Beyond the Gold Standard: A Modern Framework for Evaluating Pharmaceutical Effectiveness Through RCTs and Observational Studies
This article provides a comprehensive analysis for researchers and drug development professionals on the evolving roles of Randomized Controlled Trials (RCTs) and observational studies in evaluating pharmaceutical effectiveness.
Beyond the Gold Standard: A Modern Framework for Evaluating Pharmaceutical Effectiveness Through RCTs and Observational Studies
Abstract
This article provides a comprehensive analysis for researchers and drug development professionals on the evolving roles of Randomized Controlled Trials (RCTs) and observational studies in evaluating pharmaceutical effectiveness. It explores the foundational principles of both methodologies, contrasting their traditional strengths and limitations. The content delves into modern innovations such as adaptive platform trials and causal inference methods that are blurring the methodological lines. Through practical applications and case studies, including lessons from COVID-19 drug repurposing, it offers guidance for selecting appropriate designs and mitigating biases. The article synthesizes evidence on how these approaches can be integrated to generate robust, real-world evidence for regulatory and clinical decision-making, ultimately advocating for a complementary rather than competitive framework in pharmaceutical research.
Understanding the Pillars of Evidence: Core Principles of RCTs and Observational Studies
In the rigorous world of pharmaceutical research, two methodological paradigms form the cornerstone of evidence generation: the experimental framework of Randomized Controlled Trials (RCTs) and the observational nature of Real-World Observational Studies. The former is widely regarded as the "gold standard" for evaluating the efficacy and safety of an intervention under ideal conditions, while the latter provides critical insights into the effectiveness of these interventions in routine clinical practice [1]. Understanding the distinct roles, advantages, and limitations of each approach is fundamental for researchers, scientists, and drug development professionals who must navigate the complex evidence landscape for regulatory approval and clinical decision-making. This guide provides a structured comparison of these methodologies, focusing on their application in assessing pharmaceutical products.
The fundamental distinction lies in investigator intervention. RCTs are interventional studies where investigators actively assign treatments to participants, while observational studies are non-interventional, meaning investigators merely observe and analyze treatments and outcomes as they occur in normal clinical practice without attempting to influence them [1]. This core difference drives all subsequent methodological variations and determines the types of conclusions each approach can support.
Methodological Foundations and Key Characteristics
Defining the Core Paradigms
Randomized Controlled Trials (RCTs) are prospective studies in which participants are randomly assigned to receive one or more interventions (including control treatments such as placebo or standard of care) [2]. The key components of this definition are:
- Prospective Design: The study is planned and participants are enrolled and followed forward in time.
- Random Assignment: A computer or other random process determines treatment allocation, preventing systematic bias in group assignment.
- Controlled Comparison: Outcomes in the investigational group are compared against a control group, which may receive a placebo, no treatment, or the current standard of care [2].
Observational Studies encompass a range of designs where investigators assess the relationship between interventions or exposures and outcomes without assigning treatments. Participants receive interventions as part of their routine medical care, and the investigator observes and analyzes what happens naturally [3] [1]. The major observational designs include:
- Cohort Studies: Subjects are selected based on their exposure status and followed to determine outcome incidence.
- Case-Control Studies: Subjects are selected based on their outcome status, with investigators then looking back to assess prior exposures.
- Cross-Sectional Studies: Exposure and outcome are assessed at the same point in time [3].
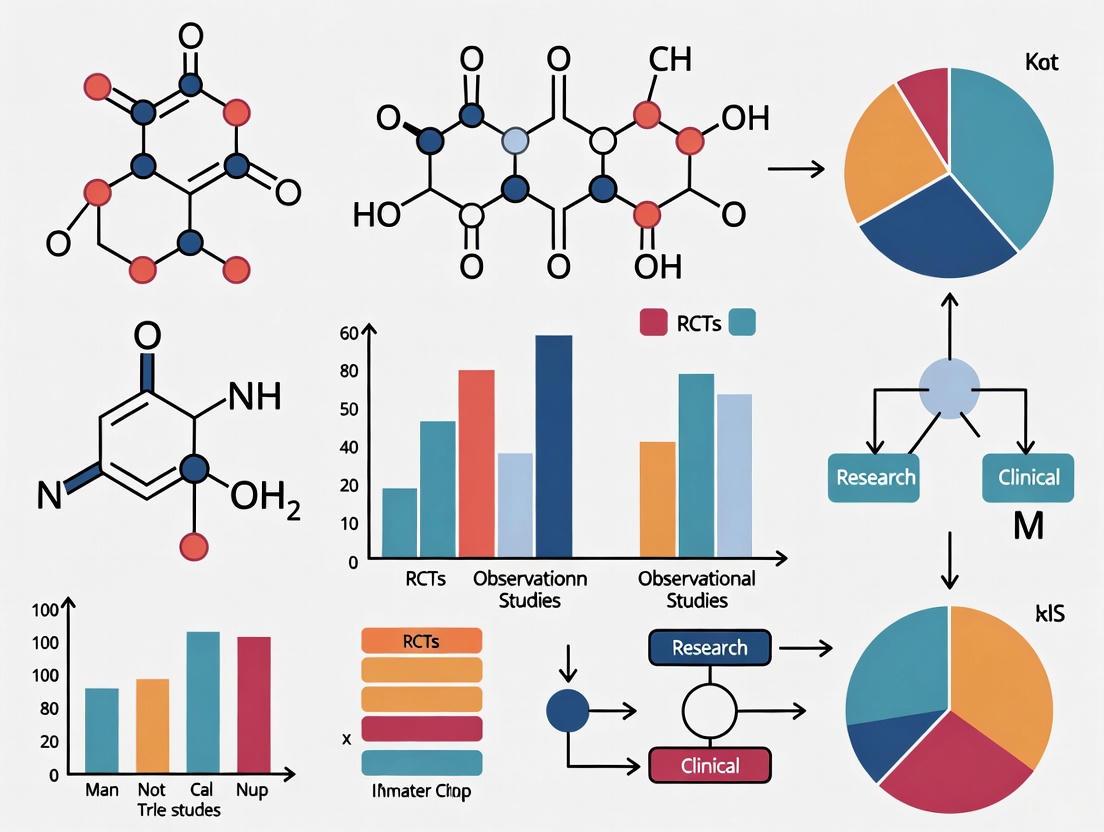
Visualizing the Research Workflow
The following diagram illustrates the fundamental pathways and decision points that differentiate RCTs from observational studies in pharmaceutical research.
Comparative Analysis: RCTs vs. Observational Studies
Structured Comparison of Study Characteristics
The table below provides a detailed, side-by-side comparison of the fundamental characteristics distinguishing RCTs from observational studies.
| Characteristic | Randomized Controlled Trials (RCTs) | Observational Studies |
|---|---|---|
| Fundamental Design | Experimental, interventional | Non-interventional, observational |
| Participant Selection | Highly selective based on strict inclusion/exclusion criteria [1] | Broad, real-world populations from clinical practice [1] |
| Group Assignment | Random allocation by computer/system [2] | Naturally formed through clinical decisions/patient choice [3] |
| Control Group | Always present (placebo, standard of care) [2] | Constructed statistically from comparable untreated individuals |
| Blinding | Often single, double, or triple-blinded [1] | Generally not possible due to observational nature |
| Intervention | Strictly protocolized and standardized | Varies according to routine clinical practice |
| Primary Objective | Establish efficacy (effect under ideal conditions) and safety for regulatory approval [1] [2] | Establish effectiveness (effect in routine practice) and monitor long-term/rare safety [1] |
| Key Advantage | High internal validity; minimizes confounding through randomization [4] | High external validity/generalizability; assesses long-term outcomes and rare events [3] |
| Primary Limitation | Limited generalizability to broader populations; high cost and complexity [4] [2] | Susceptible to confounding and bias; cannot prove causation [3] [5] |
| Typical Context | Pre-marketing drug development (Phases 1-3) [1] | Post-marketing surveillance (Phase 4), comparative effectiveness [1] |
Quantitative Data Comparison
The table below summarizes key quantitative differences between these research approaches, highlighting how these differences impact their application and interpretation.
| Quantitative Metric | Randomized Controlled Trials (RCTs) | Observational Studies |
|---|---|---|
| Typical Sample Size | ~100-3,000 participants (Phases 1-3) [1] | Can include thousands to millions of participants using databases/registries [1] |
| Study Duration | Weeks to months (Phase 2/3); up to several years for long-term outcomes [4] [1] | Can extend for many years to assess long-term outcomes and safety [3] |
| Patient Population | Narrow, homogeneous population; may exclude elderly, comorbidities, polypharmacy [4] [1] | Heterogeneous, representative of real-world patients including those excluded from RCTs [1] |
| Cost & Resource Requirements | Very high (monitoring, site fees, drug supply, lengthy timelines) [6] [2] | Relatively lower cost, especially when using existing databases/registries [1] |
| Ability to Detect Rare Adverse Events | Limited by sample size and duration; underpowered for rare events [4] | Superior for detecting rare or long-term adverse events due to large sample sizes [3] [1] |
| Regulatory Status for Approval | Required as primary evidence for drug approval (pivotal trials) [1] | Supportive evidence for safety; generally not sufficient alone for initial approval [5] |
Experimental Protocols and Methodologies
Protocol for a Phase 3 Randomized Controlled Trial
A typical Phase 3 RCT follows a rigorous, predefined protocol to ensure validity and reliability:
Protocol Development: A detailed study protocol is created specifying objectives, design, methodology, statistical considerations, and organization. This includes precise eligibility criteria for participants to create a homogeneous study population [1].
Randomization and Blinding: After screening and informed consent, participants are randomly assigned to study groups using a computer-generated randomization sequence. Allocation concealment prevents researchers from influencing which group participants enter. Studies are often double-blinded, meaning neither participants nor investigators know treatment assignments [1] [2].
Intervention and Follow-up: The investigational drug, placebo, or active comparator is administered according to a fixed schedule and dosage. Participants are followed prospectively at predefined intervals with standardized assessments, including efficacy endpoints, safety monitoring (e.g., adverse events, lab tests), and adherence checks [1].
Endpoint Adjudication: Clinical endpoints are often reviewed by an independent endpoint adjudication committee blinded to treatment assignment to minimize bias in outcome assessment.
Statistical Analysis: Primary analysis follows the Intent-to-Treat (ITT) principle, analyzing participants according to their randomized group regardless of adherence. Statistical methods like ANOVA, ANCOVA, or mixed models are used to compare outcomes between groups, with a predefined primary endpoint and statistical power [1].
Protocol for a Cohort Observational Study
A typical protocol for a prospective cohort observational study involves:
Data Source Selection: Researchers identify appropriate real-world data sources, such as electronic health records, insurance claims databases, disease registries, or pharmacy databases that capture the exposures and outcomes of interest [1].
Cohort Definition: The study population is defined based on exposure status (e.g., users of a specific drug vs. users of a different drug) or based on a specific diagnosis. Inclusion and exclusion criteria are applied, but are typically broader than in RCTs to reflect real-world practice [3] [1].
Baseline Assessment and Confounder Measurement: Characteristics are measured at baseline for all cohort members, including potential confounders (e.g., age, sex, disease severity, comorbidities, concomitant medications). This allows for statistical adjustment in analyses [3].
Follow-up and Outcome Measurement: Participants are followed for the development of predefined outcomes, which are identified using diagnostic codes, pharmacy records, or mortality data. The follow-up is observational, without intervention in clinical care [3].
Statistical Analysis to Control Bias: Techniques like propensity score matching or regression adjustment are used to create balanced comparison groups and control for measured confounding. Unlike RCTs, observational studies cannot control for unmeasured confounders, which remains a key limitation [3] [5].
Essential Research Reagents and Solutions
The table below details key methodological components and tools essential for conducting rigorous RCTs and observational studies in pharmaceutical research.
| Research Component | Primary Function | Application Context |
|---|---|---|
| Randomization Sequence Generator | Generates unpredictable allocation sequences to eliminate selection bias | Critical for RCTs; ensures groups are comparable for known and unknown factors [2] |
| Blinding/Masking Procedures | Conceals treatment assignment from participants, investigators, and outcome assessors | Used in RCTs to prevent performance and detection bias [1] |
| Standardized Treatment Protocol | Ensures uniform intervention administration across all study participants | Essential for RCT internal validity; minimizes variation in treatment delivery [1] |
| Propensity Score Methods | Statistical method to balance measured covariates between exposed and unexposed groups | Used in observational studies to simulate randomization and reduce confounding [1] |
| Electronic Health Record (EHR) Systems | Provides comprehensive longitudinal data on patient care, outcomes, and covariates | Primary data source for many observational studies; enables large-scale population research [1] |
| Data Safety Monitoring Board (DSMB) | Independent expert committee that monitors patient safety and treatment efficacy data | Required for RCTs; periodically reviews unblinded data to ensure participant safety [1] |
| Case Report Forms (CRFs) | Standardized data collection instruments for capturing research data | Used in both RCTs (prospective collection) and some prospective observational studies |
| Claims and Pharmacy Databases | Administrative data capturing prescriptions, procedures, and diagnoses for billing | Valuable data source for pharmacoepidemiology studies assessing drug utilization and safety [3] |
Current Landscape and Future Directions
The contemporary clinical research landscape recognizes the complementary value of both RCTs and observational studies rather than viewing them as hierarchical [1] [5]. While RCTs remain foundational for regulatory decisions due to their high internal validity, observational studies provide critical information about how drugs perform in diverse patient populations and over longer timeframes than typically feasible in trials [3] [1].
Recent trends include the emergence of Pragmatic Clinical Trials (PrCTs) that incorporate elements of both designs by maintaining randomization while operating in real-world clinical settings [1]. Additionally, current policy shifts, including NIH grant terminations and legislative changes, are disproportionately affecting certain types of research, with one analysis indicating approximately 3.5% of NIH-funded clinical trials (n=383) experiencing grant terminations, disproportionately affecting prevention trials (8.4%) and infectious disease research (14.4%) [7]. These disruptions highlight the fragility of clinical trial infrastructure and may inadvertently increase reliance on observational designs for some research questions.
In conclusion, the choice between RCTs and observational studies is not a matter of selecting a superior methodology but rather of matching the appropriate design to the specific research question at hand. For establishing causal efficacy under controlled conditions, RCTs remain indispensable. For understanding real-world effectiveness, long-term safety, and patterns of use in clinical practice, well-designed observational studies provide evidence that RCTs cannot. The most comprehensive understanding of pharmaceutical benefit-risk profiles emerges from the thoughtful integration of evidence from both paradigms.
Within the rigorous framework of evidence-based medicine, Randomized Controlled Trials (RCTs) occupy the highest echelon for evaluating the efficacy and safety of pharmaceutical interventions. Their premier status is not merely conventional but is fundamentally rooted in their unparalleled ability to ensure high internal validity through methodological safeguards against bias. In the context of comparative effectiveness research, where observational studies derived from real-world data (RWD) offer complementary strengths, RCTs provide the critical anchor of causal certainty. The core of this advantage lies in the deliberate and systematic process of randomization, which effectively neutralizes confounding—a pervasive challenge in observational research. For researchers, scientists, and drug development professionals, understanding the mechanistic operation of randomization is essential for interpreting clinical evidence and designing studies that yield unbiased estimates of treatment effects. This guide objectively examines the experimental data and methodological protocols that underscore the RCT's advantage, providing a comparative analysis with observational studies to inform strategic decisions in pharmaceutical research and development.
Foundational Principles: Internal Validity and Confounding
The Pillar of Internal Validity
Internal validity refers to the extent to which the observed effect in a study can be accurately attributed to the intervention being tested, rather than to other, alternative explanations [8]. It is the cornerstone of causal inference. In an ideal study with perfect internal validity, a measured difference in outcomes between treatment and control groups is caused only by the difference in the treatments received. RCTs are explicitly designed to achieve this through random allocation, which balances both known and unknown prognostic factors across study arms, thereby creating comparable groups from the outset [9] [10].
The Problem of Confounding
Confounding is a situation in which a non-causal association between an exposure (e.g., a drug) and an outcome is created or distorted by a third variable, known as a confounder [9]. A confounder must meet three criteria:
- It must be a cause (or a proxy for a cause) of the outcome.
- It must be associated with the exposure.
- It must not be a consequence of the exposure.
- Example from Observational Research: Consider an observational study investigating the effect of alcohol consumption on lung cancer. Smoking is a potent confounder in this scenario, as it is a known cause of lung cancer and is also associated with alcohol consumption. A naive analysis that fails to adjust for smoking would likely misleadingly suggest that alcohol causes lung cancer [9].
Observational studies must employ sophisticated statistical methods post-hoc to adjust for measured confounders, but they remain vulnerable to unmeasured or unknown confounding. Randomization in RCTs is the primary methodological defense against this threat.
The RCT Mechanism: Experimental Protocol for Randomization
The following workflow details the standard experimental protocol for randomizing participants in a parallel-group RCT, the most common design in pharmaceutical research.
Diagram 1: Experimental workflow for participant randomization in RCTs.
Detailed Methodological Steps
- Eligibility Screening & Informed Consent: Potential participants are screened against pre-defined inclusion and exclusion criteria to create a homogenous study population. Eligible individuals provide informed consent before any study procedures [10].
- Baseline Assessment: Comprehensive data on demographic and clinical characteristics are collected. These variables can later be used to verify the success of randomization and may inform stratified randomization in small studies to ensure balance on key prognostic factors [10].
- Random Allocation Sequence Generation: A computer-generated random sequence is produced to determine the group assignment (e.g., intervention or control) for each participant. This is the core of the RCT methodology [8] [10].
- Allocation Concealment: The random sequence is concealed from the investigators enrolling participants (e.g., via a central, automated system). This prevents selection bias by ensuring the researcher cannot influence which assignment the next participant will receive [8].
- Intervention Administration: Participants receive their allocated intervention. Blinding (or masking) is often implemented, where participants, clinicians, and outcome assessors are unaware of the assignment to further prevent performance and detection bias [8].
- Follow-up and Outcome Assessment: Participants are followed for a pre-specified period, and outcome data are collected systematically.
- Data Analysis: Outcomes are compared between the groups. The analysis is typically conducted according to the Intention-to-Treat (ITT) principle, which analyzes participants in the groups to which they were originally randomized, preserving the benefits of randomization [11].
Quantitative Comparison: RCTs vs. Observational Studies
Empirical evidence systematically comparing pooled results from RCTs and observational studies provides quantitative support for the RCT advantage in controlling bias.
Experimental Data on Effect Estimate Concordance
A 2021 systematic review compared relative treatment effects of pharmaceuticals from observational studies and RCTs across 30 systematic reviews and 7 therapeutic areas [12].
Table 1: Concordance of Relative Treatment Effects between Observational Studies and RCTs [12]
| Metric of Comparison | Number of Pairs Analyzed | Finding | Interpretation |
|---|---|---|---|
| Overall Statistical Difference | 74 pairs from 29 reviews | 79.7% showed no statistically significant difference | The majority of comparisons are concordant. |
| Extreme Difference in Effect Size | 74 pairs from 29 reviews | 43.2% showed an extreme difference (ratio <0.70 or >1.43) | A substantial proportion of observational estimates meaningfully over- or under-estimated the treatment effect. |
| Significant Difference with Opposite Direction | 74 pairs from 29 reviews | 17.6% showed a significant difference with estimates in opposite directions | In a notable minority of cases, observational studies could lead to fundamentally wrong conclusions about the benefit or harm of a treatment. |
Comparative Analysis of Methodological Features
The fundamental differences in design between RCTs and observational studies directly impact their susceptibility to bias and their applicability.
Table 2: Methodological Comparison of RCTs and Observational Studies [8] [13] [9]
| Feature | Randomized Controlled Trials (RCTs) | Observational Studies |
|---|---|---|
| Core Principle | Experimental; investigator assigns intervention. | Observational; investigator observes exposure and outcome. |
| Confounding Control | Randomization balances both measured and unmeasured confounders at baseline. | Statistical adjustment (e.g., regression, propensity scores) for measured confounders only. |
| Internal Validity | High, due to randomization, blinding, and allocation concealment. | Variable and lower, highly dependent on study design, data quality, and analytical methods. |
| External Validity (Generalizability) | Can be limited due to strict eligibility criteria and artificial trial settings. | Typically higher, as studies often involve broader patient populations in real-world settings. |
| Key Strengths | Strong causal inference for efficacy; gold standard for regulatory approval of efficacy. | Insights into long-term safety, effectiveness in routine care, and rare outcomes; hypothesis-generating. |
| Key Limitations & Biases | High cost, long duration, limited generalizability, ethical/logistical constraints for some questions. | Vulnerable to unmeasured confounding, selection bias, and immortal time bias [14] [11]. |
Case Study: Immortal Time Bias – A Specific Threat to Observational Validity
Immortal Time Bias (ITB) is a pervasive methodological pitfall in observational studies that can create a spurious impression of treatment benefit [14]. It occurs when follow-up time for the treated group includes a period during which, by definition, the outcome (e.g., death) could not have occurred because the patient had not yet received the treatment.
- Mechanism: In a naive analysis comparing survival between treated and untreated patients, the period between cohort entry and treatment initiation in the treated group is misclassified as "exposed" time. Since patients must survive this period to receive treatment, this "immortal" time artificially inflates the survival probability in the treated group [14].
- Experimental Evidence: A 2025 analysis using the IMMORTOOL tool demonstrated that previously published, influential observational studies suggesting a large survival benefit for intravenous immunoglobulin (IVIG) in streptococcal toxic shock syndrome (STSS) were likely explained, at least in part, by immortal time bias [14]. When proper analytical methods (like treating the intervention as a time-varying exposure) were applied in benchmark studies, the protective association was substantially attenuated.
- RCT Safeguard: The RCT protocol, with its fixed time zero (randomization) and concurrent follow-up of both groups, inherently prevents this type of bias.
The Scientist's Toolkit: Key Reagents & Analytical Solutions for Causal Inference
Table 3: Essential Methodological and Analytical Tools for Clinical Research
| Tool / Solution | Function / Definition | Application Context |
|---|---|---|
| Random Allocation Sequence | A computer-generated protocol that randomly assigns participants to study groups, forming the foundation of an RCT. | RCTs; ensures comparability of groups at baseline. |
| Stratified Randomization | A technique to ensure balance of specific prognostic factors (e.g., age, disease severity) across treatment groups, particularly useful in small trials. | Small RCTs (<400 participants) to improve power and balance [10]. |
| Allocation Concealment | The stringent process of hiding the allocation sequence from those enrolling participants, preventing selection bias. | RCTs; ensures randomness is not subverted. |
| Intention-to-Treat (ITT) Analysis | Analyzing all participants in the groups to which they were randomized, regardless of what treatment they actually received. | RCTs; preserves the unbiased comparison created by randomization. |
| Propensity Score Methods | A statistical method (matching, weighting, stratification) used in observational studies to adjust for measured confounders by making treated and untreated groups appear similar. | Observational studies; attempts to approximate the conditions of an RCT [9] [11]. |
| Time-Varying Exposure Analysis | A statistical technique where a patient's exposure status (e.g., treated/untreated) can change over time during follow-up. | Observational studies; the correct method to avoid immortal time bias [14]. |
| Target Trial Emulation Framework | A structured approach for designing observational studies to explicitly mimic the protocol of a hypothetical RCT (the "target trial") [11]. | Observational studies; improves causal inference by pre-specifying eligibility, treatment strategies, and follow-up. |
| (Z/E)-GW406108X | (Z/E)-GW406108X, MF:C20H11Cl2NO4, MW:400.2 g/mol | Chemical Reagent |
| DP50 | DP50, MF:C58H72N8O7, MW:993.2 g/mol | Chemical Reagent |
The RCT advantage in securing internal validity and controlling for confounding through randomization remains empirically sound and methodologically uncontested. Quantitative comparisons show that while observational studies often yield similar results, they carry a measurable risk of significant and sometimes dangerously misleadingåå·® [12]. Specific biases like immortal time bias further highlight the vulnerabilities of observational data when causal claims are pursued [14] [11].
However, the evolving landscape of clinical research is not one of replacement but of integration. Observational studies using real-world data are indispensable for assessing long-term safety, effectiveness in heterogeneous populations, and clinical questions where RCTs are unethical or infeasible [13] [9] [15]. Innovations such as causal inference methods, the target trial emulation framework, and hybrid designs like registry-based RCTs are blurring the lines between methodologies, creating a more robust, convergent paradigm [9] [10]. For the pharmaceutical research professional, the optimal approach is not a rigid allegiance to a single methodology, but a critical understanding of the strengths and limitations of each, leveraging the uncontested internal validity of RCTs for establishing efficacy, while harnessing the breadth and generalizability of observational studies to complete the picture of a drug's performance in the real world.
In the landscape of clinical research, randomized controlled trials (RCTs) have traditionally been regarded as the gold standard for establishing causal inference in pharmaceutical efficacy [16] [9]. However, the pursuit of real-world evidence in comparative effectiveness research has highlighted significant limitations of RCTs, particularly concerning external validity—the extent to which study findings can be generalized to other populations, settings, and real-world practice conditions [17] [18]. This guide objectively compares the performance of observational studies and RCTs, framing them not as competitors but as complementary methodologies within a comprehensive evidence generation strategy. We examine how observational studies carve a distinct niche by addressing critical questions of feasibility, ethics, and generalizability that RCTs often cannot, supported by experimental data and detailed protocols.
Defining the Comparative Framework: Internal vs. External Validity
The choice between an RCT and an observational study design often involves a trade-off between internal validity and external validity.
- Internal Validity refers to the degree of confidence that a causal relationship is not influenced by other factors or variables. RCTs achieve high internal validity through random assignment, which balances both measured and unmeasured patient characteristics across treatment groups, thereby minimizing confounding [9].
- External Validity refers to the extent to which research findings can be generalized to other situations, people, settings, and measures [18]. It is subdivided into:
- Population Validity: The generalizability of results from the study sample to a broader target population.
- Ecological Validity: The generalizability of results to real-world situations and settings [18].
This relationship is a fundamental trade-off in clinical research. The highly controlled conditions of an RCT ensure high internal validity but can create an artificial environment that poorly reflects routine clinical practice, thus limiting external validity [16] [17]. Conversely, observational studies, which observe the effects of exposures in real-world settings without assigned interventions, are often better positioned to provide evidence with high external validity [9].
The following diagram illustrates the core trade-off and the distinct strengths of each study type in the research ecosystem.
Quantitative Performance Comparison: RCTs vs. Observational Studies
The comparative effectiveness estimates from RCTs and observational studies have been systematically evaluated. The table below summarizes key quantitative findings from a 2021 systematic review of 29 prior reviews across 7 therapeutic areas, which analyzed 74 pairs of pooled relative effect estimates from RCTs and observational studies [12].
Table 1: Comparability of Relative Treatment Effects from RCTs and Observational Studies
| Comparison Metric | Findings | Implication |
|---|---|---|
| Statistical Significance | No statistically significant difference in 79.7% of paired estimates. | Majority of comparisons show agreement between study designs. |
| Extreme Difference | 43.2% of pairs showed an extreme difference (ratio of relative effect estimates <0.70 or >1.43). | Notable variation exists in a substantial proportion of comparisons. |
| Opposite Directions | 17.6% of pairs showed a significant difference with estimates pointing in opposite directions. | Underlines potential for conflicting conclusions in a minority of cases. |
A specific example of observational study performance is demonstrated in a 2025 study by Li et al., which utilized Natural Language Processing (NLP) to extract data from electronic health records (EHRs) of advanced lung cancer patients [19].
Table 2: Performance of an NLP-Based Observational Study in Advanced Lung Cancer
| Performance Parameter | Result | Benchmarking |
|---|---|---|
| Data Extraction Time | 8 hours for 333 patient records. | Extremely time-efficient compared to manual chart review. |
| Data Completeness | Minimal missing data (Smoking status: n=2; ECOG status: n=5). | High feasibility for capturing key clinical variables. |
| Identified Prognostic Factors | For NSCLC: Male gender (HR 1.44), worse ECOG (HR 1.48), liver mets (HR 2.24). For SCLC: Older age (HR 1.70), liver mets (HR 3.81). | Findings were consistent with established literature, supporting external validity. |
Experimental Protocols and Methodological Workflows
Protocol for a Modern Observational Study Using Real-World Data
The workflow for generating reliable evidence from observational data requires rigorous design to mitigate bias. The following protocol, drawing from contemporary methods, outlines key steps for a robust observational analysis [19] [9].
Table 3: Essential Protocol Steps for a Robust Observational Study
| Protocol Phase | Key Activities | Tool/Technique Examples |
|---|---|---|
| 1. Data Source & Cohort | Identify a data source (e.g., EHR, registry) that captures the real-world population. Apply inclusion/exclusion criteria to define the cohort. | EHRs (e.g., Princess Margaret Cancer Centre data [19]), health insurance claims, disease registries. |
| 2. Exposure & Outcome | Clearly define the exposure (e.g., specific pharmaceutical) and the outcome of interest (efficacy or safety endpoint). | NLP extraction of unstructured clinical notes [19], ICD codes, procedure codes. |
| 3. Causal Design & Analysis | Design the study to emulate a target trial. Use statistical methods to control for measured confounding. Conduct sensitivity analyses. | Directed Acyclic Graphs (DAGs), Propensity Score Matching, E-value calculation for unmeasured confounding [9]. |
The workflow for this protocol is visualized below, highlighting the iterative and structured approach required to ensure validity.
Protocol for a Pragmatic Randomized Controlled Trial
Pragmatic RCTs are designed to bridge the gap between explanatory RCTs and observational studies by testing effectiveness in routine practice conditions [20]. The key elements of their protocol are summarized below.
Table 4: Key Differentiators of a Pragmatic RCT Protocol
| Protocol Element | Pragmatic RCT Approach | Goal |
|---|---|---|
| Participant Selection | Broad, minimally restrictive eligibility criteria to reflect clinical population. | Maximize Population Validity. |
| Intervention Delivery | Flexible delivery mimicking real-world practice, with limited protocol-mandated procedures. | Maximize Ecological Validity. |
| Setting | Diverse, routine clinical care settings (e.g., community hospitals, primary care). | Enhance generalizability of findings. |
| Outcomes | Patient-centered outcomes that are clinically meaningful. | Ensure relevance to practice and policy. |
The Niche Applications of Observational Studies
Observational studies are not merely a fallback when RCTs are too expensive; they are the superior design for specific research niches defined by external validity requirements, feasibility constraints, and ethical imperatives [16] [9] [15].
- Enhancing External Validity and Generalizability: Observational studies include a broader range of patients, including those with comorbidities, polypharmacy, and diverse demographics who are often excluded from RCTs [20] [9]. This results in evidence that is directly applicable to "real-world" clinical populations and practice settings [17].
- Addressing Critical Feasibility Constraints: Observational designs are indispensable when RCTs are not practical. This includes studying rare diseases where patient recruitment for an RCT is impossible, long-term safety outcomes (e.g., assessing the risk of a rare adverse event years after drug approval), and rapidly evolving clinical fields where the slow pace of RCTs would render results obsolete by trial completion [12] [15].
- Providing Ethical Pathways for Evidence Generation: It is considered unethical to randomize patients when: a) an intervention is already the standard of care based on pathophysiological reasoning or longstanding use (e.g., the effect of intraoperative opioids); or b) there is a strong prior belief of harm or benefit that would make randomization unacceptable to clinicians or patients [16] [15]. In such scenarios, well-designed observational studies provide the only ethical source of comparative evidence.
The Scientist's Toolkit: Essential Reagents & Materials
The following table details key "research reagents" and methodological solutions essential for conducting high-quality observational studies in the era of big data [19] [9].
Table 5: Essential Reagents and Methodological Solutions for Observational Research
| Tool / Solution | Category | Function & Application |
|---|---|---|
| Electronic Health Records (EHRs) | Data Source | Provide comprehensive, real-world clinical data on patient history, treatments, and outcomes for large populations [19] [9]. |
| Natural Language Processing (NLP) | Data Extraction | An AI technique to automate the extraction of unstructured clinical data (e.g., physician notes) into structured formats for analysis, dramatically improving feasibility [19]. |
| Directed Acyclic Graphs (DAGs) | Causal Design | A graphical tool used to visually map out assumed causal relationships between variables, informing the selection of confounders to adjust for and minimizing bias [9]. |
| Propensity Score Methods | Statistical Analysis | A technique to simulate randomization by creating a balanced comparison group based on the probability of receiving the treatment given observed covariates, reducing selection bias [9]. |
| E-Value | Sensitivity Analysis | A metric that quantifies how strong an unmeasured confounder would need to be to explain away an observed treatment-outcome association, assessing robustness to unmeasured confounding [9]. |
| Lomonitinib | Lomonitinib, CAS:2923221-56-9, MF:C27H24N4O2, MW:436.5 g/mol | Chemical Reagent |
| TDI-10229 | TDI-10229, MF:C16H16ClN5, MW:313.78 g/mol | Chemical Reagent |
The body of evidence demonstrates that observational studies are not a inferior substitute for RCTs but a powerful methodology with a distinct and critical niche in the clinical research ecosystem. While RCTs remain the gold standard for establishing efficacy under ideal conditions, observational studies are paramount for understanding real-world effectiveness, addressing questions where RCTs are unfeasible or unethical, and providing timely evidence on long-term safety and rare outcomes. The advancement of sophisticated data sources like EHRs, and analytical methods like NLP and causal inference frameworks, has significantly enhanced the reliability and feasibility of observational research [19] [9]. For researchers and drug development professionals, the strategic integration of both RCTs and observational studies—leveraging their complementary strengths—is the most robust path to generating the comprehensive evidence base needed to inform clinical practice and healthcare policy.
For decades, the randomized controlled trial (RCT) has been universally regarded as the gold standard for clinical evidence, occupying the apex of the evidence hierarchy due to its experimental design that minimizes bias through random allocation [21]. This historical primacy has been fundamental to pharmaceutical development and regulatory decision-making. Conversely, observational studies derived from real-world data (RWD) have often been viewed with skepticism, considered inferior for causal inference due to potential confounding and other biases [12].
However, the era of big data and advanced methodological innovations is catalyzing a paradigm shift. A more nuanced, complementary view is emerging, recognizing that both methodologies possess distinct strengths and limitations, and that the research question and context should ultimately drive the choice of method [9]. This guide objectively compares the performance of RCTs and observational studies within pharmaceutical comparative effectiveness research, providing the data and frameworks necessary for modern drug development professionals to navigate this evolving landscape.
Quantitative Comparison of Methodological Performance
Comparative Effectiveness and Safety Outcomes
A systematic landscape review assessed the comparability of relative treatment effects of pharmaceuticals from both observational studies and RCTs. The analysis of 74 paired pooled estimates from 30 systematic reviews across 7 therapeutic areas revealed a complex picture of concordance and divergence [12].
Table 1: Comparison of Relative Treatment Effects between RCTs and Observational Studies
| Metric of Comparison | Finding | Statistical Implication |
|---|---|---|
| Overall Statistical Difference | No statistically significant difference in 79.7% of pairs | Majority of comparisons showed agreement based on 95% confidence intervals [12] |
| Extreme Differences in Effect Size | Extreme difference (ratio <0.7 or >1.43) in 43.2% of pairs | Nearly half of comparisons showed clinically meaningful variation in effect magnitude [12] |
| Opposite Direction of Effect | Significant difference with estimates in opposite directions in 17.6% of pairs | A substantial minority of comparisons produced fundamentally conflicting results [12] |
Key Methodological Characteristics and Applications
The performance differences between RCTs and observational studies stem from their fundamental design characteristics, which make each suited to different research applications within drug development.
Table 2: Methodological Characteristics and Applications of RCTs vs. Observational Studies
| Characteristic | Randomized Controlled Trials (RCTs) | Observational Studies |
|---|---|---|
| Primary Strength | High internal validity; controls for both known and unknown confounders via randomization [21] [9] | High external validity (generalizability); assesses effects under real-world conditions [9] |
| Primary Limitation | Limited generalizability due to selective populations and artificial settings [9] | Susceptibility to bias (e.g., confounding by indication) requiring sophisticated adjustment [22] |
| Ideal Application | Establishing efficacy under ideal conditions; regulatory approval [12] | Post-market safety surveillance; effectiveness in broader populations; rare diseases [12] [23] |
| Ethical Considerations | Required when clinical equipoise exists [21] | Preferred when RCTs are unethical (e.g., harmful exposures) [9] |
| Time & Cost | High cost, time-intensive, complex logistics [23] | Typically faster and more cost-efficient [23] |
Experimental Protocols and Methodological Standards
Core Protocol for a Traditional Randomized Controlled Trial
The following workflow outlines the standard methodology for a parallel-arm pharmaceutical RCT, highlighting steps designed to minimize bias.
Key Experimental Components:
- Random Allocation: Participants are randomly assigned to intervention or control groups, ensuring balance in both known and unknown baseline characteristics, which is the cornerstone of internal validity [21] [9].
- Blinding (Masking): Participants, investigators, and outcome assessors are often blinded to treatment assignment to prevent performance and detection bias.
- Intention-to-Treat (ITT) Analysis: Analyzes all participants in their originally assigned groups, regardless of adherence, to preserve the benefits of randomization [20].
- Protocolized Intervention: The treatment is delivered under standardized, controlled conditions to isolate its specific effect.
Core Protocol for a Modern Observational Study
Modern observational studies aiming for causal inference emulate the structure of an RCT using real-world data (RWD), such as electronic health records (EHRs) or claims databases.
Key Experimental Components:
- Target Trial Emulation: The study begins by explicitly defining the protocol for a hypothetical RCT that would answer the research question, then emulates it with observational data [9].
- Confounding Adjustment: This is a critical step to address bias by indication. Techniques include:
- Propensity Score Methods: The conditional probability of receiving the treatment given several measured confounding variables. Patients are matched or weighted based on their propensity score to create balanced comparison groups [23].
- Risk Adjustment: An actuarial tool that uses claims or clinical data to calculate a risk score for a patient based on their comorbidities, calibrating for the relative health of the compared populations [23].
- Sensitivity Analysis for Unmeasured Confounding: Techniques like the E-value are used to quantify how strong an unmeasured confounder would need to be to explain away the observed association, thus testing the robustness of the results [9].
The Scientist's Toolkit: Essential Reagents for Comparative Effectiveness Research
Table 3: Key Methodological Reagents for Modern Comparative Effectiveness Research
| Tool / Reagent | Category | Primary Function | Considerations |
|---|---|---|---|
| Propensity Score | Statistical Method | Balances measured covariates between exposed and unexposed groups in observational studies, mimicking randomization [23]. | Only adjusts for measured confounders; reliance on correct model specification. |
| E-Value | Sensitivity Metric | Quantifies the required strength of an unmeasured confounder to nullify an observed association, testing result robustness [9]. | Does not prove absence of confounding, but provides a quantitative measure of concern. |
| Directed Acyclic Graphs (DAGs) | Causal Framework | Visual models that map assumed causal relationships between variables, guiding proper adjustment to minimize bias [9]. | Relies on expert knowledge and correct assumptions about the causal structure. |
| Cohort Intervention Random Sampling Study (CIRSS) | Novel Study Design | Combines strengths of RCTs and cohorts; participants from a prospective cohort are randomly selected for intervention offer [20]. | Aims to optimize implementation and generalizability while retaining some random element. |
| Large Language Models (LLMs) | Emerging Technology | Assists in designing RCTs, potentially optimizing eligibility criteria and enhancing recruitment diversity and generalizability [24]. | Requires expert oversight; lower accuracy in designing outcomes and eligibility noted in early studies [24]. |
| Gcn2iB | Gcn2iB, MF:C18H12ClF2N5O3S, MW:451.8 g/mol | Chemical Reagent | Bench Chemicals |
| STL127705 | STL127705, MF:C22H20FN5O4, MW:437.4 g/mol | Chemical Reagent | Bench Chemicals |
The historical view of a rigid evidence hierarchy with RCTs at the apex is giving way to a more integrated and pragmatic framework. The body of evidence shows that while RCTs and observational studies can produce congruent findings, significant disagreement occurs in a meaningful proportion of comparisons [12]. The key for researchers and drug development professionals is to recognize that no single study design is equipped to answer all research questions [9].
The future of robust comparative effectiveness research lies in triangulation—the strategic use of multiple methodologies, with different and unrelated sources of bias, to converge on a consistent answer [9]. By understanding the specific performance characteristics, experimental protocols, and advanced tools available for both RCTs and observational studies, scientists can better design research programs and interpret evidence to ultimately improve pharmaceutical development and patient care.
Innovations in Trial Design and Real-World Evidence Generation
Randomized Controlled Trials (RCTs) remain the gold standard for evaluating pharmaceutical interventions. However, traditional explanatory RCTs, which test efficacy under ideal and controlled conditions, have limitations in generalizability, speed, and cost. This has spurred the development of advanced trial designs—adaptive, platform, and pragmatic trials—that aim to generate evidence more efficiently and applicable to routine clinical practice. This guide objectively compares these innovative designs against traditional RCTs and observational studies, framing the analysis within the broader thesis of comparative effectiveness research.
The fundamental goal of any clinical trial is to provide a reliable answer to a clinical question. Explanatory trials ask, "Can this intervention work under ideal conditions?" whereas pragmatic trials ask, "Does this intervention work under routine care conditions?" [25]. This distinction forms a continuum, not a binary choice, and is critical for understanding the place of advanced designs in the evidence ecosystem [26]. Simultaneously, the life cycle of clinical evidence is being reshaped by designs that can efficiently evaluate multiple interventions, such as platform trials, and those that can incorporate real-world data (RWD) to enhance generalizability and efficiency [27] [28]. These designs do not replace traditional RCTs but offer complementary tools whose selection depends on the specific research question, available resources, and the desired balance between internal validity and generalizability.
Comparative Analysis of Trial Designs
The table below summarizes the core characteristics, advantages, and limitations of advanced RCT designs alongside traditional RCTs and observational studies.
Table 1: Comparison of Advanced RCT Designs, Traditional RCTs, and Observational Studies
| Design Feature | Traditional (Explanatory) RCT | Observational Study | Pragmatic RCT (pRCT) | Platform Trial |
|---|---|---|---|---|
| Primary Question | "Can it work?" (Efficacy) [25] | "How is it used?" (Association) | "Does it work?" (Effectiveness) [25] | "What is the best intervention?" (Comparative Efficacy) |
| Key Objective | Establish causal efficacy under ideal conditions [26] | Describe effectiveness/safety in routine practice [29] | Establish causal effectiveness in routine practice [26] | Efficiently compare multiple interventions against a common control [27] |
| Randomization | Yes, rigid | No | Yes, often flexible [28] | Yes, with potential for response-adaptation [27] |
| Patient Population | Highly selected, homogeneous [26] | Broad, heterogeneous, representative [29] | Broad, heterogeneous, representative [28] [26] | Can be broad, with potential for subgroup testing [27] |
| Setting & Intervention | Highly controlled, strict protocol | Routine clinical practice | Routine clinical practice, flexible delivery [28] | Can leverage a standing, shared infrastructure [27] |
| Comparator | Often placebo or strict standard of care | Various real-world comparators | Often usual care or active comparator [28] | A shared control arm (e.g., standard of care) [27] |
| Data Collection | Intensive, research-specific endpoints | Routinely collected data (e.g., EHR, claims) [29] | Streamlined, often using routine clinical data [28] | Varies, but often streamlined within the platform |
| Statistical Flexibility | Fixed, pre-specified analysis | Methods to control for confounding (e.g., propensity scores) [29] | Pre-specified, but may use intention-to-treat | Pre-specified adaptive rules (e.g., dropping futile arms) [27] |
| Relative Speed & Cost | Slow; High cost per question | Faster; Lower cost (but requires curation) [29] | Moderate to Fast; Moderate cost [28] | Slow initial setup; Lower cost per question over time [27] |
| Key Strength | High internal validity, minimizes bias | Large, diverse populations; long-term follow-up [29] | High external validity with retained randomization | Operational efficiency; rapid answer generation [27] |
| Key Limitation | Limited generalizability; may not reflect real-world use | Susceptible to confounding and bias [29] | Potential for lower adherence; larger sample sizes may be needed [26] | High initial cost and operational/complexity [27] |
Supporting Quantitative Data: A 2021 systematic review of 30 systematic reviews compared relative treatment effects of pharmaceuticals from RCTs and observational studies. It found that in 79.7% of 74 analyzed pairs, there was no statistically significant difference between the two designs. However, 43.2% of pairs showed an "extreme difference" (ratio of relative effect estimates <0.70 or >1.43), and in 17.6%, the estimates pointed in opposite directions [29]. This highlights that while many observational studies can produce results comparable to RCTs, a significant minority do not, underscoring the value of randomized designs like pRCTs for balancing internal and external validity.
Methodological Protocols and Experimental Workflows
Protocol for a Pragmatic Cluster-Randomized Trial
The Hyperlink hypertension trials provide a clear example of how design choices impact trial execution and outcomes [26].
- Workflow Objective: To compare the effects on blood pressure of a pharmacist-led telehealth intervention versus usual clinic-based primary care in a real-world setting.
- Trial Design: Cluster-randomized design, with primary care clinics as the unit of randomization to prevent contamination.
- Key Pragmatic Elements:
- Eligibility & Recruitment: Eligibility was based on criteria mirroring routine quality measures. In the pragmatic Hyperlink 3 trial, recruitment was integrated into the clinical workflow. An automated EHR algorithm identified eligible patients during primary care visits, and clinic staff (not researchers) managed enrollment [26].
- Intervention Delivery: The telehealth intervention was delivered by existing Medication Therapy Management (MTM) pharmacists within the healthcare system, not research staff.
- Follow-up & Data Collection: Patient follow-up and outcome data (blood pressure measurements) were primarily collected through routine clinical care and the EHR, minimizing extra research procedures.
- Outcome: The pragmatic Hyperlink 3 design successfully enrolled a much higher proportion of eligible patients (81% vs. 2.9% in the more explanatory Hyperlink 1) and better represented traditionally under-represented groups (more women, minorities, and patients with lower socioeconomic status). However, the trade-off was significantly lower adherence to the initial pharmacist visit (27% vs. 98% in Hyperlink 1), reflecting real-world challenges [26].
Protocol for a Bayesian Platform Trial
Platform trials represent a paradigm shift from standalone, fixed-duration trials to a continuous, adaptive learning system [27].
- Workflow Objective: To evaluate multiple interventions for a disease area under a single, ongoing master protocol, allowing interventions to be added or dropped as evidence accumulates.
- Core Protocol Features:
- Master Protocol: A single, overarching protocol governs the trial's operations, including a shared control arm, common infrastructure, and pre-specified rules for adaptation.
- Intervention Arms: Multiple intervention arms are tested simultaneously against a shared control (e.g., standard of care).
- Adaptive Rules: Pre-defined statistical rules guide the trial's evolution. These include:
- Futility Stopping: Dropping interventions that are highly unlikely to prove beneficial.
- Efficacy Stopping: Concluding that an intervention is superior to control and potentially making it the new control arm.
- Response-Adaptive Randomization: Adjusting randomization probabilities to favor interventions performing better.
- Adding New Arms: New interventions can be introduced into the platform as they become available, as long as they fit the master protocol.
- Operational Workflow: The entire process is supported by a shared infrastructure (clinical sites, data management, committees) and requires frequent, scheduled interim analyses to inform adaptations.
Successfully implementing advanced trial designs requires a suite of methodological, statistical, and operational tools.
Table 2: Essential Toolkit for Advanced Trial Designs
| Tool Category | Specific Tool/Resource | Function & Application |
|---|---|---|
| Trial Design & Planning | PRECIS-2 (Pragmatic Explanatory Continuum Indicator Summary-2) [28] [26] | A 9-domain tool to help trialists design trials that match their stated purpose on the explanatory-pragmatic continuum. |
| Master Protocol Template [27] | A core protocol defining shared infrastructure, control arm, and adaptation rules for platform trials. | |
| Statistical Analysis | Bayesian Statistical Methods [27] | A flexible framework for sequential analysis, information borrowing across subgroups/arms, and probabilistic interpretation of efficacy in adaptive designs. |
| Computer Simulation [27] | Essential for determining statistical power and operating characteristics (type I error, etc.) of complex adaptive and platform trial designs. | |
| Data Sources & Management | Electronic Health Records (EHR) & Claims Data [28] | Real-world data sources used in pRCTs for patient identification, outcome assessment, and long-term follow-up to enhance efficiency. |
| Covidence / Rayyan [30] | Software tools that streamline the study screening and data extraction process for systematic reviews of existing literature during trial design. | |
| Operational Governance | Independent Data Monitoring Committee (DMC) | A standard committee for monitoring patient safety and efficacy data in all RCTs, critical for reviewing interim analyses in adaptive trials. |
| Statistical Advisory Committee [27] | A dedicated committee of statisticians to navigate the additional complexities of platform and adaptive trial designs. |
The landscape of clinical evidence generation is evolving. While traditional RCTs remain vital for establishing initial efficacy under controlled conditions, advanced designs offer powerful, complementary approaches. Pragmatic RCTs provide a robust method for assessing how an intervention performs in the messy reality of clinical practice, bridging the gap between RCT efficacy and real-world effectiveness. Platform trials offer unparalleled efficiency for answering multiple clinical questions in a dynamic, sustainable system, particularly in areas of persistent clinical equipoise. The choice of design is not a matter of which is universally "best," but which is most fit-for-purpose. By understanding the strengths, limitations, and specific methodologies of these advanced designs, researchers, and drug development professionals can better generate the evidence needed to inform medical practice and improve patient outcomes.
In the evidence-based world of pharmaceutical research, the comparative effectiveness of treatments has traditionally been established through Randomized Controlled Trials (RCTs). While RCTs remain the gold standard for establishing efficacy under controlled conditions, Real-World Data (RWD) is now indispensable for understanding how these treatments perform in routine clinical practice [31]. This guide provides a comparative overview of the three primary RWD sources—Electronic Health Records (EHRs), registries, and claims databases—to help researchers select the right tools for generating robust Real-World Evidence (RWE).
The table below summarizes the core characteristics, strengths, and limitations of each major RWD source, providing a foundation for selection and study design.
| Source Type | Primary Content & Purpose | Key Strengths | Inherent Limitations |
|---|---|---|---|
| Electronic Health Records (EHRs) | Clinical data from patient encounters: diagnoses, medications, lab results, vital signs, progress notes [31]. | Rich clinical detail (e.g., disease severity, lab values); provides context for treatment decisions [31]. | Inconsistent data due to documentation for clinical care, not research; potential for missing data [31] [32]. |
| Claims Databases | Billing and administrative data for reimbursement: diagnoses (ICD codes), procedures (CPT codes), prescriptions [31]. | Large, population-level data; good for capturing healthcare utilization and costs; structured data [31]. | Limited clinical granularity (no lab results, disease severity); potential for coding inaccuracies [31]. |
| Registries | Prospective, structured data collection for a specific disease, condition, or exposure [31] [33]. | Data quality often higher due to collection for research; can capture patient-reported outcomes (PROs) [31] [33]. | Can be costly and time-consuming to maintain; potential for recruitment bias [33]. |
Methodological Frameworks for RWD Analysis
The observational nature of RWD introduces challenges, primarily confounding and selection bias, which require advanced methodologies to approximate causal inference [31] [34]. The following workflow outlines a structured approach to RWD analysis, from source selection to evidence generation.
Key Analytical Techniques
After defining the research question and preparing the data, selecting an appropriate analytical method is critical for robust evidence generation.
Propensity Score (PS) Methods: This approach balances covariates between treated and untreated groups to simulate randomization [31] [33]. A propensity score, the probability of a patient receiving the treatment given their observed characteristics, is estimated for each patient. Key techniques include:
- Propensity Score Matching (PSM): Pairs each treated patient with one or more untreated patients who have a similar propensity score, creating a matched cohort for comparison [31].
- Inverse Probability of Treatment Weighting (IPTW): Weights patients by the inverse of their propensity score, creating a synthetic population where treatment assignment is independent of measured confounders [34].
Causal Machine Learning (CML): Advanced ML models like boosting, tree-based models, and neural networks can handle high-dimensional data and complex, non-linear relationships better than traditional logistic regression for propensity score estimation [34].
- Doubly Robust Methods: Techniques like Targeted Maximum Likelihood Estimation (TMLE) combine outcome regression and propensity score models. They provide a valid effect estimate even if one of the two models is misspecified, enhancing the robustness of findings [34].
G-Computation (Parametric G-Formula): This method involves building a model for the outcome based on treatment and covariates. It is then used to simulate potential outcomes for the entire population under both treatment and control conditions, estimating the average treatment effect by comparing these simulations [34].
The Researcher's Toolkit: Essential Reagents for RWE
Successfully leveraging RWD requires a blend of data sources, methodological expertise, and technological tools. The table below details key components of the modern RWE researcher's toolkit.
| Tool / Resource | Function & Application | Key Considerations |
|---|---|---|
| ONC-Certified EHR Systems (e.g., Epic, Oracle Cerner) [35] | Provides structured, standardized clinical data with interoperability via FHIR APIs for research. | Requires data curation for missingness and consistency; ensure API access for data extraction [36] [35]. |
| Advanced Statistical Software (R, Python with Causal ML libraries) | Enables implementation of PS methods, G-computation, and Doubly Robust estimators. | Causal inference requires explicit assumptions (e.g., no unmeasured confounding); model validation is critical [34]. |
| FHIR (Fast Healthcare Interoperability Resources) Standards | Modern API-focused standard for formatting and exchanging healthcare data, crucial for aggregating data from multiple EHR systems [36] [35]. | Check vendor support for specific FHIR resources and versions [35]. |
| TEFCA (Trusted Exchange Framework and Common Agreement) | A nationwide framework to simplify secure health information exchange between different networks, expanding potential data sources [36]. | Participation among networks is still evolving; understand data availability through Qualified HINs (QHINs) [36]. |
Propensity Score Software Packages (e.g., MatchIt in R) |
Facilitates the practical application of PSM, IPTW, and other propensity score techniques. | The choice of matching algorithm (e.g., nearest-neighbor, optimal) can influence results [31] [34]. |
| CCB02 | CCB02, MF:C14H9N3O, MW:235.24 g/mol | Chemical Reagent |
| Parp-1-IN-32 | Parp-1-IN-32, MF:C21H16N2O5, MW:376.4 g/mol | Chemical Reagent |
RWE in Action: Case Studies and Regulatory Context
RWE is increasingly accepted by regulatory bodies like the FDA to support drug approvals and new indications, particularly when RCTs are impractical or unethical [32] [33].
- Expanding Treatment Options: The FDA approved a new "valve-in-valve" procedure for a transcatheter aortic valve replacement device by evaluating clinical and functional data from a registry of over 100,000 procedures. This RWE demonstrated the procedure's improvement without requiring a new RCT [32].
- Informing Chronic Disease Management: RWE studies have prompted critical re-evaluation of long-standing practices, such as the use of aspirin and beta-blockers for cardiovascular risk management, by revealing variations in effectiveness and safety profiles in real-world populations that were not apparent in initial RCTs [32].
The choice between RWD sources and analytical methods is not about finding a superior alternative to RCTs, but about selecting the right tool for the research question. The future of clinical evidence lies in a synergistic integration of RCTs and RWE [31] [37]. RCTs provide high internal validity for efficacy, while RWE from EHRs, claims, and registries offers critical insights into effectiveness, long-term safety, and treatment outcomes in heterogeneous patient populations seen in everyday practice. By systematically understanding the strengths and limitations of each RWD source and applying rigorous causal inference methodologies, researchers can robustly bridge the efficacy-effectiveness gap and advance patient-centered care.
The pursuit of causal knowledge represents a fundamental challenge in clinical research and drug development. For decades, randomized controlled trials (RCTs) have been regarded as the "gold standard" for establishing causal relationships between interventions and outcomes due to their ability to minimize bias through random assignment [1] [38]. However, RCTs face significant limitations including high costs, strict eligibility criteria that limit generalizability, ethical constraints for certain research questions, and protracted timelines that can render findings less relevant to current practice by publication time [9] [33]. These limitations have accelerated interest in robust methodological approaches for deriving causal inferences from observational data, creating a dynamic landscape where these approaches complement rather than compete with traditional RCTs.
The emergence of causal inference methods for observational data represents a paradigm shift in evidence generation, enabling researchers to approximate the conditions of randomized trials using real-world data (RWD) [9]. These methodological advances are particularly valuable in scenarios where RCTs are impractical, unethical, or insufficient for understanding how interventions perform in heterogeneous patient populations encountered in routine clinical practice [15] [33]. This article provides a comprehensive comparison of causal inference methodologies for observational data against traditional RCTs, offering drug development professionals a framework for selecting appropriate approaches based on specific research contexts and constraints.
Foundational Concepts: Efficacy Versus Effectiveness
Understanding the distinction between efficacy and effectiveness is crucial for contextualizing the complementary roles of RCTs and observational studies. Efficacy refers to the extent to which an intervention produces a beneficial effect under ideal or controlled conditions, such as those in explanatory RCTs [1]. In contrast, effectiveness describes the extent to which an intervention achieves its intended effect in routine clinical practice [1]. This distinction explains why an intervention demonstrating high efficacy in RCTs may show reduced effectiveness in real-world settings where patient comorbidities, adherence issues, and healthcare system factors introduce complexity.
Pragmatic clinical trials (PrCTs) that use real-world data while retaining randomization have emerged as a hybrid approach that bridges the gap between explanatory RCTs and noninterventional observational studies [1]. These trials maintain the strength of initial randomized treatment assignment while evaluating interventions under conditions that more closely mirror actual clinical practice, thus providing evidence on both efficacy and effectiveness from the same study [1].
Table 1: Efficacy Versus Effectiveness in Clinical Research
| Dimension | Efficacy (RCTs) | Effectiveness (Observational Studies) |
|---|---|---|
| Study Conditions | Ideal, controlled conditions | Routine clinical practice settings |
| Patient Population | Highly selective based on strict inclusion/exclusion criteria | Broad, representative of real-world patients |
| Intervention Delivery | Standardized, tightly controlled | Variable, adapting to clinical realities |
| Primary Advantage | High internal validity | High external validity |
| Key Limitation | Limited generalizability | Potential for confounding bias |
Methodological Approaches: RCTs Versus Observational Studies
Randomized Controlled Trials: The Traditional Gold Standard
RCTs are prospective studies in which investigators randomly assign participants to different treatment groups to examine the effect of an intervention on relevant outcomes [9]. The fundamental strength of RCTs lies in the random assignment of the exposure of interest, which, in large samples, generally results in balance between both observed (measured) and unobserved (unmeasured) group characteristics [9]. This design ensures high internal validity and can provide an unbiased causal effect of the exposure on the outcome under ideal conditions [9].
The drug development process typically employs RCTs across multiple phases. Phase 1 trials primarily assess safety and pharmacokinetic/pharmacodynamic profiles with small numbers (20-80) of healthy volunteers [1]. Phase 2 trials evaluate safety and preliminary efficacy in approximately 100-300 patients with the target condition [1]. Phase 3 trials, considered pivotal for regulatory approval, are large-scale RCTs including approximately 1000-3000 patients conducted over prolonged periods to establish definitive safety and efficacy profiles [1]. Phase 4 trials occur after regulatory approval and collect additional information on safety, effectiveness, and optimal use in general patient populations [1].
Observational Studies: Leveraging Real-World Data
Observational studies include designs where investigators observe the effects of exposures on outcomes using existing data (e.g., electronic health records, administrative claims data) or prospectively collected data without intervening in treatment assignment [9] [39]. Major observational designs include:
- Case-control studies: Retrospective studies comparing groups with a disease or condition (cases) to those without (controls) to identify factors associated with the disease [39].
- Cohort studies: Longitudinal studies following groups of participants who share common characteristics, which can be prospective (following participants forward in time) or retrospective (using historical data) [39].
- Cross-sectional studies: Designs that assess both exposure and outcome at the same point in time [39].
The key disadvantage of observational studies is the lack of random assignment, opening the possibility of bias due to confounding and requiring researchers to employ more sophisticated methods to control for this important source of bias [9].
Causal Inference Methods for Observational Data
Causal inference methods refer to an intellectual discipline that allows researchers to draw causal conclusions from observational data by considering assumptions, study design, and estimation strategies [9]. These methods employ well-defined frameworks and assumptions that require researchers to be explicit in defining the design intervention, exposure, and confounders [9]. Key approaches include:
- Directed Acyclic Graphs (DAGs): Visual representations of causal assumptions that help identify potential confounders and sources of bias [9].
- Propensity Score Methods: Statistical approaches that create balance between treatment groups based on observed covariates, including matching, stratification, and inverse probability weighting [33].
- Instrumental Variable Analysis: Methods that use variables associated with treatment but not directly with outcome to account for unmeasured confounding [33].
- E-value Assessment: A metric that quantifies how strong unmeasured confounding would need to be to explain away an observed treatment-outcome association [9].
Table 2: Causal Inference Methods for Observational Data
| Method | Key Principle | Best Use Cases | Key Assumptions |
|---|---|---|---|
| Propensity Score Matching | Balances observed covariates between treated and untreated groups | When comparing two treatments with substantial overlap in patient characteristics | No unmeasured confounding; overlap assumption |
| Instrumental Variables | Uses a variable associated with treatment but not outcome | When unmeasured confounding is suspected | Relevance, exclusion restriction, independence |
| Regression Discontinuity | Exploits arbitrary thresholds in treatment assignment | When treatment eligibility follows a clear cutoff | Continuity of potential outcomes at cutoff |
| Difference-in-Differences | Compares changes over time between treated and untreated groups | When pre- and post-intervention data are available | Parallel trends assumption |
| Synthetic Control Methods | Constructs weighted combinations of untreated units as counterfactual | When evaluating interventions in aggregate units (states, countries) | No interference between units |
Comparative Analysis: Quantitative and Qualitative Dimensions
Methodological Strengths and Limitations
The comparative evaluation of RCTs and observational studies with causal inference methods requires consideration of multiple dimensions, including internal validity, external validity, implementation feasibility, and ethical considerations.
Table 3: Comprehensive Comparison of RCTs and Observational Studies with Causal Inference Methods
| Dimension | Randomized Controlled Trials | Observational Studies with Causal Inference |
|---|---|---|
| Internal Validity | High (due to randomization) | Variable (depends on method and assumptions) |
| External Validity | Often limited by strict eligibility | Generally higher (broader patient populations) |
| Time Requirements | Typically lengthy (years) | Shorter (can use existing data) |
| Cost Considerations | High (thousands to millions) | Lower (leverages existing data infrastructure) |
| Patient Population | Highly selective (narrow criteria) | Representative of real-world practice |
| Ethical Constraints | May be prohibitive for some questions | Enables study of questions unsuitable for RCTs |
| Confounding Control | Controls both measured and unmeasured | Controls only measured confounders |
| Generalizability | Limited to similar populations | Broader applicability to diverse patients |
| Implementation Complexity | High operational complexity | High analytical complexity |
| Regulatory Acceptance | Established as gold standard | Growing acceptance with robust methods |
Quantitative Performance Assessment
Recent research has provided empirical evidence comparing results from RCTs and observational studies employing causal inference methods. A study investigating the capability of large language models to assist in RCT design reported that while observational studies face methodological challenges, advances in causal inference methods are narrowing the gap between traditional RCT findings and real-world data [40]. Side-by-side comparisons suggest that analyses from high-quality observational databases often give similar conclusions to those from high-quality RCTs when proper causal inference methods are applied [15].
However, systematic reviews of observational studies frequently commit methodological errors by using unadjusted data in meta-analyses, which ignores bias by indication, immortal time bias, and other biases [41]. Of 63 systematic reviews published in top medical journals in 2024, 51 (80.9%) presented meta-analyses of crude, unadjusted results from observational studies, while only 22 (34.9%) addressed adjusted association estimates anywhere in the article or supplement [41]. This highlights the critical importance of applying appropriate causal inference methods rather than relying on naive comparisons when analyzing observational data.
Experimental Protocols and Applications
Protocol for Propensity Score Matching
Propensity score matching is one of the most widely used causal inference methods in observational studies of pharmaceutical effects. The standard protocol involves:
Define the Research Question: Clearly specify the target trial that would ideally be conducted, including inclusion/exclusion criteria, treatment strategies, outcomes, and follow-up period.
Create the Study Cohort: Apply inclusion/exclusion criteria to the observational database to create the analytical cohort, ensuring adequate sample size for matching.
Estimate Propensity Scores: Fit a logistic regression model with treatment assignment as the outcome and all presumed confounders as predictors to calculate each patient's probability of receiving the treatment of interest.
Assess Overlap: Examine the distribution of propensity scores in treated and untreated groups to ensure sufficient overlap for matching.
Execute Matching: Use an appropriate matching algorithm (e.g., 1:1 nearest neighbor matching with caliper) to create matched sets of treated and untreated patients.
Assess Balance: Evaluate whether matching achieved balance in measured covariates between groups using standardized mean differences (<0.1 indicates good balance).
Estimate Treatment Effects: Analyze the matched sample using appropriate methods (e.g., Cox regression for time-to-event outcomes) to estimate the treatment effect.
Conduct Sensitivity Analyses: Evaluate how sensitive results are to unmeasured confounding using methods like E-value calculations.
Protocol for Instrumental Variable Analysis
When unmeasured confounding is a significant concern, instrumental variable (IV) analysis provides an alternative approach:
Identify a Valid Instrument: Select a variable that satisfies three key assumptions: (1) associated with treatment assignment, (2) affects outcome only through its effect on treatment, and (3) independent of unmeasured confounders.
Test Instrument Strength: Assess the association between the instrument and treatment assignment (F-statistic >10 indicates adequate strength).
Estimate Two-Stage Model:
- First stage: Regress treatment assignment on the instrument and covariates
- Second stage: Regress outcome on the predicted treatment values from the first stage and covariates
Interpret the Results: The IV estimate represents the local average treatment effect (LATE) among patients whose treatment status was influenced by the instrument.
Validate Assumptions: Conduct sensitivity analyses to evaluate the plausibility of exclusion restriction and independence assumptions.
The Scientist's Toolkit: Essential Research Reagents
Implementing causal inference methods requires both data resources and analytical tools. Key elements of the research toolkit include:
Table 4: Essential Reagents for Causal Inference Research
| Tool/Resource | Function | Application Context |
|---|---|---|
| Electronic Health Records | Provide detailed clinical data from routine practice | Source data for observational studies |
| Administrative Claims Databases | Offer comprehensive healthcare utilization data | Studying treatment patterns and outcomes |
| Propensity Score Software | Implement matching, weighting, or stratification | Balance covariates in non-randomized studies |
| Directed Acyclic Graphs | Visualize causal assumptions and identify confounders | Study design and bias assessment |
| Sensitivity Analysis Tools | Quantify impact of unmeasured confounding | Assess robustness of causal conclusions |
| Registry Data | Provide structured disease- or procedure-specific data | Study specialized patient populations |
| Causal Inference Packages | Implement advanced methods (IV, G-methods) | Complex longitudinal treatment studies |
| Dota-psma-EB-01 | Dota-psma-EB-01, MF:C87H113N15Na2O28S2, MW:1927.0 g/mol | Chemical Reagent |
The comparative analysis of RCTs and observational studies with causal inference methods reveals that neither approach is universally superior; rather, they offer complementary strengths for generating evidence across different research contexts. RCTs remain indispensable for establishing efficacy under controlled conditions with high internal validity, particularly during early drug development and for regulatory approval [1] [38]. However, observational studies with robust causal inference methods provide valuable evidence on effectiveness in real-world populations, study of interventions where RCTs are impractical or unethical, and generation of hypotheses for future randomized trials [9] [15] [33].
The evolving landscape of clinical evidence generation suggests that the future lies not in privileging one method over another, but in thoughtful integration of multiple evidence sources. As noted in recent methodological discussions, "No study is designed to answer all questions, and consequently, neither RCTs nor observational studies can answer all research questions at all times. Rather, the research question and context should drive the choice of method to be used" [9]. Furthermore, triangulation of evidence from observational and experimental approaches can furnish a stronger basis for causal inference to better understand the phenomenon studied by the researcher [9].
For drug development professionals and clinical researchers, the strategic approach involves matching the method to the research question while acknowledging the relative strengths and limitations of each approach. By employing causal inference methods with rigorous attention to their assumptions and limitations, observational studies can provide robust evidence that complements RCTs and expands our understanding of how pharmaceutical interventions perform across the spectrum from efficacy to real-world effectiveness.
The COVID-19 pandemic served as an unprecedented global stress test for translational science, forcing the medical and research community to accelerate innovations and collapse the traditional barriers between laboratory discoveries and clinical application [42]. In the face of an emergent virus and mounting casualties, traditional drug development timelines proved untenable, creating a crisis environment that demanded unprecedented agility in therapeutic development. A central strategy that emerged early was drug repurposing—the search for new therapeutic uses for existing drugs—which offered a pragmatic shortcut by leveraging medications with established human safety profiles [42]. This case study examines how agile translational research frameworks were deployed during the pandemic, comparing the evidentiary value of randomized controlled trials (RCTs) and observational studies in generating practice-ready findings under extreme time constraints.
Analytical Framework: Comparing Research Methodologies
Methodological Characteristics and Applications
The pandemic prompted an extensive debate about the appropriate roles of different study designs in generating timely yet reliable evidence. The table below compares the key characteristics and contributions of RCTs and observational studies during the COVID-19 pandemic.
Table 1: Comparative Analysis of RCTs and Observational Studies in COVID-19 Research
| Characteristic | Randomized Controlled Trials (RCTs) | Observational Studies |
|---|---|---|
| Primary Role | Establishing causal efficacy | Generating rapid, real-world effectiveness signals |
| Key Strength | Controls for confounding via randomization | Greater practicality, cost-effectiveness, and speed |
| Time to Evidence | Typically 6-9 months in adaptive platforms [42] | Provided confirmation 8+ months faster than RCTs [43] |
| Major Limitation | Resource-intensive, slower to implement | Requires greater expertise to address confounding [43] |
| Pandemic Application | Pivotal efficacy evidence for regulatory decisions | Early therapeutic signals and post-authorization monitoring |
| Representative Examples | RECOVERY, SOLIDARITY [42] | CORONA Registry, VISION Network [44] [45] |
Quantitative Comparison of Evidentiary Outputs
Analysis across 211 COVID-19 treatments revealed no systematic difference in results between RCTs and observational studies, with a relative risk (RR) of 0.98 (92% CI 0.92-1.04) [43]. This finding challenges the pre-pandemic assumption that observational studies consistently overestimate treatment effects in emergency settings. The comparable performance of both methodologies during the pandemic highlights that rigorous observational studies can provide valuable evidence when RCTs are impractical or unethical.
Table 2: Drug Case Studies Demonstrating Methodological Strengths and Limitations
| Therapeutic Agent | Initial Evidence | RCT Outcome | Key Lesson |
|---|---|---|---|
| Dexamethasone | Positive observational signals [45] | Reduced mortality by 35% in ventilated patients [42] | Observational data can correctly identify true positives |
| Hydroxychloroquine | Promising in vitro and observational data [45] | No benefit across 18 RCTs [45] | Mechanistic plausibility alone insufficient without RCT validation |
| Tocilizumab | Mixed observational data [45] | Effective in severely ill patients with inflammation [42] | RCTs essential for defining specific patient populations who benefit |
| mRNA Vaccines | High efficacy in pivotal RCTs [46] | Real-world effectiveness confirmed in observational studies [44] [46] | Both methodologies demonstrated utility across translational spectrum |
Agile Frameworks for Rapid Evidence Generation
Adaptive Platform Trials
The pandemic normalized adaptive platform trials such as the UK's RECOVERY trial and the WHO's SOLIDARITY trial, which replaced stand-alone, single-drug studies [42]. These innovative frameworks tested multiple therapeutic candidates concurrently against a shared control group, used response-adaptive randomization to allocate more patients to promising treatments, and employed flexible master protocols that allowed for the seamless addition or removal of investigational arms based on prespecified efficacy thresholds. This design functioned as a translational escalator, continually feeding updated evidence to clinicians and policymakers while conserving patient populations and research resources [42]. The RECOVERY trial notably delivered practice-changing mortality data for multiple therapies within approximately six to nine months of first patient enrollment—dramatically compressing the traditional six-to-seven-year timeline for advancing infectious disease candidates from proof-of-concept to pivotal testing [42].
Integrated Evidence Feedback Loop
The pandemic forged a new conceptual framework where clinical efficacy, implementation feasibility, and economic value co-evolved through a continuous feedback mechanism [42]. This framework operationalized rapid translation from laboratory insight to worldwide deployment through three interconnected mechanisms: (1) adaptive platform trials that generated high-quality efficacy data; (2) real-world evidence from large electronic health record networks, hospital discharge datasets, and national registries that complemented randomized evidence with practical effectiveness data; and (3) early health-economic assessment that embedded cost-utility modeling and budget-impact projections within the translational pipeline to ensure resource allocation reflected both scientific merit and fiscal sustainability [42]. This integrated approach enabled the scientific community to pivot rapidly from basic virological insights to global implementation of effective countermeasures.
Experimental Protocols & Research Reagents
Key Methodological Approaches
Adaptive Platform Trial Protocol
The RECOVERY trial established a methodology that became paradigmatic for pandemic research [42]. The protocol enrolled hospitalized COVID-19 patients across numerous sites and randomly assigned them to receive either the usual standard of care or the usual care plus one or more investigational treatments. Key design elements included: pragmatic inclusion criteria that maximized generalizability; randomization stratified by site, age, and respiratory support; clearly defined primary outcomes (e.g., 28-day mortality); frequent interim analyses by an independent data monitoring committee; and adaptive entry and exit of treatment arms based on prespecified stopping rules. This methodology enabled the trial to efficiently identify both beneficial (dexamethasone, tocilizumab) and ineffective (hydroxychloroquine, lopinavir-ritonavir) treatments within months rather than years.
Test-Negative Vaccine Effectiveness Design
The CDC's VISION and IVY networks employed a test-negative design to estimate COVID-19 vaccine effectiveness (VE) in real-world settings [44]. The methodology identified adults with COVID-19-like illness who received molecular (RT-PCR) or antigen testing for SARS-CoV-2. Case-patients were defined as those with a positive SARS-CoV-2 test result, while control patients were those with a negative test result. Vaccination status was ascertained from state immunization registries, electronic health records, and medical claims. The analysis used logistic regression to compare the odds of vaccination between case-patients and controls, adjusting for potential confounders including age, geographic region, calendar time, and comorbidities. This design generated crucial evidence supporting the continued benefit of COVID-19 vaccination against emerging variants [44].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents and Methodological Tools for Agile Translational Research
| Tool/Reagent | Function | Application Example |
|---|---|---|
| Adaptive Platform Protocol | Master framework for evaluating multiple interventions | RECOVERY trial evaluating dexamethasone, tocilizumab, etc. [42] |
| Test-Negative Design | Observational method to assess vaccine effectiveness | CDC VISION network monitoring 2024-2025 vaccine performance [44] |
| State Immunization Information Systems | Vaccination registries for ascertaining exposure status | Vaccine effectiveness studies using verified vaccination dates [44] |
| Electronic Health Record Networks | Source for real-world clinical and outcome data | VISION network analysis of 373 ED/UCs and 241 hospitals [44] |
| SARS-CoV-2 Variant Sequencing | Viral characterization for stratification | IVY network central RT-PCR testing and lineage identification [44] |
| Living Meta-Analysis | Continuously updated evidence synthesis | Systematic review incorporating studies through March 2025 [42] |
Discussion: Methodological Complementarity in Crisis Research
The COVID-19 pandemic demonstrated that the RCT versus observational study dichotomy represents a false choice; rather, these methodologies function most effectively as complementary components of a comprehensive evidence generation system [43] [42] [45]. Observational studies provided early signals and continued monitoring of real-world effectiveness across diverse populations and settings, while RCTs delivered definitive evidence of causal efficacy necessary for confident clinical decision-making and regulatory authorization. The coordinated deployment of both approaches enabled the global scientific community to accelerate the identification and implementation of effective interventions while minimizing the adoption of ineffective or harmful treatments.
Methodological Innovations with Lasting Impact
The agile translational research frameworks developed during the pandemic have established a new paradigm for therapeutic evaluation during public health emergencies. The compression of the T0-T4 translational spectrum—where months, rather than years, separated basic scientific insight from population-level implementation—demonstrates the potential for more efficient evidence generation even beyond crisis settings [42]. The normalization of adaptive trial designs, the systematic incorporation of real-world evidence, and the early integration of health economic assessment represent methodological advances that will continue to shape pharmaceutical research and development in the post-pandemic era. These innovations collectively address the perennial challenge of balancing scientific rigor with urgent practical need in therapeutic development.
The COVID-19 pandemic catalyzed a unprecedented evolution in translational research methodologies, forcing the scientific community to develop more agile, efficient, and complementary approaches to evidence generation. The experience demonstrated that observational studies can provide valuable early signals and real-world effectiveness data without systematic overestimation of effects when properly conducted [43], while randomized controlled trials remain essential for establishing causal efficacy and preventing the widespread adoption of ineffective treatments [45]. The most significant advance, however, was the development of integrative frameworks that strategically deployed both methodologies in a coordinated manner, with adaptive platform trials like RECOVERY [42] and test-negative observational designs like VISION [44] working in concert to accelerate evidence generation. This coordinated approach, which embeds economic evaluation and implementation considerations throughout the translational pipeline, provides a pragmatic blueprint for balancing urgency with scientific rigor in future global health emergencies. The methodological innovations forged in the COVID-19 crucible have not only delivered life-saving interventions during the pandemic but have established a new, more agile paradigm for therapeutic development that will continue to benefit patients long after the current crisis has receded.
Navigating Bias, Confounding, and Practical Challenges in Real-World Research
In the field of clinical research and drug development, the comparative effectiveness of pharmaceuticals is typically evaluated through two primary study designs: randomized controlled trials (RCTs) and observational studies. RCTs are widely regarded as the gold standard for evaluating efficacy because their design—specifically, the random allocation of participants to intervention or control groups—minimizes bias by balancing both known and unknown prognostic factors [9] [47]. This experimental approach provides high internal validity, allowing researchers to establish causal inferences about treatment effects under ideal conditions [48]. However, RCTs are resource-intensive, time-consuming, and may lack generalizability to real-world patient populations due to strict inclusion and exclusion criteria [47] [48].
Observational studies, including cohort and case-control designs, offer a complementary approach by measuring intervention effectiveness in routine clinical settings, thus providing valuable real-world evidence (RWE) [29] [9]. These studies observe effects without investigator-assigned interventions, making them particularly valuable when RCTs are impractical or unethical [48]. Despite their strengths in assessing effectiveness and detecting rare or long-term adverse events, observational studies are inherently more susceptible to systematic errors that can compromise result validity [29] [49]. The most critical of these biases—confounding, selection, and information bias—represent significant methodological challenges that researchers must identify and mitigate to produce reliable evidence for regulatory and clinical decision-making [22] [49].
Quantitative Comparison of Research Designs
Recent large-scale comparisons have quantified the agreement between RCTs and observational studies. A 2021 systematic review analyzing 74 pairs of pooled relative effect estimates from 29 reviews found no statistically significant difference between RCTs and observational studies in 79.7% of comparisons [29] [50]. However, the same review noted extreme differences (ratio < 0.7 or > 1.43) in 43.2% of pairs, with 17.6% showing statistically significant differences in opposite directions [29].
A more recent 2024 Cochrane review encompassing 34 systematic reviews (comprising 2,869 RCTs and 3,924 observational studies) found similarly minimal differences in effect estimates between study designs (ratio of ratios 1.08, 95% CI 1.01 to 1.15) [51]. Slightly larger discrepancies were observed in subgroup analyses focusing exclusively on pharmaceutical interventions (ratio of ratios 1.12, 95% CI 1.04 to 1.21) [51].
Table 1: Comparison of Key Characteristics between RCTs and Observational Studies
| Aspect | Randomized Controlled Trials | Observational Studies |
|---|---|---|
| Randomization | Yes | No |
| Risk of Selection Bias | Low | Can be high |
| Risk of Confounding | Low (through randomization) | High (requires statistical adjustment) |
| Cost | High (++++) | Moderate (++) |
| Duration | Moderate (++) | Long (++++) |
| Appropriate for Efficacy | Excellent (++++)) | Fair to Good (++ to +++) |
| Appropriate for Effectiveness | Poor (+) | Excellent (++++) |
| Appropriate for Adverse Events | Fair to Good (++ to +++) | Excellent (++++) |
| Real-world Generalizability | Often limited | High |
Table 2: Comparison of Effect Estimates between RCTs and Observational Studies
| Comparison Metric | Findings | Source |
|---|---|---|
| Overall Agreement | No significant difference in 79.7% of comparisons | Hong et al. (2021) [29] |
| Extreme Differences | Present in 43.2% of comparisons | Hong et al. (2021) [29] |
| Opposite Direction Effects | Present in 17.6% of comparisons | Hong et al. (2021) [29] |
| Pooled Ratio of Ratios | 1.08 (95% CI 1.01 to 1.15) | Toews et al. (2024) [51] |
| Pharmaceutical Interventions Only | Ratio of ratios 1.12 (95% CI 1.04 to 1.21) | Toews et al. (2024) [51] |
Identifying Key Biases: Definitions and Mechanisms
Confounding Bias
Confounding occurs when an extraneous factor is associated with both the exposure (treatment) and outcome of interest, creating a spurious association or masking a true effect [9]. In observational studies of pharmaceuticals, confounding by indication represents a particularly challenging bias, as the underlying reason for prescribing a specific treatment is often related to the patient's prognosis [22]. For example, in comparing treatments for lung cancer, the choice between radiosurgery and surgical resection is influenced by tumor size and patient performance status—factors that independently affect survival outcomes [48]. Without randomization, these confounding factors can distort treatment effect estimates unless properly addressed through study design and statistical methods.
Selection Bias
Selection bias arises when the study population is not representative of the target population due to systematic differences in participation or retention [49]. In RCTs, stringent eligibility criteria may exclude up to 85% of potential participants, particularly in fields like neurology, limiting generalizability [47]. In observational studies, selection bias can occur through various mechanisms, including self-selection into treatment groups, loss to follow-up, or differential participation based on factors related to both treatment and outcome. This bias is especially problematic in systematic reviews of observational studies, with recent research indicating that approximately 81% of such reviews perform meta-analyses using unadjusted results that fail to account for selection mechanisms [22].
Information Bias
Information bias, also known as misclassification bias, occurs when errors in measuring exposure, outcome, or key covariates systematically differ between study groups [49]. In pharmaceutical research, this can include inconsistent diagnostic criteria, variable outcome assessment methods, or missing data on important prognostic factors. The reliance on real-world data sources such as electronic health records and insurance claims introduces additional challenges, as these data may not routinely capture the specific interventions, indications, and endpoints used in RCTs [29]. Unlike random measurement error, which typically attenuates effect estimates, information bias can either exaggerate or underestimate true effects depending on its nature and direction.
Methodological Protocols for Bias Mitigation
Advanced Statistical Adjustment Methods
Propensity Score Methods represent a powerful approach to address confounding in observational studies. These techniques involve creating a single composite score that captures the probability of receiving a treatment given observed baseline characteristics [48]. The primary propensity score applications include:
- Propensity Score Matching: Pairing treated and untreated subjects with similar propensity scores to create balanced comparison groups
- Propensity Score Stratification: Dividing subjects into strata based on propensity score quantiles and analyzing treatment effects within each stratum
- Propensity Score Weighting: Using inverse probability of treatment weights to create a synthetic population where treatment assignment is independent of measured covariates
Multivariable Regression Adjustment provides an alternative approach by simultaneously including the treatment and potential confounders in a statistical model predicting the outcome. While conceptually straightforward, this method requires correct model specification and sufficient sample size to precisely estimate multiple parameters.
Table 3: Research Reagent Solutions for Bias Mitigation
| Method/Tool | Primary Function | Applicable Bias |
|---|---|---|
| Propensity Score | Creates composite score balancing measured covariates | Confounding |
| Multivariable Regression | Simultaneously adjusts for multiple confounders | Confounding |
| Quantitative Bias Analysis (QBA) | Quantifies impact of systematic errors | All biases |
| E-value | Measures robustness to unmeasured confounding | Unmeasured confounding |
| Directed Acyclic Graphs (DAGs) | Maps theoretical relationships between variables | Confounding |
| Sensitivity Analysis | Tests how results change under different assumptions | All biases |
Quantitative Bias Analysis (QBA) Protocols
QBA encompasses a suite of methods designed to quantify the impact of systematic errors on study results [49]. A recent systematic review identified 57 QBA methods for summary-level epidemiologic data, with 29 methods addressing unmeasured confounding, 20 focusing on misclassification bias, and 5 targeting selection bias [49]. The implementation protocol includes:
- Parameter Specification: Defining bias parameters based on external knowledge (e.g., from validation studies or literature)
- Bias Modeling: Applying mathematical models to simulate how specified biases would affect observed results
- Sensitivity Evaluation: Examining how conclusions change across plausible values of bias parameters
For unmeasured confounding, a particularly accessible QBA tool is the E-value, which quantifies the minimum strength of association an unmeasured confounder would need to have with both treatment and outcome to fully explain away an observed association [9].
Design-Based Approaches
Target Trial Emulation involves designing observational studies to explicitly mimic the key features of an RCT that would answer the same research question [29]. This protocol includes:
- Specifying eligibility criteria that correspond to RCT inclusion/exclusion criteria
- Defining a precise treatment strategy and initiation point (time zero)
- Identifying an appropriate comparator group
- Measuring outcomes using similar definitions and assessment methods
- Implementing analytical approaches that preserve the intended comparison
When successful, this approach can generate real-world evidence that complements RCT findings, as demonstrated in several studies that have reproduced RCT results using observational data [29].
Emerging Innovations and Future Directions
The traditional dichotomy between RCTs and observational studies is increasingly blurred by methodological innovations that incorporate elements of both approaches. Embedded RCTs within electronic health record systems represent one such innovation, combining randomization with real-world data collection to enhance both internal and external validity [9]. Adaptive trial designs, including platform trials that evaluate multiple interventions simultaneously, offer greater flexibility and efficiency while maintaining randomization benefits [9].
In observational research, causal inference methods have matured substantially, providing formal frameworks for drawing causal conclusions from non-experimental data [9]. These approaches emphasize explicit specification of the target population, treatment strategies, and causal assumptions through tools like directed acyclic graphs (DAGs) [9]. The growing application of these methods across diverse clinical domains, from pharmacoepidemiology to primary care, signals an important paradigm shift in how observational evidence is generated and evaluated.
Future progress will require improved methodological standards, particularly for systematic reviews of observational studies. Current practices remain concerning, with one recent analysis finding that 80.9% of systematic reviews in top medical journals perform meta-analyses using crude, unadjusted results from observational studies [22]. Establishing mandatory reporting standards for adjusted analyses and bias assessment would substantially enhance the reliability of evidence synthesis from observational research.
The comparative effectiveness of pharmaceuticals requires careful consideration of both RCT and observational evidence, with explicit attention to the distinct bias profiles of each design. While recent comprehensive analyses demonstrate that effect estimates from well-conducted observational studies often align with RCT findings [51], significant discrepancies occur in a substantial minority of comparisons [29]. These differences underscore the necessity of rigorous bias assessment and mitigation strategies throughout the research process.
For confounding bias, advanced adjustment methods like propensity scores and quantitative bias analysis provide powerful tools when implemented with appropriate attention to their assumptions. Selection bias demands thoughtful study design and analytical approaches to ensure representative populations. Information bias requires diligent measurement protocols and sensitivity analyses. No single study design can answer all therapeutic questions; rather, triangulation of evidence from multiple methodological approaches provides the strongest foundation for causal inference [9].
As methodological innovations continue to evolve, the research community must prioritize education in these advanced techniques, cross-disciplinary methodological exchange, and the development of reporting standards that ensure transparent communication of methodological limitations and bias mitigation efforts. Through these collective efforts, the field can enhance the reliability of both experimental and observational evidence for pharmaceutical development and clinical decision-making.
The Challenge of Unmeasured Confounding and Tools for Assessment (e.g., E-values)
Comparative effectiveness research (CER) is "the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care" [23]. In pharmaceutical research, this evidence derives primarily from two sources: randomized controlled trials (RCTs), considered the gold standard for clinical research, and observational studies, which analyze data from routine clinical practice [16] [52]. The fundamental challenge in observational studies is confounding, especially by unmeasured factors, which can lead to biased estimates of treatment effects [53] [54].
Unmeasured or poorly measured confounding remains a major threat to the validity of observational research [53]. While RCTs eliminate both measured and unmeasured confounding through random allocation, observational studies can only adjust for measured covariates [53] [54]. This limitation has spurred the development of methodological tools to quantify and assess the potential impact of unmeasured confounding, with the E-value emerging as a prominent sensitivity analysis tool [53].
Study Design Comparisons: RCTs vs. Observational Studies
The choice between RCTs and observational studies involves trade-offs between internal validity (confidence in causal inference) and external validity (generalizability to real-world populations) [16] [52].
Table 1: Key Characteristics of RCTs and Observational Studies in CER
| Characteristic | Randomized Controlled Trials (RCTs) | Observational Studies |
|---|---|---|
| Primary Strength | High internal validity through randomization [52] | Superior external validity/generalizability [52] |
| Confounding Control | Controls for both measured and unmeasured confounders [53] | Can only adjust for measured and adequately captured confounders [53] |
| Patient Population | Highly selected, homogeneous [52] | Broad, heterogeneous, reflects "real-world" practice [16] [52] |
| Cost & Feasibility | Expensive, time-consuming, sometimes ethically impractical [16] [23] | Typically faster and more cost-efficient [23] |
| Key Limitation | Limited generalizability to broader populations [52] | Susceptibility to unmeasured confounding and selection bias [53] [16] |
Comparative Evidence on Treatment Effect Estimates
A systematic landscape review investigated the comparability of relative treatment effects from RCTs and observational studies across therapeutic areas, analyzing 74 pairs of pooled effect estimates from 29 systematic reviews [55]. The results revealed both concordance and notable divergence:
- No statistically significant difference was found in 79.7% of comparisons between RCT and observational study effect estimates [55].
- Extreme differences (ratio < 0.7 or > 1.43) occurred in 43.2% of pairs [55].
- Significant differences with opposite directions of effect were observed in 17.6% of pairs, indicating potentially serious confounding [55].
These findings underscore that while many observational studies produce results comparable to RCTs, a substantial proportion show significant variation, highlighting the persistent risk of bias [55].
The E-Value: A Tool for Quantifying Unmeasured Confounding
Definition and Calculation
The E-value is a quantitative sensitivity analysis tool that assesses the minimum strength of association that an unmeasured confounder would need to have with both the exposure and the outcome to fully explain away an observed association [53]. A larger E-value suggests that stronger unmeasured confounding would be required to nullify the observed effect, providing more confidence in the result.
The E-value is calculated based on the observed risk ratio (RR) using a straightforward formula. For a risk ratio greater than 1.0, the calculation is:
E-value = RR + √[RR × (RR - 1)] [53]
The same approach applies to odds ratios and hazard ratios when the outcome is rare [53]. The E-value can also be calculated for the confidence interval, indicating the strength of confounding needed to shift the confidence interval to include the null value [53].
Applied Example: Antidepressants in Pregnancy and Miscarriage Risk
A meta-analysis examining the association between first-trimester antidepressant use and miscarriage risk found a combined risk ratio (RR) of 1.41 [53]. Applying the E-value formula:
- E-value = 1.41 + √[1.41 × (1.41 - 1)] = 2.17
This E-value of 2.17 indicates that an unmeasured confounder would need to be associated with both antidepressant use and miscarriage by a risk ratio of at least 2.17-fold each to fully explain away the observed association [53]. The researchers then assessed plausible confounders:
- Substantial alcohol use was associated with antidepressant use (RR~EU~ = 10.25) and miscarriage (RR~UD~ = 3.1), both exceeding the E-value of 2.17, suggesting alcohol could plausibly explain the association [53].
- Smoking had an association with antidepressant use (RR~EU~ = 2.06), slightly below the E-value, and an association with miscarriage (RR~UD~ = 1.32) below the required strength (RR~UD~ = 2.3), making it less likely to fully explain the association on its own [53].
Figure 1: Causal Diagram of Antidepressants and Miscarriage with Plausible Confounders. The E-value of 2.17 indicates both paths (exposure-confounder and confounder-outcome) must have RR ≥ 2.17 to explain away the observed association. Alcohol meets this criterion, while smoking does not [53].
Joint Bounding Factor and E-Value Extensions
Beyond the basic E-value, Ding and VanderWeele introduced the joint bounding factor (B), which describes different combinations of the confounder-exposure (RR~EU~) and confounder-outcome (RR~UD~) associations that would have the joint minimum strength to explain away the observed association [53]. The relationship is defined as:
B = (RR~EU~ × RR~UD~) / (RR~EU~ + RR~UD~ - 1) [53]
The E-value represents the special case where RR~EU~ = RR~UD~ [53]. This extension allows researchers to assess scenarios where the strength of association differs for the confounder-exposure and confounder-outcome relationships, as demonstrated in the smoking example above.
Methodological Protocols for Confounding Assessment
Protocol for E-Value Sensitivity Analysis
- Calculate Effect Estimate: Obtain the adjusted risk ratio, odds ratio (if outcome is rare), or hazard ratio (if outcome is rare) from the observational analysis [53].
- Compute E-value: Apply the E-value formula to the point estimate and to the confidence interval limits [53].
- Interpret E-value: Assess the magnitude of the E-value in context of the research question - larger E-values indicate more robust associations [53].
- Evaluate Plausible Confounders: Identify known risk factors for the outcome that are associated with the exposure but not adequately measured in the study. Estimate their potential strength with both exposure and outcome based on existing literature [53].
- Compare Strengths: Determine if the known or suspected confounders have associations strong enough to explain away the observed effect by comparing them to the E-value [53].
Protocol for Harmonizing RCTs and Observational Studies
When comparing effect estimates between RCTs and observational studies, a structured harmonization approach is essential [56]:
- Harmonize Study Protocols: Define eligibility criteria, treatment strategies, outcome definitions, start/end of follow-up, and causal contrast to ensure both studies target the same causal effect [56].
- Harmonize Data Analysis: Align statistical approaches to estimate the same causal contrast (e.g., intention-to-treat or per-protocol effects) [56].
- Conduct Sensitivity Analyses: Investigate the impact of discrepancies that could not be accounted for in the harmonization process, potentially including E-value analysis for the observational component [56].
Figure 2: Workflow for Comparing RCT and Observational Study Estimates. Systematic harmonization ensures meaningful "apples-to-apples" comparisons rather than "apples-to-oranges" [56].
Advanced Considerations in Confounding Adjustment
Confounder Adjustment with Multiple Risk Factors
A methodological review of 162 observational studies investigating multiple risk factors found substantial variation in confounder adjustment methods [57]. The most appropriate approach—adjusting for potential confounders separately for each risk factor-outcome relationship—was used in only 6.2% of studies [57]. The most common method was mutual adjustment (including all risk factors in a single multivariable model), which was employed in over 70% of studies but can lead to overadjustment bias and misleading effect estimates [57].
Time-Varying Treatments and Confounding
In longitudinal observational data with time-varying treatments, traditional propensity score methods may be inadequate if they only use baseline covariates [58]. A mapping review found that 25% of studies with time-varying treatments potentially used propensity score methods inappropriately [58]. More advanced methods like inverse probability weighting (IPW) for time-varying exposures are better suited for these scenarios but were used in only 45% of applicable studies [58].
Research Reagent Solutions: Methodological Tools
Table 2: Key Methodological Tools for Confounding Assessment and Adjustment
| Method/Tool | Primary Function | Key Applications | Important Considerations |
|---|---|---|---|
| E-Value | Quantifies minimum unmeasured confounder strength needed to explain away an effect [53] | Sensitivity analysis for unmeasured confounding in observational studies | Does not prove absence of confounding; context-dependent interpretation [53] |
| Propensity Score | Balances measured covariates between treatment groups [54] | Reduces confounding in observational studies; creates comparable groups | Requires all confounders are measured; different variants (matching, weighting, stratification) [54] |
| Inverse Probability Weighting | Creates a pseudo-population where treatment is independent of covariates [58] | Handles time-varying confounding; marginal structural models | Particularly important for longitudinal data with time-varying treatments [58] |
| G-Computation | Models potential outcomes under different treatment scenarios [54] | Estimates marginal treatment effects; useful for policy decisions | Relies on correct model specification; can be computationally intensive [54] |
| Doubly Robust Methods | Combines outcome regression and propensity score models [54] | Provides unbiased estimates if either the outcome or propensity model is correct | More robust to model misspecification than single-method approaches [54] |
Unmeasured confounding remains a fundamental challenge in observational studies of pharmaceutical comparative effectiveness. The E-value provides a valuable, easily interpretable tool for quantifying the potential impact of unmeasured confounders, enhancing the transparent interpretation of observational research findings [53]. No single study design is universally superior; rather, RCTs and observational studies serve as complementary partners in the evolution of medical evidence [52]. Well-designed RCTs provide high internal validity, while well-conducted observational studies with appropriate confounding adjustment, including sensitivity analyses for unmeasured factors, offer essential information about real-world effectiveness across diverse patient populations [16] [52]. Through careful methodological approaches, including structured harmonization protocols and appropriate sensitivity analyses, researchers can better interpret the consistency and discrepancies between these complementary evidence sources.
Randomized controlled trials (RCTs) represent the gold standard for evaluating pharmaceutical efficacy, but their validity can be severely compromised by post-randomization pitfalls. Two critical challenges—non-adherence to prescribed treatment regimens and loss to follow-up—can introduce substantial bias that undermines the integrity of trial results. These issues become particularly significant when framing the comparative effectiveness of pharmaceuticals between RCTs and observational studies, as they represent fundamental methodological distinctions with direct implications for result interpretation.
Non-adherence occurs when participants do not follow the prescribed treatment protocol, potentially blurring the distinction between intervention and control groups. Loss to follow-up arises when researchers cannot collect outcome data on all randomized participants, creating potentially systematic gaps in the evidence. Understanding the magnitude, impact, and mitigation strategies for these challenges is essential for researchers, scientists, and drug development professionals who must critically appraise evidence from both RCTs and observational studies.
Quantifying the Problems: Prevalence and Impact
Loss to Follow-up: Calculation and Consequences
Loss to follow-up represents a critical threat to trial validity because patients lost often have systematically different prognoses than those who complete the study. Proper calculation requires using the correct denominator—all randomly assigned participants in an RCT, not just those who received treatment or provided data [59].
Table 1: Loss to Follow-up Calculation Example in a Hypothetical RCT
| Study Group | Randomized Patients | Patients Analyzed | Incorrect LTF Calculation | Correct LTF Calculation |
|---|---|---|---|---|
| Group A | 61 | 40 | 9/49 = 18% | 21/61 = 34% |
| Group B | 59 | 41 | 11/52 = 21% | 18/59 = 31% |
The impact of loss to follow-up can be quantified through worst-case scenario analyses. For instance, in a trial comparing artificial disc replacement (ADR) with fusion where ADR initially shows half the rate of adjacent segment disease (25% vs. 50%), assuming all lost ADR patients had events and all lost fusion patients did not would equalize outcomes at 40% for both groups, fundamentally altering conclusions [59].
Table 2: Impact Thresholds for Loss to Follow-up
| Loss Level | Potential Bias Impact | Recommended Action |
|---|---|---|
| <5% | Minimal bias | Unlikely to affect conclusions |
| 5-20% | Moderate bias potential | Requires sensitivity analysis |
| >20% | Serious threat to validity | Results interpretation severely compromised |
Non-Adherence: Prevalence and Predictors
Medication non-adherence is particularly problematic in older adult populations, where polypharmacy is common. The World Health Organization estimates adherence to long-term therapies in the general population is approximately 50%, with even lower rates in low- and middle-income countries [60]. A systematic review of 37 randomized studies involving 28,600 participants identified multiple predictors of non-adherence, including complex medication regimens, multiple dosage forms, and limited health literacy [60].
Methodological Approaches for Handling Post-Randomization Pitfalls
Experimental Protocols for Minimizing and Measuring Adherence
Digital Adherence Monitoring Protocol Recent advances in digital adherence technologies (DAT) provide sophisticated methodological approaches for monitoring and improving adherence in clinical trials. A comprehensive meta-analysis of 19 RCTs involving over 10,000 tuberculosis patients demonstrated that DAT significantly improved medication adherence compared to directly observed therapy, with a pooled odds ratio of 2.853 (95% CI: 2.144-3.796; p < 0.001) [61].
The experimental workflow involves:
- Technology Selection: Choosing appropriate DAT based on context (SMS reminders, video-observed therapy, medication event reminder monitors, biometric monitoring systems, or ingestible sensors)
- Implementation: Integrating technology into treatment regimen with patient training
- Data Collection: Capturing adherence metrics electronically
- Analysis: Comparing adherence rates between intervention and control groups
Subgroup analyses revealed differential effectiveness by technology type, with the highest effect sizes seen in ingestion sensors and biometric monitoring systems, though with wider confidence intervals [61].
Multi-Component Adherence Intervention Protocol For complex clinical conditions, especially in older adults with polypharmacy, educational and behavioral interventions combined with regimen simplification have demonstrated effectiveness. A systematic review found that interventions delivered by pharmacists and nurses showed better results in improving adherence and outcomes than those delivered by general practitioners [60].
Key methodological components include:
- Screening: Identify non-adherent patients and determine the type of non-adherence
- Patient Education: Provide comprehensive information about treatment purpose and consequences of omission
- Regimen Simplification: Reduce dosing complexity and medication burden
- Follow-up Education: Offer ongoing feedback and reinforcement
Adherence Intervention Workflow
Statistical Handling of Missing Data
Worst-Case Scenario Analysis Protocol When loss to follow-up occurs despite prevention efforts, statistical methods can quantify its potential impact on results. The worst-case scenario analysis provides a systematic approach:
- Calculate Event Rates: Determine observed event rates in each study group
- Define Worst Case: Assume all participants lost to follow-up in the treatment group had unfavorable outcomes
- Define Best Case: Assume all participants lost to follow-up in the control group had favorable outcomes
- Recalculate Outcomes: Compute revised event rates under these extreme assumptions
- Compare Results: Determine whether conclusions would change under these scenarios
This method provides a sensitivity analysis that helps researchers and readers understand the robustness of trial findings to missing data [59].
Comparative Evidence: RCTs vs. Observational Studies
Quantitative Comparison of Treatment Effects
A systematic landscape review of 29 systematic reviews across 7 therapeutic areas directly compared relative treatment effects between RCTs and observational studies. The analysis of 74 pairs of pooled relative effect estimates revealed both consistencies and divergences [55].
Table 3: Comparison of Relative Treatment Effects Between RCTs and Observational Studies
| Comparison Metric | Percentage of Pairs | Interpretation |
|---|---|---|
| No statistically significant difference | 79.7% | Majority show consistency |
| Extreme difference (ratio <0.7 or >1.43) | 43.2% | Substantial variation in magnitude |
| Significant difference with opposite direction | 17.6% | Clinically important discrepancy |
The sources of variation between RCTs and observational studies may stem from differences in patient populations, biased estimates arising from study design, or analytical methodologies. This has important implications for the broader thesis on comparative effectiveness research, suggesting that while observational studies often provide similar results, significant discrepancies occur in a substantial minority of cases [55].
Methodological Strengths and Limitations
The fundamental distinction in handling post-randomization pitfalls between RCTs and observational studies lies in their design. RCTs benefit from randomization to balance both known and unknown confounders, but remain vulnerable to post-randomization biases. Observational studies typically have more complete follow-up in real-world settings but face greater challenges with unmeasured confounding [15].
Study Design Comparison
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Research Reagents and Solutions for Addressing Post-Randomization Pitfalls
| Tool Category | Specific Solutions | Function and Application |
|---|---|---|
| Adherence Monitoring Technologies | Medication Event Reminder Monitors (MERM), Ingestible Sensors (IS), Biometric Monitoring Systems (BMS) | Electronically capture medication ingestion or dosing events to objectively measure adherence [61] |
| Digital Communication Platforms | Video-Observed Therapy (VOT), SMS Reminder Systems | Enable remote supervision and reminders for medication adherence without physical presence [61] |
| Statistical Analysis Packages | Multiple Imputation Software, Worst-Case Scenario Analysis Tools | Handle missing data through sophisticated modeling and sensitivity analyses [59] |
| Patient-Reported Outcome Measures | Validated Adherence Scales, Quality of Life Instruments | Capture subjective experiences and self-reported adherence behaviors [60] |
| Data Integration Systems | Electronic Health Record Interfaces, Claims Data Linkages | Combine multiple data sources to enhance follow-up completeness [15] |
Post-randomization pitfalls represent fundamental methodological challenges that differentially affect RCTs and observational studies in pharmaceutical effectiveness research. While loss to follow-up threatens RCT validity by potentially introducing systematic bias, non-adherence blurs the distinction between treatment groups and may dilute treatment effect estimates. The comparative effectiveness framework reveals that each study design offers complementary strengths—RCTs provide greater internal validity through randomization, while observational studies may better reflect real-world adherence patterns and have more complete follow-up.
Methodological advances in digital adherence technologies and sophisticated statistical approaches for handling missing data continue to improve researchers' ability to address these challenges. For drug development professionals, critical appraisal of both RCTs and observational studies requires careful assessment of how these post-randomization pitfalls have been addressed, as they significantly impact the validity and generalizability of evidence informing pharmaceutical development and clinical practice.
Strategies for Enhancing Data Quality and Standardization in Observational Studies
The comparative effectiveness of pharmaceuticals is typically established through Randomized Controlled Trials (RCTs), which serve as the gold standard for regulatory decision-making due to their experimental designs that minimize bias [55]. However, in recent decades, observational studies using real-world data (RWD) have increasingly supplemented our understanding of treatment benefits and risks in broader patient populations [55]. This expansion has created an urgent need for robust strategies to enhance data quality and standardization in observational research, particularly as healthcare decision-makers explore expanding the use of real-world evidence (RWE) for regulatory purposes.
The critical importance of data quality emerges from systematic comparisons of treatment effects derived from different study designs. A comprehensive 2021 review examining 74 pairs of pooled relative effect estimates from RCTs and observational studies found that while there was no statistically significant difference in 79.7% of comparisons, extreme differences (ratio < 0.7 or > 1.43) occurred in 43.2% of pairs, with 17.6% showing significant differences pointing in opposite directions [55]. These discrepancies underscore the potential consequences of poor data quality, which can lead to misleading conclusions about therapeutic effectiveness and safety.
This guide objectively compares frameworks, methodologies, and tools for enhancing observational data quality, providing researchers with evidence-based strategies to strengthen the reliability of real-world evidence in pharmaceutical research.
Comparative Evidence: Treatment Effects from RCTs vs. Observational Studies
Understanding the relationship between RCT and observational study results provides critical context for why data quality initiatives matter in comparative effectiveness research.
Table 1: Comparison of Treatment Effect Estimates from RCTs vs. Observational Studies
| Analysis Focus | Number of Comparisons | Agreement Rate | Extreme Difference Rate | Opposite Direction Effects |
|---|---|---|---|---|
| Overall comparison | 74 pairs from 29 reviews | 79.7% showed no significant difference | 43.2% showed extreme differences | 17.6% showed significant differences in opposite directions |
| Pharmaceutical interventions only | Not specified | Ratio of ratios: 1.12 (95% CI 1.04-1.21) | Not specified | Not specified |
A more recent Cochrane review encompassing 47 systematic reviews and 34 primary analyses reinforced these findings, indicating that effect estimates of RCTs and observational studies differ only very slightly on average (ratio of ratios 1.08, 95% CI 1.01 to 1.15) [51]. This comprehensive analysis included 2,869 RCTs with 3,882,115 participants and 3,924 observational studies with 19,499,970 participants, providing substantial power to detect differences between study designs [51].
These findings suggest that while observational studies can produce similar effect estimates to RCTs on average, the substantial variation in a significant minority of comparisons highlights the need for rigorous data quality management to identify and mitigate sources of bias that may lead to discrepant results.
Strategic Frameworks for Data Quality Enhancement
Foundational Data Governance Structures
Implementing a strategic framework is essential before addressing individual data errors. This foundation establishes the rules, roles, and structures that govern data across an organization.
Institute Robust Data Governance: Effective data governance defines the policies, standards, and procedures for how data is collected, stored, used, and protected across the entire data lifecycle [62]. This framework clarifies ownership and accountability through a data governance council comprising stakeholders from various departments, complemented by data stewards responsible for overseeing data quality within specific business domains [62].
Develop a Data Quality Plan: This formal document translates high-level strategy into an actionable roadmap with specific, measurable objectives tied to business outcomes [62]. A comprehensive plan defines data quality dimensions (accuracy, completeness, consistency, timeliness, validity) and establishes clear standards for data formats, definitions, and acceptable values [62].
Implement Master Data Management (MDM): MDM addresses the challenge of critical data fragmentation across multiple systems by centralizing this information into an authoritative "single source of truth" [62]. This discipline ensures all departments work from consistent, reliable data, fundamentally enhancing data quality at an enterprise scale.
Core Data Quality Improvement Processes
Once strategic frameworks are established, organizations can implement tactical processes for identifying and correcting data quality issues through a systematic approach.
Table 2: Core Data Quality Improvement Processes and Methodologies
| Process Stage | Key Activities | Tools and Techniques |
|---|---|---|
| Data Profiling and Analysis | Analyze datasets to understand structure, content, and quality; identify missing values, patterns, and outliers | Data profiling tools, automated scanning |
| Data Cleansing and Standardization | Correct errors in existing data; remove duplicates; fill missing values; transform to consistent formats | Data scrubbing tools, standardization algorithms |
| Proactive Data Validation | Implement validation rules at point of data entry; verify formats; ensure completeness; check against acceptable values | Automated validation rules, mandatory field requirements |
| Continuous Monitoring | Track data against quality metrics; set up dashboards and alerts; detect issues proactively | Monitoring dashboards, automated alerts, KPI tracking |
These processes form a continuous cycle of assessment, improvement, and monitoring that maintains data quality over time [62]. The approach shifts from reactive cleanup of existing problems to proactive prevention of future data quality issues.
Standardization Approaches for Observational Research Data
Common Data Models and Standardized Vocabularies
Data standardization addresses the fundamental challenge of healthcare data variability across organizations, where information is collected for different purposes (provider reimbursement, clinical research, direct patient care) and stored in different formats using diverse database systems [63].
The OMOP Common Data Model (CDM) has emerged as a prominent open community standard designed to standardize the structure and content of observational data [63]. This approach transforms data from disparate databases into a common format and common representation using standardized terminologies, then performs systematic analyses using libraries of standard analytic routines written based on this common format [63].
The OHDSI standardized vocabularies are a central component of the OMOP CDM, allowing organization and standardization of medical terms across various clinical domains [63]. These vocabularies enable standardized analytics that leverage knowledge bases when constructing exposure and outcome phenotypes for characterization, population-level effect estimation, and patient-level prediction studies [63].
Clinical Research Data Standards
Beyond common data models, comprehensive standards have been developed to support the entire research lifecycle. The Clinical Data Interchange Standards Consortium (CDISC) has developed a global, open-access suite of clinical and translational research data standards that support everything from structured protocol information through data collection, exchange, tabulation, analysis, and reporting [64].
These standards include:
- Controlled terminology through the National Cancer Institute's Enterprise Vocabulary Services
- MedDRA (Medical Dictionary for Regulatory Activities) for medical history in clinical trials and adverse events reporting
- HL7 (Health Level Seven) for structured product labels and ECG waveforms
- LOINC (Logical Observation Identifiers Names and Codes) for clinical laboratory tests and observations [64]
The implementation of these standards from the beginning of research studies can reduce study start-up times by 70% to 90% since standard case report forms, edit checks, and validation documentation already exist and can be reused from trial to trial [64].
Experimental Protocols for Data Quality Validation
Machine Learning-Based Quality Improvement
Recent research has demonstrated the effectiveness of machine learning approaches for addressing specific data quality challenges in healthcare datasets. The following experimental protocol outlines a comprehensive methodology for improving data quality using ML techniques, validated in a study published in Frontiers in Artificial Intelligence [65].
Table 3: Experimental Protocol for Machine Learning-Based Data Quality Improvement
| Protocol Phase | Activities and Methods | Outcomes and Metrics |
|---|---|---|
| Data Preparation | Use publicly available diabetes dataset (768 records, 9 variables); perform exploratory analysis with Python tools | Baseline assessment of data completeness (90.57%) |
| Missing Data Imputation | Apply K-nearest neighbors (KNN) imputation to address missing values | Data completeness improved to nearly 100% |
| Anomaly Detection | Implement ensemble techniques (Isolation Forest, Local Outlier Factor) | Identification and mitigation of anomalies improving accuracy |
| Feature Analysis | Apply Principal Component Analysis (PCA) and correlation analysis | Identification of key predictors (Glucose, BMI, Age) |
| Predictive Validation | Train and test Random Forest and LightGBM models | Random Forest achieved 75.3% accuracy, AUC 0.83 |
This experimental design demonstrates that integrating advanced machine learning techniques with rigorous data preprocessing significantly enhances healthcare data quality across multiple dimensions [65]. The methodology was fully documented with reproducibility tools to ensure the approach could be replicated and extended [65].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing effective data quality strategies requires specific tools and methodologies. The following table details key solutions used in successful data quality improvement initiatives.
Table 4: Research Reagent Solutions for Data Quality Enhancement
| Tool Category | Specific Solutions | Function and Application |
|---|---|---|
| Data Quality Tools | Automated data profiling tools, deduplication algorithms, monitoring dashboards | Identify data quality issues; merge duplicate records; provide real-time visibility into data health |
| Standardization Frameworks | OMOP Common Data Model, CDISC standards, OHDSI standardized vocabularies | Transform disparate data into common format; enable collaborative research and large-scale analytics |
| Machine Learning Libraries | K-nearest neighbors imputation, Isolation Forest, Local Outlier Factor | Address missing values; detect and correct anomalies in healthcare datasets |
| Reporting Guidelines | TARGET 2025, STROBE extensions, EQUATOR Network frameworks | Enhance transparent reporting; improve clarity and interpretation of observational studies |
These tools form a comprehensive ecosystem for addressing data quality challenges throughout the research lifecycle, from initial data collection through final analysis and reporting.
Visualization of Data Quality Improvement Workflows
Conceptual Framework for Healthcare Data Quality
The following diagram illustrates the core dimensions of healthcare data quality and the integration of technical and organizational strategies for improvement:
This conceptual framework aligns with established data quality literature, emphasizing that healthcare data quality hinges on three core dimensions—accuracy, completeness, and reusability—while integrating both technical and organizational approaches to ensure consistent, reliable, and adaptable data [65].
Data Quality Management Workflow
The following diagram illustrates the systematic workflow for implementing and maintaining data quality initiatives:
This workflow emphasizes that data quality management is a continuous cycle rather than a one-time project [62]. The process begins with establishing governance structures and progresses through planning, implementation, and ongoing monitoring to maintain high standards over time.
Enhancing data quality and standardization in observational studies requires a multifaceted approach combining strategic frameworks, technical processes, standardized data models, and advanced methodologies like machine learning. The evidence suggests that while observational studies can produce effect estimates similar to RCTs in most cases, significant discrepancies in a substantial minority of comparisons highlight the critical importance of robust data quality management.
Implementation of these strategies enables observational studies to more reliably contribute to comparative effectiveness research, potentially bridging evidence gaps when RCTs are infeasible or insufficient for understanding treatment effects in diverse real-world populations. As regulatory bodies increasingly consider real-world evidence in decision-making, the systematic enhancement of data quality through these approaches becomes essential for generating reliable evidence to guide therapeutic development and clinical practice.
Head-to-Head Comparisons and Synthesized Evidence for Decision-Making
When Do RCTs and Observational Studies Agree? Analyzing Concordant and Discordant Results
For researchers, scientists, and drug development professionals, the comparative effectiveness of evidence derived from Randomized Controlled Trials (RCTs) and observational studies is a fundamental concern. RCTs are traditionally considered the gold standard for causal inference due to their design, which minimizes confounding and selection bias through random assignment [9] [8]. However, in the era of big data and advanced analytics, observational studies using routinely collected healthcare data (RCD) are increasingly used to answer real-world questions when RCTs are impractical, unethical, or too costly [15] [9]. This guide objectively compares the performance of these two methodological approaches by analyzing the conditions under which their results align or diverge, providing a structured overview of the supporting empirical data.
Quantitative Concordance: A Meta-Analytic Perspective
A systematic review and meta-analysis of studies explicitly aiming to emulate a target RCT provides the most direct quantitative evidence on concordance. This analysis, which included 82 TTE-RCT (Target Trial Emulation-RCT) pairs, offers a high-level summary of agreement.
Table 1: Overall Concordance Between Trial Emulations and RCTs
| Metric | Summary Result | Interpretation |
|---|---|---|
| Pearson Correlation Coefficient | 0.55 (95% CI: 0.38 to 0.69) | Moderate correlation between effect estimates from emulations and RCTs [66]. |
| Summary Relative Odds Ratio (ROR) | 0.99 (95% CI: 0.94 to 1.03) | On average, the effect estimates from emulations and RCTs are nearly identical. An ROR of 1.0 indicates perfect agreement [66]. |
| Statistical Heterogeneity (I²) | 66% | High degree of variability in agreement across the studied pairs, indicating that concordance is highly context-dependent [66]. |
The high heterogeneity suggests that agreement is not uniform. Subgroup analyses reveal that concordance improves significantly under specific conditions and deteriorates for certain outcomes.
Table 2: Factors Influencing Concordance
| Factor | Impact on Concordance | Key Findings |
|---|---|---|
| Emulation Design Quality | Positive Impact | In 38 pairs with closer emulation designs, the Pearson correlation was significantly higher: 0.86 (95% CI: 0.77 to 0.92) [66]. |
| Specific Clinical Outcomes | Variable Impact | Systematic underestimation of treatment effects was observed for:- Venous Thromboembolism (ROR = 0.76, 95% CI: 0.59 to 0.98)- Major Adverse Cardiovascular Events (ROR = 0.93, 95% CI: 0.89 to 0.97) [66] |
| Population Characteristics | Negative Impact | Differences in baseline age and sex composition between the emulation and the RCT impaired concordance (p < 0.05) [66]. |
| Treatment Context | Negative Impact | Initiation of treatment during a hospitalization period was associated with poorer agreement [66]. |
Experimental Protocols for Benchmarking Observational Analyses
A key methodology for assessing the validity of observational studies is "benchmarking," where an observational analysis is explicitly designed to answer the same question as an existing RCT. The protocol and results from a study on endocrine therapies in breast cancer provide a detailed case study.
Detailed Methodology: Emulating the BIG 1-98 Trial
Target Trial: The Breast International Group (BIG 1-98) randomized trial, which compared the effect of letrozole and tamoxifen on the risk of death in postmenopausal women with hormone-receptor positive breast cancer [67].
Emulation Goal: To design a target trial emulation that asked the same question as BIG 1-98 using Swedish registry data [67].
Experimental Protocol:
- Protocol Drafting: Define the target trial's key components explicitly before analyzing the observational data. This includes specifying eligibility criteria, treatment strategies, assignment procedures, follow-up, outcome, and contrast of interest (e.g., intention-to-treat vs. per-protocol).
- Data Source Identification: Secure access to high-quality, linked administrative and clinical registries that capture the required data on patient demographics, drug prescriptions, cancer diagnoses, and vital status.
- Cohort Construction: Apply the predefined eligibility criteria to the registry data to identify the emulated trial population. This includes identifying postmenopausal women with a diagnosis of hormone-receptor-positive breast cancer who initiated either letrozole (aromatase inhibitor) or tamoxifen.
- Outcome Ascertainment: Link the cohort to death registries to ascertain all-cause mortality, the primary outcome.
- Statistical Analysis: Estimate the treatment effect, such as the 5-year risk difference and associated confidence intervals, using appropriate statistical methods for causal inference.
Discordant Results and Protocol Refinement
The primary emulation analysis produced a discordant result: it showed an increased risk of death with aromatase inhibitors compared to tamoxifen [5-year risk difference = 2.5% (95% CI, 0.2% to 4.6%)], whereas the BIG 1-98 trial found letrozole to be superior [67].
This discordance prompted a sensitivity analysis as part of the experimental protocol:
- Refined Analysis: The observational analysis was restricted to non-users of opioids or antidepressants, addressing potential unmeasured confounding related to underlying health status or palliative care.
- Result: This restriction led to more closely aligned estimates [risk difference = -0.9% (95% CI, -4.2% to 2.0%)], which were no longer discordant with the RCT [67].
This case demonstrates that even with careful alignment of eligibility criteria, additional population restrictions may be necessary to account for confounding factors not measured in the original RCT.
The Critical Role of Sensitivity Analysis in Observational Studies
Sensitivity analysis is a crucial protocol for assessing the robustness of findings, particularly in observational studies based on RCD. A systematic review of 256 observational studies of drug treatment effects reveals how this practice is applied and its impact.
Table 3: Sensitivity Analysis Practices in Observational Studies
| Aspect | Finding | Implication |
|---|---|---|
| Prevalence of Use | 59.4% (152 of 256 studies) conducted sensitivity analyses [68]. | Over 40% of studies conducted no sensitivity analysis, which is a significant methodological shortcoming [68]. |
| Common Types | Categorized into three dimensions [68]:1. Alternative Study Definitions (e.g., exposure/outcome algorithms)2. Alternative Study Designs (e.g., different data sources)3. Alternative Modeling (e.g., statistical strategies, E-value) | The most common inconsistencies with primary analyses came from alternative study definitions (59 instances) [68]. |
| Frequency of Discordance | 54.2% (71 of 131 studies) showed significant differences between primary and sensitivity analyses [68]. | Inconsistencies are not rare but are a common feature of observational research. |
| Average Effect Size Difference | 24% (95% CI: 12% to 35%) average difference in effect size between primary and sensitivity analyses when they were inconsistent [68]. | The magnitude of variation can be substantial, enough to change the interpretation of a finding. |
| Reporting and Interpretation | Only 9 of the 71 studies with inconsistent results discussed the potential impact of these inconsistencies [68]. | There is a critical gap in the interpretation of sensitivity analyses, as most studies ignored or downplayed divergent results. |
Visualizing the Pathway to Concordance
The following diagram maps the key factors that determine whether the results of an observational study and an RCT are likely to agree or disagree, based on the evidence presented.
Factors Influencing RCT-Observational Study Concordance
The Scientist's Toolkit: Key Reagents for Robust Observational Research
For researchers embarking on comparative effectiveness studies using real-world data, the following methodological "reagents" are essential.
Table 4: Essential Reagents for Observational Study Design and Analysis
| Research Reagent | Function | Application Note |
|---|---|---|
| Target Trial Emulation (TTE) Framework | Provides a structured protocol for designing observational studies to mimic the hypothetical RCT that would answer the same question. | Enhances causal reasoning and design clarity. Successful application shown to significantly improve concordance with RCTs [66]. |
| High-Quality, Linked Databases | Serves as the data source for the emulation, containing information on patient demographics, drug exposures, clinical outcomes, and potential confounders. | Multi-source linked databases (e.g., Swedish registries) are particularly valuable for improving population alignment and outcome ascertainment [66] [67]. |
| Causal Inference Methods | A suite of analytical techniques (e.g., propensity scores, inverse probability weighting) and frameworks (e.g., Directed Acyclic Graphs - DAGs) to address measured confounding. | Forces explicit definition of exposures, confounders, and design interventions, thereby reducing bias in the analysis [9]. |
| E-Value | A metric to quantify the required strength of association an unmeasured confounder would need to have to fully explain away an observed treatment-outcome association. | Helps assess robustness to unmeasured confounding in a concrete, intuitive way [68] [9]. |
| Sensitivity Analysis Protocol | A pre-planned set of analyses testing how the results change under alternative study definitions, designs, or statistical models. | Critical for assessing result robustness. Inconsistencies here often reveal hidden biases, yet are frequently under-discussed [68]. |
The body of evidence demonstrates that observational studies and RCTs can achieve a high degree of concordance, but this agreement is not automatic. It is contingent upon rigorous methodological execution, including close emulation of the target trial's design, precise alignment of population characteristics, and high-quality outcome ascertainment. Furthermore, the conduct and, most importantly, the thoughtful interpretation of comprehensive sensitivity analyses are non-negotiable for validating findings from observational data. For drug development professionals and researchers, this underscores that the value of real-world evidence is proportional to the methodological rigor applied in its generation. When these conditions are met, observational studies become a powerful and reliable tool in the comparative effectiveness arsenal, capable of complementing and extending the evidence derived from RCTs.
Within pharmaceutical research, two foundational pillars for generating evidence on drug effects are Randomized Controlled Trials (RCTs) and observational studies. The choice between these methodologies is a critical strategic decision, as each offers a distinct set of advantages and limitations. RCTs, long considered the gold standard for establishing efficacy, utilize random assignment to minimize bias and provide high internal validity [4] [9]. Conversely, observational studies, which observe the effects of exposures in real-world settings without intervention, are indispensable for assessing long-term safety, effectiveness in broader populations, and clinical outcomes where RCTs are unethical or infeasible [69] [16]. This guide provides a detailed, objective comparison of these two approaches, equipping researchers and drug development professionals with the data needed to select the appropriate methodological tool for their specific research question.
Detailed Comparison Table
The following table summarizes the core strengths and weaknesses of RCTs and observational studies across key methodological dimensions.
Table 1: Comparative Strengths and Weaknesses of RCTs and Observational Studies
| Dimension | Randomized Controlled Trials (RCTs) | Observational Studies |
|---|---|---|
| Internal Validity (Bias Control) | High. Randomization balances both known and unknown confounders at baseline, providing the strongest control for bias [4] [9]. | Variable, often lower. Susceptible to confounding and other biases; control relies on statistical adjustment for known and measured confounders [69]. |
| External Validity (Generalizability) | Can be limited. Narrow eligibility criteria and controlled settings may not reflect "real-world" patients or practice [16] [9]. | Generally higher. Study populations are often more representative of actual clinical practice and broader patient groups [69] [9]. |
| Primary Utility | Establishing efficacy – whether a treatment can work under ideal conditions [16]. | Assessing effectiveness – whether a treatment does work in routine practice, and monitoring long-term safety [16] [9]. |
| Key Strengths | • Strongest evidence for causal inference [9]• Controls for unmeasured confounding [4]• Prospective, controlled protocol | • Can investigate questions where RCTs are unethical (e.g., harmful exposures) [4] [69]• Suitable for rare or long-term outcomes [4] [69]• Generally less expensive and faster to conduct [69] |
| Key Limitations | • High cost and resource intensity [2]• Ethical or feasibility constraints for some questions [4]• May be underpowered for rare adverse events [4] | • Cannot fully rule out unmeasured confounding [69]• Findings can be influenced by selection and information bias [69]• Requires sophisticated methods for valid analysis |
| Quantitative Comparison | A 2021 review found no statistically significant difference in relative treatment effects compared to observational studies in 79.7% of 74 analyzed pairs [55]. However, 43.2% of pairs showed an extreme difference (ratio <0.7 or >1.43), and 17.6% showed significant differences with effects in opposite directions [55]. |
Methodological Protocols and Innovations
Core Experimental Protocol for RCTs
The integrity of an RCT hinges on a rigorously defined and executed protocol.
- Protocol Development: A detailed study protocol is established, defining primary/secondary endpoints, inclusion/exclusion criteria, and statistical analysis plan [16].
- Randomization & Allocation Concealment: Eligible participants are randomly assigned to intervention or control groups. Allocation is concealed to prevent selection bias [4].
- Blinding (Masking): Where feasible, participants, investigators, and outcome assessors are blinded to treatment assignments to minimize performance and detection bias.
- Intervention & Follow-up: The investigational treatment and control (placebo or standard of care) are administered according to the protocol. Participants are followed prospectively for a predefined period [2].
- Outcome Assessment: Endpoints are measured using standardized definitions. Adherence to the initial treatment assignment is monitored (Intention-to-Treat analysis).
- Data Analysis: Outcomes are compared between groups using statistical methods specified a priori.
Recent innovations include adaptive, sequential, and platform trials, which allow for pre-planned modifications based on interim data, improving efficiency and ethics [9]. The integration of Electronic Health Records (EHRs) facilitates more pragmatic trials that recruit patients and assess outcomes within real-world care settings, blurring the line with observational research [9].
Core Analytical Protocol for Observational Studies
Modern observational studies aiming for causal inference employ a structured, design-based approach.
- Define the Target Trial: Explicitly specify the protocol of the hypothetical RCT that the observational study aims to emulate, including eligibility, treatment strategies, outcomes, and follow-up [9].
- Data Source Selection: Identify suitable real-world data sources (e.g., EHRs, claims databases, clinical registries) that capture the necessary variables for the defined trial.
- Cohort Construction: Apply eligibility criteria to the data to create the study cohort.
- Confounder Adjustment: To address confounding, researchers use advanced methods:
- Propensity Score Matching: Individuals exposed and unexposed to the treatment are matched based on their probability (propensity) of receiving the exposure, creating balanced comparison groups that mimic randomization [69].
- Multivariable Regression: Statistical models adjust for multiple confounders simultaneously.
- Outcome Analysis: Compare the risk of the outcome between the exposure groups in the matched or adjusted population.
- Sensitivity Analyses: Conduct analyses, such as calculating the E-value, to quantify how strong an unmeasured confounder would need to be to explain away the observed association [9].
The emergence of causal inference frameworks and the use of Directed Acyclic Graphs (DAGs) have been critical innovations, forcing researchers to explicitly articulate and test their assumptions about sources of bias [9].
Workflow and Relationship Visualizations
RCT Participant Flow
Observational Study Analysis
Essential Research Reagent Solutions
Table 2: Key Methodological "Reagents" for Pharmaceutical Research
| Research 'Reagent' (Tool/Method) | Primary Function | Common Application Context |
|---|---|---|
| Structured EHR & Claims Databases | Provides longitudinal, real-world data on patient characteristics, treatments, and outcomes for analysis. | Observational studies on drug effectiveness, safety, and patterns of care [69] [9]. |
| Clinical Registries | Systematic collection of uniform data for a population defined by a specific disease, condition, or exposure. | Monitoring quality of care, long-term safety, and comparative effectiveness; can nest RCTs [69]. |
| Propensity Score Matching | Statistical method to create balanced comparison groups by matching individuals based on their likelihood of exposure. | Reduces selection bias in observational studies to approximate the balance achieved by randomization [69]. |
| Causal Inference Frameworks (DAGs) | Provides a structured, graphical approach to explicitly map and test assumptions about causal relationships and confounding. | Planning and validating the design of observational studies to strengthen causal claims [9]. |
| Adaptive Trial Platforms | A clinical trial design that allows for pre-planned modifications based on interim data analysis. | Increases the efficiency and ethical standing of RCTs, particularly in rapidly evolving fields [9]. |
The pursuit of robust evidence for pharmaceutical decision-making extends across diverse domains, from economic evaluations to clinical effectiveness assessments. Within this landscape, a fundamental tension exists between randomized controlled trials (RCTs)—long considered the gold standard for establishing efficacy—and observational studies that capture real-world effectiveness. While RCTs minimize bias through random assignment, their controlled conditions often fail to reflect clinical practice [16]. Conversely, observational studies leverage real-world data (RWD) to examine interventions under typical care conditions but face challenges from potential confounding variables [9].
This comparative guide examines how these research approaches apply across different contexts, with particular focus on pharmacoeconomic evaluations and rare disease research. These domains present unique methodological challenges that influence how effectively RCTs and observational studies can generate evidence for healthcare decision-makers. Understanding the strengths, limitations, and appropriate applications of each method is essential for researchers, health technology assessment (HTA) bodies, and drug development professionals navigating complex evidence requirements [9] [70].
Methodological Foundations: RCTs vs. Observational Studies
Core Characteristics and Traditional View
Randomized Controlled Trials (RCTs) are experimental studies where investigators actively assign participants to intervention or control groups through random allocation. This design aims to balance both measured and unmeasured characteristics across groups, providing high internal validity for establishing causal effects under controlled conditions [9]. RCTs are particularly valuable for establishing efficacy—whether a treatment works under ideal circumstances—and remain the preferred design for regulatory approval of new pharmaceuticals [16].
Observational Studies examine the effects of exposures on outcomes without investigator intervention in treatment assignment. These studies analyze data from real-world settings, including electronic health records (EHRs), health administrative databases, and patient registries [9]. Observational designs are particularly suited for assessing effectiveness—how treatments perform in routine clinical practice—and are indispensable when RCTs are impractical, unethical, or too costly [16].
Comparative Methodological Features
Table 1: Fundamental Characteristics of RCTs and Observational Studies
| Feature | Randomized Controlled Trials (RCTs) | Observational Studies |
|---|---|---|
| Primary Purpose | Establish efficacy under ideal conditions | Assess effectiveness in real-world settings |
| Confounding Control | Randomization balances both known and unknown confounders | Statistical methods adjust only for measured confounders |
| Patient Population | Often homogeneous with strict inclusion/exclusion criteria | Heterogeneous, reflecting diverse patient characteristics |
| Intervention Context | Standardized, protocol-driven delivery | Variable, reflecting clinical practice patterns |
| Generalizability | May be limited due to selective recruitment | Typically higher due to broader, more representative populations |
| Implementation Timeline | Often lengthy and resource-intensive | Generally more rapid to implement |
| Ethical Considerations | Possible when equipoise exists | Essential when randomization is unethical |
Methodological Innovations and Convergence
Recent methodological advances have blurred the traditional boundaries between RCTs and observational studies. Pragmatic clinical trials incorporate design elements that better reflect real-world conditions, making them particularly valuable for comparative effectiveness research (CER) [71]. These trials feature broader eligibility criteria, heterogeneous practice settings, and outcome measures relevant to clinical decision-making.
Simultaneously, observational studies have embraced causal inference methods that strengthen their validity. Techniques such as propensity score matching, instrumental variable analysis, and the use of directed acyclic graphs (DAGs) help address confounding concerns [9]. The development of metrics like the E-value quantifies how robust observational study results are to unmeasured confounding [9].
Pharmacoeconomic Applications
Evidence Requirements for Economic Evaluation
Pharmacoeconomic analysis evaluates the value proposition of pharmaceutical interventions by examining both clinical and economic outcomes. These evaluations typically require comprehensive data on long-term clinical effectiveness, quality of life impacts, healthcare resource utilization, and costs—data elements often extending beyond what is captured in traditional RCTs [72].
Advanced Therapy Medicinal Products (ATMPs) exemplify the evidence challenges in modern pharmacoeconomics. A 2025 systematic review of ATMPs for rare diseases found that economic evaluations frequently rely on combined evidence from multiple sources [72]. For instance, short-term efficacy data from RCTs are often supplemented with long-term real-world evidence (RWE) from observational studies to model lifetime cost-effectiveness.
Methodological Approaches in Practice
Table 2: Pharmacoeconomic Evaluation Methods Using Different Study Designs
| Economic Evaluation Component | RCT-Based Approach | Observational Study Approach |
|---|---|---|
| Clinical Effectiveness Data | Protocol-defined efficacy endpoints | Real-world treatment effectiveness |
| Quality of Life Measurement | Research-administered instruments at predefined intervals | Patient-reported outcomes in routine care |
| Resource Utilization | Protocol-driven resource use may not reflect real patterns | Actual healthcare consumption patterns |
| Time Horizon | Trial duration with statistical extrapolation | Longer follow-up through linked data sources |
| Comparator Groups | Often placebo or standard control | Multiple contemporaneous treatment options |
| Heterogeneity Assessment | Limited by homogeneous trial populations | Broader exploration of effect modifiers |
Economic evaluations increasingly employ hybrid models that integrate evidence from both RCTs and observational studies. For example, a cost-effectiveness analysis of chimeric antigen receptor (CAR) T-cell therapies might utilize RCT data for initial response rates while incorporating observational data for long-term survival and late-effect profiles [72]. This approach acknowledges that RCTs alone are often insufficient to fully capture the economic value propositions of complex interventions across their lifecycle [71].
Rare Disease Applications
Unique Methodological Challenges
Rare disease research presents distinct challenges that fundamentally alter the RCT-observational study dynamic. The small patient populations characteristic of rare diseases make large, powered RCTs statistically problematic and often logistically impossible [73] [70]. Additionally, the heterogeneous disease manifestations and frequently rapid disease progression create ethical concerns about randomization to placebo or inferior treatments [70].
The evidence requirements for Health Technology Assessment (HTA) of orphan drugs highlight these tensions. HTA bodies typically expect robust comparative evidence, yet manufacturers of orphan drugs face obstacles including poor natural history data, small sample sizes, single-arm trials, and a paucity of established disease-specific endpoints [70]. These limitations necessitate adapted approaches to evidence generation.
Modified Approaches and Solutions
In rare disease contexts, observational studies often serve as the primary evidence source rather than merely supplementary to RCTs. Well-designed observational studies can provide critical information on natural disease history, treatment patterns, and comparative effectiveness when RCTs are not feasible [73]. The European Medicines Agency and other regulatory bodies have developed frameworks to accept RWE for orphan drug approval, particularly when treatments address severe unmet needs [70].
Methodological adaptations for rare diseases include:
- External control arms: Using natural history data or well-characterized historical cohorts as comparators for single-arm interventional studies [70]
- Prospective registry data: Collecting standardized data on disease course and outcomes across multiple centers [73]
- Matching-adjusted indirect comparisons: Statistical techniques to compare outcomes across different study populations when head-to-head trials are unavailable [70]
- Multi-stakeholder collaborations: Partnerships between researchers, patients, clinicians, and regulators to establish meaningful endpoints and study designs [70]
Quantitative Comparison of Treatment Effects
Empirical Evidence on Methodological Concordance
A 2021 systematic review published in BMC Medicine provides crucial empirical data on the comparability of relative treatment effects between RCTs and observational studies [55]. This analysis of 30 systematic reviews across 7 therapeutic areas examined 74 pairs of pooled relative effect estimates from both study designs.
The findings reveal both convergence and divergence between methodologies. While 79.7% of comparisons showed no statistically significant difference in relative effect estimates between RCTs and observational studies, 43.2% demonstrated extreme differences (ratio <0.7 or >1.43) [55]. Perhaps most notably, 17.6% of pairs exhibited both statistically significant differences and estimates pointing in opposite directions [55].
Interpretation and Implications
These quantitative findings suggest that while RCTs and observational studies frequently produce directionally similar results, the magnitude of effect estimates can differ substantially. The observed discrepancies likely stem from multiple factors, including:
- Differences in patient populations (highly selected trial participants vs. heterogeneous real-world patients)
- Variable implementation of interventions (protocol-driven vs. routine care delivery)
- Residual confounding in observational studies despite statistical adjustments
- Outcome assessment variations (protocol-defined vs. clinically ascertained endpoints)
The substantial proportion of comparisons with extreme differences underscores the importance of critical appraisal when interpreting evidence from either methodology alone [55]. Rather than universally privileging one design over another, researchers should consider how specific study features—including population representativeness, intervention fidelity, outcome measurement, and confounding control—might influence results in particular clinical contexts.
Experimental Protocols and Methodological Workflows
Protocol 1: Retrospective Observational CER Study Design
The Patient-Centered Outcomes Research Institute (PCORI) has developed detailed methodological standards for comparative clinical effectiveness research (CER) using observational designs [74]. The following workflow outlines key protocol elements:
Figure 1: Workflow for observational comparative effectiveness research (CER) following PCORI standards [74].
Key protocol specifications:
- Data Source Requirements: Established, ready-to-analyze data sources must be secured before application submission, with evidence of data access [74]. PCORnet and other clinical research networks are commonly leveraged.
- Causal Inference Methods: Applications must implement state-of-the-art approaches for retrospective observational designs, such as propensity score matching, inverse probability weighting, or instrumental variable analysis [74].
- Outcome Selection: Outcomes must be clinically meaningful and considered important by patients, with consideration of the full range of outcomes data relevant to stakeholders [74].
- Heterogeneity of Treatment Effect (HTE) Assessment: Pre-specified plans must address how HTE will be assessed across patient subgroups [74].
Protocol 2: Rare Disease Drug Evaluation Framework
A 2024 scoping review protocol outlines methodological standards for observational studies of rare disease drugs [73]. The framework addresses specific challenges including small sample sizes and confounding control:
Figure 2: Methodological framework for rare disease drug evaluation using observational studies [73].
Key methodological considerations:
- Data Source Specification: Studies must use health administrative data from all healthcare settings and regions, with comprehensive capture of clinical outcomes and healthcare utilization [73].
- Temporal Framework: The protocol focuses on studies published between 2018-2023, reflecting recent methodological advances in RWE generation [73].
- Confounding Control Methods: The protocol systematically catalogues methods used to address confounding in rare disease contexts, including novel approaches for small samples [73].
- Feasibility Considerations: The framework acknowledges constraints specific to rare diseases, including limited sample sizes and heterogeneous disease manifestations [73].
Table 3: Essential Resources for Pharmaceutical Evidence Generation
| Resource Category | Specific Tools/Methods | Primary Application | Key Considerations |
|---|---|---|---|
| Data Networks | PCORnet, EHR systems, claims databases | Retrospective observational studies | Data quality, completeness, and linkage capabilities |
| Causal Inference Methods | Propensity scores, instrumental variables, marginal structural models | Confounding control in observational studies | Assumptions must be explicitly stated and evaluated |
| RCT Innovation Designs | Adaptive trials, platform trials, sequential trials | Increasing trial efficiency and flexibility | Statistical complexity and potential operational challenges |
| Economic Evaluation Tools | Cost-effectiveness models, budget impact models, QALY measurement | Pharmacoeconomic assessment | Perspective, time horizon, and discount rate selection |
| Rare Disease Methods | External controls, matching-adjusted indirect comparison, natural history studies | Evidence generation for small populations | Validation of historical control comparability |
| Patient-Reported Outcomes | Disease-specific PRO measures, quality of life instruments | Capturing patient-centered endpoints | Measurement properties and meaningful change thresholds |
Assessment and Validation Tools
- E-Value Calculation: Quantifies the strength of unmeasured confounding needed to explain away observed treatment effects [9]
- Directed Acyclic Graphs (DAGs): Visual tools for identifying potential confounders, mediators, and colliders in observational studies [9]
- Quality Assessment Checklists: Standardized tools for evaluating methodological rigor of both RCTs (e.g., Cochrane Risk of Bias) and observational studies (e.g., ROBINS-I) [72]
- Heterogeneity of Treatment Effect (HTE) Analysis: Statistical approaches to identify how treatment effects vary across patient subgroups [74]
The comparative analysis of RCTs and observational studies across pharmacoeconomic and rare disease contexts reveals that neither methodology is universally superior. Rather, their appropriate application depends on the specific research question, decision-making context, and practical constraints.
In pharmacoeconomic evaluations, hybrid approaches that integrate RCT efficacy data with observational effectiveness evidence provide the most comprehensive assessment of value. For rare diseases, observational studies often transition from supplementary to primary evidence sources, with methodological adaptations addressing small sample sizes and ethical constraints.
The evolving evidence landscape emphasizes methodological pluralism rather than hierarchical superiority. As one expert panel concluded, "No study is designed to answer all questions, and consequently, neither RCTs nor observational studies can answer all research questions at all times" [9]. Future progress will likely involve continued methodological innovation, with blurred boundaries between traditional study designs and increased emphasis on evidence triangulation to support healthcare decision-making.
The Role of Meta-Analysis and Hybrid Studies in Combining Methodological Strengths
Medical research is fundamentally a cumulative endeavor, where new findings must be integrated with previous studies to build a robust fabric of knowledge [75]. For most of scientific history, this integration occurred primarily through narrative reviews, which inherently limited the ability to produce quantitative syntheses of evidence [75]. The comparative effectiveness of pharmaceuticals has traditionally been assessed through two primary methodological pathways: randomized controlled trials (RCTs), long considered the gold standard for establishing efficacy, and observational studies, which provide insights into effectiveness in real-world clinical settings [1] [76]. Within this context, meta-analyses and emerging hybrid study approaches have become indispensable tools for reconciling and combining methodological strengths across different research designs.
The limitations of relying exclusively on individual studies have become increasingly apparent. Narrative approaches cannot quantitatively integrate results, limiting our ability to detect and interpret small effects or test for potential moderators that might explain variability in treatment responses [75]. This recognition has fueled increased interest in quantitative synthesis methods, particularly as technological advances in programming languages like Python and R have made it feasible to fit more complex models and even simulate missing data [75]. As pharmaceutical research evolves to incorporate real-world evidence (RWE) alongside traditional RCTs, understanding how meta-analytic and hybrid approaches can leverage the strengths of each methodology becomes crucial for researchers, regulators, and healthcare decision-makers.
Fundamental Methodologies: RCTs, Observational Studies, and Their Synthesis
Core Study Designs and Their Characteristics
Randomized controlled trials and observational studies represent complementary approaches to generating evidence about pharmaceutical effects, each with distinct advantages and limitations. RCTs are prospective studies in which investigators randomly assign subjects to different treatment groups to examine intervention effects on relevant outcomes [76]. In large samples, random assignment generally balances both observed (measured) and unobserved (unmeasured) group characteristics, providing strong internal validity for causal inference [76]. The RCT design is particularly well-suited for establishing the efficacy of pharmacologic interventions under controlled conditions [1] [76].
Observational studies, in contrast, involve investigators observing the effects of exposures on outcomes using either existing data (e.g., electronic health records, health administrative data) or collected data (e.g., through population-based surveys) without playing a role in assigning exposures to subjects [76]. These studies include designs such as cohort studies, case-control studies, and cross-sectional analyses [3]. Observational research provides valuable evidence about intervention effectiveness in real-world clinical practice and is essential when RCTs are infeasible, unethical, or too costly to conduct [1] [76].
Table 1: Core Characteristics of RCTs and Observational Studies
| Characteristic | Randomized Controlled Trials (RCTs) | Observational Studies |
|---|---|---|
| Primary Strength | High internal validity; control for confounding through randomization | High external validity; reflect real-world effectiveness |
| Key Limitation | Limited generalizability to broader populations; high cost and time requirements | Potential for confounding bias; imputation of causality less certain |
| Best Application | Establishing efficacy of pharmaceutical interventions under ideal conditions | Examining effects in real-world scenarios; studying rare or long-term outcomes |
| Confounding Control | Randomization balances both known and unknown confounders | Statistical methods must adjust for measured confounders only |
| Regulatory Acceptance | Gold standard for drug approval | Supplemental evidence for safety, effectiveness in special populations |
Quantitative Comparisons of Methodological Agreement
Recent comprehensive reviews have systematically compared treatment effects derived from RCTs and observational studies. A 2021 landscape review analyzed 74 pairs of pooled relative effect estimates from RCTs and observational studies across 7 therapeutic areas [12]. The findings demonstrated no statistically significant difference in relative effect estimates between RCTs and observational studies in 79.7% of comparisons [12]. However, extreme differences (ratio < 0.7 or > 1.43) occurred in 43.2% of pairs, and in 17.6% of pairs, there was both a significant difference and estimates pointed in opposite directions [12]. This pattern highlights that while concordance is common, substantial discrepancies occur frequently enough to warrant careful consideration of how different methodological approaches are integrated.
Table 2: Comparison of Relative Treatment Effects Between RCTs and Observational Studies
| Degree of Agreement | Frequency | Implications for Evidence Synthesis |
|---|---|---|
| No significant difference | 79.7% of pairs | Observational and RCT data can be complementary |
| Extreme difference (ratio < 0.7 or > 1.43) | 43.2% of pairs | Caution needed in interpretation; possible methodological or population differences |
| Significant difference with opposite direction | 17.6% of pairs | Fundamental disagreement requiring careful investigation of sources |
| RCT estimate outside observational 95% CI | 28.4% of pairs | Statistical disagreement despite potential conceptual agreement |
| Observational estimate outside RCT 95% CI | 41.9% of pairs | Statistical disagreement despite potential conceptual agreement |
Meta-Analysis: Traditional Framework for Evidence Synthesis
Methodological Foundations and Applications
Meta-analysis represents a well-established quantitative approach for synthesizing results across multiple separate but related studies [75]. With over 50 years of literature supporting its usefulness, meta-analysis has become increasingly common in cognitive science and medical research [75]. The fundamental principle underlying meta-analysis is the statistical combination of results from independent studies to produce a single estimate of effect size with greater precision and generalizability than any individual study.
In pharmaceutical research, meta-analyses serve several critical functions. They can enhance statistical power to detect small but clinically important effects, resolve uncertainties when individual studies disagree, improve estimates of effect size, and answer new questions not posed in the original studies [12]. Perhaps most importantly in the context of comparative effectiveness research, meta-analyses allow for the quantitative integration of both RCT and observational evidence, providing a more comprehensive understanding of a pharmaceutical's performance across different contexts and populations.
Implementation Protocols and Statistical Approaches
The standard protocol for conducting meta-analyses involves a two-stage process: first, estimation of effects within individual studies, followed by aggregation of these effects across studies [75]. The statistical models employed generally fall into two categories: fixed-effects models, which assume a single true effect size underlying all studies, and random-effects models, which allow for variability in the true effect across studies [75]. The choice between these approaches depends on both conceptual considerations (whether studies are functionally identical or meaningfully different) and statistical assessments of heterogeneity.
More recent advances in meta-analytic methods include network meta-analyses that allow for indirect comparisons of multiple interventions, individual participant data (IPD) meta-analyses that utilize raw data from each study participant, and model-based meta-analyses (MBMA) that integrate computational modeling with evidence synthesis [77]. These sophisticated approaches enhance the utility of meta-analyses for drug development and regulatory decision-making by providing more nuanced understandings of treatment effects across different patient subgroups and clinical contexts.
Hybrid and Mega-Analytic Approaches: Integrating Methodological Strengths
Conceptual Framework and Definitions
Hybrid approaches represent an innovative methodology that combines elements of meta-analysis with direct analysis of raw data [75]. These approaches are particularly valuable when raw data are available for only a subset of studies, allowing researchers to leverage the strengths of both meta-analytic and individual-level data analysis [75]. The related concept of mega-analysis involves integrated analyses of raw data collected in multiple sites using a single preprocessing and statistical analysis pipeline [75].
When data are aggregated at the individual participant level, this mega-analytic approach can be referred to as parametric individual participant data (IPD) meta-analysis [75]. These methods differ from simple analyses in their scope, dealing with more heterogeneous datasets since the sites may not have collected data in a coordinated manner, and from traditional meta-analyses in that raw data are included rather than group-based statistics [75]. The fundamental advantage of these approaches lies in their ability to directly model complex sources of variation while maintaining consistent data processing across studies.
Methodological Workflow and Implementation
The implementation of hybrid meta-mega-analytic approaches follows a structured workflow that maximizes the value of available data while acknowledging limitations in data completeness. The process begins with systematic identification and categorization of available evidence, distinguishing between studies for which only aggregate results are available and those for which raw individual-level data can be obtained.
Diagram 1: Hybrid Analysis Workflow (76 characters)
This integrated approach offers two key advantages over traditional meta-analyses: homogeneous preprocessing and superior handling of variance structures [75]. By applying consistent preprocessing steps across all available raw data, hybrid approaches eliminate a potential source of variation that is difficult to control in standard meta-analyses [75]. Additionally, the direct integration of individual-level data enables more sophisticated modeling of structured sources of variance, such as nested data hierarchies (e.g., patients within clinics, repeated measurements within patients) and cross-classified random effects [75].
Core Analytical Frameworks and Applications
Modern methodological research integrating meta-analytic and hybrid approaches relies on a sophisticated toolkit of statistical frameworks and computational resources. These tools enable researchers to overcome traditional limitations of evidence synthesis and generate more reliable, actionable insights for pharmaceutical development and clinical decision-making.
Table 3: Essential Methodological Resources for Advanced Evidence Synthesis
| Methodological Resource | Primary Function | Application Context |
|---|---|---|
| Individual Participant Data (IPD) Meta-Analysis | Reanalysis of raw data from multiple studies using consistent statistical models | Gold standard for evidence synthesis when raw data available |
| Two-Stage Meta-Analysis | Combination of aggregate statistics from published studies | Traditional approach when only summary data available |
| Causal Inference Methods | Framework for drawing causal conclusions from observational data | Real-world evidence generation; emulation of target trials |
| Bayesian Hierarchical Models | Flexible modeling of complex variance structures | Integrating heterogeneous data sources with different precision |
| Sensitivity Analyses (E-value) | Quantifying robustness to unmeasured confounding | Assessing potential bias in observational components |
| Model-Based Meta-Analysis (MBMA) | Quantitative framework for drug development decision making | Dose-response, comparative efficacy, trial design optimization |
Technological Infrastructure and Computational Tools
The implementation of advanced meta-analytic and hybrid approaches requires specific computational infrastructure and analytical capabilities. Contemporary research in this domain increasingly leverages artificial intelligence and machine learning approaches to enhance pattern recognition, predict missing data, and identify subtle subgroup effects [78] [79]. These technologies are particularly valuable for analyzing complex, high-dimensional data from electronic health records, genomic databases, and other rich sources of real-world evidence [78].
The widespread adoption of programming environments such as R and Python has dramatically expanded accessibility to sophisticated analytical methods that were previously limited to specialized statistical software [75]. Open-source packages for meta-analysis, causal inference, and machine learning have democratized advanced methodological approaches, enabling broader implementation across the pharmaceutical research ecosystem. Simultaneously, the emergence of standardized reporting guidelines (e.g., PRISMA, MOOSE) has improved the transparency, reproducibility, and overall quality of synthetic research.
Comparative Performance: Quantitative Assessments of Methodological Agreement
Empirical Evidence on Methodological Concordance
The critical question for pharmaceutical researchers and regulators is whether different methodological approaches produce concordant conclusions about treatment effects. Systematic assessments have revealed nuanced patterns of agreement and disagreement between traditional RCTs, observational studies, and their synthetic combinations. A comprehensive review across multiple therapeutic areas found that while the majority (79.7%) of comparisons showed no statistically significant difference between RCT and observational study estimates, important discrepancies occurred in a substantial minority of cases [12].
The sources of variation between methodological approaches are multifactorial. Genuine differences in patient populations between RCTs and real-world settings may lead to legitimately different treatment effects [1] [3]. Additionally, biased estimates may arise from issues with study design or analytical methods in observational research, particularly residual confounding by indication [3]. The increasing use of causal inference methods, including propensity score approaches, instrumental variable analysis, and marginal structural models, has enhanced the ability of observational studies to approximate the causal estimates derived from RCTs [76] [3].
Methodological Innovations Enhancing Validity
Recent methodological innovations have substantially improved the validity and reliability of both meta-analytic and hybrid approaches. In the realm of RCTs, adaptive trial designs, sequential trials, and platform trials have created more flexible, efficient, and ethical approaches to generating experimental evidence [76]. These designs allow for pre-planned modifications based on accumulating data while maintaining trial validity and integrity [76].
For observational studies, the development of sophisticated causal inference frameworks has enabled researchers to more explicitly define causal assumptions, identify potential sources of bias, and implement analytical strategies that more closely approximate experimental conditions [76]. The use of directed acyclic graphs (DAGs) provides a formal structure for identifying minimal sufficient adjustment sets, while quantitative tools like the E-value offer intuitive metrics for assessing robustness to unmeasured confounding [76]. These advances have systematically addressed historical concerns about bias in observational research and facilitated more meaningful integration with experimental evidence.
The integration of meta-analytic and hybrid approaches represents a significant advancement in pharmaceutical research methodology, offering a powerful framework for combining the strengths of randomized and observational evidence. Traditional meta-analyses provide robust quantitative synthesis of existing literature, while emerging hybrid methods enable more sophisticated modeling of individual-level data from multiple sources. Together, these approaches facilitate a more comprehensive understanding of pharmaceutical effects across diverse populations and clinical contexts.
For researchers and drug development professionals, these methodological innovations create new opportunities to generate evidence that is simultaneously rigorous and relevant. By leveraging the internal validity of RCTs and the external validity of observational studies within an integrated analytical framework, the pharmaceutical research community can accelerate the development of safe, effective therapies and more precisely target their use to appropriate patient populations. As methodological advances continue to blur the traditional boundaries between experimental and observational research, the strategic application of meta-analytic and hybrid approaches will play an increasingly vital role in advancing therapeutic innovation and patient care.
Conclusion
The comparative effectiveness of pharmaceuticals is no longer a question of RCTs versus observational studies, but rather how to strategically integrate both methodologies. RCTs remain unparalleled for establishing efficacy under ideal conditions with high internal validity, while modern observational studies, powered by vast real-world data and advanced causal inference methods, provide critical evidence on effectiveness in diverse, real-world populations. The future of pharmaceutical research lies in a pragmatic, complementary framework. This includes employing innovative adaptive trial designs, proactively using RWE for regulatory decisions and post-marketing surveillance, and embedding economic evaluations early in the research pipeline. By moving beyond a rigid hierarchy of evidence, researchers can generate more nuanced, generalizable, and timely evidence to accelerate drug development and improve patient outcomes.
References
- 1. Comparing Randomized Controlled Trials and Real-World ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7276323/]
- 2. Randomized Controlled Trials: Overview, Benefits and ... [https://www.clinicaltrials.astellas.com/what-is-a-randomized-clinical-trial]
- 3. Observational Research Opportunities and Limitations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3818421/]
- 4. Strengths and Limitations of RCTs - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK584466/]
- 5. The limitations of observation studies for decision making ... [https://www.sciencedirect.com/science/article/pii/S0040595718302464]
- 6. The biggest challenges clinical trials will face in 2025 [https://www.clinicaltrialsarena.com/features/clinical-trials-challenges-expect-2025/]
- 7. Navigating Research Disruptions: The Impact of NIH Grant ... [https://www.pharmacytimes.com/view/navigating-research-disruptions-the-impact-of-nih-grant-terminations-and-the-pharmacist-s-expanding-role]
- 8. Randomized controlled trials – The what, when, how and why [https://www.sciencedirect.com/science/article/pii/S147751312400617X]
- 9. Rethinking the pros and cons of randomized controlled trials ... [https://bmcproc.biomedcentral.com/articles/10.1186/s12919-023-00285-8]
- 10. Registry or randomization – must it be evidence or could it be ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12327714/]
- 11. Risk of bias in observational studies using routinely collected ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-021-02151-w]
- 12. Comparative effectiveness and safety of pharmaceuticals ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-021-02176-1]
- 13. The relevance of the real-world evidence in research, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11878099/]
- 14. Quantifying Potential Immortal Time Bias in Observational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12006797/]
- 15. The role of randomized controlled trials, registries ... [https://www.sciencedirect.com/science/article/pii/S1521692623000841]
- 16. Randomized controlled trials vs. observational studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC5073487/]
- 17. How to Assess the External Validity and Model Validity of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3963220/]
- 18. | Definition, Types, Threats & Examples External Validity [https://www.scribbr.com/methodology/external-validity/]
- 19. Assessing the feasibility and external of natural language... validity [https://pubmed.ncbi.nlm.nih.gov/39787636/]
- 20. Optimizing clinical scientific research: the cohort intervention ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580914/]
- 21. Why the randomized controlled trial is still at the apex and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12645132/]
- 22. Systematic reviews of observational studies frequently ... [https://pubmed.ncbi.nlm.nih.gov/40414366/]
- 23. Comparative Effectiveness Research [https://actuary.org/comparative-effectiveness-research/]
- 24. Large Language Models in Randomized Controlled Trials ... [https://www.jmir.org/2025/1/e67469]
- 25. Similarities and Differences Between Pragmatic Trials and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11254859/]
- 26. Comparison of explanatory and pragmatic design choices in a ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-022-06611-3]
- 27. Platform trials: key features, when to use them and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318487/]
- 28. Clinical Trials With Pragmatic Elements: A Review of Use ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12641079/]
- 29. Comparative effectiveness and safety of pharmaceuticals assessed in observational studies compared with randomized controlled trials - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8647453/]
- 30. A comprehensive guide to conduct a systematic review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366998/]
- 31. FDA-Regulated Clinical Trials vs. Real-World Data [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562589/]
- 32. The Importance of Real-World Evidence in Medical ... [https://www.appliedclinicaltrialsonline.com/view/real-world-evidence-medical-research-drug-development]
- 33. Real-World Evidence: Better than Nothing or the Future? A ... [https://link.springer.com/article/10.1007/s00270-025-04179-4]
- 34. Real-World Data and Causal Machine Learning to Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579681/]
- 35. EHR Systems: Complete Guide & Top 10 Picks (2025) [https://tadabase.io/blog/ehr-systems]
- 36. 2025 EHR Buyer's Guide: Features, Interoperability, and ... [https://www.capminds.com/2025-ehr-buyers-guide-features-interoperability-and-roi-benchmarks/]
- 37. Beyond the binary: integrating “real-world evidence†with ... [https://www.sciencedirect.com/science/article/pii/S0895435625001544]
- 38. RCTs in Medical Research: Why They're Crucial (2025) [https://cassandra.app/resources/understanding-the-importance-of-randomized-controlled-trials-in-medical-research]
- 39. Overview of clinical study designs [https://www.ceemjournal.org/m/journal/view.php?doi=10.15441/ceem.23.036]
- 40. Large Language Models in Randomized Controlled Trials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12407223/]
- 41. Systematic reviews of observational studies frequently ... [https://www.sciencedirect.com/science/article/pii/S0895435625001738]
- 42. Translational Success and Pharmacoeconomic Lessons of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205848/]
- 43. RCT vs. observational studies for COVID-19 [https://c19early.org/rctobs.html]
- 44. Interim Estimates of 2024–2025 COVID-19 Vaccine ... [https://www.cdc.gov/mmwr/volumes/74/wr/mm7406a1.htm]
- 45. Why randomized controlled trials are crucial for evaluating ... [https://cdcn.org/why-randomized-controlled-trials-are-crucial-for-evaluating-covid-19-treatments/]
- 46. Comparative Effectiveness of mRNA-1273 and BNT162b2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12006235/]
- 47. Randomized clinical trial (RCT): An overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11757218/]
- 48. Choosing wisely between randomized controlled trials and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5569603/]
- 49. Evaluating Quantitative Bias Analysis in Research - Simple Science [https://scisimple.com/en/articles/2025-08-06-evaluating-quantitative-bias-analysis-in-research--a9m8rm2]
- 50. Comparative effectiveness and safety of pharmaceuticals assessed in observational studies compared with randomized controlled trials - PubMed [https://pubmed.ncbi.nlm.nih.gov/34865623/]
- 51. How similar are estimates of treatment effectiveness derived from randomised controlled trials and observational studies? | Cochrane [https://www.cochrane.org/evidence/MR000034_how-similar-are-estimates-treatment-effectiveness-derived-randomised-controlled-trials-and]
- 52. Randomised controlled trials and population-based ... [https://www.nature.com/articles/bjc2013725]
- 53. Quantifying the impact of unmeasured confounding in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10163534/]
- 54. A Comprehensive Review and Tutorial on Confounding ... [https://www.mdpi.com/2076-3417/14/9/3662]
- 55. Comparative effectiveness and safety of pharmaceuticals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8647453/]
- 56. Effect Estimates in Randomized Trials and Observational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6670045/]
- 57. Confounder adjustment in observational studies investigating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11881322/]
- 58. Confounding adjustment methods in longitudinal ... [https://pubmed.ncbi.nlm.nih.gov/35304403/]
- 59. Loss to follow-up - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3427970/]
- 60. Medication adherence interventions and outcomes: an overview of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6613929/]
- 61. Digital adherence technology to improve medication ... [https://www.nature.com/articles/s41533-025-00457-3]
- 62. How to Improve Data Quality: A Strategic Guide for 2025 [https://www.ewsolutions.com/how-to-improve-data-quality/]
- 63. Standardized Data: The OMOP Common Data Model [https://www.ohdsi.org/data-standardization/]
- 64. Global Standardization of Clinical Research Data [https://www.appliedclinicaltrialsonline.com/view/global-standardization-clinical-research-data]
- 65. Machine learning-based strategies for improving ... [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2025.1621514/full]
- 66. Concordance between randomized controlled trials and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12555453/]
- 67. Endocrine therapies and mortality risk in postmenopausal ... [https://pubmed.ncbi.nlm.nih.gov/40838592/]
- 68. Evaluating the agreement between sensitivity and primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12220123/]
- 69. Observational studies and their utility for practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6003013/]
- 70. HTA Evidence in Rare Diseases: Just Rare or Also Special? [https://link.springer.com/article/10.1007/s40273-025-01538-4]
- 71. Generating Evidence for Comparative Effectiveness Research Using More Pragmatic Randomized Controlled Trials | PharmacoEconomics [https://link.springer.com/article/10.2165/11536160-000000000-00000]
- 72. Pharmacoeconomic Profiles of Advanced Therapy ... [https://www.mdpi.com/2227-9032/13/15/1894]
- 73. Application of observational research methods to real- ... [https://www.medrxiv.org/content/10.1101/2024.05.16.24307474v1.full-text]
- 74. Improving Health Decision Making With Comparative Clinical Effectiveness Research: Retrospective Observational Studies Leveraging Existing Data Sources PCORI Funding Announcement -- Cycle 1 2026 | PCORI [https://www.pcori.org/funding-opportunities/announcement/improving-health-decision-making-observational-comparative-clinical-effectiveness-research]
- 75. Toward Cumulative Cognitive Science: A Comparison of Meta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8746126/]
- 76. Rethinking the pros and cons of randomized controlled ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10795211/]
- 77. Advancing drug development with “Fit-for-Purpose†modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 78. Advancing drug-drug interactions research: integrating AI ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1618701/full]
- 79. AI-driven drug discovery using a context-aware hybrid ... [https://www.nature.com/articles/s41598-025-19593-4]