Comparative Drug Efficacy Research: Guidelines, Methods, and Real-World Applications
This article provides a comprehensive guide to comparative drug efficacy research for drug development professionals and researchers.
Comparative Drug Efficacy Research: Guidelines, Methods, and Real-World Applications
Abstract
This article provides a comprehensive guide to comparative drug efficacy research for drug development professionals and researchers. It covers foundational concepts, advanced methodological approaches including adjusted indirect comparisons and mixed treatment comparisons, strategies for troubleshooting common challenges in trial design and implementation, and frameworks for validation and interpretation of results. The content synthesizes current best practices to support robust evidence generation for clinical and regulatory decision-making in the absence of direct head-to-head trials.
Understanding Comparative Efficacy: Foundations and Critical Concepts
In the realm of drug development, the terms "efficacy" and "effectiveness" represent critically distinct concepts that describe drug performance at different stages of the evidence generation continuum. Efficacy refers to the capacity of a therapeutic intervention to produce a beneficial result under ideally controlled conditions, such as those found in randomized clinical trials (RCTs). In contrast, effectiveness describes its performance in real-world clinical practice among heterogeneous patient populations under routine care conditions. This whitepaper delineates the methodological, population, and contextual distinctions between these concepts, supported by contemporary regulatory frameworks and empirical evidence. It further provides structured protocols for designing studies that generate complementary evidence on both constructs, thereby supporting robust comparative drug efficacy research and informed healthcare decision-making.
Drug development relies on a progressive evidence generation pathway, moving from highly controlled experimental settings to pragmatic real-world observation. This pathway begins with efficacy establishment in clinical trials, which are designed to determine whether an intervention works under ideal circumstances. These studies prioritize high internal validity by rigorously controlling variables through strict inclusion/exclusion criteria, protocol-mandated procedures, and randomization to minimize bias [1] [2].
Following regulatory approval, evidence generation shifts toward assessing effectiveness—how the intervention performs in routine clinical practice among diverse patient populations, with comorbid conditions, concurrent medications, and varying adherence patterns. These real-world studies prioritize external validity (generalizability) to inform clinical practice, health policy, and reimbursement decisions [1] [3].
The distinction is not merely academic; it has profound implications for patient care and resource allocation. Comparative drug efficacy research must account for this continuum to produce meaningful, translatable findings. Modern regulatory guidance, including the ICH E6(R3) Good Clinical Practice guideline, now explicitly supports using real-world data and innovative trial designs to bridge this evidence gap [4] [5].
Conceptual Frameworks and Key Distinctions
Defining the Core Concepts
Efficacy: The measurable ability of a therapeutic intervention to produce the intended beneficial effect under ideal and controlled conditions, typically assessed in Phase III randomized controlled trials (RCTs). The primary question efficacy seeks to answer is: "Can this intervention work under optimal circumstances?" [2]
Effectiveness: The extent to which an intervention produces a beneficial outcome when deployed in routine clinical practice for broad, heterogeneous patient populations. The central question for effectiveness is: "Does this intervention work in everyday practice?" [1] [2]
The Efficacy-Effectiveness Relationship Diagram
The following diagram illustrates the conceptual relationship and evidence continuum between efficacy and effectiveness research:
Methodological Differences: A Comparative Analysis
The distinction between efficacy and effectiveness manifests concretely through divergent methodological approaches across key study dimensions. The table below systematically compares these methodological characteristics.
Table 1: Methodological Comparison of Efficacy vs. Effectiveness Studies
| Study Characteristic | Efficacy (Clinical Trials) | Effectiveness (Real-World Studies) |
|---|---|---|
| Primary Objective | Establish causal effect under ideal conditions | Measure benefit in routine practice |
| Study Design | Randomized Controlled Trials (RCTs) | Observational studies, pragmatic trials, registry analyses |
| Patient Population | Homogeneous; strict inclusion/exclusion criteria [2] | Heterogeneous; broad eligibility reflecting clinical practice [1] |
| Sample Size | Often limited by design and cost | Typically larger, population-based [1] |
| Intervention Conditions | Protocol-mandated, standardized, strictly enforced | Flexible, tailored to individual patient needs |
| Comparator | Placebo or active control | Routine care, multiple active comparators |
| Setting | Specialized research centers, academic institutions [2] | Diverse real-world settings (hospitals, clinics, community practices) |
| Data Collection | Prospective, structured for specific research purpose | Often retrospective, from medical records, claims databases, or registries |
| Outcome Measures | Clinical surrogate endpoints, primary efficacy endpoint | Patient-centered outcomes, composite endpoints, healthcare utilization |
| Follow-up Duration | Fixed, predetermined duration | Variable, often longer-term |
| Internal Validity | High (through randomization, blinding, protocol control) | Variable, requires rigorous methods to address confounding |
| External Validity | Limited (restrictive eligibility) | High (broadly representative populations) |
Case Study: Evidence from Fabry Disease and Multiple Myeloma
Fabry Disease Treatment Outcomes
A recent systematic literature review of Fabry disease treatments provides a compelling case study contrasting efficacy and effectiveness evidence [2]. The review analyzed 234 publications, with the majority (67%) being real-world observational studies, and the remainder (32%) clinical trials.
Efficacy Evidence from Clinical Trials: Enzyme replacement therapy (ERT) with agalsidase alfa or beta demonstrated stabilization of renal function and cardiac structure in controlled trial settings. These trials established that early initiation of ERT in childhood or young adulthood was associated with better renal and cardiac outcomes compared to later initiation [2].
Effectiveness Evidence from Real-World Studies: The large number of observational studies provided complementary evidence on treatment performance in heterogeneous patient populations over extended periods. These studies confirmed that treatment effects observed in trials generally translated to real-world practice, but also provided insights into long-term outcomes, safety profiles, and comparative effectiveness across different patient subgroups that were not represented in the original trials [2].
The Fabry disease case highlights a critical challenge in comparative efficacy research: the high heterogeneity of study designs and patient populations in real-world evidence, which often precludes direct cross-study comparisons and meta-analyses [2].
Multiple Myeloma Treatment Patterns
A population-based study specifically designed to compare clinical trial efficacy versus real-world effectiveness in multiple myeloma treatments further illustrates this dichotomy [1] [3]. Such comparative studies are essential for understanding whether efficacy benchmarks established in trials are translated into clinical practice, particularly for complex therapeutic regimens that may be challenging to implement outside research settings.
Experimental Protocols and Methodological Approaches
Clinical Trial Protocol Design (Efficacy Assessment)
The SPIRIT 2025 statement provides updated guidelines for clinical trial protocols, emphasizing comprehensive reporting to enhance study quality and transparency [6]. The following workflow outlines the core components of efficacy-oriented trial design:
Detailed Protocol Components [6]:
- Structured Summary: Comprehensive trial design overview following WHO Trial Registration Data Set
- Patient Population: Strict eligibility criteria to create homogeneous study cohort
- Intervention Protocol: Precise description of treatment regimen, dosage, administration schedule
- Comparator Selection: Placebo or active control with randomization procedures
- Primary Endpoint: Clinically relevant efficacy measure with specified assessment timeline
- Sample Size Justification: Statistical power calculation based on expected effect size
- Data Collection Methods: Standardized case report forms with rigorous quality control
- Statistical Analysis Plan: Pre-specified analysis methods, including handling of missing data
Real-World Evidence Generation Protocol (Effectiveness Assessment)
For real-world effectiveness studies, the methodological approach must address different challenges, particularly confounding and data quality issues:
Table 2: Real-World Evidence Generation Protocol
| Protocol Component | Methodological Approach | Considerations |
|---|---|---|
| Data Source Selection | Electronic health records, claims databases, disease registries | Assess completeness, accuracy, and representativeness of data |
| Study Population | Broad inclusion criteria reflecting clinical practice | Define eligibility based on treatment patterns rather than strict criteria |
| Exposure Definition | Treatment patterns based on actual prescriptions/administration | Account for treatment switching, discontinuation, and adherence |
| Comparator Group | Active treatment comparison using propensity score methods | Address channeling bias and unmeasured confounding |
| Outcome Measurement | Clinical events, patient-reported outcomes, healthcare utilization | Validate outcome definitions in specific data source |
| Follow-up Period | From treatment initiation to outcome, discontinuation, or end of study | Account for variable follow-up and informative censoring |
| Confounding Control | Multivariable adjustment, propensity scores, instrumental variables | Conduct sensitivity analyses to assess robustness |
| Statistical Analysis | Time-to-event analysis, marginal structural models | Account for time-varying confounding and competing risks |
Regulatory and Methodological Evolution
Modernizing Clinical Trial Frameworks
Recent regulatory updates reflect the growing importance of bridging the efficacy-effectiveness gap:
ICH E6(R3) Good Clinical Practice: The updated guideline introduces "flexible, risk-based approaches" and embraces "modern innovations in trial design, conduct, and technology" [4] [5]. It specifically addresses non-traditional interventional trials and those incorporating real-world data sources, facilitating more pragmatic designs that can generate both efficacy and effectiveness evidence [5].
SPIRIT 2025 Statement: The updated guideline for clinical trial protocols now includes items on patient and public involvement in trial design, conduct, and reporting, enhancing the relevance of trial outcomes to real-world stakeholders [6].
Estimand Framework Implementation
The adoption of ICH E9(R1) on estimands represents a significant methodological advancement for aligning efficacy and effectiveness assessment [4]. The estimand framework clarifies how intercurrent events (e.g., treatment switching, discontinuation) are handled in the definition of treatment effects, creating a more transparent link between the clinical question of interest and the statistical analysis.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Comparative Efficacy-Effectiveness Research
| Tool/Resource | Function/Purpose | Application Context |
|---|---|---|
| SPIRIT 2025 Checklist | 34-item checklist for comprehensive trial protocol design [6] | Ensuring methodological rigor and transparency in efficacy studies |
| ICH E6(R3) GCP Guideline | Framework for ethical, quality clinical trial conduct [4] [5] | Implementing risk-based approaches across traditional and innovative trials |
| Estimand Framework (ICH E9(R1)) | Structured definition of treatment effects addressing intercurrent events [4] | Aligning statistical estimation with clinical questions in both RCTs and RWE |
| PRISMA Guidelines | Systematic review and meta-analysis reporting standards [2] | Synthesizing evidence across efficacy and effectiveness studies |
| ROBINS-I Tool | Risk of bias assessment for non-randomized studies [2] | Critical appraisal of real-world effectiveness studies |
| Multi-Touch Attribution Models | Distributing conversion credit across customer journey touchpoints [7] | Analogous to understanding multiple contributors to treatment response |
| Real-World Data Quality Frameworks | Assessing fitness-for-use of EHR, claims, registry data | Ensuring reliability of data sources for effectiveness research |
| Pragmatic Trial Design Templates | Protocols balancing internal and external validity [6] | Generating evidence applicable to routine care settings |
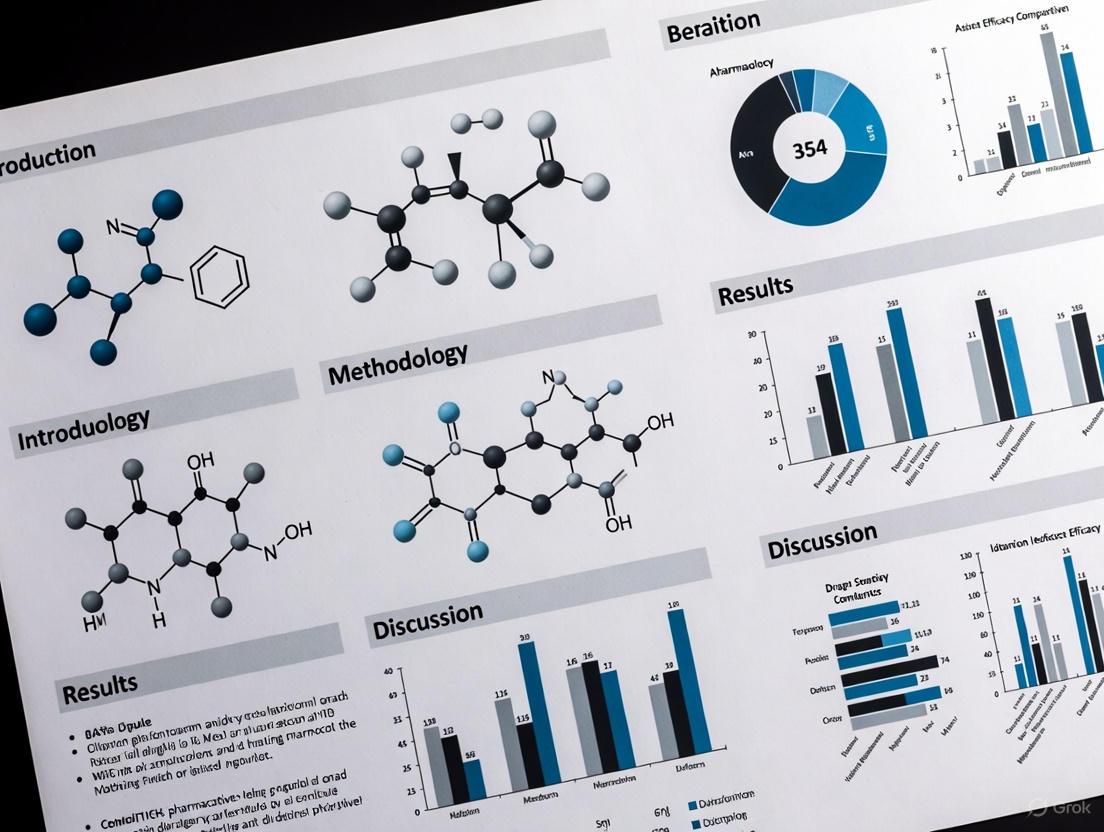
| Hydroprotopine | Hydroprotopine, MF:C20H20NO5+, MW:354.4 g/mol | Chemical Reagent |
| Spiraeoside | Spiraeoside, CAS:20229-56-5, MF:C21H20O12, MW:464.4 g/mol | Chemical Reagent |
The distinction between efficacy and effectiveness remains fundamental to evidence-based medicine and drug development. Efficacy establishes the foundational proof of concept under ideal conditions, while effectiveness demonstrates real-world value in routine practice. Rather than viewing these as competing paradigms, contemporary drug development should embrace integrated evidence generation that strategically combines both approaches.
The evolving regulatory landscape, exemplified by ICH E6(R3) and SPIRIT 2025, supports this integration through more flexible, pragmatic approaches to clinical research [6] [5]. For comparative drug efficacy research to meaningfully inform clinical practice and health policy, it must account for both the internal validity of efficacy studies and the external validity of effectiveness research. This requires methodological rigor in both randomized and observational settings, transparent reporting of study limitations, and appropriate interpretation of findings within each context's constraints.
Future advances in real-world data quality, causal inference methods, and pragmatic trial design will further enhance our ability to bridge the efficacy-effectiveness gap, ultimately accelerating the delivery of beneficial treatments to the diverse patient populations who need them.
The Critical Need for Comparative Data in Clinical and Health Policy Decision-Making
The landscape of clinical care is marked by wide variations in treatments, outcomes, and costs, resulting in significant disparities in both the quality and cost of healthcare [8]. Despite healthcare expenditures in the United States exceeding those of other countries, relatively unfavorable health outcomes persist [8]. This environment has fueled demands from healthcare decisionmakers for more evidence of the comparative effectiveness and cost effectiveness of medical interventions [8]. Comparative effectiveness research (CER) serves as a critical mechanism to fill current knowledge gaps in healthcare decisionmaking by generating and synthesizing evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor clinical conditions or to improve the delivery of care [8]. The fundamental purpose of CER is to assist consumers, clinicians, purchasers, and policy makers in making informed decisions that improve healthcare at both individual and population levels [8].
The Institute of Medicine (IOM) emphasizes that CER must directly compare alternative interventions, study patients in real-world clinical settings, and strive to tailor medical decisions to individual patient or subgroup values and preferences [8]. This approach represents a significant evolution beyond traditional efficacy studies conducted under ideal conditions, instead focusing on effectiveness in routine practice settings where patient populations are more diverse and comorbidities are common.
Methodological Frameworks for Comparative Research
Core Study Designs in Comparative Effectiveness Research
CER employs a range of methodological approaches, each with distinct advantages and limitations. The principal methods include observational studies (both prospective and retrospective), randomized trials, decision analysis, and systematic reviews [8]. Well-designed, methodologically rigorous observational studies and randomized trials conducted in real-world settings have the potential to improve the quality, generalizability, and transferability of study findings [8].
Table 1: Key Methodological Approaches in Comparative Effectiveness Research
| Study Design | Key Characteristics | Advantages | Limitations |
|---|---|---|---|
| Randomized Pragmatic Trials | Conducted in real-world settings; may have broader inclusion criteria | High internal validity; minimizes confounding | Can be costly and time-consuming; may have limited generalizability |
| Prospective Observational Studies | Participants identified before outcome occurrence; follows participants over time | Includes diverse patients from routine practice; strengthens external generalizability | Vulnerable to confounding and bias; requires careful statistical adjustment |
| Retrospective Observational Studies | Uses existing data collected for other purposes | Quickly provides low-cost, large study populations; efficient for long-term outcomes | Limited control over data quality; potential for unmeasured confounding |
| Network Meta-Analysis | Simultaneously compares multiple interventions using direct and indirect evidence | Facilitates comparison of interventions not directly studied in head-to-head trials | Requires careful assessment of transitivity and consistency assumptions |
The advantage of observational studies is their ability to quickly provide low-cost, large study populations drawn from diverse patients obtained during routine clinical practice, thereby strengthening the external generalizability of study findings [8]. However, these studies are limited by inherent bias and confounding that routinely occur in nonrandomized studies [8]. To minimize threats to internal validity, research guidelines recommend a priori specification of research questions, targeted patient populations, comparative interventions, and postulated confounders; selection of appropriate study designs; careful data source selection; and transparency in protocol development and prespecified analytic plans [8].
Methodological Standards and Analytical Considerations
To ensure the validity of CER findings, several methodological standards must be maintained. The International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Good Research Practices Task Force provides detailed recommendations on determining when to conduct prospective versus retrospective studies, the advantages and disadvantages of different study designs, and analytic approaches to consider in study execution [8]. Advanced statistical methods including regression analysis, propensity scores, sensitivity analysis, instrumental variables, and structural model equations are essential for addressing confounding in observational studies [8].
For retrospective observational studies leveraging existing data sources, applications are expected to compare existing interventions that represent a current decisional dilemma and have robust evidence of efficacy or are currently in widespread use [9]. These studies permit the observation of long-term impacts and unintended adverse events over periods longer than typically feasible in clinical trials [9]. Methods that represent state-of-the-art causal inference approaches for retrospective observational designs and utilize data from multiple health systems or multiple sites within large integrated health systems are strongly encouraged to facilitate generalizable CER results [9].
Data Presentation Standards for Comparative Research
Effective Tabulation of Quantitative Data
The presentation of quantitative data in comparative effectiveness research requires careful consideration to ensure clear communication of findings. Tabulation represents the first step before data is used for analysis or interpretation [10]. Effective tables should be numbered, contain a brief and self-explanatory title, and have clear and concise headings for columns and rows [10]. Data should be presented logically—by size, importance, chronological order, alphabetical order, or geographical distribution [10]. When percentages or averages are compared, they should be placed as close as possible, and tables should not be excessively large [10]. Vertical arrangements are generally preferable to horizontal layouts because scanning data from top to bottom is easier than from left to right [10].
For quantitative variables, data should be divided into class intervals with frequencies noted against each interval [10]. The class intervals should be equal in size throughout the distribution [10]. The number of groups or classes should be optimal—customarily between 6-16 classes—with headings that clearly mention units of data (e.g., percent, per thousand, mmHg) [10]. Groups should be presented in ascending or descending order, and the table should be numbered with a clear, concise, self-explanatory title [10].
Table 2: Data Presentation Formats for Different Variable Types
| Variable Type | Recommended Tables | Recommended Graphs/Charts | Key Considerations |
|---|---|---|---|
| Categorical Variables | Frequency distribution tables with absolute and relative frequencies | Bar charts, Pareto charts, pie charts | Include total number of observations; use appropriate legends for category identification |
| Numerical Variables | Frequency distribution with class intervals of equal size | Histograms, frequency polygons, frequency curves | Class intervals should be equal throughout; optimal number of intervals is 6-16 |
| Time-Based Data | Time series tables with consistent intervals | Line diagrams, frequency polygons | Time intervals should be consistent (month, year, decade) to depict trends accurately |
| Comparative Data | Contingency tables, multiple group comparisons | Comparative histograms, bar charts, frequency polygons | Place comparison groups adjacent to facilitate visual comparison |
Graphical Representation of Comparative Data
Graphical presentations provide striking visual impact and help convey the essence of statistical data, circumventing the need for extensive detail [10]. However, these visualizations must be produced correctly using appropriate scales to avoid distortion and misleading representations [10]. All graphs, charts, and diagrams should be self-explanatory, with informative titles and clearly labeled axes [10].
For quantitative data, histograms provide a pictorial diagram of frequency distribution, consisting of a series of rectangular and contiguous blocks where the area of each column depicts the frequency [10]. Frequency polygons are obtained by joining the mid-points of histogram blocks and are particularly useful when comparing distributions of different sets of quantitative data [10]. When numerous observations are available and histograms are constructed using reduced class intervals, the frequency polygon becomes less angular and more smooth, forming a frequency curve [10]. For comparing two groups, comparative histograms or bar charts with groups placed next to each other are effective, as are frequency polygons with multiple lines representing different groups [10].
Implementation Framework and Stakeholder Engagement
Patient and Stakeholder Engagement in CER
The Patient-Centered Outcomes Research Institute (PCORI) has formally incorporated the concept of "patient-centeredness" into CER, characterizing patient-centered outcomes research (PCOR) by: (1) comparing alternative approaches to clinical management; (2) actively engaging patients and key stakeholders throughout the research process; (3) assessing outcomes meaningful to patients; and (4) implementing research findings in clinical settings [8]. Engaging stakeholders in research improves the relevance of study questions, increases transparency, enhances study implementation, and accelerates the adoption of research findings into practice and health policy [8].
Stakeholders in CER are categorized into seven groups: patients and the public, providers (individuals or organizations), purchasers (responsible for underwriting costs of care), payers (responsible for reimbursement), policy makers, product makers (drug/device manufacturers), and principal investigators (researchers or their funders) [8]. Research indicates that patients are the most frequently engaged stakeholder group, with engagement most often occurring in the early stages of research (prioritization) [8]. Engagement strategies range from surveys, focus groups, and interviews to participation in study advisory boards or research teams [8].
PCORI's Patient and Family Engagement Rubric outlines stakeholder engagement throughout study planning, study implementation, and dissemination of results [8]. The rubric describes four key engagement principles: (1) reciprocal relationships with clearly outlined roles of all research partners; (2) colearning as a bidirectional process; (3) partnership with fair financial compensation and accommodation for cultural diversity; and (4) trust, transparency, and honesty through inclusive decisionmaking and shared information [8].
Infrastructure and Policy Support
Learning health systems and practice-based research networks provide the infrastructure for advancing CER methods, generating local solutions to high-quality cost-effective care, and transitioning research into implementation and dissemination science [8]. The passage of the Patient Protection and Affordable Care Act (PPACA) established the Patient-Centered Outcomes Research Institute (PCORI) as a government-sponsored nonprofit organization to advance the quality and relevance of clinical evidence that patients, clinicians, health insurers, and policy makers can use to make informed decisions [8]. PCORI's funding comes from the Patient-Centered Outcomes Research Trust Fund, which receives funding from the Federal Hospital Insurance Trust Fund, the Federal Supplementary Medical Insurance Trust Fund, the Treasury general fund, and fees on health plans to support CER [8].
The PPACA defines CER as "research evaluation and comparing health outcomes and clinical effectiveness, risks, and benefits of two or more medical treatments, services, and items" [8]. The law further specifies that PCORI must ensure that CER accounts for differences in key subpopulations (e.g., race/ethnicity, gender, age, and comorbidity) to increase the relevance of the research [8]. This legislative framework has moved the United States toward a national policy for CER to increase accountability for quality and cost of care [8].
Case Example: ADHD Medication Comparative Research
Experimental Protocol and Methodological Approach
A comprehensive network meta-analysis of medications for attention-deficit hyperactivity disorder (ADHD) demonstrates the application of CER methodologies to inform clinical decision-making [11]. The study aimed to estimate the comparative efficacy and tolerability of oral medications for ADHD across children, adolescents, and adults through a systematic review and network meta-analysis of double-blind randomized controlled trials [11].
Literature Search Strategy: Researchers searched multiple databases (PubMed, BIOSIS Previews, CINAHL, Cochrane Central Register of Controlled Trials, Embase, ERIC, MEDLINE, PsycINFO, OpenGrey, Web of Science Core Collection, ProQuest Dissertations and Theses, and WHO International Trials Registry Platform) from inception up to April 7, 2017, without language restrictions [11]. Search terms included "adhd" OR "hkd" OR "addh" OR "hyperkine" OR "attention deficit" combined with a list of ADHD medications [11].
Study Selection and Data Extraction: The analysis included 133 double-blind randomized controlled trials (81 in children and adolescents, 51 in adults, and one in both) [11]. Researchers systematically contacted study authors and drug manufacturers for additional information, including unpublished data [11]. This comprehensive approach minimized publication bias and enhanced the robustness of findings.
Outcome Measures and Analysis: Primary outcomes were efficacy (change in severity of ADHD core symptoms based on teachers' and clinicians' ratings) and tolerability (proportion of patients who dropped out of studies because of side-effects) at timepoints closest to 12 weeks, 26 weeks, and 52 weeks [11]. Researchers estimated summary odds ratios (ORs) and standardized mean differences (SMDs) using pairwise and network meta-analysis with random effects, assessing risk of bias with the Cochrane risk of bias tool and confidence of estimates with the Grading of Recommendations Assessment, Development, and Evaluation approach for network meta-analyses [11].
Key Findings and Clinical Implications
The analysis of efficacy closest to 12 weeks was based on 10,068 children and adolescents and 8,131 adults, while the analysis of tolerability was based on 11,018 children and adolescents and 5,362 adults [11]. For ADHD core symptoms rated by clinicians in children and adolescents closest to 12 weeks, all included drugs were superior to placebo [11]. In adults, amphetamines, methylphenidate, bupropion, and atomoxetine, but not modafinil, were better than placebo based on clinicians' ratings [11].
With respect to tolerability, amphetamines were inferior to placebo in both children and adolescents (OR 2.30) and adults (OR 3.26), while guanfacine was inferior to placebo in children and adolescents only (OR 2.64) [11]. In head-to-head comparisons, differences in efficacy were found favoring amphetamines over modafinil, atomoxetine, and methylphenidate in both children and adolescents (SMDs -0.46 to -0.24) and adults (SMDs -0.94 to -0.29) [11].
Table 3: Comparative Efficacy and Tolerability of ADHD Medications
| Medication | Efficacy in Children/Adolescents (SMD vs. placebo) | Efficacy in Adults (SMD vs. placebo) | Tolerability in Children/Adolescents (OR vs. placebo) | Tolerability in Adults (OR vs. placebo) |
|---|---|---|---|---|
| Amphetamines | -1.02 (-1.19 to -0.85) | -0.79 (-0.99 to -0.58) | 2.30 (1.36-3.89) | 3.26 (1.54-6.92) |
| Methylphenidate | -0.78 (-0.93 to -0.62) | -0.49 (-0.64 to -0.35) | Not significant | 2.39 (1.40-4.08) |
| Atomoxetine | -0.56 (-0.66 to -0.45) | -0.45 (-0.58 to -0.32) | Not significant | 2.33 (1.28-4.25) |
| Bupropion | Insufficient data | -0.46 (-0.85 to -0.07) | Insufficient data | Insufficient data |
| Modafinil | -0.76 (-1.15 to -0.37) | 0.16 (-0.28 to 0.59) | Not significant | 4.01 (1.42-11.33) |
| Guanfacine | -0.67 (-1.01 to -0.32) | Insufficient data | 2.64 (1.20-5.81) | Insufficient data |
The study concluded that, taking into account both efficacy and safety, evidence supports methylphenidate in children and adolescents and amphetamines in adults as preferred first-choice medications for the short-term treatment of ADHD [11]. This comprehensive network meta-analysis informs patients, families, clinicians, guideline developers, and policymakers on the choice of ADHD medications across age groups, demonstrating the critical role of comparative data in clinical decision-making [11].
Table 4: Key Research Reagent Solutions for Comparative Effectiveness Research
| Research Tool | Function/Application | Key Considerations |
|---|---|---|
| Existing Data Networks (e.g., PCORnet) | Provides infrastructure for large-scale observational studies using real-world data | Ensures representative populations; facilitates generalizable results; requires demonstrated data access at time of application [9] |
| Standardized Outcome Measures | Assesses clinically meaningful endpoints important to patients | Should include both clinical and patient-centered outcomes; must be validated and justified in study protocol [9] |
| Causal Inference Methodologies | Addresses confounding in observational studies through advanced statistical approaches | Includes propensity scores, instrumental variables, sensitivity analyses; represents state-of-the-art analytical techniques [8] [9] |
| Stakeholder Engagement Frameworks | Ensures research relevance and accelerates translation into practice | Incorporates patients, clinicians, payers, policymakers; follows established principles for reciprocal relationships and colearning [8] |
| Network Meta-Analysis Software | Simultaneously compares multiple interventions using direct and indirect evidence | Requires careful assessment of transitivity and consistency assumptions; uses random effects models for summary estimates [11] |
The critical need for comparative data in clinical and health policy decision-making continues to drive methodological innovations in comparative effectiveness research. Well-designed CER that incorporates rigorous methodologies, comprehensive data presentation, and meaningful stakeholder engagement provides an essential foundation for informed healthcare decisions. The ADHD medication network meta-analysis exemplifies how sophisticated comparative research methodologies can generate evidence that directly informs clinical practice across different patient populations [11].
Future directions for CER include addressing the paucity of long-term comparative outcomes beyond 12 weeks, incorporating individual patient data in network meta-analyses to better predict individual treatment response, and leveraging established data sources for efficient retrospective studies that complement randomized controlled trials [11] [9]. As CER methodologies continue to evolve, their integration into learning health systems will be essential for generating local solutions to high-quality cost-effective care and transitioning research into implementation and dissemination science [8]. This progressive approach to evidence generation will ultimately guide health policy on clinical care, payment for care, and population health, fulfilling the promise of comparative effectiveness research to improve healthcare decision-making at both individual and population levels.
In the rigorous field of comparative drug efficacy research, the hierarchy of evidence serves as a critical framework for evaluating the validity and reliability of clinical study findings. This structured approach systematically ranks research methodologies based on their ability to minimize bias, establish causal relationships, and generate clinically applicable results. At the foundation of evidence-based medicine (EBM), this hierarchy provides essential guidance for researchers, regulators, and clinicians navigating the complex landscape of therapeutic development [12]. The evidence pyramid graphically represents this ranking structure, with systematic reviews and meta-analyses at the apex, followed by randomized controlled trials (RCTs), observational studies (cohort and case-control designs), case series and reports, and finally expert opinions and anecdotal evidence at the base [12]. Understanding this hierarchy is fundamental for designing robust clinical development programs, interpreting research findings accurately, and making informed decisions about drug efficacy and safety.
The historical perspective of evidence hierarchy dates back to the mid-20th century, with British epidemiologist Archie Cochrane pioneering the emphasis on systematic reviews of RCTs. This foundational work paved the way for organizations such as the Cochrane Collaboration, which continues to advance EBM through rigorous methodology [12]. Seminal publications by Sackett et al. further popularized the evidence hierarchy, establishing it as an essential component of medical education and practice. These frameworks have continuously evolved to incorporate emerging evidence sources, including real-world data and novel analytical technologies, while maintaining core methodological principles that safeguard research integrity [12]. For drug development professionals, this hierarchical approach provides a systematic method for prioritizing high-quality evidence, critically evaluating research findings, and integrating scientific advances into therapeutic development and patient care, ultimately enhancing research quality and health outcomes.
The Evidence Pyramid: A Systematic Framework
Detailed Levels of Evidence
The evidence pyramid provides a structured representation of research methodologies, ranked according to their inherent ability to minimize bias and establish causal inference. Each level within this hierarchy offers distinct advantages and limitations that researchers must consider when designing studies or evaluating therapeutic efficacy [12].
Level I: Systematic Reviews and Meta-Analyses Occupying the highest position in the evidence hierarchy, systematic reviews and meta-analyses comprehensively synthesize data from multiple high-quality studies, typically RCTs. By systematically collecting and statistically analyzing results from numerous investigations, these studies provide the most definitive conclusions about therapeutic efficacy while minimizing bias through rigorous methodology. The quality of a systematic review is directly determined by the scientific rigor of the included studies, following the principle that "low-quality inputs produce subpar results" [12]. These comprehensive analyses form the foundation for clinical practice guidelines and healthcare policy decisions, offering the most reliable evidence for efficacy assessments.
Level II: Randomized Controlled Trials RCTs represent the gold standard for establishing causal relationships between interventions and outcomes in clinical research. Through random allocation of participants to intervention or control groups, this methodology effectively minimizes selection bias and controls for confounding variables. The rigorous design includes blinding techniques to reduce observer and participant bias, creating a controlled environment for precise efficacy assessment [12]. However, RCTs face significant challenges including ethical limitations, substantial resource requirements, inflexible protocols, and extended timelines. Furthermore, certain patient populations or interventions may be unsuitable for RCTs, creating evidence gaps that require alternative methodological approaches [12].
Level III: Cohort and Case-Control Studies As primary observational research designs, cohort and case-control studies provide valuable insights into treatment effects in real-world settings. Cohort studies track groups of participants over time to evaluate outcomes, while case-control studies compare individuals with and without a specific condition to identify potential causative factors [12]. Prospective cohort studies offer stronger causal inferences through continuous participant monitoring, ensuring reliable data collection while minimizing recall bias. Retrospective studies analyze historical data but are more susceptible to selection bias and information limitations. While these observational designs offer significant real-world applicability, they remain less reliable than RCTs due to potential confounding variables that cannot be fully controlled without randomization [12].
Level IV: Case Series and Case Reports These descriptive studies provide detailed information on individual patients or small groups, typically highlighting unusual disease presentations, innovative treatments, or rare adverse events. While valuable for hypothesis generation and identifying novel therapeutic avenues, these designs lack control groups and statistical power, severely limiting their generalizability [12]. Case series and reports primarily serve to guide future research directions rather than establish efficacy, providing preliminary observations that may inform more rigorous investigation through controlled studies.
Level V: Expert Opinion and Anecdotal Evidence Positioned at the base of the evidence hierarchy, expert opinions and anecdotal evidence rely on individual clinical experience and isolated observations rather than systematic investigation. While potentially insightful, particularly for rare conditions or novel interventions where robust evidence is lacking, these sources are inherently subjective and susceptible to significant bias [12]. Without standardization or controls, expert opinions represent the least reliable evidence for efficacy assessments, though they may provide valuable guidance when higher-level evidence is unavailable.
Table 1: Levels of Evidence in Medical Research
| Evidence Level | Study Design | Key Strengths | Major Limitations | Common Applications |
|---|---|---|---|---|
| Level I (Highest) | Systematic Reviews & Meta-Analyses | Comprehensive synthesis, minimal bias, definitive conclusions | Quality dependent on included studies, time-consuming | Clinical guidelines, policy decisions, efficacy confirmation |
| Level II | Randomized Controlled Trials (RCTs) | Gold standard for causality, minimizes selection bias, controls confounding | Resource-intensive, ethical constraints, limited generalizability | Pivotal efficacy trials, regulatory submissions |
| Level III | Cohort & Case-Control Studies | Real-world applicability, ethical feasibility, larger sample sizes | Potential confounding, selection bias, limited causal inference | Post-marketing surveillance, safety studies, comparative effectiveness |
| Level IV | Case Series & Reports | Hypothesis generation, identifies rare events, rapid dissemination | No control group, limited generalizability, susceptible to bias | Novel therapies, rare diseases, adverse event reporting |
| Level V (Lowest) | Expert Opinion & Anecdotal Evidence | Clinical insights, guides when evidence scarce | Subjective, no controls, significant bias potential | Preliminary guidance, rare conditions, methodological advice |
Visualizing the Evidence Hierarchy
Single-Arm Trials: Design, Applications, and Limitations
Methodological Framework and Characteristics
Single-arm trials (SATs) represent a specialized clinical design in which all enrolled participants receive the experimental intervention without concurrent control groups, with outcomes evaluated against historical benchmarks or predetermined efficacy thresholds [13]. This methodological approach eliminates randomization processes and control arms, instead utilizing comparable patient populations as reference standards through either pre-specified efficacy thresholds or external control comparisons [13]. The fundamental design characteristics of SATs include prospective follow-up of all participants receiving the identical investigational treatment, absence of randomization and control groups, and reliance on external historical data for outcome contextualization.
The operational advantages of SAT designs include simplified implementation, reduced resource requirements, shorter development timelines, and smaller sample sizes compared to randomized controlled trials. These practical benefits position SATs as an accelerated pathway for drug development and regulatory approval, particularly in specialized clinical contexts [13]. The ethical feasibility of SAT designs is especially relevant in serious or life-threatening conditions with no available therapeutic alternatives, where randomization to placebo or inferior standard care may be problematic. However, despite these operational advantages, the interpretation of SAT results presents significantly greater complexity than RCTs, requiring sophisticated analytical approaches and careful consideration of multiple assumptions that are inherently controlled for in randomized designs [13].
Challenges and Methodological Limitations
SATs face substantial methodological challenges that impact both the validity and reliability of their efficacy assessments. The fundamental absence of randomization creates intrinsic limitations in establishing definitive causal relationships between interventions and outcomes [13].
Compromised Internal Validity Without random allocation, SATs lack methodological safeguards against confounding from unmeasured prognostic determinants. This systematic inability to account for latent variables undermines the fundamental basis for ensuring internal validity in therapeutic effect estimation [13]. Unlike RCTs, where random allocation ensures approximate equipoise in both measured and latent prognostic factors across treatment arms, SATs cannot establish statistically robust frameworks for causal inference, leaving efficacy assessments vulnerable to multiple confounding influences.
Constrained External Validity The same methodological limitation (absence of concurrent controls) creates dual threats to external validity by precluding direct quantification of treatment effects [13]. Efficacy interpretation depends critically on two assumptions: (1) precise characterization of counterfactual outcomes (the hypothetical disease trajectory without the investigational treatment under identical temporal and diagnostic contexts), and (2) prognostic equipoise between study participants and external controls across both measured and latent biological determinants. Consequently, SAT-derived efficacy estimates exhibit inherent context-dependence, constrained to narrowly defined patient subgroups under protocol-specific conditions with limited generalizability beyond the trial's operational parameters [13].
Additional Methodological Concerns Statistical reliability represents another significant challenge for SATs. Efficacy estimates become particularly susceptible to sampling variability, especially in studies with limited sample sizes and/or high outcome variability [13]. The uncertainty inherent in estimating treatment efficacy from SATs warrants special consideration, as only variability within the experimental group is directly observable, while variability of hypothetical control groups remains unknown. Furthermore, when employing external controls—whether for threshold establishment or direct comparison—multiple bias sources can systematically impact validity estimates, including selection bias (differences in patient characteristics), temporal bias (changes in standard care over time), information bias (variations in outcome assessment), confounding bias (unmeasured prognostic factors), treatment-related bias (differences in concomitant therapies), and reporting bias (selective outcome reporting) [13].
Regulatory Context and Appropriate Applications
SATs find their primary application in specialized clinical contexts where randomized controlled trials may be impractical or unethical. These specific scenarios include orphan drug development for rare diseases with constrained patient recruitment pools, and oncology drugs targeting life-threatening conditions with no effective treatment alternatives [13]. In these situations, SATs may provide early efficacy evidence in urgent clinical contexts where conventional randomized designs are not feasible.
The regulatory landscape for SATs is evolving, with recent guidance reflecting increased methodological scrutiny. Historically, regulatory agencies including the U.S. Food and Drug Administration (FDA) have accepted SATs as support for accelerated approval, particularly in oncology [14]. However, recent draft guidance issued in March 2023 emphasizes a preference for randomized trials over single-arm designs, representing a significant policy shift [14]. This guidance explains that RCTs provide more accurate efficacy and safety profiles, enabling robust benefit-risk assessments and potentially supporting both accelerated and traditional approval through a "one trial" approach [14].
While acknowledging that RCTs may not be feasible in certain circumstances (e.g., very rare tumors), the FDA still considers SATs for accelerated approval if they demonstrate significant effects on surrogate endpoints reasonably likely to predict clinical benefit [14]. The guidance specifically notes limitations regarding certain endpoints in SATs, stating that "common time-to-event efficacy endpoints in oncology in single-arm trials are generally uninterpretable due to failure to account for known and unknown confounding factors when comparing the results to an external control" [14]. This regulatory evolution underscores the importance of early regulatory communication for sponsors considering SAT designs, with recommendation to seek FDA feedback on trial designs before initiating enrollment [14].
Table 2: Single-Arm Trials: Applications and Methodological Challenges
| Aspect | Details | Implications for Drug Development |
|---|---|---|
| Primary Applications | Rare diseases with limited patient populations, life-threatening conditions with no available therapies, initial efficacy evidence for accelerated pathways | Expedited development for urgent unmet medical needs, ethical feasibility when randomization problematic |
| Key Advantages | Faster implementation, reduced sample size, lower costs, ethical feasibility in serious conditions, accelerated regulatory pathways | Reduced development timelines and resources, particularly beneficial for small populations and serious conditions |
| Major Limitations | No concurrent controls, vulnerable to selection bias, temporal bias, confounding variables, limited causal inference | Efficacy estimates uncertain, regulatory scrutiny increasing, generalizability constrained |
| Recent Regulatory Trends | FDA preference for RCTs (March 2023 guidance), increased emphasis on randomized data, requirement for robust justification of SAT use | Shift toward randomized designs even in accelerated pathways, need for early regulatory consultation on trial design |
| Endpoint Considerations | Objective response rate (ORR) generally acceptable, time-to-event endpoints (PFS, OS) problematic in SATs | Endpoint selection critical for interpretability, avoidance of uninterpretable endpoints in single-arm context |
Randomized Controlled Trials: The Gold Standard
Methodological Rigor and Causal Inference
Randomized controlled trials represent the methodological cornerstone for establishing therapeutic efficacy, providing the most reliable evidence for causal relationships between interventions and clinical outcomes. The fundamental principle underlying RCTs—random allocation of participants to intervention groups—ensures that both known and unknown prognostic factors are distributed approximately equally across treatment arms, creating statistically comparable groups at baseline [12]. This methodological safeguard minimizes selection bias and controls for potential confounding variables, establishing a robust framework for attributing outcome differences to the investigational intervention rather than extraneous factors.
The RCT design incorporates additional methodological strengtheners including blinding procedures (masking of patients, investigators, and/or outcome assessors to treatment assignments), predefined statistical analysis plans, and prospective endpoint assessment [12]. These features collectively reduce multiple forms of bias that could otherwise compromise study validity. The controlled environment of RCTs enables precise specification of inclusion/exclusion criteria, treatment protocols, and monitoring procedures, ensuring standardized implementation across study sites and enhancing internal validity [12]. For regulatory decision-making and clinical guideline development, RCTs provide the definitive evidence foundation, particularly when well-designed, adequately powered, and properly executed.
Practical Challenges and Implementation Considerations
Despite their methodological advantages, RCTs face significant practical challenges that impact their implementation in drug development programs. These studies are typically resource-intensive, requiring substantial financial investment, lengthy timelines, and complex operational logistics [12]. The rigid protocol specifications necessary for maintaining internal validity may limit generalizability to broader patient populations and real-world clinical settings, creating an efficacy-effectiveness gap between trial results and clinical practice applications [12].
Ethical considerations present additional challenges, particularly when investigating interventions for serious conditions with established effective treatments, where randomization to placebo or inferior care may be problematic [12]. Furthermore, certain patient populations or clinical contexts may be unsuitable for RCTs due to practical or ethical constraints, creating evidence gaps that require alternative methodological approaches. Recent regulatory trends have emphasized the importance of adequate US representation in global clinical trials, with concerns raised about applicability of results from trials conducted primarily outside the US to American patient populations [15]. This consideration has become increasingly relevant in multinational drug development programs, where differential treatment effects across geographical regions may complicate efficacy interpretation and regulatory assessment [15].
Regulatory Evolution and Contemporary Design Innovations
The regulatory landscape for RCTs continues to evolve, with increasing emphasis on innovative trial designs that enhance efficiency while maintaining methodological rigor. Adaptive trial designs that allow for modification based on interim analyses, enrichment strategies targeting specific patient subpopulations, and pragmatic elements that enhance real-world applicability are being encouraged by regulatory agencies [14]. These innovative approaches can potentially accelerate drug development while generating robust evidence for regulatory decision-making.
Recent regulatory considerations have highlighted the impact of variable uptake of subsequent therapies across geographical regions in global trials, which can significantly affect the interpretability of overall survival endpoints [15]. This variability, along with analysis of other endpoints less susceptible to such confounding (e.g., progression-free survival), should be carefully considered when determining a treatment regimen's benefit-risk profile [15]. For confirmatory trials required for accelerated approval verification, the FDA now generally requires trials to be "underway" at the time of accelerated approval to minimize the "vulnerability period" during which patients may receive therapies that ultimately lack demonstrated clinical benefit [14]. This regulatory evolution underscores the importance of proactive confirmatory trial planning and execution throughout the drug development lifecycle.
Methodological Decision Framework: Selecting Appropriate Trial Designs
Strategic Considerations for Design Selection
The choice between single-arm and randomized controlled trial designs represents a critical strategic decision in drug development programs, with significant implications for development timelines, resource allocation, regulatory pathways, and ultimate evidence strength. This decision should be guided by multiple considerations including the clinical context, available therapeutic alternatives, patient population characteristics, endpoint selection, and regulatory requirements [13] [14].
SATs may be appropriate when specific conditions are met: (1) the investigational treatment is expected to produce effects substantially larger than existing therapies, making threshold exceedance a meaningful indicator of clinical benefit; (2) the natural history or existing treatments are expected to produce negligible effects on the endpoint of interest, providing a near-zero baseline against which treatment effects can be clearly distinguished [13]. The latter scenario explains the historical use of SATs in end-stage oncology indications where no approved therapies exist and tumor response rates from natural history approach zero. In such contexts, achieving a meaningful objective response rate may constitute valid evidence of efficacy given the extremely low background response rate [13].
In contrast, RCTs are typically required when: (1) anticipated treatment effects are modest or incremental compared to existing therapies; (2) substantial background effects or disease variability exists; (3) validated surrogate endpoints with established correlation to clinical outcomes are unavailable; (4) comprehensive safety assessment requires direct comparison to control groups [12] [14]. The FDA's increasing preference for randomized designs, even in accelerated approval contexts, reflects recognition that RCTs provide more accurate efficacy and safety profiles, enabling robust benefit-risk assessments [14].
Decision Pathway for Trial Design Selection
Emerging Methodological Approaches and Hybrid Designs
Contemporary drug development increasingly utilizes methodological innovations that incorporate elements from both traditional RCTs and real-world evidence approaches. These hybrid models aim to balance methodological rigor with practical efficiency, enhancing the drug development ecosystem while maintaining robust evidence standards [14] [16].
The "one trial" approach represents a significant innovation, where a single randomized controlled trial efficiently generates evidence for both accelerated approval (based on intermediate endpoints) and traditional approval (based on clinical endpoints) [14]. This strategy can potentially streamline development pathways while providing the methodological benefits of randomization throughout the regulatory process. Adaptive designs that allow modification based on interim analyses, enrichment strategies targeting specific patient subpopulations, and pragmatic elements that enhance real-world applicability are being increasingly encouraged by regulatory agencies [14].
External control arms derived from real-world data sources offer another innovative approach, potentially augmenting single-arm trials with historical comparators when randomized controls are not feasible [16]. However, these methodologies require careful implementation and validation to ensure comparability and minimize bias [13] [16]. Real-world evidence derived from healthcare databases, electronic health records, and registries is increasingly recognized as complementary to traditional clinical trials, particularly for safety assessment, effectiveness comparison, and contextualizing trial findings within routine clinical practice [16]. When utilized in a balanced manner, these approaches can offer time- and cost-saving solutions for researchers, the healthcare industry, regulatory agencies, and policymakers while benefiting patients through more efficient therapeutic development [16].
Research Reagents and Methodological Solutions
Table 3: Essential Resources for Clinical Trial Design and Evidence Synthesis
| Resource Category | Specific Tools/Platforms | Primary Function | Application Context |
|---|---|---|---|
| Trial Design Platforms | ClinicalTrials.gov, EU Clinical Trials Register | Protocol registration, results reporting, design transparency | Regulatory compliance, trial transparency, methodology documentation |
| Systematic Review Tools | Covidence, Rayyan, EndNote | Study screening, data extraction, reference management | Evidence synthesis, quality assessment, meta-analysis preparation |
| Statistical Analysis Software | R, Stata, RevMan | Meta-analysis, network meta-analysis, statistical modeling | Data synthesis, effect size calculation, heterogeneity assessment |
| Quality Assessment Instruments | Cochrane Risk of Bias Tool, Newcastle-Ottawa Scale | Methodological rigor evaluation, bias assessment | Critical appraisal, evidence grading, sensitivity analysis |
| Reporting Guidelines | PRISMA, CONSORT, STROBE | Transparent reporting, methodology documentation | Manuscript preparation, protocol development, research dissemination |
| Real-World Data Platforms | Electronic Health Records, Disease Registries, Claims Databases | Naturalistic evidence generation, post-marketing surveillance | Comparative effectiveness research, safety monitoring, external controls |
Methodological Standards and Implementation Frameworks
The conduct and reporting of clinical trials and evidence syntheses require adherence to established methodological standards to ensure validity, reliability, and reproducibility. Reporting guidelines such as PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) provide minimum recommended items to promote clear, transparent, and reproducible descriptions of research methodology and findings [17]. Lack of transparency in systematic reviews reduces their quality, validity, and applicability, potentially leading to erroneous health recommendations and negative impacts on patient care and policy [17].
The CONSORT (Consolidated Standards of Reporting Trials) guidelines similarly enhance transparency and reproducibility for randomized controlled trials, with recent updates reflecting methodological advances [18]. For network meta-analyses (NMAs), which enable comparative effectiveness assessment of multiple interventions, specific methodological guidance has rapidly evolved, with significant increases in published guidance since 2011, particularly regarding evidence certainty and NMA assumptions [19]. These methodological frameworks collectively enhance research quality, enabling critical appraisal and appropriate application of evidence to clinical and regulatory decision-making.
Recent advancements in evidence synthesis methods include the integration of artificial intelligence tools to improve efficiency and the development of specialized handbooks for diverse review types including qualitative evidence synthesis, prognosis studies, and rapid reviews [20]. Cochrane's methodological evolution reflects these developments, with new random-effects methods in RevMan, prediction intervals to aid interpretation, and updated Handbook chapters incorporating contemporary best practices [20]. These resources collectively support researchers in navigating the complexities of clinical evidence generation and synthesis, facilitating robust drug efficacy research aligned with current methodological standards.
The hierarchy of evidence provides an essential framework for navigating the complex landscape of comparative drug efficacy research, with single-arm trials and randomized controlled trials occupying distinct but complementary roles. SATs offer practical advantages in specialized contexts including rare diseases and serious conditions lacking therapeutic alternatives, but face significant methodological limitations in establishing causal inference and controlling bias [13]. In contrast, RCTs represent the gold standard for efficacy assessment through random allocation, blinding procedures, and controlled conditions that minimize bias and establish definitive causal relationships [12].
The evolving regulatory landscape reflects increasing preference for randomized designs even in accelerated approval pathways, emphasizing their value in providing comprehensive efficacy and safety profiles for robust benefit-risk assessment [14]. This evolution underscores the importance of strategic trial design selection aligned with clinical context, therapeutic alternatives, and regulatory requirements. Emerging methodological approaches including hybrid designs, adaptive trials, and real-world evidence integration offer promising avenues for enhancing drug development efficiency while maintaining methodological rigor [14] [16].
For drug development professionals, understanding this evidentiary hierarchy and its implications for research design is fundamental to generating compelling efficacy evidence, navigating regulatory pathways, and ultimately advancing therapeutic options for patients. By strategically applying appropriate methodological approaches throughout the drug development lifecycle, researchers can optimize evidence generation while maintaining scientific integrity and regulatory standards.
In the landscape of drug development, head-to-head clinical trials represent the gold standard for comparing the efficacy and safety of therapeutic interventions. These studies, where two or more active treatments are directly compared within the same trial, provide the most reliable evidence for clinical and health policy decision-making. Despite their scientific value, such trials remain notably absent for many drug classes and therapeutic areas.
This scarcity persists even as the number of treatment options expands across most therapeutic areas. The absence of direct comparative evidence creates significant challenges for clinicians, patients, and health policy makers who must navigate treatment choices without clear guidance on relative therapeutic merits [21]. This whitepaper examines the multidimensional barriers—financial, methodological, regulatory, and operational—that limit the conduct of head-to-head trials, and explores methodological alternatives that researchers employ when direct comparisons are not feasible.
Financial and Resource Constraints
Prohibitive Costs and Sample Size Requirements
Head-to-head trials designed to demonstrate non-inferiority or superiority between active treatments typically require substantially larger sample sizes and longer durations than placebo-controlled studies. This is particularly true when comparing drugs with similar mechanisms of action or when expecting modest between-group differences. The financial implications of these expanded trial requirements are substantial, creating significant disincentives for sponsors.
Table 1: Comparative Resource Requirements for Different Trial Designs
| Trial Design Aspect | Placebo-Controlled Trial | Head-to-Head Superiority Trial | Head-to-Head Non-Inferiority Trial |
|---|---|---|---|
| Typical Sample Size | Smaller | Larger (often substantially) | Largest |
| Trial Duration | Shorter | Longer | Longest |
| Operational Complexity | Moderate | High | Highest |
| Cost Implications | Lower | Higher | Highest |
Beyond basic sample size considerations, the current investment climate for clinical research presents additional headwinds. The pharmaceutical industry faces reduced investment in clinical trials, creating particular challenges for small and medium-sized biotechs with limited cash reserves [22]. This financial pressure makes resource-intensive head-to-head comparisons increasingly unattractive from a business perspective, especially when alternative pathways to regulatory approval exist.
Market and Reimbursement Pressures
Recent legislative changes have further complicated the business case for head-to-head trials. Industry experts note that regulations like the Inflation Reduction Act (IRA) in the United States are impacting trial initiation decisions, with companies shifting focus toward "fewer, high-value therapeutic areas" [22]. When profitability must be maximized across a more limited portfolio, sponsors may deprioritize expensive comparative studies that could potentially show their product is not superior to existing alternatives.
This economic reality creates a fundamental tension between commercial interests and scientific needs. As Ariel Katz, CEO of H1, explains: "As pharmaceutical companies shift their focus toward fewer, high-value therapeutic areas in light of the IRA's drug price negotiations, the overall number of clinical trials will go down" [22]. This trend may indirectly reduce the number of head-to-head comparisons conducted, as sponsors prioritize trials with higher likelihood of commercial success over those addressing comparative effectiveness questions.
Methodological and Statistical Complexities
Challenges in Trial Design and Interpretation
Designing a head-to-head trial requires careful consideration of multiple methodological factors, including choice of endpoints, non-inferiority margins, and statistical powering. These studies often face interpretation challenges, particularly when conducted in heterogeneous patient populations or when using surrogate endpoints that may not fully capture clinically important differences.
The growing complexity of modern trials exacerbates these challenges. As noted by industry experts, "Trials are getting more complex and expensive as they target smaller, more specific patient populations, rely on larger and more diverse datasets, and navigate stricter global regulations" [22]. This complexity is particularly pronounced for advanced therapies like cell and gene treatments, which may require adaptive trial designs that differ substantially from traditional randomized controlled trial models [22].
The Gold Standard Versus Practical Realities
The randomized controlled trial (RCT) model remains the methodological gold standard, but its application to head-to-head comparisons presents unique challenges. Maintaining blinding can be difficult when comparing interventions with different administration routes or distinctive side effect profiles. Additionally, selecting appropriate comparator doses requires careful justification to avoid allegations of "dosing games," where one drug might be administered at suboptimal levels to make the other appear more effective.
For rare diseases, these methodological challenges are magnified. Kevin Coker, former CEO of Proxima Clinical Research, notes that in rare diseases, "you have a very small number of target patients" [23]. This fundamental limitation of patient availability makes adequately powered head-to-head comparisons statistically and practically infeasible in many cases, forcing researchers to consider alternative methodological approaches.
Regulatory and Commercial Influences
Regulatory Pathways and Approval Requirements
Drug registration in many worldwide markets primarily requires demonstration of efficacy against placebo or standard of care, not superiority over all active alternatives [21]. This regulatory reality creates limited incentive for sponsors to invest in head-to-head comparisons when approval can be obtained through less costly and risky pathways.
The situation is well-described in the scientific literature: "Drug registration in many worldwide markets being only reliant on demonstrated efficacy from placebo-controlled trials" represents a fundamental structural barrier to conducting head-to-head studies [21]. This regulatory framework essentially makes head-to-head trials optional rather than mandatory for market entry.
Strategic Commercial Considerations
Beyond regulatory requirements, commercial considerations significantly influence trial design decisions. Pharmaceutical companies may be reluctant to conduct studies that could potentially show their product is inferior to a competitor's, particularly when the drug is already approved and generating revenue. This risk aversion is especially pronounced for blockbuster drugs with substantial market share.
Additionally, the timing of head-to-head comparisons in a product's lifecycle presents strategic challenges. Early in a drug's development, sponsors may lack confidence in its competitive advantages, making them hesitant to invest in direct comparisons. Later in the lifecycle, when market position is established, there may be limited commercial incentive to conduct studies that could undermine existing marketing claims or potentially narrow the drug's approved indications.
Practical Operational Hurdles
Patient Recruitment and Retention
Patient recruitment represents one of the most consistent challenges in clinical research, particularly for head-to-head trials that may require larger sample sizes. Industry reports indicate that patient recruitment and retention remain among the biggest roadblocks to trial success, with the average trial still failing to meet its recruitment goals [24].
The recruitment challenge is multifaceted. Patients today are "more informed, but also more selective" amid "a flood of similar-sounding studies," making it difficult for any single trial to stand out [24]. Additionally, despite years of advocacy, many trials "still fail to recruit diverse study populations," creating both scientific and regulatory challenges [24]. These recruitment difficulties are compounded in head-to-head trials that may have more stringent eligibility criteria than placebo-controlled studies.
Globalization and Regulatory Heterogeneity
The increasing globalization of clinical trials introduces additional complexity for head-to-head comparisons. Zee Zee Gueddar, senior director commercial at IQVIA, notes that "one of the most prominent challenges will be the growing complexity of global trials, with sponsors needing to navigate an increasingly intricate regulatory environment across diverse international markets" [22].
Table 2: Operational Challenges in Global Head-to-Head Trials
| Challenge Category | Specific Barriers | Potential Impacts |
|---|---|---|
| Regulatory Heterogeneity | Differing requirements across countries; inconsistent data requirements; varying ethical review processes | Protocol amendments; delayed initiations; increased costs |
| Operational Complexity | Multiple languages; different standards of care; varied healthcare infrastructures | Data heterogeneity; implementation challenges; site management difficulties |
| Patient Diversity | Cultural attitudes toward research; genetic variations; comorbidity differences | Generalizability questions; recruitment variability; retention differences |
As Kevin Coker summarizes: "Running trials across different countries sounds great but navigating different regulations, cultures, and standards is no small feat" [22]. This operational complexity adds another layer of challenge to already difficult head-to-head comparisons.
Alternative Methods for Comparing Drug Efficacy
Indirect Comparison Methodologies
When head-to-head trials are unavailable, researchers have developed statistical methods for indirect treatment comparisons. These approaches allow for the estimation of relative treatment effects through common comparators, but each carries important limitations and assumptions.
Naïve direct comparisons, which directly compare results from separate trials without statistical adjustment, are considered methodologically unsound as they "break the original randomization" and are "subject to significant confounding and bias because of systematic differences between or among the trials being compared" [21].
Adjusted indirect comparisons preserve the randomization of the original trials by comparing the magnitude of treatment effect between two treatments relative to a common comparator. This method, while more methodologically rigorous than naïve comparisons, increases statistical uncertainty as "the statistical uncertainties of the component comparison studies are summed" [21].
Mixed treatment comparisons (also called network meta-analysis) use Bayesian statistical models to incorporate all available data for a drug, including data not directly relevant to the comparator drug. These approaches can reduce uncertainty but "have not yet been widely accepted by researchers, nor drug regulatory and reimbursement authorities" [21].
Methodological Framework for Indirect Comparisons
The following diagram illustrates the conceptual relationship between different comparison methodologies available when head-to-head trial data is lacking:
All indirect comparison methods share a fundamental assumption: "that the study populations in the trials being compared are similar" [21]. When this assumption is violated, all indirect comparisons may produce biased estimates of relative treatment effects.
Case Study: Type 2 Diabetes Mellitus
The Proliferation of Treatment Options Without Direct Comparisons
The treatment of type 2 diabetes mellitus (T2DM) illustrates the challenges created by absent head-to-head evidence. As noted in the literature, "The introduction of several new drug classes (notably glucagon-like peptide-1 [GLP-1] analogues and dipeptidyl peptidase 4 [DPP4] inhibitors) over the past several years has resulted in added complexity to therapeutic choice" [21].
Despite multiple drugs being available within and across these classes, "very few GLP-1 analogues and DPP4 inhibitors have been compared in head-to-head studies" [21]. This evidence gap "poses a challenge for clinicians, patients and health policy makers" who must make treatment decisions without clear comparative effectiveness data [21].
Applied Indirect Comparison Methodology
In this clinical context, researchers have employed indirect comparison methods to address evidence gaps. Kim et al. performed a multiple adjusted indirect comparison to compare sitagliptin with insulin in T2DM with respect to change in HbA1c [21]. Since sitagliptin had only been compared with placebo and insulin had only been compared with exenatide, the researchers used a connecting trial comparing exenatide with placebo to establish the indirect comparison.
This approach demonstrates the practical application of indirect methods but also highlights their limitations. Each comparison in the chain introduces additional statistical uncertainty, and the validity of the final comparison depends on the similarity of patient populations across all three trials included in the analysis.
The Scientist's Toolkit: Essential Methodological Approaches
Table 3: Research Reagent Solutions for Comparative Effectiveness Research
| Methodological Approach | Primary Function | Key Applications | Important Limitations |
|---|---|---|---|
| Adjusted Indirect Comparison | Compares treatments via common comparator using Bucher method | Health technology assessment; clinical guideline development | Increased statistical uncertainty; requires common comparator |
| Mixed Treatment Comparisons | Bayesian network meta-analysis incorporating all available evidence | Comparative effectiveness research; drug class reviews | Complex implementation; requires statistical expertise |
| Single-Arm Studies with External Controls | Uses historical or real-world data as comparison group | Rare diseases; oncology accelerated approval | High susceptibility to bias; variable regulatory acceptance |
| Real-World Evidence Studies | Uses observational data from clinical practice to compare treatments | Post-market safety studies; effectiveness comparisons | Potential for confounding; requires sophisticated methods |
| Artemisic acid | Artemisinic Acid | Artemisinic acid, a key artemisinin precursor for antimalarial and therapeutic research. This product is For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
| Dieckol | Dieckol | Bench Chemicals |
Each methodological approach represents a "tool" with specific applications and limitations. While head-to-head trials remain the gold standard, these alternative methods provide valuable approaches for generating comparative evidence when randomized direct comparisons are not available or feasible.
The absence of head-to-head clinical trials represents a significant challenge in evidence-based medicine, affecting clinicians, patients, health technology assessment bodies, and payers. This gap stems from a complex interplay of financial, methodological, regulatory, and operational barriers that make direct comparisons challenging to execute.
While statistical methods for indirect comparison provide valuable alternatives, they cannot fully replace the evidence generated by well-designed head-to-head trials. As the development of new therapeutic options continues to accelerate across disease areas, addressing this comparative evidence gap will require innovative trial designs, greater regulatory harmonization, and potentially new funding mechanisms specifically dedicated to comparative effectiveness research.
For researchers navigating this landscape, understanding both the limitations of indirect methods and the barriers to conducting direct comparisons is essential for appropriately interpreting the available evidence and designing studies that maximize the generation of clinically meaningful comparative data.
In the field of comparative drug efficacy research, healthcare decision-makers often need to choose between multiple active interventions for the same clinical condition. Well-designed randomized controlled trials (RCTs) provide the most valid evidence of relative efficacy by minimizing selection bias through random assignment [25]. However, the rapid advancement of health technology has led to an increasing number of treatment options, many of which have never been compared directly in head-to-head clinical trials [25] [21]. This evidence gap arises partly because regulatory approval often requires only demonstration of efficacy versus placebo, and active comparator trials designed to show non-inferiority or equivalence typically require large sample sizes and are consequently expensive to conduct [21].
Indirect treatment comparisons (ITCs) have emerged as a crucial methodological approach to address this challenge. These techniques allow for the comparison of competing interventions through their relative effects versus a common comparator, thereby synthesizing a greater share of available evidence than traditional meta-analyses [26]. This technical guide examines the core principles governing the validity of these methods, with specific focus on the internal validity, external validity, and key assumptions that underpin reliable indirect comparisons in drug development research.
Fundamental Concepts and Definitions
Direct Comparisons
A direct comparison refers to the assessment of different interventions within the context of a single randomized controlled trial or a meta-analysis of trials that directly compare those same interventions [25]. This approach preserves the randomization process, which minimizes confounding and selection bias, providing the most valid evidence of relative efficacy [25] [21].
Indirect Comparisons
Indirect comparisons represent statistical techniques that estimate the relative efficacy of two interventions that have not been compared directly in RCTs, but have both been compared to a common comparator (such as placebo or another active treatment) [21]. The most basic form is the adjusted indirect comparison, which uses a common comparator as a link between two interventions [25] [21].
Naïve direct comparisons, which directly compare results from separate trials of different interventions without adjustment for differing trial characteristics, are generally inappropriate as they break the original randomization and are subject to significant confounding and bias [21].
Advanced Network Approaches
More complex methodologies include:
- Multiple adjusted indirect comparisons: Used when no single common comparator exists, constructing a chain of comparisons through multiple connecting interventions [21].
- Mixed treatment comparisons and network meta-analysis: Advanced statistical models that incorporate all available direct and indirect evidence simultaneously, often using Bayesian methods [21] [26].
Table 1: Types of Treatment Comparisons in Clinical Research
| Comparison Type | Methodology | Key Advantage | Key Limitation |
|---|---|---|---|
| Direct Comparison | Head-to-head assessment within randomized trials | Preserves randomization; minimizes bias | Often unavailable for all relevant interventions |
| Adjusted Indirect Comparison | Uses common comparator to link interventions | Provides evidence when direct comparisons are lacking | Increased statistical uncertainty |
| Naïve Direct Comparison | Directly compares results across different trials | Simple to perform | Subject to significant confounding; not recommended |
| Mixed Treatment Comparison | Incorporates all direct and indirect evidence simultaneously | Maximizes use of available evidence; reduces uncertainty | Complex methodology; requires specialized expertise |
Core Principles of Indirect Comparisons
Internal Validity
Internal validity in indirect comparisons refers to the extent to which the estimated relative treatment effect is unbiased and accurately represents the true relationship between the interventions being compared [25]. The internal validity of ITCs is fundamentally dependent on the internal validity of the individual trials included in the analysis [25]. Biases within the original trials will inevitably affect the validity of the indirect comparison.
A crucial threat to internal validity emerges when using naïve direct comparisons, which "break" the original randomization and provide no more robust evidence than naïve comparisons of observational studies [21]. The adjusted indirect comparison method proposed by Bucher et al. aims to preserve the randomization of the originally assigned patient groups by comparing the magnitude of treatment effect between two treatments relative to a common comparator [21].
Empirical evidence from a validation study comparing direct and adjusted indirect estimates in 44 published meta-analyses found significant discrepancy (P<0.05) in only three cases, suggesting that adjusted indirect comparisons usually agree with direct head-to-head randomized trials [25].
External Validity and Similarity Assumption
External validity, often referred to as generalizability, addresses whether the relative efficacy of interventions measured in the included trials is consistent across different patient populations, settings, and trial methodologies [25]. The key assumption for the validity of adjusted indirect comparisons is that the relative efficacy of an intervention is consistent in patients across different trials [25].
This similarity assumption encompasses several dimensions:
- Clinical similarity: Patients across trials should have comparable disease characteristics, prognostic factors, and concomitant treatments [25] [27].
- Methodological similarity: Trials should have similar design features (e.g., randomization methods, blinding, outcome definitions, and follow-up duration) [27].
- Statistical similarity: The treatment effects should be consistent across the network of evidence, without significant effect modification [26].
The importance of this similarity assumption was illustrated in a case comparing paracetamol plus codeine versus paracetamol alone for postsurgical pain, where significant discrepancy between direct and indirect estimates was explained by different doses of paracetamol and codeine used in the trials for indirect comparison [25].
Additional Key Assumptions
Beyond the fundamental similarity assumption, several other methodological assumptions underpin valid indirect comparisons:
- Homogeneity assumption: Within each direct comparison, treatment effects should be sufficiently similar across trials [26].
- Transitivity assumption: The interventions being compared indirectly should be similar enough that they could theoretically have been included in the same randomized trial [26] [27].
- Consistency assumption: Direct and indirect evidence should agree within a network of comparisons, which can be statistically evaluated [26].
Table 2: Core Assumptions for Valid Indirect Treatment Comparisons
| Assumption | Definition | Methodological Implication |
|---|---|---|
| Similarity | Trials across comparison groups are sufficiently similar in clinical and methodological characteristics | Ensures that differences in effects are attributable to treatments rather than trial differences |
| Homogeneity | Treatment effects are consistent between trials within the same direct comparison | Justifies pooling of results in meta-analysis |
| Transitivity | Interventions being compared indirectly are conceptually similar enough to be included in the same trial | Validates the conceptual basis for making indirect comparisons |
| Consistency | Direct and indirect evidence for a particular treatment comparison are in agreement | Allows for integration of different evidence sources in network meta-analysis |
Experimental Protocols and Methodological Framework
Protocol for Adjusted Indirect Comparison
The statistical method for adjusted indirect comparison, as initially proposed by Bucher et al., can be implemented through the following detailed protocol [21]:
Step 1: Identify the Network Structure
- Define the clinical question and competing interventions (B vs. C)
- Identify a common comparator (A) that has been compared with both B and C in separate randomized trials
- Ensure the similarity assumption is plausible by examining trial characteristics
Step 2: Extract or Calculate Effect Estimates
- For each trial, extract the relative effect of B vs. A and C vs. A
- Effects can be continuous (mean difference) or binary (log relative risk or log odds ratio)
- For binary outcomes, use the relative risk or odds ratio for each comparison
Step 3: Calculate the Indirect Estimate
- For continuous outcomes: EffectB vs. C = (EffectB vs. A) - (EffectC vs. A)
- For relative risks: RRB vs. C = RRB vs. A / RRC vs. A
- For example: If drug B reduces HbA1c by 0.5% vs. placebo and drug C reduces HbA1c by 0.3% vs. placebo, the indirect estimate of B vs. C is 0.5% - 0.3% = 0.2% greater reduction with B [21]
Step 4: Calculate Variance and Confidence Intervals
- Variance(EffectB vs. C) = Variance(EffectB vs. A) + Variance(EffectC vs. A)
- The 95% confidence interval is calculated as: EffectB vs. C ± 1.96 × √Variance(EffectB vs. C)
- This summation of variances results in greater uncertainty for indirect comparisons compared to direct evidence [21]
Step 5: Assess Discrepancy Between Direct and Indirect Evidence (if available)
- When both direct and indirect evidence exist, measure the difference (Δ) between the estimates: Δ = TBC - T'BC
- Calculate the standard error of the difference: SE(Δ) = √(SE(TBC)² + SE(T'BC)²)
- A significant difference (P<0.05) may indicate violation of the key assumptions [25]
Protocol for Multiple Adjusted Indirect Comparisons
When no single common comparator exists, a multiple adjusted indirect comparison can be conducted through a chain of comparators [21]:
Step 1: Establish the Connecting Path
- Identify a pathway connecting the interventions of interest through multiple comparators
- Example: To compare drug A with drug B, when A has been compared with C, and B with D, and C with D
Step 2: Calculate the Indirect Estimate Through the Chain
- EffectA vs. B = (EffectA vs. C) - (EffectB vs. D) + (EffectC vs. D)
- This effectively creates a connected pathway for comparison
Step 3: Calculate the Combined Variance
- Variance(EffectA vs. B) = Variance(EffectA vs. C) + Variance(EffectB vs. D) + Variance(EffectC vs. D)
- The multiple connections further increase statistical uncertainty
A real-world application of this method was demonstrated by Kim et al. in comparing sitagliptin with insulin for type 2 diabetes mellitus, using exenatide and placebo as connecting comparators [21].
Visualization of Methodological Relationships
Methodological Framework for Indirect Comparisons
Indirect Comparison Experimental Workflow
The Researcher's Toolkit: Essential Methodological Components
Table 3: Essential Components for Conducting Indirect Comparisons
| Component | Function | Application Notes |
|---|---|---|
| Common Comparator | Provides the statistical link between interventions | Typically placebo or standard care; must be consistent across comparisons |
| Effect Measure Calculator | Converts trial outcomes to comparable metrics | Handles both continuous (mean difference) and binary (relative risk, odds ratio) data |
| Variance Estimator | Quantifies statistical uncertainty | Accounts for additive uncertainty in indirect comparisons |
| Similarity Assessment Framework | Evaluates clinical/methodological comparability | Checks patient characteristics, trial design, outcome definitions |
| Consistency Model | Tests agreement between direct/indirect evidence | Identifies potential violations of key assumptions |
| Coenzyme Q0 | Coenzyme Q0, CAS:605-94-7, MF:C9H10O4, MW:182.17 g/mol | Chemical Reagent |
| Royal Jelly acid | Royal Jelly acid, CAS:765-01-5, MF:C10H18O3, MW:186.25 g/mol | Chemical Reagent |
Quantitative Validation and Empirical Evidence
Empirical studies have provided quantitative validation of the indirect comparison methodology. A comprehensive analysis of 44 published meta-analyses from 28 systematic reviews found that in most cases, results of adjusted indirect comparisons were not significantly different from those of direct comparisons [25].
The key quantitative findings include:
- Significant discrepancy (P<0.05) was observed in only 3 of the 44 comparisons (6.8%)
- Four additional meta-analyses showed borderline significance (P<0.1) in discrepancies
- Moderate agreement was found between statistical conclusions from direct and adjusted indirect comparisons (κ 0.51)
- The direction of discrepancy between the two estimates was inconsistent, with no systematic overestimation or underestimation [25]
In terms of statistical conclusions, 32 of the 44 indirect estimates (72.7%) fell within the same significance categories as the direct estimates. However, adjusted indirect estimates were less likely to be statistically significant: 10 of the 19 significant direct estimates became non-significant in the adjusted indirect comparison, while only 2 of the 25 non-significant direct estimates became significant in the adjusted indirect comparison [25]. This pattern highlights the increased statistical uncertainty inherent in indirect comparison methods due to the summation of variances from the component comparisons [21].
Indirect treatment comparisons represent a valuable methodological approach for informing healthcare decisions when direct evidence is absent or insufficient. The validity of these methods depends critically on three interconnected principles: the internal validity of the constituent trials, the similarity of trials included in the comparison, and the statistical assumptions of homogeneity, transitivity, and consistency. When properly applied with careful attention to these principles and assumptions, indirect comparisons provide useful supplementary information on the relative efficacy of competing interventions, though with greater statistical uncertainty than well-designed direct comparisons. As noted in recent guidelines, these methods have gained widespread acceptance among regulatory and health technology assessment authorities worldwide, provided they are conducted and reported with scientific rigor and transparency [27].
Methodologies for Comparison: From Indirect Techniques to Real-World Evidence
In the absence of head-to-head randomized controlled trials (RCTs), adjusted indirect comparisons provide a methodological framework for estimating relative treatment effects. These methods are paramount in comparative drug efficacy research, informing health technology assessment and reimbursement decisions. The validity of these comparisons hinges critically on the use of a common comparator, forming an "anchored" evidence structure that respects within-trial randomization and mitigates bias from cross-trial differences. This technical guide details the assumptions, methodologies, and analytical techniques for performing robust population-adjusted indirect comparisons, with a specific focus on Matching-Adjusted Indirect Comparisons (MAIC) and Simulated Treatment Comparisons (STC) within anchored settings.
Standard indirect comparisons and network meta-analysis (NMA) synthesize aggregate data from multiple trials under the key assumption of no cross-trial differences in the distribution of effect-modifying variables [28]. In practice, this assumption is frequently violated. When patient characteristics that influence treatment effect (effect modifiers) are imbalanced across trials, standard methods can yield biased estimates.
Population-adjusted indirect comparisons have been developed to relax this assumption. They use Individual Patient Data (IPD) from at least one trial to adjust for imbalances in the distribution of observed covariates between trial populations, provided these covariates are effect modifiers on the chosen scale [28]. This adjustment is essential for generating clinically meaningful and statistically valid estimates for a specific target population, such as the population in a competitor's trial or a real-world clinical population.
The cornerstone of a valid analysis is the anchored comparison, which utilizes a common comparator treatment (e.g., Treatment A) to connect the evidence. This approach preserves the randomization integrity of the original trials. In contrast, unanchored comparisons, which lack a common comparator, rely on much stronger and often infeasible assumptions, as they cannot adjust for unobserved confounding and are highly susceptible to bias [28].
Methodological Foundations and Key Assumptions
The Anchored Comparison Scenario
Consider a scenario where we wish to compare Treatments B and C. An AB trial (comparing A vs. B) provides IPD, while an AC trial (comparing A vs. C) provides only published aggregate data. The goal is to estimate the relative effect of B vs. C, denoted as ( d_{BC}(P) ), in a specific target population ( P ), which could be the population of the AC trial or another defined population [28].
A standard indirect comparison, assuming no effect modification, would simply compute: [ \hat{\Delta}{BC}^{(P)} = \hat{\Delta}{AC}^{(AC)} - \hat{\Delta}{AB}^{(AB)} ] where ( \hat{\Delta} ) represents the estimated relative effect on a suitable scale (e.g., log odds, mean difference). However, if effect modifiers are imbalanced, the estimates ( \hat{\Delta}{AB}^{(AB)} ) and ( \hat{\Delta}_{AB}^{(AC)} ) (the effect of B vs. A in the AC population) may differ.
Core Assumptions for Validity
For population-adjusted indirect comparisons to yield valid results, three core assumptions must be met:
- The Conditional Constancy of Relative Effects Assumption: This requires that, conditional on the effect modifiers included in the adjustment, the relative effect of B vs. A is the same in the AB trial population and the AC trial population. In other words, after adequate adjustment, any remaining effect modification is negligible [28].
- The Shared Effect Modifier Assumption: The variables included in the adjustment must be effect modifiers for the comparisons involving the common comparator (A). They must influence the relative treatment effect on the scale chosen for analysis [28].
- Internal Validity of Included Studies: The individual trials must provide unbiased estimates of treatment effects within their own participant populations.
Violations of these assumptions, particularly the first two, threaten the validity of the adjusted comparison. It is critical to distinguish between prognostic variables (which affect the outcome) and effect modifiers (which alter the treatment effect). While these can overlap, they are not identical.
Table 1: Key Terminology in Adjusted Indirect Comparisons
| Term | Definition | Role in Analysis |
|---|---|---|
| Common Comparator (Anchor) | A treatment arm (e.g., placebo, standard of care) common to all studies in the comparison [28]. | Connects the evidence network, allowing for anchored comparisons that respect randomization. |
| Effect Modifier | A patient characteristic that influences the relative effect of a treatment on a given scale [28]. | The primary target for adjustment; must be balanced across populations for valid inference. |
| Target Population | The population of interest for the final treatment effect estimate (e.g., the population of a competitor's trial) [28]. | The reference population to which the IPD is weighted or the outcomes are predicted. |
| Anchored Comparison | An indirect comparison made through a common comparator arm [28]. | The preferred method as it provides some protection against unobserved confounding. |
| Individual Patient Data (IPD) | Patient-level data from a clinical trial [28]. | Enables re-weighting or model-based adjustment to match aggregate data from another trial. |
The following diagram illustrates the logical structure and data flow for conducting a robust anchored indirect comparison, highlighting the critical steps and checks.
Detailed Experimental Protocols and Analytical Techniques
Protocol for Matching-Adjusted Indirect Comparison (MAIC)
MAIC is a propensity score-based method that re-weights the IPD from the AB trial to match the aggregate baseline characteristics of the AC trial population [28]. The goal is to create a "pseudo-population" from the AB trial that is comparable to the AC trial on the observed effect modifiers.
Step-by-Step Protocol:
- Variable Selection: Identify a set of candidate effect modifiers ( X ) based on clinical knowledge. These must be reported as summary statistics (e.g., means, proportions) in the AC trial publications.
- Estimate Propensity Scores: Within the IPD of the AB trial, fit a logistic regression model to estimate the odds of being in the AC trial versus the AB trial. The model includes only an intercept and the selected effect modifiers ( X ): [ \text{logit}(P( \text{Trial} = AC )) = \alpha0 + \alphaX X ] Since there are no individual-level data for the AC trial, the model is fitted to match the aggregate moments. The parameter ( \alpha0 ) is a fixed constant, and ( \alphaX ) is estimated.
- Calculate Weights: The weight for each patient ( i ) in the AB trial is calculated as: [ wi = \exp(\alphaX X_i) ] These weights are often stabilized to improve precision (e.g., by multiplying by a constant so the average weight is 1).
- Assess Balance and Fit: Compare the weighted means of the effect modifiers in the AB trial to the reported means in the AC trial. Effective balance indicates the weights have successfully created a comparable population. The effective sample size of the weighted population should be calculated to assess the precision cost of weighting.
- Estimate Adjusted Outcomes: Calculate the weighted average outcome for treatments A and B in the re-weighted AB trial population, denoted ( \hat{Y}A^{(AC)} ) and ( \hat{Y}B^{(AC)} ).
- Perform Anchored Comparison: The final adjusted indirect comparison is: [ \hat{\Delta}{BC}^{(AC)} = \left[ g(\bar{Y}C^{(AC)}) - g(\bar{Y}A^{(AC)}) \right] - \left[ g(\hat{Y}B^{(AC)}) - g(\hat{Y}_A^{(AC)}) \right] ] where ( g(\cdot) ) is the appropriate link function (e.g., logit, log).
Protocol for Simulated Treatment Comparison (STC)
STC is a model-based regression approach that uses the IPD from the AB trial to build a outcome model, which is then used to predict outcomes in the AC trial population [28].
Step-by-Step Protocol:
- Model Specification: Using the IPD from the AB trial, develop a regression model for the outcome. The model should include:
- The treatment indicator (( T ), 0 for A, 1 for B).
- The effect modifiers (( X )).
- Interaction terms between the treatment and the effect modifiers (( T \times X )). This is critical, as it allows the treatment effect to vary with patient characteristics. [ g(E(Y|T,X)) = \beta0 + \betaT T + \betaX X + \beta{TX} (T \times X) ]
- Model Validation: Assess the fit and predictive performance of the model. This may involve internal validation techniques.
- Predict Outcomes: The fitted model is used to predict the expected outcome for a patient in the AC trial. Since IPD for AC is unavailable, the prediction is performed for the average patient profile of the AC trial, using its published summary statistics for ( X ). This yields:
- ( \hat{Y}A^{(AC)} ): The predicted outcome if the AC trial population received treatment A.
- ( \hat{Y}B^{(AC)} ): The predicted outcome if the AC trial population received treatment B.
- Perform Anchored Comparison: The relative effect of B vs. A in the AC population is ( g(\hat{Y}B^{(AC)}) - g(\hat{Y}A^{(AC)}) ). The comparison of B vs. C is then: [ \hat{\Delta}{BC}^{(AC)} = \left[ g(\bar{Y}C^{(AC)}) - g(\bar{Y}A^{(AC)}) \right] - \left[ g(\hat{Y}B^{(AC)}) - g(\hat{Y}_A^{(AC)}) \right] ]
Table 2: Comparison of MAIC and STC Methodologies
| Feature | Matching-Adjusted Indirect Comparison (MAIC) | Simulated Treatment Comparison (STC) |
|---|---|---|
| Core Principle | Propensity score re-weighting [28]. | Regression model prediction [28]. |
| IPD Usage | Creates balanced pseudo-population via weights. | Estimates outcome model parameters. |
| Key Requirement | Aggregated means of EMs in AC trial. | Aggregated means of EMs; model specification. |
| Handling Effect Modification | Non-parametric; adjusts for imbalances in EMs. | Parametric; explicitly models interactions. |
| Primary Output | Re-weighted outcomes for A and B in AC population. | Predicted outcomes for A and B in AC population. |
| Major Challenge | Precision loss with extreme weights. | Risk of model misspecification and extrapolation. |
The Scientist's Toolkit: Essential Analytical Components
The successful implementation of MAIC or STC relies on a suite of methodological and statistical components. The following table details these "research reagents" and their functions in the analytical process.
Table 3: Essential Reagents for Population-Adjusted Indirect Comparisons
| Reagent / Tool | Function | Critical Considerations |
|---|---|---|
| Individual Patient Data (IPD) | The primary data source for one or more trials in the network. Allows for patient-level adjustment and modeling [28]. | Data quality and completeness are paramount. Must have sufficient detail on potential effect modifiers and outcomes. |
| Aggregate Data | Published summary statistics (e.g., means, proportions, counts) for the comparator trial(s). Serves as the target for adjustment [28]. | Limits the analysis to variables reported in publications. Incomplete reporting is a major limitation. |
| Effect Modifier List | A pre-specified set of patient characteristics believed to modify the treatment effect on the analysis scale [28]. | Selection should be guided by clinical expertise and prior evidence. Incorrect selection invalidates the adjustment. |
| Statistical Software (R, Python) | Platform for executing complex statistical analyses (weighting, regression, bootstrapping). | Requires specialized packages (e.g., stdma in R for MAIC) or custom programming. Expertise is necessary. |
| Link Function (( g(\cdot) )) | A transformation (e.g., logit, log, identity) applied to the outcome to ensure estimates are on an appropriate scale for linear combination [28]. | Choice depends on outcome type (binary, continuous, time-to-event). Consistency across studies is vital. |
| Bootstrapping Procedure | A resampling technique used to estimate the uncertainty (confidence intervals) for the adjusted treatment effect, accounting for the weighting or prediction process. | Essential for MAIC to correctly capture the variability introduced by the estimation of weights. |
| Dalbergin | Dalbergin, CAS:482-83-7, MF:C16H12O4, MW:268.26 g/mol | Chemical Reagent |
| Moslosooflavone | Moslosooflavone, CAS:3570-62-5, MF:C17H14O5, MW:298.29 g/mol | Chemical Reagent |
Visualization and Data Presentation in Complex Networks
As evidence networks grow in complexity, particularly with multicomponent interventions, standard network graphs can become difficult to interpret [29]. Novel visualization tools are being developed to better represent the data structure for analysis.
For component NMA (CNMA), which extends these concepts to complex interventions, visualizations like CNMA-UpSet plots and CNMA-circle plots can more effectively display which components are administered in which trial arms, aiding in the understanding of the evidence structure available for modeling component effects [29].
Regulatory and Practical Context in Drug Development
The principles of robust indirect comparison are directly relevant to the demonstration of biosimilarity. Regulatory guidance, such as that from the U.S. Food and Drug Administration (FDA), outlines the evidence requirements for biosimilar approval [30]. While the FDA's 2025 draft guidance acknowledges that comparative efficacy studies may not always be necessary due to advances in analytical characterization, well-executed indirect comparisons can play a crucial role in addressing residual uncertainty about clinical performance [31].
When presented to agencies like the FDA or to health technology assessment bodies such as the UK's National Institute for Health and Care Excellence (NICE), analyses must be transparent, reproducible, and statistically valid [28]. This includes clear pre-specification of the adjustment method, justification for the selection of effect modifiers, comprehensive assessment of assumptions, and appropriate quantification of uncertainty. The use of an anchored comparison is strongly recommended wherever possible to provide a more reliable foundation for inference.
Mixed Treatment Comparisons (MTC), also commonly referred to as Network Meta-Analysis (NMA), represents a significant methodological advancement in comparative effectiveness research. This approach enables the simultaneous comparison of multiple interventions through a unified statistical framework that synthesizes both direct and indirect evidence across a network of studies [32]. In the context of drug efficacy research, this methodology allows researchers and healthcare decision-makers to obtain a comprehensive assessment of all available therapeutic options, even when direct head-to-head trials are absent or limited. The Bayesian statistical paradigm provides a particularly powerful foundation for implementing MTC models due to its inherent flexibility in handling complex evidence structures and formally incorporating uncertainty at every stage of the analysis [33] [34].
The fundamental principle underlying MTC is the ability to leverage indirect evidence. When two treatments (B and C) have not been compared directly in randomized controlled trials but have both been compared to a common comparator treatment (A), their relative efficacy can be estimated indirectly through statistical combination of the A-B and A-C evidence [32]. This indirect comparison can be mathematically represented as the difference between their respective effects versus the common comparator: Effect~BC~ = Effect~AC~ - Effect~AB~ [32]. In complex treatment networks with multiple interventions, these connections form elaborate evidence structures that allow for both direct and indirect estimation of treatment effects, substantially strengthening inference beyond what would be possible from pairwise meta-analysis alone [32] [35].
The Bayesian approach to MTC offers several distinct advantages for drug efficacy research. Unlike traditional frequentist methods that rely solely on the data from completed trials, Bayesian models explicitly incorporate prior knowledge or beliefs through probability distributions, which are then updated with current trial data to form posterior distributions [36]. This framework naturally accommodates the hierarchical structure of meta-analytic data, properly accounts for uncertainty in parameter estimates, and provides intuitive probabilistic interpretations of results [37] [38]. Furthermore, Bayesian MTC models can handle sparse data scenarios more effectively than frequentist approaches, making them particularly valuable in situations where certain treatment comparisons have limited direct evidence [37] [33].
Core Methodological Principles
Fundamental Assumptions for Valid Inference
The validity of any MTC depends critically on satisfying three fundamental assumptions: transitivity, consistency, and homogeneity. Transitivity requires that the different sets of studies included in the analysis are similar, on average, in all important factors that may affect the relative effects [32]. In practical terms, this means that the available comparisons should be conceptually and methodologically compatible—for instance, involving similar patient populations, outcome definitions, and study methodologies. Violations of transitivity occur when study characteristics modify treatment effects and are distributed differently across the various direct comparisons in the network [32].
Consistency (sometimes called coherence) represents the statistical manifestation of transitivity and refers to the agreement between direct and indirect evidence for the same treatment comparison [32]. When both direct and indirect evidence exists for a particular comparison, the consistency assumption requires that these two sources of evidence provide statistically compatible estimates of the treatment effect. Methods for evaluating consistency range from simple statistical tests for specific comparisons to more comprehensive models that explicitly incorporate inconsistency parameters [35].
Homogeneity refers to the degree of variability in treatment effects within each direct comparison. Excessive statistical heterogeneity within pairwise comparisons can undermine the validity of both direct and indirect estimates and should be carefully assessed through standard meta-analytic measures such as I² statistics and between-study variance estimates [32]. Bayesian hierarchical models naturally account for this heterogeneity by treating study-specific effects as random draws from a common distribution, with the degree of borrowing across studies determined empirically by the heterogeneity of the available data [38] [34].
Bayesian Hierarchical Modeling Framework
Bayesian MTC models are typically implemented as hierarchical models that accommodate both within-study and between-study variability. For a binary outcome, the model can be specified as follows: Let y~ik~ represent the number of events out of n~ik~ participants for treatment k in study i. The number of events is assumed to follow a binomial distribution: y~ik~ ~ Bin(n~ik~, p~ik~), where p~ik~ represents the probability of an event [33]. The probabilities p~ik~ are then transformed to the linear predictor scale using an appropriate link function (e.g., logit or probit): g(p~ik~) = μ~i~ + δ~ik~ [33]. In this formulation, μ~i~ represents a study-specific baseline effect, and δ~ik~ represents the relative effect of treatment k compared to the baseline treatment in study i.
The random effects are typically assumed to follow a multivariate normal distribution: (δ~i2~, δ~i3~, ..., δ~iK~) ~ MVN(0, Σ), which accounts for the correlation between treatment effects in multi-arm trials [33]. The covariance matrix Σ captures the between-study heterogeneity in treatment effects. Prior distributions must be specified for all model parameters, including the μ~i~ parameters, the elements of Σ, and any other hyperparameters. The choice of prior distributions can range from non-informative or weakly informative priors when prior information is limited to highly informed priors derived from previous studies or meta-analyses [37].
Table 1: Key Components of Bayesian Hierarchical Models for MTC
| Model Component | Description | Implementation Considerations |
|---|---|---|
| Likelihood Structure | Defines the probability of observed data given parameters | Binomial for binary outcomes, Normal for continuous outcomes |
| Link Function | Transforms probability scale to linear predictor scale | Logit, probit, or complementary log-log for binary outcomes |
| Random Effects | Accounts for between-study heterogeneity | Typically multivariate normal to handle multi-arm trials |
| Prior Distributions | Encodes pre-existing knowledge about parameters | Non-informative, weakly informative, or informative based on available evidence |
| Consistency Assumption | Direct and indirect evidence are coherent | Can be assessed statistically using node-splitting or design-by-treatment models |
Practical Implementation and Workflow
Data Structure and Network Visualization
The first step in implementing a Bayesian MTC is to appropriately structure the data and visualize the evidence network. Data can be organized in either long format (where each row represents one treatment arm) or wide format (where each row represents all arms of a study) [39]. The essential elements include study identifiers, treatment codes, sample sizes, and outcome data (e.g., number of events for binary outcomes or means and standard deviations for continuous outcomes) [39]. Covariates for meta-regression or subgroup analysis can be incorporated as additional columns in the dataset.
Visualizing the evidence network is crucial for understanding the connectedness of treatments and identifying potential methodological challenges. Network diagrams typically represent treatments as nodes and direct comparisons as edges connecting these nodes [29] [32]. The size of nodes and thickness of edges can be proportional to the amount of available evidence. For complex networks with many treatments or component-based interventions, specialized visualization approaches such as CNMA-UpSet plots, CNMA heat maps, or CNMA-circle plots may be more informative than traditional network diagrams [29].
The following diagram illustrates a typical workflow for conducting a Bayesian MTC:
Prior Specification and Sensitivity Analysis
The specification of prior distributions represents a critical step in Bayesian MTC and should be guided by both statistical principles and clinical knowledge. For variance parameters in random-effects models, minimally informative priors such as half-normal, half-Cauchy, or uniform distributions are often recommended [37]. For basic parameters (typically defined as effects versus a reference treatment), priors can range from non-informative normal distributions with large variances to informed distributions based on previous meta-analyses or clinical expertise.
When prior information is available from previous studies, it can be formally incorporated through highly informed priors. For example, in an iterative research program, posterior distributions from a pilot study can serve as informed priors for a subsequent larger study [37]. This approach allows for cumulative learning across research stages and can improve estimation precision, particularly in small-sample settings [37]. However, the influence of prior choices should always be evaluated through comprehensive sensitivity analyses, where models are re-estimated using alternative prior distributions to assess the robustness of conclusions [33].
Sensitivity analysis is particularly important when considering potential non-ignorable missingness in the evidence base. For instance, if clinicians selectively choose treatments for trials based on perceived effectiveness, or if meta-analysts exclude certain treatment groups, the missing data mechanism may not be random [33]. Selection models can be employed to incorporate assumptions about missingness not at random, and sensitivity analyses can evaluate how conclusions might change under different missing data mechanisms [33].
Analytical Tools and Software Implementation
Software Options for Bayesian MTC
Several software platforms support the implementation of Bayesian MTC models, ranging from specialized graphical user interfaces to programming packages that offer greater flexibility. The following table summarizes key software options:
Table 2: Software Tools for Bayesian Network Meta-Analysis
| Software/Package | Platform | Key Features | Implementation Requirements |
|---|---|---|---|
| GeMTC [35] | GUI or R | Generates models for MCMC software; consistency and inconsistency models | Basic statistical knowledge; understanding of Bayesian concepts |
| BUGS/JAGS/Stan [35] | Standalone | Full flexibility in model specification; requires coding | Advanced Bayesian modeling skills; programming proficiency |
| MetaInsight [39] | Web-based | User-friendly interface; frequentist and Bayesian methods | Minimal statistical expertise; web access |
| baggr [38] | R package | Implements Bayesian aggregator models; works with published estimates | R programming knowledge; understanding of hierarchical models |
| bnma [39] | R package | Bayesian NMA using JAGS; various model types | R and JAGS installation; Bayesian methodology knowledge |
The choice of software depends on multiple factors including the analyst's technical expertise, the complexity of the evidence network, and the specific modeling requirements. For researchers new to Bayesian methods, MetaInsight provides an accessible entry point with its web-based interface and integration of both Bayesian and frequentist approaches [39]. For more advanced applications requiring custom model specifications, BUGS, JAGS, or Stan offer greater flexibility but require correspondingly greater statistical and programming expertise [35].
Model Diagnostics and Convergence Checking
After specifying and fitting Bayesian MTC models, thorough diagnostic checks are essential to ensure the validity of results. Convergence of Markov Chain Monte Carlo (MCMC) algorithms should be assessed using trace plots, autocorrelation plots, and statistical measures such as the Gelman-Rubin diagnostic [39]. Model fit can be evaluated using residual deviance, the Deviance Information Criterion (DIC), or other information criteria that balance model fit with complexity.
Consistency between direct and indirect evidence should be formally assessed using statistical methods. Local approaches such as node-splitting evaluate consistency for specific comparisons by comparing direct and indirect evidence [35]. Global approaches assess consistency across the entire network using design-by-treatment interaction models or other comprehensive assessments of inconsistency [35]. When important inconsistency is detected, investigators should explore potential sources through meta-regression or subgroup analysis, considering differences in study characteristics, patient populations, or outcome definitions across comparisons.
Advanced Applications and Interpretation
Component Network Meta-Analysis
For complex interventions consisting of multiple components, Component Network Meta-Analysis (CNMA) extends standard MTC methodology to estimate the contribution of individual intervention components [29]. In CNMA, the effect of a multicomponent intervention is modeled as a function of its constituent parts, typically assuming additive effects of components, though interaction terms can be incorporated to account for synergistic or antagonistic effects between components [29].
CNMA offers several advantages for comparative effectiveness research. It can identify which components are driving intervention effectiveness, predict the effects of untested component combinations, and inform the development of optimized interventions by determining whether certain components can be removed without compromising efficacy [29]. However, CNMA requires rich evidence structures with variation in component combinations across studies, and may not be able to uniquely estimate effects for components that always appear together in the same interventions [29].
Treatment Ranking and Decision-Making
A key output of Bayesian MTC is the ability to rank treatments according to their efficacy or safety profiles. Several metrics are available for treatment ranking, including the probability of each treatment being the best, the surface under the cumulative ranking curve (SUCRA), and P-scores [40]. These metrics summarize the uncertainty in treatment rankings across MCMC iterations and provide a quantitative basis for treatment selection.
Visualization of ranking results can be enhanced through specialized plots such as rankograms, which display the distribution of probabilities for each possible rank, or the recently developed beading plot, which presents global ranking metrics across multiple outcomes simultaneously [40]. The beading plot adapts the number line plot to display metrics such as SUCRA values or P-best probabilities for each treatment across various outcomes, with colored beads representing treatments and lines representing different outcomes [40].
The following diagram illustrates the conceptual relationship between different elements in a Bayesian MTC:
Reporting Guidelines and Quality Assessment
Transparent reporting of Bayesian MTC is essential for credibility and reproducibility. The Reporting of Bayes Used in Clinical Studies (ROBUST) scale provides a structured framework for assessing the quality of Bayesian analyses in clinical research [36]. This 7-item instrument evaluates key aspects including specification of priors, justification of prior choices, sensitivity analysis of priors, model specification, and presentation of central tendency and variance measures [36].
Recent assessments of Bayesian reporting quality in surgical research have revealed opportunities for improvement, with studies scoring an average of 4.1 out of 7 on the ROBUST scale, and only 29% of studies providing justification for their prior distributions [36]. Adherence to established reporting guidelines and thorough documentation of prior choices, model specifications, and sensitivity analyses will enhance the transparency and interpretability of Bayesian MTC in comparative drug efficacy research.
Bayesian Mixed Treatment Comparisons represent a powerful methodology for comparative effectiveness research, enabling coherent synthesis of all available evidence across networks of interventions. The Bayesian framework offers distinct advantages through its ability to formally incorporate prior evidence, explicitly model uncertainty, and provide intuitive probabilistic interpretations of results. As this methodology continues to evolve, ongoing challenges include improving the quality and standardization of Bayesian reporting, developing more sophisticated approaches for handling complex evidence structures, and enhancing the accessibility of these methods to the broader research community. When implemented with careful attention to underlying assumptions, model specification, and computational best practices, Bayesian MTC provides a rigorous quantitative foundation for evidence-based treatment decisions in drug development and clinical practice.
In the field of comparative drug efficacy research, the absence of head-to-head clinical trials often forces researchers to seek alternative methods for evaluating the relative performance of therapeutic interventions. Within this context, a frequently encountered but methodologically unsound practice is the naïve direct comparison—a approach that directly contrasts outcomes from two separate clinical trials without accounting for fundamental differences in trial design or population characteristics [21]. Such comparisons are particularly perilous because they break the original randomization that is the cornerstone of valid causal inference in clinical trials [21] [41]. When randomization is broken, systematic differences between trial populations can introduce profound confounding, effectively reducing the analysis to the reliability of an observational study despite its origin in randomized controlled trials [21]. This technical guide examines the methodological foundations of this problem, outlines its consequences, and presents robust alternative approaches aligned with emerging guidelines for comparative drug efficacy research.
Defining Naïve Direct Comparisons and Their Methodological Flaws
A naïve direct comparison refers to an assessment where clinical trial results for one drug are directly compared with clinical trial results for another drug without any attempt to adjust for differences in trial designs, populations, or comparator treatments [21]. This approach fundamentally violates the principle of randomization because, while each individual trial maintains internal validity through its randomization procedure, the comparison between trials abandons this protection [21].
The core methodological flaw lies in the inability to determine whether observed differences in efficacy measures genuinely result from the drugs themselves or instead reflect systematic differences in trial characteristics [21]. These may include variations in patient populations, baseline risk factors, concomitant treatments, outcome assessment methods, or comparator treatments [21]. Conversely, the failure to detect a true difference might also occur if trial variations inadvertently mask a genuine treatment effect [21]. As Bucher et al. established in their seminal work, such comparisons "break" the original randomization and become susceptible to the same confounding and biases that affect observational studies [42] [41].
Table 1: Hypothetical Example Illustrating Discrepancies Between Comparison Methods
| Metric | Clinical Trial 1 (Drug A vs. C) | Clinical Trial 2 (Drug B vs. C) | Naïve Direct Comparison (A vs. B) | Adjusted Indirect Comparison (A vs. B) |
|---|---|---|---|---|
| Change in Blood Glucose | -3.0 mmol/L vs. -2.0 mmol/L | -2.0 mmol/L vs. -1.0 mmol/L | -1.0 mmol/L | 0.0 mmol/L |
| Patients Reaching HbA1c < 7.0% | 30% vs. 15% | 20% vs. 10% | Relative Risk: 1.5 | Relative Risk: 1.0 |
Quantifying the Bias: Experimental Evidence and Case Studies
Empirical evidence demonstrates that naïve comparisons can produce substantially biased estimates of treatment effects. A foundational application by Bucher et al. compared prophylactic treatments for Pneumocystis carinii pneumonia in HIV-infected patients [41]. The analysis revealed strikingly different conclusions depending on the methodological approach:
- The indirect comparison using a common comparator showed a substantial increased benefit from sulphamethoxazole-trimethoprim over dapsone/pyrimethamine (odds ratio 0.37, 95% CI 0.21 to 0.65) [41].
- Direct comparisons from randomized trials suggested a much smaller difference (risk ratio 0.64, 95% CI 0.45 to 0.90) [41].
- The p-value for the difference between these effect estimates was 0.11, indicating that the naïve approach meaningfully overestimated the treatment effect [41].
This case exemplifies how naïve comparisons can lead to quantitatively different conclusions with significant implications for clinical decision-making and health policy. The fundamental problem is that any underlying differences in the patient populations or trial conditions between studies become confounded with the treatment effect estimate [21]. For instance, if Drug A was tested in a population with more severe disease than Drug B, any resulting difference in outcomes would reflect both this population difference and the actual drug effect, with no methodological means to disentangle the two.
Methodological Alternatives for Valid Comparative Effectiveness Research
Adjusted Indirect Comparisons
Adjusted indirect comparisons preserve randomization by comparing the magnitude of treatment effects of two interventions relative to a common comparator [21]. The method estimates the difference between Drug A and Drug B by comparing the difference between A and a common comparator C with the difference between B and C [21]. This approach maintains the randomization of the originally assigned patient groups within each trial [42] [41].
The statistical implementation involves calculating the relative treatment effect through the common comparator. For continuous outcomes, the formula is: [(A vs. C) - (B vs. C)]. For binary outcomes, the relative risk ratio is calculated as: (A/C) / (B/C) [21]. This method is currently the most commonly accepted approach for indirect comparisons and is recognized by drug reimbursement agencies including the Australian Pharmaceutical Benefits Advisory Committee, the UK National Institute for Health and Care Excellence (NICE), and the Canadian Agency for Drugs and Technologies in Health [21].
The primary limitation of adjusted indirect comparisons is increased statistical uncertainty, as the variances from the component comparisons are summed [21]. For example, if the variance for A vs. C is 1.0 and for B vs. C is 1.0, the variance for the indirect comparison A vs. B becomes 2.0, resulting in wider confidence intervals [21].
Mixed Treatment Comparisons and Network Meta-Analysis
Mixed treatment comparisons (MTCs), also known as network meta-analysis, use Bayesian statistical models to incorporate all available data for a drug, including data not directly relevant to the comparator drug [21]. This approach creates a connected network of treatment comparisons and allows for simultaneous comparison of multiple treatments while maintaining the internal randomization of each trial [21].
The Bayesian framework incorporates prior distributions and updates them with observed data to produce posterior distributions for treatment effects, which naturally handles uncertainty propagation throughout the network [21]. MTCs can reduce uncertainty compared to simple indirect comparisons by incorporating more data, though they have not yet been as widely accepted by researchers and regulatory authorities [21]. These methods rely on the consistency assumption—that direct and indirect evidence are in agreement—which should be carefully assessed in any application.
The Target Trial Framework for Real-World Evidence
When designing non-randomized studies using real-world data, NICE recommends emulating the randomized controlled trial that would ideally have been conducted—an approach known as the target trial framework [43]. This involves:
- Clearly articulating a protocol that specifies eligibility criteria, treatment strategies, assignment procedures, outcomes, follow-up, and causal contrasts of interest [43].
- Designing the observational study to mimic this protocol as closely as possible [43].
- Using appropriate statistical methods to address confounding and other biases [43].
This framework helps avoid selection bias due to poor design and provides a structured approach for designing valid comparative studies when randomized trials are not feasible [43].
Table 2: Advanced Methodologies for Comparative Effectiveness Research
| Methodology | Key Principle | Application Context | Regulatory Acceptance |
|---|---|---|---|
| Adjusted Indirect Comparison | Preserves randomization through common comparator | Two treatments with shared control | Widely accepted by HTA agencies |
| Mixed Treatment Comparisons | Bayesian models incorporating all available evidence | Network of multiple treatments | Growing acceptance |
| Target Trial Framework | Emulates RCT design using real-world data | When RCTs are not feasible | Recommended by NICE |
| Quantitative Bias Analysis | Quantifies impact of systematic error | Sensitivity analysis for observational studies | Emerging best practice |
The Scientist's Toolkit: Essential Methodological Approaches
Table 3: Key Methodological Approaches for Comparative Effectiveness Research
| Method | Function | Key Considerations |
|---|---|---|
| Adjusted Indirect Comparison | Compares treatments via common comparator | Requires similarity assumption between trials; sums variances |
| Network Meta-Analysis | Simultaneously compares multiple treatments | Assess consistency assumption; Bayesian methods preferred |
| Quantitative Bias Analysis | Quantifies impact of systematic errors | Uses bias parameters for confounding, selection, measurement |
| Self-Controlled Designs | Controls for time-invariant confounding | Suitable for transient exposures with acute outcomes |
| Instrumental Variable Analysis | Addresses unmeasured confounding | Requires valid instrument affecting outcome only via exposure |
| Hydroxyectoin | Hydroxyectoin, CAS:165542-15-4, MF:C6H10N2O3, MW:158.16 g/mol | Chemical Reagent |
| Momordin Ic | Momordin Ic, CAS:96990-18-0, MF:C41H64O13, MW:764.9 g/mol | Chemical Reagent |
Implementation Protocols for Valid Comparative Analyses
Protocol for Adjusted Indirect Comparison
- Identify common comparator: Establish that both Drug A and Drug B have been studied against a common control C (placebo or active control) [21].
- Assess trial similarity: Systematically evaluate whether the trials are sufficiently similar in terms of patient populations, outcome definitions, follow-up duration, and other methodological factors [21].
- Extract effect estimates: Obtain the effect estimates (e.g., mean differences, risk ratios) and their measures of variance (standard errors, confidence intervals) for A vs. C and B vs. C [21].
- Calculate indirect effect: Compute the indirect effect estimate for A vs. B as the difference between the A vs. C and B vs. C effects [21].
- Calculate variance: Sum the variances of the component comparisons to obtain the variance for the indirect comparison [21].
- Assess uncertainty: Report the point estimate with appropriate confidence intervals reflecting the combined uncertainty [21].
Protocol for Quantitative Bias Analysis
- Identify potential biases: Determine which systematic errors (confounding, selection bias, information bias) may affect the study [42].
- Specify bias parameters: Define quantitative parameters characterizing the bias (e.g., sensitivity/specificity of measurement, prevalence of unmeasured confounders) [42].
- Select analysis method: Choose appropriate level of analysis—simple (single parameter values), multidimensional (multiple parameter sets), or probabilistic (probability distributions for parameters) [42].
- Conduct bias adjustment: Apply bias models to the observed data to generate adjusted effect estimates [42].
- Interpret results: Evaluate whether conclusions change after accounting for potential biases and report the range of plausible effect estimates [42].
Visualizing Comparison Methodologies and Their Relationships
Comparison Methodology Decision Pathway
Leveraging Observational Studies and Real-World Data for Comparative Effectiveness
In the evolving landscape of healthcare research, observational studies using real-world data (RWD) have become indispensable for generating real-world evidence (RWE) about the comparative effectiveness of medical interventions. While randomized controlled trials (RCTs) remain the gold standard for establishing efficacy under controlled conditions, they have significant limitations including high costs, restrictive patient eligibility criteria, and relatively short duration that limits assessment of long-term outcomes [44]. Observational comparative effectiveness research (CER) addresses these gaps by providing evidence on how interventions perform in routine clinical practice across diverse patient populations.
The U.S. Food and Drug Administration (FDA) defines RWD as "data relating to patient health status and/or the delivery of health care routinely collected from a variety of sources," while RWE is "the clinical evidence about the usage and potential benefits or risks of a medical product derived from analysis of RWD" [45]. The 21st Century Cures Act, passed in 2016, specifically encouraged the FDA to develop frameworks for using RWE to support regulatory decisions, including drug approvals and post-market surveillance [45]. This regulatory evolution has accelerated the adoption of RWE across the drug development lifecycle.
Observational studies leveraging existing data sources can provide valuable data to address important questions for patients through timely evaluations of interventions in real-world settings [9]. These studies allow for the examination of large and representative populations and provide an important complement to RCTs, particularly when RCTs are not practical or ethically acceptable [9]. They also permit the study of clinical outcomes over a period longer than typically feasible in clinical trials, enabling observation of long-term impacts and unintended adverse events [9].
Foundational Concepts and Definitions
Key Terminology and Regulatory Framework
Comparative Effectiveness Research (CER) is defined as the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care [46]. The purpose of CER is to assist patients, clinicians, purchasers, and policy makers in making informed decisions that will improve health care at both the individual and population levels.
Real-world Data (RWD) encompasses data relating to patient health status and/or the delivery of health care routinely collected from various sources. These include electronic health records (EHRs), medical claims data, product and disease registries, and data gathered from digital health technologies [45]. RWD is characterized by its collection in routine clinical practice settings rather than controlled research environments.
Real-world Evidence (RWE) is the clinical evidence regarding the usage and potential benefits or risks of a medical product derived from the analysis of RWD [45]. RWE provides insights into how treatments perform in routine clinical practice, capturing a wider range of patient experiences and outcomes than typically seen in RCTs [47].
The fundamental distinction between traditional clinical trials and RWE studies lies in their approach to validity. RCTs excel at internal validity – proving causation through controlled settings and randomization – while RWE studies excel at external validity, showing how treatments actually perform once they reach diverse patient populations in routine clinical practice [44].
Advantages and Limitations of Observational RWE Studies
Table 1: Comparative Analysis of Randomized Trials and Observational RWE Studies
| Aspect | Randomized Clinical Trials | Observational RWE Studies |
|---|---|---|
| Setting | Controlled research environment | Routine healthcare practice |
| Population | Selected patients meeting strict criteria | Diverse, representative patients |
| Treatment | Standardized protocol | Variable, physician-directed |
| Randomization | Random assignment to treatment groups | None – observational |
| Primary Focus | Internal validity, causal proof | External validity, generalizability |
| Timeline | Fixed study duration | Months to years of follow-up |
| Cost | Higher | Lower |
| Data Collection | Purpose-driven for research | Collected during routine care |
Observational RWE studies offer several distinct advantages. They provide access to more representative patient populations, including elderly patients, those with comorbidities, and rare disease patients who are often excluded from traditional trials [44]. The lower cost and faster execution timeline of RWE studies enables more rapid insights, with some analyses completed in months rather than years [44]. These studies also facilitate long-term follow-up that can detect delayed benefits or adverse events that might not emerge during typical trial durations [9].
However, observational studies face significant methodological challenges. The absence of randomization introduces potential for confounding by indication, where treatment choices reflect underlying patient characteristics that also affect outcomes [48]. Data quality issues are prevalent, as RWD comes from busy healthcare settings where the primary focus is patient care rather than research documentation [44]. Additional challenges include missing data, measurement error, and potential for selection bias in how patients enter databases or receive specific treatments [48].
Observational Study Designs for Comparative Effectiveness
Core Study Design Architectures
Cross-sectional studies involve the simultaneous assessment of exposure and outcome in a single group of patients at a specific point in time [48]. These studies are typically used to assess prevalence and infer causes of conditions or outcomes. The general design involves defining the target population, deriving a sample, and defining the characteristics being studied. The definition of the condition and health characteristics should be standardized, reproducible, and feasible to apply on a large scale [48]. A key limitation is that the temporal relationship between exposure and outcome cannot be ascertained since data are collected at a single time point.
Case-control studies are retrospective studies that identify persons with the disease of interest (cases) and then look backward in time to identify factors that may have caused it [48]. Controls are matched groups of patients without the outcome derived from the same population. The exposure to potential causal variables is evaluated based on medical history to determine causality. These studies are particularly suitable for rare outcomes or those with a long latency between exposure and disease, and they allow simultaneous assessment of multiple etiologic factors [48]. However, they are susceptible to various biases, including recall bias and selection bias.
Cohort studies evaluate the association between a particular exposure or risk factor and subsequent development of disease [48]. These can be conducted concurrently (identifying exposed and unexposed populations at study initiation and following them forward) or retrospectively (using previously collected exposure information and surveying participants in the present to determine disease status). Cohort studies are advantageous because they establish temporal relationships between exposure and disease, provide direct estimates of incidence and relative risk, and are suitable for studying rare exposures [48].
Table 2: Comparison of Observational Study Designs for CER
| Design Feature | Cross-Sectional | Case-Control | Cohort |
|---|---|---|---|
| Temporal Direction | One time point | Retrospective | Prospective or Retrospective |
| Data Collection | Single assessment | Backward-looking | Forward-looking or historical |
| Outcome Frequency | Prevalence | Rare outcomes | Common outcomes |
| Exposure Frequency | Common exposures | Multiple exposures | Rare exposures |
| Time Required | Short | Moderate | Long (concurrent) |
| Cost | Low | Moderate | High (concurrent) |
| Key Advantages | Quick, inexpensive, multiple exposures/outcomes | Efficient for rare diseases, multiple exposures | Clear temporal sequence, incidence data |
| Key Limitations | No causality assessment, susceptible to bias | Susceptible to recall bias, single outcome | Time-consuming, expensive, loss to follow-up |
Specialized Design Variations
Nested case-control studies represent a hybrid design that reduces most biases related to selection and data collection seen in classic case-control studies [48]. In this approach, cases and controls are selected from within a large-scale prospective cohort study. Biological samples in the ongoing cohort study can be collected and stored until enough cases have accumulated to provide adequate study power. This design offers a more efficient approach to examining expensive or difficult-to-measure risk factors.
Target trial emulation has emerged as a gold standard for addressing fundamental methodological challenges in observational studies [44]. This approach involves designing observational studies to mimic randomized trials that could have been conducted but weren't. The process begins by specifying the protocol for a hypothetical randomized trial, then designing an observational study that emulates each component of this protocol as closely as possible, acknowledging where the emulation might fall short of the ideal randomized trial.
Electronic Health Records (EHRs) have become the digital backbone of healthcare, with 99% of hospitals now using EHR systems [44]. These systems capture comprehensive patient information including demographics, progress reports, problems, medications, vital signs, medical history, immunizations, lab results, and radiology reports [47]. EHR data includes both structured information (coded data) and unstructured data (clinical notes), with the latter requiring natural language processing techniques for analysis. A key advantage of EHR data is clinical richness, though data quality and completeness can vary significantly across institutions.
Claims and billing data provide valuable insights into healthcare utilization, costs, and economic outcomes, making them essential for health economics and outcomes research [47]. Insurance claims capture detailed information about treatments received, costs, and effectiveness over time. This data excels at tracking long-term outcomes across entire populations and provides comprehensive capture of healthcare utilization within specific insurance systems. Limitations include potential coding inaccuracies and lack of clinical granularity.
Disease registries serve as specialized repositories focusing on specific conditions or treatments [44]. These carefully curated databases often provide the most complete picture of how diseases progress and how treatments perform in their target populations. Registries typically include detailed clinical information specific to the condition of interest and may support long-term follow-up studies and comparative effectiveness research.
Digital health technologies (DHTs) have opened entirely new data streams, including wearable devices that continuously monitor heart rate, activity levels, and sleep patterns, and mobile applications that track medication adherence and patient-reported outcomes [47]. These technologies enable continuous, real-time health data collection in patients' natural environments, capturing data that would be unavailable in traditional clinical settings. However, validation against clinical standards and management of high-volume, high-frequency data present significant challenges.
Patient-reported outcomes (PROs) capture the patient's own perspective on their health and quality of life [44]. Digital platforms and mobile apps now facilitate collection of this valuable patient voice data. PROs provide direct insight into patient experiences and outcomes that matter to patients, though they may be subject to various reporting biases.
Methodological Approaches for Causal Inference
Propensity score methods help create fair comparisons between treatment groups in observational studies where randomization is absent [44]. These approaches involve calculating the probability that each patient would receive a particular treatment based on their observed characteristics, then using matching, weighting, or stratification to balance the groups on these propensity scores. This method effectively reduces selection bias when all important confounders are measured, though it cannot address unmeasured confounding.
Synthetic control arms offer a solution when comparison groups are needed but not available in the data [44]. This approach uses historical data or data from external sources to create virtual control groups, which has proven especially valuable in oncology studies where randomizing patients to control conditions may be unethical. These designs require careful consideration of eligibility criteria and endpoint definitions to ensure comparability between the experimental and synthetic control groups.
Bayesian methods incorporate existing knowledge or beliefs into analyses through prior distributions [44]. These approaches are particularly valuable when dealing with rare diseases or events where traditional statistics might not have sufficient power. Bayesian approaches can also facilitate borrowing information from related populations or historical data, though they require careful specification of priors and sensitivity analyses.
Implementation Framework and Research Reagents
Essential Research Reagents and Methodological Tools
Table 3: Research Reagent Solutions for Observational CER
| Reagent Category | Specific Tools/Solutions | Primary Function | Application Context |
|---|---|---|---|
| Data Quality Assessment | Data completeness profiles, Validity crosswalks, Terminology mappings | Evaluate fitness-for-purpose of RWD sources | Pre-study feasibility assessment |
| Terminology Standards | OMOP CDM, FHIR, CDISC, ICD/CPT codes | Standardize data structure and content across sources | Data harmonization and network studies |
| Causal Inference Methods | Propensity score algorithms, Inverse probability weighting, G-computation | Address confounding in treatment effect estimation | Comparative effectiveness analysis |
| Bias Assessment Tools | Quantitative bias analysis, E-value calculators, Sensitivity analyses | Quantify potential impact of unmeasured confounding | Study interpretation and validation |
| AI/ML Platforms | Natural language processing, Federated learning systems, Predictive models | Extract information from unstructured data, enable multi-site analyses | Large-scale RWD analysis across networks |
| Privacy Preservation Technologies | Safe Harbor de-identification, Expert determination, Federated analytics | Protect patient privacy while enabling research | Multi-institutional studies compliant with HIPAA/GDPR |
Practical Implementation Considerations
Successful implementation of observational CER requires careful attention to several practical considerations. Data quality validation should include systematic approaches to data cleaning and identification of coding errors, standardization of formats across different sources, and implementation of logical consistency checks [44]. The interoperability challenge requires attention to standards like FHIR and CDISC mapping to bridge gaps between different healthcare systems that often use different data languages [44].
Patient privacy protection necessitates implementation of appropriate de-identification methods under HIPAA, either through the Safe Harbor method (removing 18 specific identifiers) or the Expert Determination method (qualified statisticians assessing re-identification risk) [44]. Federated approaches represent the future of privacy-preserving research, where instead of moving sensitive patient data to central locations, the analysis is brought to where the data lives [44].
Regulatory acceptance of RWE continues to evolve, with the FDA's 2018 Real-World Evidence Framework emphasizing that RWE must be "fit for purpose" – meaning the data quality, study design, and analytical methods must match the specific regulatory question being asked [44]. Similar frameworks have been developed by the European Medicines Agency and the UK's National Institute for Health and Care Excellence [44].
Observational studies leveraging real-world data represent a powerful approach for generating evidence on comparative effectiveness in real-world clinical settings. When designed and analyzed using rigorous methodologies, these studies provide essential complementary evidence to traditional randomized trials, particularly for understanding how interventions perform in diverse patient populations over extended timeframes.
The successful implementation of observational CER requires careful selection of appropriate study designs, thoughtful consideration of data sources and their limitations, application of robust causal inference methods to address confounding, and adherence to evolving regulatory standards. As digital health technologies continue to expand the universe of available real-world data and analytical methods become increasingly sophisticated, the role of observational research in informing healthcare decisions will continue to grow.
Researchers conducting observational CER should prioritize transparency in their designs and analyses, engage appropriate methodological expertise throughout the research process, and maintain focus on answering clinically relevant questions that address genuine decisional dilemmas faced by patients, clinicians, and healthcare systems.
Systematic Reviews and Meta-Analyses as Tools for Evidence Synthesis
Systematic reviews and meta-analyses represent the pinnacle of the evidence hierarchy in medical research, driving advancements in research and practice [49]. These methodologies provide empirically supported responses to specific research questions, offering crucial information to guide clinical research and patient care [49]. A systematic review is a type of literature review that uses explicit, systematic methods to collate and synthesize findings of studies that address a clearly formulated question [50]. This scientific approach reduces the bias present in individual studies, making systematic reviews a more reliable source of information [49]. The primary goal is to support transparent, objective, and repeatable healthcare decision-making while guaranteeing the validity and reliability of the results [49].
A meta-analysis serves as a statistical extension of a systematic review. It is a statistical technique used to synthesize results when study effect estimates and their variances are available, yielding a quantitative summary of results [50]. When a meta-analysis is not possible or appropriate, researchers can use other synthesis methods, such as qualitative synthesis or synthesis without meta-analysis (SWiM) [49]. Meta-analysis enhances the accuracy of estimates and offers an overall view of the impacts of interventions, thereby increasing the study's power and the viability of the results [49]. The network meta-analysis (NMA) extends this approach to provide indirect comparisons of efficacy and safety between multiple interventions, which is particularly valuable when head-to-head randomized controlled trials are limited [51] [52].
Fundamental Principles and Protocols
Formulating the Research Question
Every systematic review or meta-analysis begins with establishing a well-defined research question to ensure a structured approach and analysis [49]. Frameworks are designed to formulate an organized research question, with the most frequently used being PICO (Population, Intervention, Comparator, Outcome) or its extension, PICOTTS (Population, Intervention, Comparator, Outcome, Time, Type of Study, and Setting) [49]. The PICO framework is mainly focused on therapy questions but due to its adaptability can also be used for questions of diagnosis and prognosis [49]. A well-defined research question provides clear guidance for each stage of the review process by helping identify relevant studies, establishing inclusion and exclusion criteria, determining relevant data for extraction, and guiding data synthesis [49].
Table 1: PICO Framework for Research Questions
| Structure | Meaning | Example 1: Crohn's Disease | Example 2: Obesity |
|---|---|---|---|
| P (Population/Patient/Problem) | People that is planned to be affected (age group, socio-demographic characteristics, duration of disease, and severity) | Adults with moderate-to-severe Crohn's disease [51] | Adults with obesity [52] |
| I (Intervention) | Medicines, procedures, health education, preventive measures | Pharmaceutical therapies for Crohn's disease [51] | Obesity management medications [52] |
| C (Comparison) | Gold standard treatment, placebo or alternative intervention | Placebo or active comparators [51] | Placebo or active comparators [52] |
| O (Outcome) | The result that intervention has on the population compared to comparison | Clinical remission, drug discontinuation rates [51] | Percentage of total body weight loss, safety parameters [52] |
Comprehensive Literature Search
A comprehensive literature search for systematic reviews and meta-analyses should be gathered from multiple bibliographic databases to ensure the inclusion of diverse studies [49]. Multiple online databases should be used, such as Embase, MEDLINE, Web of Science, and Google Scholar, with the choice based on the research topic to obtain the largest amount possible of relevant studies [49]. At least two databases should be used in the search [49]. Including both published and unpublished studies (gray literature) reduces the risk of publication bias, resulting in more exact diagnostic accuracy in meta-analysis and higher chances for exploring heterogeneity causes [49].
Reference managers such as Zotero, Mendeley, or EndNote can be used to collect the searched literature, remove duplicates, and manage the initial list of publications [49]. Tools like Rayyan and Covidence can assist in the screening process by suggesting inclusion and exclusion criteria and allowing collaboration among team members [49]. The PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) statement provides updated guidance for transparent and complete reporting of systematic reviews, facilitating the assessment of trustworthiness and applicability of review findings [50].
Quality Assessment and Data Extraction
Quality assessment using standardized tools is crucial to evaluate the methodological rigor of included studies [49]. Common tools include the Cochrane Risk of Bias Tool for randomized controlled trials and the Newcastle-Ottawa Scale for observational studies [49]. Data extraction should use standardized forms to ensure consistent information capture across studies [49]. The extracted data typically includes descriptive study information, sample size, intervention details, outcomes, study design, target population, baseline risk, and other important PICOS characteristics related to clinical, methodological, or statistical heterogeneity [53].
The GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach is widely adopted for assessing certainty (or quality) of a body of evidence [54]. GRADE specifies four levels of certainty for a body of evidence for a given outcome: high, moderate, low, and very low [54]. These assessments are determined through consideration of five domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias [54]. For evidence from non-randomized studies, assessments can then be upgraded through consideration of three further domains [54].
Statistical Synthesis and Analysis Methods
Meta-Analysis Techniques
Meta-analysis employs statistical software such as R and RevMan to compute effect sizes, confidence intervals, and assess heterogeneity [49]. Visual representations, including forest and funnel plots, facilitate the interpretation of results [49]. For dichotomous outcomes, the 'Summary of findings' table should provide both a relative measure of effect (e.g., risk ratio, odds ratio, hazard) and measures of absolute risk [54]. For continuous data, an absolute measure alone (such as a difference in means) might be sufficient [54]. It is important that the magnitude of effect is presented in a meaningful way, which may require some transformation of the result of a meta-analysis [54].
Challenges such as publication bias and heterogeneity are addressed using statistical methods like Egger regression and the trim-and-fill technique [49]. Sensitivity analyses further validate the robustness of findings [49]. Common errors, including data entry mistakes and inappropriate pooling, are mitigated through rigorous methodological adherence and critical self-evaluation [49].
Network Meta-Analysis
Network meta-analysis (NMA) is a powerful extension of traditional pairwise meta-analysis that allows for simultaneous comparison of multiple interventions, even when direct head-to-head comparisons are limited [51] [52]. This approach is particularly valuable in comparative drug efficacy research where multiple treatment options exist but few have been directly compared in randomized trials [51]. The NMA methodology uses both direct and indirect evidence to estimate relative treatment effects across a network of interventions [51].
In practice, NMA has been successfully applied to compare multiple pharmaceutical therapies for conditions such as Crohn's disease [51] and obesity [52]. For example, a systematic review and network meta-analysis of pharmacological treatments for obesity in adults evaluated the efficacy and safety of multiple obesity management medications, including orlistat, semaglutide, liraglutide, tirzepatide, naltrexone/bupropion, and phentermine/topiramate [52]. The analysis included 56 clinical trials enrolling 60,307 patients and found that all medications showed significantly greater total body weight loss percentage compared to placebo, with semaglutide and tirzepatide achieving more than 10% weight loss [52].
Reporting Guidelines and Standards
PRISMA Guidelines
The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement was developed to facilitate transparent and complete reporting of systematic reviews [50]. The PRISMA 2020 statement includes a checklist of 27 items to guide reporting of systematic reviews [50]. These items are essential for allowing decision makers to assess the trustworthiness and applicability of review findings and for allowing others to replicate or update reviews [50]. The PRISMA 2020 statement has been designed primarily for systematic reviews of studies that evaluate the effects of health interventions, irrespective of the design of the included studies [50].
Key PRISMA recommendations include identifying the report as a systematic review in the title, providing an informative title that provides key information about the main objective or question that the review addresses, and following a structured abstract format [50]. The PRISMA flow diagram provides a standardized way to document the flow of studies through the different phases of the review, including information about the number of studies identified, included, and excluded, and the reasons for exclusions [50].
'Summary of findings' tables present the main findings of a review in a transparent, structured and simple tabular format [54]. These tables provide key information concerning the certainty or quality of evidence, the magnitude of effect of the interventions examined, and the sum of available data on the main outcomes [54]. Cochrane Reviews should incorporate 'Summary of findings' tables during planning and publication, and should have at least one key 'Summary of findings' table representing the most important comparisons [54].
Standard Cochrane 'Summary of findings' tables include several essential elements: a brief description of the population and setting, a brief description of the comparison interventions, a list of the most critical outcomes (limited to seven or fewer), a measure of the typical burden of each outcome, the absolute and relative magnitude of effect, the numbers of participants and studies, a GRADE assessment of the overall certainty of the body of evidence for each outcome, space for comments, and explanations [54]. The GRADE approach to assessing the certainty of the evidence defines and operationalizes a rating process that helps separate outcomes into those that are critical, important or not important for decision making [54].
Experimental Protocols and Workflows
Systematic Review Workflow
Meta-Analysis Statistical Process
Research Reagent Solutions Toolkit
Table 2: Essential Research Reagents and Tools for Evidence Synthesis
| Tool Category | Specific Tools/Software | Primary Function | Application in Evidence Synthesis |
|---|---|---|---|
| Reference Management | EndNote, Zotero, Mendeley | Collect searched literature, remove duplicates, manage publication lists [49] | Streamline reference management and study selection, enhancing efficiency and accuracy [49] |
| Study Screening | Rayyan, Covidence | Assist in study screening by suggesting inclusion/exclusion criteria and enabling collaboration [49] | Facilitate the study selection process during systematic review [49] |
| Quality Assessment | Cochrane Risk of Bias Tool, Newcastle-Ottawa Scale | Evaluate methodological rigor of included studies [49] | Assess risk of bias in randomized trials and observational studies respectively [49] |
| Statistical Analysis | R, RevMan | Compute effect sizes, confidence intervals, assess heterogeneity [49] | Perform meta-analysis calculations and generate forest plots [49] |
| Evidence Grading | GRADEpro GDT | Develop 'Summary of findings' tables and grade evidence certainty [54] | Create standardized tables presenting key review findings and quality assessments [54] |
| Database Search | PubMed/MEDLINE, Embase | Access life sciences and biomedical literature [49] | Identify relevant studies through comprehensive database searching [49] |
| Norharmane | 9H-Pyrido[3,4-b]indole (Norharmane)|CAS 244-63-3 | High-purity 9H-Pyrido[3,4-b]indole (Norharmane), a key β-carboline for AHR, MALDI-TOF MS, and pharmacology research. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
| Pinostrobin | Pinostrobin, CAS:480-37-5, MF:C16H14O4, MW:270.28 g/mol | Chemical Reagent | Bench Chemicals |
Quantitative Data Synthesis and Presentation
Efficacy Outcomes in Comparative Drug Research
Table 3: Comparative Efficacy of Pharmaceutical Interventions from Published Network Meta-Analyses
| Therapeutic Area | Interventions Compared | Primary Efficacy Outcome | Key Findings | Certainty of Evidence |
|---|---|---|---|---|
| Crohn's Disease [51] | Adalimumab, Infliximab, Upadacitinib, Methotrexate, Azathioprine | Clinical remission | Adalimumab had highest ranking for induction; Infliximab/azathioprine combination highest for maintenance [51] | Confidence rating was moderate, low, or very low for most comparisons [51] |
| Obesity Pharmacotherapy [52] | Semaglutide, Tirzepatide, Liraglutide, Orlistat, Naltrexone/Bupropion, Phentermine/Topiramate | Percentage of total body weight loss (TBWL%) | All medications showed significantly greater TBWL% vs placebo; Semaglutide and Tirzepatide achieved >10% TBWL [52] | Quality of studies was heterogeneous; most RCTs were double-blind (66%) [52] |
| Obesity Pharmacotherapy Specific Outcomes [52] | Semaglutide, Tirzepatide | Proportion achieving ≥5% TBWL | Patients treated with obesity medications (except orlistat) were more likely to achieve ≥5% TBWL vs placebo [52] | Based on 56 RCTs enrolling 60,307 patients [52] |
Safety and Additional Outcomes
Table 4: Safety Profiles and Secondary Outcomes from Network Meta-Analyses
| Intervention Category | Specific Interventions | Safety Outcomes | Discontinuation Rates | Additional Benefits |
|---|---|---|---|---|
| Crohn's Disease Treatments [51] | Methotrexate, Azathioprine, Upadacitinib | Adverse event related discontinuation numerically highest for methotrexate, azathioprine and upadacitinib [51] | Drug discontinuation rates varied by treatment type and patient population [51] | Conventional therapies remain important in treatment algorithm [51] |
| Obesity Medications [52] | Tirzepatide, Semaglutide | Serious adverse events reported; specific safety profiles varied by medication class [52] | Weight regain after discontinuation: 67% for semaglutide and 53% for tirzepatide after 52-week treatment [52] | Tirzepatide and semaglutide showed normoglycemia restoration, type 2 diabetes remission, heart failure hospitalization reduction [52] |
Advanced Methodological Considerations
Network Meta-Analysis Geometry and Inference
Network meta-analysis requires careful consideration of the network geometry and the validity of underlying assumptions [51]. The network should be evaluated for connectivity, presence of closed loops, and consistency between direct and indirect evidence [51]. Statistical methods for evaluating inconsistency include the use of design-by-treatment interaction model and node-splitting techniques [51]. When networks are sparse and therapies have overlapping confidence intervals, conclusions should be drawn cautiously, as seen in the Crohn's disease NMA where confidence intervals were overlapping despite observed differences in surface under the cumulative ranking (SUCRA) values [51].
Handling Heterogeneity and Reporting Bias
Heterogeneity is a common challenge in meta-analyses and should be quantified using appropriate statistics such as I² and Tau² [49]. The I² statistic describes the percentage of variation across studies that is due to heterogeneity rather than chance, with values of 25%, 50%, and 75% often considered to represent low, moderate, and high heterogeneity respectively [49]. Reporting bias, including publication bias and selective outcome reporting, should be assessed through funnel plots and statistical tests such as Egger's regression test [49]. When asymmetry is detected, methods such as the trim-and-fill technique can be used to adjust for potential missing studies [49].
Systematic reviews and meta-analyses provide indispensable tools for evidence synthesis in comparative drug efficacy research. When meticulously conducted following established methodologies and reporting standards such as PRISMA and GRADE, these approaches represent the highest level of evidence in healthcare research [50] [49]. The integration of network meta-analysis methods has further enhanced their utility for comparing multiple interventions simultaneously, even when direct comparative evidence is limited [51] [52]. As the volume of primary research continues to expand, rigorous systematic reviews and meta-analyses will remain essential for generating reliable evidence to inform clinical practice guidelines, health policy decisions, and future research directions [49].
Navigating Research Challenges: Bias, Validity, and Practical Hurdles
Mitigating Bias in Single-Arm Trials and Studies Using External Controls
Single-arm trials are indispensable in oncology and rare disease research where randomized controlled trials (RCTs) are often unfeasible or unethical [55] [56]. These trials evaluate investigational treatments without concurrent internal control groups, creating an evidence gap regarding comparative effectiveness. External control arms (ECAs), constructed from historical clinical trial data or real-world data (RWD), provide a framework for contextualizing treatment effects by representing the expected outcome without the investigational intervention [57]. Without randomization, however, these analyses are vulnerable to multiple sources of bias that can compromise validity, leading to potentially incorrect conclusions about treatment efficacy and safety [58] [59].
The fundamental challenge lies in achieving comparability between the single-arm trial population and the external control population. Systematic differences in patient characteristics, disease severity, standard of care, outcome assessment, and follow-up procedures can introduce confounding that distorts the estimated treatment effect [55]. Recognition of these methodological challenges has prompted development of advanced statistical methods and study design frameworks to mitigate bias, yet current implementation remains suboptimal. A recent cross-sectional study of 180 published externally controlled trials found critical deficiencies, with only 33.3% using appropriate statistical methods to adjust for baseline covariates and a mere 1.1% implementing quantitative bias analyses [58]. This technical guide provides comprehensive methodologies for identifying, assessing, and mitigating biases throughout the ECA lifecycle, with specific experimental protocols aligned with emerging regulatory and health technology assessment standards.
Classification and Definitions of Primary Bias Types
Understanding the specific mechanisms through which bias operates is essential for developing effective mitigation strategies. The following table summarizes the primary bias types encountered when using external controls, their definitions, and potential impacts on study validity.
Table 1: Classification of Primary Bias Types in Externally Controlled Studies
| Bias Type | Definition | Potential Impact on Study Validity |
|---|---|---|
| Selection Bias [55] | Systematic differences in patient characteristics between the trial and external control populations due to differing inclusion/exclusion criteria or recruitment practices. | Confounds treatment effect estimates due to imbalanced prognostic factors between groups. |
| Unmeasured Confounding [60] | Distortion of the treatment effect estimate due to prognostic factors that differ between groups but are not measured or available in the dataset. | Leads to residual confounding even after adjustment for measured variables; particularly problematic with RWD. |
| Information Bias [55] | Systematic differences in how outcomes, exposures, or covariates are measured, defined, or ascertained between the trial and external control. | Compromises comparability of endpoint assessment; differential misclassification of outcomes. |
| Measurement Error [57] | Inaccurate or inconsistent measurement of variables, particularly concerning real-world endpoints like progression-free survival. | Obscures true treatment effects; reduces statistical power to detect differences. |
| Survivor-Led Time Bias [58] | Artificial inflation of survival times in the external control group due to start of follow-up at a later point in the disease course. | Favors the external control group, potentially masking a true treatment benefit. |
Quantitative Assessment of Current Methodological Gaps
Recent systematic assessments reveal significant methodological shortcomings in current practice. A comprehensive cross-sectional analysis of 180 externally controlled trials published between 2010-2023 identified several critical gaps [58]:
- Only 35.6% of studies provided rationale for using external controls
- Only 16.1% pre-specified the use of external controls in their protocols
- Merely 33.3% used statistical methods to adjust for important covariates
- Only 17.8% performed sensitivity analyses for primary outcomes
- A mere 1.1% implemented quantitative bias analysis
These deficiencies highlight an urgent need for improved methodological rigor in the design, conduct, and analysis of externally controlled studies to generate reliable evidence for regulatory and reimbursement decisions.
Methodological Framework for Bias Mitigation
Pre-Analysis Phase: Design and Data Source Considerations
Target Trial Emulation Framework
The target trial emulation (TTE) framework provides a structured approach for designing externally controlled studies that minimizes methodological biases by explicitly specifying the hypothetical randomized trial that would answer the research question [57]. This process involves defining all key elements of the target trial protocol before analyzing the observational data, creating a principled foundation for comparative analysis.
Experimental Protocol 1: Implementing Target Trial Emulation
- Specify the Target Trial Protocol: Define all components of an ideal RCT, including eligibility criteria, treatment strategies, assignment procedures, outcome definitions, follow-up periods, and causal contrasts of interest.
- Emulate the Target Trial Eligibility Criteria: Apply the same inclusion and exclusion criteria to both the single-arm trial population and the potential external control sources to enhance population comparability.
- Define the Treatment Strategy: Clearly specify the intervention details, including dosing, duration, and concomitant treatments, ensuring the external control reflects the appropriate comparator.
- Align Outcome Measurements: Harmonize endpoint definitions, measurement techniques, and assessment schedules between the trial and external control, prioritizing objective endpoints like overall survival when possible.
- Synchronize Follow-up Start Times: Define a consistent "time zero" for both groups, typically initiation of therapy, to avoid immortal time and survivor-led time biases.
- Specify the Causal Estimand: Define the precise treatment effect to be estimated using the ICH E9(R1) estimand framework, accounting for intercurrent events through appropriate strategies [57].
Data Source Selection and Feasibility Assessment
The validity of an ECA depends fundamentally on the quality and appropriateness of the data source from which it is derived. A feasibility assessment determines whether available data sources can adequately address the research question while meeting methodological requirements [58].
Table 2: Comparative Strengths and Limitations of External Control Data Sources
| Data Source | Key Strengths | Key Limitations |
|---|---|---|
| Historical Clinical Trials [55] [56] | - Protocol-defined data collection- High-quality efficacy outcomes- Detailed baseline characteristics | - Populations may differ due to eligibility criteria- Historic standard of care may differ- Outcome definitions may vary |
| Disease Registries [55] | - Pre-specified data collection- Good clinical detail for selected outcomes- Often includes diverse patients and settings | - May not capture all outcomes of interest- Some covariates may be unavailable- Potential selection bias in enrollment |
| Electronic Health Records [55] [61] | - Good disease ascertainment- Medications administered in hospital- Laboratory test results | - Does not capture care outside provider network- Inconsistent data recording across systems- Lack of standardization complicates outcome ascertainment |
| Health Insurance Claims [55] | - Captures covered care regardless of site- Good prescription medication details- Potential linkage to national registries | - Only captures insured populations- No medications administered during hospitalization- Limited clinical detail on outcomes |
The following workflow diagram illustrates the key decision points in selecting and preparing an external control data source.
Statistical Analysis Phase: Bias Adjustment Methods
Confounding Adjustment Methods
Addressing measured confounding through appropriate statistical methods is essential for creating comparable groups. Propensity score methods represent the most widely used approach for balancing baseline covariates between treatment and external control groups [56].
Experimental Protocol 2: Propensity Score Matching Implementation
- Define the Analysis Population: Identify eligible patients from the single-arm trial and potential external control source using consistent eligibility criteria.
- Select Prognostic Covariates: Identify baseline variables that predict both treatment assignment and outcomes based on clinical knowledge and literature review. The systematic review by [62] recommends pre-specifying these covariates and their selection rationale.
- Estimate Propensity Scores: Fit a logistic regression model predicting probability of being in the single-arm trial (vs. external control) based on selected covariates.
- Implement Matching Algorithm: Match each patient in the single-arm trial to one or more patients in the external control pool using nearest-neighbor matching within a specified caliper distance (typically 0.2 standard deviations of the logit of the propensity score).
- Assess Balance: Evaluate the success of the matching procedure by calculating standardized mean differences for all covariates, with values <0.1 indicating adequate balance.
- Estimate Treatment Effect: Analyze the matched dataset using appropriate regression models (e.g., Cox proportional hazards for time-to-event outcomes) with robust variance estimators to account for the matched nature of the data.
Alternative approaches include propensity score weighting (inverse probability of treatment weighting) and covariate adjustment using multivariate regression, each with specific advantages depending on the sample size and overlap between groups [62].
Quantitative Bias Analysis for Unmeasured Confounding
Even after comprehensive adjustment for measured confounders, unmeasured confounding remains a persistent threat to validity. Quantitative bias analysis (QBA) provides a structured approach to quantify the potential impact of unmeasured confounders on study results [60].
Experimental Protocol 3: Implementing Quantitative Bias Analysis
- Identify Potential Unmeasured Confounders: Through literature review and clinical expert input, identify key prognostic factors not adequately measured in the dataset (e.g., performance status, biomarker levels, socioeconomic factors).
- Parameterize Bias Models: For each unmeasured confounder, specify its prevalence in the treatment and control groups and its association with the outcome based on external evidence from the literature or validation studies.
- Implement Bias Analysis: Apply statistical methods such as external adjustment using the methodology described in [60], which incorporates evidence from randomized trial data, targeted literature searches, and clinician input.
- Conduct Tipping Point Analyses: Determine the strength of an unmeasured confounder that would be required to nullify the observed treatment effect (i.e., reduce the hazard ratio to 1.0).
- Interpret and Report Results: Present both adjusted and unadjusted estimates with explicit quantification of how the results might change under plausible confounding scenarios.
A recent demonstration study applying QBA in 14 randomized trial emulations found that external adjustment for unmeasured and mismeasured confounders reduced the ratio of hazard ratios from 1.22 to 1.17, moving the estimate closer to the true randomized trial result [60].
Advanced Topics and Emerging Methodologies
The Scientist's Toolkit: Essential Analytical Reagents
Table 3: Essential Methodological Reagents for Externally Controlled Analyses
| Methodological Reagent | Function/Purpose | Implementation Considerations |
|---|---|---|
| Propensity Score Models [56] | Balances measured covariates between treatment and external control groups to reduce confounding. | Requires pre-specification of covariates; effectiveness depends on overlap between groups. |
| Inverse Probability Weighting [62] | Creates a pseudo-population where the distribution of covariates is independent of treatment assignment. | Can be unstable with extreme weights; truncation or stabilization may be necessary. |
| Quantitative Bias Analysis [60] | Quantifies the potential impact of unmeasured confounding on study results. | Relies on external evidence for parameter estimation; requires transparent reporting of assumptions. |
| High-Dimensional Propensity Scores [62] | Automatically selects covariates from large datasets (e.g., claims data) to improve confounding control. | Captures both established and potential confounders; requires large sample sizes. |
| Sensitivity Analyses [58] | Evaluates the robustness of results to different methodological assumptions and data handling approaches. | Should be pre-specified; tests impact of outlier, missing data, and model specification. |
Addressing Measurement and Information Biases
Information bias arising from differential outcome ascertainment between trial and real-world settings presents particular challenges, especially for endpoints like progression-free survival that require regular radiographic assessment [57]. Measurement error in real-world endpoints can manifest as either misclassification bias (incorrect categorization of events) or surveillance bias (differential assessment schedules) [57].
Mitigation strategies include:
- Endpoint Harmonization: Where possible, use objective endpoints like overall survival that are less susceptible to assessment variability.
- Algorithmic Validation: Develop and validate sophisticated algorithms for deriving real-world endpoints that approximate clinical trial standards.
- Quantitative Assessment: Conduct simulations to quantify the potential impact of measurement errors on effect estimates.
- Contextualized Interpretation: Explicitly acknowledge and discuss limitations in endpoint comparability when interpreting results.
The following diagram illustrates a comprehensive workflow integrating multiple bias assessment and mitigation strategies throughout the research process.
The use of external controls in single-arm trials represents a promising methodology for generating comparative effectiveness evidence when RCTs are not feasible, particularly in oncology and rare diseases. However, this approach requires meticulous attention to bias mitigation throughout the research lifecycle. Current evidence suggests that methodological practice often falls short of established standards, with insufficient attention to confounding adjustment, sensitivity analysis, and quantitative bias assessment [58] [62].
The path forward requires greater adoption of target trial emulation frameworks, pre-specification of analytical methods, implementation of robust propensity score approaches, and routine application of quantitative bias analysis to address unmeasured confounding [60] [57]. Regulatory and health technology assessment bodies increasingly emphasize these methodologies in their guidelines, highlighting the need for proactive engagement with these agencies during the study planning phase [62].
As external controls continue to support regulatory submissions and health technology assessments, particularly in areas of unmet medical need, maintaining rigorous methodological standards will be essential for ensuring that these innovative approaches yield reliable, actionable evidence for drug development and patient care. Future methodological research should focus on standardizing approaches to measurement error correction, developing more sophisticated quantitative bias analysis techniques, and establishing clearer guidelines for evaluating the credibility of externally controlled studies.
In comparative drug efficacy research, heterogeneity represents the variations in treatment effects attributable to differences in patient populations, trial methodologies, and outcome measurements. Understanding and addressing these sources of variability is fundamental to generating evidence that is both statistically sound and clinically meaningful. Heterogeneity of Treatment Effects (HTE) examines why medications work differently across diverse patient populations and treatment contexts, moving beyond Average Treatment Effects (ATE) to inform personalized treatment strategies and improve patient outcomes [63].
The growing use of Real-World Data (RWD) offers larger study sizes and more diverse patient populations compared to traditional Randomized Controlled Trials (RCTs), providing enhanced opportunities to detect and characterize HTE. This technical guide examines systematic approaches to address heterogeneity across patient populations, trial designs, and outcome assessments within the framework of comparative drug efficacy research [63].
Heterogeneity in Patient Populations
Defining and Measuring Heterogeneity of Treatment Effects
HTE occurs when a treatment effect changes across levels of a patient characteristic, known as an effect modifier. True effect modifiers must be baseline characteristics measurable prior to treatment initiation, not affected by the treatment itself, to avoid introducing bias. Common effect modifiers include age, sex, genotype, comorbid conditions, and other risk factors for the outcome of interest [63].
Quantifying effect modification depends on the scale on which treatment effects are measured, a phenomenon known as scale dependence. Treatment effects may be constant across an effect modifier on one scale but vary significantly on another, as illustrated in Table 1 [63].
Table 1: Scale Dependence in Effect Modification
| Scenario | Treated | Comparator | Risk Difference | Risk Ratio |
|---|---|---|---|---|
| Constant on difference scale, effect modification on ratio scale | ||||
| Characteristic present | 0.40 | 0.30 | 0.10 | 1.33 |
| Characteristic absent | 0.50 | 0.40 | 0.10 | 1.25 |
| Constant on ratio scale, effect modification on difference scale | ||||
| Characteristic present | 0.40 | 0.32 | 0.08 | 1.25 |
| Characteristic absent | 0.50 | 0.40 | 0.10 | 1.25 |
The risk difference scale is generally most informative for clinical decision-making as it directly estimates the number of people who would benefit or be harmed from treatment. Best practices for reporting effect modification include identifying the assessment scale, reporting outcome frequency by effect modifier level, and providing measures of effect modification with common reference groups for multi-level modifiers [63].
Methodological Approaches to Characterizing HTE
Three primary methodological approaches exist for studying HTE, each with distinct tradeoffs, as summarized in Table 2 [63].
Table 2: Methodological Approaches for Studying Heterogeneity of Treatment Effects
| Method | Key Features | Advantages | Limitations |
|---|---|---|---|
| Subgroup Analysis | Examines treatment effects within specific patient subgroups | Simple, transparent, provides mechanistic insights | Difficult to resolve which subgroup combination should guide decisions; prone to spurious associations |
| Disease Risk Score (DRS) | Incorporates multiple patient characteristics into a summary outcome risk score | Relatively simple to implement; clinically useful | May obscure mechanistic insights; may not completely describe HTE |
| Effect Modeling | Directly predicts individual treatment effects using multivariate models | Potential for precise HTE characterization | Prone to model misspecification; may not provide mechanistic insights |
Each approach offers complementary strengths for different research contexts. Subgroup analysis provides intuitive, transparent results but struggles with multiple comparisons. DRS methods efficiently handle multiple covariates but may obscure biological mechanisms. Effect modeling approaches offer personalized effect estimates but require careful validation to avoid misspecification [63].
Heterogeneity in Trial Designs
Efficacy Versus Effectiveness Trials
Clinical trials exist along a spectrum from explanatory trials (efficacy) to pragmatic trials (effectiveness). Efficacy trials determine whether an intervention produces expected results under ideal, controlled circumstances, while effectiveness trials measure beneficial effects under "real-world" clinical settings [64].
Key factors distinguishing these approaches include patient characteristics, condition severity, drug regimens, compliance, co-morbidities, and concomitant treatments. Effectiveness trials typically feature broader eligibility criteria, heterogeneous patient populations, and routine clinical settings, enhancing generalizability but potentially increasing variability in treatment effects [64].
Comparative Effectiveness Trials and Single-Arm Designs
Comparative Effectiveness Trials (CETs) randomize participants to usual care alternatives to generate unbiased evidence about the relative effectiveness of existing treatments. CETs often adopt pragmatic designs that compare interventions under routine practice conditions, addressing key priorities of patients and health systems [65].
Single-Arm Trials (SATs) represent a specialized design where all subjects receive the experimental treatment without concurrent controls. SATs are particularly valuable in orphan drug development and rare diseases where RCTs may be impractical, or in oncology for life-threatening conditions with no effective treatment options. However, SATs lack randomized controls, increasing susceptibility to bias and compromising both internal and external validity. Efficacy assessment typically relies on predetermined thresholds or external controls for comparison [66].
Figure 1: Spectrum of Clinical Trial Designs Addressing Heterogeneity
The Target Trial Approach for Real-World Evidence
When using non-randomized evidence, the target trial approach involves designing studies to emulate the randomized trial that would ideally have been performed without ethical or feasibility constraints. This framework requires explicitly specifying all protocol components of the target trial, then designing the observational study to emulate each component as closely as possible [43].
Key elements of trial emulation include:
- Eligibility criteria mirroring those of the target trial
- Treatment strategies clearly defined and assigned at baseline
- Treatment assignment process documented
- Outcome measurement consistent with target trial
- Follow-up period and procedures specified
- Causal contrast of interest clearly defined
- Statistical analysis plan aligned with target trial [43]
This approach minimizes biases common in observational studies and provides more reliable estimates of intervention effects from real-world data.
Heterogeneity in Outcome Assessments
Endpoints Versus Outcomes
In clinical trial methodology, outcomes represent specific results or effects that can be measured, while endpoints are events or outcomes measured objectively to determine whether the intervention being studied is beneficial. Endpoints address the central research question and determine trial success, while outcomes represent the measurements collected to inform endpoints [67].
Endpoints are typically classified hierarchically by purpose and significance:
- Primary endpoints serve as make-or-break standards for trial success and regulatory approval
- Secondary endpoints provide supportive information on additional benefits or mechanism of action
- Exploratory endpoints generate hypotheses for future research or assess novel measurements [68]
Endpoint Selection and Multiplicity Considerations
Clinical trials frequently assess multiple endpoints to comprehensively evaluate intervention effects. However, analyzing multiple endpoints increases the likelihood of false positive conclusions due to multiplicity - the statistical phenomenon where the chance of making erroneous conclusions accumulates with each additional comparison [68].
Regulatory guidance outlines several strategies for managing multiple endpoints:
- Co-primary endpoints require effects on all specified endpoints for trial success
- Multiple primary endpoints allow success based on any individual endpoint
- Composite endpoints combine multiple clinical outcomes into a single endpoint
- Multi-component endpoints require multiple effects within each patient [68]
Table 3: Efficacy Endpoints in Clinical Trials
| Endpoint Category | Definition | Examples | Regulatory Considerations |
|---|---|---|---|
| Primary Endpoint | Directly determines trial success and supports regulatory approval | Overall survival (OS), Objective response rate (ORR) | Must be precisely defined with statistical plan controlling Type I error |
| Secondary Endpoint | Provides supportive evidence of clinically important effects | Patient-reported outcomes (PROs), Quality of life measures | Effects demonstrated can be included in labeling but insufficient alone for approval |
| Surrogate Endpoint | Biomarker or measure predictive of clinical benefit but not direct benefit | Progression-free survival (PFS), HbA1c reduction | May support accelerated approval requiring confirmatory trials |
| Composite Endpoint | Combination of multiple clinical outcomes into a single endpoint | Major Adverse Cardiovascular Events (MACE) | Uncertainty may exist about effects on individual components |
Statistical methods such as hierarchical testing, fallback procedures, and gatekeeping strategies help control familywise error rates when assessing multiple endpoints. The choice of strategy depends on trial objectives, clinical context, and regulatory requirements [68].
Patient-Reported and Clinician-Reported Outcomes
Patient-Reported Outcome Measures (PROMs) capture data directly from patients without interpretation by clinicians, assessing symptoms, functioning, and health-related quality of life (HRQoL). These provide crucial evidence of treatment benefits meaningful to patients' daily lives [69].
Clinician-Reported Outcome (ClinRO) Measures involve observations by trained clinicians, including signs of disease, clinical decisions, and global assessments. While valuable, ClinROs may introduce interpretation bias compared to direct patient reports [69].
Methodological guidance emphasizes establishing content validity - ensuring outcome assessments measure concepts relevant to patients and clinicians - through qualitative research and patient engagement during instrument development [69].
Integrated Methodological Framework
Conceptual Framework for Addressing Heterogeneity
Addressing heterogeneity requires systematic consideration across all trial dimensions, as illustrated in Figure 2.
Figure 2: Integrated Framework for Addressing Heterogeneity in Comparative Drug Efficacy Research
Case Study: Pharmacological Obesity Treatments
A 2025 network meta-analysis of obesity medications illustrates approaches to addressing heterogeneity in comparative effectiveness research. The analysis included 56 RCTs with 60,307 patients, evaluating six pharmacological treatments across multiple endpoints [52].
Table 4: Heterogeneity in Obesity Pharmacotherapy Outcomes
| Medication | TBWL% at Endpoint | ≥5% TBWL Achieved | ≥15% TBWL Achieved | Key Outcome Heterogeneity |
|---|---|---|---|---|
| Tirzepatide | >10% | Most likely | Most likely | Effective in T2D remission, OSA, MASH |
| Semaglutide | >10% | Highly likely | Highly likely | Reduces MACE, knee osteoarthritis pain |
| Liraglutide | 5-10% | Likely | Moderate likelihood | Consistent weight loss across populations |
| Phentermine/Topiramate | 5-10% | Likely | Moderate likelihood | Limited long-term data |
| Naltrexone/Bupropion | 5-10% | Likely | Less likely | Mental health considerations |
| Orlistat | <5% | Less likely | Unlikely | Gastrointestinal adverse effects |
The analysis revealed substantial heterogeneity in outcomes across medications, with tirzepatide and semaglutide demonstrating superior efficacy for total body weight loss percentage (TBWL%), while different agents showed distinct profiles for obesity-related complications such as type 2 diabetes remission, obstructive sleep apnea, and cardiovascular outcomes [52].
Research Reagent Solutions for Heterogeneity Assessment
Table 5: Methodological Tools for Addressing Heterogeneity
| Methodological Tool | Application | Key Function |
|---|---|---|
| Subgroup Analysis | Patient Population Heterogeneity | Examines treatment effects within specific patient subgroups |
| Disease Risk Score (DRS) | Patient Population Heterogeneity | Creates summary scores incorporating multiple patient characteristics |
| Effect Modeling | Patient Population Heterogeneity | Directly models how treatment effects vary by patient characteristics |
| Target Trial Emulation | Trial Design Heterogeneity | Provides framework for designing observational studies to emulate RCTs |
| Multiplicity Adjustment Methods | Outcome Assessment Heterogeneity | Controls false positive rates when assessing multiple endpoints |
| Patient-Reported Outcome Measures (PROMs) | Outcome Assessment Heterogeneity | Captures treatment effects directly from patient perspective |
| Network Meta-Analysis | Cross-Design Heterogeneity | Enables indirect comparisons across different trial designs |
Addressing heterogeneity in patient populations, trial designs, and outcome assessments requires methodologically sophisticated approaches that balance internal validity with external generalizability. The evolving framework for comparative effectiveness research integrates rigorous HTE assessment, pragmatic trial designs, and comprehensive outcome measurement to generate evidence meaningful for both clinical decision-making and healthcare policy.
Future methodological development should focus on advancing causal inference methods for heterogeneous effects, optimizing pragmatic trial designs, and validating patient-centered outcome assessments across diverse populations. Through systematic attention to heterogeneity throughout the research process, comparative drug efficacy studies can better inform personalized treatment strategies and improve patient outcomes across diverse healthcare contexts.
Managing Uncertainty and Statistical Limitations in Indirect Comparisons
Indirect treatment comparisons have become indispensable methodological tools for health technology assessment and drug development when head-to-head clinical trial evidence is unavailable. This technical guide examines the core methodologies, statistical limitations, and uncertainty management strategies for generating reliable comparative effectiveness evidence. Within the broader context of establishing guidelines for comparative drug efficacy research, we detail methodological frameworks including adjusted indirect comparisons, matching-adjusted indirect comparisons, and emerging causal inference approaches. We provide specific protocols for implementation, quantitative validation metrics, and visualization tools to enhance methodological rigor in pharmaceutical research and development.
In the rapidly evolving landscape of drug development and regulatory science, indirect comparisons address a critical evidence gap: determining the relative efficacy and safety of multiple treatment options when direct head-to-head clinical trials are absent [21]. The proliferation of novel therapeutic agents across disease areas, particularly oncology and chronic conditions, has intensified the need for robust methods to inform clinical decision-making, health technology assessment, and reimbursement policies [70].
Between 2015 and 2020, regulatory agencies approved a substantial proportion of drugs based on single-arm studies with no control arm—43% by the FDA and 21% by the EMA for non-orphan diseases [70]. This trend toward approvals based on external controls or single-arm designs creates significant challenges for comparative effectiveness assessment, necessitating advanced methodological approaches for reliable indirect treatment comparisons.
This guide examines the statistical foundations, practical implementation, and uncertainty management frameworks for indirect comparison methods, positioning them within a comprehensive paradigm for comparative drug efficacy research.
Methodological Foundations of Indirect Comparisons
Core Statistical Frameworks
Indirect treatment comparisons encompass several methodological approaches that enable estimation of relative treatment effects through common comparators. These methods preserve the randomization of original trials when properly implemented and address different types of evidence gaps in comparative effectiveness research [21].
Table 1: Core Methodological Approaches for Indirect Comparisons
| Method | Key Principle | Data Requirements | Primary Applications |
|---|---|---|---|
| Adjusted Indirect Comparison | Compares treatment effects relative to a common comparator | Aggregate data from two or more trials sharing a common comparator | HTA submissions for drug reimbursement; comparisons where individual patient data are limited |
| Matching-Adjusted Indirect Comparison (MAIC) | Re-weights individual patient data from one study to match aggregate baseline characteristics of another | IPD from one trial and aggregate data from another | Comparisons across trials with different designs or patient populations; oncology and rare diseases |
| Network Meta-Analysis | Simultaneously incorporates direct and indirect evidence within a connected network of treatments | Multiple trials forming connected treatment network | Comparative effectiveness of multiple interventions; clinical guideline development |
| Causal Inference-Based Methods | Estimates causal effects using observational data through counterfactual frameworks | Individual-level data with comprehensive baseline characteristics | HTA when randomized evidence is limited; real-world evidence generation |
The fundamental principle underlying adjusted indirect comparisons involves comparing the magnitude of treatment effect between two interventions relative to a common comparator [21]. For treatments A and B compared against a common control C in separate studies, the indirect comparison of A versus B is estimated by comparing the A versus C effect with the B versus C effect. This approach preserves the randomization within each trial but introduces additional uncertainty equal to the sum of the variances from the component comparisons [21].
Conceptual Framework for Indirect Comparisons
The following diagram illustrates the fundamental concepts and methodological relationships in indirect treatment comparisons:
Quantitative Analysis of Methodological Performance
Statistical Properties and Uncertainty Assessment
Each indirect comparison method carries distinct statistical properties and uncertainty profiles that researchers must quantify and report. Understanding these properties is essential for appropriate interpretation and application of results.
Table 2: Statistical Properties and Uncertainty Metrics of Indirect Comparison Methods
| Method | Key Assumptions | Uncertainty Sources | Validation Approaches | Common Effect Measures |
|---|---|---|---|---|
| Adjusted Indirect Comparison | Similarity of study populations and effect modifiers; consistency of treatment effects | Between-trial heterogeneity; sampling error from component studies | Sensitivity analysis for effect modifiers; exploration of heterogeneity | Hazard ratios, risk ratios, odds ratios, mean differences |
| Matching-Adjusted Indirect Comparison | All effect modifiers are measured and included; correct model specification | Effective sample size reduction; unmeasured confounding; extrapolation | Assessment of balance diagnostics; comparison of effective sample size | Hazard ratios (e.g., 0.66 with 95% CI 0.44-0.97) [71] |
| Network Meta-Analysis | Transitivity across treatment comparisons; consistency between direct and indirect evidence | Incoherence in network loops; heterogeneity across studies | Node-splitting for local inconsistency; design-by-treatment interaction | Pooled hazard ratios, relative risks with credible intervals |
| Causal Inference-Based Methods | No unmeasured confounding; correct model specification; positivity assumption | Model misspecification; unmeasured confounding; selection bias | Negative control outcomes; sensitivity analyses; E-value estimation | Average treatment effects; conditional causal risk ratios |
The uncertainty associated with adjusted indirect comparisons is particularly important to quantify. As demonstrated in prior research, if two hypothetical trials each have variances of 1.0 mmol/L for blood glucose reduction, the adjusted indirect comparison would have a combined variance of 2.0 mmol/L, reflecting the compounded uncertainty from both component studies [21].
Implementing Matching-Adjusted Indirect Comparisons: A Case Example
A recent application of MAIC methodology compared zanubrutinib versus venetoclax plus obinutuzumab in treatment-naïve chronic lymphocytic leukemia [71]. The implementation followed a rigorous protocol:
Individual patient data from the SEQUOIA trial (zanubrutinib) were weighted to match aggregate baseline characteristics from the CLL14 trial (venetoclax plus obinutuzumab). After matching and adjustment, the effective sample size for the zanubrutinib group was reduced to 163, reflecting the weighting process [71].
The MAIC analysis demonstrated a progression-free survival benefit for zanubrutinib versus venetoclax plus obinutuzumab with a hazard ratio of 0.66 (95% confidence interval 0.44-0.97; P = 0.0351) [71]. This case example illustrates the potential of MAIC to generate comparative effectiveness evidence when head-to-head trials are unavailable.
Methodological Protocols and Implementation
Protocol for Adjusted Indirect Comparisons
The implementation of adjusted indirect comparisons requires strict adherence to methodological protocols to minimize bias and ensure validity:
Identify Common Comparator: Establish a connected network through a common comparator treatment administered using similar protocols in separate trials.
Extract Effect Estimates: Obtain relative effect measures (e.g., hazard ratios, risk ratios) and measures of precision (confidence intervals, standard errors) for each treatment versus the common comparator.
Calculate Indirect Estimate: Compute the indirect comparison using the relative effect measures. For ratio measures, this typically involves division of the effect estimates.
Quantify Uncertainty: Calculate the variance of the indirect estimate as the sum of the variances of the component comparisons. For ratio measures, the standard error of the log indirect estimate is calculated as the square root of the sum of the squared standard errors.
Assess Validity: Evaluate the similarity of trial populations, methodologies, and outcome definitions that could violate the key assumption of exchangeability.
Advanced Methodological Approaches: Causal Inference and Target Trial Emulation
Emerging methodological frameworks incorporate causal inference principles to address limitations of traditional indirect comparison methods. The European Union's Health Technology Assessment guidelines are evolving to incorporate these approaches, particularly for cancer drug assessments [70].
The causal estimand framework provides a precise definition of treatment effects through five attributes: treatment, target population, outcome of interest, population-level summary measure, and strategy for addressing intercurrent events [70]. This framework offers advantages over traditional PICO (Population, Intervention, Comparator, Outcome) approaches by more precisely defining the causal question of interest.
Target trial emulation uses observational data to estimate causal effects by designing analyses that mimic pragmatic randomized trials [70]. This approach applies causal inference methodologies to model hypothetical interventions in specific target populations, potentially providing more relevant estimates for health technology assessment decisions.
The following diagram illustrates the workflow for implementing causal inference approaches in comparative effectiveness research:
Essential Methodological Tools and Research Reagents
Successful implementation of indirect comparison methods requires specific methodological tools and analytical components. The following table details essential elements of the methodological toolkit for researchers conducting indirect comparisons.
Table 3: Essential Methodological Toolkit for Indirect Comparisons
| Tool Category | Specific Components | Function and Application | Implementation Considerations |
|---|---|---|---|
| Statistical Software | R (package: metafor), Python, SAS, STATA | Implementation of statistical models for indirect comparisons; data manipulation and visualization | R preferred for MAIC implementation; commercial software may require specialized macros |
| Data Requirements | Individual patient data (IPD), aggregate data, published effect estimates | IPD enables MAIC; aggregate data sufficient for adjusted indirect comparisons | Data sharing agreements; standardization of variable definitions across studies |
| Methodological Components | Propensity score weighting, outcome models, network meta-regression | Adjust for cross-trial differences; model effect modifiers; assess heterogeneity | Balance assessment for weighting approaches; sensitivity analyses for model assumptions |
| Validation Tools | Balance diagnostics, effective sample size calculations, sensitivity analyses | Assess quality of matching; quantify information loss; test robustness of conclusions | Report effective sample size post-weighting; evaluate impact of unmeasured confounding |
Discussion and Future Methodological Directions
The methodological landscape for indirect treatment comparisons continues to evolve, with several promising directions emerging. Causal inference frameworks are increasingly integrated with traditional indirect comparison methods, offering more rigorous approaches for addressing confounding and selection bias [70]. The estimand framework aligns more closely with regulatory and health technology assessment needs by precisely defining the treatment effect of interest [70].
Future methodological development should focus on approaches that better account for between-trial heterogeneity in patient populations, protocols, and outcome assessments. Methods that explicitly model the sources of heterogeneity and their impact on treatment effect estimates will enhance the credibility of indirect comparison results. Additionally, standardized approaches for communicating uncertainty from indirect comparisons will help decision-makers appropriately weight this evidence in therapeutic assessments.
As drug development increasingly targets molecularly defined subgroups and rare diseases, indirect comparison methods must adapt to evidence landscapes characterized by single-arm trials and external controls. The integration of real-world evidence through causal inference approaches represents a promising direction for generating comparative effectiveness evidence when randomized trials are infeasible or unethical.
Indirect treatment comparisons provide valuable methodological tools for addressing evidence gaps in comparative drug effectiveness. When implemented with rigorous attention to methodological assumptions, uncertainty quantification, and validation, these approaches can inform clinical decision-making, health technology assessment, and drug development strategies. The ongoing methodological evolution toward causal inference frameworks and enhanced uncertainty characterization will further strengthen the role of indirect comparisons in the evidence ecosystem for therapeutic interventions.
Overcoming Logistical and Regulatory Hurdles in Multisite and International Trials
The successful execution of multisite and international clinical trials is pivotal for robust comparative drug efficacy research. Such studies are inherently complex, requiring meticulous navigation of divergent regulatory frameworks, intricate supply chain logistics, and evolving scientific standards. This whitepaper provides a technical guide to overcoming these challenges, with a specific focus on implications for demonstrating therapeutic equivalence and superiority. It synthesizes current regulatory shifts, detailed experimental protocols, and strategic operational models to equip researchers and drug development professionals with the methodologies necessary for generating reliable, generalizable evidence in a global context.
Clinical trial activity has demonstrated a strong recovery in 2025, with a significant increase in new studies. Recent data from the first half of 2025 indicates the initiation of 6,071 Phase I-III interventional trials, a 20% increase from the same period in 2024 [72]. This resurgence, however, unfolds against a backdrop of intensifying challenges. Global supply chains remain vulnerable to disruptions from geopolitics, pandemics, and material shortages, while regulatory environments are in a state of flux [73] [22]. For research centered on comparative efficacy, these logistical and regulatory hurdles are not merely operational concerns; they are fundamental variables that can compromise data integrity, patient safety, and the validity of the final efficacy conclusions. This guide addresses these challenges through the specific lens of comparative efficacy research, where consistency in trial product delivery and adherence to multifaceted regulations are prerequisites for a valid experimental comparison.
Navigating the Regulatory Maze
A primary hurdle in international comparative research is the lack of a unified regulatory framework. Sponsors must contend with a patchwork of requirements from agencies like the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA), which can differ significantly in their demands for data and patient populations [22].
Evolving Requirements for Efficacy Endpoints
A significant regulatory shift in 2025 is the FDA's new stance on Comparative Efficacy Studies (CES) for biosimilar development. The October 2025 draft guidance clarifies that for many biosimilars, a comprehensive combination of comparative analytical assessments and comparative pharmacokinetic (PK) data may suffice to demonstrate biosimilarity, potentially replacing the need for large, costly CES [31] [74].
Protocol Implications: For a sponsor leveraging this new pathway, the experimental protocol must be meticulously designed. The analytical studies should demonstrate that the proposed biosimilar is "highly similar" to the reference product notwithstanding minor differences in clinically inactive components. This involves orthogonal methods for structural and functional characterization, while the PK study (e.g., a single-dose, crossover, or parallel-design trial) must show no clinically meaningful differences in safety, purity, and potency [31].
Proactive Regulatory Strategy
The following workflow outlines a strategic approach to navigating the regulatory landscape for a global trial, integrating early engagement and continuous monitoring.
Diagram: A proactive regulatory strategy workflow for global trials. The process emphasizes early engagement with National Regulatory Authorities (NRAs) and continuous management of divergent requirements. (NRA: National Regulatory Authority)
Diversity and Inclusion Mandates
Regulatory guidance on trial diversity from the FDA, EMA, and WHO has solidified, moving from recommendation to expectation [22]. For comparative efficacy research, this is scientifically critical; a therapy's performance relative to a comparator may vary across demographic and genetic subgroups. In 2025, a key challenge is moving from planning to execution.
Experimental Protocol for Diverse Enrollment: A detailed methodology for meeting diversity mandates involves:
- Community Partnership: Actively collaborate with community organizations, urban leagues, faith-based groups, and Historically Black Colleges and Universities (HBCUs) to build trust and reach historically underrepresented populations [22].
- Site Selection & Feasibility: Use clinical trial intelligence platforms to identify and select investigative sites with proven access to diverse patient populations and the cultural competency to engage them effectively [75] [72].
- Protocol Design: Minimize participant burden through decentralized trial elements (e.g., home health visits, local lab draws) and patient-centric procedures, ensuring that participation is logistically feasible for a broader population [22].
Mastering Clinical Trial Logistics
The integrity of a comparative efficacy study is entirely dependent on the unimpaired delivery and storage of the investigational products. Logistics is, therefore, a foundational element of the experimental methodology.
The Challenge of Global Supply Chains
Global supply chains face persistent challenges, including rising air freight costs, port congestion, and customs delays, which can disrupt trial timelines and jeopardize product stability [73]. For US-based sponsors, export control complexities have become a significant burden in 2025, requiring extensive classification of materials, screening against restricted party lists, and adherence to strict Electronic Export Information filing rules [76].
Strategic Logistics Models
A dual-hub operational model is a proven strategy to mitigate these challenges. This approach involves using a US-based hub for domestic and American trials and a UK-based hub for European and international destinations [76].
Advantages of the UK Hub for European Operations:
- Regulatory Simplification: UK export controls for commercial pharmaceuticals are generally less complex than US EAR requirements, reducing processing time [76].
- Market Access: The UK's Trade and Cooperation Agreement with the EU provides tariff-free access for most goods, simplifying shipments to European trial sites [76].
- Operational Efficiency: Geographic proximity to Europe enables shorter transit times, reduced freight costs, and easier coordination due to overlapping business hours [76].
End-to-End Logistics Protocol
The following workflow details the critical steps for managing the journey of an investigational product in a comparative efficacy trial, from manufacturer to patient.
Diagram: An end-to-end logistics protocol for clinical trial materials. This workflow highlights critical control points for temperature, chain of custody, and regulatory documentation that are essential for trial integrity. (cGMP: Current Good Manufacturing Practice)
The Scientist's Toolkit: Key Reagent & Material Solutions
The following table details essential materials and their functions in ensuring the integrity of the clinical supply chain for a comparative efficacy study.
Table: Essential Research Reagent & Material Solutions for Clinical Trial Integrity
| Item/Category | Technical Function & Explanation |
|---|---|
| Validated cGMP Storage | Provides assured storage at specified temperature ranges (e.g., 2°C–8°C, 15°C–25°C) for finished goods and raw materials, ensuring product stability and integrity prior to distribution [77]. |
| Temperature-Controlled Shipping | Maintains the cold chain during transit using qualified packaging and equipment with continuous monitoring to prevent temperature excursions that can compromise product efficacy [76] [77]. |
| Chain of Custody Documentation | A secure, sequential record documenting every individual or system that handles the investigational product, which is critical for regulatory compliance and tracing any potential integrity issues [77]. |
| Clinical Trial Intelligence Platforms | Data analytics software (e.g., H1's Trial Landscape) used to optimize site feasibility, analyze predictive enrollment, and identify investigators, enabling data-driven decisions for faster trial execution [75] [72]. |
| Restricted Party Screening Tools | Automated systems to verify that all parties (trial sites, investigators, logistics providers) do not appear on OFAC, BIS, and other government restricted lists, a necessary step for US export compliance [76]. |
Data Management and Analytical Considerations
In international trials, data integrity is challenged by differing national data privacy laws, such as Europe's General Data Protection Regulation (GDPR) and the US Health Insurance Portability and Accountability Act (HIPAA) [75].
Methodology for Cross-Border Data Sharing:
- Standardized Protocols: Implement standardized data collection and coding protocols across all trial sites to ensure consistency and interoperability [75].
- Technology Platforms: Utilize secure, centralized data management platforms that can enforce role-based access controls and audit trails, ensuring data security while facilitating remote access for authorized personnel across the globe [75].
- Artificial Intelligence: Leverage predictive analytics and generative AI to access reliable datasets for site selection and patient recruitment planning, mitigating the risk of operational delays [75].
Overcoming the logistical and regulatory hurdles in multisite and international trials is a complex but manageable endeavor that demands a proactive, integrated, and scientifically rigorous approach. The evolving regulatory landscape, exemplified by the FDA's new stance on biosimilar efficacy studies, offers opportunities to streamline development without compromising scientific rigor. Success hinges on viewing logistics not as a support function but as a core component of the experimental protocol, ensuring the uncompromised delivery of investigational products. Furthermore, the industry's heightened focus on diversity is a scientific imperative for comparative efficacy research, ensuring that study results are generalizable to the broad patient populations that will ultimately use the therapies. By adopting the strategic frameworks, detailed protocols, and material solutions outlined in this guide, researchers and drug development professionals can navigate this complex environment to generate the high-quality, definitive evidence required to advance global public health.
Optimizing Patient Recruitment, Retention, and Data Collection Strategies
Within the critical field of comparative drug efficacy research, the integrity and success of a clinical trial are fundamentally dependent on three pillars: efficient patient recruitment, robust participant retention, and high-quality data collection. Inefficiencies in these areas remain a primary cause of trial delays, inflated costs, and inconclusive results [78] [79]. This whitepaper provides researchers, scientists, and drug development professionals with a technical guide to modernizing these core components. By adopting strategic, human-centered, and technology-enabled approaches, sponsors can enhance the reliability of comparative efficacy data and accelerate the development of new therapies.
Recent regulatory shifts further underscore the need for optimized strategies. The Food and Drug Administration (FDA) has issued new draft guidance clarifying that for certain development pathways, such as for biosimilars, comparative efficacy studies may no longer be a default requirement if sufficient analytical and pharmacokinetic data exist [31]. This evolution places a greater emphasis on the precision and quality of all collected data, making the efficiency of trial conduct more important than ever.
The Patient Recruitment Blueprint
Effective patient recruitment requires a move away from traditional, one-size-fits-all methods toward a nuanced, strategic, and empathetic process.
The Design Thinking Framework
Design thinking, a human-centered problem-solving approach, offers a structured methodology to tackle recruitment challenges by deeply understanding patient needs and behaviors [78]. The process consists of four iterative phases:
- Phase 1: Inspiration: This foundational phase is dedicated to need-finding and empathizing with potential patients and their caregivers. Techniques include direct patient interviews, social listening (monitoring patient conversations on social media and online forums), and engagement with patient advocacy groups. The goal is to gain authentic insights into patient priorities, pain points, and motivations related to their condition and trial participation [78].
- Phase 2: Ideation: With a clear understanding of user needs, multidisciplinary teams—including patients, sponsors, sites, and contract research organizations (CROs)—collaborate in brainstorming sessions. The aim is to generate a wide array of recruitment strategies, challenging assumptions and exploring untapped possibilities without seeking a single "perfect solution" [78].
- Phase 3: Prototyping: While full-scale prototyping of a recruitment process may not be pragmatic, key elements that impact enrollment can be tested and refined. This includes simplifying complex protocol designs, creating shorter and more understandable informed consent forms, and testing digital engagement tools to reduce participant burden [78].
- Phase 4: Implementation: This phase involves rolling out the refined recruitment strategy. However, the process remains dynamic, with continuous monitoring and adaptation based on real-world enrollment data and ongoing patient feedback [78].
The following diagram illustrates this iterative, human-centered process:
Leveraging Technology and Multi-Channel Outreach
Advanced technologies are revolutionizing the speed and precision of patient identification.
- Artificial Intelligence (AI) and Machine Learning (ML): AI-driven algorithms can analyze vast datasets from electronic health records (EHRs) and real-world data to identify eligible patients with unprecedented speed and accuracy, significantly minimizing recruitment timelines [80] [81]. Machine learning can further predict patient responses and help personalize outreach [80].
- Digital and Social Media Outreach: Targeted digital campaigns on social media platforms, search engines, and online patient communities are essential for maximizing reach. A multi-channel approach ensures that potential participants are engaged through their preferred platforms [82].
- Decentralized Clinical Trials (DCTs): The adoption of decentralized or hybrid trial models, facilitated by telehealth and digital platforms, expands access to participants regardless of geography. This can dramatically increase the potential patient pool and improve diversity [78] [80]. One industry report notes that 81% of research sites are now using digital tools for patient recruitment [78].
The Imperative of Diversity and Inclusion
Achieving a diverse and representative participant pool is no longer optional; it is a scientific and regulatory priority. Diverse populations ensure that comparative efficacy findings are generalizable and applicable to all groups who will use the treatment [82]. Strategies to enhance diversity include:
- Community Engagement: Building strong partnerships with patient advocacy groups and community health organizations to foster trust and understanding within underrepresented communities [82].
- Broadened Eligibility Criteria: The National Cancer Institute (NCI) emphasizes that eligibility criteria must be as broad as safely possible to maximize opportunities for diverse populations [83].
- Addressing Logistical Barriers: Providing flexible participation options, travel reimbursements, and support for digital literacy to ensure that financial or logistical hurdles do not preclude participation [78] [82].
Strategies for Enhancing Patient Retention
Patient retention is critical to maintaining statistical power and the validity of study results. High dropout rates can compromise a trial's integrity.
Understanding Patient Motivations and Barriers
A 2025 U.S. patient survey revealed key insights into patient behavior. While older adults often remain motivated by altruism, younger adults are increasingly hesitant to participate, with misinformation cited as a major barrier [84]. Common retention challenges include:
- The burden of frequent site visits and complex procedures [78].
- Lack of ongoing communication and engagement from the research team.
- Concerns about treatment efficacy and side effects.
Proven Retention Techniques
- Minimize Patient Burden: Streamline protocols by eliminating "nice to have" procedures and simplify informed consent forms to be clear and concise [78]. Adopt decentralized trial elements, such as remote visits and wearable devices, to integrate the trial into the patient's life [80] [81].
- Foster Continuous Engagement: Maintain regular contact with participants through newsletters, check-in calls, and easy access to study staff. Transparency about trial progress and findings helps participants feel valued and invested [82].
- Provide Incentives and Support: Offer reasonable compensation for time and travel. Build a supportive community environment where patients can share experiences, which the 2025 survey indicates plays a critical role in their trial experience [84].
Streamlining Data Collection for Quality and Efficiency
Modern clinical trials often suffer from excessive data collection, which increases operational burden without always contributing to key study objectives [83]. A streamlined approach is essential.
Principles of Efficient Data Collection
The NCI's Modernizing Clinical Trials initiative advocates for limiting data collection in late-phase trials to elements that are essential for the primary and secondary objectives [83]. This focus reduces the burden on sites and patients, improves data quality, and lowers costs. The following framework outlines a strategic approach to data management:
Leveraging Technology and Standards
- Electronic Data Capture (EDC) Systems: High-quality EDC systems are fundamental for efficient data collection, storage, and analysis [79].
- Electronic Health Records (EHRs): Integrating with EHR systems can automate the collection of routine clinical data, reducing duplicate data entry and errors. NCI is piloting programs to standardize EHR use in trials to improve efficiency [83].
- Digital Health Technologies (DHTs): Wearables, sensors, and mobile health applications enable the continuous, real-world collection of efficacy and safety data directly from patients, providing a richer data set while minimizing site visits [80] [81].
- Industry-Wide Standardization: The adoption of common data elements and protocol templates drives consistency, simplifies technology setup, and enables seamless data flow between systems [81].
Quantitative Landscape of Clinical Trials
A clear understanding of costs and recruitment data is crucial for strategic planning and resource allocation. The following tables summarize key quantitative benchmarks.
| Trial Phase | Primary Purpose | Typical Participant Range | Average Cost Range (USD) | Key Cost Drivers |
|---|---|---|---|---|
| Phase I | Safety & Dosage | 20 - 100 | $1 - $4 million | Investigator fees, intensive safety monitoring, specialized PK/PD testing. |
| Phase II | Efficacy & Side Effects | 100 - 500 | $7 - $20 million | Increased participant numbers, longer duration, detailed endpoint analyses. |
| Phase III | Confirm Efficacy & Monitor ARs | 1,000+ | $20 - $100+ million | Large-scale recruitment, multiple sites, comprehensive data collection/analysis, regulatory submissions. |
| Phase IV | Long-Term Effects & Effectiveness | Varies widely | $1 - $50+ million | Long study durations, extensive follow-ups, monitoring rare side effects. |
Table 2: Patient Recruitment & Retention Metrics and Strategies
| Metric / Factor | Quantitative Benchmark / Method | Implementation Strategy |
|---|---|---|
| Trial Termination Rate | 19% of trials terminated due to poor recruitment [78]. | Implement design thinking in pre-trial planning to understand patient barriers [78]. |
| Recruitment Cost | Estimated $15,000 - $50,000 per patient in the U.S. [79]. | Use AI-powered screening to improve pre-screening efficiency and reduce screen-failure rates [80] [82]. |
| Digital Tool Adoption | 81% of sites use digital tools for recruitment [78]. | Deploy a multi-channel digital strategy (social media, online communities) combined with community partnerships [82]. |
| Key Retention Barrier | Misinformation, especially among younger adults [84]. | Proactive, clear communication and education; use of patient testimonials and simplified consent forms [82] [84]. |
The Scientist's Toolkit: Research Reagent Solutions
The following table details key technological and methodological "reagents" essential for implementing modern recruitment, retention, and data collection strategies.
Table 3: Essential Solutions for Modern Clinical Trial Operations
| Tool / Solution | Primary Function | Application in Comparative Efficacy Research |
|---|---|---|
| AI-Powered Patient Recruitment Platforms (e.g., Deep 6 AI) | Rapidly identify eligible patients by analyzing EHRs and other real-world data sources using natural language processing and machine learning [80]. | Accelerates the assembly of a representative study cohort for a comparative efficacy study, ensuring timely trial start-up. |
| Decentralized Clinical Trial (DCT) Platforms (e.g., Science 37, Medable) | Enable remote trial conduct through virtual visits, electronic consent, and direct-to-patient supply logistics [80]. | Reduces participant burden, improves retention, and allows for the collection of real-world efficacy data in a patient's natural environment. |
| Electronic Data Capture (EDC) Systems | Provide a structured, secure platform for clinical data collection and management at research sites [79]. | Ensures high-quality, audit-ready data collection that is essential for a robust comparison of drug safety and efficacy. |
| Digital Health Technologies (DHTs) | Collect continuous, objective physiological data (e.g., activity, heart rate) directly from patients via wearables and sensors [81]. | Provides granular, real-world efficacy and safety endpoints, complementing traditional clinic-based assessments. |
| Model-Informed Drug Development (MIDD) | Uses quantitative models (e.g., PBPK, ER analysis) to integrate prior knowledge and support development decisions [85]. | Can inform trial design, optimize dosing for comparative studies, and potentially reduce the need for extensive head-to-head clinical trials in certain cases [31]. |
Optimizing patient recruitment, retention, and data collection is an integrated endeavor that requires a shift from traditional, operational-focused methods to a strategic, patient-centric, and technology-driven paradigm. The approaches outlined in this whitepaper—rooted in design thinking, powered by advanced technology, and guided by the principle of efficiency—provide a roadmap for conducting more robust, conclusive, and timely comparative drug efficacy research. As regulatory standards evolve to embrace more efficient pathways [31], the adoption of these modernized strategies will be paramount for researchers and drug developers aiming to deliver effective new therapies to patients faster.
Validation, Interpretation, and Decision-Making from Comparative Evidence
Demonstrating that a new therapeutic biological product is highly similar to an already approved reference product is a complex scientific and regulatory endeavor. Central to this process is assessing the need for comparative efficacy studies (CES)—clinical trials designed to analyze and compare a clinical efficacy outcome between a proposed biosimilar and its reference product [86]. For over a decade, regulatory guidelines generally presumed that such studies would be necessary to support a demonstration of biosimilarity. However, a significant shift is now underway, moving away from this default requirement based on accumulated regulatory experience and advancements in analytical science [87] [31]. This whitepaper examines the evolving regulatory landscape and provides a technical framework for assessing when a CES is necessary, focusing on the critical role of comparative analytical assessment (CAA) in modern biosimilar development programs.
The Evolving Regulatory Framework for Biosimilarity
Historical Context and the Basis for Change
The Biologics Price Competition and Innovation Act (BPCI Act) of 2010 established an abbreviated licensure pathway for biosimilars under Section 351(k) of the Public Health Service Act [31]. This statute defines "biosimilarity" as meaning "that the biological product is highly similar to the reference product notwithstanding minor differences in clinically inactive components" and that "there are no clinically meaningful differences between the biological product and the reference product in terms of the safety, purity, and potency of the product" [31].
In 2015, the U.S. Food and Drug Administration (FDA) published its original "Scientific Considerations in Demonstrating Biosimilarity to a Reference Product" guidance, which emphasized that comparative clinical studies would generally be necessary unless sponsors could provide a scientific justification for their omission [31]. This conservative approach reflected the limited regulatory experience with biosimilars at that time.
The 2025 Policy Shift: A Streamlined Approach
In October 2025, the FDA issued a draft guidance representing a substantial evolution in its regulatory thinking. Titled "Scientific Considerations in Demonstrating Biosimilarity to a Reference Product: Updated Recommendations for Assessing the Need for Comparative Efficacy Studies," this document proposes that for many therapeutic protein products, CES may not be needed to support a demonstration of biosimilarity [30] [87] [86]. The guidance outlines specific conditions under which sponsors may rely primarily on comparative analytical assessments instead of clinical efficacy studies.
This policy shift is grounded in two key developments:
- Regulatory Experience: The FDA has now approved 76 biosimilars, providing a substantial body of evidence supporting the reliability of analytical methodologies for detecting clinically meaningful differences [31].
- Analytical Advancements: Modern analytical technologies now provide exceptional specificity and sensitivity for structural characterization of purified proteins and modeling of in vivo functions [87] [31]. A CAA is now generally recognized as more sensitive than a CES in detecting differences between a biosimilar and its reference product [86].
The economic impetus for this change is significant. CES are resource-intensive, typically requiring enrollment of 400-600 subjects at an average cost of $25 million per trial and often delaying product approval by up to three years [31]. Their elimination in appropriate cases is expected to accelerate biosimilar development, increase market competition, and ultimately reduce drug costs, particularly for advanced treatments for cancer, autoimmune diseases, and rare disorders [87] [88].
Figure 1: Regulatory Evolution in Biosimilar Development Pathway
Scientific Considerations for Waiving Comparative Efficacy Studies
Conditions for Waiving CES
The updated draft guidance specifies that a CES may not be necessary when the following three conditions are satisfied [87] [88]:
- Manufacturing and Characterization: The reference product and proposed biosimilar product are manufactured from clonal cell lines, are highly purified, and can be well-characterized analytically.
- Understanding of Quality Attributes: The relationship between quality attributes (e.g., protein structure, physiochemical, and functional attributes) and clinical efficacy is generally understood for the reference product, and these attributes can be evaluated by assays included in the CAA.
- Pharmacokinetic Study Feasibility: A human pharmacokinetic (PK) similarity study is feasible and clinically relevant.
When these conditions are met and a comprehensive CAA demonstrates high similarity, the FDA indicates that an appropriately designed human PK similarity study and an assessment of immunogenicity may be sufficient to meet the statutory standard for biosimilarity [88].
The Primacy of Comparative Analytical Assessment
The updated framework places CAA at the center of the biosimilarity demonstration. A rigorous CAA evaluates critical quality attributes across multiple domains [87]:
- Primary Structure: Amino acid sequence, post-translational modifications (e.g., glycosylation patterns)
- Higher-Order Structure: Secondary, tertiary, and quaternary protein structure
- Physicochemical Properties: Molecular weight, isoform pattern, extinction coefficient, electrophoretic profiles
- Biological Activity: Functional assays measuring mechanism of action and potency
The sensitivity of modern analytical technologies—including mass spectrometry, nuclear magnetic resonance, circular dichroism, and surface plasmon resonance—now enables detection of structural and functional differences at a resolution that often exceeds the sensitivity of clinical trials to detect clinically meaningful differences [87] [88].
Table 1: Key Analytical Technologies for Biosimilarity Assessment
| Technology Category | Specific Methodologies | Attributes Assessed |
|---|---|---|
| Structural Analysis | Mass Spectrometry, Chromatography, Electrophoresis | Primary structure, post-translational modifications, molecular weight |
| Higher-Order Structure | Circular Dichroism, NMR, X-ray Crystallography | Secondary/tertiary structure, conformational integrity |
| Functional Analysis | Cell-based assays, Binding assays, Enzyme kinetics | Biological activity, mechanism of action, receptor binding |
| Immunochemical Properties | ELISA, Western Blot, Immunoassays | Antigenic properties, epitope mapping |
Methodological Framework for Biosimilarity Assessment
Tiered Approach to Analytical Similarity
A systematic, tiered approach should be employed for the CAA, with quality attributes categorized based on their potential impact on clinical performance:
- Critical Attributes: Those with a known or potential impact on clinical activity, safety, or immunogenicity. These require side-by-side comparison with the reference product with tight equivalence margins.
- Non-Critical Attributes: Those with little or no known impact on clinical performance. These require qualitative or quantitative similarity assessment.
This risk-based approach ensures appropriate statistical rigor is applied where it matters most for clinical performance.
Pharmacokinetic and Immunogenicity Assessments
When a CES is waived, the human PK study and immunogenicity assessment carry increased importance in the biosimilarity demonstration:
- PK Study Design: Should be a comparative, single-dose crossover or parallel-design study in a homogeneous population (often healthy volunteers) using a sensitive population and relevant dose [88].
- Immunogenicity Assessment: Should include adequate comparative data to address potential differences in immune response, which may include assessment in non-clinical models and/or clinical studies, depending on the product characteristics and reference product experience [88].
Figure 2: Decision Framework for Comparative Efficacy Studies
Quantitative Impact of Regulatory Change
The elimination of CES requirements represents a substantial reduction in the time and cost associated with biosimilar development. The following table quantifies the expected impact based on historical development programs.
Table 2: Quantitative Impact of Removing Comparative Efficacy Study Requirements
| Development Component | Traditional Approach (with CES) | Streamlined Approach (without CES) | Reduction |
|---|---|---|---|
| Clinical Trial Duration | Up to 3 years [31] | Not applicable | ~3 years |
| Average Patient Enrollment | 400-600 subjects [31] | Reduced number for PK study | ~400-500 subjects |
| Direct Financial Cost | ~$25 million per trial [31] | Significant portion eliminated | ~$25 million |
| Total Development Timeline | 5-7 years (estimated) | 2-4 years (estimated) | ~3 years |
The Scientist's Toolkit: Essential Reagents and Materials
A robust biosimilarity assessment program requires specific research reagents and analytical tools to conduct the necessary comparative analyses.
Table 3: Essential Research Reagents and Materials for Biosimilarity Assessment
| Reagent/Material | Function in Biosimilarity Assessment |
|---|---|
| Reference Product | Serves as the benchmark for all comparative assessments; multiple lots should be tested to understand inherent variability [87]. |
| Clonal Cell Lines | Well-characterized production system ensuring consistent manufacturing of the proposed biosimilar [88]. |
| Characterization Assays | Suite of analytical methods (e.g., MS, HPLC, CD) to compare primary/higher-order structure and function [87]. |
| Biological Activity Assays | Cell-based or biochemical assays to demonstrate similar mechanism of action and potency relative to reference product. |
| Positive/Negative Controls | Qualified system suitability controls to ensure analytical methods can detect relevant differences. |
The regulatory landscape for demonstrating biosimilarity is evolving toward a more efficient, science-driven paradigm that recognizes the superior sensitivity of modern analytical methods compared to clinical efficacy studies for detecting product differences. The FDA's 2025 draft guidance formalizes this shift, establishing specific conditions under which CES may be waived in favor of rigorous comparative analytical assessment coupled with pharmacokinetic and immunogenicity studies. This streamlined approach is expected to accelerate biosimilar development, reduce costs, and ultimately enhance patient access to critical biological medicines. As analytical technologies continue to advance, the scientific framework for biosimilarity assessment will likely continue to evolve, further refining the standards for demonstrating biosimilarity without unnecessary clinical studies.
In comparative drug efficacy research, the ability to accurately interpret results is paramount for making informed decisions that impact public health and therapeutic guidelines. This process hinges on a clear understanding of three core concepts: confidence intervals, which estimate the range of plausible values for a population parameter; uncertainty, which encompasses the limitations inherent in any study's evidence; and clinical significance, which assesses whether a observed effect is meaningful in real-world patient care. Within the framework of comparative effectiveness research (CER), defined as "the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition," the interplay of these concepts guides conclusions about which treatment works best, for whom, and under what circumstances [89]. This guide provides researchers, scientists, and drug development professionals with the technical foundation and practical methodologies for rigorously interpreting study results to support valid, evidence-based conclusions.
Confidence Intervals: Estimation and Interpretation
Core Concept and Calculation
A confidence interval (CI) provides a range of values that is likely to contain the true population parameter of interest. This interval is calculated from sample data and is constructed at a specified confidence level, typically 95%. The general formula for a CI takes the form: CI = Point estimate ± Margin of error, where the margin of error is the product of a critical value derived from the standard normal curve and the standard error of the point estimate [90]. The correct interpretation of a 95% CI is that if we were to repeat the same study over and over with random samples from the same population, we would expect 95% of the calculated intervals to contain the true population parameter [91] [90].
The calculation varies based on the type of data. For a sample mean, the CI is calculated as Sample mean ± z × (Standard deviation/√n), where 'z' is the critical value (e.g., 1.96 for 95% confidence) [90]. For a proportion, the formula is p ± z × √[p(1-p)/n], where 'p' is the sample proportion [90]. The factors affecting the width of the CI include the chosen confidence level (e.g., a 99% CI is wider than a 95% CI), the sample size (larger samples yield narrower CIs), and the variability in the data (less variability results in narrower CIs) [90].
Workflow for Interpreting Confidence Intervals in Efficacy Research
The following diagram illustrates the systematic workflow for interpreting confidence intervals in the context of drug efficacy research.
Practical Application and Examples
Consider a randomized controlled trial comparing a new drug to a standard therapy, with the primary outcome being the reduction in systolic blood pressure. The new drug shows a mean reduction of 10 mmHg with a 95% CI of [7.0, 13.0] mmHg. This result would be interpreted as follows: we are 95% confident that the true mean reduction in systolic blood pressure in the population lies between 7.0 and 13.0 mmHg [91]. Since the entire interval is above zero (a pre-specified minimal important difference), it indicates a statistically significant effect favoring the new drug.
Another example involves binary outcomes. A study might report an odds ratio (OR) for treatment success of 1.50 with a 95% CI of [1.20, 1.85]. The point estimate (1.50) suggests the odds of success are 50% higher with the new treatment. The 95% CI, which does not include 1.0 (the null value), indicates that this result is statistically significant at the 5% level. Furthermore, the lower bound (1.20) provides assurance that even the smallest plausible effect is still clinically meaningful [90].
Uncertainty in Clinical Research and Drug Development
Uncertainty is an inherent component of clinical research, arising from multiple sources throughout the drug development lifecycle. The benefit-risk assessment of a pharmaceutical product is dynamic, as the information itself changes over time [92]. Several distinct but interrelated dimensions of uncertainty contribute to the complexity of interpreting study results.
Table: Key Dimensions of Uncertainty in Drug Benefit-Risk Assessment
| Dimension of Uncertainty | Description | Primary Impact |
|---|---|---|
| Clinical Uncertainty | Arises from biological variables (age, genetics, comorbidities) and trial design limitations (short duration for chronic conditions). | Reduces generalizability of RCT results to real-world populations. |
| Methodological Uncertainty | Stems from constraints of RCT designs and differences between pre-market trials and post-market observational studies. | Affects the validity of combining evidence from different study types. |
| Statistical Uncertainty | Introduced by sampling error; clinical trials are designed to show efficacy but not necessarily to fully quantify benefits and risks. | Quantified by confidence intervals and p-values; inherent in any sample-based study. |
| Operational Uncertainty | Includes challenges in postmarket study participation and the lack of established "threshold of risk tolerance" among stakeholders. | Hinders longitudinal data collection and consensus on risk acceptability. |
Statistical uncertainty, quantified by measures such as 95% confidence intervals, addresses the component of uncertainty introduced by chance [92]. However, other dimensions like bias (e.g., confounding, time-related biases, surveillance bias) affect the internal validity of a study, while representativeness affects its external validity [92]. These uncertainties are often compounded in the post-market phase when real-world evidence from observational studies must be integrated with pre-market clinical trial data.
Methodologies for Addressing and Reducing Uncertainty
Several methodological approaches can be employed to reduce uncertainty in clinical research. For addressing chance, the calculation of 95% confidence intervals is a fundamental tool [92]. To mitigate bias, researchers can employ various design and analytic strategies, including the use of negative control outcomes, emulation of trial populations, extensive adjustment procedures, bias modeling, and sensitivity analyses [92]. Representativeness, which affects external validity, can be partially addressed in RCTs through the evaluation of subgroups [92].
A systematic approach to uncertainty reduction involves combining results from studies with different designs and data sources. As noted by Schneeweiss, "a benefit–risk assessment should include evidence from multiple study types with different data sources, intelligently arranged to maximize information available to a decision maker while complementing each study's methodological weaknesses" [92]. This approach can include randomized controlled trials, which are typically the source for information about efficacy, and large observational claims data studies, which are typically the source for information about adverse events in real-world populations [92]. Furthermore, wide public registration of clinical trials, including results and key protocol details, supports the best possible evidence-based decision making by reducing publication bias and improving transparency [92].
Clinical Significance vs. Statistical Significance
Defining the Distinction
In clinical research, it is crucial to differentiate between statistical significance and clinical significance. Statistical significance, often determined by a p-value of less than 0.05 or a confidence interval that excludes the null value, indicates that an observed effect is unlikely to be due to chance alone [93]. Clinical significance, conversely, answers whether the observed effect is meaningful for patients and clinicians in practical, real-world settings [93]. A result can be statistically significant but not clinically significant, particularly in studies with large sample sizes where very small, trivial effects can achieve statistical significance.
Clinical significance is determined by whether a treatment has a "real, noticeable effect for patients using it" [93]. The criteria for clinical significance are not universal and must be defined by researchers and clinicians based on the clinical context. For some conditions, this might be the percentage of patients who achieve a cure; for others, it might be a specific reduction in symptom severity or an improvement in quality of life [93]. For instance, a reduction in HbA1c of 0.1% might be statistically significant in a large trial but would not be considered clinically significant in diabetes management, whereas a reduction of 0.5% or more typically would be.
A Five-Step Procedure for Integrated Assessment
To increase the validity of intervention effect assessments in randomized clinical trials, a rigorous five-step procedure has been proposed that moves beyond reliance on single thresholds [94]:
- Report confidence intervals and exact P-values: This provides a more complete picture of the statistical evidence, with the CI explicitly demonstrating the range of uncertainty around the effect estimate [94].
- Report Bayes factor for the primary outcome: Bayes factor is the ratio of the probability of the data under the null hypothesis to the probability under the alternative hypothesis. It helps relate new trial results to prior evidence, compensating for a deficiency of the P-value [94].
- Adjust for interim analyses: If a trial is stopped early or interim analyses have been conducted, adjustments to the confidence intervals and significance thresholds are necessary to maintain statistical integrity [94].
- Adjust for multiplicity: Corrections to confidence intervals and P-values are required when multiple outcome comparisons are performed to avoid inflation of the type I error rate [94].
- Assess clinical significance: The final step involves a formal evaluation of whether the observed effect size is clinically meaningful, considering the predefined thresholds for clinical importance [94].
This procedure ensures that both the statistical reliability and the practical relevance of trial results are thoroughly evaluated.
Methodologies for Comparative Efficacy Research
Study Designs and Analytical Approaches
Comparative Effectiveness Research (CER) employs a variety of methods to compare the benefits and harms of alternative interventions [89]. The choice of method depends on the research question, available resources, and ethical considerations.
Table: Common Methods in Comparative Effectiveness Research
| Method | Description | Strengths | Limitations |
|---|---|---|---|
| Systematic Review | A critical assessment and evaluation of all research studies addressing a particular clinical issue using specific criteria. | Provides a comprehensive summary of existing literature; can include meta-analysis for quantitative pooling. | Quality depends on available primary studies; potential for publication bias. |
| Randomized Controlled Trial (RCT) | Participants are randomly assigned to two or more groups differing only in the intervention. | Considered the gold standard; minimizes confounding through randomization. | Can be expensive, time-consuming; may have limited generalizability. |
| Observational Study | Participants are not randomized; choice of treatments is made by patients and physicians. Can be prospective or retrospective. | Faster, more cost-efficient; suitable for studying rare diseases and real-world effectiveness. | Prone to selection bias and confounding; data quality may be variable. |
Indirect Comparison Methods
In the absence of head-to-head clinical trials, indirect statistical methods are often used to compare the efficacy of drugs. These methods vary in their complexity and acceptance.
- Naïve Direct Comparison: This inappropriate method directly compares results for one drug from one trial with results for another drug from a separate trial without adjustment for differences in trial designs or populations. It "breaks" the original randomization and is subject to significant confounding and bias [21].
- Adjusted Indirect Comparison: This accepted method preserves randomization by comparing two treatments (A and B) via a common comparator (C). The difference between A and B is estimated by comparing the difference between A and C with the difference between B and C [21]. This method is accepted by many drug reimbursement agencies but comes with increased statistical uncertainty, as the uncertainties of the individual component studies are summed [21].
- Mixed Treatment Comparisons (MTC): These advanced Bayesian statistical models incorporate all available data for a drug, including data not directly relevant to the comparator drug. MTCs can reduce uncertainty but have not yet been widely accepted by researchers and regulatory authorities [21].
The following diagram outlines the decision process for selecting an appropriate comparative efficacy research methodology based on the available evidence and research question.
Essential Research Reagents and Tools
Table: Key Analytical Tools for Addressing Uncertainty and Confounding
| Tool | Category | Primary Function | Application Context |
|---|---|---|---|
| Risk Adjustment Models | Statistical Model | Calibrates payments or identifies similar patients by predicting costs/outcomes based on claims/clinical data. | Observational studies; correcting for selection bias in non-randomized data. |
| Propensity Score Matching | Statistical Method | Balances treatment and control groups by matching patients with similar probabilities of receiving treatment. | Retrospective observational studies; mitigating confounding by indication. |
| Bayes Factor | Statistical Metric | Quantifies evidence for one hypothesis over another (e.g., alternative vs. null). | Supplemental to p-value; provides a continuous measure of evidence strength. |
| Systematic Review Software | Research Software | Facilitates the systematic collection, management, and analysis of literature for meta-synthesis. | Conducting systematic reviews and meta-analyses. |
| Indirect Comparison Software | Research Software | Performs adjusted indirect comparisons and mixed treatment comparisons. | Comparing interventions when head-to-head trials are lacking. |
The rigorous interpretation of confidence intervals, a comprehensive understanding of the dimensions of uncertainty, and the clear distinction between statistical and clinical significance are foundational to robust comparative drug efficacy research. By applying structured methodologies—including the five-step procedure for trial assessment, appropriate indirect comparison techniques when direct evidence is absent, and analytical tools like risk adjustment and propensity scores—researchers can generate more valid and reliable evidence. This evidence is critical for informing decisions made by clinicians, patients, policymakers, and purchasers, ultimately leading to improved health care at both the individual and population levels. As the field evolves, the intelligent integration of evidence from multiple study designs will continue to be paramount in reducing uncertainty and clarifying the true benefits and harms of therapeutic interventions.
Comparative effectiveness research (CER) is a cornerstone of modern therapeutic development, providing critical evidence for evaluating the relative benefits and risks of medical interventions. Framed within the broader thesis of establishing robust guidelines for comparative drug efficacy research, this technical guide examines its practical application through two complex therapeutic areas: diabetes and oncology. These fields exemplify the challenges and advanced methodologies inherent in head-to-head drug comparisons, where treatment decisions balance efficacy, safety, long-term outcomes, and patient-specific factors. The imperative for rigorous CER is underscored by the low overall success rate in drug development, recently reported at 6.2% from phase I to approval [95], highlighting the critical need for data-driven decision-making to lower attrition and optimize resource allocation. This whitepaper details the experimental protocols, data synthesis techniques, and visualization tools essential for generating high-quality comparative evidence to guide clinical practice and drug development.
Comparative Research in Diabetes Therapeutics
Case Study: Post-Transplant Diabetes Mellitus (PTDM) Network Meta-Analysis
2.1.1 Research Objective and Context Post-transplant diabetes mellitus (PTDM) is a serious complication following kidney transplantation, with an incidence ranging from 2% to 53%, adversely affecting both graft survival and patient outcomes [96]. Managing PTDM is complicated by the diabetogenic effects of immunosuppressive regimens and the need to avoid drug interactions. This creates an ideal context for applying advanced CER methodologies to determine the optimal antidiabetic agent in this specialized population.
2.1.2 Experimental Protocol for Network Meta-Analysis A network meta-analysis (NMA) protocol was implemented to simultaneously compare multiple antidiabetic interventions where few direct head-to-head trials exist [96].
- Literature Search Strategy: A systematic search was performed across PubMed, Web of Science, Embase, and Cochrane Library from inception through April 2025. The search used Boolean operators to combine keywords and Medical Subject Headings (MeSH) related to "kidney transplantation," "post-transplant diabetes," and "antidiabetic agents." The search string was:
("kidney transplantation" OR "renal transplant") AND ("new-onset diabetes" OR "post-transplant diabetes") AND ("antidiabetic agents" OR "hypoglycemic drugs" OR "glucose-lowering therapies"). - Eligibility Criteria (PICOS):
- Population: Adult kidney transplant recipients with PTDM.
- Intervention/Comparator: Any pharmacological antidiabetic treatment (e.g., insulin, SGLT2 inhibitors, DPP-4 inhibitors, GLP-1 receptor agonists, sulfonylureas) compared against another active therapy, placebo, or standard care.
- Outcomes: Primary efficacy outcomes included change in HbA1c and fasting plasma glucose (FPG). Safety outcomes included major adverse cardiovascular and kidney events (MACE and MAKE).
- Study Design: Randomized controlled trials (RCTs) and cohort studies.
- Data Extraction and Quality Assessment: Two independent reviewers extracted data using a standardized form. The Cochrane Risk of Bias tool was applied to assess methodological quality. Disagreements were resolved by a third independent adjudicator.
- Statistical Analysis: A frequentist NMA model was employed to synthesize direct and indirect evidence. Heterogeneity was assessed using the I² statistic. Treatment rankings were established using Surface Under the Cumulative Ranking Curve (SUCRA) probabilities. Contribution plots and comparison-adjusted funnel plots were generated to evaluate study influence and publication bias, respectively. Analyses were performed using Stata software.
2.1.3 Quantitative Findings from PTDM Analysis The NMA synthesized evidence from 12 studies (10 RCTs, 2 cohort studies) encompassing 7,372 patients [96]. The table below summarizes the key efficacy and safety findings.
Table 1: Comparative Efficacy and Safety of Antidiabetic Agents in PTDM (vs. Placebo) [96]
| Intervention | HbA1c Reduction (MD, 95% CI) | FPG Reduction (MD, 95% CI) | SBP Reduction (MD, 95% CI) | MACE/MAKE Risk (MD, 95% CI) |
|---|---|---|---|---|
| Insulin | -0.35% (-0.90 to 0.20) | -9.06 mmol/L (-18.66 to 0.53) | -1.95 mmHg (-5.16 to 1.26) | -1.50 (-4.10 to 1.10) |
| SGLT2 Inhibitors | -0.28% (-0.74 to 0.18) | -7.12 mmol/L (-15.98 to 1.74) | -2.12 mmHg (-5.42 to 1.18) | -1.95 (-4.85 to 0.96) |
| DPP-4 Inhibitors | -0.20% (-0.70 to 0.30) | -5.01 mmol/L (-14.89 to 4.87) | -3.57 mmHg (-7.29 to 0.16) | -1.10 (-3.90 to 1.70) |
| Sulfonylureas | -0.15% (-0.65 to 0.35) | -4.12 mmol/L (-14.00 to 5.76) | -1.01 mmHg (-4.73 to 2.71) | -0.85 (-3.65 to 1.95) |
MD: Mean Difference; CI: Confidence Interval; FPG: Fasting Plasma Glucose; SBP: Systolic Blood Pressure
2.1.4 Research Reagent Solutions for Diabetes CER The following tools and data sources are critical for conducting high-quality CER in diabetes.
Table 2: Essential Research Reagents and Tools for Diabetes CER
| Reagent/Solution | Function in Comparative Research |
|---|---|
| Network Meta-Analysis Software (Stata, R) | Statistical software packages with NMA routines to synthesize direct and indirect evidence from multiple trials. |
| Electronic Data Capture (EDC) Systems | Secure, compliant systems (e.g., from Oracle or Medidata) for collecting high-quality, standardized patient data across clinical sites [97]. |
| Continuous Glucose Monitors (CGM) | Devices (e.g., Dexcom G6) that provide dense, real-world glycemic data (e.g., time-in-range, glycemic variability) for more nuanced efficacy endpoints [98]. |
| Clinical Trial Management Systems (CTMS) | Operational systems for tracking site performance, enrollment, and query resolution, which are vital for trial quality and data integrity [97]. |
| Data Visualization Platforms (e.g., Tableau, Power BI) | Platforms used to create interactive dashboards for ongoing data review, safety signal detection, and enrollment tracking, facilitating proactive trial management [99] [97]. |
2.1.5 Visualizing the PTDM Network Meta-Analysis Workflow The following diagram outlines the sequential protocol for conducting a network meta-analysis, as applied in the PTDM case study.
Comparative Research in Oncology Therapeutics
Case Study: Tislelizumab vs. Chemotherapy in Lung Cancer
3.1.1 Research Objective and Context Lung cancer is a leading cause of cancer-related mortality worldwide. Tislelizumab is an anti-PD-1 monoclonal antibody engineered to minimize FcγR binding, potentially overcoming resistance mechanisms common to other immunotherapies [100]. This case study applies a systematic review and meta-analysis to evaluate the comparative efficacy and safety of Tislelizumab-based regimens versus chemotherapy alone.
3.1.2 Experimental Protocol for Systematic Review and Meta-Analysis The meta-analysis adhered to PRISMA guidelines and was registered in PROSPERO (CRD42025641055) [100].
- Literature Search Strategy: A comprehensive search was conducted across PubMed, Embase, Scopus, Cochrane Library, ScienceDirect, and ClinicalTrials.gov until February 2025. The strategy used MeSH and free-text terms like "Lung Neoplasm," "Tislelizumab," and "Chemotherapy" combined with Boolean operators.
- Eligibility Criteria (PICOS):
- Population: Patients with lung cancer.
- Intervention: Tislelizumab with or without chemotherapy.
- Comparator: Chemotherapy alone.
- Outcomes: Primary outcomes included Progression-Free Survival (PFS), Overall Survival (OS), Objective Response Rate (ORR), and Adverse Events (AEs).
- Study Design: Only RCTs were included.
- Data Extraction and Quality Assessment: Two reviewers independently extracted data into a pre-piloted spreadsheet. The risk of bias was assessed using the Cochrane RoB 1.0 tool.
- Statistical Analysis: A random-effects model was used to pool data. Hazard Ratios (HRs) were calculated for time-to-event outcomes (PFS, OS), and Risk Ratios (RRs) for dichotomous outcomes (ORR, AEs). Heterogeneity was assessed via the I² statistic. Publication bias was evaluated using funnel plots and Egger's test.
3.1.3 Quantitative Findings from Oncology Meta-Analysis The analysis included 6 RCTs involving 2,148 patients [100]. The results demonstrated clear superiority of Tislelizumab-based regimens over chemotherapy.
Table 3: Comparative Efficacy and Safety of Tislelizumab in Lung Cancer [100]
| Outcome Measure | Effect Estimate (Tislelizumab vs. Chemotherapy) | P-value | Statistical Significance |
|---|---|---|---|
| Progression-Free Survival (PFS) | HR = 0.62 | p < 0.0001 | Yes |
| Overall Survival (OS) | HR = 0.69 | p < 0.0001 | Yes |
| Objective Response Rate (ORR) | RR = 1.49 | p = 0.0001 | Yes |
| Disease Control Rate (DCR) | RR = 1.49 | p = 0.0010 | Yes |
| All-Cause Mortality | RR = 0.89 | p = 0.0003 | Yes |
| Any Adverse Events (AEs) | RR = 1.00 | p = 0.75 | No |
| ALT Elevation | RR = 1.36 (95% CI: 1.13–1.64) | N/A | Yes |
| AST Elevation | RR = 1.77 (95% CI: 1.17–2.67) | N/A | Yes |
HR: Hazard Ratio; RR: Risk Ratio; CI: Confidence Interval
3.1.4 Research Reagent Solutions for Oncology CER The following tools are essential for conducting robust comparative research in oncology.
Table 4: Essential Research Reagents and Tools for Oncology CER
| Reagent/Solution | Function in Comparative Research |
|---|---|
| Anti-PD-1 Monoclonal Antibodies | Key therapeutic class for immunotherapy; includes Tislelizumab, Nivolumab, Pembrolizumab used as interventions in trials [100]. |
| RECIST 1.1 Criteria | Standardized protocol for measuring tumor burden and defining objective endpoints like ORR, PFS, and DCR in solid tumor trials. |
| Cochrane Collaboration Tools | Methodological tools (e.g., RoB 1.0) for assessing the risk of bias in included RCTs, ensuring quality assessment in meta-analyses [100]. |
| Statistical Software (R, Stata) | Software with advanced packages for survival analysis (Cox models), random-effects meta-analysis, and generation of forest and funnel plots. |
| Project Management & Analytics | Platforms like Smartsheet and Tableau are used for tracking study progress and creating safety dashboards for real-time data review [99] [97]. |
3.1.5 Visualizing the Oncology Meta-Analysis Workflow The following diagram illustrates the rigorous process of a systematic review and meta-analysis for evaluating an oncology therapy.
Cross-Disciplinary Analysis and Guidelines for Research
Synthesis of Methodological Approaches
A comparative analysis of the two case studies reveals a shared foundation of rigorous methodology essential for reliable CER, while also highlighting distinct considerations tailored to each disease area.
- Unified Foundational Protocols: Both the NMA in diabetes and the pairwise meta-analysis in oncology relied on pre-registered protocols, systematic literature searches, dual independent data extraction, and standardized risk-of-bias assessments. These steps are non-negotiable for minimizing bias and ensuring reproducibility in CER [96] [100].
- Tailored Outcome Measures: The choice of primary endpoints differed appropriately. The diabetes study prioritized continuous laboratory measures of glycemic control (HbA1c, FPG) and organ-specific composite events (MACE/MAKE). The oncology study focused on time-to-event survival metrics (PFS, OS) and tumor response criteria (ORR), reflecting the distinct clinical priorities in chronic disease versus oncologic efficacy [96] [100].
- Advanced Data Handling and Visualization: In both fields, moving beyond spreadsheet-based reporting to integrated data visualization platforms (e.g., Tableau, Microsoft Power BI) is critical. These tools provide clinical project teams with interactive dashboards for real-time monitoring of study metrics, enrollment, and safety signals, enabling proactive decision-making and risk-based monitoring as advocated by FDA guidance [99] [97].
Visualizing the CER Guideline Framework
The following diagram synthesizes the core principles from both case studies into a generalized workflow for conducting comparative drug efficacy research, forming the basis for broader research guidelines.
The Scientist's Toolkit for Comparative Research
This table consolidates the key methodological and technological resources required to execute the CER guidelines outlined above.
Table 5: The Scientist's Toolkit for Comparative Efficacy Research
| Tool Category | Specific Examples | Role in CER Guidelines |
|---|---|---|
| Methodological Frameworks | PRISMA, PICOS, Cochrane Handbook | Provide standardized protocols for designing, reporting, and assessing systematic reviews and clinical trials. |
| Statistical Software & Models | R, Stata, Random-Effects Models, NMA Models | Enable robust statistical synthesis of data, handling of heterogeneity, and comparison of multiple treatments. |
| Data Visualization & Analytics | Tableau, Microsoft Power BI | Facilitate risk-based monitoring, interactive data exploration, and clear communication of complex results to stakeholders [99] [97]. |
| Clinical Outcome Assessments | HbA1c, MACE/MAKE, RECIST 1.1, PFS/OS | Provide validated, clinically relevant endpoints tailored to the therapeutic area for consistent efficacy evaluation. |
| Operational Data Systems | CTMS, EDC Systems (e.g., Medidata) | Ensure data integrity, streamline site management, and provide the clean, centralized data required for analysis [97]. |
Within the rapidly evolving landscape of comparative drug efficacy research, indirect treatment comparisons (ITCs) have emerged as crucial methodologies when head-to-head randomized controlled trials are ethically or practically challenging. The dynamic treatment landscape and the pressing need for timely clinical decision-making have accelerated the adoption of these techniques globally [27]. This framework provides a structured approach for researchers, scientists, and drug development professionals to critically appraise the quality of indirect comparisons, ensuring their appropriate application in healthcare decision-making. As numerous ITC guidelines have been published by various authorities worldwide, with many updated within the last five years, the need for standardized critical appraisal has never been more pronounced [27].
Foundational Concepts of Indirect Comparisons
Indirect treatment comparisons encompass analytical techniques used to compare interventions that have not been studied directly against each other in clinical trials. These methods are typically justified by the absence of direct comparative studies, which remains the primary rationale for their use across most jurisdictions [27]. The fundamental principle involves establishing comparison through common comparators, typically placebos or standard treatments, creating connected networks of evidence.
The methodology for ITCs has continued to evolve, with many contemporary guidelines now incorporating more complex techniques beyond basic approaches [27]. The suitability and subsequent acceptability of any specific ITC technique depends on multiple factors, including available data sources, the evidence base, and the magnitude of benefit or uncertainty [27]. Understanding these foundational concepts is essential for proper appraisal of ITC applications in comparative drug efficacy research.
Critical Appraisal Framework Structure
A robust critical appraisal framework for indirect comparisons should systematically evaluate whether a study addresses a clearly focused question, employs valid methods to address this question, produces important results, and provides findings applicable to specific patients or populations [101]. Structured checklists facilitate this assessment by ensuring consistent evaluation of key issues in indirect comparisons.
The validated checklist for critical appraisal of indirect comparisons consists of two primary components [102]:
Eliminatory Key Questions
- First Component: Three initial screening questions that determine whether further appraisal is warranted
- Gatekeeping Function: Studies failing these fundamental questions may not merit detailed methodological review
Detailed Assessment Domains
- Quality Domain: 5 items evaluating overall study rigor and reliability
- Clinical Domain: 5 items assessing clinical relevance and applicability
- Methodology/Statistics Domain: 7 items examining analytical approaches and statistical validity
Validation studies of this checklist demonstrated good inter-rater agreement for quality (median kappa = 0.83) and clinical items (median kappa = 0.61), though agreement was weaker for methodology/statistics items (median kappa = 0.36), highlighting the complexity of statistical assessment in ITCs [102].
Detailed Appraisal Criteria
Clinical Relevance Assessment
The clinical dimension of appraisal ensures that indirect comparisons address meaningful clinical questions and produce applicable results. Appraisers should evaluate whether the research question addresses critical decisional dilemmas faced by patients, families, caregivers, and clinicians [103]. The compared interventions should have robust efficacy evidence or documented widespread use if efficacy is not well established [103].
Additional clinical considerations include:
- Patient-centered outcomes: Research should measure outcomes that matter to patients, including quality of life, functional status, and adverse effects [104]
- Clinical heterogeneity: Variations in patient populations, comorbidities, and treatment modalities across studies should be clinically justifiable
- Decision-making relevance: Results should provide clear guidance for clinical practice or policy decisions
Methodological and Statistical Rigor
Methodological appraisal focuses on the technical execution of indirect comparisons. Most jurisdictions favor population-adjusted or anchored ITC techniques over naive comparisons, as the latter produce outcomes that are difficult to interpret and prone to confounding bias [27]. The specific analytical approach should be justified based on available evidence and data sources.
Key methodological considerations include:
- Study design alignment: The identified study design must be appropriately applied to answer the research question [105]
- Evidence network structure: The connectedness and homogeneity of the treatment network should be evaluated
- Statistical methods: Appropriate techniques for population adjustment, handling of multi-arm trials, and accounting for effect modifiers should be employed
- Heterogeneity assessment: Variability between studies should be quantified and addressed methodologically
Quality and Transparency Evaluation
Quality assessment ensures the reliability and credibility of indirect comparison results. Controls and governance over ITC methodology and reporting have been introduced specifically to minimize bias and ensure scientific credibility and transparency in healthcare decision making [27].
Critical quality indicators include:
- Protocol registration: Pre-specified analysis plans reduce selective reporting
- Comprehensive reporting: All methodological choices, assumptions, and uncertainties should be transparently documented
- Sensitivity analyses: Robustness of results to different assumptions should be tested
- Conflict of interest disclosure: Study sponsorship and potential conflicts should be clearly disclosed [104]
Table 1: Primary Domains for Critical Appraisal of Indirect Comparisons
| Domain | Key Components | Appraisal Focus |
|---|---|---|
| Clinical Relevance | Research question formulation, outcome selection, population applicability | Meaningfulness of the clinical question and applicability to decision-making |
| Methodological Rigor | Study design, evidence network, analytical approach, heterogeneity handling | Technical soundness of the comparative approach |
| Statistical Validity | Model specification, uncertainty quantification, assumption verification | Appropriateness of statistical methods and reliability of estimates |
| Quality & Transparency | Protocol registration, reporting completeness, sensitivity analyses, conflict disclosure | Overall study reliability and freedom from bias |
Experimental Protocols for Indirect Comparisons
Feasibility Assessment Protocol
The feasibility phase represents a distinct initial stage in comparative effectiveness research that supports study refinement, infrastructure establishment, and feasibility testing of study operations [103]. This protocol establishes whether proceeding to a full-scale indirect comparison is justified.
Step 1: Evidence Mapping
- Conduct systematic literature review to identify all relevant comparative evidence
- Map existing direct and indirect evidence into structured networks
- Document gaps in the evidence base that necessitate indirect approaches
Step 2: Methodological Selection
- Evaluate suitability of various ITC techniques (network meta-analysis, population-adjusted indirect comparisons, etc.)
- Justify selected methodology based on evidence structure and clinical context
- Pre-specify analytical approach in documented protocol
Step 3: Feasibility Testing
- Assess ability to extract necessary data from available studies
- Test computational implementation of selected methods
- Evaluate robustness of proposed approach through preliminary analyses
Network Meta-Analysis Execution Protocol
Network meta-analysis (NMA) represents one of the most widely accepted population-adjusted ITC techniques, allowing simultaneous comparison of multiple treatments through a connected evidence network [27].
Step 1: Data Collection and Preparation
- Extract data on study characteristics, patient populations, interventions, and outcomes
- Standardize outcome definitions and measurement approaches across studies
- Assess and document clinical and methodological diversity
Step 2: Model Implementation
- Select appropriate statistical model (fixed vs. random effects) with justification
- Implement consistency checks between direct and indirect evidence
- Execute primary analysis according to pre-specified methods
Step 3: Validation and Sensitivity Analysis
- Assess model convergence and statistical fit
- Conduct sensitivity analyses for key assumptions and influential data points
- Evaluate potential impact of effect modifiers through meta-regression or subgroup analyses
Diagram 1: ITC Experimental Workflow
Analytical Tools and Visualization
Research Reagent Solutions
Table 2: Essential Methodological Tools for Indirect Comparisons
| Tool Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Statistical Software Packages | R (gemtc, netmeta), SAS, WinBUGS/OpenBUGS | Implementation of statistical models for ITC | Execution of network meta-analyses and complex population-adjusted methods |
| Quality Assessment Instruments | Cochrane Risk of Bias, ROBINS-I, ITC-specific checklist [102] | Evaluation of primary study quality and potential biases | Critical appraisal of evidence base prior to inclusion in ITC |
| Evidence Synthesis Platforms | GRADE for NMA, CINeMA | Systematic assessment of confidence in estimates | Transparency in communicating certainty of ITC findings |
| Data Visualization Tools | Network plots, rank-heat plots, contribution plots | Graphical representation of evidence networks and results | Enhanced interpretation and communication of complex ITC results |
Color Application in Data Visualization
Appropriate color selection plays a critical role in effectively communicating indirect comparison results. The careful use of color allows interrelationships and patterns within complex data to be easily observed, while careless application will obscure these patterns [106].
Three major types of color palette exist for data visualization [107]:
- Qualitative palettes: Used when the variable is categorical in nature (e.g., different drug classes)
- Sequential palettes: Applied when variables are numeric or have inherently ordered values
- Diverging palettes: Appropriate for numeric variables with meaningful central values
For accessibility, approximately four percent of the population has color vision deficiency, primarily causing confusion between red and green hues [107]. Varying dimensions other than hue alone (such as lightness and saturation) to indicate values and using color blindness simulators like Coblis during palette development ensures visualizations remain interpretable to all audiences [107].
Diagram 2: ITC Method Selection Logic
Implementation in Decision-Making
The ultimate value of indirect comparisons lies in their ability to inform healthcare decision-making. The results of comparative effectiveness research have the potential to provide invaluable insight to patients and providers searching for optimal treatment options, as well as healthcare decision-makers designing affordable benefits [104]. However, these research results should be presented in a manner understandable to diverse audiences, with realistic outcome expectations and any side effects associated with studied treatments clearly disclosed [104].
While indirect comparisons provide critical evidence, AMCP does not support mandates requiring coverage based solely on such results [104]. Healthcare decision-makers serve diverse patient populations and therefore must retain flexibility to use research results in the manner they deem most appropriate for their specific populations. This principle underscores the importance of transparency in ITC methodology and limitations, enabling informed interpretation rather than mechanistic application.
This framework provides a systematic approach for critical appraisal of indirect treatment comparisons within the broader context of comparative drug efficacy research. As ITC methodologies continue to evolve, with global guidelines increasingly incorporating more complex techniques, rigorous appraisal remains essential for ensuring the appropriate application of these methods in healthcare decision-making [27]. The structured checklist approach, encompassing eliminatory questions and detailed assessment across clinical, methodological, and quality domains, offers researchers and drug development professionals a practical tool for evaluating ITC validity and applicability [102]. Through consistent application of these appraisal principles, the field can advance the scientifically rigorous use of indirect comparisons to address critical evidence gaps in comparative drug effectiveness.
The translation of comparative drug efficacy research into clinical guidelines, reimbursement policies, and regulatory frameworks represents a critical pathway for maximizing public health impact. This process forms a complex ecosystem where scientific evidence interacts with economic considerations, regulatory science, and clinical practice needs. Recent developments, including significant regulatory modernization and evolving payment models, have substantially accelerated this translation process while maintaining rigorous standards for evidence generation.
For drug development professionals and researchers, understanding this integrated ecosystem is no longer ancillary but fundamental to strategic program planning. Demonstrating a product's efficacy and safety profile relative to existing alternatives directly informs its potential placement in treatment algorithms, eligibility for reimbursement, and ultimate accessibility to patients. This guide examines the current methodologies, regulatory requirements, and policy interfaces that transform empirical evidence into actionable decisions that shape patient care.
Regulatory Evolution in Efficacy Evidence Requirements
The Shift in Biosimilar Efficacy Demonstrations
A paradigm shift in regulatory science is the Food and Drug Administration's (FDA) updated approach to demonstrating biosimilarity. The 2015 "Scientific Considerations" guidance generally expected comparative efficacy studies (CES) unless sponsors could provide scientific justification otherwise [31]. These studies were typically large, lengthy, and costly, often requiring 400-600 subjects at an average cost of $25 million per trial and taking up to three years to complete [31].
The FDA's October 2025 draft guidance fundamentally recalibrates this approach, proposing that for many therapeutic protein products (e.g., antibodies), CES may not be necessary when supported by rigorous comparative analytical assessment (CAA) and pharmacokinetic (PK) data [30] [87] [86]. This evolution reflects both the FDA's accrued experience—having approved 76 biosimilars to date—and advancements in analytical technologies that now enable structural characterization with exceptional specificity and sensitivity [31].
Table 1: Evolution of FDA Guidance on Biosimilar Efficacy Evidence
| Aspect | 2015 Guidance (Original) | 2025 Draft Guidance (Updated) |
|---|---|---|
| Default Position on CES | Generally necessary without strong justification | May not be needed with sufficient analytical data |
| Primary Evidence Focus | Clinical efficacy endpoints | Comparative analytical assessment (CAA) |
| Key Supporting Data | Residual uncertainty from prior data | Human PK similarity study |
| Technological Basis | Established analytical methods | Advanced characterization with high sensitivity |
| Stated Rationale | Conservative approach to address uncertainty | CAA is generally more sensitive than CES for detecting differences |
Conditions for Streamlined Biosimilar Development
The draft guidance specifies conditions where this streamlined approach may be appropriate [87]:
- The reference product and biosimilar are manufactured from clonal cell lines, are highly purified, and can be well-characterized analytically
- The relationship between quality attributes and clinical efficacy for the reference product is understood, and these attributes are evaluable
- A human pharmacokinetic similarity study is feasible and clinically relevant
This policy alignment with the Executive Order "Lowering Drug Prices by Once Again Putting Americans First" aims to accelerate biosimilar approvals, foster market competition, and reduce costs for advanced treatments for conditions like cancer, autoimmune diseases, and rare disorders [31] [87]. It also harmonizes with international regulatory trends, including the European Medicines Agency's recent efforts to reduce clinical data requirements for biosimilar development [31].
Methodological Frameworks for Comparative Efficacy Research
AI-Driven Molecular Representation in Drug Discovery
Modern molecular representation methods have revolutionized early drug discovery and efficacy prediction. While traditional approaches relied on simplified molecular-input line-entry system (SMILES) strings and molecular fingerprints, recent AI-driven techniques employ deep learning models to learn continuous, high-dimensional feature embeddings directly from complex datasets [108].
Table 2: Molecular Representation Methods in Efficacy Research
| Method Type | Key Technologies | Applications in Efficacy Research | Advantages |
|---|---|---|---|
| Traditional Representations | SMILES, Molecular Fingerprints, Molecular Descriptors | QSAR modeling, Similarity searching, Clustering | Computational efficiency, Interpretability |
| Language Model-Based | Transformers, BERT models applied to SMILES/SELFIES | Molecular property prediction, Generation of novel structures | Captures sequential patterns in molecular "language" |
| Graph-Based | Graph Neural Networks (GNNs) | Scaffold hopping, Activity prediction, Property optimization | Natively represents molecular structure as graphs |
| Multimodal & Contrastive Learning | Combined representation learning | Enhanced molecular property prediction, Cross-domain learning | Leverages multiple data types for robust representations |
These advanced representations are particularly valuable for scaffold hopping—identifying new core structures while retaining biological activity—which plays a crucial role in optimizing lead compounds to enhance efficacy and reduce undesirable properties like toxicity or metabolic instability [108].
Experimental Protocols for Modern Efficacy Assessment
Protocol for AI-Enhanced Scaffold Hopping
Objective: Identify novel molecular scaffolds with similar target engagement but improved efficacy or safety profiles.
Methodology:
- Representation Generation: Convert candidate molecules to continuous vector representations using graph neural networks (e.g., message-passing neural networks) or language models (e.g., BERT-style models applied to SMILES strings)
- Similarity Metric Definition: Establish multi-dimensional similarity metrics incorporating both structural features (from representations) and predicted biological activity
- Latent Space Exploration: Use generative models (e.g., variational autoencoders, generative adversarial networks) to explore chemical space and propose novel scaffolds
- In Silico Validation: Predict binding affinity, ADMET properties, and potential efficacy endpoints for candidate molecules
- Experimental Validation: Progress top candidates through in vitro and in vivo efficacy models
This approach has been successfully applied to discover novel compounds with similar biological effects but different structural features, potentially overcoming efficacy limitations or patent restrictions of existing therapies [108].
Protocol for Long-Term Treatment Efficacy Assessment
Objective: Evaluate sustained efficacy and safety of continuous therapeutic intervention.
Methodology (exemplified by lecanemab in Alzheimer's disease) [109]:
- Study Design: Phase 3 open-label extension trial of initial double-blind, placebo-controlled study
- Participant Population: Early Alzheimer's disease patients who completed the initial controlled trial
- Intervention: Continuous treatment with the therapeutic agent (e.g., lecanemab intravenous formulation)
- Duration: Extended follow-up (e.g., 48-month analysis in addition to initial 18-month core trial)
- Efficacy Endpoints: Clinical measures (e.g., Clinical Dementia Rating Scale, cognitive subscales), biomarker assessments (e.g., amyloid PET, cerebrospinal fluid biomarkers)
- Safety Monitoring: Regular assessment of adverse events (e.g., amyloid-related imaging abnormalities for anti-amyloid antibodies)
This methodology provides critical evidence about long-term treatment effects that inform clinical guidelines regarding duration of therapy and monitoring requirements.
The Policy and Reimbursement Interface
Medicare Drug Price Negotiation Program
The Inflation Reduction Act's Medicare Drug Price Negotiation Program represents a significant policy mechanism that directly links drug efficacy and value to pricing [110]. For 2027, 15 Medicare Part D drugs have been selected for negotiation, with total spending on these drugs reaching $40.7 billion between November 2023 and October 2024, covering 5.3 million Medicare beneficiaries [110].
Table 3: Medicare Drug Price Negotiation Program Overview
| Aspect | 2026 (Initial Year) | 2027 (Second Round) | 2028 and Beyond |
|---|---|---|---|
| Number of Drugs | 10 Part D drugs | 15 Part D drugs | Up to 15 Part D/B drugs (2028), then 20/year |
| Drug Eligibility | Small-molecule drugs ≥7 years post-approval; Biologics ≥11 years post-licensure | Same criteria, with updated threshold dates | Expansion to include Part B drugs (2028) |
| Exclusions | Orphan drugs, plasma-derived products, low expenditure drugs (<$200M), "small biotech" drugs | Same exclusions | Small biotech exception expires after 2028 |
| Spending Threshold | Based on 2021-2022 data | Based on 2023-2024 data | Annual updated expenditure period |
| Key Dates | Negotiations concluded August 2024; Prices effective Jan 2026 | Manufacturer agreements due Oct 2025; Prices effective Jan 2027 | Ongoing annual cycles |
The program excludes certain drug categories from negotiation, including drugs designated for only one rare disease or condition (the orphan drug exclusion), drugs with total Medicare spending below an inflation-adjusted threshold (approximately $200 million), plasma-derived products, and for 2026-2028, qualifying "small biotech" drugs [110].
Biosimilar Market Entry Considerations
The Inflation Reduction Act incorporates a "biosimilar delay" provision that postpones selection of reference biological products for negotiation if there is a "high likelihood" of biosimilar market entry within two years [110]. This policy aims to avoid creating financial disincentives for biosimilar development, as price-reduced reference products might undermine biosimilar market viability.
For 2027, CMS determined that no products qualified for this delay, indicating that no reference products facing likely biosimilar competition were among the top-ranked drugs selected for negotiation [110]. This policy interaction between regulatory pathways for biosimilars and reimbursement mechanisms creates a complex landscape that drug developers must navigate strategically.
Visualization of Research and Policy Pathways
Efficacy Evidence Generation Workflow
Policy and Reimbursement Decision Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Efficacy Research
| Reagent/Material | Function in Efficacy Research | Application Examples |
|---|---|---|
| Amyloid-β Protofibril Immunoassay | Measures target engagement of Alzheimer's therapeutics | Quantifying Aβ protofibrils in cerebrospinal fluid to establish pharmacodynamic effects [109] |
| Graph Neural Network Frameworks | Molecular representation and property prediction | Predicting efficacy-related properties from structural data; scaffold hopping [108] |
| Extended-Connectivity Fingerprints (ECFP) | Traditional molecular representation for similarity assessment | Quantitative Structure-Activity Relationship (QSAR) modeling; virtual screening [108] |
| Anti-Tau Antibodies (e.g., E2814) | Target validation and combination therapy development | Investigating dual-pathway targeting in Alzheimer's disease [109] |
| Pharmacokinetic/Pharmacodynamic Modeling Software | Predicting exposure-response relationships | Dose selection for efficacy trials; optimizing dosing regimens [31] [86] |
| Cell Lines for Biosimilar Characterization | Comparative analytical assessment | Structural and functional comparison to reference biologic products [87] |
The pathway from evidence to action represents an increasingly sophisticated and interconnected process where regulatory science, clinical practice, and reimbursement policy continuously inform one another. The recent evolution in regulatory requirements for biosimilars demonstrates how advances in analytical technologies and accumulated regulatory experience can streamline development while maintaining rigorous standards for establishing similarity.
For researchers and drug development professionals, success requires not only generating robust efficacy data but understanding how this evidence integrates into a complex ecosystem involving multiple decision-makers—regulators, guideline developers, payers, and clinicians. The modern landscape demands strategic evidence generation that addresses both traditional regulatory endpoints and the comparative effectiveness and value assessments that increasingly determine market access and appropriate use in clinical practice.
Future developments will likely continue this trend toward more efficient evidence generation, with advances in AI-driven drug discovery, real-world evidence, and biomarker development further accelerating the translation of scientific innovation into patient benefit, while evolving payment models and regulatory frameworks create new opportunities and challenges for demonstrating therapeutic value.
Conclusion
Robust comparative drug efficacy research is indispensable for informed decision-making in drug development and clinical practice, especially when direct head-to-head trials are unavailable. Mastering a suite of methodologies—from accepted techniques like adjusted indirect comparisons to advanced models like mixed treatment comparisons—is essential. Success hinges on rigorously addressing inherent challenges such as bias, heterogeneity, and uncertainty. Future directions will be shaped by the integration of real-world evidence, advances in pharmacogenomics for personalized comparisons, and the development of more sophisticated statistical frameworks to enhance the reliability and applicability of indirect evidence for regulators, clinicians, and health policymakers.
References
- 1. Comparing the clinical trial efficacy versus real-world ... [https://pubmed.ncbi.nlm.nih.gov/39219457/]
- 2. Clinical Efficacy and Real-World Effectiveness of Fabry ... [https://www.mdpi.com/2077-0383/14/14/5131]
- 3. Comparing the clinical trial efficacy versus real-world ... [https://mayoclinic.elsevierpure.com/en/publications/comparing-the-clinical-trial-efficacy-versus-real-world-effective/]
- 4. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 5. ICH E6 Good clinical practice - Scientific guideline [https://www.ema.europa.eu/en/ich-e6-good-clinical-practice-scientific-guideline]
- 6. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 7. Marketing Metrics: Measuring and Optimizing Performance ... [https://agilitycms.com/blog/marketing-metrics-measuring-and-optimizing-performance-in-2025]
- 8. Clinical Comparative Effectiveness Research Through the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4482557/]
- 9. Retrospective Observational Studies Leveraging Existing ... [https://www.pcori.org/funding-opportunities/announcement/improving-health-decision-making-observational-comparative-clinical-effectiveness-research]
- 10. Presentation of Quantitative Data [https://ihatepsm.com/blog/presentation-quantitative-data]
- 11. and tolerability of medications for... Comparative efficacy [https://pmc.ncbi.nlm.nih.gov/articles/PMC6109107/]
- 12. Understanding the Levels of Evidence in Medical Research [https://jocr.co.in/wp/2025/05/understanding-the-levels-of-evidence-in-medical-research/]
- 13. Estimating comparative effectiveness using Single-Arm trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538941/]
- 14. Accelerated approval: Navigating FDA's recent guidance ... [https://www.parexel.com/insights/blog/accelerated-approval-navigating-fdas-recent-guidance-and-confirmatory-trial-considerations]
- 15. How the May 2025 ODAC Meeting Could Still Impact ... [https://www.lungevity.org/blogs/how-may-2025-odac-meeting-could-still-impact-future-lung-cancer-clinical-trials]
- 16. The relevance of the real-world evidence in research, ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1512429/full]
- 17. Update to the PRISMA guidelines for network meta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11892999/]
- 18. Improving research transparency: an interpretation of the ... [https://www.sciencedirect.com/science/article/pii/S2949713225000795]
- 19. Methods resources for authors new to conducting ... [https://www.sciencedirect.com/science/article/pii/S0895435625000927]
- 20. Cochrane Methods Report 2025 [https://www.cochrane.org/about-us/news/cochrane-methods-report-2025]
- 21. Overview of methods for comparing the efficacies of drugs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3895352/]
- 22. The biggest challenges will face in clinical trials 2025 [https://www.clinicaltrialsarena.com/features/clinical-trials-challenges-expect-2025/]
- 23. trends in Clinical : Investment headwinds, wearables, and... trial 2025 [https://www.merative.com/blog/clinical-trial-trends-2025]
- 24. in Clinical Trial Challenges 2025 [https://www.citruslabs.com/post/clinical-trial-challenges-in-2025]
- 25. Validity of indirect comparison for estimating efficacy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC150178/]
- 26. Interpreting Indirect Treatment Comparisons and Network ... [https://www.sciencedirect.com/science/article/pii/S1098301511014045]
- 27. A Targeted Review of Worldwide Indirect Treatment ... [https://www.sciencedirect.com/science/article/pii/S1098301524024021]
- 28. Methods for Population-Adjusted Indirect Comparisons in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5774635/]
- 29. Data visualisation approaches for component network meta ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-02026-z]
- 30. Scientific Considerations in Demonstrating Biosimilarity to ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/scientific-considerations-demonstrating-biosimilarity-reference-product-updated-recommendations]
- 31. Comparative Efficacy Studies No Longer a Default for ... [https://www.alston.com/en/insights/publications/2025/11/fda-comparative-efficacy-studies-biosimilars]
- 32. Chapter 11: Undertaking network meta-analyses [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-11]
- 33. Bayesian hierarchical models for network meta-analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4731325/]
- 34. Bayesian Approach by Berry [https://www.berryconsultants.com/trials/bayesian-approach]
- 35. A Network Meta-Analysis Toolkit [https://methods.cochrane.org/cmi/network-meta-analysis-toolkit]
- 36. Bibliometric Analysis of Surgical Articles Using Bayesian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12453365/]
- 37. A Bayesian approach to small samples: Mixed-effects ... [https://www.sciencedirect.com/science/article/abs/pii/S2772766125000527]
- 38. How to do meta-analysis using a Bayesian Hierarchical ... [https://blogs.worldbank.org/en/impactevaluations/how-do-meta-analysis-using-bayesian-hierarchical-model-and-when-does-it-make]
- 39. MetaInsight v6.4.0 [https://crsu-metainsight.le.ac.uk/MetaInsight/]
- 40. Beading plot: a novel graphics for ranking interventions in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11462909/]
- 41. The results of direct and indirect treatment comparisons in ... [https://www.sciencedirect.com/science/article/abs/pii/S0895435697000498]
- 42. Quantitative Assessment of Systematic Bias: A Guide for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10714380/]
- 43. Methods for real-world studies of comparative effects [https://www.nice.org.uk/corporate/ecd9/chapter/methods-for-real-world-studies-of-comparative-effects]
- 44. Real World Data: 5 Powerful Benefits & Challenges in 2025 [https://lifebit.ai/blog/real-world-data/]
- 45. Real-World Evidence [https://www.fda.gov/science-research/science-and-research-special-topics/real-world-evidence]
- 46. Revisiting real-world data studies: Progress, value, and ... [https://www.the-innovation.org/article/doi/10.59717/j.xinn-med.2025.100143]
- 47. Harnessing digital health technologies and real-world ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12290384/]
- 48. Observational designs for real-world evidence studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8815667/]
- 49. A comprehensive guide to conduct a systematic review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366998/]
- 50. PRISMA 2020 explanation and elaboration: updated guidance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8005925/]
- 51. Systematic Reviews and Meta-analysis Comparative ... [https://www.sciencedirect.com/science/article/pii/S2772572325001517]
- 52. A systematic review and meta-analysis of the efficacy and ... [https://www.nature.com/articles/s41591-025-03978-z]
- 53. Table 3, Summary of headings for reporting the quantitative ... [https://www.ncbi.nlm.nih.gov/books/NBK132268/table/cerguideguidance.t3/]
- 54. Chapter 14: Completing 'Summary of findings' tables and ... [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-14]
- 55. Methods for external control groups for single arm trials or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7756307/]
- 56. Informing single-arm clinical trials with external controls [https://friendsofcancerresearch.org/news/nature-reviews-drug-discovery-informing-single-arm-clinical-trials-with-external-controls/]
- 57. Editorial: External control arms for single-arm studies [https://www.frontiersin.org/journals/drug-safety-and-regulation/articles/10.3389/fdsfr.2025.1579171/full]
- 58. Design, Conduct, and Analysis of Externally Controlled Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411980/]
- 59. Use of real-world external controls in indirect comparisons ... [https://www.sciencedirect.com/science/article/pii/S2950433325002708]
- 60. Quantitative Bias Analysis for Single-Arm Trials With External ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11947839/]
- 61. Bias recognition and mitigation strategies in artificial ... [https://www.nature.com/articles/s41746-025-01503-7]
- 62. Analytical Methods for Comparing Uncontrolled Trials With ... [https://www.sciencedirect.com/science/article/pii/S1098301524028420]
- 63. Characterizing Treatment Effect Heterogeneity Using Real†... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11993293/]
- 64. Criteria for Distinguishing Effectiveness From Efficacy Trials in ... [https://www.ncbi.nlm.nih.gov/books/NBK44024/]
- 65. Normalising comparative effectiveness trials as clinical practice [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05566-1]
- 66. Estimating comparative effectiveness using Single-Arm trials [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02660-9]
- 67. What's the difference? Endpoints versus outcomes in ... [https://www.tenbridgecommunications.com/2024/02/20/whats-the-difference-endpoints-versus-outcomes-in-clinical-trials/]
- 68. Guidance Recap Podcast | Multiple Endpoints in Clinical ... [https://www.fda.gov/drugs/guidances-drugs/guidance-recap-podcast-multiple-endpoints-clinical-trials]
- 69. Developing, Analyzing, and Interpreting Outcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12341871/]
- 70. Strengthening health technology assessment for cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12008668/]
- 71. Indirect Comparisons of the Efficacy and Safety ... [https://link.springer.com/article/10.1007/s40487-025-00380-0]
- 72. Mid-Year 2025 Clinical Trial Wrap – TA Scan Edition [https://www.anjusoftware.com/insights/data-science/mid-2025-clinical-trial-trends/]
- 73. Clinical Trial Supply and Logistics Market for Pharma 2025 | Regional Markets and Revenue Insights - Forecasting the CTSL Industry to 2035 [https://finance.yahoo.com/news/clinical-trial-supply-logistics-market-135600801.html]
- 74. FDA proposes to cut comparative efficacy study ... [https://www.raps.org/news-and-articles/news-articles/2025/10/fda-proposes-to-cut-comparative-efficacy-study-req]
- 75. Breaking Down Barriers to International Clinical Trials [https://acrpnet.org/2024/03/12/breaking-down-barriers-to-international-clinical-trials]
- 76. Clinical trial logistics: Navigating global distribution challenges - Greens Ltd [https://greensdigital.com/blog/post/clinical-trial-logistics-navigating-global-distribution-challenges]
- 77. Precision in Motion: Why Logistics Can Make or Break Clinical Trials - Euro-American Worldwide Logistics [https://www.eawlogistics.com/precision-in-motion-why-logistics-can-make-or-break-clinical-trials/]
- 78. Revolutionizing patient recruitment experience in trials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12591523/]
- 79. The Ultimate Guide to Clinical Trial Costs in 2025 [https://www.sofpromed.com/ultimate-guide-clinical-trial-costs]
- 80. Top Patient Recruitment Companies Transforming Clinical ... [https://www.lindushealth.com/blog/top-patient-recruitment-companies-transforming-clinical-trials-in-2025]
- 81. Trendspotting: Predictions for Clinical Research in 2025 [https://www.clinicalresearchnewsonline.com/news/2025/01/07/trendspotting-predictions-for-clinical-research-in-2025]
- 82. Planning for Patient Recruitment in 2025: Strategies to Stay ... [https://www.antidote.me/blog/planning-for-patient-recruitment-in-2025-strategies-to-stay-ahead-of-the-curve]
- 83. Clinical Trials Modernization - NCI [https://dctd.cancer.gov/research/research-areas/clinical-trials/modernization]
- 84. Launching the 2025 U.S. Clinical Trials Patient Survey [https://velocityclinical.com/launching-the-2025-u-s-clinical-trials-patient-survey/]
- 85. Advancing drug development with “Fit-for-Purpose†modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 86. Scientific Considerations in Demonstrating Biosimilarity to ... [https://www.federalregister.gov/documents/2025/11/20/2025-20380/scientific-considerations-in-demonstrating-biosimilarity-to-a-reference-product-updated]
- 87. FDA Proposes to Remove Comparative Efficacy Studies ... [https://www.jonesday.com/en/insights/2025/11/fda-proposes-removing-comparative-efficacy-studies-for-biosimilars]
- 88. FDA Proposes To Eliminate Comparative Clinical ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/11/fda-proposes-to-eliminate-biosimilar-comparative-studies]
- 89. Comparative Effectiveness Research [https://actuary.org/comparative-effectiveness-research/]
- 90. Using the confidence interval confidently - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5723800/]
- 91. 4.2.1 - Interpreting Confidence Intervals | STAT 200 [https://online.stat.psu.edu/stat200/lesson/4/4.2/4.2.1]
- 92. Identifying and Characterizing Uncertainty - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK264319/]
- 93. EBSCO - Research Databases, EBooks, Discovery Service [https://www.ebsco.com/research-starters/health-and-medicine/clinical-significance]
- 94. The thresholds for statistical and clinical – a five-step... significance [https://pmc.ncbi.nlm.nih.gov/articles/PMC4015863/]
- 95. Applications of machine learning in drug discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6552674/]
- 96. Frontiers | Comparative Efficacy and Safety of Antidiabetic Agents for Post-Transplant Diabetes Mellitus: A Network Meta-Analysis [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1653147/abstract]
- 97. CLINTEL: Data-driven clinical trials monitoring [https://www.tableau.com/solutions/customer/faster-better-less-expensive-data-driven-clinical-trials-monitoring]
- 98. UCSF Diabetes Clinical Trials for 2025 — San Francisco Bay Area [https://clinicaltrials.ucsf.edu/diabetes]
- 99. Clinical Trial Data Visualization [https://www.avaniaclinical.com/expertise/data-visualization/]
- 100. Comparative safety and efficacy of tislelizumab-based ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1628742/full]
- 101. Critical Appraisal tools [https://www.cebm.ox.ac.uk/resources/ebm-tools/critical-appraisal-tools]
- 102. A checklist for critical appraisal of indirect comparisons [https://pubmed.ncbi.nlm.nih.gov/25269948/]
- 103. Phased Large Awards for Comparative Effectiveness ... [https://www.pcori.org/funding-opportunities/announcement/phased-large-awards-comparative-effectiveness-research-pcori-funding-announcement-cycle-1-2025]
- 104. Comparative Effectiveness Research and Patient ... [https://www.amcp.org/legislative-regulatory-position/comparative-effectiveness-research-and-patient-centered-outcomes-research]
- 105. Appraising Quantitative Research in Health Education [https://pmc.ncbi.nlm.nih.gov/articles/PMC3012621/]
- 106. Color Use Guidelines for Mapping and Visualization [https://web.natur.cuni.cz/~langhamr/lectures/vtfg1/mapinfo_2/barvy/colors.html]
- 107. How to choose colors for data visualizations [https://www.atlassian.com/data/charts/how-to-choose-colors-data-visualization]
- 108. Recent advances in molecular representation methods and ... [https://www.nature.com/articles/s44386-025-00017-2]
- 109. Eisai to Present Four-Year Efficacy and Safety Data on ... [https://media-us.eisai.com/2025-07-21-EISAI-TO-PRESENT-FOUR-YEAR-EFFICACY-AND-SAFETY-DATA-ON-CONTINUOUS-TREATMENT-WITH-LECANEMAB-AT-THE-ALZHEIMERS-ASSOCIATION-INTERNATIONAL-CONFERENCE-2025]
- 110. FAQs about the Inflation Reduction Act's Medicare Drug ... [https://www.kff.org/medicare/faqs-about-the-inflation-reduction-acts-medicare-drug-price-negotiation-program/]