Bayesian Mixed Treatment Comparisons: A Comprehensive Guide for Evidence Synthesis in Drug Development
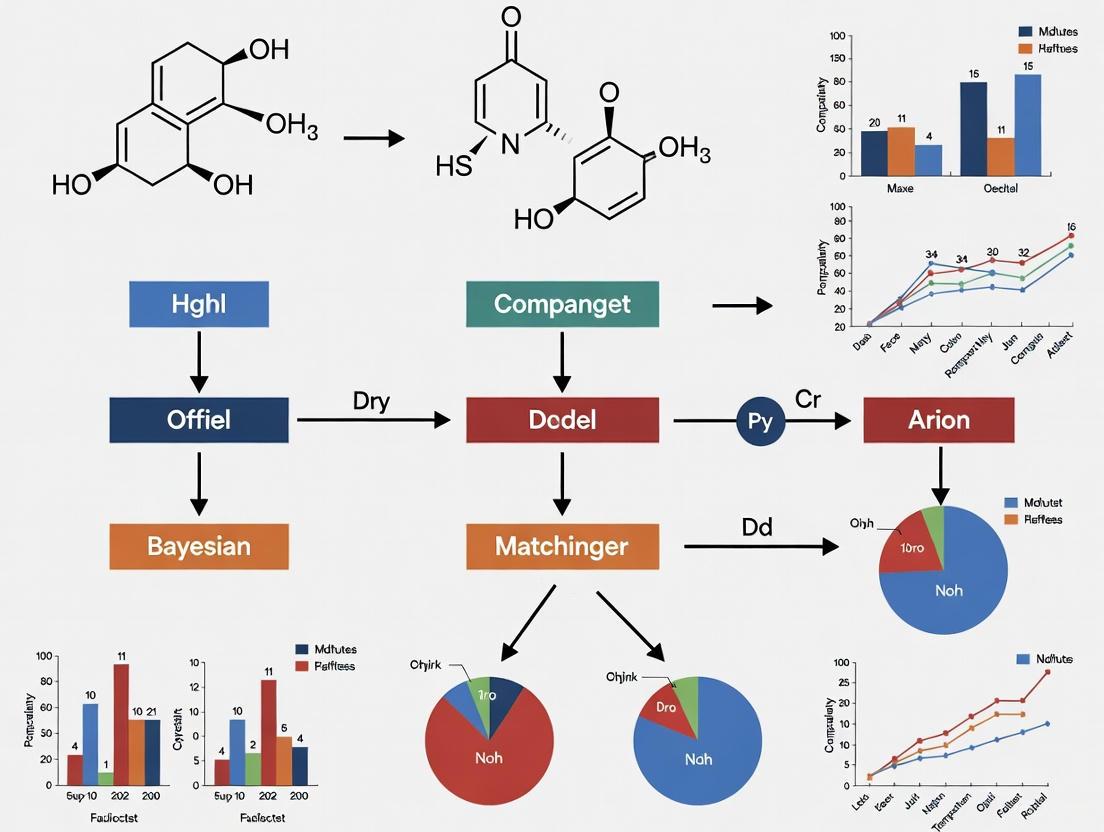
This article provides a comprehensive guide to applying Bayesian models for Mixed Treatment Comparisons (MTC), also known as Network Meta-Analysis, in biomedical and pharmaceutical research.
Bayesian Mixed Treatment Comparisons: A Comprehensive Guide for Evidence Synthesis in Drug Development
Abstract
This article provides a comprehensive guide to applying Bayesian models for Mixed Treatment Comparisons (MTC), also known as Network Meta-Analysis, in biomedical and pharmaceutical research. It covers foundational concepts, including the transitivity and consistency assumptions essential for valid MTC. The guide details methodological implementation using Bayesian hierarchical models, Markov Chain Monte Carlo estimation, and treatment ranking procedures. It addresses common challenges like outcome reporting bias, heterogeneous populations, and complex evidence networks, offering practical troubleshooting strategies. Finally, it compares Bayesian and frequentist approaches, demonstrating how Bayesian methods provide more intuitive probabilistic results for clinical decision-making. This resource is tailored for researchers, scientists, and drug development professionals seeking to leverage advanced evidence synthesis for personalized medicine and robust treatment recommendations.
Core Principles and Assumptions of Bayesian Mixed Treatment Comparisons
Network meta-analysis (NMA), also referred to as multiple treatment comparison (MTC) or mixed treatment comparison, represents an advanced statistical methodology that synthesizes evidence from multiple studies evaluating three or more interventions [1] [2] [3]. This approach extends beyond conventional pairwise meta-analysis by enabling simultaneous comparison of multiple treatments within a unified statistical framework, even for interventions that have never been directly compared in head-to-head clinical trials [4] [3].
The fundamental advancement of NMA lies in its ability to incorporate both direct evidence (from head-to-head comparisons within trials) and indirect evidence (estimated through common comparators) to derive comprehensive treatment effect estimates across all interventions in the network [4] [3]. This methodology provides clinicians, researchers, and policymakers with a powerful tool for determining comparative effectiveness and safety profiles across all available interventions for a specific condition, thereby informing evidence-based decision-making in healthcare [2] [4].
Statistical Foundations and Framework
Core Conceptual Framework
The statistical foundation of network meta-analysis rests upon the integration of direct and indirect evidence through connected networks of randomized controlled trials (RCTs) [2]. A connected network requires that each intervention is linked to every other intervention through a pathway of direct comparisons, forming what is visually represented as a network plot or graph [3]. In these visual representations, nodes (typically circles) represent interventions, while lines connecting them represent available direct comparisons from clinical trials [3].
NMA operates under several key assumptions that extend beyond those required for standard pairwise meta-analysis. The transitivity assumption requires that studies comparing different sets of treatments are sufficiently similar in their clinical and methodological characteristics to permit valid indirect comparisons [2]. The consistency assumption (sometimes called coherence) posits that direct and indirect evidence within the network are in agreement—that is, the effect estimates derived from direct comparisons align statistically with those obtained through indirect pathways [3].
Bayesian versus Frequentist Approaches
Network meta-analysis can be implemented through two primary statistical frameworks: Bayesian and frequentist methods [1]. While both approaches can yield similar results with large sample sizes, they differ fundamentally in their philosophical foundations and computational implementation [1].
The Bayesian framework incorporates prior probability distributions along with the likelihood from observed data to generate posterior distributions for parameters of interest [1] [5]. This approach calculates the probability that a research hypothesis is true by combining information from the current data with previously known information (prior probability) [1]. The Bayesian method is particularly advantageous for NMA as it does not rely on large sample assumptions, can incorporate prior clinical knowledge, and naturally produces probability statements about treatment rankings [1] [5]. Key components of Bayesian analysis include:
- Prior distributions: Represent pre-existing knowledge or beliefs about parameters before observing the current data [1] [5]
- Likelihood function: Reflects the probability of the observed data given the parameters [5]
- Posterior distributions: Represent updated knowledge about parameters after combining prior distributions with the observed data [1] [5]
In contrast, the frequentist approach determines whether to accept or reject a research hypothesis based on significance levels (typically p < 0.05) and confidence intervals derived solely from the observed data, without incorporating external information [1]. Frequentist methods compute the probability of obtaining the observed data (or more extreme data) assuming the null hypothesis is true, based on the concept of infinite repetition of the experiment [1].
Table 1: Comparison of Bayesian and Frequentist Approaches to NMA
| Feature | Bayesian Approach | Frequentist Approach |
|---|---|---|
| Philosophical Basis | Probabilistic; parameters as random variables | Fixed parameters; repeated sampling framework |
| Prior Information | Explicitly incorporated via prior distributions | Not incorporated |
| Result Interpretation | Posterior probability distributions for parameters | Point estimates with confidence intervals and p-values |
| Treatment Rankings | Direct probability statements (e.g., SUCRA values) | Based on point estimates |
| Computational Methods | Markov chain Monte Carlo (MCMC) simulation | Maximum likelihood or method of moments |
| Handling Complexity | Flexible for complex models and hierarchical structures | May have limitations with complex random-effects structures |
Bayesian Hierarchical Model for NMA
The Bayesian hierarchical model forms the statistical backbone for Bayesian network meta-analysis [5]. For a random-effects NMA, the model can be specified as follows:
For each study ( k ) comparing treatments ( a ) and ( b ), the observed effect size ( Y{kab} ) (e.g., log odds ratio, mean difference) is assumed to follow a normal distribution: [ Y{kab} \sim \mathcal{N}(\delta{kab}, sk^2) ] where ( \delta{kab} ) represents the underlying true treatment effect of ( a ) versus ( b ) in study ( k ), and ( sk^2 ) is the within-study variance [5].
The study-specific true effects ( \delta{kab} ) are assumed to follow a common distribution for each comparison: [ \delta{kab} \sim \mathcal{N}(d{ab}, \tau^2) ] where ( d{ab} ) represents the mean treatment effect for comparison ( a ) versus ( b ), and ( \tau^2 ) represents the between-study heterogeneity, assumed constant across comparisons [5].
The core of the NMA model lies in the connection between various treatment comparisons through consistency assumptions: [ d{ab} = d{1a} - d{1b} ] where ( d{1a} ) and ( d_{1b} ) represent the effects of treatments ( a ) and ( b ) relative to a common reference treatment (typically treatment 1) [5].
For multi-arm trials (trials with more than two treatment groups), the model accounts for the correlation between treatment effects within the same study by assuming the effects follow a multivariate normal distribution [5].
Experimental Protocols and Methodological Workflow
Protocol Development for NMA
Implementing a robust network meta-analysis requires meticulous planning and execution according to established methodological standards. The following workflow outlines the key stages in conducting a Bayesian NMA:
Detailed Methodological Components
Systematic Literature Review and Data Collection
The foundation of any valid NMA is a comprehensive systematic review following established guidelines (e.g., Cochrane Handbook) [2] [3]. This process should include:
- Explicit eligibility criteria defining populations, interventions, comparators, outcomes, and study designs (PICOS framework)
- Comprehensive search strategy across multiple electronic databases and clinical trial registries
- Dual independent study selection and data extraction to minimize bias
- Assessment of risk of bias in individual studies using validated tools (e.g., Cochrane Risk of Bias tool)
- Data extraction of study characteristics, patient demographics, and outcome data
Network Geometry and Connectivity
A crucial step in NMA is visualizing and evaluating the network structure [3]. The network plot should be created to illustrate:
- Nodes representing each intervention, with size potentially proportional to the number of patients or studies
- Edges representing direct comparisons, with thickness potentially proportional to the number of studies or precision
- Connectivity ensuring all interventions are connected through direct or indirect pathways
Model Implementation using Bayesian Methods
The Bayesian NMA model is typically implemented using Markov chain Monte Carlo (MCMC) methods, which iteratively sample from the posterior distributions of model parameters [1] [5]. The process involves:
- Specification of prior distributions for basic parameters (typically vague or weakly informative priors)
- Model fitting using MCMC algorithms (e.g., Gibbs sampling)
- Convergence diagnostics to ensure MCMC chains have reached the target posterior distribution (using statistics like Gelman-Rubin diagnostic)
- Posterior inference based on a sufficient number of post-convergence iterations
Table 2: Key Software Packages for Bayesian Network Meta-Analysis
| Software/Package | Description | Key Features | Implementation |
|---|---|---|---|
| R package 'gemtc' | Implements Bayesian NMA using MCMC | Hierarchical models, treatment rankings, consistency assessment | R interface with JAGS |
| JAGS/OpenBUGS | MCMC engine for Bayesian analysis | Flexible model specification, various distributions | Standalone or through R |
| R package 'netmeta' | Frequentist approach to NMA | Graph-theoretical methods, net league tables | R |
| R2WinBUGS | Interface between R and WinBUGS | Allows running BUGS models from R | R to WinBUGS connection |
Analytical Implementation and Diagnostic Evaluation
Bayesian Computation and MCMC Simulation
The implementation of Bayesian NMA relies heavily on Markov chain Monte Carlo (MCMC) simulation methods, which numerically approximate the posterior distributions of model parameters [1]. The MCMC process involves:
- Initialization: Starting with initial values for all parameters
- Iterative sampling: Generating sequences of parameter values through a Markov process
- Burn-in period: Discarding initial iterations before the chain reaches stationarity
- Convergence assessment: Verifying that multiple chains with different starting values yield similar posterior distributions
- Posterior inference: Using post-convergence iterations to summarize posterior distributions (means, medians, credible intervals)
The MCMC algorithm effectively performs what can be conceptualized as a "reverse calculation" of the area under complex posterior distribution functions that may not follow standard statistical distributions [1].
Model Diagnostics and Assumption Verification
Critical evaluation of NMA outputs requires comprehensive diagnostic assessments:
Heterogeneity and Consistency Assessment
- Heterogeneity estimation: Evaluating between-study variance (τ²) across the network
- Local inconsistency: Using node-splitting methods to assess disagreement between direct and indirect evidence for specific comparisons
- Global inconsistency: Employing design-by-treatment interaction models to assess consistency across the entire network
- Sensitivity analyses: Exploring the impact of different prior distributions, exclusion of high-risk studies, or alternative model assumptions
Model Fit and Comparison
- Residual deviance: Assessing discrepancies between observed data and model predictions
- Deviance Information Criterion (DIC): Comparing fit of different models (e.g., fixed vs. random effects, consistency vs. inconsistency models)
- Leverage and influence diagnostics: Identifying studies exerting disproportionate influence on network estimates
Interpretation and Application of NMA Results
Treatment Effects and Ranking Metrics
Bayesian NMA provides several outputs to inform clinical decision-making:
- Relative treatment effects with 95% credible intervals for all possible pairwise comparisons, including those without direct evidence
- Treatment rankings indicating the relative performance of each intervention for specific outcomes
- Rank probabilities showing the probability of each treatment being the best, second best, etc.
- Surface Under the Cumulative Ranking (SUCRA) values providing a numerical summary of ranking probabilities (ranging from 0 to 1, with higher values indicating better performance) [4]
Clinical and Policy Applications
The results of NMA directly inform evidence-based medicine and healthcare decision-making by:
- Identifying the most effective interventions across multiple outcomes (efficacy, safety, quality of life)
- Informing clinical practice guidelines with comprehensive comparative effectiveness evidence
- Guiding resource allocation and formulary decisions by healthcare systems
- Identifying evidence gaps for future research priorities
- Supporting health technology assessment and regulatory decision-making
Table 3: Interpretation of Key NMA Outputs for Clinical Decision-Making
| Output Metric | Interpretation | Clinical Utility |
|---|---|---|
| Relative Effect (95% CrI) | Estimated difference between treatments with uncertainty interval | Direct comparison of treatment efficacy/safety |
| Rank Probabilities | Probability of each treatment having specific rank (1st, 2nd, etc.) | Understanding uncertainty in treatment performance hierarchy |
| SUCRA Values | Numerical summary of overall ranking (0-1 scale) | Comparative performance metric across multiple outcomes |
| Between-Study Heterogeneity (τ²) | Estimate of variability in treatment effects across studies | Assessment of consistency of effects across different populations/settings |
| Node-Split P-values | Statistical test for direct-indirect evidence disagreement | Evaluation of network consistency and result reliability |
Advanced Considerations and Methodological Challenges
Addressing Complexity in Network Meta-Analysis
Advanced applications of NMA require careful consideration of several methodological challenges:
- Multi-arm trials: Properly accounting for correlation between treatment effects from trials with more than two intervention groups [5]
- Sparse networks: Interpretation challenges when limited direct evidence exists for specific comparisons
- Effect modifiers: Assessing and adjusting for clinical or methodological variables that may modify treatment effects across studies
- Scale and link functions: Selecting appropriate models for different outcome types (binary, continuous, time-to-event)
- Network geometry: Understanding how the structure of the evidence network influences the precision and reliability of indirect estimates
Reporting Standards and Transparency
Comprehensive reporting of NMA findings is essential for interpretation and critical appraisal. Key reporting elements include:
- Complete network description with network diagram and summary of available direct evidence
- Clear specification of statistical models, prior distributions, and computational methods
- Assessment and reporting of model fit, heterogeneity, and consistency
- Transparent presentation of all treatment comparisons with measures of uncertainty
- Sensitivity analyses exploring the impact of methodological assumptions and potential biases
The Bayesian framework for network meta-analysis represents a powerful advancement in evidence synthesis, enabling comprehensive comparison of multiple interventions through integration of direct and indirect evidence. When properly implemented with appropriate attention to methodological assumptions and statistical rigor, NMA provides invaluable information for healthcare decision-makers facing complex choices among multiple treatment options. The continued refinement of Bayesian methods for NMA promises to further enhance the reliability and applicability of this important methodology in evidence-based medicine.
Bayesian statistics is a powerful paradigm for data analysis that redefines probability as a degree of belief, treating parameters as random variables with probability distributions that reflect our uncertainty [6]. This contrasts with the frequentist view, where probability is a long-run frequency and parameters are fixed, unknown constants. The Bayesian framework allows for direct probability statements about parameters, such as "there is a 95% probability that the true mean lies between X and Y," aligning more closely with intuitive interpretations often mistakenly applied to frequentist confidence intervals [6].
The essence of the Bayesian paradigm lies in its iterative learning process, which follows a consistent logic: start with an initial belief (prior), gather data (likelihood), and combine these to form an updated belief (posterior). This process of belief updating is central to scientific inquiry and provides a coherent framework for learning from data across various applications in biostatistics, clinical research, and drug development [6].
Foundational Elements
Bayes' Theorem: The Core Engine
The mathematical foundation of Bayesian inference is Bayes' Theorem, a simple formula with profound implications for statistical reasoning and analysis [6]. The theorem is expressed as:
P(θ∣Data) = [P(Data∣θ) ⋅ P(θ)] / P(Data)
Where:
- P(θ∣Data) is the posterior distribution of parameters θ given the observed data
- P(Data∣θ) is the likelihood function of the data given parameters θ
- P(θ) is the prior distribution of parameters θ
- P(Data) is the marginal likelihood of the data
Often, the theorem is expressed proportionally as: Posterior ∠Likelihood × Prior [6]. This relationship highlights that the posterior distribution represents a compromise between our initial beliefs (prior) and what the new data reveals (likelihood).
Table 1: Components of Bayes' Theorem
| Component | Symbol | Description | Role in Inference |
|---|---|---|---|
| Posterior | P(θ∣Data) | Updated belief about parameters after observing data | Final inference, uncertainty quantification |
| Likelihood | P(Data∣θ) | Probability of observing data given specific parameters | Connects parameters to observed data |
| Prior | P(θ) | Initial belief about parameters before observing data | Incorporates existing knowledge or constraints |
| Marginal Likelihood | P(Data) | Overall probability of data across all parameter values | Normalizing constant, model evidence |
A Simple Biostatistical Example: Diagnostic Testing
Consider a new diagnostic test for a rare disease with a prevalence of 1 in 1000. The test has 99% sensitivity (P(Test Positive∣Has Disease) = 0.99) and 95% specificity (P(Test Negative∣No Disease) = 0.95) [6].
Using Bayes' Theorem, we calculate the probability that an individual actually has the disease given a positive test result:
P(Has Disease∣Test Positive) = [P(Test Positive∣Has Disease) ⋅ P(Has Disease)] / P(Test Positive)
P(Test Positive) = (0.99 ⋅ 0.001) + (0.05 ⋅ (1−0.001)) = 0.05094
P(Has Disease∣Test Positive) = (0.99 ⋅ 0.001) / 0.05094 ≈ 0.0194 or 1.94% [6]
This counterintuitive result—where a positive test from a highly accurate method yields only a 1.94% probability of having the disease—underscores the critical role of the prior (the disease prevalence) in Bayesian reasoning [6].
Table 2: Bayesian Methods Comparison in Clinical Research
| Method | Key Features | Applications | Advantages | Limitations |
|---|---|---|---|---|
| Power Priors | Weighted log-likelihood from historical data [7] | Incorporating historical controls, registry data | Straightforward implementation, intuitive weighting | Sensitivity to prior weight selection |
| Meta-Analytic-Predictive (MAP) Prior | Accounts for heterogeneity via random-effects meta-analysis [7] | Multi-regional clinical trials, borrowing across studies | Explicit modeling of between-trial heterogeneity | Requires exchangeability assumption |
| Commensurate Prior | Adaptively discounts historical data based on consistency [7] | Bayesian dynamic borrowing, real-world evidence incorporation | Robust to prior-data conflict | Computational complexity |
| Multi-Source Dynamic Borrowing (MSDB) Prior | Novel heterogeneity metric (PPCM), addresses baseline imbalance [7] | Incorporating multiple historical datasets (RCTs and RWD) | No exchangeability assumption, handles baseline imbalances | Complex implementation, computational intensity |
| Robust MAP Prior | Weakly informative component added to MAP prior [7] | Clinical trials with potential prior-data conflict | More effective discounting of conflicting data | Requires specification of robust mixture weight |
Table 3: MCMC Sampling Algorithms in Bayesian Analysis
| Algorithm | Mechanism | Convergence Diagnostics | Software Implementation | Best Use Cases |
|---|---|---|---|---|
| Metropolis-Hastings | Proposal-acceptance based on likelihood ratio [6] | Trace plots, acceptance rate | Stan, PyMC, custom code | General-purpose sampling, moderate dimensions |
| Gibbs Sampling | Iterative sampling from full conditional distributions [6] | Autocorrelation plots, Geweke diagnostic | JAGS, BUGS, PyMC | Hierarchical models, conjugate structures |
| Hamiltonian Monte Carlo (HMC) | Uses gradient information for efficient exploration [6] | Gelman-Rubin statistic (RÌ‚), E-BFMI | Stan (primary), PyMC | High-dimensional complex posteriors |
| No-U-Turn Sampler (NUTS) | Self-tuning variant of HMC [6] | Effective Sample Size (ESS), divergences | Stan (default), PyMC | Automated sampling, complex models |
Advanced Bayesian Protocols
Protocol: Multi-Source Dynamic Borrowing for Clinical Trials
The MSDB prior framework dynamically incorporates information from multiple historical sources (external RCTs and real-world data) while addressing baseline imbalances and heterogeneity [7].
Materials and Reagents:
- Current RCT dataset
- Historical clinical trial data
- Real-world data (registries, electronic health records)
- Statistical software with Bayesian capabilities (Stan, PyMC, or custom implementations)
Procedure:
Propensity Score Stratification
- Define propensity score as probability a patient belongs to current trial data using multinomial logistic regression: P(Study = Current∣X) [7]
- Estimate propensity scores using maximum likelihood estimation
- Create strata based on propensity score quantiles, ensuring approximately equal number of current RCT patients per stratum
- Trim external data patients falling outside propensity score range of current trial patients
Stratum-Specific Prior Construction
- Model patient survival times using piecewise exponential distribution within each time interval
- Assume total exposure time follows Gamma distribution with shape parameter as number of events and scale parameter as hazard rate
- Apply log transformation to hazard rates: log(λ) ~ Normal(μ, σ²) [7]
- Use weakly informative normal priors for μ with large variance (e.g., 1000)
Prior-Posterior Consistency Measurement
- Calculate PPCM metric to quantify consistency between prior information and observed data
- Compute posterior predictive probability function updated using prior information
- Measure predictive probability that is lower than current data [7]
- Use PPCM values to determine borrowing weights for historical data
Multi-Source Integration
- Merge prior distributions by considering heterogeneity between studies
- Dynamically adjust borrowing strength based on PPCM consistency measures
- Completely transform to non-informative prior when heterogeneity is excessive [7]
Validation:
- Compare performance using power, type I error, bias, and mean squared error across methods
- Application to case study (e.g., isatuximab in relapsed and refractory multiple myeloma) [7]
Protocol: Chaining Bayesian Inference with Empirical Priors
This protocol addresses situations where Bayesian inferences need to be chained on a data stream without analytic form of the posterior, using kernel density estimates from previous posterior draws [8].
Materials and Reagents:
- Sequence of datasets: (xâ‚, yâ‚), (xâ‚‚, yâ‚‚), …, (xâ‚™, yâ‚™)
- Posterior draws from previous analysis: θpost(1), …, θpost(M) ~ p(θ∣xâ‚, yâ‚)
- Computational resources for MCMC sampling
Procedure:
Initial Model Fitting
- Fit initial model p(θ, y∣x) to first dataset (xâ‚, yâ‚)
- Obtain posterior draws θpost(1), …, θpost(M) ~ p(θ∣xâ‚, yâ‚)
- Assume posterior draws can be shared across analyses [8]
Kernel Density Prior Construction
Efficient Metropolis Sampling
- Implement Metropolis sampling using only nearest neighbors of θ
- Utilize graph-enabled fast MCMC sampling for efficiency [8]
- Alternative: Use Stan for normal approximation implementation
Sequential Bayesian updating
- Use approximate posterior p(θ∣yâ‚, xâ‚) as prior for analyzing new data (xâ‚‚, yâ‚‚)
- Compute: p(θ∣xâ‚, xâ‚‚, yâ‚, yâ‚‚) ∠p(y₂∣θ, xâ‚‚) · p(θ∣yâ‚, xâ‚) [8]
- Continue chaining process for subsequent datasets
Considerations:
- Set variance parameter h to control prior concentration
- Determine optimal number of posterior draws M based on dimensionality
- Handle constrained parameters through appropriate transformations
- Compare with multivariate normal approximation approaches [8]
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for Bayesian Mixed Treatment Comparisons
| Reagent/Software | Function | Application Context | Key Features | Implementation Considerations |
|---|---|---|---|---|
| Stan | Probabilistic programming for Bayesian inference [6] | Complex hierarchical models, HMC sampling | NUTS sampler, differentiable probability functions | Requires programming expertise, good for complex models |
| JAGS/BUGS | MCMC sampling for Bayesian analysis [6] | Generalized linear models, conjugate models | Declarative language, automatic sampler selection | User-friendly, but less efficient for complex models |
| PyMC (Python) | Probabilistic programming framework [6] | Bayesian machine learning, custom distributions | Gradient-based inference, Theano/Aesara backend | Python ecosystem integration, growing community |
| RBesT | R Package for Bayesian Evidence Synthesis [8] | Meta-analytic-predictive priors, clinical trials | Pre-specified prior distributions, mixture normal approximations | Specialized for biostatistics, regulatory acceptance |
| brms | R Package for Bayesian regression models [6] | Multilevel models, formula interface | Stan backend, lme4-style syntax | User-friendly for R users, extensive model family support |
| Propensity Score Tools | Address baseline imbalances in historical data [7] | Incorporating real-world data, dynamic borrowing | Multinomial logistic regression, stratification | Essential for observational data incorporation |
| Geninthiocin | Geninthiocin, MF:C50H49N15O15S, MW:1132.1 g/mol | Chemical Reagent | Bench Chemicals | |
| 3-O-Acetylpomolic acid | 3-O-Acetylpomolic acid, MF:C32H50O5, MW:514.7 g/mol | Chemical Reagent | Bench Chemicals |
Applications in Mixed Treatment Comparisons
Bayesian methods provide particularly powerful approaches for mixed treatment comparisons (MTCs), also known as network meta-analysis, where the framework naturally handles complex evidence structures and uncertainty propagation.
Key Advantages for MTCs:
- Coherent Uncertainty Propagation: Bayesian methods naturally propagate uncertainty through all parameters in the network, providing more accurate confidence intervals for treatment effects [6]
- Flexible Hierarchical Modeling: Random-effects models can be implemented to account for heterogeneity across studies while maintaining network connectivity [7]
- Incorporation of Diverse Evidence: The MSDB framework enables borrowing of strength from real-world evidence and historical data while adjusting for baseline characteristics [7]
- Probabilistic Ranking: Direct computation of probability distributions for treatment rankings, providing more informative conclusions for decision-makers [6]
Implementation Considerations:
- Use weakly informative priors for heterogeneity parameters to avoid over-smoothing in sparse networks
- Implement consistency models assuming agreement between direct and indirect evidence
- Use node-splitting models to assess inconsistency in specific treatment comparisons
- Apply meta-regression to adjust for effect modifiers across studies
The Bayesian framework's flexibility in handling complex modeling structures, combined with its principled approach to evidence synthesis, makes it particularly suitable for mixed treatment comparisons where multiple data sources with varying quality and relevance need to be integrated for comprehensive treatment effect estimation.
The validity of a Mixed Treatment Comparison (MTC), also known as a Network Meta-Analysis (NMA), depends on several critical assumptions. These analyses simultaneously synthesize evidence from networks of clinical trials to compare multiple interventions, even when some have not been directly compared head-to-head [9] [10]. For researchers, scientists, and drug development professionals employing Bayesian MTC models, verifying the underlying assumptions of transitivity, consistency, and homogeneity (or its related concept, similarity) is not merely a statistical formality but a fundamental prerequisite for generating credible and clinically useful results [11] [12]. Violations of these assumptions can introduce bias and invalidate the conclusions of an otherwise sophisticated analysis. This document outlines detailed protocols for assessing these assumptions, framed within a broader research thesis on applying Bayesian MTC models.
Conceptual Foundations and Definitions
A clear understanding of the core assumptions is essential before undertaking their assessment.
Transitivity is a logical and clinical assumption that forms the bedrock of indirect comparisons. It posits that the studies included in the network are sufficiently similar, on average, in all important clinical and methodological characteristics that could influence the relative treatment effects [13] [11]. This means that if we have trials comparing treatment A vs. B and A vs. C, the patients, interventions, and study designs in these two sets of trials are similar enough that we can logically infer the effect of B vs. C through the common comparator A. Transitivity is a qualitative assumption assessed at the study level [11] [12].
Homogeneity/Similarity is often discussed alongside transitivity. While transitivity concerns the entire network, homogeneity traditionally refers to the statistical variability in treatment effects within a single pairwise comparison (e.g., among all A vs. B studies) [11] [12]. The methodological concept ensuring that studies are comparable enough to be combined is also termed similarity [11]. It is examined by assessing the distribution of potential effect modifiers across the different treatment comparisons.
Consistency is the statistical manifestation of transitivity. It means that the estimated treatment effect from a direct comparison (e.g., from trials directly comparing B and C) is in agreement with the estimate derived from indirect comparisons (e.g., comparing B vs. A and C vs. A) [9] [13]. In a network where both direct and indirect evidence exist for a particular comparison, this assumption can be tested statistically.
Table 1: Summary of Critical Assumptions in Mixed Treatment Comparisons
| Assumption | Conceptual Level | Core Question | Primary Method of Assessment |
|---|---|---|---|
| Transitivity | Logical/Clinical | Can the studies in the network be fairly compared to form a valid indirect comparison? | Qualitative evaluation of study characteristics and effect modifiers [13]. |
| Homogeneity/Similarity | Methodological/Statistical | Are the studies within each direct comparison similar enough to be pooled? | Evaluation of clinical/methodological characteristics and statistical heterogeneity (e.g., I²) within pairwise comparisons [11] [12]. |
| Consistency | Statistical | Do the direct and indirect estimates of the same treatment effect agree? | Statistical tests (e.g., design-by-treatment, node-splitting) and graphical methods [13] [11]. |
The following diagram illustrates the logical and statistical relationships between these core assumptions and the analysis process.
Protocol for Assessing Transitivity and Similarity
The assessment of transitivity and similarity is a methodological process that begins during the systematic review phase.
Experimental Workflow for Transitivity Assessment
The evaluation of transitivity is a qualitative, study-level process focused on identifying and comparing effect modifiers across the different treatment comparisons in the network [12].
Table 2: Key Domains for Evaluating Transitivity and Similarity
| Domain | Description | Practical Application | Common Effect Modifiers |
|---|---|---|---|
| Population (P) | Clinical characteristics of participants in the studies. | Compare baseline disease severity, age, gender, comorbidities, prior treatments, and diagnostic criteria across studies for each comparison. | Disease severity, genetic biomarkers, treatment history. |
| Intervention (I) | Specifics of the treatment regimens being investigated. | Ensure dosing, administration route, treatment duration, and concomitant therapies are comparable. | Drug formulation, dose intensity, surgical technique. |
| Comparator (C) | The control or standard therapy used in the trials. | Verify that control groups (e.g., placebo, active drug, standard care) are comparable. | Type of placebo, dose of active comparator. |
| Outcome (O) | The measured endpoint and how it was defined and assessed. | Confirm outcome definitions, measurement scales, timing of assessment, and follow-up duration are consistent. | Outcome definition (e.g., response rate), time point of measurement. |
| Study Design (S) | Methodological features of the included trials. | Assess and compare risk of bias, randomization method, blinding, and statistical analysis plan. | Study quality, blinding, multi-center vs. single-center. |
Detailed Methodology
- Identify Potential Effect Modifiers: Prior to analysis, systematically list clinical and methodological factors that are known, or suspected, to influence the relative treatment effects for the specific clinical question [13] [12]. This is based on clinical expertise and background knowledge.
- Extract Data on Effect Modifiers: During data extraction, systematically collect information on all identified potential effect modifiers for every included study.
- Compare the Distribution: Visually and statistically compare the distribution of these effect modifiers across the different treatment comparisons. For example, create summary tables or graphs showing the mean disease severity in A vs. B trials versus A vs. C trials. A notable imbalance in the distribution of a key effect modifier threatens the transitivity assumption.
- Sensitivity and Meta-Regression Analysis: If imbalance is suspected, consider conducting sensitivity analyses by excluding studies that are clear outliers. Alternatively, use meta-regression within the NMA model to adjust for continuous or categorical effect modifiers, if the data allow [11].
Protocol for Assessing Homogeneity
Homogeneity is assessed statistically within each direct pairwise comparison after the qualitative similarity assessment.
Experimental Protocol
- Perform Pairwise Meta-Analyses: Conduct standard pairwise meta-analyses for every direct comparison in the network (e.g., all A vs. B studies, all A vs. C studies) using both fixed-effect and random-effects models.
- Quantify Statistical Heterogeneity: For each pairwise meta-analysis, calculate the I² statistic, which describes the percentage of total variation across studies that is due to heterogeneity rather than chance [12]. Cochran's Q test can also be used, though it has low power when few studies are available.
- Interpret the Results:
- I² = 0%: No observed heterogeneity.
- I² > 50%: May be considered substantial heterogeneity [12].
- Investigate Sources of Heterogeneity: If substantial heterogeneity is identified (I² > 50%), investigate potential sources by returning to the transitivity/similarity assessment. Explore the influence of clinical or methodological factors through subgroup analysis or meta-regression for that specific comparison [11] [12].
Protocol for Assessing Consistency
Consistency is evaluated statistically in networks where both direct and indirect evidence exist for one or more comparisons (forming closed loops).
Experimental Workflow and Statistical Tests
Several statistical approaches can be used to evaluate consistency. The following workflow outlines a common strategy:
Global Approaches
Global approaches assess inconsistency across the entire network simultaneously.
- Design-by-Treatment Interaction Model: This is a comprehensive method that accounts for different sources of inconsistency, both from loops of evidence and from different study designs (e.g., two-arm vs. three-arm trials) [11] [14]. It is typically implemented using a hierarchical model within a Bayesian or frequentist framework. The model is fitted and compared to a consistency model. A significant difference (e.g., via deviance information criterion (DIC) in Bayesian analysis or a Wald test) suggests global inconsistency [11].
Local Approaches
Local approaches pinpoint the specific comparison(s) where direct and indirect evidence disagree.
- Node-Splitting Method: This method "splits" the information for a particular node (treatment comparison) into direct and indirect evidence. It then statistically tests the difference between the direct estimate and the indirect estimate for that specific comparison [11]. A significant p-value (e.g., < 0.05) indicates local inconsistency for that node. This is a powerful tool for diagnosing problems but should be adjusted for multiple testing.
Detailed Methodology for Node-Splitting
- Specify the Model: Using statistical software (e.g.,
gemtcin R, WinBUGS), specify a node-splitting model for the network. - Run the Analysis: Fit the model, which will estimate both direct and indirect evidence for each closed loop in the network.
- Examine Output: Review the output for the p-values and confidence/intervals of the difference between direct and indirect estimates for each comparison.
- Address Inconsistency: If inconsistency is found, investigate its causes. Revisit the transitivity assessment for the studies involved in the inconsistent loop. Consider excluding studies with a high risk of bias that may be driving the inconsistency, or use advanced models that can account for inconsistency [12].
The Scientist's Toolkit: Research Reagent Solutions
Successfully implementing these protocols requires a suite of statistical and computational tools.
Table 3: Essential Tools for Implementing MTC Assumption Assessments
| Tool / Reagent | Function | Application in Assumption Assessment |
|---|---|---|
| R Statistical Software | An open-source environment for statistical computing and graphics. | Primary platform for conducting all statistical analyses, including meta-analysis, NMA, and inconsistency tests [9] [11]. |
netmeta package (R) |
A frequentist package for NMA. | Performs NMA, provides network plots, and includes statistical tests for heterogeneity and inconsistency [14]. |
gemtc package (R) |
An interface for Bayesian NMA using JAGS/BUGS. | Used for Bayesian NMA models, node-splitting analyses, and assessing model fit (e.g., DIC) [9] [11]. |
| CINeMA Software | A web application and R package for Confidence in NMA. | Systematically guides users through the evaluation of within-study bias, indirectness, heterogeneity, and incoherence, applying the GRADE framework to NMA results [14]. |
| Stata Software | A commercial statistical software package. | Can perform NMA using specific user-written commands (e.g., network group) for both frequentist and Bayesian analyses [9] [11]. |
| GRADE Framework for NMA | A methodological framework for rating the quality of evidence. | Provides a structured approach to downgrade confidence in NMA results due to concerns with risk of bias, inconsistency, indirectness, imprecision, and publication bias [14]. |
| NH2-C2-NH-Boc-d4 | NH2-C2-NH-Boc-d4, MF:C7H16N2O2, MW:164.24 g/mol | Chemical Reagent |
| (S)-(+)-Ascochin | (S)-(+)-Ascochin, MF:C12H10O5, MW:234.20 g/mol | Chemical Reagent |
The rigorous application of the protocols outlined herein for assessing transitivity, homogeneity, and consistency is non-negotiable for producing trustworthy evidence from Mixed Treatment Comparisons. These assumptions are interconnected, and the assessment process is iterative. Within the context of a thesis on Bayesian MTC models, this document provides a foundational framework. Researchers must transparently report their methods for evaluating these assumptions, as this directly impacts the confidence that clinicians, policymakers, and drug development professionals can place in the resulting treatment rankings and effect estimates.
Understanding Direct, Indirect, and Mixed Evidence in a Network
Network meta-analysis (NMA) is a powerful statistical technique that allows for the simultaneous comparison of three or more interventions by combining evidence from a network of studies [13]. This approach addresses a common challenge in evidence-based medicine: decision-makers often need to choose between multiple competing interventions for a condition, but head-to-head randomized controlled trials (RCTs) are not available for all possible comparisons [13]. A network of interventions is formed by any set of studies that connects three or more interventions through direct comparisons [13]. The core strength of NMA lies in its ability to synthesize both direct evidence (from studies that directly compare two interventions) and indirect evidence (estimated through a common comparator) to generate mixed evidence (the combined effect estimate from the entire network) for all pairwise comparisons, even those never evaluated in direct trials [13].
The Bayesian statistical framework is particularly well-suited for NMA because it offers a principled and transparent method for combining different sources of evidence and quantifying uncertainty [15]. It allows for the incorporation of prior knowledge or beliefs through prior distributions, which is especially valuable when data are sparse [16] [15]. Furthermore, Bayesian methods provide direct probabilistic interpretations of results, such as the probability that one treatment is superior to another, which is highly informative for decision-making [15].
Core Concepts and Definitions
Types of Evidence in a Network
Direct Evidence: This evidence comes from studies, typically RCTs, that directly compare two interventions of interest (e.g., Intervention A vs. Intervention B) within the same trial and with the same protocol [13]. It preserves the benefits of within-trial randomization and is generally considered the gold standard for comparative effectiveness.
Indirect Evidence: When two interventions (e.g., B and C) have not been compared directly in a trial, their relative effect can be estimated indirectly through a common comparator (e.g., Intervention A) [13]. Mathematically, the indirect estimate for the effect of B versus C (dBC) via comparator A is derived as dBC = dAC - dAB, where dAC and dAB are the direct estimates from A vs. C and A vs. B trials, respectively [13].
Mixed Evidence: In a network meta-analysis, mixed evidence (or mixed treatment comparison) refers to the comprehensive estimate that results from statistically combining all available direct and indirect evidence for a given comparison within a single, coherent model [13]. This usually yields more precise estimates than either direct or indirect evidence alone [13].
Fundamental Assumptions
The validity of indirect and mixed evidence hinges on three key assumptions [13]:
Transitivity: This is a core methodological assumption requiring that the different sets of studies included in the network (e.g., AB trials and AC trials) are similar, on average, in all important factors that may affect the relative treatment effects (effect modifiers), such as patient populations, study design, or outcome definitions [13]. In other words, one could imagine that the AB and AC trials are, on average, comparable enough that the participants in the B trials could hypothetically have been randomized to C, and vice versa.
Coherence (or Consistency): This is the statistical manifestation of transitivity. It occurs when the different sources of evidence (direct and indirect) for a particular treatment comparison are in agreement with each other [13]. For example, the direct estimate of B vs. C should be statistically consistent with the indirect estimate of B vs. C obtained via A.
Homogeneity: This refers to the variability in treatment effects between studies that are comparing the same pair of interventions. Excessive heterogeneity within a direct comparison can threaten the validity of the entire network.
Table 1: Glossary of Key Terms in Network Meta-Analysis
| Term | Definition |
|---|---|
| Node | A point in a network diagram representing an intervention [13]. |
| Edge | A line connecting two nodes, representing the availability of direct evidence for that pair of interventions [13]. |
| Network Diagram | A graphical depiction of the structure of a network of interventions, showing which interventions have been directly compared [13]. |
| Effect Modifier | A study or patient characteristic (e.g., disease severity, age) that influences the relative effect of an intervention [13]. |
| Multi-Arm Trial | A randomized trial that compares more than two intervention groups simultaneously. These trials provide direct evidence on multiple edges in the network and must be analyzed correctly to preserve within-trial randomization [13]. |
Quantitative Landscape of Bayesian Methods in Applied Research
The application of Bayesian methods in medical research has seen significant growth. A recent bibliometric analysis of high-impact surgical journals from 2000 to 2024 identified 120 articles using Bayesian statistics, with a compounded annual growth rate of 12.3% [17]. This trend highlights the increasing adoption of these methods in applied research.
The use of Bayesian methods varies by study design and specialty. The same analysis found that the most common study designs employing Bayesian statistics were retrospective cohort studies (41.7%), meta-analyses (31.7%), and randomized trials (15.8%) [17]. In terms of surgical specialties, general surgery (32.5%) and cardiothoracic surgery (16.7%) were the most represented [17]. Regression-based methods were the most frequently used Bayesian technique (42.5%) [17].
However, the reporting quality of Bayesian analyses requires improvement. When assessed using the ROBUST scale (ranging from 0 to 7), the average score was 4.1 ± 1.6 [17]. Only 54% of studies specified the priors used, and a mere 29% provided justification for their choice of prior [17]. This underscores the need for better standardization and transparency in reporting.
Table 2: Application of Bayesian Statistics in Surgical Research (2000-2024)
| Characteristic | Findings (N=120 articles) |
|---|---|
| Compounded Annual Growth Rate | 12.3% [17] |
| Most Common Study Designs | Retrospective cohort studies (41.7%), Meta-analyses (31.7%), Randomized trials (15.8%) [17] |
| Top Represented Specialties | General Surgery (32.5%), Cardiothoracic Surgery (16.7%) [17] |
| Most Frequent Bayesian Methods | Regression-based analysis (42.5%) [17] |
| Average ROBUST Reporting Score | 4.1 ± 1.6 out of 7 [17] |
| Studies Specifying Priors | 54.0% [17] |
| Studies Justifying Priors | 29.0% [17] |
Experimental Protocols for Network Meta-Analysis
Protocol 1: Designing a Systematic Review for NMA
Objective: To systematically identify, select, and appraise all relevant studies for inclusion in a network meta-analysis.
- Define the Research Question: Formulate a clear question using the PICO framework (Population, Intervention, Comparator, Outcome). Critically, define the set of competing interventions to be included in the network [13].
- Develop Search Strategy: Conduct comprehensive searches across multiple electronic databases (e.g., MEDLINE, Embase, Cochrane Central). The search strategy should be designed to capture all studies for every possible pairwise comparison within the defined network [13].
- Study Selection and Data Extraction: Implement a systematic process for screening titles, abstracts, and full-text articles against pre-defined eligibility criteria. Extract data using standardized forms, including study characteristics, patient demographics, and outcome data for all intervention arms [13].
- Risk of Bias Assessment: Evaluate the methodological quality of each included study using appropriate tools (e.g., Cochrane Risk of Bias tool for randomized trials) [13].
- Construct Network Geometry: Map the available direct comparisons to create a network diagram, which visually represents the evidence base and identifies where direct and indirect evidence will come from [13].
Protocol 2: Statistical Analysis Using a Bayesian Framework
Objective: To fit a Bayesian network meta-analysis model to obtain mixed treatment effect estimates for all pairwise comparisons and rank the interventions.
- Model Specification: Choose an appropriate statistical model. A common choice is a Bayesian hierarchical model using Markov Chain Monte Carlo (MCMC) methods for estimation [17] [15]. The model can be formulated on the mean difference (for continuous outcomes) or log odds ratio scale (for binary outcomes).
- Prior Selection: Specify prior distributions for the model parameters. For the treatment effects, non-informative or weakly informative priors (e.g., N(0, 1002)) are often used to let the data dominate the conclusions. For heterogeneity variance, a prior that constrains it to plausible values (e.g., half-normal or log-normal) is recommended [16].
- Model Implementation: Run the model in specialized Bayesian software such as JAGS, BUGS, or STAN [17] [15]. The analysis can be implemented using statistical software like R with packages such as
brms[16]. - Convergence Diagnostics: Check the convergence of the MCMC chains using diagnostics like the Gelman-Rubin statistic (R-hat) and trace plots to ensure the model has converged to a stable posterior distribution [15].
- Inference and Ranking: Extract the posterior distributions of the treatment effects for all pairwise comparisons. Calculate probability values for each treatment being the best, second best, etc., to create a hierarchy of treatments [13].
Protocol 3: Assessing Transitivity and Coherence
Objective: To evaluate the validity of the fundamental assumptions underlying the network meta-analysis.
- Assessment of Transitivity: Identify potential effect modifiers a priori based on clinical and methodological knowledge. Then, compare the distribution of these effect modifiers across the different direct comparisons in the network (e.g., by creating summary tables of study characteristics stratified by comparison) [13].
- Assessment of Coherence: Evaluate the statistical agreement between direct and indirect evidence. This can be done using:
- Local Approaches: For a specific comparison, use the "node-splitting" method to separately estimate the direct, indirect, and mixed evidence and test for a significant disagreement [13].
- Global Approaches: Fit models that allow for and test the presence of incoherence anywhere in the entire network [13].
Visualization of Network Meta-Analysis Workflow
The following diagram illustrates the logical workflow and key components of conducting a network meta-analysis.
The Scientist's Toolkit: Essential Reagents and Software
Successful implementation of Bayesian network meta-analysis requires a set of specialized statistical tools and software.
Table 3: Key Research Reagent Solutions for Bayesian NMA
| Item | Category | Function and Application |
|---|---|---|
| R Statistical Software | Software Environment | A free, open-source environment for statistical computing and graphics. It is the primary platform for implementing most Bayesian NMA analyses through its extensive package ecosystem [15]. |
| JAGS / BUGS | MCMC Engine | Standalone software for Bayesian analysis using Gibbs Sampling. They use their own model definition language and can be called from within R. Useful for a wide range of models but can be slower for complex models [17] [15]. |
| Stan (with brms) | MCMC Engine | A state-of-the-art platform for statistical modeling and high-performance statistical computation. It uses Hamiltonian Monte Carlo, which is often more efficient for complex models. The brms package in R provides a user-friendly interface to Stan [17] [16]. |
| Cochrane ROB Tool | Quality Assessment Tool | A standardized tool for assessing the risk of bias in randomized trials. Assessing the quality of included studies is a critical step in evaluating the validity of a network meta-analysis [13]. |
| Non-informative Priors | Statistical Reagent | Prior distributions (e.g., very wide normal distributions) that are designed to have minimal influence on the posterior results, allowing the data to dominate the conclusions. They are a default starting point in many analyses [16]. |
| Informed Priors | Statistical Reagent | Prior distributions that incorporate relevant external evidence (e.g., from a previous meta-analysis or pilot study). They can be used to stabilize estimates, particularly in networks with sparse data [16] [15]. |
| ROBUST Checklist | Reporting Guideline | The Reporting of Bayes Used in Clinical Studies scale is a 7-item checklist used to assess and improve the quality and transparency of reporting in Bayesian analyses [17]. |
| L-Histidine hydrochloride hydrate | L-Histidine hydrochloride hydrate, CAS:5934-29-2, MF:C6H9N3O2.ClH.H2O, MW:209.63 g/mol | Chemical Reagent |
| Nrf2 activator-10 | Ethyl 4-chloro-1-methyl-2-oxo-1,2-dihydroquinoline-3-carboxylate | High-purity Ethyl 4-chloro-1-methyl-2-oxo-1,2-dihydroquinoline-3-carboxylate, a key intermediate for antimicrobial research. For Research Use Only. Not for human consumption. |
Advanced Applications and Future Directions
Bayesian network meta-analyses are particularly powerful in specialized research contexts. One advanced application is in the analysis of N-of-1 trials, which are randomized multi-crossover trials conducted within a single individual to compare interventions personalized to that patient [15]. Bayesian multilevel (hierarchical) models can seamlessly combine data from a series of N-of-1 trials. This allows for inference at both the population level (e.g., the average treatment effect) and the individual level, borrowing strength across participants to improve estimation for each one [15]. This is ideal for personalized medicine and for studying rare diseases where large trials are not feasible.
Another area of development is the use of highly informed priors. For example, a research program can involve an initial pilot study (Study 1) analyzed with non-informative or weakly informative priors. The posterior distributions from this analysis can then be used as highly informed priors for a subsequent, refined study (Study 2) [16]. This approach allows for the cumulative building of evidence in an efficient and statistically rigorous manner, which is especially valuable in iterative or exploratory research.
As the field evolves, emphasis is being placed on improving the quality and standardization of reporting. The consistently low rates of prior specification and justification (54% and 29%, respectively) found in the recent literature indicate a key area for improvement [17]. Adherence to guidelines like the ROBUST checklist is crucial for enhancing the transparency, reproducibility, and ultimately, the utility of Bayesian network meta-analyses for drug development professionals and healthcare decision-makers [17].
In the realm of Bayesian mixed treatment comparisons (MTC) and network meta-analysis (NMA), the choice of data structure is a fundamental methodological decision that significantly influences model specification, computational implementation, and result interpretation. Researchers face two primary approaches for data extraction and organization: arm-level and contrast-level data structures. The growing adoption of Bayesian frameworks in medical research, with a compounded annual growth rate of 12.3% in surgical research specifically, underscores the importance of understanding these foundational elements [17]. This application note provides detailed protocols for both data extraction approaches, framed within the context of Bayesian MTC research for drug development professionals and researchers.
The Bayesian paradigm, which interprets probability as a degree of belief in a hypothesis and enables incorporation of prior evidence, offers particular advantages for synthesizing complex treatment networks [17]. However, the effectiveness of Bayesian MTC models depends critically on appropriate data structure selection, as this choice influences the modeling of heterogeneity, respect for randomization within trials, and the range of estimands that can be derived [18] [19].
Theoretical Foundations and Definitions
Arm-Level Data
Arm-level data (also referred to as arm-synthesis data) consists of the raw summary measurements for each treatment arm within a study [20]. This structure preserves the absolute outcome information for individual arms, allowing for the direct modeling of arm-specific parameters before deriving relative effects [19]. For binary outcomes, this typically includes the number of events and total participants for each arm. For continuous outcomes, this would include the mean, measure of dispersion (standard deviation or standard error), and sample size for each arm [20].
The arm-level approach forms the foundation for arm-synthesis models (ASMs), which combine the arm-level summaries in a statistical model, with relative treatment effects then constructed from these arm-specific parameters [19]. This approach has the advantage of being able to compute various estimands within the model, such as marginal risk differences, and allows for the derivation of additional parameters beyond direct contrasts [18] [19].
Contrast-Level Data
Contrast-level data (also referred to as contrast-synthesis data) consists of the relative effect estimates and their measures of precision for each pairwise comparison within a study [20]. This structure directly represents the comparisons between interventions rather than the absolute performance of individual arms. For binary outcomes, this typically includes log odds ratios, risk ratios, or hazard ratios with their standard errors and covariance structure for multi-arm trials [18] [20].
The contrast-level approach provides the foundation for contrast-synthesis models (CSMs), which combine the relative treatment effects across trials [19]. These models have intuitive appeal because they rely solely on within-study information and therefore respect the randomization within trials [19]. The Lu and Ades model is a prominent example of a CB model that requires a study-specific reference treatment to be defined in each study [18].
Table 1: Fundamental Characteristics of Arm-Level and Contrast-Level Data Structures
| Characteristic | Arm-Level Data | Contrast-Level Data |
|---|---|---|
| Basic unit | Raw summary measurements per treatment arm | Relative effect estimates between arms |
| Data examples | Number of events & participants (binary); means & SDs (continuous) | Log odds ratios, risk ratios, mean differences with standard errors |
| Model compatibility | Arm-synthesis models (ASMs) | Contrast-synthesis models (CSMs) |
| Information usage | Within-study and between-study information | Primarily within-study information |
| Respect for randomization | May compromise randomization in some implementations | Preserves randomization within trials |
| Range of estimands | Wider range (e.g., absolute effects, marginal risk differences) | Limited to relative effects |
Methodological Protocols for Data Extraction
Arm-Level Data Extraction Protocol
Application Context: This protocol is appropriate when planning to implement arm-synthesis models, when absolute effects or specific population-level estimands are of interest, or when working with sparse data where borrowing strength across arms is beneficial [21] [19].
Materials and Software Requirements:
- Statistical software with Bayesian modeling capabilities (WinBUGS/OpenBUGS, JAGS, STAN)
- Data extraction template capturing arm-level details
- Bibliographic database (PubMed, Web of Science, Cochrane Central)
Step-by-Step Procedure:
Identify outcome measures: Determine the primary and secondary outcomes of interest for data extraction, ensuring consistency in definitions across studies.
Extract arm-specific data:
- For binary outcomes: Record the number of events and total participants for each treatment arm within each study [20].
- For continuous outcomes: Record the mean, standard deviation (or standard error), and sample size for each treatment arm within each study.
- For time-to-event outcomes: Record the number of events, log hazard ratios, and their standard errors (though these represent contrasts, they are typically analyzed using arm-level models).
Document study characteristics: Extract additional study-level variables that may explain heterogeneity or effect modifiers, including:
- Study design features (randomization method, blinding)
- Population characteristics (age, disease severity, comorbidities)
- Treatment details (dose, duration, administration route)
Verify data consistency: Check for logical consistency within studies (e.g., total participants across arms should not exceed overall study population in parallel designs).
Format for analysis: Structure data with one row per study arm, including study identifier, treatment identifier, and outcome data.
The following workflow diagram illustrates the arm-level data extraction process:
Contrast-Level Data Extraction Protocol
Application Context: This protocol is appropriate when planning to implement contrast-synthesis models, when the research question focuses exclusively on relative treatment effects, or when incorporating studies that only report contrast data [18] [19].
Materials and Software Requirements:
- Statistical software with network meta-analysis capabilities (R, WinBUGS, Stata)
- Data extraction template capturing contrast-level details
- Covariance matrix calculation tools for multi-arm trials
Step-by-Step Procedure:
Identify comparisons: Determine all pairwise comparisons available within each study.
Extract contrast data:
Select reference treatment: Designate a reference treatment for each study (often placebo or standard care) to maintain consistent direction of effects.
Document effect modifiers: Record study-level characteristics that may modify treatment effects, similar to the arm-level protocol.
Check consistency: Verify that contrast data is internally consistent, particularly for multi-arm trials where effects are correlated.
Format for analysis: Structure data with one row per contrast, including study identifier, compared treatments, effect estimate, and measure of precision.
The following workflow diagram illustrates the contrast-level data extraction process:
Bayesian MTC Modeling Considerations
Model Formulations
In Bayesian MTC, the choice between arm-level and contrast-level data structures leads to different model formulations with important implications for analysis and interpretation.
Arm-Synthesis Models (ASM) typically model the arm-level parameters directly. For a binary outcome with a logistic model, the probability of an event in arm (k) of study (i) ((p_{ik})) can be modeled as:
[ \text{logit}(p{ik}) = \mui + \delta_{i,bk} ]
where (\mui) represents the study-specific baseline effect (typically on the log-odds scale) for the reference treatment (b), and (\delta{i,bk}) represents the study-specific log-odds ratio of treatment (k) relative to treatment (b) [21]. The (\delta_{i,bk}) parameters are typically assumed to follow a common distribution:
[ \delta{i,bk} \sim N(d{bk}, \sigma^2) ]
where (d_{bk}) represents the mean relative effect of treatment (k) compared to (b), and (\sigma^2) represents the between-study heterogeneity [21].
Contrast-Synthesis Models (CSM) directly model the relative effects. The Lu and Ades model can be represented as:
[ \theta{ik}^a = \alpha{ibi}^a + \delta{ibik}^c \quad \text{for } k \in Ri ]
where (\theta{ik}^a) represents the parameter of interest in arm (k) of study (i), (\alpha{ibi}^a) represents the study-specific intercept for the baseline treatment (bi), and (\delta{ibik}^c) represents the relative effect of treatment (k) compared to (b_i) [18]. The relative effects are modeled as:
[ \delta{ibik}^c \sim N(\mu{1k}^c - \mu{1bi}^c, \sigmac^2) ]
where (\mu{1k}^c) represents the overall mean treatment effect for treatment (k) compared to the network reference treatment 1, and (\sigmac^2) represents the contrast heterogeneity variance [18].
Impact on Treatment Effect Estimates
Empirical evidence demonstrates that the choice between arm-level and contrast-level approaches can impact the resulting treatment effect estimates and rankings. A comprehensive evaluation of 118 networks with binary outcomes found important differences in estimates obtained from contrast-synthesis models (CSMs) and arm-synthesis models (ASMs) [19]. The different models can yield different estimates of odds ratios and standard errors, leading to differing surface under the cumulative ranking curve (SUCRA) values that can impact the final ranking of treatment options [19].
Table 2: Comparison of Model Properties and Applications
| Property | Arm-Synthesis Models (ASM) | Contrast-Synthesis Models (CSM) |
|---|---|---|
| Model type | Hierarchical model on arm-level parameters | Hierarchical model on contrast parameters |
| Information usage | Within-study and between-study information | Primarily within-study information |
| Randomization | May compromise randomization | Respects randomization within trials |
| Missing data assumption | Arms missing at random | Contrasts missing at random |
| Heterogeneity modeling | Modeled on baseline risks and/or treatment effects | Modeled on relative treatment effects |
| Available estimands | Relative effects, absolute effects, marginal risk differences | Primarily relative effects |
| Implementation complexity | Generally more complex | Generally more straightforward |
Research Reagent Solutions
The successful implementation of Bayesian MTC analyses requires specific methodological tools and computational resources. The following table details essential research reagents for this field:
Table 3: Essential Research Reagents for Bayesian MTC Analysis
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| WinBUGS/OpenBUGS | Bayesian analysis using MCMC | Historical standard for Bayesian MTC; user-friendly interface but limited development [21] |
| JAGS | Bayesian analysis using MCMC | Cross-platform alternative to BUGS; uses similar model specification [17] |
| STAN | Bayesian analysis using HMC | Modern platform with advanced sampling algorithms; requires different model specification [17] |
| R packages | Comprehensive statistical programming | Key packages: gemtc for MTC, pcnetmeta for Bayesian NMA, BUGSnet for comprehensive NMA [19] |
| ROBUST checklist | Quality assessment of Bayesian analyses | 7-item scale for assessing transparency and completeness of Bayesian reporting [17] |
| Vague priors | Default prior distributions | ( N(0, 10000) ) for location parameters; ( \text{Uniform}(0, 5) ) for heterogeneity parameters [21] |
| Consistency checks | Verification of direct/indirect evidence agreement | Node-splitting methods; design-by-treatment interaction test [21] [19] |
Case Study Application
To illustrate the practical implications of data structure choices, consider a Bayesian network meta-analysis of pharmacological treatments for alcohol dependence [21]. This network included direct comparisons between naltrexone (NAL), acamprosate (ACA), combination therapy (NAL+ACA), and placebo.
When implementing the analysis using contrast-level data with the Lu and Ades model [21], the researchers specified vague prior distributions for all parameters: ( N(0, 10000) ) for baseline and treatment effects, and ( \text{Uniform}(0, 5) ) for the common standard deviation. They assessed consistency between direct and indirect evidence using node-splitting methods and evaluated model convergence using trace plots and the Brooks-Gelman-Rubin statistic.
The analysis revealed that combination therapy (naltrexone+acamprosate) had the highest posterior probability of being the "best" treatment, a finding that was consistent across multiple outcomes [21]. This case demonstrates how Bayesian MTC with appropriate data structure selection can provide more precise estimates than pairwise meta-analysis alone, particularly for treatment comparisons with limited direct evidence.
The choice between arm-level and contrast-level data structures represents a fundamental methodological decision in Bayesian mixed treatment comparisons that significantly influences model specification, analysis, and interpretation. Arm-level data structures offer greater flexibility in the types of estimands that can be derived and may be particularly valuable when absolute effects or population-level summaries are of interest. Contrast-level data structures more directly respect randomization within trials and align with traditional meta-analytic approaches.
Empirical evidence from evaluations of real-world networks indicates that these approaches can yield meaningfully different results in practice, particularly for odds ratios, standard errors, and treatment rankings [19]. The characteristics of the evidence network, including its connectedness and the rarity of events, may influence the magnitude of these differences.
Researchers should carefully consider their research questions, the available data, and the desired estimands when selecting between these data structures. Pre-specification of the analytical approach in study protocols is recommended to maintain methodological rigor and transparency in Bayesian MTC research. As the use of Bayesian methods in medical research continues to grow at a notable pace, with a 12.3% compounded annual growth rate in surgical research specifically, proper understanding and application of these data structures becomes increasingly important for drug development professionals and clinical researchers [17].
Implementing Bayesian MTC Models: A Step-by-Step Workflow
In hierarchical models, often termed mixed-effects models, the distinction between fixed and random effects is fundamental. These models are widely used to analyze data with complex grouping structures, such as patients within hospitals or repeated measurements within individuals. The core difference lies not in the nature of the variables themselves, but in how their coefficients are estimated and interpreted [22].
Fixed effects are constant across individuals and are estimated independently without pooling information from other groups. In contrast, random effects are assumed to vary across groups and are estimated using partial pooling, where data from all groups inform the estimate for any single group. This allows groups with fewer data points to "borrow strength" from groups with more data, leading to more reliable and stable estimates, particularly for under-sampled groups [22] [23].
The following table summarizes the core differences:
Table 1: Core Differences Between Fixed and Random Effects
| Feature | Fixed Effects | Random Effects |
|---|---|---|
| Estimation Method | Maximum Likelihood (no pooling) | Partial Pooling / Shrinkage (BLUP) [23] |
| Goal of Inference | The specific levels in the data [23] | The underlying population of levels [23] |
| Information Sharing | No information shared between groups | Estimates for all groups inform each other |
| Generalization | Inference limited to observed levels | Can generalize to unobserved levels from the same population [23] |
| Degrees of Freedom | Uses one degree of freedom per level | Uses fewer degrees of freedom [23] |
Theoretical Foundations and Application Protocol
Conceptual Framework and Mathematical Formulation
The decision to designate an effect as fixed or random is often guided by the research question and the structure of the data. Statistician Andrew Gelman notes that the terms have multiple definitions, but a practical interpretation is that effects are fixed if they are of interest in themselves, and random if there is interest in the underlying population from which they were drawn [22].
A simple linear mixed-effects model can be formulated as follows [23]:
- Model Equation: ( yi = \alpha{j(i)} + \beta1 X{1i} + \beta2 X{2i} + \varepsilon_i )
- Random Effect: ( \alpha_j \sim \text{Normal}(\mu, \sigma^2) )
Here, ( yi ) is the response for observation ( i ), ( \alpha{j(i)} ) is the random intercept for the group ( j ) to which observation ( i ) belongs, ( \beta ) terms are fixed effect coefficients, and ( \varepsiloni ) is the residual error. The key is that the random effects ( \alphaj ) are assumed to be drawn from a common (usually Gaussian) distribution with mean ( \mu ) and variance ( \sigma^2 ), which is the essence of partial pooling [23].
Protocol for Defining the Model Structure
Objective: To correctly specify fixed and random effects in a hierarchical model based on the experimental design and research goals.
Procedure:
- Identify Grouping Structures: Determine the units of observation and the hierarchical or clustered structure of your data (e.g., patients within clinics, repeated measurements within subjects).
- Define the Research Goal for Each Factor:
- If the goal is to make inferences only about the specific levels included in your study (e.g., comparing three specific drug doses), model the factor as a fixed effect.
- If the goal is to make inferences about an underlying population of levels, and the levels in your study are a random sample from this population (e.g., selecting 10 clinics from a large pool of clinics nationwide), model the factor as a random effect.
- Assess Random Effects Suitability: For a factor to be a random effect, it should ideally have a sufficient number of levels to estimate the population variance reliably. A common guideline is to have at least five levels, though this is most critical when the variance of the random effect itself is of interest [23].
- Model Formulation: Write the model equation, clearly distinguishing fixed and random components. For instance, in a clinical trial with patients from multiple centers, the drug treatment would typically be a fixed effect, while the study center would be a random effect.
Workflow Visualization
The following diagram illustrates the logical decision process for specifying fixed and random effects in a hierarchical model.
Application in Bayesian Mixed Treatment Comparisons (MTCs)
The Role of MTCs in Evidence Synthesis
In the context of drug development and systematic reviews, Mixed Treatment Comparisons (MTCs), also known as network meta-analyses, are a powerful extension of standard meta-analysis. They allow for the simultaneous comparison of multiple treatments (e.g., Drug A, Drug B, Drug C, Placebo) in a single, coherent statistical model, even when not all treatments have been directly compared in head-to-head trials [10] [24].
MTCs integrate both direct evidence (from trials comparing treatments directly) and indirect evidence (e.g., inferring the A vs. C effect from A vs. B and B vs. C trials). This provides a unified, internally consistent ranking of all treatments and their relative efficacy [24].
Protocol for Implementing a Bayesian MTC
Objective: To synthesize evidence from a network of randomized controlled trials (RCTs) comparing multiple interventions for a specific condition.
Procedure:
- Define the Network: Systematically identify all relevant RCTs for the condition of interest. Clearly list all treatments and map the available direct comparisons to form a network graph (see Section 3.3).
- Model Specification:
- The relative treatment effects (e.g., log odds ratios) are typically modeled as fixed effects if assuming a common treatment effect across trials, or more often as random effects to account for heterogeneity between trials.
- The random-effects model assumes that the true treatment effects for a particular comparison vary across studies, and are drawn from a common distribution (e.g., a normal distribution). This heterogeneity is a key parameter of interest [24].
- Choose a Statistical Framework: Bayesian MTCs are preferred for their flexibility [10]. This involves:
- Likelihood: Defining the probability model for the observed data (e.g., binomial for binary outcomes).
- Priors: Specifying prior distributions for all unknown parameters, including the treatment effects and the between-trial heterogeneity parameter. Vague or weakly informative priors are often used in the absence of strong prior knowledge [17].
- Computation: Using Markov Chain Monte Carlo (MCMC) methods (e.g., in software like JAGS, BUGS, or STAN) to obtain the posterior distribution for each treatment effect [17].
- Check for Inconsistency: Assess if the direct and indirect evidence within the network are in agreement. Statistical methods, such as the Bucher method, can be used to test for inconsistency (or "lack of coherence") between different sources of evidence [24].
- Report Results: Present the posterior means and credible intervals for all pairwise comparisons. Results can be summarized as the probability that each treatment is the most effective.
MTC Network and Analysis Visualization
The diagram below visualizes the flow of evidence and analysis in a Mixed Treatment Comparison.
Table 2: Key Research Reagent Solutions for Hierarchical Modeling
| Tool / Resource | Type | Primary Function | Examples & Notes |
|---|---|---|---|
| STAN | Software | Probabilistic programming language for full Bayesian inference. | Uses Hamiltonian Monte Carlo (HMC), a state-of-the-art MCMC algorithm. Highly efficient for complex models [17]. |
| JAGS / BUGS | Software | Software for Bayesian analysis using MCMC methods. | Earlier and widely used tools. An intuitive choice for many standard hierarchical models [17]. |
| R & Packages | Software | Statistical computing environment and supporting packages. | Essential. Use with packages like brms (interface to STAN), rstan, lme4 (for frequentist mixed models), and BayesFactor [23]. |
| Python (PyMC3, PyStan) | Software | General-purpose programming with probabilistic modeling libraries. | PyMC3 offers intuitive model specification and uses modern inference algorithms. Good for integration into data pipelines. |
| Weakly Informative Priors | Statistical | Regularize model estimates and prevent overfitting. | e.g., Normal(0,1) on log-odds scale; Half-Cauchy or Half-Normal for variance parameters. Critical for stable MCMC sampling [17]. |
| MCMC Diagnostics | Protocol | Assess convergence and reliability of Bayesian model fits. | Check trace plots, Gelman-Rubin statistic (R-hat << 1.1), and effective sample size (n_eff). |
Choosing Prior Distributions for Treatment Effects and Heterogeneity
In Bayesian mixed treatment comparison (MTC) meta-analysis, the choice of prior distributions for treatment effects and between-study heterogeneity is a critical step that significantly influences the validity and interpretation of results. MTC meta-analysis, also known as network meta-analysis, extends conventional pairwise meta-analysis by simultaneously synthesizing both direct and indirect evidence about multiple treatments, enabling comparative effectiveness assessments across an entire network of interventions [25] [21]. As Bayesian methods have become increasingly prominent in medical research and even recognized in regulatory guidance [26], proper prior selection has emerged as an essential methodological consideration. This protocol provides detailed guidance on selecting, implementing, and validating prior distributions for Bayesian MTC analyses, with particular emphasis on applications in pharmaceutical development and clinical research.
The Bayesian framework offers several advantages for MTC meta-analysis, including enhanced estimation of between-study heterogeneity, improved performance when few studies are available, and the ability to directly quantify probabilities for treatment effects and rankings [27] [28]. However, these benefits depend on appropriate prior specification. Poorly chosen priors can lead to biased estimates, inappropriate precision, and distorted treatment rankings [28] [29]. This document provides detailed application notes and protocols for selecting priors that balance incorporation of existing knowledge with objective data-driven analysis.
Theoretical Framework
Bayesian Foundations for MTC Meta-Analysis
Bayesian statistics formalizes learning from accumulating evidence by combining prior information with current trial data using Bayes' theorem [26]. In the context of MTC meta-analysis, this approach treats unknown parameters—including overall treatment effects and heterogeneity variances—as random variables estimated through assignment of prior distributions and updated via observed data [25]. The fundamental Bayesian framework consists of several key components:
Prior Distribution: Mathematical representation of existing knowledge about parameters before observing current data. Priors can range from non-informative (allowing data to dominate) to highly informative (incorporating substantial pre-existing evidence) [28] [29].
Likelihood Function: Probability of observing the current data given specific parameter values, typically constructed based on the binomial distribution for binary outcomes or normal distribution for continuous outcomes [21] [30].
Posterior Distribution: Updated knowledge about parameters obtained by combining the prior distribution with the likelihood of observed data through Bayes' theorem. This distribution forms the basis for all statistical inferences [26].
For MTC meta-analysis, the posterior distribution enables simultaneous estimation of all treatment comparisons while properly accounting for correlations between direct and indirect evidence [25] [21].
Classification of Prior Information
Prior distributions are categorized based on the amount of information they incorporate relative to the current dataset:
Table 1: Classification of Prior Distributions
| Prior Type | Definition | Common Uses | Examples |
|---|---|---|---|
| Non-informative | Carries virtually no information about parameter values | Default choice when no prior information exists; allows data to drive analysis | Normal(0, 10000) for log odds ratios; Gamma(10â»Â¹â°, 10â»Â¹â°) for variances [28] [29] |
| Weakly informative | Carries more information than non-informative priors but less than actually available | Stabilizes estimation; prevents implausible parameter values | Uniform(0, 2) for heterogeneity standard deviation; Half-Normal(0, 1) [25] [28] |
| Moderately informative | Distinguishably more informative than weakly informative priors | Incorporates substantive external knowledge while allowing data influence | Log-normal priors based on empirical distributions; historical data [28] [29] [31] |
| Highly informative | Substantially influences posterior distribution | Strong prior evidence exists; sensitivity analyses | Precise normal distributions from large previous studies [26] |
Prior Distributions for Treatment Effects
Selection Guidelines
For treatment effect parameters (typically log odds ratios or mean differences), non-informative or weakly informative priors are generally recommended, particularly when comparing treatments without strong prior evidence of efficacy differences [21] [30]. The conventional choice is a normal distribution with mean zero and large variance, such as N(0, 100²), which imposes minimal influence while providing sufficient regularization for numerical stability [25] [21].
When historical data provides reliable evidence about treatment effects, moderately informative priors may be justified. However, informative priors for treatment effects require strong justification and should be accompanied by sensitivity analyses to demonstrate their influence on conclusions [26]. In regulatory settings, informative priors for treatment effects often face greater scrutiny than those for heterogeneity parameters [28] [26].
Implementation Protocol
Protocol 3.2: Implementing Treatment Effect Priors
Objective: Specify appropriate prior distributions for treatment effect parameters in Bayesian MTC models.
Materials: Statistical software with Bayesian capabilities (WinBUGS, JAGS, Stan, or R packages brms, rstanarm).
Procedure:
- Define Model Structure: Specify the statistical model using the contrast-based or arm-based parameterization [21].
- Select Prior Type:
- For analyses without strong prior evidence: Use N(0, 100²) for log odds ratios or mean differences.
- When incorporating historical data: Define normal priors with means based on previous estimates and variances reflecting the precision of those estimates.
- Code Implementation (WinBUGS example for log odds ratio):
- Validation: Conduct sensitivity analysis with alternative prior variances (e.g., N(0, 10²) and N(0, 1000²)).
Interpretation: Treatment effect priors should have minimal impact on posterior estimates when sufficient data exists; substantial changes in estimates with different priors indicates data sparsity.
Prior Distributions for Heterogeneity
Heterogeneity Parameter Challenges
Between-study heterogeneity (τ²) represents the variability in treatment effects across studies beyond sampling error. Heterogeneity priors are particularly influential in MTC because they affect the precision of all treatment effect estimates and consequently impact treatment rankings [25] [28]. The common variance assumption, which presumes equal heterogeneity across treatment comparisons, is often unrealistic but provides greater precision when data are sparse [28] [29]. Relaxing this assumption requires careful prior specification to maintain estimation stability.
Heterogeneity Prior Options
Table 2: Common Prior Distributions for Heterogeneity Parameters
| Prior Distribution | Parameter | Hyperparameter Options | Applicability |
|---|---|---|---|
| Inverse-Gamma | τ² | α = β = 0.1, 0.01, or 0.001 | Conjugate for normal likelihood; improves stability with sparse data [25] |
| Uniform | Ï„ | U(0, c) with c = 2, 5, or 10 | Common choice for log odds ratios; bounds maximum heterogeneity [25] [21] |
| Half-Normal | τ | HN(0, σ²) with σ² = 0.5, 1, or 2 | Gradually decreasing probability for larger heterogeneity values [25] |
| Log-Normal | τ² | Empirical values based on outcome and comparison type [25] [31] | Informative priors derived from large databases like Cochrane Library [25] |
Empirical Heterogeneity Priors
Empirical priors derived from large collections of meta-analyses provide increasingly popular options for heterogeneity parameters. Turner et al. developed log-normal priors categorized by outcome type and treatment comparison [25]. Recent work by Bartoš et al. used the Cochrane Database to develop discipline-specific empirical priors for binary and time-to-event outcomes [31].
Protocol 4.3: Implementing Empirical Heterogeneity Priors
Objective: Incorporate evidence-based prior distributions for heterogeneity parameters.
Materials: Access to empirical prior distributions from published sources [25] [31].
Procedure:
- Categorize Analysis: Classify the MTC by:
- Outcome type: all-cause mortality, semi-objective outcomes, or subjective outcomes
- Comparison type: pharmacological vs. placebo/control, pharmacological vs. pharmacological, or non-pharmacological comparisons
- Select Appropriate Parameters: Use published values such as:
- Pharmacological vs. placebo, all-cause mortality: LN(-4.06, 1.45²) for τ²
- Pharmacological vs. pharmacological, subjective outcomes: LN(-2.34, 1.62²) for τ² [25]
- Implement in Bayesian Code (WinBUGS example):
- Compare with Non-informative Options: Run parallel analyses with uniform or half-normal priors for sensitivity assessment.
Interpretation: Empirical priors typically produce narrower credible intervals than non-informative priors, especially for NMAs with few studies [25].
Workflow and Decision Framework
The following diagram illustrates the systematic decision process for selecting appropriate prior distributions in Bayesian MTC analysis:
Sensitivity Analysis and Model Validation
Sensitivity Analysis Protocol
Comprehensive sensitivity analysis is essential for evaluating the influence of prior choices on MTC results, particularly when analyses inform clinical or regulatory decisions [25] [26].
Protocol 6.1: Prior Sensitivity Analysis
Objective: Systematically assess the impact of prior distribution choices on MTC results.
Materials: Bayesian MTC model with multiple prior options.
Procedure:
- Define Prior Scenarios: Identify a range of plausible prior distributions for both treatment effects and heterogeneity parameters.
- Parallel Analysis: Conduct identical MTC analyses using different prior combinations.
- Compare Results: Evaluate:
- Posterior medians and 95% credible intervals for all treatment comparisons
- Between-study heterogeneity estimates
- Treatment ranking probabilities
- Surface under the cumulative ranking curve (SUCRA) values
- Quantitative Assessment: Calculate correlation coefficients between posterior medians and use Bland-Altman plots to assess agreement [25].
- Evaluate Significance Consistency: Compute kappa statistics for agreement on statistical significance across prior scenarios [25].
Interpretation: Results that are robust across prior choices increase confidence in conclusions. Substantial variations indicate dependency on prior assumptions and necessitate cautious interpretation.
Model Convergence and Fit Assessment
Adequate model convergence is essential for valid Bayesian inference. Assessment should include:
- Trace Plots: Visual inspection of Markov chain Monte Carlo (MCMC) sampling patterns
- Gelman-Rubin Diagnostics: Potential scale reduction factors (RÌ‚) approaching 1.0 [21] [30]
- Autocorrelation: Evaluation of sampling efficiency and independence
- Monte Carlo Error: Assessment of simulation precision relative to parameter uncertainty
Model fit can be compared using deviance information criterion (DIC) or Watanabe-Akaike information criterion (WAIC), with differences of 5-10 points suggesting meaningful improvements [21].
Regulatory and Reporting Considerations
Regulatory Perspectives
The FDA acknowledges that Bayesian approaches may be particularly useful when good prior information exists, potentially justifying smaller-sized or shorter-duration pivotal trials [26]. For medical devices, where mechanism of action is typically physical and effects local, prior information from previous device generations or overseas studies may provide valid prior information [26].
Key regulatory considerations include:
- Prior distributions should be pre-specified before examining trial data
- Informative priors require clear justification based on empirical evidence
- Sensitivity analyses must demonstrate robustness to prior assumptions
- Computational methods should use appropriate MCMC diagnostics [26]
Reporting Standards
Comprehensive reporting of prior distributions is essential for transparency and reproducibility. Current literature indicates substantial deficiencies, with 52.3% of Bayesian MTCs not specifying prior choices and 84.1% providing no rationale for those choices [25]. Reporting should include:
- Complete specification of all prior distributions
- Rationale for prior choices, particularly for informative priors
- Hyperparameter values and their justification
- Results of sensitivity analyses
- Assessment of model convergence and fit
Research Reagent Solutions
Table 3: Essential Tools for Bayesian MTC Implementation
| Tool Category | Specific Solutions | Function | Implementation Notes |
|---|---|---|---|
| Statistical Software | WinBUGS/OpenBUGS | MCMC sampling for Bayesian models | Legacy software with extensive MTC examples [21] [30] |
| JAGS | Cross-platform alternative to BUGS | Compatible with R through rjags package [27] | |
| Stan | Advanced Hamiltonian MCMC | Accessed via RStan, brms, or rstanarm packages [27] | |
| R Packages | brms | User-friendly interface for Stan | Formula syntax familiar to R users [27] |
| rstanarm | Precompiled Bayesian models | Faster estimation for standard models [27] | |
| MetaStan | Specialized for meta-analysis | Implements advanced heterogeneity models [27] | |
| Empirical Prior Databases | Turner et al. priors | Informative heterogeneity priors | Categorized by outcome and comparison type [25] |
| Cochrane Database | Source for empirical priors | Contains nearly half-million trial outcomes [31] |
Appropriate prior selection is a critical component of Bayesian MTC meta-analysis that balances incorporation of existing knowledge with objective data-driven analysis. Non-informative or weakly informative priors are generally recommended for treatment effects, while heterogeneity parameters benefit from empirical informed priors derived from large collections of meta-analyses. Comprehensive sensitivity analysis must accompany all prior choices to assess robustness of conclusions. Transparent reporting of prior specifications and their rationales is essential for methodological rigor and reproducibility. As Bayesian methods continue to gain acceptance in regulatory and clinical decision-making, the systematic approach to prior selection outlined in this protocol provides researchers with a framework for implementing statistically sound and clinically informative mixed treatment comparisons.
Mixed Treatment Comparison (MCMC) meta-analysis implemented within a Bayesian framework represents a powerful statistical methodology for comparing multiple treatments simultaneously, even when direct head-to-head evidence is lacking. This approach integrates both direct and indirect evidence through a connected network of trials, thereby strengthening inference and facilitating comparative effectiveness research (CER). The Bayesian paradigm provides particular advantages for these complex models, including modeling flexibility, inferential superiority, and the ability to incorporate prior knowledge through probability distributions. MCMC sampling methods serve as the computational engine that makes Bayesian inference tractable for these high-dimensional problems by allowing researchers to sample from complex posterior distributions that lack analytical solutions. These methods have become increasingly vital for healthcare researchers, scientists, and drug development professionals who must make informed decisions based on heterogeneous evidence networks spanning multiple therapeutic interventions.
Theoretical Foundations
Bayesian Framework for Mixed Treatment Comparisons
The foundation of MTC meta-analysis rests on the Bayesian hierarchical model structure, which treats all unknown parameters as random variables with probability distributions. Within the generalized linear modeling (GLM) framework, researchers can model various data types arising from the exponential family, including both binary outcomes (e.g., treatment response rates) and continuous outcomes (e.g., mean change from baseline). The Bayesian approach specifies a likelihood function for the observed data, prior distributions for unknown parameters, and yields posterior distributions for parameters of interest through application of Bayes' theorem. The flexibility of this framework allows for natural incorporation of random effects, which account for between-study heterogeneity by assuming each study's effect size is sampled from a distribution of effect sizes. This assumption is particularly appropriate in meta-analyses of randomized controlled trials where variations in participant populations, intervention implementation, and study methodologies inevitably create heterogeneity.
Markov Chain Monte Carlo Principles
MCMC methods constitute a class of algorithms for sampling from probability distributions based on constructing a Markov chain that has the desired distribution as its equilibrium distribution. The core principle involves generating a sequence of samples where each sample is dependent only on the previous one (the Markov property), with the chain eventually converging to the target posterior distribution. The power of MCMC lies in its ability to handle high-dimensional, complex posterior distributions that are common in hierarchical MTC models. In practice, MCMC algorithms work by iteratively proposing moves to new parameter values and accepting or rejecting these moves based on probabilistic rules that ensure the chain converges to the true posterior distribution. For MTC meta-analysis, this enables estimation of multiple treatment effects, heterogeneity parameters, and between-trial correlations in a unified framework.
Experimental Protocols and Workflows
Data Preparation and Network Geometry Assessment
Table 1: Data Requirements for Bayesian MTC Meta-Analysis
| Data Component | Specification | Handling Considerations |
|---|---|---|
| Outcome Types | Binary (e.g., treatment response) and continuous (e.g., mean change scores) | For binary outcomes, use true intention-to-treat (ITT) analysis with all randomized patients as denominator |
| Missing Variances | For continuous outcomes missing variances | Calculate using baseline and endpoint variances with assumed correlation of 0.5 |
| Study Design | Inclusion of multi-arm trials | Account for correlations between treatment differences through appropriate likelihood adjustments |
| Transitivity Assessment | Evaluation of populations, interventions, comparators, outcomes, timing, and settings | Ensure studies have sufficiently comparable compositions before combining in MTC |
Prior to model specification, a critical preliminary step involves assessing the transitivity assumption (sometimes referred to as similarity), which underpins the validity of MTC meta-analyses. This requires evaluating whether the included studies have sufficiently comparable compositions across key dimensions including populations, interventions, comparators, outcomes, timing, and settings. For the evidence network, researchers must document the network geometry, identifying specific patterns such as star configurations, closed loops, and ladder networks, as these patterns influence model performance and the potential for detecting inconsistency. Data extraction should recalculate outcome measures consistently across studies; for example, recalculating response rates using the number of all randomized patients as the denominator to reflect true ITT analysis and correct variations in modified ITT approaches encountered in individual studies.
Model Specification and Computational Implementation
Table 2: MCMC Parameter Configuration for Bayesian MTC
| Parameter | Specification | Rationale |
|---|---|---|
| Statistical Model | Random effects models | Accounts for between-study heterogeneity in effect sizes |
| Prior Distributions | Noninformative (flat) priors: Normal(0, 10000) for study and treatment effects | Allows data to drive posterior distributions in absence of informative priors |
| Heterogeneity Prior | Uniform prior distribution with sufficiently large variance | Minimizes prior influence on heterogeneity parameter estimation |
| Initial Values | Values relatively widely dispersed for multiple chains | Facilitates convergence assessment and minimizes influence of starting points |
| Burn-in Period | Typically 20,000 simulations | Discards initial samples before chain convergence |
| Estimation Iterations | Typically 100,000 simulations after burn-in | Provides sufficient samples for precise posterior estimation |
For all Bayesian MTC meta-analyses, implementation follows the generalized linear modeling framework with random effects to account for between-study heterogeneity. The model requires specification of likelihood functions appropriate to the outcome type and prior distributions for all unknown parameters. For most applications in the absence of rationale for informative priors, researchers should select noninformative prior distributions that allow the data to dominate the posterior distributions. The computational implementation requires careful configuration of the MCMC sampler, including determination of burn-in period (typically 20,000 simulations discarded to allow convergence) and estimation iterations (typically 100,000 simulations for posterior estimation). For multi-arm trials, appropriate adjustments to the likelihood are necessary to account for correlations between the treatment differences. Model specification should be documented with sufficient detail to enable reproducibility, including complete WinBUGS code provided in appendices where possible.
Applied Case Studies in Healthcare Research
Case Study 1: Second-Generation Antidepressants
A practical application of Bayesian MTC methods examined second-generation antidepressants (SGAs) using a dataset comprising 64 studies with a binary outcome of treatment response, defined as at least 50% improvement from baseline on the Hamilton Rating Scale for Depression (HAM-D). Researchers employed a random-effects model with noninformative priors and accounted for correlations in multi-arm trials. The analysis utilized a burn-in of 20,000 simulations followed by 100,000 estimation iterations, with convergence verified through trace plots, Monte Carlo error monitoring, and Gelman-Rubin diagnostics. A continuous outcome of mean change from baseline to endpoint on the HAM-D was also analyzed across 40 studies, with variances calculated for studies not reporting them using baseline and endpoint variances with an assumed correlation coefficient of 0.5. This approach demonstrated the practical considerations for handling incomplete reporting while maintaining methodological rigor in the Bayesian framework.
Case Study 2: Biologic Disease-Modifying Antirheumatic Drugs
In a second case study examining biologic DMARDs for rheumatoid arthritis, researchers analyzed a binary outcome of treatment response measured by achievement of ACR 50 after 12 weeks of treatment across 31 studies covering eight biologic DMARDs. The analysis again employed true ITT principles with all randomized patients as denominators to correct variations in modified ITT approaches across individual studies. The network included one multi-arm trial requiring appropriate correlation adjustments in the likelihood. This application highlighted how Bayesian MTC methods can simultaneously compare multiple treatments within a drug class, providing relative effectiveness estimates even for drug pairs with no direct head-to-head evidence. The continuous outcome of mean change from baseline in Health Assessment Questionnaire Disability Index (HAQ-DI) proved less informative due to limited eligible studies reporting adequate data, illustrating the importance of outcome reporting completeness in real-world evidence bases.
Methodological Validation and Comparison
Performance Assessment Framework
Table 3: Comparison Metrics for MCMC Method Validation
| Metric | Calculation Method | Interpretation Guidelines |
|---|---|---|
| Model Convergence | Proportion of drug-drug comparisons unable to calculate results | Lower values indicate better computational performance |
| Agreement Between Methods | Percent agreement on statistical significance/direction | Higher values indicate greater consistency between analytical approaches |
| Precision Comparison | Width of credible/confidence intervals | Narrower intervals indicate greater precision in effect estimates |
| Kappa Statistic | Measure of inter-rater agreement beyond chance | 0.21-0.40=fair; 0.41-0.60=moderate; 0.61-0.80=good; 0.81-1.00=very good |
Validation of Bayesian MTC methods requires comparison against established frequentist indirect methods, including frequentist meta-regression, the Bucher method, and frequentist logistic regression. Performance assessment should examine multiple metrics: (1) the proportion of drug-drug comparisons for which each method cannot calculate results due to model convergence issues or lack of a common comparator; (2) percent agreement between methods, considering findings to agree if both methods produce non-significant/unimportant results or both find significant results favoring the same treatment; (3) precision of findings assessed by comparing widths of credible and confidence intervals; and (4) kappa statistics measuring agreement beyond chance. This comprehensive validation framework ensures robust assessment of methodological performance across different evidence network patterns (star, loop, one closed loop, and ladder) that commonly occur in real-world comparative effectiveness research.
Research Reagent Solutions
Table 4: Essential Computational Tools for Bayesian MTC Implementation
| Tool | Specification | Application Function |
|---|---|---|
| WinBUGS | Version 1.4.3 | Bayesian software package using MCMC techniques for posterior estimation |
| Statistical Algorithms | Markov chain Monte Carlo (MCMC) | Samples from complex posterior distributions through iterative simulation |
| Convergence Diagnostics | Gelman-Rubin statistics, trace plots | Verifies MCMC chain convergence to target posterior distribution |
| Prior Distributions | Noninformative Normal(0, 10000) | Minimizes prior influence when substantive prior knowledge is unavailable |
| Data Augmentation Methods | Exact Conditional Sampling (ECS) algorithm | Handles missing data mechanisms and left-truncated observations |
Successful implementation of Bayesian MTC analyses requires specific computational tools and statistical reagents. The WinBUGS software package (Version 1.4.3) provides a specialized environment for Bayesian analysis using MCMC techniques, with available annotated code for MTC implementations. For model specification, researchers should employ random effects models that account for between-study heterogeneity, with noninformative prior distributions such as Normal(0, 10000) for study and treatment effect parameters when substantive prior knowledge is unavailable. For the heterogeneity parameter in random-effects models, a uniform prior distribution with sufficiently large variance is recommended. Convergence assessment requires multiple diagnostic tools including trace plots for visual inspection of chain mixing, Monte Carlo error monitoring for precision assessment, and formal Gelman-Rubin diagnostics for verifying convergence. For complex data structures including left-truncated observations, data augmentation techniques such as the Exact Conditional Sampling algorithm enhance computational efficiency and enable handling of realistic data scenarios encountered in practice.
Advanced Methodological Extensions
More complex methodological extensions continue to enhance the applicability of MCMC methods for Bayesian MTC meta-analysis. A two-level MCMC sampling scheme addresses situations where posterior distributions do not assume simple forms after data augmentation, with an outer level generating augmented data using algorithms like ECS combined with techniques for left-truncated data, and an inner level applying Gibbs sampling with newly developed rejection sampling schemes on logarithmic scales. For handling left-truncated data commonly encountered in real-world studies where individuals enter at different physiological ages, specialized MCMC algorithms extend standard approaches through modified data augmentation steps. These advanced techniques address the estimability issues that arise in complex models like the phase-type aging model, where profile likelihood functions are flat and analytically intractable, by leveraging the capacity of Bayesian methods to incorporate sound prior information that stabilizes parameter estimation. The nested MCMC structure exemplifies how methodological innovation expands the applicability of Bayesian MTC approaches to increasingly complex research questions in drug development and comparative effectiveness.
Core Concepts and Quantitative Data
Table 1: Key Statistical Measures in Bayesian and Frequentist Frameworks
| Measure | Definition | Interpretation in Context | Key Considerations |
|---|---|---|---|
| Odds Ratio (OR) | Ratio of the odds of an event occurring in one group versus the odds in another group. [32] | An OR > 1 indicates increased odds of the event in the first group. For example, an OR of 1.5 suggests the outcome is 1.5 times more likely in the treatment group. [32] [33] | Used for dichotomous outcomes. In meta-analysis, the OR Confidence Interval (CI) ratio (upper/lower boundary) can predict if a study meets its optimal information size. [32] |
| Relative Risk (RR) | Ratio of the probability of an event occurring in one group versus another group. [32] | An RR > 1 indicates an increased risk of the event. For instance, an RR of 0.8 implies a 20% reduction in risk relative to the control. [32] | Often more intuitive to interpret than OR. Similar to OR, its CI ratio can be used for imprecision judgments in meta-analysis. [32] |
| Credible Interval (CrI) | The Bayesian analogue of a confidence interval. A 95% CrI represents a 95% probability that the true parameter value lies within the interval, given the observed data and prior. [17] | Provides a direct probabilistic interpretation of uncertainty. For example, one can state, "There is a 95% probability that the true RR lies between 0.7 and 0.9." | Its width is influenced by both the observed data and the chosen prior distribution. Contrasts with the frequentist Confidence Interval. [17] |
| Confidence Interval (CI) | A frequentist measure expressing the range within which the true parameter value would lie in a specified percentage of repeated experiments. [17] | Does not provide a probability for the parameter. Correct interpretation: "We are 95% confident that the interval contains the true parameter." | In meta-analysis, a wide CI for RR or OR often indicates that the optimal information size has not been met, suggesting imprecision. [32] |
Experimental Protocols for Bayesian Analysis
Protocol for Conducting a Bayesian Network Meta-Analysis
Application: This protocol is designed for comparing multiple interventions simultaneously using a Bayesian framework, which is fundamental to mixed treatment comparisons. [33]
Workflow Diagram: Bayesian NMA Workflow
Procedure:
- Problem Definition & Registration: Precisely define the PICO (Population, Intervention, Comparator, Outcome) and register the review protocol on a platform like the Open Science Framework. [17]
- Systematic Search & Study Selection: Conduct a comprehensive literature search across multiple databases (e.g., PubMed, Web of Science) based on the PICO. Use predefined inclusion/exclusion criteria, with multiple independent reviewers resolving discrepancies by consensus. [17]
- Data Extraction: Extract bibliometric data, study characteristics, and outcome data (e.g., dichotomous data for OR/RR). Use standardized forms and multiple extractors. [17]
- Evaluate NMA Assumptions:
- Similarity: Ensure trials are sufficiently similar in their methodological characteristics (population, interventions, outcomes). [33]
- Transitivity: Check that effect modifiers are balanced across the available treatment comparisons. [33]
- Consistency: Statistically examine the agreement between direct and indirect evidence. [33]
- Model Specification:
- Computation: Run Markov Chain Monte Carlo (MCMC) sampling using software like JAGS, STAN, or
rstanarmin R. Use multiple chains and a sufficient number of iterations. [17] [34] - Convergence Diagnostics: Assess MCMC convergence using trace plots, the Gelman-Rubin statistic (Ȓ ≈ 1.0), and effective sample size. [17]
- Interpretation & Reporting: Report treatment rankings and effect estimates (OR/RR) with their 95% CrIs. Adhere to the ROBUST guidelines for transparent Bayesian reporting. [17]
Protocol for a PRACTical Trial Analysis
Application: This protocol outlines the analysis of a Personalised Randomised Controlled Trial (PRACTical), a design that naturally employs mixed treatment comparisons without a single standard of care. [34]
Procedure:
- Trial Design: For a condition with multiple treatments, define a "master list" of treatments. For each patient, create a personalised randomisation list containing only the treatments they are eligible for. Patients sharing the same list form a subgroup. [34]
- Data Generation: Simulate or collect trial data. The primary outcome (e.g., 60-day mortality) is often binary. The total sample size
Nis distributed across patient subgroups. [34] - Model Formulation: Fit a multivariable logistic regression model.
- Frequentist: Use maximum likelihood estimation via standard statistical packages.
- Bayesian: Use MCMC sampling (e.g., via
rstanarm). Incorporate informative priors if historical data is available. The model includes fixed effects for treatments and patient subgroups. [34]
- Performance Assessment: Compare analysis approaches using:
- Probability of predicting the true best treatment (
P_best). - A novel measure considering uncertainty: Probability of Interval Separation (
P_IS) as a proxy for power, and Probability of Incorrect Interval Separation (P_IIS) for type I error. [34]
- Probability of predicting the true best treatment (
- Implementation: Analysis can be performed using R packages such as
statsfor frequentist models andrstanarmfor Bayesian models. [34]
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Software and Computational Tools
| Tool Name | Function | Application in Analysis |
|---|---|---|
| R & RStudio | A statistical computing environment and integrated development interface. | The primary platform for executing statistical analyses, data manipulation, and generating visualizations. [35] [34] |
| JAGS / STAN | Standalone software for Bayesian analysis using MCMC sampling. | Used for fitting complex Bayesian models where conjugate priors are not employed, providing full posterior inference. [17] |
rstanarm R Package |
An R package that provides a user-friendly interface to the STAN engine for Bayesian regression modeling. | Simplifies the process of specifying and running Bayesian generalized linear models (e.g., logistic regression for PRACTical trials). [34] |
netmeta R Package |
A frequentist package for performing network meta-analysis. | Allows for the synthesis of direct and indirect evidence to compare multiple treatments. [33] |
gemtc R Package |
An R package for conducting Bayesian network meta-analysis. | Facilitates the setup, computation, and diagnostics of Bayesian NMA models. [36] |
| MetaInsight Web Application | An interactive, point-and-click web application for NMA. | Enables researchers to perform complex analyses like network meta-regression without statistical programming, improving accessibility. [36] |
| 5,7-Dihydroxycoumarin | 5,7-Dihydroxycoumarin, CAS:2732-18-5, MF:C9H6O4, MW:178.14 g/mol | Chemical Reagent |
| Stearic Acid-d35 | Stearic Acid-d35, CAS:62163-39-7, MF:C18H36O2, MW:287.5 g/mol | Chemical Reagent |
Visualization Workflow Diagram: From Data to CNMA Inference
Network meta-analysis (NMA) is a powerful statistical methodology that enables the simultaneous comparison of multiple treatments for the same health condition by synthesizing both direct and indirect evidence from a network of randomized controlled trials [37] [38]. This approach allows for the estimation of relative treatment effects between interventions that may never have been compared directly in head-to-head trials, thereby providing a comprehensive hierarchy of treatment efficacy and safety [39]. Within the framework of NMA, treatment ranking provides clinicians and researchers with valuable tools to identify optimal interventions among several competing options, making it particularly useful in evidence-based medicine and drug development decision-making [37].
The fundamental objective of treatment ranking is to order all competing treatments from best to worst based on a specific outcome of interest, such as efficacy for beneficial outcomes or harm for adverse events [38]. While point estimates of treatment effects provide some guidance for such ordering, ranking methodologies incorporate both the magnitude of effect differences and the statistical uncertainty surrounding these estimates [39] [40]. This dual consideration leads to more nuanced and reliable treatment hierarchies that better inform clinical and policy decisions, especially when dealing with complex treatment networks involving multiple interventions [37].
Theoretical Foundations of Ranking Metrics
Rank Probabilities
In Bayesian NMA, the foundation of treatment ranking lies in rank probabilities, which represent the probability that each treatment assumes a particular rank position (first, second, third, etc.) among all competing treatments [39]. These probabilities are derived from the posterior distributions of treatment effects obtained through Markov Chain Monte Carlo (MCMC) simulation. For a network of K treatments, the rank probability p_{ik} denotes the probability that treatment i has rank k (where k = 1 represents the best rank and k = K the worst) [40]. These probabilities form a K × K matrix that comprehensively captures the uncertainty in treatment rankings, providing a more complete picture than single point estimates [39].
Surface Under the Cumulative Ranking Curve (SUCRA)
The Surface Under the Cumulative Ranking Curve (SUCRA) is a numerical summary measure that transforms the complex rank probability distribution for each treatment into a single value ranging from 0 to 1 (or 0% to 100%) [37] [38]. SUCRA is calculated by averaging the cumulative probabilities for each treatment across all possible ranks, effectively representing the relative performance of a treatment compared to an imaginary intervention that is always the best without uncertainty [40]. The mathematical formulation of SUCRA for treatment i is given by:
[ SUCRA(i) = \frac{\sum{r=1}^{K-1} \sum{k=1}^{r} p_{ik}}{K-1} ]
where p_{ik} is the probability that treatment i has rank k, and K is the total number of treatments [40]. An alternative computational approach expresses SUCRA in terms of the expected rank:
[ SUCRA(i) = \frac{K - E(\text{rank}(i))}{K - 1} ]
where E(rank(i)) represents the expected rank of treatment i [40]. Higher SUCRA values indicate better treatment performance, with SUCRA = 1 (or 100%) suggesting a treatment is certain to be the best, and SUCRA = 0 (or 0%) indicating a treatment is certain to be the worst [38].
P-Scores
P-scores serve as the frequentist analogue to SUCRA values and provide a similar ranking metric without requiring resampling methods or Bayesian computation [39]. For a treatment i, the P-score is calculated based on the point estimates and standard errors of all pairwise comparisons in the network meta-analysis under the normality assumption [37] [39]. The P-score measures the mean extent of certainty that a treatment is better than all competing treatments and can be interpreted as the average of one-sided p-values from all pairwise comparisons [39]. Numerical studies have demonstrated that P-scores and SUCRA values yield nearly identical results, making them interchangeable for practical applications [39].
Predictive P-Scores
The predictive P-score represents a recent advancement in treatment ranking methodology that extends the conventional P-score to a future study setting within the Bayesian framework [37]. This metric accounts for between-study heterogeneity when applying evidence from an existing NMA to decision-making for future studies or new patient populations [37]. Unlike standard P-scores, predictive P-scores incorporate the heterogeneity parameter τ², which leads to a trend toward convergence at 0.5 (indicating greater uncertainty) as heterogeneity increases [37]. This property makes predictive P-scores particularly valuable for clinical trial design and medical decision-making in settings where transportability of evidence is a concern [37].
Calculation Methodologies and Protocols
Bayesian Computation of SUCRA
The calculation of SUCRA values within a Bayesian framework follows a structured protocol:
- Specify the Bayesian NMA model using appropriate likelihood functions and link functions based on the outcome type (e.g., binomial likelihood with logit link for binary outcomes) [37].
- Implement Markov Chain Monte Carlo (MCMC) sampling to generate posterior distributions of treatment effects. Software such as WinBUGS, JAGS, or Stan is typically employed with non-informative or weakly informative priors [37] [41].
- Compute rank probabilities from the MCMC output by counting, for each iteration, the rank position of each treatment based on their simulated treatment effects [40].
- Calculate cumulative rank probabilities for each treatment by summing the probabilities across decreasing rank positions.
- Determine SUCRA values by taking the average of the cumulative probabilities for each treatment [40].
Frequentist Computation of P-Scores
The protocol for calculating P-scores within the frequentist framework involves:
- Conduct frequentist NMA to obtain point estimates and variance-covariance matrix of all relative treatment effects [39].
- For each treatment pair (i,j), calculate the probability that treatment i is better than treatment j using the formula: [ P(\mui > \muj) = \Phi\left(\frac{\hat{\mu}i - \hat{\mu}j}{\sigma{ij}}\right) ] where Φ is the cumulative distribution function of the standard normal distribution, (\hat{\mu}i) and (\hat{\mu}j) are the point estimates for treatments i and j, and (\sigma{ij}) is the standard error of their difference [39].
- Compute the P-score for treatment i as the mean of all P(\mui > \muj) values across all j ≠i [39].
Workflow for Treatment Ranking Analysis
The following diagram illustrates the comprehensive workflow for conducting treatment ranking analysis in network meta-analysis:
Quantitative Comparison of Ranking Metrics
Table 1: Properties of Different Treatment Ranking Metrics
| Metric | Framework | Range | Interpretation | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Rank Probabilities | Bayesian | 0-1 | Probability of assuming each possible rank | Comprehensive representation of ranking uncertainty | Difficult to interpret when many treatments are compared [38] |
| SUCRA | Bayesian | 0-1 | Relative probability of being better than competing treatments | Single summary value; facilitates comparison across treatments | Does not directly communicate magnitude of effect differences [38] |
| P-Score | Frequentist | 0-1 | Mean extent of certainty of being better than competitors | No resampling required; computationally simple | Assumes normality of effect estimates [39] |
| Predictive P-Score | Bayesian | 0-1 | Expected performance in a future study | Accounts for between-study heterogeneity | More complex computation [37] |
Table 2: Comparison of SUCRA and P-score Values in a Diabetes Network Meta-Analysis (Adapted from Rücker & Schwarzer, 2015) [39]
| Treatment | SUCRA Value | P-Score Value | Difference | Interpretation |
|---|---|---|---|---|
| Treatment A | 0.92 | 0.92 | 0.00 | Highest likelihood of being most effective |
| Treatment B | 0.87 | 0.87 | 0.00 | High likelihood of being among top treatments |
| Treatment C | 0.65 | 0.64 | 0.01 | Moderate likelihood of being better than average |
| Treatment D | 0.42 | 0.43 | -0.01 | Moderate likelihood of being worse than average |
| Treatment E | 0.14 | 0.14 | 0.00 | High likelihood of being among bottom treatments |
Visualization Techniques for Treatment Ranking
Rankograms
Rankograms are fundamental graphical tools for presenting treatment ranking results, displaying the probability distribution of ranks for each treatment [38]. These plots typically show rank positions on the horizontal axis and the corresponding probabilities on the vertical axis, allowing for immediate visual assessment of ranking uncertainty [38]. Treatments with probability mass concentrated on the left side (lower rank numbers) are likely to be more effective, while those with probability mass concentrated on the right side are likely to be less effective. The spread of the probability distribution indicates the certainty in ranking—wider distributions reflect greater uncertainty, while narrower distributions indicate more precise ranking estimates [38].
Litmus Rank-O-Gram and Radial SUCRA Plots
Recent advancements in ranking visualization include the development of novel graphical displays such as the Litmus Rank-O-Gram and Radial SUCRA plots [42]. These visualizations aim to improve the presentation and interpretation of ranking results by integrating them with other important aspects of NMA, including evidence networks and relative effect estimates [42]. The Litmus Rank-O-Gram provides a multifaceted display of ranking information, while the Radial SUCRA plot offers a circular representation of SUCRA values that facilitates comparison across multiple treatments [42]. These visualization techniques have been embedded within interactive web-based applications such as MetaInsight to enhance accessibility and usability for researchers and decision-makers [42].
Comparison with Common Comparator
An alternative visualization approach involves plotting point estimates and confidence/credible intervals for each treatment compared to a common comparator, typically a standard care, placebo, or the lowest-ranked treatment [38]. This format helps contextualize the magnitude of effect differences between treatments while accounting for statistical uncertainty, providing a more complete picture than ranking metrics alone [38]. This approach is particularly valuable when the certainty of evidence varies substantially across treatment comparisons, as it prevents overinterpretation of ranking differences that may not be statistically significant or clinically important [38].
The following diagram illustrates the relationships between different ranking metrics and their associated visualization techniques:
The Scientist's Toolkit: Essential Materials and Reagents
Table 3: Essential Computational Tools for Treatment Ranking Analysis
| Tool/Software | Primary Function | Key Features for Treatment Ranking | Implementation Considerations |
|---|---|---|---|
| R Statistical Environment | Comprehensive statistical computing | netmeta package for frequentist NMA and P-scores; bugsnet for Bayesian NMA | Steeper learning curve but maximum flexibility for customization [39] |
| Stan with CmdStanR/CmdStanPy | Bayesian statistical modeling | Flexible MCMC sampling for complex hierarchical models; rank calculation | Efficient handling of complex models; requires programming expertise [41] |
| WinBUGS/OpenBUGS | Bayesian inference Using Gibbs Sampling | User-friendly interface for Bayesian NMA; automated rank probability calculation | Legacy software with limited development but extensive documentation [37] |
| JAGS (Just Another Gibbs Sampler) | Cross-platform Bayesian analysis | Compatible with R through rjags package; similar syntax to BUGS | Active development community; cross-platform compatibility [37] |
| MetaInsight | Web-based NMA application | Interactive ranking visualizations including Litmus Rank-O-Gram and Radial SUCRA | User-friendly interface; limited model customization options [42] |
| Octanoate-13C sodium | Octanoate-13C sodium, CAS:201612-61-5, MF:C8H15NaO2, MW:167.19 g/mol | Chemical Reagent | Bench Chemicals |
| Hippuryl-His-Leu-OH | Hippuryl-histidyl-leucine|ACE Substrate | Hippuryl-histidyl-leucine: A high-purity, specific synthetic substrate for angiotensin-I converting enzyme (ACE) activity assays. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
Interpretation Guidelines and Caveats
Contextualizing Ranking Results
Interpreting treatment ranking metrics requires careful consideration of several important factors to avoid misleading conclusions. First, SUCRA values and P-scores should always be evaluated in the context of the certainty (quality) of the underlying evidence [38]. Ranking metrics derived from low-quality evidence (e.g., studies with high risk of bias, imprecision, inconsistency, or indirectness) should be interpreted with caution, as they may produce spurious treatment hierarchies [38]. Second, ranking metrics alone do not convey information about the magnitude of effect differences between treatments—a treatment may have a high SUCRA value while being only marginally better than the next best option [38]. Third, clinical decision-making should consider multiple outcomes simultaneously, as a treatment that ranks highly for efficacy might perform poorly for safety or tolerability outcomes [38].
Quantifying Certainty in Treatment Hierarchies
Recent methodological advancements have focused on quantifying the certainty in treatment hierarchies through metrics such as the Precision of Treatment Hierarchy (POTH) [40]. POTH provides a single, interpretable value between 0 and 1 that quantifies the extent of certainty in producing a treatment hierarchy from SUCRA or P-score values [40]. This metric connects three statistical quantities: the variance of the SUCRA values, the variance of the mean rank of each treatment, and the average variance of the distribution of individual ranks for each treatment [40]. POTH can be particularly valuable when comparing hierarchies across different outcomes or networks, as it provides a standardized measure of ranking precision that accounts for the overlap and uncertainty in estimated treatment effects [40].
Reporting Standards
Comprehensive reporting of treatment ranking results should include both numerical and graphical presentations of ranking metrics alongside traditional treatment effect estimates with confidence or credible intervals [38]. This multifaceted approach ensures that readers can appropriately interpret the ranking information while considering the magnitude of effect differences and the precision of estimates [42]. Additionally, researchers should provide transparency in the computational methods used to generate ranking metrics, including software implementation, model specifications, and MCMC convergence diagnostics for Bayesian analyses [37].
SUCRA and rank probability metrics provide valuable tools for interpreting and communicating results from network meta-analyses, offering concise summaries of complex treatment hierarchies that incorporate both effect sizes and statistical uncertainty. When appropriately contextualized with measures of evidence certainty, magnitude of effect differences, and clinical considerations, these ranking methodologies significantly enhance the utility of NMA for evidence-based decision-making in drug development and clinical practice. The ongoing development of enhanced visualization techniques and uncertainty quantification methods continues to improve the accessibility and appropriate interpretation of treatment ranking results, supporting their effective application in healthcare decision-making.
Solving Common Challenges in Complex MTC Analyses
Addressing Outcome Reporting Bias (ORB) with Multivariate Models
Outcome reporting bias (ORB) is a significant threat to the validity of systematic reviews and meta-analyses, occurring when the selective reporting of research results is influenced by their direction or statistical significance [43]. Unlike publication bias, which involves the non-publication of entire studies, ORB operates at the level of individual outcomes within published studies [43]. Empirical evidence demonstrates that statistically significant results are more likely to be fully reported, with one study finding the odds of publication were 2.4 times greater for statistically significant versus non-significant outcomes [43]. This selective reporting introduces bias into the literature, potentially inflating estimates of beneficial effects and underestimating harms [43]. The problem is widespread, with studies indicating that 40% of trials change primary outcomes between protocol and publication, and up to 60% of trials have been found to graphically illustrate unregistered outcomes, further contributing to ORB [44] [45].
Multivariate models offer a promising methodological approach to mitigate ORB by leveraging correlations among multiple outcomes. These models enable borrowing of information across correlated outcomes, reducing the impact of selective reporting when some outcomes are missing [46] [47]. Within the framework of mixed treatment comparisons (MTC) or network meta-analysis, which synthesizes evidence across multiple treatments, multivariate approaches can substantially enhance the robustness of evidence synthesis [47]. This application note outlines protocols for implementing Bayesian multivariate models to address ORB in systematic reviews and meta-analyses.
Theoretical Framework and Mechanism
Multivariate models address ORB through several interconnected statistical mechanisms. The core principle involves using correlated outcomes to provide indirect information about missing or selectively reported outcomes [47]. When outcomes are correlated within studies, a fully reported outcome can provide information about a missing outcome through their statistical relationship. Bayesian hierarchical modeling formalizes this approach by explicitly modeling within-study and between-study correlations [46] [47].
In practice, these models account for correlations through two primary approaches: copulas for modeling within-study correlations of multivariate outcomes, and joint modeling of multivariate random effects for between-study correlations [47]. The Bayesian framework incorporates prior distributions for parameters and updates these based on the observed data, providing posterior distributions that reflect uncertainty about the true effects while accounting for potential ORB [46]. When outcomes are missing not at random (MNAR) – the scenario most indicative of ORB – the borrowing of strength across correlated outcomes can partially correct the bias introduced by selective reporting [47].
Table 1: Key Mechanisms of Multivariate Models for Addressing ORB
| Mechanism | Statistical Implementation | Bias Reduction Context |
|---|---|---|
| Borrowing of information | Joint modeling of correlated outcomes | MAR and MNAR missingness mechanisms |
| Correlation modeling | Copulas for within-study correlations; multivariate random effects for between-study correlations | Accounts for outcome interdependencies |
| Hierarchical borrowing | Bayesian random effects structures | Improves precision and reduces selection effects |
| Full uncertainty propagation | Markov Chain Monte Carlo (MCMC) sampling | Properly accounts for missing data uncertainty |
Bayesian Multivariate MTC Model Specification
The Bayesian multivariate mixed treatment comparisons (MMTC) meta-analysis framework enables simultaneous synthesis of multiple outcomes across a network of treatments while accounting for potential ORB. The model specification below provides a protocol for implementation.
Data Structure and Notation
Consider a systematic review with ( i = 1, \ldots, I ) studies, ( k = 1, \ldots, K ) outcomes, and ( t = 1, \ldots, T ) treatments. Let ( \mathbf{y}{i,k} ) represent the observed effect sizes for outcome ( k ) in study ( i ), which may include missing values due to ORB. Studies compare subsets of treatments ( \mathcal{T}i \subseteq {1, \ldots, T} ), forming a connected network of treatment comparisons [47] [48].
The basic model for a multivariate network meta-analysis can be specified as:
[ \mathbf{y}i \sim MVN(\boldsymbol{\theta}i, \mathbf{S}_i) ]
where ( \mathbf{y}i ) is the vector of observed effects for study ( i ), ( \boldsymbol{\theta}i ) is the vector of true underlying effects for study ( i ), and ( \mathbf{S}_i ) is the within-study variance-covariance matrix [48]. The true effects are then modeled as:
[ \boldsymbol{\theta}i = \mathbf{X}i\boldsymbol{\delta} + \boldsymbol{\beta}_i ]
where ( \mathbf{X}i ) is the design matrix for study ( i ), ( \boldsymbol{\delta} ) represents the baseline treatment effects, and ( \boldsymbol{\beta}i ) are random effects following a multivariate distribution [47] [48].
Accounting for Between-Study and Within-Study Correlations
The model incorporates two levels of correlation critical for addressing ORB:
Within-study correlations: The covariance matrix ( \mathbf{S}_i ) captures correlations among outcomes within the same study. When within-study correlations are unreported, which is common in practice, the calibrated Bayesian composite likelihood approach can be employed to avoid specification of the full likelihood function [48].
Between-study correlations: The random effects ( \boldsymbol{\beta}i ) are modeled using a multivariate distribution: [ \boldsymbol{\beta}i \sim MVN(\mathbf{0}, \boldsymbol{\Sigma}) ] where ( \boldsymbol{\Sigma} ) is the between-study variance-covariance matrix, capturing heterogeneity across studies and correlations between treatment effects on different outcomes [47] [48].
Diagram 1: Bayesian multivariate model structure showing relationships between observed data, parameters, and distributions. The model accounts for correlations at multiple levels to address ORB.
Handling Missing Outcomes
The Bayesian framework naturally handles missing data through the MCMC algorithm, which imputes missing values at each iteration based on the observed data and model parameters [47]. For outcomes missing due to ORB (MNAR mechanism), the borrowing of information across correlated outcomes provides a partial correction. The model can be extended with selection models or pattern-mixture models for more explicit MNAR handling, though these require stronger assumptions [47].
Implementation Protocol
Data Preparation and Modeling Workflow
Implementing multivariate models to address ORB requires systematic data collection and model specification. The following workflow provides a step-by-step protocol:
Diagram 2: Implementation workflow for Bayesian multivariate models to address ORB, showing key steps from data preparation to model validation.
Analytical Procedure
Model Specification: Define the multivariate random-effects model appropriate for the data type (e.g., binary, continuous). For binary outcomes, the model can be specified on the log-odds ratio scale with appropriate link functions [47].
Prior Elicitation: Select weakly informative priors for baseline effects and variance parameters. For variance-covariance matrices, consider Half-Normal, Half-Cauchy, or Wishart priors depending on the model structure [47] [48].
Computational Implementation: Implement models using Markov Chain Monte Carlo (MCMC) methods in Bayesian software such as Stan, JAGS, or specialized R packages. For complex networks with unavailable within-study correlations, implement the calibrated Bayesian composite likelihood approach with Open-Faced Sandwich adjustment to ensure proper posterior calibration [48].
Convergence Diagnostics: Assess MCMC convergence using Gelman-Rubin statistics, trace plots, and effective sample sizes. Run multiple chains with diverse starting values [47].
Model Checking: Perform posterior predictive checks to assess model fit. Compare residual deviance and deviance information criterion (DIC) between multivariate and univariate models [47].
Table 2: Research Reagent Solutions for Bayesian Multivariate Meta-Analysis
| Tool/Category | Specific Examples | Function in Addressing ORB |
|---|---|---|
| Statistical Software | R, Python, Stan, JAGS | Platform for implementing Bayesian multivariate models and MCMC sampling |
| Specialized Packages | gemtc, pcnetmeta, MBNMAtime in R |
Provide specialized functions for network meta-analysis and multivariate modeling |
| Computational Methods | MCMC, Hamiltonian Monte Carlo, Gibbs sampling | Enable estimation of complex multivariate models with correlated random effects |
| Prior Distributions | Half-Normal, Half-Cauchy, Wishart, Inverse-Wishart | Regularize estimation of variance-covariance parameters with limited data |
| Missing Data Methods | Bayesian multiple imputation, selection models | Explicitly handle outcome missingness mechanisms related to ORB |
Application Example: Alcohol Dependence Treatments
Case Study Implementation
The practical application of multivariate models for addressing ORB is illustrated by a systematic review of pharmacological treatments for alcohol dependence [47]. This review included 41 randomized trials assessing three primary outcomes: return to heavy drinking (RH), return to drinking (RD), and discontinuation (DIS). Substantial outcome reporting bias was present, with only 13 of 41 trials reporting RH, 34 reporting RD, and 38 reporting DIS [47].
The multivariate MTC model was specified as follows:
- Outcomes: RH, RD, DIS (all binary)
- Treatments: Placebo, acamprosate (ACA), naltrexone (NAL), and combination treatments
- Model: Bayesian multivariate random-effects MTC model with probit link function
- Correlation structure: Within-study correlations modeled using copulas; between-study correlations modeled via multivariate random effects
- Prior distributions: Non-informative priors for basic parameters; Wishart priors for precision matrices
The analysis demonstrated that by borrowing information across correlated outcomes, the multivariate model could include all 41 trials in the analysis, whereas univariate analyses would exclude studies with missing outcomes, potentially exacerbating ORB [47].
Protocol for Outcome Reporting Assessment
To systematically evaluate and address ORB in systematic reviews, implement the following assessment protocol:
Outcome Completeness Evaluation:
- Document all outcomes specified in trial protocols or registry entries
- Compare with outcomes reported in published articles
- Classify outcomes as: fully reported, partially reported, qualitatively reported, or unreported [49]
Risk of Bias Assessment:
Statistical Testing for ORB:
Performance and Validation
Simulation studies demonstrate that multivariate MTC models can substantially reduce the impact of ORB across various missingness scenarios [47]. When outcomes are missing at random, multivariate models provide more efficient estimates with narrower credible intervals compared to univariate approaches. Under missing not at random mechanisms indicative of ORB, multivariate models reduce bias in treatment effect estimates, particularly when correlations between outcomes are moderate to strong [47].
The performance of these models depends on several factors:
Correlation strength: Stronger correlations between outcomes lead to more effective borrowing of information and greater bias reduction [47]
Missingness mechanism: Models perform best when at least one outcome is consistently reported across studies, providing an anchor for borrowing information [47]
Network connectivity: Densely connected treatment networks with multiple common comparators enhance the ability to estimate both direct and indirect treatment effects [48]
Sensitivity analyses should assess robustness to prior specifications, particularly for variance-covariance parameters, and to assumptions about missing data mechanisms [47] [48]. The calibrated Bayesian composite likelihood approach has shown promising performance when within-study correlations are unknown, maintaining coverage probabilities close to nominal levels while reducing computational burden [48].
Bayesian multivariate models provide a powerful methodological framework for addressing outcome reporting bias in systematic reviews and network meta-analyses. By leveraging correlations among multiple outcomes, these models enable borrowing of information that mitigates the impact of selectively reported outcomes. The implementation protocols outlined in this application note offer researchers practical guidance for applying these methods, with particular utility for evidence synthesis in fields where multiple correlated outcomes are common, such as mental health, cardiology, and comparative effectiveness research.
Future methodological developments should focus on improving computational efficiency for large networks, enhancing MNAR handling mechanisms, and developing standardized reporting guidelines for multivariate meta-analyses. As clinical trials increasingly measure multiple endpoints, multivariate approaches will become increasingly essential for producing unbiased treatment effect estimates and valid clinical recommendations.
Handling Sparse Networks and Multi-Arm Trials
In the field of comparative effectiveness research, sparse networks and multi-arm trials present significant methodological challenges for evidence synthesis. A sparse network occurs when the available clinical evidence has many comparisons with limited or no direct head-to-head trials, creating an interconnected web with insufficient data across treatment comparisons [50]. Simultaneously, multi-arm trials (studies comparing three or more interventions) introduce complex dependency structures that require specialized statistical handling [51]. These challenges are particularly acute in drug development, where researchers must make informed decisions about multiple treatment options despite limited direct comparison data.
Bayesian statistical models provide a powerful framework for addressing these challenges through their ability to incorporate prior knowledge, model complex dependence structures, and produce probabilistic statements about all treatment comparisons—even those lacking direct evidence [51]. Within this framework, mixed treatment comparisons (MTC), also known as network meta-analysis (NMA), enable the simultaneous synthesis of both direct and indirect evidence, offering a more comprehensive understanding of relative treatment effects across a network of interventions [51]. This approach is especially valuable in sparse data environments where traditional pairwise meta-analyses would be underpowered or impossible due to missing direct comparisons.
The integration of Bayesian non-parametric (BNP) methods and graph-based computational techniques has further enhanced our ability to handle sparse networks by introducing greater flexibility in modeling assumptions and improving computational efficiency for large, irregular network structures [50] [52]. These advanced methodologies allow researchers to account for heterogeneity, detect inconsistency between direct and indirect evidence, and provide more reliable treatment effect estimates even when data are limited.
Theoretical Foundations
Bayesian Network Meta-Analysis
Bayesian Network Meta-Analysis extends traditional pairwise meta-analysis to simultaneously compare multiple treatments while synthesizing both direct and indirect evidence [51]. The fundamental concept relies on constructing a network where nodes represent treatments and edges represent direct comparisons from clinical trials. By leveraging this network structure, NMA provides coherent relative treatment effect estimates between all interventions, even those never directly compared in head-to-head trials.
The statistical foundation of NMA rests on the consistency assumption, which posits that direct and indirect evidence are in agreement—a particularly critical assumption in sparse networks where limited data may challenge its verification [51]. For a network with K treatments, the core model specifies that the observed effect size ( y_{ij} ) for a comparison between treatments i and j in a study s follows a normal distribution:
[ y{ij,s} \sim N(\theta{ij}, \sigma_{ij}^2) ]
where ( \theta_{ij} ) represents the true relative treatment effect (typically expressed as a log odds ratio, log hazard ratio, or mean difference), and the linear model satisfies the consistency relationship:
[ \theta{ij} = \mu{i} - \mu_{j} ]
Here, ( \mu_{i} ) represents the underlying effect of treatment i, often with a reference treatment set to zero for identifiability [51].
Handling Sparse Networks
Sparsity in network meta-analysis occurs when the evidence matrix contains many empty or data-poor cells, meaning many treatment pairs lack direct comparison data [50]. This sparsity manifests in several forms:
- Comparison sparsity: Limited or no direct evidence for specific treatment pairs
- Trial sparsity: Few studies available for existing comparisons
- Outcome sparsity: Missing outcome data within studies
In Bayesian NMA, several methodological approaches address these sparsity challenges:
Hierarchical modeling utilizes shrinkage estimators to borrow strength across the network, pulling estimates of imprecise comparisons toward the network mean [51]. This approach is particularly valuable in sparse networks as it prevents overfitting and produces more stable estimates for data-poor comparisons.
Bayesian non-parametric methods offer enhanced flexibility by allowing data to determine the functional form of relationships rather than imposing strict parametric assumptions [52]. These approaches are especially valuable for modeling complex effect moderators and heterogeneity patterns that may be obscured in sparse data.
Power priors and informative prior distributions can incorporate external evidence or clinical expertise to stabilize estimates in data-sparse regions of the network [51]. However, these require careful specification and sensitivity analysis to avoid introducing bias.
Multi-Arm Trial Incorporation
Multi-arm trials contribute unique methodological challenges because they introduce correlation between treatment effects estimated from the same study [51]. Properly accounting for this correlation structure is essential for valid inference in network meta-analysis.
The standard approach models the vector of relative effects from a multi-arm trial i with a multivariate normal distribution:
[ \mathbf{y}i \sim MVN(\boldsymbol{\theta}i, \boldsymbol{\Sigma}_i) ]
where the covariance matrix ( \boldsymbol{\Sigma}_i ) accounts for the fact that each treatment comparison within the trial shares a common reference group [51]. The covariance between any two comparisons j and k in a multi-arm trial with reference treatment A is given by:
[ Cov(y{AB}, y{AC}) = \sigma^2_A ]
where ( \sigma^2_A ) represents the variance of the reference treatment A.
Computational Framework and Software Tools
Bayesian Software Ecosystem
Implementing Bayesian models for sparse networks and multi-arm trials requires specialized software tools capable of handling complex hierarchical models and potentially high-dimensional parameter spaces. The table below summarizes key software packages relevant for these analyses:
Table 1: Bayesian Software Packages for Network Meta-Analysis and Sparse Data
| Software Package | Primary Language | Key Features | Sparse Network Capabilities |
|---|---|---|---|
| gCastle | Python | Causal structure learning, end-to-end pipeline | Graph neural networks for sparse pattern recognition [53] |
| bnlearn | R | Extensive BN algorithms, continuous development | Constraint-based algorithms for sparse data (PC, Grow-Shrink) [53] |
| Stan | C++ (interfaces in R, Python) | Hamiltonian Monte Carlo, flexible modeling | Robust sampling for high-dimensional sparse problems [51] |
| JAGS | C++ (interfaces in R) | Gibbs sampling, BUGS syntax | Efficient for moderately sparse networks [51] |
| Nimble | R | MCMC, model generation, programming | Custom algorithms for specific sparsity patterns [51] |
Graph Neural Networks for Sparse Structures
Graph Neural Networks (GNNs) offer a promising approach for analyzing sparse networks by representing the treatment comparison structure as a graph and leveraging node connectivity patterns to improve estimation [50]. In this framework:
- Nodes represent treatments
- Edges represent direct comparisons
- Node features encode trial characteristics or baseline risk information
- Message passing between connected nodes enables information sharing across the network
GNNs are particularly valuable for sparse matrix completion in network meta-analysis, as they can learn complex patterns of missingness and leverage both local and global network structure to impute missing comparisons [50]. The modular framework of GNNs allows extension to various network structures through user-provided generators, achieving up to 97% classification accuracy for identifying sparse matrix structures in representative applications [50].
Table 2: GNN Approaches for Sparse Network Challenges
| Sparsity Type | GNN Solution | Mechanism of Action |
|---|---|---|
| Adjacency sparsity | Graph convolutional networks | Leverage spectral graph theory to propagate information [50] |
| Neighborhood sparsity | Neighborhood sampling | Focus computation on relevant subgraphs [54] |
| Feature sparsity | Sparse feature learning | Identify latent representations in high-dimensional sparse features [54] |
Experimental Protocols and Application Notes
Protocol 1: Bayesian NMA for Sparse Networks
Objective: To conduct a valid network meta-analysis in the presence of substantial sparsity while providing accurate treatment effect estimates and uncertainty quantification.
Materials and Software:
- R statistical environment with
gemtcorBUGSnetpackages, or Python withgCastle[53] - Dataset formatted with columns: StudyID, Treatment, Response, SampleSize
- Prior distributions for model parameters
Procedure:
- Network Visualization and Exploration
- Create network diagram to visualize connectivity and identify sparse regions
- Calculate network statistics (number of studies per comparison, degree centrality)
- Identify potential evidence gaps using the DOT script below:
Model Specification
- Select appropriate likelihood function based on outcome type (binary, continuous, time-to-event)
- Define random-effects model accounting for heterogeneity
- Specify priors for basic parameters, heterogeneity variance, and multi-arm adjustment
Accounting for Sparsity
- Implement weakly informative or evidence-based priors for variance parameters
- Consider Bayesian model averaging across different heterogeneity assumptions
- Implement sensitivity analyses for influential priors
Computational Implementation
- Configure MCMC sampler with sufficient adaptation and burn-in iterations
- Run multiple chains to assess convergence
- Monitor convergence using Gelman-Rubin statistics and trace plots
Output and Interpretation
- Extract relative treatment effects with 95% credible intervals
- Calculate probability rankings and surface under cumulative ranking curve (SUCRA)
- Assess consistency between direct and indirect evidence
Troubleshooting Notes:
- For convergence issues, consider reparameterization or more informative priors
- For computational bottlenecks with large networks, implement approximation methods
- For implausibly wide credible intervals, consider Bayesian model averaging
Protocol 2: Bayesian Non-Parametric Multi-Treatment Models
Objective: To implement flexible Bayesian non-parametric models that accommodate complex effect modifications and permit ties between treatments with similar performance.
Materials and Software:
- Stan or Nimble for flexible Bayesian modeling [51]
- Dataset with individual patient data or aggregate study data
- Computational resources for MCMC sampling
Procedure:
Model Formulation
- Specify Bayesian non-parametric prior (e.g., Dirichlet process mixture)
- Define spike-and-slab components to permit treatment effect ties [51]
- Incorporate sharing mechanisms among related treatments
Computational Implementation
- Implement blocked Gibbs sampling or Polya urn scheme for posterior computation
- Configure appropriate hyperparameters for concentration parameters
- Run extended burn-in to ensure proper mixing
Treatment Clustering and Ranking
- Calculate posterior probabilities of treatment effect equality
- Generate conservative ranking sets that account for ordering uncertainty
- Identify treatment clusters with clinically equivalent effects
Application Context: This protocol is particularly suitable for networks with many treatments where some interventions may have negligible differences, creating challenges for definitive ranking [51].
Research Reagent Solutions
Table 3: Essential Analytical Tools for Sparse Network Meta-Analysis
| Tool/Category | Function | Example Implementations |
|---|---|---|
| Structure Learning Algorithms | Identify dependency structures in sparse networks | PC-stable, Grow-Shrink, Incremental Association Markov Blanket [53] |
| MCMC Samplers | Posterior inference for complex Bayesian models | Hamiltonian Monte Carlo, Gibbs sampling, Slice sampling [51] |
| Graph Neural Networks | Analyze sparse network structures and impute missing comparisons | Graph convolutional networks, message passing networks [50] |
| Consistency Evaluation | Assess agreement between direct and indirect evidence | Node-splitting, design-by-treatment interaction test [51] |
| Ranking Methods | Generate treatment hierarchies with uncertainty quantification | SUCRA, P-scores, rank probabilities [51] |
Case Study: Antidepressant Network Meta-Analysis
Application to Real-World Evidence
To illustrate the practical application of these methods, we examine a network meta-analysis of antidepressants originally reported by Cipriani et al. (2009) and reanalyzed using advanced Bayesian methods [51]. This dataset comprises 111 randomized controlled trials comparing 12 antidepressant treatments for major depression, with a focus on efficacy outcomes.
Network Characteristics:
- 12 treatments with multiple direct and indirect comparisons
- Mostly two-arm trials with two three-arm trials
- Fluoxetine (treatment 5) served as conventional reference with largest sample size
- Generally well-connected but with some comparisons lacking direct evidence [51]
Analytical Approach: The analysis employed a Bayesian non-parametric approach with spike-and-slab base measure to accommodate potential ties between treatments with similar efficacy [51]. This approach places positive probability on the event that two treatments have equal effects, providing more realistic ranking uncertainty.
Key Findings:
- The method successfully identified clusters of antidepressants with statistically indistinguishable efficacy
- Probability-based rankings provided more conservative interpretation than traditional SUCRA values
- Accounting for multiplicity reduced false positive rates in treatment comparisons
Workflow for Sparse Network Analysis
The following diagram illustrates the comprehensive workflow for analyzing sparse networks with multi-arm trials:
Advanced Methodological Considerations
Addressing Multiplicity and Ranking Uncertainty
Treatment ranking in network meta-analysis inherently involves multiple comparisons, which inflates false positive rates if not properly accounted for [51]. In a network with K treatments, there are K(K-1)/2 possible pairwise comparisons, creating substantial multiplicity challenges.
Bayesian multiplicity adjustment approaches include:
- Joint modeling of all treatment effects to properly account for their correlation structure
- Conservative ranking sets that remain silent about ordering when evidence is uncertain
- Decision-theoretic frameworks that incorporate clinical costs of misclassification
These approaches recognize that in sparse networks with many treatments, some ranking uncertainties may be irreducible with available data, and it is more scientifically honest to acknowledge these limitations than to produce potentially misleading precise rankings [51].
Non-Parametric Extensions for Complex Heterogeneity
Traditional Bayesian network meta-analysis models often assume normal random effects, which may be inadequate for capturing complex heterogeneity patterns in sparse networks [52]. Bayesian non-parametric mixtures address this limitation by:
- Allowing multimodal random effect distributions
- Automatically detecting outlier studies
- Facilitating identification of treatment-effect modifiers
- Providing robust inference when distributional assumptions are violated
These methods are particularly valuable in pediatric oncology and other specialized fields where limited trial data may exhibit complex heterogeneity patterns not adequately captured by standard models [52].
The analysis of sparse networks and multi-arm trials represents a methodologically challenging but increasingly important domain in evidence-based medicine. Bayesian methods provide a principled framework for addressing these challenges through their ability to incorporate prior information, model complex dependence structures, and quantify uncertainty from multiple sources.
The integration of advanced computational techniques including graph neural networks, Bayesian non-parametrics, and specialized MCMC algorithms has substantially enhanced our ability to derive meaningful insights from limited data. These approaches enable more realistic modeling of treatment similarities, more honest quantification of ranking uncertainties, and more efficient borrowing of information across sparse networks.
For researchers and drug development professionals, adopting these methodologies requires careful attention to model assumptions, computational implementation, and result interpretation. However, the substantial benefits—including more reliable treatment effect estimation in data-poor regions of the network and more realistic assessment of ranking uncertainty—make these approaches invaluable for informed decision-making in healthcare policy and clinical practice.
As the field continues to evolve, future methodological developments will likely focus on scaling these approaches to increasingly large treatment networks, integrating individual patient data and aggregate study data, and developing more user-friendly software implementations to make these powerful methods accessible to broader research communities.
Synthesizing Evidence from Mixed Biomarker Populations
The development of predictive genetic biomarkers in precision medicine has resulted in clinical trials conducted in mixed biomarker populations, posing a significant challenge for traditional meta-analysis methods that assume comparable populations across studies [55]. Early trials may be conducted in patients with any biomarker status without subgroup analysis, later trials may include subgroup analysis, and recent trials may enroll biomarker-positive patients only, creating an evidence base of mixed designs and patient populations across treatment arms [55].
This heterogeneity necessitates specialized evidence synthesis methods that can account for differential biomarker status across trials. For example, the development of Cetuximab and Panitumumab for metastatic colorectal cancer (mCRC) demonstrates this challenge, where retrospective analysis found patients with KRAS mutations did not benefit from EGFR-targeted therapies, leading to subsequent trials focusing only on KRAS wild-type patients [55]. The evidence base thus contains trials with mixed populations—some including both KRAS wild-type and mutant patients with no subgroup analysis, some with subgroup analysis, and some exclusively in wild-type populations [55].
Table 1: Classification of Evidence Synthesis Methods for Mixed Populations
| Method Category | Data Requirements | Key Applications | Statistical Considerations |
|---|---|---|---|
| Pairwise Meta-Analysis using Aggregate Data (AD) | Trial-level summary data | Combining evidence from studies comparing two interventions | Fixed-effect and random-effects models accommodating population heterogeneity |
| Network Meta-Analysis using AD | Trial-level summary data from multiple treatment comparisons | Comparing multiple treatments simultaneously while accounting for biomarker status | Incorporation of treatment-by-biomarker interactions |
| Network Meta-Analysis using AD and Individual Participant Data (IPD) | Combination of aggregate and individual-level data | Leveraging available IPD while incorporating AD studies | Enhanced adjustment for prognostic factors and standardization of analyses |
Core Analytical Approaches and Protocols
Bayesian Methods for Evidence Synthesis
Bayesian statistical frameworks provide particularly powerful approaches for synthesizing evidence from mixed populations by formally incorporating prior knowledge and explicitly modeling uncertainty. The Bayesian paradigm interprets probability as a degree of belief in a hypothesis that can be updated as new evidence accumulates, contrasting with frequentist approaches that define probability as the expected frequency of events across repeated trials [17].
The fundamental components of Bayesian analysis include:
- Priors: Probability distributions representing knowledge about parameters before observing current data
- Likelihood: The probability of observing the data given parameter values
- Posterior Distributions: Updated belief about parameters after combining prior knowledge with observed data
Bayesian methods are implemented using computational algorithms such as Markov Chain Monte Carlo (MCMC), with accessible software tools including JAGS, BUGS, STAN, and R packages like brms facilitating implementation [17] [16].
Individual Participant Data Meta-Analysis (IPDMA) Protocol
IPDMA represents the gold standard for evidence synthesis with mixed populations by allowing standardization of analyses and adjustment for relevant prognostic factors [55]. The protocol involves two primary approaches:
Two-Stage IPDMA Protocol:
- Stage 1: Analyze IPD from each trial separately to obtain treatment effect estimates and within-study variances
- Stage 2: Combine treatment effect estimates using conventional meta-analysis methods
One-Stage IPDMA Protocol:
- Analyze IPD from all studies simultaneously using hierarchical regression models:
yij ~ N(αi + δixij, σi²)for participant j in study iδi ~ N(d, τ²)for study-specific treatment effects
- Where yij is the observed outcome, xij is treatment assignment, αi is study-specific baseline, δi is treatment effect, d is summary treatment effect, and τ² is between-study variance
Personalized Treatment Recommendation (PTR) Development
For determining optimal treatment based on biomarker profiles, personalized treatment recommendations can be developed using randomized trial data [56]. The regression approach for PTR construction follows this protocol:
Model Specification: Fit a regression model with treatment-by-biomarker interactions:
Yi = α0 + αXi + Ai(β0 + βZi) + ei- Where X represents prognostic variables and Z represents moderating biomarkers
PTR Algorithm: Construct the treatment rule based on estimated interactions:
PTR = I(β0 + βZᵀ > 0)- Where I(·) is an indicator function recommending treatment when beneficial
Performance Validation: Estimate the population mean outcome under the PTR using:
μ{PTR} = 1/n Σ[(A + 1/2)·PTR + 1/2)/π Y + (1/2 - A)·(1/2 - PTR)/(1 - π) Y]
Data Presentation and Reporting Standards
Quantitative Data Presentation Protocols
Effective presentation of quantitative data from mixed population syntheses requires careful table design to facilitate comparisons and interpretation [57]. The following standards should be implemented:
Table Construction Principles:
- Right-flush alignment of numeric columns and their headers
- Consistent precision levels across all cells in a column
- Use of tabular fonts (Lato, Noto Sans, Roboto) to ensure vertical alignment
- Clear differentiation between prognostic and moderating biomarkers
- Explicit notation of biomarker status in each study population
Table Annotation Standards:
- Number all tables sequentially (Table 1, Table 2, etc.)
- Provide brief, self-explanatory titles
- Include clear column and row headings with measurement units
- Use footnotes for explanatory notes or additional information
- Present data in logical order (size, importance, chronological, alphabetical, or geographical)
Bayesian Reporting Quality Assessment
Transparent reporting of Bayesian analyses is essential for reproducibility and interpretation. The Reporting of Bayes Used in Clinical Studies (ROBUST) scale provides a validated framework for assessing quality [17].
Table 2: ROBUST Reporting Criteria for Bayesian Analyses
| Reporting Element | Assessment Criteria | Documentation Requirements |
|---|---|---|
| Prior Specification | Explicit description of prior distributions | Functional form, parameters, and justification of choices |
| Prior Justification | Rationale for selected priors | Clinical, empirical, or theoretical basis for priors |
| Sensitivity Analysis | Assessment of prior influence | Comparison of results under alternative prior specifications |
| Model Specification | Complete mathematical description | Likelihood, priors, and hierarchical structure |
| Computational Methods | Software and algorithm details | MCMC implementation, convergence diagnostics, sample sizes |
| Posterior Summaries | Central tendency and variance measures | Point estimates, credible intervals, and precision metrics |
Research Reagent Solutions and Computational Tools
Table 3: Essential Research Reagents and Computational Tools
| Tool/Reagent | Primary Function | Application Context |
|---|---|---|
| STAN | Probabilistic programming language | Flexible Bayesian modeling with Hamiltonian Monte Carlo |
| JAGS/BUGS | MCMC sampling engines | Bayesian analysis using Gibbs sampling and variants |
| brms R Package | Bayesian regression models | User-friendly interface for multilevel models in R |
| ROBUST Checklist | Reporting quality assessment | Ensuring transparent reporting of Bayesian analyses |
| Predictive Biomarker Panels | Patient stratification | Identifying treatment-effect modifiers in mixed populations |
| Prognostic Score Algorithms | Baseline risk adjustment | Controlling for confounding in treatment effect estimation |
Integrated Analytical Workflow
Implementation Considerations and Recommendations
Successful implementation of evidence synthesis methods for mixed biomarker populations requires careful consideration of several practical aspects:
Data Requirements and Accessibility:
- Methods utilizing IPD achieve superior statistical properties but require greater data access efforts
- Hybrid approaches combining AD and IPD can leverage available individual-level data while incorporating broader evidence bases
- Prospective planning for biomarker data collection across trials facilitates future syntheses
Computational Implementation:
- Bayesian methods require specification of prior distributions, with sensitivity analyses assessing their influence
- MCMC algorithms necessitate convergence diagnostics and sufficient iteration
- Reporting should follow ROBUST criteria to ensure transparency and reproducibility
Clinical Interpretation:
- Treatment effects should be interpreted in the context of biomarker status and between-study heterogeneity
- Probabilistic statements from Bayesian analyses provide direct clinical interpretability
- Personalized treatment recommendations should be validated in independent populations when possible
Within the framework of research applying Bayesian Mixed Treatment Comparisons (MTCs), robust model assessment is not merely a statistical formality but a fundamental pillar of credible inference. MTC models, also known as network meta-analyses, synthesize evidence from a network of clinical trials to compare multiple treatments simultaneously, often utilizing Bayesian hierarchical models [30]. The complexity of these models, typically fitted using Markov chain Monte Carlo (MCMC) methods, necessitates rigorous evaluation on two fronts: convergence and fit [58] [59]. Convergence diagnostics ensure that the MCMC sampling algorithm has adequately explored the posterior distribution, providing stable and trustworthy results. Fit assessment, often involving metrics like the Deviance Information Criterion (DIC) and its components, helps determine how well the model explains the data while penalizing for complexity, guiding model selection among competing alternatives [30]. For researchers, scientists, and drug development professionals, a transparent and thorough reporting of these steps is crucial for the reproducibility and reliability of their conclusions, which can directly inform healthcare decisions [59].
Theoretical Foundations: DIC and pD
The Deviance Information Criterion (DIC) is a Bayesian model comparison tool that balances model fit with complexity. It is particularly useful in hierarchical models, such as those used in MTCs, where the effective number of parameters is not straightforward. The DIC is calculated from the posterior distribution of the deviance, which is -2 times the log-likelihood.
The formula for DIC is: DIC = D(θ̄) + 2pD Or equivalently: DIC = D̄ + pD
Where:
- D(θ̄) is the deviance evaluated at the posterior mean of the parameters.
- DÌ„ is the posterior mean of the deviance.
- pD is the effective number of parameters, representing model complexity.
pD is calculated as: pD = D̄ - D(θ̄). A larger pD indicates a more complex model that is more prone to overfitting. When comparing models, a lower DIC value suggests a better trade-off between model fit and complexity. The following table summarizes the core components of DIC.
Table 1: Core Components of the Deviance Information Criterion (DIC)
| Component | Notation | Description | Interpretation |
|---|---|---|---|
| Posterior Mean Deviance | DÌ„ | The average deviance across posterior samples. | Measures how well the model fits the data; lower values indicate better fit. |
| Deviance at Posterior Mean | D(θ̄) | The deviance calculated using the average of the posterior parameter estimates. | An alternative measure of model fit. |
| Effective Number of Parameters | pD | pD = D̄ - D(θ̄) | Quantifies model complexity. Accounts for parameters that are constrained by priors or hierarchical structures. |
| Deviance Information Criterion | DIC | DIC = D̄ + pD or DIC = D(θ̄) + 2pD | Overall measure of model quality. Lower DIC values indicate a better-performing model that balances fit and parsimony. |
In the context of MTCs, random-effects models inherently have a higher pD than fixed-effects models due to the additional heterogeneity parameter (Ï„), which accounts for between-study variation. Therefore, DIC is essential for determining whether the increased complexity of a random-effects model is justified by a substantially better fit to the data [30] [60].
Experimental Protocol for MCMC Convergence Assessment
Ensuring MCMC convergence is a critical first step before any inference or model comparison can be trusted. The following protocol provides a detailed methodology for assessing convergence in a Bayesian MTC analysis.
Table 2: Key Research Reagents and Software for Bayesian MTC Analysis
| Category | Item | Function in Analysis |
|---|---|---|
| Statistical Software | R (with RStan, brms, packages) / Python (with PyStan) / JASP | Primary environment for data manipulation, model fitting, and result visualization. |
| Stan | State-of-the-art platform for Bayesian inference using Hamiltonian Monte Carlo (HMC) and NUTS sampler. | |
| OpenBUGS / JAGS | Alternative Bayesian software using Gibbs sampling; useful for cross-verification. | |
| Computational Resources | Multi-core processor (CPU) | Enables parallel computation of multiple MCMC chains, drastically reducing computation time. |
| High-performance computing (HPC) cluster | Essential for very large models or massive datasets. |
Protocol 1: Convergence Diagnostics for MCMC Sampling
Objective: To verify that MCMC sampling algorithms have converged to the target posterior distribution for all parameters of interest in a Mixed Treatment Comparison model.
Workflow Overview:
Step-by-Step Methodology:
Model Specification and Prior Elicitation:
- Specify the Bayesian MTC model using the generalized linear modeling framework, typically with random effects to account for between-study heterogeneity [30].
- Clearly define and justify prior distributions for all parameters. For MTCs, this includes priors for treatment effect parameters, study-specific baselines (if applicable), and the heterogeneity parameter (Ï„). Common choices are non-informative (flat) normal priors for treatment effects and a uniform prior for the heterogeneity standard deviation [30].
MCMC Simulation Setup:
- Initialize multiple independent MCMC chains (a minimum of 3 is standard, but 4 is highly recommended [59]) from dispersed starting points in the parameter space to ensure the chains are exploring the same posterior distribution from different regions [30].
- Set the total number of iterations per chain. The required number is problem-dependent but should be sufficient to achieve convergence and obtain a precise posterior estimate.
- Define a warm-up (also known as burn-in) period. This is an initial set of iterations that are discarded to ensure the sampler is not influenced by its starting values. For example, a protocol might use 20,000 warm-up iterations followed by 100,000 sampling iterations [30].
Compute Convergence Diagnostics:
- Gelman-Rubin Statistic (R-hat): Calculate the potential scale reduction factor (R-hat) for all key parameters. This statistic compares the variance within chains to the variance between chains. As convergence is achieved, the R-hat value should approach 1.0 [30] [59].
- Trace Plots: Visually inspect trace plots for key parameters (e.g., treatment effects, heterogeneity Ï„). A well-converged chain will look like a "fat, hairy caterpillar," showing stable variation around a constant mean without any pronounced trends or drifts [58] [30].
- Autocorrelation Plots: Examine autocorrelation plots. High autocorrelation within chains indicates slow mixing, meaning the sampler is not exploring the posterior distribution efficiently. The autocorrelation should drop to zero quickly as the lag increases.
- Effective Sample Size (ESS): Calculate the ESS. This estimates the number of independent samples equivalent to the autocorrelated MCMC samples. A higher ESS is better, and it should be sufficiently large (often > 400 per chain is a rough guideline) to ensure precise estimates of the posterior mean and quantiles [59].
Interpretation and Decision:
- Convergence is achieved if R-hat values for all parameters of interest are less than 1.05 (with a value of 1.01 being ideal) [59], trace plots show good mixing, and ESS is adequate.
- If convergence fails, increase the number of iterations, extend the warm-up period, or consider reparameterizing the model to improve sampling efficiency. The use of Hamiltonian Monte Carlo (HMC) samplers, as implemented in Stan, can often improve convergence for complex models compared to traditional Gibbs samplers [61] [62].
Experimental Protocol for Model Fit and Comparison
Once convergence is established, the next step is to assess and compare the fit of competing models.
Protocol 2: Model Fit Assessment and Comparison using DIC
Objective: To evaluate the goodness-of-fit of a Bayesian MTC model and compare it against alternative models (e.g., fixed-effects vs. random-effects) using the Deviance Information Criterion (DIC).
Workflow Overview:
Step-by-Step Methodology:
Define Candidate Models:
- Specify a set of plausible models for comparison. In an MTC, the most fundamental comparison is often between:
- Fixed-Effects Model: Assumes a single true effect size for all studies (i.e., no heterogeneity, Ï„ = 0).
- Random-Effects Model: Allows true effect sizes to vary across studies, assuming they follow a distribution (e.g., Normal(μ, τ²)) [60].
- Specify a set of plausible models for comparison. In an MTC, the most fundamental comparison is often between:
Ensure Convergence:
- Run the MCMC sampling for each candidate model independently.
- Apply Protocol 1 to each model to ensure all have achieved satisfactory convergence. Do not compare DIC values from models that have not converged.
Calculate DIC and pD:
- Extract the posterior samples of the deviance for each model.
- Compute the posterior mean deviance (DÌ„).
- Compute the deviance at the posterior mean of the parameters (D(θ̄)).
- Calculate the effective number of parameters (pD = D̄ - D(θ̄)).
- Finally, calculate the DIC (DIC = DÌ„ + pD).
Compare and Interpret Results:
- Create a comparison table for all candidate models. The model with the lowest DIC is typically preferred.
- A difference in DIC (ΔDIC) of less than 2-3 is usually considered negligible. A ΔDIC of 3-7 suggests the worse model has substantially less support, and a ΔDIC greater than 10 indicates essentially no support for the worse model.
- Interpret the pD value to understand model complexity. The random-effects model should have a higher pD than the fixed-effects model due to the additional heterogeneity parameter.
Supplementary Fit Checks:
- Posterior Predictive Checks: Simulate new data from the posterior predictive distribution and compare it to the observed data. A good model should generate data that looks similar to the observed data. Systematic discrepancies indicate model lack-of-fit [59].
- Residual Analysis: Examine residuals (if applicable) to check for patterns that suggest poor fit.
Table 3: Illustrative DIC Comparison for MTC Models
| Model Type | D̄ | pD | DIC | ΔDIC | Interpretation |
|---|---|---|---|---|---|
| Fixed-Effects MTC | 125.4 | 12.1 | 137.5 | 8.2 | Substantially less supported than the random-effects model. |
| Random-Effects MTC | 115.8 | 21.9 | 137.7 | 8.4 | |
| Random-Effects MTC with Covariate | 107.6 | 20.1 | 127.7 | 0.0 | Preferred model. Best fit-complexity trade-off. |
Application in Mixed Treatment Comparison
In a real-world MTC analyzing second-generation antidepressants, a Bayesian analysis might proceed as follows. The researcher would specify a random-effects model, using non-informative priors for treatment effect parameters and a uniform prior for the heterogeneity [30]. After running 4 MCMC chains for 100,000 iterations following the outlined protocols, they would confirm convergence via R-hat statistics below 1.05 and non-trending trace plots.
Subsequently, the DIC of this random-effects model would be compared to that of a fixed-effects model. A meaningfully lower DIC for the random-effects model would provide strong evidence to account for between-study heterogeneity. This robust model assessment protocol ensures that the resulting treatment effect estimates and rankings, which may inform clinical guidelines, are derived from a well-fitting and stable model.
The growing complexity of healthcare interventions and the emphasis on personalized medicine have created new challenges for traditional evidence synthesis methods. Meta-analysis, which traditionally relies on aggregate data (AD) from published study reports, faces limitations when dealing with mixed patient populations and targeted therapies. The integration of individual participant data (IPD) with AD has emerged as a powerful approach to enhance the precision and scope of treatment effect estimates, particularly within Bayesian network meta-analysis (NMA) frameworks. This integration enables researchers to conduct more detailed subgroup analyses, evaluate predictive biomarkers, and address questions that cannot be adequately answered using AD alone.
The fundamental challenge addressed by IPD-AD integration is the synthesis of evidence from trials conducted in mixed biomarker populations. For example, in metastatic colorectal cancer, the development of treatments like Cetuximab and Panitumumab resulted in an evidence base consisting of trials with varying population characteristics: some included patients with any biomarker status without subgroup analysis, others conducted subgroup analyses by biomarker status, and more recent trials enrolled only biomarker-positive patients [55]. This heterogeneity makes traditional meta-analysis problematic because it relies on the assumption of comparable populations across studies. IPD integration helps overcome this limitation by allowing more nuanced analysis of treatment effects across patient subgroups.
Methodological Foundations of IPD and AD Integration
Data Types and Their Properties
Aggregate Data (AD) refers to study-level summary statistics extracted from published trial reports, such as odds ratios, hazard ratios, or mean differences with their confidence intervals. Traditional pairwise meta-analysis and network meta-analysis have primarily utilized AD, which limits the complexity of analyses that can be performed, particularly for subgroup analyses and adjustment for prognostic factors [55].
Individual Participant Data (IPD) comprises raw, patient-level data from clinical trials, providing detailed information about each participant's characteristics, treatments received, and outcomes. The gold standard for meta-analysis is generally considered to be IPD meta-analysis, as it allows for improved data quality and scope, adjustment of relevant prognostic factors, and standardization of analysis across trials [55].
Table: Comparison of Aggregate Data and Individual Participant Data
| Characteristic | Aggregate Data (AD) | Individual Participant Data (IPD) |
|---|---|---|
| Data Structure | Study-level summary statistics | Patient-level raw data |
| Analysis Flexibility | Limited to available summaries | Enables complex modeling and subgroup analysis |
| Prognostic Factor Adjustment | Not possible | Allows adjustment for patient-level characteristics |
| Data Standardization | Challenging due to varying reporting standards | Possible through uniform data cleaning and analysis |
| Resource Requirements | Lower cost and time requirements | Significant resources for data collection and processing |
| Common Sources | Published literature, trial registries | Original trial databases, EHRs, digitized curves |
Bayesian Framework for Data Integration
Bayesian methods provide a natural framework for integrating IPD and AD within evidence synthesis models. The Bayesian approach allows for flexible hierarchical modeling and naturally accommodates the complex data structures arising from mixed sources of evidence. In the context of NMA, Bayesian models enable the simultaneous incorporation of both direct and indirect evidence while accounting for different levels of uncertainty in IPD and AD sources [63].
The fundamental hierarchical structure of Bayesian models for IPD-AD integration can be specified as follows. For a binary outcome, let $y{it}$ represent the number of events for treatment $t$ in study $i$, and $n{it}$ the total number of participants. The first stage assumes a binomial likelihood:
$$ y{it} \sim \text{Binomial}(p{it}, n_{it}) $$
where $p_{it}$ represents the probability of an event for treatment $t$ in study $i$ [64]. The second stage then models these probabilities, incorporating both IPD and AD through appropriate linking functions and random effects that account for between-study heterogeneity.
Analytical Approaches and Models
One-Stage and Two-Stage Approaches for IPD Meta-Analysis
IPD meta-analysis can be conducted using either one-stage or two-stage approaches, each with distinct advantages and limitations. The two-stage approach first analyzes IPD from each study separately to obtain study-specific treatment effect estimates ($\hat{\delta}i$) and within-study variances ($\sigmai^2$). In the second stage, these estimates are combined using conventional meta-analysis techniques [55]. This approach allows for standardization of inclusion criteria, outcome definitions, and statistical methods across studies, but may not fully leverage the individual-level nature of the data.
The one-stage approach analyzes IPD from all studies simultaneously using a hierarchical regression model:
$$ y{ij} \sim N(\alphai + \deltai x{ij}, \sigma_i^2) $$
$$ \delta_i \sim N(d, \tau^2) $$
where $y{ij}$ and $x{ij}$ represent the outcome and treatment assignment for participant $j$ in study $i$, $\alphai$ is the study-specific intercept, $\deltai$ is the study-specific treatment effect, $d$ is the overall treatment effect, and $\tau^2$ represents between-study heterogeneity [55]. The one-stage approach more fully accounts for the hierarchical structure of the data but requires more complex implementation and computational resources.
Models for Mixed Populations and Predictive Biomarkers
When synthesizing evidence from trials with mixed biomarker populations, specialized models are needed to account for variation in subgroup reporting across studies. One approach involves modeling treatment effects within biomarker subgroups, combining evidence from trials that provide subgroup analyses with those that enroll only specific subgroups [55].
For time-to-event outcomes, a Bayesian framework can be developed to evaluate predictive biomarkers by combining IPD from digital sources (such as electronic health records or digitized Kaplan-Meier curves) with AD from published trials [63]. This approach allows for estimation of treatment effects in subgroups defined by biomarker status and has been shown to reduce uncertainty in subgroup-specific treatment effect estimates by up to 49% compared to using AD alone [63].
Table: Methods for Evidence Synthesis of Mixed Populations
| Method Type | Data Requirements | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| Pairwise MA using AD | Aggregate data | Traditional treatment comparisons | Simplicity, wide applicability | Cannot handle mixed populations effectively |
| Network MA using AD | Aggregate data | Multiple treatment comparisons | Incorporates indirect evidence | Limited subgroup analysis capabilities |
| Network MA using AD and IPD | Combined AD and IPD | Predictive biomarker evaluation | Enhanced precision, subgroup analysis | Complex implementation, data access challenges |
Experimental Protocols and Workflows
Protocol for IPD-AD Integration in Bayesian NMA
Objective: To develop a comprehensive protocol for integrating IPD and AD within a Bayesian NMA framework for evaluating treatment effectiveness in predictive biomarker subgroups.
Materials and Software Requirements:
- Statistical software with Bayesian modeling capabilities (Stan, JAGS, or similar)
- R, Python, or similar programming environment
- Data management tools for harmonizing IPD from multiple sources
Procedure:
Data Collection and Preparation
- Identify relevant studies through systematic literature review
- Obtain IPD from available sources (clinical trial databases, EHRs, or digitized curves)
- Extract AD from published reports for studies where IPD is unavailable
- Harmonize variables across studies to ensure consistency
Model Specification
- Define appropriate likelihood functions for the outcome type (binary, continuous, time-to-event)
- Specify priors for model parameters based on previous knowledge or use weakly informative priors
- Implement hierarchical structure to account for between-study heterogeneity
- Include interaction terms for biomarker-treatment interactions where relevant
Model Implementation
- Code model in selected Bayesian programming environment
- Run Markov Chain Monte Carlo (MCMC) sampling with appropriate number of iterations and chains
- Assess convergence using diagnostic statistics (Gelman-Rubin statistic, trace plots)
Model Checking and Validation
- Perform posterior predictive checks to assess model fit
- Conduct sensitivity analyses to evaluate impact of prior choices
- Compare models using appropriate criteria (DIC, WAIC, or LOO-CV)
Results Interpretation and Reporting
- Extract posterior summaries for parameters of interest
- Visualize results using appropriate plots (forest plots, surface under the cumulative ranking curves)
- Report estimates with credible intervals and measures of heterogeneity
Protocol for Predictive Biomarker Evaluation Using Digital Source IPD
Objective: To evaluate predictive biomarkers by incorporating IPD from digital sources with AD in a Bayesian network meta-analytic model.
Materials:
- Electronic health records or other digital source data
- Software for digitizing Kaplan-Meier curves (where necessary)
- Bayesian analysis software with survival modeling capabilities
Procedure:
IPD Sourcing and Preparation
- Emulate target trials using electronic health records with appropriate methodology
- Digitize Kaplan-Meier curves from published studies where individual data unavailable
- Apply consistent inclusion/exclusion criteria across all data sources
- Define biomarker subgroups using consistent classification rules
Model Development
- Specify time-to-event model (e.g., Cox proportional hazards model) for the outcome
- Implement network meta-analysis structure for treatment comparisons
- Include biomarker-by-treatment interaction terms
- Account for correlation structure within studies
Analysis Implementation
- Code model in Bayesian software with appropriate sampling algorithms
- Run extended MCMC sampling to ensure convergence
- Validate model using posterior predictive checks
Results Synthesis
- Estimate biomarker-specific treatment effects with credible intervals
- Compare precision of estimates with and without IPD incorporation
- Calculate relative reduction in uncertainty through IPD inclusion
Visualization Approaches for Complex Evidence Structures
As evidence networks grow more complex with the inclusion of multiple components and mixed data sources, effective visualization becomes crucial for understanding the evidence structure and communicating results. Traditional network diagrams often prove inadequate for representing complex component network meta-analysis (CNMA) structures with numerous components and potential combinations [35].
Novel visualization approaches have been developed to address these challenges:
- CNMA-UpSet Plots: Present arm-level data and are particularly suitable for networks with large numbers of components or component combinations
- CNMA Heat Maps: Inform decisions about which pairwise interactions to consider including in CNMA models
- CNMA-Circle Plots: Visualize combinations of components that differ between trial arms and offer flexibility in presenting additional information such as the number of patients experiencing outcomes of interest [35]
These visualization techniques help researchers understand which components have been tested together in trials, identify gaps in the evidence base, and guide model selection by illustrating which interactions can be estimated given the available data.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials and Tools for IPD-AD Integration Research
| Research Tool | Function | Example Applications |
|---|---|---|
| Bayesian Modeling Software (Stan, JAGS, WinBUGS) | Enables implementation of complex hierarchical models | Fitting Bayesian NMA models with IPD-AD integration |
| Statistical Programming Environments (R, Python) | Provides data manipulation, analysis, and visualization capabilities | Data harmonization, model specification, result visualization |
| Electronic Health Record Systems | Source of real-world IPD for analysis | Target trial emulation, biomarker validation |
| Digitization Software | Extracts numerical data from published curves and figures | Converting Kaplan-Meier curves to IPD for inclusion in analysis |
| Data Harmonization Tools | Standardizes variables across different data sources | Creating consistent variable definitions across studies |
| MCMC Diagnostic Tools | Assesses convergence of Bayesian models | Evaluating model performance, identifying convergence issues |
Application in Drug Development and Personalized Medicine
The integration of IPD and AD has particular relevance in drug development, where it can enhance the evaluation of targeted therapies and predictive biomarkers. In metastatic colorectal cancer, for example, the integration of IPD has allowed more precise evaluation of EGFR inhibitors in KRAS wild-type versus mutant patients [63]. Similarly, in breast cancer, this approach has been used to assess whether taxanes show differential effectiveness in hormone receptor-positive and negative patients [63].
The use of IPD from digital sources, such as electronic health records, represents an innovative approach to expanding the evidence base for treatment evaluation. When employing EHR data, it is essential to use appropriate methodology such as target trial emulation to minimize biases inherent in observational data [63]. The incorporation of such digital source IPD can complement evidence from randomized controlled trials and may be particularly valuable when RCT evidence is limited or when studying long-term outcomes not captured in traditional trials.
From a regulatory perspective, integrated IPD-AD analyses can provide stronger evidence for biomarker qualification and help identify patient subgroups most likely to benefit from specific treatments. This is particularly important in the context of precision medicine, where treatments are increasingly targeted to specific molecular subgroups.
The integration of individual participant data and aggregate data within Bayesian network meta-analysis represents a significant methodological advancement in evidence synthesis. This approach enables more precise estimation of treatment effects, particularly in biomarker-defined subgroups, and facilitates the evaluation of complex research questions that cannot be adequately addressed using aggregate data alone. While implementation challenges exist, particularly regarding data access and modeling complexity, the potential benefits for drug development and personalized medicine make this an important methodology for researchers and drug development professionals to master.
As the field evolves, continued development of statistical methods, visualization techniques, and standardized protocols will further enhance our ability to integrate diverse data sources and generate robust evidence for healthcare decision-making. The application of these methods in drug development holds particular promise for advancing precision medicine by enabling more nuanced understanding of how treatment effects vary across patient subgroups.
Bayesian vs. Frequentist MTC: Validation and Real-World Impact
Mixed Treatment Comparisons (MTC), also known as Network Meta-Analysis (NMA), represents a powerful statistical extension of conventional pairwise meta-analysis, enabling the simultaneous comparison of multiple treatments based on both direct and indirect evidence [47] [65]. By synthesizing evidence from a network of randomized controlled trials (RCTs), this approach allows for the estimation of relative treatment effects between interventions that may never have been compared directly in head-to-head trials [66] [67]. The Bayesian framework for MTC has gained particular prominence, as it naturally incorporates uncertainty and facilitates the calculation of probabilistic statements about treatment rankings, which are highly valuable for clinical decision-making [66] [67].
The reliability of inferences drawn from a Bayesian MTC hinges on the operating characteristics of the model outputs—specifically, the coverage of credible intervals, the potential for bias in effect estimates, and the width of uncertainty intervals. These properties are not merely theoretical concerns; they are profoundly influenced by specific characteristics of the evidence network and the statistical model employed [67]. This application note provides a detailed, evidence-based overview of these key performance metrics, supported by structured data and practical protocols to guide researchers and drug development professionals in the application and critical appraisal of Bayesian MTCs.
Quantitative Performance of Bayesian Meta-Analytic Methods
The performance of Bayesian methods, particularly in challenging scenarios like the synthesis of rare events data, has been systematically evaluated against frequentist alternatives. The following table summarizes key findings from a 2025 simulation study that compared ten meta-analysis models, including three Bayesian approaches, on metrics of bias, interval width, and coverage [68].
Table 1: Performance of Meta-Analysis Models for Binary Outcomes (including Rare Events)
| Model Name | Model Type | Performance under Low Heterogeneity | Performance under High Heterogeneity | Key Findings |
|---|---|---|---|---|
| Beta-Binomial (Kuss) | Frequentist | Good performance | Generally performed well | Recommended for rare events meta-analyses [68]. |
| Bayesian Model (Hong et al.) | Bayesian (Beta-Hyperprior) | Good performance | Performed well, second to Kuss | A promising method for pooling rare events data [68]. |
| Binomial-Normal Hierarchical Model (BNHM) | Frequentist/Bayesian | Good performance | Performed well, followed Hong et al. | Suitable for rare events [68]. |
| Generalized Estimating Equations (GEE) | Frequentist | Did not perform well | Did not perform well | Performance was generally poor across scenarios [68]. |
The simulation results indicate that while several models perform adequately when between-study heterogeneity is low, performance degrades under conditions of high heterogeneity, with no model producing universally "good" performance in this challenging scenario [68]. Among the Bayesian approaches, the model incorporating a Beta-Hyperprior demonstrated robust performance, establishing Bayesian methods as a viable and often superior option for complex data synthesis tasks [68].
Key Experimental Protocols for Bayesian MTC
Implementing a Bayesian MTC involves a sequence of critical steps, from data preparation to model checking. The protocols below detail the core methodologies.
Data Preparation and Network Geometry Assessment
The initial phase involves structuring the data and understanding the evidence network.
Protocol 1: Data Extraction and Formatting
- Objective: To compile study-level summary data in a format suitable for Bayesian MTC.
- Procedure: Data can be extracted in one of two forms:
- Crucial Check: Ensure the transitivity assumption holds. This requires that the enrolled subjects in any given study would be eligible for enrollment in all other studies in the network. Violations occur if, for example, studies with different patient populations or co-interventions are inappropriately combined [66] [65].
Protocol 2: Network Geometry Evaluation
- Objective: To visualize and characterize the structure of the evidence network, identifying potential sources of bias.
- Procedure:
- Create a network graph where nodes represent treatments and edges represent direct comparisons.
- The size of nodes can be weighted by the total number of participants receiving that treatment, and the thickness of edges can be weighted by the number of studies making that direct comparison [67].
- Interpretation: Visually inspect for imbalances, such as an unequal number of studies per comparison or treatments that are only connected via long indirect paths. These features can influence bias and precision [67].
Model Formulation and Estimation
This protocol covers the core statistical modeling process.
- Protocol 3: Implementing a Bayesian Hierarchical Model
- Objective: To estimate relative treatment effects and rank probabilities while accounting for between-study heterogeneity.
- Model Specification: A common Bayesian hierarchical model for binary outcomes (arm-level data) can be specified as follows:
- Likelihood: ( r{ij} \sim \text{Binomial}(p{ij}, n{ij}) ), where ( r{ij} ) and ( n{ij} ) are the number of events and total sample size in arm ( j ) of study ( i ).
- Linear Predictor: ( \text{logit}(p{ij}) = \mui + \delta{i,j} \cdot I(\text{arm } j \neq \text{reference}) ). Here, ( \mui ) is the study-specific log-odds of the reference treatment (often modeled as a random effect), and ( \delta{i,j} ) is the study-specific log-odds ratio of treatment ( j ) versus the reference [47] [68].
- Random Effects: ( \delta{i,j} \sim N(d{t{j}} - d{t{1}}, \tau^2) ), where ( d{t} ) are the baseline parameters for each treatment relative to a common reference, and ( \tau^2 ) is the between-study heterogeneity variance [67].
- Estimation: Use Markov Chain Monte Carlo (MCMC) sampling in software like JAGS, BUGS, or Stan, often called from R [47] [66]. Run multiple chains and assess convergence using statistics like the Gelman-Rubin diagnostic.
Performance Validation and Critical Appraisal
After model estimation, it is essential to validate its performance and scrutinize the results.
Protocol 4: Assessing Key Performance Metrics
- Objective: To evaluate the coverage, bias, and precision of the model estimates.
- Procedures:
- Coverage: In simulation studies, determine the proportion of times the 95% credible interval for a treatment effect contains the true simulated value. Ideal coverage is 95% [68].
- Bias: Calculate the average difference between the estimated treatment effect and the true effect across simulations. Investigate sources of bias, such as unequal study distribution across comparisons, which can skew rank probabilities [67].
- Interval Width: Compute the average width of the 95% credible intervals across simulations. Narrower intervals indicate greater precision, but they must have the correct coverage to be trustworthy [68].
- Tool - Predictive Checking: Use posterior predictive checks to simulate new data under the fitted model and compare it to the observed data. Large discrepancies can indicate model misfit [69].
Protocol 5: Mitigating Bias in Treatment Ranking
- Objective: To critically interpret treatment rank probabilities, which are highly sensitive to network structure.
- Procedure: Be aware that an unequal number of studies per comparison can lead to biased rank probabilities. A treatment included in the fewest number of studies may have its rank probability biased upward, while a treatment in the most studies may have its rank underestimated [67].
- Recommendation: Always report and consider the geometry of the evidence network alongside rank probabilities. Decisions should not be based on rank probabilities alone but should be supported by the estimated effect sizes and their credible intervals [67].
Visualization of Workflows and Relationships
The following diagrams illustrate the core logical workflows and relationships in a Bayesian MTC.
Figure 1: Overall Workflow for a Bayesian MTC
Figure 2: Common Network Meta-Analysis Geometries
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of a Bayesian MTC requires both statistical software and a conceptual understanding of key components.
Table 2: Essential Toolkit for Bayesian Mixed Treatment Comparisons
| Tool/Component | Category | Function Description | Exemplars/Notes |
|---|---|---|---|
| MCMC Sampling Engine | Software | The computational core that performs Bayesian estimation by drawing samples from the posterior distribution. | JAGS, BUGS, Stan [66]. |
| Statistical Programming Environment | Software | Provides a framework for data management, model specification, and output analysis. | R (with packages like R2jags, gemtc, BUGSnet) [66] [67]. |
| Prior Distribution | Statistical Concept | Encodes pre-existing knowledge or uncertainty about a parameter before seeing the data. Critical for regularization. | Vague priors (e.g., ( N(0, 100^2) ) for log-OR) are common; informative priors can be used with justification [69]. |
| Hierarchical Model | Statistical Concept | The core model structure that accounts for both within-study sampling variation and between-study heterogeneity. | Allows borrowing of strength across studies in the network [47] [68]. |
| Heterogeneity Parameter (( \tau )) | Statistical Concept | Quantifies the amount of variability between studies beyond sampling error. | Its prior specification can influence results, particularly in sparse networks [47] [68]. |
| Rank Probability | Statistical Output | The probability, derived from the posterior distribution, that each treatment is the best, second best, etc. | Should be interpreted with caution due to sensitivity to network geometry [67]. |
In evidence-based medicine and pharmaceutical development, quantifying the uncertainty around effect estimates is equally as important as calculating the effects themselves. Interval estimates provide this crucial information, representing a range of values within which the true effect parameter is likely to fall. Two dominant statistical paradigms—frequentist and Bayesian—have developed fundamentally different approaches to interval estimation: confidence intervals and credible intervals. While both appear superficially similar as ranges with associated probability levels, their interpretations differ substantially in ways that critically impact decision-making in drug development [70].
The distinction between these intervals becomes particularly consequential when applying advanced statistical techniques like mixed treatment comparisons (MTC), also known as network meta-analysis. MTC methodologies allow for the simultaneous comparison of multiple treatments by combining direct and indirect evidence across a network of studies, providing a coherent framework for evaluating relative treatment efficacy when head-to-head trials are limited or unavailable [24] [13]. The choice between frequentist and Bayesian approaches for MTC analyses fundamentally shapes how results are calculated, interpreted, and applied in clinical decision-making.
Conceptual Foundations and Definitions
Confidence Intervals: The Frequentist Approach
In the frequentist framework, probability is defined as the long-term frequency of an event occurring when the same process is repeated multiple times. Frequentist methods regard population parameters (e.g., mean difference, odds ratio) as fixed, unvarying quantities, without probability distributions [71].
A confidence interval (CI) is constructed from sample data and has a specific long-run frequency interpretation. A 95% confidence interval means that if we were to draw many random samples from the same population and compute a 95% CI for each sample, then approximately 95% of these intervals would contain the true population parameter [70]. The confidence level (e.g., 95%) thus refers to the procedure used to create the interval, not to the specific realized interval [72] [71].
The interpretation of a frequentist 95% confidence interval is: "We can be 95% confident that the true (unknown) estimate would lie within the lower and upper limits of the interval, based on hypothesized repeats of the experiment" [70]. It is incorrect to interpret a specific 95% CI as having a 95% probability of containing the true parameter value, as the parameter is considered fixed and the interval is random in the frequentist framework.
Credible Intervals: The Bayesian Approach
The Bayesian framework conceptualizes probability differently, expressing a degree of belief in an event based on prior knowledge and observed data. Unlike frequentist methods, Bayesian approaches treat unknown parameters as random variables with probability distributions that represent uncertainty about their values [71].
A credible interval (CrI) is the Bayesian analogue of a confidence interval and represents a range of values within which an unobserved parameter falls with a particular probability [71] [70]. The Bayesian 95% credible interval has a more intuitive interpretation: "There is a 95% probability that the true (unknown) estimate would lie within the interval, given the evidence provided by the observed data" [70].
This direct probability statement is possible because Bayesian inference produces an entire posterior probability distribution for the parameter of interest. The 95% credible interval is simply the central portion of this posterior distribution that contains 95% of the probability [71].
Conceptual Comparison Through Analogy
The difference between these intervals can be illustrated through a heuristic example. Consider a clinical trial comparing a new drug to standard care:
A frequentist partisans might argue: "I want a method that works for ANY possible value of the parameter. I don't care about 99 values of the parameter that IT DOESN'T HAVE; I care about the one true value IT DOES HAVE." [72]
A Bayesian partisan might counter: "I don't care about 99 experiments I DIDN'T DO; I care about this experiment I DID DO. Your rule allows 5 out of the 100 to be complete nonsense as long as the other 95 are correct; that's ridiculous." [72]
This fundamental philosophical divergence manifests in practical differences in how evidence is accumulated and interpreted across studies, particularly relevant in drug development where decisions must be made based on all available evidence.
Statistical Properties and Interpretation
Comparative Properties of Confidence and Credible Intervals
Table 1: Key Characteristics of Confidence Intervals and Credible Intervals
| Characteristic | Confidence Interval (Frequentist) | Credible Interval (Bayesian) |
|---|---|---|
| Philosophical Basis | Long-term frequency of events | Degree of belief (subjective probability) |
| Parameter Status | Fixed, unknown constant | Random variable with probability distribution |
| Probability Statement | Refers to the procedure, not the parameter | Directly refers to the parameter value |
| Primary Interpretation | "95% of similarly constructed intervals would contain the true parameter" | "95% probability that the true parameter lies within this interval" |
| Prior Information | Does not formally incorporate prior knowledge | Explicitly incorporates prior knowledge via prior distribution |
| Computational Approach | Based on sampling distribution of estimator | Based on posterior distribution derived from Bayes' theorem |
| Data Considered | Only the actual observed data | The observed data combined with prior knowledge |
Practical Interpretation in Medical Research
Consider a randomized controlled trial investigating a new antidepressant where the outcome is treatment response rate, analyzed through both frameworks:
Frequentist Result: "The 95% CI for the odds ratio was 1.15 to 2.30."
- Interpretation: "We can be 95% confident that the interval from 1.15 to 2.30 contains the true odds ratio, based on hypothesized repeats of the experiment." [70]
Bayesian Result: "The 95% CrI for the odds ratio was 1.18 to 2.25."
- Interpretation: "There is a 95% probability that the true odds ratio lies between 1.18 and 2.25, given the observed data and prior distribution." [70]
The Bayesian interpretation provides a more direct probabilistic statement about the parameter, which many find more intuitive for decision-making [71] [70].
Application to Mixed Treatment Comparisons
Bayesian Framework for Mixed Treatment Comparisons
Mixed treatment comparison (MTC) analysis, also known as network meta-analysis, compares multiple interventions simultaneously by combining direct evidence (from head-to-head trials) and indirect evidence (through common comparators) [24] [13]. The Bayesian framework is particularly well-suited to MTC due to several advantages:
- Modeling flexibility in handling complex evidence networks with multiple treatments and various forms of data [30]
- Natural propagation of uncertainty through the entire network, resulting in appropriate precision estimates for all comparisons
- Ability to incorporate prior information on treatment effects or heterogeneity [30] [24]
- Straightforward calculation of probability statements for treatment rankings and decision-making [24]
In practice, Bayesian MTC analyses are typically implemented using Markov chain Monte Carlo (MCMC) methods in specialized software such as WinBUGS, OpenBUGS, or JAGS [30] [24]. These computational methods allow for fitting complex hierarchical models that would be challenging to implement using frequentist maximum likelihood approaches.
MTC Analysis Protocol: Bayesian Approach
Table 2: Experimental Protocol for Bayesian Mixed Treatment Comparison Analysis
| Protocol Step | Key Considerations | Reporting Guidelines |
|---|---|---|
| 1. Network Specification | Define all treatments and potential comparisons. Assess transitivity assumption. | Present network diagram showing all direct comparisons [13]. |
| 2. Model Specification | Choose fixed or random effects model. Specify likelihood and prior distributions. | Report prior distributions for all parameters, including rationale [59]. |
| 3. Prior Selection | Select appropriate priors for basic parameters, heterogeneity, and other hyperparameters. | Justify prior choices. Consider non-informative priors for primary analysis [30]. |
| 4. Computational Implementation | Set up MCMC sampling with sufficient iterations, burn-in period, and thinning. | Specify software, initial values, number of chains, and convergence diagnostics [59]. |
| 5. Convergence Assessment | Monitor convergence using trace plots, Gelman-Rubin statistics, and autocorrelation. | Report convergence diagnostics and ensure satisfactory convergence [30] [59]. |
| 6. Results Extraction | Extract posterior distributions for all treatment comparisons and ranking probabilities. | Present relative effects with credible intervals and ranking probabilities [24]. |
| 7. Consistency Assessment | Check for disagreement between direct and indirect evidence where possible. | Use node-splitting or other methods to assess inconsistency [13]. |
| 8. Sensitivity Analysis | Assess impact of prior choices, model assumptions, and potential effect modifiers. | Report sensitivity analyses, including alternative priors and models [59]. |
Workflow Visualization for Bayesian MTC Analysis
Figure 1: Workflow for conducting Bayesian mixed treatment comparison analysis with credible intervals, highlighting key steps from network specification to result interpretation.
The Scientist's Toolkit: Research Reagent Solutions
Essential Methodological Components for Bayesian MTC
Table 3: Key Research Reagents for Bayesian Mixed Treatment Comparison Analysis
| Research Reagent | Function/Purpose | Implementation Considerations |
|---|---|---|
| MCMC Sampling Algorithms | Generate samples from posterior distributions of model parameters | Gibbs sampling, Metropolis-Hastings; balance computational efficiency and convergence [30] |
| Prior Distributions | Quantify pre-existing knowledge or uncertainty about parameters before observing data | Non-informative priors (e.g., N(0,10000)) for primary analysis; sensitivity to prior choices should be assessed [30] [59] |
| Consistency Models | Ensure agreement between direct and indirect evidence sources in the network | Check using node-splitting approaches; inconsistency suggests violation of transitivity assumption [13] |
| Hierarchical Models | Account for heterogeneity across studies while borrowing strength | Random-effects models typically preferred; estimate between-study heterogeneity (τ²) [30] |
| Rank Probability Calculations | Estimate probability that each treatment is best, second best, etc. | Derived from posterior distributions; useful for decision-making but interpret with caution [24] |
| Convergence Diagnostics | Assess whether MCMC sampling has adequately explored posterior distribution | Gelman-Rubin statistic (R-hat < 1.05), trace plots, autocorrelation, effective sample size [59] |
Interpretation in Decision-Making Contexts
Clinical and Regulatory Interpretation
The distinction between confidence and credible intervals has significant implications for how evidence is interpreted in drug development and regulatory decision-making:
- Credible intervals facilitate direct probability statements about treatment effects, which can be more naturally integrated into risk-benefit assessments and value-based decisions [70]
- Bayesian approaches allow for explicit incorporation of prior evidence (e.g., from phase II trials) when designing and analyzing phase III studies, potentially increasing efficiency [59]
- In health technology assessment, Bayesian MTC provides a coherent framework for comparing multiple treatment options simultaneously, even when direct evidence is limited [24]
However, the subjective nature of prior specification in Bayesian analyses requires careful sensitivity analysis and transparent reporting, particularly in regulatory contexts where objectivity is paramount [59].
Logical Relationship Between Evidence Types in MTC
Figure 2: Logical relationships between evidence types, statistical assumptions, and resulting outputs in mixed treatment comparisons, highlighting how credible intervals are derived from combined evidence.
Understanding the distinction between confidence intervals and credible intervals is essential for appropriately interpreting results from mixed treatment comparisons and other advanced statistical analyses in medical research. While confidence intervals remain widely used and accepted in regulatory contexts, Bayesian approaches with credible intervals offer distinct advantages for complex evidence synthesis, particularly when multiple treatments need to be compared simultaneously.
The direct probabilistic interpretation of credible intervals aligns naturally with clinical decision-making needs, providing statements about the probability of treatment effects rather than long-run frequency properties. As drug development increasingly embraces Bayesian methods for their flexibility and efficiency, familiarity with both interval estimation approaches will remain crucial for researchers, clinicians, and decision-makers evaluating comparative treatment effectiveness.
The interpretation of clinical trial results traditionally relies on frequentist statistics, which provides a valuable but often limited snapshot of treatment efficacy. A Bayesian lens offers a powerful alternative framework, allowing for the continuous updating of evidence and the incorporation of prior knowledge into statistical inference. This approach is particularly transformative within the context of mixed treatment comparisons (MTCs), also known as network meta-analysis. MTCs enable the simultaneous comparison of multiple treatments, even when they have not been directly compared in head-to-head trials, by synthesizing both direct and indirect evidence within a connected network of trials [21]. This case study explores the application of Bayesian MTC to re-interpret the results of pharmacological trials for non-specific chronic low back pain (NSCLBP), a condition with multiple active comparators but few direct comparisons [73].
Bayesian networks are a class of probabilistic graphical models that represent variables and their conditional dependencies via a directed acyclic graph (DAG) [74]. In an MTC, the graph structure consists of treatment nodes connected by edges representing available direct comparisons. The core Bayesian principle is to calculate the posterior probability of treatment effects, which is proportional to the product of the likelihood of the observed data and the prior probability of the effects. Formally, for parameters θ and data D, Bayes' theorem states: P(θ|D) ∠P(D|θ) × P(θ). In MTC, this allows for the ranking of treatments and provides probabilistic statements about their relative efficacy and safety, offering a more nuanced interpretation for researchers and drug development professionals [75] [21].
Case Study: Pharmacological Treatments for Chronic Low Back Pain
Clinical Context and Problem Definition
Non-specific chronic low back pain is a leading global cause of disability, with a lifetime prevalence of 80–85% [73]. Numerous pharmacological interventions exist, including non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, antidepressants, anticonvulsants, and weak opioids. While many treatments demonstrate efficacy, clinical decision-making is complicated by several factors. First, each agent has a distinct balance between efficacy and side effects. Second, a lack of direct comparisons between all active treatments creates evidence gaps. Third, traditional pairwise meta-analyses cannot unify these outcomes or rank all treatments simultaneously on a single probability scale. This case study re-analyzes this evidence using a bivariate Bayesian network meta-analysis to jointly model pain intensity and treatment discontinuation due to adverse events, creating a unified ranking of pharmacotherapies from most to least effective and safe [73].
Methodological Framework and Data Synthesis
The re-analysis followed a structured protocol for systematic review and meta-analysis. Table 1 summarizes the core eligibility criteria used to identify relevant randomized controlled trials (RCTs).
Table 1: Study Eligibility Criteria
| Component | Description |
|---|---|
| Population | Adults (>18 years) with NSCLBP (symptoms >12 weeks). |
| Interventions | Pharmacotherapy (NSAIDs, antidepressants, anticonvulsants, muscle relaxants, weak opioids, paracetamol). |
| Comparators | Placebo or another active pharmacologic agent. |
| Outcomes | Efficacy: Pain intensity (visual analogue scale, numerical rating scale).Safety: Proportion withdrawing due to adverse events. |
| Study Design | Randomized Controlled Trials (RCTs). |
Data from four major databases (Medline/PubMed, Cochrane Central Register for Controlled Trials, Cochrane Database for Systematic Reviews, and CINAHL) were searched from inception to July 31, 2024 [73]. The extracted data included baseline and follow-up pain scores and the number of participants who dropped out due to adverse events. The risk of bias for each study was assessed using the Cochrane Risk of Bias tool (ROB v2).
Analytical Approach: The Bayesian MTC Model
A bivariate Bayesian random-effects MTC model was employed to synthesize the evidence. This model accounts for the correlation between the two outcomes (efficacy and safety), which can significantly impact clinical decision-making. The model was fit using Markov Chain Monte Carlo (MCMC) methods in Bayesian statistical software (e.g., WinBUGS/OpenBUGS). Vague prior distributions were used to allow the data to drive the inferences. For binary outcomes, the model can be expressed as [21]:
logit(p_ik) = μ_ib + δ_ibk
where p_ik is the probability of an event in trial i under treatment k, μ_ib is the log-odds in the baseline treatment b of trial i, and δ_ibk is the log-odds ratio of treatment k relative to baseline treatment b, assumed to be normally distributed with a pooled mean treatment effect d_bk and common variance σ².
A critical step in MTC is assessing the consistency assumption—that direct and indirect evidence are in agreement. This was evaluated using both local (node-splitting) and global (deviance information criterion, DIC) methods [21]. The output of the model includes posterior distributions for all relative treatment effects, from which treatments can be ranked based on their posterior probabilities of being the best for the combined outcome.
Visualizing the Bayesian MTC Workflow
The following diagram illustrates the logical workflow and data integration process for a Bayesian mixed treatment comparisons meta-analysis.
Diagram 1: Bayesian MTC Analysis Workflow
Key Outputs and Re-interpretation of Evidence
The primary output of a Bayesian MTC is a set of posterior distributions for all relative treatment effects. Table 2 provides a simplified, hypothetical summary of the kind of results such an analysis could yield, ranking treatments based on their posterior probability of being the most effective and safe option.
Table 2: Hypothetical Treatment Rankings from Bayesian MTC
| Treatment | Posterior Probability of Being Best | Mean Effect on Pain (95% CrI) | Odds Ratio for Dropout (95% CrI) |
|---|---|---|---|
| Drug A | 0.72 | -2.5 (-3.1, -1.9) | 0.9 (0.7, 1.2) |
| Drug B | 0.15 | -2.1 (-2.8, -1.4) | 0.8 (0.6, 1.1) |
| Drug C | 0.10 | -1.8 (-2.5, -1.1) | 1.4 (1.0, 1.9) |
| Drug D (Placebo) | 0.03 | Reference | Reference |
CrI: Credible Interval
This probabilistic ranking represents a significant re-interpretation of the evidence. Unlike a frequentist approach that might only indicate if a treatment is statistically superior to placebo, the Bayesian model provides a direct probability that each treatment is the best option. It formally incorporates uncertainty and allows for the simultaneous consideration of efficacy and harm. For instance, a treatment might have high efficacy but also a high posterior probability of leading to dropout due to adverse events, a trade-off that is clearly quantified in this framework [73]. This methodology has been successfully applied in other therapeutic areas, such as alcohol dependence, where it identified combination therapy (naltrexone + acamprosate) as having the highest posterior probability of being the best treatment, a finding not apparent from pairwise comparisons alone [21].
Detailed Experimental Protocol
Protocol for Bayesian MTC Meta-Analysis
This section provides a step-by-step protocol for conducting a Bayesian MTC, based on established methodologies [73] [21] [76].
- Protocol Registration: Prospectively register the systematic review protocol with a platform like PROSPERO.
- Search and Selection: Execute a comprehensive, multi-database literature search using a pre-defined search strategy. Two independent reviewers should screen titles/abstracts and then full-text articles against eligibility criteria (see Table 1).
- Data Extraction: Using a standardized form, extract data on study characteristics, patient demographics, interventions, comparators, and outcomes (both efficacy and safety). Also extract data for risk of bias assessment.
- Evidence Network Mapping: Map all treatment comparisons graphically to visualize the network of evidence, identifying where direct evidence exists and where inferences will rely on indirect evidence.
- Model Specification:
- Software: Use Bayesian analysis software such as WinBUGS, OpenBUGS, JAGS, or Stan.
- Model Type: Implement a Bayesian random-effects MTC model.
- Likelihood and Link: For binary outcomes (e.g., dropout), use a binomial likelihood with logit link. For continuous outcomes (e.g., pain scores), use a normal likelihood with identity link.
- Priors: Use vague (non-informative) prior distributions for basic parameters (e.g., N(0, 10000)) and for between-trial heterogeneity (e.g., Uniform(0, 5)).
- Model Estimation and Convergence:
- Run multiple MCMC chains (e.g., 2 or 3) with a sufficient number of iterations (e.g., 50,000-100,000), discarding the first 50% as burn-in.
- Assess convergence using trace plots and the Brooks-Gelman-Rubin statistic (R-hat ≈ 1.0 indicates convergence).
- Consistency Assessment: Check the consistency assumption using node-splitting methods or by comparing the fit of consistent and inconsistent models using DIC.
- Output and Interpretation:
- Extract posterior summaries (mean, standard deviation, and 95% credible intervals) for all relative treatment effects.
- Calculate the Surface Under the Cumulative Ranking Curve (SUCRA) for each treatment and for each outcome to generate a hierarchy of treatments.
- Report posterior probabilities for treatment rankings.
The Scientist's Toolkit: Essential Reagents and Software
Table 3: Key Research Reagent Solutions for Bayesian MTC
| Item | Function/Description |
|---|---|
| Statistical Software (R/Stata) | Used for data management, standard meta-analysis, and generating summary statistics and graphs. |
| Bayesian MCMC Software (WinBUGS/OpenBUGS/JAGS/Stan) | Specialized platforms for fitting complex Bayesian hierarchical models using Markov Chain Monte Carlo simulation. |
| PRISMA-NMA Checklist | Reporting guideline (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Network Meta-Analyses) to ensure transparent and complete reporting. |
| Cochrane Risk of Bias Tool (ROB2) | A structured tool to assess the methodological quality and potential for bias in included randomized trials. |
| Power Prior Formulations | A Bayesian method to incorporate historical data from previous studies while controlling its influence on the current analysis via a power parameter [76]. |
Visualizing the Evidence Network and Information Flow
The structure of the evidence and the flow of information within a Bayesian network are key to understanding MTCs. The diagram below illustrates a simplified evidence network for the back pain case study and the concept of conditional dependence.
Diagram 2: Evidence Network and Bayesian Model
In the realm of medical research and drug development, Mixed Treatment Comparisons (MTCs), also known as network meta-analyses, enable the simultaneous comparison of multiple interventions, even when direct head-to-head evidence is lacking. The Bayesian statistical framework is particularly well-suited for these complex analyses because it allows for the formal integration of prior knowledge with current trial data. A prior probability distribution (or "prior") encapsulates existing knowledge or assumptions about a treatment effect before observing the data from the current study. The process of Bayesian inference then updates this prior knowledge with new data to produce a posterior distribution, which represents the current state of knowledge [17].
The spectrum of prior knowledge ranges from non-informative priors, which exert minimal influence and let the data dominate the analysis, to highly informed priors, which systematically incorporate evidence from previous research. The transition from non-informative to evidence-based priors represents a maturation in a research field, allowing for cumulative knowledge building and more efficient use of resources, which is critical in drug development [16].
Theoretical Foundations: Categories of Priors
Non-Informative Priors
Non-informative priors (also known as vague, diffuse, or reference priors) are designed to have a minimal impact on the posterior results. They are particularly valuable in early-stage research or when analyzing a new compound where substantial prior clinical knowledge is unavailable or when the objective is to let the current data speak for itself. Common choices include a normal distribution with a very large variance (e.g., N(0, 100²)) for a log-odds ratio or a uniform distribution across a plausible range of values [16]. Their primary function is to facilitate analysis without imposing strong subjective beliefs, serving as a Bayesian baseline.
Weakly Informative Priors
Weakly informative priors introduce a degree of regularization to the analysis by gently constraining parameter estimates to biologically or clinically plausible ranges. This helps stabilize computations, particularly in complex models with limited data, and can prevent estimates from wandering into implausible territories (e.g., an impossibly large hazard ratio). An example is a normal distribution with a mean of zero and a standard deviation that encapsulates a reasonable range of effects, such as N(0, 2²) for a log-odds ratio, which places most of the prior probability on odds ratios between 0.02 and 50 [16]. These priors are more influential than non-informative priors but less so than fully evidence-based priors.
Evidence-Based (Informed) Priors
Evidence-based priors represent the most sophisticated use of prior information. They quantitatively synthesize existing knowledge from sources such as previous clinical trials, pilot studies, published meta-analyses, or real-world evidence. For instance, the posterior distribution from a pilot study can directly serve as the prior for a subsequent, larger trial [16]. This approach formally and efficiently accumulates scientific evidence, potentially leading to more precise estimates and requiring smaller sample sizes in future studies. The key to their valid application is the careful and transparent justification of the prior's source and form.
Quantitative Synthesis of Bayesian Reporting in Medical Research
A bibliometric analysis of 120 surgical articles published in high-impact journals between 2000 and 2024 provides a snapshot of how priors are currently used and reported in medical research [17]. The findings highlight both the growing adoption of Bayesian methods and areas where reporting standards need improvement.
Table 1: Use and Reporting of Bayesian Priors in Surgical Research (2000-2024)
| Aspect | Finding | Detail / Implication |
|---|---|---|
| Growth Trend | 12.3% Compound Annual Growth Rate | Indicates rapidly increasing adoption of Bayesian methods in the field. |
| Common Study Designs | Retrospective Cohort Studies (41.7%), Meta-Analyses (31.7%), Randomized Trials (15.8%) | Bayesian methods are applied across key evidential hierarchies. |
| Reporting Quality (ROBUST Scale) | Average Score: 4.1 ± 1.6 out of 7 | Indicates moderate but inconsistent adherence to reporting standards. |
| Prior Specification | 54.0% of studies | Nearly half of all studies failed to specify the priors used for their models. |
| Prior Justification | 29.0% of studies | A critical shortcoming; the vast majority did not explain or justify their choice of prior. |
This data underscores a crucial message for practitioners: while Bayesian methods are powerful, their transparency and reproducibility depend heavily on rigorous reporting, particularly concerning prior selection and justification [17].
Protocol for Application: Implementing Priors in Mixed Treatment Comparisons
The following diagram outlines a systematic workflow for developing and applying priors in a Bayesian MTC analysis, from initial assessment to model checking.
Step-by-Step Methodology for Protocol Implementation
Define the Parameter and Assess Evidence (Start, A1-A4):
- Clearly define the target parameter for the MTC (e.g., log-hazard ratio for overall survival, log-odds ratio for response).
- Conduct a systematic literature review to identify all relevant previous studies. For each study, extract the point estimate and measure of uncertainty (e.g., confidence interval) [17].
- If available, gather individual-level data from pilot studies.
- In the absence of robust published data, formal expert elicitation protocols can be used to translate clinical expertise into a probability distribution.
Select and Formalize the Prior (B1-B4, C1):
- Non-Informative (B2): Use when prior evidence is absent or unreliable. Example: For a log-odds ratio, specify
θ ~ Normal(mean=0, sd=10). This prior is so diffuse that it has negligible influence. - Weakly Informative (B3): Use for regularization. Example:
θ ~ Normal(mean=0, sd=2). This keeps estimates in a plausible range (approx. OR: 0.135 to 7.39) while being only weakly skeptical of large effects. - Evidence-Based (B4): Use when high-quality prior evidence exists. This involves performing a meta-analysis of the historical data to formulate the prior. Example: If a meta-analysis of 5 previous trials yields a pooled log-odds ratio of -0.4 with a standard error of 0.15, the informed prior would be
θ ~ Normal(mean=-0.4, sd=0.15).
- Non-Informative (B2): Use when prior evidence is absent or unreliable. Example: For a log-odds ratio, specify
Integrate with Data and Validate (D1, E1):
- Fit the Bayesian MTC model, which combines the chosen prior with the likelihood of the current data to compute the posterior distribution.
- Sensitivity analysis is mandatory. Refit the model using a range of alternative priors (e.g., a non-informative prior and a differently parametered informed prior). The stability of the posterior conclusions (e.g., the probability that the treatment is superior to control) across these analyses should be reported. If conclusions change meaningfully, this indicates that the results are prior-dependent and should be interpreted with corresponding caution [17] [16].
Research Reagent Solutions: Software and Computational Tools
Implementing Bayesian MTCs requires specialized software for model specification and computation, particularly Markov Chain Monte Carlo (MCMC) sampling.
Table 2: Essential Software Tools for Bayesian Mixed Treatment Comparisons
| Tool / Reagent | Type | Primary Function | Key Features |
|---|---|---|---|
| Stan & R Interfaces(brms, rstanarm) [16] | Probabilistic Programming Language & R Packages | Specifies and fits complex Bayesian models, including multilevel MTCs. | Uses Hamiltonial Monte Carlo (efficient). brms offers a user-friendly formula interface similar to R's lme4. |
| JAGS / BUGS [17] | MCMC Sampling Software | Early and widely-used tools for Bayesian analysis with MCMC. | Flexible model specification. Accessible but can be slower and less efficient than Stan for complex models. |
| JASP [17] | Graphical User Interface (GUI) Software | Provides a point-and-click interface for common Bayesian models. | Low barrier to entry; minimal coding required. Good for education and preliminary analysis. |
| R / Python | Programming Environments | The foundational platforms for data manipulation, analysis, and visualization. | Provide maximum flexibility and control, with extensive packages for Bayesian analysis and reporting. |
Visualizing the Bayesian Updating Process in MTCs
The core of Bayesian analysis is the updating of prior belief with data to form a posterior belief. This process, as it applies to estimating a treatment effect in an MTC, is illustrated below.
This diagram conceptualizes Bayes' theorem: Posterior ∠Likelihood × Prior. The posterior distribution is a compromise between the prior and the new data. The relative influence of each depends on their respective precisions. A very precise prior (low variance) will exert more influence, whereas with a non-informative prior, the posterior is essentially proportional to the likelihood.
Application Notes: Integrating MTC into Modern Trial Designs
Mixed Treatment Comparisons (MTC), often executed within a Bayesian Network Meta-Analysis (NMA) framework, are increasingly critical for evaluating multiple interventions across heterogeneous patient populations in personalized medicine. These approaches enable direct and indirect treatment comparisons within a single analytical framework, optimizing trial efficiency and accelerating therapeutic development.
The PRACTical Trial Design
The Personalised Randomised Controlled Trial (PRACTical) design addresses a common modern clinical challenge: the existence of multiple treatment options for a single medical condition with no single standard of care [34].
- Core Principle: Instead of comparing each treatment to a common control, patients are randomized to a "personalised randomisation list" containing only treatments suitable for their specific subgroup. The analysis then borrows information across these patient subpopulations to rank all treatments against each other [34].
- Illustrative Example: A trial for multidrug-resistant bloodstream infections can compare four antibiotic treatments (A, B, C, D). Patients are assigned to one of four subgroups based on their eligibility for these treatments (e.g., due to allergies or pathogen susceptibility). Each subgroup's randomisation list contains a different overlapping set of treatments, creating a network of comparisons [34].
- Analytical Approach: A logistic regression model is used, with the binary outcome (e.g., 60-day mortality) as the dependent variable and treatments and patient subgroups included as independent categorical variables [34]. The analysis leverages both direct comparisons (within the same randomisation list) and indirect comparisons (across different lists), analogous to a network meta-analysis.
Table 1: Comparison of Analytical Approaches in a PRACTical Design Simulation
| Analytical Method | Probability of Predicting True Best Treatment | Probability of Interval Separation (Proxy for Power) | Probability of Incorrect Interval Separation (Proxy for Type I Error) |
|---|---|---|---|
| Frequentist Approach | ≥80% (at N≤500) | Up to 96% (at N=1500-3000) | <5% (for N=500-5000) |
| Bayesian Approach (Informative Prior) | ≥80% (at N≤500) | Up to 96% (at N=1500-3000) | <5% (for N=500-5000) |
Bayesian Adaptive Platform Trials
Bayesian adaptive platform trials represent a powerful application of MTC for personalized medicine, allowing for the efficient investigation of multiple treatments across multiple patient subgroups within a single, ongoing master protocol.
- Key Features: These trials can adapt over time, adding or dropping treatment arms due to efficacy or lack of efficacy, and use statistical models to share information (borrowing strength) across subgroups [77].
- Hierarchical Modeling: A Bayesian hierarchical beta-binomial model is often employed for binary outcomes. This model includes a tuning parameter that adjusts the "strength" of information borrowing across patient subgroups within a treatment arm, improving the trial's efficiency, particularly in subgroups with smaller sample sizes [77].
- Response-Adaptive Randomization (RAR): To balance statistical power with patient benefit, RAR algorithms update patient randomization probabilities based on interim results, allocating more patients to the more promising treatments as the trial progresses [77].
- Handling Temporal Drift: A first-order normal dynamic linear model (NDLM) can be incorporated to account for potential changes in treatment response rates over time, ensuring estimates remain unbiased [77].
Table 2: Essential Components of a Bayesian Adaptive Platform Trial Design
| Component | Function | Implementation Example |
|---|---|---|
| Hierarchical Model | Borrows information across patient subgroups to improve estimation precision. | Beta-binomial model with a tuning parameter to control borrowing strength [77]. |
| Response-Adaptive Randomization | Maximizes patient benefit by skewing allocation towards better-performing treatments. | "RARCOMP" scheme seeks a compromise between high statistical power and high patient benefit [77]. |
| Drift Adjustment | Accounts for changes in underlying patient response rates over time. | Incorporation of a first-order normal dynamic linear model (NDLM) [77]. |
| Multiplicity Control | Manages familywise Type I error inflation from multiple subgroups and interim analyses. | Thresholds for decision parameters are calibrated via extensive simulation [77]. |
Experimental Protocols
Protocol 1: Implementing a PRACTical Design for Comparative Effectiveness
Objective: To rank the efficacy of multiple treatments without a single standard of care, using a PRACTical design with frequentist and Bayesian analytical models.
Methodology:
Define Master List and Subgroups:
- Establish a master list of all treatments to be investigated (e.g., 4 antibiotic regimens).
- Define patient subgroups based on characteristics that determine treatment eligibility (e.g., specific allergies, pathogen resistance profiles). Ensure a minimum overlap of treatments between subgroups to maintain network connectivity [34].
Randomization:
- For each patient, determine their eligibility for each treatment in the master list.
- Generate a personalized randomization list containing all treatments for which the patient is eligible.
- Randomize the patient with equal probability to one of the treatments on their list [34].
Data Collection:
- Collect primary outcome data (e.g., binary 60-day mortality).
- Record patient subgroup and treatment assignment.
Statistical Analysis:
- Frequentist Approach: Fit a multivariable logistic regression model with the outcome as the dependent variable and treatment and patient subgroup included as fixed effects [34].
- Bayesian Approach: Fit a similar model using Bayesian methods (e.g., via RStan). Incorporate prior information if available. For example, use strongly informative normal priors based on historical datasets [34].
- Treatment Ranking: Rank treatments based on their coefficient estimates from the model. Evaluate performance using the probability of predicting the true best treatment and metrics based on the precision of the estimates (e.g., probability of interval separation) [34].
Figure 1: PRACTical Design Workflow. This diagram outlines the patient flow and key steps in a PRACTical trial, from defining treatments to final analysis.
Protocol 2: Bayesian Hierarchical Adaptive Platform Trial
Objective: To efficiently identify the best treatment for multiple patient subgroups in a platform trial using a Bayesian hierarchical model with response-adaptive randomization.
Methodology:
Trial Structure:
- Establish a master protocol for a multi-arm, multi-stage (MAMS) platform trial.
- Define multiple, mutually exclusive patient subgroups (e.g., based on biomarkers or clinical characteristics) [77].
Model Specification:
- Use a Bayesian hierarchical beta-binomial model for binary outcomes.
- Let ( p_{jk} ) represent the response rate for treatment ( j ) in subgroup ( k ).
- Model the ( p_{jk} ) using a beta prior distribution, ( p_{jk} \sim \text{Beta}(a_{jk}, b_{jk}) ), where the parameters ( a_{jk} ) and ( b_{jk} ) are themselves drawn from hyper-priors. This structure allows information borrowing across subgroups [77].
- Incorporate a drift parameter using a dynamic linear model to account for potential time-varying response rates [77].
Response-Adaptive Randomization:
- Conduct interim analyses at pre-specified intervals.
- Update randomization probabilities for each subgroup based on the posterior probability that each treatment is the best for that subgroup.
- Implement an allocation rule like "RARCOMP" that balances exploration (statistical power) and exploitation (patient benefit) [77].
Decision Rules:
- Pre-define stopping rules for success (e.g., if the posterior probability of a treatment being superior exceeds a threshold) and for futility.
- Calibrate decision thresholds through extensive simulation to control the overall Type I error rate at 0.05 [77].
Figure 2: Bayesian Adaptive Platform Workflow. This diagram illustrates the cyclic, adaptive nature of a platform trial, including interim decisions and randomization updates.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Implementing MTC in Personalized Medicine Trials
| Category | Item | Function/Application |
|---|---|---|
| Statistical Models | Bayesian Hierarchical Model | Borrows strength across subgroups to improve precision and power in subgroup analysis [78] [77]. |
| Pairwise Independent Model | Serves as a simpler, non-borrowing baseline model for performance comparison [78]. | |
| Cluster Hierarchical Model (Dirichlet Process) | An alternative to standard hierarchical models that mitigates over-shrinkage when subgroups are heterogeneous [78]. | |
| Software & Computational Tools | R (with rstanarm package) |
Performs Bayesian regression analysis for PRACTical and adaptive trial designs [34]. |
| Fixed and Adaptive Clinical Trials Simulator (FACTS) | Software used for simulating and designing complex adaptive clinical trials [77]. | |
| RQDA Software | Aids in qualitative data analysis for design validation studies of NMA presentation formats [79]. | |
| Analytical & Design Frameworks | Network Meta-Analysis (NMA) | Core framework for synthesizing direct and indirect evidence on multiple treatments [80]. |
| Response-Adaptive Randomization (RAR) | An allocation algorithm that skews patient assignment towards better-performing treatments based on interim data [77]. | |
| Grading of Recommendations, Assessment, Development and Evaluation (GRADE) | Provides a methodology for contextualizing NMA results and assessing the certainty of evidence [79]. |
Conclusion
Bayesian Mixed Treatment Comparisons represent a powerful and flexible framework for modern evidence synthesis, moving beyond the limitations of traditional pairwise meta-analysis. By formally integrating prior evidence, directly quantifying uncertainty through posterior probabilities, and efficiently modeling complex networks of evidence, Bayesian MTC provides a more intuitive and clinically relevant output for decision-makers. This approach is particularly vital in the era of precision medicine, where it can handle mixed biomarker populations and inform personalized treatment strategies. Future directions will likely involve greater integration with real-world evidence, the use of more complex models to handle multivariate outcomes, and the application of these methods within innovative trial designs like platform trials. As the methodology and supporting software continue to mature, Bayesian MTC is poised to remain a cornerstone of robust evidence-based drug development and healthcare policy.
References
- 1. Network meta-analysis: application and practice using R ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6635665/]
- 2. Multiple treatment comparison meta-analyses: a step ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3130904/]
- 3. Network meta-analysis: a technique to gather evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5386629/]
- 4. Network meta-analysis: a powerful tool for clinicians ... [https://www.sciencedirect.com/science/article/pii/S0895435624002932]
- 5. 11.2 Bayesian Network Meta-Analysis [https://bookdown.org/MathiasHarrer/Doing_Meta_Analysis_in_R/bayesnma.html]
- 6. Bayesian Statistics: A Modern Accurate Data Analysis in ... [https://www.linkedin.com/pulse/bayesian-statistics-modern-accurate-data-s2tye]
- 7. A bayesian dynamic borrowing framework for improving the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12557851/]
- 8. Chaining Bayesian inference with priors constructed from ... [https://statmodeling.stat.columbia.edu/2025/05/13/chaining-bayes-priors-from-posteriors/]
- 9. Concepts and emerging issues of network meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8497908/]
- 10. Introduction - Use of Mixed Treatment Comparisons in ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK107325/]
- 11. Network meta-analysis: application and practice using Stata [https://pmc.ncbi.nlm.nih.gov/articles/PMC5733388/]
- 12. Assumptions of Mixed Treatment Comparisons in Health ... [https://journals.plos.org/plosone/article?id=10.1371%2Fjournal.pone.0160712]
- 13. Chapter 11: Undertaking network meta-analyses [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-11]
- 14. CINeMA: An approach for assessing confidence in the results ... [https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003082]
- 15. Bayesian Models for N-of-1 Trials [https://hdsr.mitpress.mit.edu/pub/b6efwlql]
- 16. A Bayesian approach to small samples: Mixed-effects ... [https://www.sciencedirect.com/science/article/abs/pii/S2772766125000527]
- 17. Bibliometric Analysis of Surgical Articles Using Bayesian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12453365/]
- 18. A comparison of armâ€based and contrastâ€based models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6899819/]
- 19. and arm-synthesis models for network meta-analysis [https://www.cambridge.org/core/journals/research-synthesis-methods/article/an-investigation-of-the-impact-of-using-contrast-and-armsynthesis-models-for-network-metaanalysis/8211C05BD2A2E70CE0742EFC70B23EF4]
- 20. Arm vs Contrast level data - RMW Knowledge Base [https://documentation.cochrane.org/revman-kb/arm-vs-contrast-level-data-312606799.html]
- 21. A Bayesian Mixed Treatment Comparisons Meta-Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4318856/]
- 22. What is the difference between fixed effect, random effect in ... [https://stats.stackexchange.com/questions/4700/what-is-the-difference-between-fixed-effect-random-effect-in-mixed-effect-model]
- 23. Should I use fixed effects or random effects when I have ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8784019/]
- 24. Mixed treatment comparison analysis provides internally ... [https://www.sciencedirect.com/science/article/abs/pii/S0895435609003072]
- 25. Prior Choices of Between-Study Heterogeneity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8041977/]
- 26. Guidance for the Use of Bayesian Statistics in Medical ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-use-bayesian-statistics-medical-device-clinical-trials]
- 27. A Practical Guide to Random-Effects Bayesian Meta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10021079/]
- 28. Modelling heterogeneity variances in multiple treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3554418/]
- 29. Modelling heterogeneity variances in multiple treatment ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-13-2]
- 30. Methods - Findings of Bayesian Mixed Treatment Comparison ... [https://www.ncbi.nlm.nih.gov/books/NBK126113/]
- 31. Empirical prior distributions for Bayesian meta-analyses of ... [https://arxiv.org/abs/2306.11468]
- 32. Confidence intervals of the relative risk and odds ratio can ... [https://pubmed.ncbi.nlm.nih.gov/39724989/]
- 33. Understanding Network Metaâ€Analysis: A Practical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271649/]
- 34. A comparison of frequentist and Bayesian approaches to the ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02537-x]
- 35. Data visualisation approaches for component network meta ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-02026-z]
- 36. Network meta-regression including baseline risk analysis ... [https://www.sciencedirect.com/science/article/pii/S0895435625001726]
- 37. Predictive P-score for treatment ranking in Bayesian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8520624/]
- 38. Approaches to interpreting and choosing the best treatments ... [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-017-0473-z]
- 39. Ranking treatments in frequentist network meta-analysis ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-015-0060-8]
- 40. A Metric for Quantifying Certainty in Treatment Hierarchies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181804/]
- 41. Bayesian Hierarchical Mixed Effects Model and Comparison ... [https://discourse.mc-stan.org/t/bayesian-hierarchical-mixed-effects-model-and-comparison-with-stan-glmer/17555]
- 42. A multifaceted graphical display, including treatment ... [https://www.sciencedirect.com/science/article/pii/S0895435623000252]
- 43. PROTOCOL: Assessment of outcome reporting bias in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10210598/]
- 44. Outcome reporting bias in nephrology randomized clinical ... [https://www.sciencedirect.com/science/article/pii/S2451865422000412]
- 45. Outcome reporting recommendations for clinical trial protocols ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-020-04440-w]
- 46. Bayesian Mixed Treatment Comparisons Meta-Analysis for ... [https://pubmed.ncbi.nlm.nih.gov/29540936/]
- 47. Bayesian mixed treatment comparisons meta-analysis for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5846497/]
- 48. Exploiting multivariate network meta-analysis: A calibrated ... [https://www.medrxiv.org/content/10.1101/2024.06.25.24309477v1.full]
- 49. Outcome reporting bias in randomized trials funded by the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC517858/]
- 50. Classifying Sparse Matrices with Graph Neural Networks [https://scisimple.com/en/articles/2025-10-03-classifying-sparse-matrices-with-graph-neural-networks--akxqwv1]
- 51. Non-parametric Bayesian approach to multiple treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11561732/]
- 52. Nonparametric Bayesian Multi-Treatment Mixture Cure ... [https://arxiv.org/abs/2508.08975]
- 53. A guide to bayesian networks software for structure and ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2025.1631901/full]
- 54. GNNs, Graph : 2025 Tricks That Matter | by Thinking... | Medium Sparse [https://medium.com/@ThinkingLoop/graph-gnns-2025-sparse-tricks-that-matter-ffce33ce503c]
- 55. Combining treatment effects from mixed populations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11963434/]
- 56. A comparison of approaches for combining predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7788953/]
- 57. Design of tables for the presentation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10346464/]
- 58. Bayesian Statistics: A Modern Data Analysis in 2025 [https://clinilaunchresearch.in/guide-to-bayesian-statistics/]
- 59. Bayesian Analysis Reporting Guidelines [https://www.nature.com/articles/s41562-021-01177-7]
- 60. A tutorial on Bayesian model-averaged meta-analysis in ... [https://link.springer.com/article/10.3758/s13428-023-02093-6]
- 61. Transitioning from BUGS - Stan [https://mc-stan.org/docs/stan-users-guide/for-bugs-users.html]
- 62. Stan for Bayesian Analysis | Daniel J. Hocking - WordPress.com [https://danieljhocking.wordpress.com/2012/10/23/stan-for-bayesian-analysis/]
- 63. Individual participant data from digital sources informed ... [https://www.sciencedirect.com/science/article/pii/S0895435623002780]
- 64. A review and comparison of arm-based versus contrast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11134325/]
- 65. Chapter 12 Network Meta-Analysis [https://bookdown.org/MathiasHarrer/Doing_Meta_Analysis_in_R/netwma.html]
- 66. How to Conduct a Bayesian Network Meta-Analysis [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2020.00271/full]
- 67. Bias in identification of the best treatment in a Bayesian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4259556/]
- 68. Random-effects meta-analysis models for pooling rare events ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02664-5]
- 69. Breaking the Winner's Curse with Bayesian Hybrid Shrinkage [https://arxiv.org/html/2511.06318v1]
- 70. Understanding and interpreting confidence and credible ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6630113/]
- 71. Statistics 101: Credible vs Confidence Interval [https://towardsdatascience.com/statistics-101-credible-vs-confidence-interval-af7b7e8fdd79/]
- 72. What's the difference between a confidence interval and a ... [https://stats.stackexchange.com/questions/2272/whats-the-difference-between-a-confidence-interval-and-a-credible-interval]
- 73. A Systematic Review and Bivariate Bayesian Network Meta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12481260/]
- 74. Introduction to Bayesian networks [https://bayesserver.com/docs/introduction/bayesian-networks/]
- 75. Bayesian Network [https://thedecisionlab.com/reference-guide/statistics/bayesian-network]
- 76. Bayesian meta-analysis of the effectiveness ... [https://www.frontiersin.org/journals/epidemiology/articles/10.3389/fepid.2025.1547867/full]
- 77. Optimizing a Bayesian hierarchical adaptive platform trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9446515/]
- 78. Designing and Analyzing Clinical Trials for Personalized via... Medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC8084911/]
- 79. Development and design validation of a novel network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9189833/]
- 80. Optimal trial design selection: a comparative analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10638718/]