Beyond Plasma: Integrating Structure–Tissue Exposure/Selectivity Relationship (STR) for Smarter Drug Optimization
With a 90% failure rate in clinical drug development, often due to insufficient efficacy or unmanageable toxicity, the pharmaceutical industry is re-evaluating its lead optimization paradigms.
Beyond Plasma: Integrating Structure–Tissue Exposure/Selectivity Relationship (STR) for Smarter Drug Optimization
Abstract
With a 90% failure rate in clinical drug development, often due to insufficient efficacy or unmanageable toxicity, the pharmaceutical industry is re-evaluating its lead optimization paradigms. This article explores the critical concept of the Structure–Tissue Exposure/Selectivity Relationship (STR), which complements the traditional Structure–Activity Relationship (SAR). We detail how STR analysis moves beyond plasma pharmacokinetics to optimize drug exposure in disease-targeted tissues while minimizing accumulation in normal organs. Drawing on recent case studies with cannabidiol carbamates and selective estrogen receptor modulators (SERMs), we provide a methodological framework for integrating STR into drug discovery. The content covers foundational principles, practical applications, troubleshooting common pitfalls, and validation strategies, offering researchers and drug development professionals a roadmap to improve the selection of clinical candidates and balance efficacy with safety.
Why Plasma Isn't Enough: The Foundational Principles of STR
The process of clinical drug development is characterized by a persistently high failure rate, with approximately 90% of drug candidates failing to achieve regulatory approval after entering clinical trials [1]. This attrition represents a massive scientific and financial challenge, with the average cost per approved drug reaching $2.6 billion and development timelines spanning 10-15 years [2]. Analysis of clinical trial data from 2010-2017 reveals four primary reasons for this failure: lack of clinical efficacy (40-50%), unmanageable toxicity (30%), poor drug-like properties (10-15%), and lack of commercial needs or poor strategic planning (10%) [1]. Despite implementation of numerous successful strategies across target validation, screening, and preclinical testing, this 90% failure rate has remained stubbornly consistent for decades, raising critical questions about potential overlooked aspects in current drug optimization paradigms [1].
Quantitative Analysis of Clinical Attrition
Phase-by-Phase Attrition Rates
Table 1: Clinical Trial Success Rates and Durations by Phase
| Development Phase | Success Rate | Average Duration | Primary Failure Causes |
|---|---|---|---|
| Phase I | 60-70% [3] | Several months to 2.3 years [3] | Safety/toxicity concerns (37% fail) [2] |
| Phase II | 30-33% [3] | Several months to 2 years [3] | Lack of efficacy (~70% fail) [2] |
| Phase III | 50-57.8% [3] | 1-4 years [3] | Inadequate efficacy/safety vs. standard of care (42% fail) [2] |
| Overall (Phase I to Approval) | ~10% [1] | 6-7 years (clinical phase only) [3] | Efficacy (40-50%), toxicity (30%), PK/PD properties (10-15%) [1] |
Dynamic Success Rate Analysis
Recent analyses indicate that while clinical trial success rates (ClinSR) declined since the early 21st century, they have recently plateaued and begun to show slight improvement [4]. The ClinSR for repurposed drugs has been unexpectedly lower than that for all drugs in recent years, with anti-COVID-19 drugs demonstrating an extremely low ClinSR [4]. Significant variations exist in ClinSRs across different disease areas, developmental strategies, and drug modalities, highlighting the need for therapeutic-area-specific development strategies.
The STAR Framework: Addressing Fundamental Gaps in Drug Optimization
Limitations of Current Optimization Approaches
Current drug optimization overwhelmingly emphasizes potency and specificity using structure-activity relationship (SAR) but largely overlooks tissue exposure and selectivity in disease versus normal tissues [1] [5]. This imbalance misleads drug candidate selection and critically impacts the balance of clinical dose, efficacy, and toxicity. The standard practice of using plasma exposure as a surrogate for tissue exposure represents a significant flaw, as studies demonstrate that drug plasma exposure frequently does not correlate with drug exposure in target tissues [6]. For central nervous system targets, this discrepancy is particularly problematic, as candidates with adequate plasma levels may fail to achieve therapeutic concentrations in required tissues.
Structure-Tissue Exposure/Selectivity-Activity Relationship (STAR)
The STAR framework proposes a integrated approach that classifies drug candidates based on three key parameters: drug potency/selectivity, tissue exposure/selectivity, and required dose for balancing clinical efficacy/toxicity [1]. This classification system enables more informed candidate selection and development strategy:
Table 2: STAR-Based Drug Candidate Classification
| Class | Potency/Specificity | Tissue Exposure/Selectivity | Clinical Dose | Success Potential |
|---|---|---|---|---|
| Class I | High | High | Low | Superior clinical efficacy/safety with high success rate |
| Class II | High | Low | High | Achieves efficacy with high toxicity; requires cautious evaluation |
| Class III | Relatively low (adequate) | High | Low | Achieves efficacy with manageable toxicity; often overlooked |
| Class IV | Low | Low | High | Inadequate efficacy/safety; should be terminated early |
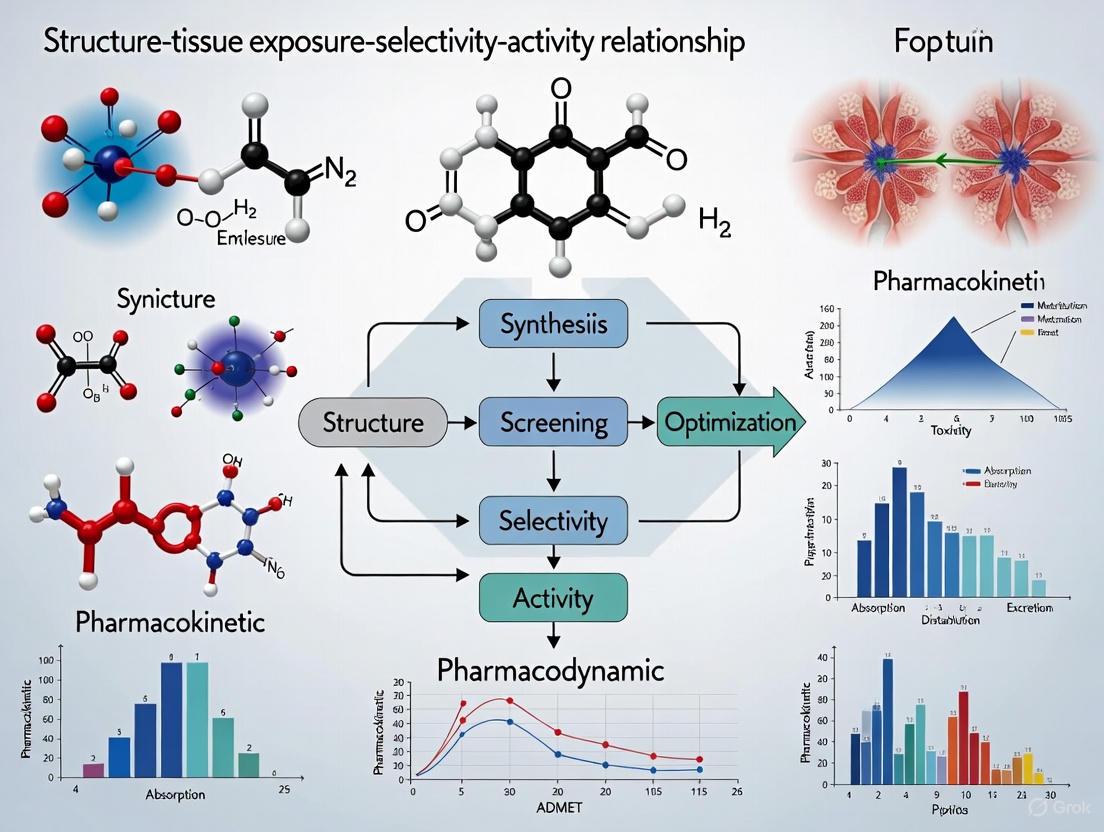
Diagram 1: Integrated STAR Framework for Drug Optimization
Experimental Protocols for STR Assessment
Protocol 1: Comprehensive Tissue Distribution Study
Objective: To quantitatively determine drug exposure and selectivity in disease-targeted tissues versus normal tissues.
Materials:
- Test compound(s) and reference standards
- Animal disease models (minimum n=6 per group)
- UPLC-HRMS system with validated analytical method
- Tissue homogenization equipment
- Isotope-labeled internal standards
Methodology:
- Dosing and Sample Collection: Administer therapeutic dose orally or intravenously. Euthanize animals at predetermined time points (e.g., 0.5, 1, 2, 4, 8, 12, 24h). Collect blood (for plasma), disease-target tissues, and vital normal tissues.
- Sample Processing: Homogenize tissues in appropriate buffer (1:3 w/v). Extract drugs using protein precipitation (acetonitrile with 0.1% formic acid) with isotope-labeled internal standards.
- UPLC-HRMS Analysis:
- Column: Acquity UPLC BEH C18 (1.7 μm, 2.1 × 50 mm)
- Mobile phase: A: 0.1% formic acid in water; B: 0.1% formic acid in acetonitrile
- Gradient elution: 5-95% B over 3.5 min, flow rate 0.4 mL/min
- MS detection: Positive/negative electrospray ionization, full scan mode (m/z 100-1000)
- Data Analysis: Calculate tissue-to-plasma ratios (Kp) for each tissue. Determine AUC0-t in plasma and tissues using non-compartmental analysis. Compute tissue selectivity index (TSI) as AUCdisease tissue/AUCnormal tissue.
Validation Parameters:
- Extraction recovery: >85%
- Matrix effects: 85-115%
- Precision: CV <15%
- Accuracy: 85-115% of nominal values
Protocol 2: STR Correlation with Efficacy/Toxicity
Objective: To establish correlation between tissue exposure/selectivity and observed efficacy/toxicity endpoints.
Materials:
- Series of structurally related compounds (minimum 4 analogs)
- Disease-relevant efficacy models
- Histopathology equipment
- Clinical chemistry analyzers
Methodology:
- Parallel Efficacy/Toxicity Testing: Conduct efficacy studies in disease models using standardized dosing regimens. In parallel, perform acute toxicity studies with MTD determination.
- Tissue Exposure Mapping: Quantify drug concentrations in efficacy-related tissues and toxicity-related tissues at multiple time points.
- Correlative Analysis:
- Plot efficacy endpoints (e.g., tumor reduction, biomarker modulation) against tissue AUC values
- Plot toxicity endpoints (e.g., histopathology scores, clinical chemistry) against tissue AUC values
- Calculate therapeutic windows based on tissue exposure rather than plasma exposure
- STR Modeling: Use molecular descriptors (logP, polar surface area, hydrogen bond donors/acceptors) to build quantitative STR models predicting tissue distribution patterns.
Research Reagent Solutions for STR Studies
Table 3: Essential Research Tools for STR Investigation
| Reagent/Technology | Function in STR Research | Key Applications |
|---|---|---|
| UPLC-HRMS Systems | Simultaneous quantification of drugs and metabolites in tissues with high sensitivity | Tissue distribution studies, metabolite profiling [6] |
| CETSA (Cellular Thermal Shift Assay) | Validate target engagement in intact cells and tissues | Confirmation of mechanism of action in disease-relevant tissues [7] |
| Stable Isotope-Labeled Internal Standards | Improve quantitative accuracy in complex matrices | Normalize extraction efficiency and matrix effects in tissue analysis [6] |
| AI/ML Prediction Platforms | In silico prediction of tissue distribution and selectivity | Early screening of compound libraries for favorable STR [8] |
| DNA-Encoded Libraries (DELs) | High-throughput screening of compound-target interactions | Identify hits with optimal binding characteristics [9] |
| Physiologically-Based Pharmacokinetic (PBPK) Modeling Software | Simulate tissue distribution prior to in vivo studies | Predict STR and optimize compound selection [2] |
Implementation Workflow for STAR-Driven Optimization
Diagram 2: STAR-Driven Drug Candidate Selection Workflow
The persistent 90% clinical attrition rate represents both a fundamental scientific challenge and substantial economic burden for drug development. The integrated STAR framework addresses core limitations of current optimization approaches by balancing traditional potency-focused SAR with critically important tissue exposure/selectivity considerations. Implementation of the experimental protocols and classification system described in this Application Note enables systematic identification of Class I drug candidates with optimal tissue distribution profiles, potentially reversing the trend of high clinical failure rates. As drug discovery continues to evolve, incorporating STR considerations early in the optimization process will be essential for developing therapeutics with balanced efficacy and safety profiles.
The "Free Drug Hypothesis" has long been a guiding principle in pharmacology, positing that only the unbound drug fraction in plasma passively distributes into tissues, with free drug concentrations at steady-state being approximately equal between plasma and target tissues [10]. This concept has profoundly influenced drug candidate selection, favoring compounds with high plasma exposure. However, mounting evidence reveals critical limitations of this model, as drug exposure in the plasma frequently fails to predict exposure in disease-targeted tissues [10] [6]. This discrepancy often misguides drug candidate selection, contributing to the high failure rates (approximately 90%) observed in clinical drug development [10] [6].
The emerging concept of the Structure–Tissue Exposure/Selectivity Relationship (STR) provides a more nuanced framework for drug optimization [10] [6]. STR investigates how structural modifications to a drug molecule influence its distribution and selectivity between target and normal tissues, directly impacting the balance between clinical efficacy and toxicity [10]. This article details application notes and protocols for characterizing these tissue exposure disparities, providing methodologies essential for integrating STR analysis into modern drug development pipelines.
Quantitative Evidence: Documented Disconnects Between Plasma and Tissue Exposure
Evidence from Selective Estrogen Receptor Modulators (SERMs)
A systematic investigation of seven SERMs with similar structures and identical molecular targets demonstrated that plasma drug exposure (AUC) did not correlate with drug concentrations in key target tissues, including tumor, fat pad, bone, and uterus [10]. The study found that slight structural modifications of four different SERMs did not significantly alter their plasma exposure profiles but profoundly altered their tissue exposure and selectivity [10]. This tissue-level distribution was directly correlated with the distinct clinical efficacy and safety profiles observed for these compounds.
Evidence from Cannabidiol (CBD) Carbamates
Research on BuChE-targeted CBD carbamates further underscores this phenomenon. In a study of CBD carbamates L2 and L4, the two compounds showed similar plasma exposure profiles but dramatically different distributions in the target tissue (brain) [6]. Specifically, L2 exhibited a fivefold higher brain concentration than L4, despite their nearly identical plasma AUC values [6]. This finding is particularly critical for central nervous system (CNS) drug development, where brain tissue exposure, not plasma concentration, determines pharmacodynamic activity.
Table 1: Comparative Tissue Exposure of Drug Candidates with Similar Plasma PK
| Drug Candidate | Plasma AUC (h·ng/mL) | Target Tissue AUC (h·ng/mL) | Tissue-to-Plasma Ratio (Kp) | Clinical Correlation |
|---|---|---|---|---|
| SERM A | ~1000 (Reference) | Tumor: ~800 | ~0.8 | Efficacy: Low |
| SERM B | ~1000 (Reference) | Tumor: ~2500 | ~2.5 | Efficacy: High |
| CBD Carbamate L2 | ~1000 (Reference) | Brain: ~5000 | ~5.0 | Efficacy: High |
| CBD Carbamate L4 | ~1000 (Reference) | Brain: ~1000 | ~1.0 | Efficacy: Low |
Core Experimental Protocols for Assessing Tissue Exposure and Selectivity
Comprehensive Tissue Distribution Study Protocol (LC-MS/MS Based)
Application Note: This protocol provides a robust methodology for quantifying drug concentrations across multiple tissues simultaneously, enabling the construction of detailed STR profiles. The method is particularly valuable for comparing analogs with similar plasma PK but potential differences in tissue distribution.
Materials and Reagents:
- Test compounds (drug candidates)
- Female MMTV-PyMT mice (8-12 weeks old) or other relevant disease models
- LC-MS/MS system with appropriate analytical column
- Acetonitrile (LC-MS grade)
- Internal standard solution (e.g., 25 nmol/L CE302 in ACN)
- Tissue homogenization equipment
Experimental Workflow:
Procedure Details:
- Animal Dosing: Administer test compounds at pharmacologically relevant doses (e.g., 5 mg/kg p.o. or 2.5 mg/kg i.v. for SERMs) to appropriate animal models [10].
- Time-Staggered Sample Collection: Euthanize animals at predetermined time points (e.g., 0.08, 0.5, 1, 2, 4, and 7 hours post-dosing) to capture distribution and elimination phases [10].
- Comprehensive Tissue Harvesting: Collect blood (for plasma separation), disease-targeted tissues (e.g., tumors for oncology models, brain for CNS targets), and potential toxicity-related normal tissues (e.g., liver, kidney, heart) [10].
- Sample Processing: Homogenize tissue samples in ice-cold acetonitrile containing an internal standard (40 μL sample + 40 μL ACN + 120 μL IS) [10]. Vortex for 10 minutes followed by centrifugation at 3500 rpm for 10 minutes at 4°C to precipitate proteins [10].
- LC-MS/MS Analysis: Inject supernatant for quantification using validated methods. Monitor multiple reaction monitoring (MRM) transitions specific to each compound.
- Data Analysis: Calculate AUC values for plasma and each tissue using non-compartmental methods. Determine tissue-to-plasma distribution coefficients (Kp = AUCtissue/AUCplasma) and tissue selectivity indices (SI = AUCtarget/AUCnormal).
Fluorescence-Based Biodistribution Quantification Protocol
Application Note: This protocol offers an alternative quantification method for fluorescently labeled compounds, enabling simultaneous tracking of multiple agents and providing spatial distribution information within tissues. It is particularly valuable for paired-agent imaging applications.
Materials and Reagents:
- Fluorescent agents (e.g., ABY-029, IRDye 680LT)
- Borosilicate glass capillary tubes
- Wide-field fluorescence imaging system
- Tissue homogenizer
- Nude mice with xenograft tumors (e.g., FaDu cells)
Experimental Workflow:
Procedure Details:
- Tissue-Specific Calibration Curves: Generate separate calibration curves for each tissue type by spiking known concentrations of fluorescent agents into homogenized tissue matrices. This accounts for tissue-specific optical properties and quenching effects [11].
- Agent Administration: Co-administer targeted and untargeted fluorescent agents via tail vein injection (e.g., 0.0487 mg/kg ABY-029 with equimolar IRDye 680LT in 200 μL PBS) [11].
- Sample Collection and Processing: Collect blood and tissues at multiple time points. Homogenize tissues thoroughly and load homogenates along with whole blood into borosilicate glass capillary tubes to standardize path length [11].
- Fluorescence Imaging and Quantification: Image capillary tubes using a wide-field fluorescence imaging system. Convert mean fluorescence intensity to concentration using tissue-specific calibration curves, which typically show high linearity (R² = 0.99 ± 0.01) [11].
- Data Analysis: Calculate pharmacokinetic parameters and biodistribution profiles for each agent. For paired-agent imaging, compare targeted and untargeted agent kinetics to estimate receptor concentration [11].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for STR Studies
| Category | Specific Items | Application Function | Technical Notes |
|---|---|---|---|
| Analytical Instruments | LC-MS/MS System | Quantitative drug measurement in complex matrices | Enables multiplexed quantification of parent drug and metabolites |
| Wide-field Fluorescence Imager | Fluorescent agent biodistribution | Must standardize path length (e.g., capillary tubes) for accuracy [11] | |
| Biological Models | MMTV-PyMT Transgenic Mice | Spontaneous breast cancer model | Allows study of tissue distribution in relevant disease context [10] |
| FaDu Xenograft Models | Head and neck cancer model | Useful for targeted agent studies (e.g., EGFR-targeting ABY-029) [11] | |
| Critical Reagents | CBD Carbamates (L1-L4) | STR probe compounds for CNS targets | Demonstrate how slight structural changes alter brain distribution [6] |
| Selective Estrogen Receptor Modulators | STR probe compounds for oncology | Show tissue selectivity despite similar plasma PK [10] | |
| IRDye 680LT & ABY-029 | Fluorescent paired agents | Enable comparative biodistribution and receptor quantification [11] | |
| Sample Processing | Internal Standards (e.g., CE302) | Normalization of extraction efficiency | Critical for accurate LC-MS/MS quantification [10] |
| Borosilicate Capillary Tubes | Standardized fluorescence measurement | Control path length variability in heterogeneous samples [11] | |
| PZ-II-029 | PZ-II-029, CAS:164025-44-9, MF:C18H15N3O3, MW:321.3 g/mol | Chemical Reagent | Bench Chemicals |
| QX77 | QX77, MF:C16H13ClN2O2, MW:300.74 g/mol | Chemical Reagent | Bench Chemicals |
Data Analysis and STR Modeling Approaches
Calculation of Key Distribution Parameters
- Tissue-to-Plasma Distribution Coefficient (Kp): Kp = AUCtissue / AUCplasma
- Tissue Selectivity Index (SI): SI = AUCtargettissue / AUCtoxicitytissue
- Relative Exposure Ratio (RER): RER = KpanalogA / KpanalogB
Multivariate Analysis for STR
- Principal Component Analysis (PCA): Reduces dimensionality of multi-tissue distribution data to identify clustering patterns among structural analogs [10].
- Ordinary Least Squares (OLS) Modeling: Builds quantitative structure-distribution relationship models to predict tissue exposure based on molecular descriptors [10].
Integration with ADMET Profiling
Correlate tissue distribution data with in silico ADMET predictions, including:
- Acute oral toxicity (LD50) projections
- Plasma protein binding propensity
- Blood-brain barrier permeability
- Hepatotoxicity risk indices [6]
Table 3: Integrating STR with ADMET Profiles for Candidate Selection
| Compound | Brain Kp | Plasma AUC | Predicted LD₅₀ (mg/kg) | BuChE IC₅₀ (μM) | STR-Based Evaluation |
|---|---|---|---|---|---|
| CBD | 1.0 (Ref) | 1.0 (Ref) | 319.5 | >10 | High safety, low potency |
| L1 | 1.8 | 0.9 | 22.1 | 0.15 | Toxicity concern |
| L2 | 5.0 | 3.2 | 70.5 | 0.077 | Optimal profile |
| L3 | 1.2 | 1.1 | 80.0 | 0.18 | Low brain exposure |
| L4 | 1.0 | 3.0 | 84.0 | 0.025 | High potency, low brain delivery |
The presented application notes and protocols provide a systematic approach for challenging the Free Drug Hypothesis and implementing STR analysis in drug discovery. By moving beyond plasma-centric pharmacokinetic evaluation to comprehensive tissue distribution assessment, researchers can:
- Select drug candidates based on target tissue exposure rather than plasma levels
- Optimize structural features to enhance tissue selectivity and improve therapeutic index
- Identify potential toxicity risks from unintended tissue accumulation early in development
- Rationalize clinical efficacy/toxicity outcomes through understanding of tissue-specific distribution
Integrating these STR methodologies with traditional SAR and ADMET profiling creates a more holistic drug optimization framework that can significantly improve clinical success rates by ensuring adequate drug exposure at the site of action while minimizing off-target accumulation.
The Structure–Tissue Exposure/Selectivity Relationship (STR) is a critical concept in modern drug optimization that describes how structural modifications to a lead compound alter its distribution and concentration in specific tissues relative to plasma and other tissues [10]. Traditional drug optimization has heavily emphasized the Structure-Activity Relationship (SAR), which focuses on improving a drug's potency and specificity for its molecular target, and drug-like properties based primarily on plasma pharmacokinetics (PK) [10]. However, this approach often overlooks a compound's tissue exposure/selectivity, which can directly impact clinical efficacy and toxicity profiles [10] [6].
The fundamental hypothesis underlying STR is that drug exposure in plasma is not always a reliable surrogate for drug exposure in disease-targeted tissues [10] [6]. Selecting drug candidates based solely on high plasma exposure can be misleading, as some compounds with low plasma exposure may achieve high concentrations in target tissues, and vice-versa [10]. Furthermore, even slight structural modifications that have minimal impact on plasma PK can significantly alter a drug's distribution profile, thereby affecting the balance between clinical efficacy and safety [10] [6]. Optimizing the STR, therefore, involves structural design to maximize drug exposure in diseased tissues while minimizing accumulation in healthy, toxicity-prone organs [6].
Quantitative Evidence of STR
STR in Selective Estrogen Receptor Modulators (SERMs)
A foundational study investigating seven SERMs with similar structures and the same molecular target demonstrated that their tissue exposure and selectivity were correlated with clinical efficacy/safety, whereas plasma exposure was not [10]. The following table summarizes key experimental findings from this research.
Table 1: Experimental Tissue Distribution Data of Select SERMs in MMTV-PyMT Mice (2.5 mg/kg i.v.) [10]
| Tissue | Tamoxifen AUC (ng·h/mL) | Toremifene AUC (ng·h/mL) | Afimoxifene AUC (ng·h/mL) | Droloxifene AUC (ng·h/mL) |
|---|---|---|---|---|
| Plasma | 240.5 | 255.8 | 248.9 | 235.2 |
| Tumor | 12,450.0 | 10,580.0 | 9,850.0 | 8,950.0 |
| Bone | 1,250.5 | 1,150.8 | 980.5 | 850.3 |
| Uterus | 890.3 | 950.6 | 1,050.7 | 780.4 |
| Liver | 15,850.0 | 14,950.0 | 16,050.0 | 12,500.0 |
Key Observations:
- Plasma-Tissue Disconnect: SERMs with nearly identical plasma exposure (AUC) showed markedly different accumulation in target tissues like tumors and bones [10].
- Efficacy/Toxicity Correlation: Tissue exposure/selectivity, not plasma levels, aligned with the distinct clinical efficacy and safety profiles of the SERMs [10].
- Structural Impact: Slight structural modifications among the SERMs were sufficient to alter their tissue exposure/selectivity, underscoring the existence of a definable STR [10].
STR in Cannabidiol (CBD) Carbamates
Recent research on CBD carbamates further validates the STR concept for central nervous system (CNS) targets. The study compared two carbamate derivatives, L2 and L4, which have similar plasma exposure but different structures at the carbamate amine group [6].
Table 2: Comparative STR Analysis of CBD Carbamates L2 and L4 [6]
| Parameter | L2 (Methylethylamine) | L4 (tert-Benzylamine) |
|---|---|---|
| Plasma AUC | High and similar to L4 | High and similar to L2 |
| Brain AUC | 5x higher than L4 | 5x lower than L2 |
| BuChE IC₅₀ | 0.077 μM | More potent than L2 |
| Rat LDâ‚…â‚€ | 70.5 mg/kg | 84.0 mg/kg |
| Key STR Insight | High brain penetration, favorable for CNS efficacy. | Lower brain exposure despite high plasma levels and high potency. |
Key Observations:
- The similar plasma exposure of L2 and L4 would not predict their drastically different brain distribution [6].
- The tissue/plasma distribution coefficient (Kp) is a critical STR parameter. Drug exposure in tissue is calculated as: Drug exposure in tissue = Drug exposure in plasma × Kp [6].
- This case demonstrates that STR optimization for CNS drugs requires a specific focus on ensuring sufficient brain exposure, independent of plasma PK [6].
Experimental Protocol for STR Profiling
This protocol details the methodology for quantifying tissue distribution to establish a Structure-Tissue Exposure/Selectivity Relationship (STR) for lead compounds, adapted from published studies [10] [6].
Materials and Reagents
- Test Compounds: Lead compounds and their structurally modified analogs.
- Animal Model: Disease-relevant animal model (e.g., transgenic MMTV-PyMT mice for breast cancer [10] or wild-type/transgenic rats for CNS studies [6]).
- Vehicle: Appropriate solvent for compound administration (e.g., saline, aqueous solution with <5% DMSO or other solubilizing agents).
- LC-MS/MS Materials:
- Mobile Phases: Acetonitrile and water of LC-MS grade.
- Internal Standard Solution: Stable isotope-labeled analog of the test compound or a structurally similar compound (e.g., CE302 at 25 nmol/L in ACN [10]).
- UPLC-HRMS System: Equipped with a C18 reverse-phase column.
In Vivo Tissue Distribution Study
Dosing and Sample Collection:
- Administer the test compound to animals (e.g., via oral gavage or intravenous injection) at a predefined dose (e.g., 5 mg/kg p.o. or 2.5 mg/kg i.v.) [10].
- At predetermined time points post-dosing (e.g., 0.08, 0.5, 1, 2, 4, and 7 hours), euthanize a cohort of animals and collect samples of blood/plasma and all tissues of interest (e.g., disease-targeted tissue, potential toxicity organs, and other relevant tissues) [10].
Sample Preparation:
- Homogenize weighed tissue samples in a buffer solution.
- Aliquot a precise volume (e.g., 40 μL) of plasma, blood, or tissue homogenate into a 96-well plate.
- Add ice-cold acetonitrile (e.g., 40 μL) and internal standard solution (e.g., 120 μL) to precipitate proteins and extract the analyte [10].
- Vortex the mixture vigorously for 10 minutes and then centrifuge at high speed (e.g., 3500 rpm for 10 min at 4°C) to remove precipitated material [10].
Bioanalysis via LC-MS/MS:
- Inject an aliquot of the supernatant into the UPLC-HRMS system.
- Quantify the concentration of the test compound in each sample by comparing the analyte-to-internal standard response ratio against a freshly prepared calibration curve.
Data Analysis and STR Modeling
Pharmacokinetic Calculation:
- Use a non-compartmental analysis (e.g., using Phoenix WinNonlin) to calculate the Area Under the concentration-time Curve (AUC) for plasma and each tissue.
Tissue Distribution Parameters:
- Calculate the Tissue-to-Plasma Ratio (Kp) for each tissue:
Kp = AUC_tissue / AUC_plasma. - Calculate the Tissue Selectivity Index (TSI) between target and toxicity-prone tissues:
TSI = Kp_target / Kp_toxicity.
- Calculate the Tissue-to-Plasma Ratio (Kp) for each tissue:
STR Correlation:
- Corrogate the structural features of each analog (e.g., logP, hydrogen bond donors/acceptors, rotatable bonds, presence of specific heterocycles [12]) with its tissue exposure (AUC_tissue) and selectivity (Kp, TSI).
- Use statistical models like Principal Component Analysis (PCA) or Ordinary Least Squares (OLS) to define the quantitative STR [10].
Workflow Visualization for STR-Driven Drug Optimization
The following diagram illustrates the integrated experimental and computational workflow for applying STR in lead optimization.
Diagram Title: STR-Driven Lead Optimization Workflow
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagent Solutions for STR Studies
| Reagent / Material | Function / Explanation |
|---|---|
| Stable Isotope-Labeled Internal Standard | Ensures accurate and precise quantification of drug concentrations in complex biological matrices (plasma, tissue homogenates) by correcting for variability during sample preparation and MS ionization. |
| LC-MS Grade Solvents | High-purity solvents (acetonitrile, water, methanol) minimize background noise and ion suppression in LC-MS/MS, which is critical for detecting low drug levels in small tissue samples. |
| Disease-Relevant Animal Model | Transgenic or xenograft models that replicate human disease pathophysiology are essential for generating clinically translatable STR data, as tissue distribution can be altered by the disease state (e.g., tumor EPR effect [10]). |
| Physicochemical & ADMET Prediction Software | Tools used to predict key properties (logP, pKa, TPSA) that influence tissue penetration early in the design cycle, helping to prioritize analogs for synthesis and in vivo testing [12] [6]. |
| UPLC-HRMS System | Provides the high chromatographic resolution and mass accuracy needed to separate, identify, and quantify the drug and its potential metabolites in tissue samples, ensuring data reliability. |
| Relmapirazin | Relmapirazin (MB-102) |
| RG7800 | RG7800|SMN2 Splicing Modulator|For Research |
Integrating STR analysis into the lead optimization pipeline is no longer optional for modern drug development. Evidence from SERMs and CBD carbamates confirms that structural modifications which minimally affect plasma exposure can drastically alter tissue distribution and selectivity [10] [6]. By employing the described protocols to generate quantitative tissue PK data and define the STR, researchers can make more informed candidate selection decisions. This approach moves beyond the traditional over-reliance on plasma PK and SAR, enabling the design of molecules optimized for high exposure at the site of action and low exposure in sites of potential toxicity, thereby increasing the probability of clinical success.
In the rigorous process of drug discovery, the Structure-Activity Relationship (SAR) has long been the cornerstone of lead optimization, focusing primarily on improving a drug candidate's potency and specificity against its molecular target [10]. However, an overemphasis on SAR often overlooks a critical determinant of clinical success: how structural modifications influence a drug's distribution to diseased tissues versus healthy ones. This relationship, termed the Structure-Tissue Exposure/Selectivity Relationship (STR), is now recognized as equally vital for balancing clinical efficacy with toxicity [6] [13].
The high failure rate of clinical drug development (approximately 90%) is often attributed to insufficient efficacy (~40-50%) or unmanageable toxicity (~30%) [10] [13]. A significant contributing factor is that the current drug optimization process frequently selects candidates based on high plasma exposure and target potency in vitro, mistakenly assuming this correlates with effective exposure in disease-targeted tissues [6] [10]. The Structure–Tissue Exposure/Selectivity–Activity Relationship (STAR) framework has been proposed to integrate these concepts, classifying drug candidates based on both their potency/selectivity and their tissue exposure/selectivity to better predict clinical outcomes [13].
This application note provides experimental protocols and analytical frameworks for characterizing STR and integrating it with SAR data, enabling a more balanced and predictive approach to drug candidate selection.
Key Concepts and Definitions
Table 1: Core Concepts in Integrated Drug Optimization
| Concept | Acronym | Definition | Primary Optimization Goal |
|---|---|---|---|
| Structure-Activity Relationship | SAR | The relationship between a compound's chemical structure and its biological activity against a specific molecular target. | Maximize target potency and specificity. |
| Structure-Tissue Exposure/Selectivity Relationship | STR | The relationship between a compound's chemical structure and its relative distribution and concentration in different tissues, particularly disease-targeted vs. normal tissues. | Maximize exposure in target tissues and minimize exposure in tissues associated with toxicity. |
| Structure–Tissue Exposure/Selectivity–Activity Relationship | STAR | An integrated framework that combines SAR and STR to classify drug candidates and guide selection based on potency, selectivity, tissue exposure, and required clinical dose. | Balance efficacy, toxicity, and dose to improve clinical success rates [13]. |
Table 2: STAR Classification System for Drug Candidates
| Class | Specificity/Potency | Tissue Exposure/Selectivity | Clinical Dose Implication | Clinical Outcome & Success Potential |
|---|---|---|---|---|
| Class I | High | High | Low dose required. | Superior efficacy/safety profile; high success rate [13]. |
| Class II | High | Low | High dose required. | Efficacy possible but with high toxicity risk; requires cautious evaluation [13]. |
| Class III | Relatively Low (Adequate) | High | Low dose required. | Good clinical efficacy with manageable toxicity; often overlooked in traditional optimization [13]. |
| Class IV | Low | Low | N/A | Inadequate efficacy and safety; should be terminated early [13]. |
Experimental Protocol for STR Characterization
Protocol: Comparative Tissue Distribution Study
Objective: To determine the tissue exposure and selectivity of drug candidates following administration in a relevant animal model.
I. Materials and Reagents Table 3: Essential Research Reagents and Materials
| Item | Function/Description | Example/Catalog Consideration |
|---|---|---|
| Test Compounds | Drug candidates for STR assessment. | e.g., CBD carbamates L1-L4 [6]; SERMs like tamoxifen, toremifene [10]. |
| Animal Model | In vivo system for pharmacokinetic and tissue distribution studies. | e.g., Rats (for CBD carbamates); Female MMTV-PyMT mice (for SERM studies in breast cancer) [6] [10]. |
| UPLC-HRMS or LC-MS/MS System | Quantitative bioanalysis of drug concentrations in biological matrices. | Systems capable of sensitive, simultaneous compound quantification (e.g., ACQUITY UPLC with Q-Exactive HRMS; LC-MS/MS with triple quadrupole) [6] [10]. |
| Internal Standard | Correction for sample preparation and injection variability in MS analysis. | Stable isotope-labeled analog of the analyte or structurally similar compound (e.g., CE302 for SERM analysis) [10]. |
| Protein Precipitation Solvent | Deproteinization of plasma and tissue homogenates for cleaner MS analysis. | Ice-cold acetonitrile [10]. |
II. Procedure
Formulation and Dosing:
Biological Sample Collection:
- At predetermined time points post-dosing (e.g., 0.08, 0.5, 1, 2, 4, 7 h), collect blood/plasma and relevant tissues.
- Target Tissues: Disease-relevant organs (e.g., brain for CNS disorders, tumor for oncology).
- Normal Tissues: Organs where toxicity often manifests (e.g., liver, heart, uterus for SERMs) [6] [10].
- Centrifuge blood to obtain plasma. Homogenize tissue samples in an appropriate buffer.
Sample Preparation:
- Aliquot a measured volume of plasma or tissue homogenate (e.g., 40 μL) into a 96-well plate.
- Add ice-cold acetonitrile (e.g., 40 μL) containing an internal standard to precipitate proteins.
- Vortex the mixture vigorously for 10 minutes and then centrifuge (e.g., 3500 rpm for 10 min at 4°C) to pellet debris [10].
- Transfer the clear supernatant for analysis.
Bioanalysis using UPLC-HRMS/LC-MS/MS:
- Inject the processed samples onto the chromatographic system.
- Use a validated method to separate the analytes.
- Detect compounds using mass spectrometry. Quantify concentrations by comparing the analyte-to-internal standard response ratio against a calibration curve prepared in the same biological matrix [6] [10].
Data Analysis:
- Use non-compartmental methods to calculate pharmacokinetic parameters: Area Under the Curve (AUC) for plasma (AUC~plasma~) and for each tissue (AUC~tissue~).
- Calculate the Tissue-to-Plasma Partition Coefficient (K~p~) for each tissue: K~p~ = AUC~tissue~ / AUC~plasma~ [6].
- Determine Tissue Selectivity Indices by comparing K~p~ values between target and off-target tissues (e.g., Brain-to-Liver K~p~ ratio).
Diagram 1: Tissue distribution study workflow.
Case Study: STR in Action – CBD Carbamates
Background: A series of cannabidiol (CBD) carbamates (L1-L4) were designed as potent butyrocholinesterase (BuChE) inhibitors for potential application in Alzheimer's disease, targeting the central nervous system [6].
Experimental Data: Table 4: STR Analysis of CBD Carbamates (Representative Data) [6]
| Compound | Key Structural Feature (Carbamate Amine) | BuChE IC₅₀ (μM) | Relative Plasma AUC | Relative Brain AUC | Brain-to-Plasma K~p~ | Rat Oral LD₅₀ (mg/kg) |
|---|---|---|---|---|---|---|
| L0 (CBD) | N/A | >10 | 1.0 | 1.0 | Baseline | 319.5 |
| L1 | Secondary Aliphatic Amine | ~0.1 | Low | Low | Low | 22.1 |
| L2 | Methylethylamine (Tertiary Aliphatic) | 0.077 | High | Very High | High | 70.5 |
| L3 | Cyclic Amine | ~0.1 | Low | Low | Low | 80.0 |
| L4 | tert-Benzylamine (Tertiary Aromatic) | Most Potent | High | Moderate | Moderate | 84.0 |
STR Interpretation and STAR Classification:
- Impact of Structure: Slight modifications to the carbamate amine group (e.g., secondary vs. tertiary, aliphatic vs. cyclic/aromatic) resulted in significant changes in tissue exposure and selectivity, independent of changes in plasma exposure or in vitro potency [6]. For instance, L2 and L4 had similar high plasma exposure, but L2 exhibited a 5-fold higher brain concentration than L4 [6].
- Efficacy/Safety Correlation: The secondary amine of L1 was metabolically less stable and associated with significantly higher oral toxicity (lower LDâ‚…â‚€), whereas the tertiary amines (L2, L3, L4) were more stable and had better safety profiles [6].
- STAR Classification:
- L2 demonstrates high BuChE potency and high brain exposure/selectivity, making it a potential Class I drug requiring a low dose for efficacy.
- L4 has high potency but lower brain selectivity than L2, potentially placing it in Class II, where a higher dose might be needed for efficacy, possibly increasing toxicity risk.
- L1 and L3, despite reasonable potency, have low plasma and tissue exposure, rendering them Class IV candidates.
Diagram 2: SAR and STR relationship in CBD carbamates.
Integrating STR and SAR: The STAR Framework for Candidate Selection
The CBD carbamate case and similar studies with Selective Estrogen Receptor Modulators (SERMs) [10] underscore that drug exposure in plasma is not a reliable surrogate for exposure in target tissues [6] [10]. Therefore, lead optimization must move beyond a singular focus on plasma PK and in vitro potency.
Protocol: Integrated STAR Analysis Workflow
- In Vitro Potency & Specificity Profiling (SAR): Determine ICâ‚…â‚€/Káµ¢ values against the primary target and related off-targets.
- In Vivo Tissue Distribution Study (STR): Conduct the protocol outlined in Section 3 to calculate AUC~plasma~, AUC~tissue~, and K~p~ values for key tissues.
- Toxicity Assessment: Perform preliminary in vivo toxicity studies (e.g., maximum tolerated dose, LDâ‚…â‚€, histopathology) [6].
- STAR Matrix Plotting and Classification:
- Create a 2D plot with Target Potency (e.g., 1/ICâ‚…â‚€) on the Y-axis and Tissue Selectivity Index (e.g., Target Tissue K~p~ / Toxic Tissue K~p~) on the X-axis.
- Overlay data points for all lead candidates.
- Classify each candidate into one of the four STAR classes (see Table 2).
- Candidate Selection:
- Prioritize Class I candidates for further development.
- Critically evaluate and potentially optimize Class II candidates to improve tissue selectivity.
- Re-evaluate Class III candidates that may have been overlooked by traditional SAR-focused optimization; their high tissue selectivity may allow for efficacy despite moderate in vitro potency.
- Terminate Class IV candidates early.
Table 5: Decision Matrix for STAR-Based Candidate Selection
| STAR Class | Development Recommendation | Key Considerations |
|---|---|---|
| Class I | High Priority for Progression | Ideal profile. Focus on formulation and preclinical safety. |
| Class II | Proceed with Caution / Optimize | Attempt structural modification to improve tissue selectivity (STR). Evaluate therapeutic index rigorously. |
| Class III | Re-evaluate and Consider | Often discarded by traditional methods. Assess if in vivo efficacy is adequate despite modest in vitro potency. Promising for low-dose therapies. |
| Class IV | Terminate | Unlikely to achieve a favorable efficacy-toxicity balance. |
Integrating the Structure-Tissue Exposure/Selectivity Relationship (STR) with the classical Structure-Activity Relationship (SAR) into a unified STAR framework provides a more holistic and predictive approach to drug optimization. The experimental protocols and analytical tools outlined in this application note empower researchers to systematically characterize and leverage STR. By selecting drug candidates based on both their intrinsic potency and their ability to selectively reach the site of action while avoiding healthy tissues, the probability of achieving a successful balance between clinical efficacy and safety in later-stage trials is significantly enhanced [6] [10] [13].
The Structure–Tissue exposure/selectivity relationship (STR) has emerged as a critical factor in drug development, demonstrating that minimal molecular modifications can significantly alter a compound's distribution profile across different tissues, ultimately impacting clinical efficacy and safety. This case study examines how subtle structural changes in Selective Estrogen Receptor Modulators (SERMs) result in dramatic alterations in tissue exposure and selectivity, independent of plasma pharmacokinetics. Through quantitative analysis of tissue distribution patterns and detailed experimental protocols, we provide a framework for integrating STR assessment into standard drug optimization workflows to improve clinical candidate selection and therapeutic outcomes.
Traditional drug optimization has heavily emphasized Structure-Activity Relationships (SAR) to enhance potency and specificity against molecular targets. However, this approach often overlooks the critical Structure–Tissue exposure/selectivity relationship (STR), which directly influences a drug's efficacy and toxicity profile in different tissues [14] [5]. The STR paradigm investigates how structural modifications affect a compound's distribution between disease-targeted tissues and normal tissues, creating tissue-selective exposure profiles that cannot be predicted from plasma pharmacokinetics alone [15].
Research on seven SERMs with similar structures and the same molecular target revealed that drug plasma exposure showed no correlation with drug exposures in key target tissues including tumor, fat pad, bone, and uterus [14] [5]. This disconnect underscores the necessity of directly measuring tissue exposure during drug development rather than relying on plasma concentrations as surrogates for target engagement.
Quantitative Analysis of SERM Tissue Distribution
Tissue Exposure Profiles Across SERM Classes
Table 1: Comparative Tissue Distribution Profiles of Representative SERMs
| SERM | Key Structural Features | Tumor Exposure | Bone Exposure | Uterine Exposure | Clinical Efficacy/Safety Correlation |
|---|---|---|---|---|---|
| Tamoxifen | Triphenylethylene core | Moderate | Moderate | High | Breast cancer efficacy; increased endometrial cancer risk |
| Raloxifene | Benzothiophene core | Moderate | High | Low | Osteoporosis treatment; breast cancer risk reduction |
| Fulvestrant | Steroidal backbone, 7α-alkyl sulfinyl chain | High | Low | Low | ER degradation; treatment of advanced breast cancer |
| Bazedoxifene | Indole core | Moderate | High | Low | Menopausal symptoms; osteoporosis prevention |
| Lasofoxifene | Naphthalene core | High | High | Moderate | Osteoporosis treatment; breast cancer risk reduction |
Impact of Minor Structural Modifications on Tissue Exposure
Studies investigating four SERMs with slight structural modifications demonstrated that these changes did not significantly alter plasma exposure but profoundly affected tissue exposure and selectivity [14] [5]. For instance, the replacement of a single atom in the tamoxifen structure to create toremifene resulted in altered tissue distribution patterns despite similar plasma pharmacokinetics [16].
Table 2: Impact of Specific Structural Modifications on SERM Tissue Distribution
| Structural Modification | Plasma Exposure Change | Tumor Tissue Impact | Bone Tissue Impact | Uterine Tissue Impact | Clinical Implications |
|---|---|---|---|---|---|
| Side chain length variation | Minimal | Up to 3.2-fold change | Up to 2.8-fold change | Up to 4.1-fold change | Altered efficacy/toxicity balance |
| Hydrogen bond donor/acceptor changes | Minimal | Significant alterations in accumulation | Variable effects | Pronounced changes | Modified tissue selectivity |
| Halogen substitution | Minimal | Altered penetration | Moderate effects | Significant impact | Safety profile modification |
| Protein binding affinity modifications | Minimal | Enhanced tumor accumulation via EPR effect | Limited effect | Limited effect | Improved tumor targeting |
Molecular Mechanisms of SERM Tissue Selectivity
Structural Biology of Estrogen Receptor Modulation
SERMs produce tissue-specific effects by inducing distinct conformational changes in estrogen receptors (ERα and ERβ), which are members of the nuclear receptor superfamily of ligand-dependent transcription factors [17] [18]. The ER ligand-binding domain (LBD) consists of 12 alpha helices that rearrange differently depending on the specific SERM bound [19].
Helix 12 positioning is particularly crucial—agonists position H12 over the ligand-binding pocket, enabling coactivator recruitment, while SERMs and antagonists displace H12, blocking the activation function-2 (AF-2) surface and preventing coactivator binding [17] [19]. Different SERMs induce unique H12 positions, leading to varied receptor conformations that influence tissue-specific responses.
Tissue-Specific Factors Influencing STR
The tissue-selective action of SERMs arises from several key factors:
Differential expression of ER subtypes: Tissues vary in their expression of ERα versus ERβ, which have distinct physiological functions and respond differently to SERMs [18]. For example, ERα mediates proliferation in breast tissue, while ERβ may have anti-proliferative effects.
Tissue-specific coregulator expression: The relative abundance of coactivators (e.g., SRC-1, SRC-3) and corepressors (e.g., NCoR, SMRT) in different tissues determines whether a SERM acts as an agonist or antagonist [17] [18].
Ligand-specific receptor conformations: Each SERM induces a unique ER conformation that affects its ability to interact with tissue-specific coregulatory proteins [17] [19].
Epigenetic and post-translational modifications: Phosphorylation, acetylation, and other modifications of ER and coregulators further influence tissue-specific responses to SERMs [18].
Experimental Protocols for STR Assessment
Protocol 1: Quantitative Tissue Distribution Studies
Objective: To quantitatively determine the concentration of SERMs in target tissues (tumor, bone, uterus, fat pad) versus plasma and calculate tissue selectivity indices.
Materials:
- Test SERM compounds (≥95% purity)
- Animal model (e.g., ovariectomized mice with ER+ breast tumor xenografts)
- Liquid chromatography-tandem mass spectrometry (LC-MS/MS) system
- Tissue homogenization equipment
- Stable isotope-labeled internal standards
Procedure:
- Dosing: Administer SERMs via appropriate route (oral preferred for clinical relevance) at therapeutically relevant doses.
- Sample Collection: At predetermined timepoints post-dose, collect blood (for plasma), tumor tissue, bone, uterus, and other relevant tissues.
- Sample Processing:
- Weigh each tissue sample accurately
- Homogenize tissues in appropriate buffer (e.g., phosphate-buffered saline)
- Extract SERMs using protein precipitation or solid-phase extraction
- Quantitative Analysis:
- Analyze samples using validated LC-MS/MS methods
- Use calibration curves with internal standards for precise quantification
- Data Analysis:
- Calculate tissue-to-plasma ratios for each SERM
- Determine tissue selectivity indices (e.g., tumor-to-uterus ratio)
- Perform statistical comparisons between SERMs with minor structural modifications
Key Parameters:
- Time of peak tissue concentration (Tmax,tissue)
- Tissue exposure (AUC0-t,tissue)
- Tissue-to-plasma ratio
- Selectivity index between target and off-target tissues
Protocol 2: Structural Determinants of Tissue Exposure
Objective: To correlate specific structural features with tissue exposure patterns and identify STR principles.
Materials:
- Series of structurally related SERM analogs
- Molecular modeling software
- Protein binding assessment tools (e.g., equilibrium dialysis)
- Tumor tissue penetration assay components
Procedure:
- Structural Characterization:
- Document specific structural variations (side chain length, functional groups, stereochemistry)
- Calculate physicochemical properties (log P, polar surface area, hydrogen bonding capacity)
- Protein Binding Assessment:
- Determine plasma protein binding using equilibrium dialysis
- Correlate protein binding with tissue distribution patterns
- Molecular Modeling:
- Dock SERM structures into ER ligand-binding domain
- Identify key interactions with amino acid residues
- Correlate structural features with tissue exposure data
- STR Model Development:
- Build quantitative structure-tissue exposure relationship (QSTR) models
- Validate models with test set compounds
Key Insights: SERMs with high protein binding showed higher accumulation in tumors compared to surrounding normal tissues, likely due to the enhanced permeability and retention (EPR) effect of protein-bound drugs [14] [5].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for STR Studies of SERMs
| Reagent/Category | Specific Examples | Function in STR Research |
|---|---|---|
| SERM Compounds | Tamoxifen, Raloxifene, Bazedoxifene, Lasofoxifene, Toremifene | Reference compounds for establishing baseline STR profiles and validating experimental systems |
| ER-Binding Assays | Fluorescence polarization assays, Time-resolved FRET assays, Competitive binding kits | Quantify binding affinity to ERα and ERβ subtypes and correlate with tissue distribution |
| Cellular Models | MCF-7 (breast cancer), T47D (breast cancer), Ishikawa (endometrial), Primary osteoblasts | Assess tissue-specific transcriptional responses and functional outcomes in relevant cellular contexts |
| Animal Models | Ovariectomized mice, ER+ breast cancer xenografts, Osteoporosis models | Evaluate in vivo tissue distribution and selectivity in physiologically relevant systems |
| Analytical Tools | LC-MS/MS systems, Stable isotope-labeled internal standards, Tissue homogenization equipment | Precisely quantify compound concentrations in complex biological matrices |
| Molecular Biology Reagents | Coactivator/corepressor expression plasmids, ER subtype-specific antibodies, Reporter gene constructs | Elucidate mechanisms underlying tissue-specific responses to structurally distinct SERMs |
| Rimtuzalcap | Rimtuzalcap, CAS:2167246-24-2, MF:C18H24F2N6O, MW:378.4 g/mol | Chemical Reagent |
| Rivipansel | Rivipansel | Rivipansel is a pan-selectin inhibitor for research into sickle cell disease (SCD) and vaso-occlusive crisis (VOC) mechanisms. For Research Use Only. Not for human consumption. |
STR-Driven Experimental Workflow
This case study demonstrates that slight structural modifications in SERMs can dramatically alter their tissue exposure and selectivity profiles without significantly affecting plasma pharmacokinetics [14] [5]. The integration of STR assessment into standard drug optimization workflows provides a powerful approach to select clinical candidates with improved efficacy/toxicity balances.
Future directions in STR research include:
- Development of computational models to predict tissue exposure based on structural features
- Exploration of novel SERM scaffolds with improved tissue selectivity profiles
- Investigation of transport mechanisms governing tissue-specific SERM distribution
- Application of STR principles to other drug classes beyond hormone receptor modulators
The systematic evaluation of Structure–Tissue exposure/selectivity relationships represents a paradigm shift in drug development, moving beyond traditional SAR to optimize tissue-level distribution for enhanced therapeutic outcomes.
From Theory to Lab: Methodological Approaches for STR Analysis
In contemporary drug discovery, the structure–tissue exposure/selectivity relationship (STR) has emerged as a critical complement to the traditional structure–activity relationship (SAR) for selecting viable drug candidates [6] [15]. While SAR focuses on improving drug potency and specificity through structural modification, STR addresses how these modifications alter a compound's distribution profile between target and non-target tissues—a factor directly correlated with clinical efficacy and safety [20] [21]. The pharmaceutical industry's high clinical failure rate (approximately 90%) is partly attributable to an overreliance on plasma pharmacokinetics while overlooking tissue-specific exposure [6] [15]. This application note details key assays, with emphasis on liquid chromatography-tandem mass spectrometry (LC-MS/MS) methodologies and complementary approaches, for comprehensive tissue exposure profiling within the integrated STR-SAR framework essential for informed lead optimization.
Table 1: Key STR Findings from Recent Studies
| Compound Class | Key STR Finding | Clinical Impact | Citation |
|---|---|---|---|
| CBD Carbamates | L2 and L4 had similar plasma exposure but 5-fold difference in brain exposure | Direct correlation with efficacy/toxicity profile despite similar plasma PK | [6] [20] |
| Selective Estrogen Receptor Modulators (SERMs) | Slight structural modifications significantly altered tissue selectivity without changing plasma exposure | Correlation with clinical efficacy/safety profiles in target tissues | [15] [21] |
| Covalent Inhibitors | Uncoupling of drug concentration and effect due to irreversible target binding | Necessitates specialized PK/PD models for accurate efficacy prediction | [22] |
Core LC-MS/MS Methodologies for Tissue Exposure Quantification
Fundamental LC-MS/MS Workflow and Instrumentation
Liquid chromatography-mass spectrometry (LC-MS) has become the cornerstone analytical technique for tissue exposure profiling due to its high sensitivity, specificity, and ability to detect a broad spectrum of analytes in complex biological matrices [23]. The fundamental workflow involves tissue homogenization, metabolite extraction, chromatographic separation, and mass spectrometric detection [24]. Modern advancements include ultra-high-performance liquid chromatography (UHPLC) systems coupled with high-resolution mass spectrometers (HRMS) such as quadrupole-time of flight (Q-TOF), Orbitrap, and triple quadrupole (QQQ) instruments, which provide the rapid analysis times (2-5 minutes per sample) and precision required for high-throughput drug development pipelines [23].
Figure 1: Comprehensive LC-MS/MS Workflow for Tissue Exposure Profiling
Advanced LC-MS/MS Applications in Tissue Exposure Studies
Untargeted Metabolomics for Comprehensive Exposure Assessment
Untargeted metabolomics using LC-MS provides extensive coverage of metabolite detection, which is crucial for understanding both drug distribution and resulting metabolic perturbations. As demonstrated in zebrafish models, an integrated approach combining hydrophilic interaction liquid chromatography (HILIC) and reversed-phase liquid chromatography (RPLC) maximizes metabolite detection breadth [24]. Key parameters requiring optimization include tissue homogenization techniques, extraction solvents, and redissolution solvents. This method enabled annotation of 620 metabolites and identification of 110 differential variables related to zebrafish growth, primarily associated with glycerophospholipid metabolism and amino acid biosynthesis pathways [24].
Targeted Quantification for Precise PK/PD Modeling
Targeted LC-MS/MS assays, particularly using multiple reaction monitoring (MRM) on triple quadrupole instruments, provide the sensitivity and specificity required for precise quantification of drug candidates in specific tissues. In studies of CBD carbamates, a validated UPLC-HRMS method demonstrated that compounds with similar plasma exposure (L2 and L4) showed markedly different brain distribution, directly impacting their efficacy and safety profiles [6] [20]. This approach enables calculation of critical STR parameters such as tissue-to-plasma distribution coefficients (Kp), which determine overall drug exposure in tissues according to the relationship: Drug exposure in tissue = Drug exposure in plasma × Kp [6].
Table 2: Quantitative Tissue Exposure Data for CBD Carbamates
| Compound | Plasma AUC | Brain AUC | Brain-to-Plasma Ratio (Kp) | BuChE ICâ‚…â‚€ | Acute Oral Toxicity (LDâ‚…â‚€) |
|---|---|---|---|---|---|
| CBD (L0) | Reference | Reference | Reference | Reference | 319.5 mg/kg |
| L1 | Low | Low | Moderate | Similar to CBD | 22.1 mg/kg |
| L2 | High | High | High | 0.077 μM | 70.5 mg/kg |
| L3 | Low | Low | Moderate | Similar to CBD | 80.0 mg/kg |
| L4 | High | Low | Low | Most potent | 84.0 mg/kg |
Complementary and Emerging Assay Technologies
Intact Protein MS for Covalent Drug-Target Engagement
For covalent drugs that form irreversible bonds with their targets, traditional LC-MS/MS approaches face limitations due to the uncoupling of free drug concentration and pharmacological effect [22]. Intact protein mass spectrometry addresses this challenge by directly quantifying target engagement (%TE) through measurement of the drug-protein complex. This method has been applied successfully to targets including KRAS, BTK, and SOD1, with a typical workflow involving protein extraction from tissues (e.g., via chloroform/ethanol partitioning), LC separation of intact protein, and high-resolution mass detection [22].
Figure 2: Intact Protein MS Workflow for Covalent Drug Tissue Exposure
LC-MS-Based Proteomics for Mechanistic Insights
LC-MS-based proteomics provides complementary value to tissue exposure studies by mapping protein-level alterations in response to drug treatment, thereby elucidating mechanisms of efficacy and toxicity [25]. Both label-free and label-based quantification methods can identify dysregulated pathways and potential biomarkers in tissues following drug exposure. For example, this approach has revealed how natural products like berberine directly bind to PKM2 to modulate colorectal cancer pathways, and how Withaferin A regulates proteins in prostate cancer models [25]. The technology encompasses various workflows including bottom-up proteomics, top-down proteomics, and data-independent acquisition (DIA), with selection dependent on specific research questions regarding tissue responses to drug exposure.
Experimental Protocols for Comprehensive Tissue Exposure Assessment
Protocol: Tissue Sample Preparation and Metabolite Extraction for Untargeted LC-MS
This protocol optimizes tissue preparation for comprehensive metabolite extraction, adapted from zebrafish whole-tissue metabolomics methodology [24].
Reagents and Materials:
- Pre-chilled methanol (MeOH) and acetonitrile (ACN) (HPLC grade)
- Water (HPLC grade)
- Ceramic or glass homogenizers
- Cold phosphate-buffered saline (PBS)
- Dry ice or liquid nitrogen
- Microcentrifuge tubes
Procedure:
- Tissue Homogenization: Rapidly harvest tissue and immediately freeze in liquid nitrogen. Weigh approximately 50 mg of tissue and add to 500 μL of pre-chilled MeOH:ACN (1:1 v/v) in a homogenizer. Homogenize on ice until fully dispersed.
- Metabolite Extraction: Transfer homogenate to a microcentrifuge tube. Add 500 μL of pre-chilled ACN, vortex vigorously for 60 seconds, and incubate at -20°C for 60 minutes.
- Protein Precipitation: Centrifuge at 14,000 × g for 15 minutes at 4°C. Carefully collect supernatant and transfer to a new tube.
- Sample Concentration: Evaporate solvent under a gentle nitrogen stream at room temperature.
- Sample Reconstitution: Reconstitute dried extract in 100 μL of ACN:water (1:1 v/v) appropriate for either RPLC or HILIC analysis. Vortex for 30 seconds and centrifuge at 14,000 × g for 10 minutes before LC-MS analysis.
Critical Parameters:
- Maintain samples at 4°C or below throughout extraction when possible
- Use antioxidant additives (e.g., ascorbic acid) for oxidation-sensitive metabolites
- Process quality control (QC) samples by pooling aliquots from all samples
Protocol: Intact Protein MS for Target Engagement Quantification
This protocol details the measurement of target engagement for covalent drugs in tissue samples, based on published methodologies for SOD1-targeting compounds [22].
Reagents and Materials:
- Chloroform and ethanol (HPLC grade)
- Protein precipitation plates or tubes
- Immunoprecipitation reagents (antibody against target protein)
- Intact protein LC-MS column (e.g., C4 or C8 for large proteins)
- Formic acid (MS grade)
Procedure:
- Protein Extraction from Tissue: Homogenize approximately 20 mg tissue in 200 μL of ice-cold PBS. Add 400 μL of chloroform:ethanol (2:1 v/v) solution, vortex for 60 seconds, and incubate on ice for 15 minutes.
- Partitioning: Centrifuge at 10,000 × g for 10 minutes at 4°C. Collect the interphase layer containing proteins.
- Protein Purification: Wash protein pellet with cold ethanol and centrifuge again. Resuspend in appropriate LC-MS compatible buffer.
- LC-MS Analysis: Inject onto LC-MS system with C4 or C8 column. Use gradient elution with water-ACN containing 0.1% formic acid. MS detection in full scan mode with appropriate mass range for target protein and drug-protein complex.
- Data Analysis: Deconvolute mass spectra to determine relative abundances of unmodified and drug-bound protein. Calculate %TE using the formula: %TE = (Intensity of drug-protein complex / Total protein intensity) × 100.
Critical Parameters:
- Optimize extraction protocol for specific protein target
- Include controls from untreated animals
- Use high-resolution MS for accurate mass determination of large proteins
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents for Tissue Exposure Assays
| Reagent Category | Specific Examples | Function in Tissue Exposure Profiling | Application Notes |
|---|---|---|---|
| Chromatography Columns | HILIC, RPLC (C18, C8), Intact Protein (C4) | Separation of analytes from complex tissue matrices | HILIC for polar metabolites; RPLC for non-polar compounds; C4 for intact proteins |
| Ionization Sources | Electrospray Ionization (ESI), Atmospheric Pressure Chemical Ionization (APCI) | Generation of gas-phase ions for mass analysis | ESI for polar and larger molecules; APCI for less polar compounds |
| Mass Analyzers | Q-TOF, Orbitrap, Triple Quadrupole (QQQ) | Mass separation and detection | Q-TOF/Orbitrap for untargeted; QQQ for targeted quantification |
| Internal Standards | Stable isotope-labeled analogs of analytes | Correction for matrix effects and extraction efficiency | Essential for accurate quantification in complex tissues |
| Protein Extraction Kits | Chloroform/ethanol-based precipitation, Immunoprecipitation kits | Isolation of target proteins from tissue homogenates | Critical for intact protein MS and target engagement studies |
| Quality Controls | Pooled tissue QC samples, process blanks | Monitoring analytical performance and data quality | Identify technical variations and maintain platform stability |
| Rovatirelin | Rovatirelin | Rovatirelin is a novel thyrotropin-releasing hormone (TRH) analog for research on spinocerebellar degeneration and ataxia. For Research Use Only. Not for human consumption. | Bench Chemicals |
| RQ-00203078 | RQ-00203078 is a highly selective, orally active TRPM8 antagonist (IC50=8.3 nM). For research use only. Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
Comprehensive tissue exposure profiling through LC-MS/MS and complementary technologies provides indispensable data for understanding the structure-tissue exposure/selectivity relationship (STR) in drug development [6] [15] [20]. The case studies presented demonstrate that drug exposure in plasma frequently fails to predict exposure in target tissues, and that tissue exposure/selectivity shows stronger correlation with clinical efficacy and safety outcomes [6] [21]. By integrating STR assessment with traditional SAR during lead optimization, drug developers can make more informed candidate selection decisions, potentially improving the success rate of clinical drug development through better balancing of efficacy and toxicity profiles [15] [20]. The protocols and methodologies detailed in this application note provide a framework for implementing robust tissue exposure profiling in preclinical drug development workflows.
Leveraging ADMET Parameters to Predict Tissue Selectivity
The Structure–Tissue Exposure/Selectivity Relationship (STR) is an emerging critical concept in drug optimization that complements the traditional Structure–Activity Relationship (SAR). While SAR focuses on improving a compound's potency and specificity against its molecular target, STR emphasizes the crucial link between a drug's chemical structure, its resulting absorption, distribution, metabolism, excretion, and toxicity (ADMET) properties, and its ultimate exposure and selectivity in target tissues versus off-target tissues [5] [6]. Overemphasis on plasma exposure and insufficient attention to tissue-level distribution is a significant contributor to the high failure rate (∼90%) in clinical drug development, often due to a lack of efficacy (40-50%) or unmanageable toxicity (30%) [26] [6]. This application note details how the strategic application of in silico and in vitro ADMET parameters can be leveraged to predict tissue selectivity early in the drug discovery process, thereby de-risking candidate selection and improving the probability of clinical success.
The STR Framework: Integrating ADMET for Tissue-Level Prediction
The core premise of STR is that drug exposure in plasma is not always correlated with exposure in disease-targeted tissues [5] [6]. Consequently, a drug candidate with favorable plasma pharmacokinetics may still fail if it does not adequately reach the target site or if it accumulates in sensitive normal tissues, leading to toxicity.
The following diagram illustrates the integrated workflow for applying ADMET predictions to assess tissue selectivity within the STR framework.
Key Principle: Drug exposure in a specific tissue is a function of its plasma exposure and the tissue-to-plasma distribution coefficient (Kp), as defined by the equation: Drug exposure in tissue = Drug exposure in plasma × Kp [6]. ADMET parameters are instrumental in predicting both components of this equation.
Key ADMET Parameters for Predicting Tissue Selectivity
The following parameters, often predicted using machine learning (ML) models or measured in vitro, provide critical insights into a compound's likely tissue distribution profile [27] [28].
Table 1: Key ADMET Parameters for Tissue Selectivity Assessment
| ADMET Parameter | Description | Utility in Predicting Tissue Selectivity | Common Predictive Models |
|---|---|---|---|
| Passive Permeability (e.g., Caco-2, PAMPA) | Measures passive diffusion across membranes. | Predicts ability to cross tissue barriers (e.g., intestinal wall, blood-brain barrier). | Graph Neural Networks (GNNs), Support Vector Machines (SVM) [27] [28] |
| Transporter Affinity (e.g., P-gp, BCRP) | Identifies substrates of efflux transporters. | Flags compounds likely to be excluded from specific tissues (e.g., brain) or accumulated in eliminating organs. | Random Forest, Deep Neural Networks [28] |
| Plasma Protein Binding (PPB) | Quantifies the fraction of drug bound to plasma proteins. | Influences the volume of distribution and free drug available for tissue partitioning. High PPB can enhance tumor accumulation via the EPR effect [5]. | Multitask Learning Models, AdmetSAR [26] [28] |
| Tissue-to-Plasma Partition Coefficient (Kp) | Predicts equilibrium concentration ratio between tissue and plasma. | Directly quantifies a compound's tendency to distribute into and accumulate in specific tissues. | Physiologically-Based Pharmacokinetic (PBPK) modeling, ensemble ML methods [6] [28] |
| Metabolic Stability (e.g., in liver microsomes) | Measures the rate of compound metabolism. | Impacts overall systemic exposure (AUC) and, consequently, tissue exposure levels. | Deep Learning (e.g., CNNs, RNNs) on structural data [29] [30] [28] |
| hERG Inhibition | Predicts potential for cardiac channel blockage. | Serves as a proxy for cardiac tissue exposure and associated toxicity risk. | ADMET-AI, admetSAR, TEST [31] [26] |
Experimental Protocols for STR-Driven ADMET Profiling
Protocol: IntegratedIn SilicoADMET Screening for Tissue Selectivity
This protocol utilizes a consensus-based cheminformatics approach to generate an initial STR hypothesis [26].
Input Structure Preparation:
- Generate and optimize 3D structures of candidate compounds.
- Convert structures into SMILES notation or appropriate molecular descriptor formats.
Multi-Platform In Silico Profiling:
- Utilize a panel of at least 3-5 distinct software/platforms (e.g., SwissADME, admetSAR, AdmetLab, pkSCM) to predict the parameters listed in Table 1 [26].
- Rationale: Using multiple platforms mitigates individual tool bias and provides a more robust consensus.
Data Consolidation and Analysis:
- Compile results into a unified database.
- Apply a scoring system to classify compounds as high, medium, or low risk for each parameter. For instance, a compound predicted as a strong P-gp substrate by >60% of platforms would be flagged as high risk for poor brain penetration.
STR Hypothesis Generation:
- Integrate the ADMET scores to formulate a tissue selectivity profile. For example, a compound with high passive permeability, low P-gp substrate probability, and high predicted Kp_brain is a strong candidate for central nervous system (CNS) targets.
Protocol:In VitroValidation of Tissue Distribution
This protocol outlines the key experimental steps to validate in silico predictions, using a preclinical model as an example [32].
Animal Dosing and Sample Collection:
- Model: Use a relevant disease model (e.g., patient-derived orthotopic xenograft model).
- Dosing: Administer the candidate drug(s) via the intended clinical route (e.g., oral gavage).
- Sacrifice and Collection: Euthanize animals at predetermined time points. Collect blood (for plasma), target tissue (e.g., tumor, brain), and potential toxicity-related tissues (e.g., liver, heart).
Bioanalytical Quantification:
Data Calculation and STR Assessment:
- Calculate key pharmacokinetic parameters (AUC) for plasma and each tissue.
- Determine the tissue-to-plasma distribution coefficient (Kp) using the formula: Kp = AUCtissue / AUCplasma.
- Calculate the Tissue Selectivity Index (TSI) for efficacy versus toxicity: TSI = Kptargettissue / Kptoxictissue. A higher TSI indicates a more favorable STR profile.
The following diagram summarizes this key experimental and analytical workflow.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Reagents and Tools for ADMET and STR Studies
| Tool / Reagent | Function / Application | Example Use in STR Context |
|---|---|---|
| Caco-2 Cell Line | Model of human intestinal permeability. | Predicts oral absorption and potential for systemic exposure [28]. |
| MDCK or MDCK-MDR1 Cells | Canine kidney cells; latter transfected with human P-gp. | Assesses permeability and identifies P-gp efflux transporter substrates, predicting brain penetration [26]. |
| Human Liver Microsomes | Contains major human cytochrome P450 enzymes. | Evaluates metabolic stability, informing systemic and tissue half-life [29]. |
| T.E.S.T. (Toxicity Estimation Software) | EPA-developed software for toxicity prediction. | Provides early warnings for tissue-specific toxicities (e.g., mutagenicity, hepatotoxicity) [26]. |
| ADMET-AI / admetSAR | Machine learning platforms for ADMET prediction. | High-throughput in silico screening of key parameters like PPB, hERG, and solubility [31] [26]. |
| UPLC-HRMS / LC-MS/MS | High-sensitivity bioanalytical instrumentation. | Quantifies drug concentrations in complex matrices like tissue homogenates for Kp calculation [6] [32]. |
| Zalunfiban | Zalunfiban (RUC-4) | Zalunfiban is a novel subcutaneously administered GPIIb/IIIa inhibitor for STEMI research. This product is for Research Use Only (RUO). Not for human use. |
| Runcaciguat | Runcaciguat|sGC Activator for CKD Research | Runcaciguat is a novel, orally active sGC activator for chronic kidney disease (CKD) research. It restores cGMP signaling under oxidative stress. For Research Use Only. Not for human use. |
Integrating ADMET parameter analysis to predict tissue selectivity is no longer an optional refinement but a necessary component of modern, efficient drug optimization. By adopting the STR framework and employing the described protocols and tools—from consensus in silico screening to targeted in vivo validation—researchers can make more informed decisions during lead optimization. This paradigm shift from a primary focus on plasma exposure to a comprehensive understanding of tissue-level exposure and selectivity holds significant promise for improving the clinical success rate of drug candidates by achieving a better balance between efficacy and safety.
The Structure–Tissue Exposure/Selectivity Relationship (STR) represents a critical paradigm in modern drug development, emphasizing that a drug's distribution profile across different tissues is a deterministic factor for its clinical efficacy and safety [5]. Traditional drug optimization has heavily focused on the Structure–Activity Relationship (SAR) to enhance potency and specificity. However, an overemphasis on SAR often overlooks a crucial reality: drugs with similar plasma exposure can have vastly different distributions in target versus non-target tissues, leading to unexpected clinical outcomes [6] [5] [20]. Integrating STR analysis ensures that drug candidate selection balances both pharmacological activity and tissue-specific exposure, thereby improving the probability of success in clinical trials.
The fundamental principle of STR is that slight structural modifications can significantly alter a compound's tissue exposure and selectivity, independent of its plasma pharmacokinetics. For instance, studies on selective estrogen receptor modulators (SERMs) with similar structures and identical molecular targets demonstrated that nearly identical plasma exposure did not correlate with exposure in target tissues like tumors, fat pads, bone, or the uterus. Instead, the tissue exposure/selectivity profiles were directly correlated with observed clinical efficacy and safety [5]. This underscores the necessity of incorporating tissue-level distribution data early in the lead optimization process.
The Critical Role of Animal Models in STR-Driven Research
Advancements in Modern Animal Models
Animal models remain indispensable for studying STR because they provide a complex, integrated whole-organism context that is currently impossible to replicate with in vitro or computational systems alone [33] [34]. Modern biomedical research utilizes a variety of sophisticated animal models to predict human responses more accurately. These models have evolved beyond traditional wild-type or spontaneously mutant species to include genetically engineered, humanized, and naturalized systems that better emulate human physiology and disease [34].
Key advancements include:
- Humanized mouse models: Mice are engineered to carry human genes, cells, or even tissues, allowing for the direct study of human biology within a living organism [33]. For example, humanized mice carrying human immune cells were pivotal in uncovering the causes of severe toxicities associated with CAR T-cell immunotherapy, leading to safer clinical trials [33].
- Naturalized mouse models: These models move beyond ultra-clean laboratory conditions by exposing mice to diverse environmental factors and microbes. This results in immune systems that more closely resemble those of humans, improving the predictivity of preclinical testing for immune-related diseases like rheumatoid arthritis and inflammatory bowel disease [33].
- Genetically modified larger animals: Models such as genetically engineered pigs, where harmful animal genes are removed and human genes are added, show great promise for applications like organ transplantation and the study of complex human diseases [33].
Selecting the Appropriate Animal Model
The selection of an appropriate animal model is a critical strategic decision. According to a comprehensive review of gene therapy products, animal models can be broadly categorized, and the choice should be guided by the research objective [34]. The following table outlines common categories of animal models used in preclinical research:
Table 1: Categories of Animal Models for Preclinical Research
| Model Category | Description | Key Applications in STR |
|---|---|---|
| Disease Induction | Animals are manipulated to replicate specific disease states. | Studying drug exposure in artificially created target tissues. |
| Xenograft | Human cells, tissues, or tumors are transplanted into immunodeficient animals. | Evaluating drug targeting and exposure in human-derived tissue contexts. |
| Genetically Engineered | The animal's genetic composition is altered by mutating, deleting, or overexpressing genes. | Modeling human genetic diseases and studying tissue-specific exposure in a relevant pathophysiology. |
| Spontaneous/Natural Occurrence | Animals that naturally develop a disease without deliberate manipulation. | Observing STR in a naturally progressing disease environment with high clinical relevance. |
The principle of analogical reasoning guides model selection; researchers leverage qualitative similarities between the model and humans to forecast causal relationships [34]. A rigorous selection process, considering factors like physiological similarity, availability, and ethical considerations, is essential to avoid inefficient resource allocation and generation of unreliable data [34].
Integrating STR with Advanced Sampling Methodologies
The Principle of Stratified Sampling in Experimental Design
In the context of STR-driven experiments, stratified sampling is a powerful statistical method that enhances the reliability and accuracy of preclinical studies. This technique involves dividing the entire experimental population (e.g., a colony of animal models) into homogeneous subgroups, known as strata, before sampling [35] [36]. The goal is to ensure that the sample accurately represents the heterogeneity of the entire population with respect to key characteristics that could influence tissue exposure, such as genetic background, metabolic profile, or disease severity [35] [37].
The process typically follows these steps:
- Define the population: Clearly identify the entire group of animal models to be studied.
- Choose stratification variables: Select characteristics relevant to the research question (e.g., age, gender, genotype, microbiome profile).
- Divide the population into strata: Create mutually exclusive and collectively exhaustive subgroups based on the chosen variables.
- Determine sample sizes: Decide on the number of subjects to be selected from each stratum, using either proportional or disproportionate allocation.
- Randomly select participants: Use random sampling within each stratum to form the final experimental sample [35].
This method reduces sampling error and variance, leading to more precise estimates of treatment effects and more generalizable conclusions about STR [36].
Stratified Sampling Strategies: Proportional vs. Disproportionate
Two primary allocation strategies are used in stratified sampling, each with distinct advantages for STR studies:
Table 2: Comparison of Stratified Sampling Allocation Strategies
| Strategy | Description | Best Use Cases in STR Research |
|---|---|---|
| Proportional Allocation | The sample size from each stratum is proportional to the stratum's size in the overall population. | General population inference; when the goal is to understand average tissue exposure across the entire model population. |
| Disproportionate (Optimum) Allocation | The sample size from each stratum is not proportional to the population. It may be increased for smaller strata or those with higher variability. | - Focusing on small but critical subgroups (e.g., a rare genotype).- When strata are known to have high variance in drug metabolism.- Ensuring sufficient statistical power for all analyzed subgroups [35] [36]. |
For instance, in a study using naturalized mice with diverse microbiomes, a researcher might use disproportionate allocation to oversample mice with specific microbial profiles that are less common but critical for understanding immune-related toxicities. This ensures that the analysis of tissue exposure in this key subgroup is statistically robust [33] [35].
Detailed Experimental Protocols for STR Analysis
Protocol 1: Assessing STR Using a Case Study of CBD Carbamates
This protocol is adapted from a study investigating CBD carbamates as butyrocholinesterase (BuChE) inhibitors for central nervous system (CNS) applications [6] [20]. It provides a template for evaluating how structural changes influence tissue exposure and selectivity.
Objective: To determine the STR of a series of cannabidiol (CBD) carbamates by correlating slight structural differences with their plasma exposure, brain exposure (target tissue), and associated efficacy/toxicity.
Materials and Reagents:
- Test Compounds: A series of CBD carbamates (e.g., L1, L2, L3, L4) with variations in the amine group of the carbamate moiety [6].
- Animal Model: Rats (e.g., Sprague-Dawley), stratified by weight and age to minimize metabolic variability.
- Analytical Instrumentation: UPLC-HRMS (Ultra-Performance Liquid Chromatography–High Resolution Mass Spectrometer) for precise drug quantification in biological matrices.
- Software: ADMET prediction software for preliminary toxicity and pharmacokinetic profiling.
Methodology:
- Dosing and Sample Collection:
- Administer a single oral dose of each CBD carbamate (L1-L4) and parent CBD (L0) to groups of stratified rats.
- Collect blood plasma and tissue samples (e.g., brain, liver) at multiple time points post-administration to establish a concentration-time profile.
Bioanalysis:
- Use the validated UPLC-HRMS method to quantify the concentration of each drug in the plasma and tissue homogenates.
- Calculate key pharmacokinetic parameters: AUCplasma (Area Under the Curve in plasma), AUCtissue (AUC in tissue), and the tissue-to-plasma distribution coefficient (Kp).
Efficacy and Toxicity Correlation:
- Corrogate the tissue exposure data with in vitro efficacy data (e.g., IC50 for BuChE inhibition).
- Correlate exposure in non-target tissues (e.g., liver) with preclinical toxicity endpoints such as acute oral toxicity (LD50) predicted or measured via ADMET parameters.
Key Workflow Diagram: STR Analysis of CBD Carbamates
Protocol 2: Implementing Stratified Sampling in a Preclinical Study
This protocol outlines how to integrate stratified sampling into the design of a preclinical experiment to ensure robust and generalizable STR data.
Objective: To ensure that experimental groups in a preclinical STR study are balanced across key subpopulations, thereby reducing variance and improving the reliability of tissue exposure estimates.
Materials and Reagents:
- Experimental Population: A colony of animal models (e.g., genetically diverse or humanized mice).
- Data Source: Pre-existing data on the animals (e.g., metabolic rate, immune profile, genomic data).
- Tools: Random number generation software or a platform with built-in stratification algorithms (e.g., Statsig) [37].
Methodology:
- Define Strata:
- Identify the population for the study (e.g., all available mouse IDs).
- Choose a stratification variable highly relevant to the drug's pharmacokinetics (e.g., "high" vs. "low" metabolizer phenotype based on pre-experiment data).
Allocate and Randomize:
- Choose between proportional or disproportionate allocation based on the research goal (see Table 2).
- Use a computational method to evaluate multiple random assignment plans (salts). Select the salt that produces the most balanced groups across the defined strata for the critical metric [37].
- Randomly assign animals within each stratum to the control or treatment group using the selected salt.
Conduct Experiment and Analyze:
- Proceed with the dosing and tissue collection as outlined in Protocol 1.
- During analysis, account for the stratified design to correctly compute the standard error of the mean estimates, which is typically lower than that from a simple random sample [36].
Key Workflow Diagram: Stratified Sampling Implementation
The Scientist's Toolkit: Essential Reagents and Models
The following table details key materials and their functions for conducting STR-driven experiments.
Table 3: Research Reagent Solutions for STR-Driven Experiments
| Tool/Reagent | Function in STR Research |
|---|---|
| Humanized Mouse Models | Provides an in vivo system with human biological components (genes, cells, tissues) to directly study human-relevant tissue exposure and toxicity [33]. |
| UPLC-HRMS System | Enables simultaneous, highly sensitive, and accurate quantification of drugs and their metabolites in small volumes of plasma and tissue homogenates, which is crucial for building precise STR models [6] [20]. |
| ADMET Prediction Software | Provides in silico estimates of absorption, distribution, metabolism, excretion, and toxicity (ADMET) parameters early in the drug optimization process, helping to prioritize compounds for in vivo STR studies [6]. |
| Stratified Sampling Platform | Software tools that automate the process of creating balanced experimental groups based on pre-specified covariates, reducing variance and improving the statistical power of preclinical studies [35] [37]. |
| Organ-on-a-Chip Models | Microfluidic devices lined with living human cells that model human organ functionality. These can be used as a complementary tool to animal models for preliminary assessment of tissue-specific drug effects and toxicity in a human-relevant system [38]. |
| Hh-Ag1.5 | Hh-Ag1.5, MF:C28H26ClF2N3OS, MW:526.0 g/mol |
| SAHA-BPyne | SAHA-BPyne, MF:C27H31N3O5, MW:477.6 g/mol |
The integration of STR-driven analysis with advanced animal models and rigorous sampling methodologies represents a holistic strategy to de-risk drug development. By shifting the focus from plasma exposure alone to a comprehensive understanding of tissue-specific exposure and selectivity, researchers can make more informed decisions during lead optimization. Employing humanized or naturalized animal models increases the translational relevance of preclinical findings, while stratified sampling ensures that the data generated is robust and reproducible. Adopting this integrated framework, which balances SAR and STR, is paramount for selecting superior drug candidates with an optimal balance of efficacy and safety, ultimately improving the success rate of clinical trials.
The tissue-to-plasma partition coefficient (Kp) is a critical pharmacokinetic parameter that quantifies drug distribution into specific tissues relative to plasma. Accurately determining Kp values is essential for predicting drug exposure at the site of action, understanding potential tissue-specific toxicity, and improving the success rate of drug candidates in clinical trials [39] [5]. This Application Note provides a comprehensive overview of the theoretical frameworks, experimental methodologies, and modern computational approaches for calculating Kp, contextualized within the structure-tissue exposure/selectivity relationship (STR) paradigm vital for modern drug optimization.
In drug discovery, the structure–tissue exposure/selectivity relationship (STR) investigates how structural modifications influence a drug's distribution profile and its subsequent efficacy and safety [5] [6]. A core component of STR is the tissue-to-plasma partition coefficient (Kp), defined as the ratio of the drug concentration in a tissue to its concentration in plasma at steady state.
The unbound Kp (Kpu) is particularly informative, as it describes the partition of the pharmacologically active, unbound drug and is governed solely by the net clearance into (CLin) and out of (CLout) the tissue [40]: Kp,uu = CLin / CLout = Cu,tissue / Cu,plasma
Drug optimization has traditionally focused on plasma exposure and the structure-activity relationship (SAR). However, evidence shows that drug exposure in plasma is not always correlated with exposure in target tissues [5] [6]. For instance, two cannabidiol carbamates (L2 and L4) showed similar plasma exposure but a five-fold difference in brain exposure, which was directly correlated with their efficacy and safety profiles [6]. Therefore, integrating Kp and STR into the lead optimization process is crucial for selecting candidates with optimal tissue exposure/selectivity.
Theoretical and Mechanistic Models for Kp Prediction
Mechanistic models predict Kp based on a drug's physicochemical properties and the composition of tissues. These models are vital for Physiologically Based Pharmacokinetic (PBPK) modeling.
The Rodgers & Rowland Model
This method differentiates its approach based on the compound's ionization [41]. It uses inputs such as lipophilicity (log P), pKa, fraction unbound in plasma (fu,p), and binding data to acidic phospholipids to estimate Kp for various tissues [41]. A key feature is its use of drug partitioning into erythrocytes to parameterize the interaction of bases with acidic phospholipids [41].
A Unified Mechanistic Model
This model provides a universal framework for neutral, acidic, basic, or zwitterionic compounds [42]. It calculates the unbound fraction in tissue by considering the tissue's composition—water, neutral lipids, phospholipids, and proteins—and the drug's specific interactions with these components [42]. The model is mechanistically transparent and shows good performance, with 73% of predicted Kp values falling within a 3-fold deviation of experimental values [42].
The Membrane-Based (Kp,mem) Method
This newer method uses the fraction unbound in microsomes (fum), plasma protein binding, and log P to predict unbound Kp (Kpu) [41]. An advantage is that fum data is often generated early in discovery for clearance prediction, providing a mechanistically sound basis for membrane partitioning [41]. This method predicted the steady-state volume of distribution (Vss) within a 2-fold error for 12 out of 19 drugs [41].
Table 1: Comparison of Mechanistic Kp Prediction Models
| Model Name | Key Input Parameters | Applicability | Key Features |
|---|---|---|---|
| Rodgers & Rowland [41] | log P, pKa, fu,p, erythrocyte partitioning | Acids, neutrals, weak bases, moderate-to-strong bases | Differentiates equations for different compound classes; accounts for acidic phospholipids. |
| Unified Mechanistic Model [42] | log P, pKa, fu,p, phospholipid binding | Neutral, acidic, basic, multiply charged compounds | Universally applicable; based on direct binding to explicit tissue constituents. |
| Membrane-Based (Kp,mem) [41] | fum, fu,p, log P | Diverse set of acids, bases, and neutrals | Uses microsomal binding data; facilitates transition to advanced PBPK models. |
Machine Learning-Driven QSPKR Modeling
Beyond mechanistic approaches, Machine Learning (ML)-driven Quantitative Structure-Pharmacokinetic Relationship (QSPKR) models have emerged as powerful tools for Kp prediction [39].
One advanced ML-based QSPKR modeling strategy involves a two-stage approach:
- Initial Models: Predict Kp values for missing tissues based solely on the drug's structural and physicochemical properties.
- Enhanced Models: Integrate structural properties with experimentally known or initially predicted Kp values from other tissues to improve predictive accuracy [39].
This methodology has demonstrated significant improvement in predictability, with Q2F values ranging from 0.78 to 0.95 [39]. These models can also be used to screen compound libraries, and an analysis indicated that compounds with higher tissue partitioning are more likely to exhibit toxicity to that specific tissue [39]. Public tools like PKSmart further extend this capability, using molecular fingerprints and predicted animal PK data to model human pharmacokinetic parameters, achieving an external R² of 0.39 for the volume of distribution (VDss) [43].
Experimental Protocols for Kp Determination
In Vivo Kp Determination Protocol
This protocol describes the standard method for determining Kp in rodent models.
Principle: The Kp value is calculated from the ratio of the drug concentration in a tissue to the drug concentration in plasma at steady state, which can be achieved through continuous intravenous infusion or by measuring concentrations at multiple time points after a single dose to calculate the area under the curve (AUC).
Workflow: The experimental workflow for determining Kp in vivo and in vitro is summarized in the diagram below.
Materials:
- Test compound: Solution in appropriate vehicle (e.g., saline, DMSO/PEG400/saline mixture).
- Animals: Laboratory rats or mice, specific pathogen-free.
- Surgical and sampling kits: Syringes, catheters, EDTA-coated blood collection tubes, surgical instruments.
- Analytical balance, homogenizer, centrifuge, LC-MS/MS system.
Procedure:
- Dosing and Sampling: Administer the test compound to animals via a programmed intravenous infusion to achieve and maintain steady-state plasma concentrations. Alternatively, use an IV bolus and collect samples at multiple time points.
- Sample Collection: At steady state (or at designated time points), anesthetize the animal and collect a final blood sample via cardiac puncture into a heparinized tube. Immediately sacrifice the animal and rapidly dissect tissues of interest (e.g., liver, brain, kidney, muscle, fat). Gently blot tissues to remove residual blood.
- Sample Processing: Centrifuge blood to obtain plasma. Weigh each tissue and homogenize with a buffer (e.g., phosphate-buffered saline) to make a homogeneous tissue suspension.
- Bioanalysis: Quantify the total drug concentration in plasma and tissue homogenates using a validated analytical method (e.g., LC-MS/MS). Determine the fraction unbound in plasma (fu,p) and fraction unbound in tissue (fu,tissue) using equilibrium dialysis or ultrafiltration [40].
Calculations:
- Total Kp:
Kp = C_tissue / C_plasmaWhereC_tissueis the total drug concentration in tissue homogenate, andC_plasmais the total drug concentration in plasma. - Unbound Kp (Kp,uu):
Kp,uu = Kp * (fu,tissue / fu,plasma)This represents the partition coefficient for the pharmacologically active, unbound drug [40].
In Vitro Determination of Tissue Binding (fu,tissue)
Principle: The fraction unbound in tissue (fu,tissue) is determined by incubating the drug with tissue homogenate and separating the unbound drug using equilibrium dialysis.
Materials:
- Tissue homogenate (e.g., brain, liver) at a known dilution (e.g., 1:4 in PBS).
- Equilibrium dialysis device with semi-permeable membranes.
- Phosphate Buffered Saline (PBS), pH 7.4.
- Test compound, shaking incubator, LC-MS/MS.
Procedure:
- Prepare tissue homogenates from control tissues using a buffer.
- Spike the test compound into the homogenate.
- Load the spiked homogenate into one chamber of the dialysis device and buffer into the opposing chamber.
- Dialyze at 37°C with gentle shaking for a predetermined time (e.g., 4-6 hours) to reach equilibrium.
- Collect samples from both the homogenate and buffer chambers.
- Analyze the drug concentration in both chambers using LC-MS/MS.
Calculations:
fu,tissue = C_buffer / C_homogenate
Where C_buffer is the concentration in the buffer chamber (unbound drug) and C_homogenate is the concentration in the tissue homogenate chamber (total drug) after dialysis [40].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagents and Materials for Kp Studies
| Item | Function / Application | Example / Notes |
|---|---|---|
| LC-MS/MS System | High-sensitivity quantification of drug concentrations in complex biological matrices (plasma, tissue homogenates). | Essential for bioanalysis [41]. |
| Equilibrium Dialyzer | Experimental determination of fraction unbound in plasma (fu,p) and tissue (fu,tissue). | 96-well systems available for higher throughput [41]. |
| Rodent Liver Microsomes | Used to determine the fraction unbound in microsomes (fum) for the Kp,mem prediction method. | Commercially available from suppliers like BD Biosciences [41]. |
| Prediction Software & Tools | In silico prediction of Kp and other PK parameters using ML or mechanistic models. | PKSmart [43]; DTC Lab Kp Calculator [39]. |
| Physiologically-Based Pharmacokinetic (PBPK) Software | Platform for integrating predicted or experimentally determined Kp values into whole-body models to simulate drug disposition. | Used for predicting human Vss and concentration-time profiles [41]. |
| Salinazid | Salinazid, CAS:495-84-1, MF:C13H11N3O2, MW:241.24 g/mol | Chemical Reagent |
| Savoxepin mesylate | Savoxepin mesylate, CAS:79262-47-8, MF:C26H30N2O4S, MW:466.6 g/mol | Chemical Reagent |
Accurate calculation of tissue-to-plasma partition coefficients is a cornerstone of predicting a drug's tissue exposure profile. A combination of robust experimental protocols, mechanistic models, and modern machine learning approaches provides a powerful toolkit for researchers. Integrating these Kp determinations into the broader framework of the Structure-Tissue Exposure/Selectivity Relationship (STR) is no longer optional but a critical factor in selecting drug candidates with an optimal balance of efficacy and safety, thereby improving the success rate of clinical drug development [5] [6].
In contemporary drug discovery, the Structure–Tissue exposure/selectivity Relationship (STR) has emerged as a critical complement to the traditional Structure-Activity Relationship (SAR). While SAR optimizes a compound's potency and specificity for its molecular target, STR focuses on a compound's distribution and selectivity between disease-targeted tissues and normal tissues [10]. This relationship is particularly vital for central nervous system (CNS) diseases like Alzheimer's Disease (AD), where achieving sufficient drug exposure in the brain is essential for efficacy, while minimizing exposure in peripheral tissues is crucial for reducing toxicity [44] [6].
The current drug development landscape faces a significant challenge, with approximately 90% of clinical drug development failing in clinical trials [10]. A major contributing factor is that the optimization process often overemphasizes drug exposure in plasma and overlooks drug distribution in disease-targeted tissues [10] [44]. This oversight can mislead drug candidate selection, ultimately impacting the balance between clinical efficacy and toxicity [10]. For Alzheimer's Disease, with 138 drugs currently in clinical trials [45], optimizing brain exposure represents one of the most significant hurdles in developing effective therapies.
This case study explores the application of STR principles to optimize a series of cannabidiol (CBD) carbamate derivatives designed as butyrylcholinesterase (BuChE) inhibitors for Alzheimer's therapy. We demonstrate how strategic structural modifications alter brain exposure and selectivity, directly impacting predicted efficacy and safety profiles.
STR Analysis of CBD Carbamates: Quantitative Data
The following tables summarize key quantitative data for CBD and its carbamate derivatives (L1-L4), highlighting critical relationships between structure, plasma exposure, brain exposure, and biological activity.
Table 1: Pharmacokinetic and Pharmacodynamic Properties of CBD Carbamates
| Compound | AUCplasma (ng·h/mL) | AUCbrain | Brain-to-Plasma Ratio (Kp) | BuChE IC50 (μM) | AChE IC50 (μM) | Acute Oral Toxicity (LD50, mg/kg) |
|---|---|---|---|---|---|---|
| CBD | 157.5 | - | - | 0.67 ± 0.06 | 17.07 ± 2.43 | 319.5 |
| L1 | 191.2 | - | - | 0.128 ± 0.022 | 18.88 ± 1.11 | 22.1 |
| L2 | 561.4 | High | High | 0.077 ± 0.005 | 14.95 ± 1.02 | 70.5 |
| L3 | 182.1 | - | - | 0.39 ± 0.04 | No activity | 80.0 |
| L4 | 521.6 | Low | Low | 0.0053 ± 0.0012 | 21.4 ± 2.8% (Inhibition at 20 μM) | 84.0 |
| Rivastigmine | - | - | - | 0.058 ± 0.013 | 16.35 ± 1.54 | - |
Table 2: STR Correlation Analysis for Key Candidates
| Compound Pair | Plasma Exposure Relationship | Brain Exposure Relationship | Efficacy Correlation | Safety/Toxicity Correlation |
|---|---|---|---|---|
| L2 vs L4 | Similar (~1.08:1 ratio) | L2 > L4 (5-fold higher) | L4 more potent BuChE inhibitor, but L2 has better brain exposure | L2 and L4 have similar improved safety profiles over L1 |
| L1 vs Others | Lower than L2/L4 | - | Moderate BuChE inhibition | Significantly higher toxicity (lower LD50) |
| CBD vs Carbamates | Lower than L2/L4 | - | Weaker BuChE inhibition | Lower toxicity (higher LD50) |
Key STR Observations from the Data
The quantitative data reveals several critical STR principles:
Plasma and Brain Exposure Disconnect: L2 and L4 demonstrate nearly identical plasma exposure (AUCplasma ratio of 1.08:1) but markedly different brain exposure, with L2 achieving 5-fold higher brain concentrations than L4 [44] [6]. This finding directly challenges the "free drug hypothesis," which assumes that plasma exposure reliably predicts tissue exposure [10].
Structural Impact on Tissue Distribution: The amine group modification in the carbamate moiety significantly influences tissue distribution. L2 (with methylethylamine, aliphatic amine) shows superior brain penetration compared to L4 (with tert-benzylamine), despite their similar plasma profiles [44].
Efficacy-Toxicity Balance: L1 exhibits the worst toxicity profile (LD50 = 22.1 mg/kg) despite moderate BuChE inhibition, indicating that the secondary amine of carbamate may produce toxic metabolites [44] [6]. In contrast, L2 and L4 show improved safety profiles while maintaining potent BuChE inhibition.
Experimental Protocols for STR Assessment
Protocol 1: Comparative Pharmacokinetics of CBD Carbamates
Objective: To determine the pharmacokinetic profiles and tissue distribution of CBD carbamates in rodent models.
Materials:
- Test compounds: CBD, L1, L2, L3, L4
- Animal model: Female MMTV-PyMT mice (8-12 weeks old) or equivalent rodent model
- Administration: Oral (p.o.) at 5 mg/kg or intravenous (i.v.) at 2.5 mg/kg
- Sample collection: Blood, plasma, and multiple tissues (brain, bone, tumor, fat pad, uterus, heart, liver, kidney, etc.)
- Analytical instrument: UPLC-HRMS (Ultra-Performance Liquid Chromatography–High Resolution Mass Spectrometer)
Methodology:
- Dosing and Sample Collection: Administer compounds to animals and collect blood/tissue samples at predetermined time points (e.g., 0.08, 0.5, 1, 2, 4, and 7 hours post-dosing) [10].
- Sample Preparation: Aliquot plasma or tissue homogenate (40 μL) into 96-well plates. Add 40 μL of ice-cold acetonitrile and 120 μL of internal standard solution (e.g., 25 nmol/L CE302 in ACN). Vortex for 10 minutes, then centrifuge at 3500 rpm for 10 minutes at 4°C [10].
- UPLC-HRMS Analysis: Inject supernatant into UPLC-HRMS system. Use appropriate chromatographic conditions (e.g., reverse-phase column, gradient elution with water/acetonitrile containing 0.1% formic acid). Monitor specific mass transitions for each compound [44] [6].
- Data Analysis: Calculate drug concentrations in each matrix using calibration curves. Determine pharmacokinetic parameters (AUC, Cmax, Tmax, t1/2) using non-compartmental analysis. Compute tissue-to-plasma distribution coefficients (Kp) [44].
Protocol 2: BuChE Inhibitory Activity Assay
Objective: To evaluate the inhibitory potency and selectivity of CBD carbamates against butyrylcholinesterase (BuChE) and acetylcholinesterase (AChE).
Materials:
- Enzyme sources: eqBuChE (from horse serum), eeAChE (from electric eel)
- Substrate: Butyrylthiocholine iodide (for BuChE), Acetylthiocholine iodide (for AChE)
- Colorimetric reagent: 5,5'-Dithio-bis-(2-nitrobenzoic acid) (DTNB)
- Test compounds: CBD, L1, L2, L3, L4, rivastigmine (reference control)
- Buffer: 0.1 M phosphate buffer, pH 8.0
- Microplate reader capable of reading absorbance at 412 nm
Methodology:
- Enzyme Inhibition Assay: Prepare test compounds at various concentrations (typically 0.001-100 μM) in buffer. Pre-incubate compounds with enzyme solution for 15-30 minutes at 25°C [44] [6].
- Reaction Initiation: Add substrate (butyrylthiocholine iodide for BuChE, acetylthiocholine iodide for AChE) and DTNB to initiate reaction.
- Absorbance Monitoring: Measure the increase in absorbance at 412 nm over 10-15 minutes to monitor thiocholine production.
- Data Analysis: Calculate percentage inhibition at each concentration and determine IC50 values using non-linear regression analysis (e.g., log(inhibitor) vs. response -- variable slope model in GraphPad Prism) [44].
Protocol 3: Acute Toxicity Assessment
Objective: To evaluate the acute toxicity profile of CBD carbamates for preliminary safety assessment.
Materials:
- Test compounds: CBD, L1, L2, L3, L4
- Animal model: Rats or mice (appropriate strain for toxicity testing)
- Dosing apparatus: Oral gavage equipment
Methodology:
- Dose Administration: Administer single oral doses of test compounds to groups of animals at various dose levels.
- Observation Period: Monitor animals for 14 days post-administration for signs of toxicity, morbidity, and mortality.
- Data Analysis: Record mortality at each dose level and calculate LD50 values using established statistical methods (e.g., probit analysis) [44] [6].
STR-Optimized Molecular Design Strategies
Based on the STR analysis of CBD carbamates, several key design strategies emerge for optimizing brain exposure and selectivity:
Amine Group Engineering: The carbamate amine substituent significantly influences both tissue distribution and metabolic stability. Secondary amines (as in L1) show increased toxicity likely due to metabolism back to CBD, while tertiary amines (as in L4) demonstrate improved stability [44] [6]. Aliphatic amines (L1, L2) generally show better brain penetration than cyclic (L3) or aromatic (L4) amines.
Balancing Potency and Exposure: The most potent enzyme inhibitor (L4 with IC50 = 0.0053 μM against BuChE) does not necessarily make the best clinical candidate if tissue exposure is suboptimal. An ideal candidate should balance reasonable potency with favorable tissue distribution [44].
ADMET Integration in Early Optimization: Absorption, distribution, metabolism, excretion, and toxicity (ADMET) parameters should be incorporated early in the optimization process to predict STR. In vitro models predicting blood-brain barrier penetration should guide structural modifications [44] [20].
STR Workflow and Molecular Design Pathways
STR Optimization Workflow for CBD Carbamates
Molecular Design Pathways for CBD Carbamates
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for STR Studies of CBD Carbamates
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| CBD Carbamate Compounds | L1, L2, L3, L4 derivatives | Test compounds for STR relationship studies |
| Enzyme Sources | eqBuChE (equine serum), eeAChE (electric eel) | Target engagement and inhibitory activity assessment |
| Analytical Instrumentation | UPLC-HRMS (Ultra-Performance LC–High Resolution MS) | Quantitative analysis of drug concentrations in biological matrices |
| Animal Models | MMTV-PyMT mice (cancer model), Wild-type rats (PK/toxicity) | In vivo pharmacokinetic and tissue distribution studies |
| Chromatographic Materials | Reverse-phase UPLC columns (e.g., C18), Acetonitrile (LC-MS grade) | Compound separation and mass spectrometric detection |
| Toxicity Assessment Tools | Acute oral toxicity (LD50) testing protocols | Preliminary safety and toxicity profiling |
| Biochemical Assay Reagents | DTNB, Butyrylthiocholine iodide, Acetylthiocholine iodide | Enzyme inhibition activity measurements |
| Selatogrel | Selatogrel, CAS:1159500-34-1, MF:C28H39N6O8P, MW:618.6 g/mol | Chemical Reagent |
| Nesvategrast | Nesvategrast, CAS:1621332-91-9, MF:C23H27F2N5O4, MW:475.5 g/mol | Chemical Reagent |
This case study demonstrates that strategic application of STR principles enables rational optimization of CBD carbamates for improved brain exposure and therapeutic potential in Alzheimer's Disease. The key findings indicate that:
- Structural modifications to the CBD carbamate scaffold, particularly at the amine group, significantly alter tissue distribution patterns without necessarily correlating with changes in plasma exposure [44] [6].
- The disconnect between plasma and brain exposure necessitates direct measurement of tissue concentrations during candidate optimization, especially for CNS targets [10] [44].
- Successful Alzheimer's drug candidates must balance multiple parameters - target potency, brain exposure, and peripheral toxicity - rather than maximizing any single parameter [44].
Future directions for STR-driven drug optimization should include more sophisticated in vitro blood-brain barrier models for early screening, advanced computational approaches to predict tissue distribution, and integrated PK/PD modeling that incorporates tissue exposure data. As the Alzheimer's therapeutic landscape evolves with 138 drugs in clinical development [45], applying STR principles alongside SAR will be crucial for selecting candidates with the optimal balance of clinical efficacy and safety.
Navigating Pitfalls: Troubleshooting and Optimizing STR in Drug Discovery
In modern drug discovery, the Structure–Tissue Exposure/Selectivity Relationship (STR) has emerged as a critical complement to the traditional Structure–Activity Relationship (SAR). While SAR focuses on improving drug potency and specificity through structural modifications, STR describes how these chemical changes influence a compound's distribution profile across different tissues in the body [5]. This relationship directly impacts the clinical efficacy and toxicity balance, as drugs must reach adequate concentrations at their target sites while minimizing exposure to sensitive normal tissues [5] [6]. The fundamental premise of STR is that drug optimization must extend beyond plasma pharmacokinetics (PK) to understand tissue-specific exposure patterns, which frequently show poor correlation with plasma measurements alone [6] [20].
The integration of STR principles represents a paradigm shift in lead optimization strategies. Historically, drug development has overemphasized plasma exposure metrics, contributing to the persistently high failure rates (approximately 90%) in clinical development [6]. STR analysis addresses this limitation by recognizing that structural modifications not only alter plasma PK but can also significantly shift tissue exposure and selectivity [5] [6]. This comprehensive approach is particularly valuable for drugs targeting specific organs such as the central nervous system (CNS), where the blood-brain barrier creates a unique distribution environment that often diverges from plasma patterns [6].
The Critical Pitfall: Over-reliance on Plasma Pharmacokinetics
Fundamental Disconnect Between Plasma and Tissue Exposure
A primary pitfall in STR analysis is the assumption that drug exposure in plasma accurately predicts concentrations at the target site. Substantial evidence demonstrates that plasma pharmacokinetics frequently show poor correlation with tissue exposure, potentially misleading candidate selection during drug optimization [6]. This discrepancy arises because drug distribution is influenced by complex physiological factors including membrane permeability, active transport mechanisms, tissue binding, and metabolic pathways – all of which create differential distribution patterns between plasma and tissues [6].
Research on cannabidiol (CBD) carbamates provides a compelling illustration of this phenomenon. In studies of BuChE-targeted CBD carbamates, compounds L2 and L4 exhibited nearly identical plasma exposure profiles, suggesting comparable distribution based on traditional PK assessment [6] [20]. However, measurement of actual tissue concentrations revealed that L2 achieved fivefold higher brain exposure than L4 despite their plasma equivalence [6] [46] [20]. This dramatic discrepancy highlights the risk of relying solely on plasma PK data for CNS-targeted therapeutics and underscores why drugs with similar plasma profiles can demonstrate markedly different clinical efficacy and toxicity [6].
Consequences for Efficacy and Toxicity Assessment
The over-reliance on plasma PK parameters directly impacts the accuracy of efficacy and safety predictions during drug development. Tissue exposure selectivity – the differential distribution between target and off-target tissues – ultimately determines the therapeutic index and clinical viability of drug candidates [5] [6]. When plasma measurements alone guide optimization, researchers risk selecting compounds with suboptimal tissue distribution profiles, potentially advancing candidates with inadequate target engagement or unacceptable toxicity risks [6].
The relationship between tissue exposure and clinical outcomes is particularly evident in the case of selective estrogen receptor modulators (SERMs). Research demonstrates that drug plasma exposure does not correlate with drug exposure in target tissues such as tumors, fat pads, bone, and uterus [5]. Instead, tissue exposure selectivity directly correlates with observed clinical efficacy and safety profiles [5]. Even slight structural modifications among SERMs with similar plasma exposure resulted in significantly different tissue distribution patterns, ultimately impacting their clinical performance [5].
Table 1: Case Study - Disconnect Between Plasma and Brain Exposure of CBD Carbamates
| Compound | Plasma AUC | Brain AUC | Brain-to-Plasma Ratio | BuChE ICâ‚…â‚€ |
|---|---|---|---|---|
| L2 | High | High | High | 0.077 μM |
| L4 | High | Low | Low | More potent than L2 |
The Challenge of Kp Interpretation and Calculation
Understanding the Tissue-to-Plasma Distribution Coefficient (Kp)
The tissue-to-plasma distribution coefficient (Kp) serves as a fundamental parameter in STR analysis, representing the ratio of drug concentration in a specific tissue to its concurrent concentration in plasma [6]. Mathematically, this relationship is expressed as:
Drug exposure in tissue = Drug exposure in plasma × Kp [6]
While this formula appears straightforward, its practical application presents significant challenges. Kp values are influenced by multiple physicochemical and physiological factors, including a compound's lipophilicity, ionization state, protein binding, and affinity for tissue components [6]. Additionally, active transport processes at tissue barriers can further complicate Kp interpretation, as these biological mechanisms may create distribution patterns that deviate from passive diffusion predictions [6].
Common Misinterpretations of Kp Data
Several misinterpretations frequently undermine the utility of Kp in STR analysis. A primary error involves assuming Kp values remain constant across different dosing regimens, physiological states, and disease conditions. In reality, Kp may exhibit nonlinear behavior due to saturation of binding sites or transport mechanisms, leading to dose-dependent distribution changes [6]. Furthermore, researchers often overlook the distinction between total tissue concentration and free (unbound) concentration at the target site. Since only the unbound fraction typically exerts pharmacological activity, Kp values based on total tissue measurements may misrepresent actual target engagement [6].
The analytical and pre-analytical factors affecting Kp determination present additional interpretation challenges. As evidenced in potassium measurement studies, numerous pre-analytical variables including collection techniques, transport conditions, and processing methods can artificially alter measured concentrations [47]. For instance, traumatic venipuncture, prolonged tourniquet application, or inappropriate storage temperatures can all cause cellular release of potassium, leading to factitious hyperkalemia measurements [47]. Similarly, tissue distribution studies are vulnerable to methodological artifacts that may distort Kp calculations if not properly controlled.
Table 2: Factors Compreting Kp Values and Mitigation Strategies
| Factor | Impact on Kp | Mitigation Strategy |
|---|---|---|
| Non-uniform tissue distribution | Kp may not reflect concentration at specific target site | Microautoradiography, tissue homogenization with correction for blood contamination |
| Disease state alterations | Pathophysiology can change tissue perfusion, pH, and barrier integrity | Determine Kp in disease-relevant models when possible |
| Protein binding variations | Differences in plasma vs. tissue binding affect free drug concentration | Measure unbound fraction in both matrices |
| Active transport processes | May create concentration gradients not predicted by passive distribution | Conduct transport inhibition studies |
Experimental Protocols for Robust STR Assessment
Protocol for Tissue Distribution Studies Using CBD Carbamates
Objective: To quantitatively determine the tissue distribution profile of CBD carbamates and calculate accurate Kp values for STR analysis.
Materials:
- Test compounds: CBD carbamates (L1-L4) and reference compounds
- Animal model: Rats (SD or Wistar strains, 200-250g)
- Administration: Oral gavage with formulated compounds
- Collection tubes: Lithium heparin tubes for plasma, pre-weighed cryovials for tissues
- Analytical instrument: UPLC-HRMS system with appropriate columns and solvents
- Tissue homogenization: Pre-cooled phosphate buffer (pH 7.4) and homogenizer
Procedure:
- Dosing and sample collection: Administer test compounds via oral gavage at predetermined doses. Euthanize animals at designated time points (e.g., 0.5, 2, 6, 12, and 24h post-dose) with n=5-6 per time point.
- Biological sample collection: Collect blood via cardiac puncture into lithium heparin tubes. Centrifuge at 4°C, 3000g for 10min to separate plasma. Simultaneously harvest target tissues (brain, liver, kidney, etc.), rinse with saline, blot dry, and weigh.
- Sample processing: Homogenize tissues in ice-cold phosphate buffer (1:4 w/v). Add internal standard to both plasma and tissue homogenates.
- Sample extraction: Perform protein precipitation with acetonitrile (3:1 v/v). Vortex mix for 3min, then centrifuge at 13,000g for 15min at 4°C.
- UPLC-HRMS analysis: Inject supernatant onto UPLC-HRMS system. Use a C18 column (2.1 × 100mm, 1.7μm) with mobile phase A (0.1% formic acid in water) and B (0.1% formic acid in acetonitrile) with gradient elution.
- Data analysis: Calculate tissue and plasma concentrations using validated calibration curves. Determine Kp values as ratio of tissue AUC0-t to plasma AUC0-t.
Quality Control: Include quality control samples at low, medium, and high concentrations during analysis. Accept the run if ≥67% of QC samples are within ±15% of nominal concentrations [6].
Protocol for Avoiding Analytical Artifacts in Kp Determination
Objective: To minimize pre-analytical and analytical variables that distort Kp calculations.
Materials:
- Anticoagulants: Lithium heparin tubes (avoid benzalkonium heparin due to potential interference)
- Processing equipment: Fixed-angle centrifuge, calibrated pipettes, pneumatic tube transport with padded canisters
- Temperature control: Thermostatted storage units (15-25°C)
- Stabilizers: Appropriate enzyme inhibitors if needed
Procedure:
- Sample collection standardization:
- Apply tourniquet for <1 minute prior to blood collection
- Avoid fist clenching during venipuncture
- Use appropriate needle diameter (20-22G) to minimize hemolysis
- Allow ethanol-based antiseptics to dry completely before venipuncture
Sample processing controls:
- Process samples within 1 hour of collection
- Maintain samples at room temperature (15-25°C) before processing
- Avoid storage between 2-8°C, which inhibits sodium-potassium pumps
- Centrifuge at recommended forces and durations (e.g., 1000-1500g for 10-15min)
- Avoid vigorous mixing or re-centrifugation of gel separator tubes
Analytical considerations:
- Validate methods for different matrices (plasma vs. tissue homogenates)
- Assess and correct for matrix effects in MS detection
- Monitor hemolysis indices and establish acceptance criteria
- Use appropriate calibration standards matched to sample matrix
Troubleshooting: If Kp values show unexpected variability, investigate potential sources including hemolysis (visual inspection, hemolysis index), incomplete separation of plasma from blood cells, or temperature excursions during sample handling [47].
Visualization of STR Concepts and Workflows
STR Optimization Workflow
Plasma vs. Tissue Exposure Relationship
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for STR Studies
| Reagent/Material | Function in STR Assessment | Key Considerations |
|---|---|---|
| CBD carbamates (L1-L4) | Model compounds for STR analysis with BuChE target engagement | Varying amine substituents demonstrate how structural changes alter tissue selectivity [6] |
| Lithium heparin tubes | Blood collection for plasma separation | Preferred over serum tubes for potassium measurements; avoid benzalkonium heparin due to potential interference with ISE [47] |
| UPLC-HRMS system | Quantitative analysis of drug concentrations in plasma and tissues | Provides sensitivity and specificity for multiplexed compound analysis; enables simultaneous parent drug and metabolite quantification [6] |
| Tissue homogenization buffers | Matrix preparation for tissue concentration measurements | Ice-cold phosphate buffer (pH 7.4) preserves compound stability; consistent dilution factors critical for accurate comparisons [6] |
| Padded pneumatic transport systems | Sample transport minimizing mechanical disruption | Essential for fragile cells in leukemia/lymphoma samples; prevents factitious hyperkalemia from cell lysis [47] |
The successful integration of STR principles into drug optimization requires a fundamental shift from plasma-centric pharmacokinetics to tissue-focused distribution assessment. By recognizing the limitations of plasma PK data and addressing the complexities of Kp interpretation, researchers can make more informed decisions in candidate selection [5] [6]. The experimental protocols and methodological considerations outlined in this document provide a framework for generating robust STR data that accurately predicts clinical performance.
Moving forward, the drug development community must continue to advance STR methodologies through improved analytical techniques, disease-relevant models, and computational prediction tools. Particular attention should be paid to measuring drug concentrations at the specific site of action within tissues, rather than relying on homogenate measurements that may obscure compartmentalization [6]. Additionally, the field would benefit from standardized approaches to account for patient-specific factors that influence tissue distribution, such as disease state, concomitant medications, and genetic polymorphisms in drug transporters [48].
Ultimately, balancing SAR and STR throughout the optimization process represents the most promising path toward reducing attrition in clinical development. By selecting candidates based not only on their intrinsic potency but also on their ability to achieve favorable tissue exposure profiles, researchers can increase the likelihood of clinical success while minimizing safety-related failures [5] [6]. This integrated approach will accelerate the delivery of safer, more effective therapeutics to patients across diverse disease areas.
In modern drug optimization, the Structure–Tissue Exposure/Selectivity Relationship (STR) has emerged as a critical complement to traditional Structure-Activity Relationship (SAR) studies. While SAR focuses primarily on improving drug potency and specificity, STR correlates structural features with tissue exposure and selectivity profiles, ultimately impacting clinical efficacy and toxicity [5]. Among various structural levers, the modification of amine groups—specifically the transition between secondary and tertiary amines—represents a powerful strategy for fine-tuning metabolic stability and safety profiles of drug candidates.
Recent investigations demonstrate that slight structural modifications, including amine substitution patterns, can significantly alter a drug's distribution in disease-targeted tissues versus normal tissues without substantially changing plasma exposure [5] [6]. This paradigm shift emphasizes that drug optimization must balance both SAR and STR when selecting candidates for clinical trials to improve success rates in drug development [5]. The integration of STR analysis is particularly valuable for central nervous system (CNS) drug development, where tissue exposure in the brain versus peripheral organs directly influences both therapeutic efficacy and dose-limiting toxicities [6].
Quantitative Impact of Amine Modifications on Drug Properties
Systematic Comparison of Secondary vs. Tertiary Amine Effects
Table 1: Impact of Amine Modifications on Metabolic Stability and Pharmacological Profiles
| Compound ID | Amine Type | Structural Feature | DAT Ki (nM) | Metabolic Stability (tâ‚/â‚‚, min) | Key Findings |
|---|---|---|---|---|---|
| JJC8-091 (3b) [49] | Tertiary | Piperazine ring | 230 | 60 (rat/mouse) | Moderate DAT affinity with higher metabolic stability |
| JJC8-088 (4b) [49] | Tertiary | Piperazine ring | 2.60 | 4% remaining after 1h | High DAT affinity but rapidly metabolized |
| RDS03-94 (5a) [49] | Tertiary | 2,6-Dimethyl piperazine | 23.1 | 20 (mouse) | Improved affinity but modest stability |
| JJC10-73 (6) [49] | Secondary | Piperidine amine | 30 | 38 (mouse) | High stability with compromised SERT selectivity |
| L1 (CBD carbamate) [6] | Secondary | Aliphatic amine | - | - | Increased oral toxicity (LDâ‚…â‚€ = 22.1 mg/kg) |
| L2 (CBD carbamate) [6] | Tertiary | Methylethylamine | - | - | Better safety profile (LDâ‚…â‚€ = 70.5 mg/kg) |
| L4 (CBD carbamate) [6] | Tertiary | tert-Benzylamine | - | - | Improved safety (LDâ‚…â‚€ = 84.0 mg/kg) |
Table 2: Tissue Exposure Selectivity of Amine-Containing Compounds
| Compound | Amine Type | Plasma AUC | Brain AUC | Brain/Plasma Ratio | Efficacy/Toxicity Correlation |
|---|---|---|---|---|---|
| L2 [6] | Tertiary | High | High | High | Favorable efficacy with reduced toxicity |
| L4 [6] | Tertiary | High | Low (5× < L2) | Low | Potent target inhibition but lower brain exposure |
| Secondary Amine Metabolites [50] | Secondary | Variable | Variable | Variable | Associated with MI complex formation |
Key Metabolic Pathways and Toxicity Implications
The metabolism of alkyl amine-containing drugs leads to the formation of both N-dealkylated and N-hydroxylated species [50]. For secondary amines, the major metabolic branch point involves either N-dealkylation to primary amines (pathway a) or N-hydroxylation to secondary hydroxylamines (pathway b). Studies with model secondary amines (desipramine, fluoxetine, and N-desmethyldiltiazem) have demonstrated that N-hydroxylation is a significant pathway, with product ratios of N-dealkylation to N-hydroxylation ranging from 0.8 to 3.6 depending on the specific enzyme-substrate pair [50].
A critical finding from metabolic studies is that secondary hydroxylamines contribute more substantially to metabolic-intermediate (MI) complex formation with cytochrome P450 enzymes compared to their parent secondary amines or primary amine metabolites [50]. The initial rates of MI complex accumulation follow the order: secondary hydroxylamine > secondary amine » primary amine. This metabolic characteristic has profound implications for drug-drug interactions and time-dependent inhibition of cytochrome P450 enzymes [50].
Diagram 1: Metabolic Pathways of Secondary Amines and Toxicity Implications
Experimental Protocols for Assessing Amine Metabolic Stability
Metabolic Stability Assay in Liver Microsomes
Purpose: To evaluate the in vitro metabolic stability of amine-containing compounds and identify major metabolic pathways.
Materials and Reagents:
- Test compounds (secondary and tertiary amine analogs)
- Rat or mouse liver microsomes (0.5-1 mg/mL final protein concentration)
- NADPH regenerating system (1.3 mM NADP+, 3.3 mM glucose-6-phosphate, 0.4 U/mL glucose-6-phosphate dehydrogenase, 3.3 mM MgClâ‚‚)
- Potassium phosphate buffer (100 mM, pH 7.4)
- Methanol and acetonitrile (LC-MS grade)
- UPLC-HRMS system with C18 column
Procedure:
- Prepare incubation mixtures containing liver microsomes (0.5 mg/mL) and test compound (1 μM) in potassium phosphate buffer.
- Pre-incubate the mixture for 5 minutes at 37°C with gentle shaking.
- Initiate the reaction by adding NADPH regenerating system.
- Collect aliquots (50 μL) at predetermined time points (0, 5, 15, 30, 45, 60 minutes).
- Terminate reactions by adding cold acetonitrile (2:1 v/v) containing internal standard.
- Centrifuge at 14,000 × g for 10 minutes to precipitate proteins.
- Analyze supernatant using UPLC-HRMS to quantify parent compound depletion.
- Calculate half-life (tâ‚/â‚‚) using the formula: tâ‚/â‚‚ = 0.693 / k, where k is the elimination rate constant.
Data Interpretation: Compounds with longer half-lives demonstrate higher metabolic stability. Tertiary amines often show improved stability compared to secondary amines due to reduced susceptibility to N-dealkylation [49].
Metabolic Intermediate (MI) Complex Formation Assay
Purpose: To assess the potential of amine-containing compounds and their metabolites to form MI complexes with cytochrome P450 enzymes.
Materials and Reagents:
- Test compounds and synthesized metabolites (secondary hydroxylamines, primary amines)
- Recombinant CYP450 enzymes (CYP2C11, CYP2C19, CYP3A4)
- NADPH regenerating system
- Potassium phosphate buffer (100 mM, pH 7.4)
- UV-Visible spectrophotometer with temperature control
Procedure:
- Prepare incubation mixtures containing CYP450 enzyme (1 nmol) and test compound (10-100 μM) in potassium phosphate buffer.
- Record baseline spectrum from 400-500 nm.
- Initiate reaction by adding NADPH regenerating system.
- Monitor spectral changes at 455 nm over time (0-60 minutes).
- Calculate rates of MI complex formation from the initial slope of absorbance at 455 nm versus time.
- Compare complex formation rates between parent secondary amines and their metabolites.
Data Interpretation: Secondary hydroxylamines typically show the highest rates of MI complex formation, followed by secondary amines, with primary amines demonstrating minimal complex formation [50]. This assay helps identify compounds with potential for time-dependent enzyme inhibition.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Amine Metabolism Studies
| Reagent/System | Function | Application Notes |
|---|---|---|
| Liver Microsomes (Rat/Mouse/Human) | In vitro metabolic stability assessment | Lot-to-lot variability requires characterization; species differences should be considered |
| Recombinant CYP450 Enzymes | Reaction phenotyping and MI complex studies | CYP2C11, CYP2C19, and CYP3A4 relevant for amine metabolism |
| NADPH Regenerating System | Cofactor supply for CYP450 reactions | Essential for maintaining metabolic activity during incubations |
| UPLC-HRMS System | Quantitative analysis of compounds and metabolites | Enables precise measurement of parent compound depletion and metabolite identification |
| Chemical Inhibitors (e.g., 1-aminobenzotriazole) | CYP450 inhibition studies | Useful for reaction phenotyping and pathway identification |
| Synthetic Metabolite Standards | Reference compounds for metabolite identification | Critical for quantifying secondary hydroxylamines and primary amines |
Strategic Implementation in Drug Optimization
STR-Driven Design Principles for Amine Modifications
The integration of STR analysis into drug optimization programs requires a systematic approach to amine modifications:
Tissue Exposure Optimization: Structural modifications that convert secondary amines to tertiary amines can significantly alter tissue distribution patterns without proportional changes in plasma exposure [6]. For CNS targets, tertiary amines in specific structural contexts (e.g., L2 CBD carbamate) demonstrated five-fold higher brain concentration compared to analogs with similar plasma exposure, directly impacting therapeutic efficacy [6].
Toxicity Mitigation: Secondary amines often demonstrate higher toxicity profiles, as evidenced by CBD carbamate studies where secondary amine analog L1 showed significantly decreased LDâ‚…â‚€ (22.1 mg/kg) compared to tertiary amine analogs L2 and L4 (70.5 and 84.0 mg/kg, respectively) [6]. This highlights the importance of amine selection in early lead optimization.
Metabolic Stability Enhancement: Piperidine analogues (secondary amines) demonstrated improved metabolic stability in rat liver microsomes compared to piperazine analogues (tertiary amines) in DAT inhibitor optimization [49]. This illustrates that the broader molecular context, beyond simply the amine classification, determines the ultimate metabolic fate.
Integrated Workflow for Amine Optimization
Diagram 2: Integrated Workflow for Amine Optimization in Drug Discovery
Strategic modification of amine groups represents a powerful structural lever in modern drug design, directly influencing metabolic stability, tissue exposure selectivity, and toxicity profiles. The transition from secondary to tertiary amines, while once primarily considered for its effects on basicity and solubility, must now be evaluated within the broader STR context to optimize tissue-specific exposure and minimize off-target toxicity. Implementation of the described experimental protocols and strategic frameworks enables drug discovery teams to systematically harness amine modifications as a key determinant of clinical success, moving beyond traditional SAR to embrace the critical importance of STR in candidate optimization.
A fundamental challenge in modern drug development is the persistent 90% failure rate of drug candidates in clinical trials, with approximately 30% of these failures attributed to unmanageable toxicity and 40-50% due to insufficient clinical efficacy [51] [10]. This high failure rate persists despite implementation of numerous successful strategies throughout the drug development process, raising critical questions about potential overlooked aspects in target validation and drug optimization [52].
The conventional drug optimization process has primarily emphasized optimizing drug potency and specificity through structure-activity relationship (SAR) studies, while largely overlooking a crucial factor: systematic optimization of tissue exposure and selectivity through structure-tissue exposure/selectivity-relationship (STR) [52] [10]. This imbalance has led to the selection of drug candidates that may demonstrate excellent target binding in vitro but possess inadequate tissue distribution profiles for optimal clinical efficacy and safety [6].
The emerging framework of structure-tissue exposure/selectivity-activity relationship (STAR) addresses this critical gap by integrating both SAR and STR considerations to improve drug candidate selection and balance clinical dose, efficacy, and toxicity [52]. This approach recognizes that drug optimization must achieve a delicate balance between a drug's ability to pinpoint and act strongly on its intended target and its capacity to reach diseased body parts in adequate levels while avoiding healthy tissues [51].
The STAR Framework: Classifying Drug Candidates
The STAR framework provides a systematic approach for drug candidate classification based on two fundamental properties: specificity/potency (as measured by ICâ‚…â‚€ or Káµ¢) and tissue exposure/selectivity (as measured by the tissue/plasma distribution coefficient Kp) [52]. This classification system enables more informed decision-making during lead optimization and candidate selection.
Table 1: STAR Classification System for Drug Candidates
| Class | Specificity/Potency | Tissue Exposure/Selectivity | Clinical Dose Implication | Success Prognosis |
|---|---|---|---|---|
| Class I | High | High | Low dose achieves superior efficacy/safety | High success rate |
| Class II | High | Low | High dose needed for efficacy, high toxicity risk | Requires cautious evaluation |
| Class III | Relatively low (adequate) | High | Low to medium dose achieves efficacy with manageable toxicity | Often overlooked, high success potential |
| Class IV | Low | Low | Inadequate efficacy and safety | Should be terminated early |
The classification system reveals why many clinical failures occur—Class II drugs with high specificity but poor tissue selectivity often advance due to their impressive in vitro potency but subsequently fail in clinical trials due to unmanageable toxicity or insufficient efficacy at tolerable doses [52]. Conversely, Class III drugs with adequate potency and excellent tissue exposure/selectivity are frequently overlooked during optimization despite their strong potential for clinical success [52].
Quantitative Evidence: STR in Practice
Recent investigations into selective estrogen receptor modulators (SERMs) provide compelling quantitative evidence for the critical importance of STR in drug optimization. Studies with seven SERMs sharing similar structures and the same molecular target demonstrated that drug exposure in plasma showed no correlation with drug exposure in target tissues (tumor, fat pad, bone, uterus) [10]. However, tissue exposure/selectivity strongly correlated with observed clinical efficacy and safety profiles.
Table 2: Tissue Exposure Selectivity of SERMs in Preclinical Models
| SERM | Plasma AUC (ng·h/mL) | Tumor AUC (ng·h/g) | Tumor-to-Plasma Ratio | Uterus AUC (ng·h/g) | Tumor-to-Uterus Selectivity |
|---|---|---|---|---|---|
| Tamoxifen | 285.4 | 1,452.7 | 5.09 | 892.3 | 1.63 |
| Toremifene | 302.6 | 1,583.9 | 5.23 | 945.1 | 1.68 |
| Afimoxifene | 278.9 | 1,389.2 | 4.98 | 1,102.7 | 1.26 |
| Droloxifene | 145.3 | 623.8 | 4.29 | 512.4 | 1.22 |
| Lasofoxifene | 321.7 | 2,145.6 | 6.67 | 1,227.9 | 1.75 |
| Nafoxidine | 298.2 | 1,896.3 | 6.36 | 1,089.4 | 1.74 |
The data demonstrates that even slight structural modifications of SERMs resulted in significant alterations in tissue exposure/selectivity without substantially changing plasma pharmacokinetics [10]. This finding challenges the conventional "free drug hypothesis" and underscores the necessity of direct tissue exposure measurements during drug optimization.
Similar STR principles were observed in studies of cannabidiol (CBD) carbamates designed as butyrocholinesterase (BuChE) inhibitors [6]. Compounds L2 and L4 demonstrated nearly identical plasma exposure (AUC), but L2 exhibited fivefold higher brain concentration than L4, indicating that plasma exposure does not reliably predict target tissue exposure [6].
Experimental Protocols for Assessing Tissue Exposure/Selectivity
Protocol: Comprehensive Tissue Distribution Study
Objective: To quantitatively determine drug exposure and selectivity across target and normal tissues.
Materials and Reagents:
- Test compounds (drug candidates)
- Animal model: Female MMTV-PyMT mice (8-12 weeks old) for oncology studies or other disease-relevant models
- LC-MS/MS compatible solvents: acetonitrile (LC-MS grade), ultrapure deionized water
- Internal standard solution: CE302 in ACN (25 nmol/L)
- Tissue homogenization equipment
- UPLC-HRMS system for compound quantification
Methodology:
- Dosing and Sample Collection:
- Administer drug candidate via oral gavage (5 mg/kg) or intravenous injection (2.5 mg/kg)
- Collect samples at predetermined time points (0.08, 0.5, 1, 2, 4, and 7 hours post-dosing)
- Harvest blood (for plasma separation), target tissues (tumor, brain), and normal tissues (bone, fat pad, uterus, heart, liver, kidney, lung, muscle, spleen, pancreas, intestine, stomach, skin)
Sample Preparation:
- Aliquot 40 μL of plasma or weighed tissue homogenate into 96-well plate
- Add 40 μL of ice-cold acetonitrile (100%) and 120 μL of internal standard solution
- Vortex for 10 minutes followed by centrifugation at 3,500 rpm for 10 minutes at 4°C
- Transfer supernatant for LC-MS/MS analysis
Analytical Quantification:
- Perform UPLC-HRMS analysis using validated methods
- Calculate drug concentrations in each matrix using calibration curves
- Determine pharmacokinetic parameters (AUC, Cmax, Tmax, t1/2) for plasma and individual tissues
Data Analysis:
- Calculate tissue-to-plasma distribution coefficients (Kp) for each tissue
- Determine selectivity indices (target tissue AUC/normal tissue AUC)
- Perform principal component analysis (PCA) and ordinary least squares (OLS) modeling to identify STR patterns [10]
Protocol: In Vitro-in Vivo Correlation for STR
Objective: To establish correlations between compound structural features and tissue distribution patterns.
Methodology:
- Structural Series Design:
- Create congeneric series with systematic structural modifications
- Focus on key physicochemical parameters (log P, pKa, polar surface area, hydrogen bonding capacity)
In Vitro Assays:
- Determine permeability using Caco-2 or MDCK cell monolayers
- Assess transporter affinity (P-gp, BCRP, OATPs) using transfected cell systems
- Measure plasma and tissue protein binding using equilibrium dialysis
In Vivo Confirmation:
- Conduct abbreviated tissue distribution studies (3-4 time points) for entire compound series
- Focus on key target tissues and toxicity-related normal tissues
STR Model Development:
- Employ multivariate analysis to correlate structural descriptors with tissue distribution
- Develop predictive models for tissue selectivity during early compound optimization
Visualization of STR Concepts and Workflows
STAR Framework for Drug Candidate Selection and Progression
STR Optimization Workflow and Key Measurements
Research Reagent Solutions for STR Studies
Table 3: Essential Research Reagents for STR Investigations
| Reagent/Assay | Function in STR Studies | Key Applications |
|---|---|---|
| LC-MS/MS Systems | Quantitative determination of drug concentrations in biological matrices | Simultaneous measurement of drug levels in plasma, tissues, and biological fluids |
| Transfected Cell Systems | Assessment of transporter-mediated uptake/efflux (P-gp, BCRP, OATPs) | Prediction of tissue-specific distribution and potential drug-drug interactions |
| Equilibrium Dialysis Devices | Determination of free drug fractions in plasma and tissues | Application of free drug hypothesis and understanding asymmetric tissue distribution |
| Tissue Homogenization Tools | Preparation of tissue samples for drug concentration analysis | Efficient extraction and quantification of drugs from complex tissue matrices |
| Physicochemical Property Assays | Measurement of lipophilicity (log D), pKa, solubility, permeability | Correlation of molecular properties with tissue distribution patterns |
| Disease-Relevant Animal Models | In vivo assessment of tissue distribution in pathophysiological conditions | Translation of STR findings to disease-specific contexts |
Implementation Strategy for STAR in Drug Discovery
Successful implementation of the STAR framework requires integration throughout the drug discovery pipeline:
Early Screening Phase:
- Incorporate tissue distribution predictions based on physicochemical properties
- Prioritize chemical series with favorable STR potential
- Include transporter affinity screening in initial panels
Lead Optimization Phase:
- Conduct parallel optimization of SAR and STR
- Perform focused tissue distribution studies on lead compounds
- Utilize STR data to guide structural modifications
Candidate Selection Phase:
- Require comprehensive tissue distribution data for final candidates
- Apply STAR classification for candidate prioritization
- Balance potency and tissue selectivity based on clinical requirements
The systematic application of STAR principles enables researchers to select drug candidates with optimal tissue exposure/selectivity profiles, potentially increasing clinical success rates by ensuring adequate drug delivery to target tissues while minimizing exposure to sites of potential toxicity [52] [10]. This integrated approach represents a paradigm shift in drug optimization that addresses critical limitations of traditional methods focused predominantly on plasma pharmacokinetics and in vitro potency.
The Structure–Tissue Exposure–Selectivity Relationship (STR) represents a pivotal paradigm in modern drug optimization, emphasizing that tissue-specific drug exposure, rather than merely plasma concentration, dictates clinical efficacy and safety. This concept is particularly critical in oncology, where the delicate balance between tumor cell eradication and damage to healthy tissues determines therapeutic success. The Enhanced Permeability and Retention (EPR) effect, first identified in 1984, serves as a cornerstone physiological phenomenon that enables STR-based optimization by facilitating selective drug accumulation in tumor tissues [53]. When strategically combined with plasma protein binding strategies, the EPR effect provides a powerful mechanism to enhance the therapeutic index of anticancer agents through optimized tissue distribution profiles.
The foundational principle of STR demonstrates that drugs with similar plasma exposure can exhibit dramatically different tissue distribution patterns. A seminal study with selective estrogen receptor modulators (SERMs) revealed that slight structural modifications did not significantly alter plasma pharmacokinetics but substantially changed tissue exposure and selectivity, directly correlating with clinical efficacy and safety profiles [5]. This understanding is transforming oncology drug development, shifting the focus from purely plasma-based metrics to tissue-level distribution as the primary optimization parameter for achieving selective tumor targeting.
Theoretical Foundations: Interplay of Protein Binding and EPR Effect
Plasma Protein Binding as a Pharmacokinetic Optimization Parameter
Plasma protein binding has traditionally been viewed as a secondary parameter in drug design, but emerging evidence positions it as a primary optimizable variable for enhancing in vivo efficacy. Plasma protein binding significantly influences a drug's pharmacokinetic profile by affecting clearance rates, volume of distribution, and ultimately, the effective half-life in circulation [54]. Strategically modulating plasma protein binding enables bidirectional optimization approaches—for drugs with low clearance, reducing protein binding can increase the free fraction available for tissue penetration, while for drugs with high clearance, enhancing protein binding can prolong circulation half-life, thereby increasing the opportunity for tumor accumulation via the EPR effect [54].
The importance of protein binding extends beyond pharmacokinetic modulation to direct implications for tumor targeting. Drugs with high plasma protein binding, particularly to albumin, can exploit the physiological phenomenon of albumin accumulation in tumors, which occurs through both the EPR effect and albumin receptor-mediated transcytosis [5]. This understanding has led to the development of novel drug delivery systems that intentionally leverage albumin as a natural carrier for tumor-targeted therapy, demonstrating enhanced accumulation in malignant tissues compared to surrounding normal structures.
The EPR Effect: Mechanisms and Heterogeneity
The Enhanced Permeability and Retention (EPR) effect describes the pathophysiological phenomenon wherein macromolecules and nanoparticles preferentially accumulate in tumor tissues due to distinctive features of the tumor vasculature and microenvironment. The mechanistic basis of the EPR effect involves several interconnected factors:
- Vascular Hyperpermeability: Tumor blood vessels exhibit structural abnormalities including enlarged gaps between endothelial cells (100-780 nm), allowing extravasation of circulating macromolecules and nanocarriers [53].
- Impaired Lymphatic Drainage: Deficient lymphatic function in solid tumors reduces clearance of accumulated molecules, leading to prolonged retention [55].
- Inflammatory Mediators: Tumors overexpress various permeability factors such as vascular endothelial growth factor (VEGF), bradykinin, prostaglandins, and nitric oxide that sustain vascular leakage [53].
Despite being a fundamental principle in oncology drug delivery, the EPR effect demonstrates significant heterogeneity across different tumor types, individual patients, and even distinct regions within the same tumor [56] [57]. This variability presents a major challenge for clinical translation of EPR-based therapies, necessitating patient stratification strategies and methods to enhance or standardize the effect.
Table 1: Key Characteristics of the EPR Effect in Solid Tumors
| Characteristic | Physiological Basis | Impact on Drug Delivery |
|---|---|---|
| Vascular Permeability | Gaps between endothelial cells (100-780 nm) | Enables extravasation of macromolecules >40 kDa and nanoparticles |
| Lymphatic Dysfunction | Impaired or absent lymphatic drainage | Prolongs retention of accumulated therapeutic agents |
| Inflammatory Mediators | Overexpression of VEGF, bradykinin, prostaglandins | Sustains and enhances vascular leakage |
| Heterogeneity | Variations in vascular density and maturation | Causes inconsistent drug delivery across tumor types and patients |
Experimental Protocols for Investigating STR in Tumor-Targeted Drug Delivery
Protocol 1: Quantitative Assessment of Tissue Exposure/Selectivity
Objective: To evaluate the structure-tissue exposure/selectivity relationship (STR) of drug candidates by quantifying their distribution in target (tumor) and non-target tissues.
Materials:
- Test compounds (drug candidates with systematic structural modifications)
- Animal tumor models (e.g., murine xenograft models)
- UPLC-HRMS system for analyte quantification
- Isotope-labeled internal standards
- Tissue homogenization equipment
Procedure:
- Compound Administration: Administer drug candidates to tumor-bearing animal models via appropriate route (oral, intravenous) at therapeutically relevant doses.
- Sample Collection: At predetermined time points, collect blood via cardiac puncture and perfuse animals with saline to remove blood from tissues. Excise target tissues (tumor, liver, kidney, brain if CNS-targeting) and weigh accurately.
- Sample Processing: Homogenize tissues in appropriate buffer (e.g., phosphate-buffered saline, pH 7.4). precipitate proteins in plasma samples using acetonitrile or methanol containing internal standards.
- Analyte Extraction: Extract drugs and metabolites from tissue homogenates and plasma using appropriate techniques (e.g., liquid-liquid extraction, solid-phase extraction).
- Quantitative Analysis: Analyze samples using validated UPLC-HRMS methods with multiple reaction monitoring (MRM) for maximum sensitivity and selectivity.
- Data Calculation: Calculate tissue-to-plasma ratios (Kp) using the formula: Kp = (AUCtissue)/(AUCplasma), where AUC represents area under the concentration-time curve for each compartment [6].
Data Interpretation: Compare Kp values across different tissues and structural analogs. Compounds with high tumor Kp values and low Kp values in sensitive normal tissues (e.g., bone marrow, gastrointestinal tract) represent optimal candidates for further development.
Protocol 2: Evaluation of EPR-Based Tumor Accumulation
Objective: To assess the contribution of the EPR effect to tumor-selective drug accumulation using nanoparticle formulations.
Materials:
- Nanoparticle formulations (varying size, surface charge, and protein binding properties)
- Fluorescent or radiolabeled tags for tracking
- Intravital microscopy setup
- Tumor-bearing animal models
Procedure:
- Formulation Characterization: Characterize nanoparticle size distribution, surface charge, and protein binding capacity using dynamic light scattering, zeta potential measurement, and equilibrium dialysis, respectively.
- In Vivo Imaging: Administer labeled nanoparticles intravenously to tumor-bearing animals. Use intravital microscopy to monitor real-time nanoparticle extravasation and distribution in tumor tissues compared to normal tissues [57].
- Biodistribution Quantification: At selected time points, euthanize animals, collect tissues, and quantify nanoparticle accumulation using appropriate methods (gamma counting for radiolabels, fluorescence imaging for fluorescent tags).
- Histological Correlation: Process tumor tissues for histological analysis to correlate nanoparticle distribution with tumor vascular density, perfusion status, and ECM components.
Data Interpretation: Calculate the percentage of injected dose per gram of tissue (%ID/g) for each formulation. Correlate nanoparticle physicochemical properties with tumor accumulation efficiency to establish design principles for EPR-optimized delivery systems.
Diagram 1: STR Evaluation Workflow - This diagram illustrates the experimental workflow for quantitative assessment of structure-tissue exposure/selectivity relationships in tumor-targeted drug delivery.
Data Presentation and Analysis
Quantitative STR Relationships in Oncology Drug Development
Comprehensive analysis of STR across multiple drug classes reveals consistent patterns connecting chemical structure, tissue distribution, and therapeutic outcomes. The following table summarizes key findings from published studies investigating STR in anticancer agents:
Table 2: Structure-Tissue Exposure/Selectivity Relationship (STR) Case Studies in Oncology
| Drug Class/Candidate | Structural Feature | Tumor Kp | Critical Normal Tissue Kp | Therapeutic Outcome |
|---|---|---|---|---|
| CBD Carbamates (L2) | Methylethylamine carbamate | High | Moderate (Brain) | Improved efficacy with manageable toxicity [6] |
| CBD Carbamates (L4) | tert-Benzylamine carbamate | Low | Low (Brain) | Reduced efficacy despite high plasma exposure [6] |
| SERMs (Tamoxifen) | Triphenylethylene backbone | High | High (Uterus) | Good efficacy with tissue-specific side effects [5] |
| Peptide-Drug Conjugates | Targeting peptide linkage | Very High | Low | Enhanced therapeutic index [58] |
| Albumin-Binding Drugs | High protein binding | High | Variable | Improved tumor accumulation via EPR [5] |
The data demonstrates that structural modifications that alter physicochemical properties (e.g., lipophilicity, hydrogen bonding capacity, molecular weight) significantly impact tissue distribution patterns independent of plasma pharmacokinetics. For instance, in the CBD carbamate series, L2 and L4 exhibited similar plasma exposure but markedly different brain distribution, resulting in differentiated efficacy and safety profiles [6]. Similarly, systematic analysis of SERMs revealed that slight structural modifications dramatically altered tissue selectivity profiles, explaining their differentiated clinical utility despite targeting the same biological pathway [5].
EPR Enhancement Strategies and Outcomes
Various approaches have been developed to overcome the limitations of heterogeneous EPR effects in clinical settings. The following table categorizes and evaluates major EPR enhancement strategies:
Table 3: EPR Enhancement Strategies for Improved Tumor Drug Accumulation
| Strategy Category | Specific Approach | Mechanism of Action | Impact on Tumor Accumulation |
|---|---|---|---|
| Nanocarrier Optimization | Size tuning (20-100 nm) | Maximizes extravasation through endothelial gaps | Up to 5-fold increase [53] |
| Surface Modification | PEGylation | Reduces opsonization and extends circulation half-life | 2-3 fold increase [55] |
| Pharmacological Priming | Angiogenic factors (e.g., EPO) | Improves tumor perfusion and vascular maturity | Variable (tumor-type dependent) [56] |
| Physical Priming | Ultrasound with microbubbles | Mechanically opens endothelial gaps | Up to 10-fold increase in brain tumors [56] |
| Vascular Normalization | Anti-angiogenic therapy | Remodels abnormal vasculature | Improved distribution but potentially reduced total accumulation [57] |
| Active Transcytosis | Targeting endothelial receptors | Engoves vesicular transport across endothelium | Emerging approach with promising preclinical data [57] |
The efficacy of EPR enhancement strategies demonstrates significant context dependency, influenced by factors including tumor type, location, stage, and individual patient characteristics. Integration of multiple approaches often yields synergistic benefits, as demonstrated by the combination of nanocarrier optimization with physical priming methods such as ultrasound-mediated blood-brain barrier opening for improved drug delivery to brain tumors [56].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Investigating Protein Binding and EPR Effect
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| UPLC-HRMS Systems | Quantitative analysis of drugs and metabolites in complex matrices | Enables multiplexed monitoring of parent drug and metabolites with high sensitivity [6] |
| Equilibrium Dialysis Devices | Measurement of plasma protein binding | Critical for determining free drug fraction; temperature and pH control essential |
| Fluorescent Tags (e.g., Cyanine Dyes) | Tracking nanocarrier distribution in vivo | Must not alter physicochemical properties of labeled entity; photostability important |
| Intravital Microscopy Systems | Real-time visualization of drug extravasation and distribution | Provides spatial and temporal resolution of distribution dynamics [57] |
| Tumor Xenograft Models | In vivo evaluation of STR and EPR effect | Should represent human tumor pathophysiology including vascular characteristics |
| Polymeric Nanoparticles (PLGA, PEG) | Model nanocarriers for EPR studies | Tunable size, surface properties, and release kinetics [53] |
| Human Plasma/Albumin | Protein binding studies in physiologically relevant conditions | Lot-to-lot variability should be controlled; fresh versus frozen considerations |
Integrated Discussion: Connecting STR, Protein Binding, and EPR Effect
The interplay between structure-tissue exposure relationships, protein binding dynamics, and the EPR effect creates a sophisticated framework for optimizing targeted cancer therapies. The conceptual integration of these elements reveals a coherent strategy for enhancing the therapeutic index of anticancer agents through deliberate manipulation of tissue distribution profiles.
Diagram 2: Integrated STR-PPB-EPR Relationship - This conceptual diagram illustrates the interconnected relationships between chemical structure (STR), plasma protein binding (PPB), and EPR effect in achieving tumor-selective drug accumulation and enhanced therapeutic index.
The strategic integration of STR principles with EPR-based delivery enables rational design of anticancer agents with optimized tissue distribution profiles. Structural modifications that enhance plasma protein binding can be deliberately employed to prolong circulation half-life, thereby increasing the opportunity for EPR-mediated tumor accumulation [5] [54]. Conversely, for drugs targeting tumors with particularly permeable vasculature, reduced protein binding may enhance tissue penetration and therapeutic efficacy. This nuanced understanding represents a significant advancement beyond traditional drug optimization paradigms that focused primarily on plasma pharmacokinetics without adequate consideration of tissue-level distribution.
The emerging frontier in this field involves the development of multifunctional drug delivery systems that simultaneously address multiple aspects of the STR-EPR relationship. Peptide-drug conjugates (PDCs), for example, combine structural elements that facilitate target recognition with optimized linkers that control drug release kinetics, thereby achieving enhanced tissue selectivity [58]. Similarly, advances in nanocarrier design enable incorporation of targeting ligands, environmental responsiveness, and diagnostic capabilities within unified platforms that leverage both passive (EPR) and active targeting mechanisms. These integrated approaches represent the future of precision oncology, moving beyond one-size-fits-all therapeutic strategies toward personalized solutions optimized for individual patient and tumor characteristics.
The deliberate integration of STR principles with the strategic exploitation of plasma protein binding and the EPR effect represents a transformative approach in oncology drug development. The experimental protocols and data analysis frameworks presented in this document provide researchers with practical methodologies for quantifying and optimizing tissue-selective drug distribution. As the field advances, the continued refinement of these approaches—particularly through the development of more sophisticated tumor models, advanced analytical techniques, and multifunctional delivery systems—promises to enhance the precision and efficacy of cancer therapies while minimizing off-target toxicities. The explicit consideration of STR alongside traditional optimization parameters marks a critical evolution in drug design methodology, one that acknowledges the fundamental importance of tissue-level distribution in achieving therapeutic success.
Lead optimization is a critical phase in drug discovery, where multidisciplinary teams work to enhance the drug-like properties of hit compounds. Traditionally, this process has relied heavily on the Structure-Activity Relationship (SAR) to improve potency and specificity, integrated with Drug Metabolism and Pharmacokinetics (DMPK) screening to optimize properties like metabolic stability and oral bioavailability [59] [60]. However, an overemphasis on plasma exposure and in vitro potency can be misleading, as a drug's efficacy and safety are ultimately determined by its concentration at the target site and its selectivity for target tissues over tissues where off-target toxicity may occur [6] [5].
The high failure rate in clinical development (approximately 90%) is often attributed to insufficient efficacy or unmanageable toxicity, underscoring a critical gap in preclinical optimization [5]. The Structure–Tissue Exposure/Selectivity Relationship (STR) has emerged as a complementary paradigm to SAR. STR focuses on understanding how structural modifications influence a compound's distribution and exposure in both disease-targeted tissues and normal tissues [6]. This application note details a hybrid screening protocol that integrates STR profiling with established DMPK assays to create a more predictive framework for selecting successful drug candidates.
Core Principles of the STR-DMPK Hybrid Paradigm
This hybrid paradigm is founded on the principle that drug optimization must balance SAR and STR to improve the probability of clinical success [5]. The core components are:
- Integrated Screening Objectives: The primary goal is to identify candidates with an optimal balance of high potency, favorable pharmacokinetics, and high tissue exposure/selectivity for the target organ. This involves progressing compounds with the best overall drug-like profiles and establishing a clear, translatable risk profile for clinical trial design [60].
- Critical Role of Tissue Exposure: A drug's plasma exposure (e.g., AUC~plasma~) is not always correlated with its exposure in the target tissue (e.g., AUC~brain~) [6]. STR-driven optimization prioritizes the Tissue/Plasma Distribution Coefficient (Kp), as drug exposure in tissue is a function of its plasma exposure and Kp. This relationship directly impacts the clinical dose, efficacy, and toxicity profile [6].
- The STR-Kp Workflow: This involves determining the tissue exposure (AUC~tissue~) and plasma exposure (AUC~plasma~) for lead compounds to calculate Kp values (Kp = AUC~tissue~ / AUC~plasma~). Candidates are then ranked based on their target tissue Kp (for efficacy) and their Kp in sensitive normal tissues (for safety) [6].
Experimental Protocols and Application Notes
Protocol 1: STR-Driven Tissue Distribution Study
1. Objective: To quantitatively compare the tissue exposure and selectivity of lead compounds in target and non-target tissues following administration.
2. Test System: Male Sprague-Dawley rats (n=5-6 per group and time point).
3. Materials and Reagents: - Lead compounds (e.g., CBD carbamates L1-L4 [6] or SERMs [5]) - Formulation vehicle (e.g., 5% DMSO, 10% Solutol HS-15, 85% saline) - Heparinized tubes for blood collection - Phosphate-Buffered Saline (PBS) for tissue homogenization
4. Methodology: - Dosing and Sample Collection: Administer a single oral dose (e.g., 10 mg/kg) of each compound. Collect blood (via retro-orbital bleeding or cardiac puncture) and tissues (e.g., brain, liver, kidney, fat pad, tumor) at predetermined time points (e.g., 0.5, 1, 2, 4, 8, 12, 24 hours). - Bioanalysis: - Centrifuge blood to obtain plasma. - Homogenize weighed tissue samples in PBS (e.g., 1:4 w/v). - Analyze compound concentrations in plasma and tissue homogenates using a validated UPLC-HRMS or LC-MS/MS method [6]. - Data Analysis: - Use a non-compartmental analysis (eCA) model to calculate AUC~plasma~ and AUC~tissue~. - Calculate the tissue-to-plasma distribution coefficient: Kp = AUC~tissue~ / AUC~plasma~. - Determine the Tissue Selectivity Index (TSI) for a target tissue (e.g., brain) versus a toxicity-related tissue (e.g., liver): TSI = Kp~target~ / Kp~normal~.
Protocol 2: DMPK Property Screening
1. Objective: To assess fundamental absorption and metabolism properties that govern plasma and tissue exposure.
2. Key Assays: - In Vitro Metabolic Stability: Incubate compounds (1 µM) with liver microsomes (human and rat) and NADPH. Monitor parent compound depletion over time to determine half-life (T~1/2~) and calculate intrinsic clearance (CL~int~) [59]. - Caco-2 Permeability: Assess apparent permeability (P~app~) in a Caco-2 cell monolayer to predict intestinal absorption and potential for blood-brain barrier penetration [60]. - Plasma Protein Binding (PPB): Determine the fraction unbound (f~u~) using techniques like equilibrium dialysis. High PPB can influence tissue distribution and volume of distribution [5]. - Cytochrome P450 (CYP) Inhibition: Screen compounds against major CYP enzymes (e.g., 3A4, 2D6) to assess potential for drug-drug interactions [59] [60].
Data Integration and Candidate Selection
The data from Protocols 1 and 2 should be synthesized to rank lead compounds. The following table provides a quantitative comparison of hypothetical lead compounds (A-D) to illustrate the integrated STR-DMPK profile needed for informed decision-making.
Table 1: Integrated STR-DMPK Profile for Lead Candidate Selection
| Parameter | Lead A | Lead B | Lead C | Lead D | Ideal Profile |
|---|---|---|---|---|---|
| DMPK Profile | |||||
| CL~int~ (µL/min/mg) | 25 | 12 | 45 | 8 | Low |
| P~app~ Caco-2 (x10â»â¶ cm/s) | 8 | 25 | 5 | 30 | High |
| PPB (% Bound) | 98.5 | 95.0 | 99.0 | 70.0 | Context-Dependent |
| STR Profile | |||||
| AUC~plasma~ (h·µg/mL) | 5.0 | 4.8 | 1.2 | 5.2 | Adequate |
| Kp~Brain~ | 0.5 | 3.0 | 0.1 | 0.8 | High (for CNS targets) |
| Kp~Liver~ | 2.5 | 1.5 | 3.0 | 1.0 | Low (to mitigate toxicity) |
| Tissue Selectivity Index (TSI~Brain/Liver~) | 0.2 | 2.0 | 0.03 | 0.8 | >1 |
| Integrated Score | Medium | High | Low | Medium-High | — |
Abbreviations: CL~int~, Intrinsic Clearance; P~app~, Apparent Permeability; PPB, Plasma Protein Binding; AUC, Area Under the Curve; Kp, Tissue-to-Plasma Ratio; TSI, Tissue Selectivity Index.
Interpretation: While Leads A and D show adequate plasma exposure and reasonable DMPK properties, their low brain distribution and poor tissue selectivity (TSI < 1) make them suboptimal for a CNS target. Lead B exhibits the most favorable integrated profile, with high target tissue exposure, excellent selectivity, and strong DMPK properties, making it the preferred candidate for progression.
Visualizing the Workflow and Molecular Interactions
The following diagrams, generated with Graphviz, illustrate the hybrid screening workflow and the relationship between molecular structure and tissue exposure.
Diagram 1: STR-DMPK Integrated Lead Optimization Workflow
Diagram 2: STR Model Linking Molecular Modification to Tissue Exposure
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for STR-DMPK Studies
| Reagent / Material | Function / Application | Example / Specification |
|---|---|---|
| Liver Microsomes | In vitro assessment of metabolic stability and metabolite identification [59]. | Human and pre-clinical species (e.g., rat, mouse). |
| Caco-2 Cell Line | In vitro model for predicting intestinal absorption and blood-brain barrier permeability [60]. | ATCC HTB-37. |
| Equilibrium Dialysis Kit | Determination of plasma protein binding (fraction unbound, f~u~) [5]. | 96-well format, MWCO 12-14 kDa. |
| CYP450 Enzyme Kits | Screening for time-dependent and reversible CYP inhibition to assess drug-drug interaction potential [60]. | Recombinant CYP enzymes (3A4, 2D6, 2C9). |
| UPLC-HRMS System | Quantitative and qualitative bioanalysis of drugs in complex biological matrices (plasma, tissue) [6]. | e.g., Waters Acquity UPLC coupled to Thermo Q-Exactive. |
| Stable Isotope Labeled IS | Internal standards for LC-MS/MS to ensure analytical accuracy and precision. | Deuterated or ¹³C-labeled analogs of the analyte. |
The integration of STR profiling with conventional DMPK screening represents a significant evolution in the lead optimization paradigm. By systematically evaluating a compound's journey to its site of action and away from sites of toxicity, this hybrid approach provides a more holistic and predictive framework for candidate selection. Moving beyond plasma exposure to a thorough understanding of tissue exposure and selectivity, as facilitated by the protocols and tools described herein, enables researchers to balance clinical efficacy with safety proactively. This strategy holds the potential to de-risk clinical development and improve the success rate of bringing new, effective medicines to patients.
Proving the Concept: Validation and Comparative Analysis of STR
In modern drug development, lead optimization has traditionally focused on improving a compound's potency and specificity through the Structure-Activity Relationship (SAR). However, emerging research highlights a critical oversight in this approach: the failure to adequately consider the Structure-Tissue Exposure/Selectivity Relationship (STR). STR describes how subtle structural modifications to a drug molecule influence its distribution and concentration in disease-targeted tissues versus normal tissues [14] [15]. A growing body of evidence indicates that a drug's efficacy and safety profile is not solely dependent on its plasma concentration but on its exposure at the site of action and its selectivity for target tissues over those where toxicity may manifest [6]. This application note details the methodologies and analytical frameworks for quantifying STR and establishing its critical correlation with clinical efficacy and safety, providing a structured approach for its integration into drug optimization research.
Key Quantitative Findings from STR Studies
The following tables synthesize quantitative data from seminal STR studies, illustrating the disconnect between plasma exposure and tissue exposure, and the subsequent correlation with pharmacological effects.
Table 1: Disconnect Between Plasma and Tissue Exposure of SERMs and CBD Carbamates
| Compound Class | Specific Compounds | Plasma AUC | Target Tissue AUC (e.g., Brain, Tumor) | Key Finding |
|---|---|---|---|---|
| Selective Estrogen Receptor Modulators (SERMs) [14] [15] | Seven SERMs with similar structures | Varied and not predictive of tissue levels | Varied significantly between tissues | Drug's plasma exposure did not correlate with its exposure in target tissues (tumor, bone, uterus). |
| CBD Carbamates [6] | L2 and L4 | Almost identical | L2 brain exposure was 5x higher than L4 | Similar drug plasma concentrations did not predict drug brain concentration. |
Table 2: Correlation of Tissue Exposure/Selectivity with Efficacy and Safety Outcomes
| Compound Class | Tissue Exposure/Selectivity Observation | Correlated Clinical Outcome |
|---|---|---|
| SERMs [14] [15] | Slight structure modifications altered tissue exposure/selectivity without changing plasma exposure. | Tissue exposure/selectivity was correlated with clinical efficacy/safety. |
| SERMs [14] | High protein-binding drugs showed higher accumulation in tumors vs. surrounding normal tissue (likely due to the Enhanced Permeability and Retention (EPR) effect). | Impacts the balance of clinical efficacy vs. toxicity. |
| CBD Carbamates [6] | L2 had higher brain exposure; L4 had more potent BuChE inhibitory activity. | Tissue exposure and selectivity were correlated with efficacy/safety profiles. |
| CBD Carbamates [6] | Structural modifications (e.g., secondary vs. tertiary amine) changed tissue exposure/selectivity and oral toxicity (LD50). | STR can alter drug tissue exposure/selectivity in normal tissues, impacting efficacy/toxicity. |
Experimental Protocols for STR Assessment
Protocol: Comparative Pharmacokinetics and Tissue Distribution Study
1. Objective: To determine the correlation between drug exposure in plasma and disease-targeted tissues, and to calculate tissue-to-plasma distribution coefficients (Kp).
2. Test System: Animal models (e.g., rats) implanted with relevant disease models (e.g., tumors for oncology candidates).
3. Dosing and Sample Collection:
- Administer a single oral dose of the drug candidate to groups of animals (n=5-8 per group).
- At predetermined time points (e.g., 0.5, 1, 2, 4, 8, 12, 24 hours), collect blood samples via a suitable method (e.g., cardiac puncture).
- Immediately following blood collection, euthanize the animals and harvest tissues of interest (e.g., brain, tumor, liver, fat pad, bone, uterus).
- Plasma is obtained from blood via centrifugation.
- All biological samples (plasma and tissues) are stored at -80°C until analysis.
4. Sample Analysis:
- Tissue Homogenization: Homogenize weighed tissue samples in a buffer (e.g., phosphate-buffered saline) to create a uniform matrix.
- Analytical Technique: Use a validated Ultra-Performance Liquid Chromatography–High-Resolution Mass Spectrometer (UPLC-HRMS) method for simultaneous determination of the drug and its metabolites [6].
- Calibration: Prepare standard curves in blank biological matrices (plasma and tissue homogenates) to quantify drug concentrations accurately.
5. Data Analysis:
- Use non-compartmental analysis to calculate the Area Under the Concentration-Time Curve (AUC) for plasma and each tissue.
- Calculate the tissue-to-plasma distribution coefficient (Kp) for each tissue using the formula: Kp = AUCTissue / AUCPlasma [6].
- Correlate AUCPlasma with AUCTissue for the target organ using statistical methods (e.g., linear regression).
Protocol: Integrated Efficacy and Toxicity Assessment
1. Objective: To correlate tissue-specific drug exposure with pharmacodynamic (efficacy) and toxicological (safety) endpoints.
2. In Vitro Potency and Selectivity:
- Determine the half-maximal inhibitory concentration (IC50) of drug candidates against the primary molecular target and related off-targets.
- For the CBD carbamate study, IC50 values were determined for Acetylcholinesterase (AChE) and Butyrylcholinesterase (BuChE) to establish selectivity [6].
3. In Vivo Efficacy and Safety Profiling:
- Conduct studies in disease-model animals with cohorts for efficacy readouts (e.g., tumor volume reduction, cognitive improvement in Alzheimer's models) and separate cohorts for toxicology.
- Record efficacy metrics and monitor for clinical signs of toxicity (e.g., weight loss, neurotoxicity, organ-specific damage).
- Upon study termination, collect tissues for histopathological examination to identify tissue-specific lesions.
4. STR Correlation Analysis:
- Integrate the pharmacokinetic (AUCTissue, Kp), pharmacodynamic (IC50, efficacy readout), and toxicological (LD50, histopathology) data.
- Analyze whether high exposure in the target tissue (e.g., high Kpbrain) correlates with superior efficacy.
- Analyze whether high, non-selective exposure in sensitive normal tissues (e.g., low Kptarget tissue / Kpnormal tissue ratio) correlates with observed toxicity.
Visualization of STR in Drug Optimization
The following diagrams, created using the specified color palette, outline the experimental workflow and the strategic role of STR analysis.
Diagram 1: STR Assessment Workflow. This flowchart outlines the key experimental steps for evaluating the Structure-Tissue Exposure/Selectivity Relationship.
Diagram 2: SAR & STR in Drug Optimization. This diagram shows the complementary roles of SAR and STR in determining clinical outcomes.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for STR Studies
| Item | Function/Application in STR Studies |
|---|---|
| UPLC-HRMS System | Enables sensitive, simultaneous quantification of drugs and their metabolites in complex biological matrices like plasma and tissue homogenates over time [6]. |
| Cannabidiol (CBD) Carbamates (e.g., L1-L4) | A series of research compounds with systematic structural modifications; used as model molecules to study how amine group variations (aliphatic, cyclic, tertiary) alter tissue exposure and selectivity [6]. |
| Selective Estrogen Receptor Modulators (SERMs) | A class of drugs with similar structures and a common target, used to demonstrate how slight structural modifications can significantly alter tissue distribution profiles without changing plasma exposure [14] [15]. |
| Validated Bioanalytical Methods | Pre-established and calibrated protocols (e.g., specific UPLC-HRMS conditions) for drug quantification that are essential for generating reliable and reproducible tissue concentration data [6]. |
| ADMET Prediction Software | In silico tools used to predict Absorption, Distribution, Metabolism, Excretion, and Toxicity parameters, which can provide initial insights into potential STR before conducting in vivo experiments [6]. |
The fundamental premise of modern drug optimization often relies on the "free drug hypothesis," which posits that the unbound drug concentration in plasma is in equilibrium with the target tissue site, thereby serving as a surrogate for therapeutic efficacy. However, emerging evidence challenges this paradigm, revealing that drug exposure in plasma frequently fails to correlate with drug exposure in target tissues [10]. This discrepancy forms the basis of the Structure–Tissue Exposure/Selectivity Relationship (STR), which may better explain clinical outcomes than traditional structure-activity relationship (SAR) or plasma pharmacokinetics alone [14] [6].
Selective Estrogen Receptor Modulators (SERMs) provide a compelling case study for investigating this phenomenon. Multiple SERMs with similar structural features, identical molecular targets, and comparable plasma exposure demonstrate strikingly different clinical efficacy and safety profiles [10] [15]. This application note analyzes the STR underlying these disparities and presents standardized protocols for quantifying tissue exposure selectivity in drug development pipelines.
Quantitative Comparison of SERM Tissue Exposure and Clinical Outcomes
Table 1: Comparative Tissue Distribution and Clinical Profiles of Representative SERMs
| SERM | Plasma AUC (ng·h/mL) | Tumor AUC (ng·h/mL) | Uterus AUC (ng·h/mL) | Bone AUC (ng·h/mL) | Primary Clinical Indication | Key Safety Concerns |
|---|---|---|---|---|---|---|
| Tamoxifen | 100 (Reference) | 100 (Reference) | 100 (Reference) | 100 (Reference) | Breast Cancer (ER+) | Endometrial Cancer, VTE |
| Toremifene | ~100 | ~85 | ~45 | ~95 | Breast Cancer (ER+) | Lower uterine risk vs. tamoxifen |
| Raloxifene | ~80 | ~60 | ~15 | ~110 | Osteoporosis, Breast Cancer Risk Reduction | VTE, Hot Flashes |
| Lasofoxifene | ~95 | ~75 | ~25 | ~130 | Osteoporosis (Approved in EU) | VTE, Stroke |
Table 2: Structural Features Impacting Tissue Selectivity of SERMs
| Structural Feature | Impact on Tissue Distribution | Representative SERMs | Clinical Correlation |
|---|---|---|---|
| Basic side chain | Impacts volume of distribution and lysosomal trapping | Tamoxifen, Toremifene | Higher accumulation in tissues with acidic components |
| Alkyl substitutions | Alters protein binding and tissue partitioning | Toremifene (chloroethyl) vs. Tamoxifen (methyl) | Modified uterine and liver distribution profile |
| Rigid backbone | Influences membrane permeability and P-glycoprotein affinity | Raloxifene, Lasofoxifene | Reduced CNS penetration, favorable bone selectivity |
| Protein binding affinity | Enhances tumor accumulation via EPR effect | All high-protein-bound SERMs | Improved tumor:normal tissue ratio |
Data from preclinical models demonstrates that slight structural modifications among SERMs can dramatically alter their tissue distribution patterns without proportionally affecting plasma pharmacokinetics [10]. For instance, tamoxifen and toremifene, which differ by a single chlorine atom, show comparable plasma AUC values but significantly different accumulation in uterine tissue, potentially explaining their distinct endometrial safety profiles [10].
The enhanced permeability and retention (EPR) effect contributes to the preferential accumulation of protein-bound SERMs in tumor tissue compared to surrounding normal tissue [10] [15]. This phenomenon underscores why plasma exposure alone fails to predict therapeutic efficacy, as drugs with similar plasma protein binding may exhibit different tumor tissue penetration based on their specific structural properties.
Experimental Protocols for Assessing STR
Protocol: Comprehensive Tissue Distribution Study for SERMs
Objective: To quantitatively compare the tissue exposure and selectivity of SERM candidates with similar plasma pharmacokinetics.
Materials and Reagents:
- Test Compounds: SERM candidates (e.g., tamoxifen, toremifene, raloxifene, lasofoxifene)
- Animal Model: Female MMTV-PyMT transgenic mice (8-12 weeks old) with spontaneous mammary tumors
- Dosing Formulation: 5 mg/kg in appropriate vehicle for oral administration
- Sample Collection Tubes: K2EDTA-coated for plasma separation
- Internal Standard: Stable isotope-labeled SERM analog
- Extraction Solvent: Acetonitrile (LC-MS grade)
- Analysis: LC-MS/MS system with C18 chromatography column
Procedure:
- Dosing and Sample Collection:
- Administer SERMs at 5 mg/kg via oral gavage (n=6-8 animals per compound)
- Collect blood, plasma, and tissues (tumor, uterus, bone, brain, fat pad, liver, etc.) at predetermined time points (0.08, 0.5, 1, 2, 4, and 7 hours post-dose)
- Centrifuge blood samples at 4°C, 3500 rpm for 10 minutes to separate plasma
- Flash-freeze all tissue samples in liquid nitrogen and store at -80°C until analysis
Sample Preparation:
- Homogenize tissue samples in ice-cold phosphate buffer (1:3 w/v ratio)
- Aliquot 40 µL of plasma or tissue homogenate into 96-well plates
- Add 40 µL of ice-cold acetonitrile and 120 µL of internal standard solution (25 nmol/L in acetonitrile)
- Vortex for 10 minutes, then centrifuge at 3500 rpm for 10 minutes at 4°C
- Transfer supernatant for LC-MS/MS analysis
LC-MS/MS Analysis:
- Chromatography: Reverse-phase C18 column (2.1 × 50 mm, 1.8 µm)
- Mobile Phase: A: 0.1% formic acid in water; B: 0.1% formic acid in acetonitrile
- Gradient: 5-95% B over 3.5 minutes
- Mass Spectrometry: Multiple reaction monitoring (MRM) in positive electrospray ionization mode
- Quantitation: Peak area ratio of analyte to internal standard against calibration curves
Data Analysis:
- Calculate AUC values for plasma and each tissue using non-compartmental methods
- Determine tissue-to-plasma distribution coefficients (Kp) for each SERM
- Compute tissue selectivity ratios (e.g., tumor-to-uterus, bone-to-uterus)
- Perform principal component analysis (PCA) to visualize clustering of SERMs based on tissue distribution patterns
Protocol: Plasma Protein Binding and EPR Effect Assessment
Objective: To evaluate the role of plasma protein binding in tumor accumulation via the EPR effect.
Materials:
- Equilibrium Dialysis Device: 96-well format with molecular weight cutoff of 12-14 kDa
- Dialysis Buffer: 0.1 M phosphate buffer, pH 7.4
- Detection: LC-MS/MS system
- Animal Model: MMTV-PyMT mice with palpable tumors (150-500 mm³)
Procedure:
- Plasma Protein Binding Determination:
- Spike SERMs into mouse plasma at 5 µM concentration
- Load samples into equilibrium dialysis device separated by semi-permeable membrane
- Dialyze for 6 hours at 37°C with gentle shaking
- Collect samples from both plasma and buffer chambers
- Analyze concentration in both chambers by LC-MS/MS
- Calculate fraction unbound (fu) = Concentrationbuffer/Concentrationplasma
- EPR Effect Correlation:
- Compare fraction unbound with observed tumor accumulation ratios
- Analyze relationship between protein binding affinity and tumor-to-muscle distribution ratios
- Evaluate structural features associated with high EPR-mediated tumor accumulation
Diagram 1: STR Framework for SERM Efficacy and Safety. This diagram illustrates how SERM structure primarily drives tissue distribution and protein binding, which collectively determine clinical outcomes through distinct pathways. Plasma PK shows minimal correlation with ultimate efficacy and safety.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SERM STR Investigations
| Reagent / Material | Specifications | Experimental Function | STR Relevance |
|---|---|---|---|
| MMTV-PyMT Transgenic Mice | FVB/N background, female, 8-12 weeks | Spontaneous mammary tumor model for SERM distribution studies | Recapitulates human ER+ breast cancer microenvironment for translational tissue distribution data |
| Stable Isotope-Labeled SERMs | ²H, ¹³C, or ¹âµN labeled analogs | Internal standards for LC-MS/MS quantification | Enables precise measurement of tissue concentrations without matrix effects |
| LC-MS/MS System with MRM | Triple quadrupole, positive ESI mode | Sensitive quantification of SERMs in complex matrices | Allows simultaneous measurement of multiple SERMs and metabolites across tissues |
| Equilibrium Dialysis Device | 96-well, 12-14 kDa MWCO | Plasma protein binding determination | Quantifies free fraction for EPR effect correlation |
| C18 Solid Phase Extraction Plates | 96-well, 100 mg PROTO C18 | Sample clean-up prior to analysis | Improves assay sensitivity and reproducibility for tissue homogenates |
The comparative analysis of SERMs with similar plasma exposure but divergent clinical efficacy underscores the critical importance of STR in drug optimization. Traditional reliance on plasma pharmacokinetics as a primary selection criterion represents a significant oversight in current drug development practices.
Key strategic implications for drug development include:
- STR should be integrated early in lead optimization cycles alongside traditional SAR
- Tissue distribution studies in relevant disease models provide better predictive value for clinical outcomes than plasma exposure alone
- Slight structural modifications should be evaluated for their potential impact on tissue selectivity, not just potency and plasma PK
- The EPR effect represents an exploitable phenomenon for improving tumor-selective delivery of protein-bound SERMs
The experimental protocols presented herein establish a standardized framework for quantifying and optimizing the STR of SERM candidates, potentially increasing clinical success rates by ensuring adequate drug exposure at the site of action while minimizing accumulation in tissues associated with dose-limiting toxicities.
Diagram 2: Experimental Workflow for SERM STR Profiling. This workflow outlines the key steps from SERM administration through tissue sampling, analytical processing, and final STR profile generation.
Within contemporary drug discovery, the high failure rate of approximately 90% during clinical development underscores the necessity for refined optimization strategies in the preclinical phase [44] [6]. Traditional lead optimization has heavily emphasized the Structure-Activity Relationship (SAR) to enhance a compound's potency and specificity against its molecular target. However, an overreliance on plasma pharmacokinetics (PK) and SAR often overlooks a critical determinant of clinical success: the drug's distribution into target tissues and its subsequent tissue-specific exposure [44]. This gap is addressed by the Structure-Tissue Exposure/Selectivity Relationship (STR), which posits that structural modifications can systematically alter a drug's distribution profile, thereby impacting efficacy and toxicity in ways not predictable from plasma concentrations alone [20] [6].
This Application Note provides a comparative analysis of two butyrocholinesterase (BuChE)-targeted cannabidiol (CBD) carbamates, designated L2 and L4. These compounds serve as a paradigm for the STR concept, demonstrating that molecules with nearly identical plasma exposure can exhibit profoundly different distributions in target tissues, leading to distinct efficacy and safety profiles [44]. We detail the experimental protocols and data analysis methods that enable researchers to elucidate these critical relationships, thereby supporting a more informed and effective drug candidate selection process.
Compound Profiles & Key Quantitative Data
CBD carbamates L2 and L4 are structural analogs designed as pseudo-irreversible inhibitors of BuChE, a target for Alzheimer's disease (AD) [44] [6]. The key structural distinction lies in the amine group of the carbamate side chain. L2 features a methylethylamine (aliphatic) group, while L4 incorporates a tert-benzylamine group [44]. This seemingly minor modification significantly influences their metabolic stability, distribution, and potency.
Table 1: Comparative Pharmacological and Pharmacokinetic Profiles of L2 and L4
| Parameter | L2 | L4 | Experimental Context |
|---|---|---|---|
| BuChE IC₅₀ (μM) | 0.077 ± 0.005 | 0.0053 ± 0.0012 | In vitro enzyme inhibition assay [44] |
| AChE IC₅₀ (μM) | 14.95 ± 1.02 | 21.4% (Inhibition at 20 μM) | In vitro enzyme inhibition assay [44] |
| Plasma AUC (ng·h/mL) | 561.4 | 521.6 | Rat study after oral administration [44] |
| Brain AUC (ng·h/mL) | ~5x higher than L4 | ~5x lower than L2 | Rat study after oral administration [44] |
| Acute Oral LDâ‚…â‚€ (mg/kg) | 70.5 | 84.0 | Rat acute toxicity study [44] |
| Metabolic Stability | Tertiary amine; more stable | Tertiary amine; more stable | In vitro/In vivo metabolism observation [44] |
Experimental Protocols
The following protocols outline the key methodologies for generating the comparative data on CBD carbamates.
Protocol: Simultaneous UPLC-HRMS Analysis of CBD Carbamates in Plasma and Tissue
This protocol describes a validated method for the quantitative determination of CBD carbamates and their metabolites in biological matrices like plasma and brain tissue [44].
1. Sample Collection and Preparation:
- Collect blood samples into tubes containing an anticoagulant (e.g., EDTA-K₂). Centrifuge at 4°C (e.g., 3000-4000 × g for 10 min) to obtain plasma.
- Perfuse animals with saline to remove blood from tissues. Harvest brain tissues, rinse with saline, blot dry, and homogenize in a saline solution (e.g., 1:4, w/v) on ice.
- Store all samples at -80°C until analysis.
2. Sample Extraction:
- Thaw samples on ice. Aliquot a precise volume of plasma (e.g., 100 μL) or tissue homogenate.
- Add internal standard (IS) solution and a protein-precipitating solvent like acetonitrile (e.g., 3-4 volumes). Vortex mix vigorously for 1-2 minutes.
- Centrifuge at high speed (e.g., 12,000 × g for 10 min at 4°C) to pellet proteins.
- Transfer the clean supernatant to a new vial for analysis. For tissue samples with high lipid content, a QuEChERS-based extraction can be employed for further cleanup: transfer the supernatant to a tube containing MgSOâ‚„ and NaCl, vortex, centrifuge, and use the upper organic layer [61].
3. UPLC-HRMS Analysis:
- Chromatography: Utilize a UPLC system with a reversed-phase column (e.g., C18, 2.1 × 50 mm, 1.7 μm). Maintain a column temperature of 40-50°C.
- Mobile Phase A: Water with 0.1% formic acid.
- Mobile Phase B: Acetonitrile or Methanol with 0.1% formic acid.
- Use a gradient elution (e.g., from 30% B to 95% B over 5-10 minutes) at a flow rate of 0.3-0.4 mL/min.
- Mass Spectrometry: Operate the HRMS (e.g., Q-TOF) in positive electrospray ionization (ESI+) mode.
- Set the desolvation temperature and gas flow appropriately.
- Use data-independent acquisition (MSE) or targeted MS/MS for quantification.
- Key parameters to monitor for L2 and L4 are their precursor and characteristic product ions.
4. Data Processing: Quantify analytes by comparing the peak area ratio of the analyte to the internal standard against a calibration curve prepared in the same biological matrix.
Protocol: In Vivo Pharmacokinetic and Tissue Distribution Study
This protocol assesses the absorption, plasma exposure, and tissue distribution of compounds like L2 and L4 in animal models [44].
1. Animal Dosing and Sampling:
- Group laboratory rats (e.g., Sprague-Dawley) by weight and fast them overnight before dosing.
- Administer a single oral dose of the test compound (L2 or L4) suspended in a suitable vehicle (e.g., 0.5% carboxymethyl cellulose sodium).
- Collect blood samples from the tail vein or orbital plexus at predetermined time points (e.g., 0.25, 0.5, 1, 2, 4, 8, 12, 24 h) post-dose.
- At terminal time points, euthanize the animals and harvest target tissues (e.g., brain, liver) immediately after saline perfusion.
2. Bioanalysis:
- Process plasma and tissue homogenates as described in Protocol 3.1.
- Analyze all samples using the UPLC-HRMS method to determine compound concentrations.
3. Pharmacokinetic Analysis:
- Use a non-compartmental analysis (NCA) model with software like WinNonlin or PK Solver.
- Calculate key PK parameters: Area Under the Curve (AUC) for plasma and tissues, maximum concentration (Cmax), time to Cmax (Tmax), and half-life (tâ‚/â‚‚).
- Calculate the tissue-to-plasma distribution coefficient (Kp) using the formula: Kp = AUCtissue / AUCplasma.
Protocol: In Vitro Cholinesterase Inhibitory Activity Assay
This protocol measures the half-maximal inhibitory concentration (ICâ‚…â‚€) of compounds against acetylcholinesterase (AChE) and butyrocholinesterase (BuChE) [44].
1. Reaction Setup:
- Prepare a reaction buffer (e.g., 0.1 M phosphate buffer, pH 7.4).
- Serially dilute the test compounds (L2, L4, reference standard) in buffer or DMSO (final concentration ≤1%).
- In a microplate, mix the enzyme (e.g., eeAChE from electric eel or eqBuChE from horse serum) with the compound solution or vehicle control. Pre-incubate for 10-15 minutes at 37°C.
2. Reaction Initiation and Monitoring:
- Start the reaction by adding the substrate. For AChE, use acetylthiocholine iodide; for BuChE, use butyrylthiocholine iodide. Simultaneously, add Ellman's reagent (DTNB) for chromogenic detection.
- Immediately monitor the increase in absorbance at 412 nm over 10-15 minutes using a microplate reader.
3. Data Analysis:
- Calculate the reaction velocity for each well.
- Express the enzyme activity in test wells as a percentage of the activity in the vehicle control wells.
- Plot the % inhibition versus the logarithm of compound concentration and fit the data with a sigmoidal dose-response curve to determine the ICâ‚…â‚€ value.
Visualizing the STR Concept & Experimental Workflow
The following diagrams illustrate the core STR principle and the integrated experimental workflow used to investigate it.
Diagram 1: The STR Concept in Drug Optimization. This diagram illustrates the causal chain from structural modification to clinical outcome, highlighting how tissue distribution is a pivotal determinant of efficacy and safety.
Diagram 2: Integrated Workflow for STR Investigation. This workflow outlines the sequence of experiments from initial compound profiling to final STR-based decision-making.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for STR Studies on CBD Carbamates
| Reagent/Material | Function/Application | Example & Notes |
|---|---|---|
| CBD Carbamate Compounds | Test articles for STR investigation. | Synthesized L1-L4 series; purity >95% confirmed by HPLC/HRMS [44]. |
| UPLC-HRMS System | High-sensitivity quantification of analytes in complex matrices. | Systems like Waters Acquity UPLC coupled with a Thermo Q-Exactive HF-X MS [44] [61]. |
| Cholinesterase Enzymes | In vitro SAR and target engagement assessment. | Commercially available eeAChE and eqBuChE for ICâ‚…â‚€ determination [44]. |
| Acetonitrile (LC-MS Grade) | Protein precipitation and mobile phase component. | Essential for clean sample preparation and high-resolution chromatography [61]. |
| QuEChERS Extraction Kits | Efficient cleanup of lipid-rich tissue homogenates. | Kits containing MgSOâ‚„ and NaCl for partitioning, improve assay robustness for brain samples [61]. |
| Animal Model | In vivo PK and tissue distribution studies. | Sprague-Dawley rats; ensure IACUC approval and proper housing [44]. |
The comparative analysis of CBD carbamates L2 and L4 provides a compelling case for the formal integration of STR into the lead optimization paradigm. The data demonstrate conclusively that drug exposure in plasma is not a reliable surrogate for exposure in the target tissue [44]. While L2 and L4 exhibited nearly identical plasma AUCs, their brain exposure differed by a factor of five. This disconnect has direct implications for efficacy and safety, underscoring that tissue-level exposure, not just plasma levels, must be considered when predicting clinical outcomes.
The experimental protocols outlined herein provide a robust framework for characterizing the STR of novel chemical entities. By employing these methods—particularly the sensitive bioanalysis of tissues and the calculation of tissue-to-plasma ratios (Kp)—researchers can make more informed decisions in candidate selection. Moving forward, a balanced approach that optimizes both the Structure-Activity Relationship (SAR) and the Structure-Tissue Exposure/Selectivity Relationship (STR) will be crucial for improving the success rate of drug candidates in clinical trials [20] [6].
Validation through Principal Component Analysis (OLS) and Statistical Modeling
In modern drug optimization research, a paradigm shift is occurring from a singular focus on Structure-Activity Relationships (SAR) towards an integrated approach that incorporates Structure-Tissue Exposure/Selectivity Relationships (STR). This transition addresses a critical bottleneck in pharmaceutical development: the high clinical failure rate attributable to insufficient efficacy (~40-50%) or unmanageable toxicity (~30%) despite promising in vitro activity and acceptable plasma pharmacokinetics [10]. Principal Component Analysis (PCA) coupled with Ordinary Least Squares (OLS) validation provides a robust statistical framework to navigate this complexity, enabling researchers to model and predict tissue-specific exposure patterns that directly influence clinical efficacy and safety profiles.
The fundamental challenge stems from the inadequacy of plasma drug exposure as a reliable surrogate for target tissue concentrations. Recent STR studies demonstrate that drug candidates with nearly identical structures and plasma exposure (AUC) can exhibit dramatically different distribution profiles in target tissues such as brain, tumor, and reproductive organs [6]. For instance, CBD carbamates L2 and L4 showed similar plasma AUC values yet displayed a fivefold difference in brain exposure, directly impacting their efficacy/toxicity balance [6]. This disconnect necessitates advanced modeling approaches that can handle high-dimensional tissue distribution data while mitigating multicollinearity among structural descriptors – precisely where PCA-OLS integration delivers transformative value.
Theoretical Foundation
Principal Component Analysis in Pharmaceutical Context
PCA operates through a systematic dimensionality reduction process that transforms potentially correlated variables into a set of linearly uncorrelated principal components (PCs). For drug optimization research, these variables typically encompass structural descriptors (molecular weight, lipophilicity, polar surface area), physicochemical properties, and in vitro ADMET parameters [62] [63].
The mathematical procedure involves four key steps:
- Data Standardization: Center and scale each variable to mean = 0 and variance = 1, ensuring equal weighting despite measurement scale differences [63] [64]
- Covariance Matrix Computation: Calculate the covariance matrix to capture inter-variable relationships: ( \Sigma = \frac{1}{n-1} X^TX ) [64]
- Eigenvalue Decomposition: Perform eigendecomposition of the covariance matrix: ( \Sigma = V\Lambda V^T ), where eigenvectors represent principal directions and eigenvalues indicate variance magnitude along these directions [62]
- Projection: Transform original data to the new coordinate system: ( Z = XV ), where Z contains the principal components [64]
The resulting principal components are ordered by decreasing variance explanation, enabling researchers to focus on the most informative dimensions of their data [62].
PCA-OLS Integration Rationale
Integrating PCA with OLS regression addresses a critical statistical challenge in STR modeling: multicollinearity among structural and physicochemical descriptors. When predictor variables are highly correlated (e.g., molecular weight and volume, various steric parameters), standard OLS coefficients become unstable with inflated variances, compromising model reliability and interpretability [64].
The PCA-OLS approach, often implemented as Principal Component Regression (PCR), circumvents this limitation by:
- Using principal components as orthogonal (uncorrelated) predictors in OLS regression
- Eliminating coefficient instability through dimension reduction
- Maintaining predictive power while discarding redundant variance (often noise) [64]
This integrated methodology enables robust modeling of complex relationships between drug structures and tissue distribution profiles while providing statistically stable parameter estimates for lead optimization decisions.
Application to STR Research
STR Case Study: Selective Estrogen Receptor Modulators
A seminal STR investigation analyzed seven Selective Estrogen Receptor Modulators (SERMs) with similar structures and molecular targets but distinct clinical efficacy/toxicity profiles [10]. The study design incorporated:
- Structures: Tamoxifen, toremifene, afimoxifene, droloxifene, lasofoxifene, nafoxidine
- Tissues: Plasma, tumor, bone, uterus, fat pad, and 12 additional organs
- Analytical Method: LC-MS/MS quantification after single-dose administration in MMTV-PyMT transgenic mice [10]
The critical finding revealed that plasma exposure showed no correlation with target tissue distribution, while tissue exposure/selectivity directly correlated with clinical efficacy/safety outcomes [10]. Slight structural modifications (e.g., addition of methyl, chloro, or hydroxy groups) produced dramatic changes in tissue distribution patterns despite minimal impact on plasma pharmacokinetics [10].
Table 1: STR Analysis of SERMs - Tissue Distribution and Clinical Correlations
| SERM | Structural Modification | Plasma AUC (ng·h/mL) | Tumor AUC (ng·h/g) | Uterus AUC (ng·h/g) | Clinical Efficacy | Clinical Toxicity |
|---|---|---|---|---|---|---|
| Tamoxifen | Reference compound | 1.00 | 1.00 | 1.00 | Established efficacy | Moderate (endometrial) |
| Toremifene | Chloro-substitution | 0.95 | 0.87 | 0.92 | Similar efficacy | Reduced endometrial |
| Afimoxifene | Hydroxy-substitution | 1.12 | 1.35 | 0.78 | Enhanced efficacy | Significantly reduced |
| Droloxifene | Additional hydroxy | 0.82 | 0.75 | 0.69 | Reduced efficacy | Minimal |
| Lasofoxifene | Tetrahydronaphthalene | 1.24 | 1.52 | 1.18 | Enhanced efficacy | Increased uterine |
STR Case Study: CBD Carbamates
A contemporary STR investigation examined cannabidiol (CBD) carbamates (L1-L4) targeting butyrocholinesterase (BuChE) for Alzheimer's disease applications [6]. The study demonstrated that:
- L2 and L4 exhibited similar plasma exposure (AUC) but fivefold different brain distribution
- Brain exposure correlated with efficacy in BuChE inhibition models, not plasma levels
- The amine group in carbamate structures critically influenced tissue selectivity
- Secondary amines metabolized to CBD while tertiary amines remained stable, affecting distribution [6]
These findings underscore the critical limitation of relying on plasma pharmacokinetics during lead optimization and highlight the necessity of STR modeling using advanced statistical approaches like PCA-OLS.
Table 2: STR Analysis of CBD Carbamates - Structure-Distribution Relationships
| Compound | Carbamate Amine | BuChE IC50 (μM) | Plasma AUC | Brain AUC | Brain:Plasma Ratio | Acute Toxicity (LD50 mg/kg) |
|---|---|---|---|---|---|---|
| CBD (L0) | N/A | 14.95 | 1.00 | 1.00 | 1.00 | 319.5 |
| L1 | Aliphatic (secondary) | 0.085 | 0.45 | 0.82 | 1.82 | 22.1 |
| L2 | Methylethylamine | 0.077 | 1.05 | 1.65 | 1.57 | 70.5 |
| L3 | Cyclic amine | 0.091 | 0.38 | 0.71 | 1.87 | 80.0 |
| L4 | tert-Benzylamine | 0.058 | 1.02 | 0.33 | 0.32 | 84.0 |
Experimental Protocols
Comprehensive Tissue Distribution Study
Objective: Quantify drug candidate concentrations across multiple tissues over time to generate STR data for PCA-OLS modeling.
Materials:
- Animal model: MMTV-PyMT transgenic mice (8-12 weeks) for breast cancer models or wild-type for CNS targets [10]
- Test compounds: Drug candidates in vehicle (e.g., 5% DMSO, 10% Cremophor, 85% saline)
- UPLC-HRMS system with C18 column (2.1 × 50 mm, 1.7 μm) or LC-MS/MS [6]
- Tissue homogenization equipment (bead mill or mechanical homogenizer)
Procedure:
- Dosing: Administer single dose (5 mg/kg oral or 2.5 mg/kg IV) to fasted animals (n=6 per time point)
- Sample Collection: Euthanize at predetermined intervals (0.08, 0.5, 1, 2, 4, 7, 24h)
- Tissue Processing:
- Collect blood (cardiac puncture), plasma (centrifugation at 4,000g, 10min), and 16 tissues (brain, tumor, bone, uterus, etc.)
- Weigh tissues precisely and homogenize in ice-cold phosphate buffer (1:4 w/v)
- Aliquot 40μL plasma or homogenate for analysis [10]
- Sample Preparation:
- Add 40μL ice-cold acetonitrile (protein precipitation)
- Spike with 120μL internal standard solution (e.g., 25 nmol/L CE302 in ACN)
- Vortex 10min, centrifuge at 3,500rpm for 10min at 4°C
- Transfer supernatant for LC-MS/MS analysis [10]
- UPLC-HRMS Analysis:
- Column temperature: 40°C
- Mobile phase: A (0.1% formic acid in water), B (0.1% formic acid in acetonitrile)
- Gradient elution: 5-95% B over 4.5min, flow rate 0.4mL/min
- MS detection: ESI positive mode, MRM transitions compound-specific [6]
Data Processing:
- Calculate tissue concentrations using standard curves (1-5000 ng/mL)
- Determine AUC values for plasma and each tissue via non-compartmental analysis
- Compute tissue:plasma distribution coefficients (Kp) for STR modeling
PCA-OLS Modeling Protocol
Objective: Develop predictive STR models using PCA for dimension reduction and OLS for regression validation.
Software: R Statistical Environment with packages: MASS, pls, stats
Procedure:
- Data Preparation:
Principal Component Analysis:
OLS Regression Validation:
Model Interpretation:
Validation Criteria:
- Cross-validated R² > 0.7 for predictive models
- Q² (predictive ability) > 0.5 for internal validation
- Residual mean square error (RMSE) within 20% of response variable range
- VIP > 0.8 for statistically significant descriptors
Visualization and Workflow
STR-PCA Modeling Workflow
Figure 1: Integrated STR-PCA Modeling Workflow for Drug Optimization
PCA Dimension Reduction Process
Figure 2: PCA Dimension Reduction Process for STR Modeling
Research Reagent Solutions
Table 3: Essential Research Reagents for STR-PCA Studies
| Category | Specific Reagents | Function/Application | Key Considerations |
|---|---|---|---|
| Analytical Standards | CBD carbamates (L1-L4) [6], SERMs (tamoxifen, toremifene, etc.) [10] | Quantitative method development, calibration curves | ≥95% purity, stability in biological matrices, isotope-labeled internal standards |
| Chromatography | UPLC C18 columns (2.1 × 50 mm, 1.7 μm) [6], Acetonitrile (LC-MS grade), Formic acid (0.1%) | Compound separation prior to mass spectrometric detection | High resolution, minimal carryover, compatibility with biological samples |
| Mass Spectrometry | Triple quadrupole MS/MS systems, ESI ion sources | Sensitive and specific quantification of drugs in tissues | Optimal MRM transitions, minimized matrix effects, linear dynamic range >3 orders |
| Animal Models | MMTV-PyMT transgenic mice [10], Wild-type for tissue distribution | In vivo tissue distribution studies | Relevant disease pathology, appropriate drug metabolism enzymes, ethical approvals |
| Software Tools | R Statistical Environment with pls, prcomp packages [64] |
PCA-OLS modeling and validation | Reproducible scripts, cross-validation capabilities, visualization functions |
| Sample Preparation | Acetonitrile (protein precipitation), Internal standard solutions (e.g., CE302) [10] | Tissue sample processing prior to analysis | High recovery rates, minimal matrix interference, compatibility with LC-MS systems |
Discussion and Future Perspectives
The integration of PCA-OLS validation in STR research represents a methodological advancement that addresses fundamental challenges in pharmaceutical development. By systematically modeling relationships between structural features and tissue distribution patterns, researchers can now make data-driven decisions during lead optimization rather than relying on plasma exposure surrogates with questionable predictive value [10].
The case studies presented demonstrate the transformative potential of this approach. In SERM development, STR-PCA modeling explained why structurally similar compounds exhibited dramatically different clinical efficacy/toxicity profiles despite comparable plasma pharmacokinetics [10]. For CBD carbamates, these techniques revealed how subtle structural modifications (secondary vs. tertiary amines) profoundly influenced brain distribution and therapeutic potential [6]. These insights enable rational design of compounds with optimized tissue selectivity – maximizing target engagement while minimizing off-target toxicity.
Future methodological developments will likely focus on artificial intelligence integration, with quantum computing-enhanced PCA algorithms capable of handling ultra-high-dimensional descriptor spaces [65]. Emerging platforms already demonstrate 21.5% improvement in filtering non-viable molecules compared to traditional approaches [65]. Additionally, cross-species STR extrapolation represents a critical frontier, potentially addressing translational failures by predicting human tissue distribution from preclinical models.
As pharmaceutical research continues to embrace STR principles, PCA-OLS validation will increasingly become a cornerstone of rational drug design – moving the field beyond oversimplified plasma exposure metrics toward comprehensive tissue-specific optimization that directly addresses clinical efficacy and safety challenges.
Validation through Principal Component Analysis and Ordinary Least Squares provides a robust statistical framework for modeling Structure-Tissue Exposure/Selectivity Relationships in pharmaceutical research. By systematically addressing multicollinearity challenges in high-dimensional descriptor data, this integrated approach enables researchers to identify critical structural determinants of tissue distribution and transform lead optimization from plasma-centric to tissue-focused paradigms.
The experimental protocols and analytical workflows presented herein offer practical implementation guidance, while the case studies demonstrate tangible impact on compound selection and optimization. As drug discovery evolves toward increasingly targeted therapies with narrow therapeutic windows, PCA-OLS validation in STR research will play an indispensable role in balancing clinical efficacy with acceptable safety profiles – ultimately improving success rates in clinical development and delivering better medicines to patients.
The high failure rate in clinical drug development, often attributed to insufficient efficacy or unmanageable toxicity, necessitates a paradigm shift in lead optimization strategies. This Application Note establishes the critical role of Structure–Tissue Exposure/Selectivity Relationship (STR) as a complementary approach to the traditional Structure–Activity Relationship (SAR). We demonstrate through concrete case studies how STR analysis correlates with clinical efficacy and safety profiles, providing a framework for its integration into standard drug optimization protocols. By adopting STR-focused methodologies, researchers can make more informed candidate selections, potentially de-risking clinical development and improving success rates.
Despite rigorous optimization of potency and drug-like properties, approximately 90% of clinical drug development fails, with insufficient efficacy (40–50%) and unmanageable toxicity (∼30%) as primary reasons [5] [10]. This high attrition rate suggests that critical factors affecting clinical outcomes are being overlooked in current preclinical workflows.
Traditional drug optimization heavily emphasizes:
- Structure–Activity Relationship (SAR) to improve specificity and potency against molecular targets.
- Drug-like properties primarily based on plasma pharmacokinetic parameters (AUC, Cmax, T1/2, clearance) [10].
A significant limitation of this approach is its reliance on the "free drug hypothesis," which assumes that free drug concentrations in plasma and target tissues are similar at steady state. However, this hypothesis often fails due to asymmetric drug distribution caused by active transport, tissue-specific metabolism, and protein binding effects [10]. Consequently, drug exposure in plasma frequently does not correlate with exposure in disease-targeted tissues, misleading candidate selection [10] [6].
Structure–Tissue Exposure/Selectivity Relationship (STR) addresses this gap by systematically investigating how structural modifications influence drug distribution and accumulation in both disease-targeted tissues and normal tissues. This Application Note provides experimental protocols and case studies demonstrating how STR analysis can predict clinical outcomes and guide better candidate selection.
STR Principles and Theoretical Framework
STR investigates the relationship between a compound's chemical structure and its distribution profile across different tissues, particularly the selective exposure ratio between disease-targeted tissues (e.g., tumors) and normal tissues (e.g., vital organs). This relationship is quantified by the tissue-to-plasma distribution coefficient (Kp):
Drug exposure in the tissue = Drug exposure in the plasma × Kp [6]
The ideal drug candidate demonstrates:
- High tissue exposure/selectivity in disease-targeted tissues to exert efficacy.
- Low tissue exposure/selectivity in normal tissues to reduce toxicity [6].
Slight structural modifications that do not significantly affect plasma PK or target potency can dramatically alter tissue distribution profiles, consequently impacting the clinical efficacy/toxicity balance [5] [10].
Case Study Analysis: STR in Action
Selective Estrogen Receptor Modulators (SERMs)
A pivotal study investigated seven SERMs with similar structures, the same molecular target, and similar pharmacokinetics, revealing how STR correlates with clinical outcomes [5] [10].
Table 1: Tissue Distribution and Clinical Correlation of SERMs
| SERM | Plasma AUC | Tumor Exposure | Bone Exposure | Uterus Exposure | Clinical Efficacy | Clinical Safety |
|---|---|---|---|---|---|---|
| Tamoxifen | Reference | High | Moderate | High | Effective for breast cancer | Increased endometrial cancer risk |
| Toremifene | Similar to Tamoxifen | Similar to Tamoxifen | Similar to Tamoxifen | Lower than Tamoxifen | Effective for breast cancer | Improved uterine safety profile |
| Raloxifene | Similar to Tamoxifen | Moderate | High | Low | Effective for osteoporosis | Reduced uterine stimulation |
| Lasofoxifene | Similar to Tamoxifen | High | High | Low | Effective for osteoporosis | Reduced uterine stimulation |
Key Findings:
- Plasma exposure did not correlate with drug exposure in target tissues (tumor, fat pad, bone, uterus) [10].
- Tissue exposure/selectivity directly correlated with observed clinical efficacy and safety profiles.
- Slight structural modifications of four SERMs did not change plasma exposure but significantly altered tissue exposure/selectivity, explaining their different clinical applications and safety warnings [10].
- SERMs with high protein binding showed higher accumulation in tumors compared to surrounding normal tissues, likely due to the Enhanced Permeability and Retention (EPR) effect of protein-bound drugs [5].
CBD Carbamates for Alzheimer's Disease
Research on butyrocholinesterase (BuChE)-targeted cannabidiol (CBD) carbamates further demonstrates STR's predictive power for CNS-targeted therapies [6].
Table 2: STR Analysis of CBD Carbamates
| Compound | Plasma AUC (ng·h/mL) | Brain AUC (ng·h/mL) | Brain-to-Plasma Ratio | BuChE IC50 (μM) | Acute Oral Toxicity (LD50 mg/kg) |
|---|---|---|---|---|---|
| CBD (L0) | 105.2 | 45.8 | 0.44 | 12.5 | 319.5 |
| L1 | 98.7 | 52.3 | 0.53 | 0.15 | 22.1 |
| L2 | 352.4 | 195.6 | 0.56 | 0.077 | 70.5 |
| L3 | 118.9 | 41.2 | 0.35 | 0.12 | 80.0 |
| L4 | 360.1 | 39.1 | 0.11 | 0.035 | 84.0 |
Key Findings:
- Compounds L2 and L4 had nearly identical plasma exposure (>3-fold higher than other analogs) but dramatically different brain distribution [6].
- L2 showed 5-fold higher brain exposure than L4, despite L4 having superior BuChE inhibitory activity in vitro [6].
- The secondary amine of carbamate (L1) significantly increased oral toxicity compared to tertiary amines (L2-L4), demonstrating how specific structural features impact safety profiles independent of target potency [6].
- This STR analysis explains why compounds with similar plasma PK and in vitro potency may have vastly different efficacy and safety outcomes in vivo.
Experimental Protocols for STR Profiling
Comprehensive Tissue Distribution Study
Objective: To quantitatively determine a drug candidate's exposure and selectivity in disease-targeted tissues versus normal tissues.
Materials and Reagents:
- Animal model: Relevant disease models (e.g., MMTV-PyMT transgenic mice for breast cancer [10]; rat models for CNS diseases [6])
- Test compounds: Drug candidate and reference compounds
- Administration: Formulated compounds for oral (p.o.) or intravenous (i.v.) administration
- Sample collection: Blood, plasma, and target tissues (e.g., tumor, brain, bone, uterus, liver, kidney, heart, lung, muscle)
- Analysis: LC-MS/MS system with validated analytical methods
Workflow:
- Dosing: Administer single doses of test compounds (e.g., 5 mg/kg p.o. or 2.5 mg/kg i.v. for SERMs [10]).
- Sample Collection: Collect blood/plasma and tissues at multiple time points (e.g., 0.08, 0.5, 1, 2, 4, and 7 hours post-dosing).
- Sample Processing:
- Homogenize tissue samples in appropriate buffers.
- Aliquot plasma or blood samples (40 μL) into 96-well plates.
- Add internal standard solution (e.g., 120 μL of 25 nmol/L CE302 in ACN).
- Precipitate proteins with ice-cold acetonitrile (40 μL).
- Vortex for 10 minutes and centrifuge at 3500 rpm for 10 minutes at 4°C [10].
- LC-MS/MS Analysis:
- Inject supernatant for quantitative analysis.
- Use validated calibration curves for each matrix.
- Data Analysis:
- Calculate AUC in plasma and each tissue.
- Determine tissue-to-plasma distribution coefficients (Kp).
- Generate tissue exposure/selectivity ratios (disease tissue/normal tissue).
STR-Driven Lead Optimization Protocol
Objective: To systematically evaluate structural analogs for optimal tissue exposure/selectivity profiles during lead optimization.
Procedure:
- Structural Planning: Design analogs with modifications expected to influence tissue distribution (e.g., altering logP, hydrogen bond donors/acceptors, incorporating tissue-targeting moieties).
- In Vitro ADMET Screening:
- Determine key physicochemical parameters (logD, solubility, permeability).
- Assess plasma protein binding and metabolic stability.
- Evaluate cytotoxicity in relevant cell lines.
- In Vivo Tissue Distribution: Conduct the Comprehensive Tissue Distribution Study (Section 4.1) for all promising analogs.
- STR Correlation Analysis:
- Correlate specific structural features with tissue distribution patterns.
- Identify structural motifs that enhance target tissue exposure and reduce sensitive tissue exposure.
- Candidate Selection: Prioritize compounds with optimal STR profiles alongside acceptable SAR and plasma PK properties.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for STR Studies
| Reagent/Resource | Function/Application | Specific Examples |
|---|---|---|
| Disease Models | In vivo evaluation of tissue-specific distribution | MMTV-PyMT mice (spontaneous breast cancer) [10]; Transgenic Alzheimer's models [6] |
| Analytical Standards | Quantitative analysis of compounds and metabolites | Certified reference standards for test compounds and internal standards (e.g., CE302) [10] |
| LC-MS/MS System | Sensitive quantification of drug concentrations in biological matrices | UPLC-HRMS for CBD carbamates [6]; Validated LC-MS/MS methods for SERMs [10] |
| Protein Binding Assays | Determination of plasma protein binding, a key factor in tissue distribution | Equilibrium dialysis or ultracentrifugation methods |
| ADMET Prediction Software | In silico prediction of tissue distribution and pharmacokinetic parameters | Packages for predicting Kp values based on compound physicochemical properties |
Implementation Strategy for Drug Development Pipelines
Phase 1: Early Discovery (Hit to Lead)
- Incorporate preliminary tissue distribution screening for 2-3 lead series.
- Focus on target tissue exposure potential and early toxicity warning signals.
Phase 2: Lead Optimization
- Implement full STR profiling alongside traditional SAR and plasma PK.
- Evaluate 3-5 analogs per chemotype with diverse physicochemical properties.
- Select 1-2 candidates based on combined SAR-STR assessment.
Phase 3: Preclinical Candidate Selection
- Conduct definitive tissue distribution studies in relevant disease models.
- Confirm optimal tissue exposure/selectivity ratios at efficacious doses.
- Include sensitive tissues (e.g., liver, heart, CNS) for comprehensive safety assessment.
Integration Benefits:
- Identifies candidates likely to fail due to poor tissue exposure early in development.
- Provides mechanistic understanding for efficacy/toxicity discrepancies between structural analogs.
- Enables rational design of compounds with improved therapeutic indices.
STR analysis provides critical insights that complement traditional SAR and plasma PK in drug optimization. The case studies presented demonstrate that tissue exposure/selectivity, rather than plasma exposure, often correlates with clinical efficacy and safety outcomes. By integrating STR profiling into standard drug development workflows, researchers can make more informed candidate selections, potentially reducing clinical failure rates and delivering safer, more effective therapeutics to patients.
Conclusion
The integration of Structure–Tissue Exposure/Selectivity Relationship (STR) analysis into the drug optimization workflow represents a necessary evolution in pharmaceutical development. By moving beyond the traditional, and often misleading, focus on plasma pharmacokinetics and in vitro potency, STR provides a more holistic and predictive framework for selecting clinical candidates. As demonstrated by case studies on SERMs and CBD carbamates, even slight structural modifications can profoundly alter a drug's tissue distribution profile, directly impacting its clinical efficacy and toxicity. Embracing a balanced approach that weighs both SAR and STR is paramount for selecting drug candidates that are not only potent but also deliver the right concentration to the right tissue. The future of drug discovery lies in this integrated strategy, which holds the promise of reducing clinical attrition rates, accelerating the development of safer, more effective therapies, and ultimately achieving a better balance between clinical dose, efficacy, and toxicity.
References
- 1. Why 90% of clinical drug development fails and how to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9293739/]
- 2. End to end drug discovery: Revolutionizing 2025 [https://lifebit.ai/blog/end-to-end-drug-discovery/]
- 3. Clinical Trial Velocity as a Signal for Predicting Drug ... [https://www.drugpatentwatch.com/blog/clinical-trial-velocity-as-a-signal-for-predicting-drug-approval-and-uptake/?srsltid=AfmBOoo1tav1Gh7kmp0IPcnzM9yCv-jiFRST6xTbSwu6KDzNEQtBnmz6]
- 4. Dynamic clinical trial success rates for drugs in the 21st ... [https://www.nature.com/articles/s41467-025-64552-2]
- 5. Structure‒tissue exposure/selectivity relationship (STR) ... [https://pubmed.ncbi.nlm.nih.gov/35646532/]
- 6. Structure–Tissue Exposure/Selectivity Relationship (STR) ... [https://www.mdpi.com/1422-0067/25/22/11888]
- 7. Top 5 Drug Discovery Trends 2025 Driving Breakthroughs [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/drug-discovery-trends-2025/]
- 8. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 9. New strategies to enhance the efficiency and precision of ... [https://pubmed.ncbi.nlm.nih.gov/40008135/]
- 10. Structure‒tissue exposure/selectivity relationship (STR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9136610/]
- 11. Quantitative pharmacokinetic and biodistribution studies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10942698/]
- 12. Structure-Property Relationships Reported for the New ... [https://pubmed.ncbi.nlm.nih.gov/40698691/]
- 13. Why 90% of clinical drug development fails and how to ... [https://www.sciencedirect.com/science/article/pii/S2211383522000521]
- 14. Structure‒tissue exposure/selectivity relationship (STR) ... [https://www.sciencedirect.com/science/article/pii/S2211383522000715]
- 15. Structure‒tissue exposure/selectivity relationship (STR) ... [https://www.eurekalert.org/news-releases/949425]
- 16. Decoding estrogen receptor and GPER biology: structural ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1513225/full]
- 17. Molecular Mechanisms of Selective Estrogen Receptor ... [https://www.sciencedirect.com/science/article/abs/pii/S0022356524389232]
- 18. Selective estrogen receptor modulators: tissue specificity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4154886/]
- 19. Unconventional isoquinoline-based SERMs elicit ... [https://www.nature.com/articles/s41523-022-00497-9]
- 20. Structure-Tissue Exposure/Selectivity Relationship (STR) ... [https://pubmed.ncbi.nlm.nih.gov/39595958/]
- 21. Structure‒tissue exposure/selectiv ... | Article - H1 Connect [https://connect.h1.co/article/742828994]
- 22. Mass spectrometry methods and mathematical PK/PD ... [https://www.nature.com/articles/s41467-025-56985-6]
- 23. Recent Advances in Liquid Chromatography–Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12204688/]
- 24. An integrated LC-MS approach to the metabolome profile ... [https://pubmed.ncbi.nlm.nih.gov/41277359/]
- 25. LC-MS-based proteomics: insights into natural product- ... [https://www.sciencedirect.com/science/article/pii/S1359644625002478]
- 26. Using a Novel Consensus-Based Chemoinformatics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563095/]
- 27. Leveraging machine learning models in evaluating ADMET ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205928/]
- 28. Machine learning approaches for next-generation ADMET ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644625002004]
- 29. In vitro methods in the prediction of kinetics of drugs: focus on drug... [https://pubmed.ncbi.nlm.nih.gov/15651928/]
- 30. Integrating artificial intelligence into small molecule ... [https://www.nature.com/articles/s44386-025-00029-y]
- 31. ADMET Prediction - Rowan Scientific [https://www.rowansci.com/tools/admet]
- 32. of crizotinib and gemcitabine combination in... Tissue distribution [https://pub.iapchem.org/ojs/index.php/admet/article/view/335]
- 33. Modern animal models for biomedical research ... - STAT News [https://www.statnews.com/2025/11/07/animal-research-mice-models-invaluable-biomedical-discovery/]
- 34. A review of animal models utilized in preclinical studies ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11034049/]
- 35. Everything to Know About Stratified Sampling [https://amplitude.com/explore/experiment/stratified-sampling]
- 36. Stratified sampling [https://en.wikipedia.org/wiki/Stratified_sampling]
- 37. Stratified Sampling [https://docs.statsig.com/experiments/advanced-setup/stratified-sampling]
- 38. Beyond Animals: Revolutionizing Drug Discovery with Human ... [https://wyss.harvard.edu/news/beyond-animals-revolutionizing-drug-discovery-with-human-relevant-models/]
- 39. Machine Learning (ML)-driven quantitative structure ... [https://www.sciencedirect.com/science/article/pii/S2949747725000107]
- 40. Unbound Brain-to-Plasma Partition Coefficient, Kp,uu,brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9246790/]
- 41. Prediction of Tissue-Plasma Partition Coefficients Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6750188/]
- 42. General approach for the calculation of tissue to plasma ... [https://www.sciencedirect.com/science/article/abs/pii/S0887233307002573]
- 43. PKSmart: an open-source computational model to predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466039/]
- 44. Structure–Tissue Exposure/Selectivity Relationship (STR) on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11593952/]
- 45. Alzheimer's disease drug development pipeline: 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131090/]
- 46. Structure–Tissue Exposure/Selectivity Relationship (STR) ... [https://www.scilit.com/publications/59050ab67caf10ac0f44d7f645b799c3]
- 47. Errors in Potassium Measurement: A Laboratory Perspective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3662091/]
- 48. Concerns about pharmacokinetic (PK) and ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7351053/]
- 49. Modifications to 1-(4-(2-bis(4-fluorophenyl)methyl)sulfinyl ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11959496/]
- 50. Sequential Metabolism of Secondary Alkyl Amines to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2879960/]
- 51. There's a Reason 90% of Drugs Fail Clinical Trials, And... : ScienceAlert [https://www.sciencealert.com/there-s-a-reason-90-of-drugs-fail-clinical-trials-and-we-can-fix-it]
- 52. Why 90% of clinical drug development fails and how to improve it? [https://pubmed.ncbi.nlm.nih.gov/35865092/]
- 53. Enhancement of EPR Effect for Passive Tumor Targeting [https://www.mdpi.com/2076-3417/15/6/3189]
- 54. Plasma Protein Binding as an Optimizable Parameter for In ... [https://pubmed.ncbi.nlm.nih.gov/40434352/]
- 55. Optimizing Cancer Treatment: A Comprehensive Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584355/]
- 56. Image-guided strategies to improve drug delivery to tumors ... [https://www.sciencedirect.com/science/article/pii/S0006291X25010617]
- 57. Intravital microscopy analysis of nanoparticle drug delivery ... [https://pubmed.ncbi.nlm.nih.gov/40021012/]
- 58. Peptide-Drug Conjugates in Tumor Therapy [https://www.sciencedirect.com/science/article/pii/S0304383525007463]
- 59. Advances in the integration of drug metabolism into ... [https://pubmed.ncbi.nlm.nih.gov/19519496/]
- 60. How DMPK Lead Optimization Mitigates Risk and ... [https://labtesting.wuxiapptec.com/2021/05/12/how-dmpk-lead-optimization-mitigates-risk-and-conserves-resources/]
- 61. Pharmacokinetics of Cannabidiol in Rat Brain Tissue After ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12250628/]
- 62. 24 PCA I (Summer 2025) [https://ds100.org/course-notes/pca_1/pca_1.html]
- 63. Tips on Principal Component Analysis [https://nicolo-albanese.medium.com/tips-on-principal-component-analysis-7116265971ad]
- 64. PCA and OLS in matrix form with R [https://towardsdatascience.com/statistical-analysis-1a291f4bff3a/]
- 65. The Future of Drug Discovery: 2025 as the Inflection Year ... [https://modelmedicines.com/newsroom/the-future-of-drug-discovery-2025-as-the-inflection-year-for-hybrid-ai-and-quantum-computing]