Beyond Direct Comparison: A Modern Framework for Evaluating Therapeutic Equivalence with Network Meta-Analysis
Network meta-analysis (NMA) has become an indispensable tool for comparative effectiveness research, enabling the evaluation of therapeutic equivalence and hierarchy among multiple interventions in the absence of head-to-head trials.
Beyond Direct Comparison: A Modern Framework for Evaluating Therapeutic Equivalence with Network Meta-Analysis
Abstract
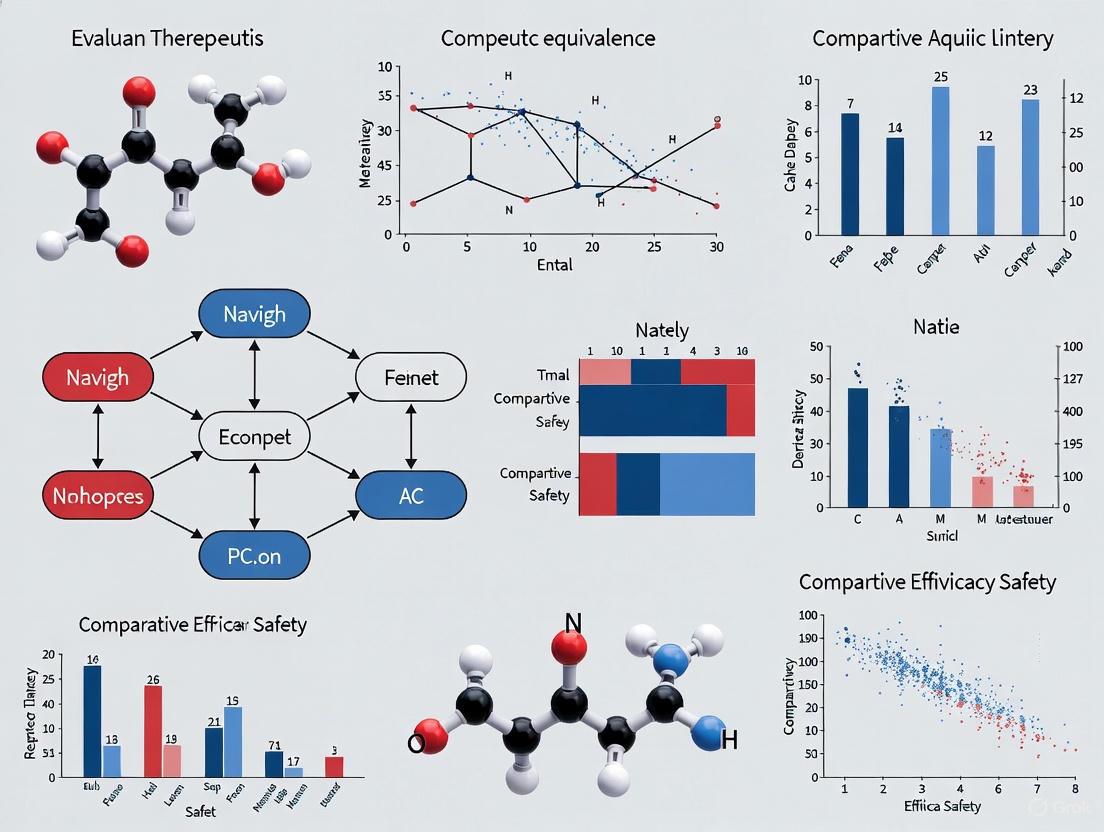
Network meta-analysis (NMA) has become an indispensable tool for comparative effectiveness research, enabling the evaluation of therapeutic equivalence and hierarchy among multiple interventions in the absence of head-to-head trials. This article provides a comprehensive guide for researchers and drug development professionals on the foundational principles, advanced methodologies, and critical appraisal techniques required for robust NMA. Drawing on contemporary case studies from cardiology, oncology, and rare diseases, we explore the entire NMA workflow—from systematic literature review and network feasibility assessment to the application of novel statistical metrics like SUCRA and loss-adjusted expected value for risk-averse decision-making. The content addresses common pitfalls in establishing transitivity, interpreting uncertainty, and validating findings, ultimately empowering scientists to generate reliable evidence for clinical guidelines and health technology assessments.
The Foundations of Therapeutic Equivalence: Core Concepts and When to Use NMA
Defining Therapeutic Equivalence and Treatment Hierarchy in Modern Drug Development
In modern drug development, therapeutic equivalence is a fundamental regulatory and clinical concept. For generic drugs, it is established by demonstrating bioequivalence to a reference listed drug, proving that the generic drug has the same active ingredient, dosage form, strength, and route of administration, and that it is absorbed at the same rate and extent as the innovator product [1]. This principle allows generic manufacturers to utilize an Abbreviated New Drug Application (ANDA) pathway, bypassing the need for extensive and costly new clinical trials by relying on the FDA's previous finding of safety and efficacy for the reference drug [1].
Beyond the generic drug context, comparing multiple treatment options for a condition requires advanced statistical methodologies. Network Meta-Analysis (NMA) has emerged as a powerful extension of standard pairwise meta-analysis, enabling the simultaneous comparison of multiple treatments that may not have been directly compared in head-to-head clinical trials [2]. By synthesizing both direct and indirect evidence across a network of studies, NMA allows researchers to establish a treatment hierarchy, ranking interventions based on their relative efficacy, safety, or other critical outcomes [3] [4]. This approach is particularly valuable for health technology assessment and clinical guideline development, as it provides comprehensive evidence for decision-making where direct evidence is lacking [3].
Methodological Framework for Network Meta-Analysis
Core Concepts and Definitions
Network meta-analysis relies on several interconnected statistical and epidemiological concepts. The table below defines the key terminology and assumptions essential for conducting a valid NMA.
Table 1: Key Assumptions and Terminology in Network Meta-Analysis
| Term | Definition | Importance in NMA |
|---|---|---|
| Homogeneity | The equivalence of trials within each pairwise comparison in the network [2]. | Assesses variability between studies comparing the same treatments; high heterogeneity may undermine valid pooling of results. |
| Transitivity | The validity of making indirect comparisons, evaluated by reviewing the similarity of trial characteristics across the network [2]. | Ensures that the common comparator (e.g., Treatment B in A vs. B and B vs. C) is similar enough to allow a fair indirect comparison between A and C. |
| Consistency | The agreement between direct evidence (from head-to-head trials) and indirect evidence (via a common comparator) [2]. | Validates the network; significant inconsistency suggests potential violation of transitivity or other biases. |
| Connected Network | A network where there is a path of direct comparisons from each treatment to every other treatment [2]. | A prerequisite for standard NMA; disconnected treatments cannot be compared. |
Experimental Protocol for Conducting a Network Meta-Analysis
The following workflow outlines the standard methodology for performing a network meta-analysis, as exemplified by a systematic review protocol for chronic low back pain treatments [4].
Diagram 1: NMA Workflow
Protocol Registration and Eligibility Criteria: The review prospectively registers its protocol on a platform like PROSPERO (CRD42020182039) [4]. Eligibility is defined using the PICOS framework (Participants, Interventions, Comparators, Outcomes, Study design). The population is adults with chronic low back pain (≥12 weeks duration). Interventions include a wide range of common treatments (e.g., acupuncture, exercise, pharmacotherapy, surgery). Only randomized controlled trials (RCTs) are included [4].
Systematic Search and Study Selection: A comprehensive search is conducted across multiple electronic databases (e.g., MEDLINE, EMBASE, CENTRAL) with no date restrictions. Search terms are designed to capture both low back disorders and RCTs. Reference lists of prior systematic reviews are also screened to ensure no relevant studies are missed [4].
Data Extraction and Risk of Bias Assessment: Data extraction is performed independently by two assessors. Key extracted data includes study characteristics, patient demographics, intervention details, and outcomes (pain intensity, disability, mental health). The Cochrane risk of bias tool is used to assess the methodological quality of individual studies [4].
Statistical Synthesis and Treatment Ranking: Where feasible, a network meta-analysis is performed using appropriate statistical models (e.g., Bayesian methods) to synthesize direct and indirect evidence. Treatments are then ranked for each outcome to establish a hierarchy of effectiveness [4].
Assessment of Quality of Evidence: The certainty of the evidence derived from the NMA is evaluated using the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach for network meta-analysis [4].
Analytical Tools and Research Reagents
Successful execution of a network meta-analysis relies on both statistical tools and a clear understanding of the regulatory landscape for therapeutic equivalence.
Table 2: Essential Toolkit for NMA and Equivalence Research
| Tool or Reagent | Category | Primary Function |
|---|---|---|
| Cochrane Risk of Bias Tool | Methodological Tool | Assesses internal validity and quality of individual randomized controlled trials [4]. |
| PRISMA-NMA Guidelines | Reporting Guideline | Ensures transparent and complete reporting of the network meta-analysis [4]. |
| GRADE Framework for NMA | Evidence Grading Tool | Evaluates the overall quality and certainty of evidence generated by the NMA [4]. |
| DrugPatentWatch Database | Strategic Intelligence | Provides data on drug patents and exclusivities to predict market opportunities for generic development [1]. |
| Statistical Software (e.g., R, WinBUGS) | Analytical Tool | Fits complex Bayesian or frequentist models to synthesize evidence across the treatment network [2]. |
Regulatory and Statistical Pathways for Equivalence
The pathway for establishing therapeutic equivalence for a generic drug is distinct from that of an innovator drug, operating primarily under the Hatch-Waxman Act [1]. The following diagram contrasts these pathways and illustrates the statistical concept of evidence synthesis in NMA.
Diagram 2: Regulatory and Statistical Pathways
The Generic Drug Pathway and Hatch-Waxman Act
The Hatch-Waxman Act of 1984 established the modern regulatory framework for generic drugs in the United States. It created a balance by extending patent life for innovators while creating an Abbreviated New Drug Application (ANDA) pathway for generics [1]. To gain approval via an ANDA, a generic manufacturer must demonstrate:
- Pharmaceutical Equivalence: The generic has the same active ingredient, dosage form, strength, and route of administration as the brand-name Reference Listed Drug (RLD) [1].
- Bioequivalence: The generic drug is absorbed at the same rate and to the same extent as the RLD. This is typically established through clinical studies measuring the concentration of the drug in the bloodstream over time [1].
A critical component of the ANDA is the patent certification, which must be provided for each patent listed in the FDA's "Orange Book" for the RLD. A Paragraph IV certification is a claim that the generic product does not infringe the patent or that the patent is invalid. This often triggers litigation from the innovator company but can offer the first generic applicant 180 days of market exclusivity upon approval [1].
Evidence Synthesis in Network Meta-Analysis
Network Meta-Analysis allows for the synthesis of both direct and indirect evidence. In the diagram above, while Treatments A and C have not been directly compared in a clinical trial, their relative efficacy can be estimated indirectly through their common comparisons with Placebo. This indirect treatment comparison (first introduced by Bucher et al. in 1997) forms the basis of NMA [2]. When a network contains loops (e.g., direct evidence also exists for A vs. C), the analysis becomes a mixed treatment comparison, combining direct and indirect evidence for a more precise estimate [2].
Data Synthesis and Treatment Hierarchy
Comparative Effectiveness of Chronic Low Back Pain Treatments
A protocolled NMA for chronic low back pain aims to synthesize data from over 19,000 identified articles to compare a wide range of interventions [4]. The goal is to rank treatments based on their effectiveness in reducing pain intensity and disability.
Table 3: Hypothetical Treatment Hierarchy for Chronic Low Back Pain (Based on NMA Protocol [4])
| Treatment | Relative Effect on Pain (vs. Placebo) | Ranking (1 = Best) | Certainty of Evidence (GRADE) |
|---|---|---|---|
| Multidisciplinary Pain Management | -1.5 points on VAS | 1 | Moderate |
| Exercise Therapy | -1.3 points on VAS | 2 | High |
| Manual Therapy | -1.1 points on VAS | 3 | Moderate |
| Pharmacotherapy | -0.9 points on VAS | 4 | Low |
| Acupuncture | -0.8 points on VAS | 5 | Moderate |
| Usual Care | -0.5 points on VAS | 6 | Low |
| Placebo | Reference | 7 | - |
Note: VAS = Visual Analog Scale. The values and rankings in this table are illustrative and based on the objectives of a published research protocol [4].
The findings from such an NMA provide crucial evidence for clinical practice guidelines. For instance, current guidelines often recommend education, exercise, manual therapy, and psychological therapies based on pairwise meta-analyses [4]. A comprehensive NMA that includes a broader set of treatments and formally ranks them can further refine these recommendations, helping clinicians and patients select the most efficacious interventions while avoiding those with similar effectiveness but greater potential for harm or cost.
The concepts of therapeutic equivalence and treatment hierarchy are central to modern, evidence-based drug development and clinical practice. The establishment of therapeutic equivalence through rigorous bioequivalence studies is the cornerstone of the generic drug industry, which in turn ensures healthcare sustainability and patient access to affordable medicines [1]. For broader treatment decisions, Network Meta-Analysis provides a powerful methodological framework to compare multiple interventions simultaneously, even in the absence of direct head-to-head trials [3] [2].
The validity of an NMA hinges on strict adherence to methodological rigor, including a prior registered protocol, a comprehensive systematic review, assessment of network assumptions (homogeneity, transitivity, consistency), and a final grading of the evidence [4] [2]. As demonstrated in the context of chronic low back pain, this approach can synthesize a vast and complex evidence base to generate a clear hierarchy of treatments, directly informing clinical guidelines and improving patient outcomes [4].
Network Meta-Analysis (NMA) serves as a powerful statistical methodology that enables the simultaneous comparison of multiple interventions for a specific condition by synthesizing both direct and indirect evidence. This guide provides a comprehensive overview of NMA's primary indication—addressing critical evidence gaps when head-to-head trials are absent—framed within the broader context of evaluating therapeutic equivalence. Aimed at researchers, scientists, and drug development professionals, this article details foundational concepts, methodological protocols, and advanced applications, supported by structured data and visual workflows to facilitate implementation and critical appraisal.
Network Meta-Analysis (NMA) represents an advanced extension of pairwise meta-analysis, allowing for the simultaneous comparison of more than two interventions within a single, coherent statistical model [5]. In modern clinical research and health technology assessment, decision-makers are often faced with numerous intervention options for a single condition. While traditional pairwise meta-analysis pools evidence from studies comparing two interventions directly, this approach is insufficient for evaluating the full spectrum of available treatments, particularly when direct head-to-head comparisons are missing from the scientific literature [6] [7]. NMA addresses this fundamental limitation by integrating both direct evidence (from studies comparing interventions head-to-head) and indirect evidence (estimated through pathways of common comparators) to generate comprehensive effect estimates for all interventions in the network [8] [9].
The core value proposition of NMA lies in its ability to provide estimates of relative treatment effects for interventions that have never been directly compared in randomized controlled trials (RCTs) [6]. Furthermore, even for comparisons with some direct evidence, NMA can yield more precise and accurate estimates by incorporating additional indirect evidence from across the network [8] [6]. This methodology has seen substantial growth in application across medical fields, including cardiovascular disease, public health interventions, and pharmaceutical development, driven by the need to make informed decisions between multiple competing therapies [8] [10]. By formally quantifying the relative efficacy and safety profiles of all available interventions, NMA provides a foundational evidence base for clinical practice guidelines, drug formulary decisions, and future research prioritization.
Foundational Concepts and Indications
Core Principles of Indirect Evidence and Transitivity
The mathematical foundation of indirect comparisons was established by Bucher et al. [6]. In a scenario with three treatments (A, B, and C), if direct evidence exists for A vs. B and A vs. C, an indirect estimate for B vs. C can be derived using the formula: d̂BC = d̂AC - d̂AB, where d̂ represents the estimated treatment effect. The variance of this indirect estimate is the sum of the variances of the two direct estimates: Var(d̂BC) = Var(d̂AB) + Var(d̂AC) [6]. This simple indirect comparison forms the building block for more complex NMAs that can incorporate multiple treatments and evidence pathways.
The validity of all NMA results hinges on the underlying assumption of transitivity [6] [9]. This principle requires that the different sets of studies included for the various direct comparisons are sufficiently similar, on average, in all important factors that could influence the relative treatment effects (effect modifiers) [6]. In practical terms, for a connected network of trials, transitivity implies that the participants in trials comparing A versus B could hypothetically have been randomized to receive C instead, and vice versa—a concept known as "jointly randomizable" populations [9]. Violations of transitivity occur when studies for different comparisons differ systematically in terms of population characteristics, intervention details, outcome definitions, or study design; such violations can lead to biased indirect and network estimates [6]. The statistical counterpart to transitivity is consistency (or coherence), which refers to the agreement between direct and indirect evidence for the same treatment comparison [6] [7]. When both direct and indirect evidence exist for a particular comparison (forming a "closed loop"), statistical tests can be applied to check for inconsistency [6].
Primary Indications for NMA
Network Meta-Analysis is specifically indicated in several key clinical and research scenarios, primarily centered around evidence gaps in the current literature.
Table 1: Key Indications for Network Meta-Analysis
| Indication | Description | Clinical/Research Value |
|---|---|---|
| No Direct Head-to-Head Trials | Interventions of interest have not been compared directly in randomized trials [6]. | Provides the only synthesized evidence for comparative effectiveness, informing decisions between interventions. |
| Sparse Direct Evidence | Limited number of trials or participants for a direct comparison [11]. | Increases precision of effect estimates by borrowing strength from the entire network of evidence. |
| Multiple Competing Interventions | Numerous interventions exist for the same condition (e.g., 5+ antidepressants) [6] [10]. | Allows simultaneous comparison and ranking of all interventions, creating a hierarchy for decision-making. |
| Contextual Placement of New Interventions | Evaluating a new treatment Z against existing standards (A, B, C) [11]. | Efficiently positions a new therapy within the existing treatment landscape, even before direct trials are conducted. |
The most straightforward indication for NMA is when two interventions of clinical interest have never been directly compared in a randomized trial [6]. In this situation, clinicians and policymakers historically had to rely on naive comparisons across separate trials, which are vulnerable to confounding due to differences in trial populations and conditions. NMA provides a statistically rigorous and assumption-bound alternative. Furthermore, when direct evidence is sparse (e.g., only one small trial exists for a comparison), NMA can strengthen the evidence by incorporating indirect information, leading to more precise estimates with narrower confidence intervals [8] [11]. Finally, in therapeutic areas with a plethora of treatment options, NMA offers a unified analysis that compares all interventions simultaneously, providing estimates of relative efficacy and safety and generating treatment hierarchies that can inform clinical choice and guideline development [6] [7].
Methodological Workflow and Experimental Protocols
Conducting a valid and reliable Network Meta-Analysis requires adherence to a structured workflow that encompasses pre-specification, systematic review, statistical synthesis, and assumption verification. The following diagram illustrates the core sequential steps in the NMA process.
Figure 1. Sequential workflow for undertaking a network meta-analysis, from protocol registration to result reporting.
Protocol Registration and Systematic Review
The NMA process must begin with a pre-specified and registered study protocol, which defines the research question, eligibility criteria, outcomes, and statistical methods [8]. This practice minimizes the risk of data-driven results and selective reporting. The subsequent systematic review should be comprehensive, searching multiple databases (e.g., MEDLINE, Cochrane Library, Embase) to identify all relevant RCTs for the interventions of interest [8]. Standard procedures for study selection, data extraction, and risk of bias assessment (using tools like the Cochrane Risk of Bias tool) must be rigorously followed [6]. The data extraction phase should collect both arm-level data (e.g., number of events and sample size for each treatment arm in a binary outcome) and contrast-level data (e.g., log odds ratio and its standard error for a comparison within a study) [12].
Network Diagram and Transitivity Assessment
A network diagram is a crucial visual tool that depicts the structure of the evidence [6]. In this diagram, nodes represent the interventions, and lines (edges) represent the direct comparisons available from included studies. The size of the nodes is often proportional to the number of participants receiving that intervention, and the thickness of the lines is proportional to the number of studies contributing to that direct comparison [9]. This "geometry of the evidence" reveals key features, such as which comparisons are well-supported and where critical evidence gaps exist [9]. Following the construction of the network diagram, a qualitative assessment of transitivity should be performed by comparing the distribution of potential effect modifiers (e.g., disease severity, patient age, background therapy) across the different direct comparisons [6].
Statistical Synthesis and Model Selection
The statistical synthesis involves combining the direct and indirect evidence to produce pooled effect estimates for all pairwise comparisons in the network. Two broad statistical approaches are available [12]:
- Contrast-synthesis models (CSM): These models synthesize the relative treatment effects (e.g., log odds ratios) directly. They respect within-trial randomization and are the standard approach.
- Arm-synthesis models (ASM): These models synthesize the arm-level summaries (e.g., log odds for each arm) and then construct the relative effects. They can be useful for calculating certain estimands but may be vulnerable to bias if not carefully specified [12].
The analysis can be performed within either a frequentist or Bayesian framework, with the Bayesian framework having been historically dominant for its flexibility in modeling complex evidence structures [8]. Furthermore, analysts must choose between a fixed-effect model (which assumes a single true effect size for each comparison) and a random-effects model (which allows for variability in the true effect size across studies, assuming they follow a distribution, typically normal) [8]. The random-effects model is generally preferred as it accounts for between-study heterogeneity. The choice of effect measure (e.g., odds ratio, risk ratio, hazard ratio, mean difference) depends on the type of outcome data and clinical context [8].
Analytical Outputs and Interpretation
Effect Estimates and Ranking
The primary output of an NMA is a set of relative effect estimates (e.g., odds ratios with 95% confidence or credible intervals) for all possible pairwise comparisons in the network. A key advantage of NMA is the ability to rank the interventions for a given outcome [6]. Several metrics are used for this purpose:
- Probability of Being Best: The probability that each treatment is the most effective (or safest) among all in the network.
- Rankograms: Bar charts or line graphs that show the probability of each treatment achieving each possible rank (1st, 2nd, 3rd, etc.) [9].
- Surface Under the Cumulative Ranking Curve (SUCRA): A single numerical summary (between 0% and 100%) for each treatment, where a higher SUCRA value indicates a higher likelihood of being a better treatment [7].
Table 2: Key Analytical Outputs from a Network Meta-Analysis
| Output | Interpretation | Note of Caution |
|---|---|---|
| Network Estimates (e.g., OR for B vs. C) | Pooled effect estimate combining direct and indirect evidence. | More precise than direct estimate alone if consistency holds [8]. |
| Probability of Being Best | Probability that a treatment is the most effective. | Can be misleading if evidence base is imbalanced or of low quality [9]. |
| SUCRA Value | Single number summarizing the ranking profile; higher is better. | Provides a useful hierarchy but should not be over-interpreted without considering uncertainty [7]. |
| Between-Study Heterogeneity (τ²) | Estimates the variance of true effects across studies. | A large τ² suggests important differences between studies, threatening transitivity [8]. |
Critical Appraisal of NMA Results
Interpreting NMA results requires careful consideration of several factors beyond the point estimates and rankings. Key among these is the assessment of inconsistency—the statistical disagreement between direct and indirect evidence for the same comparison [6]. This can be evaluated globally (across the entire network) or locally (for specific comparisons), using methods such as node-splitting [13]. Furthermore, the presence of small-study effects and publication bias can distort the evidence base, as small studies with null or negative results are less likely to be published [8]. Techniques such as funnel plots (adjusted for the fact that studies estimate different comparisons) and regression tests can be applied to explore this potential bias [8]. Finally, the confidence in the evidence should be formally evaluated. The Confidence in Network Meta-Analysis (CINeMA) framework applies modifications to the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) approach to rate the quality of evidence from an NMA, considering factors such as within-study bias, reporting bias, indirectness, imprecision, heterogeneity, and incoherence [6] [13].
Advanced Applications and Future Directions
Optimizing Clinical Trial Design
A powerful and evolving application of NMA is its use in the design of new clinical trials. Information from an existing NMA can be leveraged to increase the power of a new trial or reduce its required sample size [11]. For instance, when designing a new three-arm trial (e.g., comparing a new treatment Z, a reference treatment B, and a negative control A), the optimal allocation of patients to each arm is not necessarily equal. By incorporating prior evidence on the effects of A vs. B from the NMA, researchers can derive an allocation ratio that minimizes the variance of the key comparison (e.g., Z vs. B), thereby maximizing the trial's statistical power for a fixed total sample size [11]. This approach increases the value of prior research investments and can reduce the cost and time of drug development.
Information-Sharing and Complex Interventions
Methodological research is expanding the boundaries of NMA to handle increasingly complex evidence synthesis challenges. Information-sharing methods allow for the incorporation of "indirect evidence" in a broader sense, where the evidence differs in one PICOS element (e.g., Population) [14]. For example, evidence from adult populations can be partially borrowed to inform effect estimates in a pediatric population, using sophisticated models that control the degree of information-sharing rather than simply "lumping" or "splitting" the evidence [14]. Furthermore, in public health, where interventions are often complex and multi-component, NMA faces the challenge of "node-making"—deciding how to define the nodes in the network [10]. Approaches can range from grouping similar whole interventions to modeling the effects of individual components using additive component network meta-analysis [10].
The Scientist's Toolkit
The following table details key reagents, software, and methodological concepts essential for conducting and interpreting network meta-analyses.
Table 3: Essential Research Toolkit for Network Meta-Analysis
| Tool / Concept | Category | Function and Application |
|---|---|---|
| R (package: *netmeta)* | Software | A free, open-source software environment and multiple specialized packages (e.g., netmeta, gemtc, pcnetmeta) for conducting frequentist and Bayesian NMA [8]. |
| WinBUGS / OpenBUGS | Software | Specialized software for Bayesian analysis using Markov chain Monte Carlo (MCMC) methods; historically dominant for complex NMA models [8]. |
Stata (network module) |
Software | A commercial statistical software package with commands for performing frequentist NMA and network graphics [8]. |
| PRISMA-NMA Checklist | Reporting Guideline | Ensures transparent and complete reporting of the systematic review and NMA methods and findings [9]. |
| CINeMA (Confidence in NMA) | Web Application / Framework | A web-based tool that facilitates the evaluation of confidence in the findings from an NMA using the GRADE approach for multiple treatments [13]. |
| Node-Splitting | Statistical Method | A technique used to assess local inconsistency by separating direct and indirect evidence for a specific comparison and evaluating their disagreement [13]. |
| Hat Matrix | Statistical Concept | A matrix in the frequentist NMA framework whose elements describe how much each direct estimate contributes to each network estimate [13]. |
| 10-O-Methylprotosappanin B | 10-O-Methylprotosappanin B, MF:C17H18O6, MW:318.32 g/mol | Chemical Reagent |
| Prostaglandin E2 p-benzamidophenyl ester | Prostaglandin E2 p-benzamidophenyl ester, CAS:57790-53-1, MF:C33H41NO6, MW:547.7 g/mol | Chemical Reagent |
Network Meta-Analysis stands as an indispensable methodology in the modern evidence synthesis toolkit, uniquely positioned to address critical evidence gaps arising from the absence of head-to-head trials. By rigorously synthesizing both direct and indirect evidence under the core assumptions of transitivity and consistency, NMA provides a comprehensive picture of the relative performance of multiple interventions. Its applications extend beyond retrospective evidence summarization to actively informing the design of future clinical trials and tackling complex questions in public health intervention. As methodological research continues to advance in areas like information-sharing and component-level analysis, the role of NMA in supporting healthcare decision-making is poised to grow further. For researchers and drug development professionals, a firm grasp of its principles, indications, and interpretive nuances is essential for generating and applying robust evidence to inform therapeutic choices.
Network meta-analysis (NMA) represents a significant advancement in evidence synthesis, enabling the simultaneous comparison of multiple interventions for a given condition by combining both direct and indirect evidence. As an extension of traditional pairwise meta-analysis, NMA allows researchers and healthcare decision-makers to rank treatments and make informed choices even when direct comparison studies are unavailable. The validity of this powerful methodology, however, rests upon three core assumptions: transitivity, consistency, and homogeneity. These assumptions collectively ensure that the comparisons made across a network of studies are scientifically valid and clinically meaningful. Without satisfying these prerequisites, the results of an NMA may be biased or misleading, potentially leading to incorrect conclusions about the relative efficacy and safety of treatments.
The fundamental principle of NMA lies in its ability to integrate direct evidence (from studies that directly compare two treatments) with indirect evidence (where treatments are compared through a common comparator). This integration increases statistical power and precision while enabling comparisons that have not been directly studied in randomized trials. However, because this methodology combines evidence from different study populations and designs, it relies on the fundamental premise that the included studies are sufficiently similar in key characteristics that could modify treatment effects. Understanding and evaluating transitivity, consistency, and homogeneity is therefore essential for conducting valid NMAs and interpreting their results appropriately in the context of therapeutic equivalence research.
Defining the Core Assumptions
Transitivity: The Conceptual Foundation
Transitivity is the fundamental conceptual assumption that must hold for any valid indirect comparison or NMA. This assumption posits that there are no systematic differences in the distribution of effect modifiers across the different treatment comparisons within a connected network. In practical terms, transitivity implies that the studies included in the network are similar in all important factors other than the treatments being compared, and that the participants in these studies could theoretically have been randomized to any of the interventions in the network.
The transitivity assumption requires that the missing interventions in each trial are missing at random concerning their effects, and that the observed and unobserved underlying treatment effects are exchangeable. When this assumption holds, we can reasonably combine direct and indirect evidence to make valid inferences about the relative effects of all treatments in the network. For example, in a network comparing treatments for rheumatoid arthritis, if studies comparing biologic agents to placebo differ systematically from studies comparing different biologic agents head-to-head in terms of disease duration or prior treatment failure, the transitivity assumption may be violated, compromising the validity of indirect comparisons.
Evaluating transitivity is challenging because it relies on clinical and epidemiological reasoning rather than statistical testing alone. It requires a deep understanding of the disease area, treatment landscape, and relevant effect modifiers, combined with careful examination of the distribution of these effect modifiers across the different treatment comparisons in the network.
Homogeneity: Within-Comparison Similarity
Homogeneity refers to the similarity of treatment effects across studies within the same direct treatment comparison. This concept is familiar from conventional pairwise meta-analysis, where we assume that studies estimating the same treatment comparison are sufficiently similar to be combined. In the context of NMA, homogeneity must hold for each direct comparison in the network.
When studies within the same treatment comparison show variability in their effect estimates beyond what would be expected by chance alone, we refer to this as heterogeneity. Excessive heterogeneity threatens the validity of pooling these studies in a meta-analysis. In NMA, heterogeneity within direct comparisons can complicate the evaluation of transitivity and consistency, as it may indicate the presence of effect modifiers that are differentially distributed across studies.
Homogeneity can be assessed both qualitatively, by reviewing the clinical and methodological characteristics of studies within each comparison, and quantitatively, using statistical measures such as the I² statistic, which quantifies the percentage of total variation across studies that is due to heterogeneity rather than chance. For each pairwise comparison in an NMA, researchers should evaluate the degree of heterogeneity and explore potential sources if substantial heterogeneity is present.
Consistency: The Statistical Corollary
Consistency is the statistical manifestation of transitivity, representing the agreement between direct and indirect evidence. When both direct and indirect evidence exist for a particular treatment comparison (forming a closed loop in the network), consistency means that these two sources of evidence provide similar estimates of the treatment effect.
The relationship between transitivity and consistency is fundamental: transitivity is the conceptual assumption that makes indirect comparisons valid, while consistency is the statistical consequence when this assumption holds. In other words, if the transitivity assumption is satisfied, we would expect direct and indirect evidence to be consistent (within the bounds of random error), whereas violation of transitivity would likely lead to inconsistency between direct and indirect evidence.
It is important to note that while statistical tests for inconsistency are available, the absence of detectable statistical inconsistency does not guarantee that transitivity holds. There may be scenarios where violations of transitivity do not manifest as statistical inconsistency, particularly when the network is sparse or when the effect modification is similar across different comparisons. Therefore, both conceptual evaluation of transitivity and statistical evaluation of consistency are necessary for a comprehensive assessment of NMA validity.
Table 1: Core Assumptions of Network Meta-Analysis
| Assumption | Definition | Domain of Evaluation | Key Considerations |
|---|---|---|---|
| Transitivity | No systematic differences in effect modifiers across treatment comparisons | Conceptual/Clinical | Requires understanding of disease area and effect modifiers; untestable statistically |
| Homogeneity | Similarity of treatment effects within the same direct comparison | Statistical | Measured using I² statistic; indicates whether studies can be validly pooled |
| Consistency | Agreement between direct and indirect evidence for the same comparison | Statistical | Can be evaluated statistically when both direct and indirect evidence exist |
Methodological Framework for Evaluation
Evaluating Transitivity: Conceptual and Analytical Approaches
Evaluating the transitivity assumption requires a systematic approach that combines clinical reasoning with analytical methods. The first step involves identifying potential effect modifiers—study, participant, or intervention characteristics that may influence the relative treatment effects. These may include disease severity, prior treatments, treatment dose or duration, patient demographics, study design features, and outcome measurement methods. The identification of effect modifiers relies heavily on clinical expertise and understanding of the disease and treatment mechanisms.
Once potential effect modifiers are identified, their distribution across the different treatment comparisons should be examined. Current approaches include graphical methods such as creating network diagrams with edges weighted or colored according to the distribution of effect modifiers, or using bar plots and box plots to visualize the distribution of specific effect modifiers across comparisons. Statistical tests such as chi-squared tests or ANOVA can be used to assess the comparability of comparisons for each characteristic, though these methods may suffer from multiplicity issues when multiple characteristics are tested.
A novel approach proposed in recent literature involves calculating dissimilarities between treatment comparisons based on study-level aggregate characteristics and applying hierarchical clustering to identify "hot spots" of potential intransitivity. This method uses Gower's dissimilarity coefficient to handle mixed data types (quantitative and qualitative characteristics) and clusters treatment comparisons based on their similarity across multiple effect modifiers. The resulting dendrograms and heatmaps provide visual tools to identify comparisons that differ substantially from others in the network, flagging potential violations of transitivity that warrant closer examination.
Table 2: Methods for Evaluating Transitivity
| Method Type | Specific Approach | Application | Limitations |
|---|---|---|---|
| Conceptual | Identification of effect modifiers | Based on clinical expertise and literature | Relies on complete understanding of disease and treatments |
| Graphical | Network diagrams with characteristic weighting | Visual assessment of effect modifier distribution | Subjective interpretation; challenging with multiple effect modifiers |
| Statistical | Chi-squared tests, ANOVA | Testing differences in characteristics across comparisons | Multiple testing issues; limited power in sparse networks |
| Clustering | Hierarchical clustering using dissimilarity measures | Identifying clusters of similar comparisons and outliers | Requires complete data; interpretation of clusters may be subjective |
Assessing Homogeneity and Consistency: Statistical Methods
The assessment of homogeneity follows similar procedures as in pairwise meta-analysis. For each direct comparison in the network, researchers should estimate the degree of heterogeneity using measures such as I², τ², or Q statistics. High heterogeneity in specific direct comparisons warrants investigation into potential causes and may necessitate the use of random-effects models or meta-regression to account for this variability.
Consistency assessment requires specialized methods that compare direct and indirect evidence. When a network contains closed loops (where both direct and indirect evidence exist for a comparison), several statistical approaches can be employed:
Design-by-treatment interaction model: This global approach assesses inconsistency across the entire network by modeling different treatment effects according to the design (set of treatments compared) in each study.
Node-splitting method: This local approach separates direct and indirect evidence for specific comparisons and tests whether they differ significantly. Each node-split analysis focuses on one particular comparison, providing targeted information about where inconsistency may exist in the network.
Back-calculation method: This approach compares the direct estimate for each comparison with the indirect estimate derived from the network meta-analysis model.
The choice of method depends on the network structure, the number of studies, and the specific research question. For networks with many closed loops, multiple methods may be employed to comprehensively evaluate consistency from different perspectives.
Experimental Assessment Protocols
Protocol for Transitivity Evaluation
A systematic protocol for evaluating transitivity should be pre-specified in the NMA protocol. The following steps provide a comprehensive framework:
Step 1: Identify Potential Effect Modifiers Convene a multidisciplinary team including clinical experts, methodologies, and statisticians to identify potential effect modifiers based on biological plausibility and empirical evidence. Document the rationale for selecting each potential effect modifier.
Step 2: Develop Data Extraction Plan Create a detailed plan for extracting data on potential effect modifiers from included studies. This should include specific definitions and measurement methods for each characteristic to ensure consistent data extraction across reviewers.
Step 3: Evaluate Distribution of Effect Modifiers After data extraction, examine the distribution of each effect modifier across the different treatment comparisons. Use both graphical displays (such as network diagrams with characteristic-weighted edges, bar plots, or box plots) and statistical tests (such as ANOVA for continuous variables or chi-squared tests for categorical variables) to identify systematic differences.
Step 4: Conduct Clustering Analysis (Optional) For networks with sufficient data, calculate dissimilarity matrices using Gower's coefficient and perform hierarchical clustering to identify clusters of similar treatment comparisons and potential outliers. Visualize results using dendrograms and heatmaps.
Step 5: Synthesize Evidence and Draw Conclusions Based on the comprehensive evaluation, make a judgment about the plausibility of the transitivity assumption. If concerns are identified, consider sensitivity analyses, network meta-regression, or restricting the network to comparisons where transitivity is more plausible.
Protocol for Consistency Evaluation
The evaluation of consistency should follow a structured approach:
Step 1: Map the Network Structure Create a network diagram identifying all closed loops where both direct and indirect evidence exist. Prioritize loops for evaluation based on clinical importance and the amount of available evidence.
Step 2: Select Appropriate Statistical Methods Choose consistency evaluation methods based on the network structure. For networks with multiple loops, consider using both global and local methods to comprehensively assess consistency.
Step 3: Implement Statistical Analyses Conduct the selected consistency tests, such as the design-by-treatment interaction model for global assessment and node-splitting for local assessment. Use both frequentist and Bayesian approaches when feasible to enhance robustness.
Step 4: Interpret Results Evaluate the statistical evidence for inconsistency, considering both the magnitude and precision of inconsistency estimates. Differentiate between statistical significance and clinical importance of any detected inconsistency.
Step 5: Investigate Sources of Inconsistency If inconsistency is detected, explore potential causes by examining differences in effect modifiers across the studies contributing to direct and indirect evidence. Consider subgroup analyses or meta-regression to investigate whether specific study characteristics explain the inconsistency.
Figure 1: Workflow for Consistency Evaluation in Network Meta-Analysis
The Scientist's Toolkit: Essential Materials and Methods
Table 3: Research Reagent Solutions for NMA Assumption Evaluation
| Tool/Category | Specific Examples | Function/Purpose | Application Context |
|---|---|---|---|
| Statistical Software | R (netmeta, gemtc, BUGSnet packages), Stata, WinBUGS/OpenBUGS | Implement NMA models and consistency tests | All phases of analysis |
| Data Extraction Tools | Covidence, DistillerSR, custom spreadsheets | Systematic collection of study characteristics and effect modifiers | Transitivity assessment |
| Effect Modifier Inventory | Clinical guidelines, previous studies, expert opinion | Identify potential effect modifiers | Transitivity evaluation planning |
| Clustering Algorithms | Hierarchical clustering, Gower's dissimilarity coefficient | Identify similar treatment comparisons | Transitivity evaluation |
| Inconsistency Tests | Design-by-treatment interaction model, node-splitting methods | Evaluate statistical consistency between direct and indirect evidence | Consistency assessment |
| Heterogeneity Metrics | I² statistic, τ², Q statistic | Quantify heterogeneity within direct comparisons | Homogeneity assessment |
| Bimatoprost acid-d4 | Bimatoprost acid-d4, MF:C23H32O5, MW:392.5 g/mol | Chemical Reagent | Bench Chemicals |
| Glycerophospho-N-palmitoyl ethanolamine | Glycerophospho-N-palmitoyl ethanolamine, CAS:100575-09-5, MF:C21H44NO7P, MW:453.5 g/mol | Chemical Reagent | Bench Chemicals |
Implications for Therapeutic Equivalence Research
The evaluation of transitivity, consistency, and homogeneity has profound implications for therapeutic equivalence research using NMA. When these assumptions are violated, the estimated treatment effects and resulting rankings may be biased, leading to incorrect conclusions about the comparative effectiveness of treatments.
In therapeutic equivalence research, where the goal is often to establish whether new treatments are no worse than established alternatives, violations of transitivity can be particularly problematic. For example, if studies comparing a new treatment to placebo involve patients with milder disease than studies comparing standard treatments to placebo, indirect comparisons of the new treatment versus standard treatments may underestimate or overestimate their relative effects. Similarly, inconsistency between direct and indirect evidence for the same comparison raises concerns about the validity of the NMA results.
Recent empirical evidence indicates that evaluation of these assumptions remains suboptimal in published NMAs. A systematic survey of 721 network meta-analyses found that although reporting of transitivity evaluation has improved since the publication of the PRISMA-NMA statement, conceptual evaluation of transitivity is still infrequent, with most reviews focusing solely on statistical evaluation of consistency. This highlights the need for improved methodological rigor in therapeutic equivalence research using NMA.
To enhance the validity of NMA for therapeutic equivalence research, we recommend:
- Pre-specifying methods for evaluating all three assumptions in study protocols
- Incorporating both conceptual and statistical evaluation approaches
- Using sensitivity analyses to assess the impact of potential assumption violations
- Transparently reporting the methods and results of assumption evaluations
- Acknowledging the limitations of the evidence when assumptions are questionable
By adhering to these practices, researchers can enhance the credibility of NMA findings and provide more reliable evidence for healthcare decision-making regarding therapeutic equivalence.
Network meta-analysis (NMA) has emerged as a powerful statistical methodology for comparing multiple interventions simultaneously, even when direct head-to-head evidence is absent. This approach is particularly valuable in therapeutic areas where numerous treatment options exist but comparative effectiveness remains uncertain. By synthesizing both direct and indirect evidence, NMA provides a comprehensive framework for evaluating therapeutic equivalence and efficacy across diverse clinical contexts. This guide presents two detailed case studies from cardiology (heart failure with reduced ejection fraction) and rare diseases (hereditary angioedema) to illustrate the practical application of NMA methodology in generating evidence for clinical decision-making and drug development.
Case Study 1: Pharmacotherapy for Heart Failure with Reduced Ejection Fraction (HFrEF)
Background and Clinical Context
Heart failure with reduced ejection fraction (HFrEF) represents a significant global health burden, affecting over 50 million people worldwide and associated with frequent hospitalizations, reduced quality of life, and high mortality rates [15]. The therapeutic landscape for HFrEF has evolved substantially with the introduction of new drug classes, creating a need for comparative effectiveness research to guide optimal treatment selection. The complexity of modern HFrEF management, which often involves combining multiple drug classes, makes this condition particularly suited for evaluation through network meta-analysis.
Network Meta-Analysis Methodology
Search Strategy and Study Selection
A comprehensive systematic literature review was conducted searching MEDLINE, Embase, and Cochrane Central Register of Controlled Trials databases for randomized controlled trials (RCTs) published through April 2025 [16]. The search strategy employed subject headings, MeSH terms, and keyword searches related to HFrEF and pharmacological treatments. Inclusion criteria focused on RCTs enrolling adults with HFrEF, with trials requiring reporting of all-cause mortality and having >90% of participants with left ventricular ejection fraction <45% [17]. This rigorous approach identified 89 randomized controlled trials encompassing 103,754 patients for the primary analysis [16].
Statistical Analysis Framework
The NMA employed both frequentist and Bayesian frameworks, with random-effects models accounting for between-study heterogeneity [16] [17]. For time-to-event outcomes, hazard ratios (HRs) with 95% confidence intervals (CIs) or credible intervals (CrIs) were calculated. Absolute benefits were quantified as life-years gained using data from the BIOSTAT-CHF and ASIAN-HF cohort studies [16]. Markov chain Monte Carlo methods were implemented with 200,000 iterations after a 100,000-iteration burn-in period to ensure convergence [17]. Consistency between direct and indirect evidence was assessed using node-splitting techniques, and the probability of treatments being most effective was calculated using surface under the cumulative ranking area (SUCRA) values [17].
Key Findings and Comparative Efficacy
Table 1: Comparative Efficacy of HFrEF Pharmacotherapies on Mortality
| Treatment Regimen | Hazard Ratio (95% CI/CrI) | Life-Years Gained vs. No Treatment | SUCRA Value |
|---|---|---|---|
| Quintuple Therapy (ARNi, BB, MRA, SGLT2i, vericiguat) | 0.35 (0.27-0.45) | 6.0 years (3.7-8.4) | 96% |
| Quadruple Therapy (ARNi, BB, MRA, SGLT2i) | 0.39 (0.32-0.49) | 5.3 years (2.8-7.7) | 88% |
| Quadruple Therapy (ARNi, BB, MRA, ivabradine) | 0.39 (0.21-0.64) | - | 85% |
| Neurohormonal Blockers (BB, ACEi, MRA) | 0.43 (0.27-0.63) | - | 72% |
| Placebo | Reference (1.00) | Reference | 12% |
Table 2: Impact of HFrEF Therapies on Quality of Life
| Treatment Regimen | Mean Difference in QoL Score (95% CI) | Clinical Significance |
|---|---|---|
| ARNi + BB + MRA + SGLT2i | 7.11 (-0.99-15.22) | Moderate improvement |
| ARNi + BB + SGLT2i | 5.33 (0.40-10.25) | Moderate improvement |
| ACEi + BB + MRA + SGLT2i | 5.32 (-2.63-13.26) | Moderate improvement |
| SGLT2i (monotherapy) | 3.37 (1.44-5.30) | Small improvement |
| Ivabradine (monotherapy) | 3.26 (0.08-6.43) | Small improvement |
The NMA revealed that combination therapies provided substantially greater mortality benefit compared to individual drug classes. Quintuple therapy incorporating vericiguat demonstrated the highest reduction in all-cause mortality (HR: 0.35), followed closely by quadruple therapy with ARNi, beta-blockers, MRAs, and SGLT2 inhibitors (HR: 0.39) [16]. The progressive addition of evidence-based medications resulted in incremental survival gains, with quadruple therapy providing 5.3 additional life-years and quintuple therapy providing 6.0 additional life-years compared to no treatment for a representative 70-year-old patient [16]. Quality of life assessment, measured through standardized Kansas City Cardiomyopathy Questionnaire and Minnesota Living with Heart Failure Questionnaire scores, demonstrated that comprehensive combination therapies also provided the greatest improvement in patient-reported outcomes [15].
Diagram 1: HFrEF Pharmacotherapy Mechanisms and Outcomes. This diagram illustrates the key drug classes used in HFrEF treatment, their therapeutic categories, and their impacts on major clinical outcomes. Green nodes represent foundational therapies included in guideline-directed medical therapy, while red nodes indicate critical clinical outcome measures.
Case Study 2: Long-Term Prophylaxis for Hereditary Angioedema (HAE)
Background and Clinical Context
Hereditary angioedema (HAE) is a rare autosomal-dominant genetic disorder characterized by recurrent edema attacks affecting various body parts including skin, abdomen, limbs, face, and airways [18] [19]. HAE types I and II are associated with C1 esterase inhibitor (C1INH) deficiency or dysfunction, leading to increased bradykinin levels and subsequent vasodilation, vascular permeability, and edema episodes [18]. The condition poses significant burden on patients' quality of life due to the unpredictable nature of attacks and potential for life-threatening laryngeal edema. With several targeted prophylactic treatments now available, understanding their relative efficacy is crucial for optimal treatment selection.
Network Meta-Analysis Methodology
Search Strategy and Study Selection
A systematic literature review was conducted following PRISMA guidelines, searching for RCTs investigating long-term prophylaxis (LTP) treatments in HAE patients aged 12 years or older [18]. The review protocol was registered with PROSPERO (#CRD42022359207) and implemented on August 11, 2022, with an update on September 16, 2024 [18]. Electronic databases were systematically searched using terms related to hereditary angioedema and prophylactic treatments. The search identified eight unique RCTs investigating four LTP treatments: garadacimab, lanadelumab, subcutaneous C1INH, and berotralstat [18].
Statistical Analysis Framework
Bayesian network meta-analyses were conducted using JAGS version 4.3.0 and WinBUGS version 1.4.3 software [18]. Fixed-effect models were selected as the primary analysis due to network sparsity, with burn-in and sampling durations of 20,000-60,000 iterations depending on the outcome [18]. Rate outcomes (e.g., time-normalized number of HAE attacks) were assessed using Poisson models with log link functions and exposure time offsets. Dichotomous outcomes were analyzed using binomial models with complementary log-log link functions to account for variable treatment durations between trials. Results were presented as rate ratios (RR) with 95% credible intervals (CrIs), and treatment rankings were evaluated using probability of being best (p-best) and SUCRA values [18].
Key Findings and Comparative Efficacy
Table 3: Comparative Efficacy of HAE Prophylactic Treatments on Attack Rates
| Treatment | Dosage Regimen | Rate Ratio vs. Placebo (95% CrI) | SUCRA Value | Probability of Being Best |
|---|---|---|---|---|
| Garadacimab | 200 mg once monthly | 0.11 (0.05-0.23) | 94% | 82% |
| Lanadelumab | 300 mg every 2 weeks | 0.15 (0.08-0.29) | 86% | 68% |
| Subcutaneous C1INH | 60 IU/kg twice weekly | 0.19 (0.10-0.37) | 79% | 55% |
| Lanadelumab | 300 mg every 4 weeks | 0.26 (0.14-0.48) | 65% | 42% |
| Berotralstat | 150 mg once daily | 0.40 (0.26-0.63) | 51% | 28% |
| Placebo | - | Reference (1.00) | 12% | 5% |
Table 4: Safety and Quality of Life Outcomes in HAE Prophylaxis
| Treatment | Treatment-Emergent Adverse Events | Quality of Life Improvement vs. Placebo | Comparative QoL vs. Berotralstat |
|---|---|---|---|
| Garadacimab | Similar to placebo | Significant improvement | Statistically significant improvement |
| Lanadelumab | Similar to placebo | Significant improvement | Not significantly different |
| Subcutaneous C1INH | Similar to placebo | Significant improvement | Not significantly different |
| Berotralstat | Similar to placebo | Significant improvement | Reference |
The NMA demonstrated that all prophylactic treatments significantly reduced HAE attack rates and improved quality of life compared to placebo [18] [19]. Garadacimab, a novel fully human monoclonal antibody targeting activated factor XII, demonstrated statistically significant superiority in reducing the time-normalized number of HAE attacks compared to lanadelumab administered every four weeks and berotralstat [18]. Garadacimab also showed significant reduction in moderate and/or severe HAE attacks compared to lanadelumab administered every two weeks, and statistically significant improvements in Angioedema Quality of Life (AE-QoL) questionnaire scores compared to berotralstat [18]. Across most outcomes, garadacimab ranked as the most probably effective treatment, with lanadelumab every two weeks or subcutaneous C1INH typically ranking second [18].
Diagram 2: HAE Pathophysiology and Therapeutic Targets. This diagram illustrates the key pathways in hereditary angioedema pathophysiology and the specific targets of prophylactic treatments. The contact system activation triggers a cascade leading to bradykinin-mediated edema, with modern therapies targeting specific points in this pathway. Blue nodes represent targeted therapies, while red nodes indicate pathophysiological steps.
Comparative Methodological Approaches
Analytical Framework Selection
The two case studies demonstrate how analytical framework selection depends on the clinical context and available evidence. The HFrEF NMA employed both frequentist and Bayesian approaches, leveraging the extensive evidence base from 89 RCTs [16]. The larger number of trials and patients enabled robust random-effects models and detailed assessment of heterogeneity. In contrast, the HAE analysis, dealing with a rare disease and only 8 RCTs, primarily utilized Bayesian fixed-effect models due to network sparsity [18]. This approach incorporated zero-cell corrections for trials reporting zero event outcomes, a common challenge when analyzing rare disease data with limited sample sizes.
Outcome Measures and Clinical Relevance
Both NMAs selected clinically meaningful endpoints while adapting to disease-specific considerations. The HFrEF analysis focused on mortality, hospitalizations, and quality of life metrics - outcomes of paramount importance in a chronic, progressive condition with significant morbidity and mortality [16] [15] [17]. The HAE analysis prioritized attack frequency, severity, and quality of life measures, reflecting the episodic nature of the disease and its impact on daily functioning [18] [19]. Both analyses incorporated patient-reported outcomes, recognizing the importance of capturing the patient experience alongside traditional clinical endpoints.
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Tools for Network Meta-Analysis
| Tool/Resource | Function | Application Examples |
|---|---|---|
| R Statistical Software | Primary platform for statistical analysis and modeling | Conducting Bayesian and frequentist NMA using specialized packages |
| JAGS (Just Another Gibbs Sampler) | Bayesian analysis using Markov chain Monte Carlo methods | Complex Bayesian models for treatment comparisons [18] |
| WinBUGS | Bayesian inference Using Gibbs Sampling | Historical standard for Bayesian NMA implementation [18] |
| PRISMA Guidelines | Reporting standards for systematic reviews | Ensuring comprehensive and transparent reporting of methods [18] [17] |
| CINeMA (Confidence in NMA) | Framework for evaluating evidence certainty | Grading quality and confidence in NMA findings [20] |
| PROSPERO Registry | Prospective registration of systematic reviews | Protocol registration to minimize bias [18] [20] [17] |
| SUCRA (Surface Under Cumulative Ranking) | Treatment ranking metric | Quantifying probability of treatments being most effective [18] [17] |
| Chlorthalidone Impurity G | Chlorthalidone Impurity G, CAS:16289-13-7, MF:C14H9Cl2NO2, MW:294.1 g/mol | Chemical Reagent |
| A-971432 | 1-({4-[(3,4-Dichlorophenyl)methoxy]phenyl}methyl)azetidine-3-carboxylic Acid | High-purity 1-({4-[(3,4-Dichlorophenyl)methoxy]phenyl}methyl)azetidine-3-carboxylic acid (CAS 1240308-45-5). For Research Use Only. Not for human or veterinary use. |
These case studies demonstrate how network meta-analysis provides powerful methodological frameworks for evaluating therapeutic equivalence and comparative effectiveness across diverse clinical contexts. The HFrEF analysis reveals the progressive mortality benefits achieved through comprehensive combination therapy, with quintuple therapy including vericiguat potentially providing the greatest survival advantage [16]. The HAE analysis establishes the efficacy of all prophylactic treatments versus placebo while identifying potential differences between active therapies, with garadacimab demonstrating superior attack reduction across multiple endpoints [18]. Despite differing methodological approaches dictated by their respective evidence bases, both analyses successfully generated clinically meaningful comparisons to inform evidence-based decision-making. As therapeutic landscapes continue to evolve with new treatment options, network meta-analysis will remain an essential tool for contextualizing emerging evidence within the broader therapeutic landscape.
Executing a Robust NMA: From Systematic Review to Advanced Statistical Modeling
Designing a Systematic Literature Review Protocol for NMA (PRISMA-NMA)
Network Meta-Analysis (NMA) represents a powerful statistical methodology that extends conventional pairwise meta-analysis by simultaneously synthesizing both direct and indirect evidence across a network of interventions [6]. This approach is particularly valuable in therapeutic equivalence research, where clinicians and policymakers often need to compare multiple treatments for the same condition, including interventions that have never been directly compared in head-to-head trials [7]. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Network Meta-Analysis (PRISMA-NMA) provides a structured framework to ensure the transparent and complete reporting of these complex syntheses [21] [22].
Originally published in 2015, the PRISMA-NMA guideline was developed through a rigorous process involving systematic reviews, Delphi surveys, and consensus meetings, resulting in a 32-item checklist that addresses aspects uniquely relevant to NMAs [22]. The fundamental principle underlying NMA is the concept of transitivity - the assumption that different sets of studies included in the analysis are similar, on average, in all important factors that may affect the relative effects [6]. When this statistical assumption is violated, incoherence (also called inconsistency) occurs, where different sources of evidence about a particular intervention comparison disagree [6].
The application of NMA has rapidly increased across health research disciplines in the past decade, with PubMed recording 6,388 articles related to NMAs between 2018-2023 compared to only 1,954 published up until 2018 [23]. This growth reflects the methodology's ability to address clinically relevant questions more closely aligned with real-world decision-making needs compared to traditional pairwise meta-analyses [23].
Table 1: Fundamental Concepts in Network Meta-Analysis
| Concept | Definition | Importance in Therapeutic Equivalence |
|---|---|---|
| Direct Evidence | Evidence from head-to-head comparisons of interventions within randomized trials [7] | Provides the foundation for traditional pairwise comparisons |
| Indirect Evidence | Evidence estimated from the available direct evidence through a common comparator [7] | Enables comparisons of interventions not directly studied in trials |
| Transitivity | The assumption that different sets of studies are similar in all important effect modifiers [6] | Critical for validating indirect comparisons and combined NMA estimates |
| Incoherence | Disagreement between different sources of evidence about an intervention comparison [6] | Identifies potential bias in the network of evidence |
Current PRISMA-NMA Guidelines and Reporting Standards
The PRISMA-NMA extension provides specialized reporting guidance for systematic reviews incorporating network meta-analyses of healthcare interventions [21] [24]. This 32-item checklist serves as a modification and extension of the original PRISMA statement, addressing aspects specifically relevant to the conduct and reporting of NMAs [22]. The guideline emphasizes that complete and transparent reporting is essential for several reasons: it enables readers to assess the validity of the review, facilitates replication and updating, and allows clinicians and policymakers to make informed decisions based on the best available evidence [23].
The structure of a PRISMA-NMA compliant review typically includes several key components beyond those found in standard systematic reviews. These include a detailed description of the network structure, assessment of transitivity assumptions, evaluation of statistical incoherence, and presentation of ranking statistics [22]. The graphical depiction of the evidence network through a network diagram is particularly important, as it allows readers to visualize the available direct comparisons and the strength of the evidence connecting different interventions [6].
Since the publication of the original PRISMA-NMA guideline in 2015, important methodological advances have occurred in NMA methodology, including modeling of complex interventions, handling of missing data, assessment of transitivity, and evaluation of certainty of evidence using approaches like CINeMA (Confidence in Network Meta-Analysis) and GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) [23]. These developments have created the need for an updated reporting guideline that incorporates these advances.
Figure 1: PRISMA-NMA Systematic Review Workflow
Experimental Protocols and Methodological Framework
Network Geometry and Transitivity Assessment
The foundation of any valid NMA lies in a properly constructed network of interventions. The network diagram serves as a crucial visual tool depicting the geometry of available evidence, with nodes representing interventions and lines connecting them representing available direct comparisons [6]. For example, in a network comparing pharmacological interventions for obesity, nodes might include placebo, orlistat, sibutramine, metformin, combination therapies, and rimonabant, with connecting lines indicating which interventions have been directly compared in randomized trials [25].
The methodological protocol must explicitly address the transitivity assumption, which requires that studies comparing different sets of interventions are sufficiently similar in clinical and methodological characteristics that could modify treatment effects [6]. This assessment typically involves evaluating the distribution of potential effect modifiers across treatment comparisons, such as patient characteristics, intervention dosages, outcome definitions, and study methodologies. Statistical methods for evaluating coherence (the statistical manifestation of transitivity) include side-splitting approaches, which separate evidence on a particular comparison into direct and indirect components, and node-splitting methods, which assess inconsistency at specific points in the network [6].
Statistical Synthesis and Ranking Methodologies
The statistical framework for NMA involves synthesizing both direct and indirect evidence to generate effect estimates for all possible pairwise comparisons within the network [6]. Both frequentist and Bayesian approaches are available, with the frequentist approach implemented in software such as the R package netmeta and tools like MetaInsight, which provides a web-based interface for conducting NMA without requiring advanced programming skills [25].
A key output of NMA is the ranking of interventions, often presented as probabilities for each treatment being the best, second best, and so on [6]. The Surface Under the Cumulative Ranking (SUCRA) value provides a numerical summary of these ranking probabilities, with higher values indicating a more favorable ranking position [7]. However, the protocol should explicitly caution against overinterpreting these rankings without considering the magnitude of actual differences between interventions and the certainty of the evidence [6] [7].
Table 2: Key Methodological Considerations in NMA Protocol Design
| Methodological Aspect | Protocol Requirements | Recommended Approaches |
|---|---|---|
| Network Geometry | Describe all interventions and available comparisons | Create network diagram with nodes (interventions) and edges (direct comparisons) [6] |
| Transitivity Assessment | Evaluate similarity across studies in effect modifiers | Assess distribution of patient characteristics, intervention details, outcome definitions across comparisons [6] |
| Statistical Synthesis | Specify model for combining direct and indirect evidence | Choose between frequentist or Bayesian framework, fixed or random effects models [25] [6] |
| Incoherence Assessment | Evaluate consistency between direct and indirect evidence | Use side-splitting or node-splitting methods, design-by-treatment interaction model [6] |
| Certainty Assessment | Evaluate confidence in NMA estimates | Apply GRADE or CINeMA frameworks for network estimates [6] [7] |
Updates and Evolving Methodological Standards
The field of NMA is rapidly evolving, necessitating ongoing updates to reporting guidelines. A 2025 scoping review identified 61 studies relevant to updating PRISMA-NMA, including 23 guidance documents and 38 overviews assessing the completeness or quality of NMA reporting [26]. This review identified 37 additional reporting items that will inform the upcoming PRISMA-NMA update through a Delphi consensus process [26].
Several pressing reasons necessitate updating the 2015 PRISMA-NMA guideline. First, assessments of reporting completeness have revealed that some NMA elements remain incompletely reported, suggesting that additional items or modifications to existing items may be needed [23]. Second, important methodological advances have occurred since 2015, including techniques for modeling complex interventions, handling missing data, assessing transitivity, and evaluating certainty of evidence [23]. Third, the PRISMA statement was updated in 2020 to reflect advances in systematic review conduct and reporting, and the NMA extension requires alignment with this updated structure [23] [27].
The updating process follows rigorous methodology, including comprehensive scoping reviews, Delphi surveys involving diverse stakeholders, consensus meetings, and the development of explanation and elaboration documents [23] [26]. This process also incorporates perspectives previously omitted from guideline development, including patients and the public, alongside journal editors, clinicians, policymakers, statisticians, and methodologists [23].
Figure 2: PRISMA-NMA Guideline Development and Update Timeline
Research Reagent Solutions: Tools for NMA Implementation
Successful implementation of a PRISMA-NMA compliant review requires familiarity with specialized software tools and methodological resources. These "research reagents" facilitate various stages of the NMA process, from data synthesis to visualization and reporting.
MetaInsight represents a particularly valuable tool for researchers new to NMA, as it provides a web-based, point-and-click interface for conducting NMAs without requiring knowledge of specialist statistical packages [25]. This open-access tool leverages established R routines (specifically the netmeta package) but operates behind the scenes on a webserver, eliminating the need for users to install statistical software [25]. MetaInsight supports both binary and continuous outcomes for fixed and random effects models and facilitates sensitivity analyses through interactive inclusion and exclusion of studies [25].
For advanced applications and customized analyses, statistical programming environments remain essential. R with packages such as netmeta for frequentist approaches and BUGS or JAGS for Bayesian implementations provide greater flexibility but require substantial statistical programming expertise [25] [6]. The Cochrane Handbook provides comprehensive guidance on the application of these methods, though it appropriately notes that "authors will need a knowledgeable statistician to plan and execute these methods" [6].
Table 3: Essential Research Tools for PRISMA-NMA Implementation
| Tool Category | Specific Tools | Primary Function | Access Requirements |
|---|---|---|---|
| Reporting Guidelines | PRISMA-NMA Checklist [21] | Ensures complete reporting of NMA methods and findings | Freely available from prisma-statement.org |
| Statistical Software | R with netmeta package [25] | Conducts frequentist NMA with comprehensive statistical options | Open source, requires programming knowledge |
| Web Applications | MetaInsight [25] | Provides point-and-click interface for NMA without coding | Freely available web application, no installation required |
| Methodological Guidance | Cochrane Handbook Chapter 11 [6] | Offers comprehensive guidance on NMA methodology and conduct | Freely available from cochrane.org/handbook |
Comparative Analysis of NMA Reporting Completeness
Empirical evaluations of NMA reporting have identified persistent gaps despite the availability of the PRISMA-NMA guideline. A 2025 scoping review highlighted that key recommendations on statistical methods were often missed in NMA reporting [26]. This finding aligns with earlier observations that some elements of the PRISMA-NMA checklist are incompletely reported, even in high-impact journals [23].
The forthcoming update to PRISMA-NMA aims to address these reporting gaps by incorporating items related to recent methodological developments. These include methods for assessing effect modification, defining intervention nodes in complex networks, implementing advanced statistical models, and applying frameworks for evaluating the certainty of evidence from NMAs [23] [26]. The updated guideline will also align with the structure of PRISMA 2020, which uses broad elements rather than the more specific items of the original PRISMA statement [23].
Transparent reporting of NMAs has implications beyond academic completeness. Inadequate reporting hampers proper quality assessment, potentially leading to erroneous health recommendations and negative impacts on patient care and policy [23]. Furthermore, as NMAs are increasingly used by health technology assessment bodies like NICE (National Institute for Health and Care Excellence) to inform coverage decisions, complete reporting becomes essential for justifying resource allocation decisions [25].
The development of the PRISMA-NMA update incorporates multi-stakeholder perspectives, including patients and the public, to ensure that the reporting guideline addresses aspects important to all consumers of systematic reviews [23]. This inclusive approach strengthens the relevance and applicability of the guideline across diverse user groups, from clinical decision-makers to policy developers and patient advocates.
The PRISMA-NMA guideline provides an essential framework for conducting and reporting systematic reviews incorporating network meta-analyses, particularly in the context of therapeutic equivalence research. As the methodology continues to evolve with advancements in statistical modeling, evidence assessment, and implementation tools, the reporting standards must similarly advance to ensure transparency, reproducibility, and utility for decision-makers.
The forthcoming update to PRISMA-NMA, informed by comprehensive scoping reviews and multi-stakeholder consensus, will address persistent reporting gaps while incorporating recent methodological developments. Researchers designing systematic review protocols for NMA should adhere to the current PRISMA-NMA checklist while remaining attentive to the updated guideline upon its publication. Through complete and transparent reporting of NMAs, the scientific community can enhance the validity and impact of this powerful methodology for comparing multiple healthcare interventions.
Conducting a Feasibility Assessment for Network Connectivity and Clinical Heterogeneity
Indirect treatment comparisons (ITCs) and network meta-analyses (NMAs) enable comparative effectiveness assessments of multiple treatments, which is particularly valuable when head-to-head randomized controlled trials (RCTs) are unavailable [3]. A feasibility assessment systematically evaluates whether the available RCT evidence base is suitable for robust ITC/NMA by identifying methodological and clinical challenges that could introduce bias [28] [29]. This assessment is a critical preliminary step mandated by various health technology assessment (HTA) agencies to ensure the validity of subsequent comparative analyses [3].
The core objective of a feasibility assessment is to evaluate transitivity - the likelihood that patients in different trials are sufficiently similar to allow meaningful comparison - and network connectivity - whether trials are adequately linked through common comparators to form a connected evidence network [28] [29]. When conducted within the context of evaluating therapeutic equivalence, this assessment ensures that comparative efficacy estimates reliably inform clinical and reimbursement decisions.
Key Methodological Challenges in Feasibility Assessment
Critical Barriers to Robust Network Meta-Analysis
Feasibility assessments systematically identify challenges across trial design, population characteristics, and outcome measurement that threaten the validity of ITCs. Evidence from therapeutic areas including generalized myasthenia gravis (gMG) and chronic low back pain disorders reveals several consistent methodological barriers [28] [4].
Table 1: Key Challenges Identified in Feasibility Assessments
| Challenge Category | Specific Barriers | Impact on ITC/NMA Validity |
|---|---|---|
| Population Heterogeneity | Cross-trial differences in treatment effect modifiers (e.g., antibody status, disease duration, prior treatments) [28] | Violates exchangeability assumption; introduces bias in effect estimates |
| Trial Design Variations | Inconsistent dosing strategies (cyclical vs. continuous), placebo administration characteristics, background therapies [28] [29] | Compromises network connectivity and transitivity |
| Outcome Assessment | Variable assessment timepoints, different measurement instruments, small trial sizes [28] [4] | Reduces reliability of pooled effect estimates |
| Network Connectivity | Limited common comparators, sparse evidence networks, within-trial imbalances [28] | Limits feasibility of anchored comparisons |
Quantitative Assessment of Feasibility Parameters
A structured feasibility assessment evaluates specific quantitative and qualitative parameters across the available evidence base. The assessment of 15 gMG RCTs demonstrated how systematic evaluation identifies methodological concerns [28] [29].
Table 2: Quantitative Parameters for Feasibility Assessment
| Assessment Domain | Data Extraction Requirements | Acceptability Threshold |
|---|---|---|
| Patient Characteristics | Baseline disease severity, disease duration, antibody status, prior treatment exposure, demographic factors [28] | Similar distributions across trials (<15% standardized mean differences) |
| Intervention Characteristics | Dosing schedules, treatment strategies (cyclic/continuous), administration routes, background therapies [29] | Consistency in intensity, frequency, and concomitant treatments |
| Outcome Measurement | Assessment timepoints, measurement instruments, follow-up duration, missing data handling [28] [4] | Comparable timepoints (±25% of trial duration); consistent instruments |
| Network Connectivity | Number of trials per treatment, common comparator availability, evidence network structure [28] [3] | Connected network with at least one common comparator |
Experimental Protocols for Feasibility Assessment
Protocol 1: Systematic Literature Review Framework
A systematic literature review (SLR) following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines forms the evidence base for feasibility assessments [29] [4].
Methodology:
- Search Strategy: Identify biomedical databases, conference proceedings, regulatory agency websites, and clinical trial registries using PICOS (Participants, Interventions, Comparators, Outcomes, Study design) framework [29]
- Study Selection: Implement dual independent review with pre-specified eligibility criteria, with disagreements resolved through adjudication [4]
- Data Extraction: Standardized extraction of trial design, population characteristics, interventions, outcomes, and results
- Quality Assessment: Evaluate risk of bias using appropriate tools (e.g., Cochrane Risk of Bias tool)
The SLR protocol should be developed a priori and registered in platforms like PROSPERO to enhance transparency and reduce selective reporting bias [4].
Protocol 2: Network Connectivity and Transitivity Assessment
This protocol evaluates whether trials can form a connected network and whether the transitivity assumption holds across treatment comparisons.
Methodology:
- Evidence Network Mapping: Graphically represent all treatments and trials, identifying common comparators and network structure [28]
- Treatment Effect Modifier Identification: Identify potential effect modifiers through clinical input and systematic literature review [28] [29]
- Cross-Trial Similarity Assessment: Compare distribution of effect modifiers across trials using standardized mean differences and visual inspection (forest plots, radar charts) [28]
- Placebo Response Evaluation: Assess variation in placebo response across trials, which may reflect imbalances in unreported effect modifiers [29]
Diagram 1: Feasibility Assessment Workflow
Protocol 3: Comparative Performance of ITC Methods
This protocol evaluates the relative performance of different ITC approaches under identified feasibility constraints.
Methodology:
- Method Selection: Identify appropriate ITC methods based on feasibility assessment findings (e.g., network meta-analysis, matching-adjusted indirect comparison, simulated treatment comparisons) [29]
- Analytical Comparison: Implement multiple ITC methods where feasible to assess consistency of results
- Sensitivity Analysis: Evaluate robustness of findings to different methodological assumptions (e.g., fixed vs. random effects, adjustment variables)
- Bias Assessment: Identify potential sources of bias specific to each method given the evidence base limitations [28]
The Researcher's Toolkit: Essential Materials for Feasibility Assessment
Table 3: Essential Research Reagents and Tools for Feasibility Assessment
| Tool/Resource | Function in Assessment | Implementation Considerations |
|---|---|---|
| PRISMA-NMA Guidelines [4] | Standardized reporting framework for systematic reviews and network meta-analyses | Ensure protocol includes all recommended elements before commencing assessment |
| Grading of Recommendations Assessment, Development and Evaluation (GRADE) [4] | Quality assessment of evidence from NMA | Assess quality of direct, indirect, and network estimates separately |
| Systematic Review Software (e.g., Covidence) [4] | Manage screening, data extraction, and quality assessment | Implement dual independent review with adjudication process |
| Network Meta-Analysis Software (e.g., R, Stata) | Statistical implementation of NMA models | Select software based on complexity of evidence network and analytical needs |
| Gantt Chart Project Management [30] [31] | Visual timeline for managing assessment phases and milestones | Update regularly to reflect progress and adjust timelines for challenges |
| AES-135 | AES-135, MF:C33H29F6N3O5S, MW:693.7 g/mol | Chemical Reagent |
| Amino-PEG4-hydrazide-Boc | Amino-PEG4-hydrazide-Boc, MF:C16H33N3O7, MW:379.45 g/mol | Chemical Reagent |
Visualization of Evidence Network Assessment
The evidence network structure fundamentally determines the feasibility of different ITC approaches. Networks must be connected through common comparators, with sufficient trials per treatment to enable reliable estimation.
Diagram 2: Evidence Network Structure
Feasibility assessments for network connectivity and clinical heterogeneity are methodologically rigorous processes that should precede any ITC or NMA. The assessment systematically identifies challenges related to population heterogeneity, trial design variations, outcome assessment inconsistencies, and network connectivity limitations [28] [29]. By implementing structured protocols for systematic literature review, network connectivity evaluation, and comparative method performance, researchers can determine the appropriate analytical approach and interpret results within identified limitations. The growing emphasis on these assessments by HTA agencies worldwide underscores their critical role in generating reliable evidence for healthcare decision-making [3]. When therapeutic equivalence is the research objective, a thorough feasibility assessment provides the necessary foundation for valid comparative effectiveness estimates that can confidently inform clinical practice and health policy.
In the field of medical research, particularly in evaluating therapeutic equivalence through network meta-analysis (NMA), the choice of statistical framework is far from merely academic. Researchers and drug development professionals must navigate between two dominant statistical paradigms: Frequentist and Bayesian approaches. These frameworks offer fundamentally different philosophies for interpreting probability, incorporating evidence, and quantifying uncertainty. The Frequentist approach interprets probability as the long-term frequency of an event occurring, treating parameters as fixed unknown values to be estimated through procedures like null hypothesis significance testing (NHST) with p-values [32] [33]. In contrast, the Bayesian framework views probability as a measure of belief or certainty about an event, allowing parameters to be described with probability distributions that are updated as new data becomes available [32] [33].
Within evidence synthesis, NMA has emerged as a powerful statistical method that enables the simultaneous comparison of multiple treatments, even when they haven't been directly compared in head-to-head trials, by combining direct and indirect evidence into a coherent analysis [34] [35]. This capability is particularly valuable for health technology assessment and clinical guideline development, where decisions must be made across a spectrum of available interventions. The fundamental difference in how these approaches handle prior information is noteworthy: Bayesian methods explicitly incorporate prior knowledge or beliefs through prior distributions, which are then updated with trial data to form posterior distributions [34] [33]. Frequentist methods, meanwhile, rely solely on the data at hand, using maximum likelihood estimation and hypothesis testing without formal incorporation of external evidence [32].
Theoretical Foundations and Comparative Mechanics
Core Philosophical Differences
The theoretical divergence between Frequentist and Bayesian statistics manifests most profoundly in their interpretation of probability and treatment of uncertainty. The Frequentist paradigm is grounded in the concept of long-run frequencies, where probabilities represent the relative frequency of an event occurring over many repeated trials or experiments [33]. This framework treats population parameters as fixed, unknown quantities and relies on sampling distributions—what one would expect to see if an experiment were repeated numerous times. Inference is typically conducted through null hypothesis significance testing and confidence intervals, with the infamous p-value measuring the probability of observing data as extreme as, or more extreme than, the actual results, assuming the null hypothesis is true [32].
The Bayesian framework offers a fundamentally different perspective, interpreting probability as a subjective measure of belief or certainty about propositions [32]. Within this paradigm, parameters are treated as random variables described by probability distributions, reflecting the uncertainty about their true values. Bayesian inference formally incorporates prior beliefs about parameters through prior distributions, which are then updated with observed data via Bayes' theorem to form posterior distributions [34] [33]. This posterior distribution represents a complete summary of current knowledge about the parameters, combining both prior information and new evidence. For hypothesis testing, Bayes factors provide a natural mechanism for comparing the relative evidence for two competing hypotheses, representing the ratio of the marginal likelihood of the data under each hypothesis [32].
Implementation in Network Meta-Analysis
In the specific context of network meta-analysis, both statistical frameworks have established methodologies for synthesizing evidence across a network of trials. The Bayesian approach to NMA typically employs Markov Chain Monte Carlo (MCMC) sampling methods implemented in software like WinBUGS/OpenBUGS or Stan to estimate posterior distributions of treatment effects [36] [34]. This method naturally accommodates complex hierarchical models and provides direct probability statements about treatment effects and rankings. A key advantage is the ability to incorporate informative prior distributions when genuine prior information exists, though vague or non-informative priors are often used in the absence of strong prior knowledge [34] [35].
The Frequentist approach to NMA typically employs generalized linear mixed models or multivariate meta-analysis techniques, estimated using maximum likelihood or restricted maximum likelihood methods [35]. Implementation is often facilitated through packages in R or Stata, with inference based on confidence intervals and p-values. While this approach doesn't formally incorporate prior evidence through probability distributions, it benefits from computational efficiency and more straightforward implementation for standard models [35]. For the assumption of evidence consistency—the fundamental principle that direct and indirect evidence should agree, within random error—both frameworks offer evaluation methods, with Bayesian approaches using node-splitting or model comparison via deviance information criterion (DIC), and Frequentist approaches employing statistical tests for inconsistency [34] [35].
Performance Comparison in Research Applications
Analytical Framework and Experimental Protocols
To objectively evaluate the performance characteristics of Bayesian and Frequentist approaches across various research contexts, we have synthesized evidence from multiple methodological studies and applied analyses. The comparative framework examines performance across several dimensions: statistical properties (bias, coverage), operational characteristics (computational demands, convergence behavior), and practical utility (interpretability, decision-making support). These dimensions are assessed across different data scenarios, including variations in sample size, missing data, and model complexity.
The experimental protocols from key comparative studies share a common structure: (1) definition of data-generating mechanisms, (2) specification of analytical models in both frameworks, (3) implementation using standard software packages, and (4) evaluation using predefined performance metrics. For instance, in the epidemic forecasting study by Karami et al., both approaches were implemented using deterministic compartmental models, with Frequentist estimation via nonlinear least squares optimization and Bayesian estimation using MCMC sampling via Stan [36]. Performance was assessed on both simulated datasets (with known R0 values of 2 and 1.5) and historical datasets including the 1918 influenza pandemic and COVID-19 pandemic, using metrics including Mean Absolute Error, Root Mean Squed Error, Weighted Interval Score, and 95% prediction interval coverage [36].
In Alzheimer's disease research, longitudinal modeling of hippocampal volume was conducted using linear mixed effects models under both frameworks, with performance evaluated across datasets with varying levels of completeness and sample sizes [37]. The Frequentist approach was implemented using standard maximum likelihood estimation, while the Bayesian approach employed MCMC sampling with Hamiltonian Monte Carlo in Stan. Performance metrics included model convergence rates, precision of parameter estimates, and ability to detect known group differences across different data configurations [37].
Figure 1: Experimental Protocol for Method Comparison
Quantitative Performance Metrics
Table 1: Comparative Performance Across Research Domains
| Research Domain | Performance Metrics | Bayesian Approach | Frequentist Approach |
|---|---|---|---|
| Epidemic Forecasting [36] | Mean Absolute Error (MAE) | Higher accuracy in pre-peak phases | Better performance at peak and post-peak phases |
| 95% Prediction Interval Coverage | More robust uncertainty quantification | Interval estimates may be less robust | |
| Longitudinal Modeling (AD) [37] | Model Convergence with Sparse Data | Successful even with high missing data | Failed with high missing data points |
| Subjects Needed for Detection | ~115 subjects for conversion detection | ~147 subjects for group differentiation | |
| Cardioprotection NMA [38] | Treatment Effect Detection | No significant benefits detected | Significant benefits for AA and BB treatments |
| Conclusion Consistency | Insufficient evidence for prophylaxis | Supported AA or BB cardioprotection | |
| Alcohol Dependence MTC [34] | Treatment Ranking | Combination therapy highest probability of being best | Limited ability to rank infrequently compared treatments |
| Evidence Incorporation | Effectively combines direct and indirect evidence | Pairwise meta-analysis less efficient |
Context-Dependent Performance Patterns
The comparative performance evidence reveals a consistent pattern of context-dependent advantages rather than universal superiority of either approach. In epidemic forecasting, the choice between frameworks depends significantly on the epidemic phase and data characteristics [36]. Bayesian methods, particularly those with uniform priors, demonstrated superior accuracy during early epidemic phases when data is typically sparse and noisy, while Frequentist methods performed better at peak and post-peak phases when more data is available. This pattern underscores how the data environment influences relative performance.
In longitudinal modeling of Alzheimer's disease progression, the Bayesian approach demonstrated remarkable robustness to data sparsity, successfully estimating linear mixed effects models even with high rates of missing data where Frequentist methods failed to converge [37]. This advantage is particularly valuable in real-world clinical research settings where missing data is common due to patient dropout, missed visits, or other practical constraints. The Bayesian framework also required fewer subjects to detect conversion from mild cognitive impairment to Alzheimer's disease (115 vs. 147 subjects), highlighting its efficiency with smaller sample sizes when prior information is incorporated [37].
Perhaps most intriguing are the cases where the two frameworks lead to different substantive conclusions from the same data. In the network meta-analysis of cardioprotective agents for breast cancer patients receiving anthracycline chemotherapy, the Bayesian analysis showed no significant difference in left ventricular ejection fraction preservation between any active treatment and placebo, while the Frequentist analysis detected significant benefits for angiotensin-converting enzyme inhibitors/angiotensin receptor blockers and beta-blockers [38]. This divergence highlights how the fundamental differences in statistical philosophy can translate to meaningfully different clinical interpretations, particularly in settings with limited evidence.
Practical Implementation in Therapeutic Evaluation
Methodological Workflow for NMA
Table 2: Essential Research Reagents for NMA Implementation
| Research Reagent | Function/Purpose | Implementation Considerations |
|---|---|---|
| Statistical Software (R/Stata) | Provides computational environment for Frequentist NMA | R packages: netmeta, gemtc; Stata: network group commands |
| Bayesian MCMC Software (WinBUGS/Stan) | Enables Bayesian posterior sampling | WinBUGS/OpenBUGS for standard models; Stan for complex models requiring Hamiltonian Monte Carlo |
| Prior Distribution Specifications | Encodes pre-existing evidence in Bayesian framework | Vague priors (e.g., N(0,10000)) when limited prior information; informed priors based on historical data |
| Consistency Evaluation Tools | Assesses agreement between direct and indirect evidence | Node-splitting methods; inconsistency models; deviance information criterion (DIC) comparison |
| Convergence Diagnostics | Verifies reliability of Bayesian MCMC sampling | Gelman-Rubin statistic (R-hat); trace plots; effective sample size; autocorrelation assessment |
Implementing network meta-analysis for therapeutic evaluation requires careful attention to methodological details specific to each statistical framework. The Bayesian workflow typically begins with model specification, including choice of fixed or random effects, selection of appropriate likelihood functions, and specification of prior distributions for all parameters [34]. For binary outcomes, such as relapse or mortality, logistic regression models with difference parameterizations are commonly employed, while continuous outcomes typically use normal likelihoods with identity links [34]. The computational engine involves MCMC sampling, which requires careful monitoring for convergence using diagnostics like the Gelman-Rubin statistic, trace plots, and effective sample size calculations [34]. Model criticism and comparison may utilize measures like the deviance information criterion (DIC) to compare alternative model formulations [34].
The Frequentist implementation follows a different pathway, typically employing generalized linear mixed models estimated via maximum likelihood or restricted maximum likelihood [35]. The process involves model specification, parameter estimation through optimization algorithms, and inference based on confidence intervals and p-values. Assessment of heterogeneity and consistency assumptions is crucial, with statistical tests available to evaluate the agreement between direct and indirect evidence [35]. For both approaches, the recent development of automated software packages has significantly improved accessibility, though understanding the underlying assumptions remains essential for appropriate application [35].
Figure 2: NMA Workflows for Therapeutic Evaluation
Decision Framework for Researchers
Selecting between Bayesian and Frequentist approaches requires careful consideration of the specific research context, available resources, and analytical objectives. Based on the synthesized evidence, the following decision framework provides guidance for researchers conducting therapeutic evaluations:
Choose Bayesian approaches when: Working with complex models requiring hierarchical structures; analyzing sparse data or studies with high missing data rates; incorporating genuine prior information from previous studies; making direct probability statements about parameters or treatment rankings is important; modeling uncertainty in complex uncertainty structures [34] [37].
Prefer Frequentist approaches when: Analyzing complete datasets with sufficient sample sizes; computational efficiency is a primary concern; straightforward interpretation through confidence intervals and p-values is preferred; limited statistical expertise for Bayesian model checking and convergence diagnostics is available; traditional reporting formats requiring p-values are necessary [32] [37].
Consider hybrid approaches when: Conducting sensitivity analyses to assess robustness of conclusions; leveraging complementary strengths of both frameworks; addressing reviewer concerns from diverse methodological perspectives; developing methods that combine computational advantages of both approaches [38].
For researchers specifically working in network meta-analysis for therapeutic evaluation, current evidence suggests that when analysts choose appropriate models, there are seldom important differences in the results of Bayesian and Frequentist approaches [35]. The focus should therefore be on model features rather than the statistical framework per se, selecting approaches that best address the specific research question while providing appropriate uncertainty quantification.
The comparative evaluation of Bayesian and Frequentist approaches for network meta-analysis in therapeutic research reveals a nuanced landscape where methodological choices should be driven by specific research contexts rather than universal prescriptions. The Bayesian framework offers distinct advantages for complex evidence synthesis, particularly through its formal incorporation of prior evidence, natural handling of uncertainty, and direct probabilistic interpretation of results [34] [37]. These strengths make it particularly valuable for decision-making in drug development and health technology assessment, where ranking treatments and quantifying decision uncertainty are paramount.
The Frequentist paradigm maintains important advantages in computational efficiency, implementation simplicity for standard models, and familiarity among broader research audiences [35] [32]. Its straightforward interpretation through confidence intervals and p-values, despite well-documented limitations, continues to make it accessible for applied researchers with varying statistical backgrounds. The empirical evidence suggests that in many practical scenarios with sufficient data and well-specified models, both approaches yield substantively similar conclusions [35] [38].
For contemporary drug development professionals and researchers, the emerging consensus emphasizes methodological appropriateness over ideological allegiance. The most effective approach often involves understanding both frameworks sufficiently to leverage their complementary strengths, whether through formal Bayesian analyses with sensitivity to prior specifications, carefully conducted Frequentist analyses with appropriate attention to underlying assumptions, or innovative hybrid approaches that combine elements of both traditions [38]. As methodological research continues to advance, the integration of these frameworks promises to enhance the rigor and relevance of therapeutic evaluation, ultimately supporting more informed decisions about treatment efficacy and safety.
In the evaluation of therapeutic equivalence through network meta-analysis (NMA), researchers must accurately interpret key statistical outputs, including risk ratios, hazard ratios, and their associated intervals. These measures allow for the simultaneous comparison of multiple treatments by synthesizing both direct and indirect evidence. This guide provides an objective comparison of these outputs, detailing their calculations, interpretations, and roles in NMA to inform decision-making in drug development.
Network meta-analysis extends conventional pairwise meta-analysis by enabling the simultaneous comparison of multiple interventions for a given condition. This methodology integrates direct evidence (from studies that directly compare two treatments) and indirect evidence (where the relative effect of two treatments is inferred through a common comparator) into a single, cohesive statistical model [6] [39]. The validity of this approach hinges on the assumption of transitivity, which posits that the different sets of studies included are sufficiently similar in all important factors that could influence the relative treatment effects [6]. The statistical manifestation of this assumption is consistency, meaning that direct and indirect evidence for a particular treatment comparison are in agreement [39]. Within this framework, measures like risk ratios and hazard ratios serve as the fundamental units for comparing therapeutic efficacy and safety, while confidence and credible intervals quantify the precision and reliability of these estimates, directly impacting conclusions about therapeutic equivalence.
Defining and Comparing Key Ratio Measures
Risk ratios, odds ratios, and hazard ratios are ubiquitous in clinical research, yet they are often misused or misunderstood. The table below summarizes their core definitions, calculations, and applications.
Table 1: Comparison of Key Ratio Measures in Biomedical Research
| Measure | Calculation | Interpretation | Common Applications |
|---|---|---|---|
| Risk Ratio (RR)(Relative Risk) | ( RR = \frac{\text{Risk in Intervention Group}}{\text{Risk in Control Group}} ) [40] [41] | RR = 1: Both groups have the same risk [40].RR > 1: Intervention group bears higher risk.RR < 1: Intervention group bears lower risk. | Prospective studies like randomized controlled trials and cohort studies [41]. |
| Odds Ratio (OR) | ( OR = \frac{\text{Odds in Intervention Group}}{\text{Odds in Control Group}} )Where Odds = ( \frac{\text{Probability of Event}}{1 - \text{Probability of Event}} ) [41] | OR = 1: No difference between groups.OR > 1: Positive association between exposure and outcome.OR < 1: Negative association [41]. | Case-control studies and logistic regression models [41]. |
| Hazard Ratio (HR) | ( HR = \frac{\text{Hazard Rate in Intervention Group}}{\text{Hazard Rate in Control Group}} ) [41] | HR = 1: Both groups experience the same number of events per unit of time.HR > 1: Higher event probability in the intervention group within any given period.HR < 1: Lower event probability in the intervention group [41]. | Time-to-event analyses, such as survival analysis in clinical trials to assess duration of symptoms or mortality [40] [41]. |
Risk Ratio (RR)
The risk ratio is an intuitive measure that compares the probability of an event between two groups. Its calculation is straightforward, dividing the risk (or proportion) of an event in the intervention group by the risk in the control group [40]. For example, if a study reports that patients with a prolonged QTc interval were 2.5 times more likely to die within 90 days compared to those without (RR=2.5; 95% CI 1.5-4.1), it means the risk of death is 150% higher in the group with a prolonged interval [40]. RR is most appropriate for studies where risks can be meaningfully estimated, such as in prospective cohort studies or randomized controlled trials.
Hazard Ratio (HR)
The hazard ratio is a comparative measure of the instantaneous event rate at any specific point in time. It is commonly derived from survival analysis methods like Cox proportional hazards regression. Unlike the RR, which often considers a single event over a defined period, the HR accounts for the timing of events, providing a more dynamic view of treatment effect [41]. It is the preferred metric in clinical trials where the time until an event (e.g., death, relapse) is a critical outcome, as it can determine whether an intervention reduces symptom duration or prolongs survival [41].
Interpreting Confidence Intervals and Credible Intervals
Beyond point estimates, the intervals surrounding risk, odds, and hazard ratios are crucial for assessing the precision and uncertainty of the results.
Confidence Intervals
A confidence interval (CI) is a frequentist statistic that provides a range of values in which the population parameter (e.g., the true risk ratio) is likely to lie. A 95% CI, the standard in clinical research, is constructed such that, upon infinite repetition of the study, 95% of such intervals would contain the true population statistic [40]. Interpretation is key: if the 95% CI for a risk ratio includes the value 1.0, the results are not statistically significant at the 5% level, indicating no evidence of a difference between groups [40]. For example, a study on foot orthoses reported an RR of 1.63 but with a 95% CI of 0.96 to 2.76. Because this interval includes 1.0, there is insufficient evidence to conclude that orthoses have a significant effect on adverse events [40].
Credible Intervals
A credible interval is the Bayesian counterpart to a confidence interval. It represents the range within which an unobserved parameter (e.g., a hazard ratio) falls with a given subjective probability, based on the posterior distribution which incorporates both prior knowledge and the observed data [42]. While a confidence interval pertains to the long-run frequency of the procedure, a credible interval makes a probability statement about the parameter itself [42]. Credible intervals can be particularly valuable in scenarios with sparse data or when incorporating external information is necessary. For instance, in a trial where an adverse event occurs in 0 out of 1000 patients in both treatment and placebo groups, a frequentist CI might be uninformative, but a Bayesian analysis with a sensible prior can provide a more plausible range for the odds ratio [42].
Experimental Protocols for Network Meta-Analysis
Implementing a network meta-analysis requires a structured approach to ensure validity and reliability. The following protocol outlines the key steps.
Protocol for Conducting a Network Meta-Analysis
Objective: To synthesize direct and indirect evidence for multiple interventions to estimate their relative ranking and efficacy. Methodology:
- Define the Research Question: Pre-specify the population, interventions, comparators, and outcomes of interest.
- Systematic Literature Review: Conduct a comprehensive search across multiple databases to identify all relevant randomized controlled trials comparing any of the predefined interventions.
- Data Extraction: Extract data in a format suitable for NMA. Essential data items include:
- Study identifier.
- Treatment 1 and Treatment 2 (the compared interventions).
- Treatment effect estimate (e.g., log(RR), log(HR), or log(OR)) for the outcome.
- Standard error of the treatment effect estimate.
- Network Geometry Exploration: Create a network diagram to visualize the available direct comparisons. The
netgraphfunction in R (using packages likenetmeta) can generate this, where nodes represent treatments and edges represent direct comparisons [43]. - Statistical Synthesis and Model Fitting: Use appropriate NMA models (e.g., frequentist or Bayesian) to synthesize the data. The analysis will produce pooled effect estimates for all possible treatment comparisons, both direct and indirect.
- Assess Transitivity and Incoherence: Evaluate the validity of the transitivity assumption by comparing the distribution of potential effect modifiers across treatment comparisons. Statistically, assess incoherence (inconsistency) to check if direct and indirect evidence for a specific comparison are in agreement [6] [39].
- Rank Treatments: Estimate the relative ranking of each intervention for the given outcome (e.g., surface under the cumulative ranking curve, SUCRA).
- Evaluate Confidence in Evidence: Use tools like the CINeMA (Confidence in Network Meta-Analysis) framework to rate the quality of the evidence derived from the NMA [6].
Figure 1: NMA Workflow. A flowchart detailing the key steps in conducting a network meta-analysis.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Network Meta-Analysis
| Item | Function |
|---|---|
| R Statistical Software | A free, open-source programming language and environment for statistical computing and graphics [43]. |
netmeta R Package |
A dedicated R package that provides a comprehensive suite of functions to perform frequentist network meta-analyses, create network diagrams, and assess inconsistency [43]. |
| Bibliographic Databases | Databases such as PubMed, EMBASE, and Cochrane Central are essential for conducting the systematic review to identify all relevant primary studies. |
| Data Extraction Sheet | A standardized form (often created in Excel or similar software) for systematically recording study characteristics, interventions, and outcome data from included trials. |
| AZD-7762 hydrochloride | AZD-7762 hydrochloride, CAS:1246094-78-9, MF:C17H20ClFN4O2S, MW:398.9 g/mol |
Critical Appraisal of NMA Outputs
Evaluating a Network Diagram
The network diagram is the foundational visual tool in any NMA. It should be examined for its completeness and connectivity. A well-connected network, where treatments are linked through multiple pathways, generally leads to more robust and precise estimates. The presence of closed loops in the network allows for the statistical assessment of incoherence between direct and indirect evidence [6]. For example, a loop formed by interventions A, B, and C (where studies exist for A vs. B, B vs. C, and A vs. C) can be used to check if the direct estimate for A vs. C agrees with the indirect estimate derived from the A vs. B and B vs. C studies [39].
Interpreting Combined Evidence
In a network meta-analysis, the final output for a treatment comparison is typically a pooled estimate that combines direct and indirect evidence. It is vital to understand that indirect evidence, while valuable, often comes with greater statistical uncertainty. The variance of an indirect effect estimate is approximately the sum of the variances of the two direct estimates used to create it [39]. Therefore, while combining evidence can increase precision, estimates based solely on indirect evidence or long chains of comparisons will be less precise than those with strong, direct head-to-head evidence.
Figure 2: Direct and Indirect Evidence. This graph illustrates a network where the comparison between Treatment B and Treatment D (dashed line) can be estimated indirectly via the path B-A-C-D.
Accurate interpretation of risk ratios, hazard ratios, and their associated intervals is fundamental to deriving valid conclusions from a network meta-analysis. Risk ratios offer an intuitive measure of relative probability, while hazard ratios provide a dynamic assessment of time-to-event outcomes. Confidence intervals quantify the uncertainty of frequentist estimates, whereas credible intervals offer a Bayesian probability statement. For researchers evaluating therapeutic equivalence, a critical appraisal of the network geometry, the mix of direct and indirect evidence, and the statistical consistency of the network is imperative. By adhering to rigorous methodologies and correctly interpreting these key outputs, drug development professionals can make informed decisions about the relative efficacy and safety of competing interventions.
In the evolving landscape of comparative effectiveness research, Network Meta-Analysis (NMA) has become an indispensable tool for evaluating multiple treatments for the same condition, even when they have never been directly compared in head-to-head clinical trials. A critical output of NMA is treatment ranking, which provides clinicians and healthcare decision-makers with a hierarchy of interventions based on their relative efficacy or safety. Among the various ranking metrics developed, three prominent measures have emerged: the Probability of Being Best (Pbest), the Surface Under the Cumulative Ranking Curve (SUCRA), and the P-score. This guide objectively compares the performance, applications, and limitations of these metrics within the broader context of evaluating therapeutic equivalence in NMA research, providing researchers and drug development professionals with a framework for selecting appropriate ranking methods for their evidence synthesis needs.
Quantitative Comparison of Ranking Metrics
The table below summarizes the core characteristics, advantages, and limitations of the three primary treatment ranking metrics used in network meta-analysis.
Table 1: Comprehensive Comparison of Treatment Ranking Metrics in Network Meta-Analysis
| Feature | Probability of Being Best (Pbest) | SUCRA (Surface Under the Cumulative Ranking Curve) | P-score |
|---|---|---|---|
| Definition | The probability that a treatment is the most effective among all compared treatments [44]. | The surface under the cumulative ranking curve, representing the relative probability of a treatment being better than competing treatments [45] [46] [47]. | The mean extent of certainty that a treatment is better than competing treatments, calculated as the mean of one-sided p-values from pairwise comparisons [45] [44]. |
| Interpretation | 0 to 1 (or 0% to 100%); higher values indicate a higher probability of being the best treatment. | 0 to 1 (or 0% to 100%); higher values indicate a better overall rank [47]. | 0 to 1 (or 0% to 100%); higher values indicate a better treatment [45]. |
| Basis of Calculation | Derived from the posterior distribution of treatment effects (Bayesian) or via resampling/simulation (Frequentist). | Derived from the entire distribution of rank probabilities [44] [46]. | Based on point estimates and standard errors of network meta-analysis under normality assumption [45]. |
| Key Advantage | Intuitively simple to understand. | Considers the entire ranking distribution, not just the top rank [44]. | Does not require resampling or simulation; easy to compute from frequentist NMA output [45]. |
| Primary Limitation | Ignores the uncertainty and the entire ranking distribution; can be misleading, especially for imprecisely estimated treatments [44]. | Requires resampling in the frequentist framework. Less intuitive than Pbest. | Like SUCRA, offers no major advantage over inspecting confidence/credible intervals [45]. |
| Framework | Originally Bayesian, but can be approximated in frequentist settings. | Originally Bayesian [46]. | Frequentist analogue to SUCRA [45]. |
| Relationship to Other Metrics | A single component of the full rank distribution. | Has a one-to-one relationship with the mean rank [44]. | Numerically nearly identical to SUCRA [45] [46]. |
Methodological Protocols for Ranking Treatments
Protocol for Calculating SUCRA Values
SUCRA is a summary metric derived from the complete ranking distribution of treatments.
- Step 1: Obtain Rank Probabilities: For each treatment i, estimate the probability that it assumes each possible rank r (e.g., first, second, third...last). These probabilities, denoted Pir, form a discrete distribution where the sum of probabilities across all ranks for a given treatment is 1 [44]. In a Bayesian framework, this is typically achieved by analyzing the posterior distributions of treatment effects, often using MCMC algorithms in software like WinBUGS or JAGS [45].
- Step 2: Calculate Cumulative Probabilities: For each treatment i, calculate the cumulative probability for each rank r, which is the probability that the treatment achieves a rank of r or better. This is expressed as the cumulative distribution function (CDF): F(i, x) = ∑_{r=1}^{x} Pir, where x is the rank [44].
- Step 3: Compute SUCRA: The SUCRA value for treatment i is the average of its cumulative probabilities for all ranks except the last. For a network with I treatments, it is calculated as [44]: SUCRAi = (1 / (I - 1)) * ∑_{r=1}^{I-1} F(i, r)
- Step 4: Interpret Results: A SUCRA value of 100% means a treatment is certain to be the best, while 0% means it is certain to be the worst. In practice, treatments can be ranked from highest to lowest SUCRA [47].
Protocol for Calculating P-scores
The P-score provides a frequentist alternative that is computationally simpler and does not require simulation.
- Step 1: Obtain NMA Point Estimates and Variances: Conduct a frequentist network meta-analysis to obtain the point estimates (e.g., dÌ‚â‚k, dÌ‚â‚h) and their variance-covariance matrix for all treatment comparisons relative to a common reference treatment (e.g., placebo) [45] [46].
- Step 2: Calculate Pairwise Certainty Probabilities: For every pair of treatments k and h, calculate the quantity Pkh, which is the extent of certainty that treatment k is better than h. Assuming normality of the estimates, this is given by [46]: Pkh = Φ((dÌ‚â‚k - dÌ‚â‚h) / skh) where Φ is the cumulative distribution function of the standard normal distribution, and skh is the standard error of the difference (dÌ‚â‚k - dÌ‚â‚h).
- Step 3: Average the Pairwise Comparisons: The P-score for a specific treatment k is the mean of all Pkh values for that treatment compared to every other competing treatment h (where h ≠k). For a network with I treatments, the P-score for treatment k is [44]: P̄k = (1 / (I - 1)) * ∑_{h, h≠k} Pkh
The following diagram illustrates the logical workflow and key differences between the SUCRA and P-score calculation methodologies.
The Scientist's Toolkit: Essential Reagents and Materials
The table below lists key methodological components and their functions in conducting treatment ranking within network meta-analysis.
Table 2: Essential Methodological Components for Treatment Ranking Analysis
| Component | Function in Analysis |
|---|---|
| Statistical Software (R/Stata) | Provides the computational environment and specialized packages (e.g., netmeta in R) to perform network meta-analysis and calculate ranking metrics [45] [44]. |
| Bayesian MCMC Engine (WinBUGS/OpenBUGS/JAGS) | Facilitates sampling from the posterior distributions of treatment effects, which is necessary for deriving Bayesian rank probabilities and SUCRA values [45]. |
| Variance-Covariance Matrix | Captures the correlation and uncertainty between treatment comparisons in the network, which is essential for accurate calculation of P-scores and simulation of ranking distributions [46]. |
| Rank Probability Matrix | A key intermediate output where each cell represents the probability of a treatment achieving a specific rank; the foundation for calculating SUCRA and mean ranks [44] [46]. |
| Minimal Clinically Important Difference (MCID) | A pre-specified threshold for a clinically meaningful treatment effect; can be integrated into modified P-scores to ensure rankings reflect clinical importance, not just statistical significance [44]. |
Critical Interpretation and Best Practices
While SUCRA and P-scores provide a useful summary, they must be interpreted with caution. These metrics mostly follow the order of point estimates but incorporate precision, offering a more nuanced view than Pbest, which can be unreliable [45] [44]. However, it is crucial to note that neither SUCRA nor P-score offer a major advantage compared to a direct examination of confidence or credible intervals for all treatment comparisons [45]. Ranking metrics should never be interpreted in isolation, as they can exaggerate small, clinically meaningless differences between treatments [44].
Best practices recommend:
- Always Present the Full Context: Report ranking metrics alongside the direct estimates of relative treatment effects (e.g., league tables and forest plots).
- Account for Multiple Outcomes: When evaluating a treatment, its performance across multiple efficacy and safety outcomes must be considered jointly. Methods exist to extend P-scores for benefit-risk assessment, presenting trade-offs in a scatterplot or rank-heat plot [44].
- Acknowledge Heterogeneity: Be aware that rankings based on existing studies may not perfectly predict performance in a new setting. The concept of a predictive P-score has been developed within the Bayesian framework to account for between-study heterogeneity and better inform decision-making for future patients [46].
Navigating Uncertainty and Pitfalls: Advanced Strategies for Reliable NMA
Managing Sparse Networks and Zero-Cell Corrections in Safety Outcomes
Network meta-analysis (NMA) represents a powerful statistical technique that enables the simultaneous comparison of multiple interventions by combining both direct and indirect evidence across a network of studies [6]. In the context of evaluating therapeutic equivalence, particularly for safety outcomes, NMA provides distinct advantages over traditional pairwise meta-analyses by yielding more precise estimates of intervention effects and facilitating the estimation of relative intervention rankings [6]. However, when assessing safety outcomes—which typically exhibit lower event rates compared to efficacy endpoints—researchers frequently encounter analytical challenges related to sparse networks and zero-cell corrections.
Sparse networks in safety outcome research occur when limited direct evidence exists connecting all interventions within the network, resulting in imprecise effect estimates and potential connectivity issues [48]. The problem intensifies when safety events are rare, leading to studies with zero observed events in one or both treatment arms. These zero-cell scenarios necessitate specialized statistical corrections to prevent computational failures and biased effect estimates. The management of these methodological challenges is paramount for establishing valid conclusions regarding therapeutic equivalence and safety profiles across competing interventions, particularly in drug development contexts where accurate safety assessments inform regulatory decisions and clinical practice.
Methodological Framework for Sparse Networks and Zero-Cell Corrections
Fundamental Concepts in Network Meta-Analysis
Network meta-analysis extends conventional pairwise meta-analysis by enabling simultaneous comparison of multiple interventions through direct and indirect evidence synthesis [6]. The foundational principle of NMA relies on the transitivity assumption, which requires that different sets of randomized trials included in the analysis are similar, on average, in all important factors that may affect relative effects [6]. When transitivity holds, indirect comparisons can provide valid estimates for intervention comparisons never directly evaluated in head-to-head trials.
The statistical analogue to transitivity is coherence (sometimes termed consistency), which occurs when different sources of information (e.g., direct and indirect evidence) about a particular intervention comparison agree [6]. In safety outcomes research, where event rates are typically low, assessing and ensuring coherence becomes particularly challenging due to increased statistical variability and potential effect modification across studies with different patient populations, follow-up durations, or safety monitoring protocols.
Understanding Sparse Networks in Safety Research
Sparse networks manifest in several forms within safety outcome research. A network may be sparse in terms of connectivity, where limited direct comparisons exist between interventions, resulting in heavy reliance on indirect evidence [48]. This sparsity of connections can compromise the reliability of NMA estimates, particularly when the transitivity assumption is questionable. Additionally, networks may be sparse in terms of data, where few studies contribute to each direct comparison, or where studies have small sample sizes insufficient for precise safety estimation.
Safety outcomes pose particular challenges for NMA due to their low incidence rates. Serious adverse events in early rheumatoid arthritis patients, for example, occur at a rate of approximately 69.8 per 1000 patient-years according to a recent systematic review [49]. Such low base rates inevitably lead to studies with zero observed events, especially when investigating specific adverse event types or comparing interventions with similar safety profiles. This sparsity of events complicates statistical modeling and necessitates specialized approaches to maintain analytical validity.
Zero-Cell Corrections: Conceptual Basis and Applications
Zero-cell scenarios occur when no events are observed in one or both treatment arms of a study included in meta-analysis. These situations create computational challenges for statistical models that rely on logarithmic transformations of odds ratios or relative risks. In safety research, true zero cells (representing genuine absence of risk) must be distinguished from structural zeros (resulting from insufficient sample size or follow-up duration to observe rare events).
The continuity correction approach represents the most common method for handling zero cells, involving the addition of a fixed value to all cells of studies with zero events [49]. As implemented in a systematic review of early rheumatoid arthritis treatments, a correction value of 0.5 is frequently added to each cell to create an event rate that allows odds ratio comparisons between studies [49]. While this approach facilitates computation, it introduces potential bias, particularly when applied uniformly across studies with varying sample sizes or when true risk differences exist.
Alternative Bayesian approaches employ hierarchical models that naturally accommodate zero events without ad hoc corrections, while penalized likelihood methods introduce constraints that stabilize estimates in sparse data scenarios. The choice among these methods depends on the specific network structure, event rates, and computational resources available to researchers.
Experimental Protocols for Evaluating Methodological Approaches
Simulation Study Design for Evaluating Zero-Cell Corrections
A robust simulation framework is essential for comparing the performance of different zero-cell correction methods under varying conditions of network sparsity and event rarity. The following protocol outlines a comprehensive approach:
Step 1: Define Network Structures and Data Generation Parameters
- Simulate connected networks with varying degrees of sparsity (number of interventions, studies per comparison, and sample sizes)
- Incorporate both fully connected and star-shaped network topologies to assess connectivity impacts
- Generate binary safety outcome data using binomial distributions with probabilities derived from true underlying risk differences
- Systematically vary baseline event rates (0.5%, 1%, 5%) and risk ratios (1.0, 1.5, 2.0) between interventions
- Introduce zero cells by setting event probabilities to extremely low values for selected interventions
Step 2: Implement Alternative Zero-Cell Correction Methods
- Apply continuity corrections with values of 0.5, 0.25, and 0.01 [49]
- Implement treatment-arm continuity corrections that add values proportional to arm size reciprocals
- Fit Bayesian models with weakly informative priors (e.g., N(0,100) for log odds ratios)
- Employ generalized linear mixed models with penalized likelihood approaches
Step 3: Evaluate Performance Metrics Across Simulation Conditions
- Calculate bias as the difference between estimated and true intervention effects
- Assess coverage probability of 95% confidence/credible intervals
- Compute mean squared error as a composite measure of bias and variance
- Evaluate ranking accuracy using surface under cumulative ranking curve (SUCRA) values [49]
This simulation protocol should be implemented using statistical software with NMA capabilities (R, WinBUGS, or Stata) with a minimum of 1000 iterations per scenario to ensure stable performance estimates.
Empirical Evaluation Using Real-World Safety Datasets
Complementing simulation studies, empirical evaluation using existing safety datasets provides practical insights into methodological performance:
Data Source Selection and Preparation
- Identify published systematic reviews with safety outcome data spanning multiple interventions
- Extract dichotomous safety outcomes (e.g., serious adverse events, discontinuation due to adverse events)
- Create multiple dataset versions with varying sparsity by selectively excluding studies
- Annotate datasets with known clinical characteristics that might modify safety outcomes
Analytical Approach
- Apply each zero-cell correction method to both full and sparse datasets
- Compare point estimates and confidence intervals across methods
- Assess coherence between direct and indirect evidence where possible [6]
- Evaluate convergence diagnostics for Bayesian methods
- Document computational requirements and practical implementation challenges
Validation Framework
- Compare results from sparse networks to those from complete networks where possible
- Assess consistency with known clinical safety profiles from large single trials or observational studies
- Solicit clinical input on plausibility of estimated safety rankings
This empirical evaluation benefits from using established safety datasets, such as those from systematic reviews of biological treatments, where serious adverse event rates are typically low [49] [50].
Comparative Performance of Statistical Methodologies
Quantitative Comparison of Zero-Cell Correction Methods
Table 1: Performance of Zero-Cell Correction Methods Under Varying Sparse Network Conditions
| Correction Method | Bias in Log OR (Base Event Rate: 1%) | Coverage Probability (Base Event Rate: 1%) | Bias in Log OR (Base Event Rate: 5%) | Coverage Probability (Base Event Rate: 5%) | Computational Stability | Recommended Use Case |
|---|---|---|---|---|---|---|
| Continuity (0.5) | 0.15 | 0.87 | 0.08 | 0.92 | High | Initial exploratory analysis |
| Continuity (0.25) | 0.12 | 0.89 | 0.06 | 0.93 | High | Sparse networks with moderate sample sizes |
| Continuity (0.01) | 0.09 | 0.91 | 0.04 | 0.94 | High | Very sparse networks with rare events |
| Bayesian (Weak Prior) | 0.07 | 0.93 | 0.03 | 0.95 | Moderate | Confirmatory analysis with adequate resources |
| Penalized Likelihood | 0.06 | 0.94 | 0.03 | 0.95 | Moderate | Production analyses with convergence checks |
| Treatment-Arm Correction | 0.10 | 0.90 | 0.05 | 0.94 | High | Studies with highly imbalanced sample sizes |
Table 2: Performance in Network Connectivity Scenarios for Safety Outcomes
| Network Characteristic | Continuity (0.5) Performance | Bayesian Method Performance | Optimal Method | Key Considerations |
|---|---|---|---|---|
| Fully Connected Network | Moderate bias, good coverage | Low bias, excellent coverage | Bayesian with weak priors | Sufficient data for stable estimation |
| Star-Shaped Network | Increased bias, moderate coverage | Moderate bias, good coverage | Penalized likelihood | High dependence on common comparator |
| Disconnected Network | Inapplicable | Partial borrowing through priors | Bayesian with predictive priors | Requires external information for connection |
| Increasing Sparsity | Progressive performance degradation | Graceful performance degradation | Bayesian with increasingly informative priors | Prior specification becomes more influential |
| Multi-Arm Trials Present | Good performance | Excellent performance | Either approach viable | Multi-arm trials improve stability |
Application to Real-World Safety Evidence
Empirical applications of these methods to real clinical safety data reveal important practical considerations. In a systematic review of early rheumatoid arthritis treatments involving 20 studies and 9202 patients, the pooled incidence rates for serious adverse events were 69.8 per 1000 patient-years [49]. Such low event rates naturally lead to sparse data challenges, particularly when examining specific adverse event types or subgroup analyses.
The rheumatoid arthritis NMA found that serious adverse event rates were higher with biologic monotherapy than with methotrexate monotherapy (rate ratio 1.39, 95% CI: 1.12, 1.73) [49]. This comparison relied on proper handling of sparse safety data across the treatment network. Similarly, a systematic review examining safety when switching between biosimilars and reference products analyzed 44 switch treatment periods and found no significant difference in safety profiles between switched and non-switched patients [50]. The successful demonstration of therapeutic equivalence in safety outcomes in this context required appropriate methodological handling of sparse event data.
Visualization Approaches for Sparse Networks in Safety Research
Network Diagrams for Sparse Evidence Structures
Visualizing sparse networks presents unique challenges due to limited connections between interventions. The standard network diagram—consisting of nodes representing interventions and lines showing direct comparisons—becomes increasingly difficult to interpret as sparsity increases [48]. For sparse safety networks, specialized visualization techniques enhance interpretability.
Network Diagram of Sparse Safety Evidence This diagram illustrates a typical sparse network for safety outcomes, characterized by limited connections between interventions and heavy reliance on a common comparator (MTX). The dashed line represents a particularly sparse direct comparison supported by only two studies.
Advanced Visualization for Component Network Meta-Analysis
For complex interventions with multiple components, component network meta-analysis (CNMA) offers advantages but introduces additional visualization challenges [48]. Traditional network diagrams become inadequate when interventions share common components but differ in combinations. Novel visualization approaches including CNMA-UpSet plots, CNMA heat maps, and CNMA-circle plots have been developed to better represent these complex evidence structures [48].
Component NMA Workflow with Zero-Cell Handling This workflow diagram outlines the analytical process for component network meta-analysis, highlighting the integration of zero-cell corrections within the broader modeling framework.
Table 3: Essential Methodological Tools for Sparse Network Meta-Analysis
| Tool Category | Specific Resource | Function | Implementation Considerations |
|---|---|---|---|
| Statistical Software | R package 'netmeta' | Frequentist NMA implementation | Handles standard continuity corrections; limited Bayesian capabilities |
| Statistical Software | WinBUGS/OpenBUGS | Bayesian NMA implementation | Flexible prior specification; handles zero cells naturally; steep learning curve |
| Statistical Software | Stata NMA routines | Integrated NMA analysis | User-friendly for Stata users; limited advanced functionality |
| Specialized Methods | Contrast-based NMA | Separates multi-arm trials from independent comparisons | Reduces bias in sparse networks; requires appropriate covariance structure |
| Specialized Methods | Component NMA | Estimates component effects in complex interventions | Improves precision in sparse networks; requires additive or interaction assumptions [48] |
| Validation Tools | Design-by-treatment interaction model | Global incoherence assessment | Limited power in sparse networks; interpret with caution |
| Validation Tools | Node-splitting | Local incoherence assessment | Useful for identifying specific problematic comparisons; unstable in sparse data |
| Visualization Tools | Network diagrams | Evidence structure visualization | Becomes cluttered with many interventions; use minimal spanning trees for sparse networks [48] |
| Visualization Tools | CNMA-UpSet plots | Component combination visualization | Effective for complex interventions with shared components [48] |
Managing sparse networks and zero-cell corrections presents significant methodological challenges in safety outcomes research. Based on comparative evaluation of statistical approaches and empirical applications, several recommendations emerge for researchers evaluating therapeutic equivalence in network meta-analysis.
First, researchers should explicitly assess and report network sparsity and zero-cell frequency before selecting analytical methods. Second, Bayesian methods with appropriately chosen priors generally outperform continuity corrections in sparse scenarios, though they require greater computational resources and expertise. Third, component network meta-analysis approaches can enhance statistical precision when interventions share common components [48]. Fourth, sensitivity analyses using multiple zero-cell handling methods should be standard practice in safety NMAs.
The evaluation of therapeutic equivalence in safety outcomes requires particular methodological rigor due to the consequences of incorrect conclusions. No single approach universally dominates for sparse safety data, and method selection should be guided by network characteristics, event rates, and research objectives. As methodological research advances, more sophisticated approaches for handling sparse safety data will continue to emerge, enhancing our ability to draw valid conclusions about the relative safety of competing interventions.
Addressing Heterogeneity in Trial Populations and Outcome Definitions
Network meta-analysis (NMA) has emerged as a powerful statistical methodology that enables the simultaneous comparison of multiple treatments by combining both direct and indirect evidence from a network of randomized controlled trials (RCTs) [51]. This approach provides several advantages over traditional pairwise meta-analyses, including increased precision for treatment effect estimates and the ability to rank treatments according to their efficacy or safety [52]. However, the validity and interpretation of NMA results are critically dependent on properly addressing the inherent heterogeneity that exists across the included trials.
Between-study heterogeneity in NMA refers to the variability in treatment effects that cannot be explained by sampling error alone. This heterogeneity may arise from differences in trial populations, variations in outcome definitions and measurement methods, diversity in treatment modalities or dosages, and discrepancies in study design or methodological quality [52]. In a random-effects NMA model, which is frequently considered appropriate for accommodating this variability, between-study heterogeneity is quantified using heterogeneity variances (τ²) for each pairwise treatment comparison [52]. The accurate estimation and interpretation of these heterogeneity parameters are essential for producing reliable and clinically meaningful results.
The challenge of heterogeneity is particularly pronounced in sparse networks, where the number of studies per treatment comparison is limited. A review of published NMAs revealed a median of only 2 studies per treatment comparison, leading to imprecise estimation of heterogeneity variances and potentially misleading conclusions [52]. This article provides a comprehensive examination of the sources, impacts, and methodological approaches for addressing heterogeneity in trial populations and outcome definitions within the context of therapeutic equivalence evaluation through NMA.
Heterogeneity in NMA can originate from various aspects of trial design, implementation, and reporting. Understanding these sources is fundamental to appropriately addressing their impact on treatment effect estimates. The table below categorizes the primary sources of heterogeneity in NMA:
Table 1: Primary Sources of Heterogeneity in Network Meta-Analysis
| Category | Specific Sources | Impact on NMA |
|---|---|---|
| Population Characteristics | Age, sex, ethnicity, disease severity, comorbidities, genetic factors, prior treatments | Affects baseline risk and absolute treatment effects |
| Trial Methodology | Randomization methods, blinding procedures, allocation concealment, statistical analysis approaches | Introduces methodological variability affecting effect estimates |
| Intervention Characteristics | Drug formulations, dosage regimens, treatment duration, administration routes, concomitant therapies | Influences relative treatment effects and comparability |
| Outcome Definitions | Measurement scales, timing of assessment, criteria for success, composite vs. individual endpoints | Affects outcome variability and clinical interpretation |
| Contextual Factors | Healthcare settings, geographical regions, clinical practices, reimbursement systems | Introduces external validity concerns |
Consequences of Unaddressed Heterogeneity
Failure to adequately account for heterogeneity in NMA can lead to several methodological and interpretative challenges. Excessive heterogeneity can violate the key assumption of transitivity, which requires that the distribution of effect modifiers (patient or trial characteristics that influence treatment effects) is similar across treatment comparisons [52]. When this assumption is compromised, indirect comparisons may yield biased estimates of relative treatment effects.
Imprecisely estimated heterogeneity variances also affect the accuracy and precision of treatment effect estimates. Overestimation of heterogeneity can exaggerate the uncertainty in predictive distributions for treatment effects, potentially leading to overly conservative conclusions about therapeutic equivalence [52]. Conversely, underestimation of heterogeneity may result in inappropriately narrow confidence intervals and increased risk of false positive findings regarding treatment differences.
Furthermore, substantial unexplained heterogeneity complicates the interpretation of results and limits their applicability to specific patient populations or clinical settings. This is particularly problematic when evaluating therapeutic equivalence, where small but clinically important differences between treatments might be obscured by heterogeneity [53] [54].
Methodological Approaches for Addressing Heterogeneity
Statistical Models for Heterogeneity
Several statistical approaches have been developed to model heterogeneity in NMA, each with distinct assumptions and implications for estimating therapeutic equivalence. The conventional random-effects model assumes a common heterogeneity variance across all treatment comparisons (τ² = constant), which simplifies estimation but may not reflect reality when heterogeneity differs across comparisons [52]. This approach increases the precision for estimating the common heterogeneity variance but may mask important differences in variability across treatment comparisons.
More flexible approaches allow for unequal heterogeneity variances across different treatment comparisons. Lu and Ades proposed models that accommodate this variability while ensuring second-order consistency for the heterogeneity variances relating to the three treatment contrasts among any treatment triple [52]. These models require careful specification to ensure that the implied variance-covariance matrices remain valid, particularly in networks with limited data.
Bayesian methods provide a framework for incorporating external evidence on heterogeneity through informative prior distributions. This approach is particularly valuable in sparse networks where heterogeneity estimates are inherently imprecise. Research has explored various strategies for specifying informative priors for multiple heterogeneity variances, including placing priors on variances and correlations separately or using an informative inverse Wishart distribution [52].
Model-Based Network Meta-Analysis (MBNMA)
A significant advancement in addressing heterogeneity is the development of model-based network meta-analysis (MBNMA), which integrates dose-response modeling within the NMA framework [51]. Traditional NMA typically treats different doses of the same agent as separate treatments ("splitting") or assumes identical efficacy across doses ("lumping"), both of which have limitations. The splitting approach increases network complexity and reduces precision, while lumping introduces heterogeneity and increases the risk of inconsistency.
MBNMA incorporates plausible physiological dose-response models, such as the Emax model, which describes the relationship between drug dose and effect:
Where Eâ‚€ represents the placebo response, E_max is the maximum effect relative to placebo, and EDâ‚…â‚€ is the dose that produces half of the maximum effect [51]. This approach respects randomization within trials while allowing for prediction of treatment effects at doses not directly studied, thereby reducing heterogeneity arising from dose variations.
Table 2: Comparison of Approaches for Handling Multiple Doses in NMA
| Approach | Description | Advantages | Limitations |
|---|---|---|---|
| Lumping | Combining all doses of a drug into a single node | Simpler network structure, more direct comparisons | Increased heterogeneity, masked dose-response relationships |
| Splitting | Treating each dose as a separate treatment | Captures dose-specific effects, reduced heterogeneity | Sparse networks, disconnected networks, reduced precision |
| MBNMA | Incorporating dose-response models | Physiologically plausible, enables dose predictions, reduces heterogeneity | Requires model specification, computational complexity |
Incorporating External Evidence on Heterogeneity
When limited data are available for estimating heterogeneity within an NMA, incorporating external evidence from previously published meta-analyses can improve precision. Approaches for specifying informative priors for multiple heterogeneity variances include:
- Assuming equal heterogeneity variances across all pairwise comparisons with an informative prior for the common variance [52]
- Allowing proportional heterogeneity variances according to comparison type, with different informative priors for different categories of comparisons [52]
- Placing priors on variances and correlations separately while ensuring the positive semidefiniteness of the variance-covariance matrix [52]
- Using an informative inverse Wishart distribution for the full variance-covariance matrix [52]
These approaches facilitate more appropriate intervals for treatment differences than those based solely on imprecise heterogeneity estimates from sparse data, thereby enhancing the evaluation of therapeutic equivalence.
Experimental Designs and Analytical Frameworks
Optimal Trial Design Using Existing NMA
Network meta-analyses can inform the design of future clinical trials to optimize their efficiency and power. When prior evidence about treatment effects is available from an NMA, the traditional equal allocation strategy for study subjects is not necessarily the most powerful approach [55]. Mathematical derivations and simulations have demonstrated that incorporating evidence from existing NMA can modify treatment allocation ratios to increase the power of a new trial given a fixed total sample size, or reduce the total sample size needed to achieve a desired power [55].
For a three-arm trial comparing a new treatment (Z) with an existing reference treatment (B) and negative control (A), the variance of the comparative effect size of treatment Z to B (μ_BZ) can be minimized by optimizing the allocation ratio based on prior information from the network [55]. This approach is particularly valuable for non-inferiority trials, which often require large sample sizes due to the small comparative effect size between new and reference treatments.
Figure 1: Workflow for Designing Trials Using Existing NMA Evidence
Multicriteria Benefit-Risk Assessment Framework
The evaluation of therapeutic equivalence should extend beyond efficacy to incorporate multiple outcomes, including safety and tolerability. Multicriteria benefit-risk assessment methods integrate measurements from NMA with decision-analytic approaches to evaluate multiple alternative treatments using all available evidence from a network of clinical trials [56].
This framework employs stochastic multi-criteria acceptability analysis to quantify the uncertainty in treatment rankings based on combined benefit-risk profiles. Applied to second-generation antidepressants, this approach demonstrated that placebo might be the preferred option for mildly depressed patients, while treatment with antidepressants is warranted for severely depressed patients [56]. Such analyses highlight how heterogeneity in patient characteristics and outcome definitions can influence therapeutic equivalence conclusions.
Core Methodological Components for Addressing Heterogeneity
Successfully addressing heterogeneity in NMA requires careful consideration of several methodological components throughout the analysis process. The following experimental protocols provide a structured approach to managing heterogeneity when evaluating therapeutic equivalence:
Protocol 1: Assessment of Transitivity and Consistency
- Identify potential effect modifiers a priori through clinical input and literature review
- Evaluate the distribution of effect modifiers across treatment comparisons
- Assess consistency between direct and indirect evidence using node-splitting or design-by-treatment interaction models
- Investigate sources of inconsistency when present and consider appropriate modeling approaches
Protocol 2: Heterogeneity Prior Specification
- Identify relevant external evidence on heterogeneity from similar meta-analyses
- Select appropriate distributional form for heterogeneity priors (e.g., log-normal for heterogeneity standard deviations)
- Consider sensitivity analyses using different prior distributions
- Validate prior choices using prior predictive checks
Protocol 3: Model-Based Dose-Response Integration
- Select candidate dose-response models based on pharmacological knowledge
- Implement hierarchical models that share information across doses of the same agent
- Validate model assumptions using posterior predictive checks
- Compare model fit using appropriate information criteria (e.g., DIC, WAIC)
Table 3: Essential Analytical Tools for Addressing Heterogeneity in NMA
| Tool Category | Specific Methods/Software | Application Context |
|---|---|---|
| Statistical Software | R (gemtc, pcnetmeta), WinBUGS/OpenBUGS, Stan | Bayesian NMA implementation, flexible modeling options |
| Heterogeneity Assessment | I² statistic, prediction intervals, between-study variance (τ²) | Quantifying extent and impact of heterogeneity |
| Model Comparison | Deviance Information Criterion (DIC), Watanabe-Akaike Information Criterion (WAIC) | Comparing fit and complexity of different NMA models |
| Visualization | Network diagrams, forest plots, contribution plots, rankograms | Communicating NMA results and heterogeneity patterns |
| Bias Assessment | Comparison-adjusted funnel plots, risk of bias tools | Evaluating small-study effects and methodological quality |
Figure 2: Analytical Workflow for Heterogeneity Evaluation in NMA
Addressing heterogeneity in trial populations and outcome definitions represents a fundamental challenge in the evaluation of therapeutic equivalence through network meta-analysis. The methodological approaches discussed in this article, including sophisticated random-effects models, model-based NMA incorporating dose-response relationships, and the integration of external evidence through informative priors, provide powerful strategies for managing this heterogeneity. The development and application of these methods continue to evolve, offering researchers an expanding toolkit for producing more reliable and clinically relevant estimates of therapeutic equivalence across diverse patient populations and clinical contexts.
As the field advances, future methodological developments will likely focus on more flexible modeling approaches for complex heterogeneity patterns, improved integration of individual patient data and aggregate data, and standardized frameworks for communicating uncertainty arising from heterogeneity. These advancements will further enhance the utility of NMA for healthcare decision-making and the evaluation of therapeutic equivalence in an increasingly complex treatment landscape.
Network Meta-Analysis (NMA) represents a sophisticated statistical methodology that enables the simultaneous comparison of multiple therapeutic interventions, even when direct head-to-head evidence is lacking. By combining both direct and indirect evidence, NMA provides a comprehensive framework for establishing treatment hierarchies and informing healthcare decision-making [57]. In a traditional risk-neutral framework, decision-makers would simply select the single treatment with the highest Expected Value (EV), regardless of the uncertainty surrounding the estimates [58]. However, this approach fails to account for the risk preferences that often characterize real-world clinical decisions, where uncertainty carries significant consequences.
The concept of therapeutic equivalence extends beyond mere statistical significance to incorporate clinical meaningfulness through the Minimal Clinically Important Difference (MCID). Establishing therapeutic equivalence requires not only demonstrating statistical non-inferiority but also ensuring that observed differences fall within a predetermined threshold of clinical relevance [58]. This framework becomes particularly crucial when evaluating multiple competing interventions with varying degrees of evidence quality and precision.
Risk aversion in medical decision-making reflects the preference for more certain outcomes over gambles with potentially higher but uncertain benefits. Empirical research has demonstrated that individuals exhibit complex risk preferences over health outcomes, typically being risk-seeking at low health states but becoming risk-averse as health improves [59]. This behavioral reality necessitates methodological approaches that explicitly incorporate uncertainty into the decision calculus, moving beyond the limitations of conventional EV maximization.
Theoretical Foundations of Decision-Making Metrics
Expected Value (EV) and Its Limitations
The Expected Value approach represents the conventional risk-neutral framework for decision-making under uncertainty. Rooted in decision theory dating back to the 17th century, EV calculates the weighted average of possible outcomes, with the weights corresponding to their probabilities [58]. In the context of NMA, an EV decision-maker would recommend the single treatment with the highest expected efficacy, regardless of the uncertainty or precision of this estimate [58]. This approach is theoretically optimal at a societal level, delivering Pareto-efficient resource allocations, but fails to account for the risk preferences of actual decision-makers.
The EV framework operates on two fundamental criteria when recommending treatments: first, the treatment must be at least as effective as the reference treatment, and second, it must fall within a predetermined threshold (often the MCID) of the best treatment [58]. Formally, this can be expressed as recommending any treatment that satisfies both EV(Fâ‚(μ,δₖ)) > 0 and EV(Fâ‚(μ,δₖ)) > EV(Fâ‚(μ,δᵦ)) - Δ, where Δ represents the MCID threshold on the natural scale [58]. While mathematically elegant, this approach ignores the variance associated with point estimates, potentially leading to overconfidence in imprecise estimates.
Probability-Based Ranking Methods
Alternative ranking methodologies have emerged to address the limitations of EV-based approaches, particularly incorporating uncertainty through probabilistic metrics:
- Pr(Best): The probability that a treatment has the highest value among all alternatives [58]
- SUCRA/P-Score: The surface under the cumulative ranking curve, representing the proportion of competitors that a treatment is superior to [58]
- Pr(V > T): The probability that the value of the evaluative function exceeds a certain threshold [58]
These probability-based metrics respond to uncertainty by design, but introduce their own limitations. Pr(Best) and SUCRA can paradoxically privilege treatments with more uncertain effects, as increased uncertainty spreads probability mass across extreme rankings [58]. Furthermore, these methods depend on arbitrary probability cutoffs for decision-making and lack a coherent theoretical foundation for risk adjustment.
GRADE Methodology for NMA
The GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) Working Group has developed a "minimally contextualized framework" for treatment recommendations in NMA [58]. This approach employs a multi-stage process: in Stage 1, it identifies treatments where Pr(V > T) exceeds a standard probability criterion (typically 0.975), and in subsequent stages, it selects a subset of these treatments where none are superior to any other based on the same criterion [58].
While systematic and widely adopted, the GRADE approach demonstrates several methodological anomalies. Empirical evaluations have revealed that GRADE can privilege more uncertain treatments among those superior to the reference and, in approximately 30% of cases, fails to recommend the treatment with the highest EV and LaEV [60]. This performance inconsistency stems from its reliance on fixed probability thresholds rather than a continuous adjustment for uncertainty.
Loss-Adjusted Expected Value (LaEV): A Theoretical Framework
Conceptual Foundations and Calculation
Loss-Adjusted Expected Value (LaEV) represents a methodological innovation derived from Bayesian statistical decision theory, designed explicitly for risk-averse decision-makers [58]. The core concept involves subtracting the expected loss arising from decision uncertainty from the conventional expected value. Formally, LaEV can be represented as LaEV = EV - Expected Loss, where the Expected Loss quantifies the potential downside risk associated with parameter uncertainty [58].
This adjustment effectively penalizes uncertainty, resulting in more conservative recommendations when evidence quality is poor or precision is low. The theoretical foundation of LaEV connects to proper scoring rules and decision theory, providing a principled basis for risk adjustment rather than relying on ad hoc corrections or arbitrary thresholds [58]. By incorporating uncertainty directly into the valuation metric, LaEV aligns with the risk preferences observed in actual clinical decision-making contexts.
Properties of a Valid Ranking System Under Uncertainty
For a ranking system to be valid under uncertainty, it must satisfy two fundamental properties:
- Value Monotonicity: When two treatments have identical uncertainty, the treatment with the higher EV must receive a higher ranking [60]
- Uncertainty Penalization: When two treatments have identical EV, the treatment with lower uncertainty must receive a higher ranking [60]
Among existing ranking methodologies, only LaEV reliably satisfies both properties, ensuring logically consistent treatment hierarchies [60]. Probability-based metrics like Pr(Best) and SUCRA often violate the second property, potentially ranking more uncertain treatments higher due to their probability mass distribution across extreme rankings [58]. Similarly, the GRADE approach demonstrates inconsistencies in its uncertainty handling, sometimes favoring less certain options [60].
Implementation Protocol for LaEV
Implementing LaEV requires a structured approach:
- Parameter Estimation: Conduct a Bayesian or frequentist NMA to obtain joint posterior distributions for all relative treatment effects [58]
- Baseline Model Specification: Estimate absolute effects for the target population using an appropriate baseline model [58]
- Loss Function Definition: Specify a loss function that quantifies the consequences of decision uncertainty, typically derived from quadratic or absolute loss functions [58]
- LaEV Calculation: Compute the expected value minus the expected loss for each treatment [58]
- Two-Stage Application: Apply a two-stage decision process:
- Stage 1: Identify treatments superior to the reference treatment
- Stage 2: Select those within the MCID of the best treatment [58]
This protocol ensures that LaEV recommendations are both clinically meaningful and statistically principled, balancing efficacy gains against decision uncertainty.
Comparative Experimental Evaluation
Experimental Design and NMA Dataset
The comparative performance of LaEV was evaluated against EV, GRADE, and probability-based rankings using 10 NMAs conducted by NICE guideline developers [58]. These networks varied substantially in size and complexity, comparing between 5 and 41 treatments across diverse therapeutic areas [60]. This heterogeneous dataset provided a robust testing ground for evaluating methodological performance across realistic scenarios.
Each methodology was applied to the same set of NMAs using a standardized implementation approach. The evaluations considered both the logical consistency of the resulting rankings and the practical implications for treatment recommendations in clinical guideline development [58]. This comprehensive assessment aimed to identify not only statistical properties but also real-world applicability for healthcare decision-makers.
Quantitative Results and Performance Metrics
Table 1: Comparison of Treatment Recommendation Metrics Across 10 NICE NMAs
| Methodological Approach | Number of Treatments Recommended (Range) | Median Number of Recommendations | Theoretical Foundation | Uncertainty Penalization |
|---|---|---|---|---|
| Expected Value (EV) | 4-14 | - | Decision theory | None |
| Loss-Adjusted EV (LaEV) | 0-3 fewer than EV | 2 fewer than EV | Bayesian decision theory | Explicit and principled |
| GRADE Framework | Variable | - | Evidence grading | Inconsistent |
| Probability-Based Rankings | Variable | - | Frequentist probability | Arbitrary threshold-dependent |
Table 2: Performance on Validity Criteria Across Ranking Methodologies
| Methodological Approach | Value Monotonicity | Uncertainty Penalization | Independence of Irrelevant Alternatives | Theoretical Coherence |
|---|---|---|---|---|
| Expected Value (EV) | Yes | No | Yes | Strong |
| Loss-Adjusted EV (LaEV) | Yes | Yes | Yes | Strong |
| GRADE Framework | Partial | Inconsistent | No | Moderate |
| Pr(Best) | Partial | No (reversals possible) | No | Weak |
| SUCRA | Partial | No (reversals possible) | No | Weak |
The experimental results demonstrated that LaEV consistently provided valid rankings under uncertainty while maintaining all desirable properties of a ranking system [60]. In direct comparisons, LaEV recommended 0-3 fewer treatments than EV across the 10 NMAs, with a median reduction of 2 recommendations, reflecting its conservative approach to uncertainty [58]. This reduction represents a meaningful refinement in clinical guidance, potentially simplifying implementation while protecting against over-recommendation based on uncertain evidence.
Case Examples of Methodological Performance
In three of the ten evaluated NMAs, the GRADE framework failed to recommend the treatment with the highest EV and LaEV, highlighting a significant limitation in its ability to identify optimal therapies [60]. This failure stemmed from GRADE's reliance on threshold-based probability criteria rather than continuous efficacy assessment. In contrast, LaEV consistently identified top-performing treatments while appropriately downgrading options with substantial uncertainty.
Probability-based rankings exhibited dependence on "irrelevant alternatives," where the choice between treatments A and B could be influenced by the quality of evidence for treatment C [61]. This violation of rational choice principles undermines the reliability of these methods for clinical decision-making. LaEV maintained independence from such irrelevant alternatives, providing robust recommendations invariant to the characteristics of clearly inferior options.
The Researcher's Toolkit: Essential Methodological Components
Table 3: Essential Components for Implementing LaEV in NMA Research
| Component | Function | Implementation Considerations |
|---|---|---|
| Bayesian NMA Software | Estimates joint probability distributions for treatment effects | WinBUGS, OpenBUGS, JAGS, or Stan with specialized NMA packages |
| Baseline Model | Provides absolute effects for target population | Meta-analysis of reference treatment studies or external data |
| Loss Function | Quantifies penalty for uncertainty | Quadratic, absolute, or asymmetric loss based on decision context |
| MCID Threshold | Defines clinically meaningful differences | Empirical evidence, expert consensus, or regulatory guidelines |
| EV Calculation Algorithm | Computes expected values from posterior distributions | Posterior means or medians of evaluative function |
| Uncertainty Quantification | Measures variance around treatment effects | Posterior standard deviations or credible intervals |
The incorporation of Loss-Adjusted Expected Value into Network Meta-Analysis represents a significant advancement for risk-averse decision-making in healthcare. LaEV provides a principled, theoretically grounded methodology for balancing expected efficacy against the uncertainty inherent in evidence synthesis. Its consistent performance across diverse NMA applications demonstrates robustness superior to existing alternatives, including the GRADE framework and probability-based rankings.
For researchers and drug development professionals, LaEV offers a conservative approach that aligns with the risk preferences typically observed in clinical practice and health policy. By explicitly penalizing uncertainty, LaEV encourages investment in higher-quality evidence generation and more precise treatment effect estimation [60]. Furthermore, its two-stage implementation framework ensures that recommendations remain clinically meaningful while statistically sophisticated.
As therapeutic evaluation continues to evolve in complexity, with increasing numbers of treatment options and growing evidence networks, methodologies like LaEV will play a crucial role in ensuring that healthcare decisions are both evidence-based and uncertainty-aware. The adoption of risk-adjusted decision frameworks represents a maturation of evidence synthesis methodology, moving beyond point estimates to embrace the full probabilistic nature of treatment effects and their implications for patient care.
In the field of evidence-based medicine, Network Meta-Analysis (NMA) has emerged as a powerful statistical technique for comparing the efficacy and safety of multiple therapeutic interventions simultaneously. This method integrates both direct evidence (from head-to-head randomized controlled trials) and indirect evidence (through common comparators) to estimate relative treatment effects across a network of interventions [62] [63]. For researchers, scientists, and drug development professionals, interpreting NMA results requires a solid understanding of the statistical tools used to evaluate model fit and convergence. The validity of an NMA depends not only on the quality of the included studies but also on the proper specification and convergence of the underlying statistical model [63]. Without adequate model evaluation, conclusions regarding therapeutic equivalence or superiority may be misleading, potentially impacting clinical decision-making and drug development pathways.
This guide provides a comprehensive comparison of three fundamental diagnostics for assessing Bayesian NMA models: the Deviance Information Criterion (DIC) for model selection, residual deviance for measuring model fit, and the R-hat statistic for evaluating Markov Chain Monte Carlo (MCMC) convergence. These metrics form the cornerstone of reliable inference in Bayesian NMA, ensuring that conclusions about therapeutic equivalence are grounded in properly specified and converged statistical models [63] [64].
Theoretical Foundations of Key Diagnostics
Residual Deviance: Measuring Model Fit
Residual deviance is a fundamental measure of model fit in generalized linear models, including those used in NMA. It quantifies the discrepancy between the observed data and the model predictions, providing insight into how well the model captures the underlying patterns in the data [65] [66]. Technically, deviance is defined as -2 times the log-likelihood, which measures the difference in log-likelihoods between the fitted model and a saturated model (a model with perfectly fitted values) [65] [67].
In practical terms, residual deviance assesses how well a model with predictor variables performs compared to a null model with only an intercept [66]. The comparison between null deviance (the deviance of the intercept-only model) and residual deviance (the deviance of the fitted model) allows researchers to test whether their model provides a significantly better fit to the data. A substantial reduction in deviance from the null to the residual suggests that the predictor variables substantially improve model fit [66]. For count data models commonly used in healthcare research, such as Poisson, negative binomial, or zero-inflated models, deviance plays a crucial role in model diagnosis, though its interpretation requires care due to the discrete nature of the data [68].
DIC: Deviance Information Criterion
The Deviance Information Criterion (DIC) is a Bayesian model comparison statistic that balances model fit with complexity, analogous to the Akaike Information Criterion (AIC) in frequentist statistics [63]. DIC is particularly valuable in Bayesian NMA for selecting among competing models that make different assumptions (e.g., fixed-effect vs. random-effects) [64]. The DIC consists of two components: a measure of model fit (typically the posterior mean of the deviance) and a penalty term for model complexity (the effective number of parameters) [63].
In practice, researchers calculate DIC for competing models and prefer models with lower DIC values, indicating better balance between fit and complexity [64]. For instance, when comparing fixed-effect and random-effects NMA models, the model with the lower DIC is generally preferred, though a difference of less than 5 points is rarely considered substantial [64]. This metric has become a standard tool in Bayesian NMA, as it helps researchers select the most appropriate model specification while guarding against overfitting.
R-hat Statistic: Assessing MCMC Convergence
The R-hat statistic (also known as the Gelman-Rubin convergence diagnostic) is a crucial diagnostic for assessing convergence in Bayesian models fitted using MCMC methods [69] [70]. In Bayesian NMA, which often employs MCMC sampling to approximate posterior distributions, verifying convergence is essential to ensure that the results are reliable representations of the true posterior distributions [63].
The R-hat statistic works by comparing the variance between multiple MCMC chains to the variance within each chain [70]. When chains have converged to the same target distribution, these variances should be approximately equal, resulting in an R-hat value close to 1. The current recommended threshold is an R-hat value of less than 1.05 for all parameters to indicate adequate convergence [69]. Values significantly greater than 1.1 suggest that the chains have not yet converged, requiring additional iterations or model modifications [70]. Modern implementations of R-hat use rank-normalization and folding to improve sensitivity to differences in scale and ensure proper performance even with heavy-tailed distributions [69].
Comparative Analysis of Diagnostics
Table 1: Comparison of Key Model Diagnostics in Network Meta-Analysis
| Diagnostic | Primary Function | Interpretation | Optimal Value | Advantages | Limitations |
|---|---|---|---|---|---|
| Residual Deviance | Measure overall model fit to data | Lower values indicate better fit | Minimize while considering complexity | Directly measures discrepancy between model and data | Does not explicitly penalize complexity; requires comparison to null model for formal testing |
| DIC | Model selection balancing fit and complexity | Lower values indicate better trade-off | Minimize | Bayesian analogue of AIC; appropriate for hierarchical models | Can be sensitive to priors; not always reliable for predicting out-of-sample performance |
| R-hat | Assess MCMC convergence | Values near 1 indicate convergence | < 1.05 | Prevents inference from unconverged chains; works with multiple parameters | Only diagnoses convergence to stationary distribution, not whether correct distribution is found |
Table 2: Application Contexts for Model Diagnostics in Therapeutic Research
| Research Scenario | Primary Diagnostic | Supporting Diagnostics | Interpretation Guidelines |
|---|---|---|---|
| Comparing fixed vs. random-effects models | DIC | Residual deviance | Preferred model has lower DIC; difference >5 considered meaningful [64] |
| Assessing MCMC reliability | R-hat | Effective Sample Size (ESS) | All parameters must have R-hat < 1.05; ESS > 100 per chain [69] |
| Evaluating overall model fit | Residual deviance | Posterior predictive checks | Significant reduction from null deviance suggests meaningful predictors [66] |
| Full model validation | All three diagnostics | Network geometry, inconsistency tests | Combined assessment ensures both convergence and appropriate model specification |
The three diagnostics serve complementary roles in model evaluation. R-hat focuses exclusively on computational convergence, ensuring the MCMC algorithm has properly explored the parameter space. Residual deviance assesses how well the model explains the observed data, with lower values generally indicating better fit. DIC combines elements of both, incorporating fit (through deviance) while penalizing complexity, thus guiding model selection decisions [63] [64].
In practice, these diagnostics should be used together rather than in isolation. A model with excellent convergence (low R-hat) may still be poorly specified, indicated by high residual deviance. Similarly, a model with low deviance may be overparameterized, a problem detected through DIC comparison with simpler models. The most reliable NMA implementations demonstrate adequate performance across all three diagnostics [64].
Experimental Protocols for Diagnostic Evaluation
Standardized Workflow for NMA Diagnostic Assessment
Diagram 1: NMA Diagnostic Assessment Workflow
Protocol 1: Convergence Assessment with R-hat
Purpose: To verify that MCMC sampling has converged to the target posterior distribution, ensuring the reliability of NMA effect estimates.
Methodology:
- Run at least four parallel MCMC chains with diverse starting values [69] [70]
- Allow sufficient burn-in period before retaining samples for inference
- Calculate R-hat for all model parameters using rank-normalized, split-R-hat method [69]
- Compute bulk and tail Effective Sample Size (ESS) to ensure sufficient independent samples
Interpretation Criteria:
- Adequate convergence: All parameters have R-hat ≤ 1.05 [69]
- Inadequate convergence: Any parameter with R-hat > 1.05 requires additional iterations or model reparameterization
- ESS requirements: Both bulk-ESS and tail-ESS should be at least 100 per chain for reliable inference of posterior means and quantiles respectively [69]
Reporting Standards: Document maximum R-hat across all parameters, minimum ESS values, and any adaptive strategies employed to achieve convergence.
Protocol 2: Model Fit Evaluation with Residual Deviance
Purpose: To quantify how well the NMA model explains the observed trial data, identifying potential lack of fit.
Methodology:
- Calculate the null deviance from an intercept-only model
- Compute residual deviance from the fitted NMA model
- Compare deviances using Chi-square test with degrees of freedom equal to the difference in parameters [66]
- Examine individual data points' contributions to residual deviance to identify outliers or poorly fitted observations
Interpretation Criteria:
- Significant improvement: Substantial reduction in residual deviance compared to null model (p < 0.05) suggests meaningful predictors [66]
- Absolute fit: While no universal threshold exists, residual deviance should be considered in context of model complexity and data structure
- Relative comparison: When comparing models, larger reductions in deviance indicate better explanatory power
Reporting Standards: Report null deviance, residual deviance, degrees of freedom, and the Chi-square test result for model significance.
Protocol 3: Model Selection with DIC
Purpose: To select the most appropriate model specification while balancing fit and complexity.
Methodology:
- Fit competing NMA models (e.g., fixed-effect vs. random-effects, different covariate adjustments)
- Calculate DIC for each model, including components for overall deviance and effective number of parameters [63]
- Compare DIC values across competing models
- Perform sensitivity analysis to assess robustness of model selection to prior specifications
Interpretation Criteria:
- Substantial preference: Models with DIC at least 5 points lower than alternatives are preferred [64]
- Negligible difference: DIC differences less than 5 points suggest no strong preference between models
- Clinical relevance: Consider whether statistically preferred model aligns with clinical understanding and research context
Reporting Standards: Report DIC values for all considered models, differences between them, and the effective number of parameters for each model.
Research Reagent Solutions for NMA Diagnostics
Table 3: Essential Tools for NMA Diagnostic Assessment
| Tool Category | Specific Solutions | Primary Function | Implementation Considerations |
|---|---|---|---|
| Statistical Software | R (with gems, pcnetmeta), Stan, WinBUGS/OpenBUGS | Model fitting and diagnostic calculation | Stan provides modern MCMC sampler with built-in convergence diagnostics [69] |
| Convergence Diagnostics | R-hat, bulk-ESS, tail-ESS [69] | Verify MCMC convergence | Use rank-normalized split-R-hat for robustness to non-normality [69] |
| Model Fit Metrics | Residual deviance, DIC [63] [64] | Assess model fit and compare models | DIC preferred for Bayesian model comparison in NMA [64] |
| Visualization Tools | Network plots, trace plots, rankograms | Visual assessment of network structure and convergence | Network geometry visualization essential for transitivity assessment |
Application in Therapeutic Equivalence Research
In therapeutic equivalence research, proper application of these diagnostics is crucial for valid inference. A recent Bayesian NMA of aldosterone synthase inhibitors for hypertension demonstrated appropriate use of these metrics [64]. The researchers reported using DIC to compare fixed-effect and random-effects models, ultimately selecting the random-effects specification based on better fit to the data. They assessed convergence using R-hat statistics, ensuring all parameters met the convergence threshold before basing conclusions on the posterior distributions [64].
The integration of these diagnostics provides a systematic approach to model criticism in NMA. For instance, in the hypertension NMA, the combination of adequate convergence (R-hat < 1.05), appropriate model selection (via DIC), and examination of residual deviance provided comprehensive evidence that the results were reliable for informing clinical practice [64]. This multi-diagnostic approach is particularly important when assessing therapeutic equivalence, where subtle differences between treatments may have significant clinical implications.
When evaluating NMAs for therapeutic equivalence, researchers should verify that all three diagnostics have been properly assessed and reported. Convergence problems (high R-hat) may indicate that the model is poorly specified or requires more computational resources. Poor model fit (high residual deviance) may suggest missing effect modifiers or inappropriate statistical assumptions. Suboptimal DIC values may indicate that an alternative model specification would better balance complexity and fit. Through careful attention to these diagnostics, researchers can have greater confidence in conclusions regarding therapeutic equivalence and relative treatment efficacy.
Ensuring Validity and Impact: Critical Appraisal and Real-World Implementation
Network meta-analysis (NMA) represents a significant advancement in evidence synthesis methodology by enabling simultaneous comparison of multiple interventions through a combination of direct and indirect evidence [62]. This approach allows researchers to determine the comparative effectiveness of treatments that may never have been directly compared in clinical trials and provides more precise estimates for existing comparisons [7]. However, the validity of NMA conclusions depends critically on statistical assumptions that require rigorous evaluation [6]. The complexity of NMA inherits all assumptions from pairwise meta-analysis while introducing additional considerations that must be carefully addressed to ensure results are reliable and trustworthy for clinical decision-making [62].
Within the context of evaluating therapeutic equivalence in network meta-analysis research, validation techniques serve as essential safeguards against biased or spurious conclusions. Two fundamental approaches have emerged for validating NMA findings: sensitivity analyses, which test the robustness of results to different assumptions or methodological choices, and node-splitting methods, which specifically evaluate the consistency between direct and indirect evidence [71] [72]. These techniques address different potential threats to validity but share the common goal of strengthening confidence in NMA results when informing clinical guidelines or health policy decisions [73] [74]. This guide provides a comprehensive comparison of these validation techniques, their methodologies, applications, and interpretations to support researchers, scientists, and drug development professionals in conducting rigorous network meta-analyses.
Theoretical Foundations of NMA Validation
Core Assumptions and Potential Threats to Validity
The validity of network meta-analysis rests on three fundamental assumptions: transitivity, consistency, and homogeneity. Transitivity refers to the similarity of studies across different treatment comparisons in terms of key effect modifiers [6]. When the distribution of effect modifiers (such as patient characteristics, intervention dosage, or study methodology) differs across comparisons, the transitivity assumption is violated, potentially leading to biased results [6]. Consistency, the statistical manifestation of transitivity, requires that direct and indirect evidence for the same treatment comparison are in agreement [6] [62]. Homogeneity assumes that variability in treatment effects across studies investigating the same comparison is due to chance alone [75].
Violations of these assumptions manifest as inconsistency (disagreement between direct and indirect evidence) or heterogeneity (excessive variation in treatment effects between studies of the same comparison) [73]. Both problems threaten the validity of NMA findings and can lead to incorrect conclusions about therapeutic equivalence or superiority [6]. The validation techniques discussed in this guide specifically target these potential threats, allowing researchers to quantify and address them methodically.
Conceptual Framework of Validation Techniques
Validation techniques in NMA operate under a common conceptual framework that involves testing the stability of results under different conditions or assumptions. Sensitivity analyses examine how robust the findings are to changes in inclusion criteria, analytical methods, or assumptions about missing data [74] [76]. Node-splitting methods specifically evaluate potential inconsistencies by separating direct and indirect evidence for particular comparisons [73] [72]. These approaches can be viewed as complementary components of a comprehensive validation strategy, with each addressing different aspects of potential bias.
The theoretical foundation for these methods stems from recognizing that NMA combines evidence from studies with different designs and populations, creating potential for confounding when evidence is synthesized across studies [6]. As the complexity of treatment networks increases, with multiple interventions and various pathways connecting them, the need for robust validation becomes increasingly important [62]. This is particularly critical when evaluating therapeutic equivalence, where small biases can lead to incorrect conclusions about comparable treatment effects.
Sensitivity Analysis in Network Meta-Analysis
Methodological Approaches
Sensitivity analysis in NMA involves systematically testing how sensitive the results are to changes in analytical approaches, inclusion criteria, or underlying assumptions. The pattern-mixture model provides a sophisticated framework for handling missing participant outcome data (MOD), which represents a common threat to validity in systematic reviews [74]. This model maintains the randomized sample of studies in the analysis, conforming with the intention-to-treat principle generally preferred in evidence synthesis [74]. The model can be represented as:
θ{ik} = θ{ik}^o • (1 - q{ik}) + θ{ik}^m • q_{ik}
Where θ{ik} is the underlying outcome, θ{ik}^o is the underlying outcome in observed participants, θ{ik}^m is the underlying unobserved outcome in missing participants, and q{ik} is the probability of missing data in arm k of study i [74].
For binary outcomes, the relationship between observed and unobserved outcomes is quantified using the informative missingness odds ratio (IMOR), while for continuous outcomes, the informative missingness difference of means (IMDoM) parameter is used [74]. These parameters allow researchers to incorporate clinically plausible assumptions about the missingness mechanism and test how sensitive results are to different assumptions.
Another important sensitivity approach involves testing the impact of excluding specific treatments from the network [76]. This is particularly relevant when treatments have different evidence bases or when control groups vary across studies. The arm-based NMA model offers advantages in this context, as it allows retention of single arms when connected treatments are removed, whereas contrast-based methods must exclude entire studies when one treatment arm is omitted [76].
Implementation Protocols
Implementing sensitivity analysis for missing data requires careful planning and execution:
Define the primary analysis: Specify the primary analytical approach and assumptions about missing data, typically based on missing-at-random assumptions [74].
Specify alternative scenarios: Define clinically plausible alternative scenarios for the missing data mechanism. For binary outcomes, this involves specifying different IMOR values; for continuous outcomes, different IMDoM values [74].
Calculate the robustness index (RI): Quantify the similarity between primary analysis results and results under alternative assumptions using the robustness index. The RI measures the deviation between effect estimates across different assumptions, with higher values indicating greater fragility of results [74].
Compare with current standards: Current sensitivity analysis standards often rely on statistical significance, but the RI offers a more formal definition of similar results without undue reliance on significance testing [74].
Interpret and report: Document how results change under different assumptions and clearly communicate the robustness (or fragility) of conclusions.
Table 1: Sensitivity Analysis Approaches for Different Data Types
| Data Type | Primary Model | Sensitivity Parameter | Interpretation |
|---|---|---|---|
| Binary outcomes | Pattern-mixture model | Informative Missingness Odds Ratio (IMOR) | IMOR > 1 indicates missing participants more likely to have an event |
| Continuous outcomes | Pattern-mixture model | Informative Missingness Difference of Means (IMDoM) | Positive IMDoM indicates larger outcomes in missing participants |
| Treatment exclusion | Arm-based NMA | Comparison of networks with/without treatments | Large changes suggest sensitivity to treatment selection |
Applications and Interpretation
Sensitivity analysis has proven particularly valuable in addressing missing outcome data, a ubiquitous challenge in systematic reviews. Empirical studies have demonstrated that when studies with substantial missing data dominate analyses, conclusions become more fragile [74]. The robustness index (RI) has revealed that approximately 59% of primary analyses fail to demonstrate robustness, compared to only 39% when using current sensitivity analysis standards that rely solely on statistical significance [74]. This discrepancy highlights the importance of using formal measures of robustness rather than relying solely on significance testing.
When excluding treatments from networks, research has shown that contrast-based NMA results can be substantially influenced by the removal of specific treatments [76]. For example, in a network examining statins for cholesterol management, exclusion of placebo arms significantly altered the relative effect estimates between active treatments [76]. Arm-based models demonstrate greater stability in such sensitivity analyses, as they can retain information from single-arm studies even when connected treatments are removed from the network [76].
Node-Splitting Methods for Detecting Inconsistency
Theoretical Basis and Methodological Variations
Node-splitting represents a specific technique for evaluating inconsistency in NMA by separating direct and indirect evidence for particular treatment comparisons [73]. This method is conceptually attractive because it tests for inconsistency one comparison at a time, providing easily interpretable results that pinpoint specific areas of concern in the evidence network [73] [72]. The fundamental concept involves splitting a treatment comparison (denoted as d{x,y}) into two distinct parameters: a parameter for direct evidence (d{x,y}^{dir}) and a parameter for indirect evidence (d{x,y}^{ind}) [73]. The method then tests whether these parameters are in agreement, effectively evaluating the hypothesis that d{x,y}^{dir} = d_{x,y}^{ind} [73].
Different parameterizations of node-splitting models have been developed, each with distinct implications for interpretation [72]. The symmetrical method assumes that both treatments in a comparison contribute equally to inconsistency, while asymmetrical parameterizations attribute inconsistency primarily to one treatment or the other [72]. These parameterizations correspond to different design-by-treatment interactions and can yield slightly different results, particularly when multi-arm trials are involved in the evaluation [72]. The choice between these approaches should be guided by clinical understanding of the evidence base and potential sources of inconsistency.
Automated approaches to node-splitting have been developed to address the labor-intensive nature of manually implementing separate models for each comparison of interest [73]. These methods employ decision rules to select which comparisons to split, ensuring that only comparisons in potentially inconsistent loops are investigated while circumventing problems with the parameterization of multi-arm trials [73].
Implementation Protocol
Implementing node-splitting analysis requires careful execution of the following steps:
Identify comparisons for splitting: Determine which treatment comparisons have both direct and indirect evidence. Automated algorithms can select comparisons in potentially inconsistent loops, ensuring all potentially inconsistent loops in the network are investigated [73].
Specify the node-splitting model: For each selected comparison, specify a model that separates direct and indirect evidence. The model can be implemented in both Bayesian and frequentist frameworks, with the choice depending on researcher preference and software capabilities [72] [77].
Estimate direct and indirect effects: Obtain estimates for the treatment effect based solely on direct evidence (from studies directly comparing the treatments) and based solely on indirect evidence (derived from the remaining network) [73] [71].
Test for disagreement: Evaluate whether direct and indirect estimates are statistically significantly different. In Bayesian frameworks, this often involves examining the posterior distribution of the difference between direct and indirect estimates; in frequentist approaches, confidence intervals and p-values are used [71] [77].
Interpret and address inconsistencies: When significant discrepancies are found, investigate potential causes by examining study characteristics, risk of bias, or clinical differences between studies contributing direct versus indirect evidence [73].
Table 2: Node-Splitting Parameterization Methods
| Parameterization | Inconsistency Attribution | Best Use Case |
|---|---|---|
| Symmetrical | Both treatments contribute equally | No prior knowledge about inconsistency source |
| Asymmetrical (Treatment A) | Primarily attributed to Treatment A | Clinical rationale for expecting one treatment to be problematic |
| Asymmetrical (Treatment B) | Primarily attributed to Treatment B | Clinical rationale for expecting one treatment to be problematic |
Applications and Interpretation
Node-splitting has been widely applied in NMAs across therapeutic areas. For example, in a network meta-analysis of drug therapies for early rheumatoid arthritis, node-splitting was used to test consistency between direct and indirect evidence for several comparisons, including Abatacept versus Abatacept plus Methotrexate and Adalimumab versus Adalimumab plus Methotrexate [71]. The analysis revealed no significant differences between direct and indirect evidence, increasing confidence in the consistency of the network [71].
The interpretation of node-splitting results requires careful consideration of statistical power and clinical context. Non-significant results do not necessarily prove consistency, as tests may be underpowered to detect important differences, particularly when direct evidence is sparse [73]. Conversely, statistically significant results may not always indicate clinically important inconsistency. Researchers should consider the magnitude of differences and their potential impact on conclusions about therapeutic equivalence or superiority.
When inconsistency is detected, possible responses include excluding studies contributing to inconsistency, using inconsistency models that incorporate both consistent and inconsistent evidence, or exploring effect modifiers through meta-regression [73]. The appropriate response depends on the likely causes of inconsistency and the goals of the analysis.
Comparative Evaluation of Validation Techniques
Relative Strengths and Limitations
Sensitivity analyses and node-splitting methods address different aspects of NMA validation and offer complementary strengths. Sensitivity analyses provide a broad assessment of result robustness to various assumptions and methodological choices, while node-splitting specifically targets the agreement between direct and indirect evidence [73] [74]. The choice between these approaches should be guided by the specific validation needs and potential threats to validity in a given network.
Table 3: Comparison of Validation Techniques for NMA
| Characteristic | Sensitivity Analysis | Node-Splitting |
|---|---|---|
| Primary purpose | Test robustness to assumptions/methods | Detect inconsistency between direct/indirect evidence |
| Scope of evaluation | Broad (multiple potential threats) | Narrow (specific to consistency) |
| Implementation complexity | Variable (depends on type) | High (separate models for each comparison) |
| Interpretability | Generally straightforward | Straightforward for individual comparisons |
| Statistical power | Depends on approach | May be limited for comparisons with sparse direct evidence |
| Handling of multi-arm trials | Varies by approach | Requires careful parameterization |
Integration in Comprehensive Validation Strategies
For a thorough assessment of NMA validity, sensitivity analyses and node-splitting should be integrated into a comprehensive validation strategy. This integrated approach might begin with global assessments of inconsistency using design-by-treatment interaction models, followed by localized evaluation of specific comparisons using node-splitting [73] [72]. Sensitivity analyses should then address other potential threats to validity, including missing data, selection of included treatments, and alternative statistical modeling choices [74] [76].
This sequential approach maximizes efficiency by focusing detailed investigations on areas of potential concern identified through initial screening. It also recognizes that different validation techniques address distinct aspects of validity, providing a more complete picture of result reliability than any single method alone.
Empirical evidence suggests that the combination of these approaches is particularly important given the frequency of robustness concerns in NMA. Studies have found that approximately 59% of primary analyses demonstrate fragility when rigorously evaluated with sensitivity analyses [74], while inconsistency is not uncommon in networks with multiple sources of direct and indirect evidence [73] [71].
Research Reagent Solutions
Implementing effective validation strategies for NMA requires specialized methodological tools and software solutions. The following table outlines key resources available to researchers:
Table 4: Research Reagent Solutions for NMA Validation
| Tool/Resource | Type | Primary Function | Implementation |
|---|---|---|---|
| Robustness Index (RI) | Statistical metric | Quantifies similarity between primary and sensitivity analysis results | Pattern-mixture models for missing data |
| Automated node-splitting algorithms | Software method | Implements node-splitting for all relevant comparisons | Decision rules for comparison selection [73] |
| Informative Missingness Odds Ratio (IMOR) | Statistical parameter | Quantifies relationship between observed and missing outcomes | Bayesian or frequentist pattern-mixture models |
| Network geometry assessment | Analytical approach | Evaluates network connectivity and potential for inconsistency | Network graphs and connectivity metrics |
| Design-by-treatment interaction model | Statistical model | Global test of inconsistency across network | Bayesian or frequentist framework |
These methodological tools continue to evolve, with ongoing research focused on improving their implementation, interpretation, and integration into comprehensive validation frameworks. Researchers should stay abreast of methodological developments to ensure they are using the most appropriate and up-to-date validation techniques for their network meta-analyses.
Network meta-analysis (NMA) has become an established methodology for comparing multiple interventions simultaneously by synthesizing both direct evidence from head-to-head trials and indirect evidence through common comparators [78]. This advanced statistical technique allows researchers to compare the relative effectiveness of numerous treatments, even when some have never been directly compared in clinical trials [9]. The fundamental principle enabling these comparisons is transitivity—the assumption that study populations and methodological characteristics are sufficiently similar across the network to allow for valid indirect comparisons [78].
Assessing inconsistency (also referred to as coherence) between direct and indirect evidence forms a critical methodological foundation for validating NMA results [78]. Statistical inconsistency arises when the treatment effects estimated from direct evidence systematically differ from those derived through indirect evidence pathways [9]. Such discrepancies can indicate violations of transitivity assumptions or methodological biases within the evidence network, potentially compromising the validity of NMA conclusions. For researchers, clinicians, and drug development professionals, understanding how to detect, evaluate, and interpret inconsistency is essential for critically appraising NMA findings and making evidence-based decisions regarding therapeutic equivalence or superiority.
Methodological Frameworks for Detecting Inconsistency
Statistical Approaches to Inconsistency Assessment
Several statistical methods have been developed to evaluate inconsistency in network meta-analyses, each with distinct approaches and applications. The following table summarizes the primary methodological frameworks available to researchers:
Table 1: Methods for Assessing Inconsistency in Network Meta-Analysis
| Method Type | Specific Approach | Key Features | Implementation |
|---|---|---|---|
| Global Methods | Higgins' Global Inconsistency Test [79] | Evaluates inconsistency across the entire network simultaneously | Multivariate meta-regression framework |
| Local Methods | Loop-specific Approach [9] | Examines inconsistency in closed loops with both direct and indirect evidence | Compares direct and indirect estimates within each loop |
| Model-Based Frameworks | Jackson's Random Inconsistency Model [79] | Incorporates inconsistency as random effects | Accounts for heterogeneity in inconsistency |
| Path-Based Methods | Netpath Plot & Quantitative Measure [80] | Novel method exploring all evidence sources without separating direct/indirect | Visualizes inconsistencies between various evidence paths |
Global methods like Higgins' test provide an overall assessment of inconsistency throughout the network but may mask specific localized problems [79]. Conversely, local approaches such as loop-specific methods allow researchers to pinpoint exactly where inconsistency occurs within the network geometry, facilitating more targeted investigations into potential causes [9]. The recently developed path-based approach addresses limitations of conventional methods by quantitatively capturing inconsistency through squared differences and visualizing discrepancies between various evidence paths without aggregating all indirect sources together [80].
Implementation in Statistical Software
Multiple R packages now implement comprehensive tools for inconsistency assessment. The NMA package provides a user-friendly interface for implementing Higgins' global inconsistency test, Jackson's random inconsistency model, and various graphical tools for evaluating transitivity [79]. This package is particularly valuable as it offers a general frequentist tool based on multivariate meta-analysis and meta-regression models previously unavailable in R. Similarly, the netmeta package has been extended to incorporate the novel path-based approach for detecting and visualizing inconsistency [80].
Experimental Protocols for Inconsistency Assessment
Standardized Workflow for Evaluation
Implementing a rigorous approach to inconsistency assessment requires following a structured workflow that incorporates multiple complementary methods. The diagram below illustrates the key steps in this process:
Diagram 1: Workflow for inconsistency assessment in NMA
Protocol for Global Inconsistency Testing
Global tests evaluate whether inconsistency exists anywhere within the entire network. The implementation protocol involves:
Model Specification: Fit both consistency and inconsistency models using multivariate meta-regression frameworks. The consistency model assumes no disagreement between direct and indirect evidence, while the inconsistency model allows for these differences [79].
Statistical Comparison: Conduct likelihood ratio tests comparing the fit of consistency and inconsistency models. A significant result (typically p < 0.05) indicates presence of global inconsistency in the network [79].
Magnitude Assessment: Quantify the extent of inconsistency using appropriate statistics such as the multivariate I² statistic for heterogeneity, which indicates the percentage of total variability due to inconsistency rather than sampling error [79].
Protocol for Local Inconsistency Assessment
Local methods identify specific locations within the network where direct and indirect evidence disagree:
Loop Identification: Identify all closed loops within the network geometry where both direct and indirect evidence exist for a treatment comparison [9].
Difference Estimation: Calculate the difference between direct and indirect estimates for each comparison within identified loops. The loop-specific approach computes the inconsistency factor (IF) as the absolute difference between direct and indirect treatment effects [9].
Statistical Testing: Evaluate whether the inconsistency factor significantly differs from zero using Z-tests with variance estimates derived from the standard errors of both direct and indirect effects.
Node-Splitting: Implement node-splitting techniques that separately estimate treatment effects from direct and indirect evidence for each comparison, then test for statistically significant differences between these estimates.
Protocol for Path-Based Inconsistency Evaluation
The novel path-based approach provides a more granular assessment:
Evidence Path Enumeration: Identify all possible evidence paths connecting each treatment pair within the network, without aggregating into direct versus indirect categories [80].
Quantitative Measurement: Calculate inconsistency measures based on squared differences between path-specific treatment effect estimates [80].
Visualization: Generate Netpath plots to graphically display inconsistencies between various evidence paths, allowing researchers to identify which specific pathways contribute most to overall inconsistency [80].
The Researcher's Toolkit for Inconsistency Assessment
Table 2: Essential Tools for Inconsistency Assessment in Network Meta-Analysis
| Tool Category | Specific Tool/Resource | Function in Inconsistency Assessment | Implementation Considerations |
|---|---|---|---|
| Statistical Software | NMA R Package [79] | Comprehensive frequentist implementation of global tests, meta-regression, and graphical tools | Based on multivariate meta-analysis models; handles arm-level and summary-level data |
| Statistical Software | netmeta R Package [80] | Contrast-based NMA with path-based inconsistency methods and network graphics | Implements novel path-based approach for detecting masked inconsistencies |
| Reporting Guidelines | PRISMA-NMA Extension [26] | Standardized reporting framework for NMAs including inconsistency assessments | Critical for transparent reporting; currently being updated to address methodological advances |
| Evidence Assessment | CINeMA (Confidence in NMA) [23] | Web-based application for evaluating confidence in NMA findings | Facilitates GRADE-based assessment of evidence certainty across multiple domains including inconsistency |
| Methodological Framework | GRADE for NMA [23] | Systematic approach for rating certainty of evidence in treatment comparisons | Provides structured approach for downgrading evidence due to inconsistency |
Interpretation and Reporting of Findings
Clinical and Methodological Interpretation
When inconsistency is detected, researchers must investigate potential causes through several analytical approaches:
Assessment of Effect Modifiers: Examine whether the distribution of potential effect modifiers (e.g., disease severity, concomitant treatments, patient characteristics) differs across treatment comparisons. Such differences violate the transitivity assumption and can explain observed inconsistencies [78].
Methodological Heterogeneity: Evaluate whether studies contributing to different evidence pathways vary systematically in their risk of bias, outcome definitions, or follow-up durations [9].
Statistical Investigation: Implement network meta-regression or subgroup analyses to explore whether specific study-level covariates account for the detected inconsistency [79].
The clinical interpretation of inconsistency findings depends on their magnitude, statistical significance, and potential explanations. Minor inconsistency in secondary outcomes may not substantially affect conclusions, while substantial inconsistency in primary outcomes for key treatment comparisons may seriously undermine confidence in network estimates.
Transparent Reporting Standards
Complete reporting of inconsistency assessments is essential for NMA credibility. The PRISMA-NMA extension provides specific guidance for reporting inconsistency evaluations [26]. Key reporting elements include:
- Description of statistical methods used to evaluate inconsistency
- Results of global and local inconsistency tests, preferably with confidence intervals
- For each closed loop in the network, presentation of both direct and indirect estimates alongside measures of their disagreement
- Discussion of potential explanations for any identified inconsistency
- Assessment of how inconsistency affects the certainty of evidence using structured approaches like GRADE [23]
Ongoing updates to PRISMA-NMA aim to address persistent gaps in reporting of inconsistency assessments and incorporate recent methodological developments [26].
Assessing inconsistency between NMA results and direct evidence represents a fundamental methodological component of network meta-analysis validation. Through the application of global tests, local approaches, and emerging path-based methods, researchers can evaluate the coherence of evidence networks and identify potential threats to validity. The integration of these assessments with investigations of transitivity and methodological quality provides a comprehensive framework for evaluating the reliability of NMA findings regarding therapeutic equivalence or superiority.
As NMA methodologies continue to evolve, with ongoing updates to reporting guidelines like PRISMA-NMA and development of more sophisticated software tools, the rigor and transparency of inconsistency assessments are expected to improve further. For drug development professionals and clinical researchers, understanding these principles and applications remains essential for critically appraising comparative effectiveness research and making evidence-based treatment decisions.
The treatment landscape for metastatic prostate cancer has evolved significantly, moving from androgen deprivation therapy (ADT) alone to combination regimens incorporating androgen receptor pathway inhibitors (ARPIs) and chemotherapy. For researchers and drug development professionals, evaluating the therapeutic equivalence and comparative safety of these systemic therapies is crucial for optimizing treatment selection and sequencing. This case study employs network meta-analysis (NMA) methodology to provide indirect comparisons of safety outcomes across multiple treatment regimens for metastatic hormone-sensitive prostate cancer (mHSPC), where head-to-head randomized controlled trials are limited. By synthesizing evidence from recent clinical trials, this analysis aims to inform clinical decision-making and future drug development strategies.
Methodological Framework
Network Meta-Analysis Design
This evaluation follows established systematic review and NMA methodologies based on PRISMA guidelines and NICE requirements [81]. The analysis incorporated randomized controlled trials (RCTs) investigating systemic treatments for mHSPC published before July 2022, identified through systematic searches of Embase, MEDLINE, Cochrane CENTRAL, and CDSR databases via the Ovid platform [81].
Population, Intervention, Comparator, Outcomes, Study (PICOS) Criteria:
- Population: Men (aged ≥18 years) with mHSPC
- Interventions: ADT alone or in combination with ARPI (apalutamide, enzalutamide, darolutamide, or abiraterone acetate plus prednisone [AAP]), docetaxel, or both docetaxel and ARPI
- Comparators: Active interventions within the connected network
- Outcomes: Grade ≥3 adverse events (AEs), serious AEs (SAEs), and any AEs
- Study Design: RCTs only
Statistical Analysis
Bayesian NMA was performed using aggregated safety outcomes with fixed- and random-effects models run under the Bayesian framework [82] [81]. Four Markov chain Monte Carlo chains with different starting values were implemented with a burn-in of at least 2,000 iterations and a further sample of at least 10,000 iterations [82]. For studies with multiple data cutoffs, the time point closest to the median follow-up of 44 months (corresponding to the TITAN final analysis) was selected to reduce heterogeneity in treatment exposure duration [81]. Relative risks with 95% credible intervals were calculated for all safety outcomes versus ADT alone.
Quality Assessment and Feasibility
Risk of bias was assessed using the Cochrane Risk of Bias tool by one reviewer with verification by a second independent reviewer [81]. A feasibility assessment evaluated network connectivity and clinical/methodological heterogeneity across trials, including study design, population characteristics, comparators, and outcome definitions [82].
Comparative Safety Profiles of Systemic Therapies
Grade ≥3 Adverse Events
The analysis of grade ≥3 adverse events provides crucial insights into treatment tolerability. The table below summarizes the relative risks compared to ADT monotherapy.
Table 1: Relative Risk of Grade ≥3 Adverse Events for mHSPC Systemic Therapies Versus ADT Alone
| Treatment Regimen | Relative Risk | 95% Credible Interval |
|---|---|---|
| Apalutamide + ADT | 1.18 | 1.02–1.35 |
| Enzalutamide + ADT | 1.34 | 1.17–1.52 |
| Docetaxel + ADT | 1.44 | 1.33–1.56 |
| AAP + ADT | 1.48 | 1.39–1.58 |
| Darolutamide + Docetaxel + ADT | 1.53 | 1.33–1.72 |
| AAP + Docetaxel + ADT | 1.60 | 1.41–1.79 |
Among doublet ARPI regimens, apalutamide plus ADT demonstrated the most favorable safety profile with the lowest relative risk (1.18) of grade ≥3 AEs [81]. Enzalutamide plus ADT showed intermediate risk (1.34), while AAP plus ADT carried higher risk (1.48) [81]. Docetaxel-based doublet and triplet regimens consistently demonstrated higher risks of severe adverse events, with AAP plus docetaxel plus ADT showing the highest risk (1.60) [81].
Serious Adverse Events
Serious adverse events represent those that result in hospitalization, significant disability, or life-threatening conditions. The analysis revealed distinct patterns across treatment regimens.
Table 2: Relative Risk of Serious Adverse Events for mHSPC Systemic Therapies Versus ADT Alone
| Treatment Regimen | Relative Risk | 95% Credible Interval |
|---|---|---|
| Apalutamide + ADT | 1.26 | 1.03–1.53 |
| AAP + ADT | 1.33 | 1.12–1.57 |
| Enzalutamide + ADT | 1.54 | 1.28–1.84 |
| Docetaxel + ADT | 3.78 | 3.35–4.26 |
| Darolutamide + Docetaxel + ADT | 3.83 | 3.39–4.31 |
The risk of SAEs followed a different pattern than overall grade ≥3 AEs. While apalutamide plus ADT again demonstrated the lowest risk among ARPI-based regimens (1.26), the docetaxel-containing regimens showed substantially higher risks of SAEs, with approximately 3.8-fold increases compared to ADT alone [81]. This pronounced increase in serious adverse events with chemotherapy-containing regimens highlights an important safety consideration for treatment selection.
Adverse Event Profile in Biochemically Recurrent Non-Metastatic HSPC
For high-risk biochemically recurrent non-metastatic hormone-sensitive prostate cancer (nmHSPC), safety considerations differ from mHSPC. A separate NMA found that enzalutamide with ADT demonstrated superior efficacy outcomes but with a higher risk of treatment-related adverse events compared to ADT alone [82] [83]. Enzalutamide combination therapy showed similar safety performance to enzalutamide monotherapy despite superior efficacy across all measured endpoints [82]. Notably, treatment-related adverse events were least common for ADT alone, reflecting the increased toxicity burden associated with treatment intensification [83].
Mechanistic Insights and Adverse Event Profiles
Different treatment classes exhibit distinct adverse event profiles rooted in their mechanisms of action. Understanding these relationships is essential for both clinical management and drug development.
Figure 1: Mechanism-based adverse events in prostate cancer therapies. ARPIs: androgen receptor pathway inhibitors; Chemo: chemotherapy; ADT: androgen deprivation therapy.
ARPIs demonstrate class-specific adverse events including hypertension (particularly with AAP), rash (with apalutamide), and cognitive impairment/memory loss (with enzalutamide) [81]. Docetaxel-based regimens primarily cause neutropenia and fatigue due to their cytotoxic effects on rapidly dividing cells [81]. ADT contributes broadly to metabolic syndrome and fatigue through profound hormonal suppression [84]. These mechanism-specific profiles explain the differential safety signals observed in the network meta-analysis and provide insights for managing expected toxicities in clinical practice.
Research Reagents and Methodological Tools
Implementing robust network meta-analyses in prostate cancer research requires specific methodological approaches and tools. The table below outlines essential components for conducting such analyses.
Table 3: Essential Research Reagents and Methodological Tools for Prostate Cancer NMA
| Component | Function/Application | Examples/Specifications |
|---|---|---|
| Systematic Review Databases | Identification of relevant RCTs | Embase, MEDLINE, Cochrane CENTRAL, CDSR [81] |
| Statistical Software | Bayesian NMA implementation | R (version 4.2.1+) with "multinma" package [82] |
| Quality Assessment Tools | Risk of bias evaluation | Cochrane Risk of Bias tool (v1 or RoB-2) [82] [81] |
| Outcome Metrics | Standardized safety assessment | Grade ≥3 AEs, SAEs, any AEs (CTCAE criteria) [81] |
| Follow-up Time Standardization | Reduce exposure heterogeneity | Time point closest to 44 months (TITAN trial reference) [81] |
These methodological components ensure the reproducibility and validity of indirect treatment comparisons. The use of Bayesian framework with appropriate burn-in iterations and sampling, combined with standardized outcome assessments, allows for robust quantification of relative safety across treatment regimens [82] [81]. The feasibility assessment for network connectivity and clinical heterogeneity is particularly important when incorporating trials with varying patient populations and study designs.
This network meta-analysis demonstrates significant differences in safety profiles among systemic therapies for metastatic prostate cancer. ARPI-based doublet regimens, particularly apalutamide plus ADT, show more favorable safety profiles compared to docetaxel-containing regimens, which exhibited substantially higher risks of serious adverse events. These findings must be interpreted alongside established efficacy benefits when making treatment decisions. The mechanistic understanding of class-specific adverse events provides valuable insights for toxicity management and future drug development. For researchers, this case study highlights the importance of indirect treatment comparisons using rigorous methodology when direct head-to-head evidence is unavailable, supporting the evaluation of therapeutic equivalence and risk-benefit profiles in prostate cancer management.
Translating NMA Findings into Clinical Practice and Health Policy Guidelines
Network meta-analysis (NMA) has emerged as a powerful statistical methodology that enables the simultaneous comparison of multiple interventions, even when direct head-to-head evidence is unavailable. By integrating both direct and indirect evidence across a network of randomized controlled trials (RCTs), NMA provides a comprehensive framework for evaluating therapeutic equivalence, relative efficacy, and safety profiles of competing treatments [85] [78]. This advanced evidence synthesis technique addresses critical clinical and policy questions that extend beyond conventional pairwise meta-analysis, particularly in therapeutic areas with numerous intervention options but limited direct comparative evidence [85].
The translation of NMA findings into clinical practice and health policy requires rigorous methodology and careful interpretation. As the complexity of healthcare interventions increases, NMA serves as a bridge between clinical research and decision-making by providing comparative effectiveness data essential for formularies, treatment guidelines, and resource allocation [16]. This article examines the methodological foundations of NMA, outlines frameworks for interpreting results within therapeutic equivalence contexts, and provides guidance for applying these findings to clinical and policy decisions.
Methodological Foundations of Network Meta-Analysis
Core Principles and Assumptions
NMA functions by constructing a network of interventions connected through direct and indirect comparisons, with the validity of results dependent on three fundamental assumptions [78]:
- Similarity: Trials included in the network must share key methodological characteristics including study populations, interventions, comparators, and outcome measures.
- Transitivity: Effect modifiers—study characteristics that influence treatment outcomes—must be similarly distributed across treatment comparisons. This assumption ensures that indirect comparisons are statistically valid [85].
- Consistency (Coherence): Direct and indirect evidence for a specific treatment comparison must be statistically compatible. Significant differences between direct and indirect estimates (incoherence) suggest violation of transitivity or similarity assumptions [85].
Table 1: Fundamental Assumptions of Valid Network Meta-Analysis
| Assumption | Definition | Implication for Validity |
|---|---|---|
| Similarity | Shared methodological characteristics across trials | Ensures trials address similar research questions |
| Transitivity | Balanced distribution of effect modifiers across comparisons | Enables valid indirect treatment comparisons |
| Consistency | Agreement between direct and indirect evidence | Supports combining different evidence sources |
Analytical Frameworks and Outcome Measures
NMA can be conducted within both Bayesian and frequentist statistical frameworks, with choice dependent on the specific research question, complexity of the network, and available computational resources [18]. Effect estimates are typically expressed as risk ratios (RR) or odds ratios (OR) for dichotomous outcomes and mean differences (MD) or standardized mean differences (SMD) for continuous outcomes, accompanied by confidence or credible intervals representing statistical uncertainty [78].
Recent methodological advances have enhanced NMA capabilities, including modeling of complex interventions, dose-response relationships, handling missing data, and assessing certainty of evidence using approaches like CINeMA (Confidence in Network Meta-Analysis) and GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) [23].
Framework for Clinical Application of NMA Findings
Interpreting NMA Geometry and Treatment Rankings
The foundation for interpreting NMA results begins with understanding the network geometry—a graphical representation of the evidence structure. In network diagrams, nodes represent interventions, with their size proportional to the number of patients receiving that treatment. Lines connecting nodes represent direct comparisons, with thickness indicating the number of trials supporting that comparison [85] [78].
Treatment ranking statistics such as the Surface Under the Cumulative Ranking Curve (SUCRA) and probability of being best (p-best) provide relative performance metrics, with values ranging from 0-100% (higher values indicating better performance) [18]. However, these rankings must be interpreted cautiously, considering both the magnitude of effect differences and the certainty of evidence, as rankings based on small, low-quality trials with large effect sizes may be misleading [85].
Assessing Therapeutic Equivalence and Comparative Effectiveness
Determining therapeutic equivalence requires evaluating both statistical significance and clinical relevance of effect size differences. The following workflow outlines the critical appraisal process for NMA findings:
Critical considerations for therapeutic equivalence assessment:
- Precision of estimates: Examine confidence/credible intervals for range of plausible effects
- Clinical significance: Determine if statistically significant differences translate to clinically meaningful benefits
- Outcome selection: Prioritize patient-important outcomes over surrogate endpoints
- Safety profile: Balance efficacy with adverse event profiles and tolerability
Clinical Application Examples Across Therapeutic Areas
Hereditary Angioedema Prophylaxis
A 2025 NMA comparing long-term prophylactic treatments for hereditary angioedema (HAE) demonstrated how NMA informs clinical decision-making between newer and established therapies. The analysis found that garadacimab (200 mg monthly) significantly reduced the rate of HAE attacks compared to lanadelumab and berotralstat, while also showing statistical improvements in quality of life scores compared to berotralstat. Across most outcomes, garadacimab ranked as the most probably effective treatment, followed by lanadelumab or subcutaneous C1INH [18].
Table 2: Comparative Efficacy of HAE Prophylaxis Treatments (Adapted from PMC12185836)
| Intervention | Dosage Regimen | Rate Ratio vs. Placebo | SUCRA Value | Key Comparative Findings |
|---|---|---|---|---|
| Garadacimab | 200 mg monthly | 0.27 (0.15-0.45) | 92% | Superior to lanadelumab Q4W and berotralstat |
| Lanadelumab | 300 mg every 2 weeks | 0.31 (0.21-0.46) | 85% | Second-line option across most outcomes |
| Subcutaneous C1INH | 60 IU/kg twice weekly | 0.34 (0.21-0.55) | 78% | Comparable to lanadelumab Q2W |
| Berotralstat | 150 mg daily | 0.57 (0.41-0.80) | 45% | Improved QoL but less effective for attack reduction |
Heart Failure with Reduced Ejection Fraction (HFrEF)
An updated NMA on HFrEF pharmacotherapy demonstrates the evolving nature of treatment recommendations based on accumulating evidence. The analysis of 89 RCTs found that quadruple therapy with ARNi, β-blockers, MRAs, and SGLT2i reduced all-cause mortality by 61% (HR: 0.39; 95% CI: 0.32-0.49) compared to placebo. The addition of vericiguat to quadruple therapy (quintuple therapy) provided further mortality reduction (HR: 0.35; 95% CI: 0.27-0.45), translating to an additional 0.7 life-years gained for a representative 70-year-old patient [16].
Chronic Rhinosinusitis with Nasal Polyps (CRSwNP)
In CRSwNP, an NMA of 22 RCTs evaluating biologic therapies demonstrated how treatment ranking varies across different outcome domains. Dupilumab consistently ranked among the top three agents across most efficacy outcomes, including nasal polyp score, nasal congestion score, and quality of life measures. CM310 and Tezepelumab also demonstrated strong performance in objective and symptom-based outcomes, while all biologics showed similar safety profiles [86].
Methodological Protocols for NMA Implementation
Systematic Review and Study Selection
The foundation of a valid NMA is a comprehensive systematic review conducted according to PRISMA-NMA guidelines [23]. The process includes:
- Protocol registration with PROSPERO or similar platforms
- Systematic search across multiple databases with explicit search strategy
- Dual independent study selection and data extraction
- Assessment of risk of bias using tools like Cochrane RoB 2
- Evaluation of transitivity by examining distribution of effect modifiers across treatment comparisons
Statistical Analysis and Model Implementation
NMA statistical implementation involves several key decisions:
- Choice of statistical model: Fixed-effect vs. random-effects models based on heterogeneity assessment
- Handling of multi-arm trials: Appropriate modeling to account for correlation between interventions from the same trial
- Zero-cell corrections: Methods to handle sparse data with zero events
- Assessment of inconsistency: Statistical evaluation of differences between direct and indirect evidence using node-splitting or design-by-treatment interaction models
- Convergence diagnostics: For Bayesian NMAs, evaluation of model convergence using R-hat statistics and effective sample sizes [18]
Certainty of Evidence Assessment
The GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) approach for NMA provides a systematic framework for rating confidence in effect estimates [85]. Assessment domains include:
- Risk of bias in included studies
- Imprecision of effect estimates
- Heterogeneity and inconsistency between studies
- Indirectness of evidence to the research question
- Publication bias and other reporting biases
- Incoherence between direct and indirect evidence
Evidence certainty is rated as high, moderate, low, or very low, with potential rating downgrades based on limitations in these domains [85].
Translating NMA Findings to Health Policy and Guidelines
From Evidence to Recommendations
Incorporating NMA findings into clinical practice guidelines and health policy requires consideration of multiple factors beyond efficacy:
- Balance of benefits and harms: Quantitative integration of efficacy and safety outcomes
- Certainty of evidence: Confidence in effect estimates based on GRADE assessment
- Patient values and preferences: Consideration of outcome importance and risk tolerance
- Resource implications and cost-effectiveness: Economic evaluation of alternative interventions [87]
Cost-Effectiveness Analysis Integration
NMA provides comparative efficacy data essential for cost-effectiveness analysis (CEA), as demonstrated in a study of Cetuximab-β versus Cetuximab for metastatic colorectal cancer. The NMA showed comparable efficacy (OS HR: 1.10; 95% CI: 0.67-1.90) but a trend toward better safety for Cetuximab-β. Subsequent CEA found Cetuximab-β dominated standard Cetuximab, reducing costs by $12,005 with minimal QALY gain (0.10), resulting in a dominant incremental cost-effectiveness ratio [87].
Implementation Considerations
Successful implementation of NMA-informed recommendations requires:
- Stakeholder engagement: Involving clinicians, patients, and policymakers throughout guideline development
- Clear communication of NMA findings: Transparent presentation of benefits, harms, and evidence certainty
- Identification of research gaps: Prioritization of future studies based on network limitations and evidence gaps
- Contextual adaptation: Consideration of local resources, values, and healthcare system constraints
Essential Research Toolkit for NMA
Table 3: Research Reagent Solutions for Network Meta-Analysis
| Tool Category | Specific Tools/Software | Primary Function | Application Context |
|---|---|---|---|
| Statistical Software | R (netmeta, gemtc, BUGSnet) | NMA statistical implementation | Data analysis and model fitting |
| Bayesian Analysis | JAGS, WinBUGS, OpenBUGS | Bayesian model estimation | Complex random-effects models |
| Quality Assessment | Cochrane RoB 2, ROBINS-I | Risk of bias assessment | Study methodology evaluation |
| Evidence Grading | GRADE, CINeMA | Certainty of evidence rating | Results interpretation |
| Protocol Registration | PROSPERO | Systematic review registration | Protocol development |
| Reporting Guidelines | PRISMA-NMA | Reporting standards | Manuscript preparation |
Network meta-analysis represents a significant advancement in evidence synthesis, providing a robust methodological framework for comparing multiple interventions and informing clinical practice and health policy. Translating NMA findings into guidelines requires careful attention to methodological rigor, appropriate interpretation of results, and consideration of the broader clinical and policy context. As NMA methodologies continue to evolve, with ongoing updates to PRISMA-NMA guidelines and statistical approaches, their role in evaluating therapeutic equivalence and guiding healthcare decisions will expand accordingly. Researchers, clinicians, and policymakers must maintain critical appraisal skills to effectively interpret and apply NMA findings to improve patient care and health outcomes.
Network meta-analysis (NMA) has emerged as a powerful statistical methodology that enables the simultaneous comparison of multiple interventions for a given condition, even when direct head-to-head comparisons are absent from the literature. By combining both direct evidence (from trials comparing interventions directly) and indirect evidence (through a common comparator), NMA provides a comprehensive framework for ranking treatments and informing healthcare decisions [88]. This methodology is particularly valuable in therapeutic equivalence research, where clinicians and policymakers need to understand the relative effectiveness and safety profiles of all available treatment options.
The fundamental principle of NMA lies in its ability to create a connected network of treatments. For example, if Treatment A has been compared to Treatment B in clinical trials, and Treatment B has been compared to Treatment C, an NMA can provide an indirect estimate for the comparison between Treatment A and Treatment C [88]. This network approach is graphically represented through network maps, where nodes represent treatments and connecting lines represent direct comparisons. The size of nodes typically corresponds to the number of patients receiving that treatment, while the thickness of connecting lines represents the number of trials available for that direct comparison [88].
However, the increased complexity of NMA introduces additional methodological challenges beyond those encountered in traditional pairwise meta-analysis. Two key concepts specific to NMA are transitivity and incoherence. Transitivity refers to the similarity of study characteristics across the network, ensuring that studies are sufficiently homogeneous to allow valid indirect comparisons. Incoherence (also called inconsistency) occurs when direct and indirect evidence for a particular comparison disagree beyond chance [88]. These methodological considerations are crucial when evaluating the credibility of NMA findings, particularly in therapeutic equivalence research where precise effect estimates are essential for informed decision-making.
The GRADE Framework for Network Meta-Analysis
Foundation and Evolution of GRADE
The Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) working group emerged in 2000 as an international collaboration aimed at addressing the shortcomings of existing evidence grading systems in healthcare [89]. GRADE provides a systematic and transparent approach for rating the certainty of evidence (also referred to as quality of evidence or confidence in effect estimates) and the strength of recommendations. Since its inception, GRADE has become the standard method used by numerous international organizations for guideline development and evidence assessment [89].
The application of GRADE to network meta-analysis represents an important methodological advancement. Originally developed for pairwise comparisons, the GRADE framework was extended to NMA in 2014, with subsequent refinements based on practical application experiences [90]. The fundamental principle of GRADE for NMA is that the certainty of evidence must be assessed separately for each pairwise comparison within the network, considering both the direct and indirect evidence that contribute to the network estimate [90].
GRADE defines the certainty of evidence as "the certainty that the true effect, accuracy measure, or association lies on one side of a particular threshold, or in a particular range" [89]. This conceptualization emphasizes the role of evidence certainty in decision-making contexts, particularly for therapeutic equivalence assessments where determining whether interventions perform similarly or differently has significant clinical implications.
Core GRADE Domains for Certainty Assessment
The GRADE approach evaluates certainty of evidence through eight key domains, five of which may lead to downgrading the evidence quality, while three may lead to upgrading [89]. These domains provide a systematic framework for assessing the limitations of evidence from NMA:
Risk of Bias: Assessment of methodological limitations in the primary studies contributing to the network estimate, including shortcomings in randomization, allocation concealment, blinding, incomplete outcome data, and selective reporting [91] [89].
Imprecision: Evaluation of whether the confidence interval around the effect estimate is sufficiently narrow to support a clear decision, considering the optimal information size and whether the estimate crosses the threshold for clinical decision-making [89].
Inconsistency: Assessment of variability in results across studies contributing to a particular comparison, including statistical heterogeneity and differences in point estimates or confidence intervals [89].
Indirectness: Determination of how directly the available evidence addresses the research question, considering differences in populations, interventions, comparisons, and outcomes [89].
Publication Bias: Evaluation of the potential for unpublished studies or selective outcome reporting to distort the evidence base [89].
Factors that may lead to upgrading the certainty of evidence include large magnitude of effect, dose-response relationships, and effect estimates that remain consistent despite plausible confounding factors that would typically reduce the observed effect [89].
Table 1: Core GRADE Domains for Assessing Certainty of Evidence in NMA
| Domain | Assessment Focus | Considerations for NMA |
|---|---|---|
| Risk of Bias | Methodological limitations of individual studies | Evaluate bias across all studies contributing to direct and indirect evidence |
| Imprecision | Width of confidence intervals and sample size | Consider optimal information size for each pairwise comparison |
| Inconsistency | Variability in results across studies | Assess heterogeneity within direct and indirect evidence sources |
| Indirectness | Directness of evidence to research question | Evaluate population, intervention, comparator, and outcome similarities across network |
| Publication Bias | Potential for missing studies | Assess for missing studies that might alter network connectivity or effect estimates |
| Large Effect | Magnitude of treatment effect | Unusually large effects may increase confidence in estimate |
| Dose-Response | Presence of dose-response gradient | Consistent pattern of increasing effect with increasing dose |
| Plausible Confounding | Effect of confounding factors | Evidence remains robust despite plausible confounding |
Conceptual Advances in GRADE for NMA
Recent methodological work has refined the application of GRADE to NMA, resulting in four significant conceptual advances that improve efficiency and strengthen the conceptual foundation [90]:
First, consideration of imprecision is not necessary when rating the direct and indirect estimates separately to inform the rating of NMA estimates. Instead, imprecision should be evaluated directly for the network estimate, streamlining the assessment process without compromising rigor [90].
Second, there is no need to rate the indirect evidence when the certainty of the direct evidence is high and the contribution of the direct evidence to the network estimate is at least as great as that of the indirect evidence. This principle recognizes that when high-quality direct evidence dominates the network estimate, exhaustive assessment of indirect evidence may not be necessary [90].
Third, a statistical test of global incoherence of the network should not be trusted to assess incoherence at the pairwise comparison level. Global tests may miss important local inconsistencies, and therefore assessment of incoherence should focus on specific comparisons of interest [90].
Fourth, in the presence of incoherence between direct and indirect evidence, the certainty of the evidence of each estimate can help decide which estimate to believe. When direct and indirect estimates disagree, the higher certainty evidence should be prioritized. If both have similar certainty, the network estimate may still be used but should be downgraded for incoherence [90].
Practical Application of GRADE in NMA
Structured Approach to Certainty Assessment
Implementing the GRADE approach for NMA requires a systematic, sequential process to ensure comprehensive and consistent assessment across all comparisons in the network. The following workflow provides a structured approach:
Define the Network Structure: Clearly map all interventions and their connections, identifying which comparisons are informed by direct evidence, indirect evidence, or both [88].
Assess Certainty of Direct Comparisons: For each pairwise comparison with direct evidence, apply standard GRADE criteria for risk of bias, imprecision, inconsistency, indirectness, and publication bias [90] [89].
Assess Certainty of Indirect Comparisons: For comparisons informed solely by indirect evidence, evaluate the certainty based on the weakest link in the indirect comparison pathway, while also considering the coherence of the network [90].
Determine Network Estimates and Their Certainty: Calculate network estimates for all comparisons and rate their certainty, considering the contributions of both direct and indirect evidence, and applying the conceptual advances described in section 2.3 [90].
Address Incoherence: Formally assess for disagreement between direct and indirect evidence where both exist, and adjust certainty ratings accordingly [90] [88].
Present Results Transparently: Use GRADE evidence profiles or summary of findings tables to present both the network estimates and their associated certainty for all critical and important outcomes [89].
The following diagram illustrates the logical workflow for applying GRADE to NMA:
Critical Appraisal of NMA Using Systematic Frameworks
Beyond GRADE, several structured frameworks exist for the critical appraisal of network meta-analyses, ensuring comprehensive assessment of methodological rigor and credibility of findings. These frameworks are particularly important in therapeutic equivalence research, where conclusions directly impact treatment decisions and resource allocation.
The ISPOR (International Society for Pharmacoeconomics and Outcomes Research) checklist provides a comprehensive set of items for evaluating NMA methodology [92]. Key domains include:
- Rationale and Objectives: Clarity of clinical question and study objectives [92]
- Methods Rigor: Comprehensive literature search, explicit eligibility criteria, systematic study selection, appropriate data extraction, and risk of bias assessment of individual studies [92]
- Analysis Methods: Appropriate statistical models, handling of potential biases and inconsistency, and sensitivity analyses [92]
- Results Presentation: Clear summary of included studies, network structure, and evidence synthesis results [92]
- Interpretation: Discussion of findings' internal and external validity, and implications for decision-makers [92]
An alternative framework organizes critical appraisal around three fundamental questions [93]:
Are the results valid? Examining the clinical relevance of the question, comprehensiveness of literature search, and potential biases in primary studies [93]
What are the results? Assessing the amount of evidence in the network, consistency across studies, agreement between direct and indirect comparisons, treatment effects and rankings, and robustness of findings [93]
How can I apply the results to patient care? Evaluating whether all patient-important outcomes and treatment options were considered, credibility of subgroup effects, and overall quality and limitations of evidence [93]
Table 2: Comparison of Critical Appraisal Frameworks for Network Meta-Analysis
| Appraisal Domain | GRADE Approach | ISPOR Checklist | Three-Question Framework |
|---|---|---|---|
| Question Formulation | Explicit PICO required | Clear rationale and objectives | Sensible clinical question |
| Evidence Identification | Systematic review foundation | Exhaustive search documented | Exhaustive search for evidence |
| Study Quality Assessment | Risk of bias using GRADE domains | Validity assessment of individual studies | Evaluation of major biases |
| Synthesis Methods | NMA with direct/indirect integration | Appropriate analysis methods described | Appropriate analysis methods |
| Incoherence Assessment | Formal evaluation of direct/indirect disagreement | Handling of inconsistency | Consistency between direct/indirect |
| Certainty Assessment | Explicit rating (high to very low) | Not explicitly addressed | Overall quality of evidence |
| Results Application | Evidence to Decision frameworks | Implications for target audience | Application to patient care |
Methodological Protocols and Research Reagents
Essential Methodological Protocols for NMA
Implementing a methodologically sound NMA with GRADE assessment requires adherence to established protocols across several key stages:
Literature Search and Study Selection Protocol:
- Develop comprehensive search strategies across multiple databases (MEDLINE, EMBASE, Cochrane Central)
- Implement duplicate screening process with predefined eligibility criteria
- Document the study selection process using PRISMA flow diagrams
- Resolve conflicts through consensus or third-party adjudication [91]
Data Extraction and Management Protocol:
- Use standardized, piloted data extraction forms
- Extract data in duplicate with verification procedures
- Collect detailed information on study characteristics, participants, interventions, comparators, outcomes, and study design
- Document key sources of clinical and methodological diversity [91]
Risk of Bias Assessment Protocol:
- Select appropriate risk of bias tools based on study designs (e.g., Cochrane RoB 2 for randomized trials)
- Train assessors in tool application and conduct calibration exercises
- Conduct assessments independently by at least two reviewers
- Implement procedures for resolving disagreements [91]
Statistical Analysis Protocol:
- Pre-specify statistical models (fixed vs. random effects) and justification
- Document approaches for handling multi-arm trials
- Plan assessment of heterogeneity and inconsistency
- Prescribe methods for treatment ranking and evaluation of uncertainty [88]
GRADE Assessment Protocol:
- Define critical and important outcomes for decision-making
- Establish processes for rating each GRADE domain
- Develop rules for determining overall certainty ratings
- Plan sensitivity analyses exploring impact of methodological choices [90] [89]
Research Reagent Solutions for NMA
Conducting a high-quality NMA with GRADE assessment requires both methodological expertise and specialized analytical tools. The following table outlines essential "research reagents" – the conceptual and practical tools needed for rigorous NMA implementation:
Table 3: Essential Research Reagent Solutions for Network Meta-Analysis
| Research Reagent | Function/Application | Implementation Examples |
|---|---|---|
| Systematic Review Software | Facilitate literature screening and data management | Covidence, Rayyan, DistillerSR |
| Risk of Bias Tools | Standardized assessment of methodological quality of primary studies | Cochrane RoB 2, ROBINS-I, Newcastle-Ottawa Scale [91] |
| Statistical Analysis Packages | Perform network meta-analysis and generate estimates | R (netmeta, gemtc), Stata (network group), WinBUGS/OpenBUGS |
| GRADE Assessment Tools | Structured approach for rating certainty of evidence | GRADEpro GDT, electronic GRADE worksheets [89] |
| Network Visualization Tools | Create network graphs depicting evidence structure | R (igraph, networkD3), Stata, Python (networkX) |
| Incoherence Assessment Methods | Evaluate consistency between direct and indirect evidence | Side-splitting methods, node-splitting approaches, design-by-treatment interaction model [90] |
| Evidence to Decision Frameworks | Structure development of recommendations based on evidence | GRADE EtD framework [89] |
The integration of the GRADE framework within network meta-analysis represents a significant methodological advancement in evidence-based medicine, particularly for therapeutic equivalence research. By providing a systematic and transparent approach to assessing the certainty of evidence from complex networks of treatment comparisons, GRADE enhances the credibility and utility of NMA findings for clinical and policy decision-making.
The conceptual advances in GRADE for NMA – including streamlined assessment of imprecision, efficient evaluation of indirect evidence, focused assessment of local incoherence, and guidance for handling discrepant direct and indirect estimates – have strengthened the methodological foundation while maintaining rigor [90]. When combined with structured critical appraisal frameworks such as the ISPOR checklist or the three-question approach, researchers and clinicians are equipped with comprehensive tools to evaluate, interpret, and apply NMA findings appropriately [93] [92].
For therapeutic equivalence research in drug development, the rigorous application of GRADE to NMA provides decision-makers with clearer understanding of the strength of evidence supporting comparative effectiveness claims. This is particularly important when evaluating whether interventions can be considered therapeutically equivalent or when making choices between multiple active treatments. As evidence synthesis methods continue to evolve, the integration of GRADE principles will remain essential for ensuring that healthcare decisions are informed by the most reliable evidence, appropriately contextualized for specific clinical scenarios and patient populations.
Conclusion
Network meta-analysis provides a powerful, evidence-based framework for evaluating therapeutic equivalence and establishing treatment hierarchies, directly informing drug development and clinical decision-making. The key to robust NMA lies in rigorously assessing its foundational assumptions, appropriately handling statistical uncertainty, and transparently reporting limitations. Future directions will involve integrating individual patient data, developing standardized methods for complex treatment sequences, and refining approaches for real-world evidence incorporation. As therapeutic landscapes grow more complex, NMA will remain crucial for determining not just whether treatments are different, but whether they are meaningfully equivalent for specific patient populations and clinical contexts.
References
- 1. From Molecule to Market: The Generic Drug Development ... [https://www.drugpatentwatch.com/blog/from-molecule-to-market-the-generic-drug-development-process-explained/?srsltid=AfmBOopzEh_zoGZsfMM_wwmVOEypbQJUyFZ5QBE4C3aOz076c--00BhW]
- 2. What is network meta-analysis? [https://www.quantics.co.uk/blog/what-is-network-meta-analysis/]
- 3. A Comparison of National Guidelines for Network Meta ... [https://www.sciencedirect.com/science/article/pii/S1098301514018841]
- 4. Network meta-analysis for comparative effectiveness of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8634013/]
- 5. Research Techniques Made Simple: Network Meta-Analysis [https://www.sciencedirect.com/science/article/pii/S0022202X18327933]
- 6. Chapter 11: Undertaking network meta-analyses [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-11]
- 7. Network meta-analysis: a powerful tool for clinicians ... [https://www.sciencedirect.com/science/article/pii/S0895435624002932]
- 8. Network Meta-analysis to Synthesize Evidence for Decision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4845707/]
- 9. 5 Tips For Understanding Network Meta-Analysis [https://absolutelymaybe.plos.org/2024/02/01/5-tips-for-understanding-network-meta-analysis/]
- 10. A methodological review of network meta-analyses applied ... [https://www.sciencedirect.com/science/article/pii/S0895435625001891]
- 11. Using information from network meta-analyses to optimize ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9682784/]
- 12. and arm-synthesis models for network meta-analysis [https://www.cambridge.org/core/journals/research-synthesis-methods/article/an-investigation-of-the-impact-of-using-contrast-and-armsynthesis-models-for-network-metaanalysis/8211C05BD2A2E70CE0742EFC70B23EF4]
- 13. The statistical importance of a study for a network meta- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7386174/]
- 14. Methods for information-sharing in network meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527489/]
- 15. A Network Meta-Analysis of Quality of Life in Heart Failure ... [https://www.medrxiv.org/content/10.1101/2025.03.12.25323680v1.full-text]
- 16. Meta-Analysis Pharmacologic Treatment of Heart Failure ... [https://www.sciencedirect.com/science/article/pii/S0735109725075722]
- 17. Network metaâ€analysis of medical therapy efficacy in more ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9546056/]
- 18. Network Meta-Analysis of Pharmacological Therapies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12185836/]
- 19. Comparing Long-Term HAE Treatments: Insights from a ... [https://www.eversana.com/insights/comparing-long-term-hae-treatments-insights-from-a-robust-network-meta-analysis/]
- 20. a systematic review and network meta-analysis of randomized ... [https://ojrd.biomedcentral.com/articles/10.1186/s13023-025-03735-y]
- 21. NMA — PRISMA statement [https://www.prisma-statement.org/nma]
- 22. The PRISMA extension statement for reporting of ... [https://pubmed.ncbi.nlm.nih.gov/26030634/]
- 23. Update to the PRISMA guidelines for network meta-analyses and scoping reviews and development of guidelines for rapid reviews: a scoping review protocol - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11892999/]
- 24. The PRISMA Extension Statement for Reporting ... [https://www.equator-network.org/reporting-guidelines/prisma-extension-network-meta-analyses/]
- 25. MetaInsight: An interactive webâ€based tool for analyzing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6973101/]
- 26. Updating the PRISMA reporting guideline for network meta-analysis: a scoping review - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S089543562500318X]
- 27. An updated guideline for reporting systematic reviews [https://www.equator-network.org/reporting-guidelines/prisma/]
- 28. a feasibility assessment of indirect treatment comparisons [https://pubmed.ncbi.nlm.nih.gov/40321129/]
- 29. a feasibility assessment of indirect treatment comparisons - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12142382/]
- 30. Achieving Better Results with Gantt Charts for Research. [https://www.instagantt.com/project-management/gantt-chart-for-research-projects]
- 31. Gantt Chart [https://digital.ahrq.gov/health-it-tools-and-resources/evaluation-resources/workflow-assessment-health-it-toolkit/all-workflow-tools/gantt-chart]
- 32. Frequentist vs. Bayesian methods: Choosing appropriate ... [https://www.sciencedirect.com/science/article/abs/pii/S2772766125000771]
- 33. Frequentist vs. Bayesian: Comparing Statistics Methods for ... [https://amplitude.com/blog/frequentist-vs-bayesian-statistics-methods]
- 34. A Bayesian Mixed Treatment Comparisons Meta-Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4318856/]
- 35. Theory and practice of Bayesian and frequentist ... [https://pubmed.ncbi.nlm.nih.gov/35760451/]
- 36. Comparative study of Bayesian and Frequentist methods ... [https://arxiv.org/abs/2509.05846]
- 37. Evaluating the performance of Bayesian and frequentist ... [https://www.nature.com/articles/s41598-022-18129-4]
- 38. A Combined Bayesian and Frequentist Network Meta- ... [https://pubmed.ncbi.nlm.nih.gov/38184425/]
- 39. Chapter 12 Network Meta-Analysis [https://bookdown.org/MathiasHarrer/Doing_Meta_Analysis_in_R/netwma.html]
- 40. What's the Risk: Differentiating Risk Ratios, Odds Ratios, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7515812/]
- 41. Risk Ratios vs. Odds Ratios vs. Hazard Ratios - Editage [https://www.editage.com/blog/risk-ratios-odds-ratios-and-hazard-ratios-for-biomedical-researchers/]
- 42. Credibility Intervals - bayesian - Cross Validated [https://stats.stackexchange.com/questions/49671/credibility-intervals]
- 43. Network Meta-analysis in R part 1 - by Darko Medin [https://darkomedin.com/network-meta-analysis-in-r1]
- 44. Extensions of the probabilistic ranking metrics of competing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7078966/]
- 45. Ranking treatments in frequentist network meta-analysis ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-015-0060-8]
- 46. Predictive P-score for treatment ranking in Bayesian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8520624/]
- 47. SUCRA [https://examine.com/glossary/sucra/?srsltid=AfmBOopFBO5xarwSFRPx0_Rvwd16eT4nyRME91V7ZMyKKhJgD6gVyI6R]
- 48. Data visualisation approaches for component network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10502971/]
- 49. A systematic review and network meta-analysis of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8487311/]
- 50. Safety outcomes when switching between biosimilars and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10547155/]
- 51. A Framework for Evidence Synthesis of Clinical Trial Data [https://pmc.ncbi.nlm.nih.gov/articles/PMC4999602/]
- 52. Incorporating external evidence on betweenâ€trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6492109/]
- 53. Orange Book Preface [https://www.fda.gov/drugs/development-approval-process-drugs/orange-book-preface]
- 54. Therapeutic Equivalence - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/therapeutic-equivalence]
- 55. Using information from network meta-analyses to optimize the ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-022-01792-6]
- 56. Multicriteria benefit–risk assessment using network meta ... [https://www.sciencedirect.com/science/article/pii/S0895435611002812]
- 57. Introduction to network meta-analysis: understanding what ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11879513/]
- 58. Rules for risk-averse decision-makers [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527546/]
- 59. Risk preferences over health: Empirical estimates and ... [https://www.sciencedirect.com/science/article/pii/S016762962400002X]
- 60. rules for risk-averse decision-makers [https://www.medrxiv.org/content/10.1101/2024.07.01.24309758v1]
- 61. E E seminar - Tony Ades - Oct 2025 [https://www.york.ac.uk/che/events-and-seminars/events-seminars-2025/tony-ades/]
- 62. Network meta-analysis: a technique to gather evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5386629/]
- 63. Interpreting and assessing confidence in network meta- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9338903/]
- 64. a Bayesian network meta-analysis of randomised controlled rials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530399/]
- 65. Comparing models using the deviance and log-likelihood ... [https://stats.stackexchange.com/questions/237702/comparing-models-using-the-deviance-and-log-likelihood-ratio-tests]
- 66. How to Interpret Null & Residual Deviance (With Examples) [https://www.statology.org/null-residual-deviance/]
- 67. Deviance – Knowledge and References [https://taylorandfrancis.com/knowledge/Engineering_and_technology/Engineering_support_and_special_topics/Deviance/]
- 68. A comparison of residual diagnosis tools for diagnosing ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-020-01055-2]
- 69. Convergence and efficiency diagnostics for Markov Chains [https://mc-stan.org/rstan/reference/Rhat.html]
- 70. Understanding the R-hat Statistic | by 1749.io [https://medium.com/@nialloulton/understanding-the-r-hat-statistic-d83b3b5ca162]
- 71. Sensitivity Analyses for Network Meta-Analyses - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK524937/]
- 72. Node-Splitting Generalized Linear Mixed Models for ... [https://www.sciencedirect.com/science/article/pii/S1098301516305812]
- 73. Automated generation of nodeâ€splitting models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5057346/]
- 74. How robust are findings of pairwise and network meta ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-021-02195-y]
- 75. Chapter 10: Analysing data and undertaking meta-analyses [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-10]
- 76. Sensitivity to excluding treatments in network meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4892976/]
- 77. Node-splitting model for testing consistency at the treatment ... [https://hugaped.github.io/MBNMAdose/reference/nma.nodesplit.html]
- 78. Understanding Network Metaâ€Analysis: A Practical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271649/]
- 79. NMA: Network meta-analysis based on multivariate ... [https://www.medrxiv.org/content/10.1101/2025.09.15.25335823v1.full-text]
- 80. Path-Based Approach for Detecting and Assessing ... [https://arxiv.org/abs/2506.20364]
- 81. A network meta-analysis of the safety of systemic treatments in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498157/]
- 82. Comparing the safety and efficacy of systemic therapies for ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1638405/full]
- 83. Comparing the safety and efficacy of systemic therapies for ... [https://pubmed.ncbi.nlm.nih.gov/40951348/]
- 84. Metastatic Prostate Cancer—A Review of Current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9856730/]
- 85. A clinician's guide to network meta-analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9307840/]
- 86. A Network Meta-Analysis of Efficacy and Safety Across 22 ... [https://www.mdpi.com/1424-8247/18/10/1455]
- 87. Network meta-analysis and cost-effectiveness ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1568385/full]
- 88. A clinician's guide to network meta-analysis | Eye [https://www.nature.com/articles/s41433-022-01943-5]
- 89. GRADE home [https://www.gradeworkinggroup.org/]
- 90. Advances in the GRADE approach to rate the certainty in ... [https://pubmed.ncbi.nlm.nih.gov/29051107/]
- 91. Critical Appraisal - Systematic Reviews and Meta-Analyses [https://guides.lib.vt.edu/SRMA/appraisal]
- 92. Table 6, Critical Appraisal of Network Meta-Analysis ... [https://www.ncbi.nlm.nih.gov/books/NBK562922/table/rc1233.app3.tab1/?report=objectonly]
- 93. Table 1 Critical appraisal guide for a Network Meta-Analysis[85] [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/2046-4053-2-18/tables/1]