Addressing Heterogeneity in Network Meta-Analysis of Drugs: A Comprehensive Guide from Detection to Decision-Making
This article provides a comprehensive framework for researchers and drug development professionals to address heterogeneity in network meta-analysis (NMA).
Addressing Heterogeneity in Network Meta-Analysis of Drugs: A Comprehensive Guide from Detection to Decision-Making
Abstract
This article provides a comprehensive framework for researchers and drug development professionals to address heterogeneity in network meta-analysis (NMA). Covering foundational concepts, methodological approaches, troubleshooting strategies, and validation techniques, we explore the critical assumptions of transitivity and consistency, statistical measures (I², τ², Q), and advanced methods including network meta-regression and class-effect models. The guide emphasizes practical implementation using modern software tools and offers evidence-based strategies for robust interpretation and risk-averse clinical decision-making in the presence of heterogeneity.
Understanding Heterogeneity in NMA: Core Concepts, Sources, and Impact on Drug Evidence Synthesis
Frequently Asked Questions
What is heterogeneity in the context of a Network Meta-Analysis? In Network Meta-Analysis (NMA), heterogeneity refers to the variability in treatment effects between the individual studies included in the network. This variability goes beyond what would be expected from chance alone. It arises from differences in study populations, interventions, dosages, trial design, and outcome measurements across the trials. Assessing heterogeneity is crucial as it impacts the reliability and interpretation of the NMA results [1] [2].
Why is assessing heterogeneity so important for my NMA? Evaluating heterogeneity is fundamental to the validity of your NMA conclusions. Substantial heterogeneity can mean that the studies are not estimating a single common treatment effect, making a simple pooled estimate misleading. It can bias the NMA results and lead to incorrect rankings of treatments. Understanding the degree and sources of heterogeneity helps researchers decide if a random-effects model is appropriate, guides the exploration of reasons for variability through subgroup analysis or meta-regression, and provides context for how broadly the findings can be applied [1] [2].
What is the difference between heterogeneity and inconsistency? While sometimes used interchangeably, these terms have distinct meanings in NMA.
- Heterogeneity refers to differences in treatment effects within a single direct comparison (e.g., variability among all trials that compare Treatment A vs. Treatment B).
- Inconsistency refers to differences between direct and indirect evidence for the same treatment comparison within a network. For example, if the estimate from direct trials of A vs. C differs significantly from the estimate obtained by indirectly comparing A to C via a common comparator B, this is inconsistency. Special statistical tests, such as Higgins' global inconsistency test, are used to evaluate this [1] [3].
My NMA has high heterogeneity (I² > 50%). What should I do? A high I² value indicates substantial heterogeneity. Your troubleshooting steps should include:
- Verify Data and Model: Double-check your data for errors and ensure you are using an appropriate statistical model (e.g., a random-effects model).
- Explore Sources: Conduct subgroup analysis or meta-regression to investigate whether specific study-level covariates (e.g., patient baseline risk, publication year, trial design) can explain the variability.
- Assess Network Geometry: Examine the structure of your evidence network. Sparse networks or comparisons with few studies are more prone to heterogeneity.
- Consider Alternative Methods: If you have individual patient data for a subset of trials, using it can help account for heterogeneity. Advanced models like Jackson's random inconsistency model can also be considered.
- Report Transparently: Clearly report the heterogeneity statistics and discuss the potential implications for the robustness of your findings [1] [3] [2].
Statistical Measures of Heterogeneity: A Troubleshooting Guide
The table below summarizes the key statistical measures used to diagnose and quantify heterogeneity in meta-analyses.
Table 1: Key Statistical Measures for Heterogeneity Assessment
| Measure | What It Quantifies | Interpretation & Thresholds | Common Pitfalls & Solutions |
|---|---|---|---|
| Q Statistic [2] | Whether differences between study results are larger than expected by chance. | A significant p-value (<0.05) suggests the presence of heterogeneity. | Pitfall: Its power is low with few studies and oversensitive with many.Solution: Never interpret in isolation; use alongside I² and τ². |
| I² Statistic [2] | The percentage of total variability in effect estimates due to heterogeneity rather than chance. | 0-40%: might not be important; 30-60%: moderate; 50-90%: substantial; 75-100%: considerable. These are only rough guides. | Pitfall: Does not measure the actual magnitude of heterogeneity. A high I² can occur with precise studies even if absolute differences are small.Solution: Always report and interpret τ² alongside I². |
| τ² (tau-squared) [2] | The absolute magnitude of the variance of true treatment effects across studies. Reported in the same units as the effect size (e.g., log odds ratio). | A τ² of 0 indicates homogeneity. Larger values indicate greater dispersion of true effects. There are no universal thresholds; interpretation should be based on clinical context. | Pitfall: The default DerSimonian-Laird (DL) estimator is often biased.Solution: Use more robust estimators like Restricted Maximum Likelihood (REML) or Paule-Mandel. |
| Prediction Interval [2] | The expected range of true treatment effects in a future study or a specific setting, accounting for heterogeneity. | If a 95% prediction interval includes no effect (e.g., a risk ratio of 1), the treatment effect is inconsistent across study populations. | Pitfall: Often omitted from reports, giving a false sense of precision.Solution: Routinely calculate and report prediction intervals to better communicate the uncertainty in your findings. |
Methodologies for Investigating Heterogeneity
Protocol for Subgroup Analysis and Meta-Regression Subgroup analysis and meta-regression are used to explore whether study-level covariates explain heterogeneity [1].
- A Priori Planning: Pre-specify potential effect modifiers (e.g., mean patient age, disease severity, trial design, drug dose) in your study protocol to avoid data dredging.
- Data Extraction: Systematically extract data on the chosen covariates from each included study.
- Statistical Analysis:
- For subgroup analysis, stratify the network by the categorical covariate and perform separate NMAs within each stratum. Compare the treatment effects across strata.
- For meta-regression, incorporate the covariate directly into the NMA model. This tests if the covariate has a statistically significant interaction with treatment effects. The NMA package in R provides functions for this [3].
- Interpretation: Be cautious in interpreting findings, as these analyses are observational in nature. A significant association does not prove causation.
Protocol for Assessing Network Geometry The structure of the evidence network itself can influence heterogeneity. The following metrics, adapted from graph theory, help describe this geometry [4].
Table 2: Key Metrics for Describing Network Meta-Analysis Geometry
| Metric | Definition | Interpretation |
|---|---|---|
| Number of Nodes | The total number of interventions being compared. | A higher number indicates a broader comparison but may increase complexity. |
| Number of Edges | The total number of direct comparisons available in the network. | More edges indicate more direct evidence is available. |
| Density | The number of existing connections divided by the number of possible connections. | Ranges from 0 to 1. Values closer to 1 indicate a highly connected, robust network. |
| Percentage of Common Comparators | The proportion of nodes that are directly linked to many other nodes (like a placebo). | A higher percentage indicates a more strongly connected network. |
| Median Thickness | The median number of studies per direct comparison (edge). | A higher value suggests more precise direct evidence for that comparison. |
The Scientist's Toolkit: Essential Reagents for NMA
Table 3: Key Software and Methodological Tools for NMA Heterogeneity Assessment
| Tool / Resource | Function | Use Case in Troubleshooting Heterogeneity |
|---|---|---|
| R Package 'NMA' [3] | A comprehensive frequentist package for NMA based on multivariate meta-analysis models. | Performs network meta-regression, Higgins' global inconsistency test, and provides advanced inference methods. |
| Random-Effects Model [2] | A statistical model that assumes the true treatment effect varies across studies and estimates the distribution of these effects. | The standard model when heterogeneity is present. It incorporates the between-study variance τ² into the analysis. |
| Restricted Maximum Likelihood (REML) [2] | A method for estimating the between-study variance τ². | A robust alternative to the DerSimonian-Laird estimator; recommended for accurate quantification of heterogeneity. |
| Global Inconsistency Test [3] | A statistical test to check for disagreement between direct and indirect evidence in the entire network. | Used to validate the assumption of consistency, which is fundamental to a valid NMA. |
| Pesampator | Pesampator, CAS:1258963-59-5, MF:C18H20N2O4S2, MW:392.5 g/mol | Chemical Reagent |
| PF-05020182 | PF-05020182, CAS:1354712-92-7, MF:C18H30N4O4, MW:366.46 | Chemical Reagent |
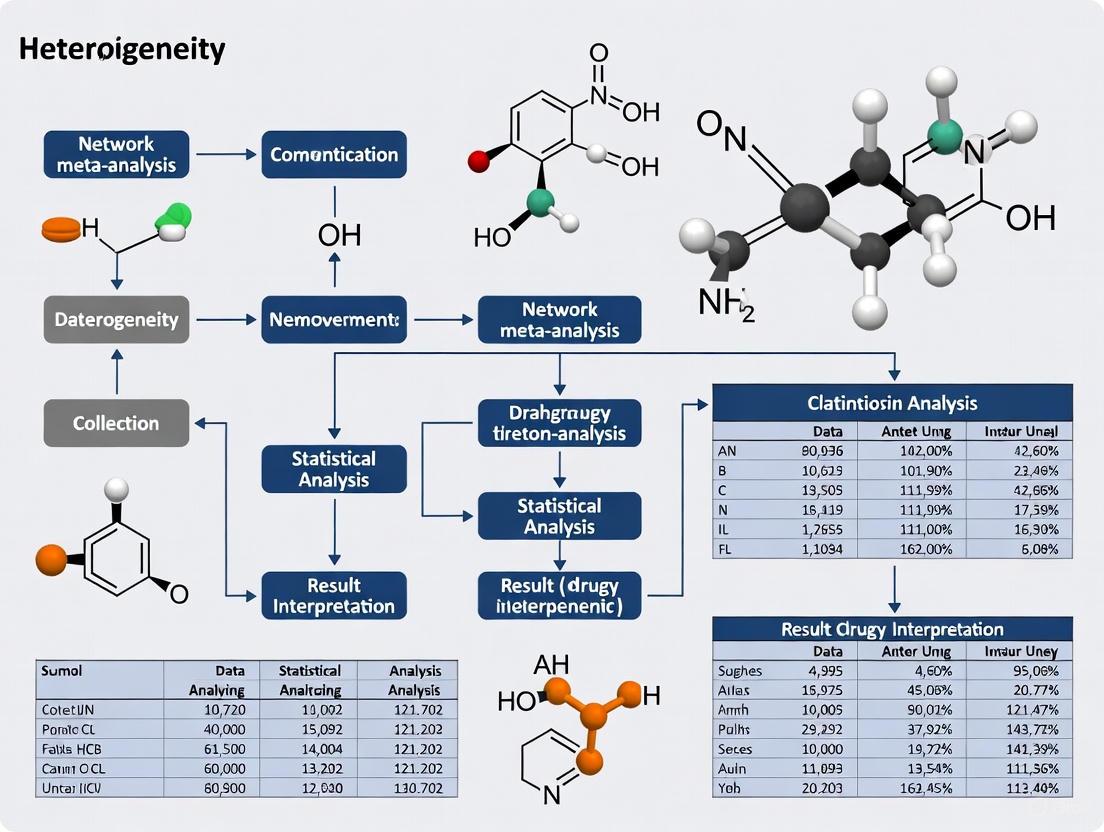
Workflow and Relationships Diagram
The following diagram illustrates the logical workflow for assessing and addressing heterogeneity in a drug NMA.
FAQs: Core Concepts and Common Challenges
What are transitivity and consistency, and how do they differ? Transitivity and consistency are fundamental assumptions in Network Meta-Analysis (NMA), but they are assessed differently. Transitivity is a clinical and methodological assumption that must be evaluated before conducting the NMA. It posits that there are no systematic differences in the distribution of effect modifiers (e.g., patient demographics, disease severity) across the different treatment comparisons within the network [5] [6]. Essentially, the studies should be similar enough that the participants could hypothetically have been randomized to any of the interventions in the network [7]. Consistency is the statistical manifestation of transitivity. It refers to the agreement between direct evidence (from head-to-head trials) and indirect evidence (derived via a common comparator) for the same treatment comparison [7] [8]. While transitivity is conceptually assessed, consistency can be evaluated statistically once the NMA is performed [7].
What are the practical consequences of violating the transitivity assumption? Violating the transitivity assumption compromises the validity and credibility of the NMA results [5]. Since the benefits of randomization do not extend across different trials, systematic differences in effect modifiers can introduce confounding bias into the indirect and mixed treatment effect estimates [5] [8]. This can lead to incorrect conclusions about the relative effectiveness or harm of the interventions, potentially misinforming clinical decisions and health policies [7].
My network is star-shaped (all trials compare other treatments to a single common comparator, like a placebo). Can I check for transitivity? Yes, you must still evaluate transitivity. A star-shaped network precludes the evaluation of statistical consistency because there are no closed loops to compare direct and indirect evidence [5]. However, the assessment of transitivity—scrutinizing the distribution of effect modifiers across the different treatment-versus-placebo comparisons—remains critically important for the validity of your indirect comparisons [5] [6].
I have identified potential intransitivity in my network. What are my options? If transitivity is questionable, you have several options [5]:
- Network Meta-Regression: Use this to adjust for the effect modifiers causing the imbalance, provided you have a sufficient number of trials [5] [6].
- Subnetworks: Split the network into smaller, more homogenous subnetworks where the transitivity assumption is more plausible [5].
- Refrain from NMA: If the concerns are severe and cannot be adjusted for, it may not be valid or feasible to perform an NMA [5].
Troubleshooting Guides
Problem: Incoherence (Inconsistency) is Detected in a Network Loop
Issue: Statistical tests indicate a significant disagreement between the direct and indirect evidence for one or more treatment comparisons.
Investigation & Resolution Protocol:
Step 1: Verify Data Extraction and Analysis
- Double-check the data entered into your statistical model for accuracy.
- Ensure that multi-arm trials have been correctly handled in the analysis to preserve within-trial randomization [8].
Step 2: Conduct a Local Inspection
- Use the node-splitting method to isolate the inconsistent comparison. This method separates the direct and indirect evidence for a specific node (treatment) and estimates the difference between them [7].
Step 3: Investigate Conceptual Causes
- Incoherence is often a sign of a violation of the transitivity assumption. Return to the conceptual evaluation of transitivity [8]. Use the following table to guide your investigation of potential effect modifiers:
Table: Checklist for Investigating Sources of Intransitivity
Investigation Area Key Questions to Ask Common Effect Modifiers Population Is the patient population comparable across comparisons? Are there differences in disease severity, duration, or demographic profiles? Disease duration, baseline severity, age, sex, comorbidities [6]. Intervention Are the interventions administered in a similar way? Is the dose or delivery method comparable? Dosage, formulation, treatment duration, concomitant therapies [6]. Study Methods Do the trials informing different comparisons have similar designs and risk of bias? Risk of bias items (e.g., randomization, blinding), study duration, outcome definitions [6] [8]. Step 4: Implement a Solution
- Based on your findings from Step 3, you can:
- Perform a meta-regression to adjust for the identified effect modifier.
- Use a network meta-regression model if the effect modifier is measured at the study level [5] [6].
- Consider presenting results for subgroups if the transitivity violation is limited to a specific patient population or intervention type.
- Based on your findings from Step 3, you can:
Problem: Evaluating Transitivity with Many Potential Effect Modifiers
Issue: It is challenging to visually or statistically assess the distribution of numerous clinical and methodological characteristics across all treatment comparisons.
Investigation & Resolution Protocol:
Step 1: Identify and Prioritize Effect Modifiers
Step 2: Calculate Dissimilarity Between Comparisons
- Adopt a novel methodological approach that uses Gower's Dissimilarity Coefficient [6]. This metric calculates the overall dissimilarity between pairs of studies (and by extension, between treatment comparisons) based on a mix of quantitative (e.g., mean age) and qualitative (e.g., concomitant medication use) characteristics [6].
- The result is a dissimilarity matrix that quantifies the clinical and methodological heterogeneity within the network.
Step 3: Apply Hierarchical Clustering
- Use the dissimilarity matrix to perform hierarchical clustering [6]. This unsupervised learning method groups highly similar treatment comparisons into clusters while separating dissimilar ones.
- Visualize the results using a dendrogram and heatmap. This helps identify "hot spots" of potential intransitivity where certain comparisons cluster separately from others, warranting closer scrutiny [6].
Step 4: Interpret and Act on Findings
- The clustering pattern provides a semi-objective judgment on the plausibility of transitivity. If studies are organized into several distinct clusters based on key characteristics, this suggests potential intransitivity [6].
- This finding necessitates a closer examination of the evidence base to decide if NMA is feasible or if adjustments are needed [6].
Data Presentation
Table: Reporting and Evaluation of Transitivity Before and After PRISMA-NMA Guidelines (Survey of 721 NMAs) [5]
| Reporting and Evaluation Item | Before PRISMA-NMA (%) | After PRISMA-NMA (%) | Odds Ratio (95% CI) |
|---|---|---|---|
| Provided a protocol | -- | -- | 3.94 (2.79–5.64) |
| Pre-planned transitivity evaluation | -- | -- | 3.01 (1.54–6.23) |
| Reported the evaluation and results | -- | -- | 2.10 (1.55–2.86) |
| Defined transitivity | -- | -- | 0.57 (0.42–0.79) |
| Discussed implications of transitivity | -- | -- | 0.48 (0.27–0.85) |
| Evaluated transitivity statistically | 40% | 54% | -- |
| Evaluated transitivity conceptually | 12% | 11% | -- |
| Used consistency evaluation | 34% | 47% | -- |
| Inferred plausibility of transitivity | 22% | 18% | -- |
Experimental Protocol: A Framework for Evaluating Transitivity
Objective: To conceptually and empirically evaluate the transitivity assumption in a network meta-analysis.
Methodology: This protocol outlines a step-by-step process for a thorough transitivity assessment, integrating both traditional and novel methods.
Pre-specification in Protocol:
- State the transitivity assumption in the systematic review protocol.
- Pre-plan the evaluation methods and list all potential effect modifiers justified by clinical or methodological reasoning [5].
Data Collection:
- From each included study, extract a common set of participant and study characteristics that are suspected effect modifiers. These can be quantitative (e.g., mean age, disease duration) or qualitative (e.g., prior treatment failure, study design feature) [6].
Conceptual Evaluation:
- Tabulate or Visualize: Create summary tables, bar plots, or box plots to show the distribution of each effect modifier across the different treatment comparisons [6].
- Assess Comparability: Judge whether the distributions are sufficiently similar across comparisons. This relies on subjective judgment informed by clinical expertise [5] [8].
Empirical Evaluation using Clustering (Optional but Recommended):
- Calculate Dissimilarity: Use Gower's Dissimilarity Coefficient to compute a dissimilarity matrix for all study pairs across the extracted characteristics [6].
- Perform Clustering: Apply hierarchical clustering to the dissimilarity matrix.
- Visualize and Interpret: Generate a dendrogram and heatmap. Examine if studies cluster by treatment comparison rather than being intermingled, which would signal potential intransitivity [6].
Conclusion and Reporting:
- Based on the conceptual and empirical evaluations, make an overall judgment on the plausibility of transitivity.
- Justify the conclusion in the review report, citing the comparability of trials and/or the results of any statistical or clustering evaluations [5].
Logical Workflow and Pathway Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Methodological Tools for Transitivity and Consistency Evaluation
| Tool / Method | Function in NMA | Key Considerations |
|---|---|---|
| Gower's Dissimilarity Coefficient [6] | Quantifies the overall dissimilarity between two studies across multiple mixed-type (numeric and categorical) characteristics. | Handles missing data by considering only characteristics reported in both studies. Essential for the clustering approach. |
| Hierarchical Clustering [6] | An unsupervised machine learning method that groups similar treatment comparisons based on their characteristics. Identifies potential "hot spots" of intransitivity. | Results are exploratory. The choice of the optimal number of clusters may require subjective judgment supplemented by validity measures. |
| Node-Splitting Method [7] | A statistical technique used to detect local inconsistency. It separates direct and indirect evidence for a specific comparison and tests if they disagree. | Useful for pin-pointing which specific loop in the network is inconsistent. Requires a closed loop in the network. |
| Network Meta-Regression [5] [6] | Adjusts treatment effect estimates for study-level covariates (effect modifiers). Can help mitigate confounding bias if transitivity is questionable. | Requires a sufficient number of studies to be informative. Power is often low in sparse networks. |
| PRISMA-NMA Checklist [5] | A reporting guideline that ensures transparent and complete reporting of NMA methods and results, including the assessment of transitivity and consistency. | Following the checklist improves the review's credibility. Systematic reviews published after PRISMA-NMA show better reporting in some aspects [5]. |
| PF-06685249 | `PF-06685249|LPA Receptor Antagonist|Research Use Only` | PF-06685249 is a potent LPA receptor antagonist for research. This product is For Research Use Only and not intended for diagnostic or therapeutic use. |
| Pralidoxime Iodide | Pralidoxime Iodide | Pralidoxime iodide is a research-grade oxime for studying organophosphate poisoning mechanisms. This product is for Research Use Only (RUO), not for human consumption. |
FAQs on Core Heterogeneity Concepts
Q1: What do the Q, I², and τ² statistics each tell me about my meta-analysis? These three statistics provide complementary information about the variability between studies in your meta-analysis.
- Q statistic (Cochran's Q): This is a test statistic that assesses whether the observed differences in study results are larger than would be expected by chance alone. A significant p-value (typically <0.05) suggests the presence of genuine heterogeneity [9] [2].
- I² statistic: This quantifies the proportion of total variability in effect estimates that is due to heterogeneity rather than sampling error (chance). It is expressed as a percentage. For example, an I² of 75% means that 75% of the total variation across studies is attributable to real differences in effect sizes [9] [10].
- τ² statistic (Tau-squared): This quantifies the absolute magnitude of the between-study variance. It is measured in the same units as your effect size (e.g., log odds ratio, mean difference), providing a direct measure of the dispersion of true effects [2] [10].
Q2: How should I interpret different I² values in my drug efficacy analysis? While I² should not be interpreted using rigid thresholds, the following guidelines are commonly used as a rule of thumb [10]:
- I² = 25%: Considered low heterogeneity.
- I² = 50%: Considered moderate heterogeneity.
- I² = 75%: Considered substantial heterogeneity. Important Caveat: I² can be unreliable when the number of studies or the number of events in studies is small. It also depends on the precision of the included studies. Always consider the confidence interval for I² and the clinical context of the observed variation [11].
Q3: My meta-analysis has few studies. Are my heterogeneity statistics reliable? Meta-analyses with a limited number of studies pose challenges for interpreting heterogeneity. With few studies, the Q statistic has low power to detect heterogeneity, which may lead to an underestimation of true variability [9] [11]. The I² statistic can be unstable and imprecise. One empirical study suggested that estimates may fluctuate until a meta-analysis includes approximately 500 events and 14 trials [11]. It is therefore crucial to report and consider the confidence intervals for I² in such situations, as they better reflect the underlying uncertainty [11].
Q4: When should I use a random-effects model instead of a fixed-effect model? The choice of model depends on your assumptions about the studies included.
- Use a fixed-effect model only if you believe all studies are estimating a single, common effect size, and that any observed differences are solely due to sampling error [9] [2].
- Use a random-effects model if you believe that the true effect size can vary from study to study due to differences in populations, interventions, or other factors. The random-effects model explicitly incorporates the between-study variance τ² into its calculations and is often considered a more natural choice in medical and drug development contexts [9] [2].
Troubleshooting Guides
Issue 1: High and Significant Q Statistic
Problem: Your analysis yields a Cochran's Q statistic with a significant p-value, indicating substantial variability between studies.
Diagnosis and Interpretation:
- A significant Q statistic confirms that heterogeneity exists beyond sampling error [2]. The next step is to quantify and interpret this heterogeneity using I² and τ².
Recommended Actions:
- Quantify the Heterogeneity: Calculate I² to understand the proportion of total variability due to heterogeneity, and τ² to understand its absolute magnitude [2] [10].
- Investigate Sources: Do not stop at the statistics. Perform subgroup analyses or meta-regressions to explore potential clinical or methodological sources of the heterogeneity (e.g., drug dosage, patient demographics, study risk of bias) [2].
- Report Appropriately: Always present the estimates of τ² and I² alongside the Q statistic and its p-value to give a complete picture of the heterogeneity [2] [10].
Issue 2: High I² Value
Problem: Your meta-analysis shows a high I² value (e.g., >75%), suggesting a large proportion of the variability is due to heterogeneity.
Diagnosis and Interpretation:
- A high I² indicates that the percentage of variability from heterogeneity is high [10]. However, it does not inform you about the magnitude or clinical importance of this heterogeneity. A high I² can occur even with small, clinically irrelevant differences if the included studies are very precise (e.g., have large sample sizes) [10].
Recommended Actions:
- Check τ²: Examine the τ² value. A high I² with a small τ² may indicate that the absolute magnitude of heterogeneity is not clinically worrisome, despite being a large proportion of the total variation.
- Consider the Clinical Relevance: Judge whether the predicted range of effects, perhaps visualized using a prediction interval, includes clinically important differences [2].
- Avoid Over-reliance: Do not use I² in isolation. It should be interpreted alongside τ² and the clinical context of the analyzed outcome [2] [10].
Issue 3: Choosing an Estimator for τ²
Problem: You are unsure which statistical estimator to use for calculating the between-study variance τ² in a random-effects model.
Diagnosis and Interpretation:
- The choice of estimator can impact the pooled estimate and its confidence interval, especially when the number of studies is small [2].
Recommended Actions:
- Prefer Advanced Estimators: The DerSimonian-Laird (DL) estimator is historically common but is known to be biased, particularly with few studies or high heterogeneity. It is no longer recommended as the default [2].
- Use Modern Defaults: Opt for the Restricted Maximum Likelihood (REML) or Paule-Mandel estimators, which are generally less biased and are now considered standard for frequentist meta-analysis [2].
- Consider Bayesian Methods: For complex models like network meta-analyses or when dealing with very sparse data, Bayesian methods can be a flexible alternative, allowing you to incorporate prior knowledge about the heterogeneity [2].
Key Statistical Protocols & Data
Protocol 1: Calculating Heterogeneity Statistics
This protocol outlines the standard methodology for deriving key heterogeneity measures from your meta-analysis data [10].
Formula:
- Cochran's Q: ( Q = \sum\limits{k=1}^K wk (\hat\thetak - \frac{\sum\limits{k=1}^K wk \hat\thetak}{\sum\limits{k=1}^K wk})^{2} ) Where (k) is an individual study, (K) is the total number of studies, (\hat\thetak) is the effect estimate of study (k), and (wk) is the weight (typically the inverse of the variance) of study (k).
- I² Statistic: (I^{2} = max \left{0, \frac{Q-(K-1)}{Q} \right})
- τ² Statistic: Several estimators exist (see Troubleshooting Guide, Issue 3). The DerSimonian-Laird estimator is: ( \tau^{2} = \frac{Q - (K-1)}{\sum wi - \frac{\sum wi^2}{\sum w_i}} )
Workflow Diagram:
Protocol 2: Applying a Random-Effects Model
This protocol details the steps for pooling studies using a random-effects model, which accounts for heterogeneity via τ².
Formula: The weight assigned to each study in a random-effects model is ( wk^* = 1 / (vk + \tau^2) ), where (vk) is the within-study variance for study (k) and (\tau^2) is the estimated between-study variance. The pooled effect is then: ( \theta^* = \frac{\sum wk^* \thetak}{\sum wk^*} )
Workflow Diagram:
Research Reagent Solutions: Statistical Toolkit
Table: Essential Components for Heterogeneity Analysis in Meta-Analysis
| Item Name | Function/Description | Key Considerations |
|---|---|---|
| Cochran's Q Statistic | A hypothesis test to determine if observed heterogeneity is statistically significant [2]. | Low power with few studies; high power with many studies, which may flag trivial differences as significant [9] [2]. |
| I² Statistic | Describes the percentage of total variation across studies that is due to heterogeneity rather than chance [9] [10]. | Can be misinterpreted; a high value does not necessarily mean the heterogeneity is clinically important, especially with high-precision studies [10]. |
| τ² (Tau-squared) | Quantifies the actual magnitude of between-study variance in the units of the effect measure [2]. | Choosing an unbiased estimator (e.g., REML) is critical for accurate results, particularly when the number of studies is small [2]. |
| Prediction Interval | A range in which the true effect of a new, similar study is expected to lie, providing a more useful clinical interpretation of τ² [2]. | Directly communicates the implications of heterogeneity for practice and future research [2]. |
| Restricted Maximum Likelihood (REML) | A preferred method for estimating τ² that is less biased than the older DerSimonian-Laird method [2]. | Now considered a standard approach for frequentist random-effects meta-analysis [2]. |
| Propargyl-PEG5-amine | Propargyl-PEG5-amine, MF:C13H25NO5, MW:275.34 g/mol | Chemical Reagent |
| Propargyl-PEG6-acid | Propargyl-PEG6-acid, MF:C16H28O8, MW:348.39 g/mol | Chemical Reagent |
In Network Meta-Analysis (NMA), network geometry refers to the structure and arrangement of connections between different treatments based on the available clinical trials. This geometry is not merely a visual aid; it fundamentally shapes how evidence flows through the network and directly influences the statistical heterogeneity—the variation in treatment effects across studies. Understanding this relationship is crucial for interpreting NMA results reliably, especially in drug research where multiple treatment options exist.
The geometry of an evidence network reveals potential biases in the research landscape. Certain treatments may be extensively compared against placebos but rarely against each other, creating "star-shaped" networks. This imbalance can affect the confidence in both direct and indirect evidence, subsequently impacting heterogeneity. This technical support guide provides targeted troubleshooting advice to help researchers diagnose and address geometry-related heterogeneity issues in their NMA projects.
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: How can I visually assess if my network's geometry might be causing heterogeneity?
- Problem: You suspect the structure of your evidence network is contributing to inconsistent results.
- Solution: Begin by creating and critically examining a network diagram. Look for imbalances, such as:
- Star-shaped networks: Where one treatment (often a placebo or standard care) is the sole connector for many other treatments.
- Thick and thin lines: Comparisons with many trials (thick lines) will have more robust direct evidence, while those with single trials (thin lines) rely more heavily on the transitivity assumption.
- Disconnected networks: Isolated groups of treatments with no connecting path, which prevent some comparisons altogether. The diagram below illustrates a sample network geometry, highlighting key features like closed loops and evidence thickness.
Sample Network Geometry Showing Evidence Flow
FAQ 2: My inconsistency tests are significant. How do I determine which comparison is the culprit?
- Problem: Statistical tests indicate a significant disagreement between direct and indirect evidence in your network (a lack of coherence) [12].
- Solution:
- Identify Closed Loops: Use your network diagram to find all closed loops of evidence (e.g., where treatments A, B, and C have been compared in a triangle: A vs. B, B vs. C, and A vs. C) [12].
- Separate Direct and Indirect Evidence: For each loop, statistically separate the direct evidence (from head-to-head trials) from the indirect evidence (inferred via the common comparator).
- Use Node-Splitting Models: Employ statistical methods like node-splitting to test for inconsistency in each specific loop. This helps pinpoint exactly which direct comparison is in conflict with the rest of the network [12].
FAQ 3: The treatments in my network seem too diverse. How do I evaluate the transitivity assumption?
- Problem: You are concerned that clinical or methodological differences between trials (e.g., in patient population, dose, or study duration) violate the transitivity assumption, leading to heterogeneity [12].
- Solution:
- Create Subnetworks: Group trials that are more clinically homogeneous (e.g., only studies with severe disease, or only studies using a high drug dose).
- Compare Effects: Conduct separate NMAs on these subnetworks. If the treatment effect estimates differ significantly between subnetworks, transitivity may be violated, and the overall NMA may be unreliable.
- Use Meta-Regression: Statistically model whether study-level covariates (like disease severity or publication year) explain the heterogeneity in the network.
FAQ 4: How can I effectively visualize results from a complex NMA with many outcomes?
- Problem: Presenting results for multiple treatments across multiple outcomes is challenging.
- Solution: Consider using advanced graphical tools like the Kilim plot [13]. This plot compactly summarizes results for all treatments and outcomes, displaying absolute effects (e.g., event rates) rather than relative effects. Cells within the plot can be color-coded to represent the strength of statistical evidence, making it easier to identify treatments that perform well or poorly across the board.
Experimental Protocols for Investigating Heterogeneity
Protocol for Testing Local Incoherence via Node-Splitting
Objective: To identify specific comparisons within the network where direct and indirect evidence are inconsistent.
Materials: Statistical software with NMA capabilities (e.g., R with netmeta or gemtc packages, Stata with network suite).
Methodology:
- Model Specification: Fit a node-splitting model to your network. This model separately estimates the effect size for a specific comparison using both its direct evidence and its indirect evidence from all other paths in the network.
- Iteration: Run the model for every possible treatment comparison that forms a closed loop in the network.
- Statistical Testing: For each comparison, the model will provide a p-value for the difference between the direct and indirect estimate.
- Interpretation: A statistically significant p-value (e.g., < 0.05) indicates local incoherence for that particular comparison. This suggests that the specific loop contributing to that comparison may be a major source of overall heterogeneity.
Protocol for Visualizing Complex Component NMA (CNMA) Structures
Objective: To clearly visualize the data structure of a Component NMA, where interventions are broken down into their individual components, which is often complex and prone to heterogeneity.
Materials: R or Python for generating specialized plots.
Methodology:
- Data Structuring: Organize your arm-level data to indicate which components are present in each intervention arm of each trial [14].
- Plot Selection: Based on your needs, generate one or more of the following novel CNMA visualizations [14]:
- CNMA-UpSet Plot: Ideal for networks with a large number of components, this plot effectively shows which combinations of components have been tested and how many trials contribute evidence for each combination.
- CNMA Heat Map: A grid where rows are components and columns are trials. This illustrates the distribution of components across the evidence base, revealing which components are commonly studied together or in isolation.
- CNMA-Circle Plot: Visualizes the combinations of components that differ between trial arms, helping to understand the direct evidence for additive or interactive effects.
The Scientist's Toolkit: Essential Research Reagents & Materials
The table below lists key methodological tools and concepts essential for diagnosing and managing heterogeneity in NMA.
| Tool/Concept | Function & Explanation |
|---|---|
| Network Diagram | A visual map of the evidence. It uses nodes (treatments) and lines/edges (direct comparisons). The thickness of lines and size of nodes often represent the amount of evidence, immediately highlighting potential imbalances in the network geometry [12]. |
| Transitivity Assessment | The theoretical foundation of NMA. It is the assumption that the included trials are sufficiently similar in their clinical and methodological characteristics (e.g., patient populations, outcomes) to allow for valid indirect comparisons. Violations cause heterogeneity [12]. |
| Statistical Incoherence | The statistical manifestation of transitivity violation. It is a measurable disagreement between direct and indirect evidence for the same treatment comparison. Tools like node-splitting and design-by-treatment interaction models are used to test for it [12]. |
| Component NMA (CNMA) Models | A modeling approach that estimates the effect of individual intervention components (e.g., 'behavioral therapy,' 'drug dose') rather than whole interventions. This can help reduce heterogeneity and uncertainty by pooling evidence more efficiently across different combinations of components [14]. |
| Kilim Plot | A graphical tool for visualizing NMA results on multiple outcomes simultaneously. It presents results as absolute effects (e.g., event rates) and uses color to represent the strength of statistical evidence, aiding in the interpretation of complex results and identification of heterogeneity patterns across outcomes [13]. |
| Propargyl-PEG6-N3 | Propargyl-PEG6-N3, MF:C15H27N3O6, MW:345.39 g/mol |
| Nesolicaftor | Nesolicaftor, CAS:1953130-87-4, MF:C18H18N4O4, MW:354.4 g/mol |
Visualizing Evidence Flow and Decision Pathways
The following diagram outlines a logical workflow for troubleshooting heterogeneity, linking diagnostic questions to analytical techniques and potential solutions.
Heterogeneity Troubleshooting Workflow
Network meta-analysis (NMA) is an advanced statistical technique that compares three or more interventions simultaneously by combining both direct and indirect evidence across a network of studies [8]. Unlike conventional pairwise meta-analyses that are limited to direct comparisons, NMA enables researchers to estimate relative treatment effects even between interventions that have never been directly compared in clinical trials [15] [7]. This approach is particularly valuable in pharmaceutical research where multiple competing interventions often exist for a single condition, and conducting a "mega-RCT" comparing all treatments is practically impossible [7].
Heterogeneity refers to the variability in study characteristics and results, and represents a fundamental challenge in NMA. Properly understanding, assessing, and managing heterogeneity is crucial for producing valid and reliable results that can inform clinical decision-making and health policy [16] [7]. Heterogeneity in NMA can be categorized into three main types: clinical heterogeneity (variability in participants, interventions, and outcomes), methodological heterogeneity (variability in study design and risk of bias), and statistical heterogeneity (variability in the intervention effects being evaluated across studies) [16].
Core Concepts and Terminology
Key NMA Terminology
Direct Evidence: Comparison of two or more interventions within individual studies [7].
Indirect Evidence: Comparisons between interventions made through one or more common comparators [8] [7]. For example, if intervention A has been compared to B, and A has also been compared to C, then B and C can be indirectly compared through their common comparator A [8].
Transitivity: The assumption that different sets of randomized trials are similar, on average, in all important factors other than the intervention comparison being made [8]. This requires that studies comparing different interventions are sufficiently similar in terms of effect modifiers [8].
Consistency (Coherence): The statistical agreement between direct and indirect evidence for the same comparison [8] [7]. Incoherence occurs when different sources of information about a particular intervention comparison disagree [8].
Network Geometry and Visualization
A network diagram graphically depicts the structure of a network of interventions, consisting of nodes representing interventions and lines showing available direct comparisons between them [8]. The geometry of the network reveals important information about the available evidence:
- Closed Loop: Exists when both direct and indirect comparisons are available for a treatment pair [7].
- Open Triangle: Exists when the shape formed by direct comparisons is incomplete [7].
- Network Connectivity: All included studies must be connected to allow comparisons across all interventions [7].
Network Geometry Showing Direct and Indirect Comparisons
Troubleshooting Guides: Identifying and Managing Heterogeneity
Clinical Heterogeneity
Problem: Variability in participant characteristics, intervention implementations, or outcome measurements across studies introduces clinical heterogeneity that may compromise transitivity assumptions [16].
Symptoms:
- Significant statistical heterogeneity (I² > 50%) in pairwise meta-analyses
- Incoherence between direct and indirect evidence
- Differing patient case-mix across treatment comparisons
- Variable intervention fidelity or delivery methods
Solutions:
- Stratified Randomization: In primary trials, stratify randomization on center and key prognostic factors to prevent imbalance [16].
- Relax Selection Criteria: Use minimal exclusion criteria to better represent the target population [16].
- Account for Center Effects: Use random-effects models that better accommodate between-center heterogeneity [16].
- Subgroup Analysis Limitation: Limit subgroup analyses to those that meaningfully inform clinical decision-making [16].
Methodological Heterogeneity
Problem: Variability in study designs, risk of bias, or outcome assessment methods introduces methodological heterogeneity that can affect treatment effect estimates [16].
Symptoms:
- Differing randomization or blinding procedures across studies
- Variable follow-up durations
- Inconsistent outcome measurement tools or timing
- Differential application of eligibility criteria across centers
Solutions:
- Comprehensive Risk of Bias Assessment: Use standardized tools (e.g., Cochrane RoB 2.0) to evaluate all included studies.
- Sensitivity Analyses: Exclude studies with high risk of bias to assess their impact on overall estimates.
- Standardized Outcome Definitions: Where possible, use objective outcomes that are routinely collected in clinical practice [16].
- Meta-regression: Explore whether methodological features explain heterogeneity in treatment effects.
Statistical Heterogeneity and Incoherence
Problem: Discrepancies between direct and indirect evidence (incoherence) threaten the validity of NMA results [8] [7].
Symptoms:
- Significant disagreement between direct and indirect estimates for the same comparison
- Incoherence P-values < 0.05 in statistical tests
- Inconsistent treatment rankings across different outcome measures
Solutions:
- Local Incoherence Assessment: Use node-splitting methods to evaluate inconsistency at specific treatment comparisons.
- Global Incoherence Assessment: Employ design-by-treatment interaction models to assess overall network consistency.
- Use Higher Certainty Evidence: When incoherence exists, prioritize evidence from direct comparisons with higher certainty [15].
- Investigate Effect Modifiers: Explore clinical or methodological differences that might explain the observed incoherence.
Table 1: Common Sources of Heterogeneity in Pharmaceutical NMAs
| Source Category | Specific Sources | Impact on NMA | Management Strategies |
|---|---|---|---|
| Patient Characteristics | Age, disease severity, comorbidities, genetic factors, socioeconomic status | Affects treatment response and generalizability | Relax selection criteria [16], adjust for prognostic factors, subgroup analyses |
| Intervention Factors | Dosage, administration route, treatment duration, concomitant medications | Alters effective treatment intensity and safety | Dose-response meta-analysis, class-effect models, treatment adherence assessment |
| Methodological Elements | Randomization methods, blinding, outcome assessment, follow-up duration | Introduces bias varying across comparisons | Risk of bias assessment, sensitivity analyses, meta-regression [16] |
| Setting-related Factors | Care setting (primary vs. tertiary), geographical region, healthcare system | Affects implementation and effectiveness | Center stratification [16], random-effects models, contextual factor analysis |
Experimental Protocols for Heterogeneity Assessment
Transitivity Assessment Protocol
Purpose: To evaluate whether the transitivity assumption is reasonable for the network of studies.
Materials: Comprehensive dataset of included studies with detailed characteristics.
Procedure:
- List all potential effect modifiers relevant to the research question.
- Create a table comparing the distribution of these effect modifiers across different treatment comparisons.
- Assess whether studies comparing different interventions are sufficiently similar in terms of these effect modifiers.
- Qualitatively judge whether transitivity assumption is plausible.
- Document any potential violations of transitivity that might explain future incoherence.
Interpretation: If important effect modifiers are imbalanced across treatment comparisons, the transitivity assumption may be violated, and NMA results should be interpreted with caution.
Incoherence Evaluation Protocol
Purpose: To statistically assess agreement between direct and indirect evidence.
Materials: Network dataset with direct and indirect evidence sources.
Procedure:
- Local Incoherence Assessment:
- Use node-splitting method to separate direct and indirect evidence for each comparison.
- Test for statistically significant differences (P < 0.05) between direct and indirect estimates.
- Apply appropriate multiple testing corrections.
- Global Incoherence Assessment:
- Fit both consistency and inconsistency models.
- Use likelihood ratio test or Deviance Information Criterion (DIC) to compare model fit.
- If inconsistency model fits better, identify specific comparisons contributing to incoherence.
- Investigate Sources: Explore clinical or methodological differences that might explain identified incoherence.
Interpretation: Significant incoherence suggests violation of transitivity assumption and may limit the validity of NMA results.
Frequently Asked Questions (FAQs)
Q1: How much heterogeneity is acceptable in an NMA?
There are no universally accepted thresholds for acceptable heterogeneity in NMA. The impact depends on the research context and the magnitude of treatment effects. Rather than focusing solely on statistical measures, consider whether heterogeneity affects the conclusions and clinical applicability of results. The key question is whether heterogeneity prevents meaningful conclusions that can inform clinical decision-making.
Q2: What should I do when I detect significant incoherence between direct and indirect evidence?
When incoherence is detected: (1) Present both direct and indirect estimates separately rather than the combined network estimate; (2) If the direct evidence has higher certainty, prioritize it over the network estimate [15]; (3) Investigate potential effect modifiers that might explain the discrepancy through subgroup analysis or meta-regression; (4) Acknowledge the uncertainty in your conclusions and consider presenting alternative analyses.
Q3: How can I plan a primary trial to facilitate future inclusion in NMAs?
To enhance future NMA compatibility: (1) Select comparators that are relevant to clinical practice, not just placebos; (2) Use standardized outcome measures consistent with other trials in the field; (3) Report detailed patient characteristics and potential effect modifiers; (4) Follow CONSORT reporting guidelines; (5) Consider using core outcome sets where available.
Q4: What are the most common mistakes in assessing and reporting heterogeneity in NMAs?
Common mistakes include: (1) Focusing only on statistical heterogeneity without considering clinical relevance; (2) Not adequately assessing transitivity assumption before conducting NMA; (3) Overinterpreting treatment rankings without considering uncertainty; (4) Using inappropriate heterogeneity measures (e.g., applying pairwise I² to network estimates); (5) Not conducting or properly reporting sensitivity analyses for heterogeneous findings.
Research Reagent Solutions: Methodological Tools
Table 2: Essential Methodological Tools for Heterogeneity Assessment in NMA
| Tool Category | Specific Tools/Methods | Primary Function | Application Context |
|---|---|---|---|
| Statistical Software | R (netmeta, gemtc packages), Stata, WinBUGS/OpenBUGS | Perform NMA statistical calculations | Bayesian and frequentist NMA implementation [7] |
| Heterogeneity Measurement | I² statistic, between-study variance (τ²), predictive intervals | Quantify statistical heterogeneity | Assessing variability in treatment effects across studies |
| Incoherence Detection | Node-splitting, design-by-treatment interaction test, side-splitting method | Identify discrepancies between direct and indirect evidence | Evaluating NMA validity assumptions [8] [7] |
| Risk of Bias Assessment | Cochrane RoB 2.0, ROBINS-I | Evaluate methodological quality of included studies | Identifying methodological heterogeneity sources [16] |
| Visualization Tools | Network diagrams, forest plots, rankograms, contribution plots | Visual representation of evidence network and results | Communicating NMA structure and findings clearly [8] |
Advanced Methodologies: Emerging Approaches
New Approach Methodologies (NAMs) are gaining regulatory momentum and represent a pivotal shift in how drug candidates are evaluated [17]. These include in vitro systems (3D cell cultures, organoids, organ-on-chip) and in silico approaches that can reduce animal testing while providing human-relevant mechanistic data [17].
The integration of artificial intelligence and machine learning with NMA offers promising approaches for handling heterogeneity: AI/ML can help distinguish signal from noise in biological data, reduce data dimensionality, and automate the comparison of alternative mechanistic models [17]. These approaches are particularly valuable for translating high-dimensional phenotypic data into clinically meaningful predictions.
NMA Heterogeneity Assessment Workflow
Effectively managing heterogeneity in pharmaceutical NMAs requires a systematic approach throughout the research process. Key best practices include:
- Proactive Planning: Consider NMA compatibility when designing primary trials and systematic review protocols.
- Comprehensive Assessment: Evaluate transitivity before conducting NMA and test for incoherence after analysis.
- Appropriate Interpretation: Consider both statistical measures and clinical relevance when interpreting heterogeneous results.
- Transparent Reporting: Clearly document sources of heterogeneity and their potential impact on conclusions.
- Methodological Rigor: Use appropriate statistical models that account for heterogeneity and uncertainty.
By implementing these strategies, researchers can enhance the validity and utility of NMAs for informing drug development decisions and clinical practice guidelines.
Advanced Methods for Investigating and Explaining Heterogeneity in Drug Networks
Frequently Asked Questions (FAQs)
1. What is network meta-regression and how does it differ from standard network meta-analysis? Network meta-regression (NMR) is an extension of network meta-analysis (NMA) that adds study-level covariates to the statistical model [18]. While standard NMA estimates the relative effects of multiple treatments, NMR investigates how these treatment effects change with study-level characteristics, often called effect modifiers [19]. This is particularly valuable for exploring heterogeneity (differences in treatment effects across studies) and inconsistency (disagreements between direct and indirect evidence) within a treatment network [18]. NMR allows researchers to explore interactions between treatments and study-level covariates, providing insights into why treatment effects might vary across different populations or settings [18].
2. When should I consider using network meta-regression in my analysis? You should consider NMR when your NMA shows substantial heterogeneity or inconsistency that might be explained by study-level characteristics [19]. This approach is particularly useful when you suspect that patient demographics (e.g., average age, disease severity), study methods (e.g., risk of bias, study duration), or treatment modalities might influence the relative treatment effects [8] [19]. NMR helps determine whether certain covariates modify treatment effects, which is crucial for making appropriate treatment recommendations for specific patient populations [18].
3. What are the key assumptions for valid network meta-regression? NMR relies on the same core assumptions as NMA but extends them to include covariates:
- Transitivity: The distribution of effect modifiers (covariates) should be similar across treatment comparisons [20] [8]. For example, studies comparing A vs. B should have similar covariate distributions to studies comparing A vs. C.
- Consistency (Coherence): The direct and indirect evidence for a treatment comparison should agree after accounting for the covariate effects [8] [21]. Statistical tests can examine whether disagreement remains after including covariates in the model.
- Similarity: Studies included in the network should be sufficiently similar in terms of populations, interventions, comparators, and outcomes [20].
- Linear Relationship: NMR typically assumes a linear relationship between covariates and treatment effects, though this can be checked and addressed if violated [19].
4. What types of covariates can be analyzed using network meta-regression? NMR can analyze various study-level covariates, including:
- Clinical Diversity: Average patient age, baseline risk, disease severity, comorbidities [19]
- Methodological Diversity: Risk of bias, study duration, year of publication [19]
- Treatment Characteristics: Dose, administration route, treatment duration
- Contextual Factors: Geographic region, healthcare setting [8]
5. How does MetaInsight facilitate network meta-regression? MetaInsight is a free, open-source web application that implements NMR through a point-and-click interface, eliminating the need for statistical programming [18]. It offers:
- Interactive covariate exploration with visualizations showing distribution of covariate values across studies [18]
- Novel visualizations showing which studies contribute to which comparisons simultaneously [18]
- Support for different types of regression coefficients (shared, exchangeable, unrelated) [18]
- Correct handling of uncertainty in baseline risk analysis [18]
Table 1: Types of Regression Coefficients in Network Meta-Regression
| Coefficient Type | Description | When to Use |
|---|---|---|
| Shared | Assumes the same relationship between the covariate and each treatment | When you expect the covariate to affect all treatments similarly |
| Exchangeable | Allows different but related relationships for each treatment | When the covariate effect might vary by treatment but you want to borrow strength across treatments |
| Unrelated | Estimates completely separate relationships for each treatment | When you suspect fundamentally different covariate effects for different treatments |
Troubleshooting Common NMR Implementation Issues
Problem: High Heterogeneity Persists After Adding Covariates
Potential Causes and Solutions:
- Insufficient Covariate Selection: The chosen covariates might not be the true effect modifiers. Consider conducting a systematic literature review to identify potential effect modifiers you may have overlooked [19].
- Non-linear Relationships: The relationship between the covariate and treatment effect might not be linear. Explore using fractional polynomials or restricted cubic splines to capture non-linear effects [19].
- Missing Important Covariates: Critical effect modifiers might not have been measured or reported in the primary studies. Acknowledge this limitation in your interpretation [8].
- Incorrect Functional Form: Continuous covariates might need transformation (e.g., log transformation) to properly model their relationship with treatment effects [19].
Problem: Computational Convergence Issues in NMR Models
Troubleshooting Steps:
- Simplify the Model: Start with a basic model with fewer parameters and gradually add complexity [19].
- Check Covariate Scaling: Rescale continuous covariates (e.g., mean-center) to improve numerical stability [19].
- Increase Iterations: Allow more iterations for the estimation algorithm to converge [19].
- Try Different Estimation Methods: Switch between estimation methods (e.g., REML vs. maximum likelihood) if available [19].
Problem: Inconsistency (Disagreement Between Direct and Indirect Evidence)
Diagnosis and Resolution:
- Use Statistical Tests: Employ specific inconsistency tests (e.g., node-splitting) to identify where inconsistency occurs [8].
- Check for Effect Modifiers: Inconsistency often indicates unaccounted effect modifiers. Explore whether adding covariates resolves the inconsistency [8].
- Examine Network Structure: Some network configurations (e.g., large loops with limited direct evidence) are more prone to inconsistency [8].
Table 2: Common NMR Errors and Solutions
| Error | Possible Causes | Solution Approaches |
|---|---|---|
| Model won't converge | Too many parameters, extreme covariate values, complex random effects structure | Simplify model, check for outliers, use different starting values, try alternative estimation methods |
| Implausible effect estimates | Model misspecification, data errors, insufficient data | Verify data quality, check model assumptions, conduct sensitivity analyses, consider alternative functional forms |
| Conflicting direct and indirect evidence | Violation of transitivity assumption, unmeasured effect modifiers | Test transitivity assumption, explore additional covariates, use inconsistency models if appropriate |
| High uncertainty in covariate effects | Limited sample size, insufficient variation in covariates, collinearity | Acknowledge limitation, consider Bayesian approaches with informative priors if justified, report results with appropriate caution |
Experimental Protocols and Methodologies
Protocol 1: Implementing Network Meta-Regression Using MetaInsight
Materials and Software Requirements:
- MetaInsight web application (https://apps.crsu.org.uk/MetaInsight) [18]
- Structured dataset with treatment effects and covariates
- Web browser with JavaScript enabled
Step-by-Step Methodology:
Data Preparation:
- Organize your NMA data with columns for study ID, treatment comparisons, effect sizes, variances, and covariates
- Ensure categorical covariates are properly coded
- Check for missing data in covariates
Model Specification:
- Select the regression coefficient type (shared, exchangeable, or unrelated) based on your assumptions about how covariates affect treatments [18]
- Choose appropriate link functions based on your outcome type (e.g., logit for binary outcomes)
- Specify random effects structure to account for between-study heterogeneity
Model Fitting and Diagnostics:
- Run the NMR model in MetaInsight
- Check convergence statistics
- Examine residual plots for patterns suggesting model misspecification
- Conduct sensitivity analyses with different prior distributions (if using Bayesian methods)
Interpretation and Visualization:
- Interpret covariate coefficients in the context of your outcome measure
- Use MetaInsight's novel visualizations to present which studies contribute to which comparisons [18]
- Create prediction plots showing how treatment effects vary across covariate values
Protocol 2: Assessing Transitivity Assumption in NMR
Background: The transitivity assumption requires that the distribution of effect modifiers is similar across treatment comparisons [8]. Violation of this assumption can lead to biased estimates.
Assessment Methodology:
Identify Potential Effect Modifiers:
- Conduct systematic literature review to identify patient or study characteristics that may modify treatment effects
- Consider clinical rationale for how covariates might influence treatment effects
Compare Covariate Distributions:
- Create summary tables comparing the distribution of covariates across different treatment comparisons
- Use statistical tests (e.g., ANOVA for continuous variables, chi-square for categorical) to assess differences
- Consider the clinical relevance of any differences, not just statistical significance
Evaluate Transitivity Violation Impact:
- Conduct sensitivity analyses excluding studies with extreme covariate values
- Fit separate models to subsets of studies with similar covariate profiles
- Use meta-regression to directly test whether treatment-by-covariate interactions explain observed differences
Figure 1: Network Meta-Regression Implementation Workflow
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Tools for Network Meta-Regression Analysis
| Tool/Resource | Function/Purpose | Implementation Notes |
|---|---|---|
| MetaInsight Application | Point-and-click interface for performing NMR without programming [18] | Free web-based tool; supports various regression coefficient types and visualization |
| R packages (gemtc, bnma) | Statistical programming packages for advanced NMR models [18] | Required for complex models beyond MetaInsight's capabilities; steep learning curve |
| PRISMA-NMA Guidelines | Reporting standards for network meta-analyses and extensions [20] | Ensure comprehensive reporting of methods and results |
| Cochrane Risk of Bias Tool | Assess methodological quality of included studies [8] | Important covariate for exploring heterogeneity due to study quality |
| GRADE Framework for NMA | Assess confidence in evidence from network meta-analyses [22] | Adapt for assessing confidence in NMR findings |
| ColorBrewer Palettes | Color selection for effective data visualizations [23] | Ensure accessibility for colorblind readers; use appropriate palette types |
| Pyrintegrin | Pyrintegrin, MF:C23H25N5O3S, MW:451.5 g/mol | Chemical Reagent |
| PZ-2891 | PZ-2891, CAS:2170608-82-7, MF:C20H23N5O, MW:349.438 | Chemical Reagent |
Figure 2: Conceptual Framework for Addressing Heterogeneity Through NMR
Advanced Implementation Considerations
Handling Different Types of Covariates in NMR:
- Continuous Covariates: Assess linearity assumption; consider transformations or flexible modeling approaches if non-linear relationships are suspected [19].
- Categorical Covariates: Use appropriate reference categories; be cautious with sparse categories which can lead to estimation problems.
- Baseline Risk: Special consideration is needed as it represents the outcome risk in the control group and requires proper accounting of uncertainty [18].
Statistical Implementation Details:
The statistical model for random-effects NMR can be represented as [19]:
[ \hat\thetai = \beta0 + \beta1 x{i1} + \beta2 x{i2} + \cdots + \betap x{ip} + ui + \varepsiloni ]
Where:
- (\hat\theta_i) is the estimated effect size in study (i)
- (\beta_0) is the intercept
- (\beta1, \beta2, \ldots, \betap) are regression coefficients for covariates (x{i1}, x{i2}, \ldots, x{ip})
- (u_i) is the random effect for study (i), assumed to follow (N(0, \tau^2))
- (\varepsiloni) is the sampling error, assumed to follow (N(0, \sigmai^2))
The model simultaneously estimates the regression coefficients ((\beta) parameters) and the between-study heterogeneity ((\tau^2)).
Best Practices for Reporting NMR Results:
- Transparent Methods: Clearly describe how covariates were selected, including both clinical rationale and statistical considerations [8].
- Model Specification: Report the type of regression coefficients used (shared, exchangeable, or unrelated) and the justification for this choice [18].
- Assumption Checks: Document how transitivity and consistency assumptions were assessed, including any statistical tests performed [8].
- Uncertainty Quantification: Report confidence/credible intervals for all covariate effects and acknowledge limitations in precision when sample sizes are small [19].
- Visualization: Use MetaInsight's visualization capabilities or create custom plots to show how treatment effects vary with covariates [18].
- Clinical Interpretation: Translate statistical findings into clinically meaningful information that can guide treatment decisions for specific patient populations.
Frequently Asked Questions
1. What is the core difference between a standard Network Meta-Analysis (NMA) and a Component NMA (CNMA)?
In a standard NMA, each unique combination of intervention components is treated as a separate, distinct node in the network [24] [25]. For example, the combinations "Exercise + Nutrition" and "Exercise + Psychosocial" would be two different nodes. The analysis estimates the effect of each entire combination.
In contrast, a CNMA model decomposes these complex interventions into their constituent parts [24] [25]. It estimates the effect of each individual component (e.g., Exercise, Nutrition, Psychosocial). The effect of a complex intervention is then modeled as a function of its components, either simply as the sum of its parts (additive model) or including interaction terms between components (interaction model) [25].
2. When should I consider using a CNMA model?
A CNMA is particularly useful when [24] [25]:
- Your research question aims to identify which specific components of an intervention are driving its effectiveness or harm.
- You want to predict the effect of a novel combination of components that has not been directly tested in a trial.
- The evidence network is sparse, with many unique combinations but few trials connecting them, leading to imprecise estimates in a standard NMA.
3. My CNMA model failed to run or produced errors. What are common culprits?
A frequent issue is that the evidence structure does not support the model you are trying to fit [24]. Specifically:
- Non-Identifiable Components: If two or more components always appear together in every trial (perfectly co-linear), the additive CNMA model cannot distinguish their individual effects [24].
- Insufficient Data for Interactions: An interaction CNMA model requires a rich evidence base. If there are not enough studies testing the relevant combinations, the model may fail to converge or produce estimates with extreme uncertainty [24] [25].
4. How can I visualize a network of components when a standard network diagram becomes too cluttered?
For complex component networks, novel visualizations are recommended over standard NMA network diagrams [24]:
- CNMA-UpSet Plot: Ideal for large networks, it effectively presents the arm-level data and shows which combinations of components have been studied.
- CNMA-Circle Plot: Visualizes the combinations of components that differ between trial arms and can be flexible in presenting additional information like the number of events.
- CNMA Heat Map: Can be used to inform decisions about which pairwise component interactions to consider including in the model.
Troubleshooting Guides
Problem: Determining the Unit of Analysis for Nodes
Background: A foundational step in planning a CNMA is deciding how to define the nodes in your evidence network. An incorrect strategy can lead to a model that is uninterpretable or does not answer the relevant clinical question.
Solution: Your node-making strategy should be driven by the review's specific research question. The following table outlines common strategies.
Table: Node-Making Strategies for Component Network Meta-Analysis
| Strategy | Description | Best Used When | Example from Prehabilitation Research [25] |
|---|---|---|---|
| Lumping | Grouping different complex interventions into a single node. | The question is whether a general class of intervention works compared to a control. | All prehabilitation interventions (regardless of components) vs. Usual Care. |
| Splitting (Standard NMA) | Treating every unique combination of components as a distinct node. | The question requires comparing specific, multi-component packages. | "Exercise + Nutrition" and "Exercise + Psychosocial" are separate nodes. |
| Component NMA | Defining nodes based on the presence or absence of individual components. | The goal is to disentangle the effect of individual components within complex interventions. | Nodes are the components themselves: "Exercise", "Nutrition", "Psychosocial". |
Problem: Selecting an Appropriate CNMA Model
Background: After defining components, you must choose a statistical model that correctly represents how these components combine to produce an effect. An incorrect model can lead to biased conclusions.
Solution: Follow this step-by-step protocol to select and check your model.
Experimental Protocol: Model Selection for CNMA
- Specify Components: Clearly list all intervention components from the included studies. In the prehabilitation example, these were Exercise (EXE), Nutrition (NUT), Cognitive (COG), and Psychosocial (PSY) [25].
- Fit the Additive CNMA Model: Start with the simplest model, which assumes the effect of a combination is the sum of the effects of its individual components (e.g., the effect of EXE+NUT = effect of EXE + effect of NUT) [24] [25].
- Check for Model Inadequacy: Assess if the additive model is sufficient. Significant disagreement between the CNMA model estimates and the direct evidence from standard NMA may suggest that important component interactions (synergy or antagonism) are present [25].
- Fit an Interaction CNMA Model: If the additive model is inadequate, include specific interaction terms. This model is a compromise between the additive model and the standard NMA [25].
- Clinical Input: Engage clinical experts to select biologically plausible interactions to test (e.g., an interaction between Exercise and Nutrition).
- Statistical Considerations: Only include interaction terms for which the evidence network provides sufficient data.
- Compare Models: Use statistical fit indices (e.g., Deviance Information Criterion) to compare the additive and interaction models, balancing fit and complexity.
Problem: Visualizing the Component Network and Data Structure
Background: A standard network graph can become unreadable with many components. You need a clear way to communicate which component combinations have been tested.
Solution: Creating a CNMA-Circle Plot The following workflow and diagram illustrate the logic behind creating a CNMA-circle plot, which is effective for this purpose [24].
Diagram: Workflow for Generating a CNMA-Circle Plot
The Scientist's Toolkit
Table: Essential Reagents for Component Network Meta-Analysis
| Reagent / Resource | Function / Description | Example Tools & Notes |
|---|---|---|
| R Statistical Software | Primary environment for statistical computing and modeling. | Base R environment. |
netmeta Package |
Implements frequentist network meta-analysis, a foundation for some CNMA models. | Key package for NMA and CNMA in frequentist framework [24]. |
tidygraph & ggraph |
A tidy API for graph (network) manipulation and visualization in R. | Used to create custom network visualizations [26]. |
| CNMA-UpSet Plot | A visualization method to display arm-level data and component combinations in large networks. | An alternative to complex network diagrams [24]. |
| Component Coding Matrix | A structured data frame (e.g., in CSV format) indicating the presence (1) or absence (0) of each component in every intervention arm. | The essential data structure for fitting CNMA models. |
| Factorial RCT Design | The ideal primary study design for cleanly estimating individual and interactive component effects. | Rarely used in practice due to resource constraints, which is why CNMA is needed [25]. |
| Quininib | Quininib|CysLT1 Antagonist|For Research | Quininib is a CysLT1 receptor antagonist for cancer and ocular disease research. This product is for research use only and not for human use. |
| Rabeximod | Rabeximod, CAS:872178-65-9, MF:C22H24ClN5O, MW:409.9 g/mol | Chemical Reagent |
## Frequently Asked Questions (FAQs)
1. What are class-effect models in Network Meta-Analysis and when should I use them? Class-effect models are hierarchical NMA models used when treatments can be grouped into classes based on shared mechanisms of action, chemical structure, or other common characteristics. You should consider them when making recommendations at the class level, addressing challenges with sparse data for individual treatments, or working with disconnected networks. These models can improve precision by borrowing strength from treatments within the same class [27] [28].
2. My network is disconnected, with no direct or indirect paths between some treatments. Can class-effect models help? Yes, implementing a class-effect model is a recognized method to connect disconnected networks. When disconnected treatments share a similar mechanism of action with connected treatments, assuming a class effect can provide the necessary link, allowing for the estimation of relative effects that would otherwise be impossible in a standard NMA [29].
3. What is the difference between common and exchangeable class-level effects? In a common class effect, all treatments within the same class are assumed to have identical class-level components—that is, there is no within-class variation. In contrast, an exchangeable class effect (or random class effect) assumes that the class-level components for treatments within a class are similar but not identical, and are drawn from a common distribution, allowing for within-class heterogeneity [27] [28].
4. How do I check if the assumption of a class effect is valid in my analysis? It is crucial to assess the class effect assumption as part of the model selection process. This involves testing for consistency, checking heterogeneity, and evaluating model fit. A structured model selection strategy should be employed to compare models with and without class effects, using statistical measures to identify the most suitable model for your data [27].
5. I have both randomized trials and non-randomized studies. Can I use class-effect models? Yes, hierarchical NMA models can be extended to synthesize evidence from both randomized controlled trials (RCTs) and non-randomized studies. These models can account for differences in study design, for instance by including random effects for study design or bias adjustment terms for non-randomized evidence, while also incorporating treatment class effects [30].
6. What software can I use to implement a class-effect NMA?
You can implement class-effect NMA models using the multinma R package. This package provides practical functions for fitting these models, testing assumptions, and presenting results [27] [28].
## Troubleshooting Common Experimental Issues
Problem: High Heterogeneity or Incoherence in the Network
Issue: The model shows signs of high heterogeneity (variation within treatment comparisons) or incoherence (disagreement between direct and indirect evidence).
Solution:
- Consider Hierarchical Models: Implement a hierarchical model that includes exchangeable class-level effects. This model can account for and help explain some of the heterogeneity by grouping treatments into classes [27] [30].
- Test Consistency Assumption: Use node-splitting or other diagnostic tests to check for inconsistency, especially in networks with closed loops [31].
- Model Fit Assessment: Compare the fit of different models (e.g., with fixed vs. random treatment-level effects) using measures like Deviance Information Criterion (DIC) or posterior mean residual deviance to select the one that best accounts for the observed heterogeneity [27].
Problem: Sparse Data for Individual Treatments
Issue: Some treatments in the network have very limited direct evidence, leading to imprecise effect estimates.
Solution:
- Use Random Class Effects: An NMA model with exchangeable (random) effects within classes allows information to be borrowed between treatments in the same class. This "borrowing of strength" can stabilize and improve the precision of estimates for sparsely-connected treatments [27] [28].
- Leverage Class-Level Inference: If the research question permits, focus on making inferences at the class level, which aggregates information across all treatments within a class and is more robust to sparse data for individual agents [27].
Problem: Disconnected Network of Evidence
Issue: The network of interventions is disconnected, meaning there are no direct or indirect paths between some treatments, preventing a complete NMA.
Solution:
- Apply Class Effect NMA: If disconnected treatments can be logically grouped into classes with other, connected treatments, a class-effect model can effectively connect the network. The assumption of a shared class effect provides a statistical bridge [29].
- Evaluate Alternative Methods: If class effects are not justifiable, other methods like component NMA or multiple outcomes NMA could be considered, though they rely on different assumptions [29].
Problem: Incorporating Data from Non-Randomized Studies
Issue: You wish to include data from non-randomized studies (e.g., to increase generalizability or fill evidence gaps) but are concerned about bias.
Solution:
- Use a Hierarchical Model Accounting for Design: Do not naively pool data from different study designs. Instead, use a hierarchical model that differentiates between RCTs and non-randomized studies. This can be done by including a separate random effect for study design [30].
- Apply Bias-Adjustment Extensions: Consider more advanced models that include a random bias term for non-randomized studies, adjusting for potential over- or underestimation of effects. These models can be further extended to allow the degree of bias to vary by treatment class [30].
## Model Selection and Comparison
Table 1: Overview of Key Class-Effect NMA Models and Their Applications
| Model Type | Key Assumption | Best Used When... | Key Consideration |
|---|---|---|---|
| Common Class Effect | All treatments within a class share an identical class-level component. | Prior knowledge strongly suggests minimal variation within classes. | Very strong assumption; can be unrealistic and may oversimplify. |
| Exchangeable Class Effect (Random) | Treatment-level effects within a class are similar and come from a common distribution. | Some within-class variation is expected; you want to "borrow strength" for sparse data. | Explains heterogeneity; more flexible and commonly used. |
| Hierarchical Model with Study Design | Study design (RCT vs. non-RCT) introduces a systematic layer of variation. | Combining randomized and non-randomized evidence. | Helps prevent bias from non-randomized studies and improves generalizability. |
| Bias-Adjustment Model | Non-randomized studies contain an estimable bias. | Including real-world evidence prone to unmeasured confounding. | Requires careful specification of bias structure; can increase uncertainty. |
## Experimental Protocols for Key Analyses
Protocol 1: Implementing a Basic Class-Effect NMA withmultinma
This protocol outlines the core steps for setting up and running a class-effect network meta-analysis in a Bayesian framework using the multinma R package [27] [28].
1. Define Network and Treatment Classes:
- Compile a dataset of all included studies, their compared interventions, and the observed relative effect sizes (e.g., log odds ratios) with their standard errors.
- Create a network object that defines the structure of the evidence.
- Map each treatment in the network to its respective class (e.g., "SSRI", "SNRI").
2. Model Specification:
- Select the type of class effect. For an exchangeable class effect, the model would hierarchically structure the treatment effects within a class to be similar but not identical.
- A simplified model formulation for the relative effect of treatment ( k ) relative to reference treatment 1 in class ( c ) can be represented as: ( d{1k} = \gammac + \zeta{k} ) where ( \gammac ) is the class-level effect (common or random), and ( \zeta_{k} ) is the treatment-specific effect (fixed or random) [27] [30].
3. Model Fitting and Convergence:
- Run the model using Markov Chain Monte Carlo (MCMC) methods.
- Check for convergence of the MCMC chains using diagnostics like the Gelman-Rubin statistic ((\hat{R} \approx 1.0)) and trace plots.
4. Assumption Checking and Model Fit:
- Test the consistency assumption if both direct and indirect evidence exist.
- Assess model fit using residual deviance and compare models with and without class effects using the DIC. A lower DIC indicates a better fit [27].
Protocol 2: Synthesizing RCT and Non-Randomized Data with Hierarchical Models
This protocol is for analyses that incorporate both RCT and non-randomized study data, using hierarchical models to account for design differences [30].
1. Data Preparation:
- Code studies by their design (e.g.,
design = 0for RCT,design = 1for non-randomized). - Ensure outcome measures are comparable or can be transformed to a common scale.
2. Model Specification with Study Design Effect:
- Extend the basic NMA model to include a random effect for study design. The model for the observed mean ( y{ik} ) in study ( i ), arm ( k ) can be written as: ( y{ik} \sim N(\theta{ik}, se{ik}^2) ) ( \theta{ik} = \mu{ij} + \delta{i,jk} + \beta{design[i]} )
- Here, ( \beta_{design[i]} ) is a bias adjustment term for the study's design, which can be given a prior distribution to reflect the expected direction and magnitude of bias in non-randomized studies [30].
3. Extended Bias-Adjustment (Optional):
- For a more sophisticated approach, allow the bias term ( \beta ) to vary by treatment class, acknowledging that bias might be different for different types of interventions [30].
4. Interpretation:
- The final treatment effect estimates will be adjusted for the inclusion of non-randomized data. Note that this often comes with increased uncertainty around the estimates, which is a more honest representation of the evidence [30].
## Visual Workflows
Diagram 1: Logic of Class-Effect Model Selection
Short Title: Class-Effect Model Selection Logic
Diagram 2: Hierarchical Structure of an Exchangeable Class-Effect Model
Short Title: Hierarchical Model Structure
## The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents and Resources for Implementing Class-Effect NMA
| Tool / Resource | Type | Primary Function | Example / Note |
|---|---|---|---|
multinma R package |
Software | Provides a comprehensive suite for fitting class-effect NMA models in a Bayesian framework. | The primary tool recommended for implementing the models discussed in this guide [27] [28]. |
| JAGS / Stan | Software | Bayesian inference engines that can be called by front-end packages to perform MCMC sampling. | multinma may use these under the hood for model fitting. |
| Treatment Class Taxonomy | Conceptual Framework | A pre-defined grouping of interventions into classes based on mechanism, structure, etc. | Essential for defining the hierarchy (e.g., grouping antidepressants into SSRIs, SNRIs) [27]. |
| Gelman-Rubin Diagnostic | Statistical Tool | Checks convergence of MCMC chains; values close to 1.0 indicate convergence. | A critical step to ensure model results are reliable. |
| Deviance Information Criterion (DIC) | Statistical Tool | Measures model fit and complexity for comparison and selection. | Used to decide between standard NMA, common, and exchangeable class-effect models [27]. |
| Node-Splitting Method | Statistical Tool | Tests for inconsistency between direct and indirect evidence in the network. | Important for validating the consistency assumption in connected networks [31]. |
| Ralaniten | Ralaniten, CAS:1203490-23-6, MF:C21H27ClO5, MW:394.9 g/mol | Chemical Reagent | Bench Chemicals |
| Ralmitaront | Ralmitaront, CAS:2133417-13-5, MF:C17H22N4O2, MW:314.4 g/mol | Chemical Reagent | Bench Chemicals |
Core Concepts: FAQs for Researchers
FAQ 1: What is the fundamental difference between a subgroup analysis and a sensitivity analysis?
A subgroup analysis is performed to assess whether an intervention's effect is consistent across predefined subsets of the study population. These groups are typically identified by characteristics such as age, gender, race, or disease severity. Its primary goal is to explore whether the treatment effect differs in these specific patient cohorts [32]. In contrast, a sensitivity analysis is a methodological procedure used to assess the robustness of the meta-analysis results. It systematically explores how different assumptions and methodological choices (like statistical models or inclusion criteria) impact the pooled results, helping to ensure that conclusions are not unduly influenced by specific studies or potential biases [32].
FAQ 2: When is a sensitivity analysis considered mandatory in a meta-analysis?
A sensitivity analysis is deemed necessary in several key scenarios [32]:
- Eligibility Criteria Concerns: Wide ranges in participant age, heterogeneity in the type of intervention (dose or route), or variable study designs.
- Heterogeneous Data Types: The analysis combines different data types (e.g., from clustered trials or crossover trials, continuous and ordinal data measuring the same outcome).
- Methodological Confusion: When there is uncertainty about the choice of statistical model (fixed-effect vs. random-effects) or the effect measure (odds ratio vs. risk ratio).
- High Risk of Bias: When included studies have a high risk of bias, or when a single study has a disproportionately large weight in the analysis.
FAQ 3: What is inconsistency in Network Meta-Analysis (NMA), and why is it a problem?
Inconsistency in NMA occurs when the direct evidence (from studies directly comparing treatments A and B) and the indirect evidence (for A vs. B, derived via a common comparator C) are in conflict [33]. This challenges a key assumption of NMA and can lead to biased treatment effect estimates, making the results difficult to interpret and unreliable for decision-making. Inconsistency can arise from biases in direct comparisons (e.g., publication bias) or when effect modifiers are distributed differently across different treatment comparisons [33].
FAQ 4: How does meta-regression differ from subgroup analysis?
While a subgroup analysis explores how treatment effects vary across distinct patient groups within the study, meta-regression is a statistical technique used to investigate whether specific study-level characteristics (e.g., average patient age, study duration, methodological quality) explain the heterogeneity in the observed results across the included studies [32]. It is a more formal method to model the relationship between study features and effect size.
Troubleshooting Guides for Analytical Challenges
Guide 1: Addressing Inconsistency in Network Meta-Analysis
Problem: Statistical tests or plots indicate the presence of inconsistency in your treatment network.
Solution Steps:
- Confirm Inconsistency: Use multiple methods to verify inconsistency. Do not rely on a single test. Key methods include [33]:
- Node-Splitting: Separates the direct and indirect evidence for a specific treatment comparison and assesses the discrepancy between them.
- Loop Inconsistency Approach: Assesses inconsistency within closed loops of three treatments (e.g., A vs. B, B vs. C, A vs. C) by comparing direct and indirect estimates.
- Inconsistency Parameter Model: A comprehensive model that includes parameters specifically for inconsistency within the network.
Investigate Sources: Once inconsistency is identified, investigate its potential causes [33]:
- Clinical Diversity: Are there differences in patient characteristics, co-interventions, or treatment dosages between the studies forming the direct and indirect evidence?
- Methodological Diversity: Do the studies in different comparisons have varying risks of bias (e.g., differences in blinding, randomization procedures)?
Model and Report: If inconsistency cannot be explained or resolved, use statistical models that account for it (e.g., the inconsistency model by Lu and Ades [33]). Always transparently report the presence of inconsistency and its potential impact on your conclusions.
Guide 2: Handling Excessive Heterogeneity in a Pairwise Meta-Analysis
Problem: The I² statistic indicates high heterogeneity, raising concerns about the validity of pooling results.
Solution Steps:
- Check Data and Analyses: First, verify for errors in data extraction or statistical coding.
- Explore Sources via Subgroup Analysis: Perform pre-specified subgroup analyses to see if the effect size is consistent across categories like patient age group, intervention dose, or study risk of bias.
- Assess Robustness via Sensitivity Analysis:
- Exclusion of Studies: Systematically exclude studies one at a time, particularly those with a high risk of bias or those that are outliers, to see if the overall result changes significantly [32].
- Model Choice: Re-run the analysis using both fixed-effect and random-effects models and compare the results. A random-effects model is often more appropriate when heterogeneity is present.
- Interpret and Report: If heterogeneity remains high and unexplained, avoid presenting a single summary estimate as definitive. Instead, discuss the range of effects and the possible reasons for the variability.
Guide 3: Ensuring Robust Sensitivity Analyses
Problem: Reviewers question the robustness of your meta-analysis findings.
Solution Steps:
- Pre-specify the Plan: The sensitivity analysis plan should be detailed in the study protocol before the analysis begins [32] [34]. This prevents data-driven decisions that can introduce bias.
- Define Scenarios: Clearly state what scenarios will be tested. Common ones include [32] [34]:
- The impact of studies with a high risk of bias.
- The choice of statistical model (fixed vs. random effects).
- The effect of different inclusion criteria (e.g., excluding unpublished studies).
- How missing data is handled.
- Compare Results: For each scenario, compare the pooled estimate and confidence interval to those from the primary analysis.
- Draw Conclusions: If the results and conclusions remain unchanged across all sensitivity analyses, you can state that the findings are robust. If results change materially, the results of the primary analysis must be interpreted with caution, and the reasons for the discrepancy should be discussed [32].
Data Presentation: Analytical Methods at a Glance
Table 1: Common Methods for Assessing Inconsistency in Network Meta-Analysis
| Method Name | Brief Description | Key Strength | Key Limitation |
|---|---|---|---|
| Node-Splitting [33] | Separates direct and indirect evidence for each comparison and tests for a significant difference. | Provides a local, comparison-specific assessment of inconsistency. | Can be cumbersome in large networks with many possible comparisons. |
| Loop Inconsistency Approach [33] | Evaluates inconsistency in each three-treatment loop by comparing direct and indirect evidence. | Intuitive and simple for networks of two-arm trials. | Becomes complex in large networks; requires adjustment for multiple testing. |
| Inconsistency Parameter Model [33] | A global model that includes parameters to account for inconsistency within the entire network. | Provides a comprehensive statistical framework for modeling inconsistency. | Model fit can depend on the structure of the network and the order of treatments. |
| Net Heat Plot [33] | A graphical tool that displays the contribution of each study design to the overall network inconsistency. | A visual aid for locating potential sources of inconsistency. | The underlying statistics may be misleading and do not reliably signal inconsistency [33]. |
Table 2: Thresholds for Interpreting Heterogeneity and Robustness
| Metric/Scenario | Threshold / Indicator | Interpretation |
|---|---|---|
| I² Statistic [34] | 0% to 40% | Might not be important. |
| 30% to 60% | May represent moderate heterogeneity. | |
| 50% to 90% | May represent substantial heterogeneity. | |
| 75% to 100% | Considerable heterogeneity. | |
| Sensitivity Analysis [32] | Results align with primary analysis | Findings are considered robust. |
| Results are grossly different | Primary results need to be interpreted with caution. |
Experimental Protocol: A Workflow for Robust Analysis
The following workflow outlines a systematic approach for integrating subgroup and sensitivity analyses into a meta-analysis to ensure reliable and credible results.
Workflow for Heterogeneity and Robustness Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Statistical and Methodological Tools
| Item / Tool | Function / Purpose | Application Example |
|---|---|---|
| Cochran's Q Statistic [33] | A statistical test to quantify the total heterogeneity across studies in a meta-analysis. | Used to calculate the I² statistic and to test the null hypothesis that all studies share a common effect size. |
| Random-Effects Model [34] | A statistical model that accounts for both within-study sampling error and between-study variation (heterogeneity). | The model of choice when heterogeneity is present, as it provides a more conservative confidence interval around the pooled estimate. |
| Inverse Variance Weighting [34] | A standard method for pooling studies in a meta-analysis, where studies are weighted by the inverse of their variance. | Ensures that more precise studies (with smaller variances) contribute more to the overall pooled effect estimate. |
| Risk of Bias Tool (e.g., Cochrane RoB 2) | A structured tool to assess the methodological quality and potential biases within individual studies. | Identifies studies with a high risk of bias, which can then be excluded in a sensitivity analysis to test the robustness of the results [32] [34]. |
| Reldesemtiv | Reldesemtiv|Fast Skeletal Troponin Activator|RUO | Reldesemtiv is a potent fast skeletal muscle troponin activator (FSTA) for research use only (RUO). Explore its mechanism in muscle function. |
Core Concepts: Why Baseline Risk Matters
What is baseline risk and why is it a critical factor in clinical trials?
Baseline risk refers to a patient's probability of experiencing a study outcome (e.g., mortality, disease progression) without the allocated intervention being tested [35]. In trial analysis, it is the control group event rate.
It is critical because the absolute treatment benefit a patient experiences is a function of both the relative treatment effect (often assumed constant) and their baseline risk [35]. A patient with a high baseline risk will derive a greater absolute benefit from a treatment that reduces relative risk than a patient with a low baseline risk. Accurately accounting for this variation is essential for translating average trial results to individual patient care and for designing properly powered trials [36].
How does baseline risk variation impact Network Meta-Analysis (NMA)?
Network Meta-Analysis compares multiple treatments simultaneously using both direct and indirect evidence [7] [15]. Transitivity is a key assumption of NMA, meaning that studies included in the network are sufficiently similar in their clinical and methodological characteristics to allow for valid indirect comparisons [15].
Significant variation in baseline risk across trials can violate the transitivity assumption if baseline risk is an effect modifier—a variable that influences the treatment effect size [35]. If patients in trials comparing Treatment A to B have systematically different risks than those in trials comparing A to C, the indirect estimate for B vs. C may be biased. This can lead to incoherence, where direct and indirect estimates for the same comparison disagree [15].
Troubleshooting Common Scenarios
The Power Problem: My trial risk was lower than expected
- Scenario: A trial fails to show a statistically significant benefit for an intervention. The investigators note that the baseline event rate in the control group was substantially lower than what was used for the initial sample size calculation.
- Underlying Issue: The Absolute Risk Reduction (ARR) is often not a fixed attribute of an intervention. For many acute conditions, the ARR decreases as the baseline risk of the control group decreases, even if the Relative Risk (RR) remains constant [36]. Your study was underpowered to detect a smaller-than-expected ARR.
- Solution:
- Pre-trial: During the design phase, use the best available data to estimate the control group risk. Consider increasing the sample size to account for the possibility of a lower-than-expected baseline risk [36].
- Post-trial: Report the findings transparently, highlighting the discrepancy in baseline risk. A pooled meta-analysis using relative measures (like Risk Ratios) may be more appropriate if control group risks vary widely across studies [36].
The NMA Incoherence Problem: Direct and indirect estimates disagree
- Scenario: In your NMA, the direct comparison of Treatments B and C shows a significant benefit for B, but the indirect comparison (via common comparator A) shows no significant difference. A statistical test confirms incoherence.
- Underlying Issue: Differences in effect modifiers—patient or study characteristics that influence treatment effect—between the direct and indirect evidence can cause incoherence [15]. Baseline risk is a common effect modifier.
- Solution:
- Investigate Transitivity: Check if the distribution of baseline risks or other prognostic factors differs between the studies providing direct evidence (B vs. C) and those providing indirect evidence (B vs. A and C vs. A).
- Use Multivariable Risk Models: Instead of one-at-a-time subgroup analyses, assess effect modification using a multivariable risk model. This involves developing or applying a prognostic model to estimate each patient's baseline risk and then testing for an interaction between this risk score and the treatment effect [35].
- Report by Risk Stratum: If effect modification is found, present relative treatment effects stratified by baseline risk quartiles or present absolute risk reductions for different baseline risk levels [35].
The Generalization Problem: How do I apply an average trial result to my unique patient?
- Scenario: A clinician wants to know if a drug with a reported 15% relative risk reduction in a large trial is appropriate for their specific patient, whose baseline risk appears different from the trial average.
- Underlying Issue: The average relative effect from a trial may not be applicable to all individuals within it, and certainly not to all patients in clinical practice [35].
- Solution:
- Estimate Individual Baseline Risk: Use a validated multivariable risk model to calculate the patient's specific baseline risk for the outcome.
- Calculate Individual Absolute Effect: Apply the relative risk reduction from the trial (or, if available, a risk-stratified estimate) to the patient's individual baseline risk to estimate their likely Absolute Risk Reduction.
- Weigh Benefit and Harm: Use this personalized absolute benefit estimate, along with the patient's specific risk for treatment-related harms, to support shared decision-making [35].
Methodological Guides & Protocols
Protocol: Assessing Treatment Effect Modification by Baseline Risk
This prespecified analysis protocol helps determine if a treatment's relative effect varies by a patient's underlying risk [35].
Step 1: Derive or Select a Risk Model
- Ideally, use a previously validated, multivariable prognostic model for the trial's primary outcome.
- If no suitable model exists, derive a new model within the trial's control arm using relevant patient characteristics.
Step 2: Calculate the Linear Predictor
- For each patient in the trial (both treatment and control groups), calculate the linear predictor from the risk model. This represents their individual baseline risk score.
Step 3: Test for Interaction
- Fit a Cox proportional hazards model (for time-to-event data) or a similar generalized linear model.
- The model should include the treatment allocation, the linear predictor (baseline risk score), and a term for their interaction.
- A statistically significant interaction term (e.g., P < 0.05) indicates that the relative treatment effect changes as the baseline risk changes [35].
Step 4: Present the Findings
- If a significant interaction is found, stratify the population into quartiles by baseline risk and present hazard ratios and absolute risk reductions for each quartile.
- This demonstrates the clinical relevance of the statistical finding.
Table 1: Impact of Lower-than-Expected Baseline Risk on Trial Power This table illustrates how a lower control group event rate drastically reduces statistical power, assuming a constant Relative Risk of 0.80 (20% reduction) [36].
| Planned Control Risk | Actual Control Risk | Sample Size Per Group (Planned) | Actual Power (%) |
|---|---|---|---|
| 40% | 40% | 564 | >80% |
| 40% | 32% | 564 | ~70% |
| 40% | 24% | 564 | ~50% |
| 40% | 16% | 564 | ~30% |
Table 2: Methods for Risk Rating Estimation in Analysis A comparison of approaches for grading risk in a healthcare setting, applicable to assessing risk of bias or prognostic factors in trial populations [37].
| Method | Description | Best Use Case |
|---|---|---|
| Quantitative | Uses numerical values for impact and probability. Results are objective and allow for cost-benefit analysis. | When robust historical frequency or statistical data are available. |
| Qualitative | Uses descriptive scales (e.g., High/Medium/Low). Fast, inexpensive, and good for initial prioritization. | When numerical data are inadequate, or for intangible consequences (e.g., reputational harm). |
| Semi-Quantitative | Ranks risks using a predefined scoring system. Balances speed and quantitative structure. | Common in healthcare organizations; useful when some data exists but is not fully comprehensive. |
Workflow Visualization
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Baseline Risk Analysis
| Tool / Solution | Function in Analysis |
|---|---|
| Multivariable Prognostic Model | A statistical model that combines multiple patient characteristics (e.g., age, disease severity, comorbidities) to estimate an individual's baseline risk of an outcome. Serves as the foundation for risk assessment [35]. |
| Cox Proportional Hazards Model | A regression model used for time-to-event data. It is the standard method for testing the interaction between treatment allocation and a continuous baseline risk score [35]. |
| Network Meta-Analysis Framework | A statistical methodology that synthesizes both direct and indirect evidence to compare multiple treatments simultaneously. Its validity depends on satisfying the transitivity assumption [7] [15]. |
| Risk Matrix | A qualitative or semi-quantitative tool (often a grid) used to rank risks based on their probability and impact. Useful for prioritizing which sources of heterogeneity or bias to address first in an analysis [37]. |
| GRADE for NMA | A systematic framework (Grading of Recommendations, Assessment, Development, and Evaluations) for rating the certainty of evidence in NMAs. It incorporates assessments of incoherence and intransitivity [15]. |
Solving Heterogeneity Challenges: Inconsistency Detection and Model Selection Strategies
Detecting and Resolving Inconsistency Between Direct and Indirect Evidence
Frequently Asked Questions (FAQs)
Q1: What is the difference between "inconsistency" and "heterogeneity" in a Network Meta-Analysis? Inconsistency (sometimes called incoherence) occurs when different sources of evidence for the same intervention comparison disagree, specifically when direct evidence (from head-to-head trials) disagrees with indirect evidence. Heterogeneity, in contrast, refers to variability in treatment effects between studies that make the same direct comparison. Inconsistency is a violation of the statistical assumption of coherence, while heterogeneity concerns variability within a single comparison [8].
Q2: Under what conditions is testing for inconsistency not possible? Testing for inconsistency is not feasible in a "star-shaped" network, where all trials compare various interventions against a single common comparator (e.g., placebo) but never against each other. In such a network, all evidence is direct, and there are no alternative pathways to provide conflicting indirect estimates [8].
Q3: What is the fundamental assumption required for a valid indirect comparison? The validity of an indirect comparison rests on the assumption of transitivity. This means that the different sets of randomized trials included in the analysis must be similar, on average, in all important factors that could modify the treatment effect (effect modifiers), such as patient population characteristics, trial design, or outcome definitions [8].
Q4: Can I perform a NMA if some trials have a mix of two-drug and three-drug interventions? Yes, but it requires careful "node-making"—the process of defining what constitutes a distinct intervention node in your network. For complex interventions, you must decide whether to "lump" similar interventions into a single node or "split" them into separate nodes based on their components. This decision should be guided by the clinical question and the plausibility of the transitivity assumption [38].
Q5: My NMA shows significant inconsistency. What are my options? When significant inconsistency is detected, you should:
- Re-check your network: Verify that the transitivity assumption holds.
- Investigate the source: Use methods like the Separating Indirect from Direct Evidence (SIDE) or node-splitting to locate the problematic comparison.
- Use advanced models: Employ models that account for inconsistency, such as an inconsistency-by-treatment-interaction model.
- Report transparently: Clearly state the findings, including the presence and location of inconsistency, and interpret results with caution [8].
Troubleshooting Guides
Issue 1: Unexplained Inconsistency in a Specific Loop of the Network
Problem: A statistical test indicates significant inconsistency in one of the closed loops of your network, but you cannot identify an obvious clinical or methodological reason.
Resolution Protocol:
Statistical Investigation:
- Employ a local approach to inconsistency, such as a node-splitting analysis. This method separates the direct evidence for a specific comparison from the indirect evidence and assesses whether they disagree significantly [8].
- Use the Loop-specific approach to calculate an inconsistency factor (IF) with its confidence interval for the problematic loop. An IF that differs from zero indicates inconsistency.
Methodological and Clinical Interrogation:
- Re-examine Effect Modifiers: Systematically check for differences in the distribution of potential effect modifiers (e.g., baseline risk, disease severity, prior treatments) between the trials contributing to the direct and indirect evidence. Create a table to compare these characteristics across studies.
- Assess Risk of Bias: Evaluate if studies in one direct comparison have a systematically higher risk of bias than studies in the other, which could be driving the discrepancy.
Reporting and Interpretation:
- If the source of inconsistency remains unexplained, present both the direct and indirect estimates separately in your report.
- Clearly state that the results for the affected comparisons are uncertain due to unexplained inconsistency and that the NMA estimates should be interpreted with great caution.
- Do not ignore the inconsistency; it invalidates the assumption that direct and indirect evidence can be combined without bias.
Issue 2: The Entire Network Appears Structurally Incoherent
Problem: Global tests for inconsistency indicate a problem across the entire network, not just in a single loop.
Resolution Protocol:
Global Assessment:
- Use a design-by-treatment interaction model. This is a comprehensive global test that evaluates inconsistency from all possible sources in the network, including loop inconsistency and the effect of multi-arm trials [8].
Strategic Re-evaluation:
- Reconsider Transitivity: Perform a thorough clinical review of all trials in the network. The transitivity assumption is likely violated. Are there fundamental differences between the trials comparing, for example, Drug A vs. Drug B and the trials comparing Drug A vs. Drug C?
- Revisit Node Definitions: Critically assess whether your intervention nodes are defined appropriately. For complex interventions used in public health, the "node-making" process is crucial. Aggregating dissimilar interventions into a single node is a common cause of global inconsistency [38].
- Evaluate Meta-Regression: If an effect modifier can be measured at the study level (e.g., year of publication, average patient age), consider using network meta-regression to adjust for it and see if the inconsistency is reduced [39].
Fallback Option:
- If inconsistency cannot be resolved, it may not be valid to present a single, unified NMA result. Consider presenting the evidence as a systematic review with multiple pairwise meta-analyses and a narrative discussion of the potential reasons for the observed inconsistencies.
Issue 3: Inconsistent Findings Between Updated and Previous NMA
Problem: After updating your NMA with new trial data, the relative ranking of treatments or the estimates for key comparisons have changed dramatically, leading to conclusions that are inconsistent with previous NMAs on the same topic.
Resolution Protocol:
Comparative Analysis:
- Compare the list of included studies and the network structure between the old and new NMA. Identify the newly added trials and their position in the network.
- Check if the new trials introduce a new direct comparison that was previously only estimated indirectly, as this can resolve or create inconsistency.
Investigate New Evidence:
- Critically appraise the new trials. Do they have unique characteristics (e.g., a different patient subgroup, a new standard of care as background therapy) that might act as an effect modifier?
- Perform sensitivity analyses by running the NMA both with and without the new trials to quantify their impact on the results.
Contextualize the Findings:
- As seen in the field of obesity pharmacotherapy, new, highly effective drugs like tirzepatide and semaglutide can shift the landscape. Earlier NMAs may not have included these agents, and their introduction can change the interpretation of older drugs' efficacy [40] [41].
- Report that the evidence is evolving and that the updated analysis reflects the most current picture, which may supersede previous understandings.
Essential Methodologies & Protocols
Protocol 1: Node-Splitting Analysis for Localizing Inconsistency
Purpose: To isolate and test for a disagreement between direct and indirect evidence for a specific treatment comparison.
Procedure:
- Identify Comparisons: List all treatment comparisons in your network that are informed by both direct evidence (from studies that make the head-to-head comparison) and at least one independent indirect evidence pathway.
- Split the Node: For each of these comparisons, the analysis is performed twice:
- Direct Estimate: Calculated using only the studies that directly compare the two treatments.
- Indirect Estimate: Calculated using all other evidence in the network except the direct studies.
- Statistical Test: Compare the direct and indirect estimates. A significant p-value (e.g., < 0.05) indicates inconsistency for that particular comparison.
- Interpretation: The analysis produces a summary of which specific comparisons in the network are inconsistent.
Protocol 2: Assessing the Transitivity Assumption
Purpose: To evaluate the clinical and methodological similarity of studies across different direct comparisons before pooling them in an NMA.
Procedure:
- Identify Potential Effect Modifiers: Before analysis, use clinical and subject-area knowledge to list variables that could influence the treatment effect (e.g., baseline severity, disease duration, prior lines of therapy, trial design, year of publication).
Create Comparison Tables: For each direct comparison in the network (e.g., A vs. B, A vs. C, B vs. C), create a table summarizing the distribution of the identified effect modifiers across the studies that contribute to that comparison.
Example Table for Comparison A vs. B:
Study ID Mean Baseline Severity Disease Duration (Years) Proportion of Patients with Comorbidity X Risk of Bias Study 1 High 5.2 45% Low Study 2 Medium 4.8 50% Some concerns
Compare the Tables: Assess whether the distributions of these effect modifiers are similar across the different direct comparisons. For instance, check if the patients in trials of A vs. B are systematically different from those in trials of A vs. C.
- Judgment: If important effect modifiers are unbalanced across comparisons, the transitivity assumption is likely violated, and the NMA may be invalid.
The Scientist's Toolkit: Research Reagent Solutions
Table: Key Methodological Tools for Inconsistency Analysis
| Tool Name | Function/Brief Explanation | Example Use Case |
|---|---|---|
| Node-Splitting Model | A statistical model that separates direct and indirect evidence for a specific comparison to test if they disagree. | To determine if the direct comparison of Drug B vs. Drug C is inconsistent with the indirect estimate derived via Drug A. |
| Design-by-Treatment Interaction Model | A global model that tests for inconsistency from all possible sources in a network of interventions. | To check if the entire network is statistically coherent before proceeding to interpret the pooled results. |
| Loop-Specific Inconsistency Approach | Calculates an inconsistency factor (IF) for each closed loop in the network diagram. | To identify which particular triangular or quadratic loop in a complex network is contributing most to overall inconsistency. |
| Network Meta-Regression | Extends NMA to adjust for study-level covariates (potential effect modifiers). | To test if the observed inconsistency can be explained by a covariate like trial duration or baseline risk. |
| PRISMA-NMA Checklist | A reporting guideline that ensures transparent and complete reporting of NMA methods and findings, including inconsistency assessments. | To ensure all necessary steps for assessing and discussing inconsistency are documented in the final manuscript [42]. |
Diagnostic & Analytical Workflows
Diagram: Workflow for Investigating Inconsistency in NMA
## Frequently Asked Questions (FAQs)
1. What is the core difference between fixed-effect and random-effects models in network meta-analysis?
The core difference lies in their underlying assumptions about the true treatment effects across studies. The fixed-effect model (also called common-effect model) assumes that all studies are estimating one single, true treatment effect. It presumes that observed differences in results are due solely to chance (within-study sampling error). In contrast, the random-effects model acknowledges that studies may have differing true effects and assumes these effects follow a normal distribution. It explicitly accounts for between-study heterogeneity, treating it as another source of variation beyond sampling error [43] [44].
Table: Comparison of Fixed-Effect and Random-Effects Models
| Feature | Fixed-Effect Model | Random-Effects Model |
|---|---|---|
| Assumption | All studies share a single common effect | True effects vary across studies, following a distribution |
| Handling Heterogeneity | Does not model between-study heterogeneity | Explicitly estimates and incorporates between-study variance (τ²) |
| Weights Assigned to Studies | More balanced weights; larger studies have proportionally greater influence | More balanced weights; larger studies have less relative influence compared to fixed-effect |
| Interpretation | Inferences are conditional on the included studies | Inferences can be generalized to a population of studies |
| When to Use | When heterogeneity is negligible or absent | When clinical/methodological diversity is present and heterogeneity is expected |
2. When should I consider using a class-effects model?
You should consider a class-effects model when the interventions in your network can be logically grouped into classes (e.g., different drugs from the same pharmacological class). This approach is particularly valuable for:
- Informing recommendations at the class level rather than for individual treatments.
- Addressing sparse data for individual treatments by borrowing strength from other treatments within the same class.
- Handling disconnected networks by connecting them through class-level effects [27] [45]. These models introduce an additional hierarchical layer, assuming that treatment effects within a class are either exchangeable (random class effects) or identical (common class effects).
3. What is the transitivity assumption and why is it critical for model selection?
Transitivity is the core clinical and methodological assumption that underpins the validity of indirect comparisons and network meta-analysis. It posits that the different sets of studies making different direct comparisons (e.g., A vs. B and B vs. C) are sufficiently similar, on average, in all important factors that could influence the relative treatment effects (such as patient characteristics, trial design, or outcome definitions) [8]. Its statistical counterpart is known as consistency [46]. It is critical for model selection because if the transitivity assumption is violated, the entire network of evidence is flawed, and any model—fixed, random, or class-effects—will produce biased results. Therefore, assessing the plausibility of transitivity is a prerequisite before selecting a specific statistical model [8] [47].
4. How can I assess inconsistency in my network meta-analysis?
Inconsistency arises when direct and indirect evidence for a specific treatment comparison disagree. Assessment methods include:
- Local Approaches: For a specific comparison, you can use the node-splitting method, which separates direct and indirect evidence and checks for disagreement.
- Global Approaches: Models like design-by-treatment interaction or models with random inconsistency effects can assess inconsistency across the entire network. These models add an extra variance component (inconsistency variance) to account for disagreement between different sources of evidence [43] [31]. The presence of significant inconsistency indicates a violation of the transitivity assumption and requires investigation into its potential causes.
## Troubleshooting Guides
Problem: High heterogeneity in the network. Solution:
- Confirm with Statistics: Check the estimated between-study variance (τ²) or I² statistic from your random-effects model.
- Investigate Sources: Perform subgroup analysis or meta-regression to explore whether specific study-level covariates (e.g., baseline risk, year of publication, dose) explain the heterogeneity.
- Model Selection: A random-effects model is typically more appropriate than a fixed-effect model in the presence of non-negligible heterogeneity. If heterogeneity remains high and unexplained, clearly report it and interpret results with caution, considering the use of prediction intervals [43] [48].
Problem: The network is disconnected, preventing some comparisons. Solution:
- Check Network Geometry: Visualize your network diagram to identify which treatments or groups of treatments are not connected to the main network.
- Consider Class-Effects Models: This is a primary application for class-effects models. By grouping individual treatments into classes, you can connect disconnected parts of the network at the class level, allowing for indirect comparisons [27] [45].
- Alternative: If class-effects are not justifiable, you cannot compare disconnected components via NMA and must report their results separately.
Problem: Model fitting is unstable or fails to converge. Solution:
- Check for Sparse Data: Networks with many treatments but few studies per comparison can lead to estimation problems.
- Simplify the Model: Consider using fixed-effect models at the treatment level if heterogeneity is low, or use class-effects models to reduce the number of parameters that need to be estimated [27] [45].
- Prior Distributions (Bayesian): In a Bayesian framework, use appropriately informative prior distributions for variance components (heterogeneity, inconsistency), as truly vague priors can make these parameters difficult to estimate [43].
## The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Components for Network Meta-Analysis
| Tool / Resource | Function | Implementation Example |
|---|---|---|
multinma R package |
Implements a range of NMA models, including hierarchical models with class effects, and provides a model selection strategy. | Used to fit fixed, random, and class-effects models and test assumptions of heterogeneity, consistency, and class effects [27]. |
metafor R package |
A comprehensive package for meta-analysis that can also be used to fit some network meta-analysis models using likelihood-based approaches. | Can be used to obtain (restricted) maximum-likelihood estimates for random-effects models [43]. |
| WinBUGS / OpenBUGS | Bayesian statistical software using Markov Chain Monte Carlo (MCMC) methods. A traditional tool for fitting complex NMA models. | Used for Bayesian NMA models, including models with random inconsistency effects [43]. |
| Importance Sampling Algorithm | An alternative to MCMC for Bayesian inference; can avoid difficulties with "burning-in" chains and autocorrelation. | Provides a method for fitting models with random inconsistency effects using empirically-based priors [43]. |
| Network Diagram | A graphical depiction of the evidence structure, showing interventions (nodes) and available direct comparisons (edges). | Critical for visualizing network connectivity, identifying potential comparators, and assessing transitivity assumptions. Often created with R packages like igraph or netmeta [8] [31]. |
## Experimental Protocols & Workflows
Protocol 1: A Structured Model Selection Algorithm
A proposed strategy for model selection involves the following steps [27] [45]:
- Fit a Standard Random-Effects NMA Model: Start with a model that allows for between-study heterogeneity.
- Test for Heterogeneity: Assess the magnitude and impact of between-study variation. If heterogeneity is negligible, a fixed-effect model may be sufficient.
- Test for Inconsistency: Use global or local methods to check for disagreement between direct and indirect evidence.
- Fit Class-Effects Models: If treatments can be grouped, fit hierarchical models with exchangeable or common class effects.
- Compare Model Fit: Use statistical criteria like Deviance Information Criterion (DIC) in Bayesian analysis or Akaike Information Criterion (AIC) in frequentist analysis to compare the relative fit and parsimony of the different models.
- Assume and Check: The final model should be the one that best balances statistical fit, parsimony, and biological plausibility, while its underlying assumptions have been thoroughly checked.
Model Selection Workflow: A stepwise algorithm for selecting between NMA models, emphasizing assumption checks.
Protocol 2: Implementing a Class-Effects NMA
The following methodology outlines the process for implementing a class-effects model [27] [45]:
- Define Classes: Based on pharmacological properties or mechanism of action, group individual treatments into predefined classes (e.g., SSRIs, TCAs).
- Specify the Model: Choose between:
- Common Class Effects: Assumes all treatments within a class have identical effects.
- Exchangeable (Random) Class Effects: Assumes treatment effects within a class are similar but not identical, and are exchangeable, following a normal distribution.
- Model Estimation: Use Bayesian hierarchical modeling (e.g., in
multinmaor BUGS) to estimate both the class-level effects and the individual treatment effects within each class. - Check Class Effect Assumption: Evaluate if the data support the grouping by comparing the class model to a model with independent treatment effects and by examining the estimated between-class and within-class variance.
Hierarchical Structure of a Class-Effects Model: Illustrates how individual treatments (e.g., drugs) nest within broader classes, and how the class-level effect influences the estimation of individual treatment effects.
Addressing Sparse Networks and Evidence Gaps with Hierarchical Bayesian Approaches
Frequently Asked Questions (FAQs): Core Concepts
Q1: What is a Hierarchical Bayesian Model (HBM) in the context of Network Meta-Analysis? A Hierarchical Bayesian Model (HBM) for NMA is a sophisticated statistical framework that allows for the simultaneous synthesis of evidence from multiple studies comparing three or more treatments. It uses a Bayesian approach, which means it combines prior knowledge or beliefs (expressed as prior probability distributions) with the data from included studies (the likelihood) to produce updated posterior probability distributions for the treatment effects [30]. The "hierarchical" component refers to its structure, which naturally models the different levels of data—for example, modeling variation both within studies and between studies. This is particularly useful for modeling complex data structures, such as treatments belonging to common classes or studies of different designs (e.g., randomized and non-randomized) [30].
Q2: Why are HBMs particularly useful for sparse networks or evidence gaps? HBMs are powerful in sparse network scenarios due to a concept called "borrowing of strength." In a connected network, the information about any single treatment comparison is not only derived from its direct head-to-head studies but is also informed by indirect evidence from the entire network [8]. In a sparse network where direct evidence is absent or limited, the HBM can leverage this indirect evidence through the common comparators, providing more robust effect estimates than would be possible by looking at direct evidence alone [49] [30]. Furthermore, HBMs can intelligently share information across the hierarchy; for instance, when data for a specific treatment is sparse, the model can partially "borrow" information from other treatments in the same class to produce a more stable estimate [50] [30].
Q3: What are the key assumptions that must be met for a valid HBM-NMA? The validity of an NMA, including one using an HBM, rests on several key assumptions [7]:
- Transitivity: This is the core assumption that the studies forming the different direct comparisons in the network are sufficiently similar in all important factors that could modify the treatment effect (e.g., patient population, study design, outcome definitions). In a network comparing A-B, A-C, and B-C, the distribution of effect modifiers should be similar across the A-B and A-C studies.
- Consistency: This is the statistical manifestation of transitivity. It means that the direct evidence (e.g., from studies directly comparing B and C) and the indirect evidence (e.g., comparing B and C via the common comparator A) are in agreement for all comparisons within the network.
- Homogeneity: This refers to the similarity of treatment effects across studies within the same direct comparison.
Troubleshooting Guides: Common Experimental Issues
Problem 1: Model Fails to Converge or Has Poor Mixing
Symptoms:
- Trace plots of Markov Chain Monte Carlo (MCMC) samples show chains that are not stationary or are not mixing well (failing to explore the full posterior distribution).
- High Gelman-Rubin diagnostic values (typically >1.05) indicate a lack of convergence.
Solutions:
- Adjust MCMC Parameters: Increase the number of iterations and tuning samples. Consider using multiple chains with different initial values to ensure they all converge to the same distribution [51].
- Reparameterize the Model: Sometimes, changing the model's mathematical formulation can improve sampling efficiency. For instance, using centering or non-centered parameterizations for hierarchical models can help.
- Check for Highly Correlated Parameters: Use correlation matrices to identify parameters that are highly correlated and consider alternative model structures.
- Review Prior Distributions: Overly vague or inappropriate priors can sometimes lead to convergence issues. Consider using more informative priors based on external evidence or pilot studies [30].
Problem 2: Handling High Heterogeneity or Inconsistency in the Network
Symptoms:
- High estimates of between-study heterogeneity (τ²).
- Statistical tests or plots (e.g., node-splitting) indicate significant disagreement between direct and indirect evidence for one or more comparisons [7].
Solutions:
- Account for Study Design: Use a hierarchical model that differentiates between study types (e.g., RCTs vs. non-randomized studies). This allows the model to handle the different levels of bias and variability inherent in different designs [30].
- Incorporate Bias Adjustment: Extend the HBM to include random bias terms for non-randomized studies, acknowledging that these studies may systematically over- or underestimate the true treatment effect [30].
- Explore Covariates with Meta-Regression: If transitivity is suspected to be violated, use meta-regression to adjust for known effect modifiers (e.g., baseline risk, patient age). This can help explain the source of heterogeneity or inconsistency [8].
- Use Predictive Checks: Perform posterior predictive checks to assess the model's goodness-of-fit by comparing replicated data generated from the model to the observed data [49].
Problem 3: Incorporating Data from Non-Randomized Studies
Symptoms:
- The network of RCTs is disconnected or too sparse to yield precise estimates.
- A need to generalize findings to broader populations typically excluded from RCTs.
Solutions:
- Do Not Naïvely Pool: Simply combining RCT and non-randomized data in a standard meta-analysis is not recommended, as it ignores design-specific biases [30].
- Apply a Hierarchical Model by Design: Implement a model that treats the study design (RCT vs. non-randomized) as a separate layer in the hierarchy. This allows the model to estimate different levels of variability for each design type [30].
- Consider a Bias-Adjusted Hierarchical Model: Introduce an additional parameter to the hierarchical model to adjust for the average bias in non-randomized studies. This bias term can also be allowed to vary by treatment class for greater flexibility [30].
Experimental Protocols & Methodologies
Protocol 1: Standard HBM-NMA for Sparse RCT Networks
Objective: To synthesize direct and indirect evidence from a network of RCTs to compare multiple interventions when direct evidence is sparse.
Methodology:
- Model Definition: A Bayesian random-effects NMA model is fitted. The model for a continuous outcome in trial (i) and arm (k) is typically specified as:
- ({y}{ik} \sim N({\theta}{ik}, {se}{ik}^{2})) (Likelihood)
- ({\theta}{ik} = {\mu}{i} + {\delta}{i, bk} \cdot I(k \ne b)) (Linear predictor)
- ({\delta}{i, bk} \sim N({d}{bk}, {\sigma}^{2})) (Random effects) where ({y}{ik}) is the observed effect, ({\theta}{ik}) is the true effect, ({\mu}{i}) is the baseline effect in trial (i) (with a reference treatment (b)), and ({\delta}{i, bk}) is the trial-specific effect of treatment (k) compared to (b). The ({d}_{bk}) are the parameters of interest—the pooled relative treatment effects [30].
- Prior Specification:
- Vague priors are often used for basic parameters, e.g., ({d}_{1k} \sim N(0, 1000)).
- A weakly informative prior is used for the heterogeneity parameter, e.g., (\sigma \sim Uniform(0, 5)) [30].
- Implementation: The model is implemented using Markov Chain Monte Carlo (MCMC) sampling in software like WinBUGS/OpenBUGS, JAGS, or Stan (via R or Python interfaces) [7] [30].
- Inference: Results are based on the posterior distributions of the ({d}_{bk}), from which all pairwise comparisons, rankings, and probabilities of being the best treatment can be derived.
Protocol 2: Three-Level HBM for Treatment Classes and Study Designs
Objective: To perform an NMA that accounts for both the grouping of treatments into classes and the inclusion of different study designs (RCTs and non-randomized studies).
Methodology:
- Model Structure: This model extends the standard HBM by adding hierarchical layers.
- Level 1 (Within-study model): ({y}{ik} \sim N({\theta}{ik}, {se}{ik}^{2}))
- Level 2 (Between-study model): The relative effects ({\delta}{i, bk}) can be modeled to depend on the study design (s[i]): ({\delta}{i, bk} \sim N({d}{bk,s[i]}, {\sigma}^{2})).
- Level 3 (Treatment class model): The effects of individual treatments ({d}{bk}) can be modeled as coming from a distribution of effects for their class (c[k]): ({d}{bk} \sim N({D}{c[k]}, {\psi}^{2})), where ({D}{c[k]}) is the class-level effect and ({\psi}^{2}) is the within-class variance [50] [30].
- Bias Adjustment (Extension): For non-randomized studies, a bias term ({\beta}{s[i]}) can be added: ({\delta}{i, bk} \sim N({d}{bk} + {\beta}{s[i]}, {\sigma}^{2})) [30].
- Implementation & Interpretation: This complex model requires careful specification of priors and assessment of convergence. The output provides class-level effects, individual treatment effects "shrunken" towards their class mean, and estimates that account for design-related bias.
Key Research Reagents & Computational Tools
Table 1: Essential Software and Packages for HBM-NMA
| Tool/Package Name | Primary Function | Key Features |
|---|---|---|
| WinBUGS/OpenBUGS [7] [30] | Bayesian inference using MCMC | Specialized language for complex Bayesian models; historically a standard for NMA. |
| JAGS | Bayesian inference using MCMC | Similar functionality to BUGS, with a different engine. |
| Stan | Bayesian inference | Uses Hamiltonian Monte Carlo, often more efficient for complex models. |
| R (with packages) [7] [51] | Statistical programming environment | Core platform for analysis. Key packages include: |
  ∙ gemtc [7] |
NMA interface | Provides an interface to WinBUGS/OpenBUGS/JAGS for NMA. |
  ∙ bnlearn [51] |
Bayesian network learning | For structure learning and parameter training of Bayesian networks. |
  ∙ gRain [51] |
Graphical independence networks | For probabilistic inference in Bayesian networks. |
  ∙ pcnemeta, BUGSnet [7] |
NMA-specific functions | Provide specialized functions for conducting and reporting NMA. |
| Stata [7] | Statistical software | Has modules for frequentist approaches to NMA. |
| shinyBN [51] | Web-based GUI | An R/Shiny application for interactive Bayesian network inference and visualization, useful for non-programmers. |
Visual Workflows and Logical Diagrams
Diagram 1: High-Level Workflow for Conducting an HBM-NMA
Diagram 2: Hierarchical Structure for a Class-Based HBM
Troubleshooting Guides
How do I resolve conflicting heterogeneity estimates between different estimation methods?
Problem: You obtain different estimates for between-study variance (τ²) when using DerSimonian-Laird (DL), Restricted Maximum Likelihood (REML), and Bayesian methods, creating uncertainty about which result to report.
Solution: Understand that these differences are expected, particularly in datasets with high heterogeneity or small study sizes.
- Interpretation: While all three methods typically yield similar estimates for the overall effect size, they often produce different estimates for between-study variability [52].
- Action Plan:
- Report multiple estimates if differences are substantial, with a justification for your primary choice.
- Prefer REML or Bayesian methods over DL when high heterogeneity is present. Research shows no practical difference between REML and Bayesian methods, but both are recommended over DL, especially when heterogeneity is high [52].
- Investigate the impact of the different τ² estimates on the final pooled estimate and confidence intervals through sensitivity analysis.
Prevention: Decide on your primary estimation method during your analysis plan development, based on your data characteristics. REML is often a good default choice for frequentist analyses.
How should I handle a network meta-analysis when inconsistency is detected?
Problem: Global or local inconsistency tests indicate disagreement between direct and indirect evidence in your network, threatening the validity of your effect estimates.
Solution: Systematically assess, locate, and address the inconsistency.
- Diagnostic Steps:
- Use the net heat plot to render transparent which direct comparisons drive each network estimate and display hot spots of inconsistency [53].
- Apply node-splitting to separate evidence for particular treatment comparisons into direct and indirect components and assess discrepancies [33].
- Check for transitivity violations - ensure studies are sufficiently similar in their clinical and methodological characteristics [54].
Resolution Approaches:
- If inconsistency is minor: Present both consistent and inconsistent models and note the limited impact.
- If inconsistency is substantial:
- Report the inconsistent model results with appropriate caveats.
- Use multivariable meta-regression to explain heterogeneity by more than one variable, which reduces more variability than any univariate models [52].
- Consider excluding outlying studies if justified by clinical rationale.
Prevention: Carefully plan your network geometry at the protocol stage and assess potential effect modifiers across treatment comparisons.
Frequently Asked Questions (FAQs)
When should I choose REML over DerSimonian-Laird for my meta-analysis?
Answer: Choose REML over DL when:
- You have high heterogeneity in observed treatment effects across studies [52]
- Your analysis includes preclinical data with many small studies [52]
- You need to explain heterogeneity through covariates in meta-regression (REML provides more accurate estimates of the proportion of heterogeneity explained by covariates) [52]
- You are conducting network meta-analysis with complex evidence structures [53]
Exception: DL may be sufficient for simple pairwise meta-analyses with limited heterogeneity and when computational simplicity is prioritized.
What are the practical advantages of Bayesian methods for heterogeneity estimation?
Answer: Bayesian methods provide:
- Natural uncertainty quantification for τ² through posterior distributions
- Flexibility to incorporate prior information about heterogeneity
- Direct probability statements about heterogeneity parameters
- Enhanced output options including ranking plots and treatment risk posterior distribution plots [54]
- Handling of complex models particularly valuable in network meta-analysis [54]
Implementation Tip: Use R packages like gemtc or BUGSnet for Bayesian network meta-analysis [54].
How can I visually assess and communicate heterogeneity and inconsistency in my network?
Answer: Several graphical tools are available:
- Net heat plot: Highlights hot spots of inconsistency and shows which direct comparisons drive network estimates [53]
- Vitruvian plot: Facilitates communication of multiple outcomes from NMAs to patients and clinicians using radial bar plots [55]
- Forest plots: Display effect estimates and confidence intervals for individual studies and meta-analyses [48]
Accessibility Note: Ensure sufficient color contrast (at least 4.5:1 for normal text) in all visualizations [56].
Experimental Protocols & Methodologies
Protocol for Implementing REML Heterogeneity Estimation
Purpose: To implement REML estimation for random-effects meta-analysis, providing improved heterogeneity estimates compared to DL method.
Materials:
- Dataset of effect sizes and their variances from included studies
- Statistical software with REML capability (R, Stata, SAS)
Procedure:
- Data Preparation: Calculate effect sizes (e.g., log odds ratios, mean differences) and their sampling variances for each study.
- Model Specification: Implement the random-effects model:
Y_i = θ + u_i + ε_iwhereu_i ~ N(0, τ²)andε_i ~ N(0, v_i)- where Yi is the observed effect in study i, θ is the overall effect, ui is the study-specific deviation, and ε_i is the sampling error
- REML Estimation: Maximize the restricted log-likelihood function to estimate τ²:
- The REML estimator accounts for degrees of freedom lost in estimating fixed effects
- Effect Estimation: Calculate the overall effect size using inverse-variance weights:
w_i = 1/(v_i + τ²)
Troubleshooting Notes:
- REML may have convergence issues with very small numbers of studies
- With few studies (<10), consider Bayesian methods with informative priors
Protocol for Bayesian Heterogeneity Estimation using R and JAGS
Purpose: To implement Bayesian random-effects meta-analysis for estimating between-study heterogeneity.
Materials:
- Dataset of effect sizes and their variances
- R statistical environment with
rjagsorR2jagspackage - JAGS (Just Another Gibbs Sampler) software
Procedure:
- Data Preparation: Organize data into list format containing:
- y: effect sizes for each study
- sigma: standard errors for each study
- N: total number of studies
- Model Specification in JAGS:
Model Fitting:
- Run 3 chains with overdispersed initial values
- Use adaptive phase of 10,000 iterations
- Sample 50,000 iterations after burn-in of 20,000
- Assess convergence with Gelman-Rubin statistic (R-hat < 1.1)
Output Interpretation:
- Report posterior median and 95% credible interval for τ²
- Examine posterior distribution shape for τ²
- Calculate probability that τ² exceeds clinically important thresholds
Validation: Compare results with REML estimates as sensitivity analysis.
Quantitative Data Comparison
Performance Comparison of Heterogeneity Estimation Methods
Table 1: Comparison of heterogeneity estimation methods based on empirical evaluation
| Method | Between-Study Variance Estimation | Overall Effect Estimation | Handling High Heterogeneity | Covariate Explanation | Implementation Complexity |
|---|---|---|---|---|---|
| DerSimonian-Laird (DL) | Less accurate with high heterogeneity | Similar to other methods | Poor performance | Underestimates proportion explained | Low |
| Restricted Maximum Likelihood (REML) | More accurate than DL | Similar to other methods | Good performance | Better estimation of explained heterogeneity | Medium |
| Bayesian Methods | Similar to REML | Similar to other methods | Good performance | Similar to REML | High |
Source: Adapted from PMC8647574 [52]
Inconsistency Detection Methods in Network Meta-Analysis
Table 2: Methods for detecting inconsistency in network meta-analysis
| Method | Type of Assessment | Key Statistic | Strengths | Limitations |
|---|---|---|---|---|
| Cochran's Q | Global | Q statistic | Simple calculation | Low power with few studies |
| Loop Inconsistency Approach | Local (per loop) | Z-test for direct vs. indirect | Intuitive for simple loops | Cumbersome in large networks |
| Node-Splitting | Local (per comparison) | Difference between direct and indirect | Pinpoints specific inconsistent comparisons | Depends on reference treatment in multi-arm studies |
| Inconsistency Parameter Approach | Global/local | Inconsistency factors | Comprehensive modeling | Model selection arbitrary |
| Net Heat Plot | Graphical | Q-diff statistic | Visual identification of inconsistency hotspots | No formal statistical test |
Source: Adapted from PMC6899484 [33] and BMC Medical Research Methodology [53]
Visualization of Method Selection and Workflow
Heterogeneity Estimator Selection Guide
Network Meta-Analysis Inconsistency Assessment Workflow
Research Reagent Solutions
Statistical Software and Packages for Advanced Meta-Analysis
Table 3: Essential software tools for implementing advanced heterogeneity estimators
| Tool Name | Type | Key Functions | Implementation | Use Case |
|---|---|---|---|---|
R metafor package |
Statistical package | REML estimation, meta-regression, forest plots | Frequentist | Standard pairwise and network meta-analysis |
R gemtc package |
Bayesian NMA package | Bayesian NMA, ranking plots, inconsistency assessment | Bayesian | Network meta-analysis with mixed treatment comparisons |
R BUGSnet package |
Bayesian NMA package | Comprehensive NMA, data visualization, league tables | Bayesian | Arm-level network meta-analysis |
| JAGS/OpenBUGS | Gibbs sampler | Bayesian modeling, custom prior specification | Bayesian | Complex Bayesian models not available in packages |
Stata metan suite |
Statistical commands | Various estimation methods, network meta-analysis | Frequentist/Bayesian | Integrated data management and analysis |
| CINeMA | Web application | Confidence in NMA results, evidence grading | Multiple | Quality assessment and confidence rating |
Source: Adapted from PMC8647574 [52], PMC6899484 [33], and Frontiers in Veterinary Science [54]
Frequently Asked Questions
1. What are diagnostic plots and why are they important in Network Meta-Analysis? Diagnostic plots are visual tools designed to evaluate the validity of statistical assumptions made by a model, including linearity, normality of residuals, homoscedasticity (constant variance), and the absence of overly influential points [57]. In the context of Network Meta-Analysis (NMA) and component NMA (CNMA), they are crucial for assessing model fit and identifying heterogeneity, which can arise from complex, multi-component interventions [14]. They help researchers identify potential problems with the model, guiding informed decisions about model improvement or transformation to ensure robust and reliable results [57].
2. I've fitted a model. Which is the most important diagnostic plot to check for heterogeneity? The Scale-Location Plot (also called the Spread-Location plot) is the primary diagnostic tool for identifying patterns of heteroscedasticity, which is a form of heterogeneity where the variance of residuals is not constant [58] [57]. It directly assesses the assumption of equal variance across all levels of the predicted outcome.
3. What does a "good" vs. "bad" Scale-Location plot look like? In a well-behaved model, you should see a horizontal line with points randomly spread across the range of fitted values [58]. This suggests homoscedasticity. A "bad" plot will show a systematic pattern, typically where the spread of residuals increases or decreases with the fitted values. The red smoothing line on the plot will not be horizontal and may show a steep angle, clearly indicating heteroscedasticity [58] [57].
4. A case in my data is flagged as influential. What should I do? First, do not automatically remove the point. Investigate it closely [58]. Check the original data source for potential data entry errors. If the data is correct, examine the case's clinical or methodological characteristics. Is it a fundamentally different population or intervention? Understand why it is influential. The decision to exclude, transform, or keep the point should be based on scientific judgment and documented transparently in your research.
5. My Residuals vs. Fitted plot shows a clear curve. What does this mean? A distinct pattern, such as a U-shape or curve, in the Residuals vs. Fitted plot suggests non-linearity [58] [59]. This indicates that your model may be misspecified and is failing to capture a non-linear relationship between the predictors and the outcome variable. This unaccounted-for structure can be a source of heterogeneity.
6. How can I make my diagnostic plots more accessible to readers with color vision deficiencies? Adhere to Web Content Accessibility Guidelines (WCAG). Ensure all graphics elements achieve a minimum 3:1 contrast ratio with neighboring elements [60]. Crucially, do not rely on color alone to convey meaning [61] [60]. Use a combination of visual encodings such as point shapes, patterns, or direct text labels to differentiate elements. Using a dark theme for charts can also provide a wider array of color shades that meet contrast requirements [60].
Troubleshooting Guides
Problem 1: Heteroscedasticity (Non-Constant Variance)
Observed Pattern: On the Scale-Location plot, the spread of residuals (or the square root of the absolute standardized residuals) widens or narrows systematically along the x-axis (fitted values). The red smooth line is not horizontal [58] [57].
Interpretation: The variability of the treatment effects is not consistent across the range of predicted values. This violates a key assumption of the model and can impact the precision of estimates.
Potential Solutions:
- Model Transformation: Apply a variance-stabilizing transformation to your outcome variable (e.g., log transformation).
- Robust Variance Estimation: Use statistical methods that are robust to heteroscedasticity, which adjust the standard errors to account for the unequal variance.
- Meta-Regression: Explore whether a known covariate (e.g., trial duration, baseline risk) can explain the changing variance. Including this covariate in a meta-regression model may resolve the heterogeneity.
Problem 2: Non-Linearity
Observed Pattern: On the Residuals vs. Fitted plot, the residuals show a clear systematic pattern, such as a curved band or a parabola, instead of being randomly scattered around zero [58] [59].
Interpretation: The linear model form is incorrect. There is a non-linear relationship that your model has not captured.
Potential Solutions:
- Polynomial Terms: Introduce quadratic or higher-order terms for the predictor variable to capture the curve.
- Non-Linear Models: Consider using a generalized additive model (GAM) or other non-linear modeling techniques.
- Spline Terms: Use regression splines to flexibly model the non-linear relationship.
Problem 3: Non-Normal Residuals
Observed Pattern: On the Normal Q-Q plot, the points deviate significantly from the straight dashed line, particularly at the tails [58] [57] [59].
Interpretation: The residuals are not normally distributed. This can affect the validity of p-values and confidence intervals.
Potential Solutions:
- Data Transformation: Transform the outcome variable (e.g., log, square-root) to make the residuals more normal.
- Robust Methods: Use bootstrapping techniques to derive confidence intervals that do not rely on the normality assumption.
- Investigate Outliers: Check if the non-normality is driven by a few extreme outliers and investigate their cause.
Problem 4: Influential Observations
Observed Pattern: On the Residuals vs. Leverage plot, one or more points fall outside of the Cook's distance contour lines (the red dashed lines) [58] [57].
Interpretation: Specific studies or data points have a disproportionate influence on the model's results. The regression results could change significantly if these points are removed.
Potential Solutions:
- Sensitivity Analysis: Run the model both with and without the influential cases. Report the results of both analyses to demonstrate the robustness (or lack thereof) of your findings.
- Examine the Cases: Scrutinize the influential studies for methodological quirks, differences in population, or risk of bias that might justify a separate analysis or interpretation.
Diagnostic Plots at a Glance
The table below summarizes the four primary diagnostic plots, their purpose, and how to interpret their patterns.
| Plot Name | Primary Purpose | What a "Good" Plot Looks Like | Problem Pattern & Interpretation |
|---|---|---|---|
| Residuals vs. Fitted [58] [57] | Check the linearity assumption and identify non-linear patterns. | Random scatter of points around the horizontal line at zero, with no discernible pattern. | Curvilinear pattern (e.g., U-shaped): Suggests a non-linear relationship not captured by the model [58]. |
| Normal Q-Q [58] [57] [59] | Assess if residuals are normally distributed. | Points fall approximately along the straight dashed reference line. | Points deviate from the line, especially at the tails: Indicates departures from normality, which can affect inference [57]. |
| Scale-Location [58] [57] | Evaluate homoscedasticity (constant variance of residuals). | Horizontal line with randomly (equally) spread points. The red smooth line is flat. | Funnel or cone shape: Indicates heteroscedasticity; the spread of residuals changes with fitted values [58]. |
| Residuals vs. Leverage [58] [57] | Identify influential cases/studies that disproportionately affect the results. | All points are well within the Cook's distance lines (red dashed lines). No points in the upper or lower right corners. | Points outside the Cook's distance lines: Flags highly influential observations that may alter results if removed [58]. |
Experimental Protocol: Generating and Interpreting Diagnostic Plots
This protocol details the methodology for creating and analyzing diagnostic plots using the statistical environment R, a standard tool for meta-analysis.
1. Software and Packages
- R Statistical Software: The core computational environment.
ggplot2: A powerful package for creating sophisticated and customizable graphics [57].gridExtra: A helper package for arranging multiple plots in a single figure [57].
2. Code Workflow The following diagram illustrates the procedural workflow for model diagnostics:
Step-by-Step Procedure:
- Load Data and Libraries: Install and load the required R packages. Load your dataset (e.g., a data frame containing trial-level effect sizes and covariates).
- Specify and Fit Model: Fit your linear (meta-regression) model using the
lm()function. For example, a model predicting effect size (effect_size) based on a moderator variable (moderator). - Generate Diagnostic Plots: Use the following function to create the four core diagnostic plots simultaneously [57].
- Interpretation and Iteration: Systematically examine each plot for the problem patterns described in the Troubleshooting Guides and summarized in the table above. Use these insights to refine your model, for example, by adding a quadratic term for non-linearity or using a robust variance estimator.
The Scientist's Toolkit: Essential Research Reagents & Software
The following table details key "reagents" – the software, packages, and functions – essential for conducting diagnostic analyses in NMA.
| Tool Name | Type | Primary Function | Example/Usage |
|---|---|---|---|
| R Statistical Software [57] | Software Environment | Provides the core platform for statistical computing, modeling, and graphics. | The foundational environment in which all analyses are run. |
ggplot2 package [57] |
R Package | Creates flexible, layered, and publication-quality visualizations. | ggplot(model_data, aes(x, y)) + geom_point() |
gridExtra package [57] |
R Package | Arranges multiple ggplot2 graphs into a single composite figure. |
grid.arrange(plot1, plot2, plot3, plot4, ncol=2) |
lm() function [57] |
R Function | Fits linear models, including meta-regression models, using ordinary least squares. | my_model <- lm(y ~ x1 + x2, data = dataset) |
Base R plot() [58] |
R Function | Generates the four standard diagnostic plots for an lm object with a single command. |
plot(my_lm_model) |
| Cook's Distance [58] [57] | Statistical Metric | Quantifies the influence of each data point on the regression model. Identified in the Residuals vs. Leverage plot. | Points with high Cook's D are potential influential outliers. |
Ensuring Robust Conclusions: Validation Frameworks and Decision-Making Under Uncertainty
Frequently Asked Questions (FAQs)
1. What is the core principle behind rating the certainty of evidence in an NMA using GRADE? The core principle is that the certainty of evidence must be rated separately for each pairwise comparison within the network (e.g., for intervention A vs. B, A vs. C, and B vs. C). This rating is based on a structured assessment of both the direct evidence (from head-to-head trials) and the indirect evidence (estimated through a common comparator), ultimately leading to an overall certainty rating for the network estimate for each comparison [62] [8].
2. What are "transitivity" and "incoherence," and why are they critical for a valid NMA?
- Transitivity is the methodological assumption that the different sets of studies included in the network are sufficiently similar, on average, in all important factors that could modify the treatment effect (effect modifiers), such as patient population, outcome definitions, or standard care. It is the foundation for believing that an indirect comparison is valid [15] [8].
- Incoherence (also called inconsistency) is the statistical manifestation of a breach in transitivity. It occurs when the direct estimate of an intervention effect disagrees with the indirect estimate of that same effect [15] [8]. The presence of significant incoherence can lower the confidence in the network estimates.
3. Should I always combine direct and indirect evidence to rate the network estimate? Not necessarily. If there is important incoherence between the direct and indirect evidence, it is recommended to present the higher-certainty estimate rather than the combined network estimate. If both have the same certainty, you can use the network estimate but should downgrade the certainty of evidence by one level due to the incoherence [15] [62].
4. How should I approach rating the certainty of evidence for complex networks with many interventions? Begin by evaluating the confidence in each direct comparison that makes up the network. These domain-specific assessments (e.g., for risk of bias, inconsistency, imprecision) are then combined to determine the overall confidence in the evidence from the entire network [8]. For rapid reviews, a pragmatic approach is to focus on rating the certainty of the direct evidence and then check for incoherence with the indirect evidence, downgrading if needed [63].
5. Is it necessary to formally rate the indirect evidence in every case? No. Recent advances in the GRADE for NMA guidance state that if the certainty of the direct evidence is high and its contribution to the network estimate is at least as great as the indirect evidence, there is no need to formally rate the indirect evidence [62]. This makes the rating process more efficient.
6. What is a common pitfall in interpreting treatment rankings from an NMA? A major pitfall is relying solely on ranking metrics like the Surface Under the Cumulative Ranking Curve (SUCRA) without considering the certainty of the evidence. SUCRA values rank treatments from "best" to "worst" but do not account for the precision of the effect estimates or the underlying study quality. An intervention supported by small, low-quality trials that report large effects can be ranked highly, which can be misleading. It is crucial to interpret rankings in the context of the GRADE certainty ratings [15].
Troubleshooting Common Issues
| Issue | Possible Cause | Diagnostic Check | Solution |
|---|---|---|---|
| High Incoherence | Violation of transitivity assumption (studies in different comparisons have different effect modifiers). | Evaluate similarity of studies across comparisons for key population or design characteristics. | Present the direct or indirect estimate with the higher certainty of evidence instead of the network estimate [15]. |
| Consistently Low/Very Low Certainty Ratings | High risk of bias in included trials, imprecise effect estimates, or large heterogeneity/incoherence. | Check the risk of bias assessments and width of confidence intervals for major comparisons. | Acknowledge the limitation and state that the evidence does not permit a confident conclusion. Sensitivity analyses excluding high-bias studies may be informative [15]. |
| Indirect Evidence Dominates a Comparison | Lack of head-to-head (direct) trials for a specific comparison of interest. | Review the network geometry to identify which connections are informed by direct evidence. | The certainty of the indirect comparison cannot be higher than the lowest certainty rating of the two direct comparisons used to create it [8]. |
| Uninterpretable Treatment Rankings | Over-reliance on SUCRA values without consideration of certainty or precision. | Compare the ranking order against the league table of effect estimates and their certainty. | Use a minimally or partially contextualized ranking approach that considers the magnitude of effect and the certainty of evidence, rather than SUCRA alone [15]. |
Methodological Protocols for Applying GRADE to NMA
Table 1: Domains for Assessing Certainty of Evidence in NMA
| Domain | Assessment in Pairwise Meta-Analysis | Additional Consideration in NMA |
|---|---|---|
| Risk of Bias | Assess limitations in design/execution of individual studies. | Same process, applied to all studies contributing to the network [15]. |
| Inconsistency | Unexplained variability in results across studies (heterogeneity). | Assess heterogeneity within each direct comparison. Also consider incoherence (see below) [15] [8]. |
| Indirectness | Relevance of evidence to the PICO question. | Assess applicability of the entire network. Also, indirect comparisons are inherently less direct than head-to-head trials [63]. |
| Imprecision | Whether evidence is sufficient to support a conclusion, based on sample size and confidence intervals. | Assess for each network estimate. In rapid reviews, imprecision may not need to be considered when rating the direct and indirect estimates separately [62] [63]. |
| Publication Bias | Potential for unpublished studies to change conclusion. | Evaluate using funnel plots for comparisons with sufficient studies, though challenging for the whole network [15]. |
| Incoherence | Not applicable in standard pairwise meta-analysis. | Formally test for disagreement between direct and indirect evidence for a specific comparison. Downgrade if present [15] [62]. |
Table 2: A Pragmatic Workflow for Applying GRADE in NMA
This protocol is adapted from general GRADE guidance and rapid review methodologies [62] [63].
| Step | Procedure | Key Considerations |
|---|---|---|
| 1. Define the Framework | Select critical outcomes (prioritized by knowledge users) and all competing interventions. | Limit the number of outcomes to critical benefits and harms to manage workload [63]. |
| 2. Assess Direct Evidence | For every direct comparison, perform a standard GRADE assessment (rate risk of bias, inconsistency, etc.). | Start with high certainty for RCTs. This forms the foundation for the network rating [8]. |
| 3. Assess Indirect Evidence | For the indirect estimate of a comparison, its certainty is limited by the lowest certainty of the two direct estimates used to create it. | In some cases (e.g., high-certainty direct evidence dominates), formal rating of indirect evidence may be skipped [62]. |
| 4. Rate NMA Estimate | For each pairwise comparison, judge the certainty of the network (combined) estimate. | Consider the contribution of direct and indirect evidence and the presence of any incoherence [62]. |
| 5. Present Findings | Use Summary of Findings tables with explanatory footnotes for each critical outcome. | Clearly state the final certainty rating (High, Moderate, Low, Very Low) for each comparison [63]. |
Visual Workflow: Applying GRADE to a Network Meta-Analysis
The diagram below illustrates the logical process for assessing the certainty of evidence for a single pairwise comparison within a network meta-analysis.
The Scientist's Toolkit: Essential Reagents for NMA & GRADE
| Item / Resource | Function in NMA/GRADE | Explanation |
|---|---|---|
| GRADEpro GDT (Software) | To create and manage 'Summary of Findings' tables and evidence profiles. | This open-access software helps standardize the application of GRADE, improves efficiency, and ensures transparent reporting of the reasons for upgrading or downgrading evidence [63]. |
| Network Diagram | To visualize the evidence base for each outcome. | This graph with nodes (interventions) and lines (direct comparisons) is essential for understanding the connectedness of the network and identifying potential intransitivity [8]. |
| CINeMA (Software) | To assess Confidence in Network Meta-Analysis. | A web-based tool that implements the GRADE approach for NMA, facilitating the evaluation of multiple domains (imprecision, heterogeneity, etc.) across all comparisons. |
| League Table | To present the relative effects between all pairs of interventions in the network. | A matrix that displays the effect estimates and confidence intervals for all comparisons, which is crucial for contextualizing treatment rankings [15]. |
| ROBIS Tool | To assess the risk of bias in systematic reviews. | A tool to evaluate the methodological quality of the systematic review process that underpins the NMA, which is a foundational step before applying GRADE [15]. |
Frequently Asked Questions
Q1: What is the core problem with traditional, risk-neutral decision-making in Network Meta-Analysis? A risk-neutral decision-maker, following statistical decision theory, recommends the single treatment with the highest Expected Value (EV), ignoring any uncertainty in the evidence [64]. In practice, decision-makers often recommend multiple treatments and are influenced by the degree of uncertainty, suggesting a risk-averse stance. Traditional methods like ranking by probability of being best (Pr(Best)) or SUCRA can have the perverse effect of privileging treatments with more uncertain effects [64].
Q2: How does Loss-Adjusted Expected Value (LaEV) incorporate risk-aversion? LaEV is a metric derived from Bayesian statistical decision theory. It adjusts the standard Expected Value by subtracting the expected loss arising from making a decision under uncertainty [64]. This provides a penalty for uncertainty, making it suitable for risk-averse decision-makers. It is conservative, simple to implement, and has an independent theoretical foundation [64] [65].
Q3: In a two-stage decision process, what are the criteria for recommending a treatment? A robust, two-stage process can be used to recommend a clinically appropriate number of treatments [64]:
- Stage 1: Identify all treatments that are superior to a standard reference treatment.
- Stage 2: From the superior treatments, select all those that are also within a Minimal Clinically Important Difference (MCID) of the best treatment [64].
Q4: How does LaEV compare to GRADE in real-world applications? In an analysis of 10 NMAs used in NICE guidelines, LaEV and EV were compared to GRADE [64] [65]:
- An EV decision-maker would recommend 4–14 treatments per NMA.
- LaEV was more conservative, recommending 0–3 (median 2) fewer treatments.
- GRADE rules gave rise to anomalies and, in 3 out of 10 cases, failed to recommend the treatment with the highest EV and LaEV.
- Among treatments superior to the reference, GRADE was found to privilege the more uncertain ones [64] [65].
Experimental Protocols
Protocol 1: Implementing a Two-Stage Decision Framework with LaEV
Objective: To rank and recommend multiple treatments from a Network Meta-Analysis using a risk-averse, two-stage framework.
Materials: Output from a Bayesian or frequentist NMA, including posterior distributions (or point estimates and standard errors) for all relative treatment effects versus a reference.
Methodology:
- Calculate Expected Values: For each treatment, compute the expected value of the relative treatment effect versus the reference,
E[δ_i][64]. - Calculate Loss-Adjusted Expected Values (LaEV): For each treatment, compute the LaEV. This involves subtracting a loss function from the EV. The specific loss function depends on the chosen evaluative function (e.g., treatment efficacy, Net Benefit) [64].
- Stage 1 - Superiority Filter: Define a reference treatment (often a placebo or standard of care). Identify all treatments where the EV or LaEV indicates a clinically meaningful superiority over the reference.
- Stage 2 - MCID Filter: Identify the best treatment (the one with the highest EV or LaEV). Then, from the treatments that passed Stage 1, select all those whose EV or LaEV is within a pre-specified Minimal Clinically Important Difference (MCID) of the best treatment [64].
- Ranking: Rank the treatments that pass both stages according to their LaEV values. A valid ranking under uncertainty requires that a higher EV is ranked above a lower one at the same uncertainty, and a lower uncertainty is ranked above a higher one at the same EV [64].
Interpretation: The final list of treatments from Stage 2 are the recommended options. The LaEV ranking provides a risk-averse hierarchy among them.
Protocol 2: Comparing LaEV against Traditional Ranking Metrics
Objective: To evaluate the performance of LaEV against probability-based metrics (Pr(Best), SUCRA) and the GRADE minimally contextualised framework.
Materials: Output from multiple NMAs (e.g., the 10 NMAs from NICE guidelines used in the referenced study) [64] [65].
Methodology:
- Compute Metrics: For each NMA, calculate the following metrics for all treatments:
- Expected Value (EV)
- Loss-Adjusted EV (LaEV)
- Probability of being the best (Pr(Best))
- SUCRA or P-Score
- Probability the value exceeds a threshold (Pr(V > T)) for GRADE Stage 1 [64].
- Apply Decision Rules:
- For EV/LaEV, apply the two-stage process from Protocol 1.
- For GRADE, apply its multi-stage scheme: in Stage 1, select treatments where Pr(V > T) exceeds a probability criterion (e.g., 0.975). In subsequent stages, identify a subset of these treatments where none are better than any other on the same criterion [64].
- For Pr(Best) and SUCRA, note the top-ranked treatments but observe that these metrics do not define how many should be recommended.
- Compare Outcomes: Record the number of treatments recommended by each method and note any anomalies, such as a top-ranked treatment by probability metrics having low EV/LaEV or high uncertainty.
Interpretation: Analyze the results for consistency and validity. The referenced study found that only LaEV reliably delivered valid rankings under uncertainty and avoided privileging treatments with more uncertain effects [64].
Data Presentation
Table 1: Comparison of Decision Metrics from 10 Network Meta-Analyses
The following table summarizes a comparative evaluation of different decision metrics as applied in 10 real-world NMAs [64] [65].
| Decision Metric | Theoretical Foundation | Incorporates Uncertainty? | Number of Treatments Recommended (Range across 10 NMAs) | Key Limitations |
|---|---|---|---|---|
| Expected Value (EV) | Statistical Decision Theory [64] | No (Risk-Neutral) | 4 - 14 [65] | Ignores uncertainty; recommends a single best treatment by default. |
| Loss-Adjusted EV (LaEV) | Bayesian Decision Theory [64] | Yes (Risk-Averse) | 2 - 11 (0-3 fewer than EV) [64] [65] | Requires definition of a loss function. |
| Probability of Being Best (Pr(Best)) | Frequentist/Probability | Yes | Not defined by metric alone [64] | Can privilege treatments with more uncertain effects [64]. |
| SUCRA / P-Score | Frequentist/Probability | Yes | Not defined by metric alone [64] | Can privilege treatments with more uncertain effects; ranking is relative to a simulated "best" and "worst" [64]. |
| GRADE Framework | Expert Consensus | Yes (via probability thresholds) | Varies based on arbitrary cut-offs [64] | Can lead to anomalies; in 3/10 cases failed to recommend the highest EV/LaEV treatment [64] [65]. |
Table 2: The Scientist's Toolkit - Essential Reagents for NMA and Risk-Averse Decision Analysis
| Item | Function / Explanation |
|---|---|
| Network Meta-Analysis Software | Software like R (with gemtc, netmeta packages), WinBUGS/OpenBUGS, or JAGS is essential for performing the complex statistical calculations to synthesize direct and indirect evidence and obtain posterior distributions of treatment effects [64] [66]. |
| Reference Treatment | A common comparator (e.g., placebo or standard of care) used to anchor the network of treatment comparisons. It is the foundation for calculating all relative effects and for the first stage of the decision process (superiority filter) [64] [66]. |
| Evaluative Function | The outcome measure used to judge treatments. This could be a measure of efficacy (e.g., log-odds for a clinical event), Net Benefit (monetized health gain minus costs), or a function from Multi-Criteria Decision Analysis [64]. |
| Minimal Clinically Important Difference (MCID) | A pre-specified threshold for the smallest difference in the evaluative function that patients and clinicians would consider important. It is used in the second stage of the decision process to select treatments close to the best [64]. |
| Loss Function | A function that quantifies the "cost" of uncertainty for a risk-averse decision-maker. It is subtracted from the Expected Value to calculate the Loss-Adjusted Expected Value (LaEV) [64]. |
Workflow Visualization
Decision Workflow for Risk-Averse NMA
This diagram illustrates the logical flow of the two-stage decision process for recommending treatments based on Network Meta-Analysis, incorporating the Loss-Adjusted Expected Value.
NMA Connectivity and Treatment Effects
This diagram conceptualizes how Network Meta-Analysis connects different treatments to estimate relative effects, even in the absence of direct head-to-head trials.
Frequently Asked Questions
1. What is the core difference between the Probability of Being Best (Pbest), SUCRA, and P-scores? These metrics summarize treatment ranking distributions differently. Pbest is the probability a treatment is the most effective, but it ignores the entire ranking distribution and can be misleading for imprecisely estimated treatments [67]. SUCRA (Surface Under the Cumulative Ranking Curve) is a Bayesian metric representing the relative probability a treatment is better than other competing treatments, summarized across all possible ranks [67] [68]. The P-score is the frequentist analogue to SUCRA, measuring the mean extent of certainty that a treatment is better than its competitors, and their numerical values are nearly identical [68].
2. My treatment has a high Pbest but a low SUCRA/P-score. What does this mean? This typically occurs for a treatment with high uncertainty in its effect estimate. A treatment studied in only a few small trials might have an equal probability of assuming any rank (e.g., 25% for each rank in a network of four treatments), resulting in a moderately high Pbest of 25% but a flat ranking distribution. The SUCRA or P-score, which considers the entire distribution, would be low (e.g., 50%), correctly reflecting the high uncertainty and poor average rank [67].
3. When should I use P-scores over SUCRA values? The choice is primarily determined by your statistical framework. Use P-scores if you are conducting a frequentist network meta-analysis, as they are derived analytically from point estimates and standard errors without resampling [68]. Use SUCRA values if you are performing a Bayesian analysis, as they are computed from the posterior distribution of rank probabilities [68].
4. The confidence intervals for two treatments overlap, but one has a much higher P-score. Is this ranking reliable? Not necessarily. Ranking metrics like P-scores and SUCRA mostly follow the order of point estimates. A much higher P-score usually results from a more favorable point estimate. However, if the confidence intervals overlap substantially, the clinical importance of the difference may be small, and the ranking should be interpreted with great caution. Confidence intervals provide a more complete picture of the uncertainty in the relative effects [68].
5. How can I rank treatments for multiple outcomes simultaneously, like both efficacy and safety? Ranking for multiple outcomes requires a benefit-risk assessment. Simple graphical approaches include:
- Creating a scatterplot of SUCRA/P-scores for one outcome against another [67].
- Using a rank-heat plot to visualize rankings across several outcomes [67]. For a more formal analysis, you can use methods that incorporate a minimal clinically important difference (CIV). This allows the creation of a hierarchy based on whether a treatment is better than its competitors by a specific, clinically relevant amount for each outcome [67].
Troubleshooting Guides
Problem: My ranking metrics seem to exaggerate small, clinically unimportant differences between treatments.
- Solution: Incorporate the Minimal Clinically Important Difference (MCID) or Clinically Important Value (CIV) into your ranking assessment. Instead of asking, "Is Treatment A better than Treatment B?" you can calculate the probability that Treatment A is better than Treatment B by at least the CIV. This modifies the P-score to reflect the mean extent of certainty that a treatment is better than the others by a certain, meaningful amount [67].
Problem: I am getting different treatment hierarchies from different ranking metrics and don't know which one to report.
- Solution: This confusion often arises from not defining the "Treatment Hierarchy Question" first. Different metrics answer different questions. You must pre-define the question your ranking aims to address and then select the appropriate metric [69].
- Define Your Hierarchy Question: Before analysis, clearly state the criterion for preferring one treatment over others. For example:
- "Which treatment is most likely to be the best?" → Use the Probability of Being Best (Pbest).
- "Which treatment has the highest average performance across all possible ranks, considering uncertainty?" → Use SUCRA/P-score.
- "Which treatment is most likely to produce an outcome better than a specific threshold (e.g., mean survival >5 years)?" → This requires calculating the probability of the absolute effect exceeding the threshold [69].
The table below summarizes which ranking metric to use based on your defined question.
| Treatment Hierarchy Question | Recommended Ranking Metric |
|---|---|
| Which treatment is most likely to be the single best? | Probability of Being Best (Pbest) |
| What is the overall hierarchy, considering all possible ranks and uncertainty? | SUCRA (Bayesian) or P-score (Frequentist) |
| Which treatment is most likely to achieve a target outcome (e.g., >5% weight loss)? | Probability of exceeding the target (requires absolute effects) |
| Which treatment is most likely to be better than others by a clinically important margin? | Modified P-score/SUCRA conditional on the MCID [67] |
Problem: I need to implement P-scores in my frequentist NMA but don't have specialized software.
- Solution: P-scores can be calculated directly from the results of your frequentist NMA. The P-score for a treatment is the mean of the one-sided p-values from all pairwise comparisons where it is better than another treatment. The methodology is as follows [68]:
- From your NMA, obtain the point estimates and standard errors for all pairwise comparisons between treatments.
- For a beneficial outcome, for each treatment i, calculate the one-sided p-value for the test that treatment i is better than every other treatment j (i.e., ( p{i>j} = \Phi( (\hat{\mu}i - \hat{\mu}j) / \sigma{ij} ) ), where ( \Phi ) is the standard normal cumulative distribution function).
- The P-score for treatment i is the mean of these one-sided p-values: ( P\text{-score}i = \frac{1}{(I-1)} \sum{j, j\neq i} p_{i>j} ), where I is the total number of treatments.
The Scientist's Toolkit: Essential Research Reagents & Methods
The table below lists key methodological concepts and "tools" essential for understanding and implementing treatment ranking in network meta-analysis.
| Item | Function & Brief Explanation |
|---|---|
| Rankogram | A graphical tool that displays the full distribution of rank probabilities for each treatment, showing the probability that a treatment assumes each possible rank (1st, 2nd, etc.) [67]. |
| Treatment Hierarchy Question | A pre-specified question that defines the criterion for choosing one treatment over others. Using this is critical for selecting the correct ranking metric and avoiding misinterpretation [69]. |
| Minimal Clinically Important Difference (MCID) | The smallest difference in an outcome that patients would perceive as beneficial. Used to ensure rankings are based on clinically meaningful, not just statistically significant, differences [67]. |
| Frequentist NMA Framework | A statistical approach for NMA where treatment effects are considered fixed parameters. P-scores are the native ranking metric within this framework [68]. |
| Bayesian NMA Framework | A statistical approach where treatment effects are represented by probability distributions. SUCRA is the native ranking metric within this framework [68]. |
| Network Diagram | A graph of the evidence base, with nodes for treatments and lines for direct comparisons. It is the first step in assessing the validity of an NMA and any subsequent ranking [8]. |
| Transitivity/Coherence Assessment | The evaluation of the underlying assumption that the different studies in the network are sufficiently similar to allow for valid indirect comparisons and ranking. Violations can severely bias results [8]. |
Experimental Protocol & Workflow for Treatment Ranking
The following diagram maps the logical workflow and critical decision points for a robust ranking analysis in network meta-analysis.
Figure 1. Logical workflow for treatment ranking in NMA.
Detailed Methodology:
- Define the Research Question and Assemble the Network: Start with a clearly defined Population, Intervention, Comparator, and Outcome (PICO). Systematically search for and select randomized controlled trials (RCTs). Create a network diagram to visualize all treatments (nodes) and available direct comparisons (lines) [8].
- Assess Key Assumptions:
- Transitivity: Evaluate whether the studies comparing different interventions are sufficiently similar in their clinical and methodological characteristics (e.g., patient populations, outcome definitions) to be fairly combined. This is a clinical judgement [8].
- Coherence (Consistency): Statistically check for disagreement between direct evidence and indirect evidence for any treatment comparison in the network. Incoherence suggests a violation of the transitivity assumption [8].
- Perform the Network Meta-Analysis: Fit an NMA model (Bayesian or frequentist) to obtain the relative treatment effects for all pairwise comparisons in the network, along with their measures of uncertainty (credible or confidence intervals).
- Define the Treatment Hierarchy Question: Before calculating any metrics, explicitly state the question the ranking should answer. For example: "Which treatment is most likely to have the highest mean efficacy?" or "Which treatment has the best overall performance across all ranks?" [69]
- Select and Calculate Ranking Metrics:
- Based on your hierarchy question and statistical framework, calculate the appropriate metrics (Pbest, SUCRA, or P-scores).
- If using a frequentist framework, compute P-scores directly from the NMA output as described in the troubleshooting guide [68].
- If using a Bayesian framework, use Markov Chain Monte Carlo (MCMC) simulation to obtain the posterior distribution of ranks and calculate SUCRA and Pbest from this distribution [67] [68].
- Report and Interpret Results:
- Present the ranking metrics alongside the relative treatment effects and their confidence/credible intervals. The relative effects are the primary output; rankings are a secondary summary [69] [68].
- Use graphical aids like rankograms to show the full ranking distribution and avoid over-interpreting small differences in SUCRA/P-scores [67].
- Always discuss whether the observed differences between treatments are clinically important.
Prediction Intervals and Their Role in Clinical Decision-Making
Frequently Asked Questions (FAQs)
Q1: What is a prediction interval, and how does it differ from a confidence interval or a point estimate? A prediction interval (PI) is a range of values that is likely to contain the future value of an observation, given a specified level of confidence (e.g., 95%) [70]. Unlike a confidence interval, which quantifies the uncertainty around a population parameter (like a mean), a prediction interval quantifies the uncertainty for a specific, individual prediction. A point estimate provides a single "best guess" value, but a prediction interval provides a probabilistic range, offering a more complete picture of the forecast uncertainty [71] [70].
Q2: Why are prediction intervals critical for clinical decision-making based on models like polygenic scores (PGS) or vital sign forecasting? In clinical settings, decision-makers need to understand not just a predicted outcome, but also the reliability of that prediction. A point estimate from a model may indicate a high risk for a patient, but if the associated prediction interval is very wide, the confidence in that risk classification is low. Well-calibrated PIs directly address this by quantifying the uncertainty, helping clinicians distinguish between a meaningful warning and mere model noise. This is essential for reliable genetic risk assessment and interpreting forecasts of critical indicators like heart rate and blood pressure [71] [70].
Q3: What does it mean for a prediction interval to be "well-calibrated"? A well-calibrated prediction interval means that the stated confidence level matches the observed frequency in real-world data. For example, for a 95% prediction interval, approximately 95 out of 100 future observations should fall within the provided range. Mis-calibrated intervals, which are too optimistic or pessimistic, can lead to over- or under-confidence in clinical predictions, potentially resulting in poor decision-making [70].
Q4: How can heterogeneity in a Network Meta-Analysis (NMA) impact the construction of prediction intervals? Heterogeneity—the variability in effects across different studies—is a core consideration in NMA. A random-effects model is often preferred as it accounts for this variability, assuming that the true effect size may differ from study to study [72]. When making predictions for a new study or context, this between-study heterogeneity must be incorporated into the uncertainty. Prediction intervals in this context are designed to account for this heterogeneity, providing a range within which the effect of a new, similar study would be expected to fall. This is crucial for public health decision-making where interventions are complex and implemented across diverse settings [38] [72].
Q5: My model's point predictions are accurate, but the prediction intervals are too narrow and mis-calibrated. What could be the cause? Narrow and mis-calibrated PIs often indicate that the model is overconfident and is underestimating the true sources of variability. This can happen if the model fails to account for all sources of heterogeneity or uncertainty in the data. Solutions include using methods specifically designed for robust uncertainty quantification (like PredInterval or RUE-based methods) [71] [70], ensuring your model accounts for between-study heterogeneity (e.g., using a random-effects model and reporting Ï„) [72], and performing sensitivity analyses to test the robustness of your intervals.
Troubleshooting Guides
Issue 1: Mis-calibrated Prediction Intervals
Problem: The constructed 95% prediction intervals only contain the true observed value 80% of the time.
Solution Steps:
- Diagnosis: Confirm the miscalibration by calculating the Prediction Interval Coverage Probability (PICP) on a held-out test dataset [73].
- Method Selection: Consider switching to a non-parametric method for constructing PIs, which does not rely on strict distributional assumptions. The PredInterval method, for instance, uses quantiles of phenotypic residuals from cross-validation to achieve well-calibrated coverage across diverse genetic architectures [70].
- Implementation: For vital sign forecasting, explore methods based on Reconstruction Uncertainty Estimate (RUE), which are sensitive to data shifts. A non-parametric k-nearest neighbours (KNN) approach can empirically estimate the conditional error distribution for high-frequency data [71].
- Validation: Recalculate the PICP after implementing the new method. The goal is for the PICP to be very close to the nominal confidence level (e.g., 95%) [70].
Issue 2: Accounting for Heterogeneity in Network Meta-Analysis Predictions
Problem: You need to construct a prediction interval for the treatment effect in a new clinical setting, but the NMA shows significant between-study heterogeneity.
Solution Steps:
- Model Selection: Ensure your NMA uses a random-effects model. This model explicitly estimates the between-study variance (τ²), which is essential for creating accurate prediction intervals [72].
- Quantity the Heterogeneity: Extract the estimate of Ï„ (the standard deviation of the true effects). This parameter directly influences the width of the prediction interval [72].
- Construct the Interval: A prediction interval for a new study in a random-effects meta-analysis is typically calculated as the pooled estimate ± a t-value (with k-2 degrees of freedom, where k is the number of studies) multiplied by the square root of (τ² + SE²), where SE is the standard error of the pooled estimate.
- Reporting: Report the prediction interval alongside the pooled estimate and I² statistic to give a complete picture of both the average effect and the range of expected effects in different settings [72].
Issue 3: Wide Prediction Intervals Reducing Clinical Usefulness
Problem: Your 95% prediction intervals are well-calibrated but so wide that they are not useful for making specific clinical decisions.
Solution Steps:
- Feature Engineering: Re-evaluate your input variables. Use multiple feature selection methods to identify and retain only the most significant factors influencing the outcome. This can reduce extraneous noise and lead to narrower intervals [73].
- Multi-objective Optimization: Employ a multi-objective optimization algorithm to refine the PIs. The goal is to simultaneously optimize for two objectives: achieving the desired coverage probability and minimizing the width of the prediction interval (e.g., Prediction Interval Normalized Average Width) [73].
- Model Integration: Combine quantile regression with deep learning models (e.g., Quantile Regression LSTM) to better capture the underlying data distribution and complex patterns, which can lead to more precise intervals [73].
Experimental Protocols & Data Presentation
Table 1: Comparison of Prediction Interval Performance in Polygenic Score Applications
This table summarizes the performance of the PredInterval method against two alternatives across 17 real-data traits, demonstrating its superior calibration [70].
| Method Name | Input Data Supported | Key Principle | Average Coverage Rate (Target 95%) | Compatibility |
|---|---|---|---|---|
| PredInterval (Non-parametric) | Individual-level or summary statistics | Uses quantiles of phenotypic residuals from cross-validation. | 96.0% (Quantitative), 96.7% (Binary) | Works with any PGS method. |
| BLUP Analytical Form | Individual-level | An approximate analytical form relying on independent SNP assumption. | 91.0% (Quantitative), 83.4% (Binary) | Restricted to specific PGS methods. |
| CalPred | Individual-level | Not specified in detail in the provided context. | 80.2% (Quantitative), 88.7% (Binary) | Compatible with various PGS methods. |
Table 2: Key Reagents and Computational Tools for Interval Prediction Research
A toolkit of essential methodological "reagents" for researchers developing or working with prediction intervals.
| Research Reagent | Type | Primary Function | Example Application |
|---|---|---|---|
| PredInterval | Statistical Software/Method | Constructs non-parametric, well-calibrated prediction intervals for phenotypic predictions. | Quantifying uncertainty in polygenic score applications for clinical risk assessment [70]. |
| RUE (Reconstruction Uncertainty Estimate) | Uncertainty Metric | Provides an uncertainty estimate sensitive to data shifts, enabling label-free calibration of PIs. | Forecasting vital signs (e.g., heart rate) with trustworthy prediction intervals [71]. |
| Random-Effects Model | Statistical Model | Accounts for between-study heterogeneity in meta-analysis, which is critical for constructing accurate prediction intervals. | Predicting the range of a treatment effect in a new clinical setting during network meta-analysis [72]. |
| QRLSTM (Quantile Regression LSTM) | Deep Learning Model | A hybrid model that combines quantile regression for uncertainty with LSTM networks to capture long-term dependencies in sequences. | Forecasting volatile time series data like commodity prices with robust uncertainty bounds [73]. |
| Multi-Objective Optimization Algorithms (e.g., MOSSA) | Optimization Algorithm | Simultaneously optimizes multiple, often competing, objectives of a prediction interval (e.g., coverage and width). | Refining the upper and lower bounds of a copper price prediction interval to be both reliable and narrow [73]. |
Protocol: Constructing Non-parametric Prediction Intervals with PredInterval
Objective: To create well-calibrated prediction intervals for phenotypes predicted from polygenic scores. Materials: Individual-level genetic/phenotypic data or summary statistics; any PGS method of choice (e.g., DBSLMM). Methodology: [70]
- PGS Training: Using a training dataset, construct the polygenic score (PGS) model using your chosen method.
- Cross-Validation: In a validation dataset, perform cross-validation to obtain predicted phenotypic values for each individual.
- Residual Calculation: For each individual in the validation set, calculate the residual: the absolute difference between the observed phenotypic value and the predicted value.
- Quantile Determination: From the distribution of these residuals in the validation set, find the quantile that corresponds to the desired confidence level (e.g., the 95th percentile for a 95% PI).
- Interval Construction: For a new individual's PGS-based prediction, the prediction interval is constructed as:
Predicted value ± the residual quantile from Step 4.
Workflow and Relationship Diagrams
Diagram 1: Workflow for clinical prediction intervals.
Diagram 2: Prediction intervals in network meta-analysis.
Validating NMA Findings Through Cross-Validation and External Validation Techniques
Frequently Asked Questions
What is the core purpose of validation in Network Meta-Analysis? Validation ensures that the comparative effectiveness rankings and estimates generated by an NMA are robust, reliable, and generalizable beyond the specific set of studies included in the analysis. It helps confirm that findings are not unduly influenced by specific study characteristics, biases, or network structure [21].
Why is assessing cross-study heterogeneity critical in NMA? Failure to assess and adjust for cross-study heterogeneity can significantly alter the clinical interpretations of NMA findings. Statistical models that adjust for covariates, such as baseline risk, provide a better model fit and more reliable results. Lack of such adjustment can lead to incorrect conclusions about the comparative efficacy of interventions [74].
What is the difference between internal and external validation? Internal validation uses data-splitting methods (like cross-validation) on the available dataset to evaluate model performance. External validation involves testing the NMA model or its predictions on completely new, independently collected datasets. This is considered stronger evidence for generalizability [75].
How can I validate an NMA when a single external dataset is unavailable? The concept of convergent validation can be applied. This involves using multiple external datasets from different sources. A model is considered robust if it consistently shows good predictive performance across these diverse datasets, strengthening confidence in its generalizability [75].
Troubleshooting Guides
Problem: Findings are Highly Sensitive to the Inclusion of a Single Study
Potential Cause: The network may be unstable or suffer from significant intransitivity due to cross-study differences.
Solutions:
- Assess and Adjust for Heterogeneity: Conduct analyses to identify and adjust for covariates responsible for cross-trial differences. Baseline risk (placebo response) is often a key covariate to consider [74].
- Evaluate Transitivity Assumption: Check that studies are sufficiently similar in their patient populations, interventions, and outcomes to be fairly connected in a network. Inconsistency between direct and indirect evidence can be a sign of violated assumptions [21].
- Use Sensitivity Analyses: Perform multiple NMAs, each time excluding a different study, to identify if any single study is exerting undue influence on the overall results.
Problem: NMA Model Performs Poorly on New, External Data
Potential Cause: The original NMA model may be overfitted to the idiosyncrasies of the initial dataset or may not account for all relevant effect modifiers present in the broader population.
Solutions:
- Leverage External Validation: Use independently derived datasets to test the performance of the model trained on your initial data. A model that performs well on external data is more likely to be domain-relevant and generalizable [75].
- Check for Data Consistency: Ensure that the definitions of interventions, populations, and outcomes are consistent between your original analysis and the external dataset. Inconsistent definitions can lead to poor performance.
- Use Partially Contextualized Methods: Consider using GRADE's minimally or partially contextualized methods for presenting NMA results, which categorize interventions based on the magnitude of effect and certainty of evidence, making them more interpretable and potentially more transferable [22].
Potential Cause: Incomplete or inconsistent reporting of trial design and results across different public data sources.
Solutions:
- Triangulate Data Sources: Do not rely on a single data source. Consult multiple sources, including journal articles, regulatory documents (e.g., Drugs@FDA), and trial registries (e.g., ClinicalTrials.gov), to get the most complete and accurate picture of a trial [76].
- Prioritize Data Sources: When information conflicts, establish a hierarchy of source reliability. For example, one might prioritize regulatory documents, then journal articles, and finally trial registrations, which sometimes provide the least information [76].
- Report Transparency: Document all data sources used and any discrepancies found. Transparent reporting allows readers to understand the potential for reporting bias.
Experimental Protocols for Key Validation Analyses
Protocol 1: Assessing and Adjusting for Cross-Study Heterogeneity
Objective: To evaluate the impact of cross-study differences (heterogeneity) on NMA estimates and adjust for them to improve model validity.
Methodology:
- Define Covariates: Identify potential clinical or methodological covariates that may explain differences between studies (e.g., baseline risk, prior biologic use, disease duration, age) [74].
- Fit Multiple Models: Conduct several Bayesian NMAs:
- An unadjusted model (no covariates).
- A series of models, each adjusting for a different covariate.
- A baseline risk-adjusted model, which can adjust for multiple observed and unobserved effect modifiers [74].
- Evaluate Model Fit: Use appropriate statistical measures (e.g., Deviance Information Criterion - DIC) to determine which model fits the data best. A lower DIC generally indicates a better fit [74].
- Compare Interpretations: Examine the clinical interpretations (e.g., treatment rankings, effect estimates) from the best-fitting model versus the unadjusted model to understand the impact of heterogeneity.
Protocol 2: External Validation Using an Independent Dataset
Objective: To test the generalizability of the NMA findings by applying them to a completely independent dataset.
Methodology:
- Lock the Model: Finalize the NMA model (including all preprocessing steps, chosen covariates, and statistical methods) based on the original "discovery" dataset. No modifications should be made after this point [77].
- Acquire External Data: Obtain a new dataset collected independently from the discovery data. Ensure the outcome definitions and interventions are comparable [75].
- Apply the Model: Use the locked model to generate predictions or estimates for the external validation dataset.
- Evaluate Performance: Compare the model's predictions against the observed outcomes in the validation set. Calculate performance metrics such as the mean squared error (MSE) for continuous outcomes or accuracy, sensitivity, and specificity for binary outcomes [75].
- Validate Across Subgroups: If subgroup information is available for the external data, assess the model's performance within these subgroups to identify any variation in generalizability [77].
Key Research Reagent Solutions
The following table details key methodological components essential for conducting and validating Network Meta-Analyses.
| Research Component | Function in NMA Validation |
|---|---|
| Bayesian Statistical Models | Provides a flexible framework for conducting NMA, allowing for the incorporation of prior knowledge and direct estimation of probabilities for treatment rankings [74]. |
| GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) | A systematic approach to rate the certainty of evidence for each pairwise comparison in the network, which is crucial for interpreting the validity of NMA findings [22]. |
| Public Regulatory Databases (e.g., Drugs@FDA) | Serve as valuable sources for trial summaries and data submitted for drug approval, useful for validating findings from published literature and checking for reporting biases [76]. |
| Trial Registries (e.g., ClinicalTrials.gov) | Provide information on both published and unpublished trials, helping to identify potential publication bias and to gather additional data for validation [76]. |
| Minimally/Partially Contextualized Methods | Presentation formats that categorize interventions from "best" to "worst" based on effect and certainty. These were developed and validated with clinicians to improve clarity and interpretability of complex NMA results [22]. |
Experimental Workflow Diagram
NMA Validation Workflow
NMA Validation Techniques Taxonomy
Conclusion
Effectively addressing heterogeneity in network meta-analysis requires a systematic approach spanning from proper assumption verification to advanced statistical modeling and careful interpretation. Foundational concepts of transitivity and consistency must guide network construction, while modern methodological tools like network meta-regression and class-effect models offer powerful ways to explain and account for variability. Troubleshooting requires vigilant inconsistency checking and appropriate model selection, and validation should incorporate both statistical metrics and decision-theoretic frameworks like loss-adjusted expected value for risk-averse recommendations. Future directions include improved AI-assisted tools, standardized reporting guidelines for heterogeneous networks, and greater integration of patient-centered outcomes in heterogeneity exploration. Ultimately, transparent acknowledgment and thorough investigation of heterogeneity strengthens the credibility of NMA findings and their utility in drug development and clinical guideline development.
References
- 1. and Subgroup Analysis Heterogeneity - in Network Meta Analysis [https://link.springer.com/chapter/10.1007/978-3-030-40105-4_18]
- 2. Interpreting Heterogeneity - in : A Unified Meta ... Analysis Framework [https://www.preprints.org/manuscript/202508.1527/v2]
- 3. NMA: Network meta-analysis based on multivariate ... [https://www.medrxiv.org/content/10.1101/2025.09.15.25335823v1.full-text]
- 4. Description of network meta-analysis geometry: A metrics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6382117/]
- 5. Low awareness of the transitivity assumption in complex ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-024-03322-1]
- 6. Exploring the Transitivity Assumption in Network Meta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11983674/]
- 7. Concepts and emerging issues of network meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8497908/]
- 8. Chapter 11: Undertaking network meta-analyses [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-11]
- 9. Heterogeneity in Meta-analysis (Q, I-square) [https://www.statsdirect.com/help/meta_analysis/heterogeneity.htm]
- 10. 7.1 Heterogeneity statistics | Doing Meta-Analysis in R and ... [https://cjvanlissa.github.io/Doing-Meta-Analysis-in-R/heterogeneity-statistics.html]
- 11. Evolution of Heterogeneity (I2) Estimates and Their 95% ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3405079/]
- 12. 5 Tips For Understanding Network Meta-Analysis [https://absolutelymaybe.plos.org/2024/02/01/5-tips-for-understanding-network-meta-analysis/]
- 13. The Kilim plot: A tool for visualizing network metaâ€analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7818463/]
- 14. Data visualisation approaches for component network meta ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-02026-z]
- 15. A clinician's guide to network meta-analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9307840/]
- 16. Heterogeneity in pragmatic randomised trials - BMC Medicine [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-022-02569-w]
- 17. New Approach Methodologies: What Clinical Pharmacologists ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404678/]
- 18. Network meta-regression including baseline risk analysis ... [https://www.sciencedirect.com/science/article/pii/S0895435625001726]
- 19. How to Perform a Meta-Regression [https://www.publichealth.columbia.edu/research/population-health-methods/meta-regression]
- 20. Understanding Network Metaâ€Analysis: A Practical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271649/]
- 21. Network meta-analysis: a powerful tool for clinicians ... [https://www.sciencedirect.com/science/article/pii/S0895435624002932]
- 22. Development and design validation of a novel network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9189833/]
- 23. How to choose colors for data visualizations [https://www.atlassian.com/data/charts/how-to-choose-colors-data-visualization]
- 24. Data visualisation approaches for component network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10502971/]
- 25. Analysing complex interventions using component network ... [https://www.medrxiv.org/content/10.1101/2025.06.30.25330567v1.full-text]
- 26. 7 Networks – ggplot2: Elegant Graphics for Data Analysis ... [https://ggplot2-book.org/networks.html]
- 27. Network Meta-Analysis with Class Effects: A Practical ... [https://pubmed.ncbi.nlm.nih.gov/41204833/]
- 28. Network Meta-Analysis with Class Effects: A Practical Guide and ... [https://read.qxmd.com/read/41204833/network-meta-analysis-with-class-effects-a-practical-guide-and-model-selection-algorithm]
- 29. Network Meta-analysis on Disconnected Evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9459361/]
- 30. Hierarchical network meta-analysis models for synthesis of ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-01925-5]
- 31. Network meta-analysis: a technique to gather evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5386629/]
- 32. and Sensitivity in a meta- subgroup – What we... analysis analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC11498262/]
- 33. Identifying inconsistency in network metaâ€analysis: Is the net ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6899484/]
- 34. 10 Evidence-based Steps for Robust Individual Participant Data... [https://www.numberanalytics.com/blog/10-evidence-based-steps-robust-individual-participant-data-meta-analysis]
- 35. Impact of a Patient's Baseline Risk on the Relative Benefit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9075204/]
- 36. Importance of the baseline risk in determining sample size ... [https://jeccm.amegroups.org/article/view/4550/5130]
- 37. Risk Analysis in Healthcare Organizations: Methodological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8275831/]
- 38. A methodological review of network meta-analyses applied ... [https://www.sciencedirect.com/science/article/pii/S0895435625001891]
- 39. Methods for Indirect Treatment Comparison: Results from a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11036291/]
- 40. The quantity, quality and findings of network meta-analyses ... [https://www.ncbi.nlm.nih.gov/books/NBK616834/]
- 41. A systematic review and meta-analysis of the efficacy and ... [https://www.nature.com/articles/s41591-025-03978-z]
- 42. Update to the PRISMA guidelines for network meta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11892999/]
- 43. Two new methods to fit models for network meta-analysis with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4964019/]
- 44. A brief note on the random-effects meta-analysis model ... [https://www.sciencedirect.com/science/article/pii/S0895435624002488]
- 45. Network meta-analysis with class effects: a practical guide ... [https://research-information.bris.ac.uk/en/publications/network-meta-analysis-with-class-effects-a-practical-guide-and-mo/]
- 46. Chapter 12 Network Meta-Analysis [https://bookdown.org/MathiasHarrer/Doing_Meta_Analysis_in_R/netwma.html]
- 47. Research Techniques Made Simple: Network Meta-Analysis [https://www.sciencedirect.com/science/article/pii/S0022202X18327933]
- 48. Chapter 10: Analysing data and undertaking meta-analyses [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-10]
- 49. A case study of water distribution systems [https://www.sciencedirect.com/science/article/abs/pii/S0951832021002684]
- 50. Network meta-analysis: development of a three-level ... [https://pubmed.ncbi.nlm.nih.gov/25595242/]
- 51. shinyBN: an online application for interactive Bayesian ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-019-3309-0]
- 52. Comparison of commonly used methods in random effects... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8647574/]
- 53. A graphical tool for locating inconsistency in network meta ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-13-35]
- 54. Frontiers | How to Conduct a Bayesian - Network Meta Analysis [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2020.00271/full]
- 55. Vitruvian plot: a visualisation tool for multiple outcomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9811072/]
- 56. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 57. Diagnostic Plots for Model Evaluation [https://www.geeksforgeeks.org/r-machine-learning/diagnostic-plots-for-model-evaluation/]
- 58. Understanding Diagnostic Plots for Linear Regression Analysis [http://library.virginia.edu/data/articles/diagnostic-plots]
- 59. Section 9 Diagnostic Plots | MATH3714 Linear Regression ... [https://seehuhn.github.io/MATH3714/S09-plots.html]
- 60. How Accessibility Standards Can Empower Better Chart ... [https://www.smashingmagazine.com/2024/02/accessibility-standards-empower-better-chart-visual-design/]
- 61. How to build accessible graph visualization tools [https://cambridge-intelligence.com/build-accessible-data-visualization-apps-with-keylines/]
- 62. Advances in the GRADE approach to rate the certainty in ... [https://pubmed.ncbi.nlm.nih.gov/29051107/]
- 63. Rapid reviews methods series: Guidance on assessing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10850678/]
- 64. Rules for risk-averse decision-makers [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527546/]
- 65. rules for risk-averse decision-makers [https://www.medrxiv.org/content/10.1101/2024.07.01.24309758v1]
- 66. Network meta-analysis explained - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6761999/]
- 67. Extensions of the probabilistic ranking metrics of competing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7078966/]
- 68. Ranking treatments in frequentist network meta-analysis ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-015-0060-8]
- 69. Introducing the Treatment Hierarchy Question in Network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9071581/]
- 70. Statistical construction of calibrated prediction intervals for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597821/]
- 71. [2509.01319] Towards Trustworthy Vital Sign Forecasting [https://arxiv.org/abs/2509.01319]
- 72. Model behavior: fixed ideas, random thoughts [https://www.epain.org/journal/view.html?uid=1915&vmd=Full]
- 73. A novel hybrid interval prediction framework integrating ... [https://www.nature.com/articles/s41598-025-20490-z]
- 74. Importance of assessing and adjusting for cross-study ... [https://pubmed.ncbi.nlm.nih.gov/30277080/]
- 75. Extensions of the External Validation for Checking Learned ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7691387/]
- 76. Rapid network meta-analysis using data from Food and Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6773505/]
- 77. Out of Sample Cross-Validation — NeuroMiner Manual [https://neurominer-git.github.io/NeuroMiner_1.2/4.8_mainmenu_OOCV_analysis.html]