations. |
netmeta Package (R) |
A widely used frequentist package for performing standard contrast-based NMA, including network meta-regression and basic inconsistency checks [5]. |
gemtc Package (R) |
An R package that provides an interface for conducting Bayesian NMA using JAGS, supporting advanced models including node-splitting. |
| OpenBUGS / JAGS | Bayesian software for flexible model specification using Gibbs sampling, essential for complex arm-based models and novel methodologies like tipping point analysis [41]. |
| PRISMA-NMA Checklist | A reporting guideline (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) that ensures transparent and complete reporting of NMA methods and findings. |
| Component NMA (CNMA) Models | A modeling approach that deconstructs interventions into components, useful for understanding which active ingredients drive effects and for managing inconsistency in complex interventions [5]. |
Ensuring Robustness: Comparing Methods and Validating NMA Outcomes
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between heterogeneity and inconsistency in the context of Network Meta-Analysis (NMA)?
In NMA, the term heterogeneity traditionally refers to variability in effect sizes that permeates the entire network, often assumed to follow a normal distribution in random-effects models. Inconsistency is a broader term that refers to discrepancies between studies' results arising from any cause, including subgroup effects, the presence of outlying studies, or a non-normal distribution of effects. Most critically, in NMA, inconsistency specifically refers to a disagreement between direct evidence (from head-to-head comparisons) and indirect evidence (estimated from the available network of comparisons) [42] [43].
Q2: What are the practical consequences of using a test for inconsistency with low statistical power?
A test with low statistical power may fail to detect the presence of true inconsistency in the network. This can lead to authors inappropriately pooling inconsistent data, resulting in network estimates that are biased and misleading for clinical decision-making. This is a particular risk in meta-analyses with a small number of studies [42].
Q3: Beyond the global test, what methods can I use to investigate inconsistency in my NMA?
A key method is to evaluate local inconsistency. This involves using the Separate Indirect from Direct Evidence (SIDE) approach or the node-splitting method. These techniques isolate specific comparisons in the network (e.g., a single treatment contrast) to check for disagreement between the direct estimate of that comparison and the indirect estimate derived from the rest of the network [43].
Q4: My network is sparse, and the conventional Q test is not significant, but I suspect inconsistency. What should I do?
You should consider using alternative tests or measures of inconsistency. The conventional Q statistic, based on the sum of squares, may have low power in sparse networks or when the true between-study distribution is non-normal (e.g., skewed or heavy-tailed). In such cases, a hybrid test that adaptively combines multiple test statistics or tests based on the sum of absolute deviates with different mathematical powers may be more effective at detecting specific inconsistency patterns [42].
Troubleshooting Guides
Problem 1: Detecting Inconsistency in a Sparse Network with Few Studies
Issue: You are conducting an NMA with a limited number of studies (e.g., fewer than 10) and are concerned that standard tests for inconsistency may not be reliable or powerful enough to detect real problems.
Solution: Employ a combination of alternative statistical tests and careful visual and clinical inspection.
Statistical Solution:
- Do not rely solely on the global Q test. Its power is low when the number of studies is small [42].
- Use a hybrid test if available. This type of test combines several test statistics (e.g., based on sums of squares, absolute values, and maximum deviates) to achieve robust power across different inconsistency patterns [42].
- Calculate the power of your inconsistency test. Some advanced statistical software packages allow for the estimation of power for detecting inconsistency. Reporting this can help contextualize a non-significant result.
Methodological & Clinical Solution:
- Perform a node-split analysis. This is crucial for identifying in which specific part of the network direct and indirect evidence disagree [43].
- Check for clinical and methodological heterogeneity. Use a tool like the GRADE framework for NMA to assess intransitivity. Inconsistency often arises from fundamental differences in the studies making the direct and indirect comparisons (e.g., different patient populations, interventions, or outcomes) [43].
- Visualize the network. A network graph can help identify potential sources of conflict, such as a particular study or comparison that is an outlier.
Problem 2: Interpreting a Significant Inconsistency Test Result
Issue: Your global or local inconsistency test has returned a statistically significant result (p-value < 0.05), and you need to determine the next steps.
Solution: A significant test indicates that the assumption of consistency (that direct and indirect evidence are in agreement) is likely violated. Proceed as follows:
Locate the Inconsistency:
- Use a node-splitting analysis to identify which specific treatment contrast(s) are contributing most to the inconsistency [43].
Investigate the Cause:
- Subgroup Analysis and Meta-Regression: Explore whether specific study-level covariates (e.g., year of publication, baseline risk, drug dose) can explain the inconsistency. If a covariate resolves the inconsistency, you may present subgroup-specific or covariate-adjusted estimates.
- Sensitivity Analysis: Exclude studies one-by-one or in groups (e.g., studies at high risk of bias, outliers identified statistically) to see if the inconsistency disappears. Report all analyses transparently.
Report and Conclude:
- Do not ignore the finding. Report the inconsistency clearly in your manuscript.
- Present both direct and indirect estimates for the problematic comparison alongside the inconsistent network model estimate.
- Downgrade the certainty of evidence for the affected comparisons using the GRADE framework, explicitly citing inconsistency as a reason.
- In severe cases where the inconsistency cannot be explained or resolved, avoid reporting a single network estimate for the affected comparisons, as it may be misleading [43]. Instead, conclude that the evidence is conflicting and highlight the need for more direct studies.
Experimental Protocols for Inconsistency Detection
Protocol 1: Standard Procedure for Global Inconsistency Assessment
Aim: To evaluate the presence of overall inconsistency in the entire network of evidence.
Methodology: The Q statistic is the standard approach for testing global heterogeneity and inconsistency. The test statistic is calculated as follows [42]:
Formula:
Q = Σ wi (Yi - Ŷ)²
Where:
wiis the weight of each study (typically the inverse of the variance).Yiis the observed effect size in studyi.Ŷis the summary effect size estimate under the common-effect model.
Procedure:
- Model Fitting: Fit a consistency model to your network (a model that assumes direct and indirect evidence are in agreement).
- Calculate the Q statistic: The model will output a value for the total Q.
- Hypothesis Testing: Under the null hypothesis of consistency, the Q statistic follows a chi-squared distribution with degrees of freedom (df) equal to the number of comparisons minus one.
- Interpretation: A p-value below a pre-specified significance level (e.g., 0.10 or 0.05 due to the test's often low power) suggests significant global inconsistency in the network.
Protocol 2: Application of Alternative and Hybrid Tests
Aim: To detect inconsistency with higher power in scenarios where the conventional Q test may fail, such as with non-normal between-study distributions or outliers.
Methodology: This involves using a family of alternative test statistics and a procedure to combine them [42].
Procedure:
- Calculate Standardized Deviates: For each study
i, compute the standardized deviate. - Compute Alternative Statistics: Calculate a suite of test statistics,
T(p), using the formula:T(p) = Σ |deviate_i|^pfor different integer powersp(e.g., p=1, 2, 3).p=2yields the conventional Q statistic.p=1is more robust to outliers.- As
papproaches infinity, the statistic converges to the maximum deviate, which is powerful for detecting single outliers.
- Hybrid Test:
- Compute the p-value for each of the individual
T(p)statistics. - The hybrid test statistic is the minimum of these p-values.
- A parametric resampling procedure (e.g., bootstrapping) is used to derive the null distribution of this minimum P-value and obtain an accurate empirical p-value for the hybrid test.
- Compute the p-value for each of the individual
- Interpretation: The hybrid test adapts to the pattern of inconsistency in the data, providing robust power across various scenarios, including heavy-tailed or skewed distributions.
Quantitative Data on Inconsistency Tests
Table 1: Comparison of Statistical Tests for Detecting Inconsistency
| Test Statistic | Mathematical Power (p) | Strengths | Limitations | Ideal Use Case |
|---|---|---|---|---|
| Conventional Q | 2 (Sum of Squares) | Standard, widely used, well-understood theoretical properties under normality [42]. | Low power for small studies, non-robust to outliers, power loss under non-normal distributions [42]. | Large networks with approximately normal between-study distribution. |
| Absolute Value-based (T(1)) | 1 (Sum of Absolute Values) | More robust to the influence of outlying studies [42]. | Less familiar to researchers, requires resampling for P-value. | Networks where you suspect a few moderate outliers. |
| Higher Power (T(3)) | 3 (Sum of Cubes) | Gives more weight to larger deviates, can be more sensitive to specific non-normal patterns [42]. | Can be overly sensitive to a single large deviate, requires resampling for P-value. | Skewed between-study distributions. |
| Maximum Deviate | ∞ (Maximum) | Highly powerful for detecting a single outlying study [42]. | Insensitive to inconsistency spread across multiple studies, requires resampling for P-value. | Screening for a single dominant outlier in a network. |
| Hybrid Test | Adaptive (Minimum P-value) | Robustly high power across diverse inconsistency patterns (heavy-tailed, skewed, outliers) [42]. | Computationally intensive, requires specialized software or coding. | Default choice when the pattern of inconsistency is unknown. |
The Scientist's Toolkit: Essential Reagents & Materials
Table 2: Key Reagent Solutions for NMA Inconsistency Research
| Item / Reagent | Function / Purpose in the Experiment |
|---|---|
| Statistical Software (R/Stata) | Platform for performing all statistical computations, model fitting, and hypothesis tests. Essential for executing meta-analysis packages. |
NMA Package (e.g., netmeta in R) |
Software library specifically designed to fit network meta-analysis models, calculate the Q statistic, and perform basic inconsistency checks. |
| Node-Splitting Module | A specialized software tool or procedure to separate direct and indirect evidence for each comparison, which is critical for locating inconsistency [43]. |
| GRADE Framework for NMA | A methodological tool to assess the certainty of evidence (quality) in an NMA, providing a structured way to rate down for inconsistency and intransitivity [43]. |
| Parametric Resampling Code | Custom or pre-written code (e.g., in R) to perform bootstrapping or permutation tests, which is necessary for calculating P-values for alternative and hybrid tests [42]. |
| Network Graph Visualization Tool | Software to generate a diagram of the treatment network, which helps in understanding its structure and identifying potential sources of intransitivity. |
Visualization of Workflows
NMA Inconsistency Assessment Workflow
Hybrid Test Methodology
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q: What is the most critical, yet often poorly reported, step when defining interventions for a Network Meta-Analysis (NMA) of complex public health interventions? A: The node-making process—how interventions or their components are grouped into distinct nodes for comparison—is critically important but often poorly reported [44] [45]. Insufficient reporting of this process makes it difficult to interpret and apply NMA results.
Q: Our NMA includes both pharmacological and complex non-pharmacological interventions (e.g., for diabetes management). How should we define nodes to ensure a valid and interpretable network? A: For complex interventions, you must explicitly choose and report your node-making approach. The two primary strategies are [45]:
- Lumping: Grouping similar whole interventions or intervention types into single nodes. This is common but requires clear justification for the groupings.
- Splitting: Defining nodes based on specific, distinct components of the interventions, which can help understand the effect of individual components.
Q: What are the primary methods to support the node-making process, as no formal consensus exists? A: A review of NMAs found that when a node-making process was reported, the methods used were primarily [44]:
- Fitting a previously published intervention classification.
- Using expert consensus to define intervention groups.
Q: When generating network diagrams programmatically with tools like Graphviz, how can I ensure my figures are accessible to readers with color vision deficiencies? A: Adhere to the WCAG 2.1 Level AA guidelines for non-text contrast. Ensure a minimum contrast ratio of 3:1 between the colors of graphical objects (like nodes and arrows) and their background [46] [47]. Furthermore, for any node containing text, explicitly set the text color to have a high contrast (at least 4.5:1 for normal text) against the node's fill color [37] [48].
Common Error Investigation Protocol
Issue: Inconsistency between direct and indirect evidence is detected in your NMA.
| Investigation Step | Action | Documentation / Output |
|---|---|---|
| 1. Verify Network Structure | Check if the inconsistency is localized to a specific comparison or widespread. Visually inspect the network geometry. | A network diagram generated via Graphviz or similar tool. |
| 2. Interrogate Node Definitions | Scrutinize the clinical and methodological homogeneity of interventions lumped into the nodes involved in the inconsistent loop. This is a potential major source of inconsistency. | A table justifying the composition of each node, referencing clinical guidelines or expert input [44]. |
| 3. Check for Effect Modifiers | Perform subgroup analysis or meta-regression to investigate if patient-level or study-level covariates (e.g., disease severity, background therapy) explain the disagreement. | A summary table of subgroup/meta-regression results. |
| 4. Apply Statistical Methods | Use statistical methods to evaluate and handle inconsistency, such as the design-by-treatment interaction model or node-splitting. | A summary of the inconsistency model's fit statistics (e.g., p-value, I² for inconsistency). |
Experimental Protocols & Data Presentation
Protocol: Defining Nodes for a Complex Intervention NMA
This protocol outlines a systematic approach to the node-making process, based on a typology of elements identified from a review of public health NMAs [45].
Objective: To create a clinically meaningful and methodologically sound set of nodes for a Network Meta-Analysis.
Materials:
- List of all unique interventions from the systematic review.
- Detailed descriptions of each intervention's components.
- Access to relevant clinical guidelines and published intervention classifications.
- A multi-disciplinary panel of experts (e.g., clinicians, methodologies, public health specialists).
Methodology:
- Approach & Ask: Decide on the primary analytical approach (e.g., intervention-level vs. component-level). Formulate the clinical question that defines what constitutes a "different" intervention.
- Aim & Appraise: Define the goal of the NMA (e.g., to rank whole interventions or to identify active components). Critically appraise the extracted intervention data for completeness and homogeneity.
- Apply & Adapt: Apply a pre-specified rule set to group interventions. This could be:
- Rule Set A (Lumping): Group interventions with identical or highly similar core components and delivery modes.
- Rule Set B (Splitting): Deconstruct interventions into their core components and define nodes for specific combinations or single components.
- Assess: Perform a sensitivity analysis to test how different, clinically plausible node definitions affect the NMA results and consistency.
Table 1: Methods Used to Form Nodes in Published Network Meta-Analyses of Complex Interventions [45]
| Node-Making Method | Description | Frequency in Review (n=102 networks) |
|---|---|---|
| Grouping Similar Interventions | Lumping whole interventions or intervention types based on shared characteristics. | 65 (63.7%) |
| Combining Components | Defining nodes as specific combinations of intervention components (splitting approach). | 26 (25.5%) |
| Using a Classification | Applying an underlying, pre-existing component classification system to group interventions. | 5 (4.9%) |
| Comparing Named Interventions | Treating each uniquely named intervention as a distinct node. | 6 (5.9%) |
Table 2: WCAG 2.2 Level AA Color Contrast Requirements for Diagrams [46] [47]
| Element Type | Definition | Minimum Contrast Ratio |
|---|---|---|
| Normal Text | Text smaller than 18.66px or not bold. | 4.5:1 |
| Large Text | Text at least 18.66px or at least 14pt bold (approx. 18.66px). | 3:1 |
| Graphical Objects & UI Components | Essential parts of diagrams, icons, form input borders, and node outlines. | 3:1 |
Mandatory Visualizations
Diagram 1: Node Making Approaches
Diagram 2: Evidence Inconsistency
The Scientist's Toolkit
Table 3: Research Reagent Solutions for NMA Methodologists
| Item / Solution | Function in the NMA Context |
|---|---|
| Expert Consensus Panel | A multi-disciplinary team (clinicians, content experts, methodologies) used to define and validate the clinical homogeneity of nodes, supporting the node-making process [44]. |
| Pre-existing Intervention Classification | A published taxonomy or framework (e.g., for behavioral interventions) used to systematically group complex interventions into nodes for analysis [45]. |
| Statistical Inconsistency Model | A statistical model (e.g., design-by-treatment interaction model) used to quantitatively assess the presence of inconsistency between direct and indirect evidence in the network. |
| Node-Splitting Technique | A specific statistical method that separates evidence for a particular comparison into direct and indirect components, allowing for a formal test of their disagreement. |
| Component Network Meta-Analysis (CNMA) | An analytical framework that defines nodes not as whole interventions, but as individual components, aiming to identify the most effective active ingredients [45]. |
Frequently Asked Questions
What is the primary cause of inconsistency in a Network Meta-Analysis? Inconsistency (or incoherence) occurs when the direct evidence (e.g., from studies comparing A vs. B) disagrees with the indirect evidence (e.g., A vs. B via a common comparator C) for the same intervention comparison [7]. A common cause is a violation of the transitivity assumption, which means that effect modifiers—study or population characteristics that influence the treatment effect—are not balanced across the different direct comparisons in the network [34] [33]. For example, if studies comparing Intervention A to C are conducted in a population with more severe disease than the studies comparing A to B, the resulting indirect estimate for B vs. C may be biased and inconsistent with any available direct evidence [7].
How can I statistically test for the presence of inconsistency? There are several statistical approaches to test for inconsistency [49]:
- Design-by-treatment interaction model: This is a global test that assesses inconsistency across the entire network simultaneously [7].
- Side-splitting method: This is a local test that separately evaluates the inconsistency for each comparison in the network that is informed by both direct and indirect evidence. It works by comparing the direct estimate to the indirect estimate for that specific pair of interventions [7].
- Node-splitting method: This is another local test that "splits" the contribution of a particular treatment (node) into direct and indirect evidence to see if they disagree [7].
The table below summarizes the pros and cons of these methods based on a scoping review of NMA practices [49].
| Method | Description | Advantages | Disadvantages/Limitations in Practice |
|---|---|---|---|
| Design-by-Treatment Interaction | A global model assessing inconsistency throughout the entire network [7]. | Provides an overall test for the network. | Found to be used infrequently in a review of 28 NMAs [49]. |
| Side-Splitting Method | A local test comparing direct and indirect evidence for each specific comparison [7]. | Pinpoints which specific comparison is inconsistent. | Limited reporting on its application in practice [49]. |
| Node-Splitting Method | A local test splitting evidence for a treatment node into direct and indirect contributions [7]. | Helps identify which treatment(s) are involved in inconsistency. | Used in only about 18% of the reviewed NMAs [49]. |
My NMA shows significant inconsistency. What are my options? If you detect important inconsistency, you should not simply ignore it. Here are steps you can take [7]:
- Investigate the source: Check if the inconsistency can be explained by clinical or methodological differences (effect modifiers) between the studies forming the direct and indirect evidence.
- Report both estimates: Present both the direct and indirect estimates separately and report the network estimate with caution.
- Use an inconsistency model: Some statistical models can directly incorporate and estimate inconsistency parameters.
- Present the higher-certainty evidence: If the direct and indirect evidence have different certainties (e.g., assessed by GRADE), present the estimate from the higher-certainty source. If they are equal, you may use the network estimate but consider downgrading the evidence for incoherence [34].
- Conduct sensitivity analysis: Exclude studies that are suspected to be the primary drivers of the inconsistency (e.g., studies at high risk of bias or with outlying characteristics) and re-run the analysis to see if the inconsistency resolves.
Troubleshooting Guides
Problem: Inconsistency detected between direct and indirect evidence. Solution: Follow this methodological workflow to investigate and address the issue.
Protocol: Investigating the Transitivity Assumption
- Objective: To assess whether the distribution of potential effect modifiers is sufficiently similar across the different treatment comparisons in the network.
- Method: Create a table of study characteristics for each direct comparison pair (e.g., A vs. B, A vs. C, B vs. C). The table should include [7]:
- Patient demographics: e.g., mean age, disease severity, comorbidities.
- Intervention details: e.g., dosage, delivery method, concomitant therapies.
- Methodological factors: e.g., risk of bias, year of publication, study duration.
- Analysis: Visually inspect and statistically compare (e.g., using ANOVA for continuous variables or chi-square for categorical variables) the characteristics across the different comparison groups. A notable imbalance in a known effect modifier suggests a potential violation of transitivity.
Problem: My network is poorly connected, leading to imprecise and unreliable indirect estimates. Solution: A poorly connected network has sparse direct comparisons, making the entire network fragile and indirect estimates highly uncertain.
- Diagnosis: Examine your network diagram. If it consists of long chains of comparisons (e.g., A-B, B-C, C-D) with very few or no closed loops, the network is poorly connected [33]. The width of the lines (number of studies) and nodes (sample size) in the diagram will also be small [34].
- Actions:
- Verify search strategy: Ensure your literature search was comprehensive and did not miss relevant studies.
- Reconsider network scope: Evaluate if the interventions are too diverse or if the patient population is too narrow.
- Report limitations transparently: Acknowledge that the sparse network is a major limitation and that findings, especially indirect estimates and treatment rankings, are highly uncertain. Avoid strong conclusions based on such a network [33].
Problem: Treatment rankings (like SUCRA) are being overinterpreted. Solution: The Surface Under the Cumulative Ranking (SUCRA) curve is a common but often misused ranking metric.
- The Issue: SUCRA ranks treatments from "best" to "worst" but only considers the effect estimate, ignoring the precision of the estimate and the certainty of the underlying evidence [34]. An intervention supported by small, low-quality trials that report large effects can be ranked highly, which is misleading.
- Best Practices:
- Prioritize effect estimates over ranks: Always base clinical decisions primarily on the relative effect estimates (e.g., odds ratios) and their confidence intervals between treatments, not on the rank itself [34] [43].
- Contextualize rankings: Use minimally or partially contextualized ranking approaches that consider the magnitude of the effect and the certainty of evidence, rather than relying solely on SUCRA [34].
- Report certainty of evidence: Apply the GRADE framework to rate the confidence in each pairwise comparison, which helps put the rankings into perspective [7].
Research Reagent Solutions
The table below lists key methodological tools and their functions for conducting a robust sensitivity analysis in an NMA.
| Tool / Method | Primary Function | Key Application in Sensitivity Analysis |
|---|---|---|
| GRADE for NMA [34] [7] | Evaluates the certainty (quality) of evidence for each network comparison. | To test if conclusions hold when only high-certainty evidence is included. |
| Meta-Regression [7] | Investigates how study-level covariates (effect modifiers) influence the treatment effect. | To explore and adjust for sources of transitivity violation and inconsistency. |
| Node-Splitting [7] | Statistically tests for local inconsistency for a specific comparison. | To identify which specific node or comparison is driving global inconsistency. |
| SUCRA/P-Score [34] [49] | Provides a numerical hierarchy of treatments from best to worst. | To check the stability of treatment rankings under different model assumptions. |
Experimental Protocol for Sensitivity Analysis
Objective: To test the robustness of NMA conclusions against various assumptions and potential sources of bias.
Detailed Methodology:
- Define Scenarios: Pre-specify the scenarios for your sensitivity analysis. Common scenarios include [49] [7]:
- Restricting analysis to studies at low risk of bias.
- Using an alternative statistical model (e.g., fixed-effect instead of random-effects).
- Excluding outlier studies or studies with specific characteristics (e.g., different dosage, industry-sponsored).
- Analyzing the impact of effect modifiers via meta-regression.
- Re-run the NMA: Execute the NMA model for each pre-specified scenario.
- Compare Key Outputs: For each scenario, compare the following with the primary analysis:
- Network effect estimates: Check if the direction, magnitude, and statistical significance of the core comparisons change.
- Inconsistency measures: Note any changes in global or local inconsistency.
- Treatment rankings: Observe if the hierarchy of treatments remains stable.
- Interpret Results: Conclude that your primary findings are robust if the key conclusions remain unchanged across the different sensitivity analyses. If conclusions change, you must report the findings with caution and explicitly discuss the conditions under which the conclusions hold.
The following workflow visualizes this protocol:
Assessing Certainty of Evidence in the Presence of Inconsistency
A technical guide for researchers navigating discordant sources in Network Meta-Analysis
Fundamental Concepts
What is inconsistency in Network Meta-Analysis? Inconsistency occurs when direct evidence (from head-to-head trials) and indirect evidence (from connected comparisons via a common comparator) yield meaningfully different effect estimates for the same treatment comparison. This threatens the validity of NMA results by violating the transitivity assumption - the fundamental principle that allows indirect comparisons to be valid.
How does inconsistency differ from heterogeneity? While both represent statistical challenges, heterogeneity refers to variability in treatment effects that exceeds random chance within a single comparison, whereas inconsistency specifically describes disagreement between different types of evidence (direct vs. indirect) for the same comparison. Heterogeneity can exist without inconsistency, but inconsistency often manifests as heterogeneity in network models.
Troubleshooting Guide: Identifying and Addressing Inconsistency
Q1: How do I detect inconsistency in my network?
Problem: Suspected disagreement between direct and indirect evidence.
Diagnostic Methods:
- Side-splitting approach: Separately estimates direct and indirect evidence for each comparison and statistically tests their difference
- Node-splitting method: Similar to side-splitting but specifically focuses on splitting contributions at particular nodes in the network
- Design-by-treatment interaction model: Tests consistency across the entire network simultaneously
- Net Heat plots: Visualize inconsistency contributions from specific direct evidence streams
Interpretation tips:
- Focus on clinical and statistical significance - a statistically significant inconsistency may not be clinically important
- Examine contribution matrices to identify which direct comparisons contribute most to inconsistency
- Consider power limitations - some tests have low power to detect inconsistency in sparse networks
Q2: What should I do when I identify significant inconsistency?
Problem: Statistical tests confirm concerning levels of inconsistency.
Resolution Protocol:
- Verify data integrity: Check for data extraction errors, outcome misclassification, or incorrect modeling assumptions
- Investigate clinical and methodological effect modifiers:
- Examine differences in patient characteristics across trials
- Identify variations in treatment dosages, formulations, or administration routes
- Assess risk of bias differences between direct comparison trials
- Model adjustment approaches:
- Implement network meta-regression to account for effect modifiers
- Use inconsistency models that estimate both consistent and inconsistent effects
- Consider component NMA for complex interventions where components may interact [50]
When inconsistency persists:
- Present both direct and indirect estimates separately with appropriate caveats
- Use modified GRADE approaches that downgrade for inconsistency
- Consider excluding problematic comparisons if justified clinically and methodologically
Q3: How should I assess certainty of evidence when inconsistency is present?
Problem: GRADE certainty assessments need modification for inconsistent networks.
Adapted GRADE Framework:
| GRADE Dimension | Standard Application | Modified Approach for Inconsistency |
|---|---|---|
| Risk of Bias | Evaluate individual study limitations | Assess whether bias patterns differ between direct and indirect evidence |
| Inconsistency | Unexplained heterogeneity in effect estimates | Direct vs. indirect disagreement; magnitude and pattern of inconsistency |
| Indirectness | Population, intervention, comparator, outcome issues | Additional consideration of transitivity violations |
| Imprecision | Confidence intervals and optimal information size | Evaluate precision of both direct and indirect estimates separately |
| Publication Bias | Small-study effects and missing evidence | Consider different bias patterns across various comparisons |
Certainty rating adjustments:
- Downgrade by one level: Unexplained inconsistency with large confidence interval overlap between direct and indirect estimates
- Downgrade by two levels: Major, unexplained inconsistency with minimal confidence interval overlap and plausible explanations for differences
- Rate direct and indirect evidence separately when they tell different stories with different clinical implications
Experimental Protocols for Inconsistency Investigation
Protocol 1: Node-Splitting Analysis
Purpose: To detect inconsistency at specific treatment comparisons.
Methodology:
- Identify all treatment comparisons with both direct and indirect evidence
- For each such comparison, split the evidence into direct and indirect components
- Estimate the treatment effect using:
- Only direct evidence
- Only indirect evidence
- All evidence (consistent model)
- Statistically test the difference between direct and indirect estimates using Bayesian or frequentist methods
- Apply multiple testing corrections for the number of comparisons tested
Implementation considerations:
- Requires sufficient direct and indirect evidence for meaningful comparison
- Computational intensity increases with network size and complexity
- Interpretation should consider clinical context, not just statistical significance
Protocol 2: Network Meta-Regression for Inconsistency Investigation
Purpose: To identify and adjust for effect modifiers causing inconsistency.
Methodology:
- Identify potential effect modifiers through clinical reasoning and exploratory analyses
- Collect data on these modifiers for each study in the network
- Implement network meta-regression models that:
- Include interaction terms between treatments and effect modifiers
- Allow different effect sizes across subgroups defined by modifiers
- Test whether inclusion of effect modifiers reduces or eliminates inconsistency
- Validate models using leave-one-out cross-validation or similar techniques
Key considerations:
- Pre-specify potential effect modifiers based on clinical knowledge
- Balance model complexity with available data to avoid overfitting
- Present adjusted and unadjusted estimates to demonstrate impact of adjustments
Research Reagent Solutions
| Tool/Resource | Function | Implementation Notes |
|---|---|---|
| R netmeta package | Frequentist NMA with inconsistency detection | Includes design-by-treatment test and net heat plots |
| BUGS/JAGS | Bayesian NMA implementation | Flexible for node-splitting and inconsistency models |
| CINeMA | Web-based platform for certainty assessment | Implements GRADE for NMA with multiple comparisons |
| Stata network suite | Comprehensive NMA implementation | Includes network graphs and inconsistency diagnostics |
| GRADEpro for NMA | Structured certainty assessment | Guides rating process across multiple comparisons |
Visualization of Evidence Networks and Inconsistency
Evidence Flow for Inconsistency Assessment
NMA Inconsistency Investigation Pipeline
Key Recommendations for Practice
- Pre-specify inconsistency investigations in your protocol rather than conducting only exploratory analyses
- Use multiple diagnostic approaches rather than relying on a single inconsistency test
- Prioritize clinical reasoning over statistical significance when interpreting inconsistency
- Document all investigative steps thoroughly to ensure transparency and reproducibility
- Consider component NMA approaches for complex interventions where treatment components may interact differentially across trials [50]
When implementing these methods, ensure all visualizations maintain sufficient color contrast between text and background elements, with a minimum contrast ratio of 4.5:1 for normal text and 3:1 for large text to guarantee accessibility [51] [46] [52]. This is particularly important for research that may be used in regulatory or clinical decision-making contexts.
Frequently Asked Questions (FAQs)
Q1: What is the key limitation of traditional methods for detecting inconsistency in Network Meta-Analysis? Traditional methods, such as the net heat plot, have significant limitations. They rely on an arbitrary weighting of direct and indirect evidence that can be misleading and do not reliably signal inconsistency or identify which designs cause it. Furthermore, they cannot estimate inconsistency when direct evidence is absent and do not account for differences within various indirect evidence sources [2].
Q2: How does the novel path-based approach improve inconsistency detection? The path-based approach explores all sources of evidence without first separating them into direct and indirect evidence. It uses a measure based on the square of differences to quantitatively capture inconsistency and provides a "Netpath" plot for visualization. This allows it to detect and visualize inconsistencies between multiple evidence paths that would be masked when all indirect sources are considered together [53].
Q3: What is node-splitting and when should it be used? Node-splitting is a method to evaluate inconsistency for a specific treatment comparison by separating the direct evidence for that comparison from the network of indirect evidence. The discrepancy between the relative effect estimates from these two evidence sources indicates the level of inconsistency. It is particularly attractive due to its straightforward interpretation [13] [14].
Q4: My node-splitting analysis is labor-intensive. Are there automated solutions? Yes, automated generation of node-splitting models is available. A defined decision rule can select which comparisons to split, ensuring only comparisons in potentially inconsistent loops are investigated. This automation eliminates most manual work, allowing analysts to focus on interpreting results rather than model setup [13].
Q5: Why might I get different results from node-splitting models when my network has multi-arm trials? Different parameterizations of node-splitting (or "side-splitting") models handle the inconsistency parameter differently. A symmetrical method assumes both treatments in a contrast contribute to inconsistency, while other parameterizations assume only one treatment contributes. These different assumptions yield slightly different results when multi-arm trials are involved [14].
Troubleshooting Guides
Problem: Inconsistent Results Between Global and Local Inconsistency Tests
Symptoms:
- Global tests (e.g., Cochran's Q) suggest inconsistency in the network.
- Local tests (e.g., loop inconsistency approach) do not clearly identify the source.
- Net heat plot fails to highlight problematic designs [2].
Solution: Implement a path-based inconsistency assessment following this protocol:
- Fit the Model: Apply the path-based method using the
netmetaR package [53]. - Calculate Inconsistency Measure: Use the method's quantitative measure based on the square of differences between paths [53].
- Generate Visualization: Create a "Netpath" plot to visualize inconsistencies between various evidence paths [53].
- Interpretation: Identify paths with high inconsistency measures on the Netpath plot. These represent evidence flows contributing most to network inconsistency.
Underlying Principle: This method overcomes limitations of approaches that lump all indirect evidence together, allowing you to pinpoint which specific paths of evidence are in disagreement [53].
Problem: Handling Multi-Arm Trials in Node-Splitting Analysis
Symptoms:
- Difficulty specifying correct node-splitting models when multi-arm trials are present.
- Obtaining different results depending on how the model is parameterized.
- Uncertainty about which treatment in a comparison should "bear" the inconsistency parameter [14].
Solution: Follow this decision framework for node-splitting with multi-arm trials:
Understand Parameterization Options:
- Symmetrical: Both treatments in the contrast contribute equally to inconsistency.
- Asymmetrical: Only one of the two treatments contributes to inconsistency.
Selection Criteria: Choose the parameterization based on your scientific understanding of the treatments. If there is no prior reason to suspect one treatment over the other, the symmetrical method may be preferable.
Implementation: Use automated model generation tools that apply a consistent decision rule to select which comparisons to split, ensuring all potentially inconsistent loops are investigated without manual selection bias [13].
Verification: Check that your software implementation supports your chosen parameterization. The arm-based Generalized Linear Mixed Model (GLMM) can be used to evaluate the side-splitting model [14].
Problem: Visualizing Complex Evidence Networks for Component NMA
Symptoms:
- Standard network diagrams become cluttered and unreadable with many components.
- Difficulty communicating which component combinations have been tested.
- Challenges in understanding the evidence base available for modeling component interactions [50].
Solution: Employ specialized visualizations for Component NMA (CNMA):
- CNMA-UpSet Plot: Best for networks with a large number of components or potential combinations. It clearly presents arm-level data [50].
- CNMA Heat Map: Useful for informing decisions about which pairwise interactions to include in the CNMA model [50].
- CNMA-Circle Plot: Effectively visualizes the combinations of components that differ between trial arms and can be adapted to show additional information like the number of patients or events [50].
Implementation: These novel visualizations improve upon standard network plots by more completely representing the complex data structure of a CNMA, aiding both in model selection and interpretation of results [50].
Method Comparison Table
Table 1: Key Methods for Detecting and Assessing Inconsistency in NMA
| Method | Key Principle | Advantages | Limitations |
|---|---|---|---|
| Path-Based Approach [53] | Explores all evidence paths without pre-separation into direct/indirect. | - Comprehensive evaluation- Detects masked inconsistencies- Provides quantitative measure & visualization (Netpath plot) | - Novel method, less established |
| Node-Splitting [13] [14] | Splits evidence for a comparison into direct and indirect to assess discrepancy. | - Straightforward interpretation- Local assessment of inconsistency | - Can be labor-intensive without automation- Results can vary with parameterization in multi-arm trials |
| Net Heat Plot [2] | Graphically displays inconsistency contribution of designs by temporarily removing them. | - Visual identification of problematic designs | - Underlying calculations can be arbitrary and misleading- Does not reliably signal inconsistency |
| Design-by-Treatment Interaction [13] | Global test for inconsistency across the entire network. | - Unambiguous model specification- Global test for inconsistency | - Harder conceptual interpretation of individual parameters |
Research Reagent Solutions
Table 2: Essential Tools and Methods for Advanced NMA Inconsistency Analysis
| Tool / Method | Function | Implementation / Notes |
|---|---|---|
netmeta R package [53] |
Fits NMA models and now includes the path-based approach for inconsistency. | Essential software environment for implementing the novel path-based method and generating Netpath plots. |
| Automated Node-Splitting Model Generation [13] | Automates the labor-intensive process of creating individual node-splitting models. | Uses a decision rule to select comparisons to split, ensuring all potentially inconsistent loops are investigated. |
| Generalized Linear Mixed Models (GLMM) [14] | Provides a framework for evaluating side-splitting (node-splitting) models. | The arm-based GLMM helps implement and compare different parameterizations of the side-splitting method. |
| Component NMA (CNMA) Models [50] | Synthesizes trials of multi-component interventions by estimating the effect of each component. | Allows prediction of effectiveness for untested component combinations; requires specialized visualizations (e.g., CNMA-UpSet plots). |
Workflow Visualization
The following diagram illustrates the strategic decision process for selecting and applying advanced inconsistency analysis methods in NMA.
Conclusion
Effectively managing inconsistency is not merely a statistical exercise but a fundamental requirement for producing trustworthy Network Meta-Analyses. This synthesis underscores that a multi-faceted approach—combining a solid grasp of foundational assumptions, proficient application of both local and global detection methods, strategic troubleshooting when problems arise, and rigorous validation of results—is essential. The future of NMA lies in the continued development of more robust methods, such as the evidence-splitting and path-based approaches, and their integration into user-friendly software. For biomedical researchers and drug developers, mastering these techniques is paramount to generating reliable evidence that can confidently inform treatment guidelines, health technology assessments, and ultimately, clinical practice. Embracing these comprehensive strategies will enhance the credibility of NMA and solidify its role as a cornerstone of evidence-based medicine.
References
- 1. Consistency and inconsistency in network meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4433772/]
- 2. Identifying inconsistency in network metaâ€analysis: Is the net ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6899484/]
- 3. Ensure High Contrast for Text Over Images [https://www.nngroup.com/articles/text-over-images/]
- 4. Change text color based on brightness of the covered ... [https://stackoverflow.com/questions/11867545/change-text-color-based-on-brightness-of-the-covered-background-area]
- 5. Data visualisation approaches for component network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10502971/]
- 6. tikzstyle default node text with fill color [https://tex.stackexchange.com/questions/48918/tikzstyle-default-node-text-with-fill-color]
- 7. Chapter 11: Undertaking network meta-analyses [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-11]
- 8. Chapter 12 Network Meta-Analysis [https://bookdown.org/MathiasHarrer/Doing_Meta_Analysis_in_R/netwma.html]
- 9. 5 Tips For Understanding Network Meta-Analysis [https://absolutelymaybe.plos.org/2024/02/01/5-tips-for-understanding-network-meta-analysis/]
- 10. Evidence Synthesis for Decision Making 4: Inconsistency in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3704208/]
- 11. Prevalence of evidence of inconsistency and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8543923/]
- 12. Prevalence of evidence of inconsistency and its association ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-021-01401-y]
- 13. Automated generation of nodeâ€splitting models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5057346/]
- 14. Node-Splitting Generalized Linear Mixed Models for ... [https://www.sciencedirect.com/science/article/pii/S1098301516305812]
- 15. Network meta-analysis made simple: a composite ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11213057/]
- 16. Update to the PRISMA guidelines for network meta ... [https://pubmed.ncbi.nlm.nih.gov/39829235/]
- 17. Methods for Indirect Treatment Comparison: Results from a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11036291/]
- 18. Node-splitting model for testing consistency at the treatment ... [https://hugaped.github.io/MBNMAdose/reference/nma.nodesplit.html]
- 19. A design-by-treatment interaction model for network meta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4285290/]
- 20. An assessment of the design-by-treatment interaction ... [https://abstracts.cochrane.org/2023-london/assessment-design-treatment-interaction-model-network-meta-analysis-inconsistency]
- 21. A design-by-treatment interaction model for network meta ... [https://pubmed.ncbi.nlm.nih.gov/29193801/]
- 22. NMA: Network meta-analysis based on multivariate ... [https://www.medrxiv.org/content/10.1101/2025.09.15.25335823v1.full-text]
- 23. Network meta-analysis: a technique to gather evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5386629/]
- 24. A design-by-treatment interaction model for network meta ... [https://www.semanticscholar.org/paper/A-design-by-treatment-interaction-model-for-network-Jackson-Barrett/67a22b71f06d3eea5689642a3b2da13582dcf90b]
- 25. netheat: Net plot in netmeta: heat Meta-Analysis using... Network [https://rdrr.io/cran/netmeta/man/netheat.html]
- 26. How to set colors for nodes in NetworkX? [https://stackoverflow.com/questions/27030473/how-to-set-colors-for-nodes-in-networkx]
- 27. How to maximize "contrast" between nodes on a graph? [https://or.stackexchange.com/questions/5423/how-to-maximize-contrast-between-nodes-on-a-graph]
- 28. Tutorial — NetworkX 3.6 documentation [https://networkx.org/documentation/stable/tutorial.html]
- 29. Network meta-analysis: application and practice using Stata [https://pmc.ncbi.nlm.nih.gov/articles/PMC5733388/]
- 30. Bayesian network meta-analysis methods for combining ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-022-01657-y]
- 31. Network Meta-Analysis with Class Effects: A Practical ... [https://pubmed.ncbi.nlm.nih.gov/41204833/]
- 32. Meta-regression models to address heterogeneity and ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-12-152]
- 33. Understanding Network Metaâ€Analysis: A Practical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271649/]
- 34. A clinician's guide to network meta-analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9307840/]
- 35. Graphical tools for visualizing the results of network meta- ... [https://pubmed.ncbi.nlm.nih.gov/36541111/]
- 36. Appearance Customization | v-network-graph - GitHub Pages [https://dash14.github.io/v-network-graph/examples/appearance.html]
- 37. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 38. Text has enhanced contrast - Rules - Siteimprove [https://alfa.siteimprove.com/rules/sia-r66]
- 39. Text Network Analysis: Methodology and Applications [https://infranodus.com/docs/text-network-analysis]
- 40. Analysing complex interventions using component network ... [https://www.medrxiv.org/content/10.1101/2025.06.30.25330567v1.full-text]
- 41. Tipping point analysis in network meta- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527527/]
- 42. Alternative tests and measures for between-study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12632047/]
- 43. Network meta-analysis: a powerful tool for clinicians ... [https://www.sciencedirect.com/science/article/pii/S0895435624002932]
- 44. Node-making process in network meta-analysis of ... [https://pubmed.ncbi.nlm.nih.gov/29196202/]
- 45. A methodological review of network meta-analyses applied ... [https://www.sciencedirect.com/science/article/pii/S0895435625001891]
- 46. Contrast Checker [https://webaim.org/resources/contrastchecker/]
- 47. Contrast requirements for WCAG 2.2 Level AA [https://www.makethingsaccessible.com/guides/contrast-requirements-for-wcag-2-2-level-aa/]
- 48. Text color must provide high contrast with its background [https://docs.acquia.com/web-governance/text-color-must-provide-high-contrast-its-background]
- 49. Network meta-analysis of prediction models using ... [https://www.sciencedirect.com/science/article/pii/S0895435625003397]
- 50. Data visualisation approaches for component network meta ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-02026-z]
- 51. Text has minimum contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/afw4f7/]
- 52. Text has minimum contrast - Rules - Siteimprove [https://alfa.siteimprove.com/rules/sia-r69]
- 53. Path-Based Approach for Detecting and Assessing ... [https://arxiv.org/abs/2506.20364]