Beyond the Average: A Strategic Framework for Handling Heterogeneity in Comparative Drug Efficacy Studies
This article provides a comprehensive guide for researchers and drug development professionals on navigating clinical heterogeneity and Heterogeneity of Treatment Effects (HTE) in comparative effectiveness research.
Beyond the Average: A Strategic Framework for Handling Heterogeneity in Comparative Drug Efficacy Studies
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on navigating clinical heterogeneity and Heterogeneity of Treatment Effects (HTE) in comparative effectiveness research. Moving beyond the limitations of the Average Treatment Effect (ATE), we detail a strategic framework that spans from foundational concepts to advanced predictive modeling. The content explores the critical definitions of clinical and statistical heterogeneity, evaluates robust methodological approaches including the PATH Statement's risk and effect modeling, addresses common pitfalls in subgroup analysis, and outlines criteria for validating credible HTE. By synthesizing current best practices and emerging methodologies, this resource aims to empower scientists to generate more nuanced, clinically actionable evidence for personalized medicine and informed decision-making.
Understanding the Spectrum of Heterogeneity: From Clinical Diversity to Statistical Variation
Definition and Scope in Comparative Drug Efficacy Research
Clinical heterogeneity refers to the variability in the design and execution of studies included in systematic reviews (SRs) and comparative effectiveness research (CER). This variability is formally captured by the PICOTS framework, encompassing differences in Populations, Interventions, Comparators, Outcomes, Timeframes, and Settings [1]. In the context of comparative drug efficacy studies, such variability can significantly influence the observed intervention-disease association, potentially leading to biased conclusions or limiting the generalizability of findings if not properly accounted for [1].
International organizations, including the Agency for Healthcare Research and Quality (AHRQ) and the Cochrane Collaboration, define clinical heterogeneity as the diversity in the populations studied, the interventions involved, and the outcomes measured [1]. It is crucial to distinguish this from statistical heterogeneity, which quantifies the degree of variation in effect sizes across studies and can arise from clinical or methodological heterogeneity, or from chance [1]. While statistical heterogeneity is a quantitative measure, clinical heterogeneity is a qualitative concept describing the underlying clinical or methodological reasons for that variation.
Framework for Assessment and Impact on Research Validity
Key Domains of Clinical Heterogeneity
The following table outlines the core domains of clinical heterogeneity and their implications for research validity.
Table 1: Domains of Clinical Heterogeneity and Their Impact on Research
| Domain | Description of Variability | Impact on Research Validity & Generalizability |
|---|---|---|
| Participant Populations | Demographics (age, sex, race/ethnicity), disease severity/stage, coexisting conditions (comorbidities), genetic profiles, risk factors [1]. | Influences whether an intervention-disease association holds across different patient subgroups. Effects may differ based on baseline risk or biological factors [1]. |
| Interventions & Comparators | Drug dosage/frequency, treatment duration, administration route, combination therapies (co-interventions), credibility of placebo, choice of active comparator (e.g., standard of care) [1]. | Impacts the ability to determine a drug's true efficacy and safety profile. Variability in control groups can make cross-trial comparisons difficult [2]. |
| Outcomes Measured | Definition of primary/secondary endpoints, method of outcome measurement (e.g., different survey instruments, laboratory techniques), timing of outcome assessment, follow-up duration [1]. | Hinders data synthesis if outcomes are not measured or reported consistently. Affects the assessment of long-term efficacy and safety [3]. |
Practical Example from Recent Research
A 2025 network meta-analysis (NMA) on first-line treatments for gastric/gastroesophageal junction cancer provides a clear example of managing clinical heterogeneity [2]. The analysis included trials of PD-1 inhibitors (tislelizumab, nivolumab, pembrolizumab) combined with chemotherapy. To enable a valid indirect comparison, the researchers assumed the chemotherapy backbones were comparable and pooled them into a single node, acknowledging this as a potential source of clinical heterogeneity [2]. Furthermore, differences in how trials defined patient subgroups based on programmed cell death-ligand 1 (PD-L1) expression levels represented variability in participant populations that needed careful consideration during analysis [2].
Methodologies for Evaluating and Managing Heterogeneity
Pre-Review Assessment Protocol
A structured feasibility assessment must be conducted before synthesizing data to evaluate clinical heterogeneity across trials [2]. This protocol involves comparing the following aspects of each included study:
- Study Design & Eligibility Criteria: Trial design (e.g., double-blind, open-label), key inclusion/exclusion criteria.
- Baseline Patient Characteristics: As summarized in Table 1 (demographics, disease status).
- Intervention/Comparator Details: As summarized in Table 1.
- Outcome Characteristics: Definitions, measurement methods, and follow-up times for outcomes like overall survival (OS) or progression-free survival (PFS) [2].
This assessment determines whether studies are sufficiently similar to permit meaningful statistical synthesis or if the clinical heterogeneity is too great.
Analytical and Statistical Techniques
When synthesis is deemed appropriate, several techniques can be used to investigate and account for heterogeneity:
- Subgroup Analysis and Meta-Regression: These are hypothesis-driven techniques to examine if specific clinical factors (e.g., age, disease severity) are effect-measure modifiers—that is, if the treatment effect differs according to the level of that factor [1]. These factors should ideally be identified a priori during protocol development to avoid data dredging [1].
- Network Meta-Analysis (NMA): NMA allows for indirect comparisons of treatments across different trials. A key step is evaluating the transitivity assumption, which requires that the studies forming the "network" are sufficiently similar in their clinical and methodological characteristics (i.e., low clinical heterogeneity) to allow for valid indirect comparisons [2] [3].
- Restriction: This involves limiting the review to studies with narrowly defined participant populations or interventions. While this reduces heterogeneity, it also limits the applicability (generalizability) of the findings to a broader population [1].
Experimental and Research Reagent Solutions
Successfully navigating clinical heterogeneity requires a toolkit of methodological and statistical resources.
Table 2: Essential Research Reagents and Methodological Tools
| Tool / Reagent | Function / Purpose | Application Note |
|---|---|---|
| PICOTS Framework | Provides a structured checklist to define the scope of a review and identify potential sources of clinical heterogeneity during study planning [1]. | Use protocol development to pre-specify key variables in populations, interventions, and outcomes. |
| GRADE (Grading of Recommendations, Assessment, Development and Evaluations) Approach | A systematic framework for rating the quality of evidence in a body of research, explicitly considering factors like inconsistency (heterogeneity) and indirectness [3]. | Apply to assess confidence in estimated treatment effects, especially when significant clinical heterogeneity is present. |
| Statistical Software (R, WinBUGS) | Platforms capable of performing complex meta-analyses, subgroup analyses, meta-regression, and network meta-analyses [2] [3]. | Essential for quantitative synthesis and modeling the impact of clinical heterogeneity on effect estimates. |
| Cochrane Risk of Bias Tool | A critical appraisal tool to assess methodological heterogeneity and the potential for bias in included randomized controlled trials. | High methodological heterogeneity can compound clinical heterogeneity and threaten validity. |
| ACT / WCAG Contrast Guidelines | Rules for ensuring sufficient visual contrast in graphical outputs, which is critical for creating accessible and ethically sound data visualizations for scientific communication [4] [5]. | Apply when creating forest plots, network diagrams, and other figures to ensure accessibility for all readers. |
Mitigation Protocols and Best Practices for Study Design
A Priori Specification and Transparent Reporting
The most effective strategy for managing clinical heterogeneity is a priori specification. Factors that may be effect-measure modifiers should be identified during the protocol development stage of a systematic review or meta-analysis, before examining the results of the included studies [1]. This prevents "data dredging" and reduces the risk of spurious findings.
Furthermore, visualization of results should follow the principle of "showing the design" [6]. The first confirmatory plot for an experiment should be a "design plot" that breaks down the key dependent variable by all key manipulations, without omitting non-significant factors or adding interesting covariates post-hoc [6]. This practice is the visual analogue of pre-registration and promotes transparency.
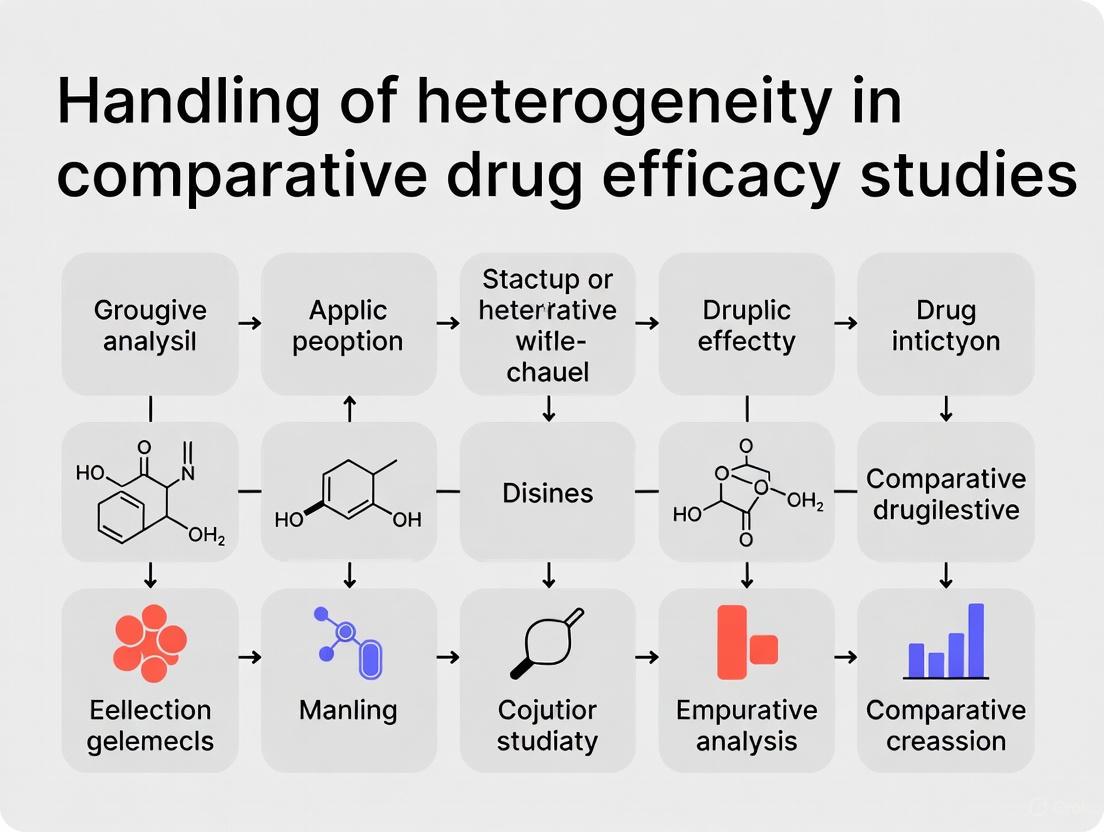
Integrated Workflow for Handling Heterogeneity
The following diagram synthesizes the core concepts and protocols into a unified workflow for defining, assessing, and managing clinical heterogeneity in comparative drug efficacy research.
In comparative drug efficacy studies, the accurate interpretation of treatment effects is fundamentally complicated by the presence of heterogeneity, which manifests in two distinct but interrelated forms: clinical and statistical heterogeneity. Clinical heterogeneity refers to differences in patient populations, intervention characteristics, or outcome measurements across studies or clinical settings [7]. This encompasses variability in factors such as patient demographics (age, sex), pathophysiology, disease severity, comorbid conditions, genetic profiles, and treatment modalities [8] [7]. In contrast, statistical heterogeneity represents the variability in treatment effects beyond what would be expected from chance alone, quantified through statistical measures [9] [10].
The causal relationship between these concepts is fundamental: clinical heterogeneity often serves as the underlying cause, while statistical heterogeneity represents its measurable effect. When clinical differences exist between patient subgroups or study populations, these differences manifest as statistical heterogeneity in the measured treatment effects [8]. This distinction is crucial for drug development professionals seeking to understand whether a treatment's variable performance represents meaningful clinical patterns or merely random statistical variation.
Failure to properly distinguish between these phenomena has significant implications for drug development and personalized medicine. Precision medicine initiatives depend on identifying clinically relevant heterogeneity to match specific treatments with patient subgroups most likely to benefit, while avoiding unnecessary treatment in those who will not respond or may experience harm [8] [11]. This paper provides application notes and experimental protocols to systematically distinguish clinical from statistical heterogeneity within comparative drug efficacy studies.
Theoretical Framework and Definitions
Conceptual Foundations
Clinical heterogeneity arises from differences in patient biology, disease manifestations, treatment contexts, or environmental factors that modify treatment response. In pharmacoepidemiology, this is formally conceptualized as heterogeneity of treatment effects (HTE), defined as how the effects of medications vary across different people and treatment contexts [8]. Common clinical effect modifiers include age, sex, race, genotype, comorbid conditions, or other baseline risk factors for the outcome of interest [8].
Statistical heterogeneity represents the quantitative manifestation of these clinical differences when measured across studies or patient populations. It is mathematically defined as the variability in study effects beyond sampling error [9] [10]. The table below summarizes the key distinguishing characteristics:
Table 1: Fundamental Distinctions Between Clinical and Statistical Heterogeneity
| Characteristic | Clinical Heterogeneity | Statistical Heterogeneity |
|---|---|---|
| Nature | Conceptual/clinical diversity | Quantitative variability |
| Origin | Biological, clinical, or methodological diversity | Sampling error + clinical heterogeneity |
| Assessment | Clinical reasoning | Statistical tests |
| Primary concern | Clinical relevance | Statistical significance |
| Quantification | Descriptive measures | I², Q, H statistics |
| Addressability | Through subgroup definitions | Statistical modeling |
Scale Dependence of Heterogeneity
A critical consideration in heterogeneity analysis is scale dependence, where treatment effects may appear homogeneous on one measurement scale but heterogeneous on another [8]. For example, treatment effects may be constant on the risk difference scale but show significant heterogeneity on the risk ratio scale, or vice versa. This has profound implications for interpretation, as there is wide consensus that the risk difference scale is most informative for clinical decision-making because it directly estimates the number of people who would benefit or be harmed from treatment [8].
Quantitative Assessment of Statistical Heterogeneity
Core Statistical Measures
Statistical heterogeneity is quantified through several complementary measures, each with distinct interpretations and applications:
Cochran's Q statistic: A weighted sum of squared differences between individual study effects and the pooled effect across studies. Q follows a χ² distribution with k-1 degrees of freedom (where k is the number of studies). A significant Q statistic (p < 0.05 or 0.10) indicates heterogeneity beyond chance [9] [10].
I² statistic: Quantifies the percentage of total variability in effect estimates due to heterogeneity rather than sampling error, calculated as I² = 100% × (Q - df)/Q, where df represents degrees of freedom [9] [10]. Interpretation guidelines suggest:
- I² = 0%-25%: Low heterogeneity
- I² = 25%-50%: Moderate heterogeneity
- I² = 50%-75%: Substantial heterogeneity
- I² = 75%-100%: Considerable heterogeneity
H statistic: The square root of the ratio Q/df, with values greater than 1.5 suggesting notable heterogeneity [9].
Table 2: Statistical Measures for Heterogeneity Assessment
| Measure | Calculation | Interpretation | Advantages | Limitations |
|---|---|---|---|---|
| Q statistic | Q = Σwᵢ(θᵢ - θ)² | p < 0.10 suggests significant heterogeneity | Direct test of heterogeneity | Low power with few studies; high power with many studies |
| I² statistic | I² = 100% × (Q - df)/Q | 0-25%: low; 25-50%: moderate; 50-75%: substantial; 75-100%: considerable | Independent of number of studies; comparable across meta-analyses | Confidence intervals often wide when number of studies small |
| H statistic | H = √(Q/df) | <1.2: negligible; 1.2-1.5: possible; >1.5: notable | Intuitive interpretation | Similar limitations to Q statistic |
| τ² (tau-squared) | Various estimators | Between-study variance | Absolute measure of heterogeneity | Sensitive to choice of estimator; difficult to interpret clinically |
Visualization Methods
Several graphical methods facilitate the assessment of statistical heterogeneity:
Forest plots: Display effect estimates and confidence intervals for individual studies alongside the pooled estimate, allowing visual assessment of consistency in effects and precision [10].
Galbraith plots: Plot standardized treatment effects (Z-statistics) against the precision of studies (1/standard error), where deviations from the regression line indicate potential outliers and heterogeneity [9].
L'Abbé plots: For binary outcomes, plot event rates in treatment groups against control groups, visually displaying heterogeneity in treatment effects across studies [9].
Methodological Approaches for Investigating Clinical Heterogeneity
Subgroup Analysis
Subgroup analysis examines whether treatment effects differ across predefined patient characteristics (e.g., age groups, disease severity, genetic markers) [8]. This method offers simplicity and transparency and can provide insights into drug mechanisms, but faces difficulties when multiple effect modifiers are present simultaneously [8].
Protocol 1: Subgroup Analysis Implementation
- Pre-specification: Identify potential effect modifiers and subgroup hypotheses before data analysis to minimize data-driven findings [8].
- Stratification variable selection: Choose variables based on biological plausibility, clinical relevance, and previous evidence [12].
- Analysis approach:
- Estimate treatment effects within each subgroup
- Test for interaction between treatment assignment and subgroup variable
- Use appropriate multiple testing corrections
- Interpretation: Focus on interaction tests rather than within-subgroup comparisons to avoid ecological fallacies.
Disease Risk Score (DRS) Methods
Disease Risk Score methods incorporate multiple patient characteristics into a summary score of baseline outcome risk, then examine treatment effect variation across risk strata [8]. This approach addresses limitations of single-variable subgroup analyses but may obscure mechanistic insights [8].
Effect Modeling Methods
Effect modeling approaches directly model individual treatment effects as a function of patient characteristics, offering potential for precise HTE characterization but requiring careful attention to model specification [8]. These include:
- Multivariable regression with treatment-covariate interaction terms
- Machine learning approaches (causal forests, Bayesian additive regression trees)
- Latent class models that identify subgroups with distinct treatment trajectories [11]
The eHTE Method for Direct HTE Estimation
A novel method termed 'estimated heterogeneity of treatment effect' (eHTE) directly tests the null hypothesis that a drug has equal benefit for all participants by comparing response distributions between treatment arms rather than testing specific covariates [11]. This approach:
- Sorts participants in each arm based on response, generating cumulative distribution functions
- Computes drug-placebo differences at each percentile
- Measures the standard deviation of these differences across percentiles as an approximation of HTE [11]
Protocol 2: eHTE Implementation
- Data requirements: Participant-level data from randomized controlled trials with continuous outcome measures [11].
- Analysis steps:
- Sort participants in each treatment arm by outcome value
- Generate cumulative distribution functions for each arm
- Compute treatment effect at each percentile
- Calculate standard deviation of these percentile-specific treatment effects
- Hypothesis testing: Compare observed eHTE to null distribution generated through permutation or simulation [11].
- Validation: Apply to simulated datasets with known heterogeneity patterns to calibrate interpretation [11].
Integrated Analytical Workflow
A comprehensive approach to distinguishing clinical from statistical heterogeneity requires sequential analytical phases:
Research Reagent Solutions
Table 3: Essential Methodological Tools for Heterogeneity Analysis
| Tool Category | Specific Methods | Primary Function | Application Context |
|---|---|---|---|
| Statistical Software | R (metafor, meta packages) | Comprehensive meta-analysis and heterogeneity quantification | General statistical analysis of aggregated data |
| Specialized Meta-analysis Tools | Stata (metan, metareg) | Flexible meta-analysis with subgroup and meta-regression capabilities | Complex modeling of heterogeneity sources |
| Machine Learning Platforms | Python (causalml, econml) | High-dimensional treatment effect modeling | Individualized treatment effect estimation |
| Data Visualization | R (ggplot2, forestplot) | Graphical assessment of heterogeneity | Forest plots, Galbraith plots, L'Abbé plots |
| Clinical Data Management | REDCap, Electronic Health Records | Structured data collection with clinical context | Real-world evidence generation for HTE |
| Genetic Analysis Tools | PLINK, SNPTEST | Pharmacogenetic effect modification analysis | Genotype-guided treatment effect heterogeneity |
Application to Real-World Data and Comparative Effectiveness Research
Real-world data (RWD) offers particular advantages for HTE assessment, including larger sample sizes, more diverse patient populations, and longer follow-up periods compared to randomized trials [8]. However, observational data introduces additional methodological challenges, particularly confounding, that require careful causal inference approaches.
Protocol 3: HTE Assessment in Real-World Data
- Data quality assessment: Evaluate completeness, accuracy, and relevance of RWD for addressing HTE questions [12].
- Confounding control: Implement propensity score methods, disease risk scores, or instrumental variables to address channeling bias and other confounding [8].
- HTE estimation: Apply subgroup analysis, effect modeling, or machine learning approaches to identify treatment effect modifiers [8].
- Validation: Use internal validation approaches (bootstrapping, cross-validation) and external validation when possible [12].
The growing availability of RWD creates unprecedented opportunities to understand treatment effect heterogeneity across diverse clinical contexts and patient populations, moving beyond the homogeneous treatment effects often assumed in randomized trials [8].
Distinguishing clinical from statistical heterogeneity requires a methodical, multi-stage approach that integrates quantitative assessment with clinical reasoning. Statistical heterogeneity serves as a signal that requires clinical interpretation, while clinical heterogeneity represents the substantive differences that may justify personalized treatment approaches. The proposed frameworks and protocols provide researchers and drug development professionals with structured methodologies to:
- Quantify and visualize statistical heterogeneity using appropriate measures
- Investigate potential clinical heterogeneity through subgroup analyses, effect modeling, and novel approaches like eHTE
- Interpret findings in the context of biological plausibility and clinical relevance
- Implement findings to advance personalized treatment strategies
Future directions in heterogeneity research include the integration of artificial intelligence and machine learning for high-dimensional treatment effect estimation, the development of standardized reporting guidelines for HTE assessments, and methodological advances for distinguishing true effect modification from various forms of bias in real-world settings.
Heterogeneity of Treatment Effects (HTE) refers to the non-random variability in the direction and magnitude of treatment effects across subgroups within a trial population [13]. In comparative drug efficacy studies, the average treatment effect often obscures significant variation in how individual patients or subpopulations respond to interventions. This variation stems from complex interactions between patient characteristics—including genetic, physiological, environmental, and clinical factors—and therapeutic mechanisms. Understanding HTE is fundamental to precision medicine, which aims to match the right treatment to the right patient by accounting for individual determinants of harm and benefit [13].
The identification and quantification of HTE face substantial methodological challenges, primarily arising from the fundamental problem of causal inference: researchers can only observe one potential outcome (the result under the administered treatment) for each patient, but never the simultaneous outcomes under both treatment and control conditions for the same individual [13]. This limitation necessitates sophisticated statistical approaches to estimate individualized treatment effects from group-level data. Furthermore, real-world data used to supplement randomized controlled trials often contain biases from unmeasured confounders, censoring, and outcome heterogeneity that must be carefully addressed [14].
Methodological Frameworks for HTE Analysis
Classification of Analytical Approaches
Regression-based methods for predictive HTE analysis can be classified into three broad categories based on how they incorporate prognostic variables and treatment effect modifiers [13].
Table 1: Methodological Approaches to HTE Analysis
| Approach Category | Key Components | Model Equation Features | Primary Output |
|---|---|---|---|
| Risk-Based Methods | Prognostic factors only; relies on mathematical dependency of absolute risk difference on baseline risk | No covariate-by-treatment interaction terms | Individualized absolute benefit predictions based on baseline risk stratification |
| Treatment Effect Modeling | Both prognostic factors and treatment effect modifiers | Includes covariate-by-treatment interaction terms on relative scale | Subgroups with similar expected treatment benefits; individualized absolute benefit predictions |
| Optimal Treatment Regime | Primarily treatment effect modifiers | Focuses on covariate-by-treatment interactions for treatment assignment rules | Binary treatment assignment rules dividing population into those who benefit and those who do not |
Risk-based methods exploit the mathematical relationship between treatment benefit and a patient's baseline risk for the outcome, even when relative treatment effect remains constant across risk levels [13]. These approaches use only prognostic factors to define patient subgroups and do not include explicit treatment-covariate interaction terms. For example, Dorresteijn et al. combined existing prediction models with average treatment effects from RCTs to estimate individualized absolute treatment benefits by multiplying baseline risk predictions with the average risk reduction observed in trials [13].
Treatment effect modeling methods incorporate both the main effects of risk factors and covariate-by-treatment interaction terms (on a relative scale) to estimate individualized benefits [13]. These methods can be used either for making individualized absolute benefit predictions or for defining patient subgroups with similar expected treatment benefits. These approaches often employ data-driven subgroup identification coupled with statistical techniques to prevent overfitting, such as penalization or use of separate datasets for subgroup identification and effect estimation.
Optimal treatment regime methods focus primarily on treatment effect modifiers (covariate by treatment interactions) for defining a treatment assignment rule that divides the trial population into those who benefit from treatment and those who do not [13]. Contrary to other methods, baseline risk or the magnitude of absolute treatment benefit are not the primary concerns; instead, the focus is on identifying the optimal treatment choice for each patient.
Advanced Statistical Methods for HTE Estimation
Several advanced statistical approaches have been developed to address the challenges of HTE estimation, particularly when integrating multiple data sources or handling complex data structures.
For survival data with right censoring, the conditional restricted mean survival time (CRMST) difference provides an interpretable measure of HTE [14]. This approach defines HTE as the difference in the treatment-specific conditional restricted mean survival times given covariates. Recent methodologies have proposed using an omnibus bias function to characterize biases caused by unmeasured confounders, censoring, and outcome heterogeneity when integrating randomized clinical trial data with real-world data [14]. The proposed penalized sieve method estimates HTE and the bias function simultaneously, with studies demonstrating that this integrative approach outperforms methods relying solely on trial data.
In pre-post study designs, several statistical methods can be employed to estimate treatment effects while accounting for baseline characteristics [15]. These include:
- ANOVA-post: Compares post-test scores between groups while ignoring pre-test responses
- ANOVA-change: Analyzes change scores from pre-test to post-test
- ANCOVA-hom: Adjusts for baseline differences by incorporating pre-test score as a covariate with homogeneous slopes
- ANCOVA-het: Allows different relationships between pre-test and post-test scores for treatment and control groups (heterogeneous slopes)
- Linear Mixed Models (LMM): Handles repeated measurements within subjects using both fixed and random effects
The performance of these methods varies significantly depending on the randomization approach employed (simple randomization, stratified block randomization, or covariate adaptive randomization) and whether influential baseline covariates are adjusted for in the analysis [15].
Figure 1: HTE Analysis Workflow: This diagram illustrates the sequential process for conducting HTE analysis, from study design through clinical application.
HTE Detection in Network Meta-Analysis
Framework for Comparative Drug Efficacy
Network meta-analysis (NMA) provides a powerful framework for detecting HTE across multiple interventions when direct head-to-head comparisons are limited [16] [17] [18]. This approach allows for indirect comparisons of treatment effects while accounting for heterogeneity across studies. Recent advances in NMA methodology have enabled more sophisticated assessment of HTE by considering variations in study design, patient populations, and outcome measures.
A Bayesian framework is commonly employed for NMA, using Markov chain Monte Carlo simulation to quantify and demonstrate consistency between indirect comparisons and direct evidence [16]. The validity of NMA depends on the assumptions of transitivity and consistency, which require that clinical and methodological effect modifiers are similarly distributed across different pairwise comparisons, and that direct and indirect evidence agree [16]. Statistical methods like the node-splitting approach can evaluate consistency for each closed loop in the network.
Table 2: HTE Assessment in Recent Network Meta-Analyses
| Therapeutic Area | Interventions Compared | HTE Assessment Method | Key Findings |
|---|---|---|---|
| Mild Cognitive Impairment [16] | 18 botanical drug interventions | Bayesian NMA with SUCRA rankings | Pycnogenol showed highest probability of improving cognitive function (SUCRA: 98.8%); treatment effects heterogeneous across cognitive domains |
| Ulcerative Colitis [17] | Biologics and small molecules | NMA stratified by trial design (re-randomized vs. treat-through) and prior therapy exposure | Upadacitinib 30mg ranked first for clinical remission in re-randomized studies (RR of failure: 0.52); efficacy heterogeneous based on trial design |
| Obese Knee Osteoarthritis [18] | Antidiabetic drugs | NMA with SUCRA rankings for efficacy and safety | Metformin most effective for pain (MD: -1.13); safety profiles heterogeneous across drug classes |
Accounting for Study Design Heterogeneity
The design of randomized controlled trials significantly influences HTE assessment in network meta-analyses. For ulcerative colitis treatments, efficacy rankings differed substantially between trials using re-randomization designs (where initial responders are re-randomized to active drug or placebo) and those using treat-through approaches (where treatment continues through follow-up without re-randomization) [17]. This highlights the importance of considering trial methodology when evaluating HTE, as different designs may estimate fundamentally different parameters.
Similarly, prior exposure to advanced therapies can substantially modify treatment effects. Network meta-analyses in ulcerative colitis have demonstrated different drug rankings for patients naive to advanced therapies compared to those with previous exposure [17]. This underscores the need for stratified analyses that account for treatment history when assessing HTE.
Experimental Protocols for HTE Detection
Protocol for HTE Analysis in Randomized Trials
Objective: To detect and quantify heterogeneity of treatment effects in a randomized controlled trial setting.
Materials and Methods:
- Study Population: Ambulatory adults (≥18 years) meeting trial eligibility criteria [17]
- Sample Size Considerations: Adequate power for subgroup analyses; often requires larger samples than average treatment effect estimation
- Randomization: Stratified block randomization or covariate adaptive randomization to balance key prognostic factors across treatment groups [15]
- Data Collection:
- Baseline covariates: Demographic, clinical, and biomarker data
- Treatment assignment: Randomized intervention
- Outcome measures: Primary and secondary efficacy endpoints, safety outcomes
- Statistical Analysis:
- Primary Analysis: Apply ANCOVA with heterogeneous slopes (ANCOVA-het) to allow different relationships between baseline and outcome for treatment and control groups [15]
- HTE Detection: Include treatment-by-covariate interaction terms to test for statistical interactions on an appropriate scale (relative or absolute)
- Subgroup Identification: Use treatment effect modeling methods with regularization to prevent overfitting [13]
- Validation: Internal validation through bootstrapping or cross-validation
Interpretation: Focus on clinically meaningful effect modification rather than statistical significance alone. Consider absolute risk differences in addition to relative effects.
Protocol for Integrating RCT and Real-World Data
Objective: To enhance HTE estimation by combining randomized clinical trial data with real-world data.
Materials and Methods:
- Data Sources:
- RCT data: Gold-standard but potentially limited in diversity and generalizability
- Real-world data: Registry data, electronic health records, claims data with potential biases [14]
- Data Structure:
- For subject i: (Xi, Ai, Ti, Ci, Δi, Si) where:
- X: p-dimensional covariate vector
- A: binary treatment (1=active, 0=control)
- T: failure time
- C: censoring time
- Δ: censoring indicator
- S: data source indicator (RCT or RWD) [14]
- For subject i: (Xi, Ai, Ti, Ci, Δi, Si) where:
- Integration Method:
- Define HTE Parameter: Conditional restricted mean survival time difference: Ï„(x) = E[Y(1) - Y(0) | X = x] where Y(a) is potential outcome under treatment a [14]
- Model Bias Function: Define omnibus bias function to characterize biases in real-world data from unmeasured confounders, censoring, and outcome heterogeneity
- Estimation: Use penalized sieve method to estimate HTE and bias function simultaneously
- Asymptotic Properties: Derive convergence rates and local asymptotic normalities using reproducing kernel Hilbert space and empirical process theory [14]
Interpretation: The integrative estimator should outperform RCT-only approaches in terms of efficiency and accuracy of HTE estimation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for HTE Research
| Tool / Method | Function | Application Context |
|---|---|---|
| ANCOVA-het [15] | Estimates treatment effect while allowing different baseline-outcome relationships in treatment vs. control groups | Pre-post study designs with continuous outcomes |
| Penalized Sieve Method [14] | Estimates HTE and bias function simultaneously when integrating RCT and real-world data | Survival data with right censoring |
| SUCRA Rankings [16] [18] | Ranks interventions by probability of being best for each outcome | Network meta-analysis of multiple interventions |
| Node-Splitting Method [16] | Evaluates consistency between direct and indirect evidence in network meta-analysis | Validating transitivity assumption in NMA |
| AIPCW Transformation [14] | Handles right-censored survival outcomes while preserving conditional expectation | Time-to-event outcomes with censoring |
| Covariate Adaptive Randomization [15] | Balances multiple prognostic factors across treatment groups | RCTs with small sample sizes or many influential covariates |
| geldanamycin | geldanamycin, MF:C29H40N2O9, MW:560.6 g/mol | Chemical Reagent |
| Benzene-1,3,5-tricarboxylic acid-d3 | Benzene-1,3,5-tricarboxylic acid-d3, MF:C9H6O6, MW:213.16 g/mol | Chemical Reagent |
Figure 2: HTE Method Classes and Their Characteristics: This diagram illustrates the three main methodological approaches to HTE analysis and their key features.
Understanding and accounting for heterogeneity of treatment effects is essential for advancing precision medicine and optimizing therapeutic decision-making. The methodologies reviewed—ranging from risk-based approaches to sophisticated integrative analyses combining RCT and real-world data—provide powerful tools for moving beyond average treatment effects to identify which patients are most likely to benefit from specific interventions. The consistent implementation of these methods in comparative drug efficacy studies will enable more personalized treatment recommendations and improve patient outcomes by ensuring that therapies are targeted to those who will derive the greatest benefit.
Future methodological development should focus on improving the robustness of HTE estimation in the presence of multiple data sources with different bias structures, enhancing validation approaches for individualized treatment effect predictions, and developing standardized reporting guidelines for HTE assessments in clinical studies. As these methods continue to evolve, they will play an increasingly critical role in drug development and evidence-based clinical practice.
The Critical Role of Effect Measure Modification
Effect Measure Modification (EMM) represents a fundamental concept in clinical epidemiology and comparative drug efficacy research, describing situations where the magnitude or direction of a treatment effect varies across levels of a third variable. Within the broader context of handling heterogeneity in comparative drug studies, EMM provides the methodological framework for understanding why medications work differently across diverse patient populations [8]. This phenomenon occurs when the causal effect of an exposure variable on an outcome depends on the level of a second variable [19]. Unlike confounding, which represents a nuisance to be eliminated, EMM often provides valuable insights for personalizing treatment strategies and understanding biological mechanisms [1] [8].
The distinction between EMM and statistical interaction is both subtle and critical. EMM exists when the effect of a primary exposure of interest varies across subgroups defined by another baseline characteristic [20]. In contrast, interaction concerns the joint effects of two exposures [19]. This distinction carries important implications for confounding adjustment: when studying EMM, only confounders of the primary exposure-outcome relationship require adjustment, whereas interaction analyses require control for confounders of both exposures [20].
Table 1: Key Terminology in Effect Measure Modification
| Term | Definition | Implications for Drug Efficacy Research |
|---|---|---|
| Effect Measure Modifier | A variable that influences the magnitude or direction of a treatment effect | Identifies patient characteristics associated with differential treatment response |
| Scale Dependence | Effect modification can be present on one scale (e.g., additive) but absent on another (e.g., multiplicative) [8] | Determines whether subgroup effects are reported as risk differences or risk ratios |
| Heterogeneity of Treatment Effects (HTE) | The broader phenomenon of treatment effects varying across patient subgroups [8] | Encompasses both explainable (via EMM) and unexplained variation in treatment response |
| Average Treatment Effect (ATE) | The overall effect of treatment averaged across all patients in a study [8] | May obscure important subgroup effects where benefits and harms cancel out |
Methodological Approaches for Investigating Effect Measure Modification
Conventional Analytical Frameworks
Traditional methods for investigating EMM rely on a priori specification of potential effect modifiers and stratified analyses. The subgroup analysis approach offers simplicity and transparency, providing easily interpretable estimates of treatment effects within predefined patient subgroups [8]. However, this method faces limitations when multiple potential effect modifiers coexist, as it cannot simultaneously account for numerous patient characteristics [8].
Disease risk score (DRS) methods incorporate multiple patient characteristics into a summary score of baseline outcome risk, addressing some limitations of simple subgroup analyses [8]. While clinically useful for identifying high-risk patients who might derive greater absolute benefit from treatment, DRS approaches may obscure insights into biological mechanisms because they create composite scores that blend multiple patient attributes [8].
Effect modeling methods directly model how treatment effects vary with patient characteristics, offering more precise characterization of heterogeneity [8]. These approaches include regression models with interaction terms between treatment and potential effect modifiers, but they require careful specification to avoid model misspecification [8].
Table 2: Comparison of Methodological Approaches for EMM Analysis
| Method | Key Features | Advantages | Limitations |
|---|---|---|---|
| Subgroup Analysis | Stratified analysis by predefined patient characteristics | Simple, transparent, provides mechanistic insights [8] | Does not account for multiple characteristics simultaneously; risk of spurious findings |
| Disease Risk Score (DRS) | Creates composite score of baseline outcome risk | Clinically useful for absolute risk assessment; relatively simple implementation [8] | May obscure mechanistic insights; requires validation |
| Effect Modeling | Directly models treatment effect heterogeneity | Potential for precise HTE characterization; can handle multiple modifiers [8] | Prone to model misspecification; complex interpretation |
Modern Machine Learning Approaches
Recent methodological advances have introduced machine learning (ML) techniques for EMM analysis, particularly valuable in high-dimensional settings with numerous potential effect modifiers [21]. Generalized Random Forests extend standard random forests to provide non-parametric estimation of heterogeneous treatment effects, capable of detecting complex interaction patterns without pre-specification [21]. Bayesian Additive Regression Trees (BART) offer a flexible approach for estimating treatment effect heterogeneity while naturally incorporating uncertainty quantification [21]. Metalearner frameworks, including S-, T-, X-, and U-learners, provide flexible estimation strategies that can be combined with various base ML algorithms [21].
These data-driven approaches serve an important role in discovering vulnerable subgroups when prior knowledge is limited, though they cannot replace domain expertise in identifying plausible effect modifiers [21]. ML methods are particularly valuable for generating hypotheses about potential treatment effect modifiers in exploratory analyses, which should then be validated in independent datasets or through mechanistic studies.
Protocols for Detecting and Reporting Effect Measure Modification
Protocol 1: Stratified Analysis for Effect Measure Modification
Objective: To assess whether a baseline characteristic modifies the effect of an intervention on a dichotomous outcome.
Preparatory Steps:
- A Priori Specification: Identify potential effect modifiers during protocol development based on biological plausibility or prior evidence [1].
- Data Collection: Ensure complete ascertainment of potential effect modifiers and confounding variables at baseline.
- Confounder Adjustment: Identify and adjust for confounders of the relationship between the primary exposure and outcome [20].
Analytical Procedure:
- Stratified Analysis: Calculate stratum-specific effect estimates (e.g., risk ratios, risk differences) for each level of the potential effect modifier [20].
- Reference Category Selection: Use a single reference category for all comparisons, preferably the stratum with the lowest outcome risk [20].
- Effect Measure Calculation: Compute both ratio and difference measures for each stratum [20].
- Formal Testing: Assess effect modification on both additive and multiplicative scales with calculation of confidence intervals [20].
Reporting Standards:
- Present relative risks, odds ratios, or risk differences with confidence intervals for each stratum of exposure and effect modifier [20].
- Report measures of effect modification on both additive and multiplicative scales with confidence intervals and p-values [20].
- List all confounders for which the relationship between exposure and outcome was adjusted [20].
Protocol 2: Analysis of Effect Modification Using Real-World Data
Objective: To characterize heterogeneity of treatment effects using real-world data (RWD) to enhance generalizability and precision.
Preparatory Steps:
- Data Quality Assessment: Evaluate completeness, accuracy, and relevance of RWD sources for addressing the research question [8].
- Confounding Control: Implement appropriate methods (e.g., propensity scores, disease risk scores) to address confounding in non-randomized data [8].
- Sensitivity Analyses: Plan analyses to assess robustness of findings to potential unmeasured confounding.
Analytical Procedure:
- ATE Estimation: Calculate the average treatment effect using appropriate methods for observational data.
- HTE Assessment: Apply ML methods or stratified analyses to identify systematic variation in treatment effects [8].
- Scale Assessment: Evaluate effect modification on both additive (risk difference) and multiplicative (risk ratio) scales [8].
- Precision Evaluation: Assess statistical precision of subgroup-specific effect estimates.
Reporting Standards:
- Clearly describe the source and characteristics of the RWD used [8].
- Report the frequency of outcomes in each level of the effect modifier with and without treatment [8].
- Present absolute risks in addition to relative measures to facilitate clinical interpretation [8].
- Acknowledge limitations of RWD, including potential residual confounding [8].
Table 3: Research Reagent Solutions for EMM Analysis
| Tool/Software | Primary Function | Application Context |
|---|---|---|
| R Statistical Environment | Implementation of ML methods for HTE (generalized random forests, BART) [21] | High-dimensional effect modification analysis |
| SAS/PROC GENMOD | Regression with interaction terms for subgroup analysis | Conventional stratified analysis of EMM |
| Python/Scikit-learn | Metalearner implementation for heterogeneous treatment effects | Flexible estimation of treatment effect modification |
| RevMan | Cochrane's tool for meta-analysis of subgroup effects [22] | Systematic review of EMM across multiple studies |
Visualization and Interpretation of Effect Measure Modification
Graphical Representation of Effect Modification
Effective visualization is crucial for interpreting and communicating complex EMM findings. The following Graphviz diagram illustrates the conceptual relationships in EMM analysis:
Scale Dependence in Effect Measure Modification
The phenomenon of scale dependence represents a critical consideration in EMM analysis, wherein effect modification may be present on one scale of measurement but absent on another [8]. This occurs because ratio measures (e.g., risk ratios) and difference measures (e.g., risk differences) reflect different mathematical properties of effect variation [8].
Table 4: Scale Dependence in Effect Measure Modification
| Scenario | Risk Difference Scale | Risk Ratio Scale | Interpretation |
|---|---|---|---|
| Constant additive effect | No effect modification | Effect modification present | Absolute benefit consistent, relative benefit varies |
| Constant multiplicative effect | Effect modification present | No effect modification | Relative benefit consistent, absolute benefit varies |
| Dual-scale effect modification | Effect modification present | Effect modification present | Both relative and absolute benefits vary substantially |
For clinical decision-making, there is wide consensus that the risk difference scale is most informative because it directly estimates the number of people who would benefit or be harmed from treatment [8]. However, ratio measures remain commonly reported in the literature due to statistical convenience and conventional practices [8].
Implementation in Drug Development and Comparative Effectiveness Research
Practical Applications in Pharmacoepidemiology
In pharmacoepidemiology, EMM analysis addresses fundamental questions about why medications work differently across individuals and populations [8]. This understanding enables tailoring of treatment strategies to maximize benefit-risk profiles for individual patients [8]. For example, identifying that patients with specific genetic polymorphisms experience higher rates of adverse drug reactions allows for targeted prescribing and monitoring [8].
The integration of RWD has expanded opportunities for EMM investigation by providing larger sample sizes and more diverse patient populations than typically available in randomized trials [8]. This enhanced statistical power allows for more precise estimation of subgroup-specific treatment effects and detection of rare adverse outcomes that may be modified by patient characteristics [8].
Methodological Considerations for Valid Inference
Robust EMM analysis requires careful attention to methodological principles to ensure valid inferences. A priori specification of potential effect modifiers should be preferred over post hoc data dredging to minimize spurious findings [1]. The distinction between EMM and interaction must be maintained, as the analytical approach and confounding control requirements differ substantially [20] [19].
When using ML methods for EMM analysis, researchers should prioritize interpretability and clinical relevance over pure predictive performance [21]. Complex ML models may identify novel subgroups with differential treatment response, but these findings require validation in independent datasets and assessment of biological plausibility before influencing clinical practice [21].
The evolving methodology for EMM analysis continues to enhance our ability to understand and predict heterogeneity in drug effects, ultimately supporting more personalized and effective pharmacotherapy across diverse patient populations.
Why the 'Average Treatment Effect' is Often Misleading for Clinical Decision-Making
The 'Average Treatment Effect' (ATE), derived from randomized controlled trials (RCTs), serves as a cornerstone of evidence-based medicine. It provides an unbiased estimate of the treatment effect on average across a study population [23]. However, a fundamental incongruity exists: while evidence is generated from groups, medical decisions are made for individuals [23]. The ATE offers a single summary statistic, implicitly assuming that patients with the same disease are identical in all factors that influence their potential to benefit or be harmed by a therapy. In reality, patients differ markedly in characteristics such as age, genetic makeup, disease severity, comorbidities, and environmental exposures [23] [24]. These differences can lead to substantial variation in how individuals respond to treatment, a phenomenon known as Heterogeneity of Treatment Effects (HTE).
Relying solely on the ATE can therefore be misleading for clinical decision-making. It can result in administering powerful treatments to some patients who will derive little benefit while exposing them to potential harms, or conversely, in withholding treatment from others who might benefit substantially [25]. This paper explores the limitations of the ATE, critiques conventional methods for investigating HTE, and presents advanced predictive approaches that move toward a more patient-centered evidence base, framed within the context of comparative drug efficacy research.
The Critical Limitations of the Average Treatment Effect
The Fallacy of the "Average Patient"
The concept of an "average patient" is a statistical abstraction that may not correspond to any real-world individual. The following table summarizes the key reasons why the ATE is an insufficient guide for individual-level decisions.
Table 1: Why the Average Treatment Effect is Misleading for Clinical Decisions
| Limitation | Underlying Cause | Consequence for Decision-Making |
|---|---|---|
| Masking of Heterogeneity | The ATE summarizes a population's response, which may be composed of a spectrum of large positive, negligible, and large negative effects for individuals [23]. | Clinicians cannot discern if their specific patient is likely to be a responder, a non-responder, or one who experiences harm. |
| Oversimplification of Outcomes | Medical decisions involve weighing multiple outcomes simultaneously (e.g., efficacy, safety, cost, quality of life) [25]. The ATE typically focuses on a single primary efficacy outcome. | A favorable ATE on a primary efficacy outcome may obscure significant detriments on other outcomes that are crucial to a patient's decision. |
| Susceptibility to Population Shifts | The ATE is specific to the distribution of effect-modifying characteristics in the trial population [25]. | An ATE from a highly selected trial population may not be generalizable to a different patient in routine practice with a distinct clinical profile. |
| Indifference to Baseline Risk | The absolute treatment benefit is mathematically dependent on a patient's baseline risk of the outcome event [23]. | Patients at low baseline risk will derive small absolute benefit even if the relative risk reduction (a common ATE) is constant across risk groups. Treating them may not be worthwhile. |
The Problem of "Sorting on the Mix"
A particularly complex challenge arises when treatment choice in the real world is based on a "mix" of expected benefits and detriments. Simulation studies show that when treatment effects are heterogeneous across multiple outcomes (e.g., survival benefit vs. risk of a severe adverse event), and treatment choices reflect this, the interpretation of treatment effect estimates becomes highly sensitive to the study population [25].
For example, a patient subgroup with a high expected survival benefit might also have a high risk of severe adverse effects. In practice, these patients might be less likely to receive the treatment (a "treatment-risk paradox") because the perceived detriment outweighs the benefit [25]. Analyses focusing only on the survival ATE would misinterpret this rational clinical decision as under-treatment, failing to capture the nuanced trade-off being made across multiple outcome dimensions.
From Simple Subgroups to Predictive Approaches
The Inadequacy of One-Variable-at-a-Time Subgroup Analysis
The conventional approach to exploring HTE is subgroup analysis, where the treatment effect is estimated separately for categories of a single variable (e.g., age, sex). This method has severe limitations:
- Low Statistical Power: Each subgroup is smaller than the full population, increasing the risk of false-negative findings.
- Inability to Account for Confounding: Subgroups defined by one variable (e.g., elderly) are often confounded by others (e.g., higher comorbidity burden), making it difficult to isolate the true effect modifier [23].
- High Risk of False Positives: Testing multiple subgroups without adjustment increases the likelihood of finding a spurious significant difference by chance alone.
Predictive Approaches to Heterogeneous Treatment Effects
Modern analytical approaches move beyond univariate subgroup analysis to develop multivariate models that predict an individual's specific treatment effect.
Table 2: Predictive Approaches for Modeling Heterogeneous Treatment Effects
| Approach | Methodology | Key Advantage | Key Challenge |
|---|---|---|---|
| Risk Modeling | Develops a model to predict an individual's baseline risk of the outcome event without treatment. The absolute treatment benefit is a function of this baseline risk [23]. | Leverages the mathematical fact that absolute benefit is often correlated with baseline risk. Can be practice-changing and is relatively straightforward to implement. | Does not directly model how specific patient variables modify the relative treatment effect. Assumes a constant relative treatment effect across risk strata. |
| Effect Modeling | Develops a model directly on clinical trial data that includes not only prognostic variables but also interaction terms between patient variables and the treatment assignment [23]. | Directly estimates how multiple variables simultaneously modify the treatment effect, potentially providing more granular, individualized effect estimates. | Prone to statistical overfitting, especially when the number of potential effect modifiers is high and the trial sample size is limited. Requires strong prior knowledge. |
The following workflow diagram illustrates the process of developing and applying these predictive models in clinical research.
Predictive HTE Analysis Workflow
Experimental Protocols for HTE Analysis
Protocol 1: Risk-Based HTE Analysis
This protocol uses baseline risk to explore heterogeneity in the absolute treatment effect.
- Objective: To assess how the absolute benefit of a treatment varies across subgroups defined by their baseline risk of the primary outcome.
- Data Source: Individual participant data from a single large RCT or, preferably, from an individual patient data meta-analysis of multiple trials to ensure adequate power.
- Prognostic Model Development:
- Using the control group data only, develop a multivariable model (e.g., Cox regression, logistic regression) to predict the probability of the primary outcome based on relevant prognostic baseline characteristics.
- Validate the model's performance (discrimination, calibration) using internal (e.g., bootstrapping) or external validation techniques.
- Risk Stratification:
- Apply the developed prognostic model to all participants in the trial (both treatment and control groups) to assign a predicted baseline risk score.
- Categorize participants into quartiles or quintiles of baseline risk.
- Treatment Effect Estimation:
- Within each risk stratum, calculate the absolute risk reduction (ARR) and its confidence interval. The number needed to treat (NNT) can be derived as 1/ARR.
- Visually present the results using a plot showing ARR (and NNT) across the continuum of baseline risk.
Protocol 2: Effect Modeling Using the Target Trial Approach with Real-World Data
When RCTs are not available, this protocol outlines a robust framework for estimating heterogeneous effects from real-world data (RWD) by emulating a hypothetical RCT [26].
- Objective: To emulate a target trial and estimate the effect of a new drug versus standard of care, and its potential heterogeneity, using observational data.
- Target Trial Protocol:
- Explicitly define the key components of the target trial: Patient eligibility criteria, Interventions, Comparators, Outcomes, Time zero (start of follow-up), and Study follow-up period.
- Data Curation:
- Select a suitable real-world data source (e.g., electronic health records, claims database) that can adequately capture the PICOTS.
- Carefully curate the data to ensure the operational definitions of variables (exposure, outcome, confounders) are consistent with the target trial.
- Statistical Analysis to Control for Confounding:
- Identify a comprehensive set of potential confounders using causal diagrams (e.g., DAGs).
- Use advanced statistical methods to address confounding. The choice depends on the data and available instruments:
- Propensity Score Methods: (e.g., matching, weighting) to create a balanced comparison group.
- Instrumental Variable (IV) Analysis: If a suitable instrument is available (e.g., regional variation in prescribing preference) and assumptions are met, this can address unmeasured confounding [26].
- HTE Analysis:
- After accounting for confounding, incorporate pre-specified interaction terms between the treatment and key patient characteristics (e.g., age, biomarker status) into the outcome model.
- Use machine learning methods like causal forests, which are designed to handle high-dimensional data and discover heterogeneous effects without pre-specification, while being robust to overfitting.
The Scientist's Toolkit: Essential Reagents for HTE Research
Table 3: Key Research Reagent Solutions for Heterogeneity of Treatment Effects Studies
| Item / Solution | Function & Application in HTE Research |
|---|---|
| Individual Participant Data (IPD) | The foundational raw material. IPD from clinical trials or high-quality observational studies is essential for developing and validating predictive models of treatment effect [23]. |
| Statistical Software (R/Python) | The primary laboratory. Environments like R (with packages for survival analysis, grf for causal forests) and Python (with libraries like EconML, scikit-learn) are used to implement risk and effect modeling techniques. |
| Causal Inference Frameworks | The theoretical blueprint. Frameworks such as Target Trial Emulation and Causal Diagrams (DAGs) provide the structure for designing valid analyses, particularly when using real-world data to investigate HTE [26]. |
| Data Visualization Tools | The communication lens. Tools like ChartExpo or advanced plotting libraries in R/Python are critical for creating clear visualizations of heterogeneous effects, such as plots of treatment effect across the spectrum of baseline risk or forest plots of subgroup effects [27] [28]. |
| Edaravone D5 | Edaravone D5 Stable Isotope |
| (R)-Cinacalcet-D3 | (R)-Cinacalcet-D3|CAS 1228567-12-1|High Purity |
The average treatment effect is a useful starting point but a dangerous endpoint for evidence-based medicine. Its uncritical application obscures the fundamental reality that treatment effects are heterogeneous across individual patients and across multiple outcomes. To advance comparative drug efficacy research, the field must move beyond the ATE and conventional, underpowered subgroup analyses. By adopting predictive approaches like risk and effect modeling, and by rigorously applying frameworks like the target trial approach to real-world data, researchers can generate the nuanced, personalized evidence needed to inform truly patient-centered therapeutic decisions. The future of evidence-based medicine lies not in knowing what works on average, but in predicting for whom it works best.
Advanced Analytical Approaches: From Subgroup Analysis to Predictive Modeling of HTE
Subgroup analyses are a fundamental step in assessing evidence from confirmatory (Phase III) clinical trials, investigating whether treatment effects are homogeneous across the study population [29]. Eligibility criteria for large trials are often broad to ensure the trial results can be generalized to a larger patient population, making subgroup analysis essential for interpreting whether conclusions for the overall study population hold for all patient subsets [30]. These analyses evaluate whether the treatment effect of a new drug varies across subgroups defined by demographic variables (e.g., age, sex, race) or variables prognostic of clinical outcomes (e.g., disease severity, biomarker status) [30].
In comparative drug efficacy studies, subgroup analyses serve distinct purposes: investigating consistency of treatment effects across clinically important subgroups, exploring treatment effects within an overall non-significant trial, evaluating safety profiles limited to specific subgroups, or establishing efficacy in a targeted subgroup included in a confirmatory testing strategy [29]. The growing biological and pharmacological knowledge driving personalized medicine makes these analyses particularly relevant for identifying subgroups with differential benefit-risk profiles [29].
Defining Subgroups and Understanding Treatment Effect Heterogeneity
Subgroup Definition Methodologies
Subgroups can be defined using various approaches, each with specific methodological considerations. Demographic subgroups (age, sex, race) are commonly examined, while subgroups defined by prognostic variables (disease severity, prior therapies) or predictive biomarkers (genotype, biomarker status) are increasingly important in targeted therapy development [30].
For continuous variables, using well-established or published cutoffs is preferred. In oncology, for example, age cutoffs of 40 and 65 years commonly classify patients into adolescent/young adult (<40), adult (40-65), and older adult (>65) subgroups [30]. When common cutoffs are unavailable, data-driven approaches such as percentiles (e.g., median) or statistical graphs may be used, though these require caution regarding plausibility and reproducibility [30].
When multiple variables contribute to subgroup definition, a continuous prediction score from a multivariable prediction model can categorize patients into risk groups (low, moderate, high). Optimal cutoff points for novel biomarkers or risk scores are often chosen to maximize outcome differences or treatment benefits between subgroups [30].
Heterogeneity of Treatment Effect
The statistical term for differential treatment effects across subgroups is treatment-by-subgroup interaction [30]. This interaction can be quantitative or qualitative:
- Quantitative interactions: Treatment effect size varies across subgroups but remains in the same direction
- Qualitative interactions: Treatment effect direction differs across subgroups (beneficial in one subgroup, harmful in another)
Table 1: Types of Treatment-Subgroup Interactions
| Interaction Type | Description | Clinical Implications |
|---|---|---|
| No Interaction | Consistent treatment effect across subgroups | Same therapeutic implication for all subgroups |
| Quantitative Interaction | Varying magnitude of effect, same direction | Same therapeutic implication but potentially different benefit magnitude |
| Qualitative Interaction | Opposite effect directions between subgroups | Critical therapeutic consequences; treatment may benefit one subgroup while harming another |
A classic example of qualitative interaction comes from the IPASS trial in non-small cell lung cancer, where gefitinib showed significantly better progression-free survival versus control in EGFR mutants but significantly worse progression-free survival in EGFR wild-type patients [30]. This makes EGFR mutation status a predictive biomarker for gefitinib response.
Statistical Power and Multiple Testing Considerations
Power Limitations in Subgroup Analyses
Subgroup analyses in randomized controlled trials designed primarily to evaluate overall treatment effects are frequently under-powered [30]. The test for treatment-by-subgroup interaction has roughly four times the variance of an overall treatment effect test when subgroup sizes are equal, necessitating substantially larger sample sizes that are seldom feasible [30]. Consequently, failure to detect a statistically significant interaction does not necessarily indicate absence of treatment effect heterogeneity.
Low power in subgroup analyses is particularly problematic when exploring multiple subgroups or when interaction effects are modest. Equal allocation of patients across subgroups yields the highest power, but this is often not reflected in trial designs [30]. For biomarker-stratified trials, specific strategies can optimize power for detecting treatment-by-subgroup interactions [30].
Type I Error Inflation and Multiple Testing Controls
Conducting multiple statistical tests across numerous subgroups substantially inflates the false positive rate [30]. With 10 independent tests conducted at a 5% significance level, the chance of at least one false positive finding is approximately 40% when no true treatment effects exist [30].
Table 2: Multiple Testing Correction Methods
| Method | Approach | Advantages | Limitations |
|---|---|---|---|
| Bonferroni Correction | Divides significance level by number of tests | Simple implementation, controls family-wise error rate | Overly conservative, ignores correlation between tests |
| Sequential Testing (Gating) | Tests overall effect before subgroup effects | Preserves power for primary analysis | May miss targeted subgroup effects when overall effect nonsignificant |
| Fallback Procedure | Allows recycling of significance level after rejecting hypotheses | More powerful than Bonferroni, incorporates testing order | More complex implementation |
| MaST Procedure | Accounts for correlation between subgroup and overall tests | Improved power compared to Bonferroni | Requires specialized statistical expertise |
More flexible multiple testing procedures like the fallback and MaST procedures account for correlation between outcomes and allow recycling significance levels after rejecting hypotheses, offering improved power over traditional Bonferroni correction [30].
A Priori Specification and Analysis Protocols
Confirmatory vs. Exploratory Subgroup Analyses
Confirmatory subgroup analyses intended to support subgroup-specific efficacy claims must be pre-specified in the trial design with clearly defined subgroups and endpoints [30]. These require strict control of type I error and appropriate sample size planning. In contrast, exploratory subgroup analyses may generate hypotheses for future research but should not form definitive conclusions about differential treatment effects [29].
The purpose of subgroup analyses should guide their design and interpretation. Four distinct purposes include: (1) investigating consistency of treatment effects across clinically important subgroups, (2) exploring treatment effects across subgroups within an overall non-significant trial, (3) evaluating safety profiles limited to specific subgroups, and (4) establishing efficacy in a targeted subgroup within a confirmatory testing strategy [29].
Statistical Analysis Protocols
Protocol 1: Testing for Treatment-by-Subgroup Interaction
- Pre-specification: Define subgroups of interest and analysis methodology in the statistical analysis plan before trial unblinding
- Model specification: Use statistical regression models including main treatment effect, subgroup variable, and treatment-by-subgroup interaction term
- Covariate adjustment: Include prognostic or confounding variables in models to adjust for potential associations with outcomes
- Interaction test: Evaluate the statistical significance of the interaction term to determine if differential treatment effects exist across subgroups
- Effect estimation: If significant interaction exists, present subgroup-specific treatment effects rather than overall average effect
Protocol 2: Controlling for Multiple Testing in Subgroup Analyses
- Define testing hierarchy: Establish a pre-specified order of hypothesis tests (e.g., overall population first, then key subgroups)
- Allocate alpha: Distribute type I error rate across multiple hypotheses using appropriate multiple testing procedures
- Account for correlations: Consider using procedures that account for correlation between tests (e.g., fallback procedure) rather than Bonferroni
- Interpret results: Evaluate findings in the context of the multiple testing strategy employed
Protocol 3: Meta-Analytic Approach for Subgroup Effects Across Studies
- Data collection: Gather subgroup-specific treatment effects and standard errors from multiple studies
- Model selection: Choose appropriate meta-analytic model (fixed-effects or random-effects) based on heterogeneity assessment
- Address aggregation bias: Use methods like SWADA (Same Weighting Across Different Analyses) to resolve inconsistencies from unbalanced subgroup distributions across studies [31]
- Synthesize evidence: Calculate summary estimates for subgroup-specific treatment effects and interaction effects
- Assess heterogeneity: Evaluate between-study heterogeneity in subgroup effects using appropriate statistics (e.g., I²)
Visualization and Interpretation of Subgroup Analyses
Graphical Approaches for Subgroup Analysis
Visualization techniques play a key role in subgroup analyses to visualize effect sizes, aid identification of differentially responding groups, and communicate results [32]. Effective graphics should display treatment effect estimates, confidence intervals, subgroup sample sizes, and ideally accommodate multivariate subgroups [32].
Forest plots are the most common visualization for subgroup analyses, displaying subgroup-specific treatment effects with confidence intervals, often with symbol sizes proportional to subgroup sample sizes [30] [32]. These plots allow direct comparison of treatment effect estimates across subgroups with low cognitive effort and can display many subgroup-defining covariates [32].
Other visualization approaches include:
- Galbraith plots: Visualize standardized treatment effects against precision to identify outliers
- UpSet plots: Display intersections of multiple subgroups for multivariate analysis
- STEPP (Subpopulation Treatment Effect Pattern Plot): Explore treatment effect changes across continuous covariates
- Contour plots: Visualize treatment effects across two continuous variables simultaneously
Interpretation Guidelines
Interpreting subgroup analyses requires careful consideration of several factors:
- Biological plausibility: Are observed subgroup differences consistent with known biological mechanisms?
- Statistical evidence: Is the treatment-by-subgroup interaction statistically significant after appropriate multiple testing adjustments?
- Consistency across studies: Have similar subgroup effects been observed in independent datasets?
- Effect magnitude: Are observed differences clinically meaningful, not just statistically significant?
- Pre-specification: Were subgroup hypotheses defined a priori rather than identified through data dredging?
Figure 1: Subgroup Analysis Workflow Protocol
Table 3: Essential Methodological Tools for Subgroup Analysis
| Tool/Resource | Function/Purpose | Implementation Considerations |
|---|---|---|
| Treatment-by-Subgroup Interaction Test | Determines if treatment effect differs across subgroups | Low power in typical RCTs; requires larger sample sizes for adequate detection |
| Forest Plots | Visualizes subgroup treatment effects with confidence intervals | Most effective when showing subgroup sample sizes and overall effect reference line |
| Multiple Testing Procedures | Controls false positive findings from multiple comparisons | Bonferroni is conservative; fallback and MaST procedures offer improved power |
| Random-Effects Meta-Analysis | Synthesizes subgroup effects across studies | SWADA approach addresses aggregation bias from unbalanced subgroup distributions |
| Predictive Biomarker Validation | Confirms biomarkers that predict treatment response | Requires demonstration of qualitative or quantitative interaction with treatment |
Figure 2: Subgroup Analysis Objectives and Corresponding Methods
Subgroup analyses present both opportunities and challenges in comparative drug efficacy research. When properly conducted with a priori specification, appropriate statistical methods, and careful interpretation, they can provide valuable insights into heterogeneous treatment effects and inform personalized treatment approaches. However, undisciplined subgroup analyses risk false positive findings and misleading conclusions.
Key recommendations for best practices include:
- Pre-specify subgroup hypotheses and analysis plans in the statistical analysis protocol
- Limit the number of subgroup analyses to reduce multiple testing problems
- Use appropriate statistical methods for interaction tests and multiple testing adjustments
- Ensure adequate power for subgroup analyses when they represent key study objectives
- Interpret findings cautiously considering biological plausibility and consistency with previous research
- Visualize results effectively using forest plots and other informative graphics
- Distinguish clearly between confirmatory and exploratory subgroup analyses
Following these guidelines will enhance the validity and interpretability of subgroup analyses in drug development, ultimately supporting more targeted and effective therapeutic approaches.
The Predictive Approaches to Treatment effect Heterogeneity (PATH) Statement provides a structured framework for moving beyond average treatment effects to understand how treatment outcomes vary across individuals. In comparative drug efficacy research, the limitation of relying on an overall average treatment effect is that it assumes all patients experience identical benefit-harm trade-offs, which rarely reflects clinical reality [33]. The PATH framework addresses this by promoting analytical methods that account for multiple patient attributes simultaneously, thereby supporting more personalized clinical decision-making [34].
The core goal of predictive HTE analysis is to provide individualized predictions of treatment effect, defined as the difference in expected outcomes for a specific patient under alternative treatments [33]. This approach is foundational for precision medicine and patient-centered outcomes research, as it acknowledges that even in positive randomized controlled trials (RCTs), some patients may not benefit or could experience net harm [35].
Core PATH Methodologies: Risk Modeling vs. Effect Modeling
The PATH Statement distinguishes two primary methodological approaches for evaluating HTE, each with distinct theoretical foundations and operational procedures.
Risk Modeling Approach
Risk modeling is a two-stage approach that focuses on baseline risk as a robust predictor of treatment effect variation [35] [33]. This method leverages the mathematical relationship where absolute treatment benefits often increase with a patient's baseline risk of experiencing the study outcome, even when relative effects remain constant [34].
- Stage 1: Develop or identify a multivariable prediction model for the outcome of interest using baseline patient characteristics, without including treatment assignment. This model can be derived externally from existing literature or internally from the trial population (using the control arm or both arms combined) [33].
- Stage 2: Apply this model to stratify trial participants into risk groups (e.g., quartiles) and examine how absolute and relative treatment effects vary across these strata [35].
The risk modeling approach is particularly valuable when substantial variation in baseline risk exists across the trial population, as this often reveals clinically important differences in harm-benefit trade-offs [33].
Effect Modeling Approach
Effect modeling uses a single model that incorporates treatment assignment, multiple baseline covariates, and treatment-covariate interaction terms to directly estimate how treatment effects vary with patient characteristics [35] [34].
This approach employs a regression framework of the form:
risk = f(α + β_tx * tx + β_1 * x_1 + … + β_p * x_p + δ_1 * x_1 * tx + … + δ_p * x_p * tx) [33]
Where the δ parameters quantify the statistical interactions between treatment and patient attributes. Effect modeling can theoretically provide more robust HTE examination but is highly vulnerable to overfitting and false discovery, especially when multiple interaction terms are tested without strong prior evidence [35].
Table 1: Core Characteristics of PATH Approaches
| Characteristic | Risk Modeling | Effect Modeling |
|---|---|---|
| Analytical Goal | Examine treatment effect variation across strata of predicted baseline risk | Directly estimate how treatment effects vary with specific patient characteristics |
| Model Structure | Two-stage process: (1) develop risk model, (2) assess effects by risk stratum | Single model with treatment-covariate interaction terms |
| Primary Output | Risk stratum-specific absolute and relative treatment effects | Individualized treatment effect predictions |
| Key Strength | Higher credibility; strong theoretical foundation via "risk magnification" | Potentially better discrimination of beneficiaries if true interactions exist |
| Key Limitation | May miss HTE unrelated to baseline risk | High vulnerability to overfitting and false positives |
Experimental Protocols for PATH Analyses
Protocol for Risk Modeling Analysis
Objective: To assess heterogeneity of treatment effects across strata of predicted baseline risk.
Materials:
- Dataset from a randomized controlled trial
- Statistical software (e.g., R, Python, SAS)
- Pre-specified outcome definition and candidate predictors
Procedure:
- Define the Risk Model:
- If using an external model, ensure it has been validated for predicting the trial's primary outcome in similar populations.
- If developing an internal model, use the control arm or the entire trial population (excluding treatment assignment) to build a multivariable prediction model for the outcome. Follow established prediction modeling guidelines (e.g., TRIPOD) [33].
- Generate Risk Scores:
- Apply the finalized risk model to all trial participants to calculate their predicted baseline risk of the outcome.
- Stratify by Risk:
- Divide participants into strata based on risk score quantiles (e.g., quartiles) or pre-defined clinical risk categories.
- Estimate Stratum-Specific Effects:
- Within each risk stratum, calculate both absolute risk differences and relative risk measures (e.g., hazard ratios, risk ratios) between treatment groups.
- Test for HTE:
- Statistically test for heterogeneity of treatment effects on the absolute and relative scales across risk strata. This can be done by including an interaction term between the linear predictor of risk and treatment assignment in a regression model [33].
- Present Results:
- Report event rates and treatment effects for each risk stratum.
- Graphically display the relationship between predicted risk and absolute treatment benefit [33].
Protocol for Effect Modeling Analysis
Objective: To develop a model that directly estimates how treatment effects vary with multiple patient characteristics.
Materials:
- Dataset from a randomized controlled trial with adequate sample size
- Statistical software with advanced modeling capabilities
- Pre-specified list of potential effect modifiers with strong biological or clinical rationale
Procedure:
- Covariate Selection:
- Limit the number of candidate effect modifiers to a small set with strong prior evidence supporting their potential role as treatment effect modifiers [35].
- Model Specification:
- Specify a regression model that includes main effects for treatment and selected covariates, plus interaction terms between treatment and the pre-specified effect modifiers.
- Model Fitting:
- Fit the model to the trial data. Consider using methods that reduce overfitting risk, such as penalized regression or pre-specifying interaction directions [35].
- Internal Validation:
- Use resampling techniques (e.g., bootstrapping) to evaluate the stability of interaction effects and assess potential overfitting.
- External Validation (Critical):
- Test the performance of the effect model in an external dataset, ideally from a different RCT. External validation is a key factor in establishing credibility for effect modeling findings [35].
- Generate Predictions:
- Use the validated model to predict absolute treatment effects for individual patients or patient subgroups.
- Evaluate Clinical Importance:
- Assess whether the variation in predicted absolute treatment effects across the population is sufficient to span clinically important decision thresholds [35].
Analytical Workflow and Decision Pathways
The following diagram illustrates the key decision points and methodological pathways when designing a predictive HTE analysis following the PATH framework:
The Scientist's Toolkit: Essential Reagents for PATH Implementation
Successful implementation of the PATH framework requires specific methodological components and analytical tools.
Table 2: Essential Research Reagents for PATH Analysis
| Tool Category | Specific Reagent/Solution | Function in PATH Analysis |
|---|---|---|
| Statistical Software | R Statistical Environment with 'RiskStratifiedEstimation' package | Provides open-source implementation of risk-based HTE assessment for observational data; enables standardized application across datasets [36] |
| Prediction Models | Validated outcome risk scores (e.g., ASCVD Risk Estimator) | Serves as external risk models for risk modeling approach; provides baseline risk stratification without needing internal model development [34] |
| Methodological Guidelines | ICEMAN (Instrument for Credibility of Effect Modification Analyses) | Provides adapted criteria for assessing credibility of HTE findings from both risk and effect modeling approaches [35] |
| Data Standards | OMOP Common Data Model | Enables standardized application of PATH framework across multiple observational databases by ensuring consistent coding of predictors and outcomes [36] |
| Validation Frameworks | Resampling methods (Bootstrapping, Cross-Validation) | Assesses internal validity of internally-developed risk or effect models; helps quantify overfitting risk [35] |
| Ceritinib D7 | Ceritinib D7, MF:C28H36ClN5O3S, MW:565.2 g/mol | Chemical Reagent |
| Flibanserin D4 | Flibanserin D4, CAS:2122830-91-3, MF:C20H21F3N4O, MW:394.4 g/mol | Chemical Reagent |
Application in Observational Studies and Future Directions
The PATH framework, initially developed for RCTs, has been successfully extended to observational comparative effectiveness research. A standardized framework for risk-based HTE assessment in observational databases involves five key steps: (1) definition of research aim; (2) database identification; (3) outcome prediction model development; (4) estimation of effects within risk strata with confounding adjustment; and (5) results presentation [36].
Recent evidence from a scoping review of PATH applications demonstrates that multivariable predictive modeling identified credible, clinically important HTE in approximately one-third of 65 examined reports [35]. Risk modeling produced credible findings more frequently (87%) than effect modeling (32%), though external validation substantially increased the credibility of effect modeling results [35].
Future methodological developments should focus on improving the robustness of effect modeling through machine learning approaches designed specifically for HTE detection and enhancing integration of PATH findings into clinical practice. As these methodologies mature, they hold the promise of generating more personalized evidence that better supports individual patient decision-making in drug development and clinical care.
Within the broader thesis on handling heterogeneity in comparative drug efficacy studies, this document provides detailed Application Notes and Protocols for implementing a specific analytical approach: risk-based assessment of Heterogeneity of Treatment Effects (HTE). A core limitation of comparative effectiveness research is that average treatment effect estimates can be inaccurate for a significant proportion of patients due to variation in individual characteristics [36]. The Predictive Approaches to Treatment effect Heterogeneity (PATH) statement established that baseline risk—a summary score representing a patient's outcome risk under the control condition—is a robust, patient-centered predictor for variation in absolute treatment benefit [33]. This protocol extends the PATH principles to the observational setting, detailing a standardized, scalable framework for stratifying patients by their predicted baseline risk to evaluate differential absolute and relative treatment effects across risk strata [36]. This methodology is crucial for personalized medicine, enabling a more nuanced benefit-harm trade-off analysis between alternative treatments.
Theoretical Foundation: PATH and Risk-Based HTE
Core Concepts
- Heterogeneity of Treatment Effects (HTE): The non-random variation in the magnitude or direction of a treatment effect across levels of a patient attribute, measured on a specific scale [33].
- Baseline Risk: The predicted risk of a clinical outcome for a patient under the control or comparator condition. It acts as a robust summary of multiple patient characteristics simultaneously [36] [33].
- Absolute Risk Difference (ARD): The difference in outcome risk between the treatment and control groups (CER - TER). The ARD is the most clinically relevant scale for decision-making and is mathematically dependent on the Control Event Rate (CER), making baseline risk a key driver of clinically important HTE [33].
- PATH Statement Guidance: Distinguishes between "risk modeling" and "effect modeling" approaches. This protocol focuses on the risk modeling approach, where a multivariable model predicts the outcome risk, and this model is then used to stratify patients and examine risk-based variation in treatment effects [33].
Rationale for Risk Stratification
Even when the relative risk reduction is constant across patients, the absolute benefit of a treatment increases as a patient's baseline risk increases. Risk-based stratification directly leverages this relationship to identify patients who stand to benefit most (or least) from an intervention in absolute terms [33]. This allows for:
- Identification of patient subgroups for whom the benefit-harm trade-off is favorable or unfavorable.
- More personalized clinical decision-making compared to relying on average treatment effects.
- A more robust and powerful alternative to one-variable-at-a-time subgroup analyses [36] [33].
Materials and Reagents
Research Reagent Solutions
Table 1: Essential Reagents and Computational Tools for Risk-Based HTE Analysis
| Item Name | Function/Description |
|---|---|
| Observational Healthcare Database | A real-world data source mapped to the OMOP Common Data Model (e.g., US claims databases like CCAE, MDCD, MDCR) [36]. |
| R Statistical Software & RStudio | The core computational environment for executing the analysis, favored for its flexibility and extensive package ecosystem [37]. |
RiskStratifiedEstimation R Package |
A dedicated, open-source R package designed for implementing the proposed 5-step framework across a network of OMOP-CDM databases [36]. |
| LASSO Logistic Regression | A machine learning algorithm used for both predictor selection in outcome prediction models and confounder adjustment in propensity score models [36]. |
| Cox Regression Models | Used within propensity score strata to estimate hazard ratios for the treatment effect on time-to-event outcomes [36]. |
Methodological Protocol
The proposed framework consists of five distinct steps, implemented here using the RiskStratifiedEstimation R package [36].
Step 1: Definition of the Research Aim
Objective: Precisely define the key components of the comparative effectiveness research question.
- Population: Define the target patient population. Example: "Patients with established hypertension."
- Treatment & Comparator: Specify the drug classes or interventions to be compared. Example: "Thiazide or thiazide-like diuretics (T) vs. Angiotensin-Converting Enzyme (ACE) inhibitors (C)."
- Outcome(s): Clearly state the efficacy and safety outcomes of interest. Example: "Efficacy: Acute Myocardial Infarction (MI), Hospitalization with Heart Failure, Stroke. Safety: Nine outcomes including hyponatremia, acute renal failure, cough, etc." [36].
Step 2: Identification of Relevant Databases
Objective: Identify and select appropriate observational databases for the analysis.
- Utilize databases mapped to the Observational Medical Outcomes Partnership (OMOP) Common Data Model (CDM) to ensure standardized analytics [36].
- Assess the suitability of each database based on sample size, data quality, and relevance to the research question.
- Example Databases: US claims databases such as IBM MarketScan Commercial Claims and Encounters (CCAE), IBM MarketScan Multi-State Medicaid (MDCD), and IBM MarketScan Medicare Supplemental Beneficiaries (MDCR) [36].
Step 3: Development of Outcome Prediction Model
Objective: Internally develop a model to predict the risk of the outcome used for stratification.
- Study Population: Use the propensity score-matched subset of the entire study population, excluding patients with the outcome prior to treatment initiation [36].
- Candidate Predictors: Include a large set of predefined covariates from the year prior to treatment index. These typically encompass demographics, disease and medication history, and comorbidity indices. Coding is uniform across OMOP-CDM databases [36].
- Model Fitting: Develop a separate prediction model for the outcome (e.g., 2-year acute MI risk) in each database using LASSO logistic regression with cross-validation for hyper-parameter selection [36].
- Model Performance: Evaluate the model's discriminative ability (e.g., using AUC) through internal validation.
Table 2: Key Specifications for the Prediction Model (Example: Acute MI Risk)
| Aspect | Specification |
|---|---|
| Outcome | 2-year risk of Acute Myocardial Infarction |
| Algorithm | LASSO Logistic Regression |
| Predictor Window | 1 year prior to treatment initiation |
| Covariates | Demographics, disease/medication history, Charlson comorbidity index |
| Validation | Internal validation via cross-validation |
Step 4: Estimation of Treatment Effects within Risk Strata
Objective: Stratify patients by predicted risk and estimate stratum-specific treatment effects, adjusting for confounding.
- Risk Stratification: Apply the developed prediction model to all patients. Stratify them into groups (e.g., quarters, or clinically relevant thresholds like <1%, 1-1.5%, >1.5%) based on their predicted baseline risk [36].
- Confounding Adjustment within Strata: Within each risk group, develop a propensity score model (again using LASSO logistic regression) for receiving the treatment vs. comparator. Then, stratify patients into 5 strata based on the propensity score [36].
- Treatment Effect Estimation:
- Relative Effects: Fit Cox regression models within each propensity score stratum to derive hazard ratios. The risk group-specific hazard ratio is obtained by averaging over the stratum-specific estimates [36].
- Absolute Effects: Calculate the difference in Kaplan-Meier estimates at a specific time point (e.g., 2 years) within each propensity score stratum. The risk group-specific absolute risk difference is obtained by averaging over these stratum-specific differences [36].
- Assessment: Ensure adequate overlap of propensity score distributions and sufficient sample size within all risk strata.
Step 5: Presentation of the Results
Objective: Clearly communicate the findings of the risk-based HTE analysis.
- Present both relative and absolute treatment effects for each outcome across the different risk strata [36].
- Use tables that list the effect estimates (Hazard Ratio, Absolute Risk Difference) for each risk group [38].
- Graphical displays, such as plots showing the absolute risk difference across the continuum of predicted risk, can be highly effective for illustrating the gradient of treatment benefit [33].
- Interpret the results in the context of clinical decision-making, highlighting risk strata where the benefit-harm trade-off is clearly favorable or unfavorable.
Anticipated Results and Interpretation
In a demonstration study comparing thiazide diuretics to ACE inhibitors in hypertension, the application of this framework revealed that patients at low predicted risk of acute myocardial infarction received negligible absolute benefits across several efficacy outcomes [36]. The absolute benefits became more pronounced in the highest risk group. This pattern underscores the value of risk-based assessment: it identifies patients who are unlikely to benefit meaningfully from a treatment, thereby avoiding unnecessary exposure to potential side effects and enabling a more efficient allocation of therapies. The analysis provides a structured way to move from an average, one-size-fits-all effect estimate to a nuanced understanding of how treatment effects are distributed across a heterogeneous patient population.
Effect Modeling with Regression and Machine Learning Algorithms
The pursuit of personalized medicine has fundamentally shifted the paradigm from assessing average treatment effects to understanding heterogeneity of treatment effects (HTE) across patient populations. Effect modeling provides a statistical framework for this exploration, enabling researchers to predict how patient characteristics influence therapeutic responses. These approaches move beyond traditional one-variable-at-a-time subgroup analyses to simultaneously consider multiple patient attributes, thereby offering more nuanced insights for drug development and clinical decision-making.
Within comparative drug efficacy research, effect modeling addresses a critical challenge: identifying which patients benefit most from specific interventions when head-to-head clinical trial evidence is limited. By leveraging both regression-based and machine learning algorithms, researchers can characterize effect heterogeneity, discover potential treatment effect modifiers, and generate individualized treatment effect estimates. This methodological foundation supports more precise treatment recommendations and informs drug development strategies.
Classifications of Methodological Approaches
Taxonomy of Effect Modeling Methods
Regression-based methods for predictive HTE analysis can be classified into three broad categories based on how they incorporate prognostic variables and treatment effect modifiers [13]. Table 1 summarizes the key characteristics, advantages, and limitations of each approach.
Table 1: Classification of Regression-Based Approaches for Heterogeneous Treatment Effect Analysis
| Method Category | Key Characteristics | Prognostic Factors | Effect Modifiers | Primary Output | Advantages | Limitations |
|---|---|---|---|---|---|---|
| Risk-Based Methods | Exploits mathematical dependency of absolute risk difference on baseline risk | Yes | No | Individualized absolute benefit predictions | Simple implementation; clinically intuitive | Assumes constant relative treatment effect; misses effect modification |
| Treatment Effect Modeling | Uses main effects and covariate-by-treatment interaction terms | Yes | Yes | Individualized absolute benefit estimates; patient subgroups | Comprehensive approach; addresses both prognosis and effect modification | Prone to overfitting; requires careful statistical handling |
| Optimal Treatment Regimes | Focuses primarily on treatment effect modifiers | No | Yes | Treatment assignment rules | Maximizes population benefit; clear decision rules | Does not quantify magnitude of benefit; ignores baseline risk |
Scale Dependence in Effect Modification
A critical consideration in effect modeling is scale dependence—the phenomenon where treatment effects may appear constant across patient subgroups on one scale but vary on another [8]. Table 2 illustrates how effect modification manifests differently on risk difference versus risk ratio scales using a hypothetical drug example.
Table 2: Scale Dependence in Treatment Effect Modification (Hypothetical Example)
| Patient Subgroup | Treated Group Risk | Control Group Risk | Risk Difference | Risk Ratio |
|---|---|---|---|---|
| Characteristic Present | 0.40 | 0.32 | 0.08 | 1.25 |
| Characteristic Absent | 0.50 | 0.40 | 0.10 | 1.25 |
| Measure of Effect Modification | - | - | 0.08 - 0.10 = -0.02 | 1.25/1.25 = 1.00 |
This scale dependence has important implications for clinical interpretation. While ratio measures (hazard ratios, odds ratios) are commonly used in statistical modeling due to convenience, risk differences are generally more informative for clinical decision-making as they directly estimate the number of patients needed to treat for benefit [8]. Best practices recommend reporting both measures along with outcome frequencies in each subgroup to enable comprehensive assessment.
Implementation Protocols for Effect Modeling
The DR-Learner Protocol for Conditional Average Treatment Effect Estimation
The DR-learner represents an advanced meta-learner approach that combines the strengths of both outcome modeling and propensity score weighting to estimate conditional average treatment effects (CATE) [39]. The methodology proceeds through three distinct stages:
Nuisance Parameter Estimation: Fit models for the outcome regression (μ̂â‚(ð±) = E[Y|X=ð±,A=a]) and propensity score (π̂(ð±) = P(A=1|X=ð±)) using base learners (e.g., random forests, gradient boosting, or regression models). Cross-fitting is recommended to avoid overfitting and ensure robustness.
Pseudo-Outcome Construction: Calculate the doubly robust pseudo-outcome for each patient using the formula that combines the observed outcome with the estimated nuisance parameters. This pseudo-outcome represents an unbiased estimate of the individual treatment effect.
CATE Estimation: Regress the pseudo-outcome on patient covariates using a separate machine learning algorithm to obtain final CATE estimates.
The doubly robust property ensures consistent treatment effect estimates if either the outcome model or the propensity score model is correctly specified, providing valuable safeguards against model misspecification [39]. This protocol is applicable to both randomized trials and observational data under standard causal assumptions.
Workflow to Assess Treatment Effect Heterogeneity (WATCH)
The WATCH framework provides a systematic approach for clinical trial sponsors to assess treatment effect heterogeneity through three core analytical objectives [39]:
Global Test for Heterogeneity: Perform hypothesis testing against the null hypothesis of treatment effect homogeneity across the patient population.
Effect Modifier Ranking: Derive a ranking of baseline covariates based on their strength as effect modifiers to prioritize variables for further investigation.
Individualized Treatment Effect Exploration: Visualize and explore how treatment effects vary with the most promising effect modifiers identified in the previous step.
This workflow integrates with the DR-learner and other meta-learners to provide a comprehensive analytical framework for HTE assessment in drug development. The protocol emphasizes pre-specification of analysis plans, appropriate adjustment for multiple testing, and multidisciplinary assessment of findings to inform development decisions.
Comparative Efficacy Assessment with Adjusted Indirect Comparisons
When head-to-head trial evidence is unavailable, adjusted indirect comparisons provide a methodology for comparing interventions through common comparators [40]. The protocol involves:
Evidence Network Identification: Identify all relevant trials connecting the interventions of interest through one or more common comparators.
Effect Size Extraction: Extract relative effect estimates (e.g., risk ratios, hazard ratios, mean differences) and their measures of precision (variances, confidence intervals) for each direct comparison.
Indirect Effect Calculation: Compute the indirect comparison using the Bucher method, where the relative effect of Intervention A versus B is calculated as the effect of A versus C divided by the effect of B versus C on the ratio scale [40].
Variance Estimation: Calculate the variance of the indirect estimate as the sum of the variances of the two direct comparisons, appropriately accounting for the increased uncertainty.
This approach preserves the randomization of the original trials and provides more valid comparisons than naïve direct comparisons across trials, which are susceptible to confounding by trial-level differences [40]. The methodology is accepted by major health technology assessment agencies including NICE (UK) and PBAC (Australia).
Applications in Real-World Evidence and Trial Settings
Real-World Data Applications
Real-world data (RWD) offers distinct advantages for HTE assessment, including larger sample sizes, more diverse patient populations, and longer follow-up times compared to traditional clinical trials [8]. When applying effect modeling to RWD, researchers should:
- Design studies to emulate a target randomized trial that would ideally answer the research question
- Identify potential confounders using systematic approaches and clearly articulate causal assumptions
- Use appropriate statistical methods to address confounding by both observed and unobserved covariates
- Assess the impact of bias from informative censoring, missing data, and measurement error
- Validate findings using sensitivity and bias analysis to assess robustness to key assumptions [26]
The expanded sample sizes in RWD enable more precise estimation of subgroup-specific treatment effects and facilitate discovery of rare safety outcomes that may not be detectable in conventional trials.
Integration Within Drug Development Pipeline
Effect modeling methodologies provide value across the drug development continuum. Table 3 outlines potential applications at different development stages.
Table 3: Effect Modeling Applications in Drug Development
| Development Stage | Primary Application | Methodological Emphasis | Decision Impact |
|---|---|---|---|
| Phase II | Signal detection for heterogeneous effects | Exploratory treatment effect modeling | Go/no-go decisions; population refinement for Phase III |
| Phase III | Confirmatory subgroup analysis; label claims | Pre-specified testing procedures; DR-learner implementation | Registration; personalized medicine claims |
| Post-Marketing | Effectiveness in broader populations; comparative effectiveness | Real-world data applications; indirect comparisons | Label updates; positioning versus competitors |
| Health Technology Assessment | Subgroup-specific cost-effectiveness | Value-based treatment regimes | Reimbursement decisions; treatment guidelines |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Methodological Components for Effect Modeling
| Research Reagent | Function | Implementation Considerations |
|---|---|---|
| Double Robust (DR) Learner | Estimates conditional average treatment effects with robustness to model misspecification | Requires separate estimation of outcome and propensity models; cross-fitting recommended for optimal performance [39] |
| Propensity Score Models | Estimates probability of treatment assignment given covariates | In RCTs, typically known by design; in observational studies, requires careful modeling to address confounding [39] |
| Machine Learning Base Learners | Flexible modeling of complex relationships between covariates and outcomes | Random forests, gradient boosting, neural networks, or ensembles; requires tuning parameter selection [13] |
| Interaction Term Selection | Identifies covariates exhibiting effect modification | Can use regularization (LASSO, MCP) to select important interactions from high-dimensional candidates [13] |
| Indirect Comparison Methods | Compares interventions through common comparators | Bucher method for simple networks; network meta-analysis for complex connected networks [40] |
| Model Evaluation Metrics | Assesses performance of predictive effect models | Includes C-for-benefit, Qini coefficient, precision in estimating heterogeneous effects; addresses challenges of unobservable counterfactuals [13] |
| Succinyl phosphonate | Succinyl phosphonate, CAS:26647-82-5, MF:C4H7O6P, MW:182.07 g/mol | Chemical Reagent |
Effect modeling with regression and machine learning algorithms provides a powerful methodological foundation for addressing heterogeneity in comparative drug efficacy research. By moving beyond average treatment effects to understand how interventions work across diverse patient populations, these approaches enable more personalized treatment recommendations and inform targeted drug development strategies.
The DR-learner and other meta-learners represent significant advances in causal inference methodology, offering robust approaches for estimating heterogeneous treatment effects even in high-dimensional settings. When integrated within systematic frameworks like WATCH and applied with appropriate attention to scale dependence and validation, these methods can generate actionable insights for researchers, clinicians, and drug developers seeking to optimize therapeutic benefits across patient populations.
Traditional explanatory randomized controlled trials (RCTs), while the gold standard for establishing efficacy, often employ highly selective populations studied in pre-defined settings, potentially limiting their applicability to the diverse patients encountered in routine clinical practice [41]. This approach can obscure critical heterogeneity in treatment effects and fail to provide evidence meaningful for real-world decision-making. Pragmatic clinical trials (PCTs) address this gap by integrating design features that closely resemble routine clinical practice, thereby directly capturing heterogeneity and enabling evidence generation that is more generalizable and patient-centered [41] [42]. Embracing heterogeneity through broad eligibility and flexible interventions is not merely a design choice but a fundamental shift towards generating evidence that reflects the spectrum of patients, providers, and settings that constitute actual healthcare delivery. The US Food and Drug Administration (FDA) Oncology Center of Excellence has recognized this potential, launching Project Pragmatica to explore the appropriate use of pragmatic design elements in trials for approved oncology products [42].
Core Pragmatic Elements for Capturing Heterogeneity
The design of a PCT exists on a continuum from explanatory to pragmatic. The PRECIS-2 tool provides a framework for evaluating and integrating pragmatic elements across nine domains, scored from 1 (very explanatory) to 5 (very pragmatic) [41]. The most common pragmatic elements identified in a recent review of use cases are detailed in the table below, which serves as a guide for protocol development.
Table 1: Key Pragmatic Trial Elements for Handling Heterogeneity
| Pragmatic Element | Traditional Explanatory Approach | Heterogeneity-Embracing Pragmatic Approach | Primary Domain(s) |
|---|---|---|---|
| Eligibility Criteria | Highly restrictive; narrow patient subset | Broad eligibility; minimal exclusions for safety [41] | Eligibility |
| Intervention Delivery | Strictly protocolized; fixed dosing & schedules | Flexible management; allows clinician/patient discretion [41] | Flexibility-Delivery |
| Comparator | Placebo or protocol-specific control | Usual care/Standard of Care (at clinician discretion) [41] | Intervention |
| Follow-Up & Data Collection | Frequent, dedicated trial visits | Minimal or no extra follow-up; use of Real-World Data (RWD) from EHRs, claims [41] | Follow-Up, Primary Outcome |
| Participant Recruitment | From research-oriented centers | From diverse routine practice settings [41] | Recruitment, Setting |
| Primary Outcome | Surrogate or laboratory measure | Patient-centered outcome meaningful in routine care [41] | Primary Outcome |
The implementation of these elements is widespread. A 2024 review of 22 use cases found that nearly all employed randomization (95.5%) and an open-label design (90.9%), with most using usual care (59.1%) or active comparators (18.2%) to reflect real-world choices [41]. Furthermore, half of the characterized use cases integrated RWD from sources like electronic health records (EHRs) and claims databases to enrich trial data or embed the trial within routine healthcare systems [41].
Experimental Protocol: A Framework for Pragmatic Trial Implementation
This protocol provides a methodological roadmap for designing and conducting a pragmatic trial that systematically embraces heterogeneity.
Protocol Title
A Phase IV Pragmatic, Randomized, Open-Label, Usual Care-Controlled Trial to Evaluate the Effectiveness and Safety of [Intervention X] in a Broad Population with [Condition Y].
Background and Rationale
[Condition Y] exhibits significant heterogeneity in patient characteristics, disease manifestations, and treatment responses. Current evidence from restrictive RCTs is insufficient to guide therapy across this diverse spectrum. This pragmatic trial aims to generate evidence on the effectiveness of [Intervention X] as used in routine practice across a heterogeneous patient population.
Primary and Secondary Objectives
- Primary Objective: To compare the patient-centered outcome of [e.g., overall survival, functional status] between [Intervention X] and usual care in a broad population with [Condition Y].
- Secondary Objectives: To assess safety, healthcare utilization, and to explore heterogeneity of treatment effect (HTE) across pre-specified subgroups.
Detailed Study Methodology
Study Design
- Framework: Prospective, randomized, open-label, usual care-controlled trial with parallel groups.
- Pragmatic Classification: High, as assessed by the PRECIS-2 tool [41].
Participant Eligibility Criteria
- Inclusion Criteria: Adult patients (≥18 years) with a clinical diagnosis of [Condition Y] for whom the treating clinician deems [Intervention X] a therapeutic option.
- Exclusion Criteria: Minimal, limited to conditions posing a safety risk (e.g., known hypersensitivity to [Intervention X]), inability to provide informed consent, or life expectancy < weeks.
Intervention and Comparator
- Intervention Arm: [Intervention X] administered according to approved labeling, with dosing and management adjustments permitted at the discretion of the treating clinician to reflect real-world practice.
- Comparator Arm: Usual Care, defined as any standard therapy(ies) for [Condition Y] selected by the treating clinician and patient. This may include other active treatments or best supportive care.
Randomization and Blinding
- Randomization: 1:1 allocation via a centralized system, stratified by key factors driving heterogeneity (e.g., age group, disease severity, comorbidity score) to ensure balance across arms.
- Blinding: Open-label design to reflect real-world conditions where clinicians and patients are aware of treatments.
Assessments and Data Collection
- Primary Endpoint: [e.g., Overall Survival] defined as time from randomization to death from any cause. Data will be collected primarily through linkage with RWD sources (e.g., national death registries, EHRs) [41].
- Secondary Endpoints: Patient-reported outcomes, emergency department visits, hospitalizations, and incidence of adverse events (collected via EHR extraction and streamlined case report forms).
- Schedule: Outcome assessments occur at times coinciding with routine clinical care. No additional study-specific visits or procedures are mandated.
Statistical Analysis Plan for Heterogeneity
- Primary Analysis: Intention-to-treat analysis comparing time-to-event for the primary endpoint using a Cox proportional hazards model, adjusted for stratification factors.
- Heterogeneity of Treatment Effect (HTE) Analysis: Pre-specified subgroup analyses will be conducted by including interaction terms in the statistical model. Subgroups are defined by:
- Clinical Factors: Age, sex, disease severity, comorbidities.
- Non-Clinical Factors: Geographic region, care setting, insurance type [43].
- Analysis Method: Interaction terms with a significance level of p<0.10 will be used to identify potential effect modifiers. The analysis will follow the taxonomy of heterogeneity, considering patient and non-patient factors [43].
Table 2: Pre-Specified Subgroups for Heterogeneity of Treatment Effect Analysis
| Stratification Factor | Subgroups | Rationale for Inclusion |
|---|---|---|
| Age | <65, 65-75, >75 years | Known differences in pathophysiology, polypharmacy, and treatment tolerance [43]. |
| Disease Severity | Mild, Moderate, Severe (per validated scale) | Treatment effect may vary with baseline prognosis. |
| Comorbidity Burden | Low (CCI 0-1), Medium (CCI 2-3), High (CCI ≥4) | Competing risks and drug-disease interactions can alter net benefit. |
| Socio-geographic | Urban vs. Rural; Insurance type (e.g., Medicare, Medicaid, Private) | Captures heterogeneity in access to care and system-level factors [43]. |
| Biomarker Status | e.g., Positive vs. Negative | For targeted therapies; a potential source of known heterogeneity [43]. |
Ethical and Regulatory Considerations
The protocol will be approved by a centralized Institutional Review Board (IRB). Informed consent will be obtained; however, the consent process may be simplified or integrated into the clinical workflow where approved. The trial will be conducted in accordance with ICH-GCP guidelines and registered on a public platform like ClinicalTrials.gov [44]. A Data Safety Monitoring Board (DSMB) will oversee participant safety.
Visualizing Workflows and Analytical Approaches
The following diagrams illustrate the core workflows and conceptual frameworks for implementing a heterogeneity-embracing pragmatic trial.
Pragmatic Trial Workflow Integrating RWD
Diagram Title: Pragmatic Trial Workflow with RWD Integration
Framework for Analyzing Heterogeneity of Treatment Effect
Diagram Title: Taxonomy of Heterogeneity Sources in Trials
Successfully conducting a PCT that embraces heterogeneity requires specific "reagents" and tools beyond traditional clinical trial supplies.
Table 3: Research Reagent Solutions for Pragmatic Trials
| Tool/Resource | Category | Function in Pragmatic Trials |
|---|---|---|
| PRECIS-2 Tool | Methodological Framework | A 9-domain tool to help trialists design trials that are fit for purpose and score their level of pragmatism [41]. |
| Real-World Data (RWD) Sources | Data Infrastructure | EHRs, claims databases, and registries enable broad recruitment, efficient follow-up, and outcome ascertainment without burdening sites [41]. |
| Structured Data Extraction Algorithms | Data Analytics | Code (e.g., in SQL, R, Python) to reliably map complex, unstructured EHR data into analyzable formats for endpoints and covariates. |
| Bayesian Statistical Models | Analytical Framework | Particularly useful for analyzing heterogeneity and borrowing information across subgroups in the absence of large sample sizes everywhere. |
| Tokenization/Matching Service | Data Privacy & Linkage | A secure service to link trial participant data with external RWD sources (e.g., registries) while protecting patient privacy [41]. |
| Patient-Reported Outcome (PRO) Platforms | Endpoint Measurement | Digital tools (web, app-based) to collect patient-centered data directly from participants in their own environment. |
Navigating Analytical Pitfalls and Enhancing the Credibility of HTE Findings
In the pursuit of personalized medicine, the investigation of heterogeneity of treatment effect (HTE) is a fundamental aspect of comparative drug efficacy studies. Subgroup analyses are essential for determining whether drug effects vary across demographic groups, disease severity levels, or biomarker status. However, unplanned post-hoc subgroup analyses conducted without proper statistical safeguards constitute data dredging (also known as p-hacking or data fishing), a practice that dramatically increases the risk of false-positive results by identifying patterns that appear statistically significant but actually occur by chance alone [45] [46].
Within drug development, this problematic practice manifests when researchers perform numerous statistical tests across multiple patient subgroups—defined by characteristics such as age, genetic markers, or prior treatments—and selectively report only those showing significant treatment effects [30]. The multiple comparisons problem arises naturally from this approach; conducting many statistical tests virtually guarantees that some will appear significant by random chance. For instance, performing 20 independent tests at a 5% significance level yields a 64% probability of at least one false-positive finding, fundamentally undermining the reliability of such findings [45] [30].
Statistical Foundations: Understanding the Mechanisms of Error
The Data Dredging Mechanism and Its Consequences
Data dredging involves testing multiple hypotheses using a single dataset through exhaustive searching for combinations of variables that show correlation or groups that demonstrate differences in their means [45]. In clinical trials, this often translates to repeatedly analyzing accumulating data without adjustment for multiple testing, excluding outliers without pre-specified criteria, or testing numerous subgroup interactions without hypothesis [45] [47].
The consequences for drug development are severe and multifaceted:
- Generation of false-positive results that mislead clinical decision-making
- Resource misallocation toward pursuing spurious leads in drug development pipelines
- Potential patient harm if treatments are incorrectly recommended for specific subgroups
- Erosion of scientific credibility when false findings are eventually refuted [45] [47]
Distinguishing Between Valid Subgroup Analysis and Data Dredging
The critical distinction between valid subgroup analysis and data dredging lies in the approach to hypothesis testing. Conventional statistical hypothesis testing begins with a research hypothesis formulated prior to data examination, followed by data collection and analysis to test this predetermined hypothesis. In contrast, data dredging uses the same dataset both to generate hypotheses and to test them, creating a self-referential loop that capitalizes on chance associations [45].
Table 1: Characteristics of Valid vs. Invalid Subgroup Analyses
| Characteristic | Valid Subgroup Analysis | Data Dredging |
|---|---|---|
| Hypothesis Formation | Pre-specified before data analysis | Generated after examining data |
| Statistical Adjustment | Adjusts for multiple comparisons | No adjustment for multiple testing |
| Transparency | Reports all analyses regardless of significance | Selective reporting of significant findings |
| Interpretation | Cautious interpretation of findings | Overstated clinical implications |
| Validation Plan | Includes plan for independent validation | No replication strategy |
Methodological Protocols for Rigorous Subgroup Analysis
Pre-Analysis Protocol: Study Design and Planning
Step 1: Define Subgroups A Priori
- Specify all subgroup variables and their cutpoints in the statistical analysis plan (SAP) before data collection or unblinding [30]
- Use established, clinically relevant cutpoints when available (e.g., age groups: <40, 40-65, >65 years) rather than data-driven percentiles [30]
- Document the scientific rationale for each subgroup based on pharmacological mechanisms or prior evidence
Step 2: Determine Analysis Methodology
- Pre-specify the statistical model for testing treatment-by-subgroup interactions, including adjustment variables [30]
- Allocate alpha (type I error rate) across primary and subgroup analyses using appropriate multiplicity adjustments [30]
- For biomarker-stratified designs, consider specialized trial designs that preserve power while controlling error rates
Step 3: Establish Stopping Rules and Data Handling Procedures
- Define fixed sample size or pre-determined interim analysis points in the protocol [45]
- Specify criteria for handling missing data and outliers prior to data collection [47]
- Document all planned data transformations and covariate adjustments
Analysis Execution Protocol: Statistical Testing and Visualization
Step 4: Implement Multiplicity Adjustments Apply appropriate statistical methods to control the overall type I error rate when testing multiple hypotheses:
- Bonferroni Correction: Simple but conservative; divides significance threshold by number of tests
- Hierarchical Testing: Tests hypotheses in pre-specified order, stopping when non-significance occurs
- Gatekeeping Procedures: Tests overall population first before proceeding to subgroups [30]
Step 5: Conduct Interaction Tests
- Test for treatment-by-subgroup interaction rather than comparing separate p-values across subgroups [30]
- Differentiate between quantitative interactions (varying effect sizes in same direction) and qualitative interactions (effect directions differ across subgroups), with the latter having greater clinical implications [30]
- Use the full dataset in a single model including treatment, subgroup, and interaction terms rather than fitting separate models for each subgroup [30]
Step 6: Visualize Results Appropriately
- Create forest plots to display treatment effects across subgroups with confidence intervals [30]
- Ensure visualization includes the subgroup size for each comparison
- Present both adjusted and unadjusted results when applicable
Diagram 1: Subgroup Analysis Workflow Protocol. This workflow outlines the sequential phases for conducting rigorous subgroup analyses while minimizing data dredging risks.
Post-Analysis Protocol: Interpretation and Reporting
Step 7: Categorize Findings Based on Analysis Type
- Confirmatory findings: Pre-specified subgroup analyses with adequate power and appropriate alpha control can support definitive conclusions [30]
- Exploratory findings: Unplanned subgroup analyses or underpowered tests should be explicitly labeled as hypothesis-generating for future studies [30]
Step 8: Report with Complete Transparency
- Document all subgroup analyses conducted, regardless of statistical significance [47]
- Report the total number of subgroups examined to provide context for readers
- Acknowledge limitations related to multiple testing and power constraints
Step 9: Plan External Validation
- Significant subgroup findings from exploratory analyses require validation in independent datasets [45]
- Consider prospective validation in future trials or through collaboration with independent researchers
Practical Implementation in Drug Development Research
Statistical Reagent Solutions for Subgroup Analysis
Table 2: Essential Methodological Tools for Robust Subgroup Analysis
| Method/Tool | Primary Function | Application Context |
|---|---|---|
| Bonferroni Correction | Controls family-wise error rate by dividing alpha by number of tests | Appropriate for small number of pre-specified subgroups |
| Hierarchical Testing | Tests hypotheses sequentially while controlling overall error rate | Useful when subgroups have logical ordering of importance |
| Gatekeeping Procedures | Tests overall population before subgroup analyses | Prevents subgroup claims when overall effect is null |
| Forest Plots | Visualizes treatment effects and confidence intervals across subgroups | Standard presentation method for subgroup analyses in publications |
| Interaction P-values | Tests whether treatment effect differs significantly across subgroups | More valid than comparing separate p-values across subgroups |
| Bootstrap Resampling | Assesses stability of subgroup findings | Useful for validating data-driven cutpoints |
Case Example: IPASS Trial of Gefitinib in NSCLC
The IPASS trial in non-small cell lung cancer (NSCLC) provides a paradigmatic example of a valid subgroup analysis that identified a qualitative interaction based on a strong biological rationale. The trial demonstrated that gefitinib was superior to carboplatin-paclitaxel in patients with EGFR mutation-positive tumors but inferior in EGFR wild-type patients [30]. This finding was credible because:
- The subgroup was defined by a predictive biomarker with clear biological plausibility
- The interaction was qualitative (opposite treatment effects in different subgroups)
- The finding transformed treatment selection in NSCLC, demonstrating clinical utility
Diagram 2: Valid vs. Data Dredging Approaches to Subgroup Analysis. This decision pathway highlights the critical methodological distinctions between rigorous and problematic analytical practices.
Power Considerations and Sample Planning
A fundamental challenge in subgroup analysis is limited statistical power. Testing treatment-by-subgroup interactions typically requires approximately four times the sample size needed to detect an overall treatment effect of the same magnitude [30]. This power constraint means that many clinically important subgroup effects may go undetected in trials designed primarily for overall population effects.
When planning studies where subgroup analyses are a key objective, researchers should:
- Conduct formal power calculations specifically for the subgroup interaction tests
- Consider stratified recruitment to ensure adequate representation in key subgroups
- Explore adaptive designs that allow for sample size increases if promising subgroup effects emerge
The investigation of heterogeneity of treatment effect is scientifically necessary but methodologically treacherous. Avoiding data dredging requires disciplined pre-specification, appropriate statistical adjustment for multiple comparisons, cautious interpretation, and complete transparency in reporting. By implementing the protocols outlined in this document, drug development researchers can responsibly investigate heterogeneous treatment effects while minimizing the risk of false discoveries that misdirect research resources and potentially harm patients.
The future of subgroup analysis lies in moving beyond simplistic data dredging approaches toward methods that integrate biological plausibility, statistical rigor, and clinical relevance. As precision medicine advances, the ability to identify true subgroup effects will become increasingly critical for optimizing therapeutic benefits across diverse patient populations.
Addressing the Multiplicity Problem and Controlling Type I Error in Subgroup Testing
The investigation of heterogeneity of treatment effects (HTE) is a fundamental goal in comparative drug efficacy research, aiming to understand why medications work differently across patient populations [8]. A primary method for exploring HTE is subgroup analysis, which evaluates how a treatment effect changes across levels of a baseline characteristic, or effect modifier [8]. While crucial for personalizing treatment strategies, this practice introduces a significant statistical challenge: the multiplicity problem.
Multiplicity arises when multiple statistical hypotheses are tested simultaneously, such as assessing treatment effects across numerous patient subgroups. Each test carries an inherent probability of a false positive finding (Type I error). Without proper control, the probability of falsely declaring at least one subgroup effect as significant—the family-wise error rate (FWER)—inflates substantially. For example, testing just five independent hypotheses at an unadjusted α=0.05 yields a ~23% chance of at least one false positive, far exceeding the nominal level [48]. This issue is pervasive in clinical trials featuring multiple endpoints, treatment arms, or populations, and its inadequate management contributes to the reproducibility crisis in life sciences, where consistent results are found in as few as 26% of replications [48]. This document outlines rigorous application notes and protocols for controlling Type I error in subgroup testing within drug development.
Quantitative Landscape of Current Practices and Challenges
The application of multiplicity adjustments in clinical research remains suboptimal. A systematic review of multi-arm trials found that only 62% of studies requiring adjustments accounted for multiplicity [48]. The table below summarizes the prevalence of adjustment practices across various medical fields, revealing great disciplinary variation and widespread underutilization.
Table 1: Prevalence of Multiplicity Adjustments in Clinical Trials Across Disciplines
| Study (First Author) | Year Published | Scientific Field | Number of Studies Investigated | Proportion of Studies with Adjustments | Most Common Method |
|---|---|---|---|---|---|
| Wason et al. | 2014 | Multi-arm Clinical Trials | 59 | 51% | Hierarchical/Closed and Bonferroni |
| Tyler et al. | 2011 | Neurology and Psychiatry | 55 | 5.8% | Bonferroni |
| Vickerstaff et al. | 2015 | Neurology and Psychiatry | 209 | 25% | Bonferroni |
| Kirkham et al. | 2015 | Otolaryngology | 195 | 10% | Bonferroni |
| Stacey et al. | 2012 | Ophthalmology (Abstracts) | 5,385 | 14% | Bonferroni and Tukey |
| Dworkin et al. | 2016 | Pain, RCTs | 101 | 21% | Bonferroni, Gatekeeping, Sidák |
| Brand | 2021 | Cardiovascular, RCTs | 130 (with subgroups) | ~2% | Unspecified |
| Nevins | 2022 | Pragmatic Clinical Trials | 262 Final Reports | 11% | Bonferroni |
| Pike | 2022 | General Medicine, RCTs | 138 | 48% (for multiple treatments) | Bonferroni, Holm, Hochberg |
Several key challenges contribute to this landscape:
- Operational Complexity: Modern trial designs are complex, involving multiple endpoints, doses, and adaptive features, making the implementation of corrections technically challenging [48].
- Cultural and Publication Biases: Academia's "publish or perish" culture often favors novel, significant results over rigorous, reproducible work, leading to selective reporting and p-hacking [48].
- Distinction Between Confirmatory and Exploratory Analyses: Exploratory, hypothesis-generating analyses may not require the same stringency as confirmatory ones, but the line is often blurred, and exploratory results are frequently presented with overstated claims [48].
Methodological Framework for Multiplicity Control
Foundational Concepts and When to Adjust
A foundational step is distinguishing between the comparison-wise error rate (pertaining to a single hypothesis) and the family-wise error rate (FWER) (the probability of at least one false positive among all hypotheses in a family) [49]. Regulatory guidance requires strong control of the FWER in confirmatory trials, meaning the error rate is controlled under all configurations of true and false null hypotheses [49].
Multiplicity adjustments are critical in studies with [48]:
- Multiple Subgroups: Analyses of treatment effects across multiple patient strata (e.g., by age, genotype, comorbid conditions).
- Multiple Endpoints: Several outcome measures are assessed.
- Repeated Measures: Outcomes are evaluated at multiple time points.
- Multiple Treatment Arms: Several doses or regimens are compared to a shared control.
Adjustments may be less critical for a small set of coprimary endpoints where success requires an effect on all outcomes, or when testing distinct, unrelated hypotheses [48].
A range of statistical methods exists to control the FWER. The choice depends on the relationship between the hypotheses (non-hierarchical vs. hierarchical) and the desired balance between power and stringency.
Table 2: Key Multiple Testing Procedures for Controlling Family-Wise Error Rate (FWER)
| Procedure | Category | Methodology | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Bonferroni | Non-Hierarchical, Single-Step | Divides alpha (α) equally among m tests. Rejects H~i~ if p~i~ ≤ α/m. | Simple, intuitive, flexible. | Overly conservative, especially with many tests or correlated outcomes. |
| Holm | Non-Hierarchical, Step-Down | Orders p-values. Sequentially tests: if p~(~1~) ≤ α/m, reject H~(~1~); if p~(~2~) ≤ α/(m-1), reject H~(~2~), etc. | Uniformly more powerful than Bonferroni. Simple application. | Does not leverage correlation structure. |
| Hochberg | Non-Hierarchical, Step-Up | Orders p-values. Starts with largest: if p~(~m~) ≤ α, all hypotheses rejected; if not, compares p~(~m-1~) ≤ α/2, etc. | More powerful than Holm when many hypotheses are false. | Assumes independent test statistics. |
| Fixed-Sequence | Hierarchical | Tests hypotheses in a pre-specified order at full α. Proceeds only if the current test is significant. | Maximizes power for primary questions. Simple. | Lacks power if an early hypothesis is not rejected. Order choice is critical. |
| Fallback | Hierarchical | Allocates alpha to hypotheses. Unused alpha is "passed down" to subsequent hypotheses. | More robust than fixed-sequence; uses allocated alpha more efficiently. | Requires careful pre-specification of weighting. |
| Gatekeeping | Hierarchical | Tests families of hypotheses in sequence. Testing in a secondary family requires success in the primary family. | Handles complex, hierarchically ordered objectives (e.g., primary vs. secondary endpoints). | Can be complex to design and communicate. |
| Graphical Approach | Flexible Framework | Represents hypotheses and alpha allocations with a weighted, directed graph. Allows recycling of alpha. | Highly flexible, visual, can emulate many other procedures. | Requires specialized software and statistical expertise. |
The following workflow diagram illustrates the decision process for selecting an appropriate multiplicity control strategy in a subgroup analysis plan.
Experimental Protocols for Implementation
Protocol: Pre-Specification and Prevention of P-Hacking
Purpose: To ensure transparency and minimize bias by detailing all subgroup analyses and the statistical approach before data collection or examination.
Procedure:
- Develop a Statistical Analysis Plan (SAP): The SAP must be finalized before database lock and, for confirmatory trials, before trial unblinding.
- Define Subgroups of Interest: Clearly list all baseline characteristics (e.g., age, sex, genotype, disease severity) that will be used for subgroup analyses. Justify their selection based on biological plausibility or prior evidence.
- Specify the Multiplicity Strategy: Apply the pre-SPEC framework [48]:
- Pre-specify all analyses before participant recruitment.
- Define a single primary analysis strategy for each subgroup test.
- Create detailed plans for each analysis, including the specific multiple testing procedure (e.g., Holm procedure).
- Provide enough detail for independent replication.
- Document Rationale: Justify the choice of multiple testing procedure based on the trial's objective and hypothesis structure.
Protocol: Applying the Holm-Bonferroni Procedure in Subgroup Analysis
Purpose: To control the FWER when testing treatment effects in multiple, pre-specified subgroups with higher power than the single-step Bonferroni correction.
Reagents and Analytical Tools: Table 3: Research Reagent Solutions for Subgroup Analysis
| Item | Function/Description | Example/Note |
|---|---|---|
| Statistical Software (R, SAS, Python) | Platform for performing statistical tests and implementing correction algorithms. | R packages: multtest, multcomp; SAS PROC MULTTEST. |
| Clinical Trial Dataset | The cleaned, locked database containing treatment arm, outcome, and subgroup variables. | Must undergo quality assurance checks for missing data and anomalies [50]. |
| Pre-Specified Analysis Plan | The protocol defining the family of subgroup tests and the correction method. | Essential for preventing p-hacking and data dredging [48]. |
Procedure:
- Formulate Hypotheses: Define the null hypothesis for each of the m subgroups (e.g., H~i~: No treatment effect in the i-th subgroup).
- Perform Statistical Tests: For each subgroup, conduct the appropriate test (e.g., Cox regression for time-to-event, logistic regression for binary outcomes) to obtain a raw p-value, p~i~.
- Order P-values: Sort the p-values from all subgroup tests from smallest to largest: p~(~1~) ≤ p~(~2~) ≤ ... ≤ p~(~m~). The corresponding hypotheses are H~(~1~), H~(~2~), ..., H~(~m~).
- Sequential Testing:
- Compare p~(~1~) to α/m. If p~(~1~) ≤ α/m, reject H~(~1~) and proceed. Otherwise, stop and reject no hypotheses.
- Compare p~(~2~) to α/(m-1). If p~(~2~) ≤ α/(m-1), reject H~(~2~) and proceed.
- Continue this pattern, comparing p~(~j~) to α/(m - j + 1).
- The procedure stops when a p-value fails to meet its critical value.
- Interpretation: All hypotheses that were rejected in the sequential steps are declared statistically significant, with the FWER controlled at α.
Protocol: Assessing Effect Modification on Different Scales
Purpose: To correctly quantify and report heterogeneity of treatment effects (HTE), acknowledging that effect modification is scale-dependent.
Procedure:
- Calculate Stratum-Specific Effects: For each level of the potential effect modifier (subgroup), calculate the treatment effect. Crucially, calculate this effect on both the additive (risk difference, RD) and multiplicative (risk ratio, RR; or hazard ratio, HR) scales [8].
- Quantify Effect Modification:
- On the Additive Scale: Compute the difference between the RDs across subgroups: RD~Strata1~ - RD~Strata2~.
- On the Multiplicative Scale: Compute the ratio of the RRs across subgroups: RR~Strata1~ / RR~Strata2~.
- Report Comprehensively: Best practices for reporting include [8]:
- Clearly state the scale on which effect modification was assessed.
- Report the frequency of the outcome in each subgroup for both treated and control groups.
- Present the measures of effect modification (difference in RDs, ratio of RRs) with confidence intervals.
The following diagram visualizes the logical sequence for a robust subgroup analysis workflow, from planning to reporting.
Effectively addressing the multiplicity problem in subgroup analysis is non-negotiable for producing reliable and reproducible evidence in comparative drug efficacy research. As explored in the broader thesis on handling heterogeneity, understanding HTE through subgroup analysis is essential for personalizing medicine, but it must be pursued with rigorous statistical discipline. This involves a steadfast commitment to pre-specification, a thoughtful selection of multiple testing procedures that align with the study's structure and goals, and transparent reporting of all findings. By integrating these protocols, researchers can robustly characterize heterogeneity of treatment effects while safeguarding against spurious false-positive claims, thereby strengthening the evidential foundation for drug development and personalized treatment strategies.
Overcoming the Low Statistical Power of Interaction Tests
The accurate detection of interaction effects, also known as effect measure modification or heterogeneous treatment effects, is crucial for advancing personalized medicine and understanding comparative drug efficacy. In studies of heterogeneous treatment effects, a drug may work effectively in some patient subpopulations but show limited efficacy in others [51]. Traditional statistical methods designed to detect average treatment effects are often underpowered for identifying these interactions, potentially causing beneficial treatments for specific subgroups to be overlooked during drug development and regulatory evaluation [51]. This application note addresses the fundamental challenges of low statistical power in interaction tests and provides practical, evidence-based solutions for researchers, scientists, and drug development professionals working to optimize comparative drug efficacy studies.
The Statistical Challenge of Detecting Interactions
Quantifying the Power Problem
Interaction tests require substantially larger sample sizes than main effect tests to achieve comparable statistical power. Under reasonable assumptions where interactions are approximately half the size of main effects, detecting an interaction requires approximately 16 times the sample size needed to detect a main effect of the same magnitude [52]. This sample size requirement stems from the larger standard errors associated with interaction terms in statistical models.
Table 1: Power Comparison Between Main Effects and Interaction Tests
| Statistical Test Type | Relative Standard Error | Relative Sample Size Needed | Typical Power Scenario |
|---|---|---|---|
| Main Effect | 1x | 1x | 80% power with standard sample size |
| Interaction Effect | 2x | 16x | 10% power with standard sample size |
The practice of raising the Type I error rate from 5% to 20% to compensate for low power provides only limited benefit. Research demonstrates that this strategy results in useful power gains (at least 10% increase, achieving power ≥70%) in only 26% of scenarios studied. In the remaining cases, power was either already adequate (30%) or so low that it remained weak even after raising the Type I error rate (44%) [53].
Additional Risks with Underpowered Tests
Low-powered interaction tests not only miss true effects but also systematically exaggerate the magnitude of effects when they are detected. In studies with low statistical power (e.g., 30% power), statistically significant results may overestimate the true effect size by a factor of three or more [54]. This inflation occurs because only the most extreme effect sizes reach statistical significance in underpowered studies, creating a biased representation of the actual treatment effect heterogeneity.
Experimental Protocols for Powerful Interaction Tests
Protocol 1: A Priori Power Analysis for Interaction Detection
Purpose: To determine the appropriate sample size required to detect interaction effects with sufficient statistical power before study initiation.
Materials:
- Statistical software with power analysis capabilities (R, SAS, PASS, G*Power)
- Preliminary estimates of main effects and interaction effect sizes
- Knowledge of outcome variable distribution and variance
Procedure:
- Define Effect Sizes: Estimate plausible effect sizes for main effects based on prior literature or pilot studies. Define the smallest interaction effect size that would be clinically meaningful.
- Set Power and Alpha: Specify desired statistical power (typically 80% or 90%) and Type I error rate (typically 0.05 for main effects, though some recommend 0.10-0.20 for interactions) [53].
- Calculate Sample Size: Use power analysis formulas for interaction terms in the planned statistical model (e.g., logistic regression, linear regression). Remember that for interactions half the size of main effects, the required sample size may be 16 times larger than for detecting the main effect alone [52].
- Account for Multiple Testing: Adjust sample size upward if testing multiple interactions to maintain appropriate family-wise error rates.
- Document Assumptions: Clearly record all assumptions and parameter estimates used in the power analysis for future reference.
Validation:
- Conduct sensitivity analyses to determine how sample size requirements change with varying assumptions about effect sizes and variance.
- For novel interactions with high uncertainty, consider adaptive designs that allow for sample size re-estimation.
Protocol 2: Targeted Statistical Analysis for Heterogeneous Treatment Effects
Purpose: To properly analyze and detect heterogeneous treatment effects using statistical methods with optimal power for interaction detection.
Materials:
- Cleaned, curated dataset with appropriate quality control measures
- Statistical software (R, SAS, Python, or other specialized packages)
- Pre-specified analysis plan documenting all intended analyses
Procedure:
- Model Specification: Use appropriate statistical models that include both main effects and interaction terms. For binary outcomes, employ logistic regression; for continuous outcomes, use linear regression; for time-to-event outcomes, utilize Cox proportional hazards models.
- Coding of Predictors: Code categorical variables using effects coding (-0.5, 0.5) rather than dummy coding (0, 1) to maintain comparable standard errors across main effects and interactions [52].
- Estimation Method: Consider using likelihood ratio tests rather than Wald tests for interaction terms, as they may provide better statistical properties [53].
- Stratified Analysis: Conduct stratified analyses to visualize and quantify interaction effects in different subgroups.
- Novel Methods for Heterogeneous Effects: Implement specialized statistical tests designed specifically for detecting heterogeneous treatment effects, such as the aziztest (available as an R package) when there is reason to believe a drug only works in a subset of patients [51].
Interpretation:
- Report both point estimates and confidence intervals for interaction terms, not just p-values.
- Evaluate the clinical significance of interaction effects, not just statistical significance.
- Consider the potential for exaggeration of effect sizes, particularly in underpowered studies [54].
Table 2: Comparison of Statistical Tests for Interaction Detection
| Statistical Test | Best Use Case | Power Considerations | Implementation Complexity |
|---|---|---|---|
| Wald Test | General purpose interaction testing | Lower power for small samples | Low (standard in most software) |
| Likelihood Ratio Test | Nested model comparisons | Generally higher power than Wald | Moderate (requires model comparison) |
| Breslow-Day Test | Heterogeneity of odds ratios | Good for categorical data | Moderate |
| Novel Heterogeneous Effect Tests (e.g., aziztest) | Suspected subgroup-specific efficacy | Superior power when heterogeneity exists | High (specialized packages) |
Visualization of the Interaction Detection Workflow
Diagram 1: Interaction Test Workflow
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Statistical Solutions for Interaction Studies
| Reagent/Solution | Function/Application | Implementation Notes |
|---|---|---|
| R Statistical Environment with 'aziztest' package | Specialized testing for heterogeneous treatment effects | Superior power when drug efficacy exists only in patient subsets [51] |
| Power Analysis Software (PASS, G*Power, R pwr package) | Sample size determination for interaction effects | Calculate requirements based on 16× sample size rule for interactions [52] |
| Effects Coding Implementation | Proper parameterization of categorical variables in models | Use (-0.5, 0.5) coding instead of (0, 1) for balanced standard errors [52] |
| Multiple Testing Correction Methods | Control of false discovery rates in interaction screening | Benjamini-Hochberg procedure for exploratory analyses |
| Likelihood Ratio Test Framework | Comparison of nested models with and without interaction terms | Generally higher power than Wald tests for interaction detection [53] |
Overcoming the low statistical power of interaction tests requires a multifaceted approach that begins with realistic power analysis and sample size planning, acknowledging the substantially greater requirements for detecting interactions compared to main effects. Researchers should employ appropriate statistical methods, including specialized tests for heterogeneous treatment effects when subgroup-specific efficacy is plausible. Proper coding of predictor variables and careful interpretation of results, with attention to potential effect size exaggeration in underpowered studies, are essential components of a robust methodology for detecting interaction effects. By implementing these evidence-based approaches, drug development professionals can enhance their ability to identify meaningful heterogeneous treatment effects, ultimately advancing the field of personalized medicine and improving patient outcomes through better understanding of comparative drug efficacy across patient subpopulations.
Strategies for Managing Heterogeneity in Pragmatic Trial Designs and Analyses
Pragmatic clinical trials (PCTs) are fundamentally designed to inform healthcare decisions by testing interventions under conditions that closely mirror routine clinical practice [55]. Unlike traditional explanatory trials that seek to understand whether a treatment can work under ideal conditions, pragmatic trials answer the question of which treatment we should prefer in real-world settings [56]. This core objective makes the management of heterogeneity—the inherent variability in patients, settings, interventions, and outcomes—a central consideration in PCT design and analysis.
Within the context of comparative drug efficacy studies, heterogeneity is not merely a statistical nuisance but a reflection of clinical reality that must be embraced and properly managed. When evaluating drugs in real-world populations, researchers encounter substantial diversity in patient characteristics, clinical settings, co-interventions, and adherence patterns [56]. Effectively managing this heterogeneity is crucial for generating evidence that is both scientifically valid and broadly applicable to diverse patient populations and healthcare settings. The strategies outlined in this application note provide a framework for researchers to address these challenges systematically while maintaining the integrity and relevance of their findings.
Theoretical Framework: Typology of Heterogeneity
In pragmatic trials, heterogeneity manifests in several distinct forms, each requiring specific management approaches. Understanding this typology is essential for selecting appropriate design and analysis strategies.
Clinical heterogeneity encompasses variability in participant characteristics, including demographics, disease severity, comorbidities, and genetic factors. This type of heterogeneity is particularly relevant in drug efficacy studies where treatment response may be modified by these patient-level factors [1]. In pragmatic trials, clinical heterogeneity is generally desirable as it enhances the generalizability of findings to broader populations [56].
Methodological heterogeneity refers to variability in trial design, intervention delivery, outcome assessment, and data collection methods across sites or studies. In pragmatic trials, this may include differences in how a drug is administered, what co-interventions are permitted, or how outcomes are measured in different clinical settings [56]. While some methodological heterogeneity is inevitable and even desirable in PCTs, excessive variability can complicate interpretation of results.
Setting-related heterogeneity arises from differences in healthcare systems, practice patterns, resources, and expertise across participating sites. A hallmark of pragmatic trials is the deliberate inclusion of diverse care settings—from academic medical centers to community hospitals—to ensure findings are applicable across the healthcare spectrum [56].
Table 1: Types of Heterogeneity in Pragmatic Trials and Their Management
| Type of Heterogeneity | Description | Desirability in PCTs | Primary Management Strategies |
|---|---|---|---|
| Clinical Heterogeneity | Variability in patient demographics, disease severity, comorbidities, and genetic factors | Generally desirable | • Broad eligibility criteria• Stratified randomization• Subgroup analysis planning |
| Methodological Heterogeneity | Variability in intervention delivery, outcome assessment, and data collection methods | Context-dependent | • Define core intervention elements• Use objective outcomes• Standardize key measurements |
| Setting-related Heterogeneity | Differences in healthcare systems, resources, and practice patterns across sites | Generally desirable | • Include diverse centers• Center-level stratification• Mixed-effects models |
Pragmatic Strategies for Managing Heterogeneity in Trial Design
Embracing Heterogeneity in Patient Populations and Settings
Pragmatic trials should deliberately incorporate heterogeneity in patients and settings to enhance the applicability and generalizability of their findings. This approach stands in stark contrast to explanatory trials, which often impose strict eligibility criteria to create homogeneous study populations [56].
Center Selection and Recruitment: PCTs should intentionally recruit a diverse range of centers that reflect the settings where the intervention will ultimately be implemented. This includes balancing academic medical centers with community hospitals, and representing variations in geographic location, resource availability, and patient demographics [56]. For example, the NUTRIREA-2 trial deliberately included both university and community hospitals (64% and 36%, respectively) to ensure its findings would be applicable across the French intensive care system [56]. When designing multi-center trials, researchers should consider maximizing the number and diversity of participating sites, potentially at the cost of reducing the number of patients per center, to enhance representativeness.
Eligibility Criteria: Pragmatic trials typically employ fewer and less restrictive selection criteria compared to explanatory trials [56]. The goal is to include "anyone who would be eligible to receive the intervention in clinical practice" rather than narrowly defined subgroups [55]. This approach respects the principle that clinicians should have discretion to enroll patients only when genuine uncertainty (equipoise) exists about which trial arm would be most beneficial [55]. For instance, a pragmatic trial of pancreaticoduodenectomy might include participants with worse performance status (e.g., up to ECOG 2) who would be considered for the procedure in routine practice, rather than restricting enrollment to optimal candidates [55].
Managing Heterogeneity in Interventions and Comparators
In pragmatic drug trials, heterogeneity in how interventions are delivered and what constitutes usual care is expected and should be accommodated in the trial design.
Intervention Flexibility: Pragmatic designs typically allow some tailoring of interventions while maintaining core elements that define the treatment being assessed [56]. This approach acknowledges that in real-world practice, clinicians adapt interventions to individual patient needs and local resources. For drug trials, this might mean permitting dose adjustments, managing side effects, or accommodating concomitant medications as would occur in routine care, rather than enforcing strict protocol-specified regimens [56].
Usual Care Comparators: Control interventions in pragmatic trials should reflect usual care practices without artificial restrictions or enhancements that would not occur outside the trial context [56]. This means avoiding the use of placebos unless absolutely necessary and allowing the same flexibility in the control arm that clinicians would normally exercise. The result is a more valid comparison of the experimental intervention against real-world alternatives, though this introduces heterogeneity in what constitutes "usual care" across sites and clinicians.
Adherence Considerations: Unlike explanatory trials that often implement extensive monitoring and enforcement of protocol adherence, pragmatic trials generally do not employ special measures to ensure compliance beyond what would be used in routine practice [55] [56]. This approach more accurately reflects the effectiveness of interventions under real-world conditions where adherence varies.
Table 2: Contrasting Approaches to Intervention Design in Explanatory vs. Pragmatic Trials
| Design Element | Explanatory Trial Approach | Pragmatic Trial Approach | Rationale for Pragmatic Approach |
|---|---|---|---|
| Inter Protocol | Highly standardized and protocolized | Permits tailoring while maintaining core elements | Mimics real-world adaptation of treatments |
| Control Intervention | Often placebo or highly standardized comparator | Reflects usual care with its inherent variability | Provides relevant comparison to actual practice |
| Co-interventions | Restricted or prohibited | Permitted as in routine care | Acknowledges reality of complex patients |
| Adherence Monitoring | Active monitoring and enforcement | No special measures beyond routine practice | Reflects real-world adherence patterns |
| Blinding | Typically double-blinded | Often open-label; avoids blinding unless essential | Reflects real-world knowledge of treatments |
Outcome Selection and Assessment in Heterogeneous Contexts
The choice and measurement of outcomes in pragmatic trials must balance scientific rigor with feasibility and relevance across diverse settings.
Outcome Relevance: Pragmatic trials should prioritize outcomes that matter to patients and other stakeholders, such as quality of life, functional status, and other patient-centered endpoints [55]. For example, the CODA trial comparing antibiotics with appendectomy for acute uncomplicated appendicitis used health-related quality of life as its primary outcome, recognizing this as the most relevant measure from the patient perspective [55].
Assessment Methods: To maintain pragmatism, outcome assessment should leverage data routinely collected in clinical care whenever possible [55]. This includes using electronic health records, administrative claims data, or disease registries rather than implementing resource-intensive, study-specific assessments [55] [56]. Objective outcomes that can be measured consistently across sites are preferred, as they reduce the need for standardization, adjudication, and blinding of outcome assessors [56].
Analytical Approaches for Heterogeneous Data
Statistical Considerations for Heterogeneous Populations
The analysis of pragmatic trials must account for the multi-level structure of the data arising from heterogeneous settings and populations.
Intention-to-Treat Principle: Pragmatic trials should primarily analyze data according to the intention-to-treat principle, including all randomized participants in the groups to which they were originally assigned [55] [56]. This approach preserves the randomized design's protection against selection bias and provides an unbiased estimate of the intervention's effectiveness as implemented in real-world practice, where not all patients receive or adhere to assigned treatments.
Handling Cluster Effects: In cluster-randomized trials or multi-center individually randomized trials, analytical methods must account for the intracluster correlation—the tendency for patients within the same cluster or center to have more similar outcomes than patients in different clusters [56]. Mixed-effects models, generalized estimating equations, or other cluster-adjusted techniques should be employed to account for this data structure.
Sample Size Considerations: The presence of heterogeneity, particularly in cluster-randomized designs, often necessitates larger sample sizes to maintain statistical power. Researchers should consider the likely extent of non-adherence, contamination, and co-interventions when specifying the effect size for sample size calculations [56].
Prespecified Subgroup and Heterogeneity Analyses
While pragmatic trials embrace overall heterogeneity, identifying specific factors that modify treatment effects is crucial for personalized medicine applications.
A Priori Specification: Analyses of heterogeneity of treatment effects should focus on a limited number of subgroups defined by factors identified a priori based on biological plausibility, clinical evidence, or previous research [1]. This approach minimizes the risk of spurious findings from data-driven "fishing expeditions."
Clinically Relevant Subgroups: Subgroup analyses should address questions relevant to usual clinical decision-making [56]. Potential effect modifiers of interest in drug efficacy studies typically include demographic characteristics (age, sex, race/ethnicity), disease severity, comorbidities, and genetic markers [1].
Appropriate Statistical Methods: Analyses of heterogeneity should use appropriate statistical tests for interaction rather than comparing P-values across separate subgroup analyses [1]. Researchers should acknowledge the reduced power of most subgroup analyses and interpret negative findings cautiously.
The following workflow diagram illustrates the strategic approach to managing heterogeneity throughout the trial lifecycle:
Regulatory and Ethical Considerations
Ethical Framework for Heterogeneous Trials
Pragmatic trials conducted in heterogeneous populations must navigate unique ethical considerations that arise when integrating research with clinical care.
Informed Consent: Traditional informed consent processes may be adapted in pragmatic trials when they align with ethical principles and regulatory requirements. Approaches such as "integrated consent" that incorporate permission into clinical-style discussions may be appropriate when interventions involve usual care [56]. In some minimal-risk situations, cluster-randomized trials may qualify for waiver or alteration of consent [56].
Inclusion of Vulnerable Populations: Pragmatic trials should generally include vulnerable participants who would normally receive the interventions in clinical practice, provided appropriate safeguards are in place [56]. This represents a departure from explanatory trials that often exclude patients with comorbidities, limited decision-making capacity, or other vulnerabilities.
Regulatory Perspectives on Pragmatic Designs
Regulatory agencies have shown increasing interest in pragmatic trial designs as a means of generating relevant real-world evidence.
FDA Initiatives: The FDA Oncology Center of Excellence's Project Pragmatica seeks to explore the appropriate use of pragmatic design elements in trials for approved oncology medical products [42]. This initiative aims to introduce functional efficiencies and enhance patient centricity by integrating aspects of clinical trials with real-world routine clinical practice [42].
Evidentiary Standards: While pragmatic trials generate evidence relevant to clinical decision-making, researchers must consider how regulatory requirements for drug approval might influence design choices. Early engagement with regulatory agencies is essential when planning pragmatic trials intended to support labeling claims or regulatory decisions.
Protocol Implementation: The Researcher's Toolkit
Successful implementation of heterogeneity management strategies requires specific methodological tools and approaches.
Table 3: Essential Methodological Tools for Managing Heterogeneity in Pragmatic Trials
| Tool Category | Specific Methods/Techniques | Primary Application | Key Considerations |
|---|---|---|---|
| Trial Design Tools | PRECIS-2 framework, Cluster randomization, Broad eligibility criteria | Optimizing trial design for real-world applicability | Balance internal validity and generalizability |
| Recruitment & Retention Tools | EHR-based screening, Minimal follow-up burden, Patient-centered outcomes | Enhancing representativeness and reducing attrition | Minimize disruption to clinical workflow |
| Data Collection Tools | Electronic health records, Disease registries, Patient-reported outcomes | Capturing outcomes efficiently in diverse settings | Ensure data quality across sources |
| Statistical Analysis Tools | Mixed-effects models, Generalized estimating equations, Interaction tests | Accounting for multi-level data structure and effect modification | Prespecify analysis plans to avoid data dredging |
| Implementation Assessment Tools | Process evaluations, Adherence measures, Fidelity assessment | Understanding how intervention implementation varies | Distinguish implementation failure from intervention failure |
Effectively managing heterogeneity is not merely a methodological challenge in pragmatic trial design but a fundamental requirement for generating evidence that is both scientifically valid and clinically relevant. The strategies outlined in this document provide a framework for researchers to embrace and account for the inherent variability of real-world patients, settings, and clinical practices while maintaining the integrity of their findings.
By deliberately incorporating heterogeneous elements into trial design and employing appropriate analytical methods to account for this variability, researchers can produce evidence that more accurately reflects how interventions will perform in routine practice. This approach is particularly valuable in comparative drug effectiveness research, where understanding how treatment effects vary across patient subgroups and care settings is essential for optimizing therapeutic decisions.
As pragmatic trial methodologies continue to evolve, ongoing dialogue between researchers, regulators, clinicians, and patients will be essential for refining these approaches and ensuring that trial evidence effectively informs clinical practice and healthcare policy.
Subgroup analyses constitute a fundamental step in the assessment of evidence from confirmatory (Phase III) clinical trials, where conclusions for the overall study population might not hold [57]. These analyses aim to investigate whether treatment effects are homogeneous across the entire study population or whether specific patient subsets demonstrate differential responses. In an era of growing biological and pharmacological knowledge leading to more personalized medicine and targeted therapies, the proper identification and interpretation of subgroup effects is increasingly critical [57].
The challenge lies in distinguishing clinically meaningful subgroup effects from spurious findings that may arise by chance. A review of major clinical trials reveals that subgroup analyses are ubiquitous, with one analysis finding that 70% of reported trials contained subgroup analyses, and of these, 60% claimed subgroup differences [57]. The proper execution and interpretation of these analyses is paramount, as erroneous conclusions can lead to both the withholding of effective treatments from those who would benefit and the administration of treatments to those who would not [58].
Table 1: Common Purposes for Subgroup Analyses in Clinical Trials
| Purpose Number | Purpose Description | Typical Context |
|---|---|---|
| 1 | Investigate consistency of treatment effects across subgroups of clinical importance | Overall significant trial |
| 2 | Explore treatment effect across different subgroups within an overall non-significant trial | Overall non-significant trial |
| 3 | Evaluate safety profiles limited to one or a few subgroup(s) | Safety-focused assessment |
| 4 | Establish efficacy in a targeted subgroup when included in a confirmatory testing strategy | Pre-specified targeted population |
The Critical Role of Prior Evidence
Bayesian Framework for Subgroup Analysis
The interpretation of a subgroup analysis is analogous to rigorously interpreting a diagnostic test [58]. Before ordering a diagnostic test, a clinician considers the probability the person has the condition (the prior probability) and the accuracy of the test. Similarly, when evaluating subgroup analyses, we must consider the prior probability of a true subgroup effect existing based on previous evidence and biological plausibility.
Bayes's rule can be seamlessly applied to the context of subgroup analysis and informs why a shotgun approach to subgroup analysis fails [58]. The formula can be represented as: Posterior odds = [Statistical Power / (1 - Specificity)] × Prior odds
In this framework:
- Sensitivity is equivalent to the statistical power of the subgroup analysis
- Specificity is generally set at 95% based on the conventional significance threshold of P<0.05
- Prior probability reflects the strength of previous theoretical or empirical evidence
Quantifying Prior Probability
Prior probability estimates are often unsettling given their inherent uncertainty and subjectivity, but failing to grapple with this tends to bias us toward falsely accepting new evidence as truth [58]. Existing criteria to judge the credibility of subgroup analyses emphasise the importance of prior probability and specifically require that a hypothesis and its direction of effect are specified a priori and that the subgroup effect is supported by within-study empirical and biological evidence.
Empirical data can provide a rough starting point for thinking about prior probability. Of roughly 1200 subgroup analyses of recent clinical trials published in high impact journals, only 83 (7%) were reportedly positive [58]. Assuming a 5% false positive rate, only a fraction of these analyses were likely true positives. This observation is supported by the finding that less than 15% of these subgroup analyses met four of 10 criteria for credibility. Thus, a high-end starting point for the prior probability for the average published subgroup analysis is probably around 5%, which can be adjusted on a case-by-case basis based on prior empirical and theoretical evidence.
Quantitative Framework for Subgroup Analysis Decisions
Statistical Considerations and Power
Compared with the power for the trial's main effect, most subgroup analyses have much less statistical power to identify subgroup effects [58]. Power might often be closer to 20-30% for subgroup effect sizes similar in magnitude to the main treatment effect sizes. The sample size needed to adequately contrast treatment effects measured in two different subgroups is much larger than the sample needed to distinguish an overall treatment effect from the null.
Table 2: Positive Predictive Value (PPV) of Subgroup Analyses Across Different Scenarios
| Prior Probability | Power: 20%1 Comparison | Power: 20%5 Comparisons | Power: 20%10 Comparisons | Power: 50%1 Comparison | Power: 50%5 Comparisons | Power: 50%10 Comparisons | Power: 80%1 Comparison | Power: 80%5 Comparisons | Power: 80%10 Comparisons |
|---|---|---|---|---|---|---|---|---|---|
| 5% | 17% | 14% | 11% | 35% | 18% | 12% | 46% | 19% | 12% |
| 10% | 31% | 25% | 20% | 53% | 32% | 22% | 64% | 33% | 22% |
| 20% | 50% | 43% | 36% | 71% | 52% | 38% | 80% | 53% | 38% |
| 30% | 63% | 56% | 49% | 81% | 65% | 52% | 87% | 65% | 52% |
| 40% | 73% | 67% | 60% | 87% | 74% | 62% | 91% | 75% | 62% |
| 50% | 80% | 75% | 69% | 91% | 81% | 71% | 94% | 82% | 71% |
| 60% | 86% | 82% | 77% | 94% | 87% | 79% | 96% | 87% | 79% |
| 70% | 90% | 87% | 84% | 96% | 91% | 85% | 97% | 91% | 85% |
| 80% | 94% | 92% | 90% | 98% | 95% | 91% | 99% | 95% | 91% |
Note: PPV = probability that all reported positive analyses are true positives for a trial reporting at least one positive subgroup effect (that is, no false positives) for a given prior probability and power in the context of conducting one, five, or ten subgroup comparisons without adjustment for multiple comparisons, assuming α=5% (0.05). Adapted from [58].
Decision Rules for Clinical Trial Subgroups
Based on the quantitative framework, we can derive practical rules of thumb for performing primary subgroup analyses:
Rule of Thumb 1: Categorical subgroup analyses should not be part of a typical clinical trial's primary (hypothesis testing) analysis unless the prior probability for a subgroup effect being present is at least 20% and preferably higher than 50% [58]. Even under optimal circumstances, a subgroup analysis of a categorical variable will rarely have greater than 50% statistical power to detect a moderate subgroup effect, and more often is closer to 20%.
Rule of Thumb 2: Rarely should more than one to two primary categorical subgroup analyses be performed [58]. The statistical cost of multiple comparisons is substantial, as shown in Table 2, where the positive predictive value drops dramatically as the number of comparisons increases.
Rule of Thumb 3: In trials with exceptional power to identify subgroup effects, hypothesis testing analyses of subgroups should be justified a priori [58]. Pre-specification alone is insufficient; the subgroup hypothesis must be grounded in strong biological rationale or compelling previous evidence.
Protocol for Evaluating Subgroup Effects
Pre-Specification and Documentation
The following protocol provides a systematic approach for handling subgroup analyses in confirmatory clinical trials:
Step 1: Define Subgroup Hypotheses A Priori
- Clearly specify all subgroup analyses in the study protocol and statistical analysis plan
- Document the biological or clinical rationale for each subgroup hypothesis
- Pre-specify the direction of expected effect modification
- Define the statistical methods for testing subgroup interactions
Step 2: Categorize by Purpose and Priority
- Classify each planned subgroup analysis according to its primary purpose using the framework in Table 1
- Assign priority levels (primary, secondary, exploratory) based on prior probability and clinical importance
- Limit primary (hypothesis-testing) subgroup analyses to 1-2 with the strongest rationale
Step 3: Plan Statistical Analysis
- For primary subgroup analyses, pre-specify adjustment for multiple comparisons
- Use tests for interaction rather than within-subgroup tests
- Ensure adequate power calculations for primary subgroup analyses
- Plan sensitivity analyses to assess robustness of findings
Interpretation Framework
Step 4: Evaluate Credibility of Positive Findings
- Calculate positive predictive value using the Bayesian framework (Table 2)
- Assess consistency with prior evidence and biological plausibility
- Evaluate magnitude of the effect and confidence intervals
- Check for consistency across related subgroups and endpoints
Step 5: Categorize Findings for Clinical Application
- Hypothesis-Testing Findings: Positive subgroup analyses with high prior probability (>50%), adequate power, and high PPV (>80%) may influence clinical practice
- Hypothesis-Generating Findings: Positive subgroup analyses with lower prior probability or PPV require confirmation in future studies
- Consistency Assessment: Even non-significant subgroup analyses can support overall trial conclusions if effects appear consistent across subgroups
Case Study: The CAPRIE Trial Example
The CAPRIE trial illustrates the challenges in subgroup interpretation [57]. This trial aimed to show superiority of clopidogrel to aspirin in secondary prevention of cardiovascular events. The intent-to-treat analysis showed a relative risk reduction (RRR) of 8.7% in favor of clopidogrel (p = 0.043). In an additional analysis, heterogeneity was observed (p = 0.042) depending on the qualification of prior cardiovascular events: prior MI: RRR = 7.3%; prior stroke: RRR = -3.7%; symptomatic peripheral arterial disease: RRR = 23.8%.
This observed heterogeneity led two regulatory agencies to different assessments. The National Institute for Health and Care Excellence (NICE) concluded a clinical benefit for the overall population, whereas the Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG) concluded efficacy only for the most beneficial subgroup (symptomatic peripheral arterial disease) [57]. This case highlights how different stakeholders may apply different thresholds and interpretations to the same subgroup findings.
Table 3: Research Reagent Solutions for Subgroup Analysis
| Tool Category | Specific Method/Technique | Function/Purpose | Key Considerations |
|---|---|---|---|
| Statistical Software | R Programming with 'subgroup' package | Advanced statistical modeling for subgroup identification and analysis | Open-source with extensive statistical capabilities; steep learning curve |
| Statistical Software | SAS PROC GLIMMIX | Generalized linear mixed models for complex subgroup analyses | Industry standard for clinical trials; requires commercial license |
| Statistical Software | Python (Pandas, NumPy, SciPy) | Custom subgroup analysis implementation and simulation | Flexible for developing novel methods; requires programming expertise |
| Bayesian Analysis | Stan or BUGS for Bayesian hierarchical models | Incorporation of prior evidence through formal Bayesian methods | Allows explicit quantification of prior probability; computationally intensive |
| Multiple Testing Adjustment | Bonferroni, Holm, Hochberg procedures | Control of false discovery rate in multiple subgroup analyses | Different balance between type I error control and power |
| Subgroup Identification | SIDES, Virtual Twins methods | Algorithmic subgroup identification in high-dimensional data | Data-driven approach; high risk of false discovery without validation |
| Interaction Analysis | Generalized additive models (GAMs) | Detection of non-linear interaction effects | Flexible modeling; requires careful interpretation |
Advanced Methodological Approaches
Quantitative Framework for Decision Making
The following workflow provides a structured approach for implementing the Bayesian quantitative framework described in Section 3:
Handling Clinical Heterogeneity in Comparative Effectiveness Research
Clinical heterogeneity refers to the variation in study population characteristics, coexisting conditions, cointerventions, and outcomes evaluated across studies that may influence or modify the magnitude of the intervention effect [24]. In systematic reviews and comparative effectiveness research, this heterogeneity presents both a challenge and an opportunity—while it complicates pooling of results, it can also inform which patients will benefit most from an intervention, who will benefit least, and who is at greatest risk of harms [24].
Methodological approaches to address clinical heterogeneity include:
- Subgroup analyses to isolate factors implicated in heterogeneity
- Meta-regression techniques applied to summary data or individual patient data
- Restriction of the range of patient characteristics examined
- Formal interaction tests within primary studies
Each approach requires careful consideration of the interplay between clinical heterogeneity (variation in patient characteristics), methodological heterogeneity (variation in study design), and statistical heterogeneity (variability in observed treatment effects beyond what would be expected by chance) [24].
Subgroup analyses remain essential for understanding heterogeneous treatment effects in clinical trials, but require disciplined approach to avoid spurious conclusions. The framework presented here emphasizes that prior evidence should be the primary guide for determining which subgroup analyses should be considered hypothesis-testing versus hypothesis-generating.
For successful implementation:
- Prioritize biologically plausible subgroups with strong prior evidence over data-driven subgroup searches
- Limit primary subgroup analyses to 1-2 pre-specified hypotheses with prior probability >20%
- Apply quantitative Bayesian framework to calculate positive predictive value of significant findings
- Interpret subgroup findings conservatively when prior probability is low or multiple comparisons are performed
- Require independent confirmation for subgroup findings that are hypothesis-generating rather than hypothesis-testing
By adopting this evidence-based approach to subgroup analysis, researchers, clinicians, and regulatory bodies can make more informed decisions about when subgroup findings should influence clinical practice and when they require further validation.
Assessing Credibility and Clinical Importance of Heterogeneity Findings
Effect modification, also referred to as "subgroup effect," "statistical interaction," or "moderation," occurs when the effect of an intervention varies between individuals based on specific attributes such as age, sex, or disease severity [59]. In systematic reviews, this may manifest as variation between studies based on their setting, year of publication, or methodological differences, often called a "subgroup analysis" [59]. Understanding effect modification is fundamental to personalized medicine, which aims to optimize how treatments are used for specific patient subgroups [60].
The assessment of effect modification presents significant methodological challenges. As many as one-quarter of randomized controlled trials (RCTs) and meta-analyses examine their findings for potential evidence of effect modification [59]. However, claims of effect modification are frequently proved spurious, potentially negatively affecting the quality of care in those patient subgroups [59]. These unreliable claims may stem from random chance, selective reporting, or misguided application of statistical analyses [59]. The Instrument to assess the Credibility of Effect Modification in Analyses (ICEMAN) was developed specifically to address these challenges through a standardized, rigorous approach to evaluating the credibility of effect modification analyses [59].
Development and Validation of the ICEMAN Tool
Systematic Development Process
ICEMAN was developed through a methodologically rigorous process that addressed limitations of previous assessment criteria. Schandelmaier and colleagues conducted a systematic survey of the literature, identifying thirty existing sets of criteria for evaluating effect modification, none of which adequately reflected their conceptual framework [59]. This comprehensive review informed the initial selection of 36 candidate criteria [59].
An expert panel of 15 members was randomly identified from a list of 40 experts found through the systematic survey [59]. This panel refined the initial item pool, paring it down to 20 required and 8 optional items through a structured process [59]. Following this development phase, the creators tested the instrument among a diverse group of 17 potential users, including authors of Cochrane reviews, RCT authors, and journal editors, using semi-structured interview techniques to ensure practicality and usability [59].
Core Components and Structure
ICEMAN provides a structured framework for evaluating effect modification analyses across key methodological domains. The tool organizes assessment into required and optional items that address fundamental aspects of analysis credibility, including pre-specification of hypotheses, statistical power, adjustment for multiple comparisons, and biological plausibility [59]. This structured approach helps users systematically evaluate potential effect modifications while minimizing the risk of spurious findings.
Table: ICEMAN Tool Development Process
| Development Phase | Key Activities | Outputs |
|---|---|---|
| Literature Review | Systematic survey of existing criteria | 30 sets of criteria identified; 36 candidate items generated |
| Expert Panel Review | 15 experts randomly selected from 40 identified experts | Refined item set to 20 required and 8 optional items |
| User Testing | Semi-structured interviews with 17 potential users | Final instrument with manual for use |
Methodological Framework for Effect Modification Analysis
Distinguishing Types of Effect Modification
Effect modification analyses can be categorized based on the nature of the relationship between the modifier variable and treatment effect. Linear effect modification (LEM) occurs when the treatment effect changes consistently across levels of a continuous modifier variable [60]. Nonlinear effect modification (NLEM) describes situations where the relationship between the modifier and treatment effect follows a more complex, non-linear pattern [60]. Understanding this distinction is crucial for selecting appropriate analytical approaches.
The terminology surrounding effect modification varies in the literature, with several related but distinct terms often used [60]. "Interaction" refers to the situation where the combined effect of two factors differs from their individual effects, typically represented by a multiplicative term in statistical models [60]. "Effect modification" specifically describes the interaction between a binary intervention indicator and a covariate (the effect modifier), where the intervention effect differs according to the level of the modifier characteristic [60]. "Subgroup effect" refers to the intervention effect within patient subsets defined by categorical characteristics [60].
Analytical Considerations for Credible Effect Modification Assessment
Several methodological considerations are essential for conducting credible effect modification analyses. Power and sample size requirements for detecting effect modification are substantially larger than for overall treatment effects [60]. For example, when compared with the sample size required for detecting an average treatment effect, a sample size approximately four times as large is needed to detect a difference in subgroup effects of the same magnitude for a 50:50 subgroup split [61]. This has important implications for study planning and interpretation.
The risk of multiple testing presents another critical challenge. When performing separate interaction tests for multiple subgroup variables, the probability of falsely detecting a difference in subgroup effects increases substantially [61]. For instance, with 100 subgroup variables tested at a significance level of 0.05, approximately five would be statistically significant by chance alone even if no true effect modification exists [61]. Statistical adjustments for multiple comparisons, while necessary to control Type I error, further increase the risk of Type II errors [61].
In individual participant data meta-analyses (IPDMA), the distinction between within-trial and across-trial information is crucial to avoid aggregation bias [60]. This occurs when a between-trial relationship (e.g., trials with more women show larger effects) is misinterpreted as a within-trial relationship (women respond better than men) [60]. Analytical approaches must separate these sources of information to ensure valid participant-level inferences [60].
Diagram: Effect Modification Analysis Workflow. This diagram outlines the key methodological steps for conducting credible effect modification analyses, highlighting critical considerations such as aggregation bias and multiple testing adjustments.
Practical Application of ICEMAN in Comparative Drug Efficacy Studies
ICEMAN Assessment Protocol
The application of ICEMAN follows a structured protocol to ensure consistent and comprehensive evaluation of effect modification analyses. Users should begin by familiarizing themselves with the tool's manual and scoring system, which provides detailed guidance on interpreting each item [59]. The assessment proceeds through evaluation of each required and optional item, with documentation of supporting evidence and rationale for each rating.
When applying ICEMAN to comparative drug efficacy studies, specific considerations include evaluation of biological plausibility for proposed effect modifiers, assessment of pre-specification in study protocols, and examination of statistical approaches for handling continuous variables and multiple comparisons [59]. The tool helps distinguish between credible effect modifications that should inform clinical decision-making and potentially spurious findings that require further validation.
Integration with Heterogeneity Assessment in Comparative Effectiveness Research
ICEMAN should be integrated within a broader framework for assessing heterogeneity of treatment effects (HTE) in comparative effectiveness research. HTE is defined as "nonrandom, explainable variability in the direction and magnitude of treatment effects for individuals within a population" [61]. The main goals of HTE analysis are to estimate treatment effects in clinically relevant subgroups and to predict whether an individual might benefit from a treatment [61].
Table: Key Considerations for Heterogeneity of Treatment Effects Analysis
| Consideration | Description | Implication for Analysis |
|---|---|---|
| Study Power | HTE analyses require larger sample sizes than ATE | Plan for 4x larger sample for equivalent detection power [61] |
| Multiple Testing | Increased false discovery risk with multiple subgroups | Implement appropriate statistical corrections [61] |
| Scale Dependence | Effect modification may vary by outcome scale | Consider different measurement scales in analysis [60] |
| Biological Plausibility | Mechanistic rationale for effect modification | Evaluate proposed biological pathways [59] |
| Clinical Relevance | Magnitude of difference across subgroups | Assess whether differences would change clinical decisions [61] |
Subgroup analysis represents the most common analytic approach for examining HTE, typically evaluating treatment effects for subgroups defined by baseline variables one variable at a time [61]. A test for interaction is conducted to evaluate whether a subgroup variable has a statistically significant interaction with the treatment indicator [61]. When significant interaction exists, treatment effects are estimated separately at each level of the categorical variable defining mutually exclusive subgroups [61].
Research Reagent Solutions for Effect Modification Analysis
Table: Essential Methodological Tools for Effect Modification Analysis
| Research Reagent | Function | Application Context |
|---|---|---|
| ICEMAN Tool | Standardized credibility assessment of effect modification | Evaluation of subgroup analyses in RCTs and meta-analyses [59] |
| One-Stage IPDMA Models | Analyze all trial data jointly while accounting for clustering | Participant-level effect modification analysis with trial stratification [60] |
| Two-Stage IPDMA Models | Analyze trials separately then combine estimates | Participant-level effect modification with less model complexity [60] |
| Interaction Tests | Statistical assessment of effect modification | Determining whether subgroup differences are statistically significant [61] |
| Fractional Polynomials | Modeling nonlinear relationships | Analysis of nonlinear effect modification without categorization [60] |
| Restricted Cubic Splines | Flexible modeling of complex relationships | Assessment of nonlinear effect modification with continuous variables [60] |
Diagram: Analytical Framework for Effect Modification. This diagram illustrates the relationship between core methodological approaches for effect modification analysis, including IPDMA methods and nonlinear modeling techniques.
Implementation in Drug Development and Regulatory Contexts
The application of ICEMAN and rigorous effect modification analysis has significant implications for drug development and regulatory decision-making. In personalized medicine, understanding how treatment effects vary across patient subgroups is essential for optimizing therapy for individual patients [60]. Drug development programs can incorporate ICEMAN assessments to enhance the credibility of subgroup claims in labeling and to inform targeted therapy approaches.
Regulatory evaluations of comparative drug efficacy can benefit from standardized assessment of effect modification credibility when considering subgroup-specific recommendations or restrictions. The structured nature of ICEMAN provides a transparent framework for evaluating the strength of evidence supporting differential treatment effects across patient characteristics. This is particularly important when subgroup findings might influence prescribing decisions or resource allocation.
When implementing ICEMAN in regulatory contexts, several factors warrant consideration. The timing of subgroup hypotheses (pre-specified vs. post-hoc) significantly influences credibility assessments [59]. Statistical power for subgroup analyses must be adequate to detect clinically meaningful differences, which often requires larger sample sizes than main effect analyses [61]. Biological plausibility and consistency with existing evidence strengthen the case for credible effect modification [59]. These factors collectively inform the overall assessment of whether subgroup findings should influence clinical practice or require further validation.
Comparative Credibility of Risk Modeling vs. Effect Modeling Approaches
In comparative drug efficacy studies, a fundamental challenge lies in moving beyond the average treatment effect to understand how treatment outcomes vary across individual patients. This variation, known as Heterogeneity of Treatment Effects (HTE, is a critical concern for researchers, clinicians, and drug development professionals aiming to deliver personalized, effective therapies [35]. Predictive modeling approaches that account for HTE enable the identification of patient subgroups most likely to benefit from a specific treatment, thereby optimizing therapeutic decision-making and advancing precision medicine.
Two principal statistical paradigms have emerged for investigating HTE: risk modeling and effect modeling [35]. The risk modeling approach develops a multivariable model predicting an individual's baseline risk of the study outcome without using treatment assignment information, then examines treatment effects across different risk strata. In contrast, the effect modeling approach directly estimates individual treatment effects by incorporating treatment-covariate interactions into a single model [62] [35]. Understanding the comparative credibility, applications, and limitations of these approaches is essential for robust drug development and clinical application.
Comparative Analysis of Modeling Approaches
Fundamental Definitions and Conceptual Frameworks
Risk Modeling (also referred to as "outcome risk modeling") is performed by developing a model that predicts a patient's baseline risk of the study outcome using multiple patient characteristics, without initially considering treatment assignment—essentially "blinded" to treatment [62] [63]. This model is typically developed using data from the control arm only or from the entire study population while ignoring treatment assignment. Once developed, researchers examine both absolute and relative treatment effects across pre-specified strata (e.g., quartiles) of predicted risk [35]. This approach capitalizes on the mathematical relationship known as "risk magnification," where absolute treatment benefit typically increases with baseline risk, even when relative treatment effects remain constant across risk strata [35].
Effect Modeling (or "treatment effect modeling") represents a more direct approach to estimating HTE. This method develops a model within the randomized clinical trial (RCT) data to directly estimate individual treatment effects by including treatment assignment, multiple covariates, and interactions between treatment and one or more covariates [35]. Effect modeling can be implemented using traditional regression methods or more flexible, data-driven machine-learning algorithms. The primary objective is to create a model that can directly predict which treatment will be better for a particular individual based on their specific characteristics [62].
Table 1: Conceptual Comparison of Risk Modeling and Effect Modeling Approaches
| Aspect | Risk Modeling | Effect Modeling |
|---|---|---|
| Primary Objective | Examine treatment effects across risk strata | Directly predict individual treatment effects |
| Model Structure | Develops risk prediction model first, then assesses treatment effects across risk strata | Single model with treatment-covariate interactions |
| Treatment Assignment in Model Development | Initially ignored ("blinded" approach) | Central component with interaction terms |
| Theoretical Basis | Risk magnification principle | Direct effect modification |
| Scale of HTE Assessment | Primarily absolute effects (risk differences) | Both absolute and relative effects |
Empirical Evidence on Comparative Performance
Recent empirical research provides critical insights into the relative performance and credibility of these two approaches. A comprehensive scoping review published in 2024 that assessed the impact of the PATH Statement (Predictive Approaches to Treatment Heterogeneity) examined 65 reports presenting 31 risk models and 41 effect models [35]. This review applied adapted ICEMAN (Instrument to assess Credibility of Effect Modification Analyses) criteria to evaluate the credibility of claimed HTE findings.
The findings revealed striking differences: risk modeling met credibility criteria more frequently (87%) compared to effect modeling (32%) [35]. For effect models, external validation proved critical in establishing credibility. In studies where overall treatment benefit was demonstrated, modeling approaches identified patient subgroups comprising 5-67% of the population that were predicted to experience no benefit or net treatment harm. Conversely, in trials showing no overall benefit, subgroups of 25-60% of patients were nevertheless predicted to benefit from treatment [35].
Simulation studies further illuminate the performance characteristics of these approaches. Research by van Klaveren et al. demonstrated that the risk modeling approach was well-calibrated for benefit, meaning that predicted benefits aligned well with observed benefits [62] [63]. In contrast, effect models were consistently overfit, significantly overestimating (and sometimes underestimating) treatment benefit for substantial proportions of patients, even with doubled sample sizes [62] [63]. This overfitting problem persisted across different analytical conditions but was substantially reduced through the application of penalized regression techniques such as Lasso and Ridge regression [62].
Table 2: Empirical Performance Comparison Based on Simulation Studies and Scoping Review
| Performance Metric | Risk Modeling | Effect Modeling | Notes |
|---|---|---|---|
| Calibration for Benefit | Well-calibrated [62] [63] | Consistently overfit [62] [63] | Overfitting reduced with penalized regression |
| Frequency of Credible Findings | 87% of reports [35] | 32% of reports [35] | Based on adapted ICEMAN criteria |
| Discrimination for Benefit | Superior in absence of true interactions [62] | Superior in presence of true interactions [62] | With penalized regression |
| Vulnerability to Overfitting | Low | High | |
| Dependence on External Validation | Moderate | Critical for credibility [35] |
Experimental Protocols and Methodologies
Risk Modeling Protocol
Protocol 1: Development and Validation of Risk Models for HTE Assessment
Objective: To develop a multivariable risk prediction model and assess heterogeneity of treatment effects across predicted risk strata.
Step 1 - Model Development:
- Select candidate predictors based on clinical relevance and established relationship with the outcome
- Develop a multivariable model predicting the probability of the study outcome using data from:
- The control arm only, OR
- The entire study population, blinded to treatment assignment
- Use appropriate regression techniques (logistic regression for binary outcomes, Cox proportional hazards for time-to-event outcomes)
- Document all model specifications and variable transformations
Step 2 - Risk Stratification:
- Calculate predicted risk for each participant in the study
- Stratify the population into risk groups (typically quartiles or quintiles) based on the predicted risk
- Ensure sufficient sample size within each stratum for precise effect estimation
Step 3 - Treatment Effect Estimation:
- Within each risk stratum, calculate both absolute and relative treatment effects
- For absolute effects: compute risk differences between treatment and control groups
- For relative effects: compute odds ratios, hazard ratios, or risk ratios as appropriate
- Present effect estimates with appropriate confidence intervals
Step 4 - Validation:
- Internally validate the risk model using bootstrapping or cross-validation
- When possible, externally validate using independent datasets
- Assess calibration and discrimination of the risk model
- Evaluate consistency of risk-based HTE patterns across validation samples
Effect Modeling Protocol
Protocol 2: Development and Validation of Effect Models for HTE Assessment
Objective: To develop a model that directly estimates individual-level treatment effects by incorporating treatment-covariate interactions.
Step 1 - Pre-specification:
- Limit the number of treatment-covariate interactions based on prior evidence or strong biological rationale
- Pre-specify the analytical approach, including model structure and validation plans
- Consider using penalized regression methods to mitigate overfitting
Step 2 - Model Development:
- Develop a model that includes:
- Main effects for baseline covariates
- Treatment assignment indicator
- Pre-specified treatment-covariate interactions
- Consider using machine learning methods specifically designed for causal inference (e.g., causal forests) when appropriate
- Apply penalization methods (Lasso, Ridge) when multiple interactions are explored
Step 3 - Individual Treatment Effect Estimation:
- Generate predictions for each participant under both treatment and control conditions
- Calculate the difference in predicted outcomes to estimate individual treatment effects
- Group individuals based on predicted treatment benefit for subgroup identification
Step 4 - Validation:
- Conduct external validation in independent datasets when possible
- Use internal validation methods (bootstrapping, cross-validation) with appropriate performance measures
- Assess calibration-for-benefit by comparing predicted and observed treatment effects across subgroups
- Evaluate discrimination-for-benefit using appropriate metrics (e.g., C-for-benefit)
Critical Considerations:
- Effect modeling should only be undertaken when there are a small number of previously established effect modifiers [35]
- Without external validation, effect modeling findings should be considered exploratory [35]
- Interpretation should be cautious, regardless of statistical significance of interaction terms
Implementation Guidance and Risk Mitigation
Framework for Credibility Assessment
Establishing model credibility requires a structured approach, particularly when models inform regulatory decisions or clinical practice. The risk-informed credibility assessment framework proposed for model-informed drug development (MIDD) offers a valuable structure for evaluating both risk and effect models [64]. This framework emphasizes several key concepts:
First, clearly define the question of interest and context of use (COU). The COU should explicitly state how the model will address the specific question, including the role of additional data sources [64]. Second, assess model risk based on both the model's influence on decision-making and the consequences of an incorrect decision [64]. Third, establish model credibility through verification and validation activities commensurate with the model risk [64].
For HTE models specifically, credibility assessment should include evaluation of:
- The strength of prior evidence for proposed effect modifiers
- The number of interactions tested relative to sample size
- The approach to handling continuous variables (avoiding data-driven cutpoints)
- The statistical evidence for interaction
- The results of external validation [35]
Recommended Applications and Decision Framework
Based on current evidence, risk modeling is recommended as the default approach for initial HTE assessment in most circumstances, particularly when no specific effect modifiers have been strongly established a priori [62] [35]. Risk modeling provides well-calibrated estimates of absolute treatment benefit across risk strata and directly informs treatment decisions based on absolute benefit considerations.
Effect modeling may be considered when:
- There are strong prior biological or clinical rationale for specific treatment-effect modifications
- The number of candidate effect modifiers is small relative to the sample size
- Penalized regression or other methods to reduce overfitting are implemented
- External validation is possible [62] [35]
Even when effect modeling is employed, it should ideally be accompanied by a risk modeling approach to provide complementary perspectives on HTE [35].
Table 3: Key Analytical Tools and Methods for HTE Assessment
| Tool/Method | Function | Implementation Considerations |
|---|---|---|
| Multivariable Regression | Baseline risk prediction; Effect modeling with interactions | Use standard packages (R, Python, SAS); Pre-specify model structure |
| Penalized Regression (Lasso, Ridge) | Reduces overfitting in effect models | Particularly valuable when exploring multiple interactions; Requires careful hyperparameter tuning |
| Machine Learning Causal Methods | Flexible estimation of heterogeneous effects | Methods include causal forests, BART; Require careful validation; May lack transparency |
| Bootstrapping | Internal validation of model performance | Provides confidence intervals for performance metrics; Assesses internal stability |
| External Validation Cohorts | Tests transportability of HTE findings | Critical for establishing credibility of effect models; Use independent RCTs or high-quality observational data |
| Calibration-for-Benefit Plots | Assess accuracy of predicted treatment benefits | Compare predicted vs. observed treatment effects across risk or benefit strata |
The comparative assessment of risk modeling versus effect modeling approaches reveals a consistent pattern: risk modeling provides more reliable and credible estimates of heterogeneous treatment effects in most circumstances, particularly when strong prior evidence for specific effect modifiers is lacking. The empirical evidence demonstrates that risk modeling approaches are consistently well-calibrated and meet credibility criteria more frequently than effect modeling approaches.
Effect modeling, while theoretically powerful for identifying more complex patterns of treatment effect heterogeneity, is prone to serious overfitting and requires stringent methodological safeguards. When employed, effect modeling should incorporate penalized regression methods, include only plausible interactions with strong prior justification, and undergo rigorous external validation to establish credibility.
For researchers and drug development professionals, these findings suggest a conservative pathway for HTE investigation: begin with risk modeling as a foundational approach, and resort to effect modeling only when specific conditions are met. This prudent approach will generate more reliable evidence for personalized treatment decisions, ultimately advancing the goals of precision medicine while avoiding the pitfalls of overinterpreted subgroup findings.
Application Notes
Theoretical Foundation: Risk Difference as a Decision-Making Metric
The risk difference (RD), calculated as the cumulative incidence in the treated group minus the cumulative incidence in the comparator group, provides the absolute measure of treatment effect most directly informative for clinical decision-making [8]. Unlike relative measures such as the risk ratio (RR), the RD quantifies the absolute number of patients who benefit or are harmed from treatment, enabling more nuanced benefit-harm trade-off assessments [8]. Heterogeneity of Treatment Effect (HTE) exists when a treatment effect changes across levels of a patient characteristic, known as an effect modifier [8]. Understanding when variation in the RD becomes clinically important is fundamental to personalizing treatment strategies and improving patient outcomes.
The clinical importance of HTE is profoundly influenced by a patient's baseline risk for the outcome of interest and their competing risks (the risk of events that compete with the outcome of interest) [65]. This is because the same relative risk reduction produces vastly different absolute benefits depending on a patient's underlying outcome risk. Furthermore, in patients with high competing risks, the opportunity to experience the target outcome is diminished, which can attenuate or even reverse the net benefit of treatment [65]. Consequently, a variation in RD that is trivial for a low-risk patient may be decisively important for a high-risk patient.
Quantitative Scenarios: When Variation in RD Alters Decisions
The following table illustrates how competing risk and baseline outcome risk interact to change the net benefit of a treatment, thereby altering clinical decisions. The scenario models adjuvant chemotherapy for breast cancer, assuming a constant 15% relative risk reduction for breast cancer death and a fixed absolute rate of serious treatment-related harm of 1.5% (15 events per 1000) [65].
Table 1: Impact of Competing Risk on Net Treatment Benefit (10-Year Horizon)
| Risk of Breast Cancer Death (No Treatment) | No Treatment Harm or Competing Risk | Treatment Harm (1.5%) but No Competing Risk | Treatment Harm & Low Competing Risk (10%) | Treatment Harm & Moderate Competing Risk (25%) | Treatment Harm & High Competing Risk (50%) |
|---|---|---|---|---|---|
| Low (10%) | RD: 0.015, NNT: 67 | RD: 0, NNT: ∞ | RD: -0.002, NNH: 667 | RD: -0.004, NNH: 267 | RD: -0.007, NNH: 133 |
| Moderate (25%) | RD: 0.038, NNT: 27 | RD: 0.023, NNT: 44 | RD: 0.019, NNT: 53 | RD: 0.013, NNT: 76 | RD: 0.004, NNT: 267 |
| High (50%) | RD: 0.075, NNT: 13 | RD: 0.060, NNT: 17 | RD: 0.053, NNT: 19 | RD: 0.041, NNT: 24 | RD: 0.022, NNT: 44 |
Abbreviations: RD, Risk Difference; NNT, Number Needed to Treat; NNH, Number Needed to Harm. A negative RD indicates net harm.
Decision Implications:
- For a patient with low baseline risk, even modest competing risk can nullify a small absolute benefit and lead to net harm, arguing against treatment.
- For a patient with moderate baseline risk, the presence of high competing risk drastically reduces the net benefit (NNT increases from 44 to 267), which may shift the decision depending on patient preferences.
- For a patient with high baseline risk, a substantial net benefit persists even with high competing risk, strongly supporting treatment.
Experimental Protocols
A Standardized Framework for Risk-Based HTE Assessment
This protocol provides a detailed methodology for assessing when variation in RD becomes clinically important using observational healthcare data, extending the PATH statement principles to the real-world evidence context [36].
Figure 1: Workflow for Risk-Based HTE Assessment
Protocol Steps
Step 1: Definition of the Research Aim
- Population: Define the target patient population (e.g., patients with established hypertension).
- Intervention & Comparator: Specify the treatment and active comparator (e.g., thiazide diuretics vs. ACE inhibitors).
- Outcomes: Pre-specify efficacy and safety outcomes (e.g., acute myocardial infarction, stroke, hospitalization for heart failure, specific adverse events) [36].
Step 2: Identification of Databases
- Identify and select observational healthcare databases mapped to a common data model, such as the OMOP-CDM, to ensure standardized analytics [36].
- Ensure databases contain sufficient numbers of patients initiating the treatments of interest and experiencing the outcomes.
Step 3: Prediction of Outcome Risk
- Objective: Develop a model to predict an individual's baseline risk for the primary outcome.
- Method:
- Use a large set of predefined candidate predictors from the year prior to treatment initiation (demographics, diagnoses, medications, procedures) [36].
- On a propensity score-matched subset of the study population, train a prediction model (e.g., using LASSO logistic regression with cross-validation) for the outcome over a defined time horizon (e.g., 2-year risk of acute MI) [36].
- Validate the model's discriminative performance internally (e.g., using cross-validation or bootstrap validation).
Step 4: Estimation of Treatment Effects within Risk Strata
- Stratification: Stratify the entire study population into groups based on percentiles of their predicted baseline risk (e.g., quarters or clinically relevant thresholds like <1%, 1-1.5%, >1.5%) [36].
- Confounding Adjustment within Strata: Within each risk stratum, account for residual confounding using propensity score (PS) methods.
- Develop a PS model within each risk stratum separately, using LASSO logistic regression to predict treatment assignment based on all available pre-treatment covariates.
- Stratify patients into quintiles based on the PS.
- Within each PS stratum, fit a Cox regression model to estimate the hazard ratio (HR).
- Pool the HR estimates across PS strata within each risk group using a meta-analytic approach [36].
- Absolute Effect Estimation: Similarly, within each PS stratum, calculate the absolute risk difference using Kaplan-Meier estimates at a specific time point (e.g., 2 years). Pool these differences across PS strata within each risk group [36].
Step 5: Presentation of the Results
- Present both relative (e.g., HR) and absolute (RD, NNT) treatment effects for each risk stratum.
- Visualize the results to show the relationship between baseline risk and absolute treatment benefit, facilitating the identification of patient subgroups for whom the benefit-harm profile is favorable or unfavorable.
Protocol for Evaluating Competing Risk in HTE Analysis
This protocol supplements the core HTE framework by formally incorporating competing risks.
Figure 2: Competing Risks Conceptual Model
Protocol Steps
- Define the Competing Event: Clearly define an event whose occurrence precludes the occurrence of the primary outcome of interest or fundamentally alters the probability of experiencing it (e.g., non-cardiovascular death as a competing risk for cardiovascular death) [65].
- Stratify by Outcome Risk and Competing Risk:
- Develop a prediction model for the competing event, similar to the outcome risk model.
- Cross-classify patients into a matrix of outcome risk (e.g., low, medium, high) and competing risk (e.g., low, medium, high).
- Estimate Net Benefit: Within each cell of this matrix, estimate the absolute risk difference for the primary efficacy outcome. Subtract the absolute risk of treatment-related harm to calculate the net absolute benefit.
- Decision Matrix: Construct a decision matrix (as in Table 1) to identify scenarios (combinations of outcome and competing risk) where the net RD shifts from positive (favoring treatment) to neutral or negative (arguing against treatment).
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Analytical Tools for HTE Research
| Item | Type | Function/Benefit |
|---|---|---|
| OMOP Common Data Model (CDM) | Data Infrastructure | Standardizes data from disparate observational sources (e.g., claims, EHRs) into a common format, enabling scalable, reproducible analytics across a network [36]. |
| LASSO Logistic Regression | Analytical Software/Algorithm | Used for developing both outcome risk and propensity score models. It performs variable selection and regularization to enhance model parsimony and prevent overfitting, which is crucial with the high-dimensional data common in RWD [36]. |
R Package RiskStratifiedEstimation |
Software Tool | An open-source R package designed to implement the standardized framework for risk-based treatment effect estimation described in Protocol 2.1, promoting methodology consistency [36]. |
| Cox Proportional Hazards Model | Statistical Model | The core model for estimating hazard ratios for time-to-event outcomes within propensity score strata during treatment effect estimation [36]. |
| Color Contrast Analyzer | Accessibility Tool | A browser extension or tool (e.g., ColorZilla) used to verify that all visualizations, such as diagrams and graphs, meet WCAG 2.2 Level AA contrast requirements (≥4.5:1 for standard text), ensuring accessibility for all researchers [66] [67]. |
The Critical Role of External Validation for Confirmatory HTE Evidence
In comparative drug efficacy research, the average treatment effect (ATE) often obscures critical variability in how different patient subgroups respond to therapies. Heterogeneity of Treatment Effects (HTE) represents the nonrandom, explainable variability in the direction or magnitude of treatment effects for individuals within a population [61]. While exploratory HTE analyses can generate hypotheses, confirmatory HTE analysis serves the distinct purpose of rigorously testing prespecified hypotheses about subgroup effects, particularly when signals of potential effect modification arise from prior trials or post-marketing surveillance [68].
The external validation of HTE findings represents a crucial step in establishing robust evidence for personalized medicine. It involves testing prespecified subgroup hypotheses in independent real-world data (RWD) sources or through replication studies across diverse populations. This process is especially vital when extending findings from randomized controlled trials (RCTs) to broader real-world populations that include patients typically underrepresented in clinical trials, such as those with multiple comorbidities, elderly patients, or ethnic minority groups [68].
Table 1: Key Definitions in Confirmatory HTE Analysis
| Term | Definition | Context in Confirmatory Analysis |
|---|---|---|
| HTE (Heterogeneity of Treatment Effects) | Nonrandom variability in the direction or magnitude of treatment effects for individuals within a population [61]. | The fundamental phenomenon being validated. |
| Effect Modification | Situation where the magnitude of treatment effect differs across levels of a patient characteristic [61]. | The specific relationship being confirmed. |
| External Validation | Testing prespecified subgroup hypotheses in independent datasets or real-world populations. | Core process of confirmatory HTE analysis. |
| Real-World Data (RWD) | Data generated from routine patient care outside the context of traditional clinical trials [68]. | Primary source for external validation. |
| Subgroup Analysis | Analytical approach evaluating treatment effects within subsets of patients defined by baseline characteristics [61]. | Primary methodological framework. |
Methodological Framework for External Validation of HTE
Prerequisites for Valid Confirmatory HTE Analysis
Before embarking on external validation of HTE, several foundational requirements must be met to ensure the validity and interpretability of findings. The scientific rationale for expecting effect modification should be strong, grounded in biological plausibility, clinical evidence, or prior research signals [68]. The subgroups of interest must be precisely prespecified in the study protocol, including clear definitions of the effect modifiers and their measurement [68]. The analysis plan should detail the statistical methods for testing interactions and estimating subgroup-specific effects, including approaches for addressing multiple testing [68]. Finally, the target population in the RWD source must contain sufficient representation of the subgroups of interest to enable adequately powered analyses [68].
A key consideration in confirmatory HTE analysis is the choice of effect scale for evaluation and reporting. HTE can be assessed on relative (ratio) or absolute (difference) scales, each with distinct implications for interpretation. Absolute measures of effect are generally more interpretable for clinical decision-making because they describe the subgroup treatment effect directly, while interpretation of relative measures requires knowledge of the baseline risk for the outcome without treatment [68]. Some methodologies recommend reporting both multiplicative (relative) and additive (absolute) interactions to provide a comprehensive picture of HTE patterns [68].
Analytical Approaches for HTE Validation in Real-World Data
When using RWD for confirmatory HTE analysis, special methodological considerations apply. The propensity score methods commonly used to address confounding in observational studies must be implemented within each prespecified subgroup rather than in the overall population to properly control for confounding within subgroups [68]. The statistical power for detecting HTE is substantially lower than for detecting overall treatment effects, requiring larger sample sizes—approximately four times as large to detect a difference in subgroup effects of the same magnitude as the ATE for a 50:50 subgroup split [61].
Interaction tests should be properly specified to evaluate whether subgroup variables have statistically significant interactions with the treatment indicator, with appropriate control for multiple testing when numerous subgroup hypotheses are examined [61]. The transportability of trial-based HTE findings to real-world populations should be formally assessed, potentially through methods that reweight subgroup effects according to prevalence across different populations [68].
Figure 1: A structured protocol for the external validation of HTE evidence, highlighting key methodological steps and essential prespecification requirements.
Experimental Protocols for Confirmatory HTE Analysis
Protocol 1: Validation of Prespecified Subgroup Effects in RWD
This protocol provides a structured approach for testing prespecified subgroup hypotheses using real-world data sources, with application to confirming suspected safety signals in specific patient subgroups.
Background and Rationale: Regulatory agencies often require postmarketing research to investigate potential treatment risks in subpopulations not detected during premarket studies [68]. This protocol addresses the need for rigorous confirmation of these signals in real-world clinical settings.
Materials and Reagents:
Table 2: Research Reagent Solutions for HTE Validation Studies
| Item | Specification | Function in Protocol |
|---|---|---|
| RWD Source | Claims data, electronic health records, or disease registries with sufficient sample size. | Provides real-world clinical context for validating subgroup effects. |
| Data Quality Framework | Standardized quality assessment tools for RWD (completeness, accuracy, provenance). | Ensures reliability of data used for HTE confirmation. |
| Propensity Score Algorithms | Software for propensity score estimation, matching, or inverse probability weighting. | Addresses confounding by indication within subgroups. |
| Interaction Test Methods | Statistical packages for testing treatment-by-covariate interactions. | Determines statistical significance of HTE. |
| Multiple Testing Correction | Bonferroni, Holm, or False Discovery Rate adjustment procedures. | Controls Type I error inflation from multiple subgroup tests. |
Procedure:
- Subgroup Definition: Define subgroups based on strong biological rationale and prior evidence. Specify all subgroup hypotheses and their directionality in the study protocol before analysis [68].
- RWD Source Evaluation: Identify appropriate RWD sources that contain adequate representation of the subgroups of interest, sufficient sample size for powered analyses, and complete data on key confounders [68].
- Cohort Construction: Apply consistent eligibility criteria to define the study population, index date ("time zero"), exposure and comparator groups, and outcome ascertainment periods [68].
- Confounding Control: Estimate propensity scores within each prespecified subgroup (not the overall population) to address confounding. Use matching, stratification, or inverse probability weighting within subgroups to achieve balance on measured covariates [68].
- Effect Modification Assessment: Test for treatment-by-subgroup interactions using appropriate statistical models. Report both relative and absolute effect measures to provide clinically interpretable results [68].
- Multiple Testing Adjustment: Apply appropriate statistical corrections (e.g., Bonferroni) to control the family-wise Type I error rate when testing multiple subgroup hypotheses [61].
- Sensitivity Analyses: Conduct sensitivity analyses to assess the robustness of findings to different modeling assumptions, missing data approaches, and unmeasured confounding [68].
Expected Outcomes: This protocol should yield validated estimates of subgroup-specific treatment effects with appropriate measures of statistical uncertainty. The results can confirm or refute signals of effect modification identified in earlier studies and provide evidence for clinical decision-making in specific patient subgroups.
Protocol 2: Transportability Analysis for Trial-Based HTE
This protocol evaluates whether HTE findings from randomized controlled trials generalize to target populations of interest, including those typically underrepresented in clinical trials.
Background and Rationale: RCT participants often differ meaningfully from real-world patient populations in factors that may modify treatment effects. This protocol provides a method for assessing the transportability of trial-based HTE findings to broader populations [68].
Procedure:
- Target Population Characterization: Define the target real-world population of interest and identify RWD sources that adequately represent this population.
- Effect Modifier Assessment: Identify and measure key variables suspected to modify treatment effects in both the trial and RWD populations.
- Standardization Approach: Apply standardization methods (e.g., weighting) to adjust for differences in the distribution of effect modifiers between trial and target populations.
- Transportability Evaluation: Compare standardized treatment effects from the trial with those directly estimated from the RWD to assess consistency of HTE patterns.
- Heterogeneity Source Investigation: Explore sources of heterogeneity by examining treatment effect variation across different clinical settings, practice patterns, and patient characteristics in the RWD.
Expected Outcomes: This protocol produces evidence regarding the generalizability of trial-based HTE findings to specific real-world populations and clinical settings, informing personalized treatment decisions across diverse patient groups.
Statistical Considerations and Reporting Standards
Key Statistical Issues in HTE Validation
Confirmatory HTE analyses face several statistical challenges that must be addressed to ensure valid inference. The power limitation for detecting HTE is substantial—sample sizes need to be approximately four times larger to detect a difference in subgroup effects of the same magnitude as the overall treatment effect for a 50:50 subgroup split [61]. The multiple testing problem arises when numerous subgroup hypotheses are examined simultaneously, increasing the risk of false positive findings without appropriate statistical correction [61]. Confounding control requires special methods in observational studies, as standard propensity score approaches applied to the overall population may not adequately address confounding within subgroups [68].
Table 3: Statistical Framework for Confirmatory HTE Analysis
| Statistical Issue | Challenge in HTE Analysis | Recommended Approach |
|---|---|---|
| Sample Size and Power | Low power to detect subgroup differences; requires larger samples than ATE estimation [61]. | Power calculations specific to interaction tests; consider RWD sources with large samples. |
| Multiple Testing | Increased false positive rates when testing multiple subgroup hypotheses [61]. | Prespecification of limited hypotheses; Bonferroni or similar corrections. |
| Confounding Control | Standard PS methods inappropriate for subgroup-specific effects [68]. | Estimate propensity scores within subgroups; within-subgroup matching/weighting. |
| Effect Scale | HTE may be present on relative but not absolute scale, or vice versa [68]. | Report both relative and absolute effects; specify primary scale in protocol. |
| Unmeasured Confounding | Residual confounding may distort subgroup effect estimates. | Quantitative bias analysis; sensitivity analyses for unmeasured confounding. |
The scale dependence of HTE represents another important consideration, as effects may appear heterogeneous on relative scales but homogeneous on absolute scales, or vice versa [68]. Some methodologies recommend assessing both scales to obtain a complete picture of HTE patterns. Finally, model specification choices can influence HTE findings, requiring careful attention to functional forms of continuous variables and interaction terms.
Figure 2: Statistical decision pathway for confirmatory HTE analysis, highlighting key methodological choice points and validation steps.
Reporting Guidelines for Validated HTE Findings
Transparent reporting of confirmatory HTE analyses enhances the interpretability and credibility of findings. The subgroup specification should be clearly described, including the rationale for each subgroup hypothesis and whether the direction of effect was correctly hypothesized a priori [68]. The analytical approach should be thoroughly documented, including methods for addressing confounding, testing interactions, and adjusting for multiple comparisons [68]. Uncertainty quantification should accompany all subgroup effect estimates through confidence intervals, with particular attention to the precision of estimates for smaller subgroups [68].
Absolute risk differences should be reported alongside relative measures to facilitate clinical interpretation and decision-making, as heterogeneous relative effects may translate to homogeneous absolute effects, or vice versa [68]. The clinical significance of any detected HTE should be discussed in terms of impact on net treatment benefit, considering both benefits and harms across subgroups [68]. Finally, limitations of the analysis should be acknowledged, including potential for residual confounding, multiple testing, and other methodological challenges specific to HTE assessment.
External validation plays an indispensable role in establishing credible evidence for heterogeneity of treatment effects. Through rigorous application of the protocols and methodologies outlined in this document, researchers can advance beyond exploratory subgroup analyses to generate confirmatory evidence capable of informing personalized treatment decisions. The integration of RCT findings with real-world data through carefully designed validation studies represents a promising pathway for translating average treatment effects into targeted therapeutic strategies that account for the inherent heterogeneity of patient populations.
Heterogeneity of Treatment Effects (HTE) is a fundamental concept in pharmacoepidemiology that addresses why medications work differently across various patient populations [8]. Understanding HTE is essential for personalizing treatment strategies to improve patient outcomes, moving beyond the average treatment effect (ATE) that often obscures the reality that some patients may benefit greatly from a treatment while others may be harmed [8]. Synthesizing HTE across studies presents unique methodological challenges, as variations in study populations, interventions, methodologies, and measurement tools can lead to heterogeneity that exceeds what would be expected by chance alone [69]. This application note provides detailed protocols for synthesizing HTE evidence through meta-analytical approaches and Individual Patient Data Meta-Analysis (IPDMA), enabling researchers to develop more personalized and effective drug therapies.
Foundational Concepts and Methodological Approaches
Defining and Measuring HTE
HTE evaluates how a treatment effect changes across different levels of patient characteristics, known as effect modifiers [8]. Proper identification and measurement of HTE requires understanding several key concepts:
- Effect Modifiers: Characteristics that influence how a patient responds to treatment, including age, sex, race, genotype, comorbid conditions, or other baseline risk factors for the outcome of interest [8]. These must be measurable at baseline, prior to treatment initiation.
- Scale Dependence: Treatment effects can be constant across levels of an effect modifier on one scale but vary on another. For example, effects may be homogeneous on the risk ratio (RR) scale but heterogeneous on the risk difference (RD) scale [8].
- Contrast Measures: The difference in RDs across strata measures effect modification on the additive scale, while the ratio of RRs across strata measures it on the multiplicative scale [8].
Table 1: Key Measures for HTE Assessment
| Measure | Calculation | Interpretation | Clinical Utility |
|---|---|---|---|
| Risk Difference (RD) | Risk~treated~ - Risk~control~ | Absolute risk change | Estimates number needed to treat/harm |
| Risk Ratio (RR) | Risk~treated~ / Risk~control~ | Relative risk change | Commonly reported in statistical software |
| Effect Modification (Additive) | RD~Strata1~ - RD~Strata2~ | Difference in absolute effects | Most informative for clinical decision-making |
| Effect Modification (Multiplicative) | RR~Strata1~ / RR~Strata2~ | Ratio of relative effects | May show different heterogeneity patterns |
Advantages of Real-World Data for HTE Assessment
Real-world data (RWD) offers distinct advantages for studying HTE compared to randomized controlled trials (RCTs) [8]:
- Larger Sample Sizes: Enable more statistically precise estimates of subgroup-specific treatment effects.
- Greater Diversity: Captures patients across diverse clinical contexts, comorbidities, and demographic backgrounds.
- Post-Marketing Surveillance: Allows detection of rare and late-onset safety outcomes not observable in pre-approval trials.
- Generalizability Assessment: Facilitates evaluation of whether trial results translate to broader clinical practice.
Quantitative Synthesis Methods for HTE
Meta-Analytical Approaches to Heterogeneity
Meta-analysis of heterogeneous data requires specialized methodological approaches to account for variability across studies while borrowing strength from related datasets [70]. The following table summarizes key methodological considerations:
Table 2: Meta-Analysis Methods for Heterogeneous Data
| Methodological Aspect | Approaches | Considerations for HTE |
|---|---|---|
| Model Selection | Fixed-effects vs. Random-effects | Random-effects preferred when heterogeneity exists [69] |
| Heterogeneity Quantification | Cochran's Q, I², τ² | I² > 50% indicates substantial heterogeneity [69] |
| Prediction Intervals | (pooled mean - z~α/2~ × τ, pooled mean + z~α/2~ × τ) | Provides range for predicted effect in new settings [69] |
| Integrative Sparse Regression | Global parameter estimation | Adapts to previously seen and predicts for unseen data distributions [70] |
| Handling High-Dimensional Data | One-shot estimators | Preserves data source anonymity while leveraging combined dataset size [71] |
Individual Patient Data Meta-Analysis (IPDMA) Protocol
IPDMA represents the gold standard for synthesizing HTE across studies, as it allows for direct investigation of patient-level effect modifiers [72].
Protocol: Conducting IPDMA for HTE Assessment
Objective: To identify patient characteristics and types of medication most associated with treatment effects (both beneficial and harmful) through pooled analysis of individual patient data from multiple studies.
Data Collection and Harmonization:
- Systematic Literature Search: Identify potentially eligible studies through database searching (e.g., PubMed, Embase) using comprehensive search terms combining condition, treatment, and study design terms [72].
- Collaborator Engagement: Contact corresponding authors of eligible studies with research protocol for collaboration and data sharing.
- Privacy Protection: Ensure transferred databases contain only anonymized data with unique study numbers.
- Variable Harmonization: Compare available variables across datasets and create a definitive list of IPDMA variables based on comparable definitions across at least two studies [72].
Data Items and Definitions:
- Patient Characteristics: Age (categorized), gender, clinical service (surgical/non-surgical), urgency of admission, polypharmacy status (typically defined as >5 drugs) [72].
- Treatment Outcomes: Effectiveness measures, safety endpoints (adverse drug events), compliance metrics.
- ADE Assessment: Trigger tools for identification, causality (certain/probable/possible), severity (using standardized classifications like CTCAE), preventability, medication accountability, error type [72].
Statistical Analysis Plan:
- Descriptive Statistics: Characterize the pooled study population overall and by individual study.
- Regression Modeling: Use Poisson or logistic regression models to identify factors associated with outcomes of interest.
- Subgroup Analyses: Conduct stratified analyses to examine treatment effects across patient subgroups.
- Multiple Testing Corrections: Apply appropriate corrections for multiple comparisons.
- Sensitivity Analyses: Assess robustness of findings to different modeling assumptions and variable definitions.
Visualizing Methodological Approaches and Workflows
HTE Synthesis Decision Pathway
IPDMA Implementation Workflow
Research Reagent Solutions for HTE Investigation
Table 3: Essential Methodological Tools for HTE Research
| Tool Category | Specific Solutions | Application in HTE Research |
|---|---|---|
| Statistical Software | R (metafor, meta packages), Python (scikit-learn, statsmodels), SAS | Implementation of meta-analytical models and HTE detection methods [8] [70] |
| Quality Assessment | Cochrane Risk of Bias, MINORS checklist, CASP for qualitative evidence | Methodological quality appraisal of included studies [72] [73] |
| HTE Methodologies | Subgroup analysis, Disease Risk Score, Effect modeling approaches | Each offers tradeoffs between simplicity, mechanistic insight, and precision [8] |
| Evidence Synthesis Frameworks | SPICE, RETREAT, GRADE-CERQual, ENTREQ | Structured approaches for qualitative evidence synthesis in HTA [73] |
| Data Visualization | ClearPoint strategy software, R ggplot2, Python matplotlib | Presentation of both quantitative and qualitative data for management reporting [74] |
Advanced Methodological Considerations
Handling Heterogeneity in Meta-Analysis
Heterogeneity is an unavoidable aspect of meta-analyses that reflects genuine differences in study outcomes beyond what is expected by chance [69]. Effective management requires:
- Quantification: Using I² statistic to measure the percentage of total variability due to heterogeneity (with values of 25%, 50%, and 75% representing low, medium, and high heterogeneity, respectively).
- Prediction Intervals: Providing the expected range of true effects in similar studies, calculated as: (pooled mean - z~α/2~ × τ, pooled mean + z~α/2~ × τ) where τ represents the between-study standard deviation [69].
- Exploration: Conducting subgroup analyses and meta-regressions to identify sources of heterogeneity.
Emerging Approaches in HTE Research
Innovative methodologies are expanding HTE research capabilities:
- Integrative Sparse Regression: Enables meta-analysis in high-dimensional settings where data sources are similar but non-identical, particularly valuable for large-scale drug treatment datasets [70] [71].
- Proteoformics: Shifting from protein-targeted to proteoform-targeted drug development acknowledges that different proteoforms within canonical protein definitions can yield varying drug responses, significantly advancing personalized therapy [75].
- Mixed Methods Synthesis: Combining quantitative HTE assessment with qualitative evidence on feasibility, meaningfulness, and acceptability using frameworks like SPICE and RETREAT [73].
Synthesizing HTE across studies requires careful methodological choices that balance practical implementation considerations with the need for clinically meaningful insights about differential treatment effects. IPDMA represents the most robust approach when feasible, while aggregate-level meta-analyses with appropriate heterogeneity quantification and exploration offer valuable alternatives. Researchers should select methods based on their specific research questions, available data resources, and the decision-making contexts their findings will inform. As personalized medicine advances, methodologies that effectively characterize and communicate HTE will play an increasingly critical role in optimizing drug therapy for individual patients.
Conclusion
Effectively handling heterogeneity is not an obstacle to overcome but an opportunity to generate more precise and clinically relevant evidence. A strategic approach that prioritizes a priori planning, employs robust multivariable methods like risk-based analysis, and rigorously validates findings is essential for moving beyond the average treatment effect. The future of comparative drug efficacy research lies in embracing heterogeneity through predictive modeling frameworks like the PATH Statement, which facilitate the transition from one-size-fits-all conclusions to personalized treatment recommendations. For researchers and drug developers, this evolution is key to answering the central question of patient-centered care: which treatment is best for which patient, and when.
References
- 1. Clinical Heterogeneity - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK53308/]
- 2. Comparative efficacy and safety of tislelizumab and other ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12630173/]
- 3. A systematic review and meta-analysis of the efficacy and ... [https://www.nature.com/articles/s41591-025-03978-z]
- 4. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 5. Text has enhanced contrast - Rules - Siteimprove [https://alfa.siteimprove.com/rules/sia-r66]
- 6. 15 Visualization [https://experimentology.io/015-viz.html]
- 7. ç ”ç©¶ä¸çš„“异质性â€ã€â€œå¼‚质性结果â€æ˜¯æŒ‡ï¼Ÿ 原创 [https://blog.csdn.net/qq_65052774/article/details/143492385]
- 8. Characterizing Treatment Effect Heterogeneity Using Real†... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11993293/]
- 9. 怎么处ç†Meta分æžå¼‚质性?看完这篇就够了原创 [https://blog.csdn.net/tongjizhiguang/article/details/126426487]
- 10. 异质性分æžæŒ‡æ ‡å¦‚何计算? [https://www.bilibili.com/read/cv27419648/]
- 11. Estimating heterogeneity of treatment effect in psychiatric ... [https://www.sciencedirect.com/science/article/abs/pii/S002239562500593X]
- 12. 怎么对数æ®è¿›è¡Œå¼‚è´¨æ€§åˆ†æž [https://www.fanruan.com/blog/article/399754/]
- 13. Predictive approaches to heterogeneous treatment effects [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-020-01145-1]
- 14. Statistical inference for heterogeneous treatment effect with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505326/]
- 15. The impact of randomization techniques on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12276662/]
- 16. Comparative efficacy and safety of botanical drugs for mild ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1657169/full]
- 17. Network Metaâ€Analysis: Efficacy of Biological Therapies and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12151545/]
- 18. a network meta-analysis of randomized controlled trials [https://link.springer.com/article/10.1007/s40520-025-03017-4]
- 19. Using mediators to understand effect modification and ... [https://www.sciencedirect.com/science/article/abs/pii/S089543562300238X]
- 20. Recommendations for presenting analyses of effect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3324457/]
- 21. An overview of modern machine learning methods for ... [https://www.sciencedirect.com/science/article/pii/S2352827325000187]
- 22. Chapter 6: Choosing effect measures and computing ... [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-06]
- 23. Overall average treatment effects from clinical trials, one ... [https://pubmed.ncbi.nlm.nih.gov/37148125/]
- 24. Introduction - Comparative Effectiveness Review Methods [https://www.ncbi.nlm.nih.gov/books/NBK53313/]
- 25. Understanding Treatment Effect Estimates When ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6437676/]
- 26. Methods for real-world studies of comparative effects [https://www.nice.org.uk/corporate/ecd9/chapter/methods-for-real-world-studies-of-comparative-effects]
- 27. Visualizing Quantitative Data: Best Experience [https://powerdrill.ai/blog/visualizing-quantitative-data-best-experience]
- 28. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 29. Subgroup analyses in confirmatory clinical trials: time to be ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4757983/]
- 30. Statistical Considerations for Subgroup Analyses - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7920926/]
- 31. Subgroup comparisons within and across studies in meta- ... [https://arxiv.org/html/2508.15531v1]
- 32. A critical review of graphics for subgroup analyses in clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8647927/]
- 33. The Predictive Approaches to Treatment effect Heterogeneity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7531587/]
- 34. The PATH Statement Explanation and Elaboration Document [https://pmc.ncbi.nlm.nih.gov/articles/PMC7750907/]
- 35. scoping review of the impact of the PATH Statement - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11100853/]
- 36. A standardized framework for risk-based assessment of ... [https://www.nature.com/articles/s41746-023-00794-y]
- 37. Data Visualisation in Clinical Research [https://careers.iconplc.com/blogs/2025-2/data-visualisation-in-clinical-research]
- 38. Understanding the anatomy and proper construction of tables [https://www.decisionfoundry.com/misc/articles/understanding-the-anatomy-and-proper-construction-of-tables/]
- 39. Using Individualized Treatment Effects to Assess Treatment Effect Heterogeneity [https://arxiv.org/html/2502.00713v1]
- 40. Overview of methods for comparing the efficacies of drugs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3895352/]
- 41. Clinical Trials With Pragmatic Elements: A Review of Use ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12641079/]
- 42. Project Pragmatica [https://www.fda.gov/about-fda/oncology-center-excellence/project-pragmatica]
- 43. A Review of Heterogeneity in Comparative Economic Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12081492/]
- 44. Protocol design for clinical trials - the complete checklist [https://clinicaltrialrisk.org/clinical-trial-design/protocol-design-for-clinical-trials-the-complete-checklist/]
- 45. Data dredging [https://en.wikipedia.org/wiki/Data_dredging]
- 46. What is data dredging? [https://www.scribbr.com/frequently-asked-questions/data-dredging/]
- 47. What is Data Dredging (data fishing)? [https://www.techtarget.com/searchdatamanagement/definition/data-dredging]
- 48. Multiplicity corrections in life sciences: challenges and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205177/]
- 49. Overview of multiple testing methodology and recent ... [https://www.sciencedirect.com/science/article/abs/pii/S1551714415300513]
- 50. Quantitative Data Quality Assurance, Analysis and Presentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056448/]
- 51. A novel statistical approach to detect the efficacy of drugs ... [https://vivli.org/a-novel-statistical-approach-to-detect-the-efficacy-of-drugs-that-have-heterogeneous-treatment-effects/]
- 52. You need 16 times the sample size to estimate an ... [https://statmodeling.stat.columbia.edu/2018/03/15/need16/]
- 53. Power for tests of interaction: effect of raising the Type I error rate [https://pmc.ncbi.nlm.nih.gov/articles/PMC1910596/]
- 54. Low Power Tests Exaggerate Effect Sizes [https://statisticsbyjim.com/hypothesis-testing/low-power-studies/]
- 55. Opportunities for Pragmatic Design Elements in Surgical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452089/]
- 56. Heterogeneity in pragmatic randomised trials - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9615398/]
- 57. Subgroup analyses in confirmatory clinical trials: time to be ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-016-0122-6]
- 58. Three simple rules to ensure reasonably credible subgroup ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4632208/]
- 59. A New Tool for Assessing the Credibility of Effect ... [https://usblog.gradeworkinggroup.org/2020/09/a-new-tool-for-assessing-credibility-of.html]
- 60. Nonlinear effects and effect modification at the participant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7616838/]
- 61. Estimation and Reporting of Heterogeneity of Treatment Effects [https://www.ncbi.nlm.nih.gov/books/NBK126188/]
- 62. Models with interactions overestimated heterogeneity of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7497896/]
- 63. Models with interactions overestimated heterogeneity of ... [https://www.sciencedirect.com/science/article/abs/pii/S0895435618310072#!]
- 64. Consideration of a Credibility Assessment Framework in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6966181/]
- 65. Competing risk and heterogeneity of treatment effect in clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2423182/]
- 66. Text color must provide high contrast with its background [https://docs.acquia.com/web-governance/text-color-must-provide-high-contrast-its-background]
- 67. Contrast requirements for WCAG 2.2 Level AA [https://www.makethingsaccessible.com/guides/contrast-requirements-for-wcag-2-2-level-aa/]
- 68. Assessing Heterogeneity of Treatment Effect in Real-World ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10273137/]
- 69. Heterogeneity in meta-analyses: an unavoidable challenge ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12326561/]
- 70. Meta-analysis of heterogeneous data: integrative sparse ... [https://jmlr.org/papers/v23/21-0739.html]
- 71. Meta-analysis of heterogeneous data: integrative sparse ... [https://arxiv.org/abs/1912.11928]
- 72. An individual patient data meta-analysis on factors associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4386940/]
- 73. Mapping frameworks for synthesizing qualitative evidence ... [https://pubmed.ncbi.nlm.nih.gov/39534917/]
- 74. How to Present Quantitative & Qualitative Data in Reports [https://www.clearpointstrategy.com/blog/qualitative-and-quantitative-data]
- 75. Personalized Drug Therapy: Innovative Concept Guided ... [https://www.sciencedirect.com/science/article/pii/S1535947624000276]